Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Siegmund S, Acosta A. Germ cell neoplasia in situ. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisitgcn.html. Accessed August 1st, 2025.
Definition / general
- Common precursor of type II germ cell tumors (i.e., seminomas and most postpubertal nonseminomatous germ cell tumors of the testis) (Nat Rev Cancer 2019;19:522)
- Neoplastic gonocyte-like cells with latent totipotent (naive) developmental potential, located in the spermatogonial niche of seminiferous tubules
Essential features
- Precursor for a subset of adult germ cell tumors (in WHO classification, referred to as germ cell neoplasia in situ [GCNIS] associated)
- Associated with uncorrected cryptorchidism, ambiguous genitalia, infertility and a prior history of contralateral postpubertal germ cell tumor or GCNIS
- Presence in testicle from a patient with extragonadal germ cell tumors may represent a burnt out germ cell tumor
- Difficult to diagnose in infantile / prepubertal testis due to morphologic and immunohistochemical overlap with normal or delayed maturation
- Frequently demonstrate aneuploidy but lack isochromosome 12p seen in invasive adult germ cell tumors
Terminology
- Germ cell neoplasia in situ (GCNIS) was introduced in the 2016 edition of WHO's Tumors of the Urinary System and Male Genital Organs
- Intratubular germ cell neoplasia (ITGCN) (not recommended / obsolete)
- Intratubular germ cell neoplasia of unclassified type (not recommended / obsolete)
- Carcinoma in situ of the testis (not recommended)
ICD coding
- ICD-O: 9064/2 - intratubular malignant germ cells
- ICD-10: C62 - malignant neoplasm of testis
- With relevant subcodes (e.g., C62.9 - malignant neoplasm of testis, unspecified whether descended or undescended)
- ICD-11: 2C80.2 & XH8AD3 - germ cell tumor of testis & intratubular malignant germ cells
Epidemiology
- Found at higher rates in patients with uncorrected cryptorchidism (2 - 4%), ambiguous genitalia (25%) or infertility (1%) (Int J Cancer 1999;83:815)
Sites
- Frequent in seminiferous tubules of testicles involved by postpubertal germ cell tumors and sometimes represents the only residual manifestation (e.g., burnt out germ cell tumor) (Cancer 1981;47:2660, APMIS 2003;111:32, Am J Surg Pathol 2007;31:1045, Eur Urol 2007;51:175)
Pathophysiology
- Thought to arise from incompletely differentiated primordial germ cells, which undergo whole genome duplication events followed by recurrent losses of chromosome arms and whole chromosomes, thus creating an aneuploid state with subsequent additional mutations (e.g., KIT, KRAS) in a subset (Br J Cancer 2001;85:213, Cell Rep 2018;23:3392)
- KIT mutations that occur early (i.e., after genome duplication) are thought to result in a subset of seminomas with global genomic hypomethylation that do not differentiate to other histologic subtypes
- Believed to represent the universal precursor of type II germ cell tumors, which represent ~95% of germ cell tumors in postpubertal males (e.g., seminoma, embryonal carcinoma, choriocarcinoma, some teratomas and yolk sac tumors)
- Show overexpression of embryonic transcription factors that increase proliferation and suppress apoptosis
Etiology
- Almost universally present in background seminiferous tubules of testis involved by adult germ cell tumor (Cancer 1981;47:2660)
- Occasionally also in contralateral testis (Eur Urol 2007;51:175, Int J Cancer 1999;83:815)
- May be seen as residual finding in a setting of burnt out adult germ cell tumor (Ann Oncol 2003;14:1412)
Clinical features
- Microlithiasis detected by ultrasonography in patients undergoing workup for infertility may be associated with a higher risk of GCNIS (especially if bilateral) (J Urol 2004;171:158)
- Testicular biopsies can be offered to patients with microlithiasis and 1 additional risk factor for GCNIS (Andrology 2020;8:1736)
Diagnosis
- Diagnosis requires histologic examination (testicular biopsy, orchiectomy)
- Biopsy of contralateral testis in patients with adult germ cell tumor is more common in Europe than North America
Laboratory
- There are no specific serum marker findings (World J Urol 1996;14:S55)
Radiology description
- There are no specific imaging findings (World J Urol 1996;14:S55)
Prognostic factors
- ~50% of cases progress to invasive adult germ cell tumor within 5 years and 90% within 7 years (Br Med J (Clin Res Ed) 1986;293:1398)
Case reports
- 30 year old man with infertility and bilateral testicular microlithiasis (Int J Surg Pathol 2008;16:21)
- 33 year old man with progressive painless testicular swelling (Urol Case Rep 2022;42:101997)
- 42 year old man with massive retroperitoneal mass and multifocal right testicular mass (Radiol Case Rep 2022;17:2732)
Treatment
- Orchiectomy if not already performed or close surveillance with routine monitoring for progression
- Chemotherapy does not reduce the risk of progression
- Low dose radiotherapy may be considered for contralateral GCNIS in patients with localized adult germ cell tumor (Ann Oncol 1998;9:657, BMC Urol 2013;13:71, Oncology 2009;77:33)
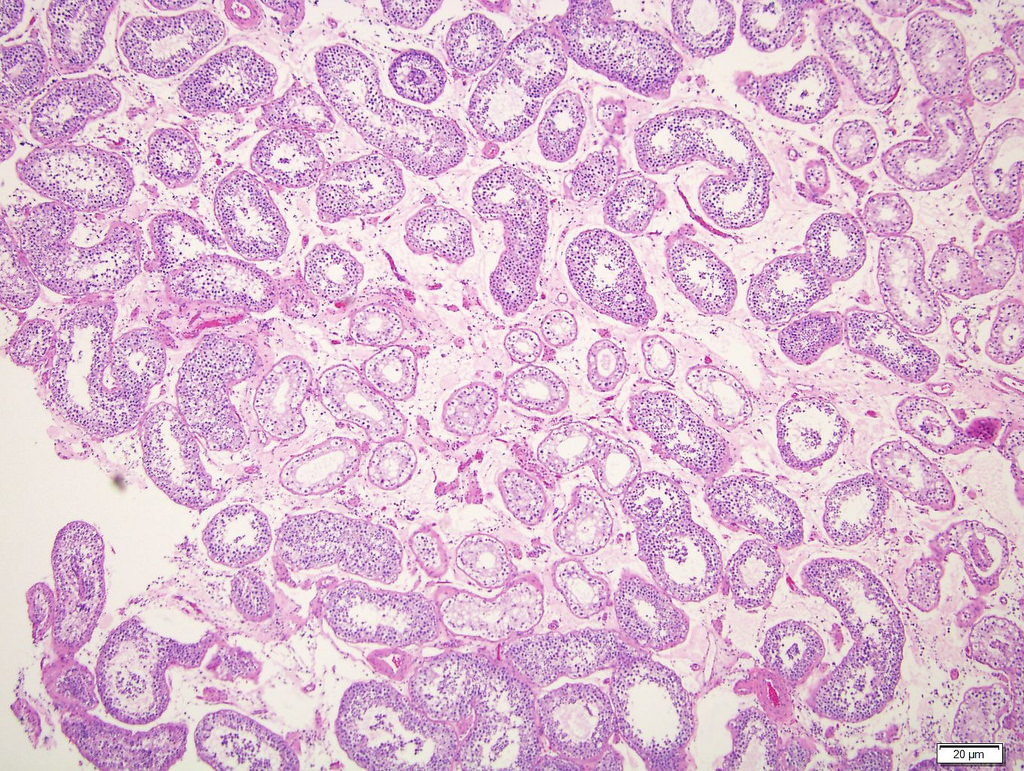
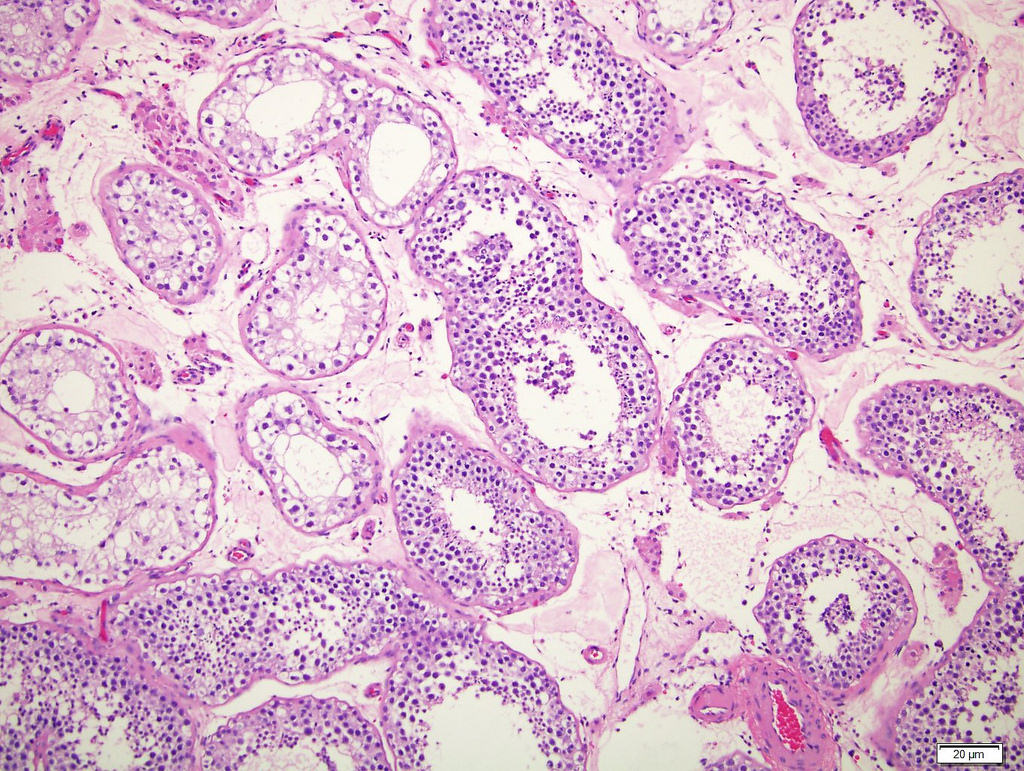
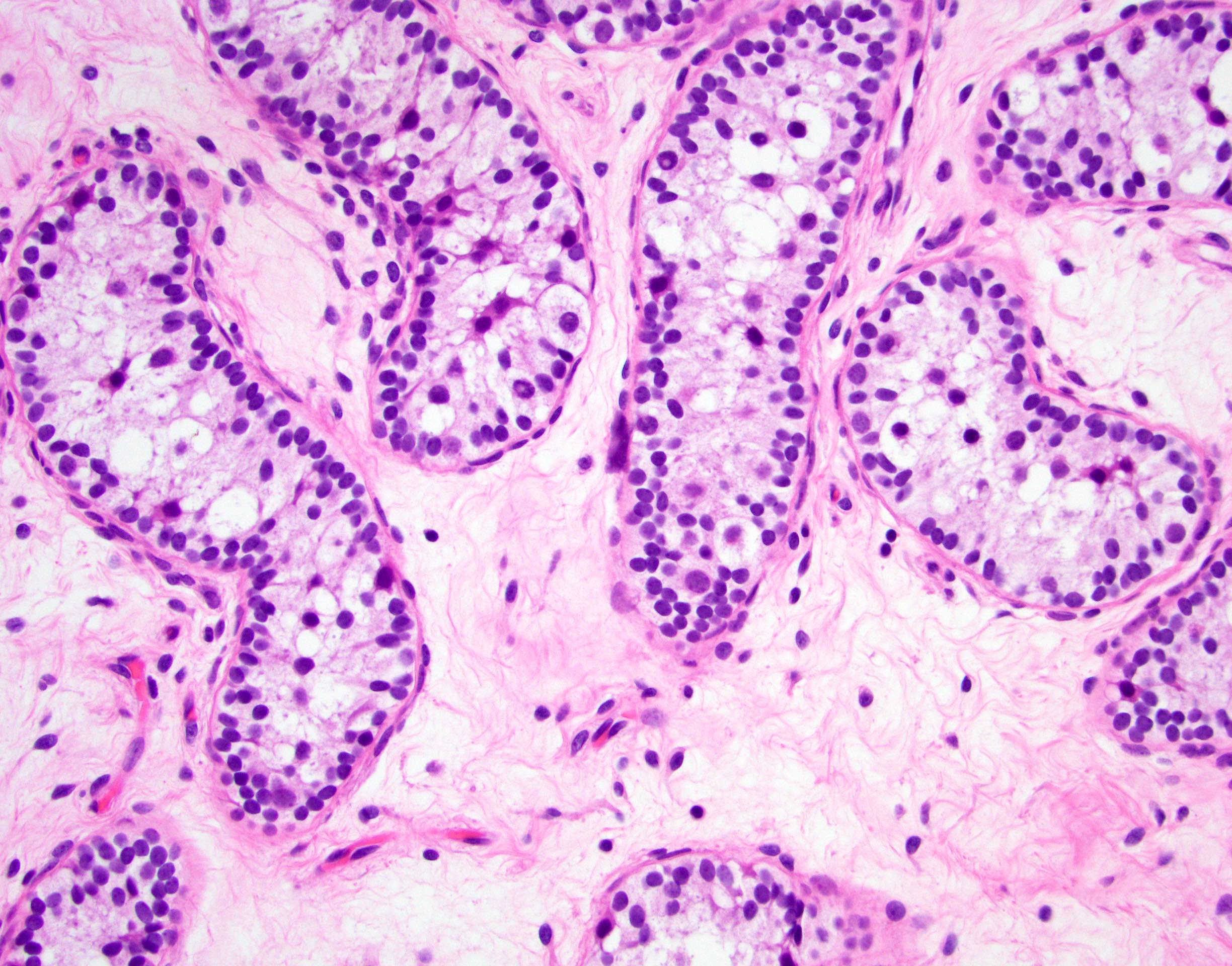
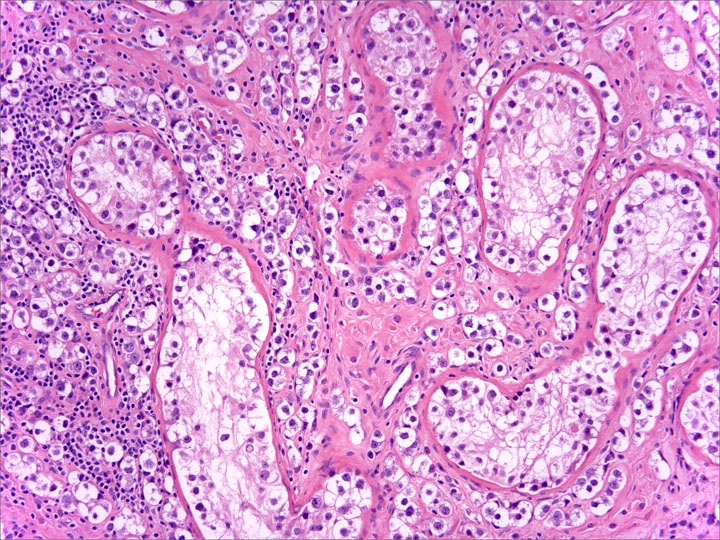
Microscopic (histologic) description
- Neoplastic cells located along the basement membrane of seminiferous tubules (spermatogonial niche)
- Cells are large atypical gonocyte-like with abundant clear cytoplasm and large (10 - 11 μm) hyperchromatic nuclei with coarse chromatin, angulated borders and prominent nucleoli; these cells are similar in appearance as seminoma (Histopathology 1978;2:157)
- Affected seminiferous tubules frequently have a thickened basement membrane / peritubular hyalinization and lack spermatogenic maturation
- Can spread in pagetoid fashion into rete testis, along the plane between the rete epithelium and the basement membrane
Microscopic (histologic) images
Contributed by Stephanie Siegmund, M.D., Ph.D., Maria Tretiakova, M.D., Ph.D., Alexander Subtelny, M.D., Ph.D. and Michelle Hirsch, M.D., Ph.D.
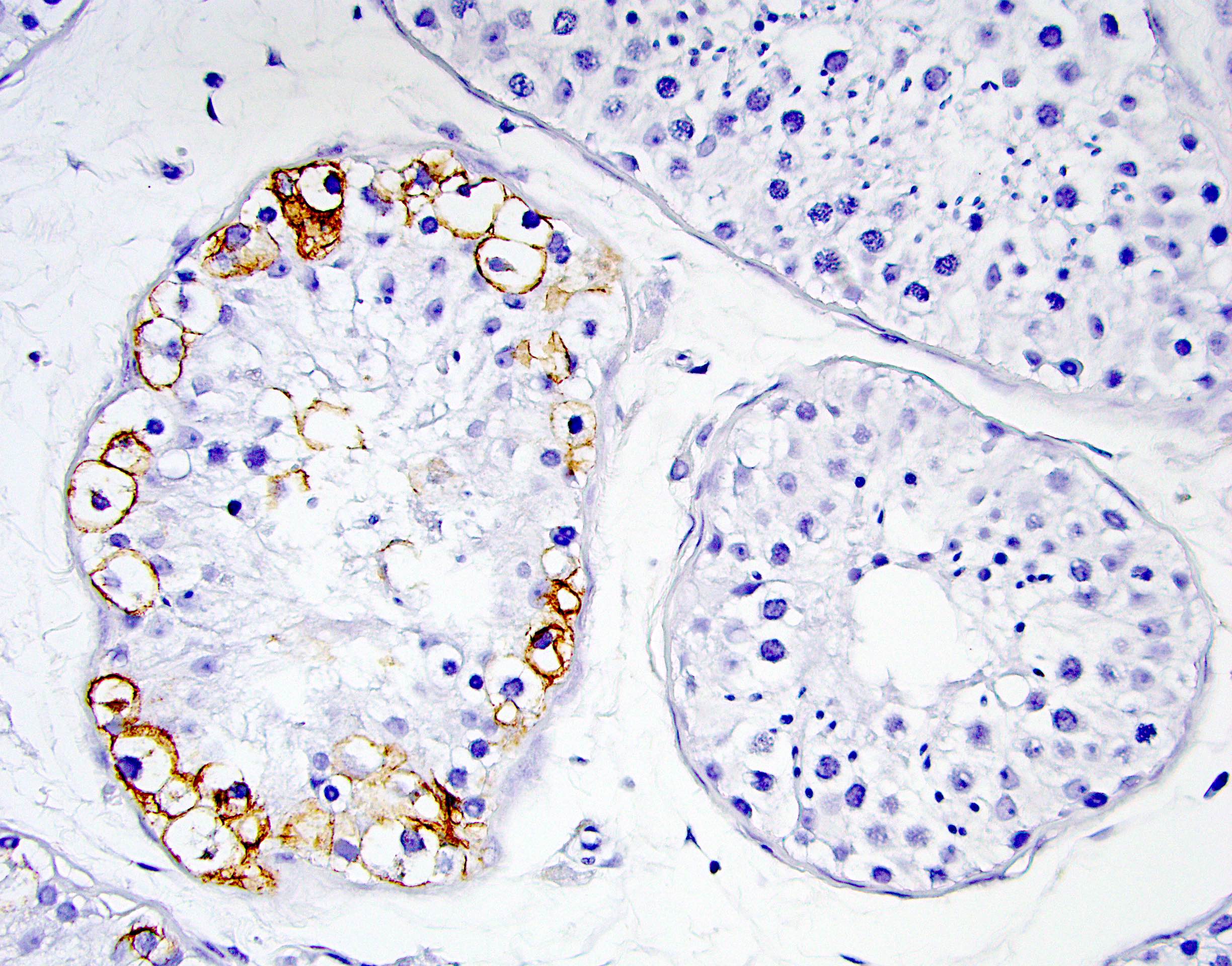
Positive stains
- OCT 3/4 (Cancer Res 2003;63:2244, Clin Cancer Res 2004;10:8544)
- SALL4
- Podoplanin / D2-40
- KIT / c-KIT / CD117
- SOX17 (J Pathol 2008;215:21)
- NANOG
- LIN28A
- AP2 gamma (Clin Cancer Res 2004;10:8521)
- PLAP (Mod Pathol 1988;1:475, Int J Androl 2011;34:e160)
- IHC can be helpful for diagnosis in difficult cases (Int J Androl 2009;32:666)
- Important consideration: c-KIT and PLAP seem to be frequently positive in normal spermatogonia beyond infantile age; therefore, D2-40 and OCT 3/4 are probably better markers for GCNIS given their higher specificity (Pediatr Surg Int 2020;36:1249)
Negative stains
Molecular / cytogenetics description
- Aneuploid (polyploid) with gain of additional findings at the time of invasion (e.g., isochromosome 12p is seen in invasive disease but not in GCNIS) (Genes Chromosomes Cancer 2003;38:117)
- Aneuploidy, absence of isochromosome 12p can be demonstrated by FISH, single nucleotide polymorphism (SNP) array or karyotype (Am J Surg Pathol 2020;44:e66)
Molecular / cytogenetics images
Sample pathology report
- Right testicle and spermatic cord, radical orchiectomy:
- Testis with fibrosis, seminiferous tubular atrophy and scattered foci of intratubular germ cell atypia, consistent with germ cell neoplasia in situ (GCNIS)
- No invasive tumor is identified
- Spermatic cord, epididymis and rete testis are negative for tumor
- No lymphovascular invasion is identified
- AJCC classification (8th edition): pTis N0
Differential diagnosis
- Infantile or prepubertal testis with gonocytes with normal or delayed maturation:
- Normal immature gonocytes are positive for OCT 3/4, KIT and PLAP by IHC but are located basally and centrally
- Difficult to differentiate from GCNIS in patients < 6 months old (Scand J Urol 2016;50:74, J Urol 2014;191:1084)
- Intratubular seminoma:
- Large atypical gonocyte-like cells filling the seminiferous tubules without invasion
- Seminoma with microinvasion:
- Subtle single cells and small clusters of large atypical gonocyte-like cells with foci of microinvasion beyond the basement membrane into testicular parenchyma
- Immunostains (OCT 3/4, KIT / c-KIT / CD117, D2-40, PLAP) can highlight cells that may be overlooked on H&E
Additional references
Practice question #1
Practice answer #1
A. Embryonal carcinoma. Germ cell neoplasia in situ (GCNIS) is associated with type II germ cell tumors (e.g., seminoma, embryonal carcinoma) and of the options listed embryonal carcinoma is the only option that fits this designation. Answers B, C, D and E are incorrect because GCNIS is not known to be associated with other testicular neoplasms such as sex cord stromal tumors (e.g., juvenile granulosa cell tumor), spermatocytic tumor or prepubertal germ cell tumors.
Comment Here
Reference: Germ cell neoplasia in situ
Comment Here
Reference: Germ cell neoplasia in situ
Practice question #2
Which of the following histologic features is associated with germ cell neoplasia in situ (GCNIS)?
- Atypical appearing gonocytes filling seminiferous tubules and extending into stroma as single cells
- Presence of i(12p)
- Seminiferous tubules lined with germinal epithelium undergoing maturation from spermatogonia to mature spermatids towards the lumen
- Sertoli only pattern
- Thickened seminiferous tubule basement membrane
Practice answer #2
E. Thickened seminiferous tubule basement membrane. Of the listed features, only a thickened basement membrane is associated with germ cell neoplasia in situ (GCNIS). Answer D is incorrect because a Sertoli only pattern would be found in testicles lacking germ cells and possessing only Sertoli cells (as in some types of infertility). Answers A and C are incorrect because atypical gonocytes invading the interstitium between seminiferous tubules would be diagnostic of invasive disease, while a population of maturing germinal epithelium ranging from spermatogonia to mature spermatids in the lumen of the tubule would be consistent with nonneoplastic, maturing spermatogenesis and unlikely in the context of GCNIS. Answer B is incorrect because the presence of i(12p) indicates molecular progression beyond in situ disease (e.g., seminoma) and is therefore absent in the precursor GCNIS lesion.
Comment Here
Reference: Germ cell neoplasia in situ
Comment Here
Reference: Germ cell neoplasia in situ