Table of Contents
Definition / general | Essential features | Embryology | Anatomy | Physiology | Diagrams / tables | Clinical implications | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Videos | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Haralabopoulos T, Clark J, Gupta R. Anatomy & histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsnormalhistology.html. Accessed September 14th, 2025.
Definition / general
- 3 paired major salivary glands:
- Parotid glands
- Submandibular glands
- Sublingual glands
- In addition, there are numerous (600 - 1000) minor salivary glands distributed throughout the submucosa of the upper aerodigestive tract
Essential features
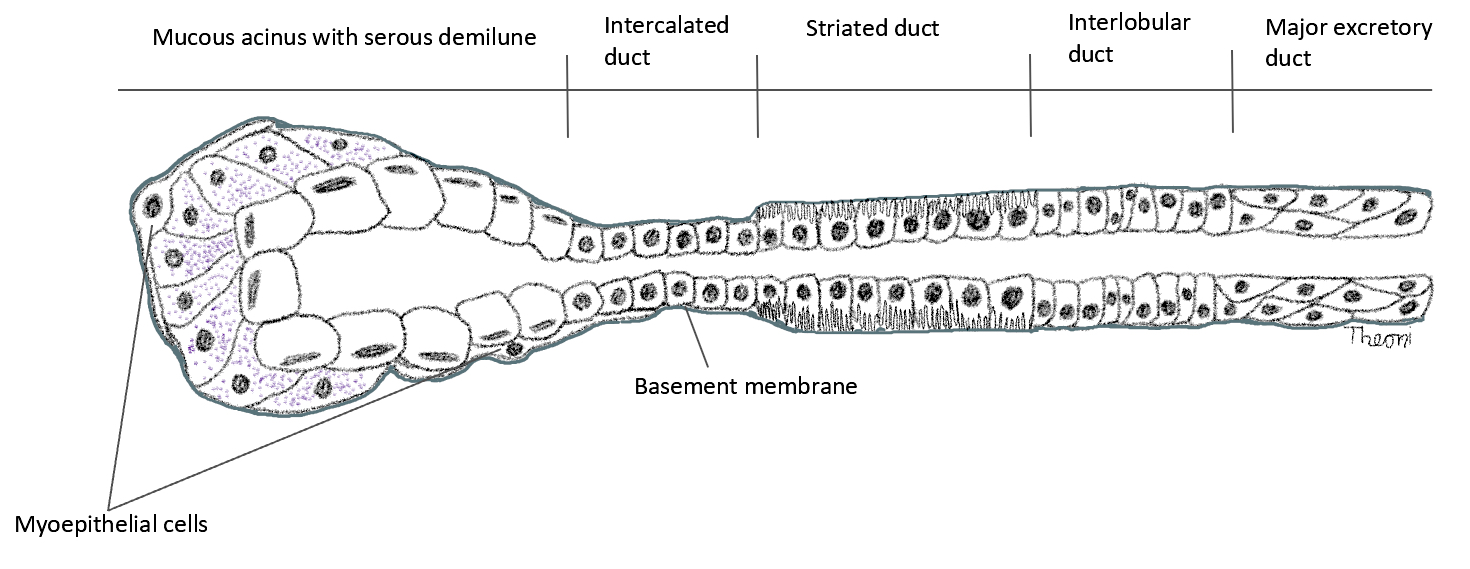
- Functional unit of all salivary glands consists of acini and ducts
- Acini can be composed predominantly of serous or mucous cells or can be mixed seromucous type
- 3 main types of ducts are intercalated, striated or interlobular
- Myoepithelial cells embrace the secretory unit and are critical for the expulsion of saliva
- Saliva has a crucial protective and digestive function within the upper aerodigestive cavity, providing mucosal lubrication, alkaline environment for dental protection, facilitating taste, initiating enzymatic digestion of carbohydrates and contributing to oral immunity
- Unique to the parotid gland is the presence of sebaceous glands and intraparenchymal lymph nodes
Embryology
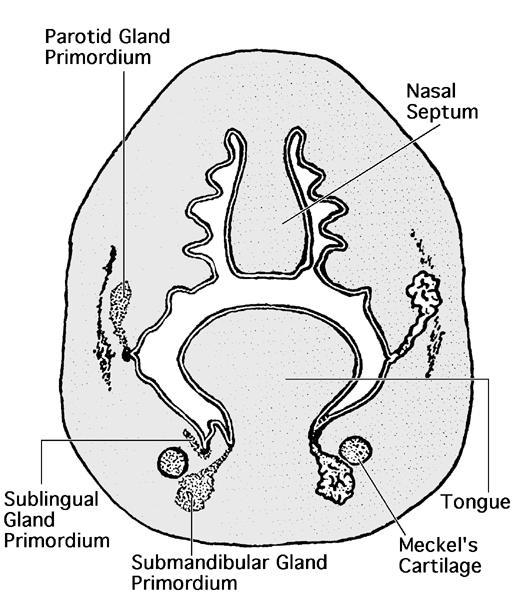
- Salivary glands are of ectodermal origin
- Developmental process begins when preacinar buds invaginate the adjacent mesenchyme, proliferating through cords, which eventually form clefts and produce extensive branching; end result is terminal bulbs, which form the secretory unit (Eur J Mol Clin Med 2020;764)
- Parotid anlage appears in the fifth week, followed by the submandibular and sublingual primordia in the sixth and eighth weeks, respectively
- Minor salivary glands develop during ninth to twelfth weeks
- Connective tissue component of the developing glands progressively lessens with maturation
- Capsule of each gland is formed by the surrounding mesenchyme, a process which is delayed for the parotid gland, therefore allowing the integration of parotid buds and lymphoid tissue:
- Results in the presence of both intraparotid lymph nodes as well as lymph nodes containing glandular and ductal inclusions
- As the parotid gland forms, its embryologic branches intertwine with branches of the facial nerve
- Minor salivary glands develop in a similar fashion to the major glands; however, the branching is less extensive and remains located within the submucosa
Anatomy
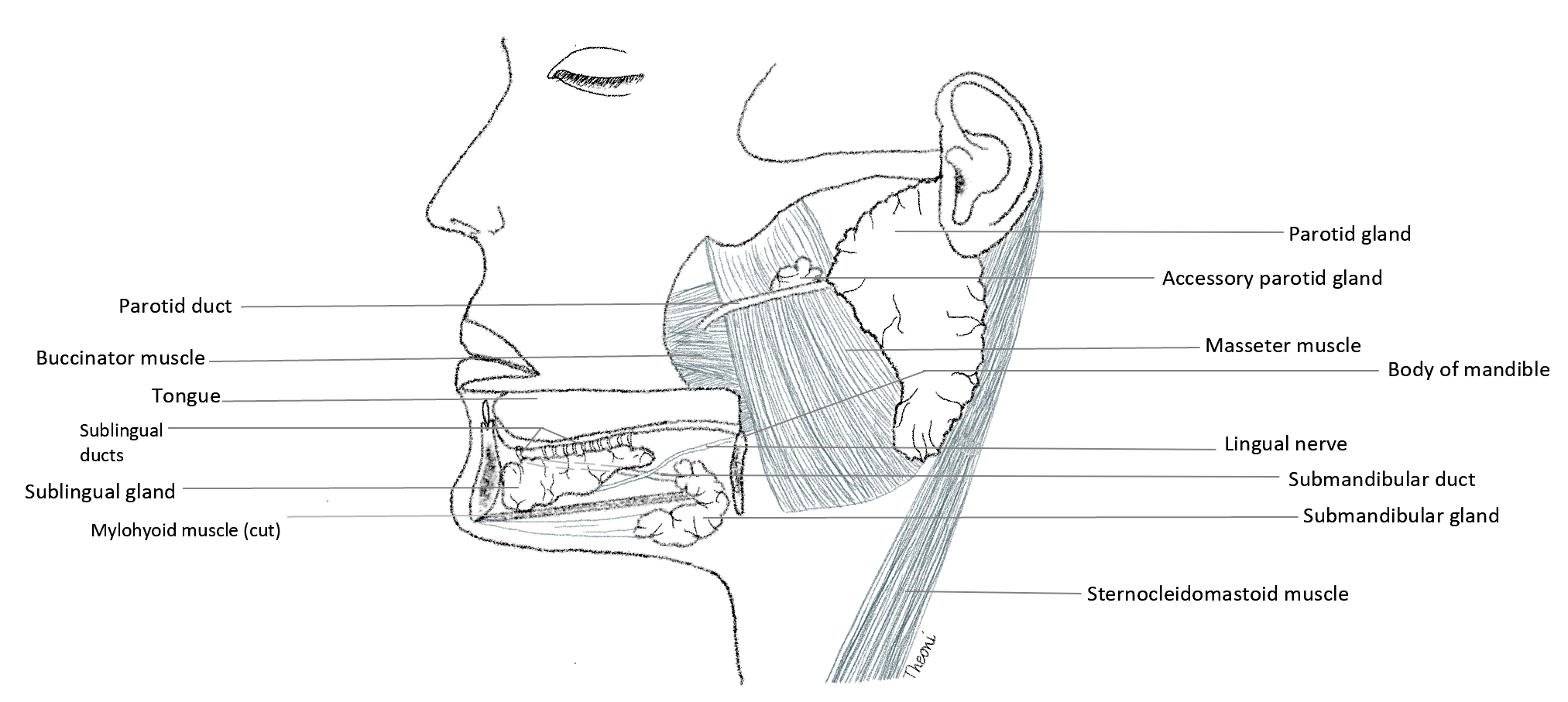
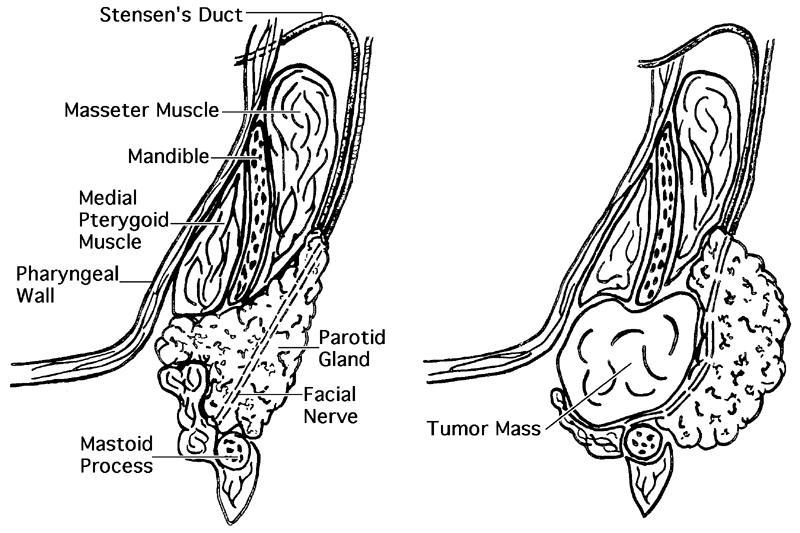
- Parotid gland:
- Largest of the major salivary glands (weight 15 - 30 g)
- Pyramidal shaped and encased in robust parotid fascia, which is a continuation of deep cervical fascia as it travels superiorly
- Located in a shallow, preauricular compartment defined by:
- Superficially: the superficial musculoaponeurotic system (SMAS) forming parotid fascia and platysma
- Inferiorly: the sternocleidomastoid muscle
- Medially: the parapharyngeal space
- Anteromedially: the mandibular ramus covered by the masseter muscle
- Posteriorly: the cartilage of the ear canal and temporal bone
- Extracranial trunk of the facial nerve extends from the stylomastoid foramen into the parotid gland and divides into upper and lower division
- Branches of the facial nerve traverse the body of the parotid gland to artificially divide the gland into superficial and deep lobes and exit in the form of 5 terminal branches from its anteromedial surface to supply 22 muscles of facial expression
- Parotidectomy requires precise dissection of the parotid gland to identify and preserve the integrity of the facial nerve, preventing ipsilateral hemifacial paralysis
- Stensen duct (~7 cm) is the main excretory duct of the parotid gland and emerges from the anterior border of the gland to travel horizontally along the superficial surface of the masseter muscle before turning medially to pierce the buccinator muscle and enter the oral cavity adjacent to the second maxillary molar
- Accessory parotid tissue, usually adjacent to Stensen duct, can be identified in approximately 20% of individuals (Otolaryngol Clin North Am 2016;49:273)
- Clinically important as salivary gland tumors can arise in this location
- Submandibular gland:
- Second largest of the major salivary glands (weight 7 - 15 g)
- Hook shaped around the mylohyoid muscle and enveloped by a capsule continuous with the superficial layer of the deep cervical fascia
- Divided into superficial and deep arms
- Superficial (largest) portion lies outside the oral cavity below the mylohyoid muscle in the submandibular triangle bound by:
- Superficial: platysma
- Superior: mandible
- Inferior: digastric muscle
- Deep portion is formed as the gland curves around the posterior border of the mylohyoid muscle to enter the oral cavity
- Superficial (largest) portion lies outside the oral cavity below the mylohyoid muscle in the submandibular triangle bound by:
- Wharton duct (~5 cm) is the main excretory duct of the submandibular gland, arises from the deep part of the gland, courses anteriorly and opens onto the sublingual caruncle adjacent to the frenulum of the tongue
- Lingual nerve crosses Wharton duct twice lateral to medial and the hypoglossal nerve (CN XII) travels inferior to the duct (Folia Morphol (Warsz) 2018;77:521)
- Vertical posterior edge of the submandibular gland and the digastric muscle can be used as a boundary between levels I and II of the neck (Arch Otolaryngol Head Neck Surg 2008;134:536)
- Sublingual gland:
- Smallest of the major salivary glands (weight 2 - 4 g)
- Almond shaped and enveloped by loose connective tissue (no discrete capsule)
- Located above the mylohyoid muscle lateral to the submandibular duct and lingual nerve
- Fills the medial groove or sublingual fossa of the mandible
- Superiorly, the gland creates a mucosal elevation (sublingual fold) on the floor of the oral cavity
- There may be multiple minor sublingual ducts, also known as ducts of Rivinus, opening directly onto the crest of the sublingual fold; these may be replaced anteriorly by the major sublingual duct (Bartholin duct), which may connect with the submandibular duct at the sublingual caruncle
- Minor salivary glands:
- Scattered throughout the oral submucosa, with the exception of the gingiva and anterior hard palate
- Not encapsulated and each gland possesses 1 duct draining directly into the oral cavity
- Predominantly mucinous apart from the purely serous von Ebner glands of the dorsal tongue that surround the circumvallate papillae
- Vasculature:
- Arterial supply
- External carotid artery supplies the major salivary glands, coursing superiorly from the carotid bifurcation and providing the facial and lingual arteries that supply the submandibular and sublingual glands
- Facial artery is intimately associated with the submandibular gland and is routinely divided above and below the submandibular gland during its removal as there are numerous branches
- External carotid artery arrives at the posteromedial surface of the parotid gland, dividing into 2 terminal branches, the superficial temporal artery and maxillary artery, which exit from superior and anteromedial surfaces, respectively
- Superficial temporal artery provides the transverse facial artery, which travels anteriorly to supply the parotid gland and parotid duct
- External carotid artery supplies the major salivary glands, coursing superiorly from the carotid bifurcation and providing the facial and lingual arteries that supply the submandibular and sublingual glands
- Venous outflow
- Retromandibular vein is formed in the body of the parotid gland by the union of the superficial temporal and maxillary veins and provides venous return for the gland, descending superficial to the external carotid artery and deep to the facial nerve before eventually joining the external jugular vein
- Retromandibular vein is intimately associated with the facial nerve and is used as a surrogate anatomic landmark to determine whether tumors are in the deep or superficial lobe of the parotid gland
- Lingual and facial veins drain the submandibular and sublingual glands and flow into the internal jugular vein
- Facial vein lies over the submandibular gland and needs to be ligated to access the gland during surgery
- Venous anatomy can be variable
- Retromandibular vein is formed in the body of the parotid gland by the union of the superficial temporal and maxillary veins and provides venous return for the gland, descending superficial to the external carotid artery and deep to the facial nerve before eventually joining the external jugular vein
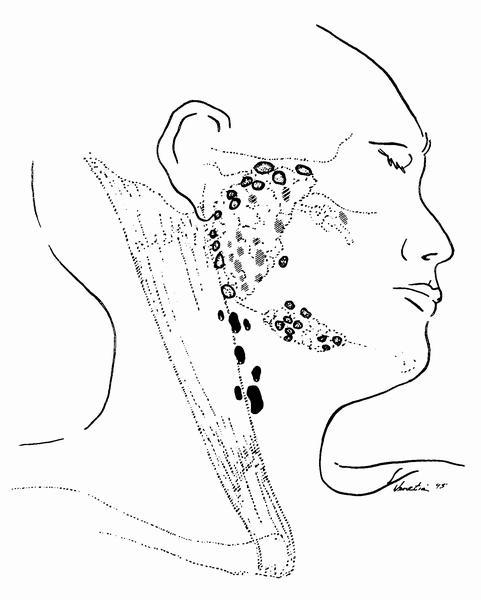
- Lymphatic drainage
- Lymphatic drainage of the parotid gland follows the venous system, draining to a superficial (fascial) and deep (intraparenchymal) group of lymph nodes before flowing into the superior deep cervical nodes
- Lymphatic drainage of the submandibular and sublingual glands is received predominantly by the submandibular lymph nodes before progressing to the jugular chain
- Arterial supply
- Innervation:
- Both parasympathetic and sympathetic fibers innervate the salivary glands
- Parasympathetic syndromes cause salivation
- Sympathetic syndromes, anxiety cause dry mouth
- Within the oral cavity, parasympathetic innervation to salivary glands is by the facial nerve (VII), branches of which join the maxillary (V2) and mandibular (V3) nerves
- Parasympathetic fibers conveyed by the chorda tympani branch of the facial nerve (VII) innervate the submandibular and sublingual glands via the lingual nerve
- Chorda tympani nerve unites with the lingual nerve of V3 in the infratemporal fossa before entering the oral cavity to synapse with postganglionic fibers in the submandibular ganglion
- Submandibular ganglion is suspended from the lingual nerve and located inferior to the submandibular duct, supplying postganglionic parasympathetic fibers that pass directly to the submandibular and sublingual glands
- Branches from lingual nerve to the submandibular gland are ligated during gland excision
- Beyond the oral cavity, the parotid gland receives parasympathetic innervation by the auriculotemporal nerve (branch of the mandibular nerve [V3]), a nerve which derives its fibers from the glossopharyngeal nerve (IX) in the infratemporal fossa
- Delayed complication of parotid surgery is Frey syndrome, characterized by gustatory sweating
- Postganglionic sympathetic fibers branch from the carotid plexus of the external carotid artery and innervate the salivary glands along blood vessels
- Both parasympathetic and sympathetic fibers innervate the salivary glands
Physiology
- Saliva has a crucial protective and digestive function within the upper aerodigestive cavity, providing mucosal lubrication and dental protection, facilitating taste, initiating enzymatic digestion of carbohydrates and contributing to oral immunity
- Saliva synthesizing acinar cells are capable of producing a volume of up to 1.5 L daily, secreted in response to parasympathetic and sympathetic stimulation
- Parasympathetic activity favors the production of serous or watery solution
- Sympathetic activity triggers protein secretion
- Parotid glands are responsible for up to 50% of saliva production upon stimulation (J Med Life 2009;2:303)
- Saliva primarily contains the enzymes amylase and lysozyme, IgA and IgG antibodies, inorganic ions and a variable quantity of mucous
- Serous and mucous cells of the salivary glands contribute to the composition of saliva and the striated ducts perform critical modification processes, specifically electrolyte reabsorption and secretion
- Initially isotonic, saliva becomes a hypotonic, bicarbonate rich solution as it passes through the mitochondria packed striated ducts that facilitate ion transport
Diagrams / tables
Contributed by Theoni Haralabopoulos, M.D. and AFIP
Images hosted on other servers:
Clinical implications
- Each cellular component can give rise to benign and malignant lesions that may present as swellings, with or without associated discomfort or pain
- Salivary gland inflammation (sialadenitis) manifests as lymphoid infiltration and destruction of serous and mucinous acini, leading to pain, swelling and dry mouth; this can be secondary to
- Bacterial or viral infection
- Autoimmune (e.g., Sjögren syndrome and IgG4 related disease)
- Impaction of calculi (sialolithiasis)
- Trauma
- Irradiation
- Dilatation of salivary gland ducts (sialectasis) may be associated with recurrent sialadenitis and typically presents as painful, diffuse parotid gland swelling
- Xerostomia following irradiation of the major or minor salivary gland tissues
- Neoplasms:
- Most (80%) of the salivary gland neoplasms arise in the parotid gland
- 80% of these are benign; on the other hand, most neoplasms of the sublingual gland are malignant
- Primary epithelial
- Pleomorphic adenoma, a benign, morphologically diverse tumor, displays both epithelial and myoepithelial derivation
- Most common (80%) salivary gland tumor
- Typically, the lesion presents as a slow growing, painless and mobile parotid mass (Wiad Lek 2020;73:2339)
- Warthin tumor, the second most frequent benign epithelial neoplasm, originates from heterotrophic salivary ducts present in intra or periparotid lymph nodes
- Dual morphological components of a lymphoid stroma and a bilayered, oncocytic epithelium that lines papillary and cystic structures
- Oncocytic epithelium rich in mitochondria is derived from the striated ducts
- This entity displays male predominance and usually presents as a symptomless, fluctuant parotid lump (J Clin Diagn Res 2014;8:ZD37)
- Mitochondria rich oncocytic epithelium can often appear PET avid
- Interlobular and intralobular salivary duct epithelium gives rise to the most common salivary gland malignancy, mucoepidermoid carcinoma, comprising mucinous, squamoid and intermediate cells arranged in a solid and cystic architecture
- Mucoepidermoid carcinoma predominantly presents as a solitary asymptomatic swelling within the parotid gland; pain and facial paralysis may occasionally occur (Adv Anat Pathol 2006;13:293)
- WHO classification system of salivary gland tumors includes nearly 30 other subtypes including adenoid cystic carcinoma, secretory carcinoma, epithelial myoepithelial carcinoma, salivary duct carcinoma and carcinoma ex pleomorphic adenoma
- Pleomorphic adenoma, a benign, morphologically diverse tumor, displays both epithelial and myoepithelial derivation
- Other neoplasms include lymphomas and metastatic malignancies from the skin and soft tissues of the scalp (squamous cell carcinoma, melanoma, angiosarcoma, pleomorphic dermal sarcoma); these are more likely to occur in the parotid gland due to the presence of native lymph nodes
- Malignancies of the parotid gland can involve the facial nerve as the nerve passes through the gland
- Minor salivary gland neoplasms generally manifest as submucosal nodules
- Most (80%) of the salivary gland neoplasms arise in the parotid gland
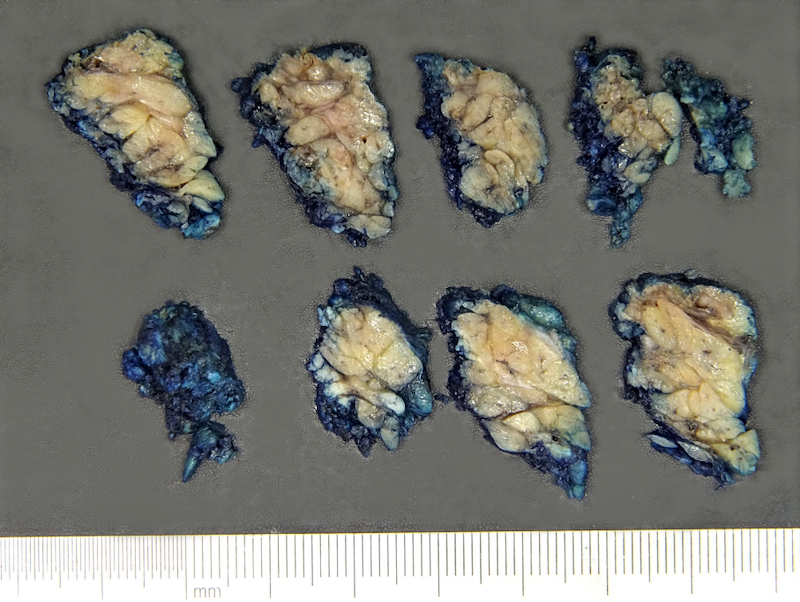
Gross description
- See Anatomy
Gross images
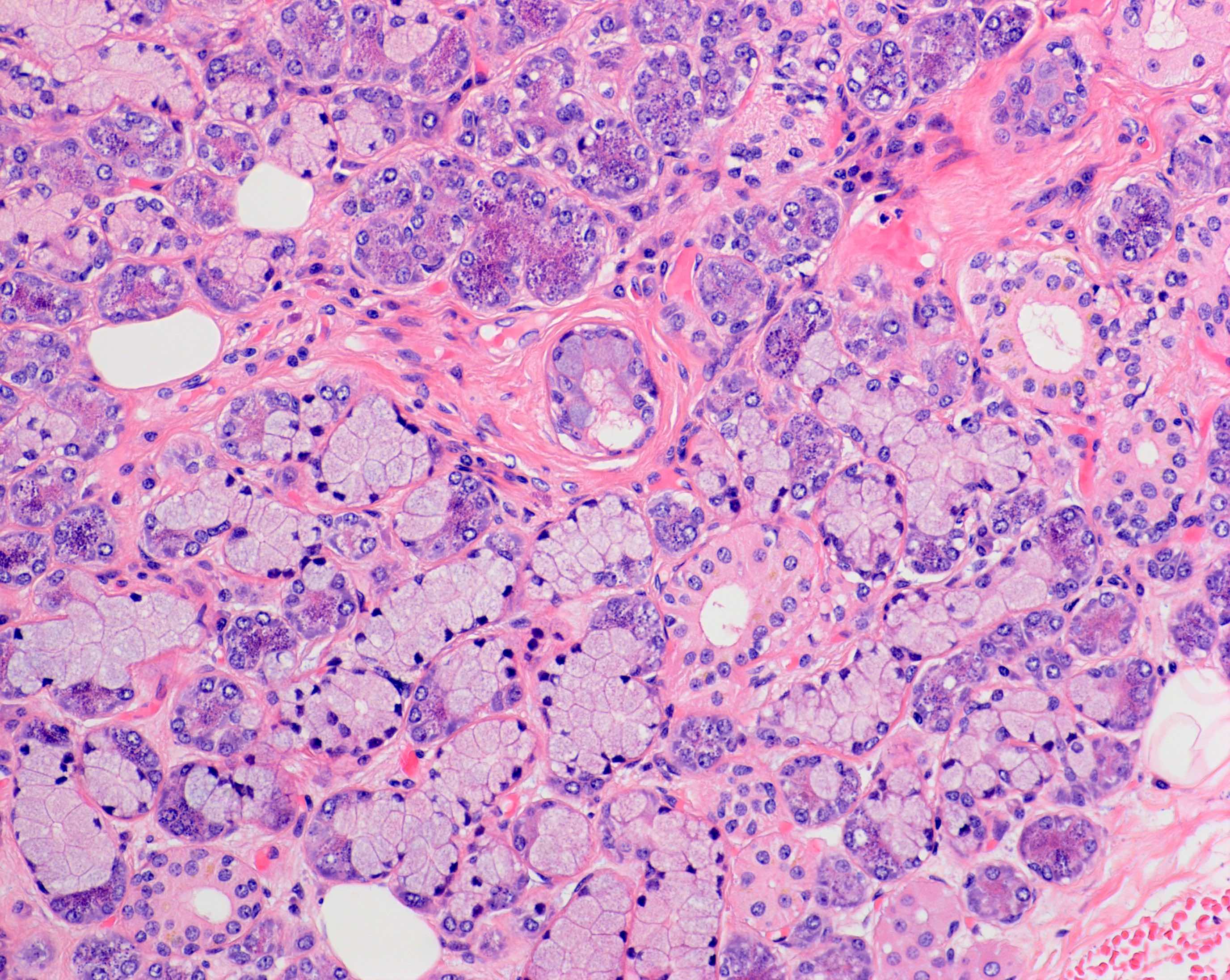
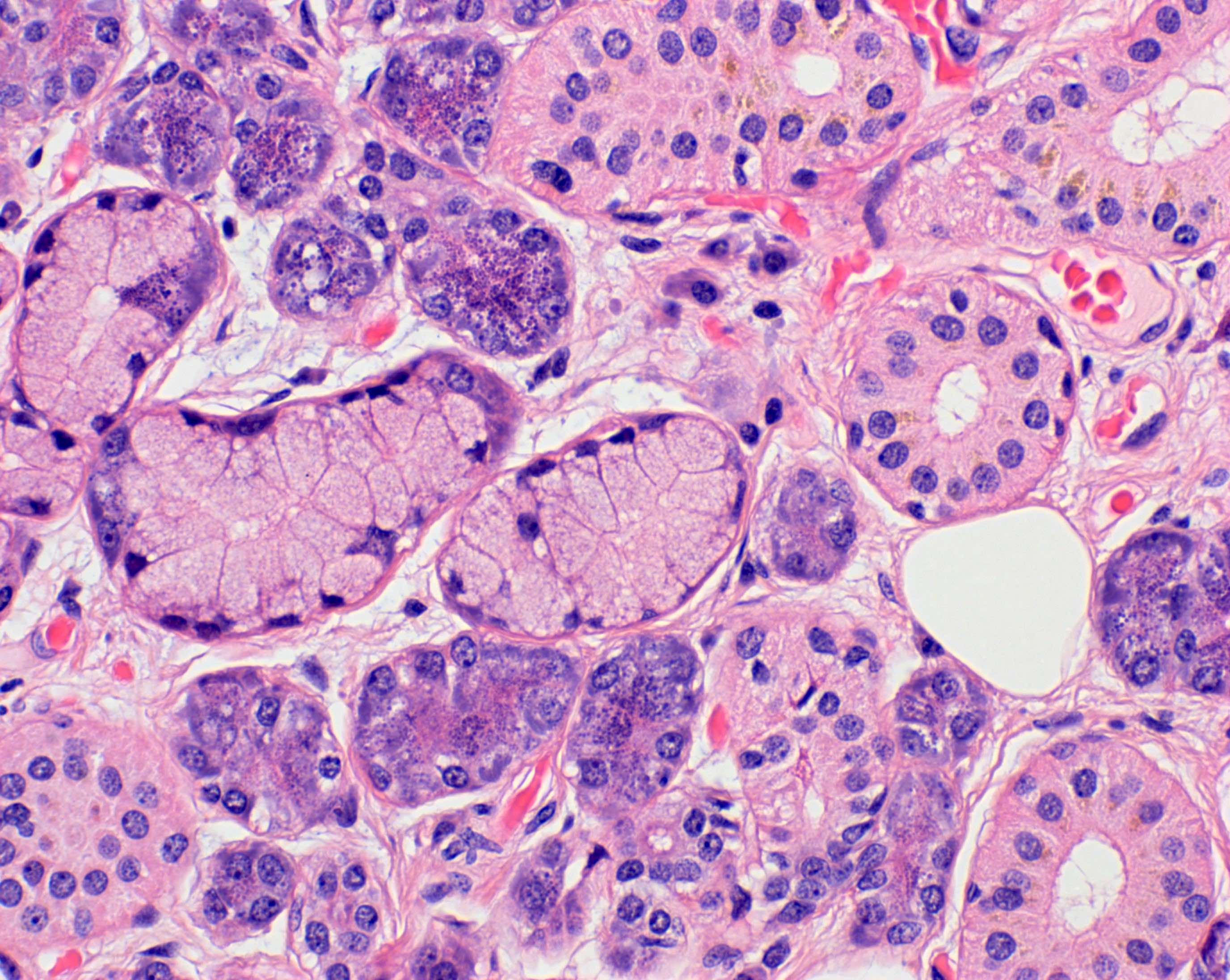
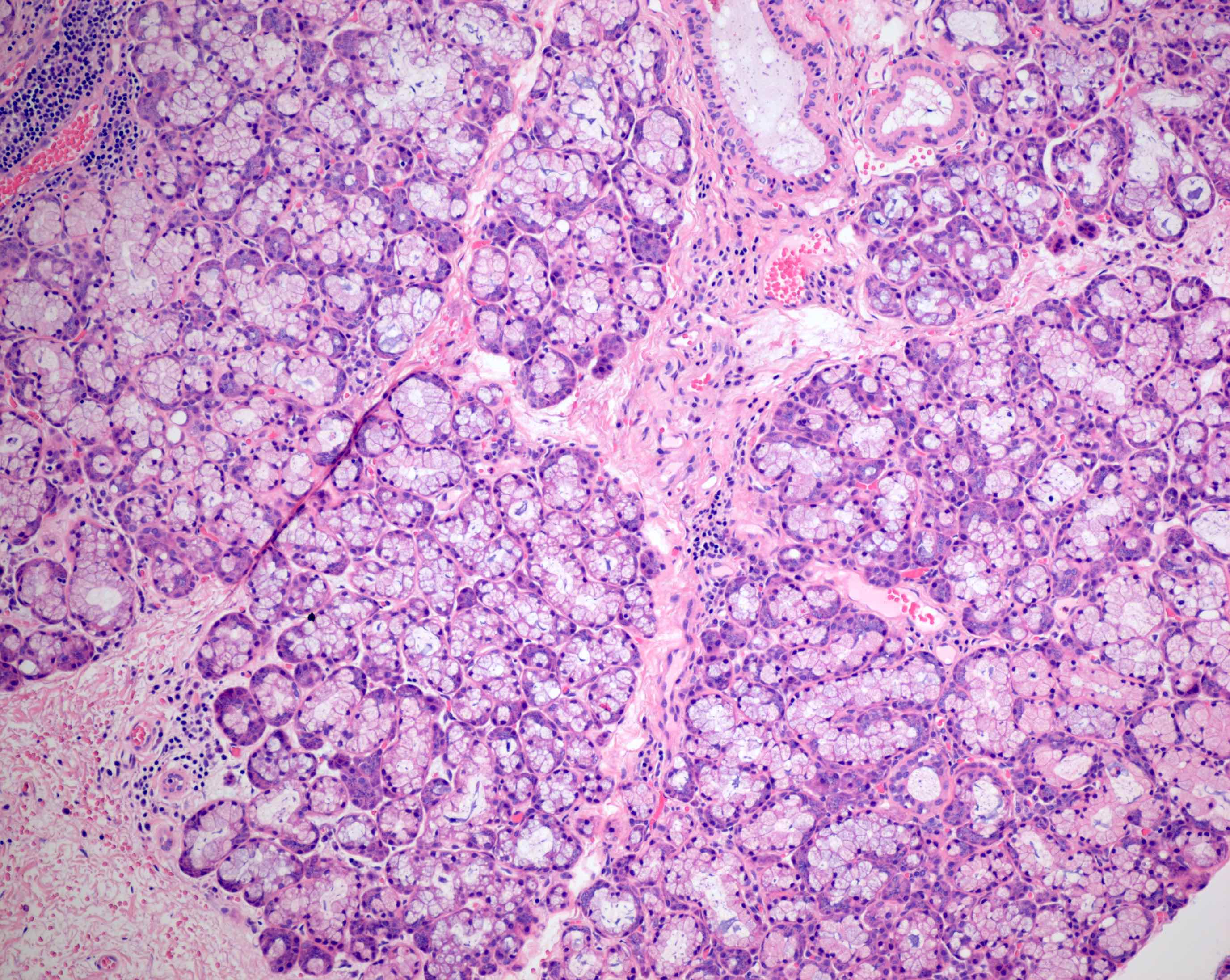
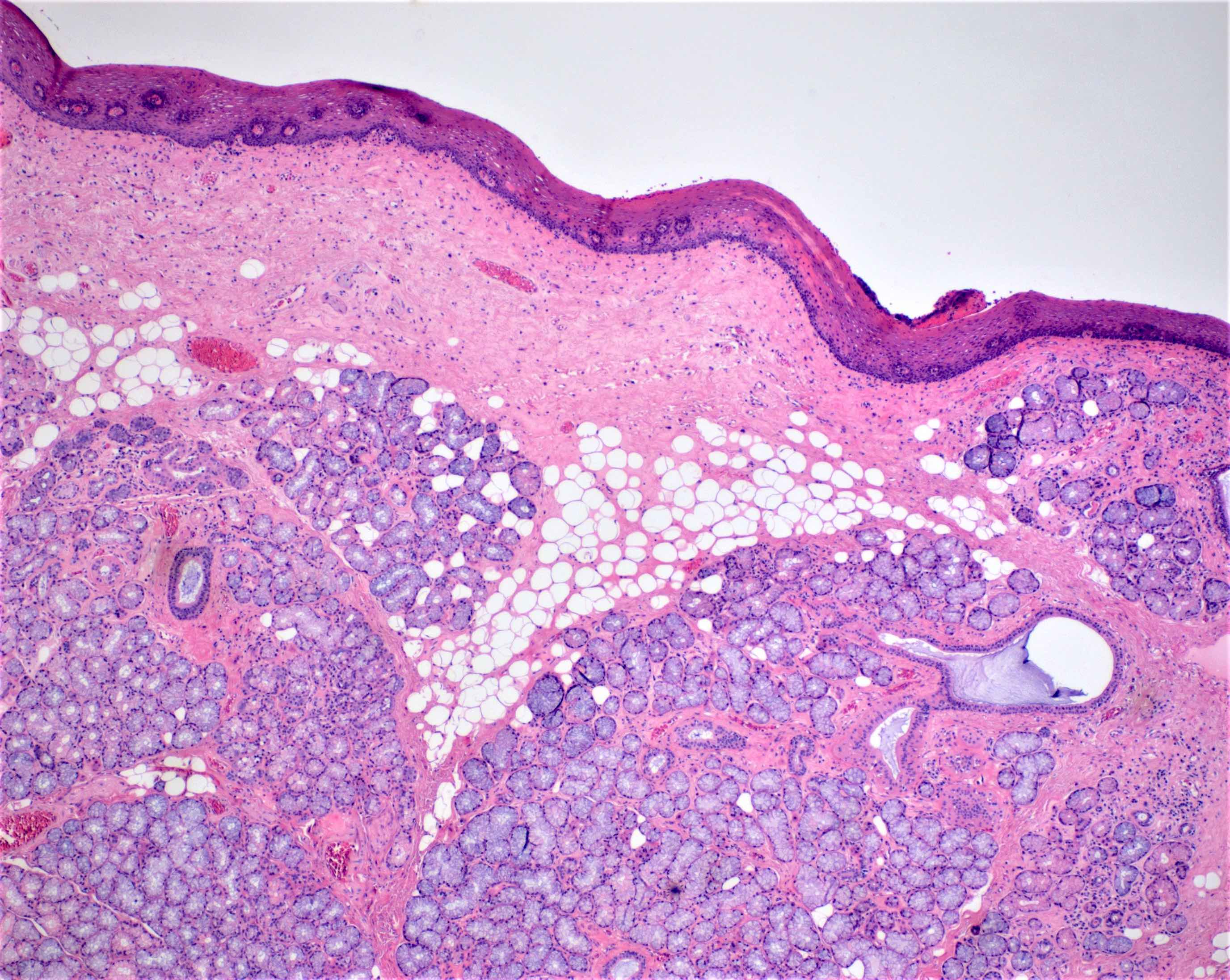
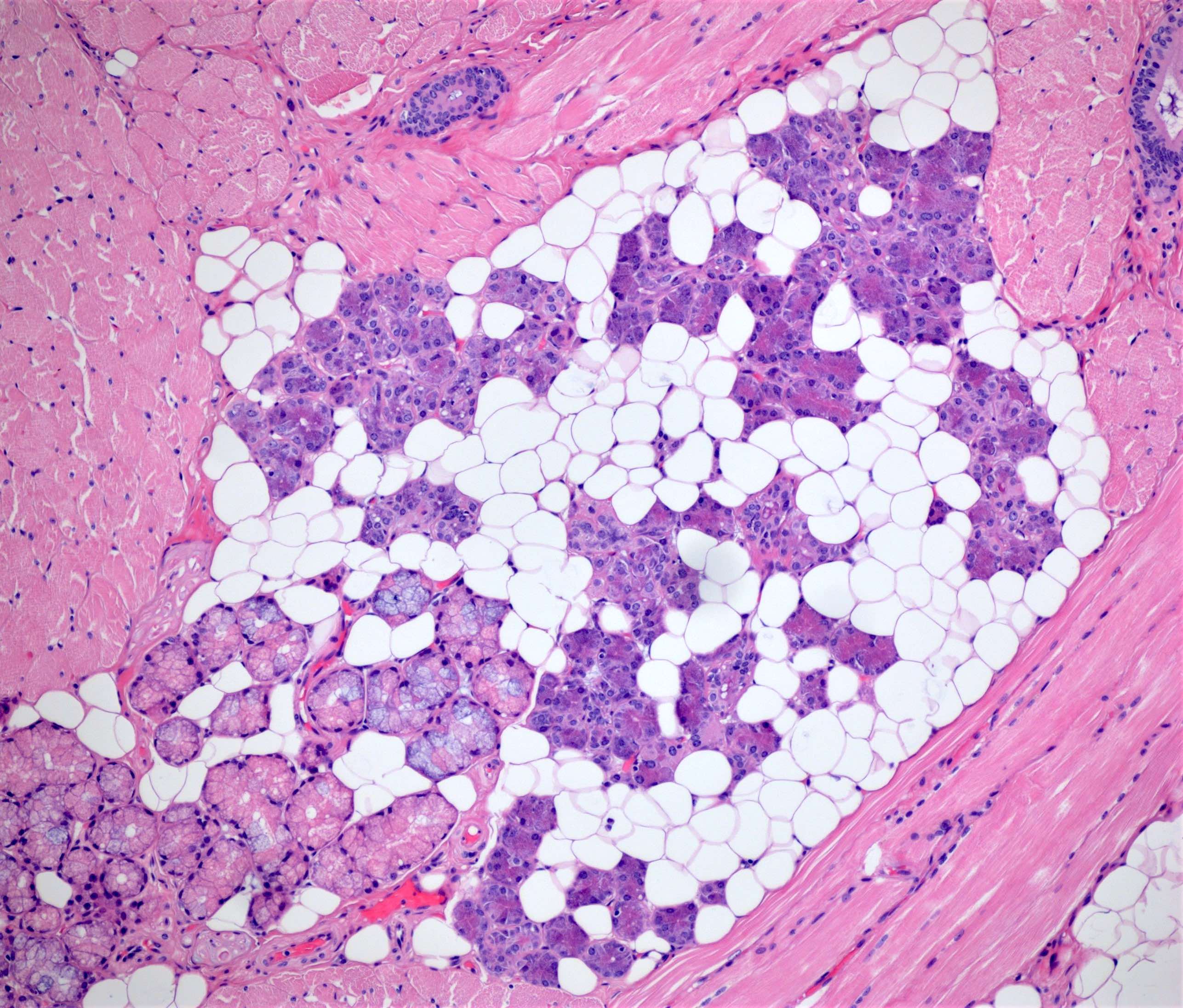
Microscopic (histologic) description
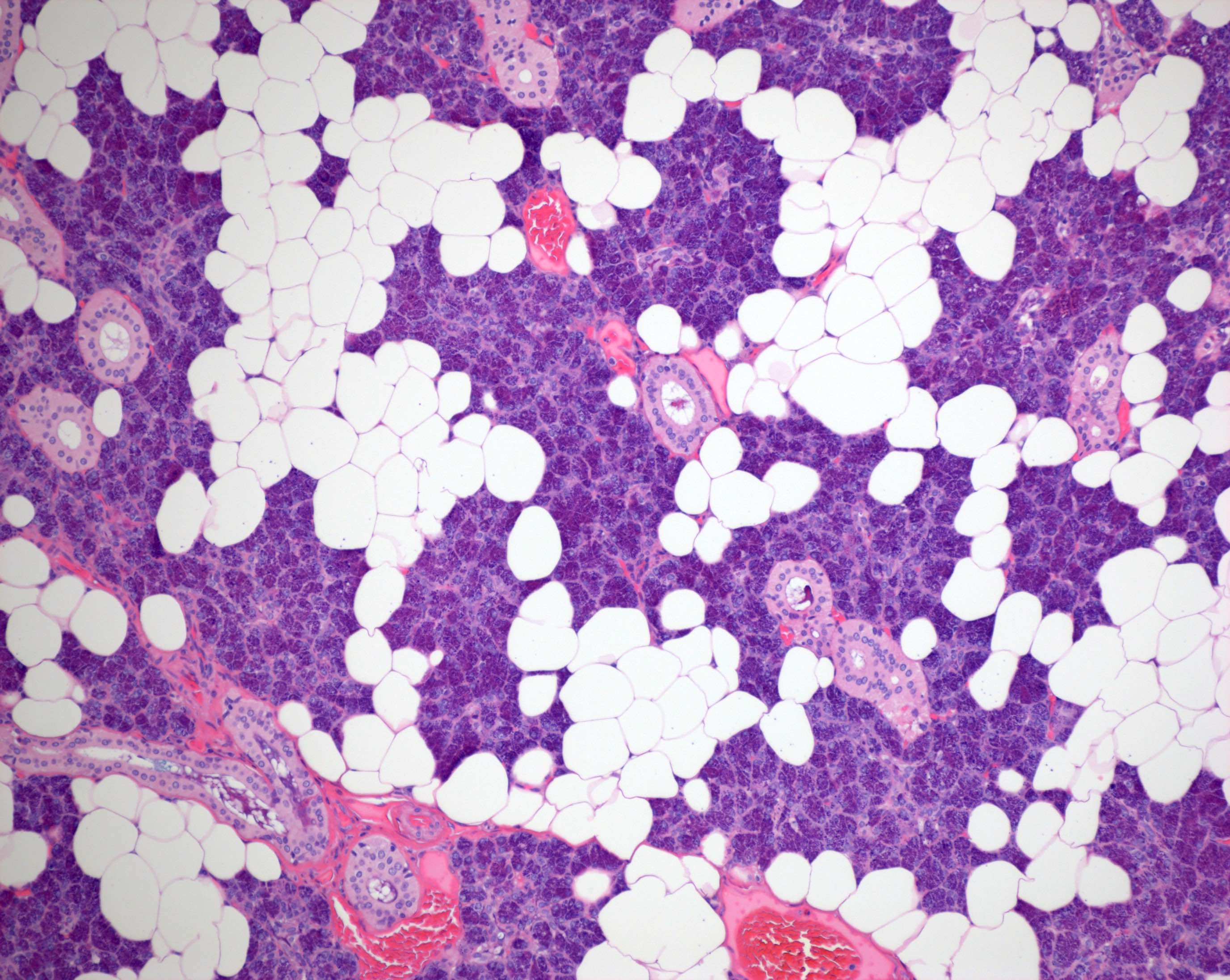
- Functional unit of all salivary glands consists of acini and ducts
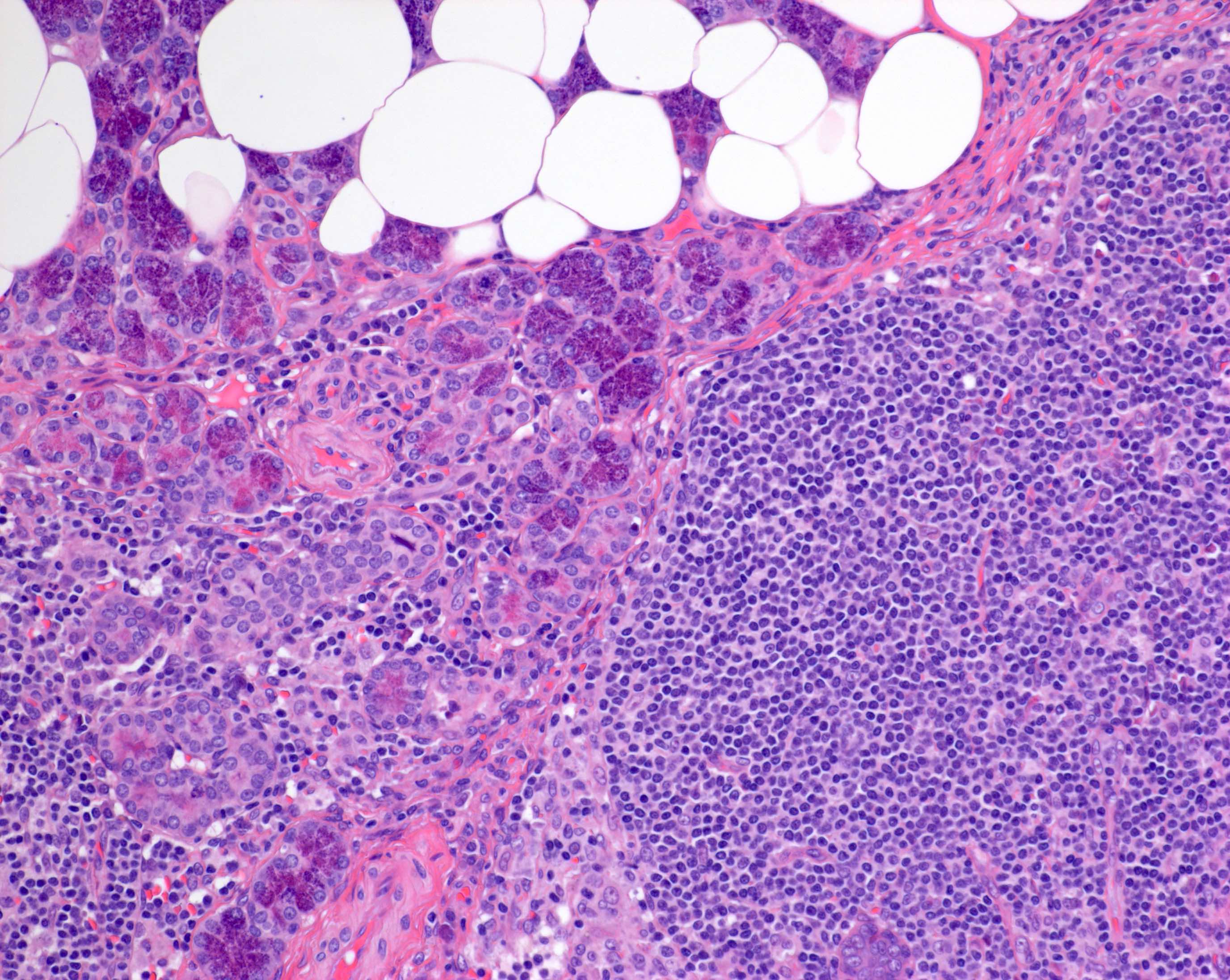
- Within the major salivary glands, these functional secretory units are arranged in lobules
- Interlobular regions include large excretory ducts and neurovascular bundles (Anat Rec A Discov Mol Cell Evol Biol 2006;288:498)
- Acini can be composed predominantly of serous or mucous cells or can be mixed seromucous type
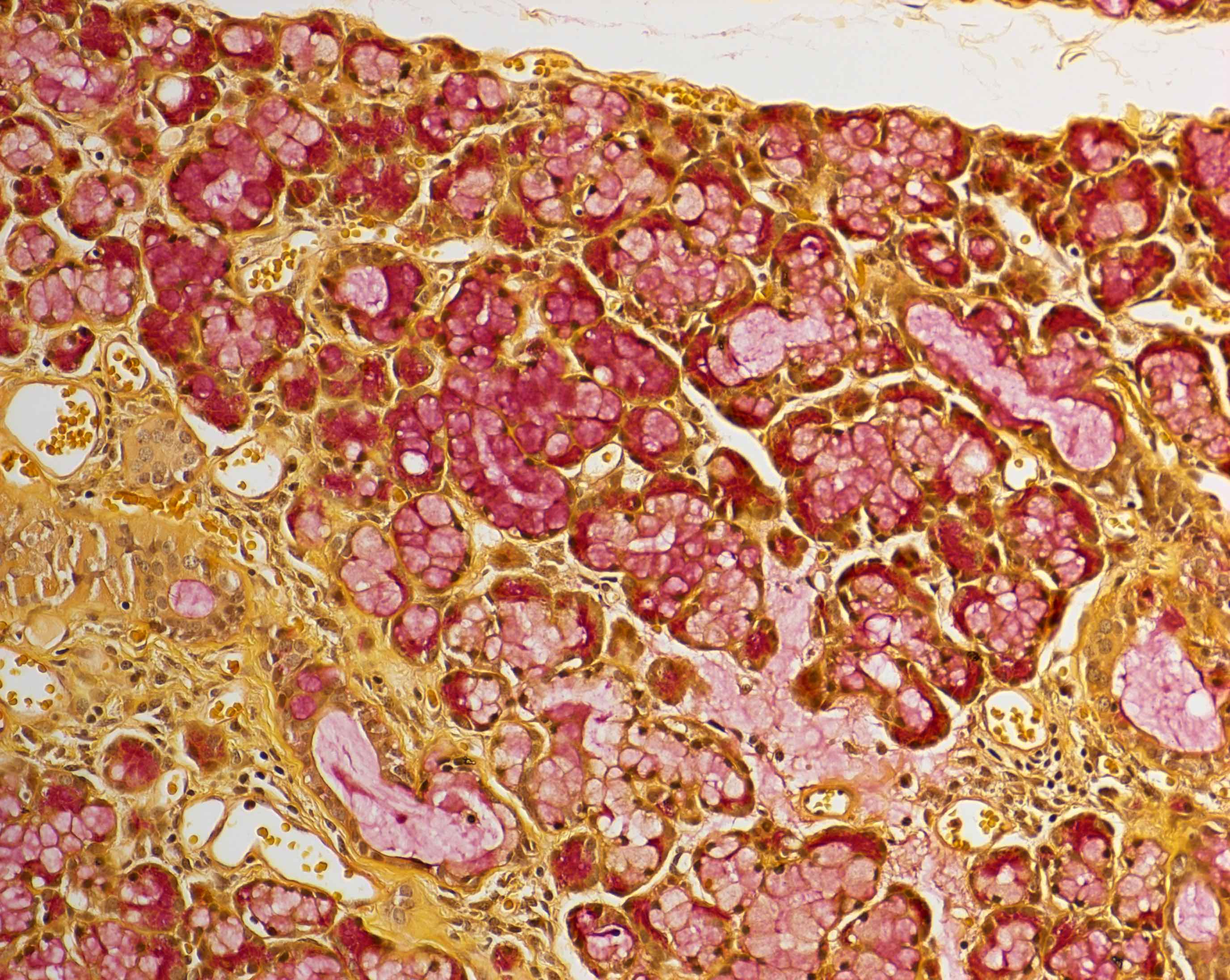
- Serous acini
- Dominant component in the parotid gland and von Ebner glands of the tongue
- Polygonal shaped cells with dense, intracytoplasmic, basophilic zymogen enzyme containing granules
- Cells are periodic acid-Schiff (PAS) reagent positive
- Mucous acini
- Dominant component in the minor salivary glands of the palate and base of tongue
- Round cells filled with mucin and containing a basally located, condensed nucleus
- Positive for mucicarmine, alcian blue and PAS with diastase resistance (DPAS)
- Mixed seromucous acini
- Dominant component in the submandibular (serous predominance) and sublingual (mucous predominance) glands, minor salivary glands of the lip, cheek and anterior tongue
- Mucous acini with crescent shaped caps (demilunes) of serous cells
- Serous acini
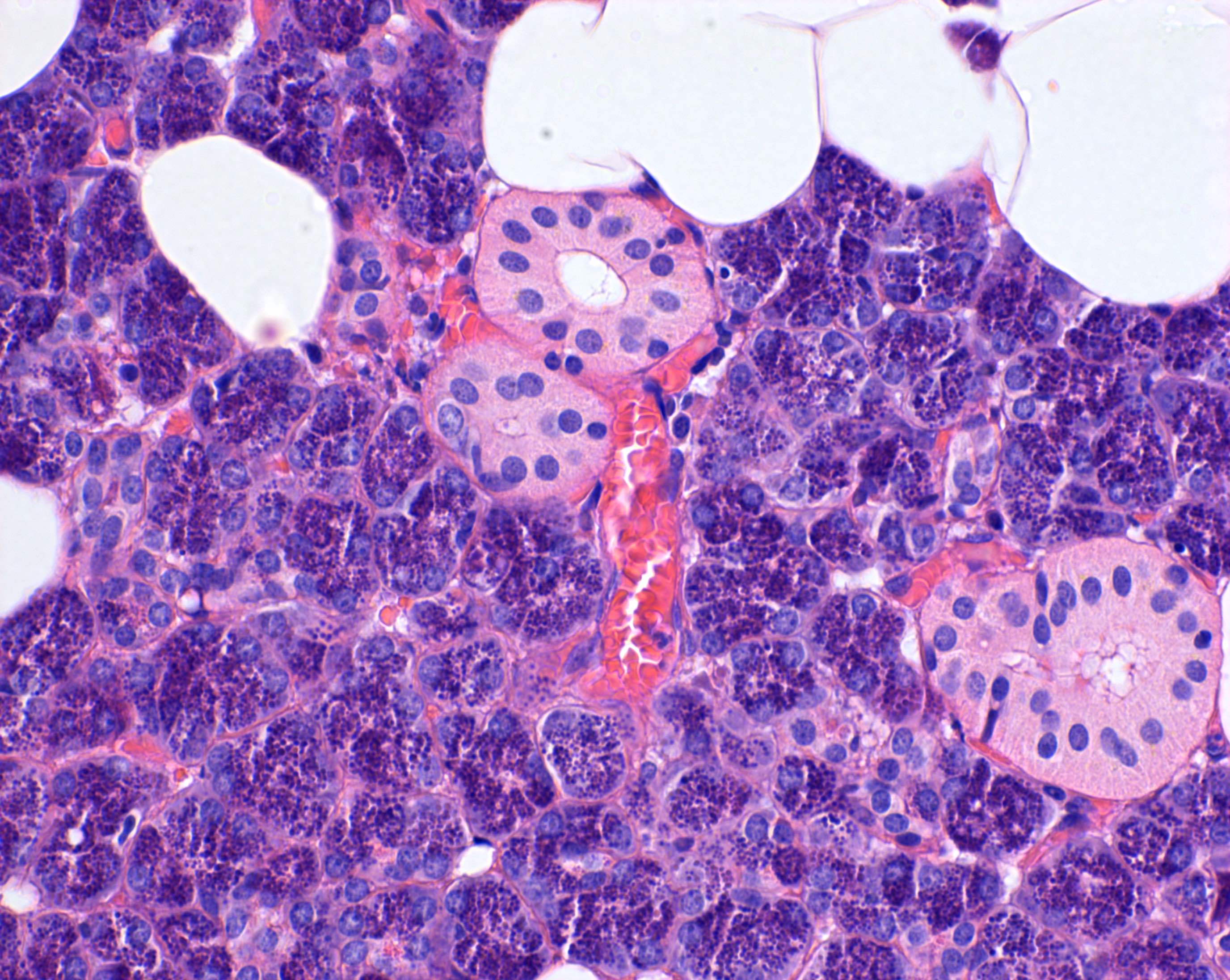
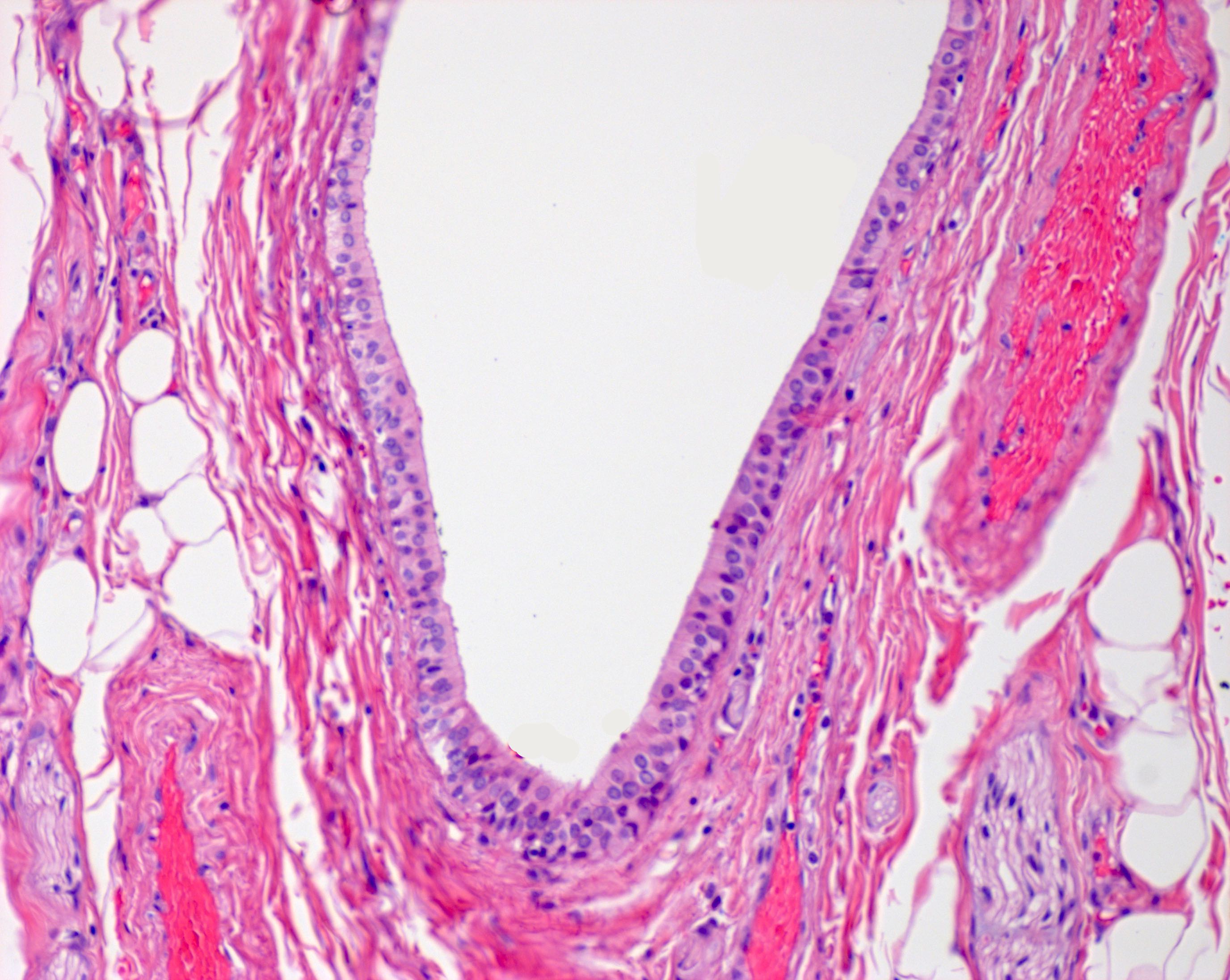
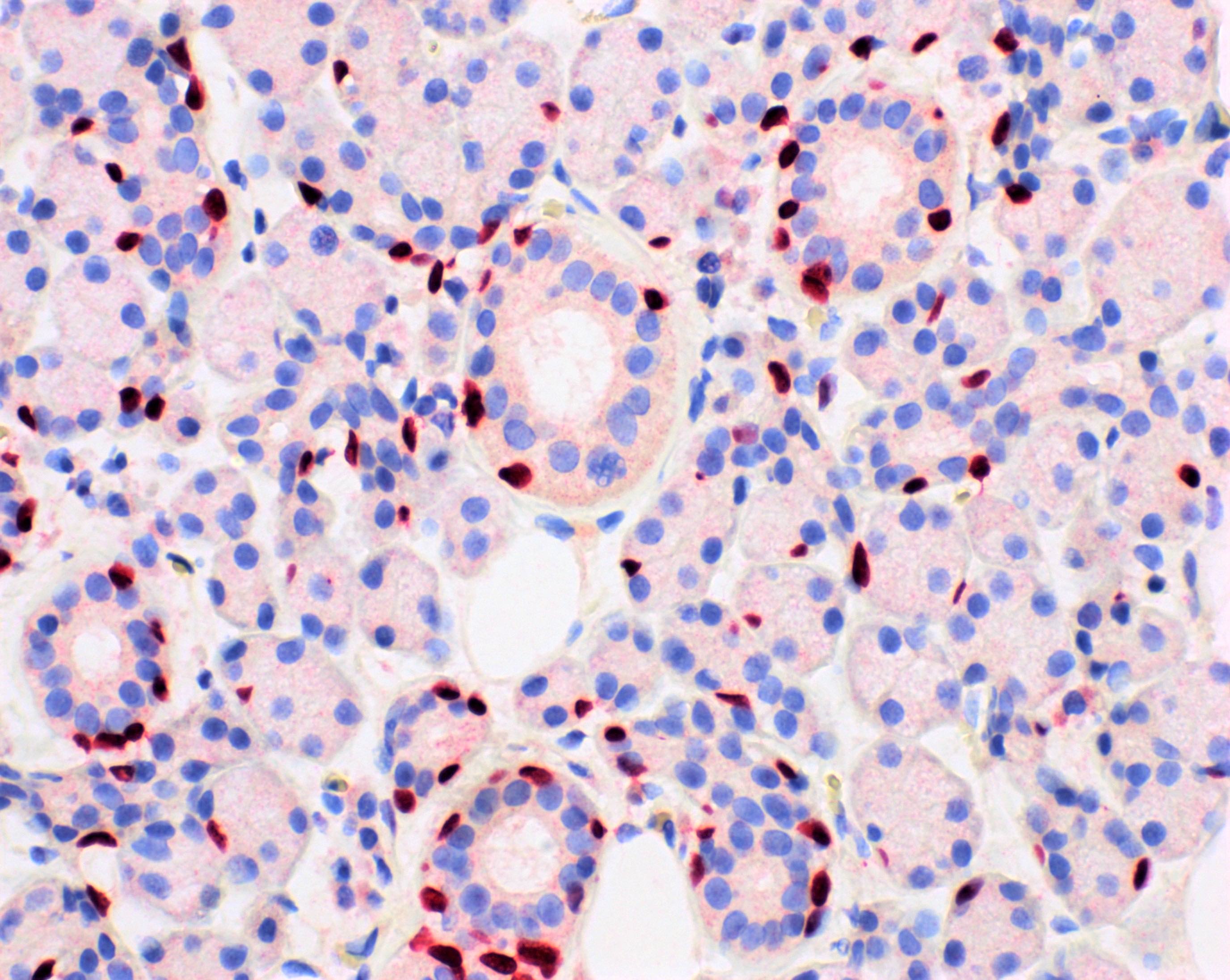
- 3 main types of ducts are intercalated, striated or interlobular:
- Intercalated ducts
- Smallest caliber
- Emerge from the acinar unit
- Lined by a single layer of cuboidal epithelium
- Contain reserve cells that regenerate the terminal secretory unit
- Striated ducts
- Proceed from the intercalated ducts
- Intralobular
- Intermediate caliber between intercalated and interlobular ducts
- Lined by columnar epithelium containing basal cytoplasmic striations, formed by rows of mitochondria alternating with folded cell membrane (Anat Rec 2001;264:121)
- Contribute to the ionic composition of the saliva
- Drain into interlobular ducts
- Interlobular ducts
- Largest caliber
- Located within interlobular septa and lined by pseudostratified columnar epithelium
- Merge to form the major excretory duct outside the gland, lined distally by nonkeratinized stratified squamous epithelium
- Intercalated ducts
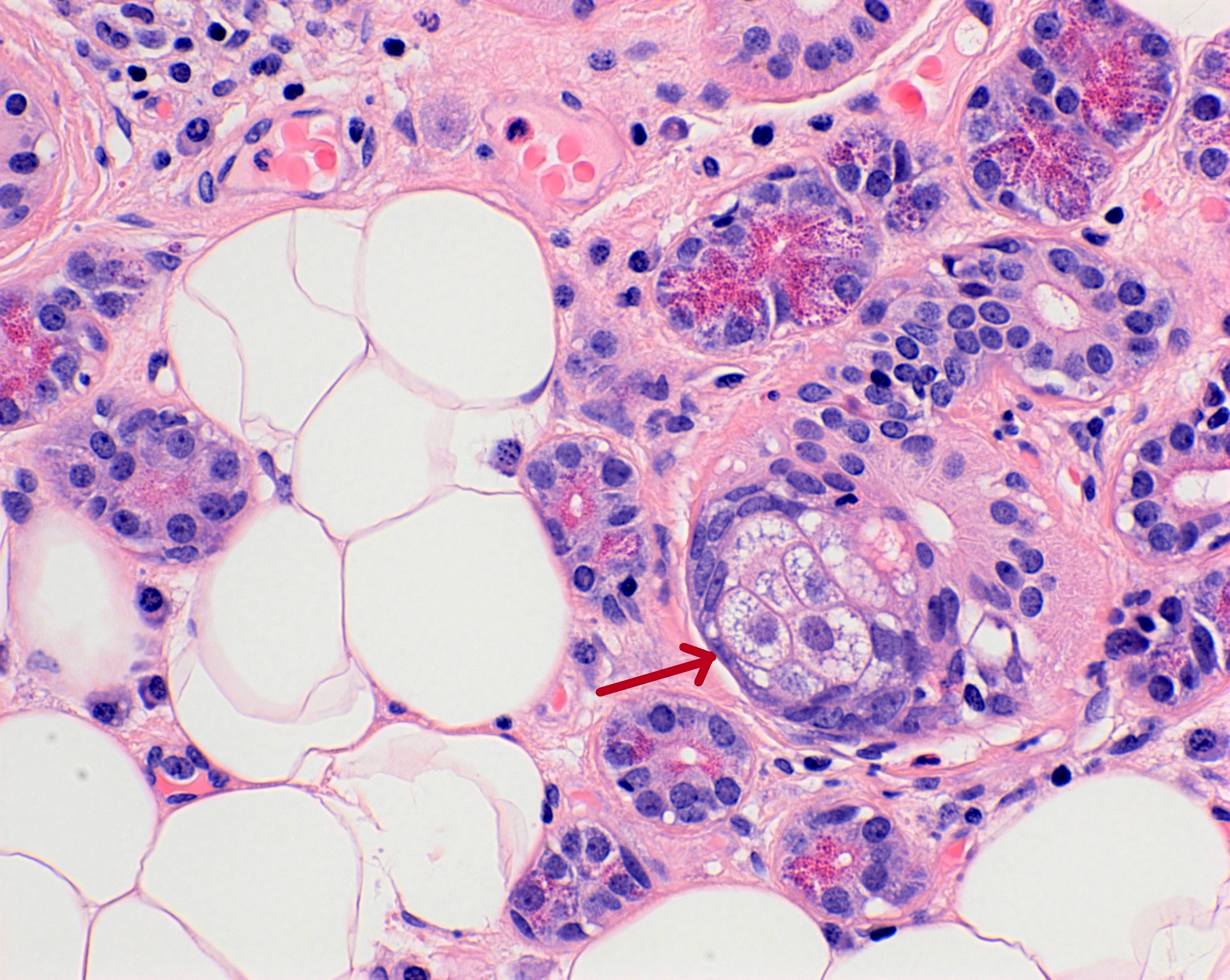
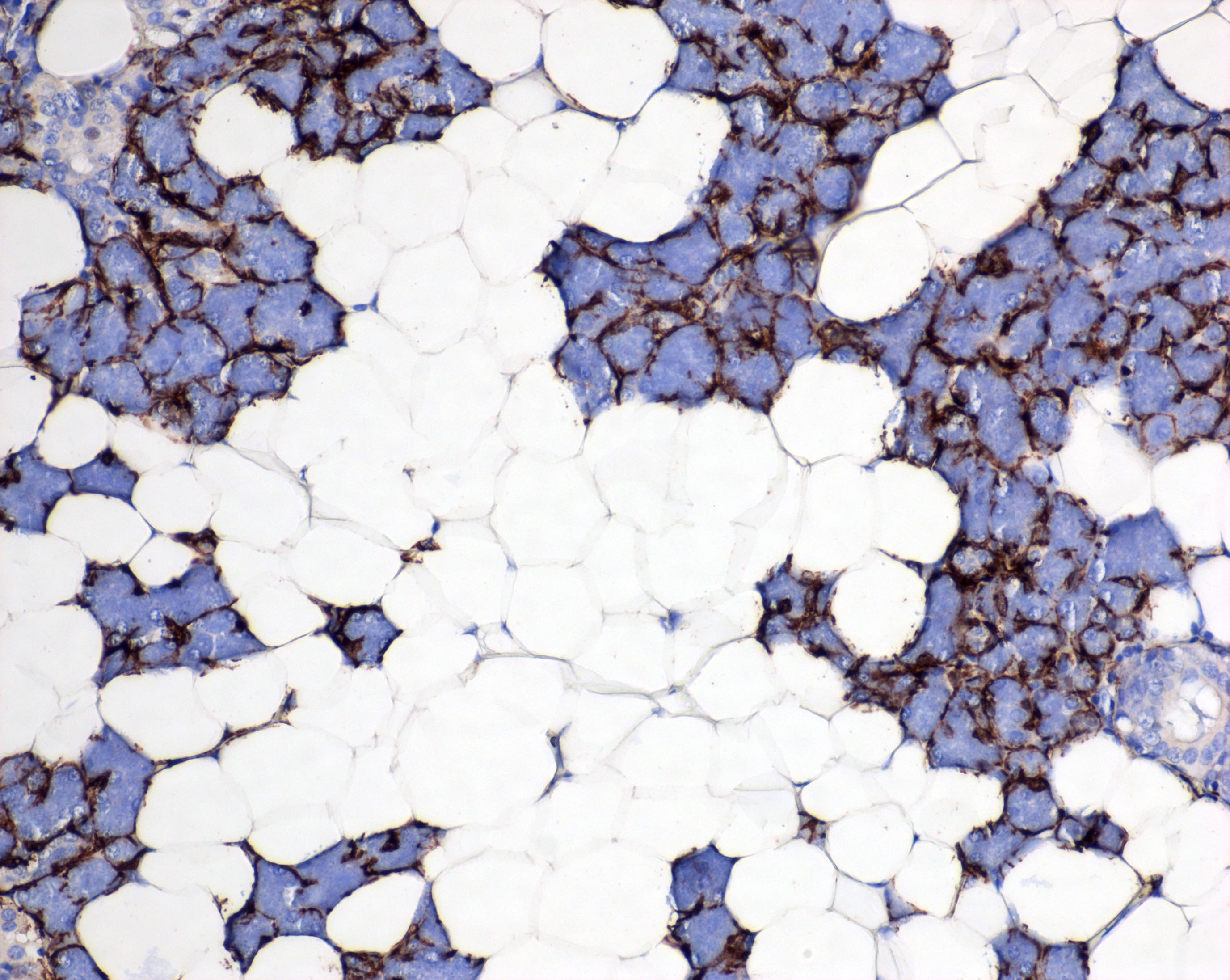
- Myoepithelial cells are critical for the expulsion of saliva
- Contractile myoepithelial cells surround acini, intercalated ducts and striated ducts
- Located between epithelial cells and the basement membrane, embracing the secretory unit with long cytoplasmic processes
- Generally spindle shaped with blunt ended nuclei and elongated cytoplasmic processes (Microsc Res Tech 1993;26:5)
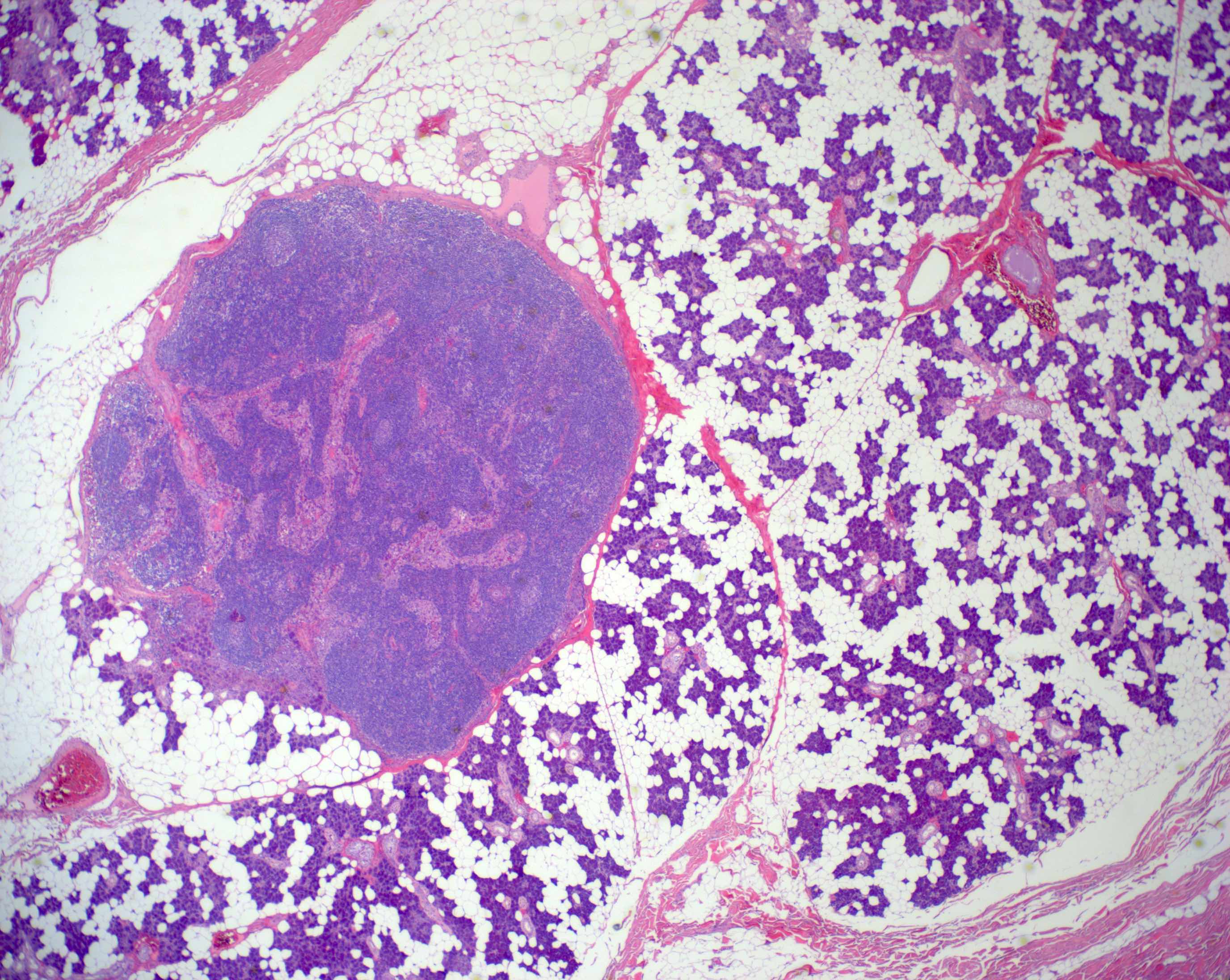
- Normal inclusions within the salivary glands:
- Presence of sebaceous glands within the parotid gland is common and are usually found associated with interlobular ducts or may exist as isolated cells within the wall of intercalated or striated ducts (Am J Surg Pathol 1989;13:879)
- Unique to the parotid gland is the presence of intraparotid lymph nodes, most of which are located superficial to the facial nerve (Br J Plast Surg 1985;38:1)
- Often the lymph nodes may lack a well defined capsule and merge with the adjacent salivary gland acini
- Fatty infiltration of the major salivary glands is an age induced variation (Am J Surg Pathol 1989;13:879)
Microscopic (histologic) images
Contributed by Ruta Gupta, M.B.B.S., M.D. and Theoni Haralabopoulos, M.D.
Major salivary glands:
Minor salivary glands:
Special stains and immunohistochemistry:
Positive stains
- Acinar cells
- Zymogen granules of serous acinar cells are periodic acid-Schiff (PAS) reagent positive
- Low molecular weight cytokeratins (e.g. CK7, CK8, CK19)
- Alpha-amylase
- Mucinous cells
- Mucous cells are positive for mucicarmine, alcian blue and PAS with diastase resistance (DPAS)
- CK5/6
- p63
- Ductal cells
- Myoepithelial cells
- May coexpress CK14, CK19 and vimentin
- Alpha smooth muscle actin (SMA)
- Calponin
- Muscle specific actin (MSA)
- p63
- Caldesmon
- Myosin heavy chain (MHC)
- Glial fibrillary acidic protein (GFAP) (variable)
- S100 (variable) (Acta Histochem Cytochem 2012;45:269)
Videos
Shotgun histology parotid gland
Shotgun histology submandibular gland
Shotgun histology sublingual gland
Practice question #1
Practice answer #1
D. The striated ducts contain abundant mitochondria to provide the energy for ion transport
Comment Here
Reference: Salivary glands - Anatomy & histology
Comment Here
Reference: Salivary glands - Anatomy & histology
Practice question #2
Which of the following is true about the parotid gland?
- The acini are purely of mucous type
- Intraparenchymal lymph nodes may contain glandular inclusions
- Wharton duct, the main excretory duct, pierces the masseter muscle to enter the oral cavity
- Sebaceous cells may be found within fatty tissue
- The facial nerve traverses the superficial surface of the gland
Practice answer #2
B. Intraparenchymal lymph nodes may contain glandular inclusions. A is incorrect because the acini are purely of serous type in the parotid gland. C is incorrect since the main excretory duct of the parotid gland is Stensen duct, which emerges from the anterior border of the gland, courses horizontally along the masseter muscle and turns medially to pierce the buccinator muscle. D is incorrect because sebaceous cells may exist within the wall of intercalated or striated ducts. E is incorrect because the facial nerve traverses the body of the gland to divide it into superficial and deep lobes.
Comment Here
Reference: Salivary glands - Anatomy & histology
Comment Here
Reference: Salivary glands - Anatomy & histology