Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Liu Q. Hypertrophied papillae. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anushypertrophiedpapillae.html. Accessed September 16th, 2025.
Definition / general
- Benign acquired polypoid projections of anal squamous epithelium and subepithelial connective tissue at the base of the anal columns
Essential features
- Benign acquired polypoid projections at the base of the anal columns
- Results from enlargement of the anal papillae, with reactive hyperplastic nature of the subepithelial connective tissue due to irritation, infection or injury (Am J Surg Pathol 1998;22:70)
- Loose fibrovascular connective tissue core surfaced by mature squamous epithelium
- Large, multinucleated, reactive stromal cells commonly seen
Terminology
- Anal tags, anal fibroepithelial polyps, anal skin tags, sentinel tag (refers to hypertrophied papillae at proximal end of an anal fissure or ulcer)
ICD coding
- ICD-10: K62.0 - anal polyp
Epidemiology
- Common: in ~45% patients undergoing proctoscopy (World J Gastroenterol 2009;15:3687)
- M > F (2:1)
- Usually middle to late adulthood but rare cases have been reported in adolescent patients (Fetal Pediatr Pathol 2020 Nov 9 [Epub ahead of print])
Sites
- Anal canal, at the base of the anal columns (columns of Morgagni)
Pathophysiology
- Results from enlargement of anal papillae
- Reactive hyperplastic nature of the subepithelial connective tissue of the anal mucosa due to irritation, infection or injury (BMJ Case Rep 2010;2010:bcr08.2009.2169)
- Mast cells may play an important role in the pathogenesis, by means of their fibrogenic, fibrolytic and angiogenic activities (Am J Surg Pathol 1998;22:70)
Etiology
- Reactive hyperplastic process of stromal connective tissue, either in isolation or secondary to nearby inflammatory process or mass lesion
- Analogous to cutaneous skin tags / acrochordons
Clinical features
- Usually asymptomatic, found in isolation as subtle swelling or a solitary firm, palpable mass on digital examination
- Tends to enlarge over time (Fetal Pediatr Pathol 2020 Nov 9 [Epub ahead of print])
- Rarely presents as large and prolapsed lesions associated with irritation, infection or chronic fistula or fissure in the anal canal (BMJ Case Rep 2010;2010:bcr08.2009.2169)
- May coexist with hemorrhoids and are confused with hemorrhoids clinically; often submitted to pathologist as hemorrhoid
Diagnosis
- Hemorrhoids may have similar appearance
- Usually requires a histopathological evaluation to establish the diagnosis and to exclude accompanying lesions, such as low or high grade squamous intraepithelial lesions
Radiology description
- Imaging is rarely done and occurs only when it becomes large enough to prolapse into the rectum
- Typical findings include polypoid stromal proliferation, no focal or diffuse restriction and no pelvic lymph node enlargement
Prognostic factors
- Tends to enlarge over time and may convert from an asymptomatic to a symptomatic mass
- No malignant potential
Case reports
- 15 year old boy, otherwise healthy, presented with a giant pedunculated mass projecting out of the anal verge that enlarged over 2 years (Fetal Pediatr Pathol 2020 Nov 9 [Epub ahead of print])
- 38 year old woman presented at the emergency department after a week of anal pain and 1.5 years of vague anal discomfort (BMJ Case Rep 2010;2010:bcr08.2009.2169)
- 67 year old woman was admitted to the emergency room with diffuse, cramping abdominal pain of progressive onset (World J Gastroenterol 2009;15:3687)
- 67 year old man presented with abdominal pain and hematochezia and was referred for colonscopy after a CT scan demonstrated a 3 cm rectal mass with adjacent lymphadenopathy and numerous lesions in the liver, pancreas and bone (Gastrointest Endosc 2015;82:763)
Treatment
- Endoscopic polypectomy or surgical resection in symptomatic cases
- When accompanying an underlying chronic process, correction of the primary etiology
Gross description
- Polypoid, flesh colored projections at the mucocutaneous junction of the upper anal canal that give a serrated appearance
- Usually small in size (2 - 5 mm) but rarely they become enlarged
- Extremely rare case of a giant hypertrophied anal papilla complicated by obstructive ileus was reported (World J Gastroenterol 2009;15:3687)
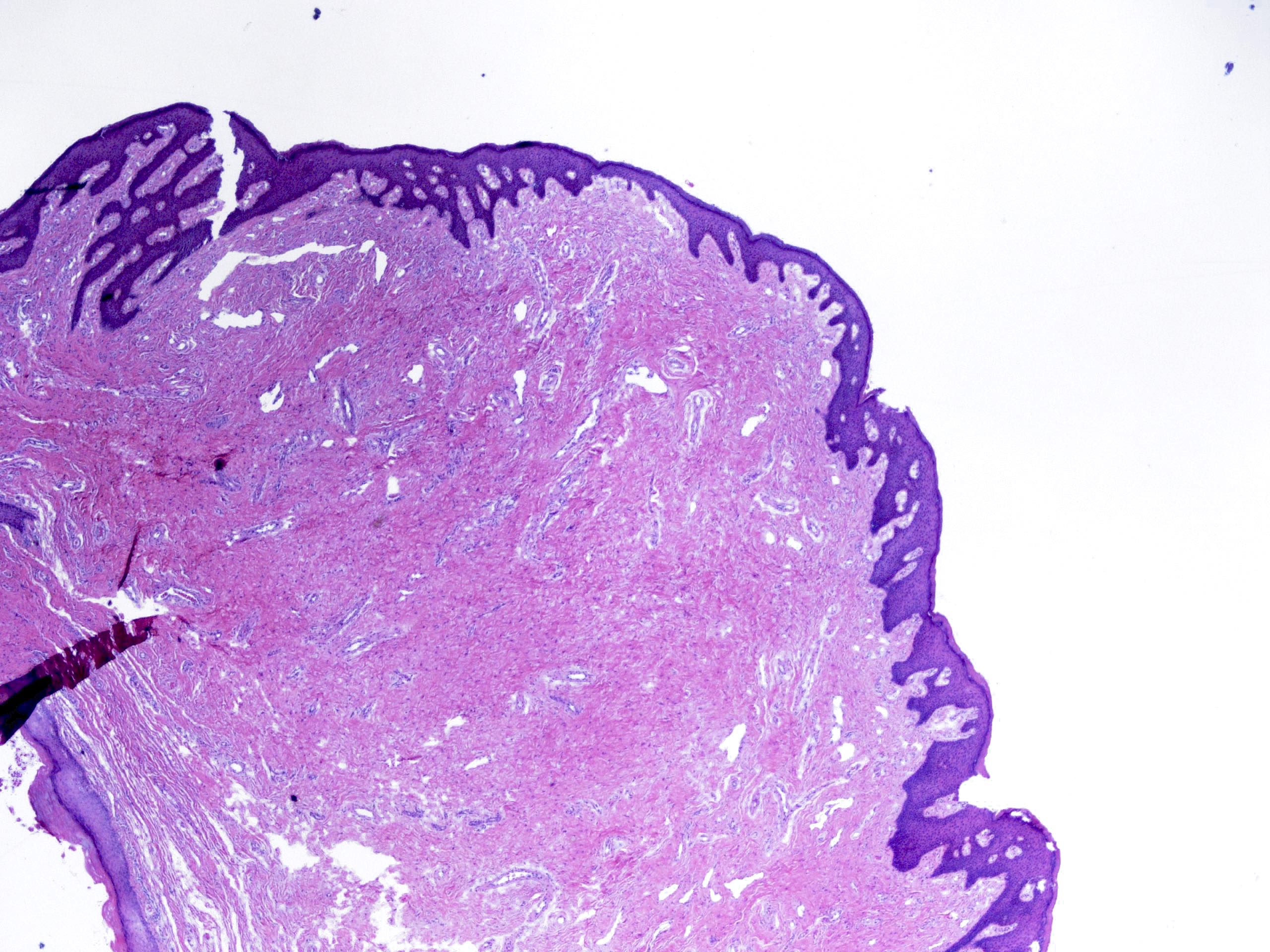
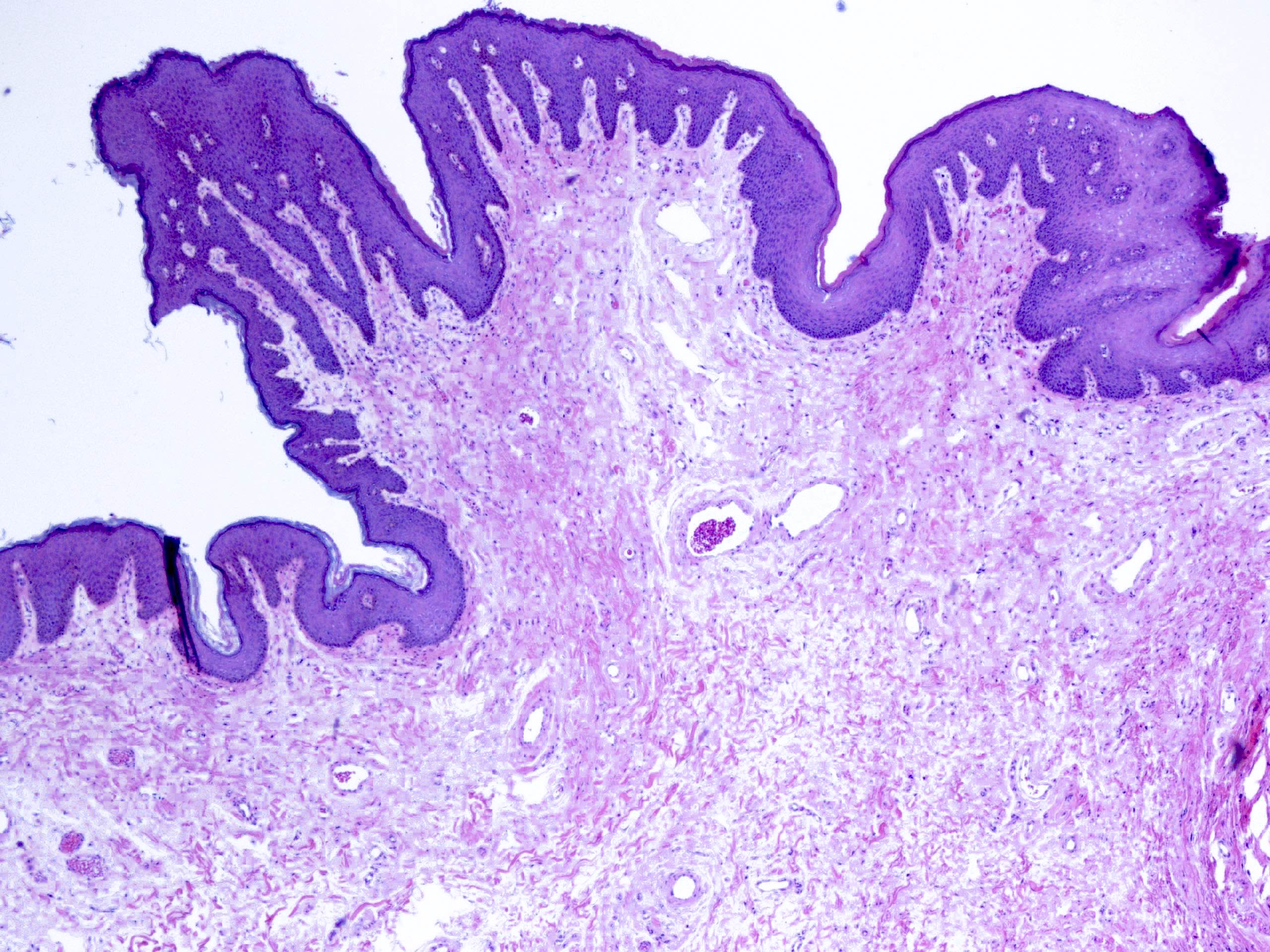
Microscopic (histologic) description
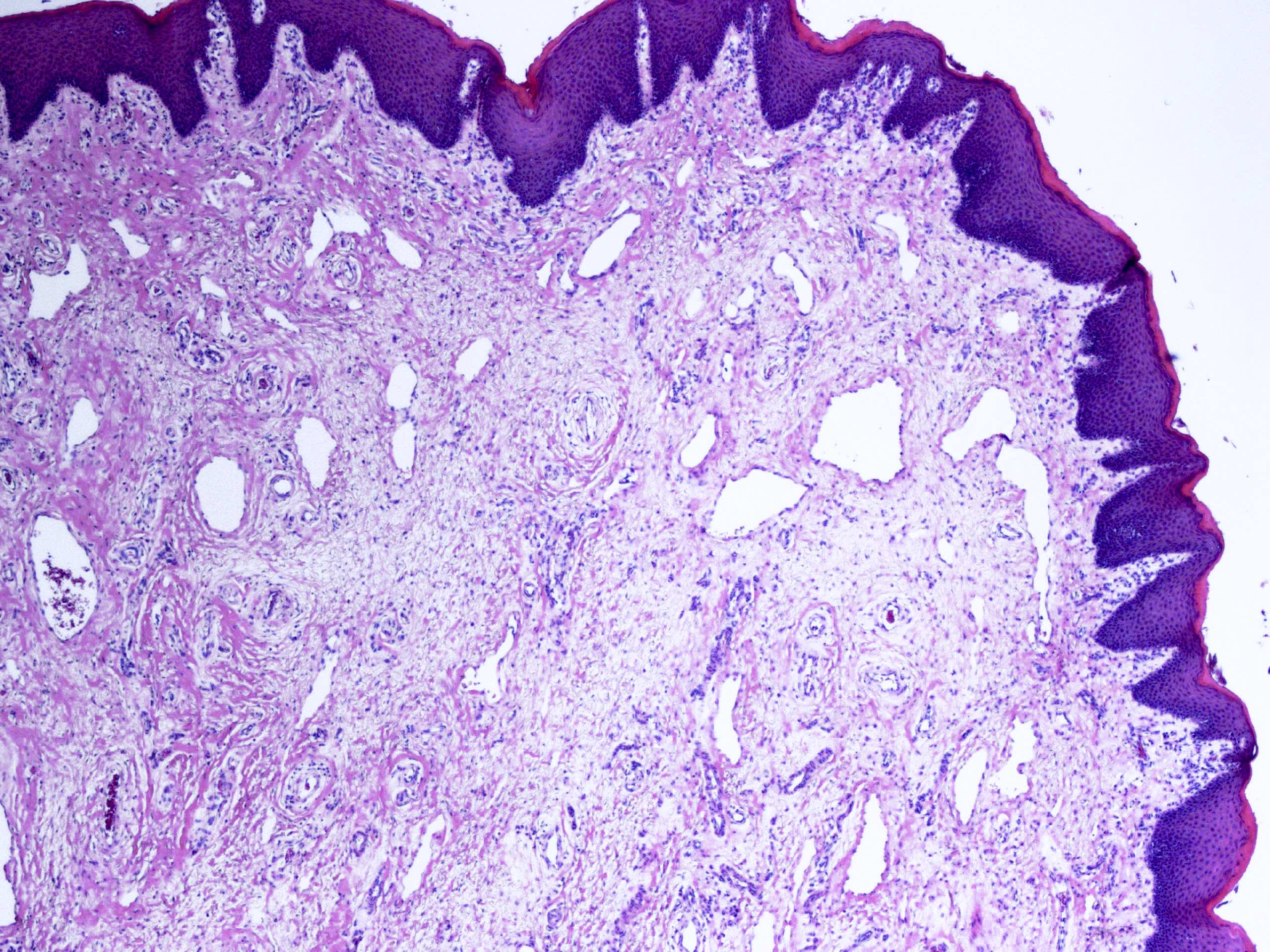
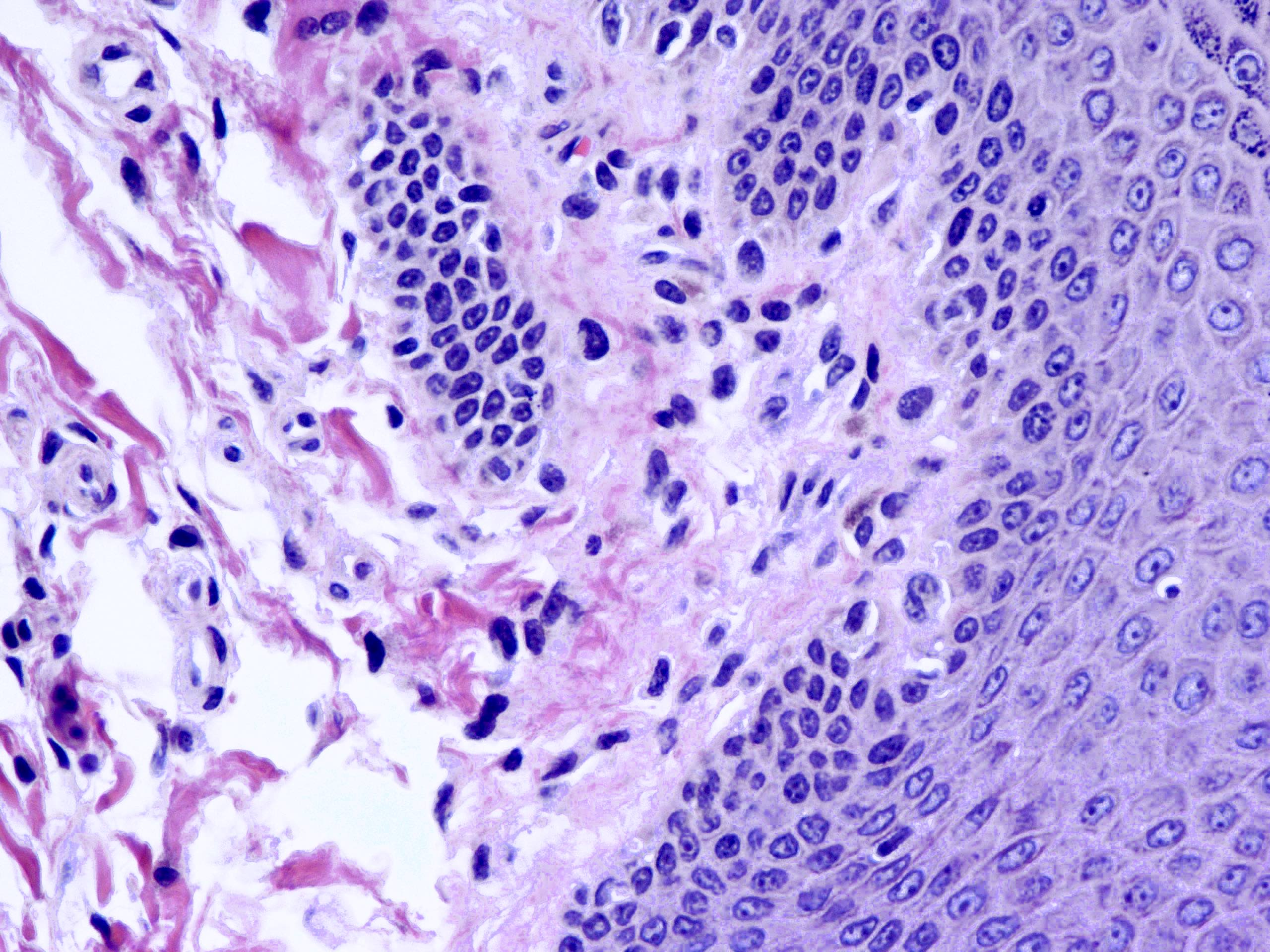
- Myxoid or collagenous stroma surfaced by mature squamous epithelium
- Squamous epithelium may be slightly hyperplastic and shows focal hyperkeratosis and parakeratosis
- Loose fibrovascular connective tissue core, morphologically similar to that of the normal anal mucosa
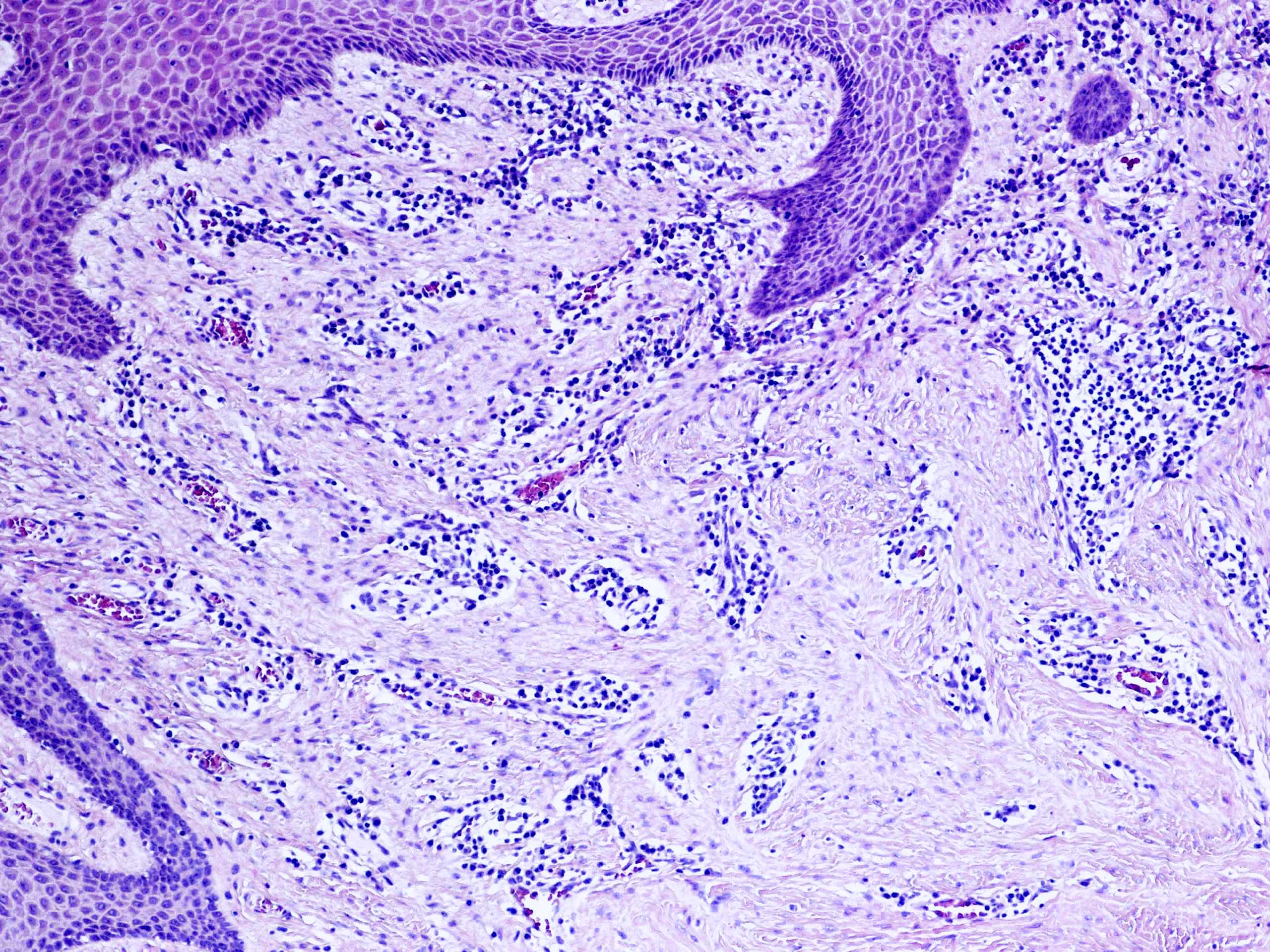
- Large, multinucleated, reactive stromal cells commonly seen (80% of hypertrophied papillae); typically scattered singly in the stroma but occasionally show small areas of aggregation (Am J Surg Pathol 1998;22:70)
- Atypical, bizarre stromal cells may be seen in a polyp of large size
- No mitotic figures present
- Scattered smooth muscle fibers seen in approximately half of polyps
- Mast cells frequently present
- Absent thick walled, thrombosed vessels (features of hemorrhoids)
- Large, multinucleated, reactive stromal cells commonly seen (80% of hypertrophied papillae); typically scattered singly in the stroma but occasionally show small areas of aggregation (Am J Surg Pathol 1998;22:70)
- Chronic inflammation, mostly in the subepithelial region
- Subepithelial zone appears to be more cellular and less collagenous than the center
- Conspicuous lymphatic dilatation
- Epithelial endovascular displacement (vascular pseudoinvasion) is uncommonly seen, associated with morphological signs of traumatism (Int J Surg Pathol 2020;28:764)
Microscopic (histologic) images
Positive stains
- Vimentin, CD34 (stromal cells) (Am J Surg Pathol 1998;22:70)
- Desmin (stromal cells in 30% of cases) (Am J Surg Pathol 1998;22:70)
- Giemsa stain, CD117 (mast cells)
- Masson trichrome (collagen)
Negative stains
- Alpha smooth muscle actin (stromal cells)
Electron microscopy description
- Stromal cells demonstrate fibroblastic and myofibroblastic features (Am J Surg Pathol 1998;22:70)
Sample pathology report
- Anal polyp, excision:
- Hypertrophied anal papillae (anal fibroepithelial polyp)
Differential diagnosis
- Hemorrhoids:
- Dilated thick walled submucosal vessels and sinusoidal spaces
- Often with thrombosis and hemorrhaging into the surrounding connective tissues
- Condyloma accuminatum:
- Acanthosis with papillomatosis
- Variable dysplastic changes, including koilocytic atypia (nuclear wrinkling with perinuclear clearing), increased nuclear atypia / size, increased / atypical mitosis
- Infection / abscess:
- Nonspecific acute and chronic inflammation and granulation tissue
- Anorectal tumors (carcinoma or anal melanoma, neuroendocrine tumor, lymphoma) (Clin Dermatol 1987;5:87)
Practice question #1
A 65 year old man visited his gastroenterologist for anal bleeding. He had experienced intermittent anal bleeding due to longstanding hemorrhoidal disease over the past 10 years. On physical examination, digital examination revealed a medium sized elastic mass with convoluted grooves on a smooth surface in the proximal anus. This lesion was excised and sent to pathology for histological evaluation. The H&E image is shown. Which of the following is the most likely diagnosis?
- External hemorrhoids
- Hypertrophied anal papillae
- Internal hemorrhoids
- Prolapsed associated inflammatory polyp
Practice answer #1
Practice question #2
Which underlying condition(s) is associated with hypertrophied anal papillae?
- Chronic fistula
- Degenerative change of perianal structure
- Elevated intra-abdominal pressure
- HPV infection
Practice answer #2