Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Hamilton C, Timmerman M, Asadbeigi SN. Nevus lipomatosus superficialis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticnls.html. Accessed September 24th, 2025.
Definition / general
- Benign hamartoma of the skin with mature fat tissue between collagen bundles within the dermis (J Family Med Prim Care 2022;11:4045)
- Either solitary or multiple (classic form)
Essential features
- Benign hamartoma of the skin
- Consists of mature fat tissue located in the superficial dermis without connection to the subcutaneous fat
- Excision is curative and rarely recurs
- Considered to be a developmental anomaly or hamartoma (Arch Plast Surg 2024;51:196)
- Subtypes include classical (multiple) and solitary (J Dermatol 2024;51:56)
Terminology
- Also called nevus lipomatosus cutaneous superficialis and dermolipoma (J Family Med Prim Care 2022;11:4045)
- First described in 1921 by Hoffmann and Zurhelle; it is also called nevus lipomatosus of Hoffman-Zurhelle (Br J Dermatol 1975;93:121)
- Nevus angiolipomatosus of Howell: a term used in lesions developed in infancy (Iran J Med Sci 2014;39:304)
ICD coding
- ICD-10
- D17.1 - benign lipomatous neoplasm of skin and subcutaneous tissue of trunk
- D17.2 - benign lipomatous neoplasm of skin and subcutaneous tissue of limb
- D17.3 - benign lipomatous neoplasm of skin and subcutaneous tissue of other and unspecified sites
- D17.39 - benign lipomatous neoplasm of skin and subcutaneous tissue of other sites
- D17.30 - benign lipomatous neoplasm of skin and subcutaneous tissue of unspecified sites
- Q82.5 - congenital nonneoplastic nevus
Epidemiology
- Uncommon
- No gender predilection
- Classic (multiple) subtype is present at birth or during the first 3 decades of life
- Solitary subtype appears in the third to sixth decade of life with a single nodule or pedunculated or sessile papule (Arch Plast Surg 2024;51:196)
- No familial tendency
Sites
- Most commonly occurs on the lower back, buttocks and thighs (Cureus 2023;15:e50388)
Pathophysiology
- Theories on the pathogenesis include
- Developmental malformation
- Degenerative changes in the dermal connective tissue lead to adipose metaplasia (An Bras Dermatol 2017;92:711)
- Alterations in adipose tissue development due to genetic or environmental factors (An Bras Dermatol 2017;92:711)
- Growth of fat cells from the walls of dermal blood vessels (Cureus 2023;15:e50388)
Clinical features
- Could be present at birth
- Classical form
- Lower back, buttocks and lower extremities
- Multiple papules or nodules in a zosteriform pattern that can coalesce in a plaque (Iran J Med Sci 2014;39:304)
- Solitary type: can appear anywhere and usually appears during the third to sixth decade of life
- Asymptomatic lesions could be ulcerated due to trauma or ischemia
- Coexisting lesions could be café au lait macules, hypertrichosis or concurrent comedones (An Bras Dermatol 2017;92:711)
Diagnosis
- Clinical and histopathologic examination
Radiology description
- Imaging is not frequently performed and the diagnosis is done based on the clinical and histopathological findings
- Ultrasound findings: ill defined hyperechoic mass in the dermis with strong posterior echo attenuation (J Dermatol 2024;51:56)
- Computed tomography (CT) findings: may appear as an elevated lesion with slightly increased fat attenuation (Skeletal Radiol 2020;49:129)
Prognostic factors
- Benign
- Does not recur after excision (Arch Plast Surg 2024;51:196)
Case reports
- 11 year old boy who presented with a lower back swelling (J Family Med Prim Care 2022;11:4045)
- 38 year old woman with nevus lipomatosis superficialis of the vulva (Cureus 2023;15:e50388)
- 41 year old man with multinodular lesion near right auricle (Arch Plast Surg 2024;51:196)
- 64 year old man with a lesion on his nose (Cureus 2024;16:e60902)
Treatment
- Excision; very rare to recur
- Less common therapies include intralesional injections, cryotherapy and carbon dioxide laser therapy
Clinical images
Gross description
- Skin with soft yellow papules (Cureus 2024;16:e60902)
- Pedunculated nodule
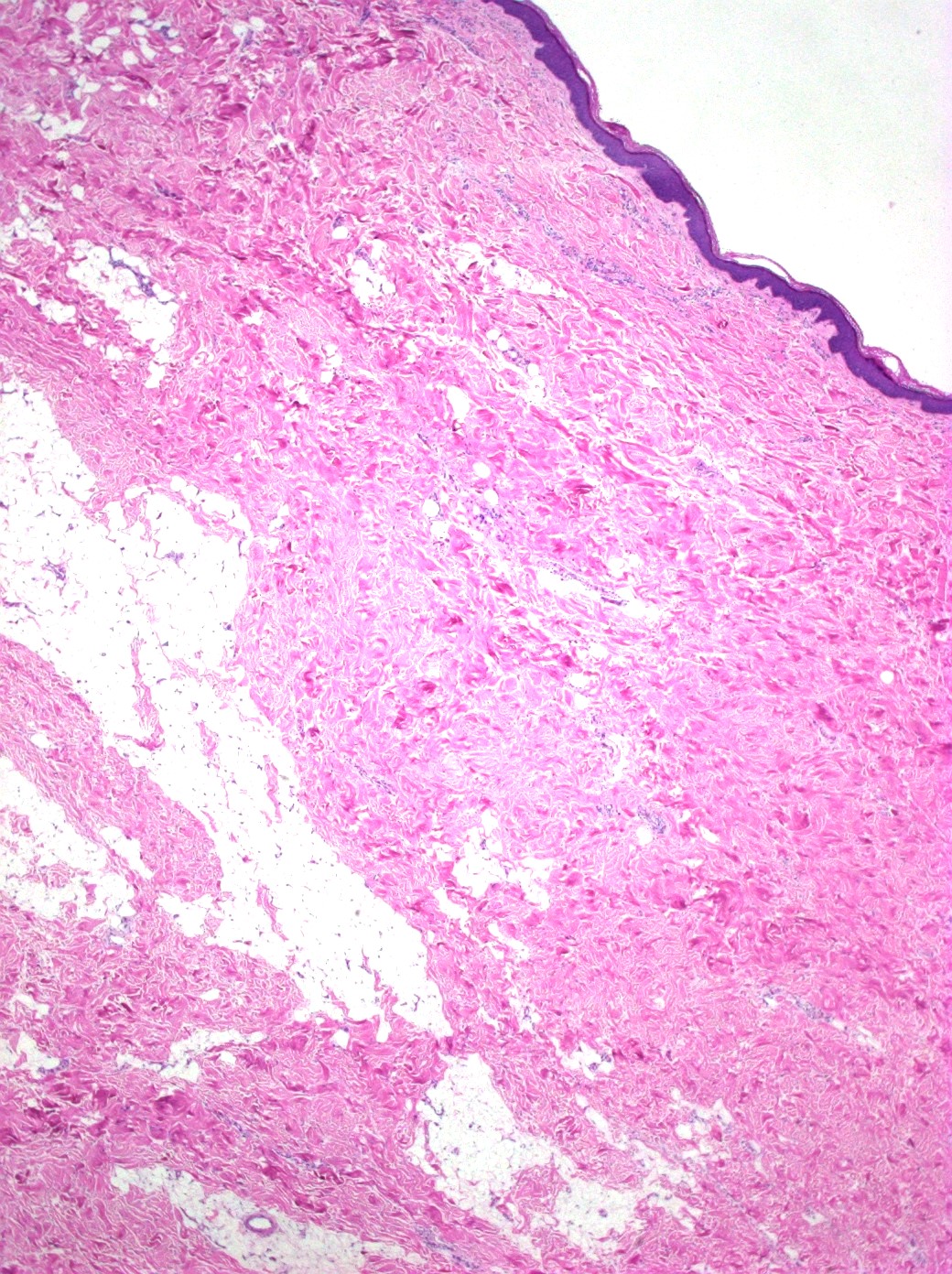
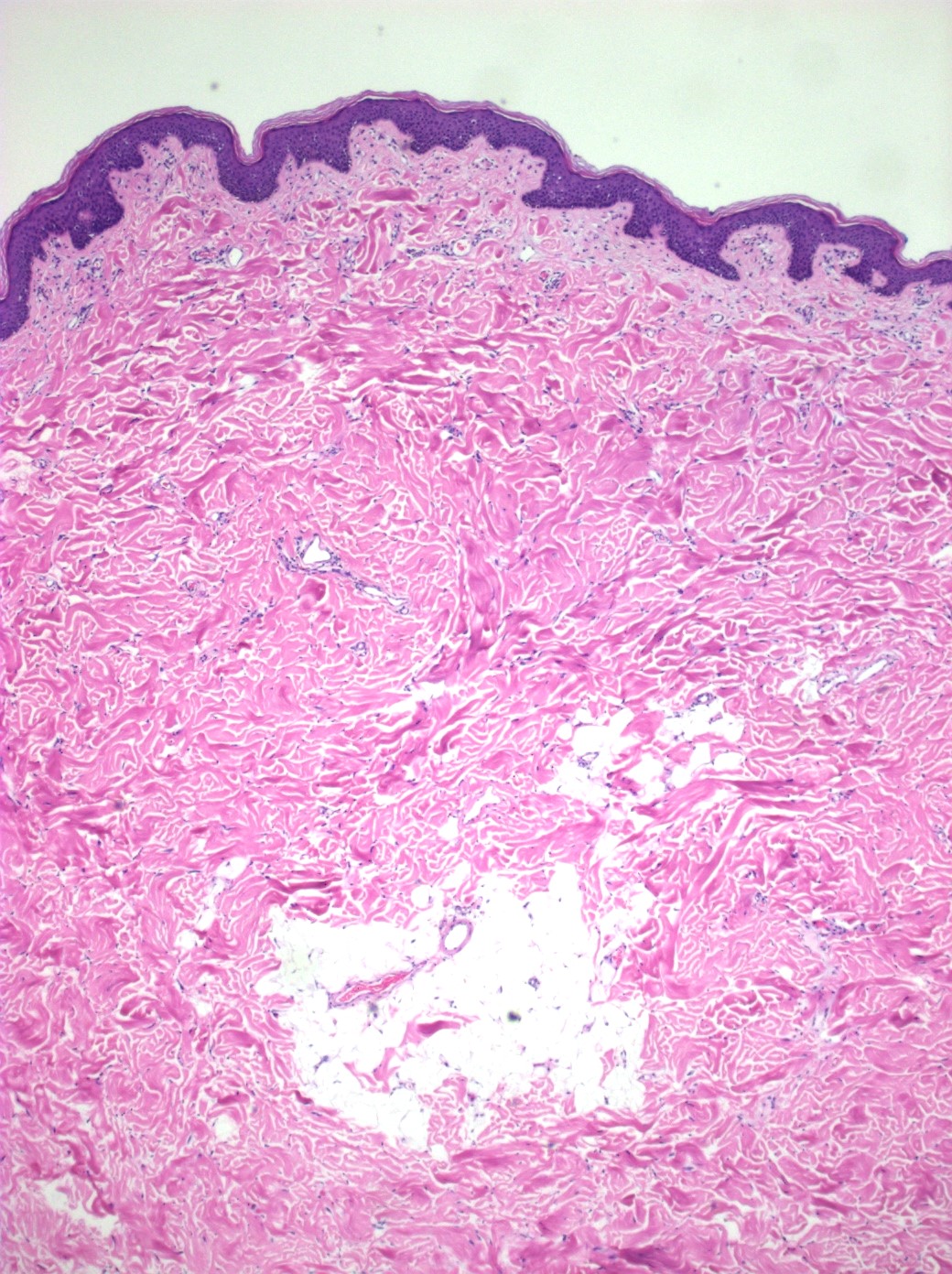
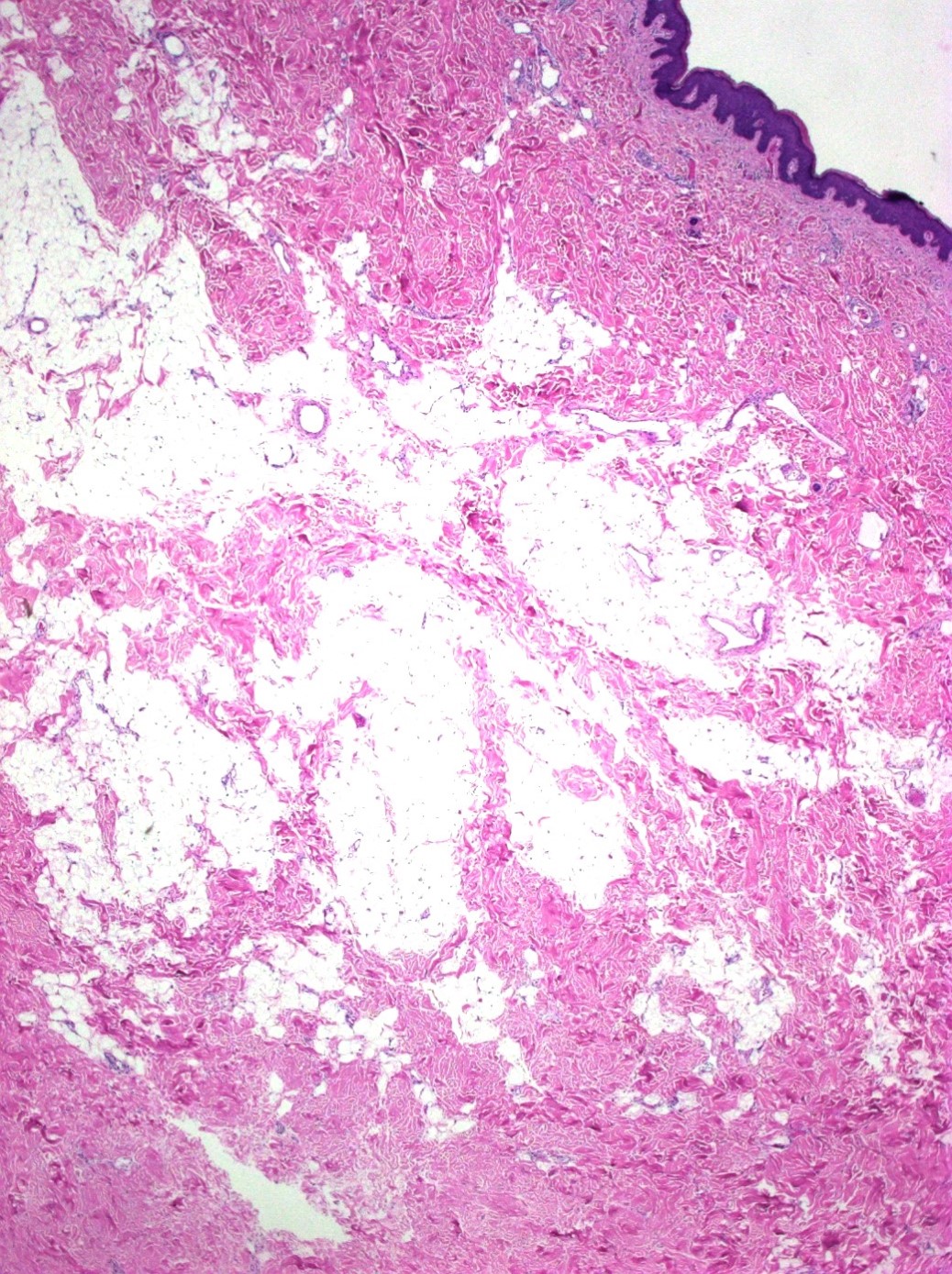
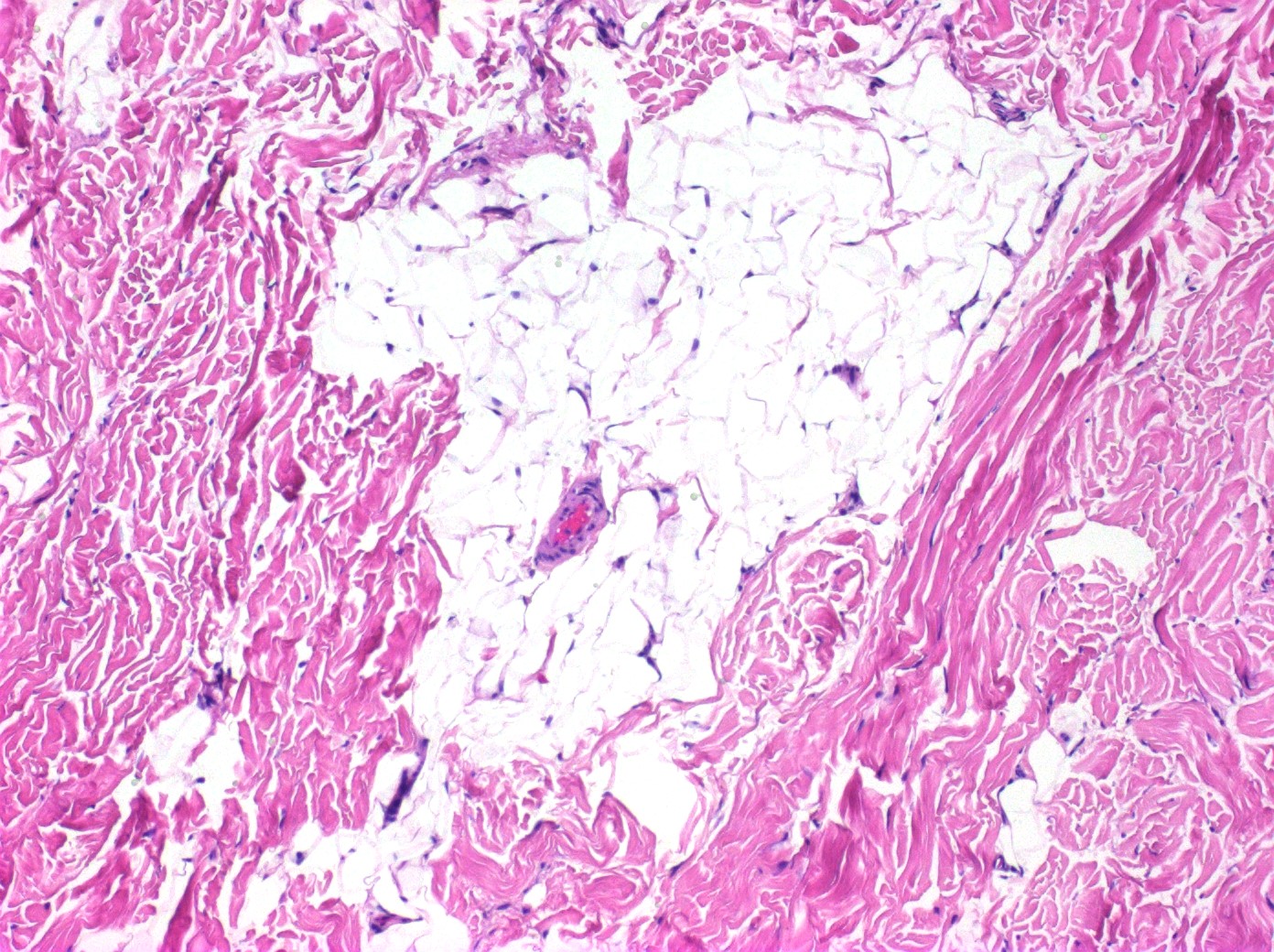
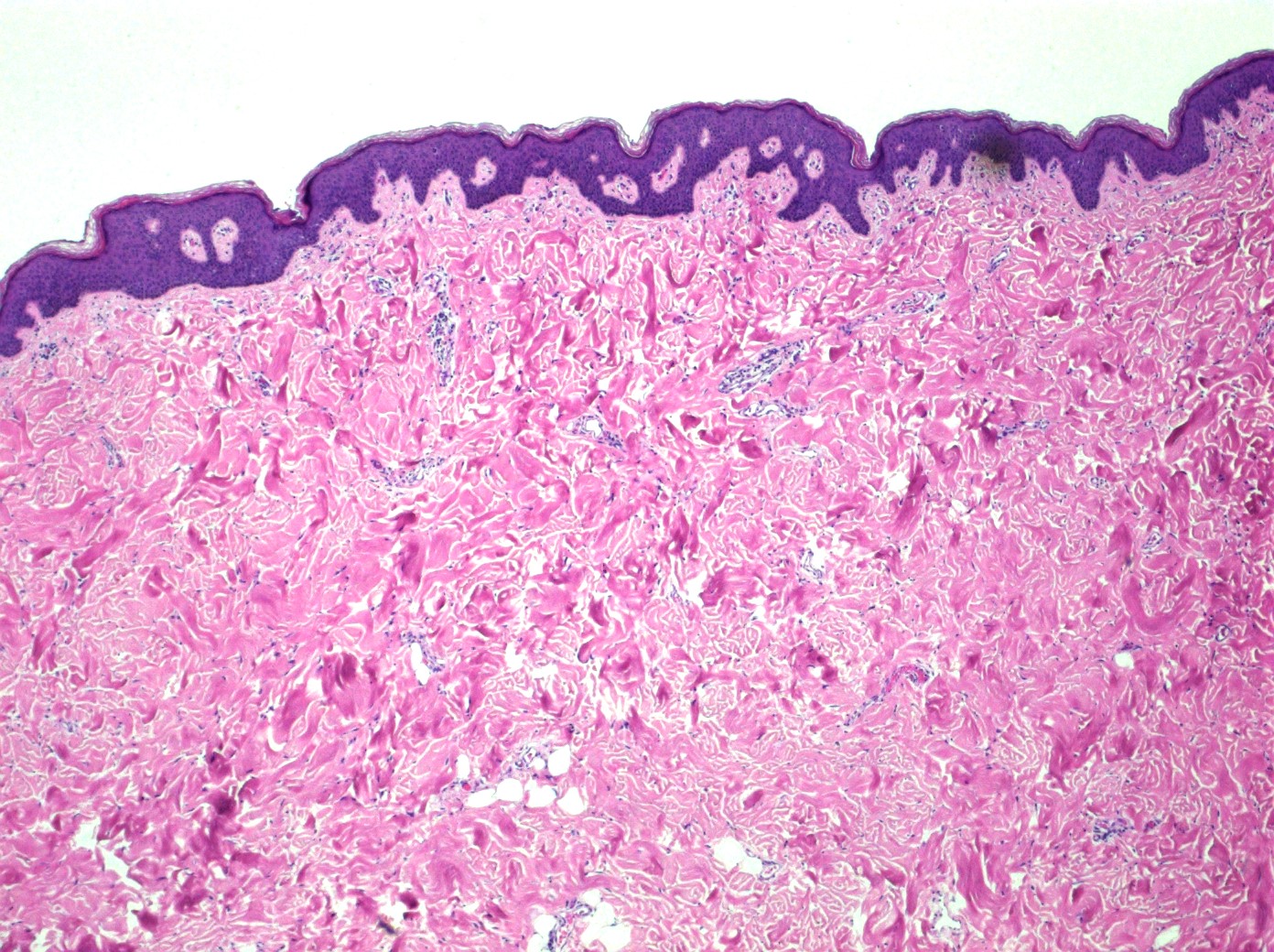
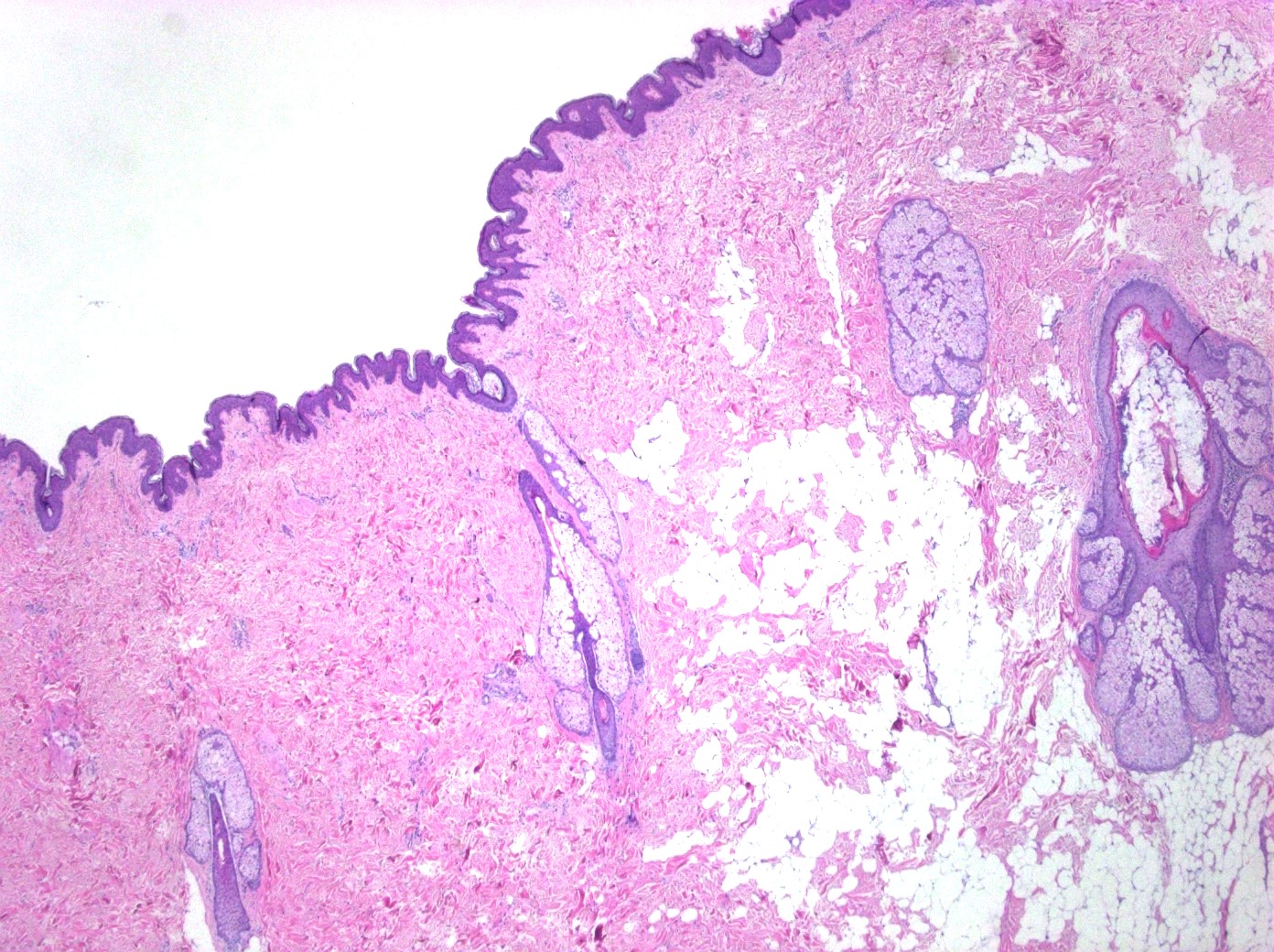
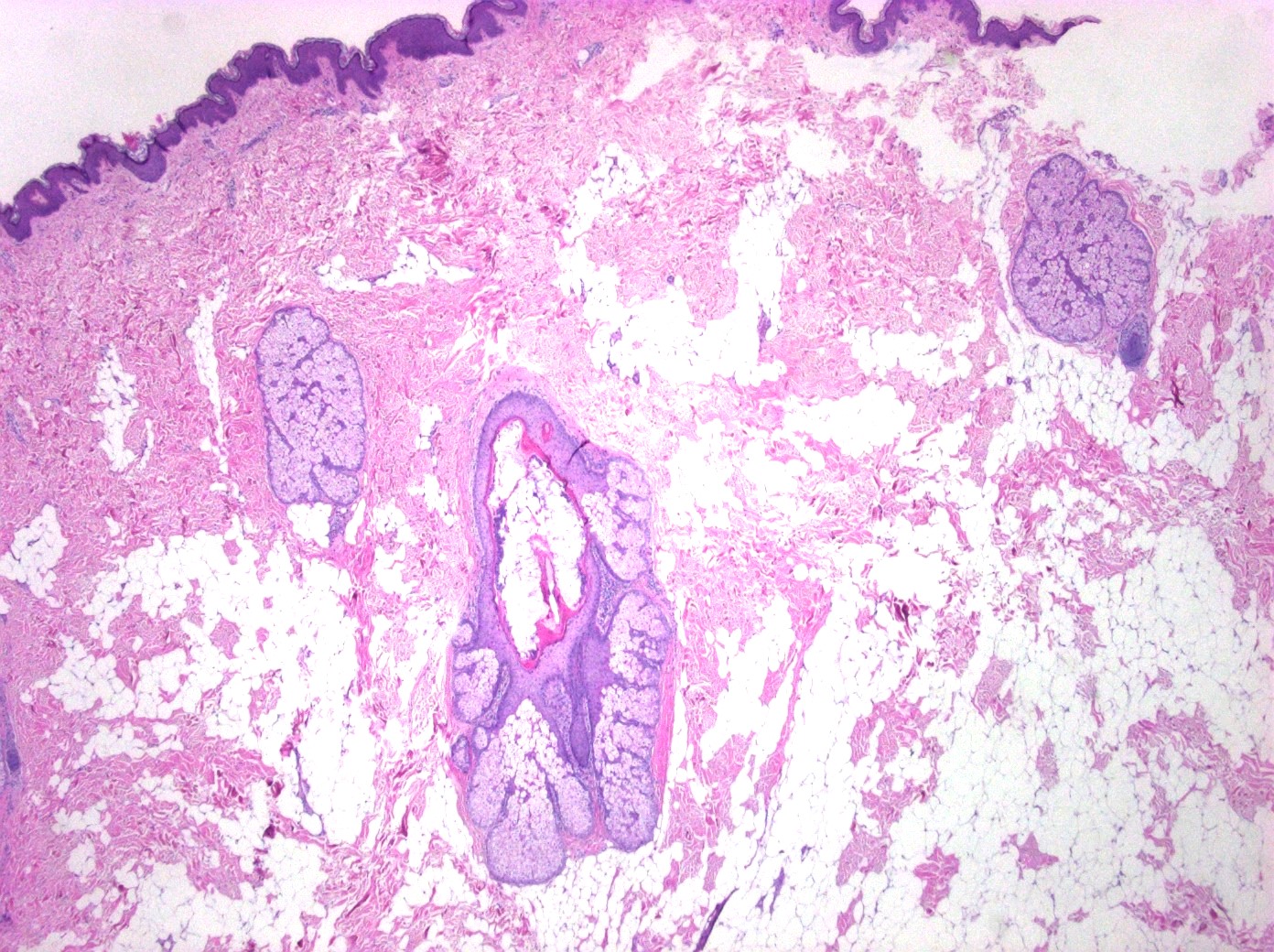
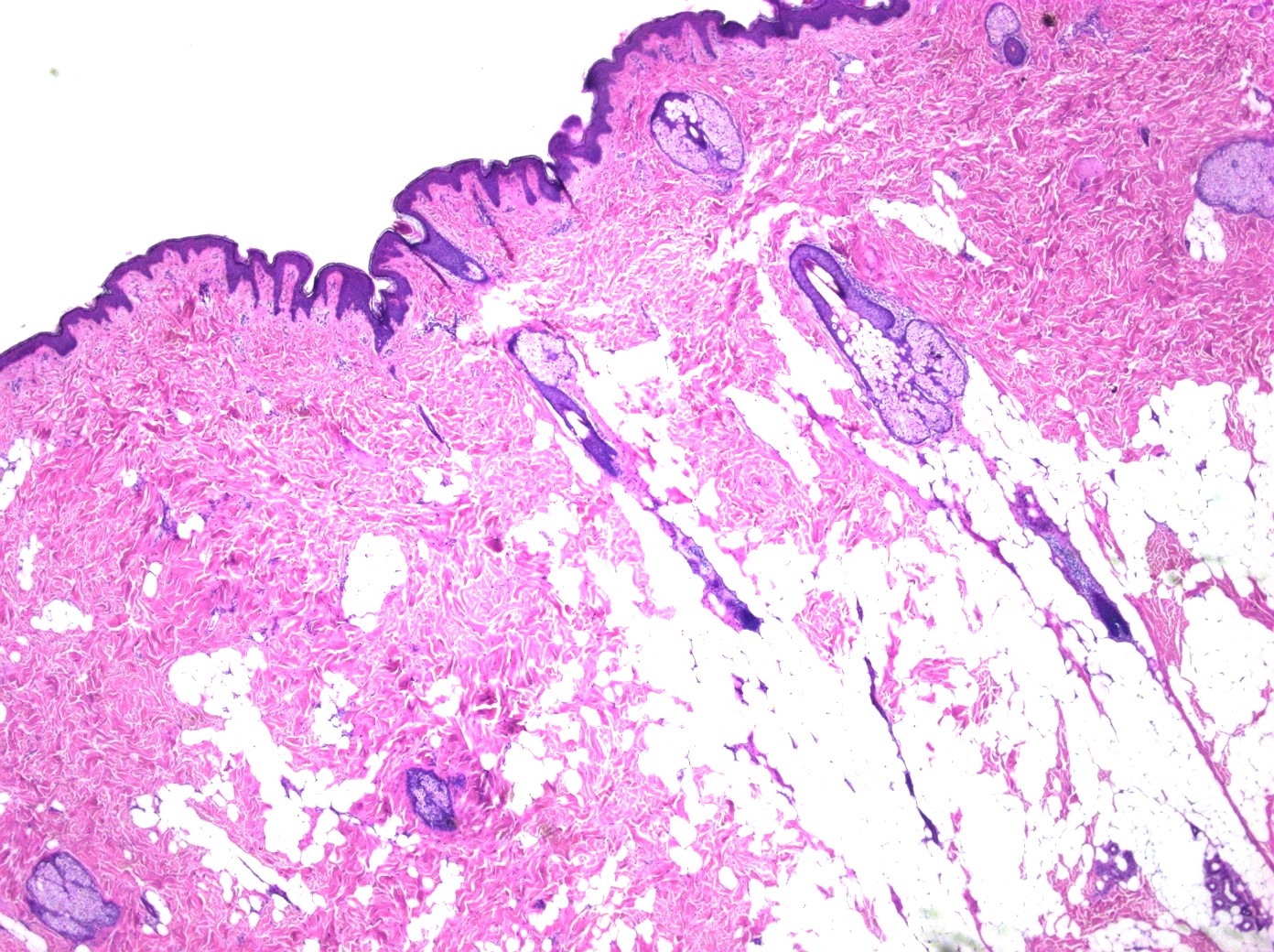
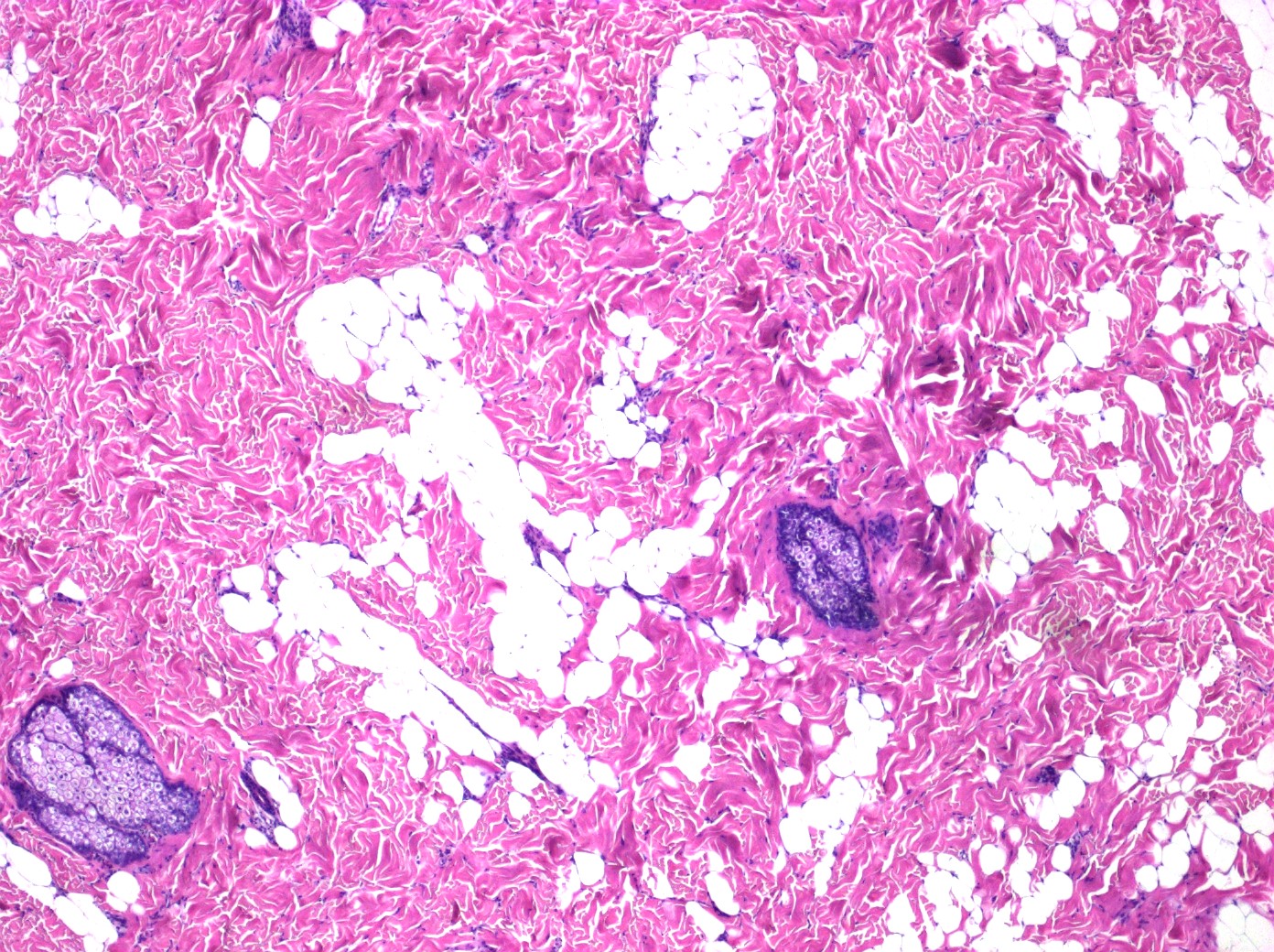
Microscopic (histologic) description
- Mature adipocytes in dermis
- No encapsulation or connection with subcutaneous fat
- Usually, the number of adnexal structures is reduced (Patholog Res Int 2011;2011:105973)
- Dilated and small caliber blood vessels within the mature adipocytes (Indian J Dermatol 2022;67:480)
- Adipocytes usually form small aggregates around the blood vessels or eccrine glands
- May also appear as isolated adipocytes between collagen bundles (J Dermatol 2024;51:56)
- Increased density of collagen fibers, fibroblasts and perivascular, spindle shaped cells can be seen in some cases
- Overlying epidermis can show hyperkeratosis or acanthosis, elongation of rete ridges and increased pigmentation in the basal cells (An Bras Dermatol 2017;92:711, Indian J Dermatol 2022;67:480)
- Cases with focal myxoid degeneration are reported (Indian J Dermatol 2022;67:480)
- In some cases, immature fat cells present as spindle cells, mimicking other cutaneous spindle cell neoplasms
Microscopic (histologic) images
Contributed by Chad Hamilton, D.O.
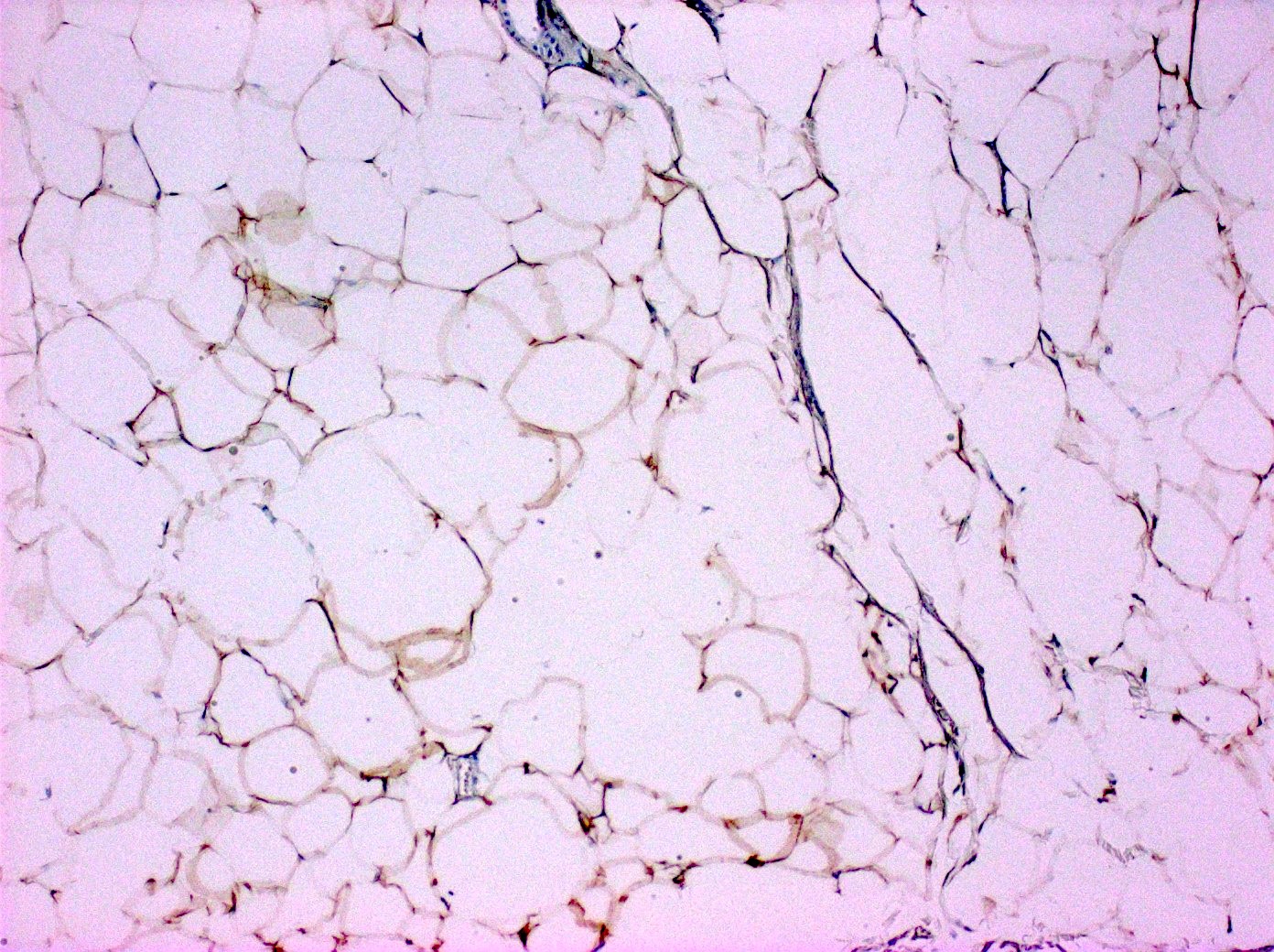
Positive stains
- S100: in adipocytes
- CD34: in mesenchymal cells
- CD1a: scattered positive cells
- Factor XIIIa: scattered positive cells
- References: Am J Dermatopathol 2015;37:704, J Cutan Pathol 2024;51:119
Videos
Nevus lipomatosus superficialis
Sample pathology report
- Skin, right upper leg, shave biopsy:
- Nevus lipomatosus superficialis
- Microscopic description: Specimen consists of a large polypoid lesion covered by a slightly acanthotic epidermis. At the core of the polyp, one finds haphazardly arranged collagen bundles intermingled with lobules of mature lipocytes and small blood vessels. Atypical features are not identified.
Differential diagnosis
- Fibroepithelial polyp:
- Conventionally lacks adipose tissue
- There is poor consensus for fibroepithelial polyp-like lesions that contain adipocytes
- Some may call pedunculated lesions with adipocytes lipofibroma unless they occur on the back or buttocks, in which case they will call it nevus lipomatosus superficialis
- Others will just call it nevus lipomatosis superficialis even if it is polypoid or not in these locations
- Neurofibroma:
- Lack of mature adipocytes
- S100 shows strong scattered positivity in spindle shaped cells
- Wavy serpentine nuclei
- Mast cells are commonly present
- Nevus sebaceous:
- Well circumscribed and complex proliferation and alteration of epidermis and adnexal structures
- Often has verrucous epidermal acanthosis
- Focal dermal hypoplasia or Goltz syndrome:
- Syndromic condition with multisystemic clinical findings
- Shows depletion of collagen within the dermis and skin appendages (Indian Dermatol Online J 2012;3:196)
- Dermal collagen is replaced by adipose tissue
- Lipofibromas:
- Fat cells are present but the skin appendages are absent (Indian Dermatol Online J 2012;3:196)
- Lipoma:
- Located subcutaneously
- May be encapsulated
Practice question #1
Practice answer #1
D. Nevus lipomatosus superficialis. Epidermis is seen in the image with an aggregate of mature adipocytes seen in the superficial reticular dermis, which describes nevus lipomatosus superficialis. Answer B is incorrect because there are no lipoblasts, myxoid or desmoplastic stroma or spindle shaped cells in the stroma. Answer C is incorrect because there are no wavy or serpentine nuclei. Answer E is incorrect because nevus sebaceous would show a proliferation of adnexal structures. Answer A is incorrect because keloid would show closely packed collagen.
Comment Here
Reference: Nevus lipomatosus superficialis
Comment Here
Reference: Nevus lipomatosus superficialis
Practice question #2
A patient presented with a clinical diagnosis of skin tag which was later signed out as nevus lipomatosis superficialis (seen above). Which of the following best reflects the prognosis of this entity?
- Commonly recurs after excision
- Excision is curative
- Frequent metastasis to the bone
- Requires adjuvant chemotherapy in most cases
- Requires radiotherapy in many cases
Practice answer #2
B. Excision is curative. Nevus lipomatosus superficialis is a benign entity. There are no cases of recurrence reported and excision is curative.
Answer A is incorrect because nevus lipomatosus superficialis rarely recurs. Answer D is incorrect because nevus lipomatosus superficialis is a benign entity and does not require chemotherapy for treatment. Answer E is incorrect because radiotherapy is not used in treating nevus lipomatosus superficialis; the mainstay of treatment is excision. However, cryotherapy, carbon dioxide or intralesional injections are utilized occasionally. Answer C is incorrect because nevus lipomatosus superficialis is a benign entity and does not metastasize anywhere.
Comment Here
Reference: Nevus lipomatosus superficialis
Comment Here
Reference: Nevus lipomatosus superficialis