Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Schukow C, Singh R, Ahmed A. Alopecia mucinosa. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumoralopeciamucinosa0.html. Accessed May 2nd, 2024.
Definition / general
- Alopecia mucinosa is an inflammatory hair loss condition, characterized by the accumulation of mucin in sebaceous glands and around hair follicles (i.e., pilosebaceous units)
- This inflammatory disorder may lead to subsequent follicular degeneration and may occur secondary to other diseases (e.g., lymphoma)
Essential features
- Hair loss condition in which mucin accumulates in sebaceous glands and hair follicles (i.e., pilosebaceous units), causing subsequent degeneration and hair loss
- It most frequently affects the head and neck regions, including the face and scalp
- More commonly affects children and young adults and may appear clinically as edematous or erythematous papules, plaques or nodules of alopecia in hair bearing skin areas
- Can either be a primary (i.e., idiopathic) or secondary condition and is typically benign and self limited, with more favorable outcomes in younger patients
- Prognosis may be poor in patients with disease due to lymphoma or of older age
Terminology
- Pinkus follicular mucinosis, follicular mucinosis
ICD coding
Epidemiology
- Mostly occurs in the head and neck regions (i.e., face, scalp) of children and young adults (Indian Dermatol Online J 2013;4:333)
- More generalized distributions (i.e., trunk, extremities) may be seen in patients with chronic disease
- Can either be primary (i.e., idiopathic) or secondary (e.g., in the setting of another disease such as cutaneous T cell lymphoma)
- Historically has been referred to as a histologic manifestation of folliculotropic mycosis fungoides (MF), although it is not specific to MF (Am J Dermatopathol 2004;26:33, Am J Dermatopathol 1988;10:478, Cutis 2015;95:E9, J Am Acad Dermatol 2012;67:1174)
Sites
- Lesions on the face, neck and scalp are the most common but other body parts may also be affected
- Affected skin areas will appear as pruritic, pink-white papules and plaques, along with subsequent hair loss (Indian Dermatol Online J 2013;4:333)
Pathophysiology
- Mucin accumulates within the pilosebaceous unit (external root sheath and sebaceous glands), causing follicular degeneration (Arch Dermatol 1983;119:690)
- Follicular degeneration may not appear as alopecia
- Pathophysiology is largely unknown, however is hypothesized to be a result of cellular changes leading to pilosebaceous unit mucin deposition from follicular keratinocytes (J Am Acad Dermatol 2012;67:1174, Indian Dermatol Online J 2013;4:333)
- Inflammation ensues, as suggested by the frequent presence of T cells, macrophages and Langerhans cells seen in histology (J Am Acad Dermatol 1984;10:760)
- Inflammatory cells may be reacting to local, persistent antigens such as Staphylococcus aureus (J Cutan Pathol 2010;37:15, Cutis 2012;89:266)
- Granulomatous inflammation should raise consideration for coexisting leprosy, especially in developing countries or endemic areas (Indian J Lepr 2002;74:341, Int J Dermatol 2020;59:e471, An Bras Dermatol 2015;90:147)
Etiology
- Etiology is not completely understood but is associated with other inflammatory, neoplastic or locally infectious conditions (Int J Dermatol 2021;60:159)
- Patients with clonal TCR rearrangements may be at higher risk of developing coexisting or subsequent lymphoma, although literature appears to be inconsistent in this regard (Blood 1988;71:1329, J Am Acad Dermatol 2002;47:856, Indian J Dermatol 2013;58:227)
Diagrams / tables
Not relevant to this topic
Clinical features
- Edematous and erythematous alopecia papules, plaques or nodules of alopecia on the head, scalp, face or neck
- Benign, self limited disease may be favored in children (i.e., spontaneous resolution within 2 - 24 months); secondary etiologies may be more common in adults (Indian Dermatol Online J 2013;4:333)
- Patterns
- Infiltrating solitary or multiple plaques associated with hair loss in the scalp or beard areas
- Group of follicular papules, either localized or extensively distributed on trunk and proximal limbs in addition to scalp and face
- Acneiform lesions with comedones, mucorrhea (discharge of mucinous fluid from follicular ostia) or severe pruritus
- May spontaneously regress within a few years or chronically relapse but demonstrates a benign course over many years
- Lesions present as an acneiform eruption, characterized by cysts or comedones, refractory to traditional acne therapies (Clin Exp Dermatol 2018;43:921, Am J Dermatopathol 2013;35:792)
- May be observed in the setting of other nonlymphoproliferative conditions, such as basaloid follicular hamartoma, squamous cell carcinoma, seborrheic keratosis, prurigo, acne vulgaris, medication induced skin toxicity / vasculitis, polymorphous light eruption, insect / tick bite and Demodex infiltration (An Bras Dermatol 2022;97:45, Am J Dermatopathol 2014;36:705)
Diagnosis
- Diagnosis is made via clinicohistopathologic correlation
Laboratory
- Copresenting lymphocytosis may suggest secondary etiology (e.g., MF, lymphoma) (Am J Clin Pathol 2011;135:221)
- Often unremarkable, especially in patients with solitary lesions without systemic symptoms (Arch Dermatol 2002;138:182)
Radiology description
Not relevant to this topic
Radiology images
Not relevant to this topic
Prognostic factors
- Younger patients (i.e., children to young adults) are more likely to experience benign disease without subsequent malignancy (Int J Dermatol 2023;62:1056)
- Coexisting lymphoma and older age are associated with a worse prognosis (Arch Dermatol 1965;92:137)
- Patients with TCR rearrangement may require long term follow up for malignant transformation (J Am Acad Dermatol 2002;47:856)
Case reports
- 3 year old boy treated successfully with pimecrolimus cream and targeted phototherapy (Case Rep Dermatol 2022;14:84)
- 9 year old boy with associated basaloid follicular hamartoma on the forehead (An Bras Dermatol 2022;97:45)
- 11 year old boy with primary disease (An Bras Dermatol 2020;95:268)
- 11 year old girl with primary disease (Cureus 2019;11:e4746)
- 51 year old man with treatment resistant disease resolved with dupilumab (JAAD Case Rep 2023;34:83)
Treatment
- Lesions may persist for months or years and resolve spontaneously without treatment
- No evidence based, guideline directed treatments have shown consistency in the literature; however, cases of resolution with minocycline, antileprosy medications, dapsone, topical steroids / retinoids and ultraviolet light have been documented (Am Acad Dermatol 1998;38:849, Br J Dermatol 2000;142:841, J Am Acad Dermatol 2010;62:139, Indian J Dermatol 2013;58:227, Br J Dermatol 1974;91:217, Clin Exp Dermatol 1989;14:382, Pediatr Dermatol 2013;30:192)
Gross description
- Hair bearing skin fragments with underlying subcutaneous tissue
- Grossly intact epidermis with follicular papules containing gelatinous, mucinous material
- Reference: Cureus 2019;11:e4746, JAAD Case Rep 2023;34:83, J Am Acad Dermatol 2019;80:1524
Gross images
Not relevant for this topic
Frozen section description
Not relevant for this topic
Frozen section images
Not relevant for this topic
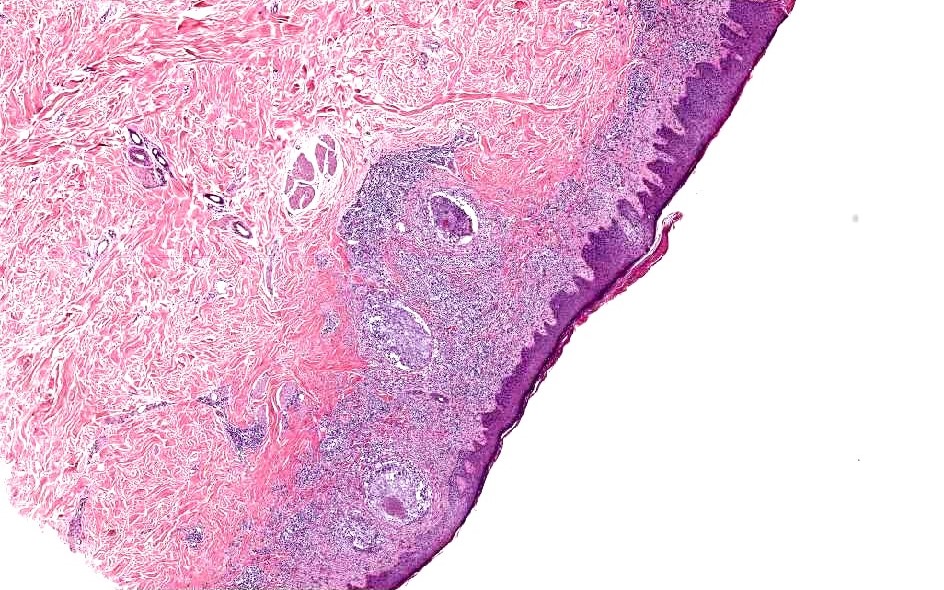
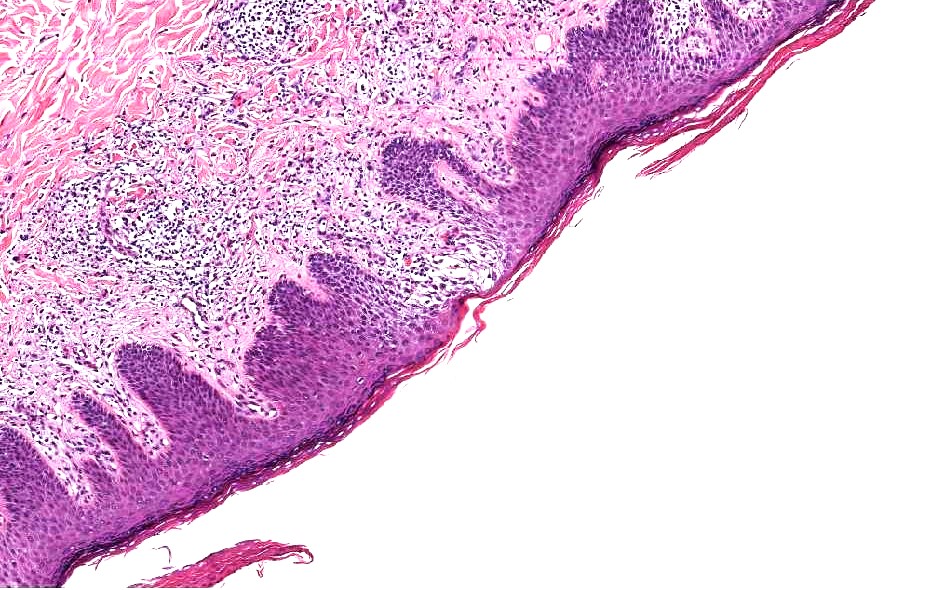
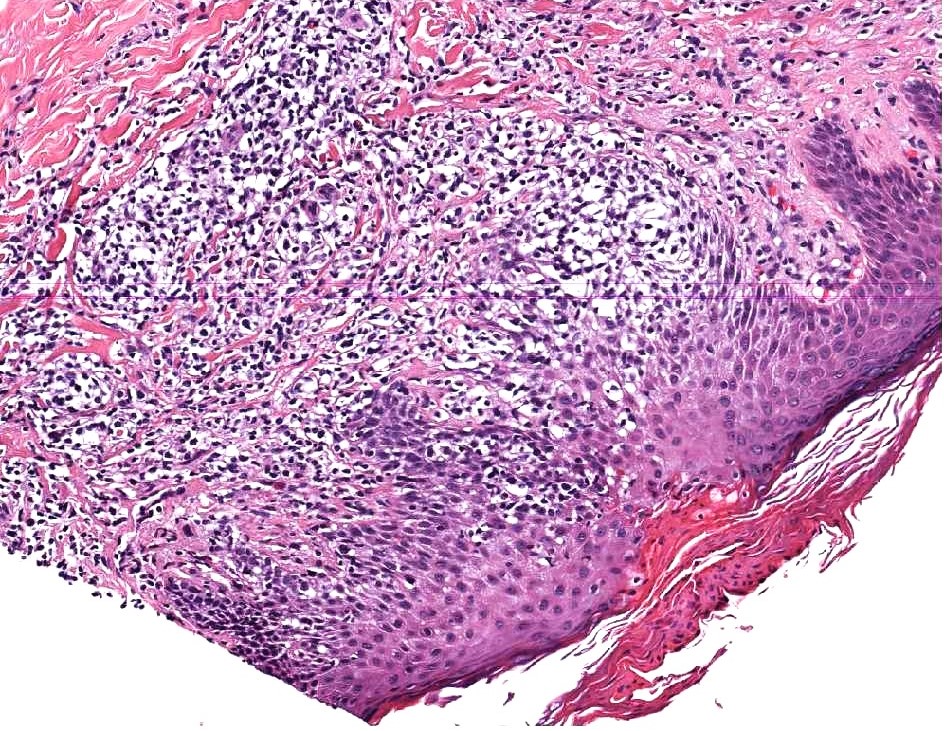
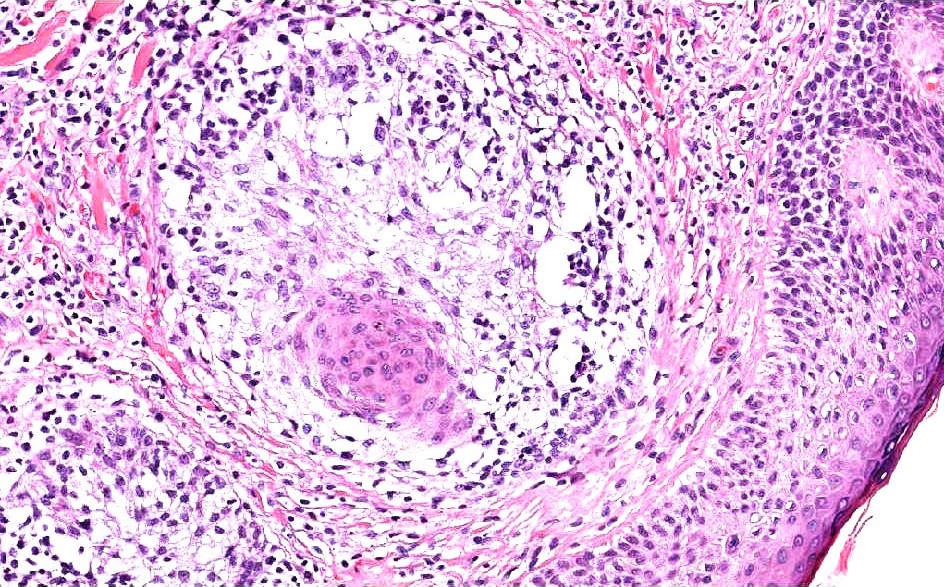
Microscopic (histologic) description
- Follicular infundibulum keratinocytes and outer root sheath are separated by pools of mucin
- Mucin may appear pale and basophilic, displacing collagen fibers and reside within the pilosebaceous unit
- Dehydrated mucin may also appear as beads on string
- There may be a mixed dermal infiltrate of lymphocytes, histiocytes and conspicuous eosinophils
- Marked follicular dilation with cyst formation and perifollicular scarring may also be seen
- In cases associated with lymphoma, folliculotropism by lymphocytes with cerebriform nuclei or large transformed cells may be seen
- Reference: Cureus 2019;11:e4746, JAAD Case Rep 2023;34:83, J Am Acad Dermatol 2019;80:1524
Microscopic (histologic) images
Virtual slides
No virtual slides found
Cytology description
Not relevant to this topic
Cytology images
Not relevant to this topic
Immunofluorescence description
- Although not routinely used today, prior direct immunofluorescence studies demonstrated complement (C3) and fibrin / fibrinogen deposition within areas of follicular degeneration (J Am Acad Dermatol 1984;10:760)
Immunofluorescence images
Not relevant to this topic
Positive stains
- Mucin directed stains can confirm the presence of mucin, however, are mostly not necessary (e.g., Alcian blue, colloidal iron) (Indian Dermatol Online J 2013;4:333, An Pediatr (Barc) 2014;81:198, An Bras Dermatol 2015;90:147, J Cutan Pathol 2016;43:1005)
- In secondary setting of cutaneous T cell lymphoma, a work up for lymphoid markers (CD3, CD4, CD8, CD2, CD5, CD7, CD30, CD20) should be pursued; flow cytometry may also be considered
Negative stains
N/A
Electron microscopy description
- Although not routinely used today, prior electron microscopy studies demonstrated dilated cystic organelles and vesicles within affected root sheath cells accompanied by amorphous collections of fine granular materials
- Extracellular hyaluronic acid accumulation may be seen (Acta Derm Venereol 1976;56:163)
Electron microscopy images
Not relevant to this topic
Molecular / cytogenetics description
- TCR rearrangement may be positive via PCR testing in the setting of cutaneous T cell lymphoma but literature does not always support this (J Am Acad Dermatol 2012;67:1174, JAAD Case Rep 2021;18:29, Cutis 2015;95:E9)
Molecular / cytogenetics images
Videos
Follicular mucinosis with Antonina Kalmykova & Phillip McKee
Sample pathology report
- Skin (scalp), punch biopsy:
- Alopecia mucinosa (see comment)
- Comment: Histologic sections demonstrate loss of hair follicles. Residual follicles show mucinous degeneration. A mixed dermal infiltrate composed of lymphohistiocytic cells is also noted. Significant epidermotropism or folliculotropism is not seen. The etiology of this condition is not completely known, however it is associated with aberrant immune system activity and can be seen in the setting of inflammatory or lymphoproliferative conditions.
Differential diagnosis
- Coexisting lymphoma (e.g., mycosis fungoides):
- Atypical or cerebriform lymphocytes with folliculotropism
- Obtain multiple biopsies as needed; correlate clinically
- TCR gene monoclonality is suggestive but may not be present (Cutis 2015;95:E9)
- Alopecia areata:
- Peribulbar lymphocytic infiltrate without follicular dropout; nonscarring alopecia (J Cutan Pathol 2013;40:887)
- Discoid lupus / lichen planopilaris / central centrifugal cicatricial alopecia (CCCA):
- May also present with periinfundibular / isthmic inflammatory infiltrate and cause alopecia
- Lupus typically also involved epidermis with follicular plugging and periadnexal infiltrate
- Lichen planopilaris shows prominent inflammation
- CCCA typically shows prominent interface changes
- Leprosy:
- Histology may be indistinct
- Presence of granulomas (although are not always present), resolution with antileprosy treatments or endemic region exposure may be suggestive (An Bras Dermatol 2015;90:147, Indian J Dermatol 2013;58:227)
Additional references
Board review style question #1
A 10 year old boy presents with painless bumps on his cheek for the past 2 months. Patient denies any systemic symptoms. Coalescing erythematous papules are present on physical exam. A skin punch biopsy is obtained with findings shown above. Which of the following is most likely true?
- Alcian blue is likely to be positive
- Granulomatous infiltration must be present to consider leprosy
- Negative TCR gene rearrangement effectively rules out malignancy
- Spontaneous resolution is uncommon this age group
- Staphylococcus aureus is not implicated in the pathophysiology of this condition
Board review style answer #1
A. Alcian blue is likely to be positive. The most likely diagnosis in this patient is alopecia mucinosis (previously known as follicular mucinosis). Although the pathogenesis of this condition is not completely understood, it is hypothesized to be a result of cellular changes leading to mucin deposition due to aberrant follicular keratinocyte activity. This condition frequently presents as erythematous papules or plaques with subsequent hair loss. In alopecia mucinosis, mucin stains (like Alcian blue) are likely to stain positive. Answer E is incorrect because histology reveals pilosebaceous unit and peribulbar mucin deposition with a mixed inflammatory infiltrate that may be reacting to local antigens like Staphylococcus aureus.
Answer B is incorrect because although granulomatous infiltration is suggestive of leprosy in patients within endemic regions, it may not always be present. Answer C is incorrect because the same can be said for TCR gene rearrangement and malignancy (i.e, lymphoma). Answer D is incorrect because as opposed to older patients, younger patients more frequently experience a benign disease course with spontaneous resolution within 2 years and have a more favorable prognosis.
Comment Here
Reference: Alopecia mucinosa
Comment Here
Reference: Alopecia mucinosa
Board review style question #2
Where is the most common location that alopecia mucinosa presents?
- Extremities
- Hands and feet
- Head and neck
- Trunk
- Buttocks
Board review style answer #2
C. Head and neck. The most common location for alopecia mucinosa to present is the head and neck region (including the face) of children and young adults. Moreover, while alopecia mucinosa has been historically referred to as a histologic manifestation of folliculotropic mycosis fungoides (MF), it is not specific to MF. Answers A, B, D and E are incorrect because more generalized distributions involving other regions may be seen in patients with chronic disease but these locations are not most common.
Comment Here
Reference: Alopecia mucinosa
Comment Here
Reference: Alopecia mucinosa