Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Asadbeigi S, Momtahen S. Pigmented purpuric dermatosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorpigmentedpurpuricdermatosis.html. Accessed September 16th, 2025.
Definition / general
- Chronic purpuric skin disorders include several skin disorders characterized by macules, patches and petechiae on a brown, red or yellow base resulting from erythrocyte extravasation and hemosiderin deposition
Essential features
- Chronic purpuric skin disorders
- Perivascular lymphocytic infiltrate along with endothelial cell swelling and erythrocyte extravasation (StatPearls: Pigmented Purpuric Dermatitis [Accessed 18 April 2023])
- Variable pigmentation resulting from the erythrocyte extravasation and hemosiderin deposition
Terminology
- Pigmented purpuric dermatitis
- Pigment purpuric eruptions (Dermatol Clin 1985;3:165)
- Purpura simplex (J Am Acad Dermatol 1991;25:642)
- Capillaritis
- Inflammatory purpura without vasculitis
Epidemiology
- Rare
- Generally occurs in adults but can involve children (Pediatr Dermatol 2001;18:299)
- M:F = 1:1.1 (J Cutan Pathol 2018;45:325, Ann Dermatol 2015;27:404)
- Idiopathic; not associated with coagulopathies or thrombocytopenia
Sites
- Lower extremities > upper extremities > trunk (Ann Dermatol 2015;27:404)
Pathophysiology
- Superficial dermal capillaritis (StatPearls: Pigmented Purpuric Dermatitis [Accessed 18 April 2023])
- Possible concomitant venous hypertension leads to endothelial cell dysfunction
- Extravasation of red blood cells
- 3 suggested pathogenetic mechanisms (J Cutan Pathol 1991;18:423, Br J Dermatol 1996;134:180, J Clin Med 2021;10:2283)
- Disturbed humoral immunity
- Cellular immune reaction
- Capillary fragility
Etiology
- Unknown
- Most cases are idiopathic
- Rare familial cases
- Potential contributors (J Am Acad Dermatol 1991;25:642, J Am Acad Dermatol 2005;53:168, J Am Acad Dermatol 2002;46:942, Am J Clin Dermatol 2014;15:65, Am J Clin Dermatol 2017;18:383, Dermatol Clin 1985;3:165, Pediatr Dermatol 2001;18:299, Cutan Ocul Toxicol 2019;38:258, Dermatol Online J 2014;21:13030)
- Systemic diseases
- Drugs
- Localized infection
- Physical activity
- Diabetes mellitus
- Antidiabetic medication (especially in Schamberg disease)
- Venous stasis
- Venous hypertension
- Capillary fragility
- Aberrant cell mediated immunity
- Contact allergens
- Hyperlipidemia
Clinical features
- Different subtypes are mainly distinguished based on the clinical presentations (StatPearls: Pigmented Purpuric Dermatitis [Accessed 18 April 2023])
- Schamberg disease (progressive pigmentary purpura)
- Most common type; pinpoint to pinhead reddish puncta known as grains of cayenne pepper, purpuric macules forming patches, bilateral with a chronic course and numerous exacerbations and remissions
- Purpura annularis telangiectodes of Majocchi disease
- Annular patches with telangiectasias and central atrophy
- Linear or arciform patches may be present, bilateral with a chronic course, relapses and remissions
- Pigmented purpuric lichenoid dermatitis of Gougerot and Blum
- Lichenoid and violaceous plaques with superimposed purpura, 1 to several centimeters in diameter, pruritic, may resemble Kaposi sarcoma, bilateral, chronic
- Lichen aureus
- Rusty yellow or gold lichenoid papules, patches and plaques, unilateral, acute onset, persistent course
- Eczematid-like purpura of Doucas and Kapetanakis
- Eczematous features, with scale overlying purpuric and petechial macules, pruritic with mild lichenification, acute onset and fluctuating course
- Itching purpura or disseminated pruriginous angiodermatitis
- Orange to brown purpuric macules with acute onset and chronic course
- Unilateral linear capillaritis or segmental pigmented purpura and quadrantic capillaropathy
- Linear, dermatomal or segmental distribution with self resolving course
- Granulomatous pigmented purpura
- Red to brown purpuric macules or papules, mostly involving knee and ankles, with a persistent course, more often in Asians
- Schamberg disease (progressive pigmentary purpura)
- Pigmented purpuric dermatosis-like variant of mycosis fungoides can overlap with mycosis fungoides or mycosis fungoides can evolve from pigmented purpuric dermatosis (Am J Dermatopathol 1997;19:108, Cutis 2014;94:297)
- This form shows large areas of confluence, violaceous hue and pruritus usually lasting > 1 year
- Dermoscopy: red or brown dots and globules, copper colored pigmentation in background, linear vasculatures, linear and reticular brown lines, rosette structure, red patches, follicular opening (An Bras Dermatol 2016;91:584, Postepy Dermatol Alergol 2019;36:687)
Diagnosis
- Diagnosis is often made by clinical presentation
- Biopsy is used for confirmation
- Blood work up and coagulation screening to exclude other conditions
- Reference: J Clin Med 2021;10:2283
Laboratory
- No associated laboratory abnormalities
Prognostic factors
- Variable progression and resolution course
- Often chronic with multiple relapses
- Pigmented purpuric dermatosis with monoclonal lymphocytic infiltrate: extensive disease (Am J Clin Pathol 2007;128:218)
- Progression to mycosis fungoides rarely reported (J Cutan Pathol 2021;48:611)
Case reports
- 4 month old boy as the youngest reported individual with pigmented purpuric dermatosis (Pediatr Dermatol 2021;38:504)
- 31 year old man with similar features of mycosis fungoides (Indian Dermatol Online J 2016;7:183)
- 45 year old woman with segmental lichen aureus (An Bras Dermatol 2017;92:704)
- 61 year old woman with pigmented purpuric lichenoid dermatosis of Gougerot-Blum (Ann Dermatol 2018;30:245)
- 61 year old Japanese woman with zosteriform pigmented purpuric dermatosis (Arch Dermatol 2007;143:1599)
- 68 year old woman with granulomatous pigmented purpuric dermatosis and Sjögren syndrome (Acta Derm Venereol 2013;93:95)
Treatment
- Treatment for symptomatic or cosmetically concerned patients (StatPearls: Pigmented Purpuric Dermatitis [Accessed 18 April 2023])
- Discontinue potential contributing factors such as causative drugs (StatPearls: Pigmented Purpuric Dermatitis [Accessed 18 April 2023])
- Rutoside 50 mg twice a day
- Ascorbic acid 500 mg twice a day
- Medium to high potency topical corticosteroids
- Systemic immunosuppression
- Antihistamines
- Topical tacrolimus or pimecrolimus
- Phototherapy, such as PUVA (Dermatology 2009;219:184, J Eur Acad Dermatol Venereol 2011;25:603)
- Other treatments (J Eur Acad Dermatol Venereol 2006;20:1378, StatPearls: Pigmented Purpuric Dermatitis [Accessed 18 April 2023])
- Pentoxifylline
- Minocycline
- Methotrexate
- Colchicine
- Laser therapy in Schamberg disease (J Clin Med 2021;10:2283)
Clinical images
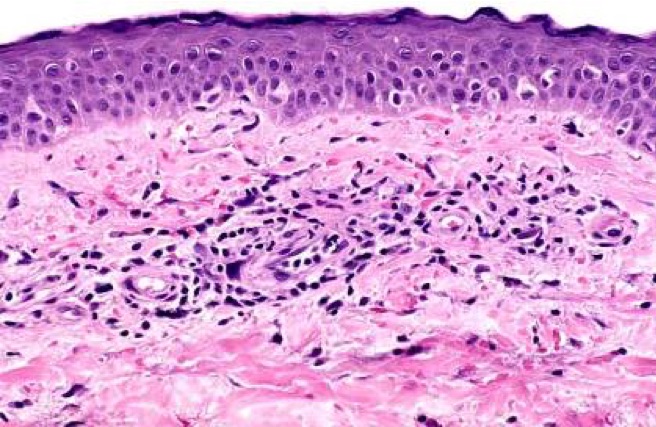
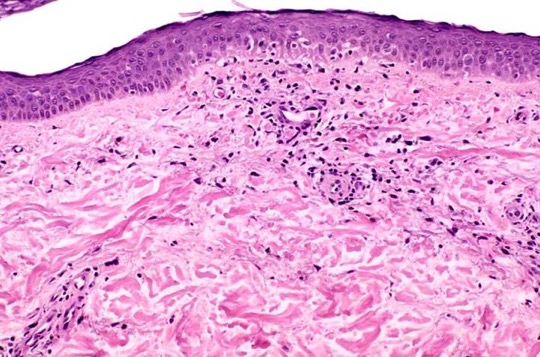
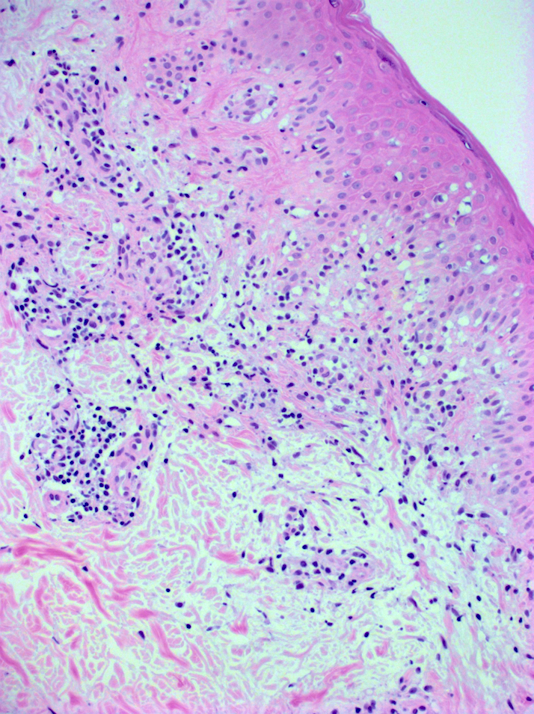
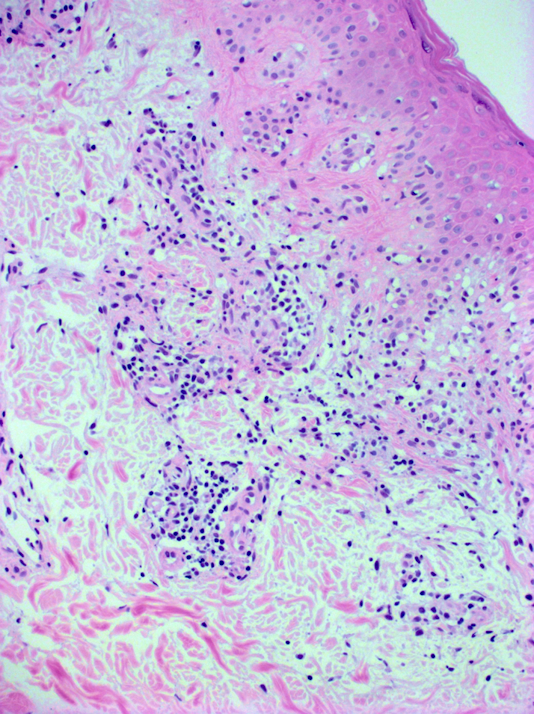
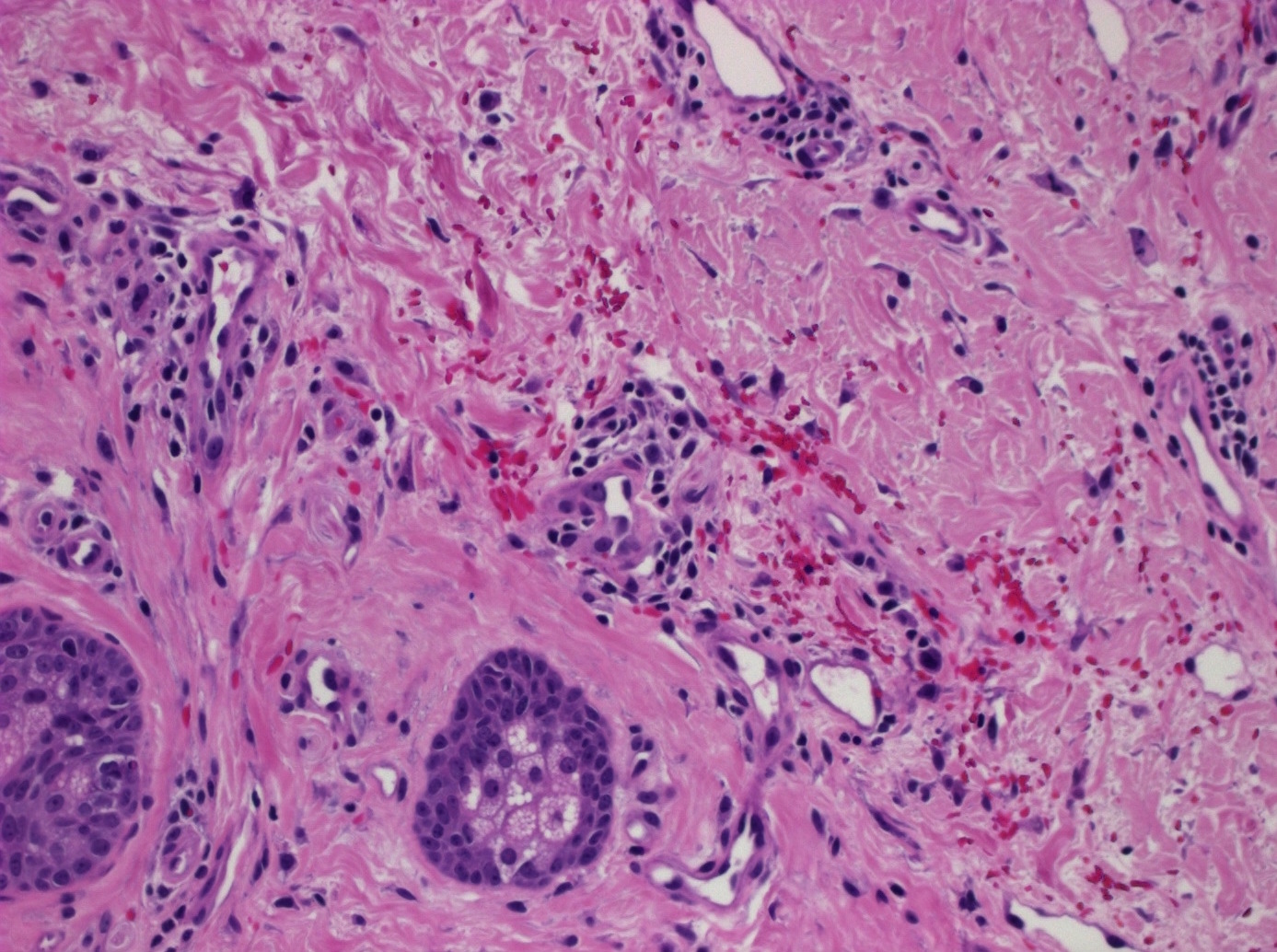
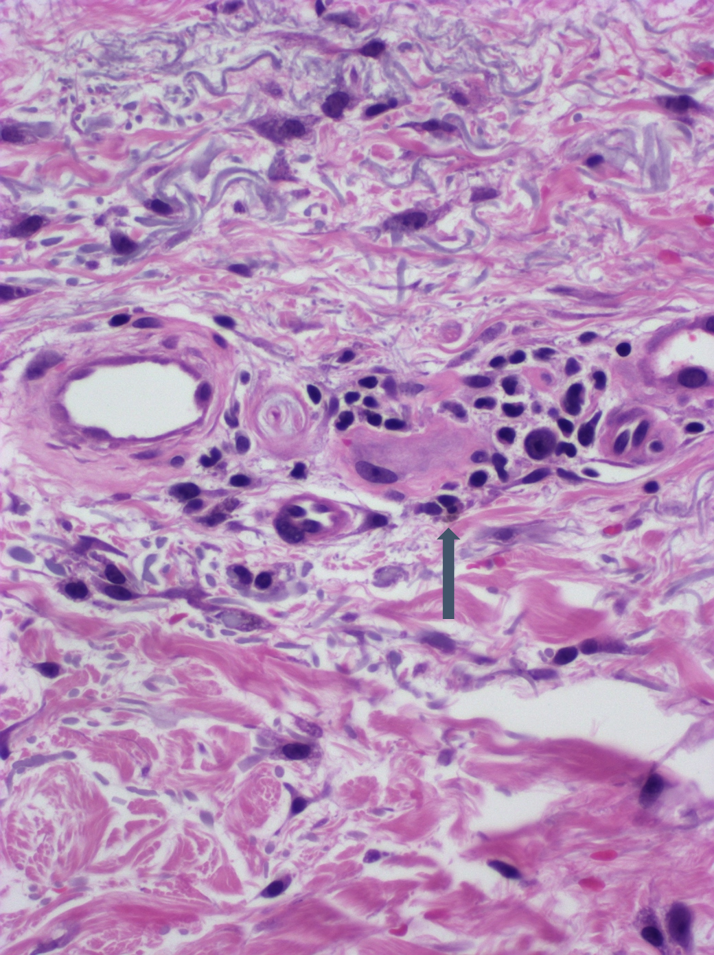
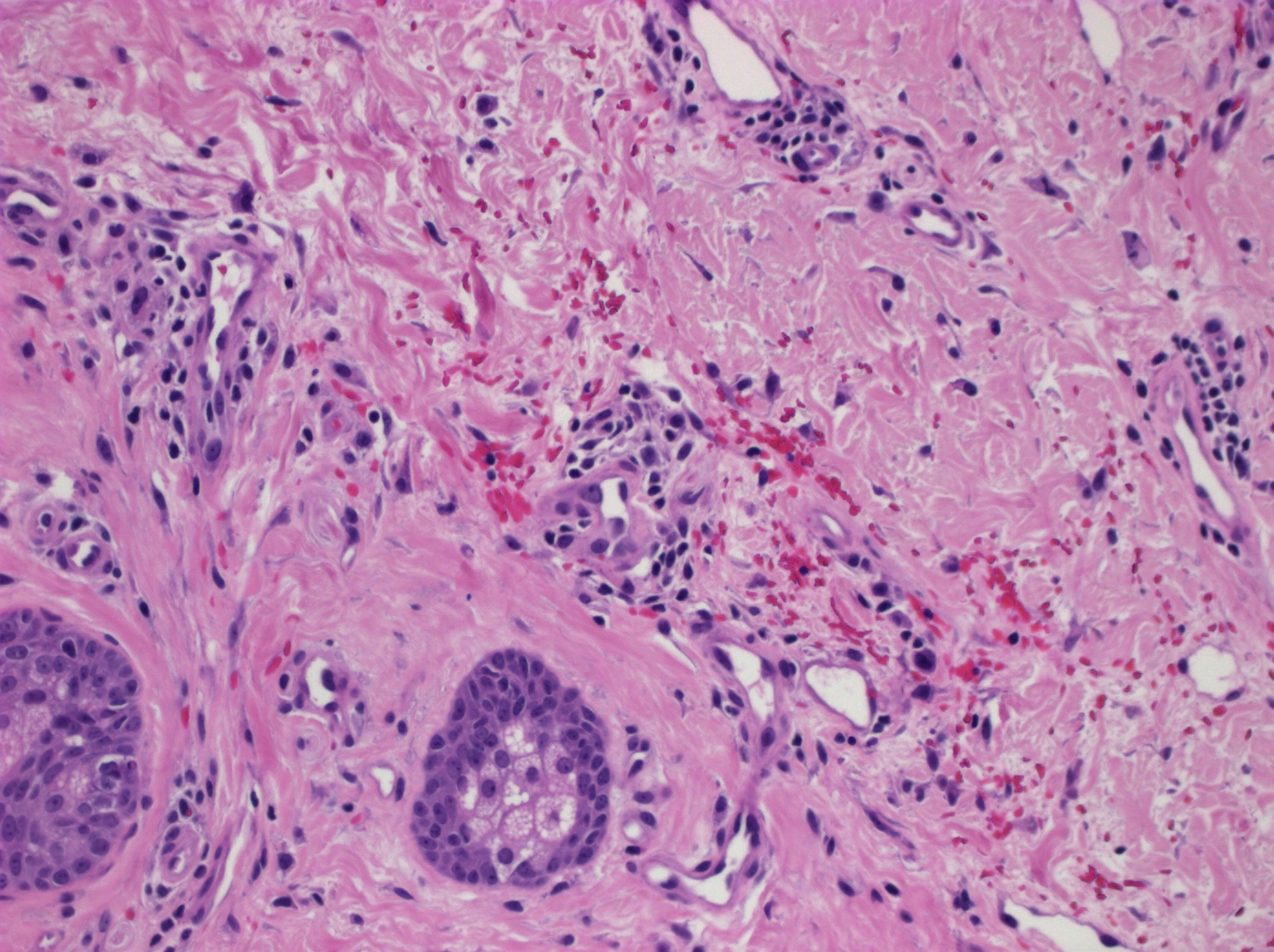
Microscopic (histologic) description
- Common histologic features in all subtypes (StatPearls: Pigmented Purpuric Dermatitis [Accessed 18 April 2023])
- CD4+ perivascular lymphocytic infiltrate
- Occasional CD1a dendritic cells and macrophages around superficial small blood vessels
- Erythrocyte extravasation
- Dilated blood vessels and endothelial cell swelling
- Hemosiderin deposition and variable pigmentation
- Mild epidermal spongiosis and lymphocyte exocytosis
- Present in all subtypes except lichen aureus
- Possible associated features
- Epidermis: focal parakeratosis, basal layer vacuolar degeneration
- Dermal - epidermal junction: interface changes (Ann Dermatol 2015;27:404)
- Vascular: endothelial edema, proliferation with narrowing of vessel lumen
- Progressive pigmentary dermatosis (Schamberg disease) (Dermatol Clin 1985;3:165)
- Variable degree of epidermal spongiosis
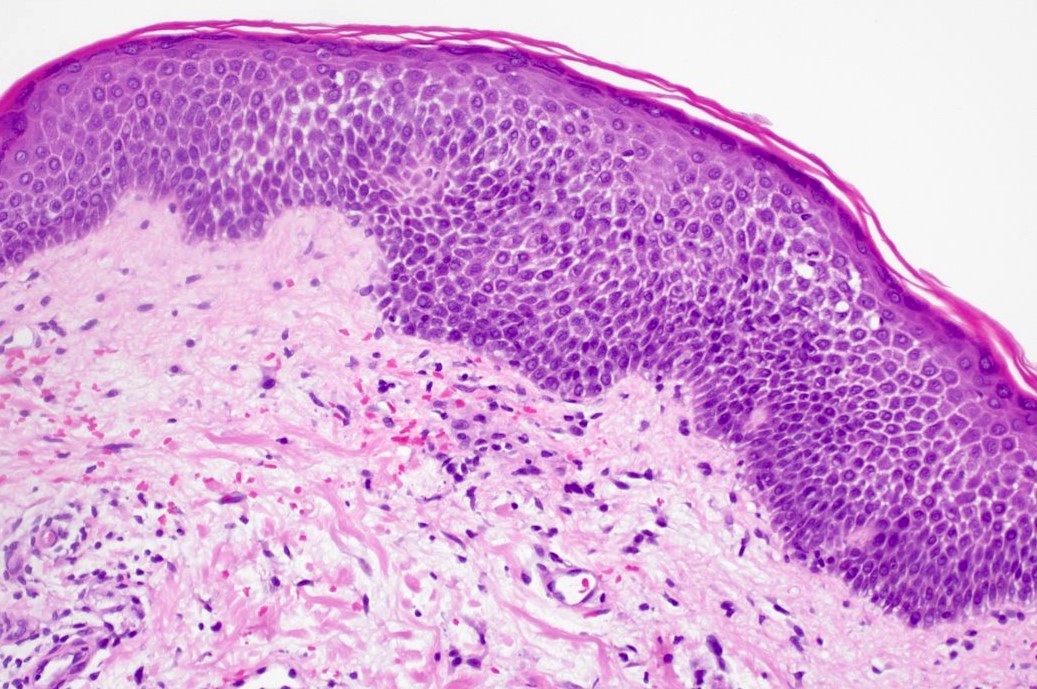
- Pigmented purpuric lichenoid dermatitis of Gougerot and Blum
- Band-like lymphocytic infiltrate in the upper dermis with or without epidermal spongiosis
- Patchy parakeratosis (J Clin Med 2021;10:2283)
- Itching purpura
- Marked spongiosis and neutrophils, hemosiderin can be minimal in early lesions
- Eczematoid purpura of Doucas and Kapetanakis (Ann Dermatol 2015;27:404)
- Epidermal spongiosis and lymphocytic exocytosis are more prominent in this subtype
- Lichen aureus (Br J Dermatol 1985;112:307)
- Band-like lichenoid lymphocytic inflammation at the dermal - epidermal junction with Grenz zone
- Granulomatous pigmented purpura (Am J Dermatopathol 2012;34:746, J Dermatol 1996;23:551)
- Dense granulomatous infiltrate in the papillary dermis, monocyte infiltrate, thickened capillaries and hemosiderin deposition
Microscopic (histologic) images
Immunofluorescence description
- Direct immunofluorescence: deposition of fibrinogen, IgM or C3 in superficial dermal vessels (J Am Acad Dermatol 1991;25:642, J Cutan Pathol 2023 Aug 11 [Epub ahead of print])
Positive stains
- Perls Prussian blue stain, iron (hemosiderin) (Actas Dermosifiliogr (Engl Ed) 2020;111:196)
Molecular / cytogenetics description
- 2 principal categories: polyclonal and monoclonal; ~40% of monoclonal cases have clinical and pathologic features of mycosis fungoides (Am J Clin Pathol 2007;128:218)
Sample pathology report
- Skin, left lower leg, punch biopsy:
- Pigmented purpuric dermatosis (see comment)
- Comment: The histopathologic examination shows mild spongiosis with vacuolization of the basal layer of the epidermis. There is cuffing of the small vessels in the papillary dermis by lymphocytes. Erythrocyte extravasation and superficial hemosiderin deposition in the dermis is present. The overall histologic features are consistent with pigmented purpuric dermatosis.
Differential diagnosis
- Stasis dermatitis:
- Increase in superficial vessels without significant perivascular lymphocytic infiltrate
- Leukocytoclastic vasculitis / cutaneous vasculitis:
- Erythrocyte extravasation with vascular destruction, leukocytoclasia, fibrinoid necrosis, vascular luminal wall fibrin deposition (J Eur Acad Dermatol Venereol 2001;15:15)
- Mycosis fungoides:
- Epidermotropism of atypical lymphocytes without papillary dermal edema
- T cell receptor clonality (Am J Dermatopathol 1997;19:108)
- Pigmented purpura-like variant of mycosis fungoides (Cutis 2014;94:297, Am J Clin Pathol 2007;128:218)
- Prominent cytologic atypia of lymphocytes infiltrating into epidermis, Pautrier microabscesses
- Mycosis fungoides / pigmented purpuric dermatosis overlap: reduction of CD7 and L selectin / CD62L (Am J Clin Pathol 2007;128:218)
- Eczematous dermatitis:
- Epidermal spongiosis
- Eosinophils are often present
- Kaposi sarcoma:
- Vascular proliferation, increase in dermal spindle cells, vascular slits, lymphoplasmacytic infiltrate (Cutis 1983;31:406)
- HHV8 stain is positive
Additional references
Practice question #1
- A 38 year old woman with an unremarkable medical history presents with a 2 week history of bilateral red macules on the shins. Physical examination reveals pinpoint petechiae resembling grains of cayenne pepper on her legs. CBC and coagulation studies are within normal limits. Biopsy shows a superficial perivascular lymphocytic infiltrate without luminal wall fibrin deposition. Mild epidermal spongiosis, erythrocyte extravasation and siderophages are present. What is the most compatible diagnosis in this patient?
- Cutaneous vasculitis
- Drug eruption
- Mycosis fungoides
- Schamberg disease
Practice answer #1
D. Schamberg disease. This patient has a progressive pigmented dermatosis, consistent with Schamberg disease. Answer A is incorrect because there is no evidence of cutaneous vasculitis, which shows erythrocyte extravasation with vascular destruction, leukocytoclasia, fibrinoid necrosis and vascular luminal wall fibrin deposition. Answer B is incorrect because drug reactions would have a relevant medical history and often show eosinophils. Answer C is incorrect because although some forms of Schamberg disease may overlap with mycosis fungoides, these biopsies show cytologic atypia of epidermotropic lymphocytes and Pautrier microabscesses, which were not present here.
Comment Here
Reference: Pigmented purpuric dermatosis
Comment Here
Reference: Pigmented purpuric dermatosis
Practice question #2
- Which of the following is true about pigmented purpuric dermatoses?
- Direct immunofluorescence studies show IgA depositions in dermal vessels
- Early stages of mycosis fungoides may have histologic overlap
- Fibrinoid necrosis of the vessel wall is a characteristic feature
- Hyperplasia of endothelial cells and an increase in superficial vessels are frequently observed
Practice answer #2
B. Early stages of mycosis fungoides may have histologic overlap with pigmented purpuric dermatoses. Answer C is incorrect because fibrinoid necrosis of the vessel wall is a feature of cutaneous vasculitis and should not be present in pigmented purpuric dermatoses. Answer D is incorrect because hyperplasia of endothelial cells and an increase in superficial vessels are seen in stasis dermatitis, which should be considered in the differential diagnosis. Answer A is incorrect because IgA depositions are seen in the dermal vessels of IgA and lupus vasculitis. PPD is not an immune complex mediated disease.
Comment Here
Reference: Pigmented purpuric dermatosis
Comment Here
Reference: Pigmented purpuric dermatosis