Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Gertsen B, Huber AR. Reflux esophagitis / gastroesophageal reflux disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophagusreflux.html. Accessed August 24th, 2025.
Definition / general
- Reflux esophagitis (RE) / gastroesophageal reflux disease (GERD) is the reflux of gastric contents into the esophagus that results in symptoms or complications; reflux esophagitis / gastroesophageal reflux disease is objectively defined as mucosal injury seen at endoscopy or abnormal esophageal acid exposure on a reflux monitoring study
- Remains one of the most common diseases seen by gastroenterologists, surgeons and primary care physicians (Am J Gastroenterol 2022;117:27)
Essential features
- One of the most common diseases in everyday pathology practice
- May affect all ages and is more common in men
- Caused by reflux of gastric contents into the distal esophagus
- Minimum criteria for histologic diagnosis have not been established
- 3 main histologic features are basal cell hyperplasia, elongation of the lamina propria papillae and inflammatory infiltrates
- Mainstay of therapy is proton pump inhibitors
ICD coding
Epidemiology
- Affects an estimated 20% of the United States population
- Prevalence is increasing worldwide
- Males affected more commonly than females
- All ages, including infants and children
- One of the most costly gastrointestinal diseases in the United States, exceeding $14 billion dollars annually
- References: Adv Anat Pathol 2009;16:161, World J Surg 2017;41:1698, Surg Clin North Am 2015;95:515
Sites
- Esophageal mucosa
Pathophysiology
- Lower esophageal sphincter (LES) is a circular muscle layer at the distal esophagus that creates a higher pressure than the intra-abdominal pressure
- Physiologic reflux does occur and is termed transient lower esophageal sphincter relaxations (TLESRs)
- TLESRs are a normal mechanism for the stomach to vent and may be activated by things such as gastric distension
- TLESRs are increased in those with reflux esophagitis / gastroesophageal reflux disease
- Inappropriate relaxation of the LES allows gastric acid to enter the distal esophagus
- Chemoreceptors are stimulated and irritation occurs, causing symptoms
- Symptoms result from mucosal injury and are directly related to frequency of the reflux, duration of reflux and the injurious potential of the refluxate
- Certain drugs may relax the tone of the LES and worsen reflux
- Hiatal hernias are associated with reflux esophagitis / gastroesophageal reflux disease
- Reference: Surg Clin North Am 2015;95:515
Etiology
- Caused by reflux of gastric contents into the lower esophagus
Clinical features
- May be asymptomatic
- Typical symptoms are heartburn and regurgitation
- May have so called extraesophageal symptoms, including hoarseness, cough, odynophagia, reflux induced asthma, laryngitis and aspiration pneumonia
- Atypical or severe symptoms (hematemesis, weight loss, dysphagia) may indicate a stricture or malignancy, endoscopic evaluation is recommended as the first test
- References: Histopathology 2012;60:864, Surg Clin North Am 2015;95:515, Am J Gastroenterol 2022;117:27
Diagnosis
- No gold standard for diagnosis
- Combination of symptoms, endoscopy, pH monitoring and response to therapy
- Classic endoscopic findings include erosions / ulcers, erythema and mucosal edema
- Some have normal or near normal endoscopy with typical reflux symptoms, so called nonerosive reflux disease (NERD)
- References: Adv Anat Pathol 2009;16:161, Am J Gastroenterol 2022;117:27
Case reports
- 34 year old man, a Swiss bagpipe player with chronic cough (Gut 2018;67:1792)
- 35 year old man with drenching night sweats (Can Fam Physician 2020;66:901)
- 54 year old woman with idiopathic pulmonary fibrosis and gastroesophageal reflux disease (Respir Med Case Rep 2016;17:40)
Treatment
- Diet and lifestyle modifications: weight loss for obese patients, elevating the head of the bed, tobacco and alcohol cessation, avoiding late night meals and bedtime snacks, staying upright after eating and not ingesting foods known to make reflux worse (coffee, chocolate, carbonated beverages, spicy foods, acidic foods and fatty foods)
- Proton pump inhibitors (PPIs) are the mainstay of therapy
- Histamine 2 receptor antagonists may be added to PPIs for persistent nocturnal symptoms
- Surgical treatment (e.g., fundoplication) is an option for those with chronic gastroesophageal reflux disease whose symptoms do not respond to medical management or have a defective lower esophageal sphincter (LES) (Goldblum: Rosai and Ackerman’s Surgical Pathology, 11th Edition, 2017)
- Reference: Am J Gastroenterol 2022;117:27
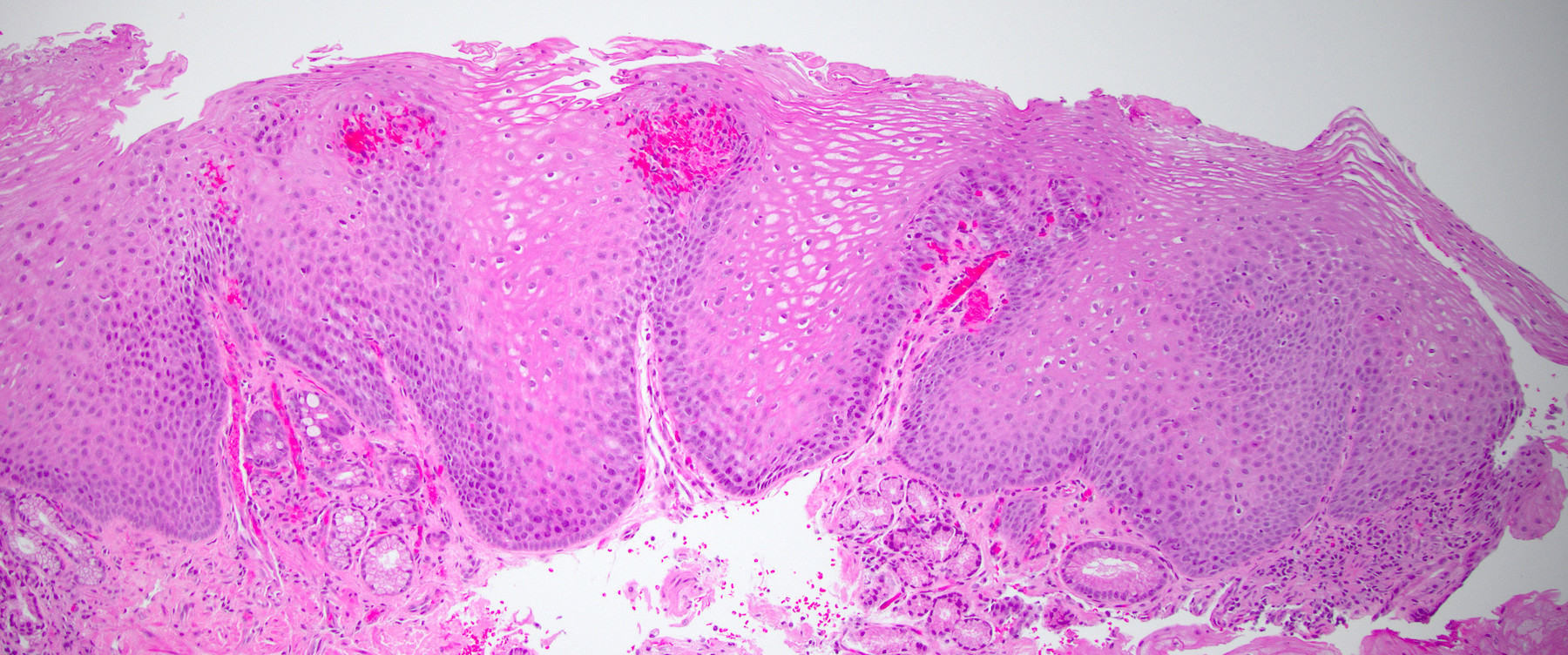
Microscopic (histologic) description
- The 3 major features of reflux esophagitis / gastroesophageal reflux disease are:
- Inflammatory cells in the squamous epithelium
- Elongation of the lamina propria papillae
- Basal cell hyperplasia
- Inflammatory infiltrate may be composed of neutrophils, eosinophils and lymphocytes
- Numerous neutrophils suggest severe injury; eosinophils are seen in 50% of cases
- Lymphocytes are present as squiggle cells, in between the squamous epithelial cells
- Normal basal cell layer is only 1 - 4 cells in thickness and makes up only the bottom 10 - 15% of the epithelial thickness; basal cell hyperplasia is defined as more than 15% of the thickness of the epithelium
- Lamina propria papillae elongation, to a height > two - thirds of the epithelial thickness, is commonly seen in reflux esophagitis / gastroesophageal reflux disease
- Capillaries within the lamina propria papillae may show congestion and red blood cell extravasation
- Distended squamous epithelial cells are nonspecific and termed balloon cells
- Spongiosis is common and may be a marker of early injury without endoscopic findings; this is seen in up to 80% of NERD cases
- Notably, none of these features are specific for reflux esophagitis / gastroesophageal reflux disease
- Minimum criteria for a diagnosis of reflux esophagitis / gastroesophageal reflux disease remain undefined
- References: Adv Anat Pathol 2009;16:161, Histopathology 2012;60:864
Microscopic (histologic) images
Sample pathology report
- Esophagus, biopsy:
- Changes consistent with reflux esophagitis
Differential diagnosis
- Eosinophilic esophagitis:
- More eosinophils, proximal and mid esophagus should be involved
- Must exclude reflux esophagitis / gastroesophageal reflux disease, after trial of high dose PPIs
- Lymphocytic esophagitis:
- Increased intraepithelial lymphocytes
- Uncertain clinical significance
- May be associated with Crohn's disease or achalasia
- Infectious esophagitis if prominent neutrophilic infiltrate or ulcer / erosion:
- Exclude with special stains for fungal or viral causes
- Pill esophagitis:
- May have crystalline polarizable or nonpolarizable material
- Systemic diseases such as collagen vascular disease, Crohn's disease, Stevens-Johnson syndrome, various bullous diseases, lichen planus and graft versus host disease
- Trauma and other injuries:
- Chemotherapy, radiation:
- Telangiectasia, bizarre cells
- Chemotherapy, radiation:
Practice question #1
A 43 year old man complains of several months of reflux and regurgitation that is worse after eating and while lying down. Upper endoscopy shows mucosal erythema and erosions of the distal esophagus. After esophageal pH monitoring, the patient is diagnosed with gastroesophageal reflux disease. A histologic image of the esophageal biopsy is shown above. What are the 3 main histologic features of reflux esophagitis / gastroesophageal reflux disease?
- Basal cell hyperplasia, elongation of the lamina propria papillae, inflammatory infiltrates
- Basal cell hyperplasia, loss of polarity, > 15 - 20 eosinophils per high power field
- Elongation of the lamina propria papillae, necrosis, increased apoptotic bodies
- Full thickness atypia, inflammatory infiltrates, > 15 - 20 eosinophils per high power field
Practice answer #1
A. Basal cell hyperplasia, elongation of the lamina propria papillae, inflammatory infiltrates
Comment Here
Reference: Reflux esophagitis / gastroesophageal reflux disease
Comment Here
Reference: Reflux esophagitis / gastroesophageal reflux disease
Practice question #2
What is the mainstay of therapy for reflux esophagitis / gastroesophageal reflux disease?
- Behavioral modification
- Fundoplication
- Histamine 2 receptor antagonists
- NSAIDs
- Proton pump inhibitors
Practice answer #2
E. Proton pump inhibitors
Comment Here
Reference: Reflux esophagitis / gastroesophageal reflux disease
Comment Here
Reference: Reflux esophagitis / gastroesophageal reflux disease