Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Patel R, Mueller J. Hemorrhoids. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anushemorrhoids.html. Accessed October 1st, 2025.
Definition / general
- Hemorrhoids are normal vascular structures present as cushions that help to maintain continence (Clin Gastroenterol Hepatol 2013;11:593)
- Although hemorrhoids are normal structures, the term hemorrhoid has been referred to as a pathologic or symptomatic process (Clin Gastroenterol Hepatol 2019;17:8)
- Typically defined as symptomatic enlargement and distal displacement of the normal anal cushions (World J Gastroenterol 2012;18:2009)
Essential features
- Guidelines for routine histological examination of hemorrhoids vary from institution to institution
- IHC stain is not required to make a diagnosis
- Incidental findings in hemorrhoidectomy specimens, including squamous dysplasia, adenocarcinoma, squamous cell carcinoma, melanoma and Kaposi sarcoma, are not uncommon
- Florid papillary endothelial hyperplasia can mimic angiosarcoma and should be differentiated from the latter
ICD coding
Epidemiology
- True epidemiology is unknown because of the use of self medication and low rate of healthcare seeking behavior (World J Gastroenterol 2012;18:2009)
- Approximate prevalence in the United States is 4.4% (Gastroenterology 1990;98:380)
- No gender predilection
- Peak prevalence between 45 - 65 years old; unusual before the age of 20 years
- More frequent in White people than in Black people and more common in individuals of higher socioeconomic status (World J Gastroenterol 2012;18:2009)
Sites
- Usually located at left lateral, right anterior and right posterior positions; multiple sites can be involved at the same time
- Right anterior is the most involved position (Ann Afr Med 2019;18:12)
- Hemorrhoids are generally classified based on their location
- Internal hemorrhoids: originate from the inferior hemorrhoidal venous plexus above the dentate line and are covered by mucosa
- External hemorrhoids: located below the dentate line and are covered with squamous epithelium
- Mixed (interno - external) hemorrhoids: arise both above and below the dentate line
Pathophysiology
- Exact pathophysiology for internal hemorrhoids is not clearly understood but the following hypotheses have been documented in literature
- Deterioration of the connective tissue that anchors hemorrhoids (Dis Colon Rectum 1984;27:442)
- Hypertrophy or increased tone of the internal anal sphincter
- Abnormal distension of the arteriovenous anastomoses within the hemorrhoidal cushions (Br J Surg 1975;62:542)
- Abnormal dilatation of the veins of the internal hemorrhoidal venous plexus
- Hemorrhoids and anorectal varices are proven to be distinct entities
- Patients with portal hypertension and varices do not have an increased incidence of hemorrhoids (Am J Gastroenterol 1991;86:1185)
Etiology
- Constipation and prolonged straining (Br J Surg 1994;81:946)
- Pregnancy
- Dietary factors including low fiber diet, spicy foods and alcohol intake
- Other risk factors: advancing age, diarrhea, pelvic tumors, prolonged sitting and patients on anticoagulation and antiplatelet therapy (Gastroenterology 1990;98:380)
Diagrams / tables
Clinical features
- External hemorrhoids are supplied by somatic nerves, thus producing pain while internal hemorrhoids are innervated by visceral nerve fibers so do not cause pain
- Approximately 40% cases are asymptomatic (Int J Colorectal Dis 2012;27:215)
- Most common presentation is painless rectal bleeding during defecation with or without prolapsing anal tissue (Ann Afr Med 2019;18:12)
- Perineal irritation or anal itching, feeling of incomplete evacuation or rectal fullness
- Anal pain in cases of thrombosed or strangulated hemorrhoids or associated anal fissure and perianal abscess
- Positive fecal occult blood or anemia is not common; if present, the patient should be evaluated for other causes (World J Gastroenterol 2012;18:2009)
- See Diagrams / tables for tabular representation for grading and types of hemorrhoids
- Internal hemorrhoids are further graded based on their appearance and degree of prolapse (Goligher’s classification)
- First degree hemorrhoids (grade I): the anal cushions bleed but do not prolapse
- Second degree hemorrhoids (grade II): the anal cushions prolapse through the anus on straining but reduce spontaneously
- Third degree hemorrhoids (grade III): the anal cushions prolapse through the anus on straining or exertion and require manual replacement into the anal canal
- Fourth degree hemorrhoids (grade IV): the prolapse stays out at all times and is irreducible
Diagnosis
- Precise patient history and careful clinical examination
- Physical examination including digital rectal examination
- Anoscopy
- Flexible sigmoidoscopy and colonoscopy (Clin Gastroenterol Hepatol 2013;11:593)
Prognostic factors
- Excellent prognosis with conservative treatments in mild cases
- Recurrence rate after conservative management is more than 50%, whereas after surgery it is < 5 - 10%
- However, postsurgical complications such as pain and urinary retention can happen
- Reference: StatPearls: External Hemorrhoid [Accessed 3 July 2023]
Case reports
- 35 year old Japanese woman with in situ diffuse large B cell lymphoma in hemorrhoidectomy tissue (EJHaem 2022;3:1050)
- 37 year old woman with endometriosis in the rectum accompanied by hemorrhoids leading to diagnostic pitfalls (BMC Womens Health 2018;18:120)
- 42 year old man with traumatic neuroma of anus 5 years after Milligan-Morgan hemorrhoidectomy (Ann Clin Lab Sci 2014;44:324)
- 45 year old man with leukoplakia of the anal verge with bleeding hemorrhoid (Rev Med Inst Mex Seguro Soc 2009;47:101)
- 60 year old man with anal neuroendocrine tumor masquerading as external hemorrhoids (Gastroenterology Res 2017;10:56)
- 69 year old man with perianal melanoma disguised as hemorrhoids (Dig Dis Sci 2007;52:1745)
Treatment
- Conservative (medical)
- Dietary and behavioral modifications (Clin Gastroenterol Hepatol 2013;11:593)
- Nonsurgical / office based treatment
- Rubber band ligation
- Sclerotherapy
- Infrared coagulation
- Bipolar diathermy, direct current electrotherapy, heater probe coagulation
- Cryosurgery
- Surgical
- Hemorrhoidectomy or hemorrhoidopexy in cases with higher grade and recurrent hemorrhoids despite conservative therapy (Hum Pathol 2021;109:12)
Clinical images
Microscopic (histologic) description
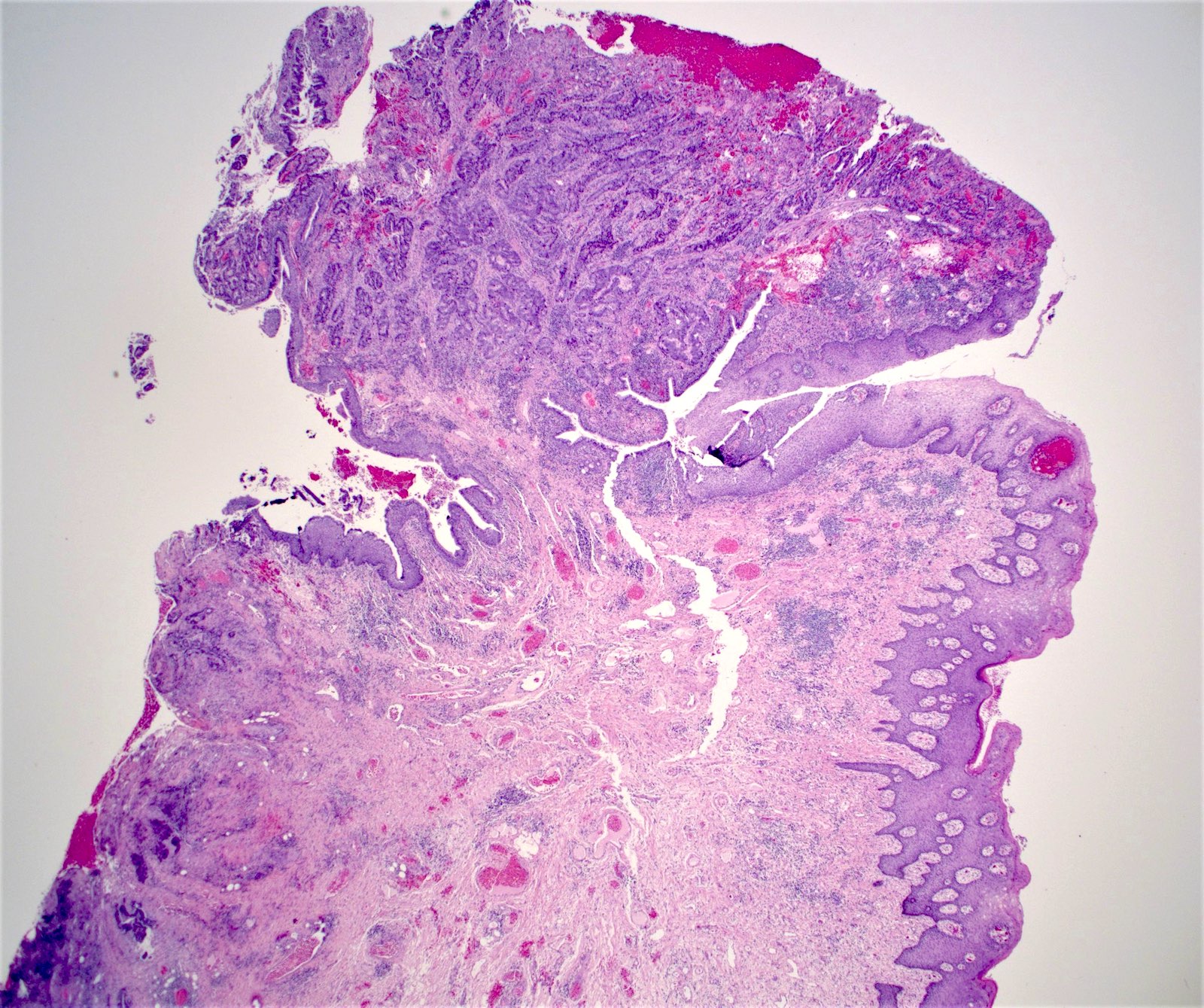
- Routine pathological examination of hemorrhoid specimens has been a topic of debate and the guidelines may vary from institution to institution (Hum Pathol 2021;109:12)
- Some incidental benign or malignant findings like adenocarcinoma, squamous cell carcinoma, melanoma and Kaposi sarcoma can be found during routine histopathological examination
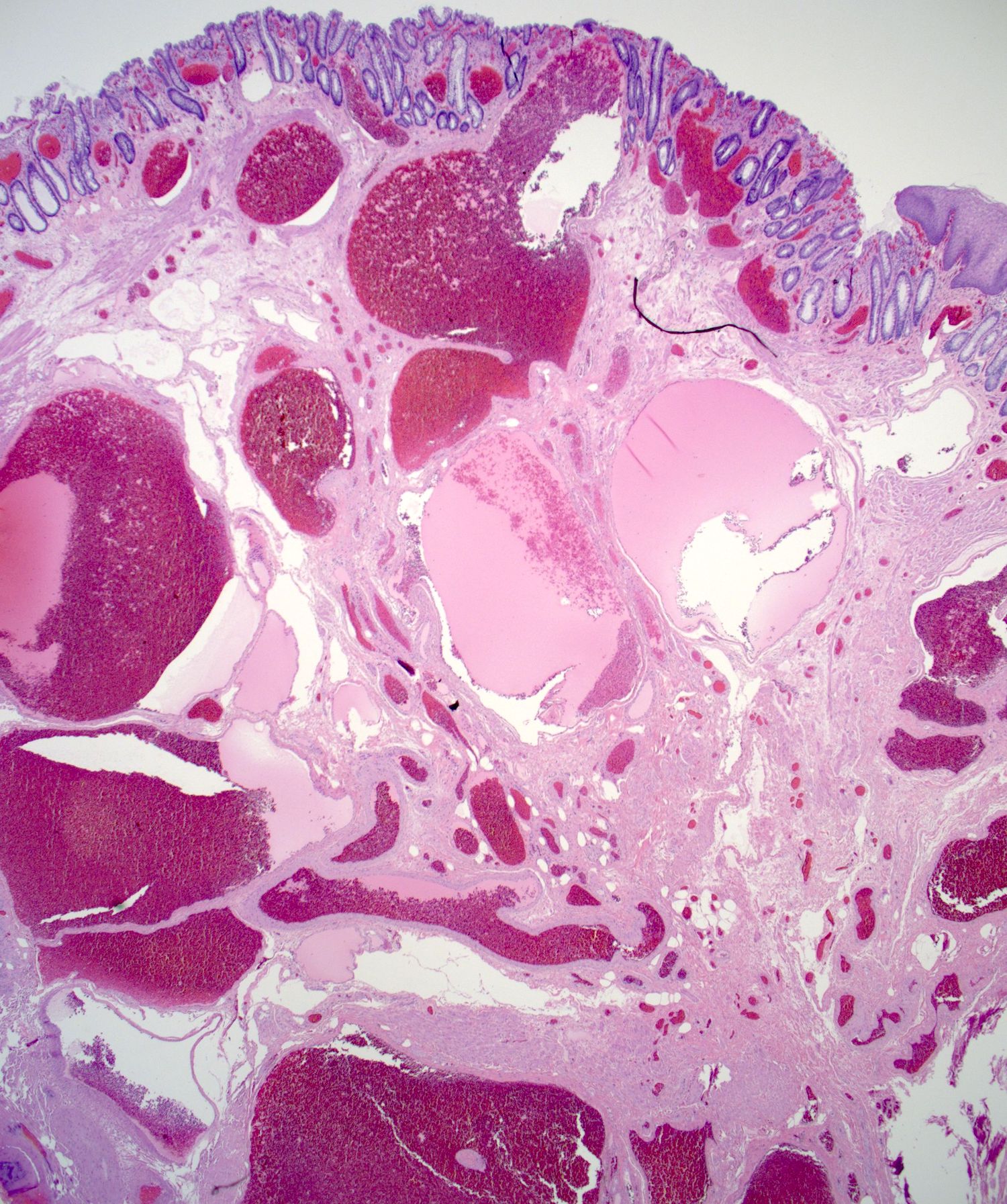
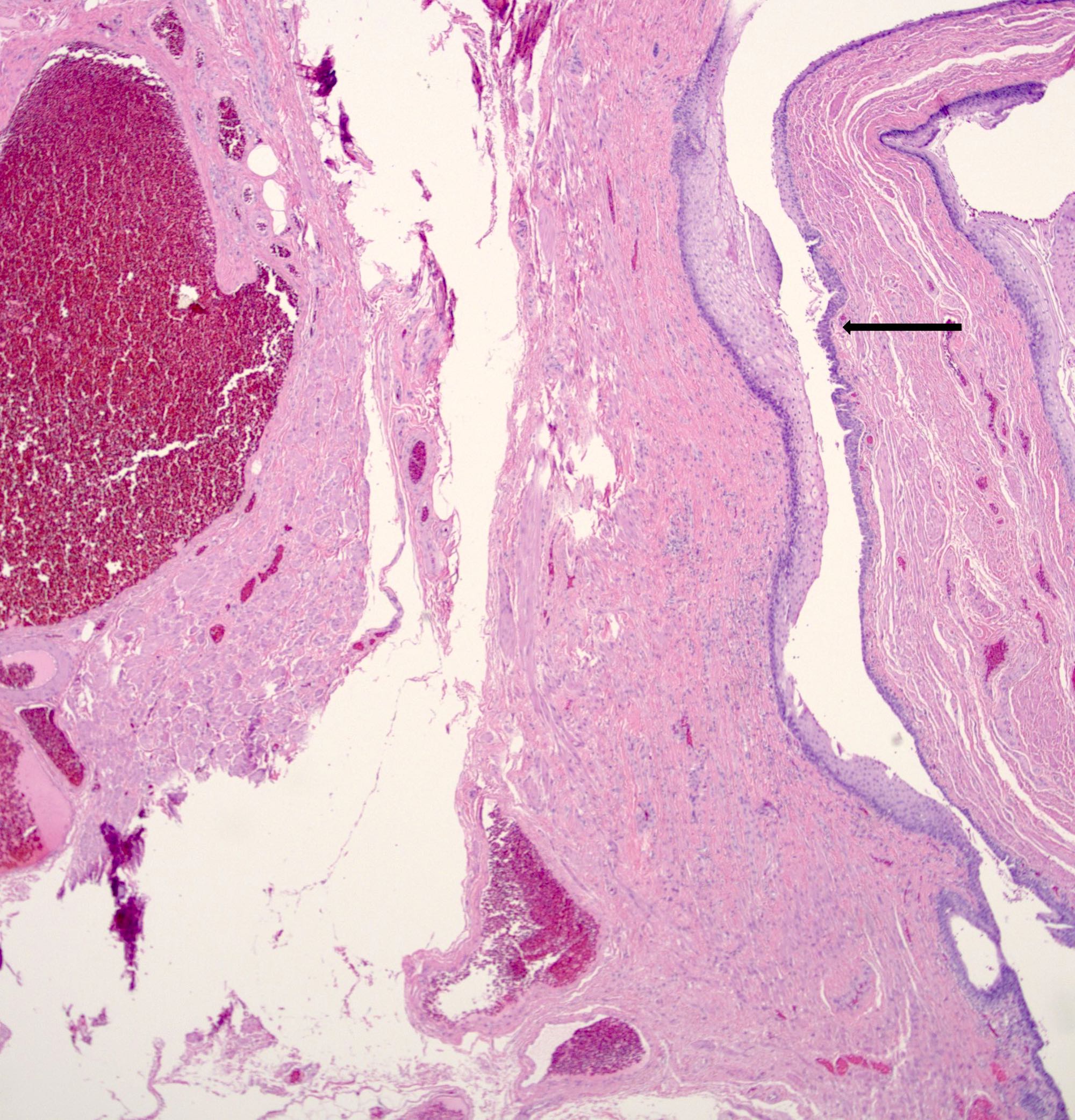
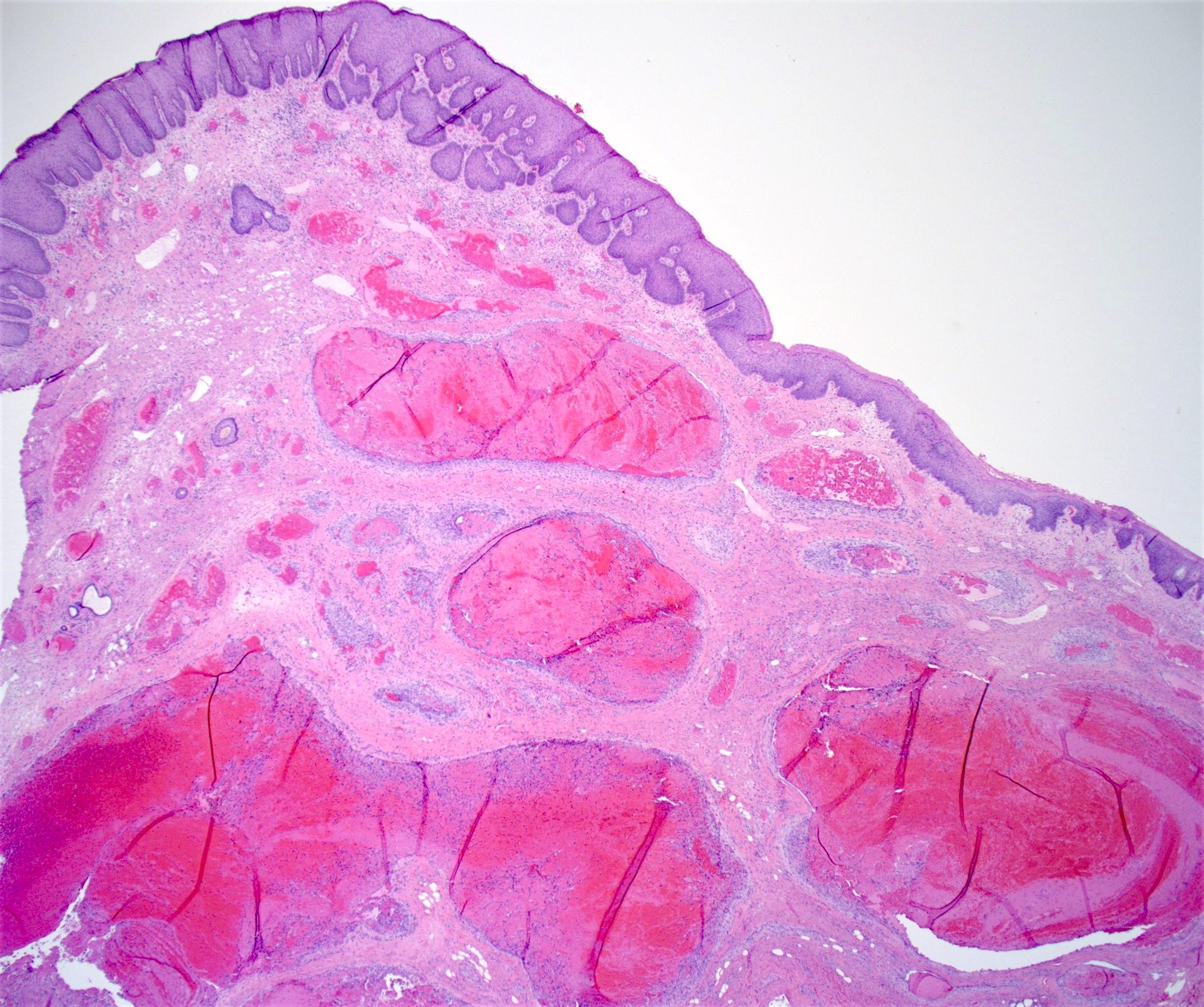
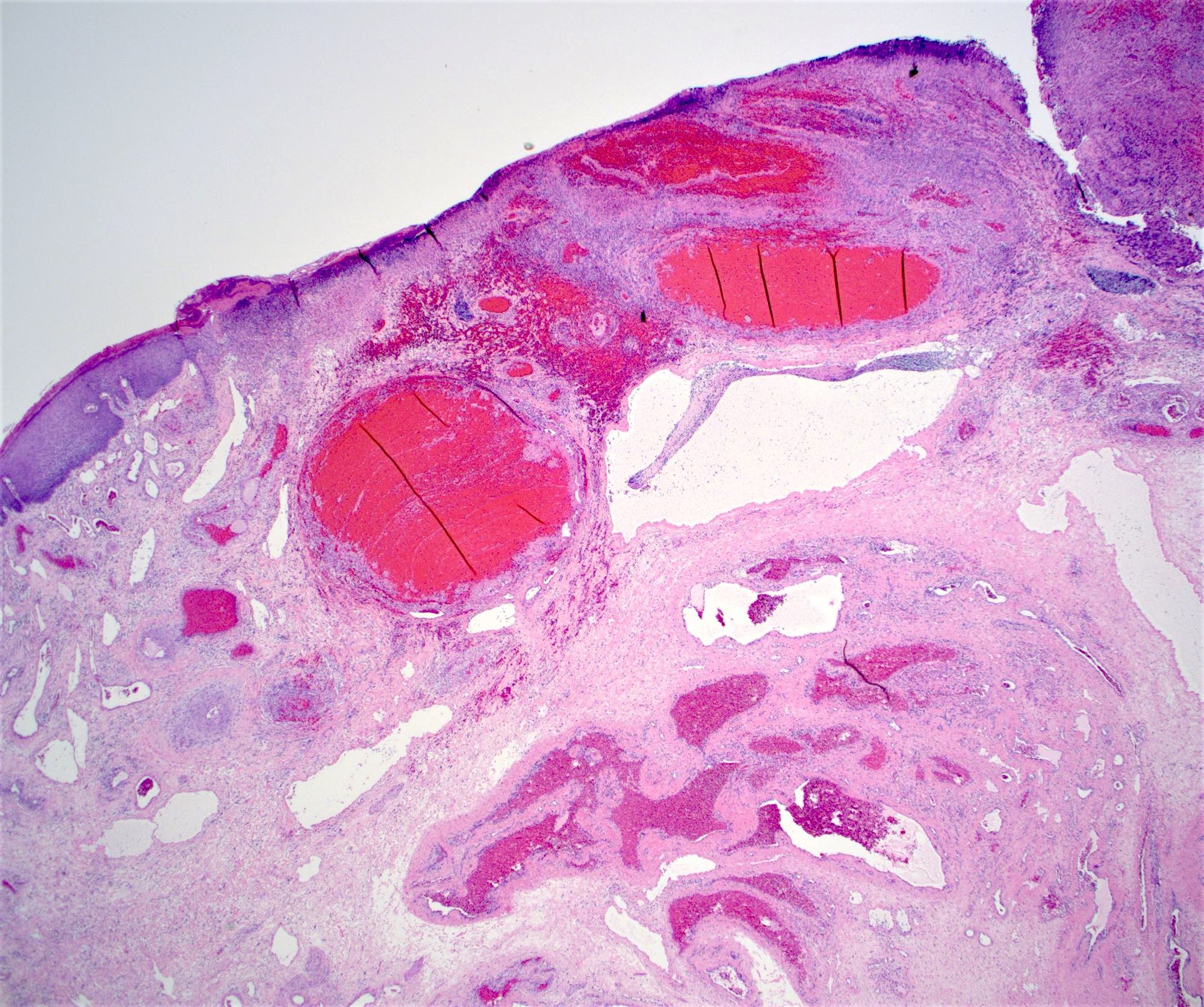
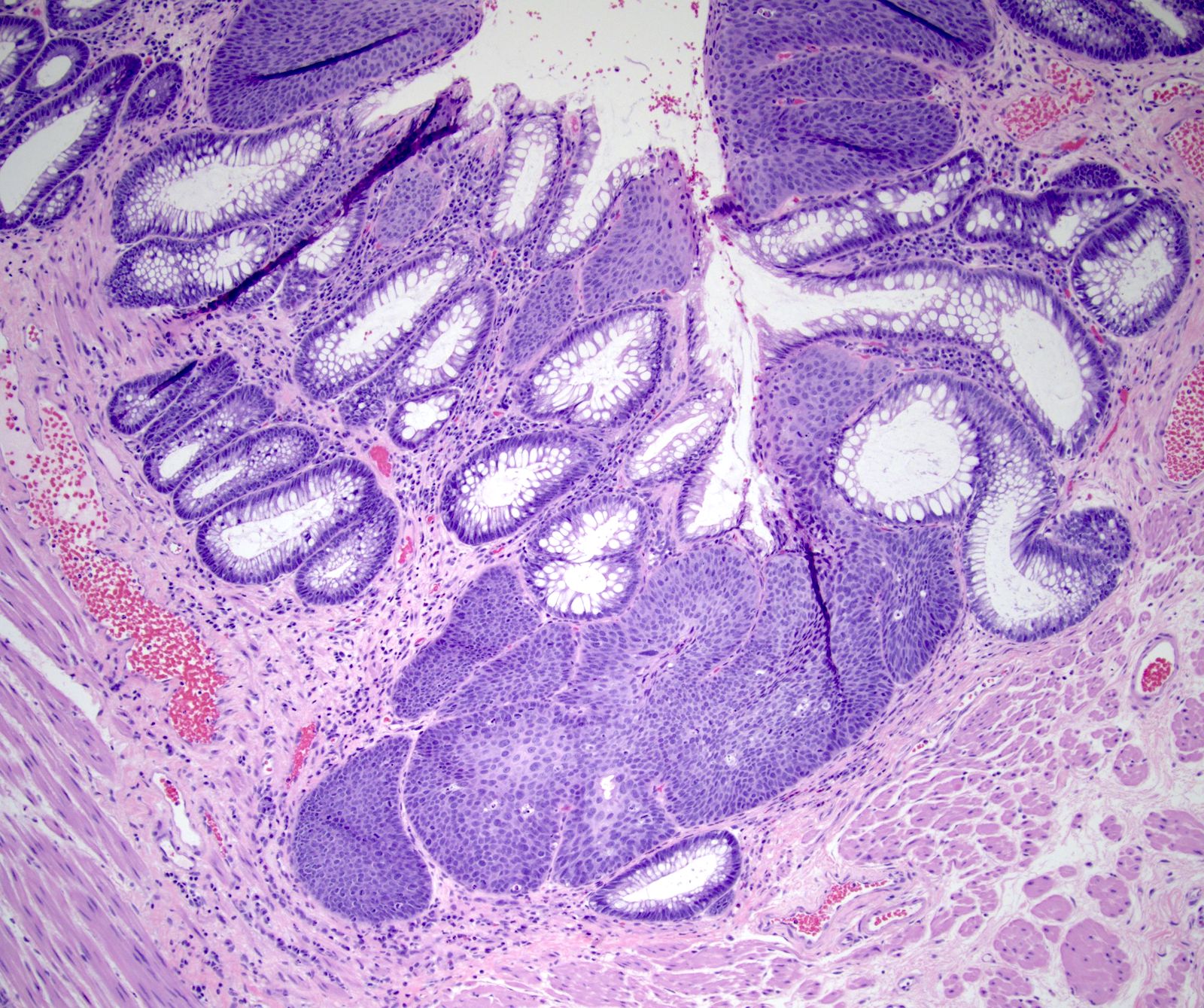
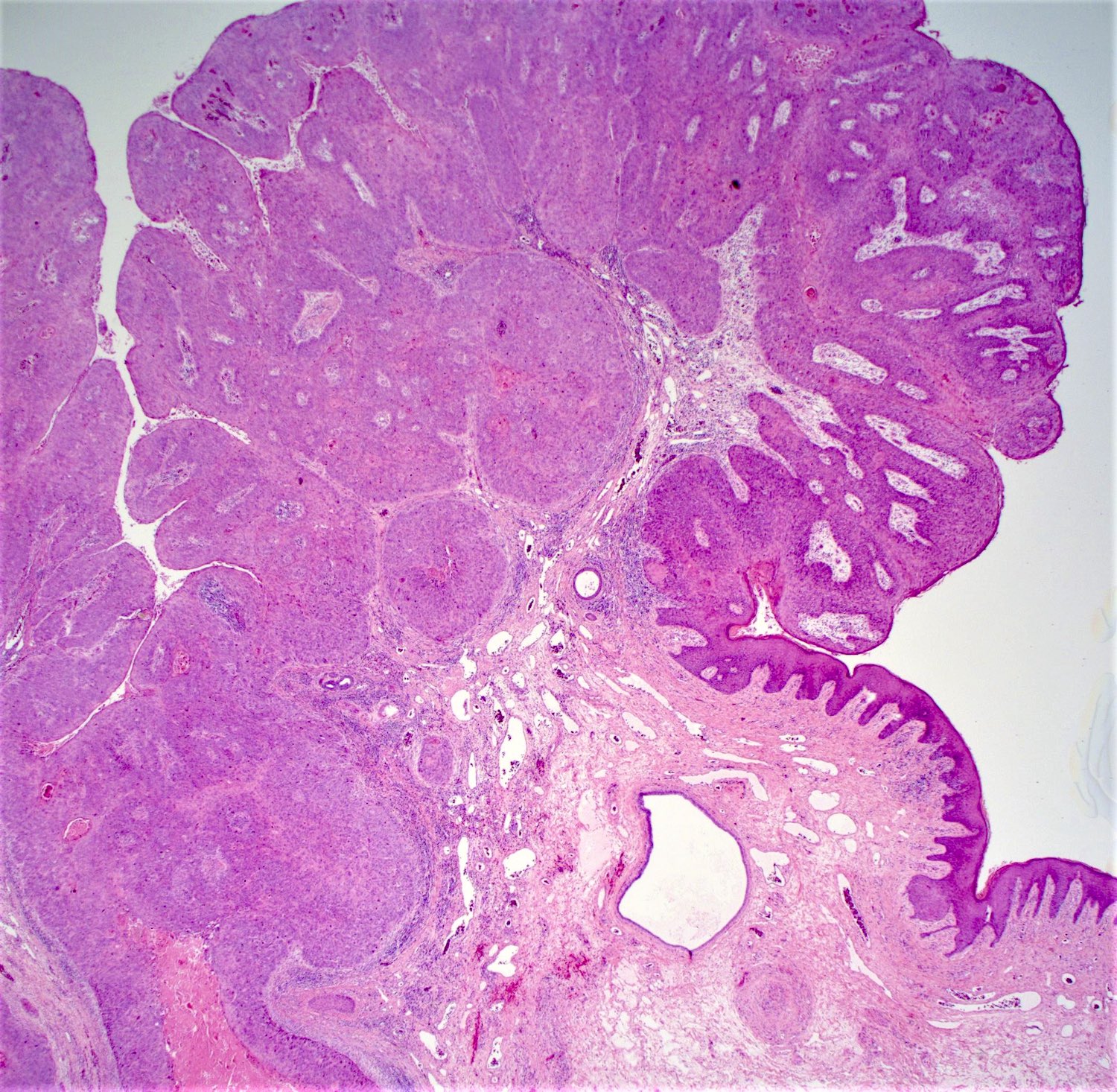
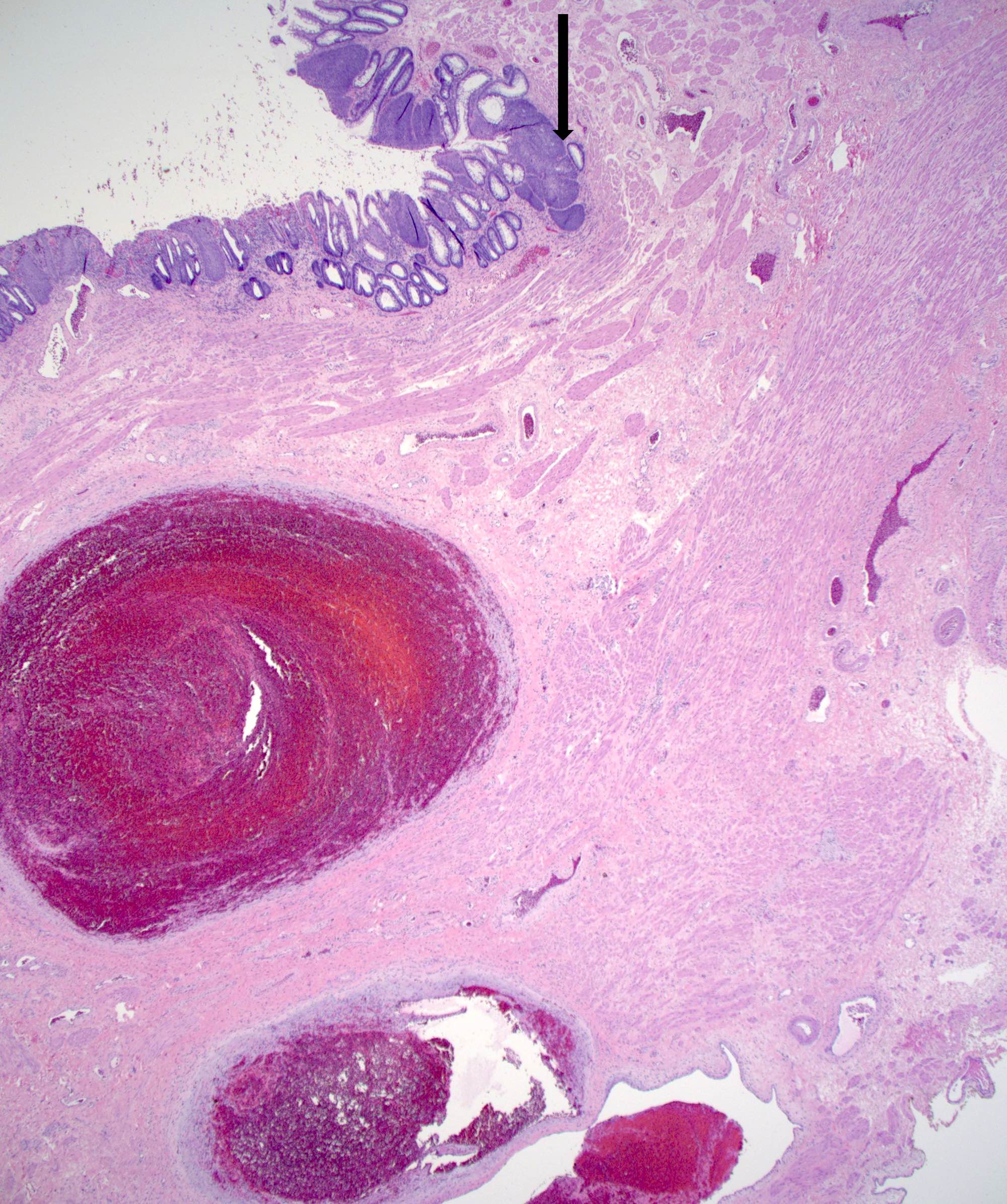
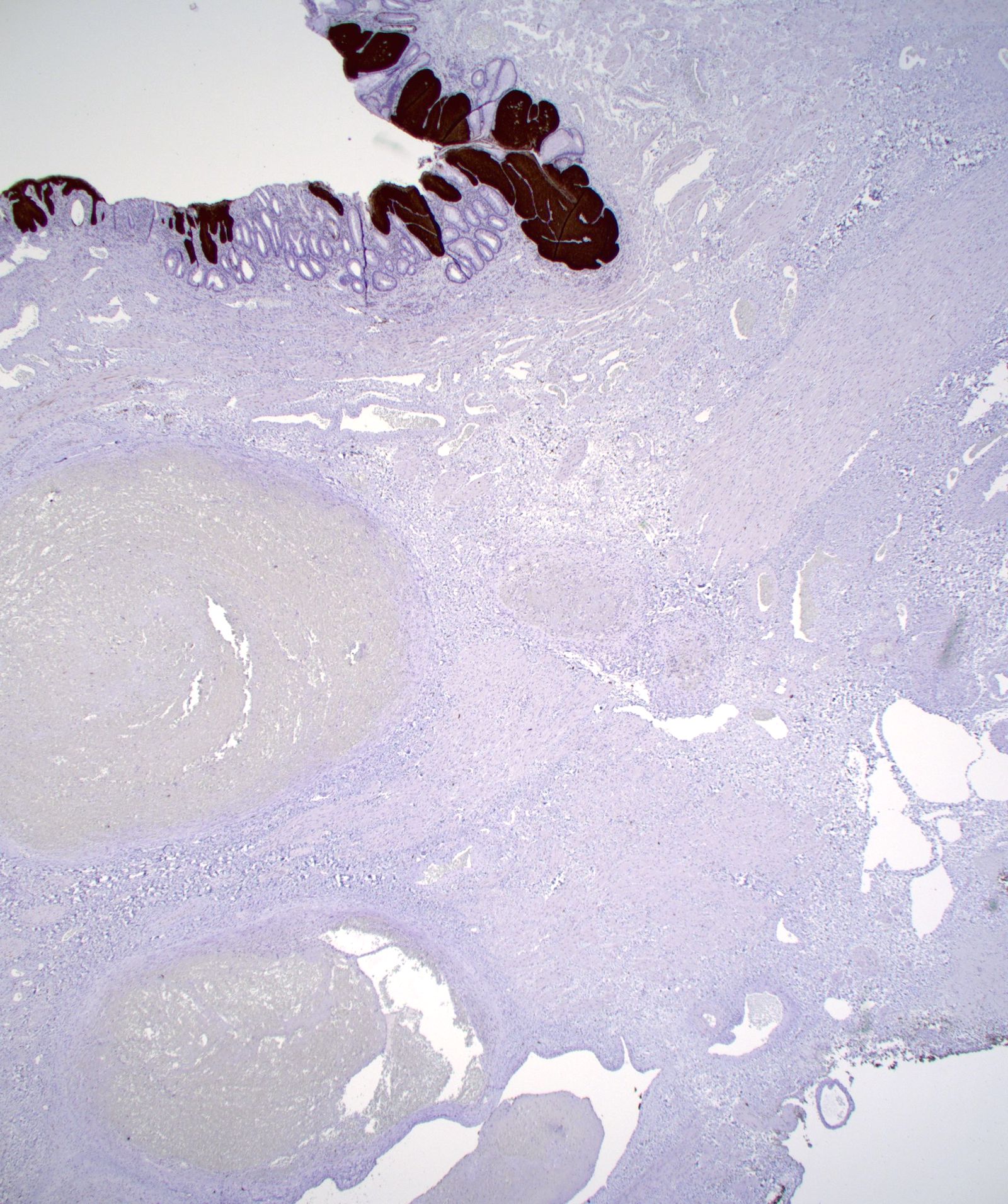
- Typical hemorrhoid histology includes (Am J Surg Pathol 1988;12:41)
- Dilated, thin walled vascular plexus that vary in size and configuration within the stroma
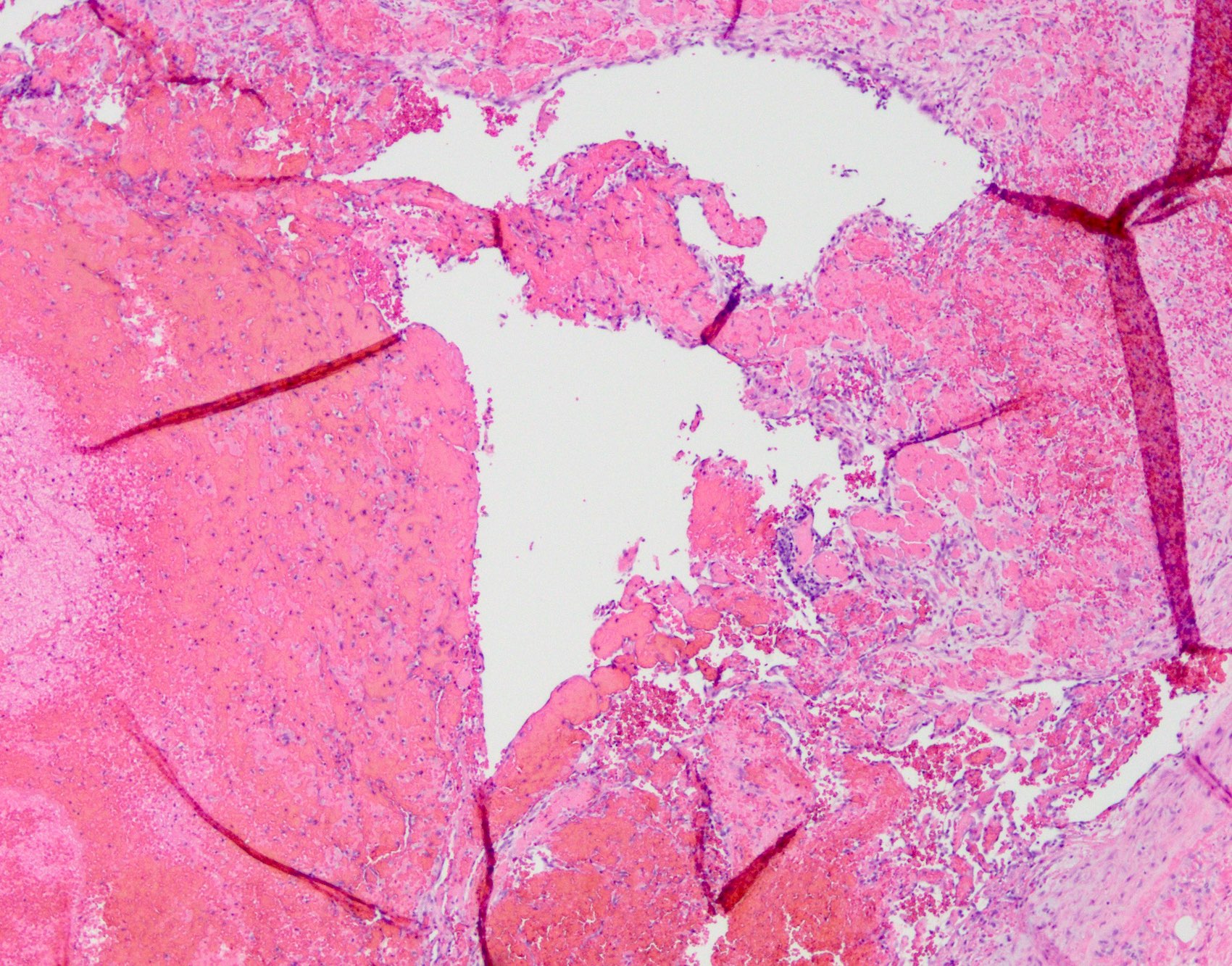
- Recent or past thrombosis can be present
- Fibrosis and scattered smooth muscle fibers may be present in the stroma
- Overlying surface epithelium depends on the degree and descent of hemorrhoid, ranging from colorectal, squamous, perianal or transitional epithelium
- Erosion, inflammatory, metaplastic or keratotic changes can happen in the surface epithelium
- Pagetoid dyskeratosis should be distinguished from HPV cytopathic changes
Microscopic (histologic) images
Contributed by James Mueller, M.D., Ph.D. and Vikram Deshpande, M.D.
Positive stains
Negative stains
- p16 is negative in pagetoid dyskeratosis
Videos
Histopathology of hemorrhoids
Overview of hemorrhoids
Sample pathology report
- Anal tissue, right anterior, hemorrhoidectomy:
- Anal squamous and colonic mucosa with dilated and congested submucosal veins consistent with hemorrhoids
Differential diagnosis
- Histologically a straightforward diagnosis; however, associated pathologies (benign or malignant) are important to find and report
- Diverse clinical differentials (i.e., anal fissure, anorectal abscess, proctitis, rectal prolapse, malignancy, polyps, anorectal varices)
- Anal fibroepithelial polyp or hypertrophied papillae:
- Clinically it may appear as a hemorrhoid when giant and protruding from the anal verge
- Fibroepithelial polyp will have varying amount of stroma covered by papillomatous epidermis and loose fibrovascular connective tissue core
- No evidence of dilated vessels, hemorrhage or organizing thrombi
- Inflammatory cloacogenic polyp:
- Located at the anorectal junction / anal transitional zone
- Morphologically mimic hemorrhoids during examination
- Histologically characterized by tubulovillous growth pattern and irregular shaped crypts displaced into the submucosa, surrounded by a prominent fibromuscular stroma with superficial ulceration
- Arteriovenous malformation:
- Rarely occur as polypoidal shape
- Histologically characterized by widespread full-thickness vasodilation from the submucosa to the serosa and are composed of an inflow artery (feeder), an abnormal blood vessel assembly (nidus) and an outflow vein (drainer)
- Solitary rectal ulcer syndrome:
- Crypt and surface epithelial hyperplasia with erosion and ulceration
- Thickened and hyperplastic muscularis mucosae
- Angiosarcoma:
- Organization and recanalization of thrombosed hemorrhoid can lead to florid papillary endothelial hyperplasia, mimicking angiosarcoma
- Angiosarcoma will have invasive growth pattern with extensive anastomosing vessels, marked atypia, necrosis and increased mitosis as opposed to florid papillary endothelial hyperplasia, which is confined to pre-existing vascular spaces only
Additional references
Practice question #1
A 56 year old woman came to the clinic complaining of a lump protruding from her anal opening. It was initially reducible but it is now irreducible. There is associated pain and itching. She also noticed bright red blood on her stool when she defecates. There is an associated history of chronic constipation. Examination of the perianal area revealed skin tags and a tender perianal mass covered with mucosa. Inspection of the anal mucosa showed no fissure. Histologic examination of the perianal mass revealed the image above. What is the most likely diagnosis?
- External hemorrhoid
- Fourth degree internal hemorrhoid
- Proctitis
- Third degree internal hemorrhoid
Practice answer #1
B. Fourth degree internal hemorrhoid. The image shows thin walled dilated blood vessels with overlying glandular mucosa. Answer A is incorrect because external hemorrhoids are covered with squamous mucosa. Answer D is incorrect because third degree hemorrhoids are reducible with manual replacement. Answer C is incorrect because proctitis does not protrude from the anal opening.
Comment Here
Reference: Hemorrhoids
Comment Here
Reference: Hemorrhoids
Practice question #2
Which of the following is most accurate about the etiology and epidemiology of hemorrhoids?
- Hemorrhoids have a male to female predilection of nearly 4:1
- Internal hemorrhoids often cause cutaneous pain because they are innervated by cutaneous nerves
- Pregnancy is not a risk factor to develop hemorrhoids
- Recognized risk factors associated with the development of hemorrhoids include lack of fiber rich diet, prolonged sitting and pelvic tumors
Practice answer #2
D. Recognized risk factors associated with the development of hemorrhoids include lack of fiber rich diet, prolonged sitting and pelvic tumors. Answer A is incorrect because hemorrhoids have no known sex predilection, although men are more likely to seek treatment. Answer B is incorrect because internal hemorrhoids cannot cause cutaneous pain since they are above the dentate line and are not innervated by cutaneous nerves. Answer C is incorrect because pregnancy is a known risk factor to develop hemorrhoids.
Comment Here
Reference: Hemorrhoids
Comment Here
Reference: Hemorrhoids