Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Zanfagnin V, Devins K. Mucinous carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumormucinouscarcinoma.html. Accessed October 1st, 2025.
Definition / general
- Invasive adenocarcinoma composed predominantly of cells with intracytoplasmic mucin, typically with gastrointestinal type differentiation
Essential features
- Defined by invasion into the stroma by a neoplastic mucinous proliferation measuring 5 mm or more
- Invasion is divided into expansile and destructive patterns, the latter carrying a worse prognosis
- Important to exclude metastatic disease from gastrointestinal (GI) tract
Terminology
- Intestinal type mucinous adenocarcinoma
ICD coding
Epidemiology
- Mean age is 55 years; typically presents at a younger age (20 - 40 years) than patients with high grade serous carcinoma
- Incidence: < 7% of all ovarian carcinomas; < 5% of mucinous ovarian tumors
- Higher incidence in Indonesia, Singapore and the Republic of Korea (Gynecol Oncol 2014;133:147)
Sites
- Ovary
Pathophysiology
- May arise in the background of mucinous cystadenoma or borderline tumor
- Occasional tumors arise from mature cystic teratoma or a Brenner tumor (Mod Pathol 2020;33:722, Arch Pathol Lab Med 2008;132:1753)
- Smoking is associated with an increased risk of mucinous carcinoma (Cancer Causes Control 2013;24:989, Gynecol Oncol 2006;103:1122)
Etiology
- Unknown
Clinical features
- Symptoms, including abdominal pain, bloating and occasionally ascites, are most often related to the presence of a pelvic mass
- Pseudomyxoma peritonei is rarely associated with ovarian mucinous adenocarcinomas and should prompt consideration of metastasis, especially from an appendiceal primary
- Reference: Curr Oncol Rep 2014;16:389
Diagnosis
- Definitive diagnosis requires microscopic examination
- Upper or lower gastrointestinal primary tumor with ovarian metastases should be excluded
- Appendectomy is recommended in patients with a suspected or confirmed mucinous ovarian tumor if the appendix appears abnormal to exclude metastasis from an appendiceal primary
- Reference: Curr Oncol Rep 2014;16:389
Laboratory
- Cancer antigen 125 (CA125): usually not elevated
- Carcinoembryonic antigen (CEA) and CA19.9 can be elevated and may be useful for monitoring for recurrence
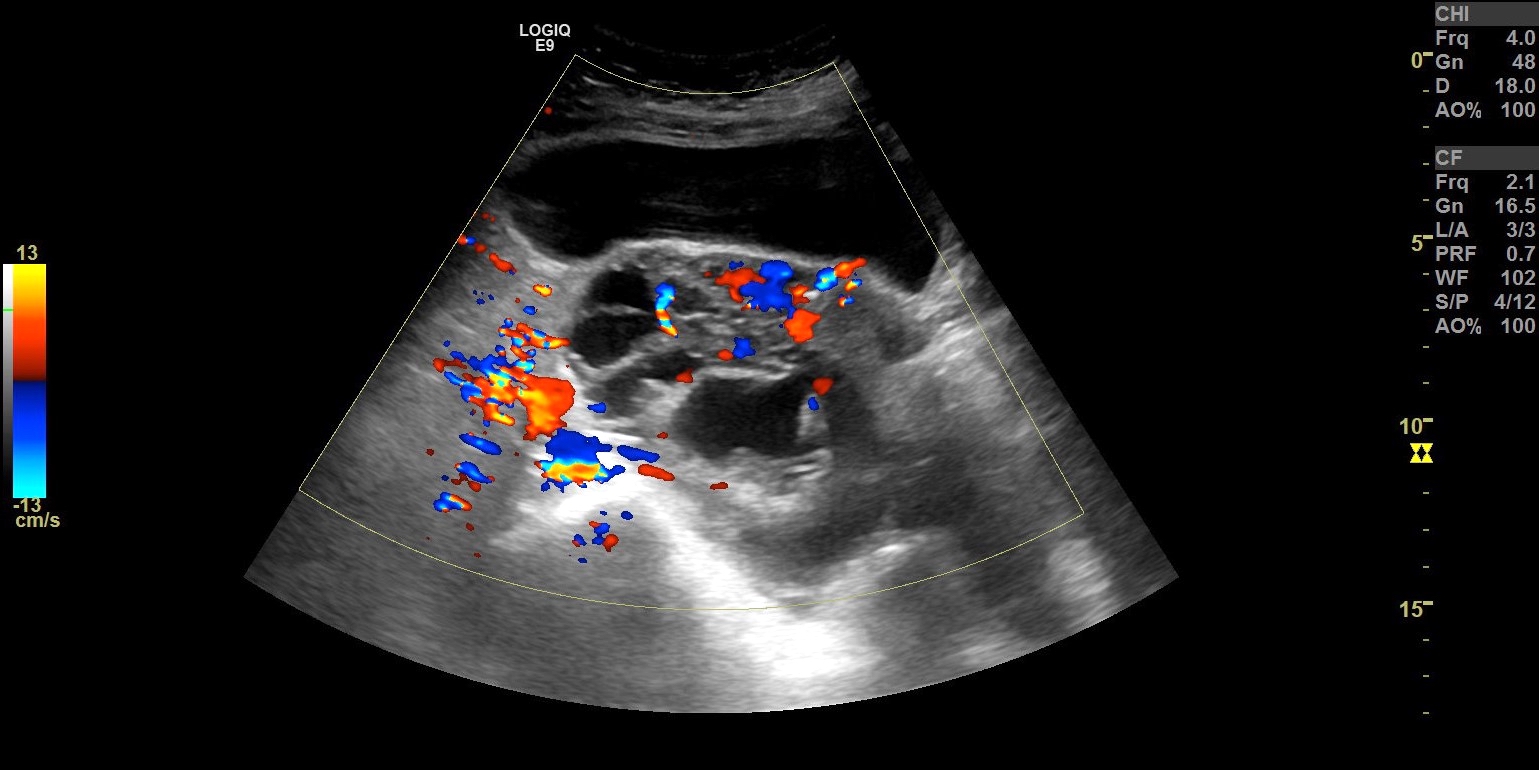
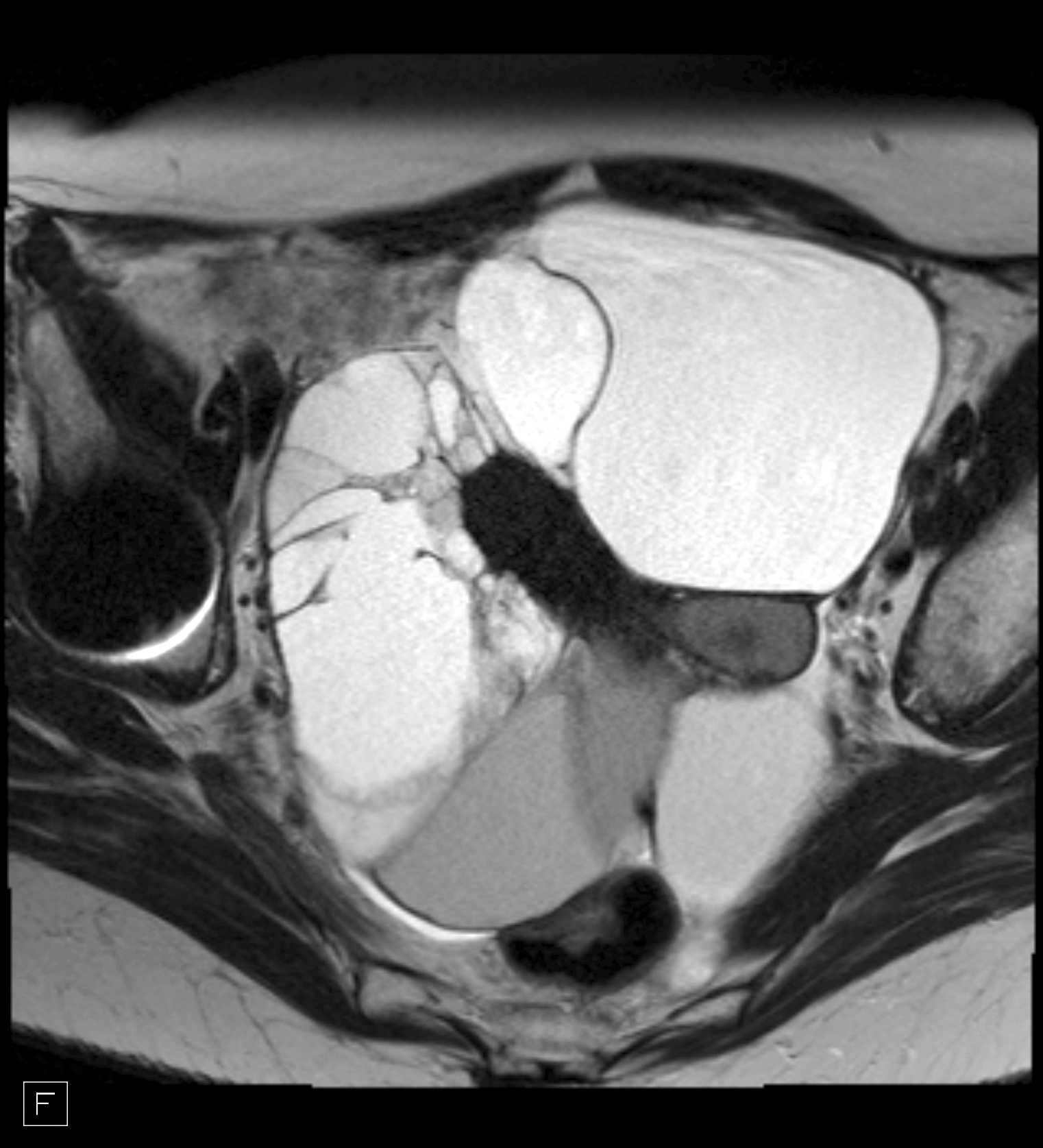
Radiology description
- Ultrasound: large (> 10 cm), unilateral, multiloculated cystic mass, with 1 or more solid parts (tumor nodule) and irregular septa; the cyst loculi vary in echogenicity, attenuation and signal intensity depending on the mucin content
- Magnetic resonance imaging (MRI): multilocular cystic lesion containing a solid part of intermediate intensity on T2 weighted MR images, hyperintense on diffusion weighted images and on perfusion sequences, with a type 3 enhancement curve (earlier enhancement relative to the myometrial curve)
- Reference: Radiographics 2019;39:982
Radiology images
Prognostic factors
- Mucinous carcinoma is often diagnosed at an early stage, which has a good prognosis; the 5 year disease free survival is ~80 - 90% (Int J Gynecol Cancer 2014;24:S14)
- Poor prognostic factors include high stage at diagnosis and destructive pattern of invasion
Case reports
- 24 year old woman with abdominal distension and dyspnea (J Family Med Prim Care 2022;11:2207)
- 28 year old woman with an increase in size of her abdomen (Case Rep Oncol 2023;16:1494)
- 65 year old woman with progressive weight loss, severe constipation and postprandial early satiety (Cureus 2022;14:e24589)
- 65 year old woman with pulmonary nodules (Pathologica 2022;114:365)
Treatment
- Surgery with comprehensive staging followed by postoperative therapy or observation
- For patients with stage IC mucinous carcinoma, postoperative options include (Int J Gynecol Cancer 2014;24:S14)
- Observation
- Intravenous (IV) carboplatin with either paclitaxel or docetaxel
- 5-fluorouracil (5-FU) / leucovorin / oxaliplatin (GI regimen)
- Capecitabine / oxaliplatin (GI regimen)
- For patients with stages II - IV mucinous carcinoma, postoperative options include
- Chemotherapy using the regimens for epithelial ovarian cancer (e.g., IV carboplatin with paclitaxel, docetaxel or liposomal doxorubicin)
- 5-FU / leucovorin / oxaliplatin (GI regimen)
- Capecitabine / oxaliplatin (GI regimen)
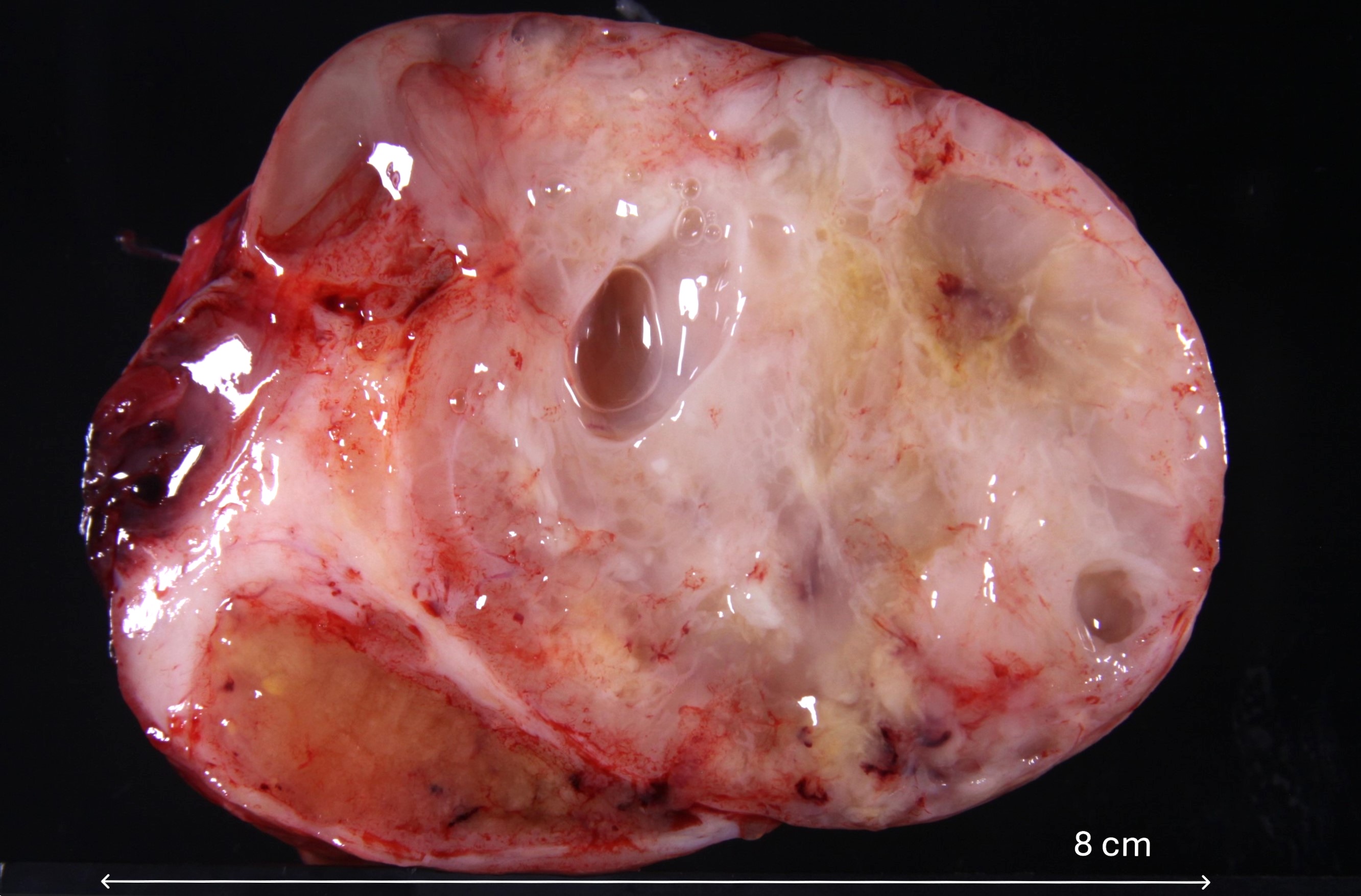
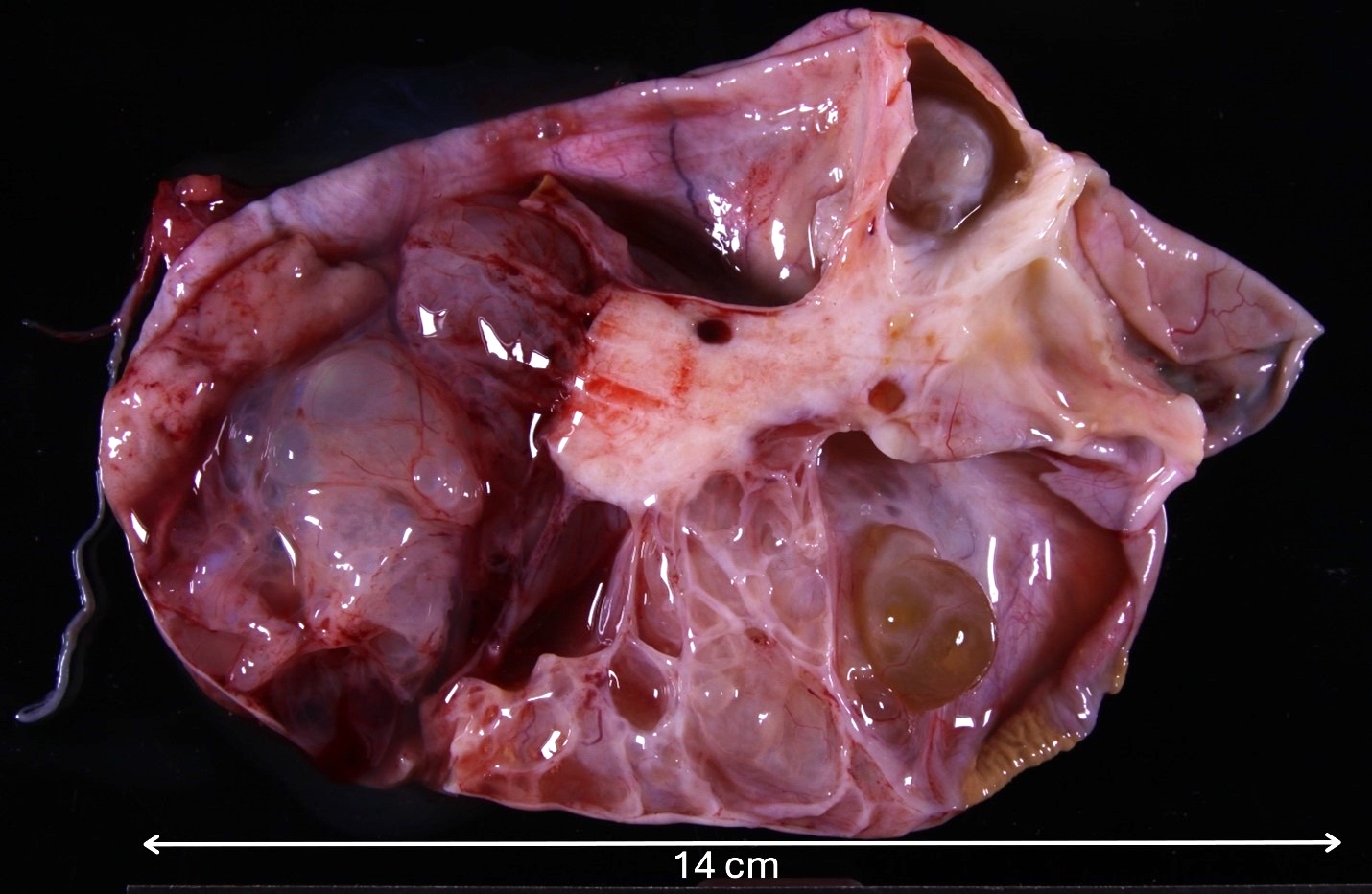
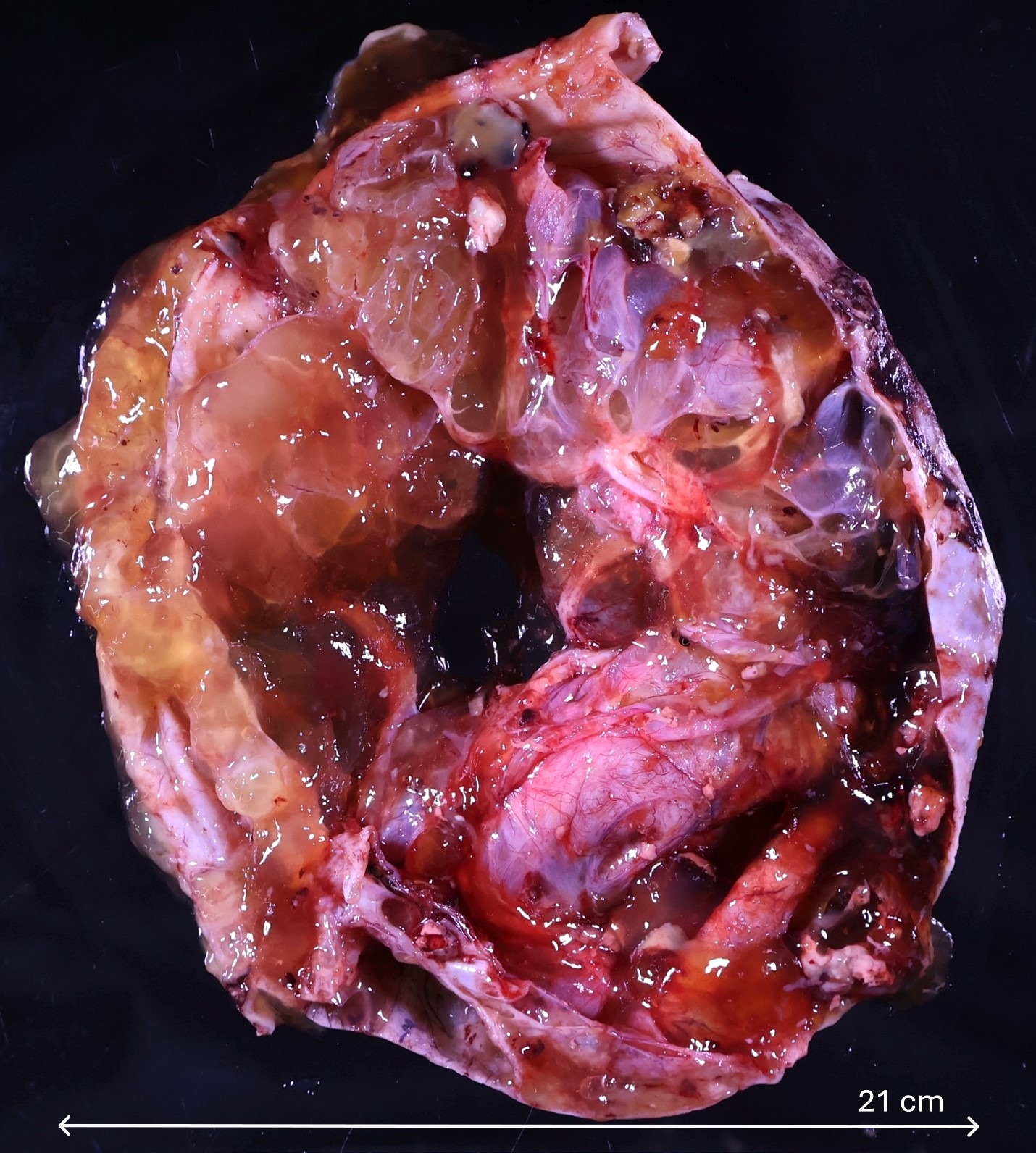
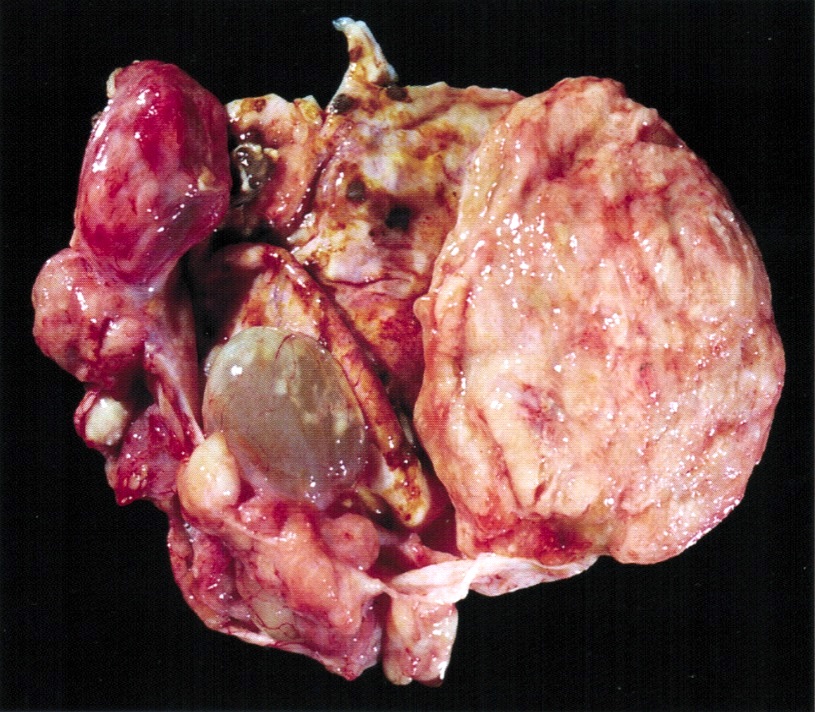
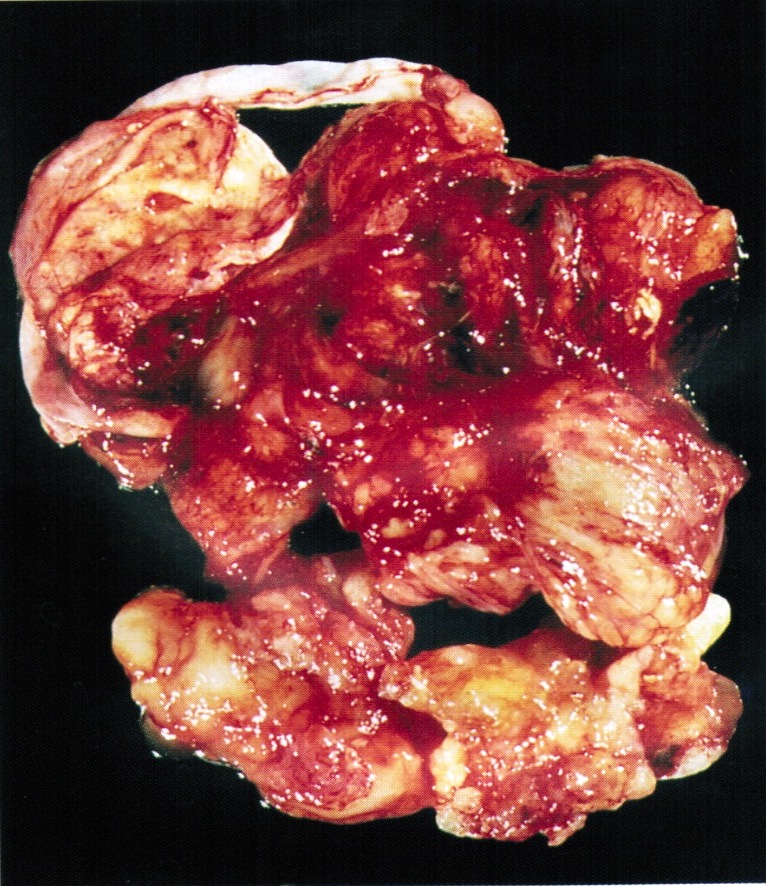
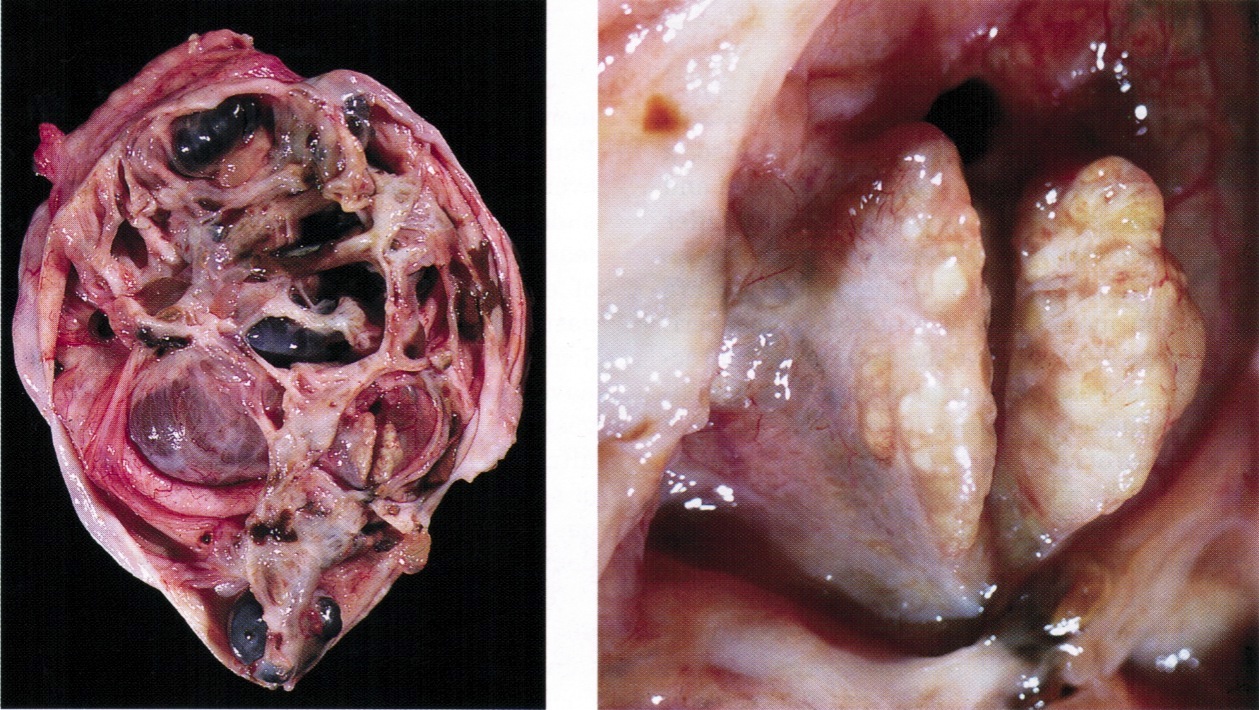
Gross description
- Size: mean is 19 cm (usually > 10 cm)
- General features: the tumors are typically large, unilateral, solid and cystic, with an intact and smooth outer surface and mucoid contents
Gross images
Frozen section description
- Mucinous tumor with cytologic atypia and expansile / confluent or infiltrative / destructive invasion, measuring at least 5 mm in linear extent
Microscopic (histologic) description
- Diagnosing mucinous carcinoma requires evidence of stromal invasion by epithelial proliferation spanning 5 mm or more in linear dimension
- The term intraepithelial carcinoma can be used if severe nuclear atypia is seen, usually with brisk mitotic activity, in the absence of stromal invasion after extensive sampling
- Microinvasive carcinoma is defined as small foci of stromal invasion (which may be multiple), measuring < 5 mm in greatest linear extent and comprising single cells or small groups of cells with marked cytologic atypia
- Morphological spectrum of stromal invasion is divided into 2 categories
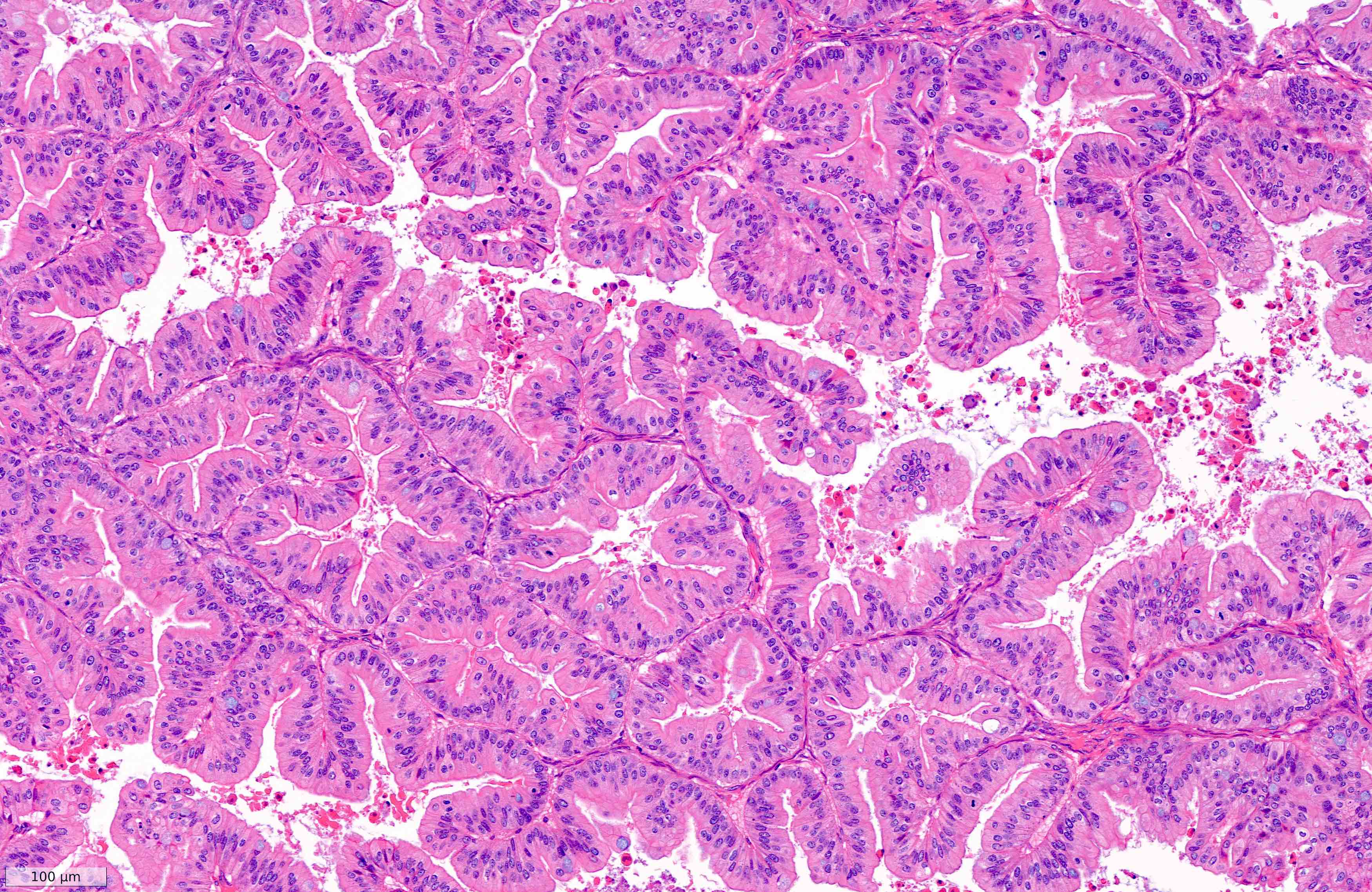
- Expansile (confluent / nondestructive) pattern: architecturally complex and confluent glands with round, convex outer outlines
- Stroma is minimal or absent and does not surround the glands entirely (back to back glands)
- This pattern is by far the most common in true primary mucinous adenocarcinomas of the ovary
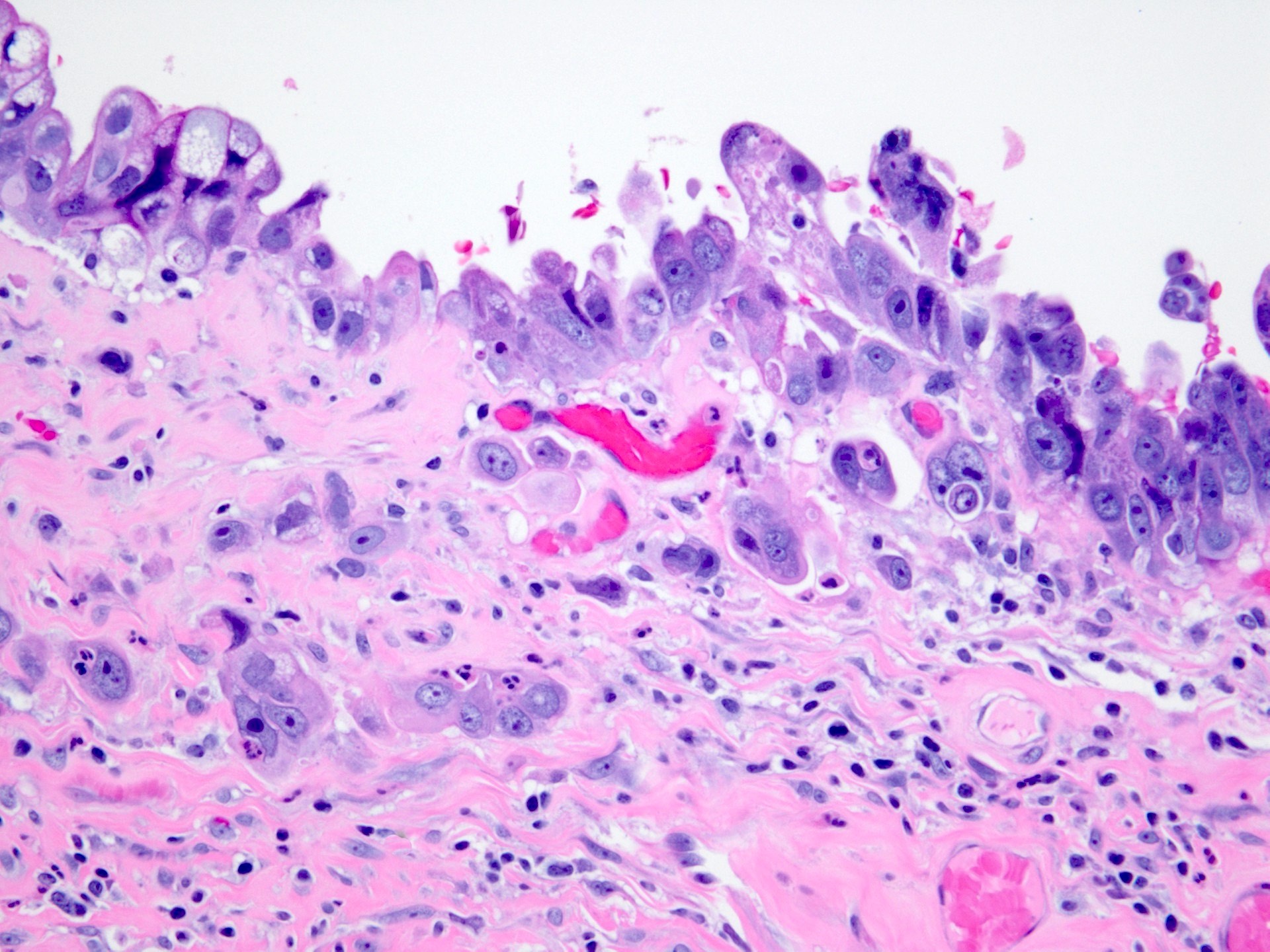
- Destructive (infiltrative) pattern: glands with irregular contours (angulated, elongated, fragmented, concave), often associated with stromal desmoplasia
- Nongland forming tumors (solid, sheets, single infiltrating cells) are included in this pattern of invasion, which carries a worse prognosis compared to expansile type (Am J Surg Pathol 2002;26:139, Eur J Cancer 2013;49:1600, Int J Gynecol Pathol 2014;33:176, Int J Gynecol Cancer 2018;28:493)
- Expansile (confluent / nondestructive) pattern: architecturally complex and confluent glands with round, convex outer outlines
- Percentage of destructive invasion relative to the entire neoplasm should be reported
- Destructive invasion is less common and should prompt consideration of metastasis
- Other features rarely seen in primary ovarian mucinous adenocarcinoma include abundant acellular stromal mucin pools, colloid carcinoma-like appearance with tumor cells floating in extracellular mucin and signet ring cells; all should prompt consideration of metastasis, particularly from a gastrointestinal primary
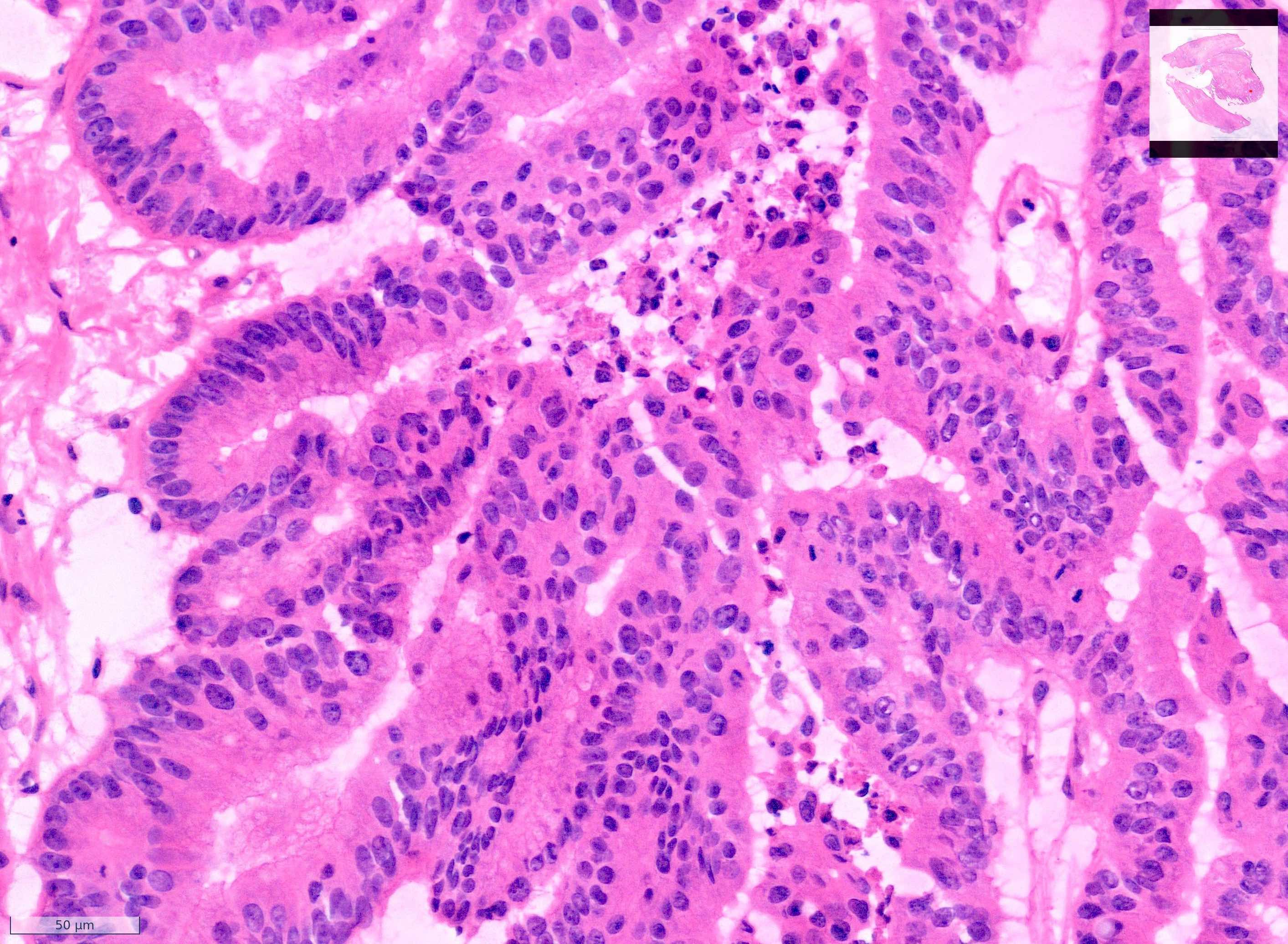
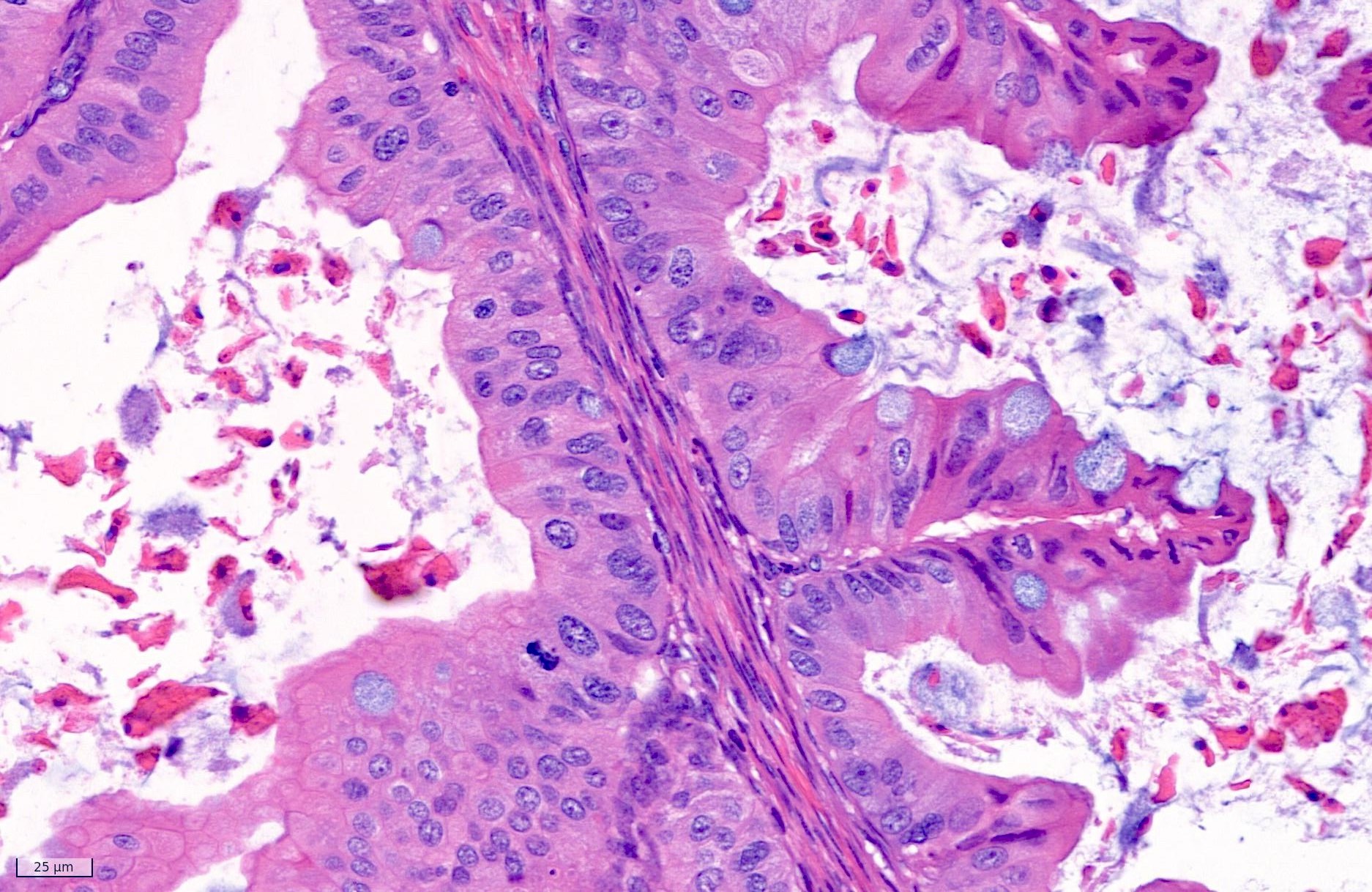
- Tumor cells resemble intestinal type epithelium and are often columnar and frequently contain intraepithelial mucin; goblet cells may be present
- Cytologic atypia is often present but variable in amount, including pseudostratification, nuclear hyperchromasia, nuclear pleomorphism and increased mitoses
- Standardized grading is currently not required for primary ovarian mucinous carcinoma and shows no clear correlation with outcomes
- Intratumoral heterogeneity is common and areas of mucinous cystadenoma and borderline morphology are often seen in the background
- Adequate sampling is often required to exclude mucinous adenocarcinoma; consider up to 2 sections per cm of maximum tumor diameter
- Mural nodules may occur
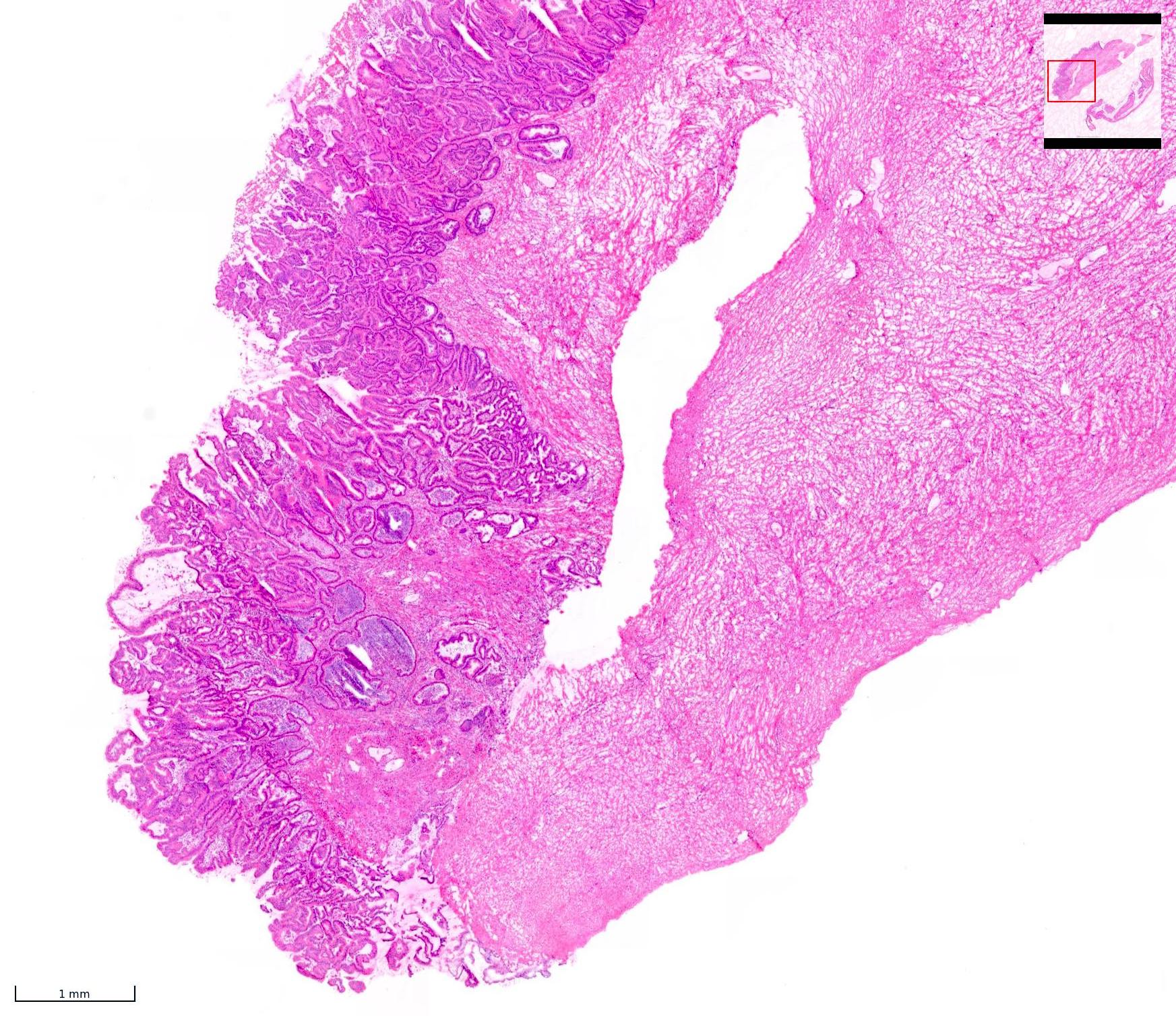
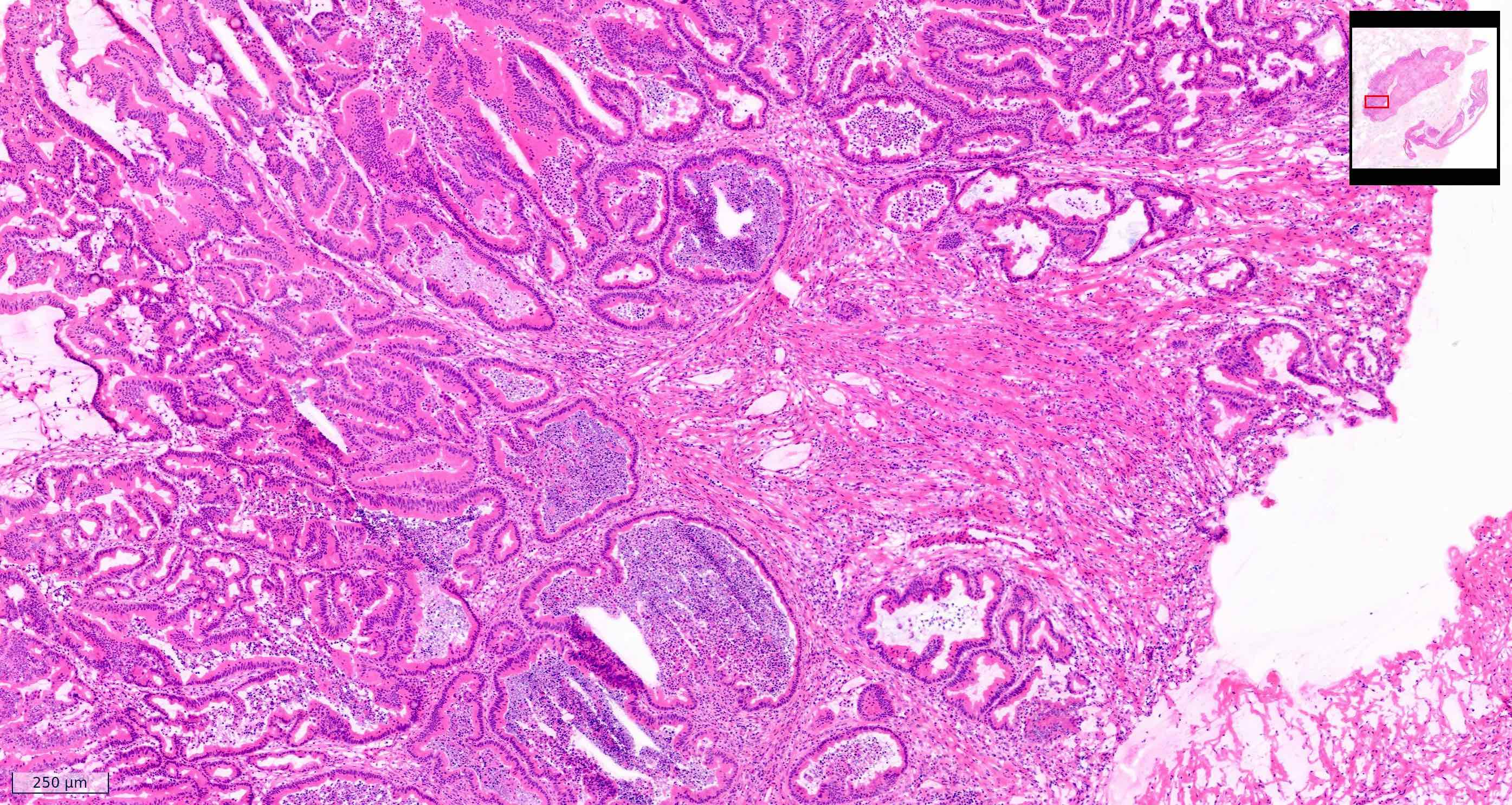
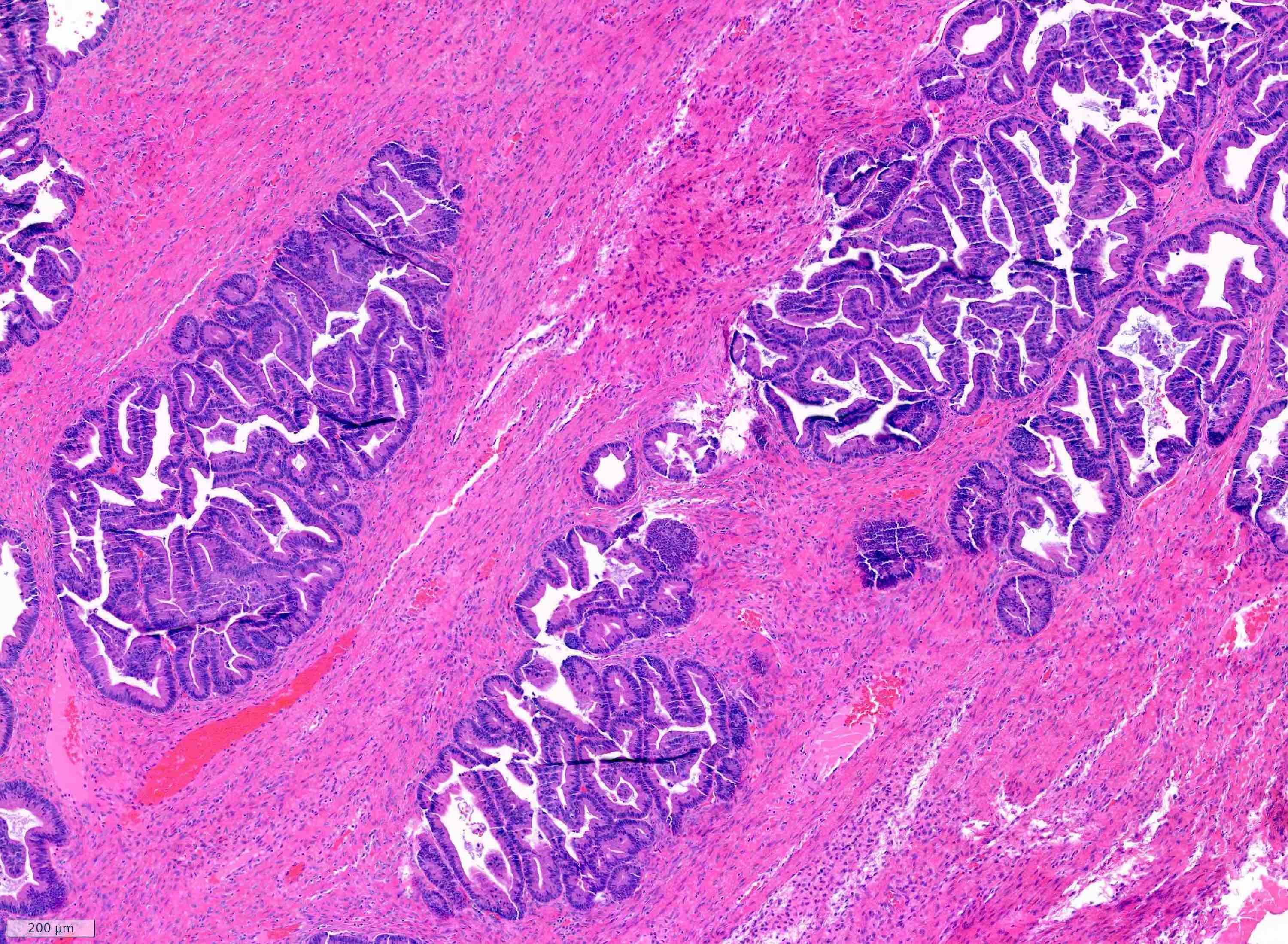
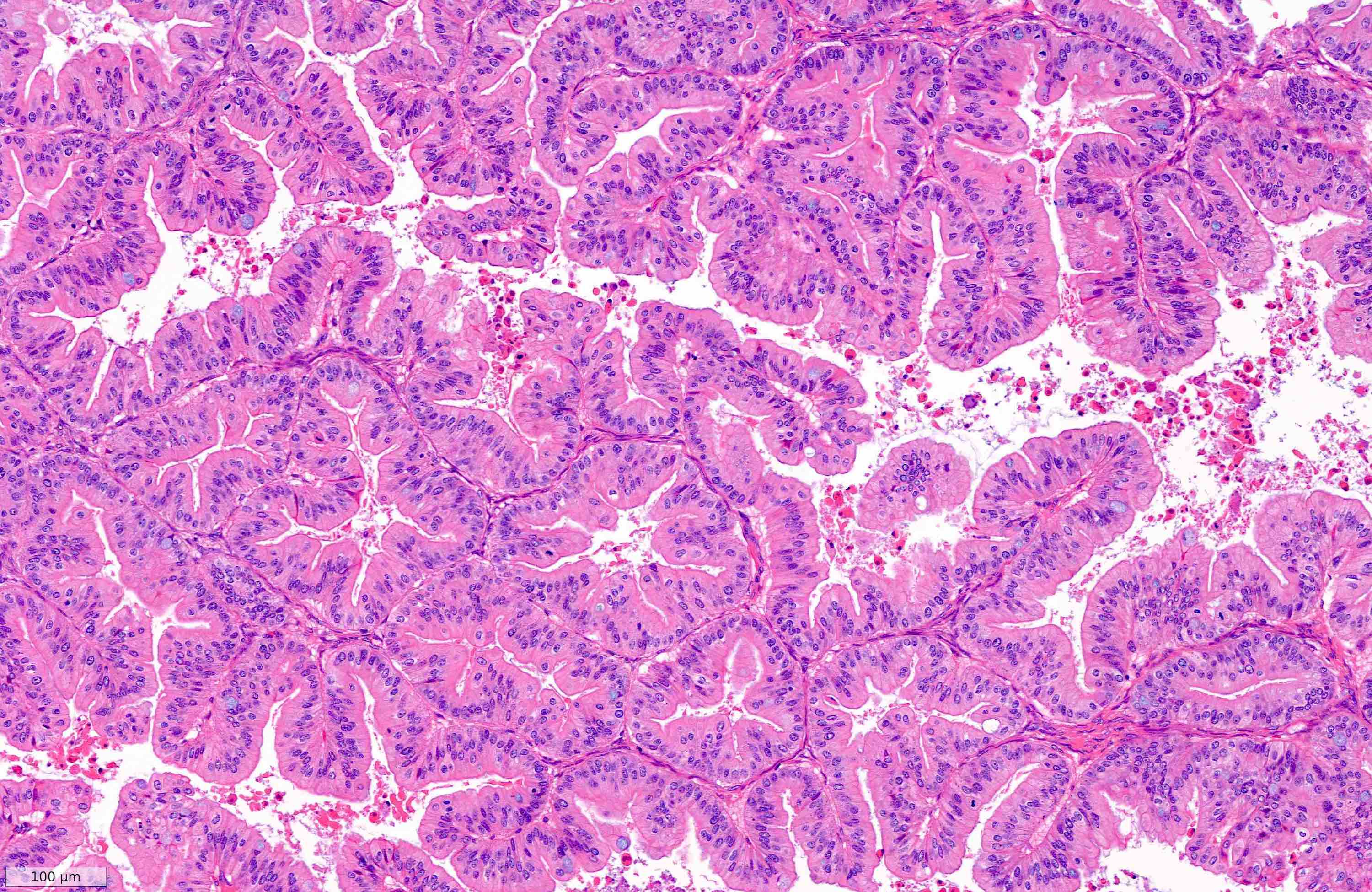
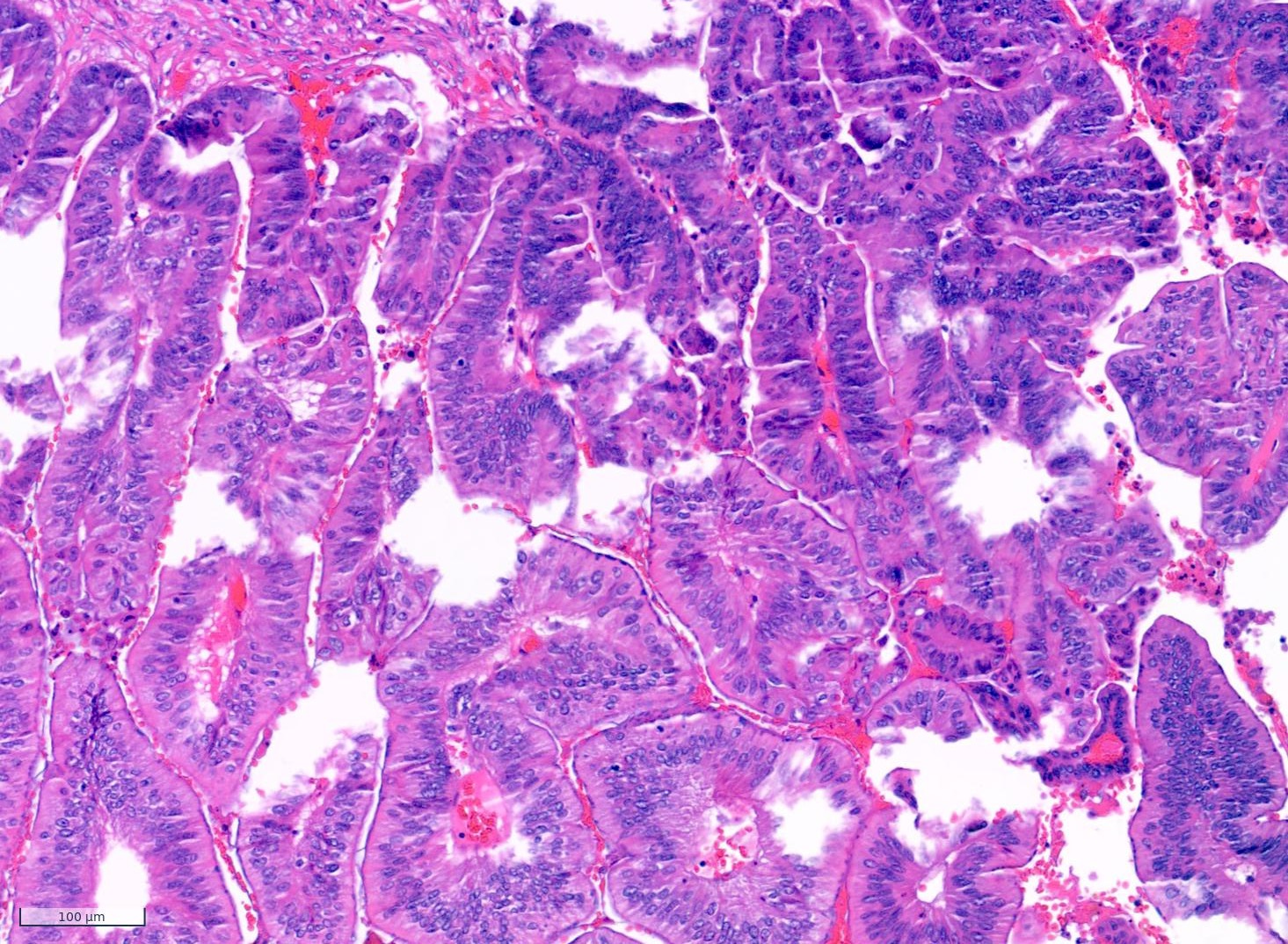
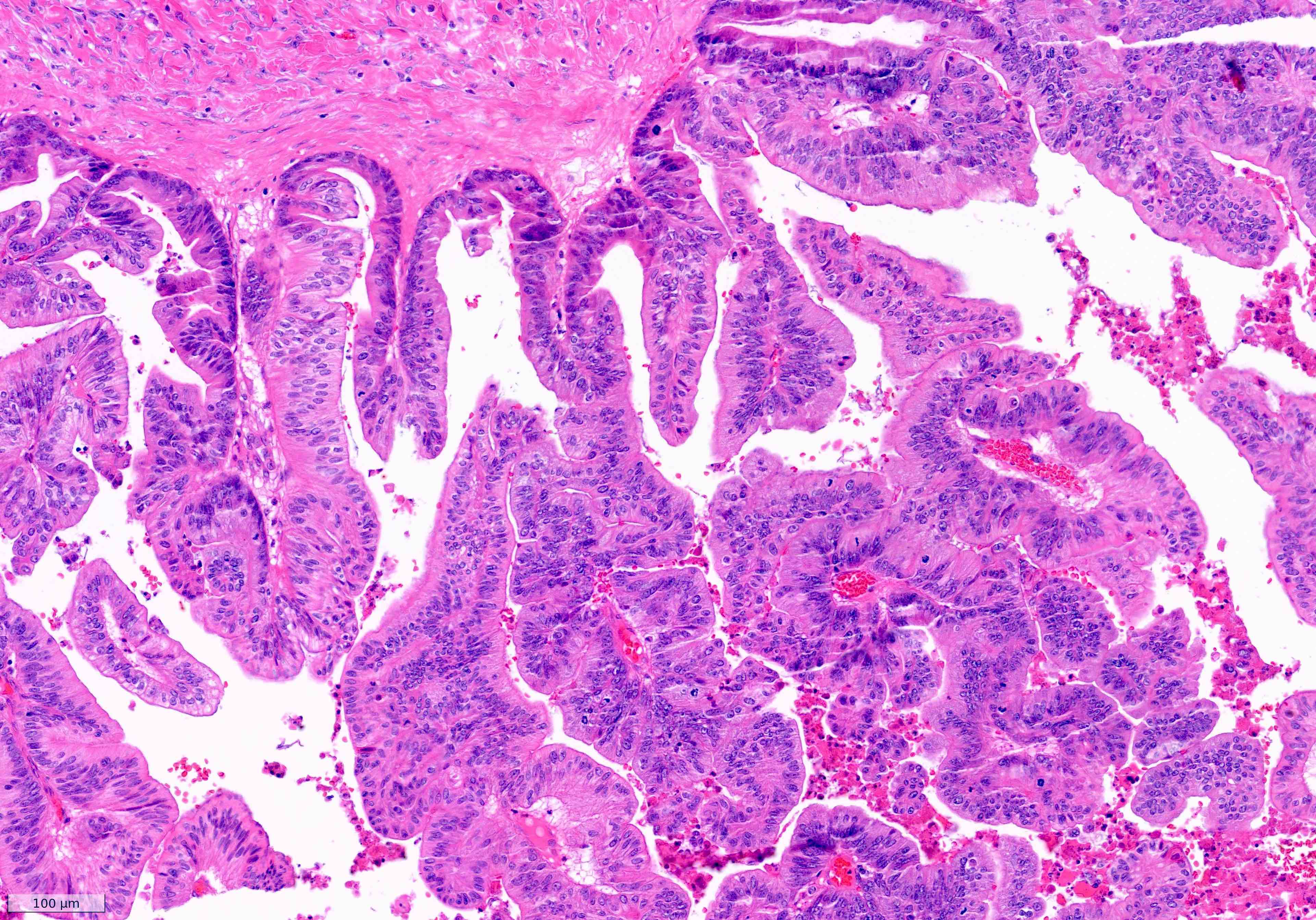
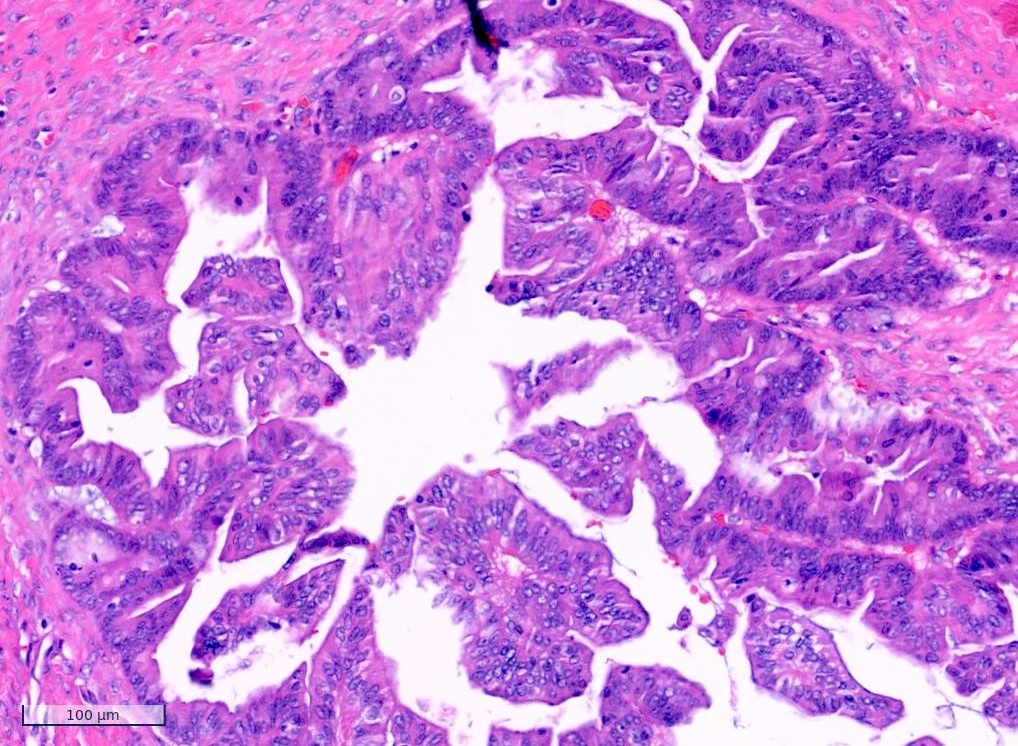
Microscopic (histologic) images
Contributed by Kyle Devins, M.D., Lawrence Hsu Lin, M.D., Ph.D., Valentina Zanfagnin, M.D. and Esther Oliva, M.D.
Cytology description
- Fine needle aspiration (FNA) of fluid
- Fluid is usually thick, gelatinous, blood tinged
- On microscopic examination, the specimen is of variable cellularity, in a background of thick mucin, necrosis and histiocytes
- Tumor cells are arranged in loosely cohesive groups, syncytial tissue fragments with papillary configuration, with or without branching
- Cells have a high N:C ratio and are pleomorphic in size
- Nuclear membrane is irregular, the chromatin has parachromatin clearing with pronounced nucleoli, while the cytoplasm is abundant with single or multiple vacuoles
- Peritoneal washing and ascites
- Malignant cells are similar to those described in the FNA of the ovary, ranging from small to large, occurring as individually dispersed cells or clusters and exhibiting a markedly pleomorphic pattern
- Mucin production is characterized by large distended cytoplasmic vacuoles
- Background is often hemorrhagic and necrotic
- Reference: Schmitt: Cytopathology - Encyclopedia of Pathology, 1st Edition, 2017
Positive stains
- CK7 often diffusely positive
- CK20, CEA, CDX2, CA19.9 variable but often positive
- p53 may show a mutant pattern in ~50%; subclonal mutant pattern or intratumoral heterogeneity maybe seen, with overexpression in the basal layer of the neoplastic glands while sparing superficial areas (terminal differentiation) (Mod Pathol 2021;34:194)
- p16 focal / patchy pattern of staining (nonblock positivity)
- Mucinous tumors arising in teratomas may exhibit an intestinal phenotype with diffuse staining for CK20, CEA, CDX2 and SATB2 (but negative for CK7)
Negative stains
- SATB2 (except in tumors arising in teratoma)
- ER, PR, WT1, napsin A, vimentin and CA125
- PAX8 and SOX17 may be positive in occasional tumors (15 - 75%, depending on the study); positivity favors an ovarian primary but both are frequently negative, even in confirmed primary ovarian mucinous adenocarcinoma (Int J Surg Pathol 2018;26:306, Mod Pathol 2023;36:100038, Mod Pathol 2023;36:100001)
Molecular / cytogenetics description
- CDKN2A alterations, either copy number loss (often seen in the context of 9p loss of heterozygosity) or mutations, in 33 - 76% of cases (Nat Commun 2019;10:3935)
- KRAS pathogenic hotspot mutations in 40 - 71% of cases (Nat Commun 2019;10:3935, Hum Genomics 2016;10:40)
- TP53 pathogenic mutations in 52 - 75% of cases (Nat Commun 2019;10:3935)
- ERBB2 (HER2 neu) amplification in 19 - 26% of cases (J Pathol 2013;229:111, Hum Genomics 2016;10:40)
- RNF43, BRAF, PIK3CA, MYO15A and ARID1A in 8 - 12% of cases (Nat Commun 2019;10:3935)
- 9p13 amplification in tumors with both KRAS and TP53 mutations (Nat Commun 2019;10:3935)
Videos
Ovarian mucinous tumors, differential diagnosis
Sample pathology report
- Ovary, left adnexa:
- Mucinous adenocarcinoma, intestinal type with expansile pattern of invasion (see synoptic report)
- Ovary, right adnexa:
- Mucinous adenocarcinoma, intestinal type with an infiltrative pattern of invasion (see comment and synoptic report)
- Comment: The infiltrative pattern represents ~10% (report percentage %) of the invasion.
Differential diagnosis
- Intestinal type mucinous borderline tumor:
- Lack of confluent or destructive invasion
- In difficult cases with complex architecture: attention to the outline of the area of proliferation is important; smooth outer borders without indentation favor intraglandular / intracystic growth, while interruption of the outer border or indentation by the proliferation is more consistent with expansile invasion
- Extensive sampling may be warranted in large / complex tumors to exclude invasion
- Metastatic mucinous adenocarcinoma:
- Features favoring metastasis
- Bilateral ovarian involvement and extraovarian disease
- Ovarian surface involvement with no rupture
- Multinodular distribution of infiltrative foci in an edematous background
- Severe atypia or numerous mitoses despite relatively simple architecture
- Signet ring morphology
- Extensive destructive invasion
- Prominent vascular invasion, particularly in the ovary hilus
- History of gastrointestinal adenocarcinoma
- If pancreatobiliary, SMAD4 loss
- If colorectal, CK7 negative / SATB2 positive
- If endocervical, p16 block staining (strong nuclear and cytoplasmic expression in a continuous segment of cells) and HPV positive
- Features favoring metastasis
- Endometrioid adenocarcinoma:
- Presence of squamous differentiation or endometriosis
- Positive ER, PR, beta catenin, ARID1A and MMR abnormalities
- Sertoli-Leydig cell tumors with extensive heterologous mucinous elements:
- Typical areas, mucinous component benign or atypical
- Dense eosinophilic secretions within the lumina
Additional references
Practice question #1
What is the primary entity that should be excluded before making a diagnosis of mucinous carcinoma of the ovary?
- Endometrioid adenocarcinoma
- High grade serous carcinoma
- Metastatic breast carcinoma
- Metastatic carcinoma of gastrointestinal origin
Practice answer #1
D. Metastatic carcinoma of gastrointestinal origin. Metastatic carcinoma of gastrointestinal origin is a common mimic of primary ovarian mucinous tumor and should be excluded prior to rendering that diagnosis. Appendectomy is recommended in patients with a suspected or confirmed mucinous ovarian tumor if the appendix appears abnormal. Answer A is incorrect because endometrioid adenocarcinomas do not typically mimic mucinous carcinomas. Answer B is incorrect because high grade serous carcinomas typically lack intracytoplasmic mucin and thus infrequently mimic mucinous tumors. Answer C is incorrect because metastatic breast cancers typically lack intracytoplasmic mucin and thus infrequently mimic mucinous tumors.
Comment Here
Reference: Mucinous carcinoma
Comment Here
Reference: Mucinous carcinoma
Practice question #2
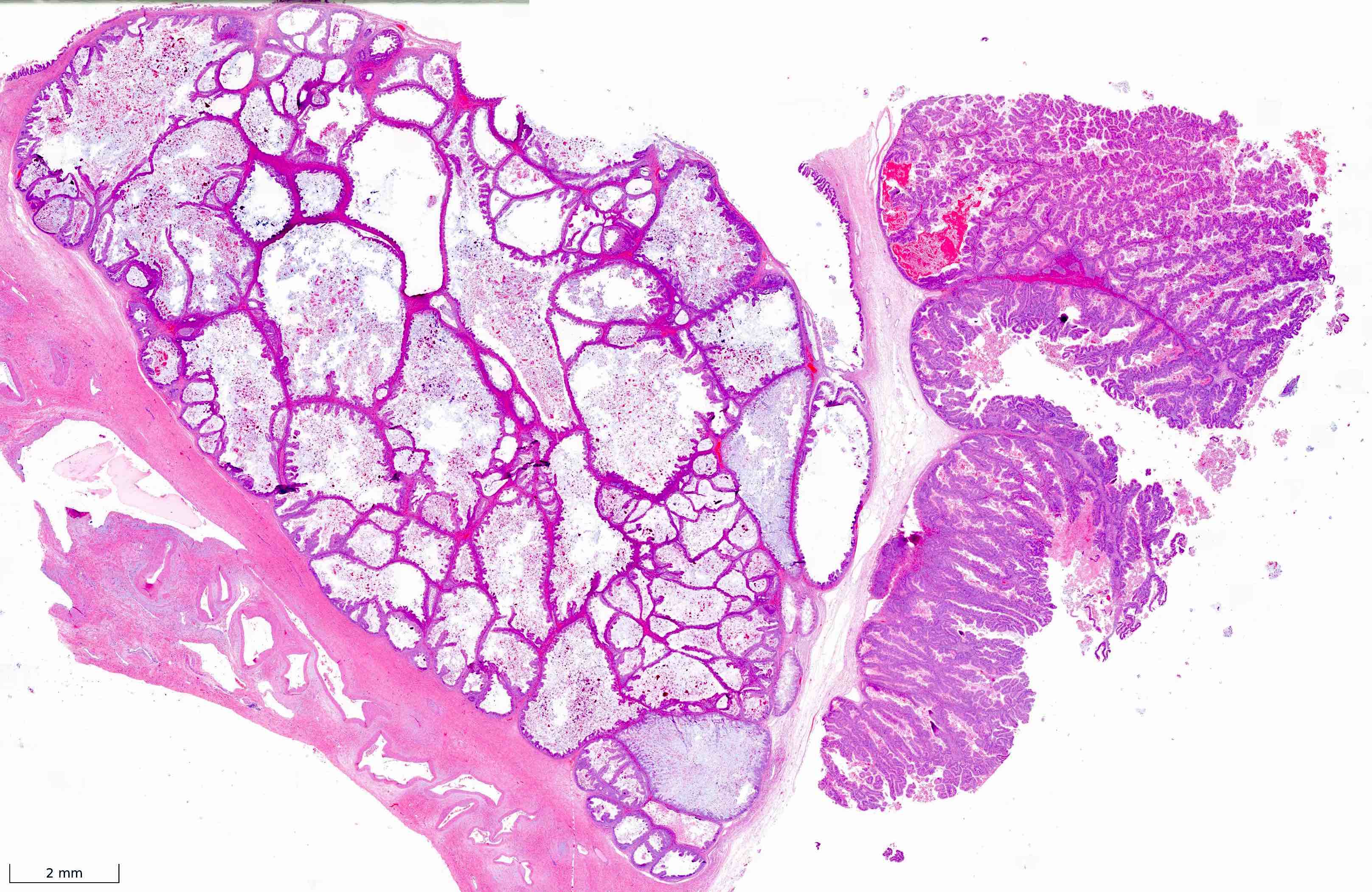
A 39 year old woman presents to the clinic with a 6 month history of mild abdominal pain and distension. A computed tomography (CT) scan of the abdomen shows a 20 cm adnexal mass. The patient undergoes surgery. The tumor is shown above. What is your diagnosis?
- Borderline mucinous tumor of the ovary
- Borderline mucinous tumor of the ovary with microinvasion
- Mucinous adenocarcinoma of the ovary
- Mucinous cystadenoma
Practice answer #2
C. Mucinous adenocarcinoma of the ovary. The tumor shows an expansile / confluent pattern of invasion with architecturally complex and confluent glands with round, convex outer outlines. The stroma is minimal or absent and does not surround the glands entirely (back to back glands). Answer A is incorrect because borderline mucinous tumors show variable degrees of epithelial stratification, tufting and villous or slender filiform papillae in at least 10% of the tumor, with an absence of stromal invasion; in contrast, the image shows an extensive expansile pattern of invasion. Answer B is incorrect because microinvasion is defined by small foci of stromal invasion (which may be multiple), comprising single cells or small groups of cells, measuring < 5 mm in the greatest linear dimension. In contrast, the image shows an extensive expansile pattern of invasion. Answer D is incorrect because in mucinous cystadenomas cysts and glands are lined by benign mucinous epithelium with no architectural complexity or cytological atypia; in contrast, the image shows significant architectural and cytologic atypia with an extensive expansile pattern of invasion.
Comment Here
Reference: Mucinous carcinoma
Comment Here
Reference: Mucinous carcinoma