Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Brunetti A, Youssef B, Wu RI. Adenosquamous. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumoradenosquamous.html. Accessed August 26th, 2025.
Definition / general
- Malignant neoplasm showing components of both squamous cell carcinoma and adenocarcinoma (each comprising at least 10% of the tumor)
Essential features
- WHO classification as non-small cell lung carcinoma with at least 10% components of both adenocarcinoma and squamous cell carcinoma by histomorphology that may be separate or intermingled
- Diagnosis made on resection specimens, although it may be suspected on biopsy or cytology with an overall rare incidence of 0.4 - 4% of all lung cancers
- Clinical presentation frequently resembles other non-small cell carcinomas but it appears to have an adverse prognosis (Oncotarget 2017;9:8133)
- Computed tomography (CT) scan shows central or peripheral location with central lesions commonly showing postobstructive inflammatory changes and peripheral tumors appearing as ground glass opacities
Terminology
- By WHO classification, adenosquamous carcinoma contains at least 10% each of malignant squamous and glandular components
- Differentiate from adenocarcinoma with squamoid features / squamous metaplasia as well as squamous cell carcinoma with pseudoglandular features
ICD coding
- Use code specific for location of tumor
- ICD-10: C34.90 - malignant neoplasm of unspecified part of unspecified bronchus or lung
Epidemiology
- Uncommon; 0.4 - 4% of lung cancers
- Similar age and sex distribution to other lung cancers (Am J Clin Oncol 1992;15:356)
Sites
- Tends to arise peripherally but may be central
Pathophysiology
- More aggressive than pure carcinomas when matched for stage
- Molecular mechanisms are not fully understood
- Environmental factors are possible contributing factors
- Chronic inflammation may influence pathogenesis
- Aggressive behavior: more aggressive than adenocarcinoma or squamous cell carcinoma, leading to poorer prognosis
- Metastatic potential: high risk of spreading to lymph nodes and distant organs
- Reference: StatPearls: Non-Small Cell Lung Cancer [Accessed 17 February 2025]
Etiology
- Association with smoking, similar to other lung cancers
Clinical features
- Similar to lung adenocarcinoma
Diagnosis
- Diagnosis made on resection specimens, though can be suggested in biopsy or cytology as follows
- Non-small cell carcinoma (see note)
- Note: glandular and squamous components are present; the findings could represent adenosquamous carcinoma
Radiology description
- Peripheral tumor, averages 3 - 4 cm
- Lobulated to spiculated, ill defined borders (Am J Clin Oncol 1992;15:356)
Prognostic factors
- Resectable adenosquamous carcinoma patients had higher pleural invasion incidence, poorer differentiation and worse survival compared with squamous cell carcinoma and adenocarcinoma patients (Jpn J Clin Oncol 2022;52:1456)
- EGFR mutated adenosquamous carcinomas appear to have better prognosis (Pathol Int 2013;63:77)
- Adenosquamous carcinomas without EGFR mutations show a moderate response to immune checkpoint inhibitor (ICI) based immunotherapy (Front Immunol 2022;13:944812)
- High CXCR4 expression predicts a poor prognosis in resected lung adenosquamous carcinoma (J Cancer 2020;11:810)
- Adenocarcinomatous predominant subtype of adenosquamous carcinoma of the lung (ASC) is associated with a better prognosis than the squamous cell carcinoma predominant subtype (J Cancer 2020;11:810)
Case reports
- 42 year old man with right upper lung adenosquamous carcinoma resection following neoadjuvant targeted therapy (Ann Palliat Med 2021;10:4987)
- 60 year old man with adenosquamous lung carcinoma presenting as an ulceroproliferative growth (J Cancer Res Ther 2020;16:922)
- 60 year old woman with EGFR mutated adenosquamous carcinoma with micropapillary pattern (Respirol Case Rep 2016;4:e00179)
- 66 year old man with adenosquamous carcinoma arising in the background of IgG4 related lung disease (J Pathol Transl Med 2019;53:188)
- 66 year old woman with adenosquamous cell lung cancer successfully treated with gefitinib (Mol Clin Oncol 2014;2:282)
- 71 year old man with cytology consistent with adenosquamous carcinoma (Diagn Cytopathol 2012;40:830)
Treatment
- Surgical resection
- EGFR tyrosine kinase inhibitors may be considered for those harboring this mutation (Cancer Manag Res 2018;10:2401)
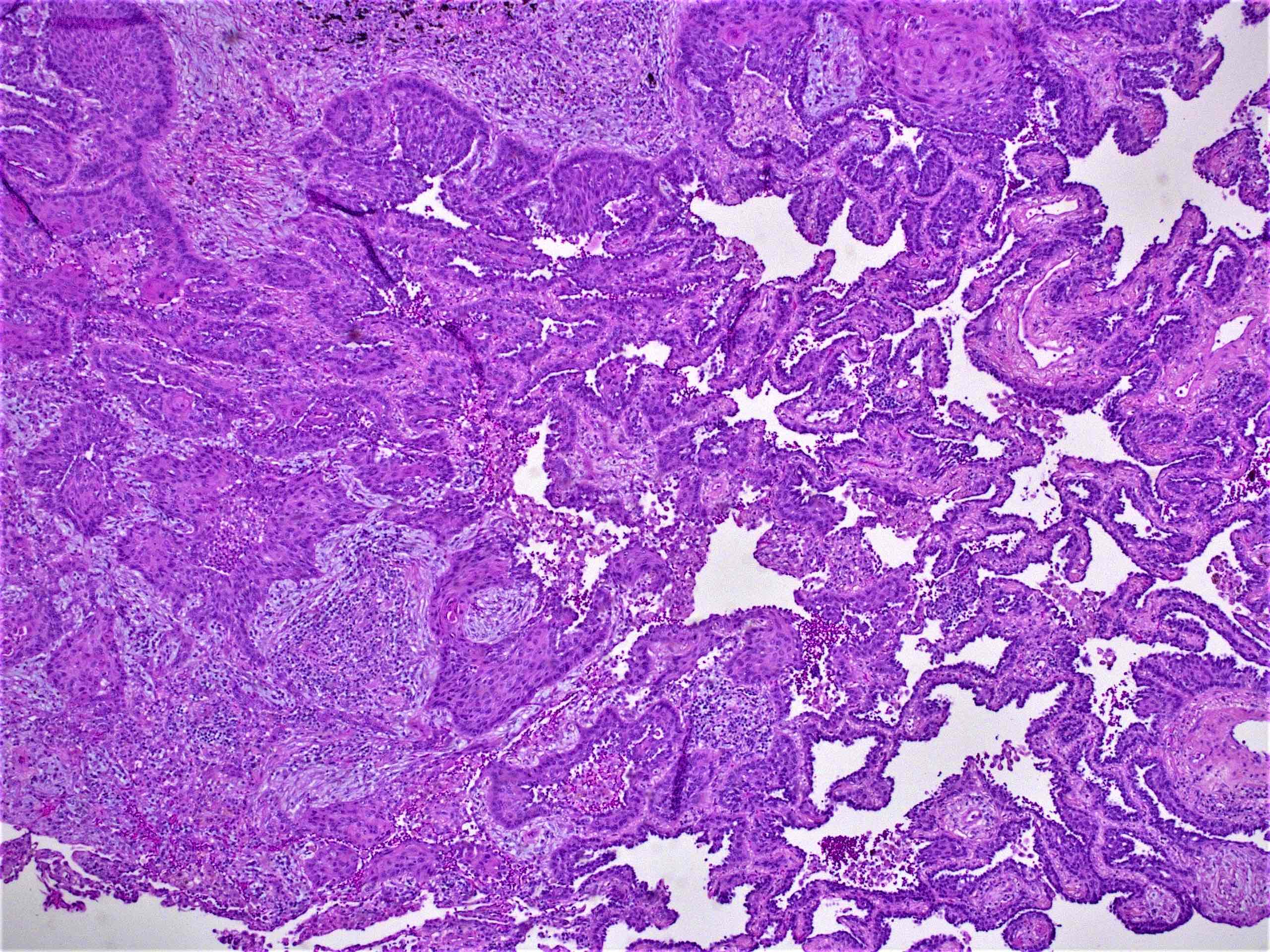
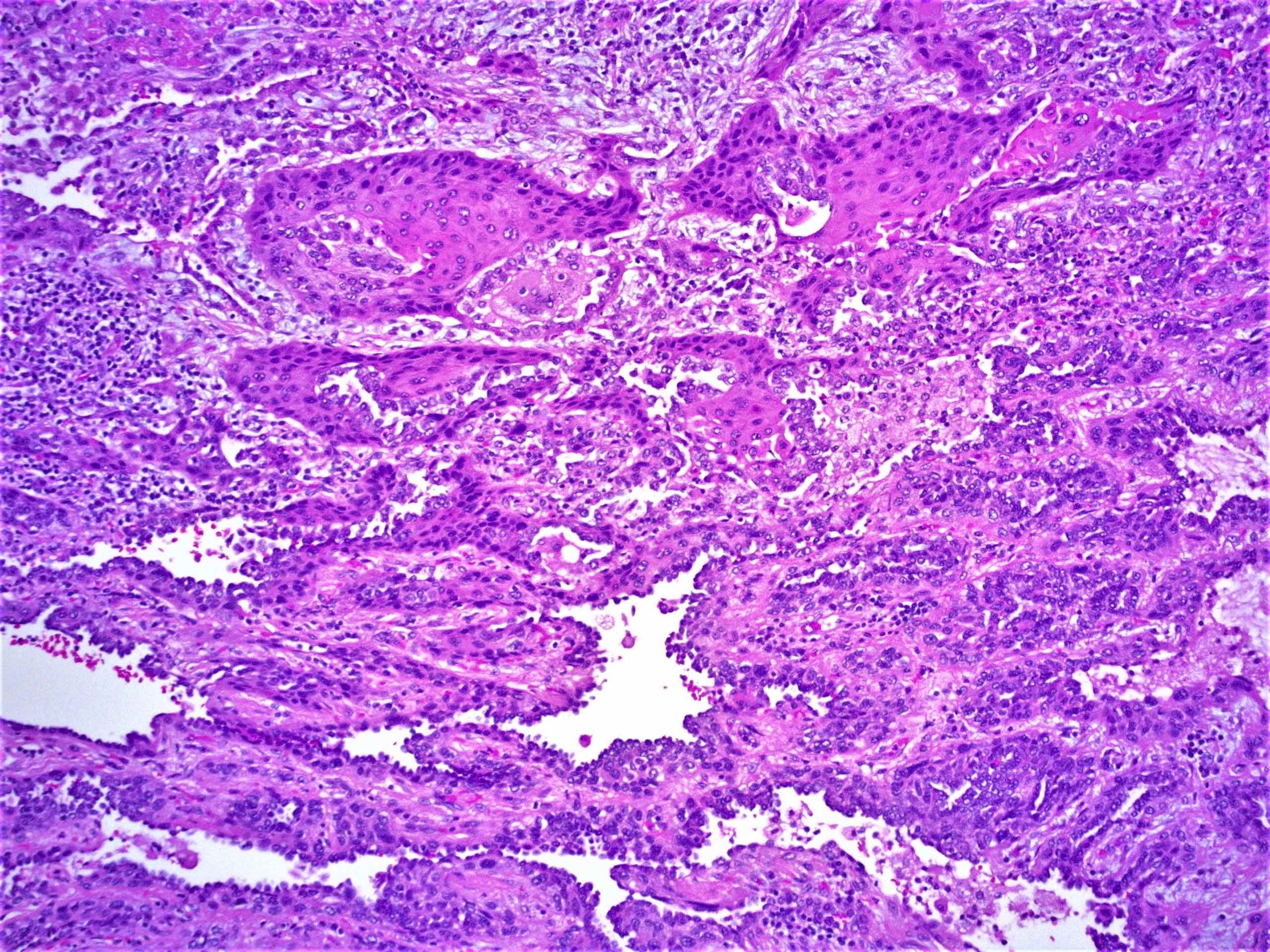
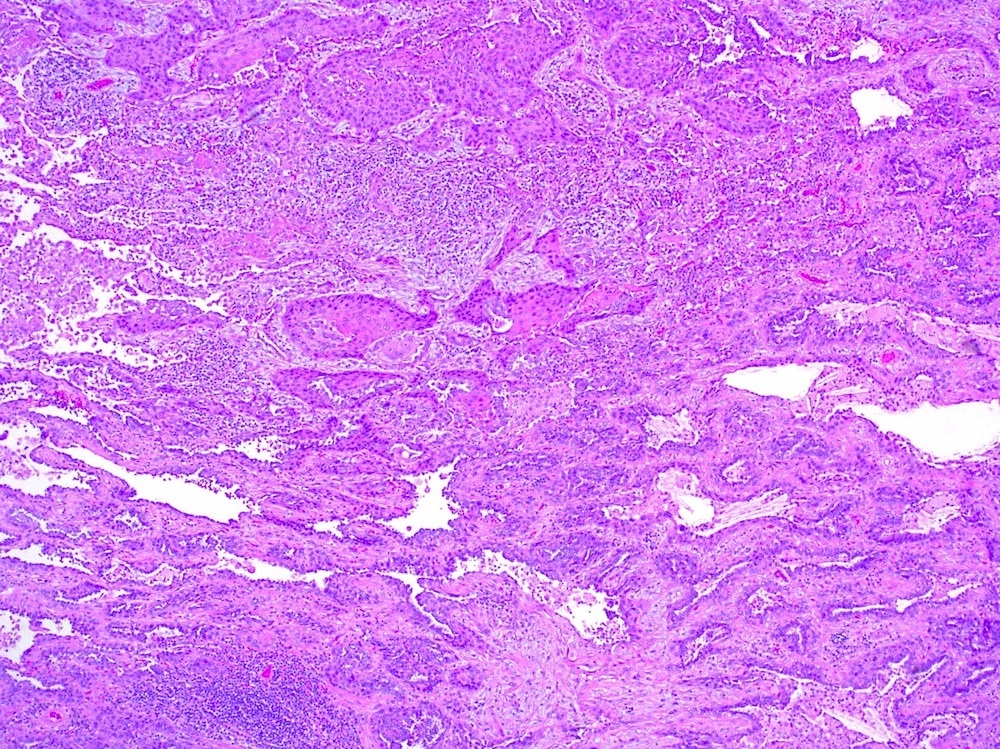
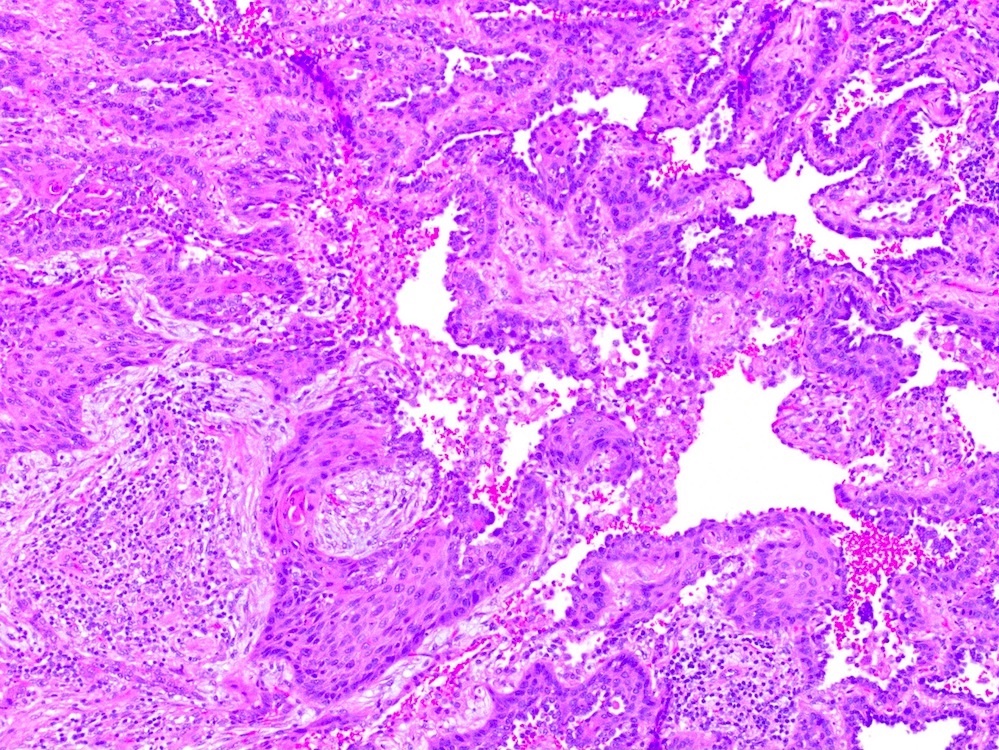
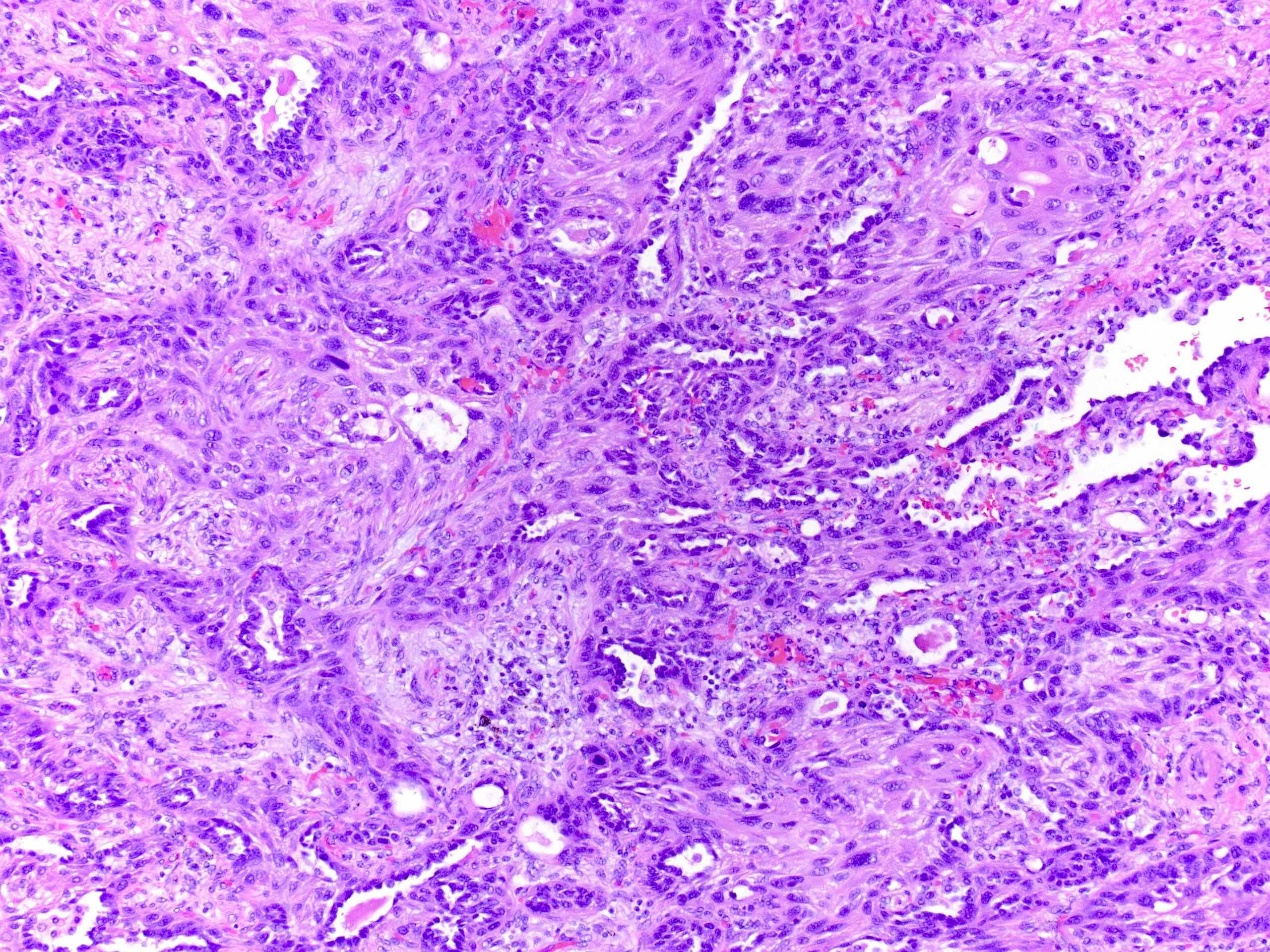
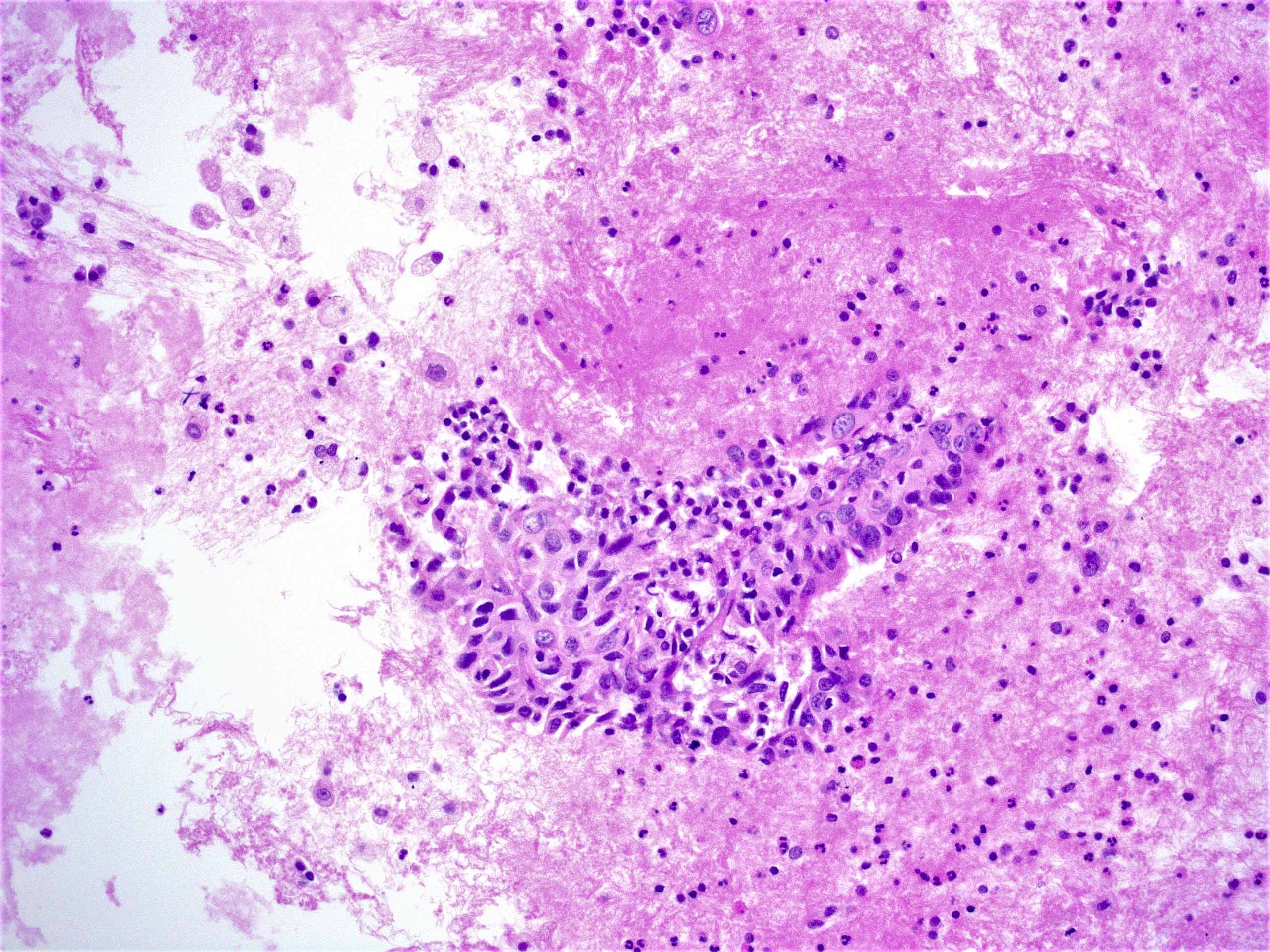
Microscopic (histologic) description
- Malignant cells with squamous or glandular differentiation with variable degree of admixture
- Squamous component may show intercellular bridges or keratin pearls
- Glandular components may show lumens with mucin; may have papillary, lepidic, acinar or tubular patterns
- Metastasis in lymph node tends to be same histologic type as the major component but not necessarily (Cancer 1991;67:649)
Microscopic (histologic) images
Contributed by Roseann Wu, M.D., M.P.H.
Virtual slides
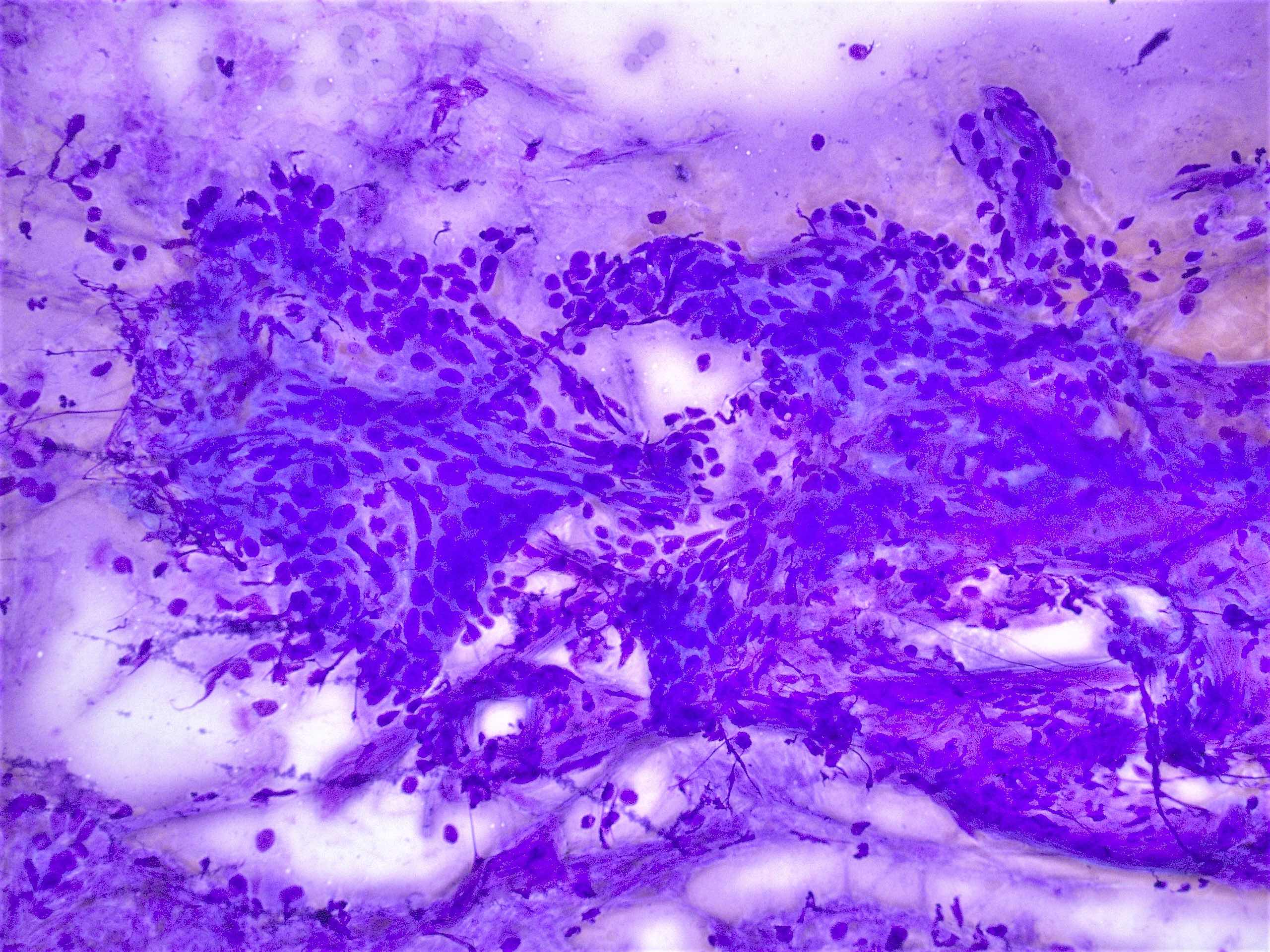
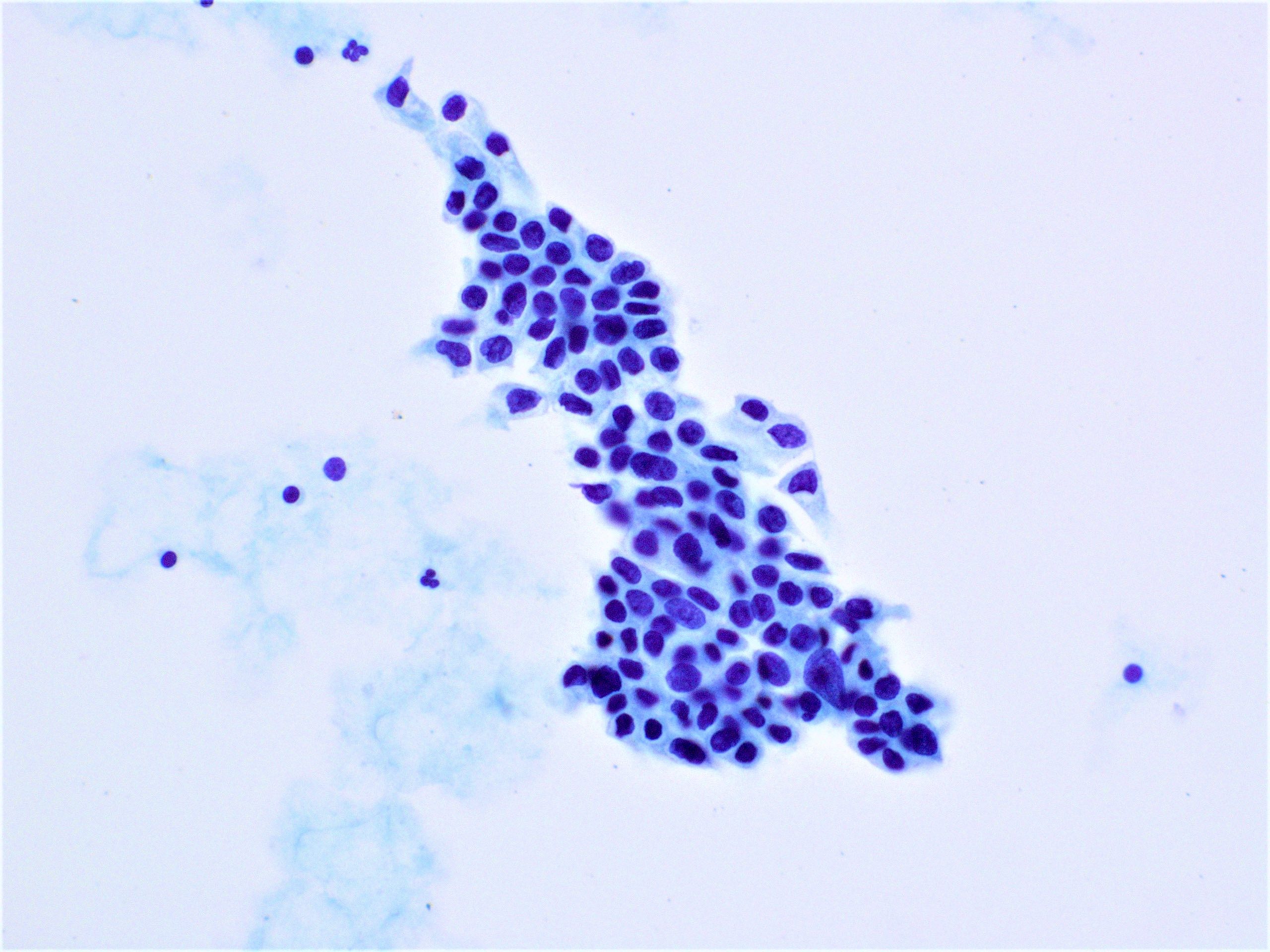
Cytology description
- Variable depending on squamous or glandular components and degree of differentiation (see lung adenocarcinoma and lung squamous cell carcinoma)
Cytology images
Positive stains
- TTF1 in adenocarcinoma component and p40 and CK5/6 in squamous component
- CK7
- Reference: StatPearls: Non-Small Cell Lung Cancer [Accessed 17 February 2025]
Negative stains
- Neuroendocrine markers (chromogranin, synaptophysin and CD56)
Electron microscopy description
- Features of both squamous cell carcinoma and adenocarcinoma (ADC) are present in adenosquamous carcinoma
- Adenocarcinoma features include intracellular and intercellular lumina and short, stubby microvilli
- Squamous cell carcinoma features include well formed desmosomes with tonofilaments and intercellular bridges
- Proportion of primitive cells (without ultrastructural features of glandular or squamous differentiation) may be present
- Reference: Am J Clin Pathol 1983;80:6
Molecular / cytogenetics description
- EGFR and KRAS mutations, both characteristic of adenocarcinoma, have been reported in adenosquamous carcinoma
- EGFR amplification is frequent in adenosquamous carcinoma
- References: J Clin Med 2024;13:5711, Am J Transl Res 2024;16:126
Videos
Metastatic adenosquamous carcinoma of the lung to wrist with squamous histology
Sample pathology report
- Lung, right lower lobe, biopsy:
- Compatible with adenosquamous carcinoma (see comment)
- Comment: The tumor displays both glandular and squamous differentiation, characteristic of adenosquamous carcinoma. This is a rare and aggressive subtype of non-small cell lung carcinoma. The patient's clinical presentation and radiological findings support the pathological diagnosis. Further molecular testing and staging studies may be necessary for appropriate treatment planning. Immunohistochemical staining shows positivity for thyroid transcription factor 1 (TTF1) in the adenocarcinoma component, confirming its pulmonary origin. Positivity for p40 and p63 is observed in the squamous component, confirming its squamous differentiation.
Differential diagnosis
- Adenocarcinoma with squamoid features or foci of benign squamous metaplasia:
- Malignant features are present only in areas of glandular differentiation
- Lacks malignant features in the foci of squamoid differentiation
- High grade mucoepidermoid carcinoma:
- Central airways
- Typical morphology shows varying proportions of epidermoid cells, intermediate cells and mucocytes
- Overt keratinization is rare
- Mucous cells embedded in epidermoid cell nests or lining cystic spaces
- Intermediate cells found within epidermoid cell nests or forming separate nests
- MAML2 rearrangement detected by FISH (helpful if present)
- Squamous cell carcinoma with pseudoglandular features or entrapped epithelium:
- Collision tumor:
- In a collision tumor, the 2 tumor components should be clearly separated, with distinct histological features for each
- In adenosquamous carcinoma, the glandular and squamous components are typically intermingled within the same tumor mass
Additional references
Practice question #1
Which of the following is true about pulmonary adenosquamous carcinoma?
- Always shows both components in metastases
- Has a better prognosis than pure adenocarcinoma or squamous cell carcinoma
- May harbor EGFR or KRAS mutations
- Requires immunohistochemistry for diagnosis
- Shows a benign squamous component
Practice answer #1
C. May harbor EGFR or KRAS mutations. It is important to recognize pulmonary adenosquamous carcinoma, as these tumors may harbor targetable mutations seen in adenocarcinomas, such as EGFR or KRAS. Answer B is incorrect because pulmonary adenosquamous carcinoma has a worse prognosis than either adenocarcinoma or squamous carcinoma. Answer A is incorrect because only 1 of the 2 components may be seen in metastatic sites. Answer D is incorrect because the diagnosis is made with at least 10% of each component by histology, not immunohistochemistry. Answer E is incorrect because both the adenocarcinoma and squamous cell carcinoma components are malignant.
Comment Here
Reference: Adenosquamous carcinoma
Comment Here
Reference: Adenosquamous carcinoma
Practice question #2
Which of the following statements regarding lung adenosquamous carcinoma is accurate?
- Always benign and does not exhibit metastatic potential
- Characterized by a glandular and squamous differentiation
- Commonly presents as a purely neuroendocrine tumor
- Exclusively composed of squamous cell carcinoma elements
- Primarily affects the bronchial cartilage and not the epithelial cells
Practice answer #2
B. Characterized by a glandular and squamous differentiation. Lung adenosquamous carcinoma is a subtype of non-small cell lung cancer (NSCLC) that contains both glandular (adenocarcinoma) and squamous (squamous cell carcinoma) differentiation. This histological pattern differentiates it from other types of lung cancer. Answer A is incorrect because adenosquamous carcinoma is, by definition, a malignant neoplasm. Answer C is incorrect because adenosquamous carcinoma cells are not neuroendocrine in origin. Neuroendocrine neoplasms are a separate entity from lung neoplasms with different morphology, clinical presentations and immunohistochemical profile. Answer D is incorrect because by definition, adenosquamous carcinomas must contain at least 10% components of both adenocarcinoma and squamous cell carcinoma by histomorphology. Answer E is incorrect because this entity arises from the epithelium of the lung.
Comment Here
Reference: Adenosquamous carcinoma
Comment Here
Reference: Adenosquamous carcinoma
Practice question #3
Which of the following clinical features is commonly associated with lung adenosquamous carcinoma?
- Limited association with smoking history
- Overexpression of the ALK gene fusion
- Paraneoplastic production of PTH related peptide
- Peripheral, cavitary lesions on chest imaging
- Strong female predominance among affected patients
Practice answer #3
D. Peripheral, cavitary lesions on chest imaging. Lung adenosquamous carcinoma often presents with peripheral cavitary lesions on chest Xray, which can be a distinguishing feature. This radiological appearance may be indicative of necrotic or cavitated areas within the tumor. Answers A, B, C and E are incorrect because they are not commonly associated with lung adenosquamous carcinoma.
Comment Here
Reference: Adenosquamous carcinoma
Comment Here
Reference: Adenosquamous carcinoma