Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Saulino D, Hernandez Gonzalo D. Lichenoid esophagitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophaguslichenplanus.html. Accessed August 27th, 2025.
Definition / general
- Lichenoid esophagitis is an umbrella term to cover a histologic pattern of injury; it is not a specific diagnosis
- Lichen planus can cause this pattern of injury
- In cases without evidence of skin disease or positive immunofluorescence (IF), the etiology can be quite variable, including:
- Infections (especially HIV and viral hepatitis)
- Crohn's disease
- Medications (NSAIDs, antihypertensives, checkpoint inhibitors, antimalarial drugs)
- Pill esophagitis
- Rheumatologic disorders
Essential features
- Umbrella term with many different etiologies, describing a pattern of injury
- Proximal and mid esophagus of middle aged or elderly women
- Endoscopy often shows white plaque or streaks
- Histology shows Civatte bodies and characteristic distribution of lymphocytes
Terminology
- Findings can be described as “lichenoid esophagitis pattern” (LEP) in patients without lichen planus (who have “lichen planus esophagitis”)
ICD coding
- ICD-10: K20.9 - esophagitis, unspecified
Epidemiology
- More frequent in females (71%)
- Median age 58 years (Am J Surg Pathol 2013;37:1889)
Sites
- Mid esophagus more frequently involved in lichenoid esophagitis pattern
- Upper and lower esophagus more frequently involved in true lichen planus esophagitis
Pathophysiology
- Lichen planus appears to be mediated by cytotoxic CD8 T cells that attack an antigen in the basal epithelium in a manner resembling graft versus host disease (GVHD) (Dis Esophagus 2003;16:47)
- Predisposing factors for oral lichen planus include medications such as antimalarial drugs, NSAIDs, antihypertensive agents and dental materials such as amalgam
Etiology
- Lichen planus
- Infections (especially HIV and viral hepatitis)
- Upper tract Crohn's disease
- Medications: nivolumab and other checkpoint inhibitors, antimalarial drugs, gold, NSAIDs and thiazides (ACG Case Rep J 2017;4:e57)
- Mucosa physically damaged by nearby pill esophagitis
- Rheumatologic disorders
Clinical features
- Rheumatologic diseases more common in patients with lichen planus esophagitis (24%) versus lichenoid esophagitis pattern (11%) (Am J Surg Pathol 2013;37:1889)
- Viral hepatitides and human immunodeficiency virus (HIV) infections are associated with lichenoid esophagitis pattern (Am J Surg Pathol 2013;37:1889)
Diagnosis
- Histologic assessment of biopsy
Prognostic factors
- Squamous dysplasia and carcinoma have been described; periodic surveillance may be useful (Eur J Gastroenterol Hepatol 2006;18:1111, Am J Surg Pathol 2013;37:1889)
- Stricture: risk of stricture formation is higher in patients with lichen planus esophagitis (38%) versus lichenoid esophagitis pattern (9%) (Am J Surg Pathol 2013;37:1889)
Case reports
- 63 year old woman with dysphagia and areas of friable mucosa and stricture at the upper / mid esophagus (World J Gastroenterol 2013;19:1652)
- 68 year old patient with isolated esophageal involvement (Z Gastroenterol 2004;42:379)
- 69 year old woman with dysphagia and odynophagia; endoscopy revealed severe strictures and web-like areas in esophagus (World J Gastroenterol 2013;19:2278)
- Two siblings with lichen planus and squamous cell carcinoma of the esophagus (Eur J Gastroenterol Hepatol 2006;18:1111)
Treatment
- Corticosteroids for esophageal lichen planus
- Esophageal dilation for patients with stricture
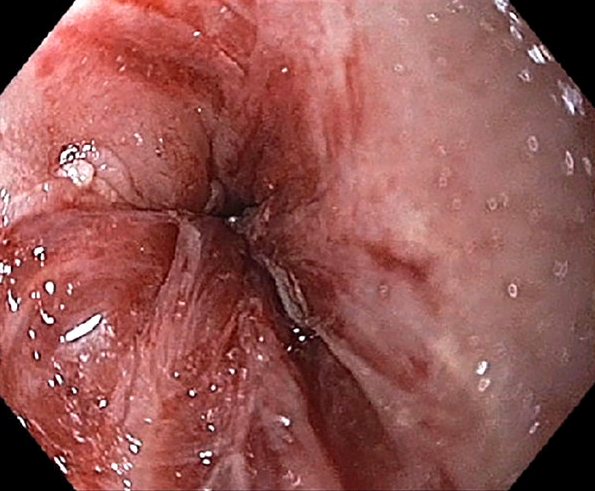
Clinical images
Gross description
- At endoscopy (Am J Surg Pathol 2013;37:1889)
- White plaques or streaks are present, mimicking candidiasis or glycogenic acanthosis
- In addition, it may cause ulceration in mid or proximal esophagus
- Strictures can also be present
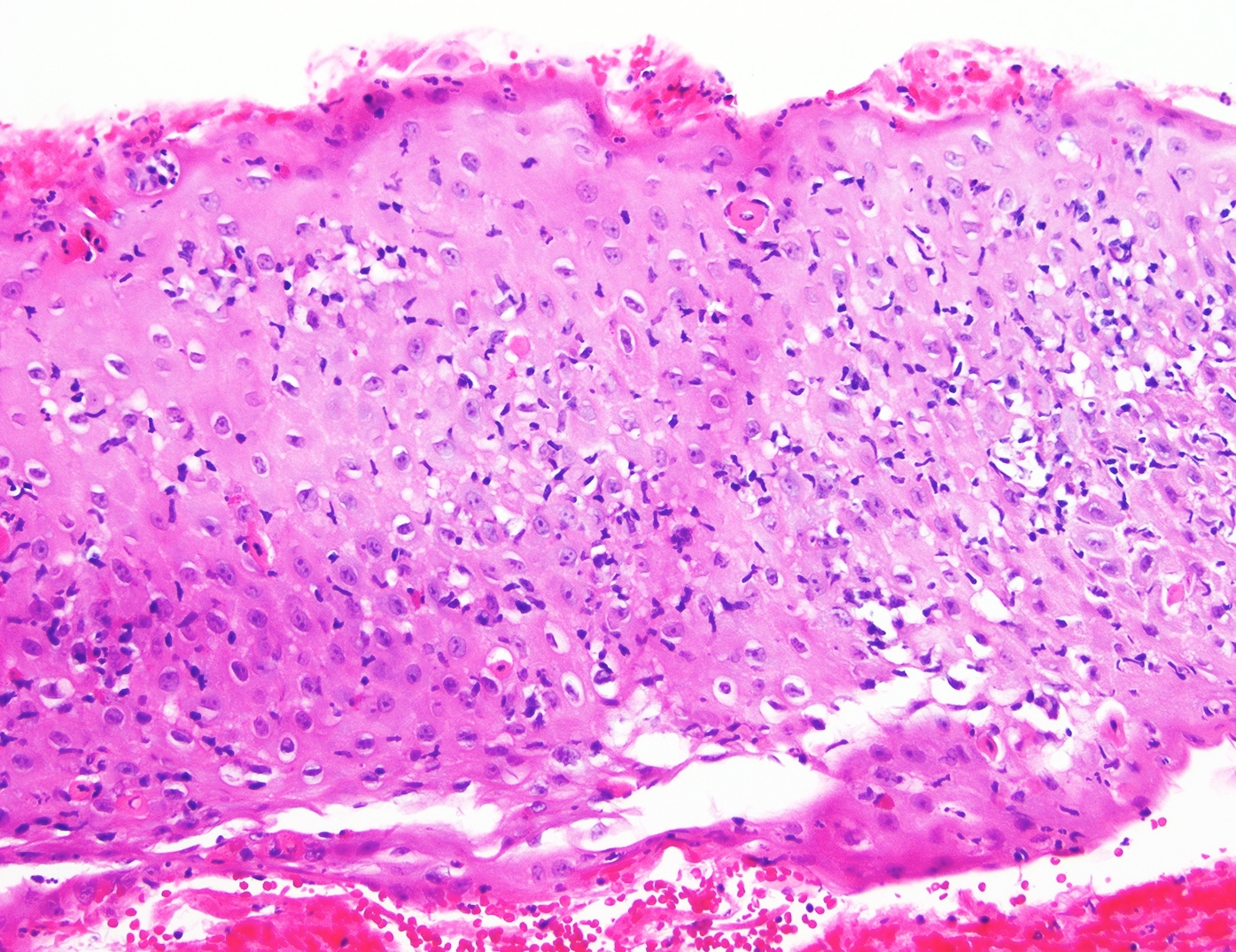
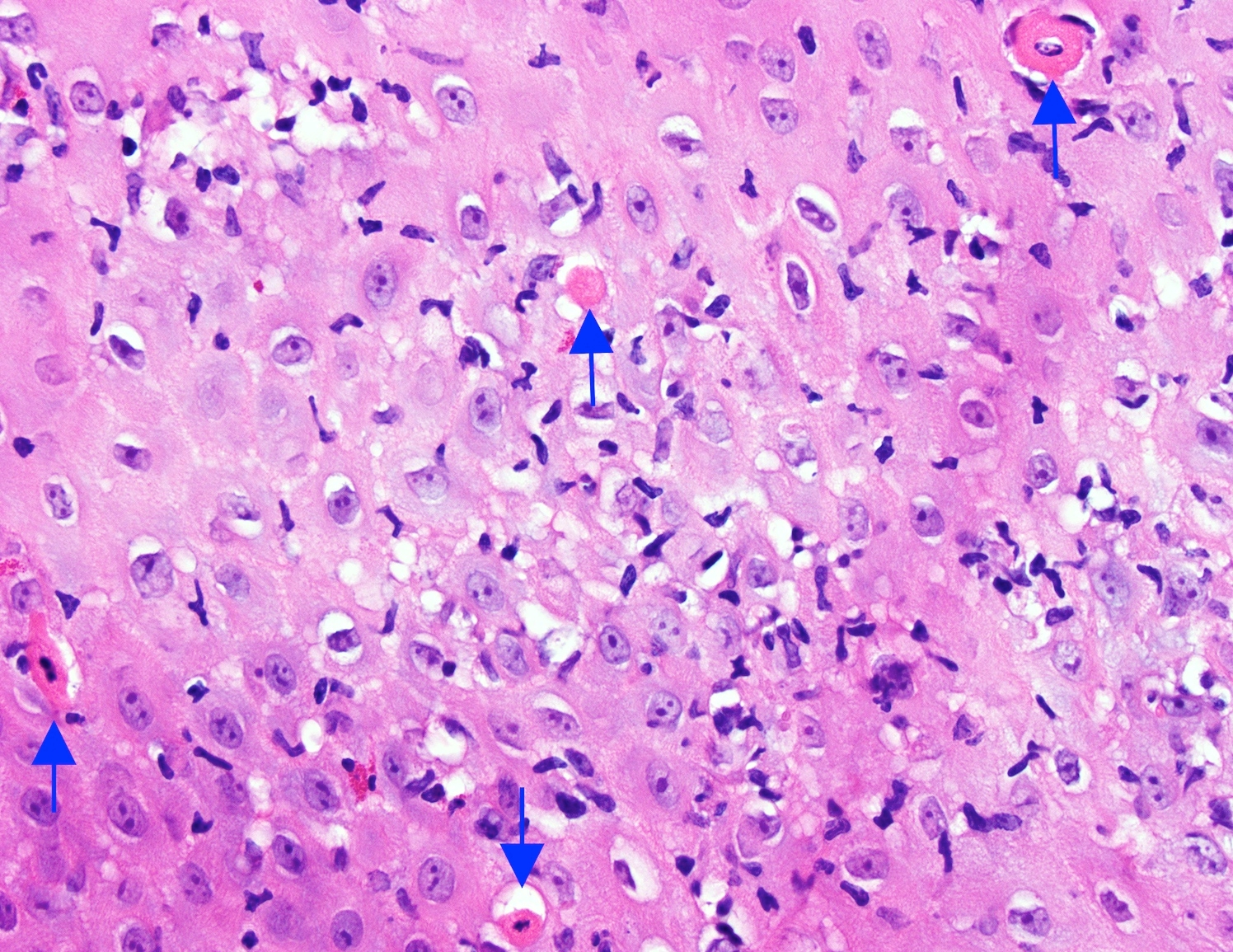
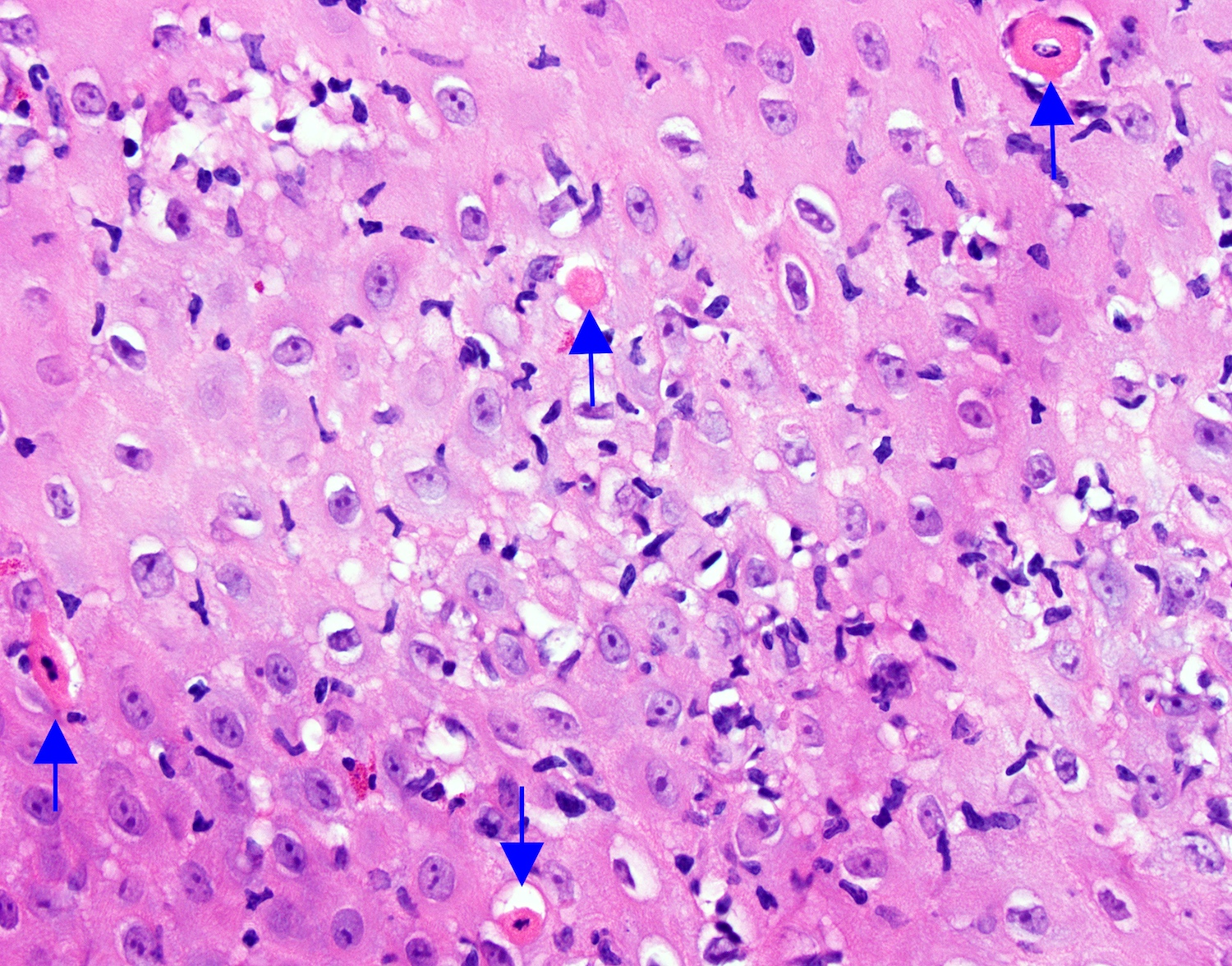
Microscopic (histologic) description
- Prominent band-like lymphocytic infiltrate involving the interface of basal epithelium and lamina propria (this feature cannot be evaluated in biopsies lacking lamina propria) (Am J Surg Pathol 2013;37:1889)
- Intraepithelial lymphocytosis
- Dyskeratotic keratinocytes (Civatte bodies)
- Acanthosis
- Junctional split seen at the junction of the epithelium and lamina propria (unlike sloughing esophagitis)
Microscopic (histologic) images
Immunofluorescence description
- Negative in lichenoid esophagitis pattern
- In lichen planus esophagitis, globular IgM deposits at the junction of the squamous epithelium and lamina propria as well as complement staining in apoptotic keratinocytes
Positive stains
Negative stains
- GMS (no fungal microorganisms)
Sample pathology report
- Proximal esophagus, biopsy:
- Esophageal squamous mucosa with lichenoid esophagitis pattern of injury (see comment)
- Comment: The biopsy demonstrates a prominent band-like lymphocytic infiltrate involving the interface of lamina propria and epithelium, intraepithelial lymphocytes and dyskeratotic keratinocytes. Unfortunately, this pattern of injury is not entirely specific and can be seen as an esophageal manifestation of lichen planus, viral infections (particularly HIV and viral hepatitis), Crohn's disease, medications (NSAIDs, antihypertensive agents, antimalarial drugs) or pill esophagitis. Correlation with the clinical findings (in particular with cutaneous, oral or genital lesions) is suggested. If lichen planus is a consideration, additional biopsies with fresh tissue for immunofluorescence studies are worth performing. No fungal organisms were identified on the GMS stain. There is no dysplasia.
Differential diagnosis
- Candida esophagitis:
- Endoscopic findings (white plaques) can be similar to lichenoid esophagitis pattern
- Microscopic similarities to lichenoid esophagitis pattern: numerous intraepithelial lymphocytes, superficial neutrophils, parakeratosis and Civatte bodies
- Desquamated and hyperpink parakeratosis
- Pseudohyphae and budding yeast: GMS positive (should always be performed when entertaining a diagnosis of lichenoid esophagitis pattern)
- Gastroesophageal reflux disease (GERD):
- Predilection for distal esophagus
- Basal cell hyperplasia, spongiosis and elongated papillae
- Intraepithelial lymphocytes can be seen but are accompanied by eosinophils and rare neutrophils
- Apoptotic keratinocytes not a diagnostic feature
- Lymphocytic esophagitis:
- Lymphocytes tend to have a peripapillary distribution while in lichenoid esophagitis pattern prominent band-like lymphocytic infiltrate involves the interface of basal epithelium and lamina propria
- In biopsies lacking lamina propria it is a challenge to assess the distribution of lymphocytes
- Eosinophilic esophagitis:
- Endoscopically similar findings to lichenoid esophagitis pattern
- Prominent eosinophils rather than lymphocytes
- Sloughing esophagitis:
- Intraepithelial split while in lichenoid esophagitis pattern split is at the junction of the epithelium and lamina propria
- Inflammation not prominent
- Isolated esophageal mucous membrane pemphigoid:
- Positive immunofluorescence with linear deposits of IgG
- Serum anti BP230 or BP180 antibodies
- Treatment requires systemic immunosuppression and may be worsened by repeated dilations alone; should be considered in patients with unexplained dysphagia accompanied by mucosal sloughing, strictures and ulcerations (Am J Gastroenterol 2019;114:1695)
- Esophageal GVHD:
- History of hematopoietic stem cell transplant
- Intraepithelial lymphocytosis, basilar vacuolization, epithelial apoptosis and necrosis in severe disease
- Esophageal webs or strictures in upper or mid third of the esophagus can be seen in chronic GVHD (Best Pract Res Clin Haematol 2008;21:251)
Additional references
Practice question #1
- A 45 year old woman with dysphagia undergoes an upper endoscopy which demonstrates mucosal breaks involving at least 75% of esophageal circumference in mid esophagus. Tissue submitted for immunofluorescence study is negative and the patient has no skin, oral or genital lesions. An esophageal biopsy demonstrates the findings shown above. Which one of the following has been associated with this pattern of injury?
- Cytomegalovirus
- Herpes virus I/II
- HIV and viral hepatitis
- Sarcina ventriculi
Practice answer #1
C. HIV and viral hepatitis
HIV and viral hepatitis have been associated with lichenoid esophagitis pattern, shown here. Sarcina ventriculi is a Gram positive coccus, recognized in gastric biopsies, particularly of patients with delayed gastric emptying characterized by basophilic staining and tetrad arrangement. Cytomegalovirus causes viral cytopathic effect seen at the base of esophageal ulcers involving endothelial cells. Herpes virus I/II would show multinucleation, margination and molding (3 M’s) within superficial epithelial cells.
Comment Here
Reference: Lichenoid esophagitis
HIV and viral hepatitis have been associated with lichenoid esophagitis pattern, shown here. Sarcina ventriculi is a Gram positive coccus, recognized in gastric biopsies, particularly of patients with delayed gastric emptying characterized by basophilic staining and tetrad arrangement. Cytomegalovirus causes viral cytopathic effect seen at the base of esophageal ulcers involving endothelial cells. Herpes virus I/II would show multinucleation, margination and molding (3 M’s) within superficial epithelial cells.
Comment Here
Reference: Lichenoid esophagitis
Practice question #2
- Which of the followings is true regarding lichenoid esophagitis pattern of injury?
- Dysphagia is not a common symptom in lichenoid esophagitis pattern patients
- Stricture formation in mid esophagus can be seen in upper endoscopy
- There are no reports of an association with squamous cell neoplasia
- White plaques in distal esophagus of young men is the typical clinical scenario
Practice answer #2
B. Stricture formation in mid esophagus can be seen in upper endoscopy
Lichenoid esophagitis pattern has been rarely reported in association with dysplasia and carcinoma and periodic surveillance should be suggested. White plaques in proximal esophagus of middle aged women is a common endoscopic finding. Endoscopically it may mimic Candida esophagitis or eosinophilic esophagitis. Stricture formation can be seen but is not a common finding in lichenoid esophagitis pattern unlike lichen planus esophagitis. Mid esophagus is more frequently involved in lichenoid esophagitis pattern. Dysphagia is a common symptom at the time of endoscopy.
Comment Here
Reference: Lichenoid esophagitis
Lichenoid esophagitis pattern has been rarely reported in association with dysplasia and carcinoma and periodic surveillance should be suggested. White plaques in proximal esophagus of middle aged women is a common endoscopic finding. Endoscopically it may mimic Candida esophagitis or eosinophilic esophagitis. Stricture formation can be seen but is not a common finding in lichenoid esophagitis pattern unlike lichen planus esophagitis. Mid esophagus is more frequently involved in lichenoid esophagitis pattern. Dysphagia is a common symptom at the time of endoscopy.
Comment Here
Reference: Lichenoid esophagitis