Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Yoshikawa, A. and Fukuoka, J. Acute fibrinous and organizing pneumonia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumordiffusealveolardamageafop.html. Accessed April 26th, 2024.
Definition / general
- In 2002, Beasley et al. first described a progressive variant of lung injury with organizing pneumonia and intra-alveolar fibrin, which does not fit the histologic pattern of diffuse alveolar damage (DAD), organizing pneumonia (OP) or eosinophilic pneumonia (Arch Pathol Lab Med 2002;126:1064)
Essential features
- It is a newly proposed subacute interstitial pneumonia similar to organizing pneumonia or organizing diffuse alveolar damage
- Histologically, remarkable fibrin deposition (or "fibrin balls") along with plugs of organizing pneumonia in air spaces are characteristic
Terminology
- Also called acute fibrinous organizing pneumonia
Epidemiology
- Rare disease (no data on prevalence available so far)
- Mean age at onset is about 60 years old, with a wide age range (Arch Pathol Lab Med 2002;126:1064, J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701, Medicine (Baltimore) 2016;95:e4073)
- No gender predominance
- No association with smoking history
Sites
- Usually bilateral or sometimes unilateral lobes of the lung
Pathophysiology
- In the initial study, acute fibrinous and organizing pneumonia (AFOP) was described as a possible variant of diffuse alveolar damage because of its similar aggressive behavior and mortality rate (Arch Pathol Lab Med 2002;126:1064)
- However, recent studies and case reports have found that the clinical course and prognosis of AFOP is better and closer to that of organizing pneumonia (J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701)
- Nowadays, AFOP is considered a histological variant of organizing pneumonia or a different type of lung disease similar to organizing pneumonia, which sometimes follows an aggressive course
- Some idiopathic AFOP may be due to infection of undiagnosed bacteria
Etiology
- Variety of possible causes and associated conditions have been reported (Arch Pathol Lab Med 2002;126:1064, J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701, Medicine (Baltimore) 2016;95:e4073):
- Idiopathic
- Infection: H. influenzae, A. baumannii, P. jirovecii, C. pneumoniae
- Autoimmune disease: polymyositis / dermatomyositis, ankylosing spondylitis, antisynthetase syndrome
- Particle exposure: animal antigens, coal dust, wood dust, hairspray
- Neoplasm: cancer, lymphoma, leukemia, myelodysplastic syndrome
- Immunosuppression: diabetes mellitus, long term corticosteroid therapy
- Drugs
- Hematopoietic stem cell transplantation (J Investig Med High Impact Case Rep 2016;4:2324709616643990)
- Lung transplantation
Clinical features
- Most patients present with mild to moderate subacute respiratory failure (J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701)
- Fever, fatigue and malaise
- Cough
- Dyspnea
- Sputum or sometimes hemoptysis
- Duration of symptoms before diagnosis is 1 - 4 weeks
- Some patients may follow fulminant course, need mechanical ventilation and die of the disease, similar to diffuse alveolar damage (Arch Pathol Lab Med 2002;126:1064, Medicine (Baltimore) 2016;95:e4073)
- Abnormal chest auscultation
- End inspiratory fine crackles in affected lobes
- Mild to moderate restrictive or obstructive pattern in pulmonary function tests (Chin Med J (Engl) 2015;128:2701)
- Decreased total lung capacity (TLC)
- Decreased forced vital capacity (FVC)
- Decreased diffusing capacity of the lung for carbon monoxide (DLCO)
Diagnosis
- Based on clinical features, radiology and histology
- No unique clinical or radiological findings have been identified to date
- Open chest lung biopsy is recommended
- Transbronchial lung biopsy or computed tomography guided needle lung biopsy may be diagnostic if clinical and radiological features are suggestive enough
- Acute fibrinous and organizing pneumonia can be a background pattern with other disease present
- If the specimen is too small and the main lesion is not included, acute fibrinous and organizing pneumonia can be underdiagnosed (Int J Clin Exp Pathol 2014;7:4493)
Laboratory
- Increased C reactive protein
- Increased serum surfactant proteins A and D
- Increased serum ferritin may predict prognosis
- Occasional positive sputum bacterial culture
- Negative serum antibodies of connective tissue diseases and hypersensitivity pneumonitis
Radiology description
- Simple chest radiography
- Bilateral or unilateral ground glass opacity and consolidation
- High resolution computed tomography (Radiographics 2013;33:1951):
- Variable images, similar to organizing pneumonia
- Typically, patchy mixture of ground glass opacity and consolidation
- Size varies from a few centimeters to a whole lobe
- Rapidly progressive variant may show bilateral diffuse opacity, similar to diffuse alveolar damage
- Variable images, similar to organizing pneumonia
Radiology images
Prognostic factors
- Most cases achieve remission with treatment (J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701)
- Some patients die of rapidly progressive disease (Arch Pathol Lab Med 2002;126:1064, Medicine (Baltimore) 2016;95:e4073)
Case reports
- Idiopathic acute fibrinous and organizing pneumonia (AFOP):
- 42 year old woman with AFOP in whole lobes (Indian J Crit Care Med 2016;20:245)
- 45 year old man with flu-like symptoms (Ann Saudi Med 2013;33:301)
- 46 year old man with rapidly progressive respiratory failure (Curr Probl Diagn Radiol 2015;44:469)
- 68 year old woman with AFOP mimicking pneumonia (BMC Res Notes 2015;8:38)
- 22 year old man who presented with AFOP after lung transplantation and underwent retransplantation (Transplant Proc 2015;47:182)
- 39 year old woman with AFOP associated with undifferentiated connective tissue disease (Case Rep Rheumatol 2012;2012:549298)
- 48 year old woman with AFOP after lung transplantation and good response to corticosteroid pulse therapy (Transplant Proc 2015;47:836)
- 62 year old man with AFOP associated with myelodysplastic syndrome (Intern Med 2016;55:3155)
- 66 year old woman died of AFOP associated with influenza A / H1N1 after lung transplantation (BMC Pulm Med 2013;13:30)
- 68 year old man with AFOP induced by nivolumab (Intern Med 2017;56:2311)
- 78 year old man with AFOP associated with amiodarone (Am J Respir Crit Care Med 2015;191:104)
Treatment
- In general, corticosteroid pulse therapy with / without cyclophosphamide improves the symptoms and prognosis (Arch Pathol Lab Med 2002;126:1064, J Clin Pathol 2015;68:441, Chin Med J (Engl) 2015;128:2701)
- Treatment for underlying cause is also important for secondary acute fibrinous and organizing pneumonia
- Antibiotics are effective for acute fibrinous and organizing pneumonia induced by bacterial infection
- It is questionable if antibiotics can be a general therapeutic choice or not
- Mechanical ventilation may be necessary for aggressive type
Gross description
- Multiple patchy consolidated lesions
- Ill defined, soft to firm gray areas
- Mild increase in weight
- Alveoli are filled with reddish fibrinous exudates
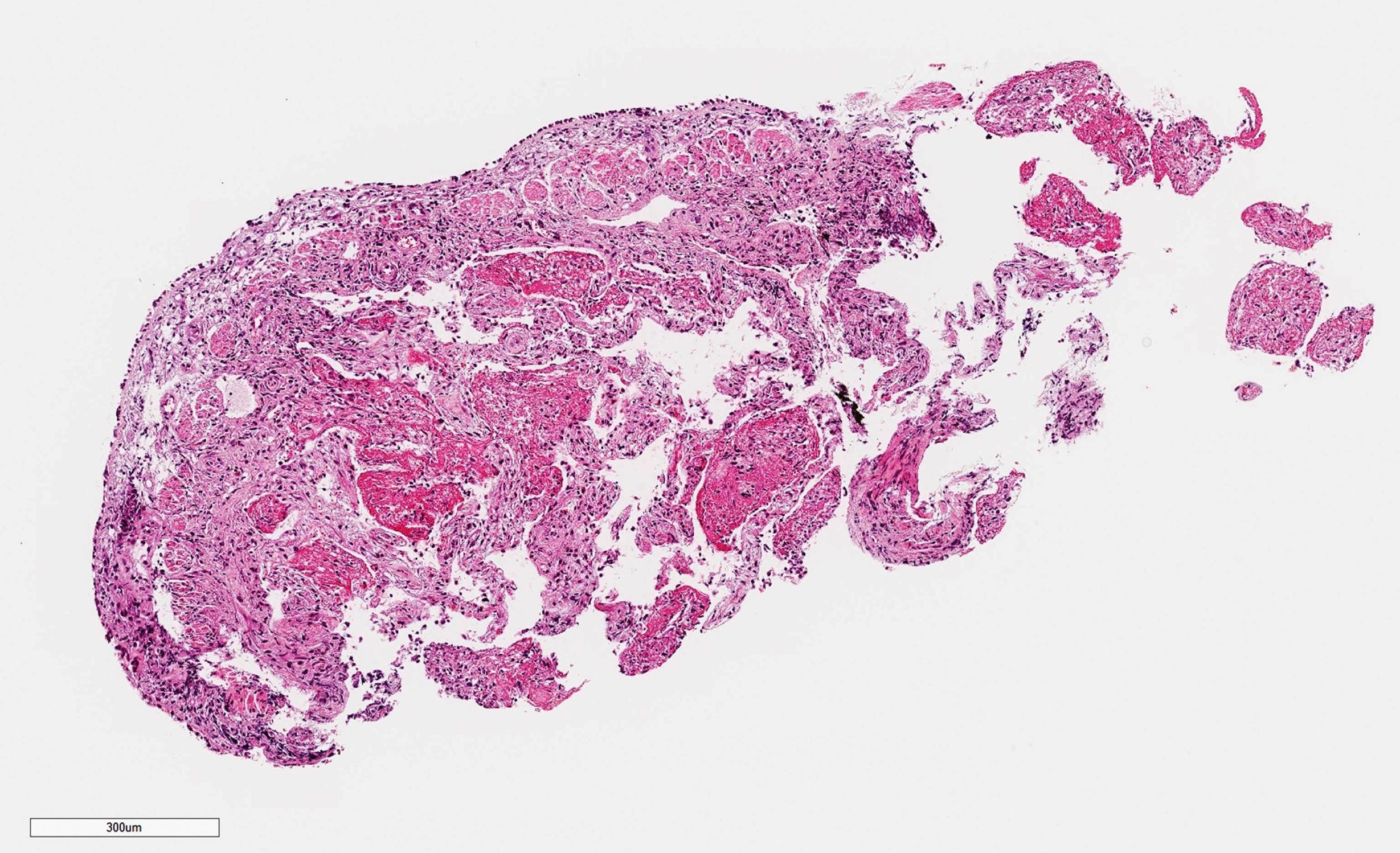
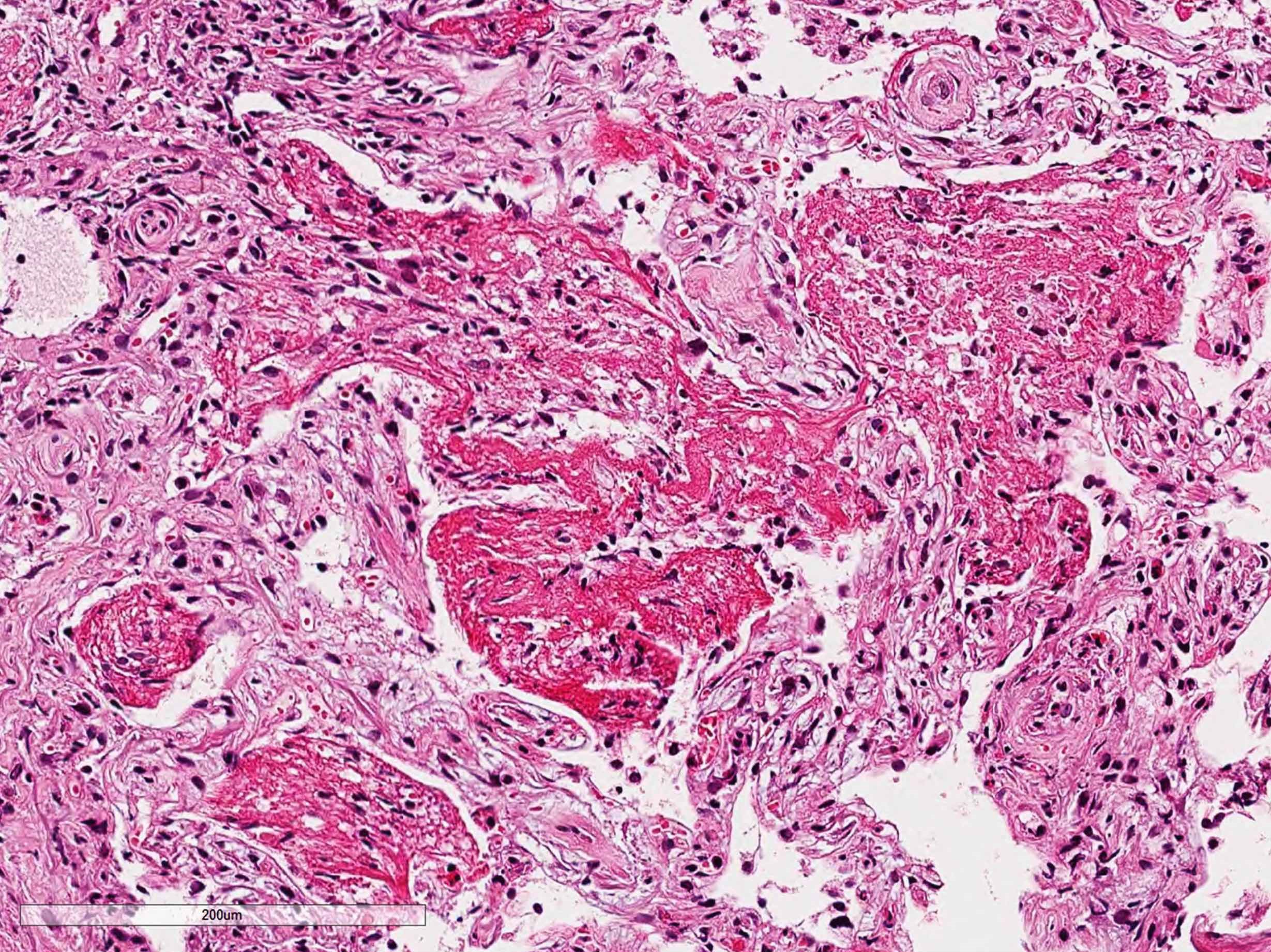
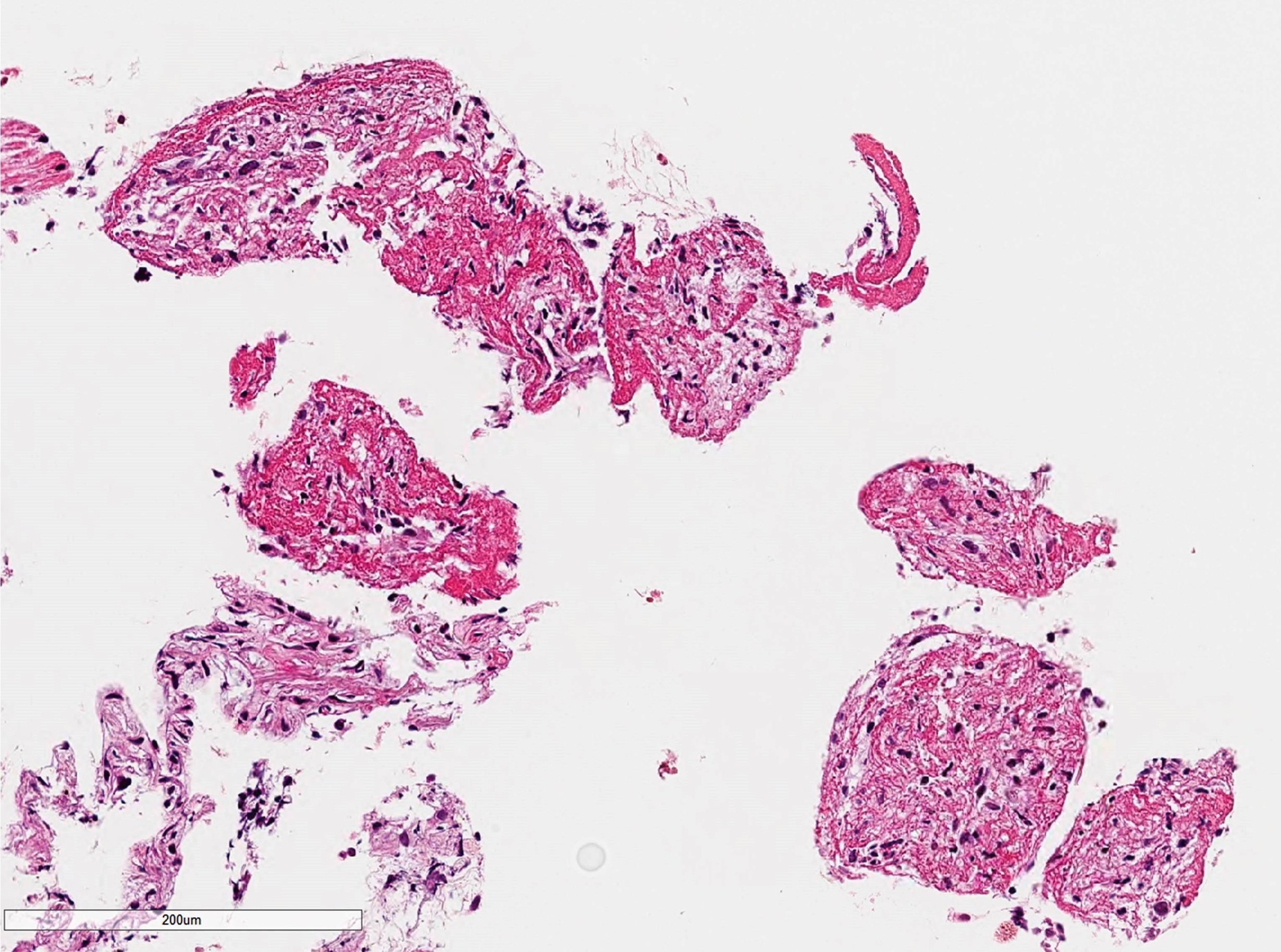
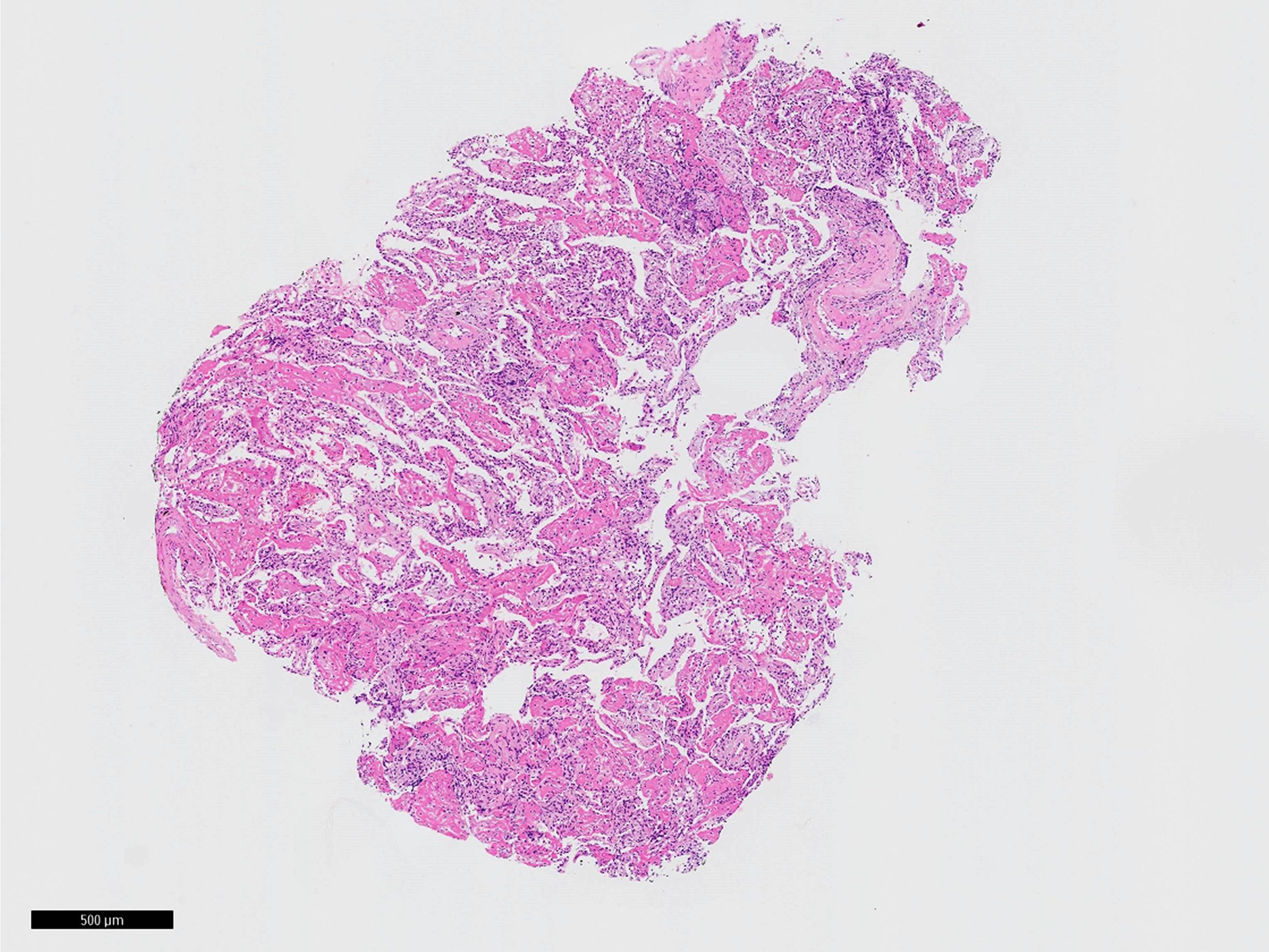
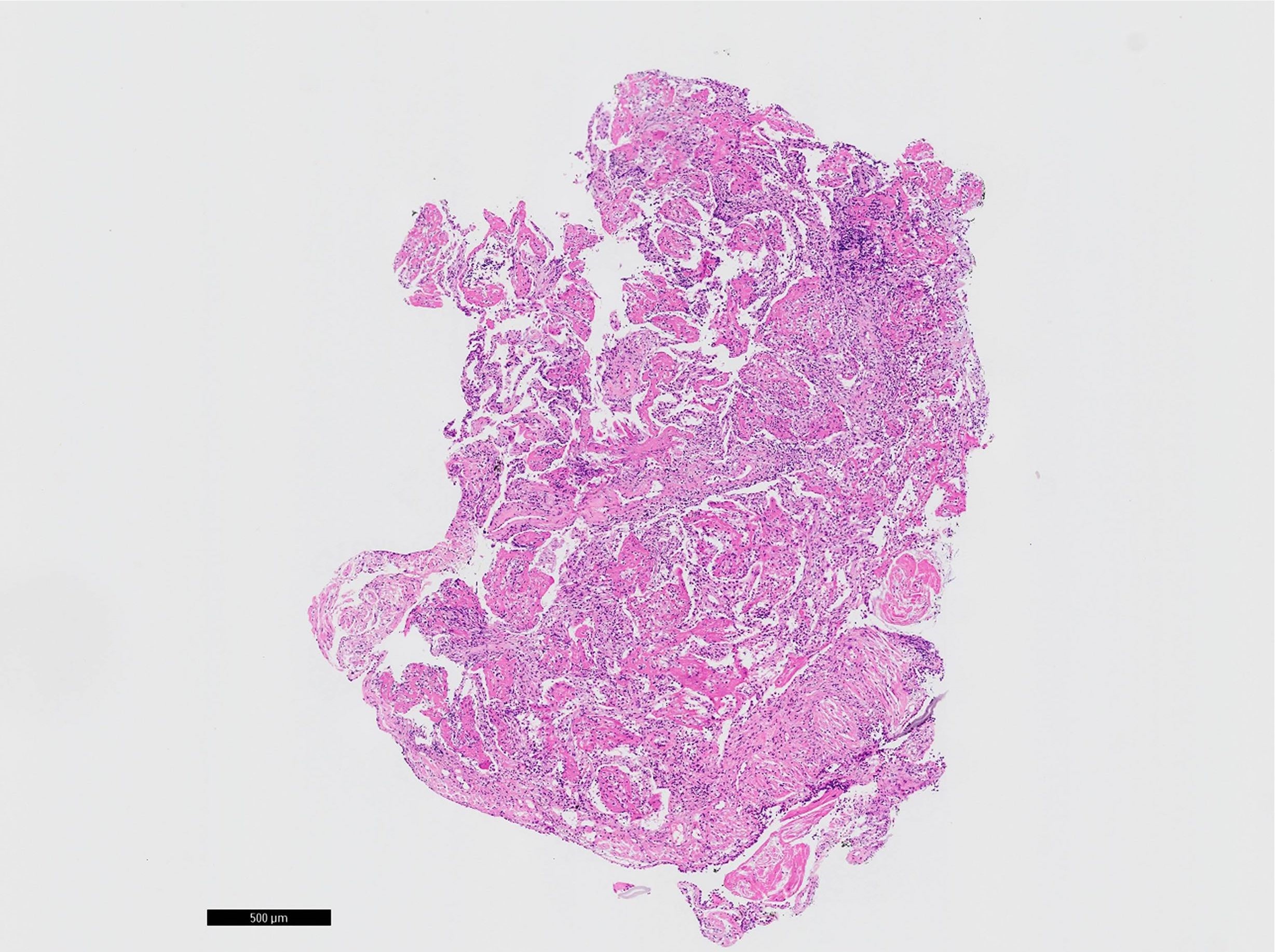
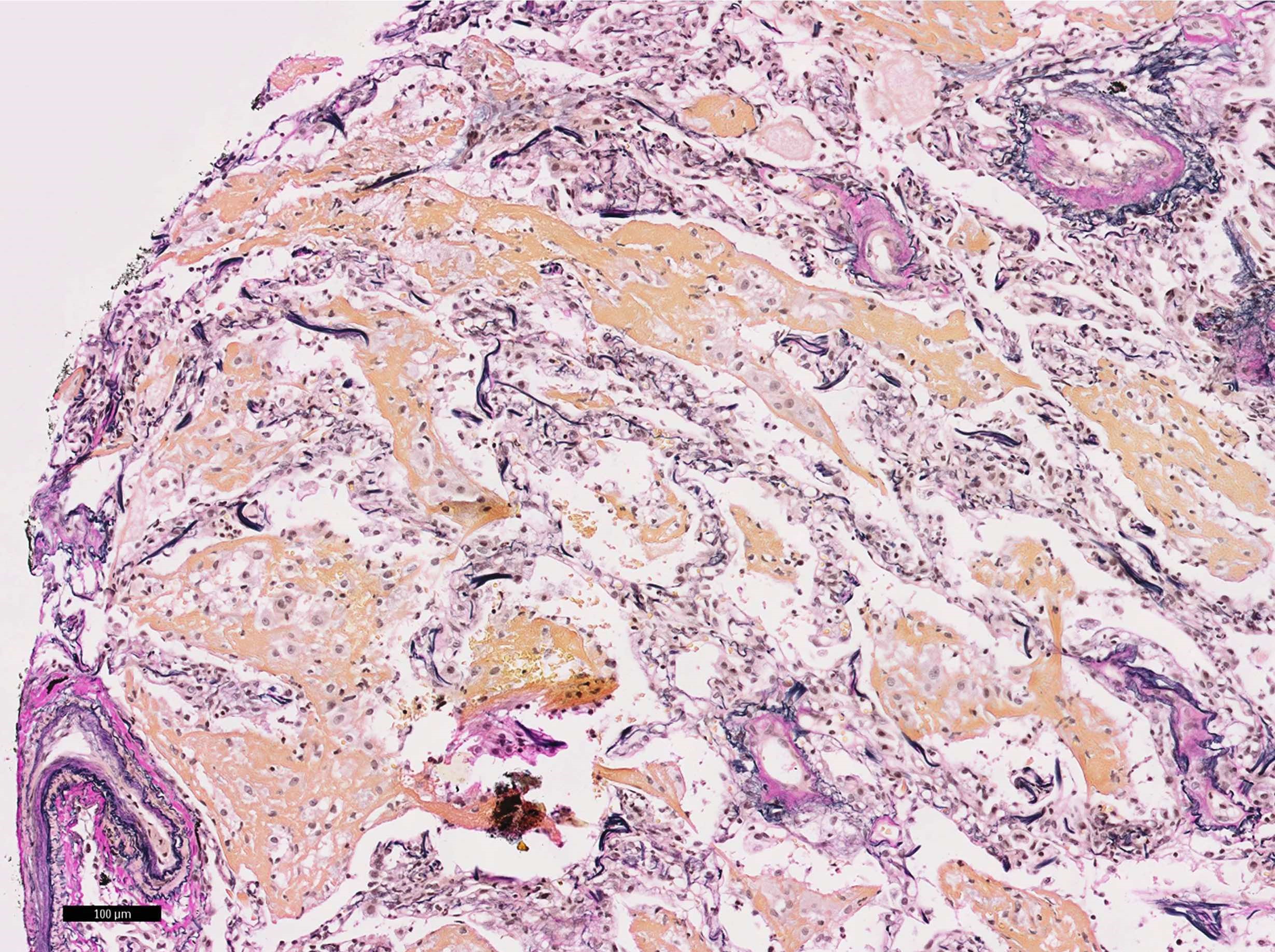
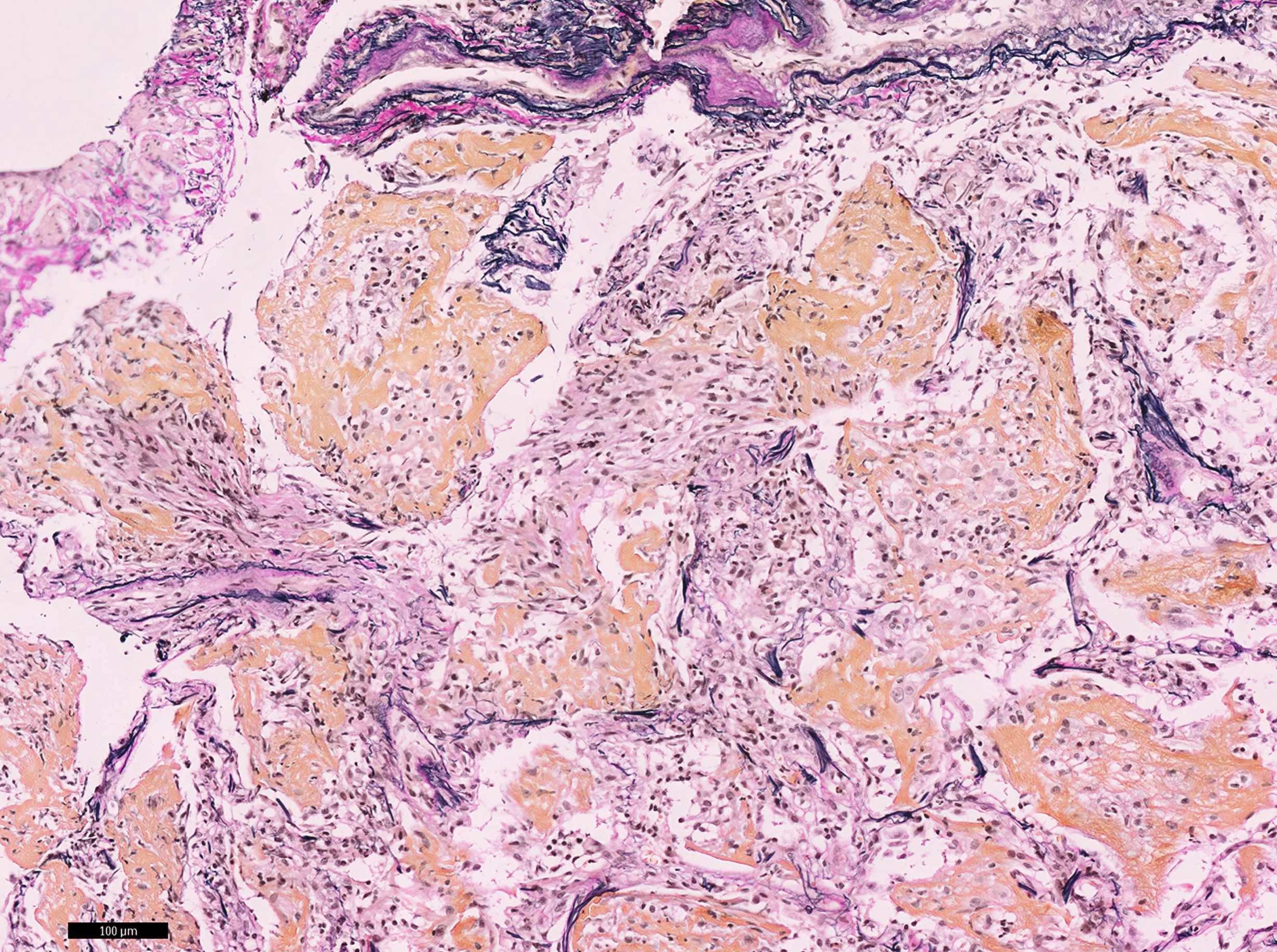
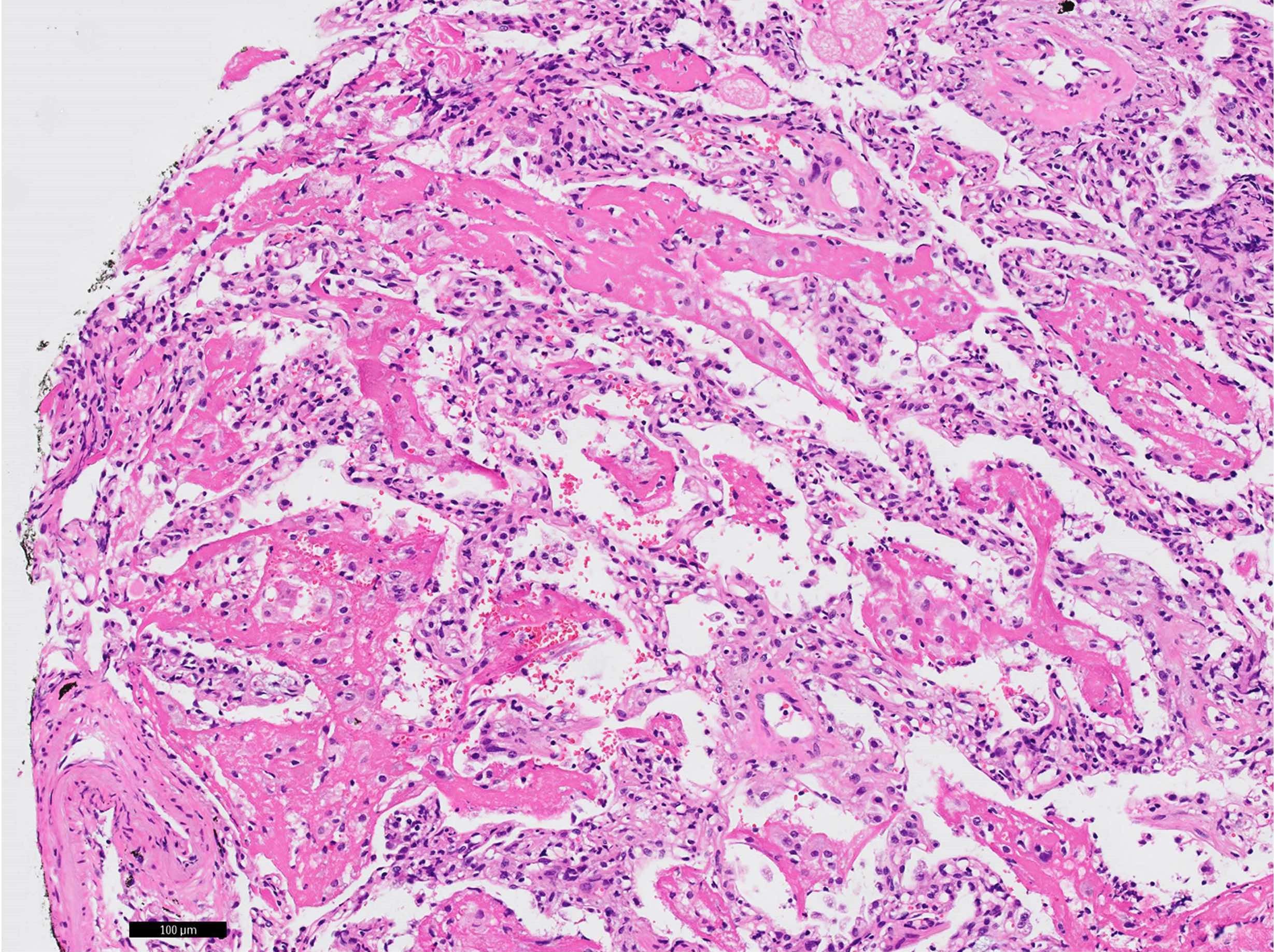
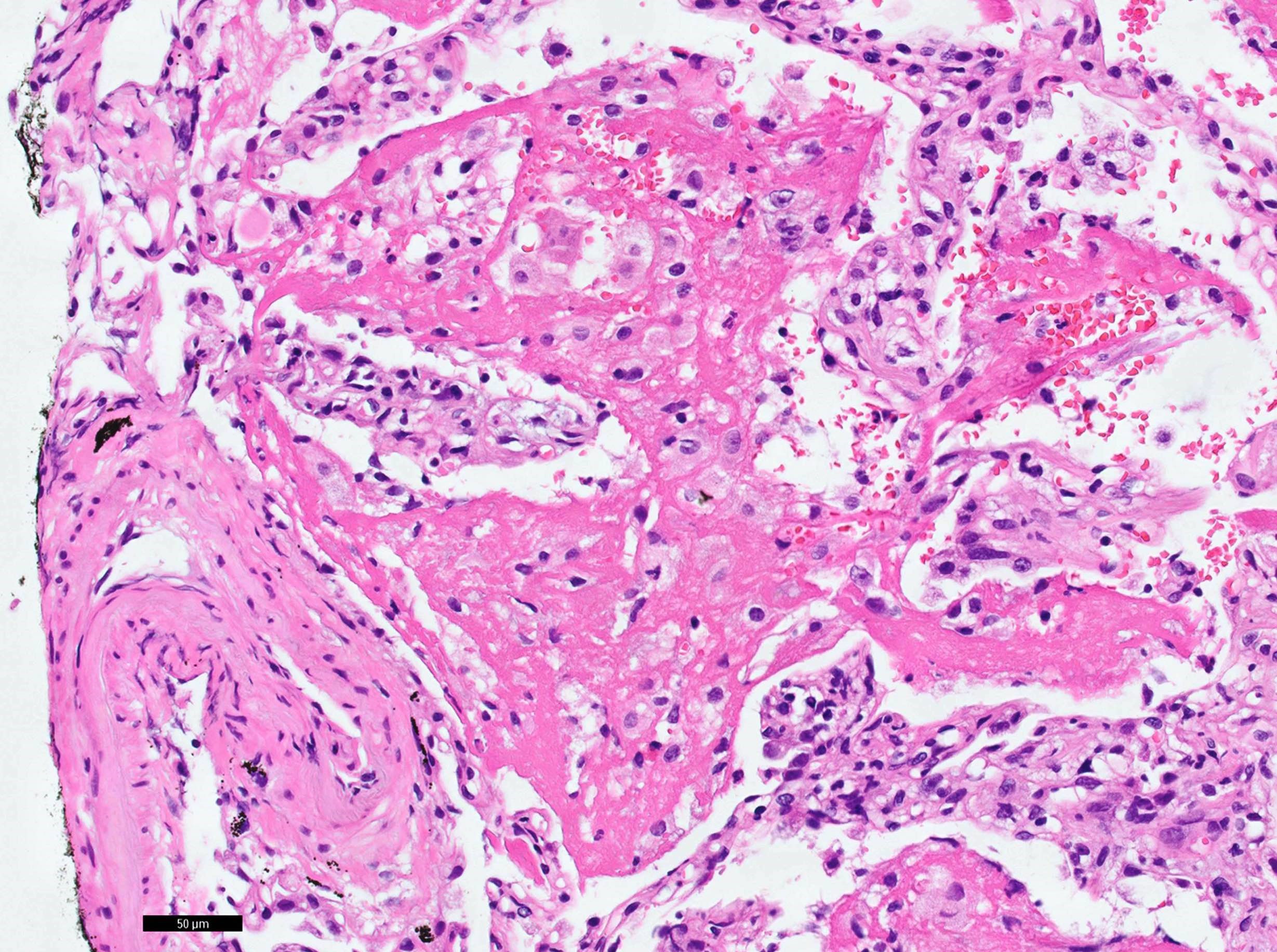
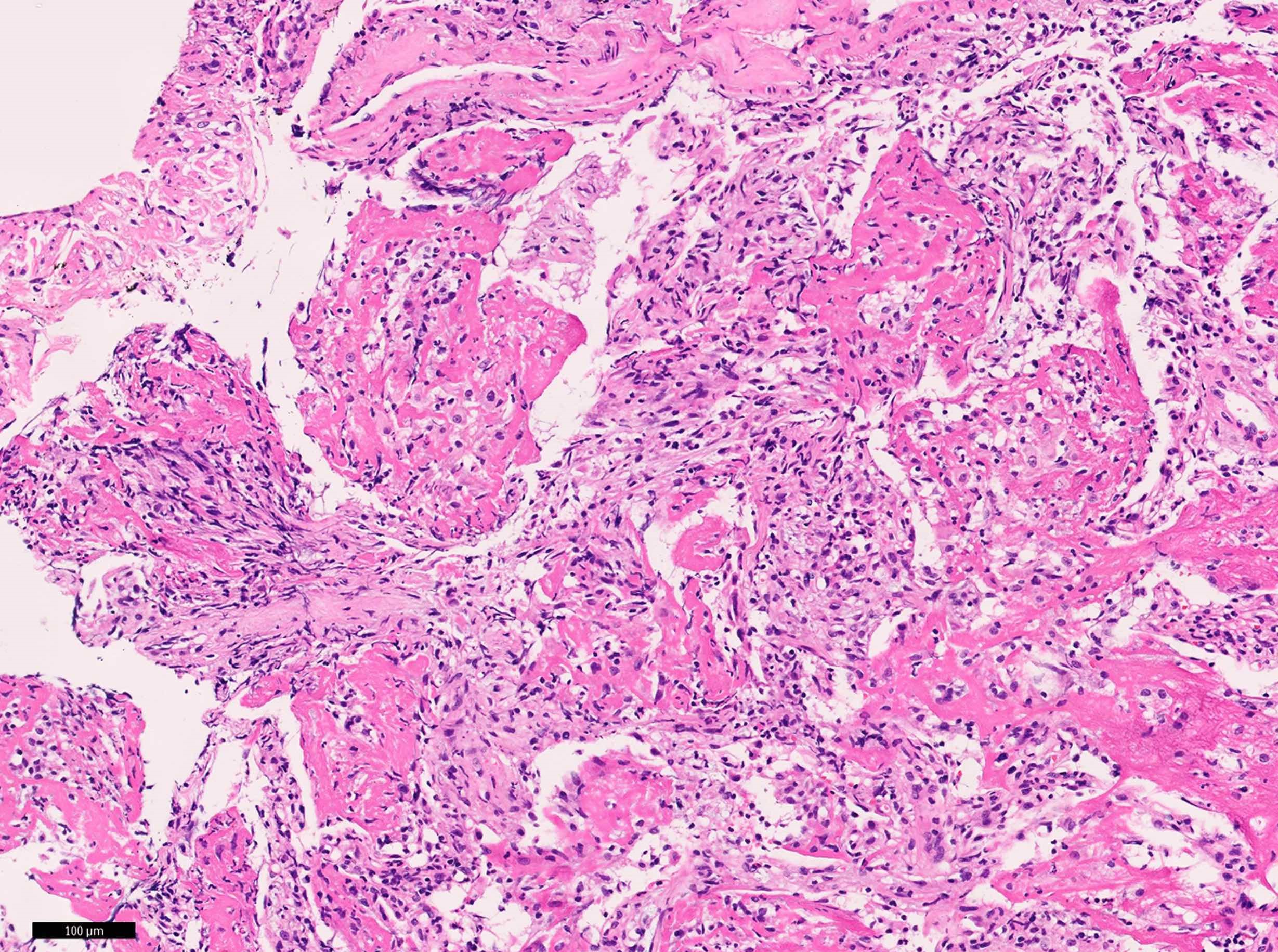
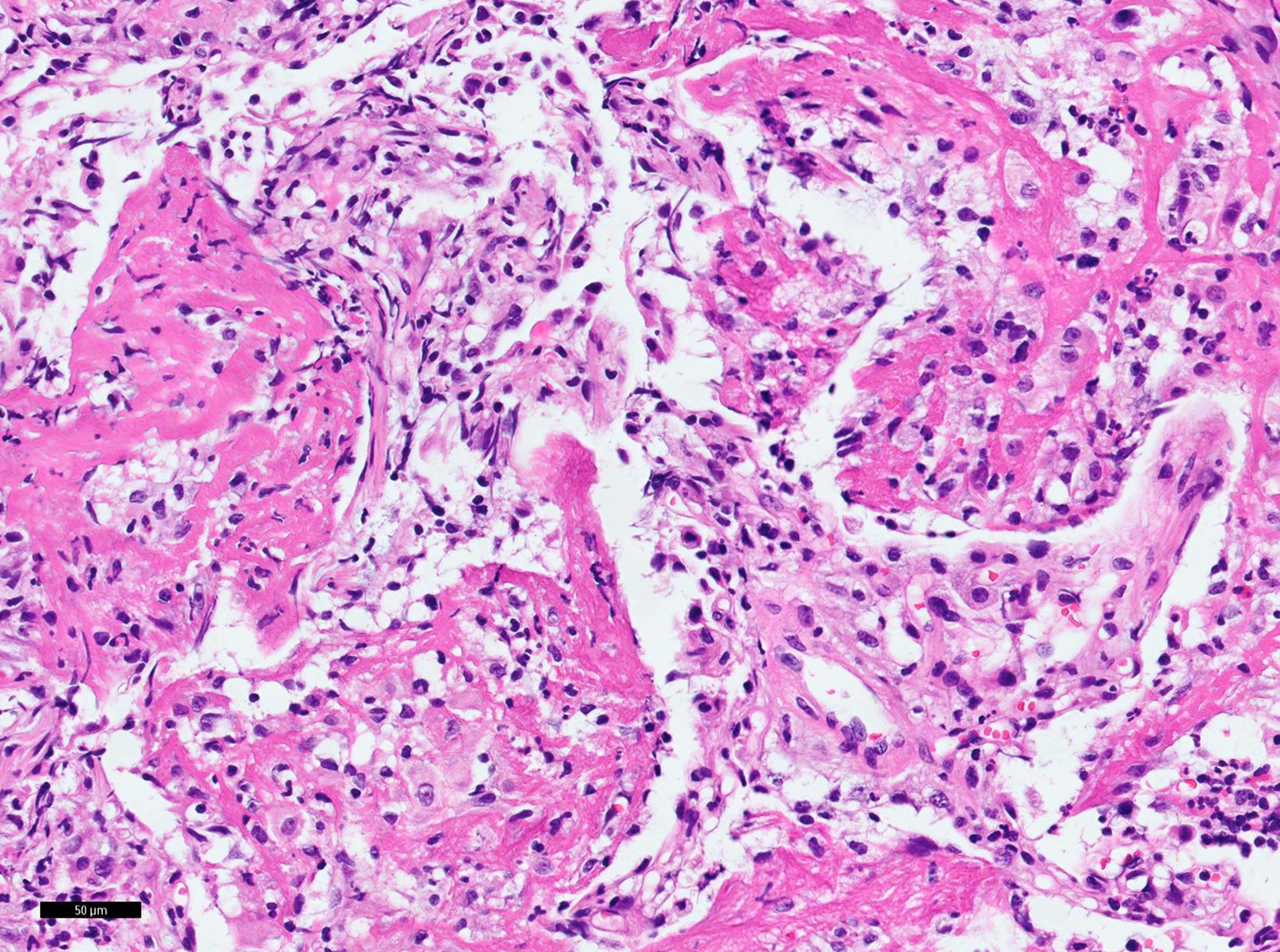
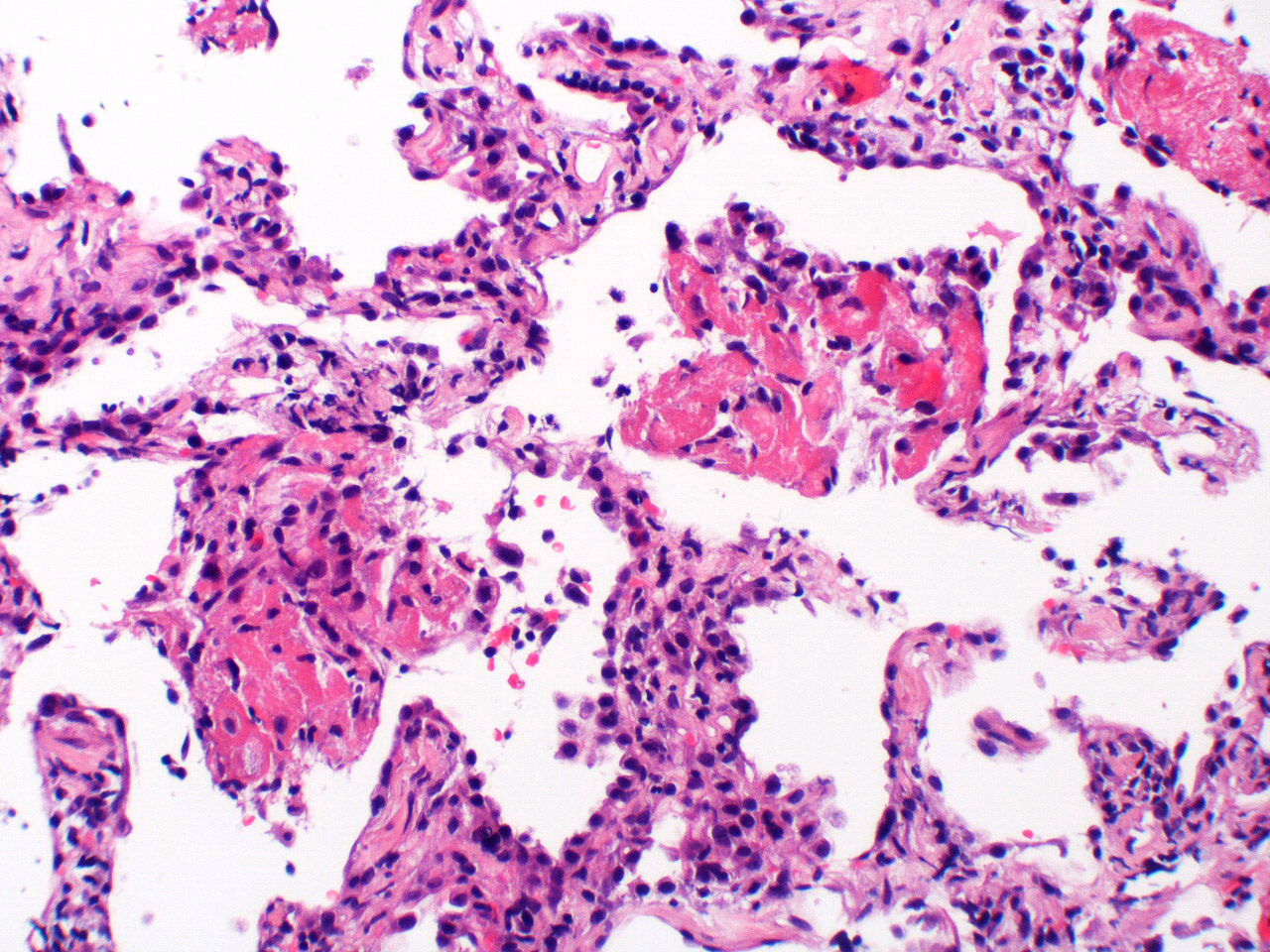
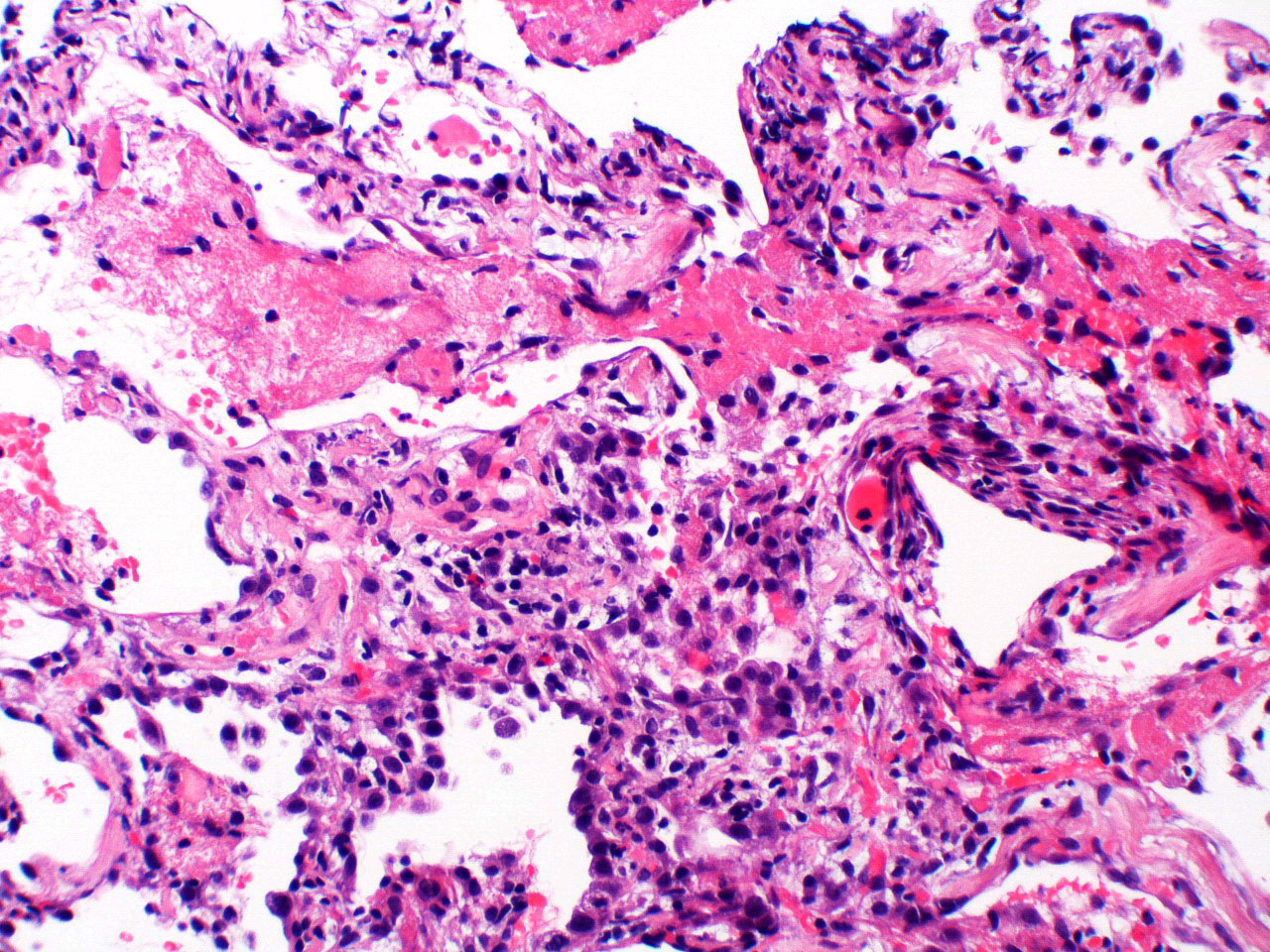
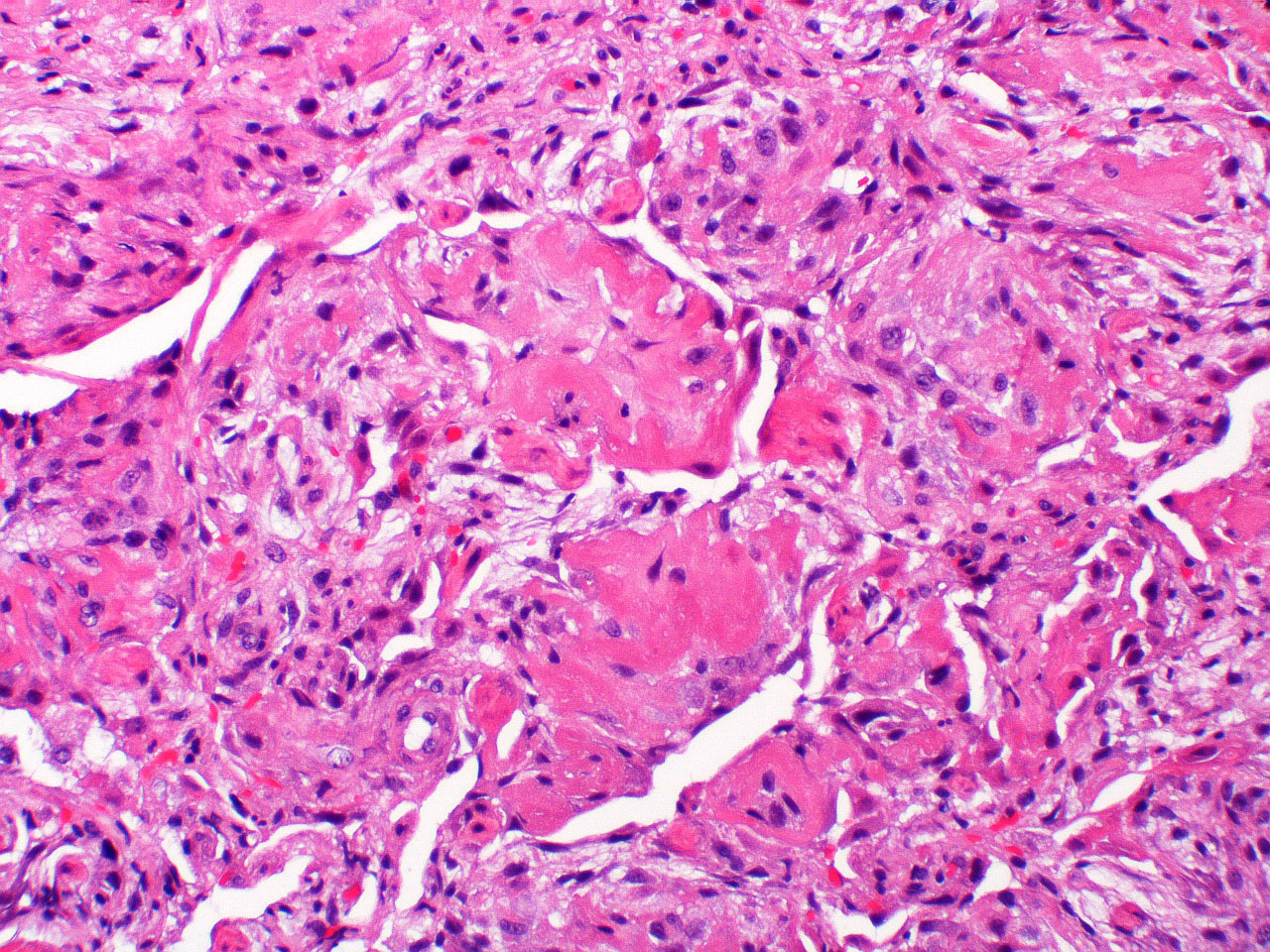
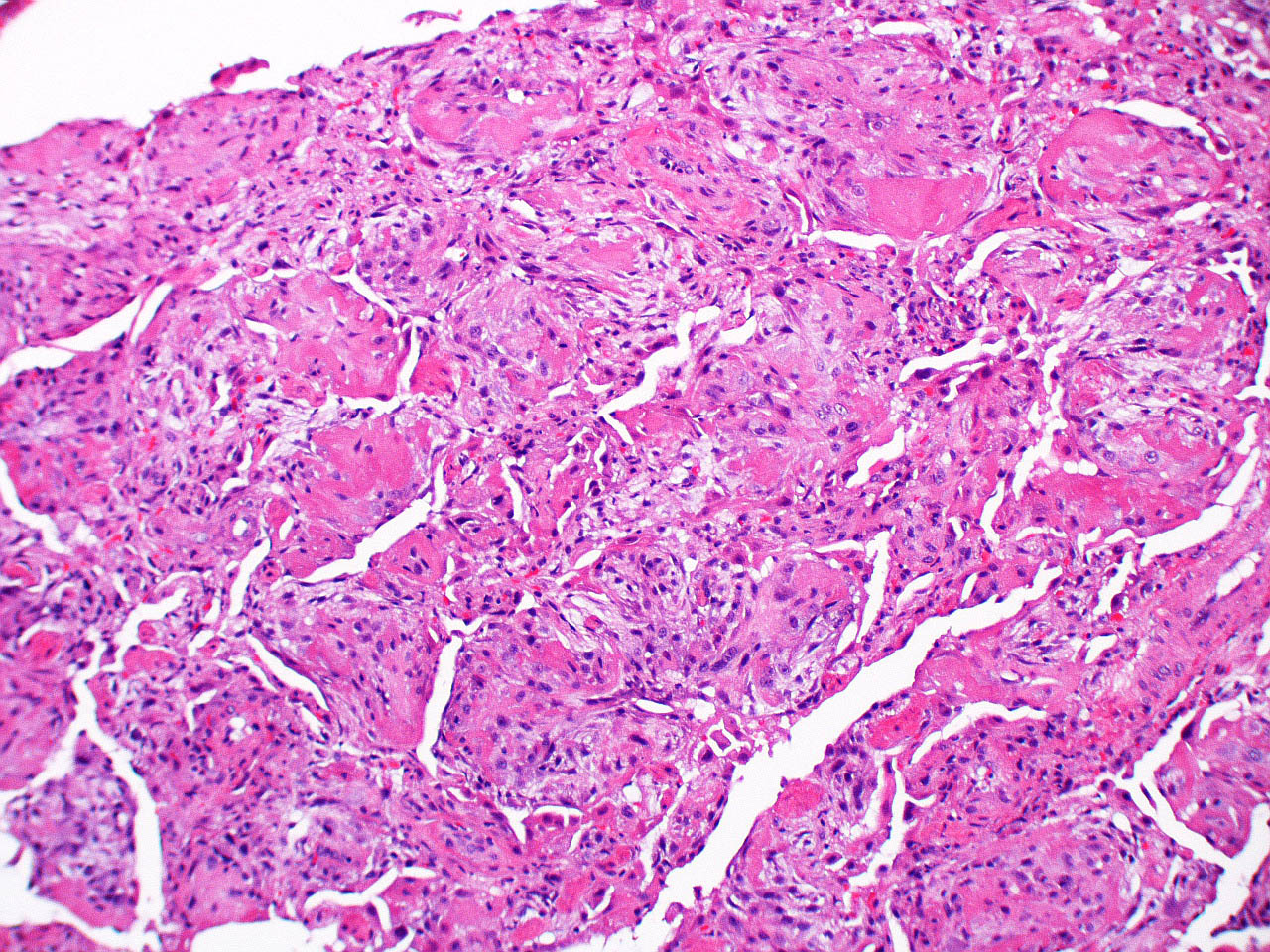
Microscopic (histologic) description
- Major findings
- Dominant findings of intra-alveolar fibrin, so called "fibrin ball"
- Involves more than 20% of the alveolar spaces in the lesion
- Neutrophils are usually scanty or absent
- Organizing pneumonia: fibroblastic plugs in alveolar sacs and ducts with loose collagen matrix
- Diffuse and patchy distribution
- Dominant findings of intra-alveolar fibrin, so called "fibrin ball"
- Minor findings
- Mild to moderate interstitial changes
- Lymphoplasmacytic infiltrate
- Alveolar septal expansion with myxoid connective tissue
- Limited within areas of fibrinous lesion
- Type 2 pneumocyte hyperplasia
- Mild to moderate interstitial changes
- Pertinent negative findings; need to rule out secondary causes and other lung disease if present
- Hyaline membranes
- Eosinophilic inflammation
- Extensive bronchopneumonia or abscess
- Granulomatous inflammation
- Vasculitis including capillaritis
- Areas of necrosis
- Marked dense fibrosis or honeycombing
- See J Clin Pathol 2015;68:441
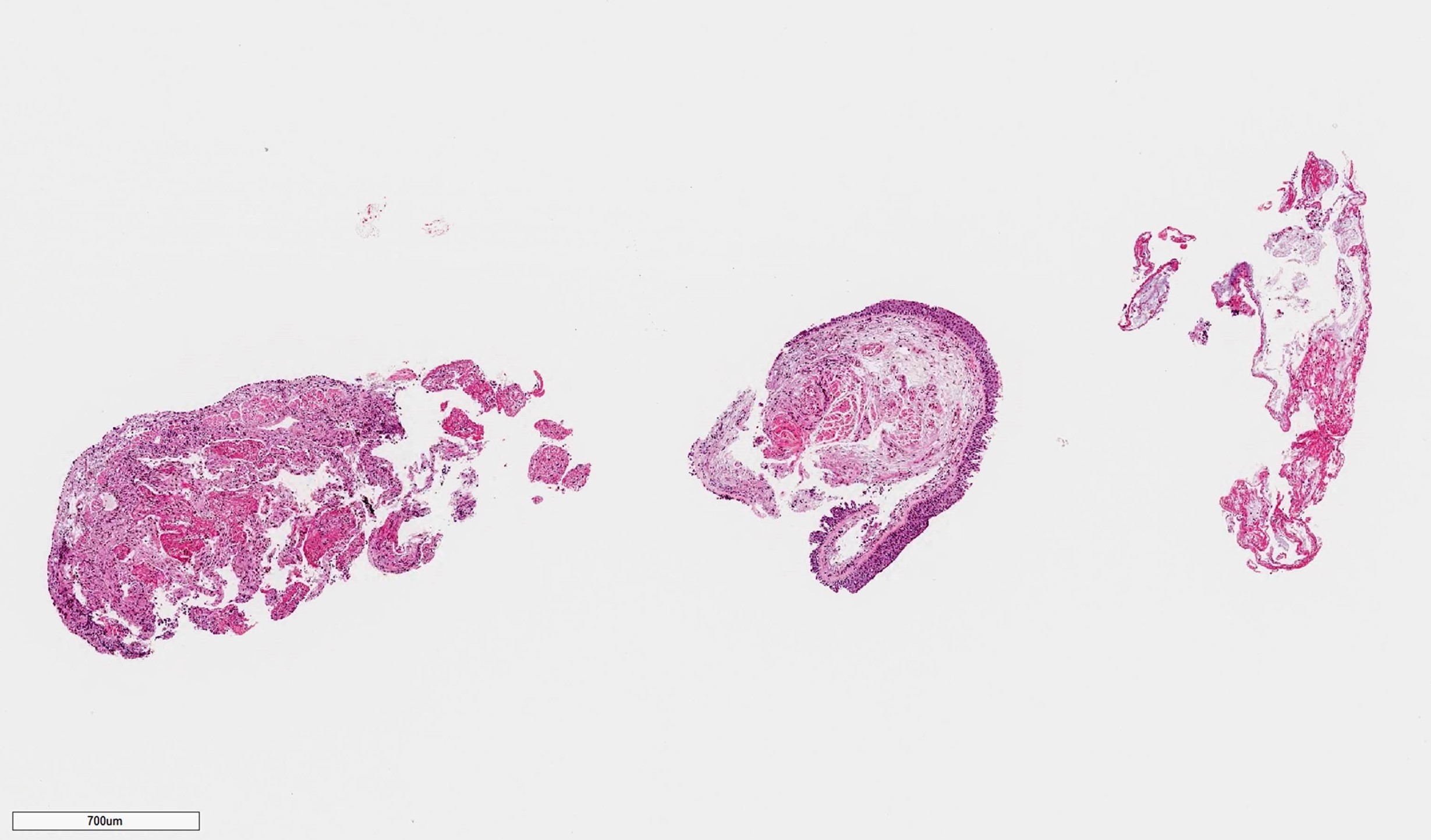
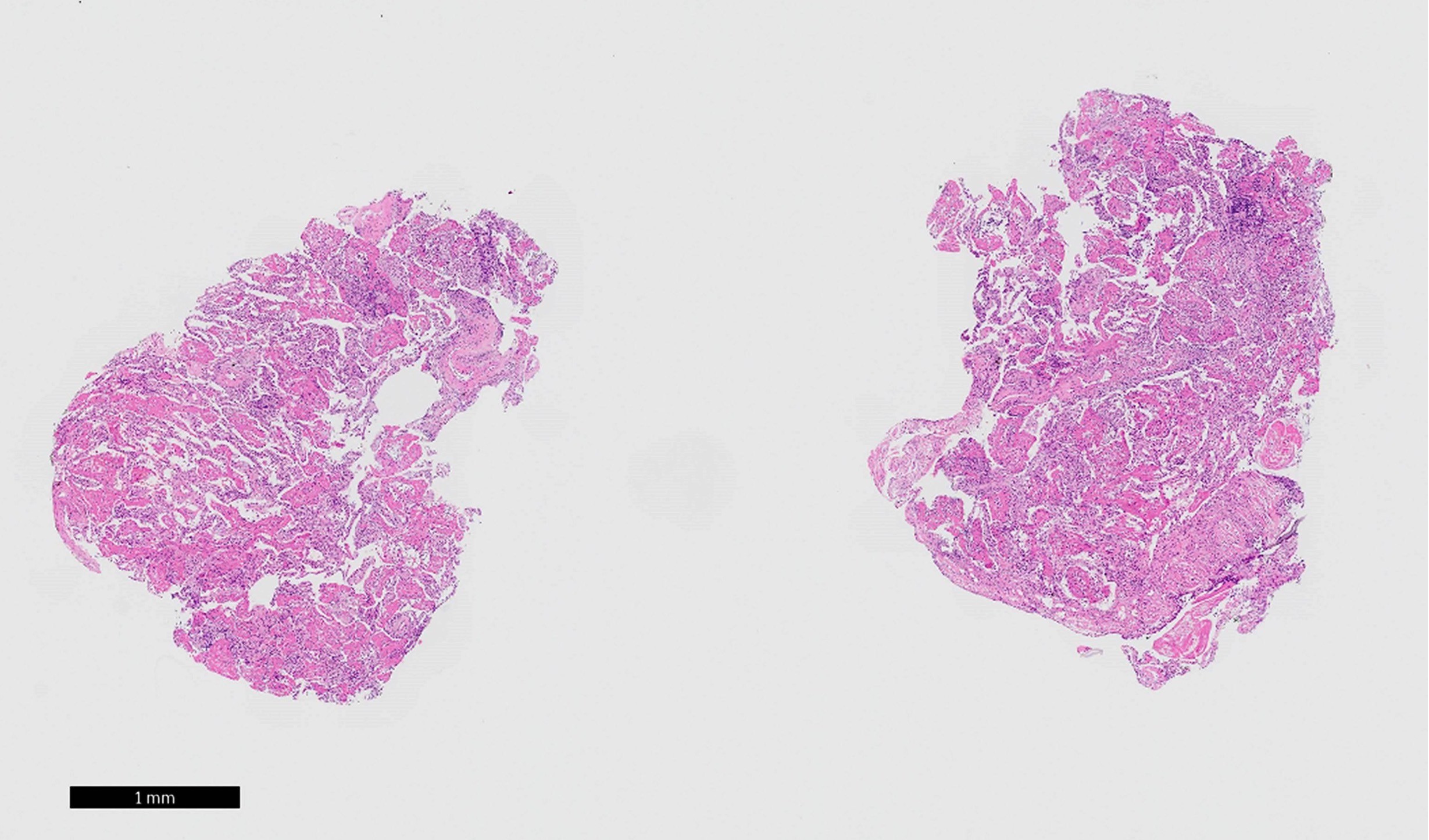
Microscopic (histologic) images
Positive stains
- Elastica van Gieson stains fibrin yellow
- Martius scarlet blue trichrome and picro Mallory staining are positive for fibrin
Negative stains
- Organizing pneumonia foci are free from elastic fiber and collagen fiber, easily confirmed by elastica van Gieson staining
- Giemsa, Grocott and Ziehl-Neelsen stains are usually mandatory to rule out infectious diseases
Differential diagnosis
- Acute exacerbation of chronic lung disease, especially hypersensitivity pneumonitis (Hum Pathol 2012;43:660)
- Cryptogenic organizing pneumonia: scanty or absent fibrin deposition
- Diffuse alveolar damage (acute interstitial pneumonia / acute respiratory distress syndrome): hyaline membranes, architectural destruction and myofibroblastic aggregation
- Eosinophilic pneumonia: prominent eosinophilic infiltrate, pink macrophages (not foamy)
- Granulomatosis with polyangiitis: geographic necrosis, alveolar hemorrhage, capillaritis, granuloma, eosinophils
- Infection: especially, fungal infection is often challenging to differentiate
- Microscopic polyangiitis: small vessel vasculitis and capillaritis with neutrophils, extravasation of neutrophils in alveolar space, alveolar hemorrhage
Additional references
Board review style question #1
Which two of the following findings are against the histological diagnosis of acute fibrinous and organizing pneumonia?
- Eosinophilic infiltration
- Hyaline membranes
- Lymphocytic infiltration
- Organizing pneumonia
- Type 2 pneumocyte hyperplasia
Board review style answer #1
A and B. Eosinophilic infiltration suggests eosinophilic pneumonia. Hyaline membranes suggest diffuse alveolar damage.
Comment Here
Reference: Acute fibrinous and organizing pneumonia
Comment Here
Reference: Acute fibrinous and organizing pneumonia