Table of Contents
Definition / general | Terminology | Epidemiology | Clinical features | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Videos | Positive stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Roychowdhury M. Carcinoma in situ. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladdercis.html. Accessed May 12th, 2024.
Definition / general
- Flat lesion composed of cells in mid to upper epithelium with high cytologic grade
- By definition, no invasion into lamina propria
- Note: high grade non-invasive papillary lesions are NOT designated carcinoma in situ to avoid confusion
Terminology
- Also known as high grade intraurothelial neoplasia (HG IUN), severe dysplasia (sometimes)
Epidemiology
- De novo CIS constitutes less than 3% of all urothelial neoplasms, but occurs in 45% with concurrent invasive bladder carcinoma
Clinical features
- Symptoms are similar to cystitis; hematuria is common
- 20 - 80% of CIS patients develop invasive disease if left untreated
- Confers poorer prognosis in patients with coexisting noninvasive papillary urothelial carcinoma
- Often involves urothelium in other areas of GU tract
- Associated with multifocal high grade invasive carcinoma
- Presence should be included in pathology reports
Prognostic factors
- Multifocality, involvement of prostatic urethra, and response to bCG (J Natl Compr Canc Netw 2009;7:48)
Case reports
- 72 year old man with hematuria underwent cystoscopy (Case of the Week #331)
- Association of primary small cell carcinoma of the bladder with transitional cell carcinoma in situ (Hum Pathol 2008;39:1258)
Treatment
- bcg therapy (Eur Urol 2010;57:410) or intravesical hyperthermia and mitomycin-C (World J Urol 2009;27:319)
- Local resection or total cystectomy
Gross description
- Flat, grossly erythematous, granular or cobblestone mucosa
- No mass
- May involve large areas of mucosal surface, ureters, urethra
Microscopic (histologic) description
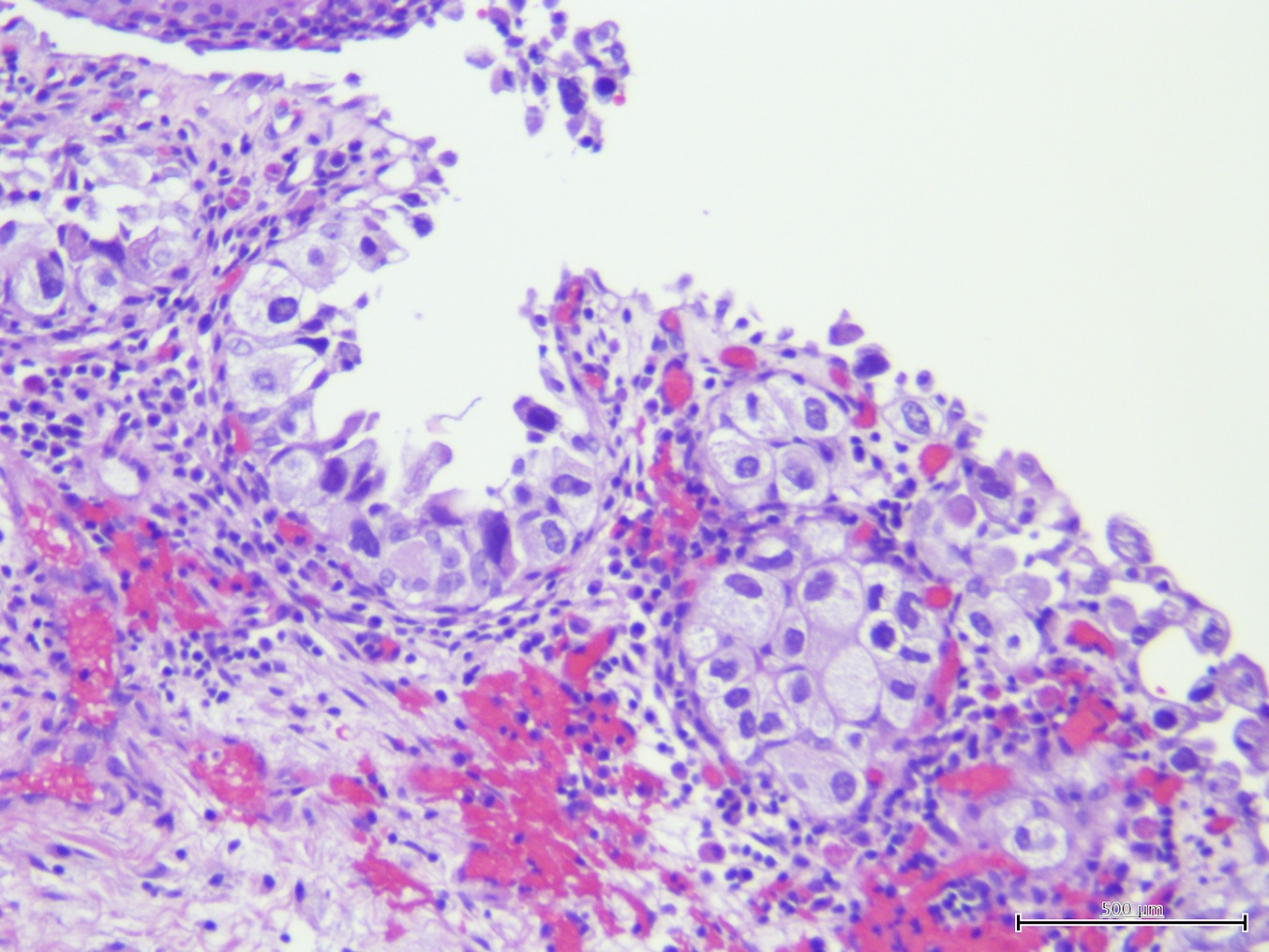
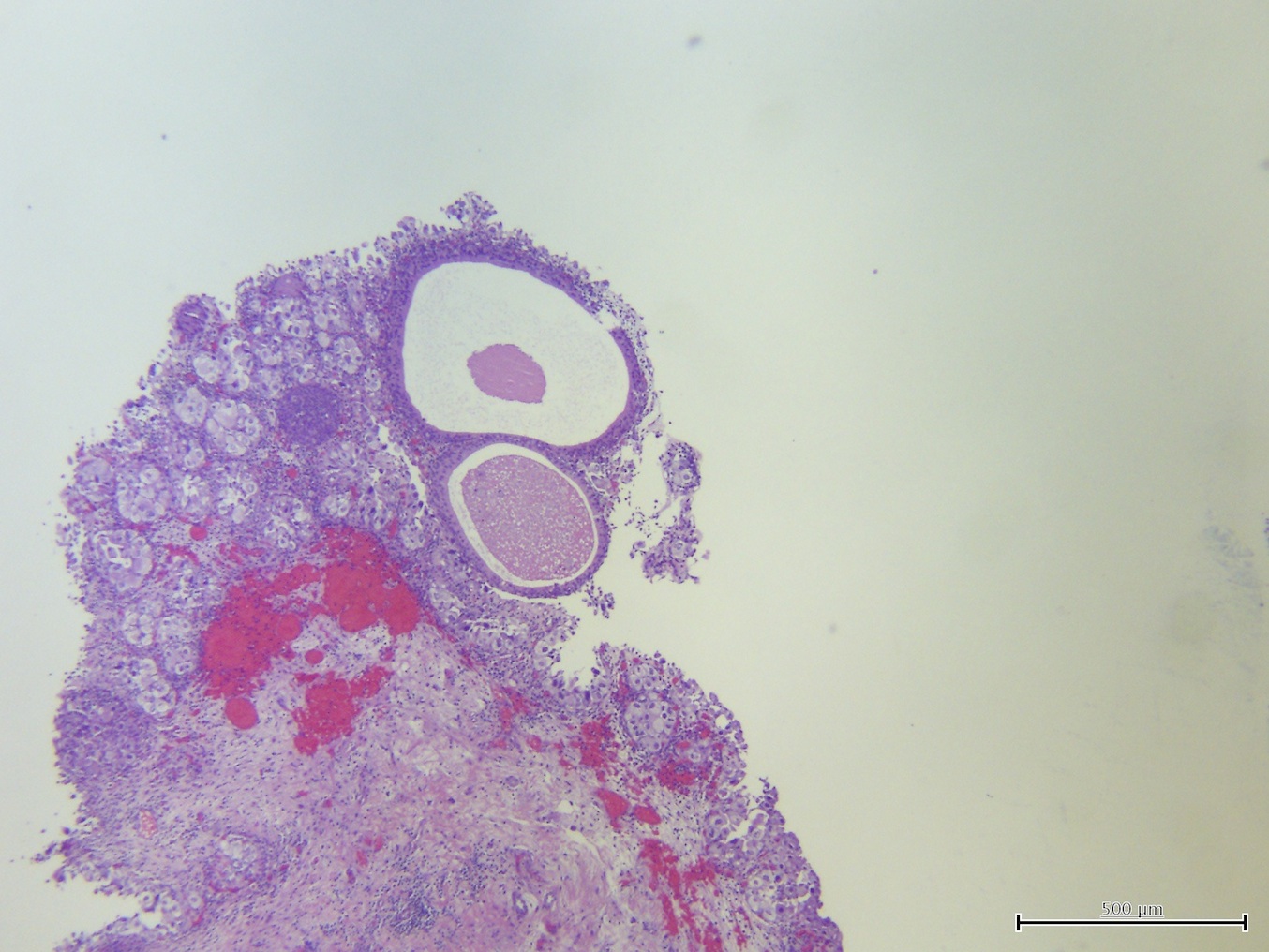
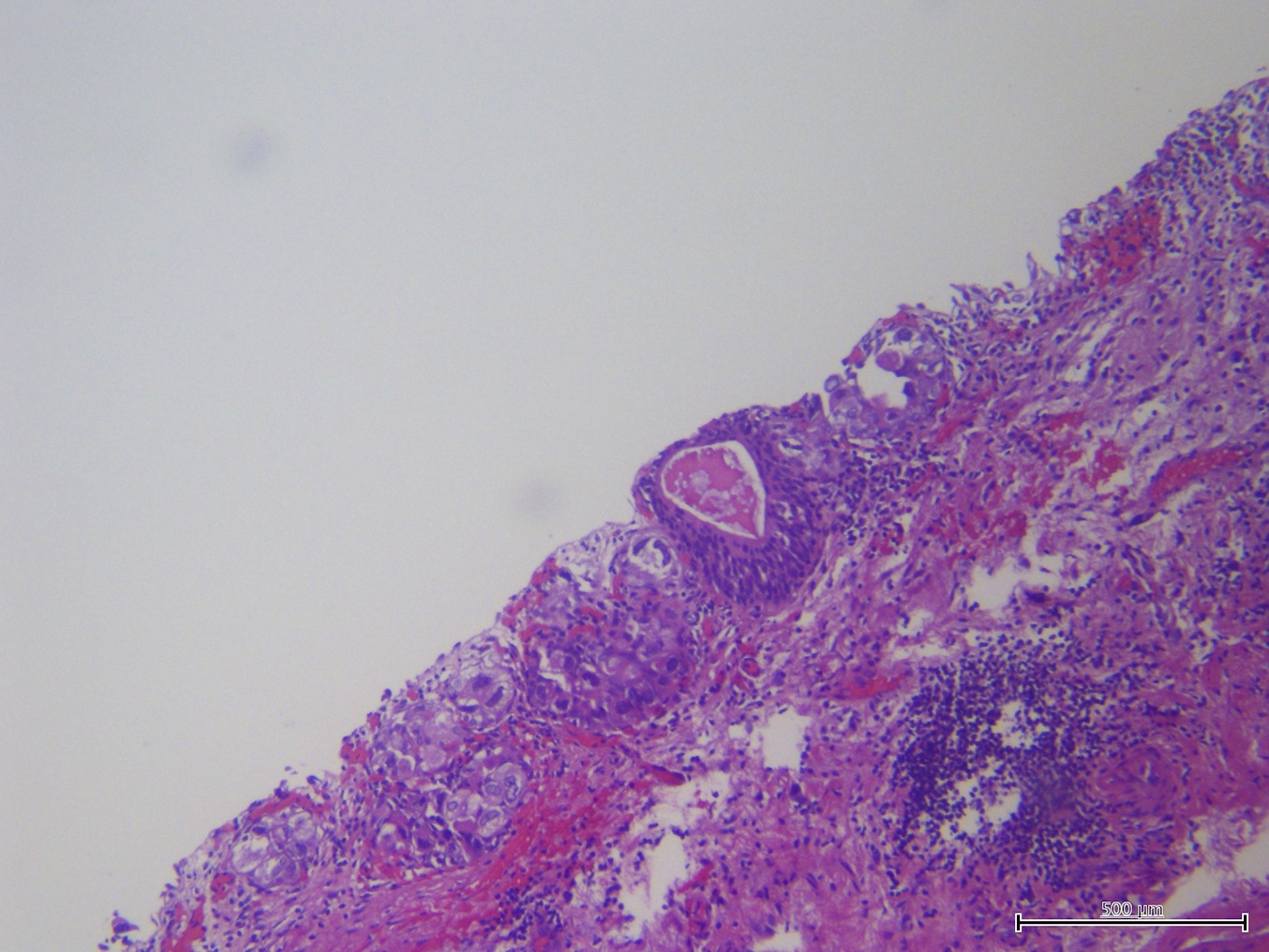
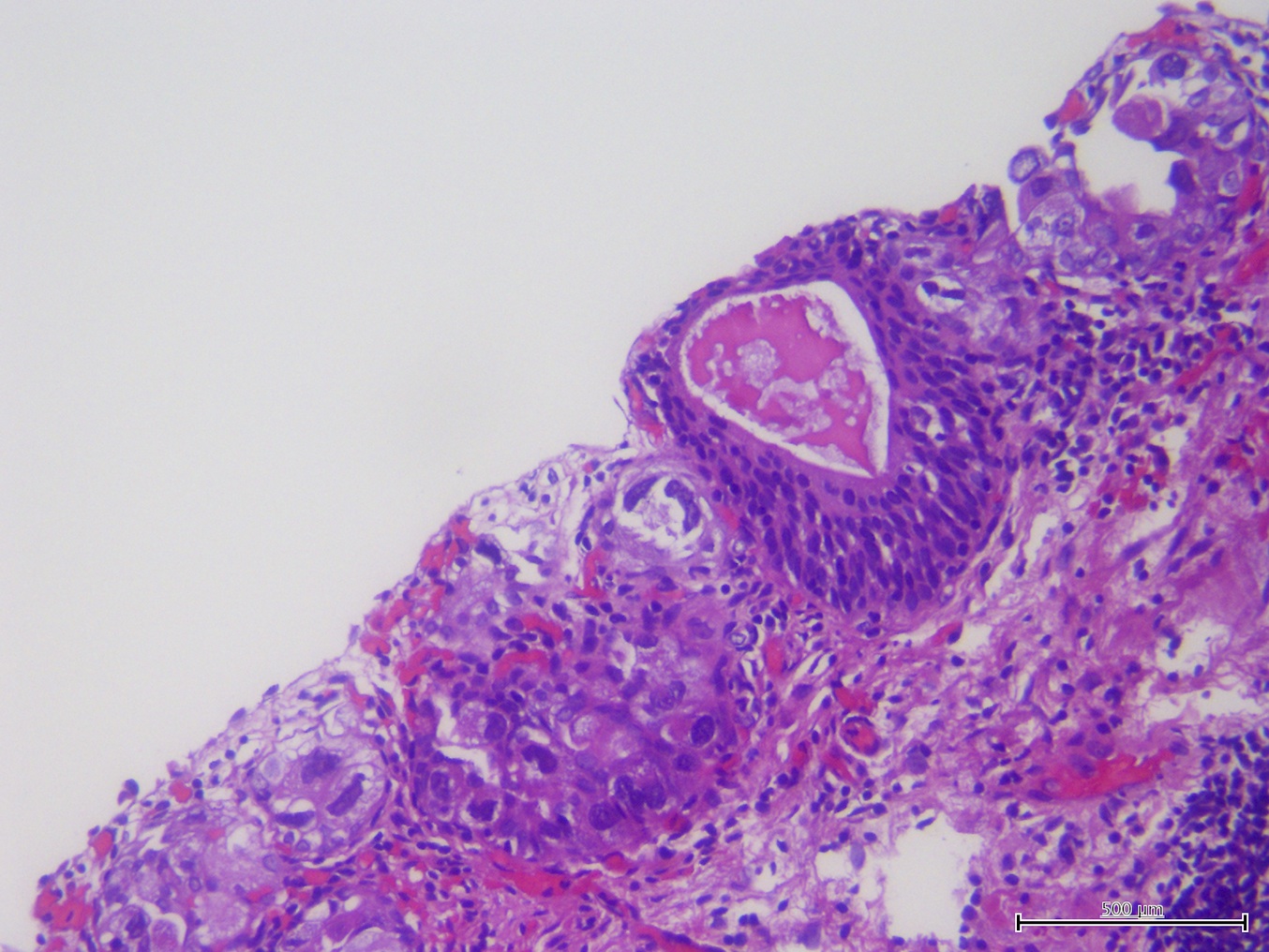
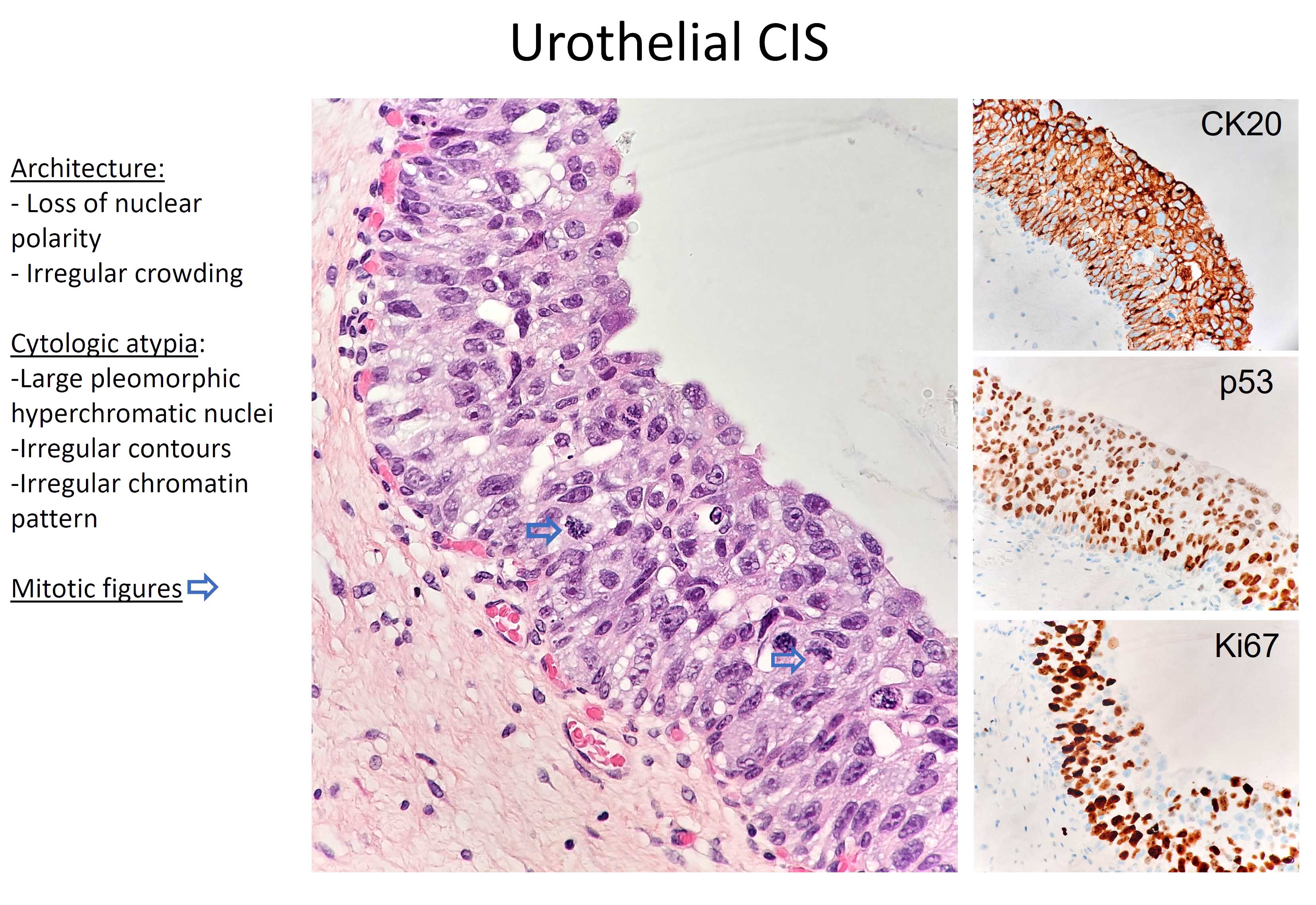
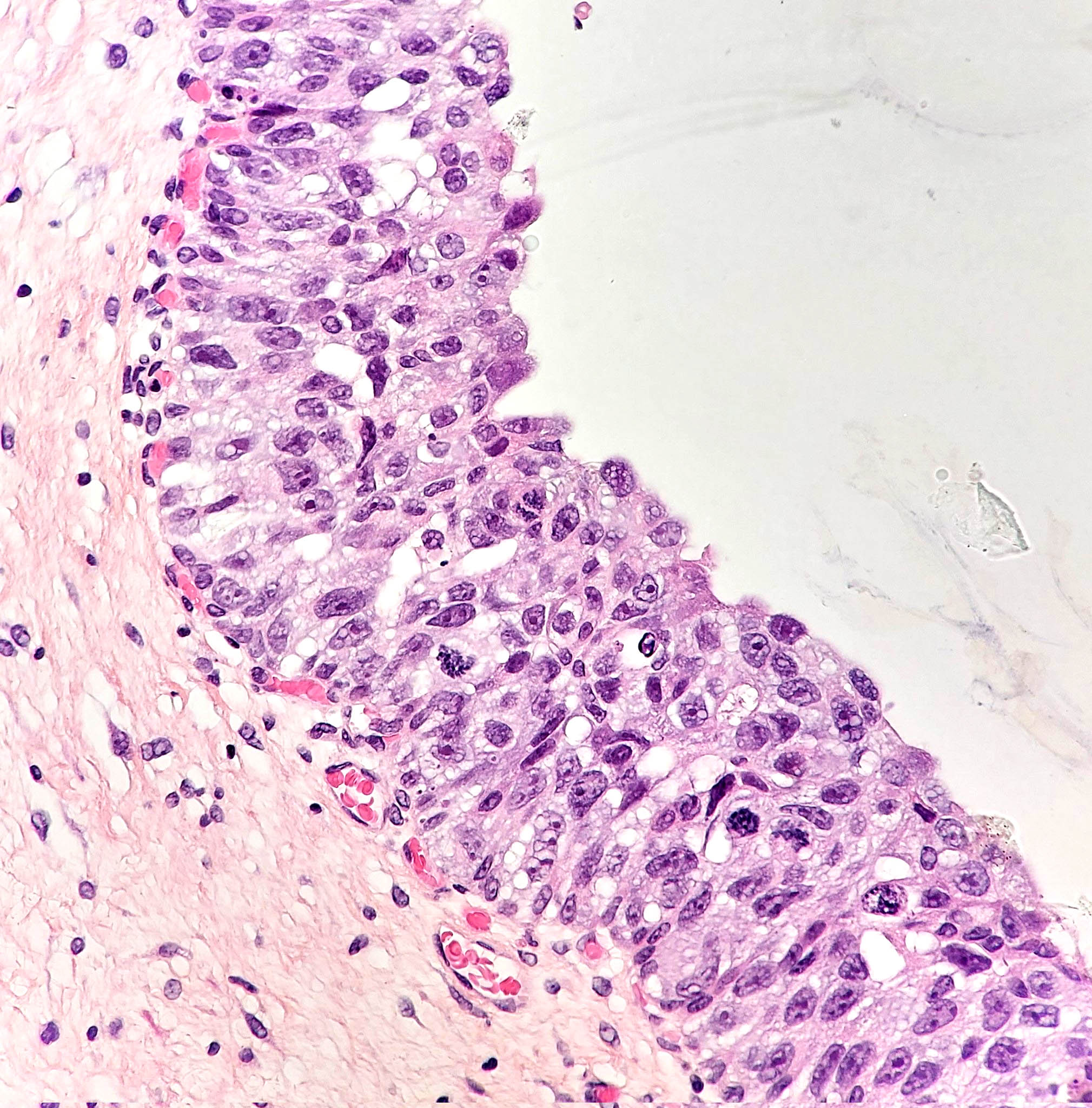
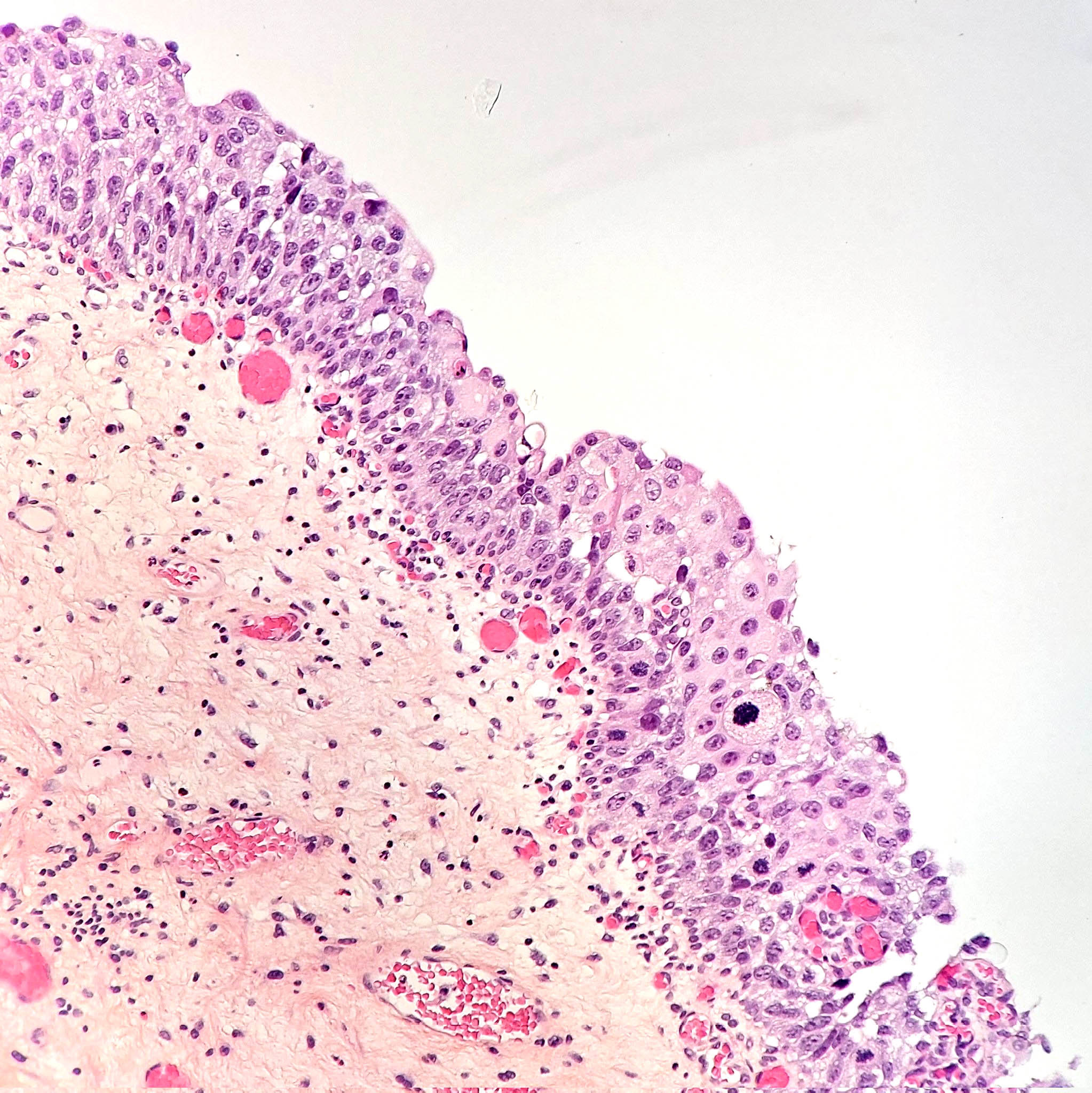
- Flat lesion composed of cells with large, irregular, hyperchromatic nuclei, prominent nuclear pleomorphism, high N/C ratio, mitotic figures in mid to upper epithelium
- Atypia may not be full thickness
- Epithelium is often denuded
- Nuclear size is 5x that of lymphocytes versus 2x lymphocytes for normal urothelium (Hum Pathol 2001;32:997)
- Also (but less important) loss of polarity, nuclear crowding, irregular thickness of urothelium
- Cells are not cohesive, leading to shedding into urine
- Occasionally present in prostatic ducts, spreads by intramucosal extension
- Note: high grade non-invasive papillary lesions are NOT designated as carcinoma in situ to avoid confusion
- Large cells with pleomorphism, large cells without pleomorphism, small cell, clinging (single layer of atypical cells on denuded urothelium), cancerization of urothelium (pagetoid - Hum Pathol 1993;24:1199, undermining or overriding)
- Pattern need not be included in surgical pathology report
- Microinvasion (2 mm or less) demonstrates invasive cells with retraction artifact mimicking vascular invasion (77% of cases of microinvasion)
- Also nests or irregular cords, rarely invades as isolated single cells with or without desmoplasia (Am J Surg Pathol 2001;25:356)
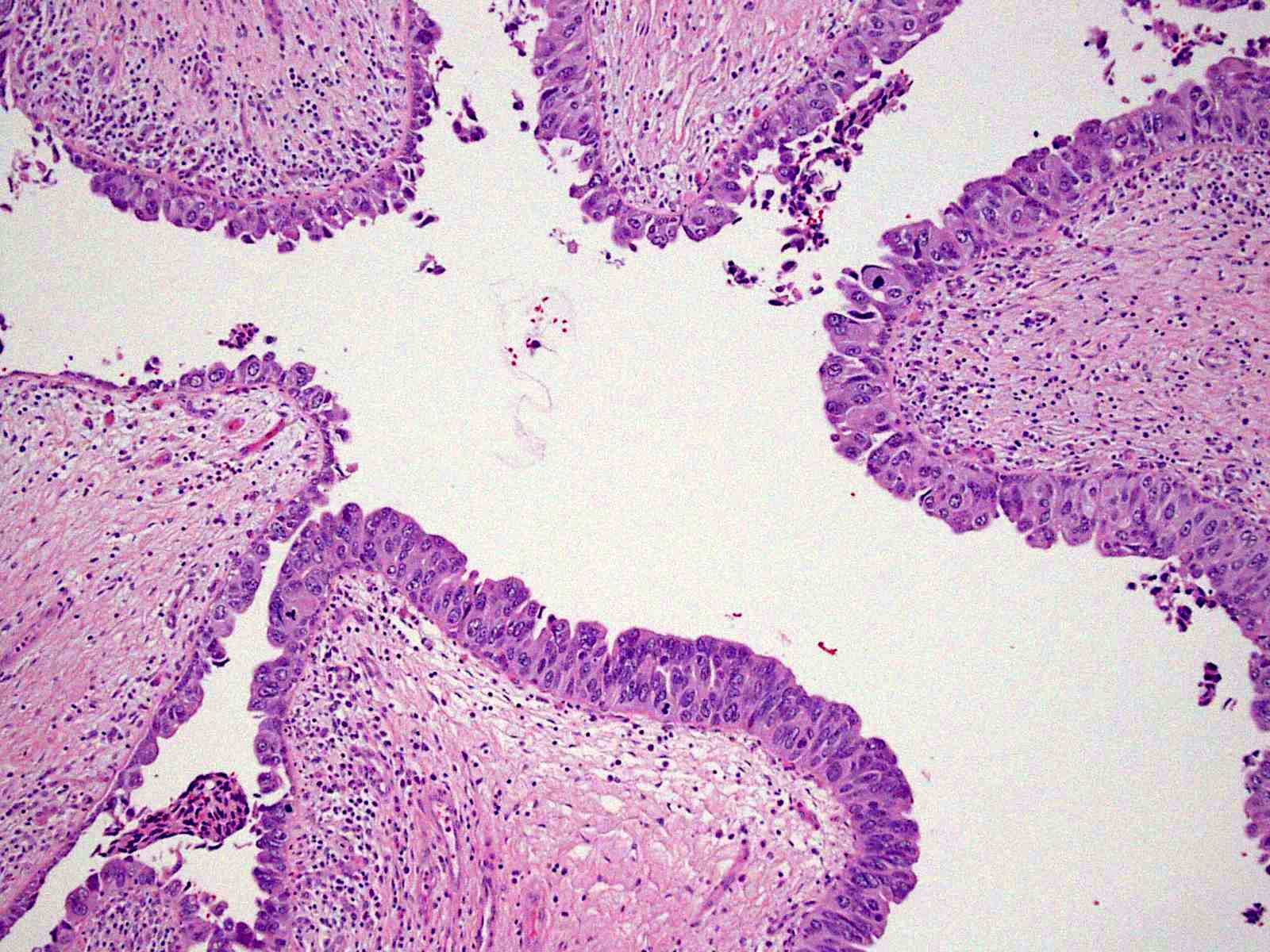
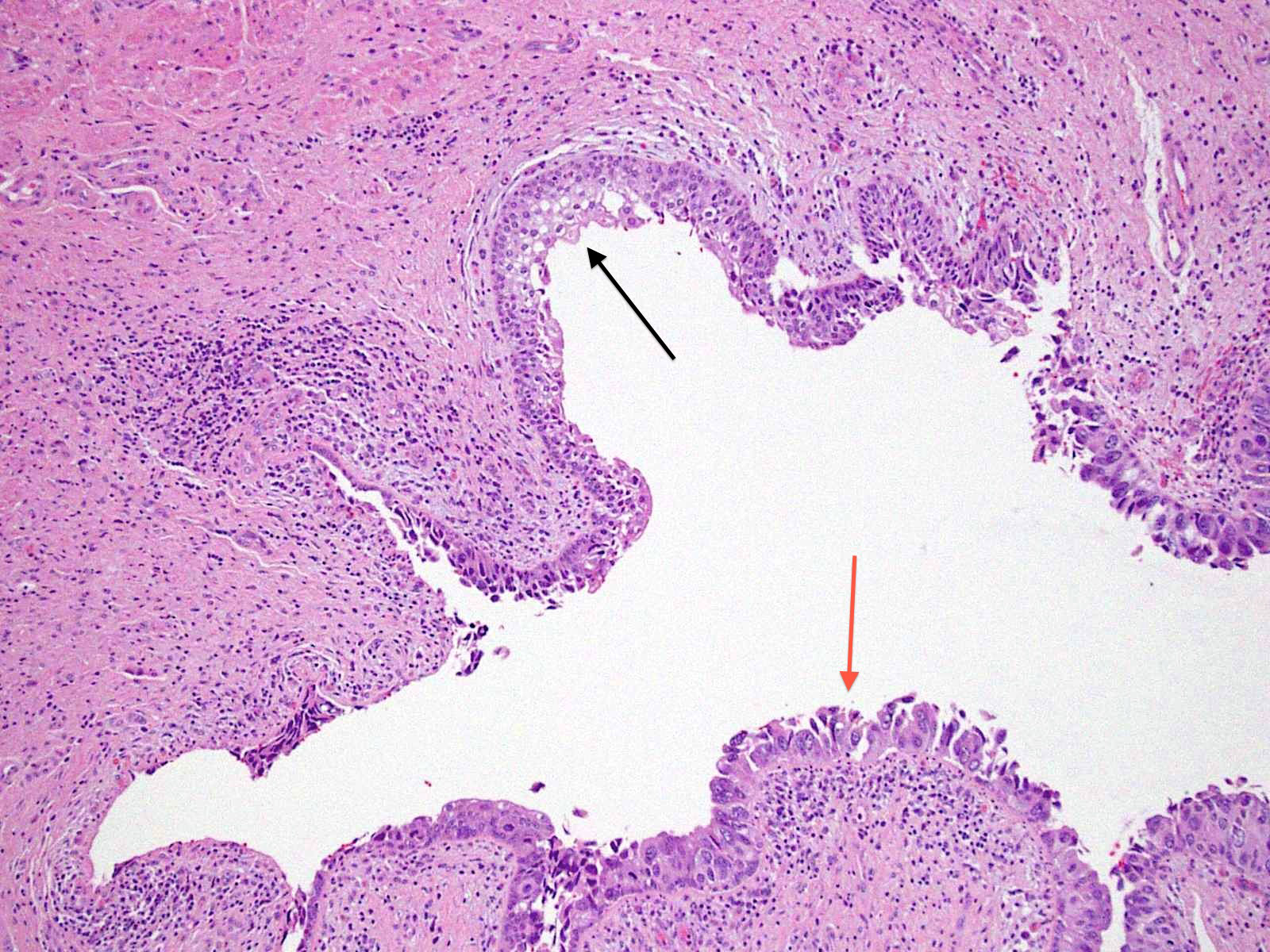
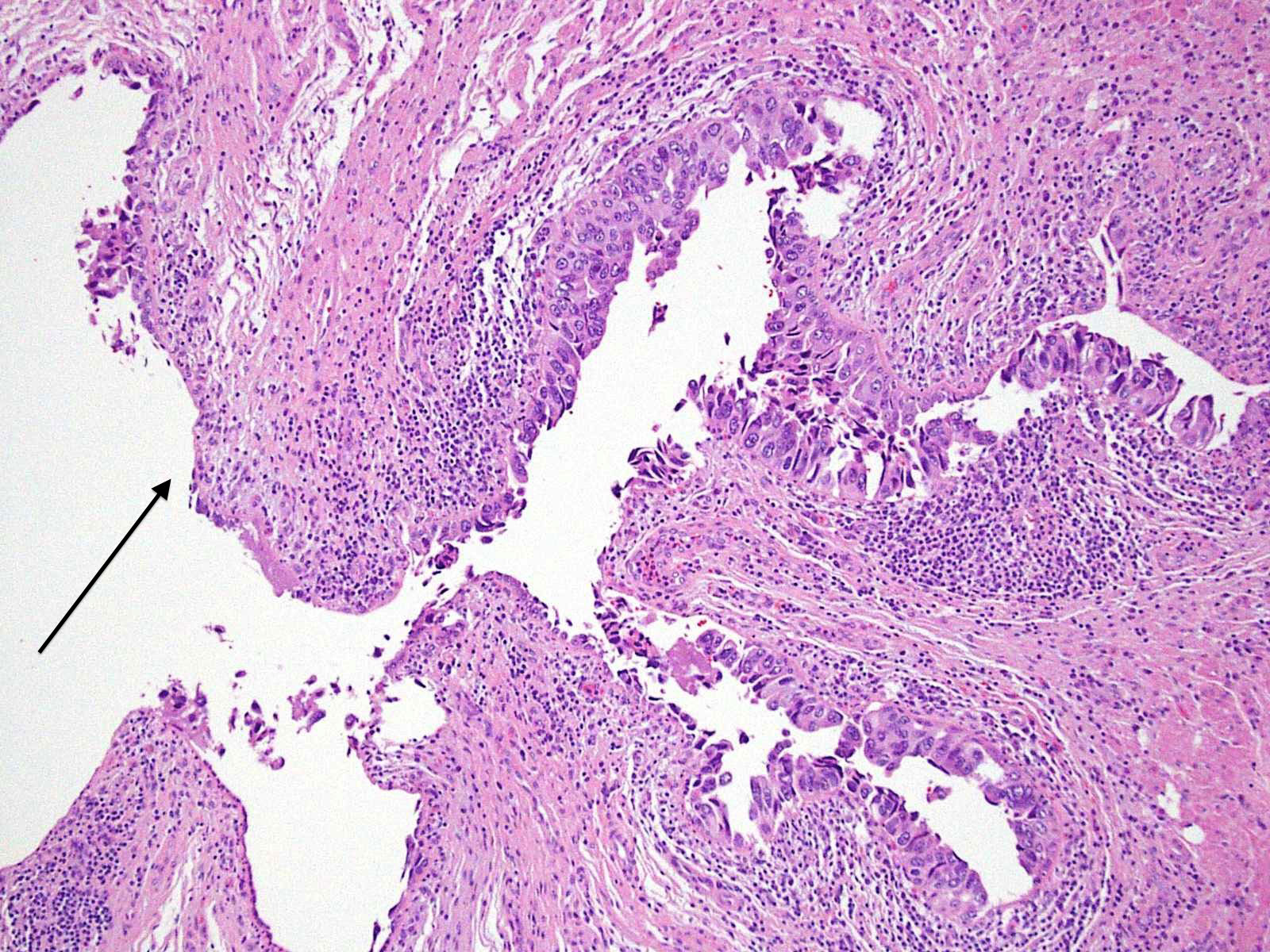
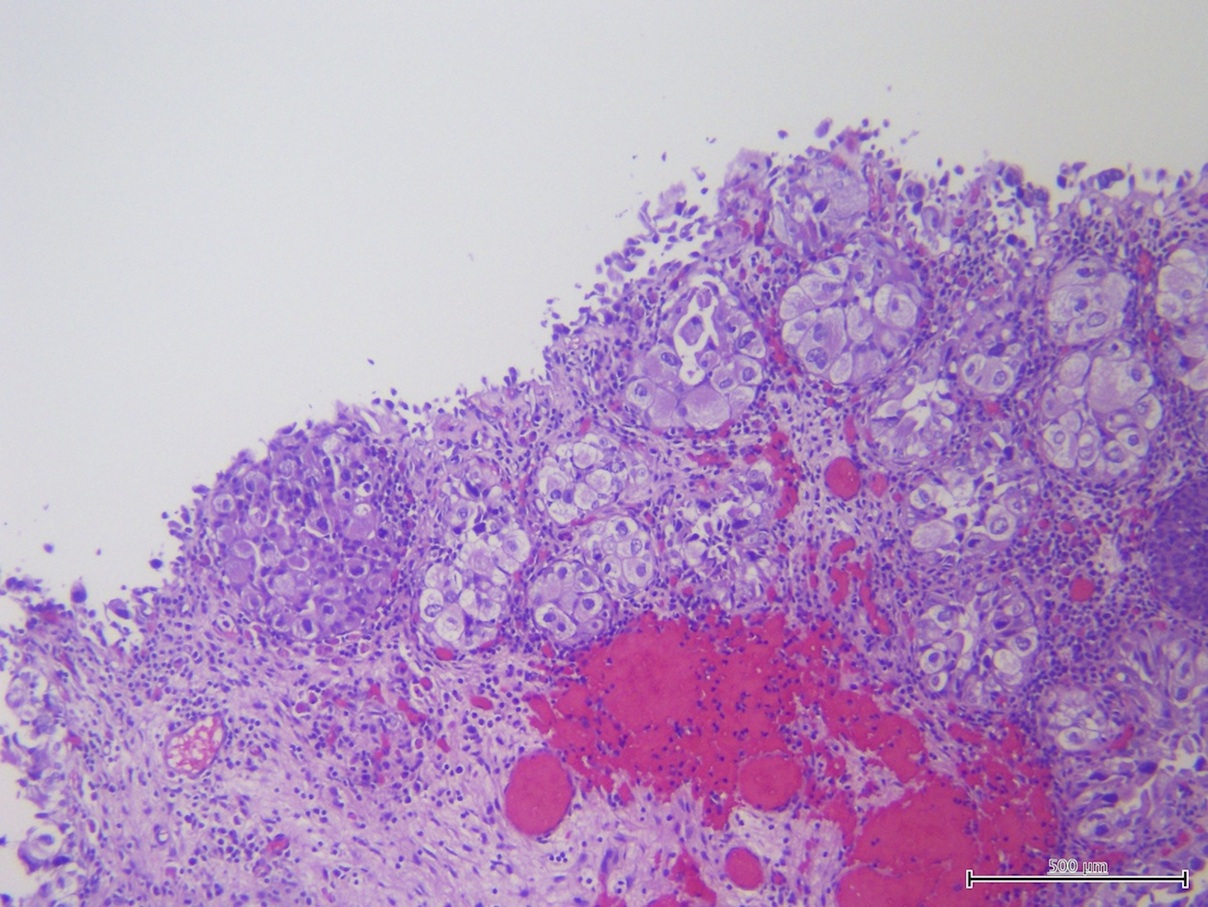
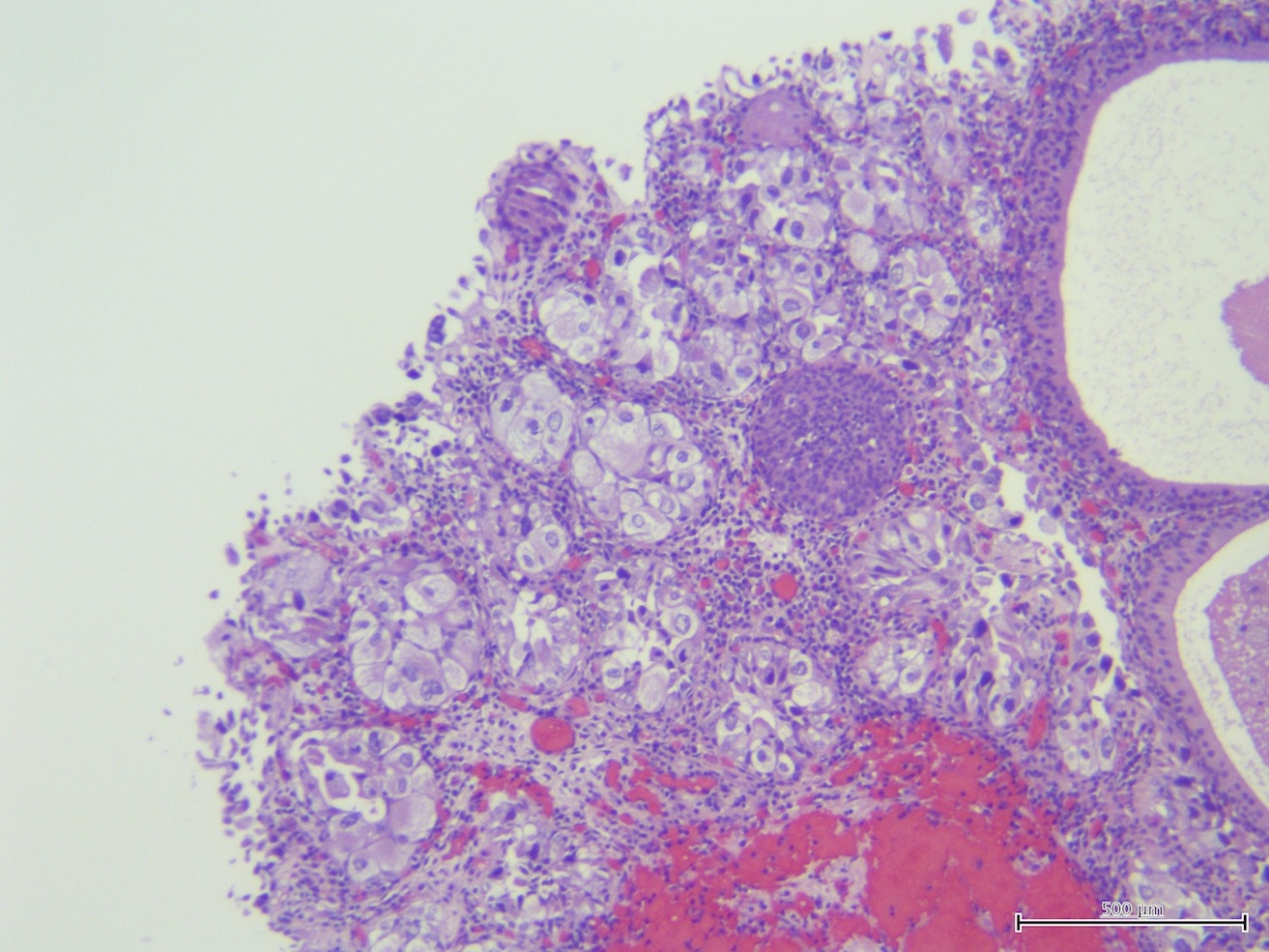
Microscopic (histologic) images
Contributed by Sean R. Williamson, M.D. and Bhavesh Papadi, M.D. (Case #331)
Contributed by @AnaPath10 on Twitter
Images hosted on other servers:
Cytology description
- Cytology is 95% sensitive for carcinoma in situ
- Nuclear changes of carcinoma with minimal pleomorphism
- Numerous high-grade neoplastic cells
- Relatively clean background
- Image analysis of bladder wash cytology may be comparable to "expert" cytologic review (Mod Pathol 1997;10:976)
Videos
Histopathology Bladder Transitional Carcinoma in situ
Positive stains
- Keratin 34betaE12 labels all urothelial layers, compared to only basal labeling in dysplasia (Hum Pathol 2000;31:745)
- Typical pattern for CIS is CK20+, p53+, Ki-67+, CD44- (Mod Pathol 2003;16:187)
- E-cadherin positive (Hum Pathol 2002;33:996)
- Strong p16(INK4) staining (Hum Pathol 2008;39:527)
- Frequent HER2+ amplification (Hum Pathol 1995;26:970)
Molecular / cytogenetics description
- Monoclonal with aneuploid DNA and more abnormal microsatellites than corresponding invasive carcinoma, if present (Hum Pathol 2009;40:988)
- Has somatic mismatch repair protein down-regulation and accumulation of tumor suppressor gene microsatellite abnormalities
- Molecular pattern of CIS is divergent from coexistent muscle invasive urothelial carcinoma
- Deletion of 9p21 or polysomy of #9 (Hum Pathol 2008;39:527)
Differential diagnosis
- Denuding cystitis: cells may look malignant
- Denuded urothelium:
- Extensively denuded epithelium is often seen in CIS ("clinging CIS" or "denuding cystitis")
- However residual malignant cells required for diagnosis
- Deeper sectioning of tissue block or examination of von Brunn nests may be helpful if epithelium is denuded
- Dysplasia: less severe atypia although distinction may be difficult
- Post-topical therapy for high grade urothelial carcinoma: still has capillaries
- Radiation effect: cells still cohesive, may have distinctive nuclear borders, may resemble pagetoid variant of CIS
- Reactive atypia: less pleomorphic nuclei than CIS; patchy CK20 in umbrella cells only, p53 weak/negative, CD44 diffusely or focally positive vs. CIS which is intensely CK20+ (81%), p53+ (57%), CD44- (100%, Am J Surg Pathol 2001;25:1074)
Additional references