Table of Contents
Definition / general | Terminology | Epidemiology | Pathophysiology | Clinical features | Laboratory | Radiology description | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosisCite this page: Parra-Herran C. Appendiceal neoplasms. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorappendiceal.html. Accessed April 26th, 2024.
Definition / general
- Mucinous neoplastic proliferations of the cecal appendix commonly manifest with signs of extra-appendiceal spread, particularly in the form of pseudomyxoma peritonei
- Involvement of other organs such as the ovary may be the first manifestation of the disease
- Current evidence supports that, in the context of pseudomyxoma peritonei, an ovarian mucinous tumor should be regarded as appendiceal in origin, with the exception of a mucinous tumor arising in a mature teratoma (Am J Surg Pathol 1991;15:415, Int J Gynecol Pathol 1997;16:1)
Terminology
- Pseudomyxoma peritonei is a clinicopathologic syndrome characterized by mucinous ascites
- Intra-abdominal mucin is abundant and can be admixed with neoplastic mucinous epithelium (Am Soc Clin Oncol Educ Book 2013;221)
- Although commonly used to refer to all metastatic carcinomas involving the ovary, the term Krukenberg tumor strictly refers to adenocarcinomas with signet-ring cell differentiation, of which most (76%) arise from the stomach (J Clin Pathol 2012;65:585)
Epidemiology
- Primary appendiceal tumors are found in < 2% of surgically removed appendices (Arch Pathol Lab Med 2011;135:1261)
- 28 - 37% of appendiceal tumors not associated with pseudomyxoma peritoneii present with ovarian metastases (Gynecol Oncol 2014;133:155)
- Among patients with ovarian mucinous tumors showing borderline features, only about 2% have a documented primary appendiceal malignancy
- Despite this low incidence, there is significant overlap of clinical, radiologic and pathologic features between primary and metastatic ovarian adenocarcinoma; in the work-up of a mucinous or endometrioid-like ovarian neoplasm, a secondary malignancy should always be considered pathologically or clinically
- Pseudomyxoma peritonei is 2 - 3 times more common in women than in men
Pathophysiology
- Spread to the ovaries can be hematogenous, lymphatic, transperitoneal or by direct extension (Rev Gastroenterol Mex 1994;59:290)
- The pathogenesis of pseudomyxoma peritonei is still unknown; current theories postulate that the mucin is produced by very low quantities (sometimes undetectable) of neoplastic intestinal-type epithelium, which colonizes the peritoneal cavity presumably after appendiceal tumor rupture
Clinical features
- Patients with metastatic appendiceal adenocarcinoma involving the ovary have a poor prognosis
- Patients with a low grade appendiceal mucinous neoplasm (LAMN) and pseudomyxoma peritonei has a protracted clinical course with multiple recurrences, progressive fibrous adhesions and complications such as fatal obstructive disease
Laboratory
- Elevated CA-125 levels (> 100 U/mL) are common, which has been suggested as a useful feature to distinguish metastatic from primary ovarian mucinous carcinomas (Gynecol Obstet Invest 2011;72:196)
- Elevated CEA levels (> 5 ng/mL) and CA19-9 levels (> 37 U/mL) are seen in a minority of cases
Radiology description
- Bilaterality is seen in up to 83.3% of cases
- On imaging, pseudomyxoma peritonei is suspected if there is irregularly localized or loculated fluid with scalloped appearance within the peritoneal cavity
- The ovarian mass can be cystic, solid or a mixture
Gross description
- Ovarian mass is frequently complex (solid and cystic) or purely solid
- Purely cystic unilocular lesions are rare
- Solid tumors have a multinodular appearance and extend to the ovarian / tumor surface
- Cut surface reveals mucinous contents in cystic areas and a soft, glistening appearance of solid areas, sometimes with easily expressed mucinous material from it
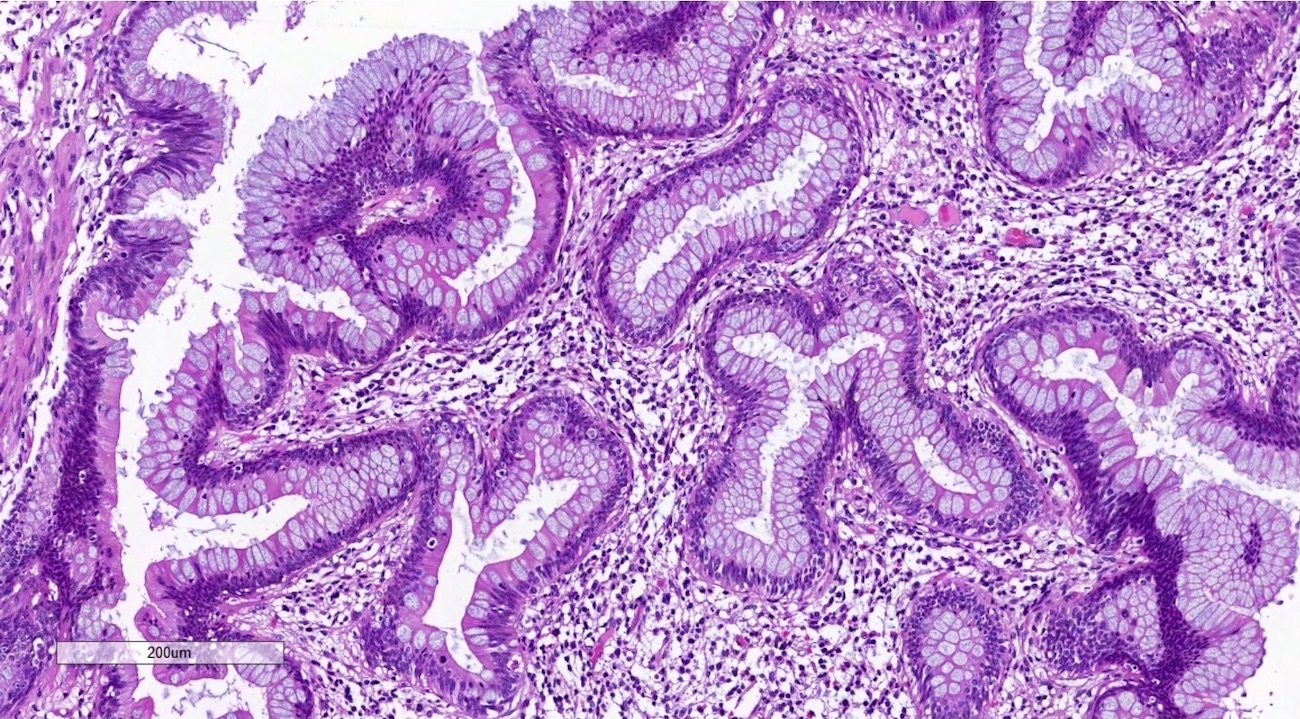
Microscopic (histologic) description
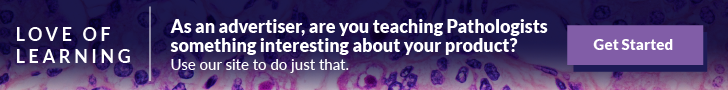
- Low grade appendiceal mucinous neoplasms (LAMN) have bland cytomorphology and mimic benign and borderline ovarian mucinous tumors
- LAMN involving the ovary display certain distinctive microscopic features (Int J Gynecol Pathol 2014;33:1):
- Bilaterality
- Tall mucinous cells with indistinct apical borders and lack of cellular stratification
- Elongated glands with shallow epithelial invaginations (scalloping)
- Subepithelial clefts
- These characteristics, however, can also be seen in up to 38.8% of ovarian mucinous borderline tumors
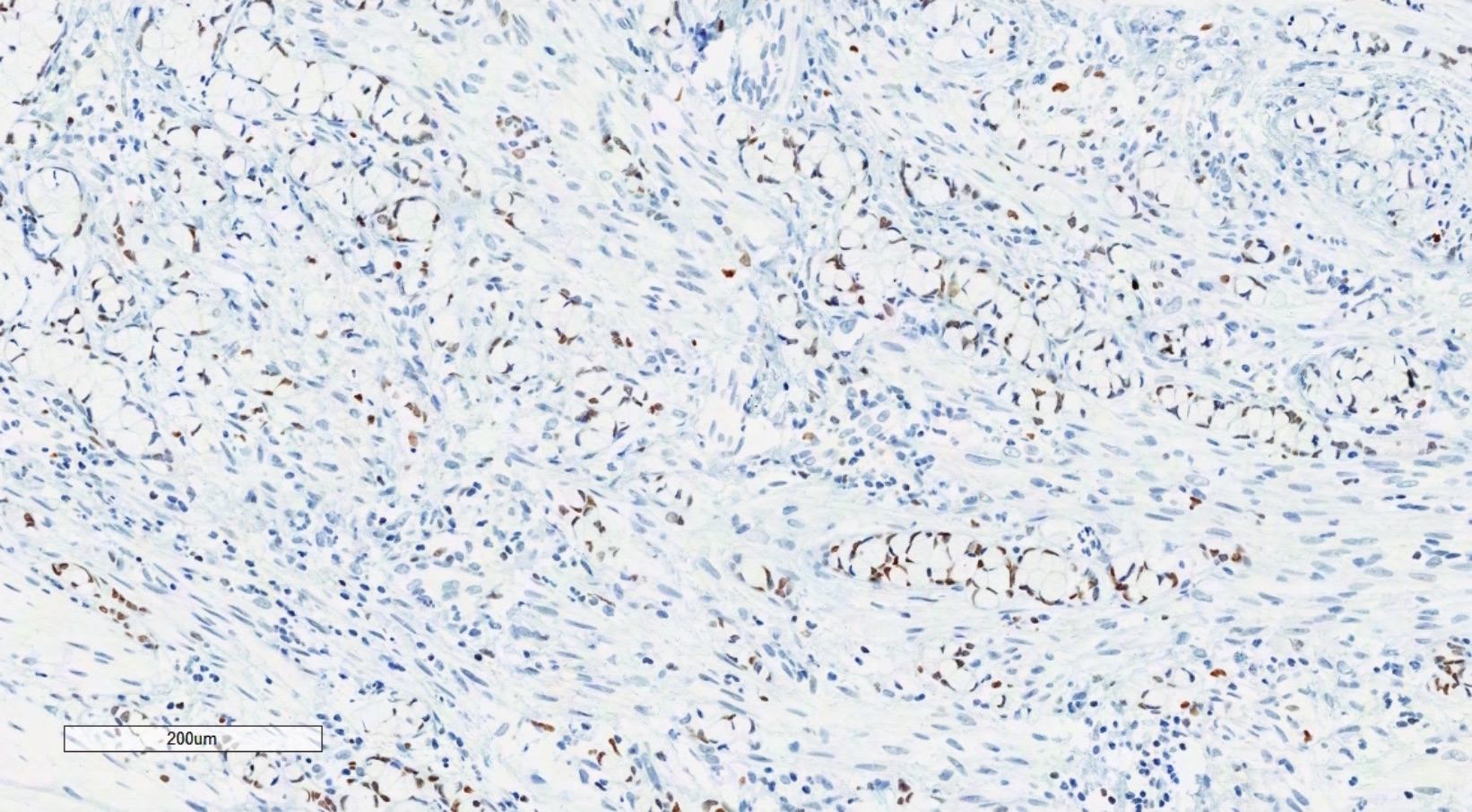
- Appendiceal adenocarcinomas can have a mucinous or a conventional (mucin-depleted) glandular appearance
- Mucinous carcinomas have intestinal (goblet cell) differentiation
- Mucin extravasation and signet-ring cell morphology can be seen
- The term Krukenberg tumor should be reserved to adenocarcinomas involving the ovary with a signet ring cell component > 10% of the tumor volume, regardless of its site of origin (Adv Anat Pathol 2006;13:205)
- Conventional tumor cytomorphology with mucin depletion mimics the architecture and cytoplasmic appearance of primary endometrioid tumors; however, nuclear pleomorphism and hyperchromasia tend to be prominent, and exceed that expected for a primary ovarian tumor
- Central glandular necrosis is also more typical of intestinal tumors, although is not entirely specific
- Several clinical and pathologic features have been described as indicative of secondary (metastatic) origin (Am J Surg Pathol 2003;27:281, J Clin Pathol 2012;65:591), including:
- Bilaterality
- Size less than 10 cm
- Surface involvement
- Infiltrative pattern of invasion
- Presence of signet ring cells
- Extensive lymphovascular space invasion
- Mucin extravasation
- If any of the above features is present, the possibility of a metastasis should be considered and prompt ancillary testing and clinical investigation
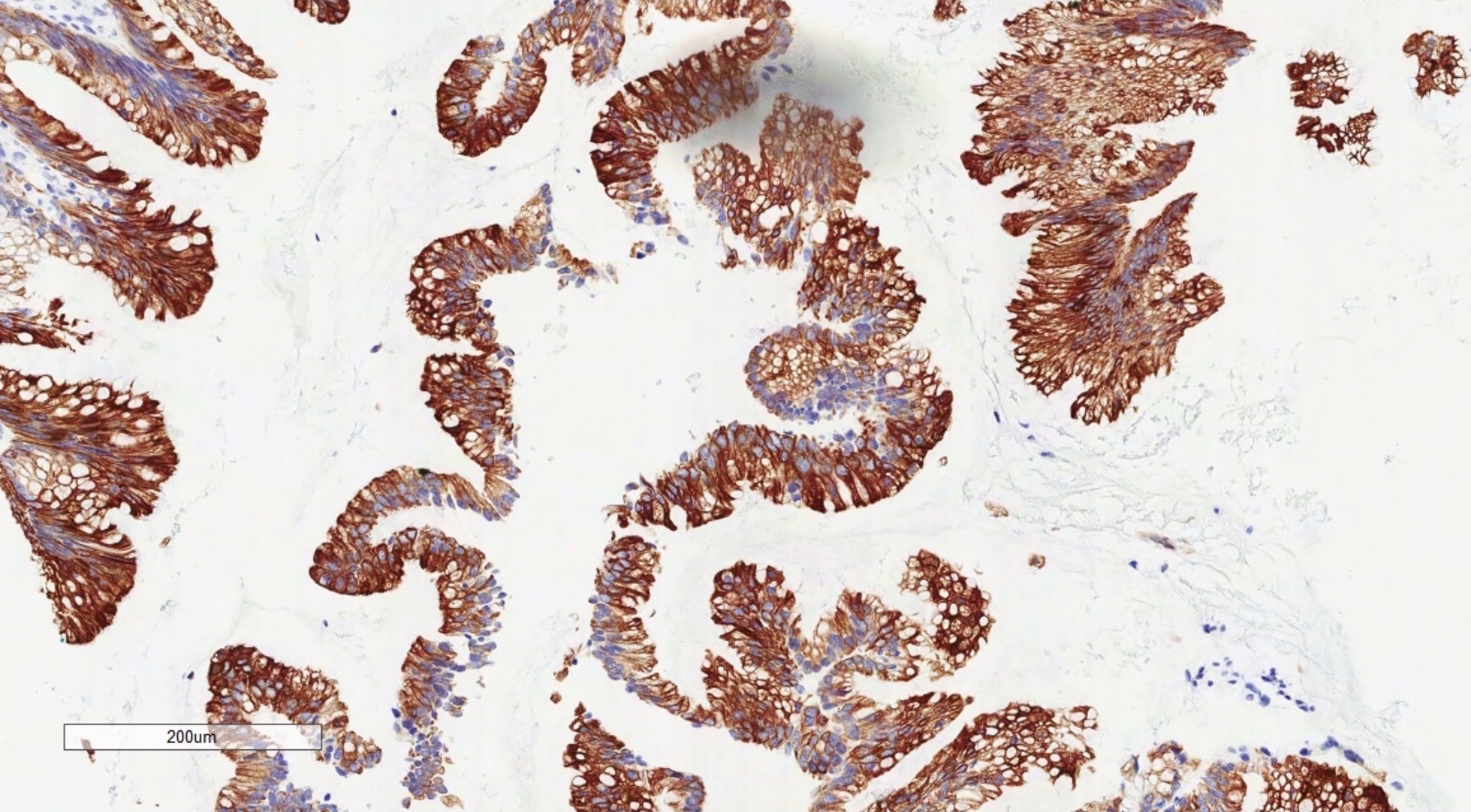
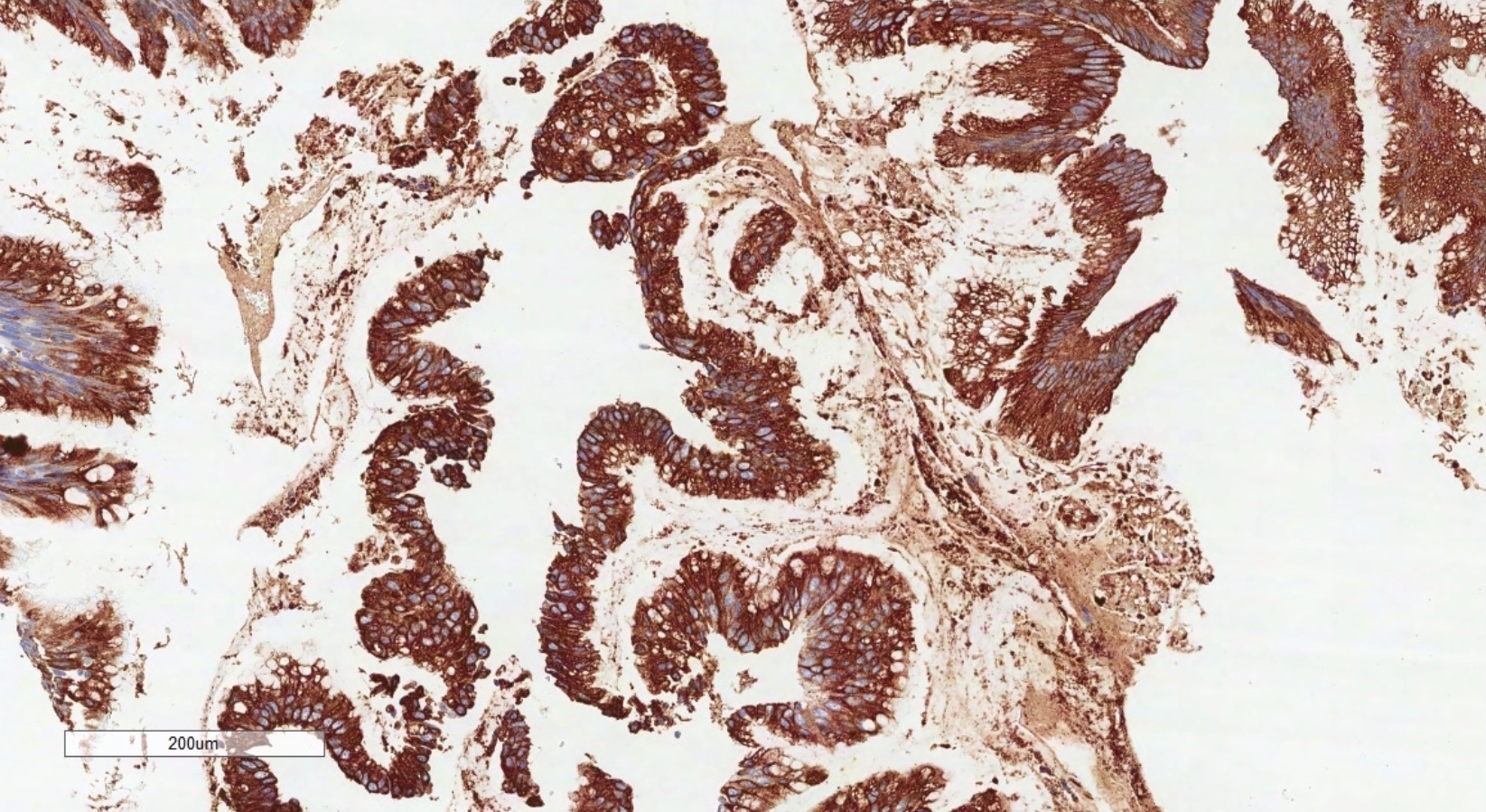
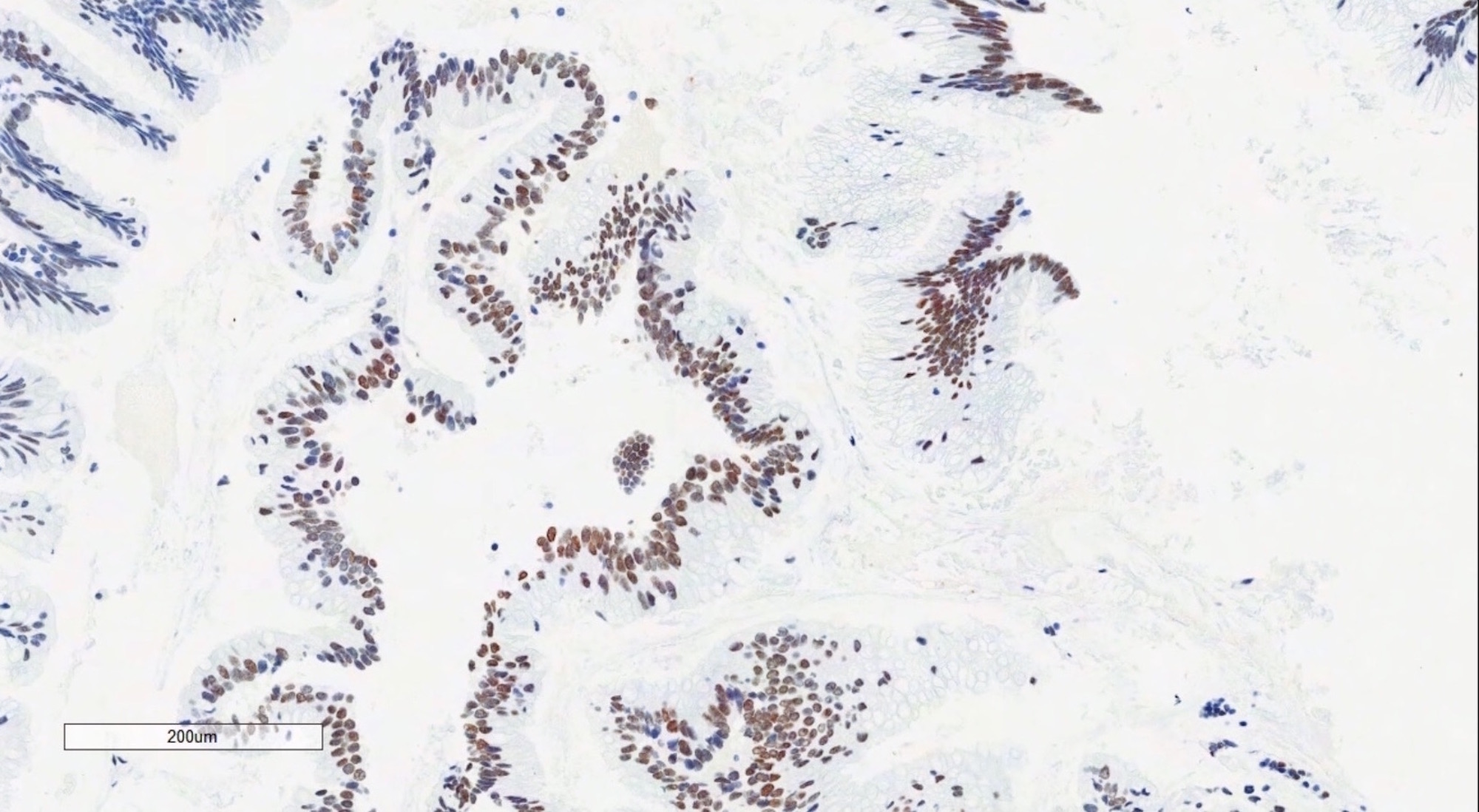
Microscopic (histologic) images
Positive stains
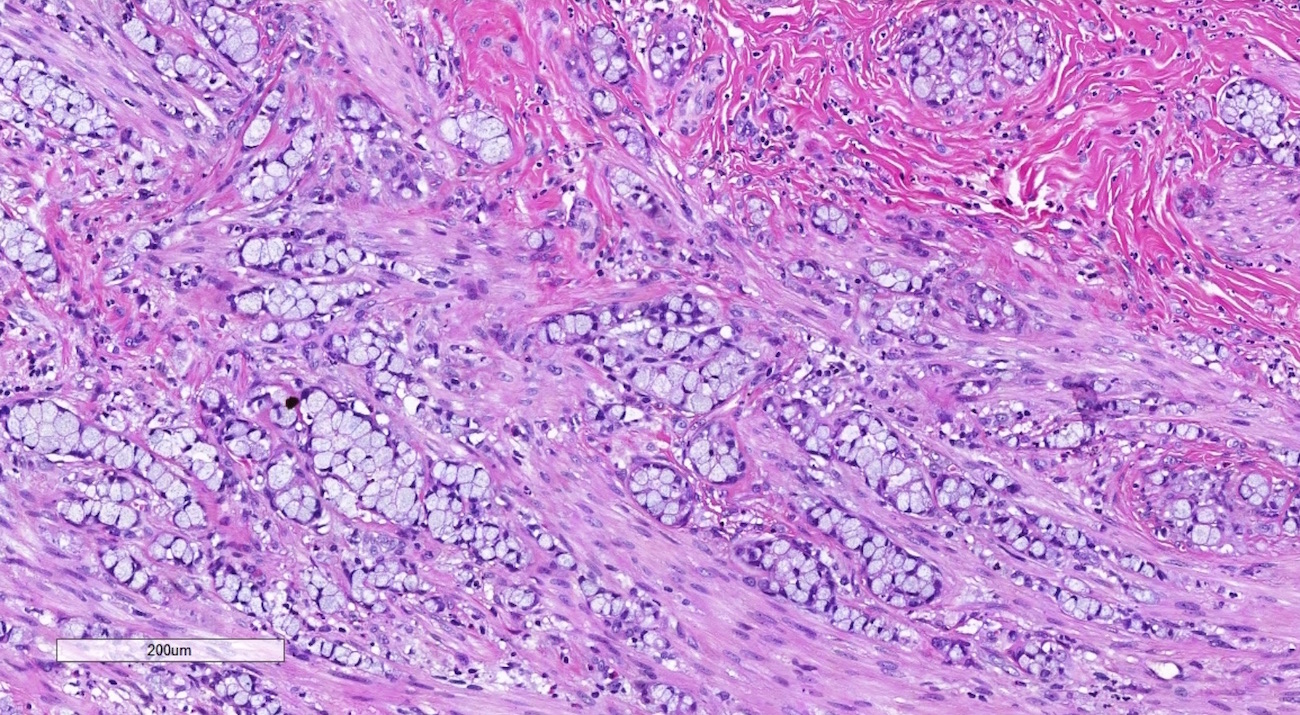
- Immunohistochemistry is a reliable tool in the distinction between primary ovarian tumors and metastases from appendiceal origin
- SATB2 is a sensitive and specific marker of colorectal epithelium
- Also positive in appendiceal epithelium
- This marker has shown 93.8% sensitivity and 97.5% specificity in determining appendiceal origin (Histopathol 2016;68:977)
- CK20, CDX2 and MUC2 are also optimal markers of appendiceal origin; although they are frequently expressed in primary ovarian tumors, such expression is usually patchy / focal
- Diffuse and strong expression for CK20, CDX2 and MUC2 has 90%, 87.5% and 95% specificity for appendiceal origin
Negative stains
Differential diagnosis
- Low grade mucinous neoplasm or mucinous carcinoma with pseudomyxoma peritonei arising in a mature cystic teratoma (Am J Surg Pathol 2007;31:854)
- Metastases from cervix: p16 positive (strong, diffuse)
- Metastases from colon and rectum: mass located in the large intestine, normal appendix (colorectal and appendiceal tumors have a similar IHC profile)
- Metastases from upper GI tract: CK7 positive, CK20 / CDX2 / SATB2 variable (mostly negative)
- Primary ovarian neoplasm (benign, borderline or malignant): absence of suspicious features described above (bilaterality, surface involvement, signet-ring cell morphology, etc), SATB2 negative, CK20 / CDX2 / MUC2 negative or patchy, PAX8 positive