Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Prognostic factors | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Busca A, Parra-Herran C. Cortical inclusion cyst. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarynontumorinclusioncyst.html. Accessed September 9th, 2025.
Definition / general
- Cystically dilated glands within the ovarian cortex that result from the invagination of the surface lining or implantation of tubal epithelium
Essential features
- 2 types based on morphology and pathophysiology:
- Peritoneal inclusion cyst: lined by flat epithelium that is invaginated from ovarian surface epithelium; these express a peritoneal phenotype (calretinin, WT1 and D2-40 positive, PAX8 and BerEP4 negative)
- Müllerian inclusion cyst: lined by ciliated tubal epithelium as a result of the implantation of tubal epithelium in the ovarian parenchyma, presumably at the time of ovulation when the ovarian surface epithelium is disrupted; these cysts express a tubal Müllerian phenotype (PAX8, BerEP4 and WT1 positive, calretinin and D2-40 negative)
- Size is less than 1 cm; if more than 1 cm, by convention the lesion is designated as cystadenoma or cystadenofibroma
Terminology
- Cortical inclusion cyst
- Some terminology overlap with endosalpingiosis
Epidemiology
- Can occur at any age but more common postmenopausal
Sites
- Ovary
Pathophysiology
- Via invagination of the ovarian surface epithelium (peritoneal type cyst) or implantation of tubal epithelium at ovulation, when the ovarian surface epithelium is disrupted (Müllerian type cyst) (Histopathology 2018;72:766, Int J Gynecol Pathol 2015;34:3, Mod Pathol 2011;24:1488)
Clinical features
- Incidental findings, usually asymptomatic
Diagnosis
- Histologic examination, usually incidental findings in oophorectomy specimens
Prognostic factors
- Benign entities
- Presence of inclusion cyst in postmenopausal women does not increase the risk of ovarian or other hormone driven cancers (breast and endometrial cancers) (BJOG 2012;119:207)
- Traditionally thought to represent a precursor lesion of ovarian carcinoma; however most ovarian serous carcinomas are now considered to be tubal in origin with serous tubal intraepithelial carcinoma (STIC) as the precursor lesion
- For a subset of ovarian serous carcinomas (in which STIC or tubal involvement is not identified), a potential origin in epithelial inclusion cyst of Müllerian (tubal) phenotype has been postulated (Gynecol Oncol 2013;130:246, Mod Pathol 2011;24:1488, Int J Gynecol Pathol 2015;34:3)
- Use of oral contraceptives for more than 5 years was shown to reduce the number of Müllerian type inclusion cysts (PAX8 positive); this suggests a possible mechanism for reducing the risk of epithelial neoplasms and supports the hypothesis that these cysts constitute a precursor lesion of ovarian serous carcinoma (Diagn Pathol 2016;11:30)
Treatment
- Not required, as these are often incidental findings
Gross description
- Most are not apparent grossly unless very superficial in the cortex
- When visible, they appear as small cysts bulging at the ovarian surface
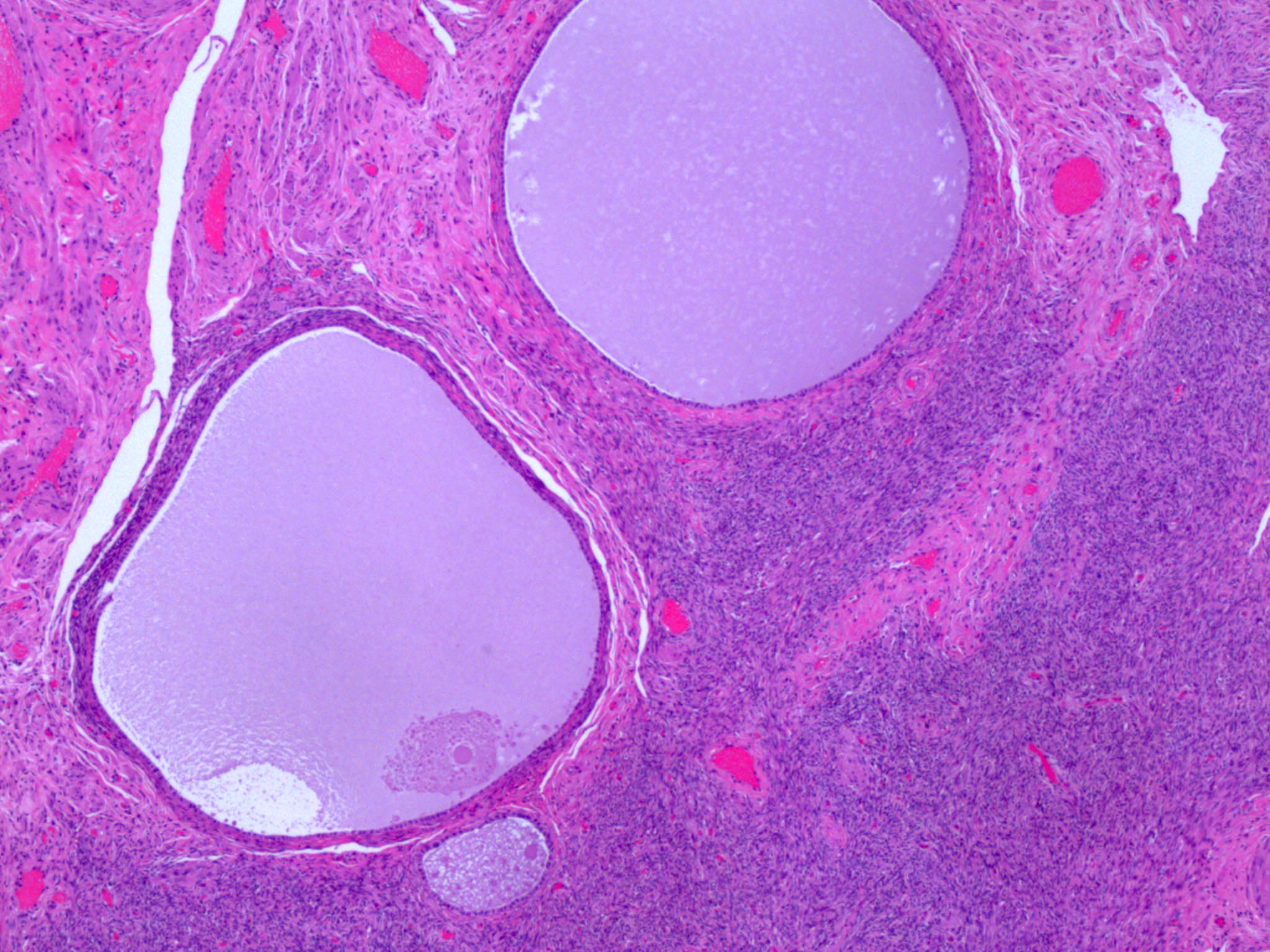
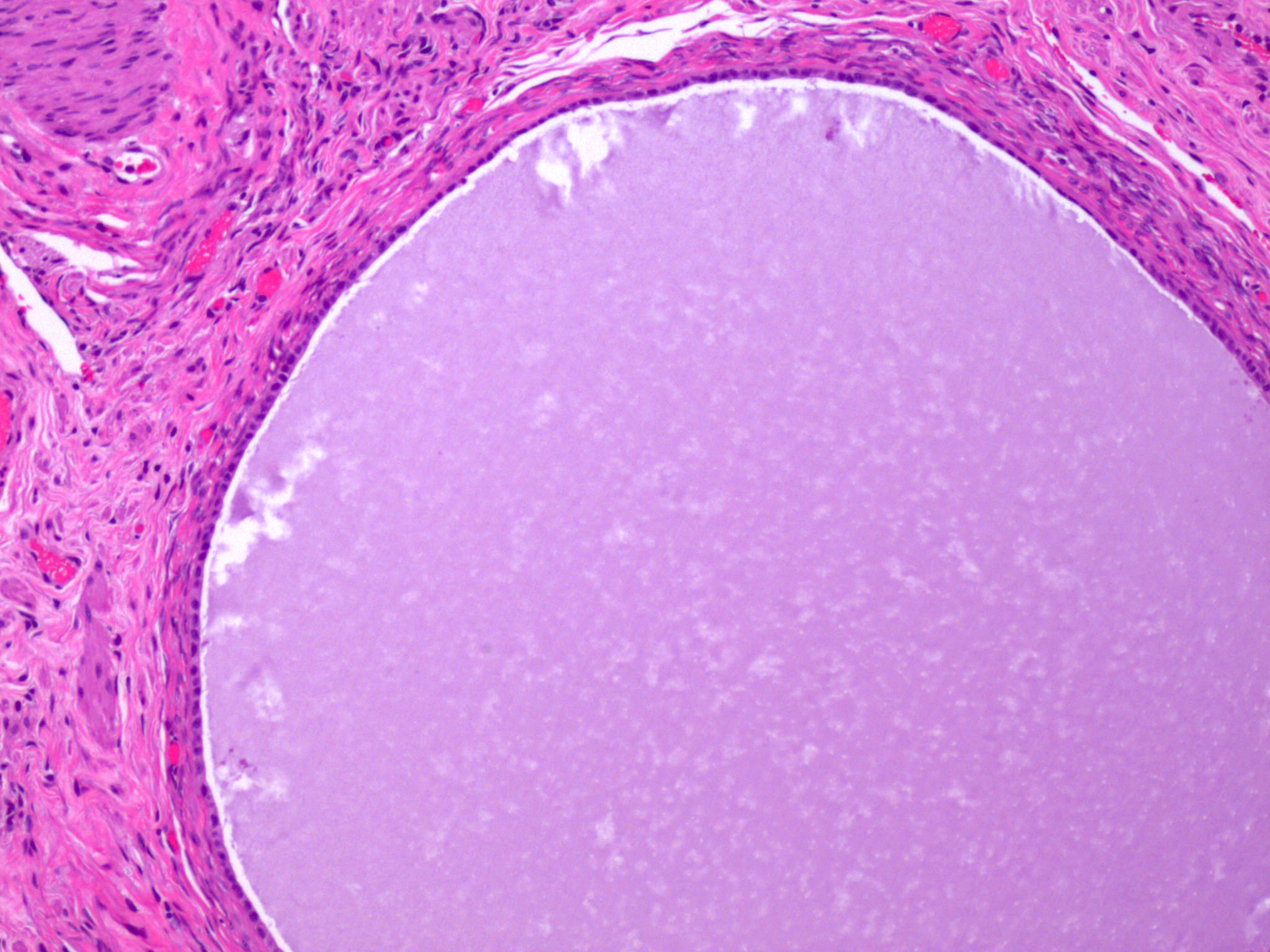
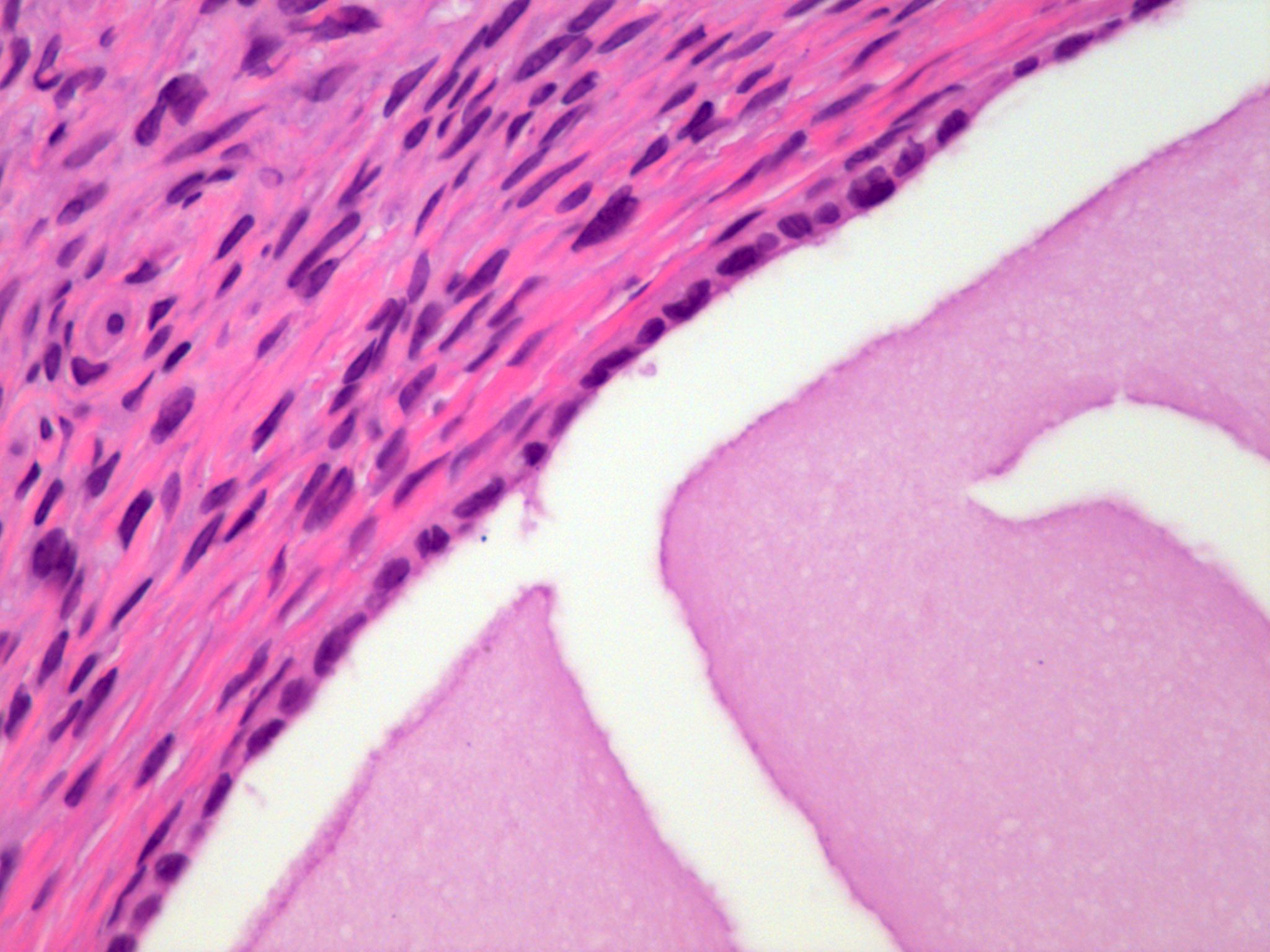
Microscopic (histologic) description
- Small cysts (< 1 cm), singly or in clusters within the ovarian cortex
- Peritoneal inclusion cyst: lined by simple flat epithelium devoid of cilia or mucinous cytoplasm
- Müllerian inclusion cyst: lined by simple cuboidal to columnar epithelium with ciliated cells, sometimes admixed with nonciliated (secretory, peg) cells
- Can have psammomatous calcifications in adjacent stroma
- Reference: Int J Gynecol Pathol 2015;34:3
Positive stains
- Müllerian type cyst: PAX8, BerEP4 and WT1 (Histopathology 2018;72:766, Hum Pathol 2015;46:948, Int J Gynecol Pathol 2000;19:158)
- Peritoneal type cyst: calretinin, WT1 and D2-40 (Int J Gynecol Pathol 2015;34:3)
Negative stains
- Müllerian type cyst: calretinin and D2-40 (Histopathology 2018;72:766, Hum Pathol 2015;46:948, Int J Gynecol Pathol 2000;19:158)
- Peritoneal type cyst: PAX8 and BerEP4 (Int J Gynecol Pathol 2015;34:3)
Sample pathology report
- Left and right ovary, bilateral oophorectomy:
- Benign ovaries with cortical inclusion cysts
- Note: many pathologists do not report the finding of inclusion cysts since they are common and benign
Differential diagnosis
- Endometriosis:
- Presence of endometrial stroma or hemosiderin laden macrophages
- Serous cystadenoma:
- Size: > 1 cm
Practice question #1
Practice answer #1
D. Usually is an incidental finding. Epithelial inclusion cysts are incidental findings and can be PAX8 positive (Müllerian type) or negative (peritoneal type). Presence of endometrial stroma distinguishes them from endometriosis, as both can have focal tubal differentiation. Although some relationship with risk of serous neoplasia, they are considered benign findings (not a serous tubal intraepithelial carcinoma [STIC] lesion).
Comment Here
Reference: Epithelial inclusion cyst
Comment Here
Reference: Epithelial inclusion cyst
Practice question #2
What is the typical immunoprofile of Müllerian type epithelial inclusion cyst of the ovary?
- BerEP4 and D2-40 positive
- BerEP4 and PAX8 positive
- Calretinin and PAX8 positive
- Calretinin and WT1 positive
Practice answer #2