Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Diagnosis | Radiology description | Case reports | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Benzerdjeb N. Mesothelial hyperplasia (peritoneum). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pleuraperitmesothelialhyper.html. Accessed October 3rd, 2025.
Definition / general
- Reactive proliferation of mesothelial cells with no or minimal cytologic atypia and without invasion
Essential features
- Common response to inflammation occurring in any process that leads to irritation of peritoneal surface
- Reactive proliferation of mesothelial cells with minor degrees of nuclear atypia
- Without invasion, positive for mesothelial markers (CK5/6, calretinin and WT1)
- BAP1 and MTAP retained
Terminology
- Simple mesothelial hyperplasia
- Florid mesothelial peritoneal hyperplasia
Epidemiology
- Exact incidence is unknown but mesothelial cell hyperplasia is not an uncommon phenomenon
- May occur at any age, whatever the sex (J Clin Pathol 2011;64:313)
Sites
- May occur at any site of the peritoneum
Pathophysiology
- Common response to inflammation occurring in any process that leads to irritation of peritoneal surface
Etiology
- Chronic effusions (ascites)
- Inflammatory processes
- Endometriosis
- Hernias
- Neoplasms (e.g. ovarian tumor, colorectal tumor)
- Reference: Int J Gynecol Pathol 2014;33:393
Diagnosis
- Exploratory laparoscopy with tissue sampling
- Often incidentally identified in peritoneal tissue obtained for other purposes
Radiology description
- No gross evidence of disease on imaging
Case reports
- 32 year old woman with a left ovarian microinvasive serous borderline tumor (Eur J Gynaecol Oncol 2004;25:236)
- 35, 53 and 59 year old women with tubal ectopic pregnancy, ovarian serous cystadenoma and ovarian adenosquamous carcinoma, respectively (Histopathology 2013;63:598)
- 36 and 37 year old women with dysmenorrhea and secondary infertility and endometriosis, respectively (Ann Diagn Pathol 2004;8:115)
Gross description
- Not commonly visible upon gross examination (incidental findings on microscopic examination)
- Occasionally observed as small nodules or flat plaques from the peritoneum (Int J Gynecol Pathol 2014;33:393)
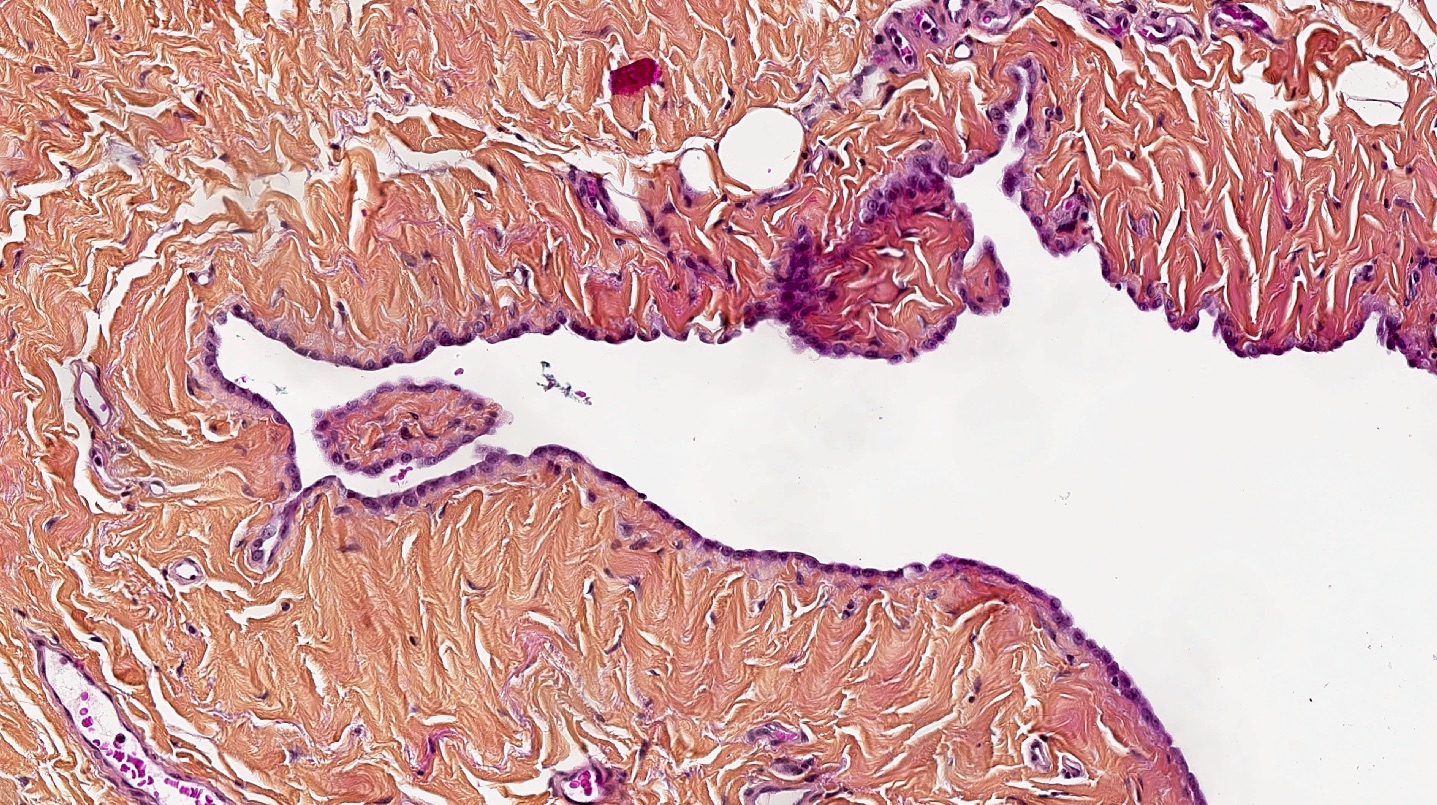
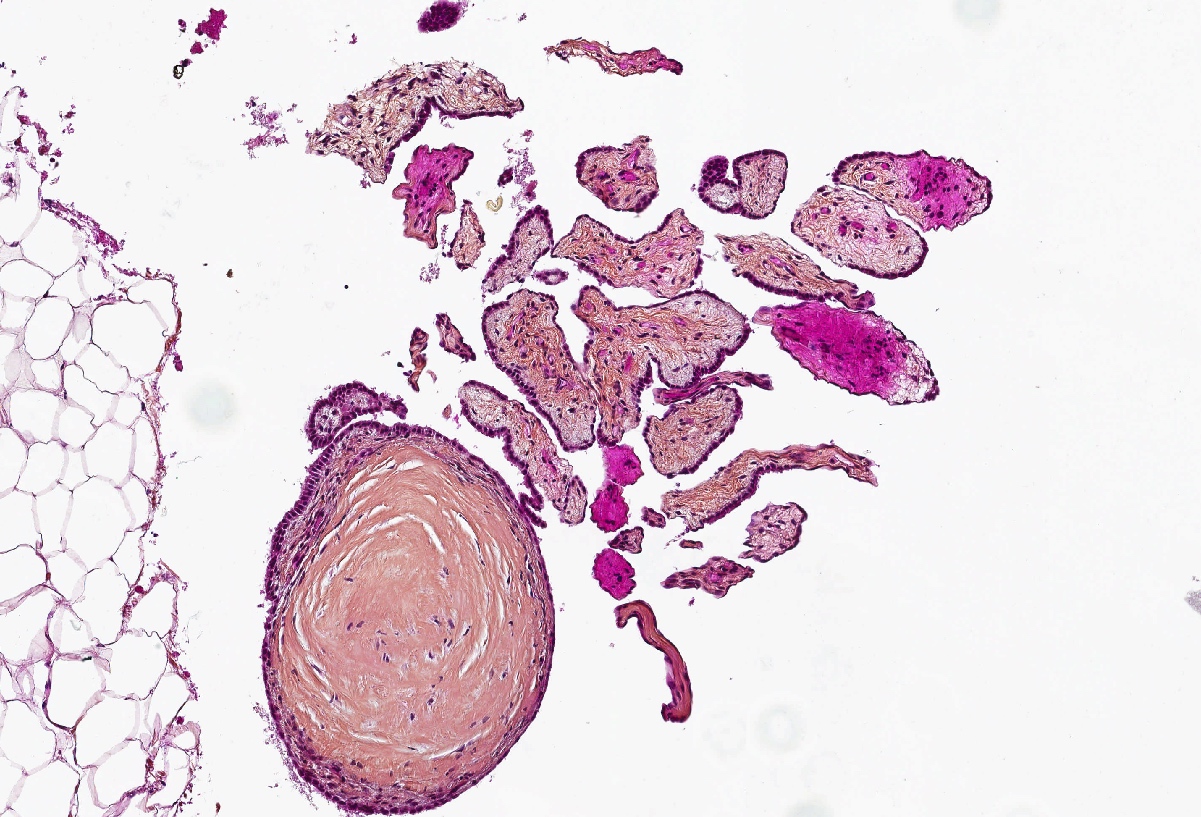
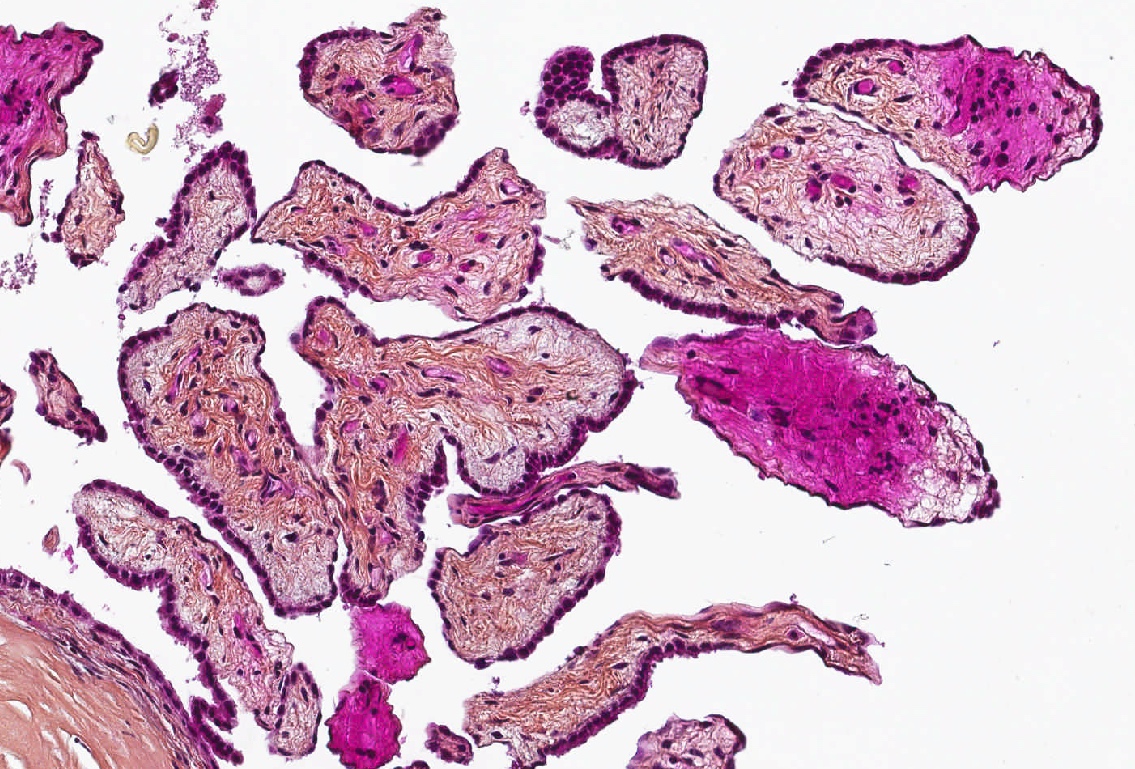
Microscopic (histologic) description
- Variety of architectural patterns (solid sheets, nests, discrete small papillary or tubulopapillary growths, gland-like structures, cord-like linear arrays or single cells) (Int J Gynecol Pathol 2014;33:393)
- Minor degrees of nuclear atypia (small, regular, round or oval and exhibit central nucleoli) without invasion; more common to be uniform in appearance
- Reactive changes may be present that are worrisome for malignancy (enlarged vesicular nuclei, multinucleation, conspicuous nucleoli and rare mitotic figures)
- Usually accompanied with inflammatory cells
- Sometimes florid mesothelial peritoneal hyperplasia or psammoma bodies may be seen (Int J Gynecol Pathol 1993;12:51)
- Rare findings:
- Eosinophilic strap-like cells resembling rhabdomyoblasts (Cancer 1975;35:165)
- Deciduoid morphology with glassy eosinophilic cytoplasm (Histopathology 2013;63:598)
Microscopic (histologic) images
Cytology description
- Usually mesothelial cells may be numerous or not, dispersed or present in small clusters
- Binucleation, multinucleation, mitosis, prominent nucleolus can be present in benign proliferations (Cytojournal 2013;10:7)
- 2 or more mesothelial cells are often separated by window or a narrow space (Cytopathology 2004;15:131)
- Benign mesothelial cells usually have recognizable halo at outer rim of cell
- Complex papillary or branching clusters should not be present (Cytojournal 2013;10:7)
Positive stains
- Positive immunostains in mesothelial cells (CK AE1 / AE3, CK7, CK5/6, calretinin, WT1, D2-40)
- Reported positivity for desmin but nonspecific (more common in reactive mesothelial cells [84%] than mesothelioma [8%] or carcinoma [2%]) (Am J Surg Pathol 2001;25:1405)
- BAP1 and MTAP are retained (positive)
Negative stains
Molecular / cytogenetics description
- FISH for CDKN2A: intact
Videos
Mesothelial proliferations
Sample pathology report
- Peritoneal biopsy:
- Mesothelial hyperplasia of the peritoneum (see comment)
- Comment: There are small papillary structures containing myxoid stroma, which are lined by a single layer of uniform cuboidal mesothelial cells without any infiltrative cells or necrosis. Immunohistochemically, the mesothelial cells are positive for calretinin and WT1. BAP1 and MTAP are retained.
Differential diagnosis
- Mesothelioma:
- Generally, diffuse involvement of the peritoneum
- Infiltration of underlying pre-existing tissue is classical
- At least moderate cytologic atypia in most cases
- Solid architecture may be present
- BAP1 loss by immunostaining or CDKN2A homozygous loss is required for diagnosis (Virchows Arch 2021;478:59)
- Mesothelioma in situ:
- Similar morphology
- BAP1 loss by immunostaining or CDKN2A homozygous loss is required for diagnosis (Virchows Arch 2021;478:59)
- Well differentiated papillary mesothelioma:
- Papillae larger with myxoid cores, each lined by a single mesothelial cell layer
- Invasion is rarely observed (Am J Surg Pathol 2014;38:990)
- Recurrent mutations in TRAF7 or CDC42 (Mod Pathol 2019;32:88)
- Found by positive L1CAM immunostain
- Adenomatoid tumor:
- Organized in vascular-like, gland-like, complex slit-like and cystic branching spaces; also tubules or combination of above
- Positive immunostain for L1CAM
- Sertoli cell tumor:
- Usually well circumscribed
- Different architecture to reactive mesothelial proliferations: often mixed patterns of tubular, cords, macro or microcystic, nested, trabecular, whorled, solid, retiform, pseudopapillary
- Often presence of cells with cytoplasmic vacuoles
- Metastatic carcinoma:
- Negative for calretinin
- Positive for claudin4, MOC31, BerEP4 and other epithelial lineage markers
Additional references
Practice question #1
Which of the following statements regarding mesothelial hyperplasia of the peritoneum is true?
- Approximately 10% of patients progress to malignant mesothelioma over 10 years
- BAP1 immunostain can be lost
- Common response to inflammation occurring in any process that leads to irritation of peritoneal surface
- Lesions harbor consistently mutation of TRAF7
- Psammoma bodies are never seen
Practice answer #1
C. Common response to inflammation occurring in any process that leads to irritation of peritoneal surface
Comment Here
Reference: Mesothelial hyperplasia
Comment Here
Reference: Mesothelial hyperplasia
Practice question #2
A small focal nodule depicted in the above photomicrograph was found incidentally during a resection of an ovarian serous cystadenoma in a 26 year old woman. Lesional cells were positive for calretinin. Which of the following is true about the depicted entity?
- CDKN2A homozygous deletion is never seen
- Deciduoid morphology can be occasionally seen
- Immunohistochemical loss of BAP1 is seen in 10% of cases
- Lesions harbor consistently mutation of TRAF7
- Most cases are causally linked to asbestos exposure
Practice answer #2
A. CDKN2A homozygous deletion is never seen. This is a peritoneal mesothelial hyperplasia.
Comment Here
Reference: Mesothelial hyperplasia
Comment Here
Reference: Mesothelial hyperplasia