Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Younus A, Bhalla R. Eosinophilic vacuolated tumor (EVT). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumorevt.html. Accessed September 23rd, 2025.
Definition / general
- Emerging oncocytic renal neoplasm, not classifiable as oncocytoma, chromophobe renal cell carcinoma or other types with eosinophilic features
- Neoplastic cells characterized by abundant eosinophilic (oncocytic) cytoplasm with intracytoplasmic vacuoles and large nuclei, often with prominent nucleoli
- Included under other oncocytic tumors of the kidney in the WHO Classification of Tumours, Urinary and Male Genital Tumours (5th edition)
Essential features
- Nests of eosinophilic (oncocytic) cells with large intracytoplasmic vacuoles and large nuclei, often with prominent nucleoli, imparting a high grade nuclear appearance
- Relatively consistent immunohistochemical profile
- PAX8, AE1 / AE3, cathepsin K and CD117 positive (cathepsin K and CD117 may be focal)
- Vimentin, HMB45, MelanA and TFE3 negative
- CK7 and CK20 variable (negative to focal)
- Sporadic but can occur in tuberous sclerosis complex (TSC)
- Nonoverlapping mutations in MTOR, TSC2 or TSC1, resulting in mTORC1 pathway activation
Terminology
- Eosinophilic vacuolated tumor was the name proposed by Genitourinary Pathology Society (GUPS) (Mod Pathol 2021;34:1167)
- High grade oncocytic renal tumor (HOT) by He et al. (Virchows Arch 2018;473:725)
ICD coding
- ICD-11: 2F98 - neoplasm of unknown behavior of urinary organs
Epidemiology
- F > M
- Wide age range (25 - 73 years)
- Indolent course
- Sporadic tumor with rare association with tuberous sclerosis
- References: Mod Pathol 2022;35:344, Mod Pathol 2021;34:1167
Sites
- Bilateral kidneys (no reported side predilection)
Pathophysiology
- Nonoverlapping mutations in MTOR, TSC2 or TSC1 are consistently observed in EVT; this results in mTORC1 pathway activation, which leads to cell growth, angiogenesis, increase in proteins, lipids and nucleotide production as well as suppression of catabolic pathways, such as autophagy
- Tumors with MTOR mutations consistently show loss of the wild type allele on chromosome 1 (locus where mTOR resides)
- 19p, 16p11 and 7q31 chromosomes losses have also been reported
- Reference: Cancers (Basel) 2023;15:4043
Etiology
- Sporadic with rare association with tuberous sclerosis (Mod Pathol 2022;35:344, Histopathology 2019;75:440, Hum Pathol 2021;116:1)
Clinical features
- Usually found incidentally on imaging (Amin: Diagnostic Pathology - Genitourinary, 3rd Edition, 2022)
Diagnosis
- Detected by imaging (commonly incidental), diagnosis is made by microscopic evaluation
Laboratory
- Unknown at this time
Radiology description
- Unknown at this time
Prognostic factors
- Indolent course (limited data) (Mod Pathol 2021;34:1167, Virchows Arch 2018;473:725)
Case reports
- 47 year old man underwent partial nephrectomy for a suspicious kidney mass (Cureus 2022;14:e24716)
- 52 year old woman with an incidental identification of left renal mass by abdominal imaging (BMC Urol 2024 September 11 [Preprint])
- 55 year old man with an incidental renal mass identified during workup of ischemic colitis (Adv Anat Pathol 2021;28:251)
Treatment
- Limited data
Gross description
- Solitary, well circumscribed, unencapsulated, solid tumor with gray, tan or mahogany brown cut surface
- Size range: 1.5 - 7 cm (mean: 4.3 cm)
- Tumors lack necrosis and macrocysts
- References: Mod Pathol 2022;35:344, Virchows Arch 2018;473:725, Cureus 2022;14:e24716, Adv Anat Pathol 2021;28:251, Mod Pathol 2021;34:1167
Gross images
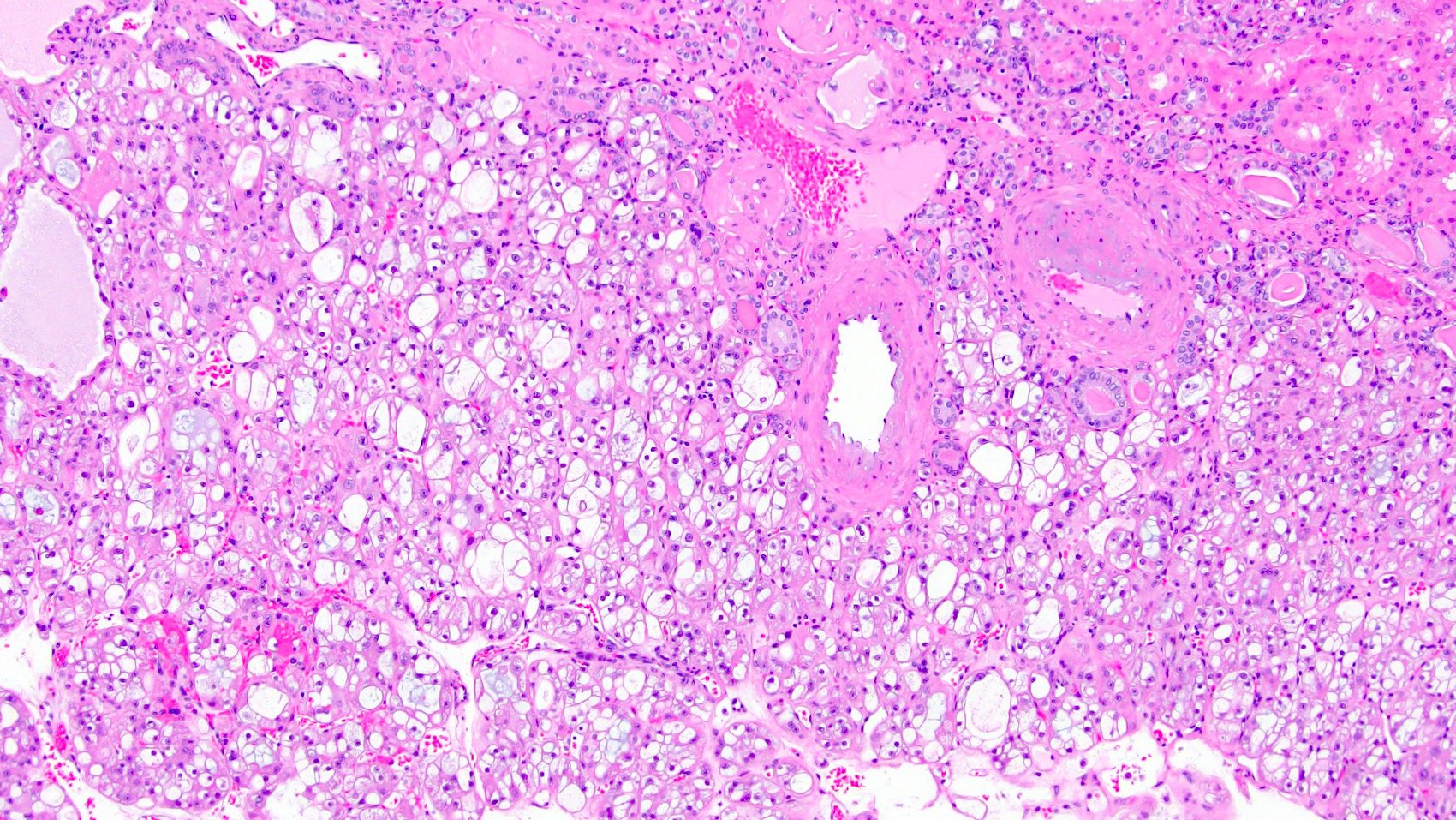
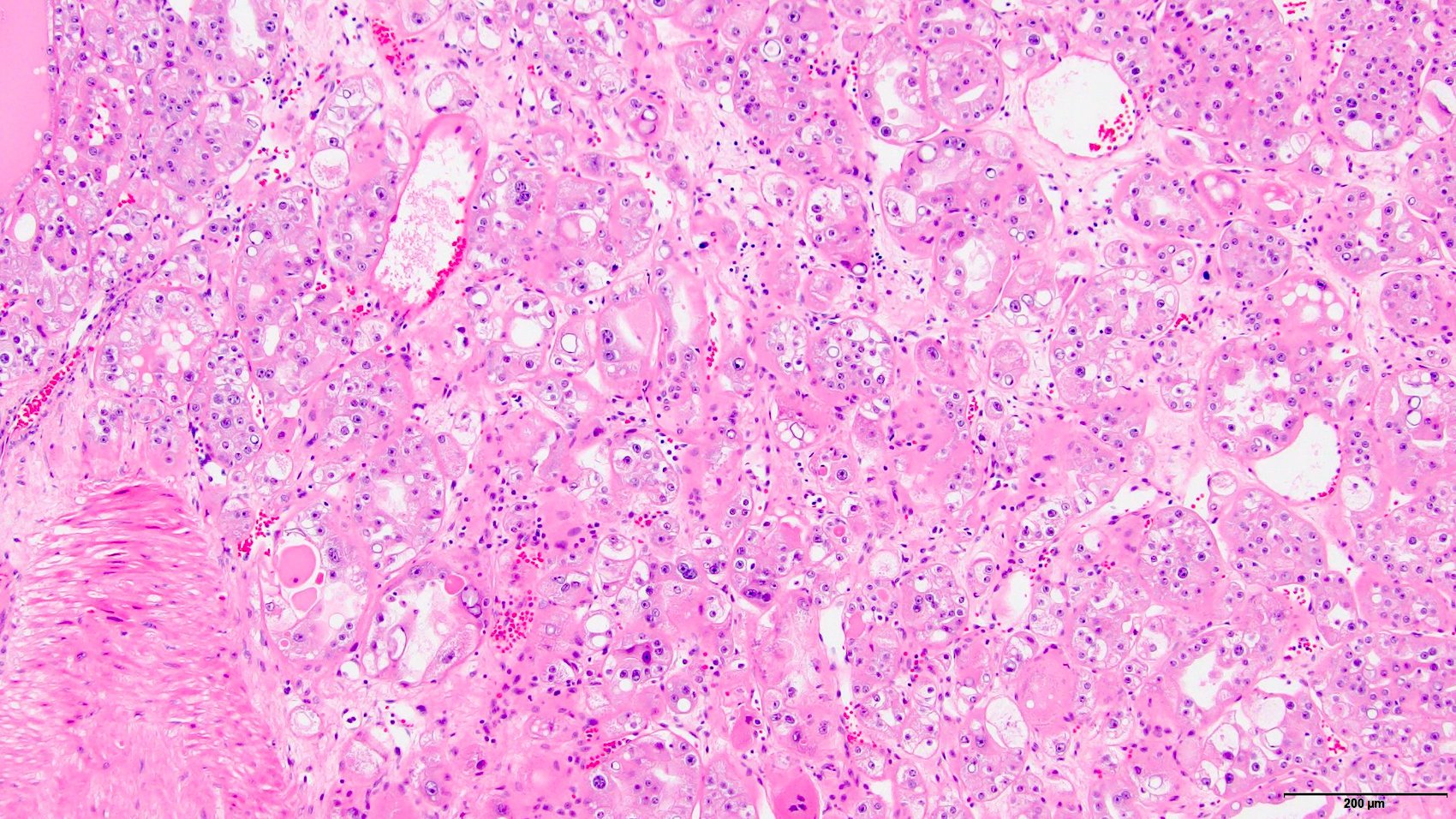
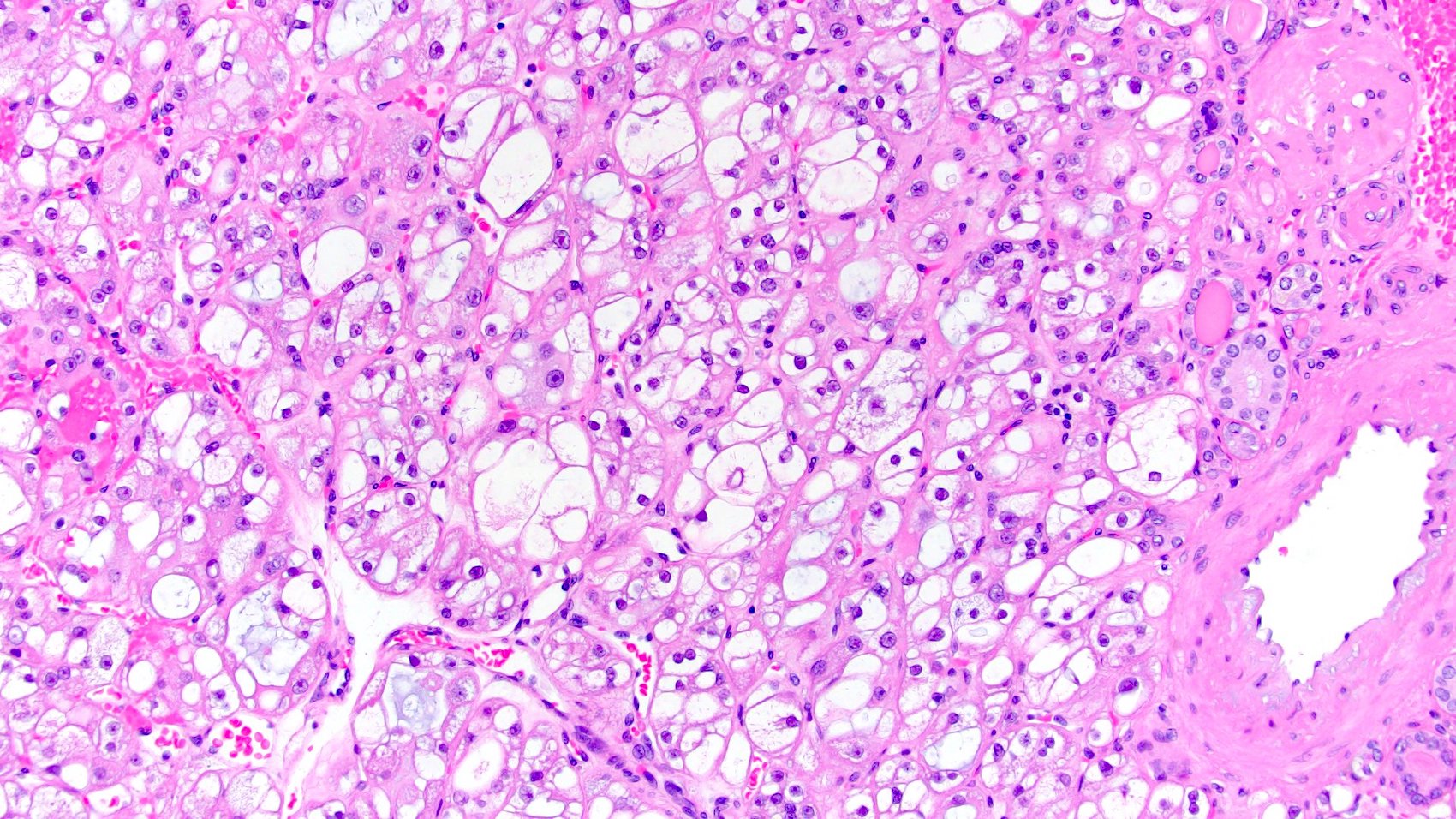
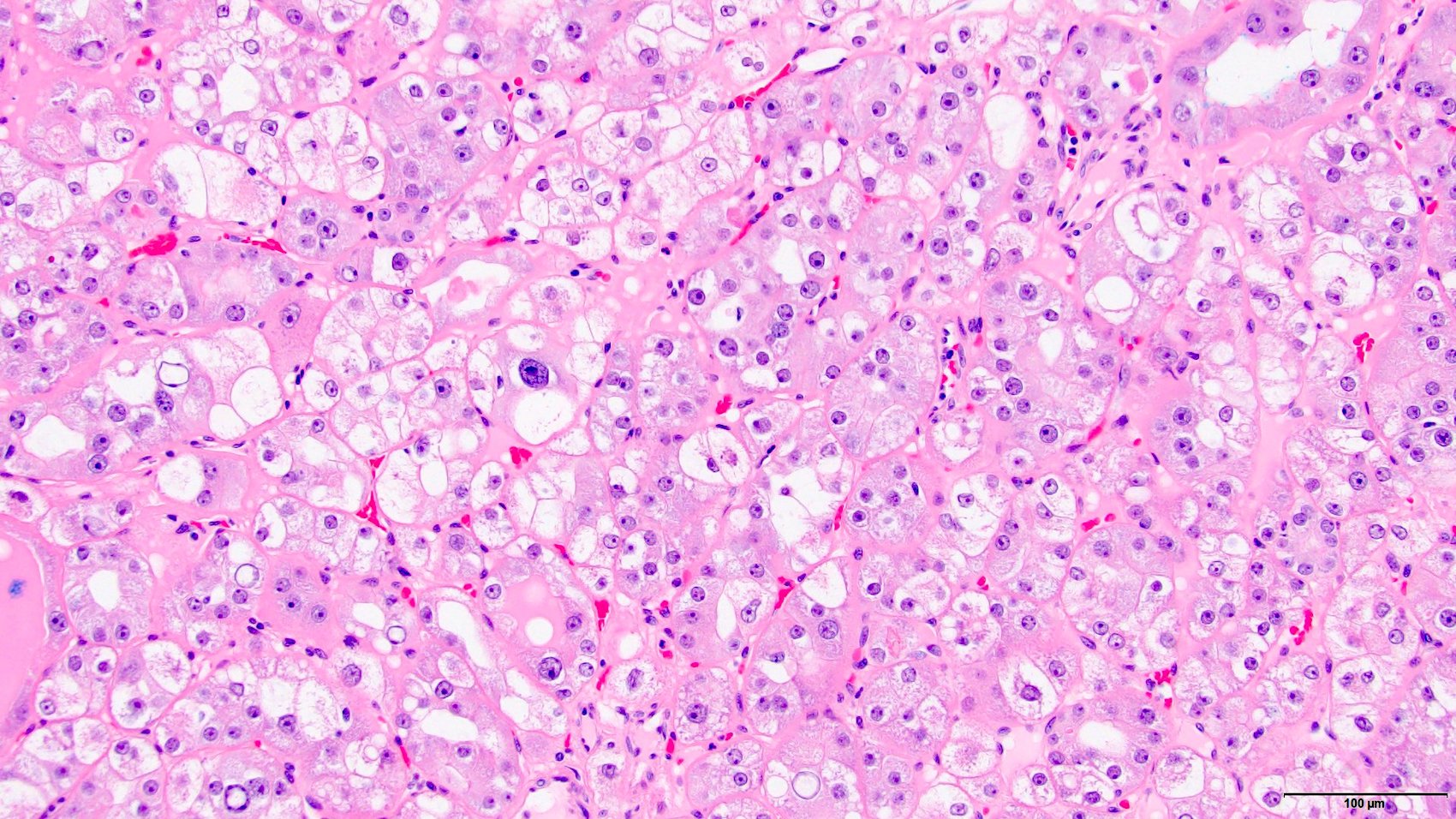
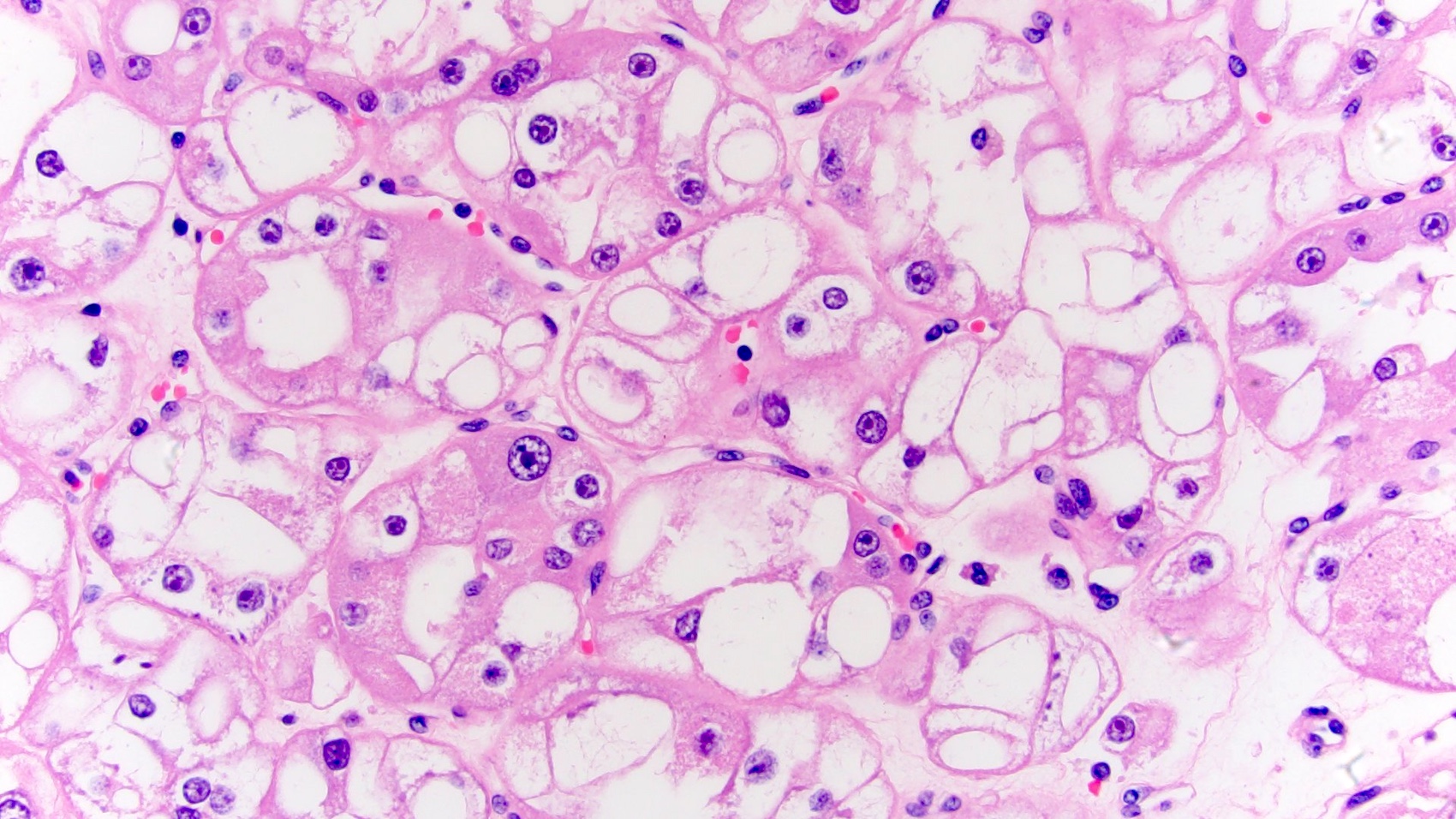
Microscopic (histologic) description
- Solid to nested growth pattern with focal tubulocystic areas
- Tumor cells possess
- Voluminous eosinophilic (oncocytic) cytoplasm, with frequent intracytoplasmic vacuoles, which often can be large
- Cytoplasm has variable granularity, typically condensed toward the cell periphery, giving prominent cell membrane appearance of chromophobe renal cell carcinoma (RCC)
- Large round to oval nuclei, often with enlarged nucleoli
- Perinuclear halos and nuclear irregularities are typically not found
- Voluminous eosinophilic (oncocytic) cytoplasm, with frequent intracytoplasmic vacuoles, which often can be large
- Normal renal tubules and thick walled vessels are frequently found at the periphery
- References: Mod Pathol 2022;35:344, Cureus 2022;14:e24716, Mod Pathol 2021;34:1167
Microscopic (histologic) images
Cytology description
- Unknown at this time
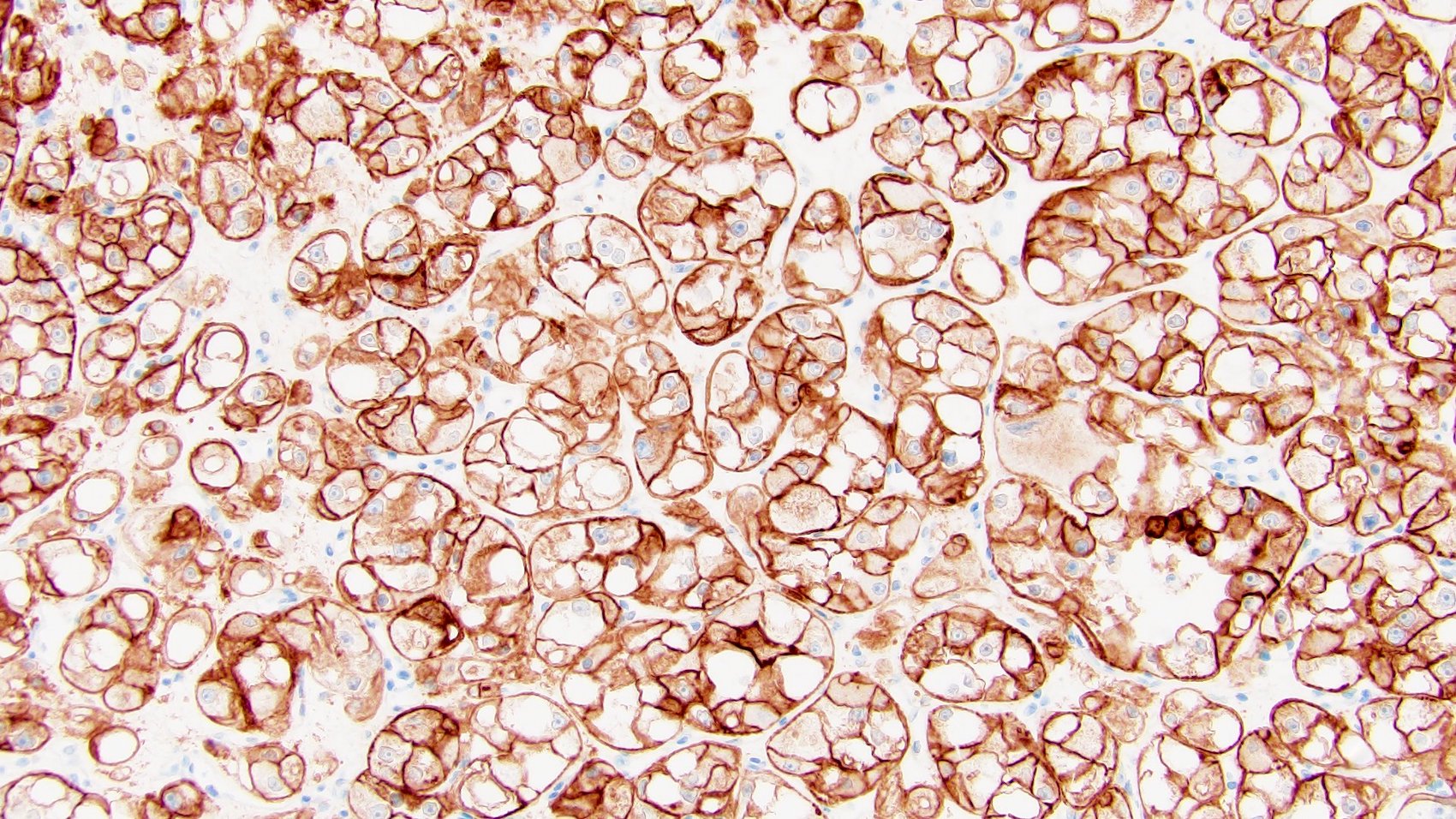
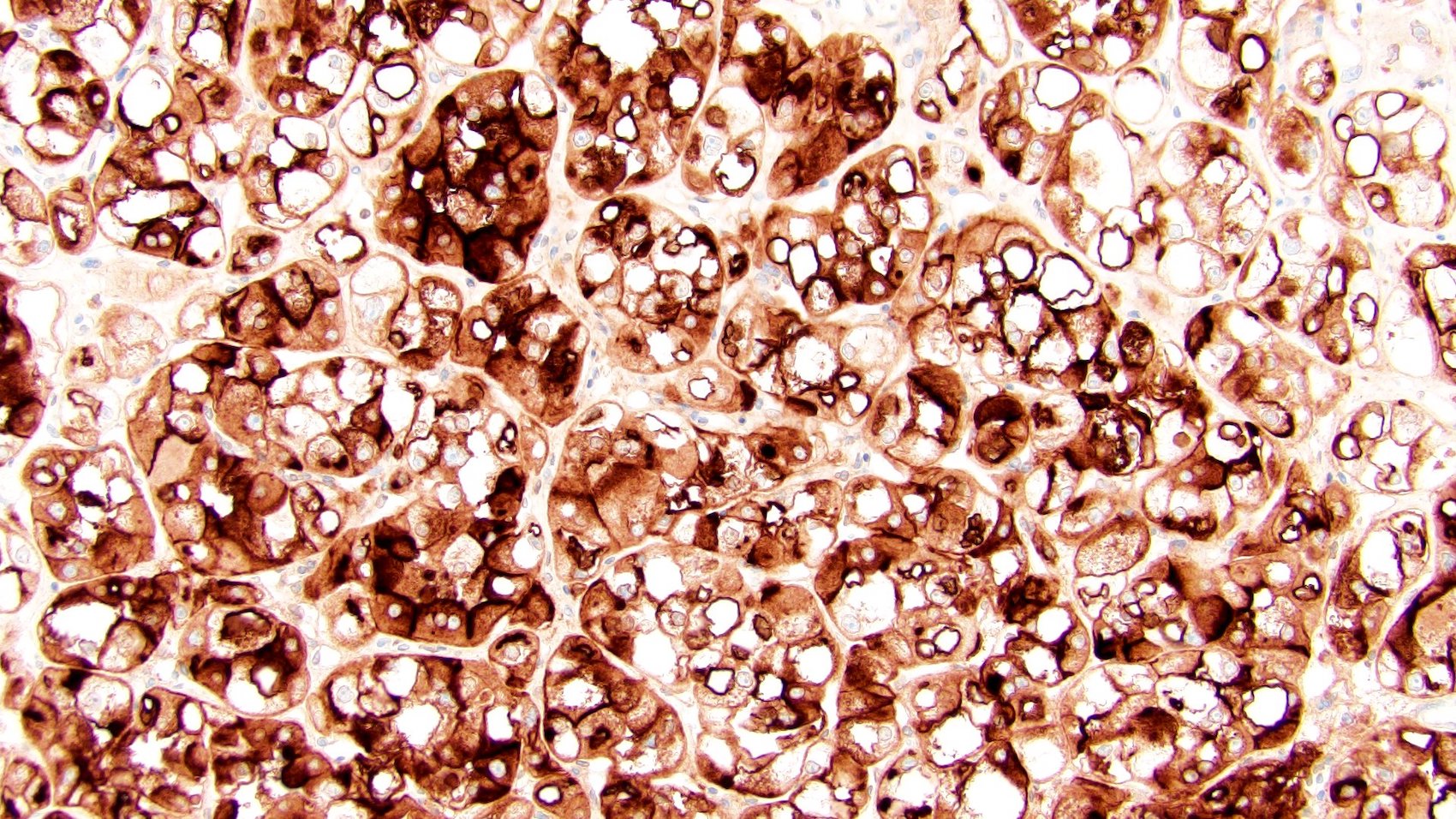
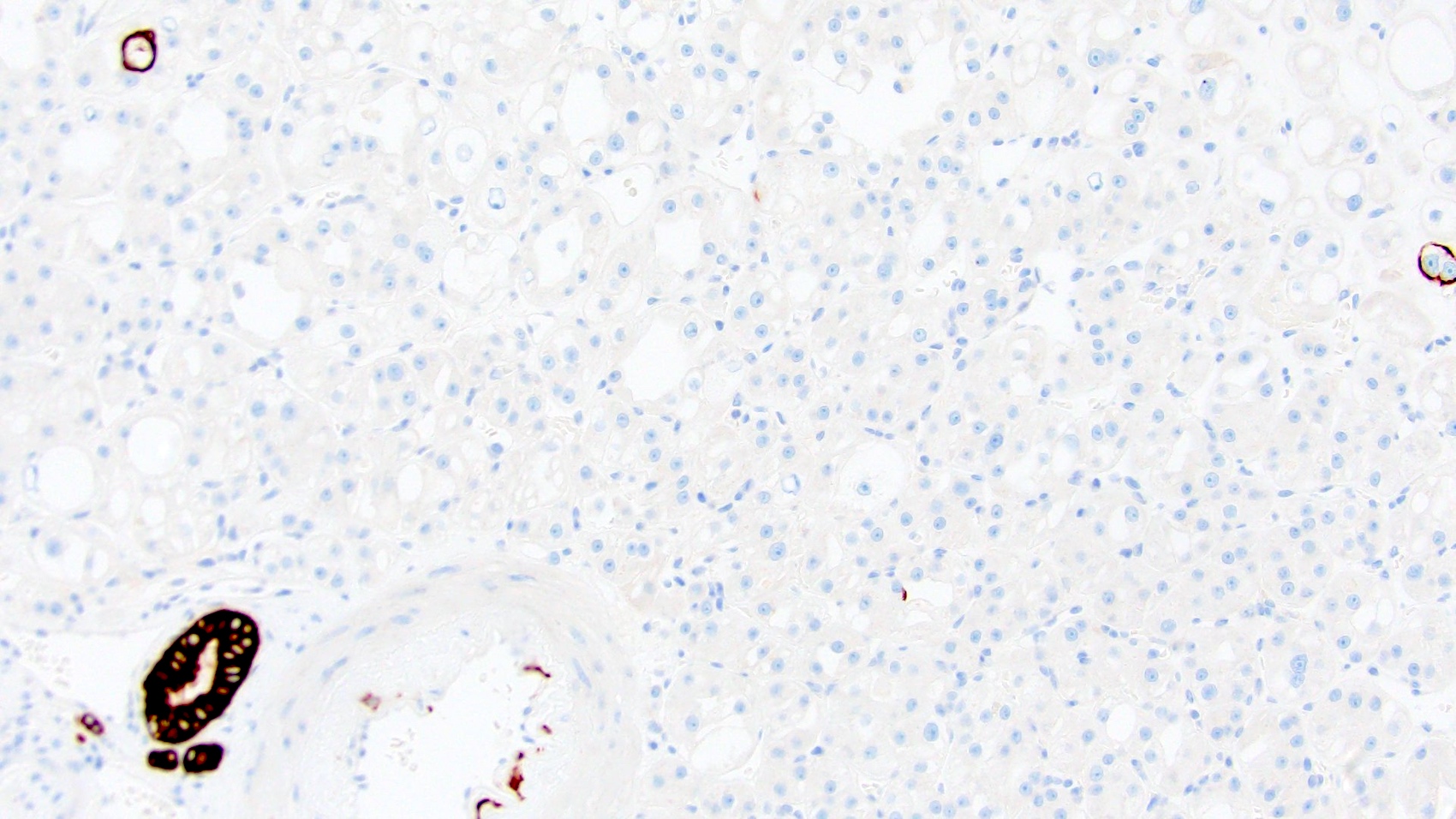
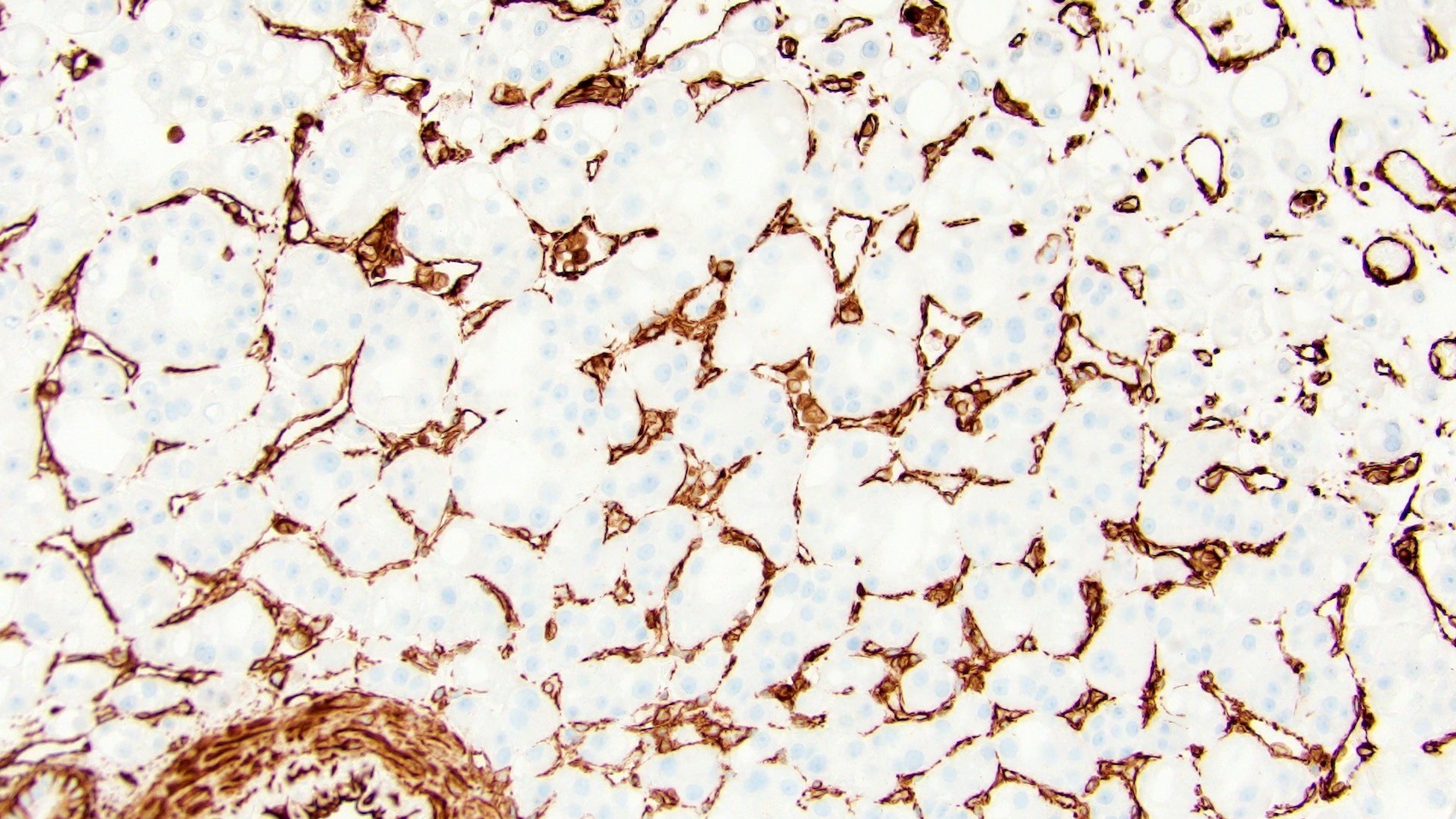
Positive stains
- PAX8, AE1 / AE3, CD10 and antimitochondrial antigens
- Cathepsin K and CD117 (both may be focal)
- SDHB and FH retained (positive)
- References: Mod Pathol 2021;34:1167, Mod Pathol 2022;35:344, Am J Surg Pathol 2022;46:1562
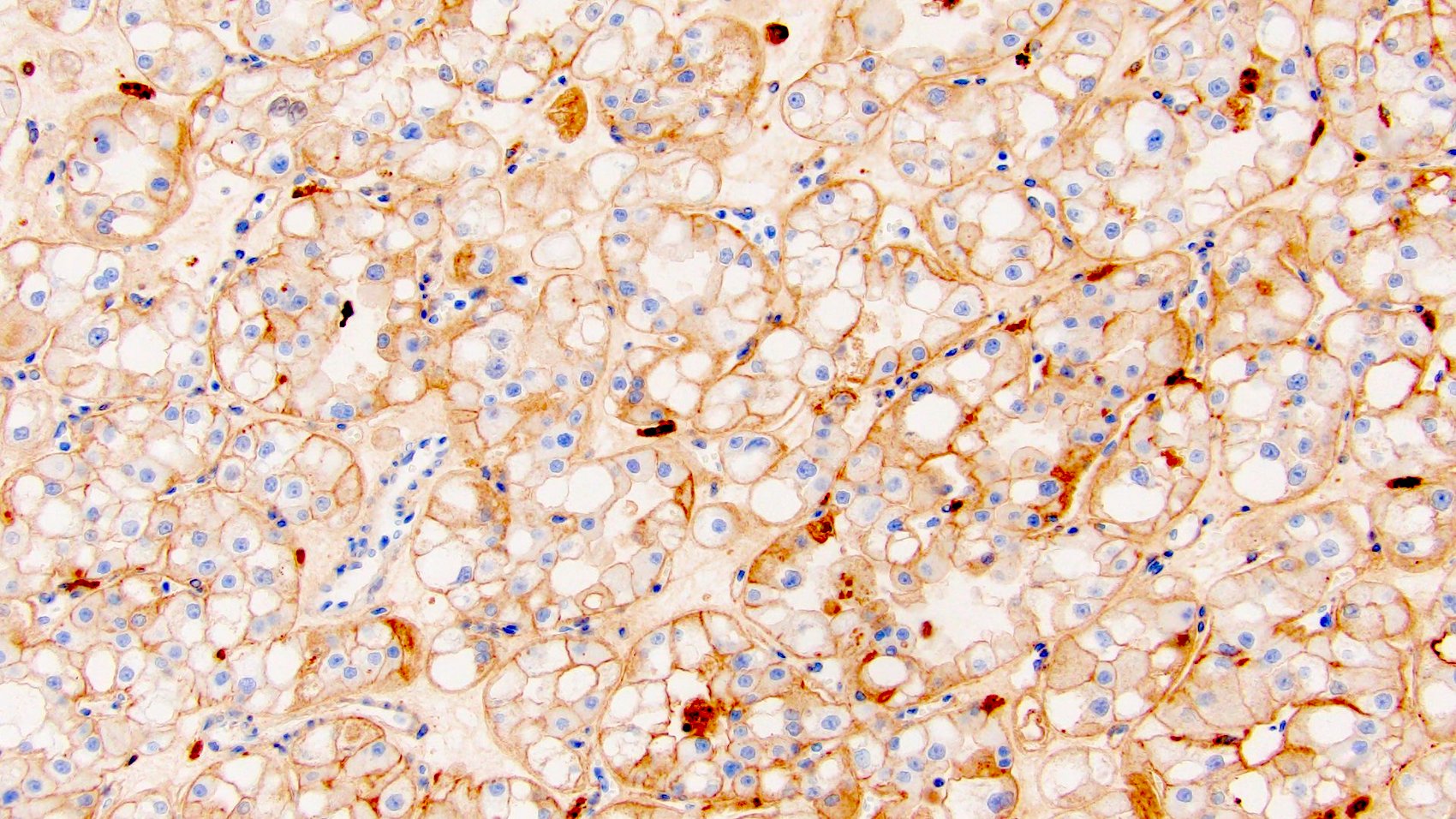
Negative stains
- Vimentin, HMB45, MelanA, CK20 and TFE3 (Mod Pathol 2021;34:1167)
- CK7 (may be focally positive) (Mod Pathol 2021;34:1167, Mod Pathol 2022;35:344)
Electron microscopy description
- Numerous intracytoplasmic mitochondria
- Dilated cisterns of rough endoplasmic reticulum (RER) corresponding to intracytoplasmic vacuoles (seen in light microscopy) (Adv Anat Pathol 2021;28:251)
Electron microscopy images
Molecular / cytogenetics description
- Nonoverlapping mutations in MTOR, TSC2 or TSC1, resulting in mTORC1 pathway activation
- Tumors with MTOR mutations demonstrate consistent loss of the wild type allele on chromosome 1 (where MTOR resides)
- Isolated losses of chromosomes 19p, 16p11 and 7q31 have also been reported
- References: Mod Pathol 2021;34:1167, Mod Pathol 2022;35:344, Cancers (Basel) 2023;15:4043, Am J Surg Pathol 2022;46:1562
Sample pathology report
- Right kidney, partial nephrectomy:
- Oncocytic renal neoplasm, with findings consistent with eosinophilic vacuolated tumor (see comment)
- Comment: The neoplastic cells possess abundant eosinophilic (oncocytic) cytoplasm, with numerous intracytoplasmic vacuoles and round to oval nuclei with prominent nucleoli. The cells express PAX8 (diffusely), CD117 (in a patchy manner) and CK7 (focally). They demonstrate retained immunoreactivity with SDHB and FH stains. No significant expression of CK20, HMB45, MelanA and TFE3 immunostains is observed. These findings are consistent with the recently described eosinophilic vacuolated tumor (EVT) of the kidney. This entity has been included under other oncocytic tumors of the kidney in the WHO Classification of Tumours, Urinary and Male Genital Tumours (5th edition).
Differential diagnosis
- Eosinophilic, solid and cystic RCC:
- Solid and cystic architecture
- Polygonal neoplastic cells possessing abundant eosinophilic cytoplasm, with cytoplasmic stippling; stippling may have leishmania-like appearance
- Hobnail cyst lining cells
- Admixed aggregates of lymphocytes and histiocytes
- PAX8, CK20 and cathepsin K positive
- CK7 and CD117 negative
- Chromophobe renal cell carcinoma, eosinophilic variant:
- Sheet-like architecture, neoplastic cells with densely eosinophilic and granular cytoplasm
- Admixture of pale and eosinophilic cells
- Nuclei are often irregular (raisinoid) with perinuclear halos
- CD117, CK7 and cathepsin K diffusely positive
- Vimentin and CD10 negative
- Low grade oncocytic tumor:
- Epithelioid angiomyolipoma:
- TFEB altered RCC:
- Young age
- Variable architecture with a biphasic pattern of large and small cells, frequent oncocytic and papillary features, with the presence of psammoma bodies
- Underexpression of epithelial markers (cytokeratins and EMA)
- Positive expression of PAX8, HMB45, MelanA and vimentin
- Nuclear immunoreactivity for TFEB protein is highly specific but technically challenging
- TFEB rearrangement / amplification by break apart fluorescent in situ hybridization (FISH); TFEB gene fusion by RNA sequencing is the preferred diagnostic test
- References: Adv Anat Pathol 2021;28:251, Mod Pathol 2021;34:1167
Additional references
Practice question #1
What are the characteristic histological features of eosinophilic vacuolated tumor of the kidney?
- Neoplastic cells with eosinophilic cytoplasm, prominent cell borders, and raisinoid nuclei
- Nests of eosinophilic (oncocytic) cells with large intracytoplasmic vacuoles and large nuclei, often with prominent nucleoli, imparting a high grade nuclear appearance
- Polygonal neoplastic cells possessing abundant eosinophilic cytoplasm, with cytoplasmic leishmania-like stippling
- Solid nests of eosinophilic cells with round nuclei and subtle perinuclear halos
Practice answer #1
B. Nests of eosinophilic (oncocytic) cells with large intracytoplasmic vacuoles and large nuclei, often with prominent nucleoli (high grade nuclear appearance) are typically seen in EVT.
Answer D is incorrect because these are the features of low grade oncocytic tumor (LOT).
Answer A is incorrect because these microscopic features are seen in chromophobe renal cell carcinoma.
Answer C is incorrect because this is the typical picture of eosinophilic solid and cystic RCC.
Comment Here
Reference: Eosinophilic vacuolated tumor (EVT)
Comment Here
Reference: Eosinophilic vacuolated tumor (EVT)
Practice question #2
Which of the following immunostaining profiles is characteristic of eosinophilic vacuolated tumor?
- CD117+ / CK7+ / cathepsin K+ / vimentin- / CD10-
- PAX8+ / CD117+ / vimentin- / CK20-
- PAX8+ / CD117- / vimentin+ / CK20+
- PAX8+ / HMB45+ / MelanA+ / EMA-
Practice answer #2
B. PAX8+ / CD117+ / vimentin- / CK20- is the immunoprofile of eosinophilic vacuolated tumor.
Answer C is incorrect because this immunoprofile is seen in eosinophilic solid and cystic RCC.
Answer D is incorrect because this immunoprofile is seen in TFEB altered RCC.
Answer A is incorrect because this immunoprofile is seen in chromophobe renal cell carcinoma.
Comment Here
Reference: Eosinophilic vacuolated tumor (EVT)
Comment Here
Reference: Eosinophilic vacuolated tumor (EVT)
Practice question #3
A 43 year old woman presents with a 2.3 cm left renal mass that was identified incidentally during imaging. The neoplasm highlights with PAX8 and CD117 and is negative for HMB45, TFE stains, CK7 and CK20. What is your diagnosis?
- Chromophobe renal cell carcinoma
- Eosinophilic vacuolated tumor
- Low grade oncocytic tumor
- Oncocytoma
Practice answer #3
B. Eosinophilic vacuolated tumor. The image of an oncocytic neoplasm possessing cells with voluminous eosinophilic cytoplasm with intracytoplasmic vacuoles and round to oval nuclei is classical for eosinophilic vacuolated tumor, along with characteristic immunohistochemistry of positive PAX8 and CD117, as well as negative CK7.
Answer D is incorrect because oncocytoma is composed of oncocytic cells possessing densely granular eosinophilic cytoplasm and round uniform nuclei. Like eosinophilic vacuolated tumors, it also expresses CD117 with negative to focal CK7 but it lacks the prominent cytoplasmic vacuolization as seen in eosinophilic vacuolated tumors.
Answer A is incorrect because chromophobe renal cell carcinoma has pale cells possessing reticulated cytoplasm with prominent cell membranes (plant cell-like morphology) and hyperchromatic raisinoid nuclei. This neoplasm highlights with CD117 and CK7 diffusely.
Answer C is incorrect because low grade oncocytic tumor has oncocytic cells with bland, low grade nuclei. The neoplasm is diffusely positive for CK7 and negative for CD117.
Comment Here
Reference: Eosinophilic vacuolated tumor (EVT)
Comment Here
Reference: Eosinophilic vacuolated tumor (EVT)