Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Negative stains | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Kazlouskaya V, Collins MK. Psoriasis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorpsoriasis.html. Accessed August 25th, 2025.
Definition / general
- Psoriasis is a chronic relapsing condition affecting skin, nails and joints that most commonly presents with well demarcated erythematous papules and plaques with silvery white scales
Essential features
- Most common clinical presentation: well demarcated erythematous plaques with silvery white scales
- Complex pathogenesis including genetic, autoimmune and environmental factors
- Common histopathological features: regular acanthosis, lymphocytic perivascular inflammation, parakeratosis with neutrophilic collections, spongiosiform pustules with neutrophils, dilated vessels in the papillary dermis, alternating areas of hyper and hypogranulosis and thinning of the suprapapillary plates
- Several different clinical and histopathologic variants
ICD coding
Epidemiology
- Adults:
- Prevalence of 0.14 - 1.99%, higher in Western Europe, central Europe, North America and high income areas of South America (BMJ 2020;369:m1590)
- Incidence ranges from 30.3 to 321.0 per 100,000 person years (BMJ 2020;369:m1590)
- Children:
- Prevalence of 0.02 - 0.22% (BMJ 2020;369:m1590)
- Incidence is less studied, from 2.6 to 70.5 per 100,000 person years (BMJ 2020;369:m1590)
- Peak incidence is at 20 - 30 years and at 50 - 60 years
- Psoriatic arthritis occurs in 5 - 30% of patients with psoriasis
- Associated with cardiovascular complications (increased rate of myocardial infarction, hypertension, hyperlipidemia, obesity, hyperlipidemia), depression, inflammatory bowel disease, diabetes, fatty liver disease and chronic kidney disease (J Am Heart Assoc 2020;9:e016956, J Am Acad Dermatol 2017;77:287, J Am Acad Dermatol 2017;76:393)
Sites
- Skin, nails, musculoskeletal system and rarely oral mucosa
Pathophysiology
- Complex pathogenesis, including genetic, autoimmune and environmental factors (J Allergy Clin Immunol 2017;140:645, Int J Mol Sci 2019;20:1475, J Dermatol 2018;45:264, J Immunol 2018;201:1605)
- T cell (Th1) activation and release of cytokines (TNFα, IFγ, IL12, etc.)
- Dendritic cells produce IL23, which activates Th17 cells, which then play a key role in the development of psoriasis; IL23 also induces macrophages to secrete TNFα
- Th17 cells produce IL17, which promotes the production of other proinflammatory molecules (Int J Mol Sci 2017;18:2684)
- IL22, produced by Th17 and Th22 cells, plays a role in stimulating the proliferation of keratinocytes and causing the development of psoriatic plaques
- Overexpression of antimicrobial peptides (β-defensins, cathelicidin and S100) stimulate inflammation
- NFκB induces expression of keratins 6 and 16, leading to acanthosis and increased turnover of keratinocytes
Etiology
- Genetic:
- PSOR1 locus map on chromosome 6 is the most important genetic region responsible for the disease
- HLA-Cw6 is associated with early onset of psoriasis
- Additional associations include HLA-B27 (pustular psoriasis, psoriatic arthritis), HLA-B13, HLA-B17 and HLA-DR7
- Triggering factors: numerous, most common are infections, HIV, hypocalcemia, stress, alcohol consumption, obesity and smoking (Front Immunol 2019;10:1807, Psoriasis (Auckl) 2016;6:65)
- Drugs: antimalarials, lithium, beta blockers, terbinafine and imiquimod (Psoriasis (Auckl) 2017;7:87)
- Paradoxically, TNF inhibitors, which are used to treat psoriasis, may also trigger psoriasis when used for other conditions
- Streptococcus infections may trigger acute guttate psoriasis
- Systemic steroid withdrawal may trigger pustular psoriasis, von Zumbusch type
Clinical features
- Variants:
- Plaque psoriasis (most common): sharply demarcated erythematous plaques with silvery scales, commonly present on extensor surfaces (elbows, knees, etc.)
- Guttate psoriasis: small scattered erythematous papules with silvery scales; often triggered by infections
- Erythrodermic psoriasis: confluent plaques affecting nearly all of the skin but often sparing the central face; lymphadenopathy, electrolyte and thermoregulation abnormalities may also be present
- Pustular psoriasis: presence of superficial pustules; generalized (von Zumbusch type), annular, palmar-plantar, localized and exanthemic variants are described
- Acrodermatitis continua of Hallopeau: pustules on the distal parts of the fingers and toes, as well as on the nail bed, which may cause shedding of the nail plate
- Scalp psoriasis: well demarcated plaques on the retroauricular areas and posterior upper neck
- Sebopsoriasis lesions on the scalp, face, upper back and chest mimicking seborrheic dermatitis
- Linear psoriasis: development of psoriasis lesions along Blaschko lines
- Annular / figurate psoriasis: annular lesions of psoriasis with central clearing
- Flexural (inverse) psoriasis: plaques affecting intertriginous folds, scaling may be less prominent
- Napkin psoriasis: may be seen in napkin (diaper) area in newborns
- Nail psoriasis: pits, splinter hemorrhages, oil drop sign (translucent yellow discoloration of the nail caused by parakeratosis of the nail bed), salmon patches and leukonychia are common on the nail plate
- Follicular psoriasis: small keratotic follicular papules with scaling (Dermatol Online J 2020;26:3)
- Psoriatic arthritis: inflammation of distal interphalangeal joints and proximal interphalangeal joints of the feet and hands
- Oral psoriasis: red patches, geographic tongue, ulcerations, gingivitis or pustules
- Signs:
- Koebner phenomenon: new psoriatic papules at sites of skin trauma
- Auspitz sign: pinpoint bleeding when scales are removed
- Woronoff ring: an area of blanching surrounding resolving psoriatic plaques
Diagnosis
- Clinical examination
- Skin biopsy
- Xray if joints are affected
- Complete blood count, comprehensive metabolic panel (kidney and hepatic function), pregnancy, tuberculosis, HIV and hepatitis tests may be considered if systemic treatment is planned
Laboratory
- Usually not needed to establish the diagnosis; should be performed if systemic treatment is desired
- Rheumatoid factor is negative
Radiology description
- 5 main types of psoriatic arthritis:
- Symmetrical peripheral polyarthritis resembling RA
- Asymmetrical mono or oligoarthritis, usually involving the knee and small peripheral joints
- Axial spondyloarthropathy
- Predominant DIP joint involvement
- Arthritis mutilans
- Dactylitis, inflammatory changes in the distal interphalangeal joints and proximal interphalangeal joints, finger deformities (pencil in cup)
- Increase of radiographic density of the distal phalanx due to extra bone formation (ivory phalanx)
- Enthesitis
- Abnormalities of the sacroiliac joints (J Ultrason 2016;16:65, J Ultrason 2016;16:163)
Radiology images
Prognostic factors
- Chronic disease with frequent relapses; early systemic treatment to achieve control and prevent systemic comorbidities
Case reports
- 5 year old girl developed guttate psoriasis after throat infection (Am Fam Physician 2019;99:575)
- 45 year old woman with nail psoriasis treated with intralesional methotrexate (An Bras Dermatol 2019;94:491)
- 65 year old man with history of psoriasis exacerbating to erythroderma after HIV infection (An Bras Dermatol 2018;93:438)
- 66 year old woman with acrodermatitis continua of Hallopeau responded to adalimumab therapy (SAGE Open Med Case Rep 2019;7:2050313X19829620)
- 81 year old man with verrucous psoriasis plaque mimicking squamous cell carcinoma (JAAD Case Rep 2019;5:723)
Treatment
- Topical treatment: corticosteroids (most common); vitamin D analogs (calcipotriene and calcitriol); topical retinoids; immunomodulators (pimecrolimus and tacrolimus); coal tar; keratolytics (salicylic acid and urea)
- Intralesional steroids to resistant plaques
- Light therapy (UVB, PUVA)
- Systemic therapies (methotrexate, cyclosporine and mycophenolate mofetil, JAK inhibitors)
- Biological therapies:
- TNF inhibitors: infliximab, etanercept, adalimumab
- IL12 / 23 inhibitor: ustekinumab
- IL17 inhibitors: ixekinumab, brodalumab, secukinumab
- IL23 inhibitors: guselkimab, tildrakizumb, risankizumab
- Phosphodiesterase-4 inhibitors: apremilast
- Reference: Int J Mol Sci 2019;20:1475
Clinical images
Gross description
Gross images
- See clinical images
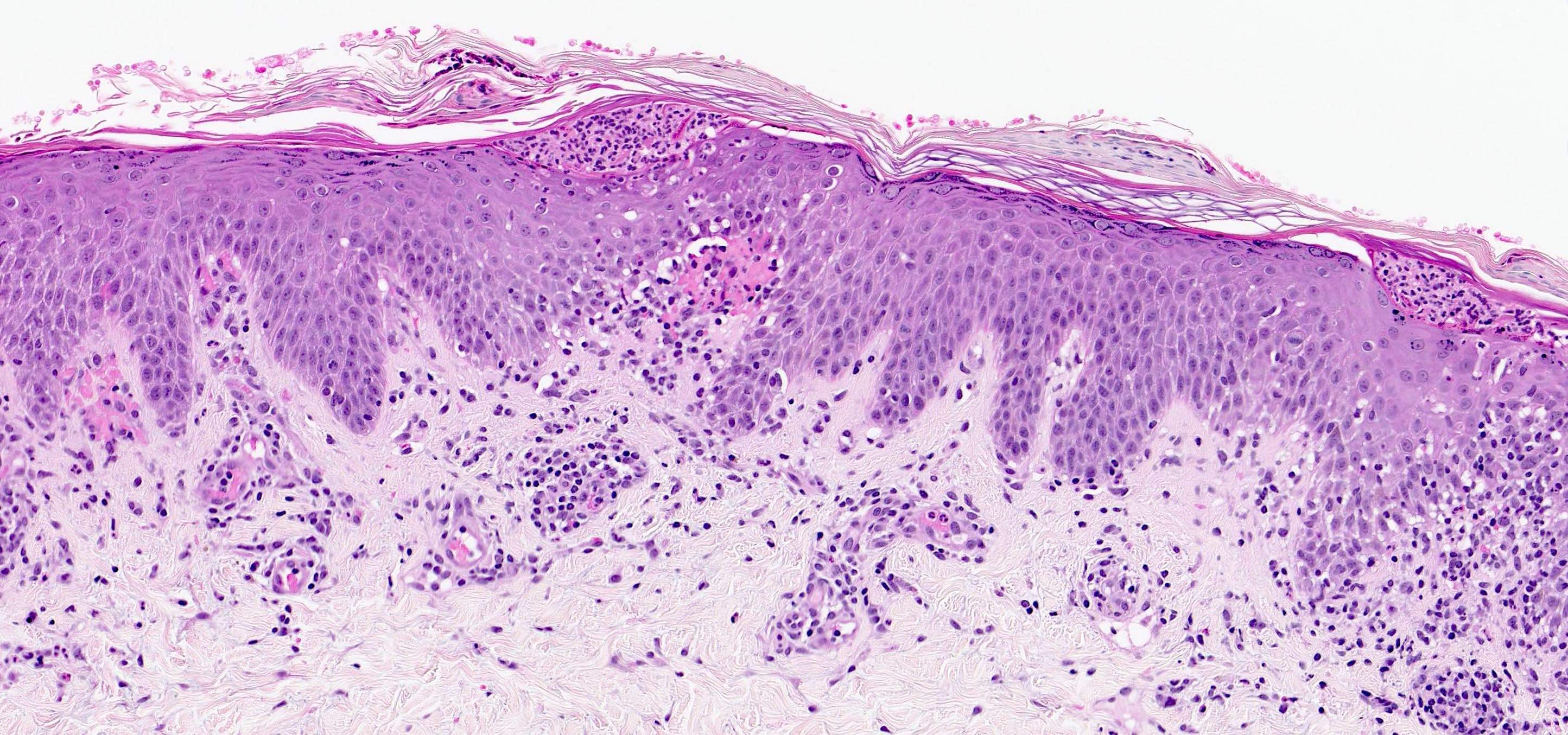
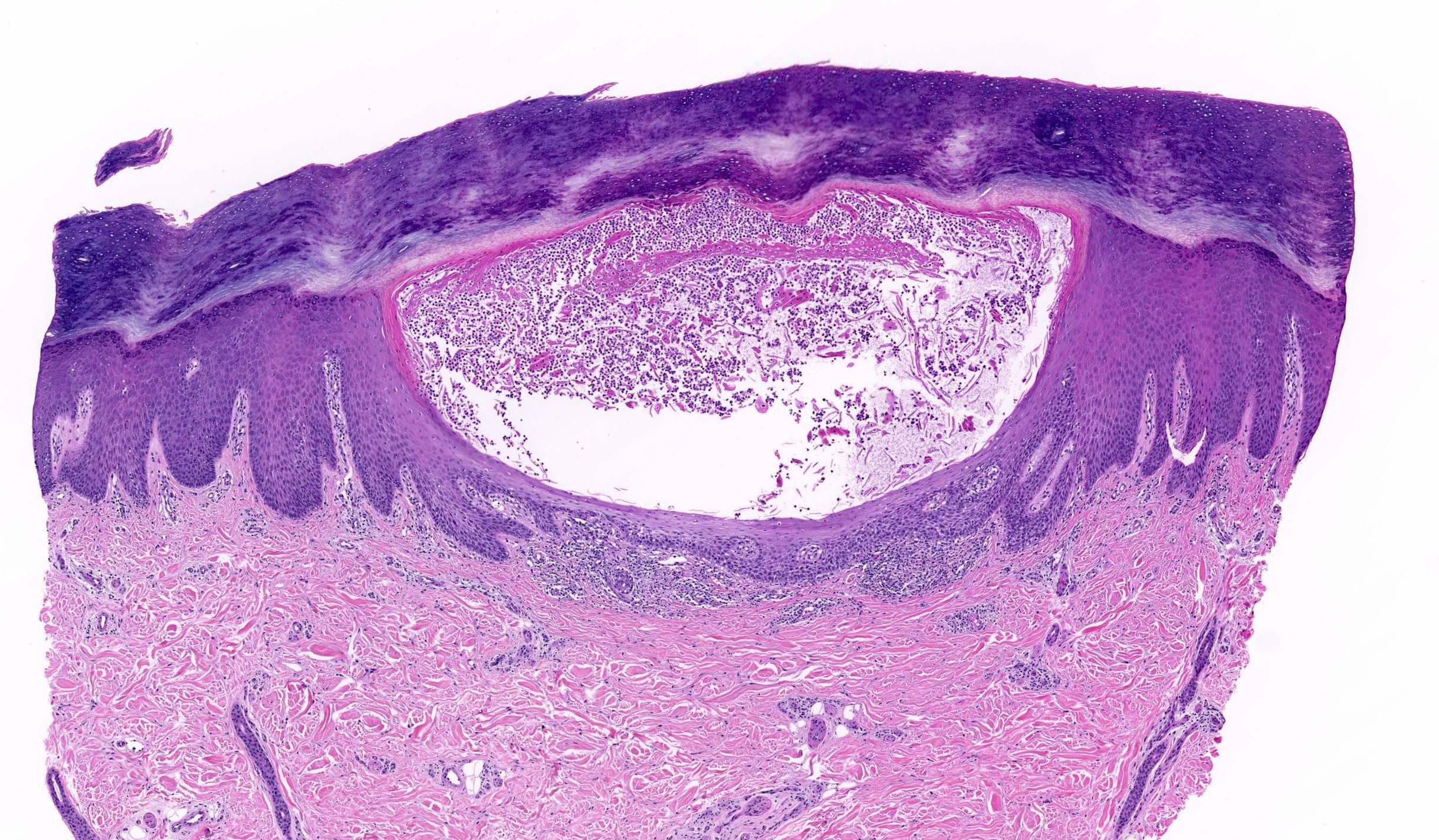
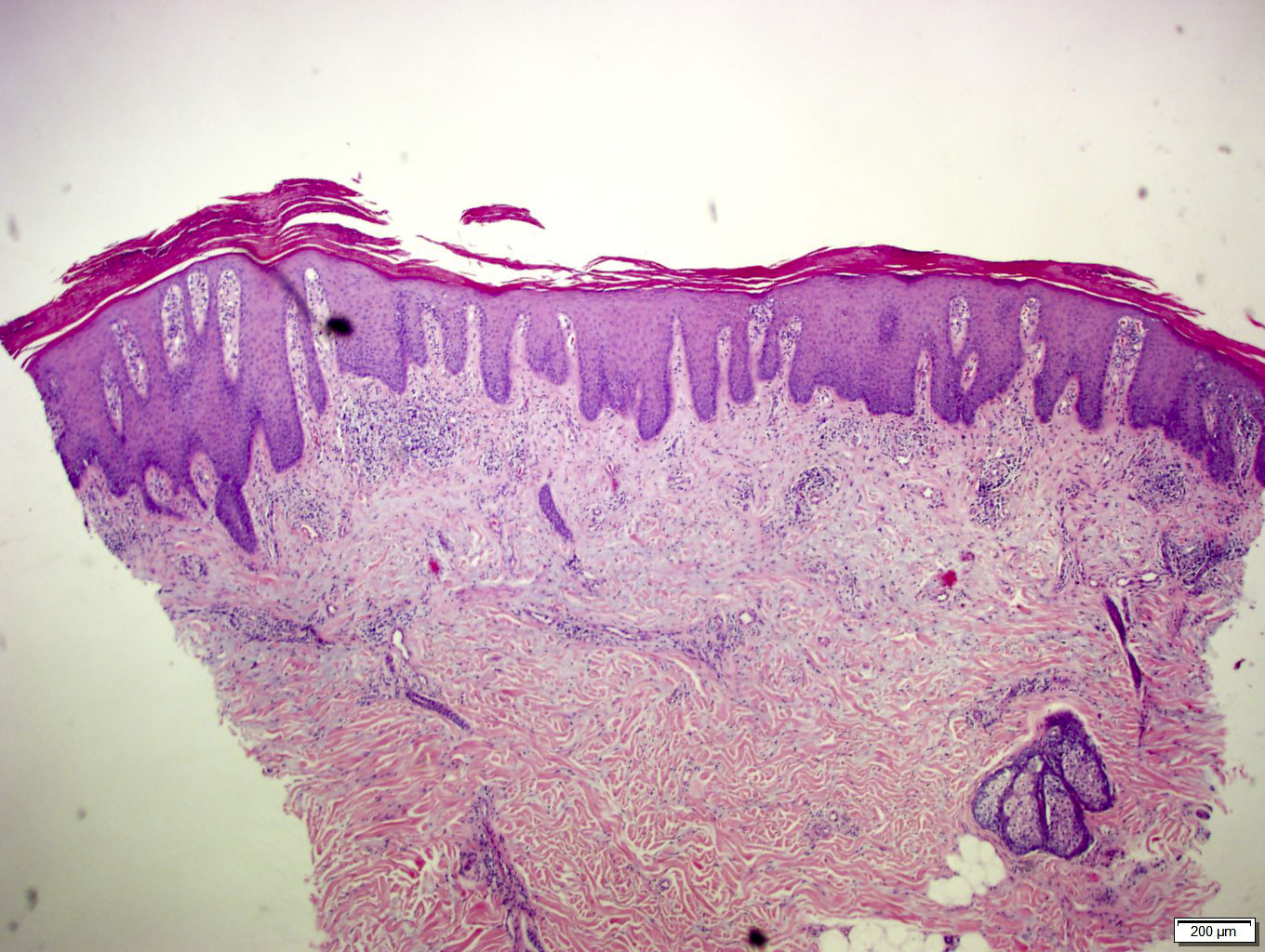
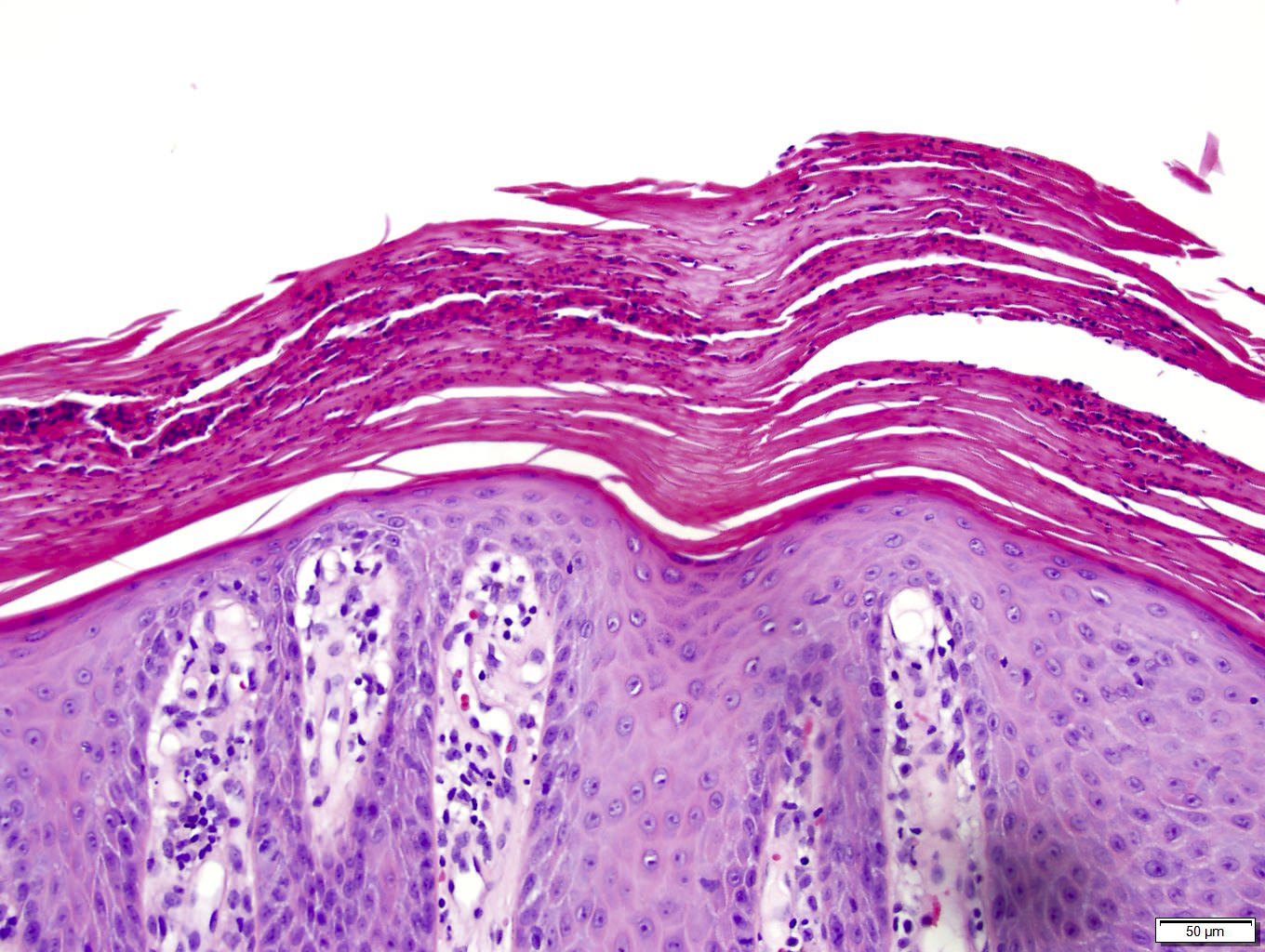
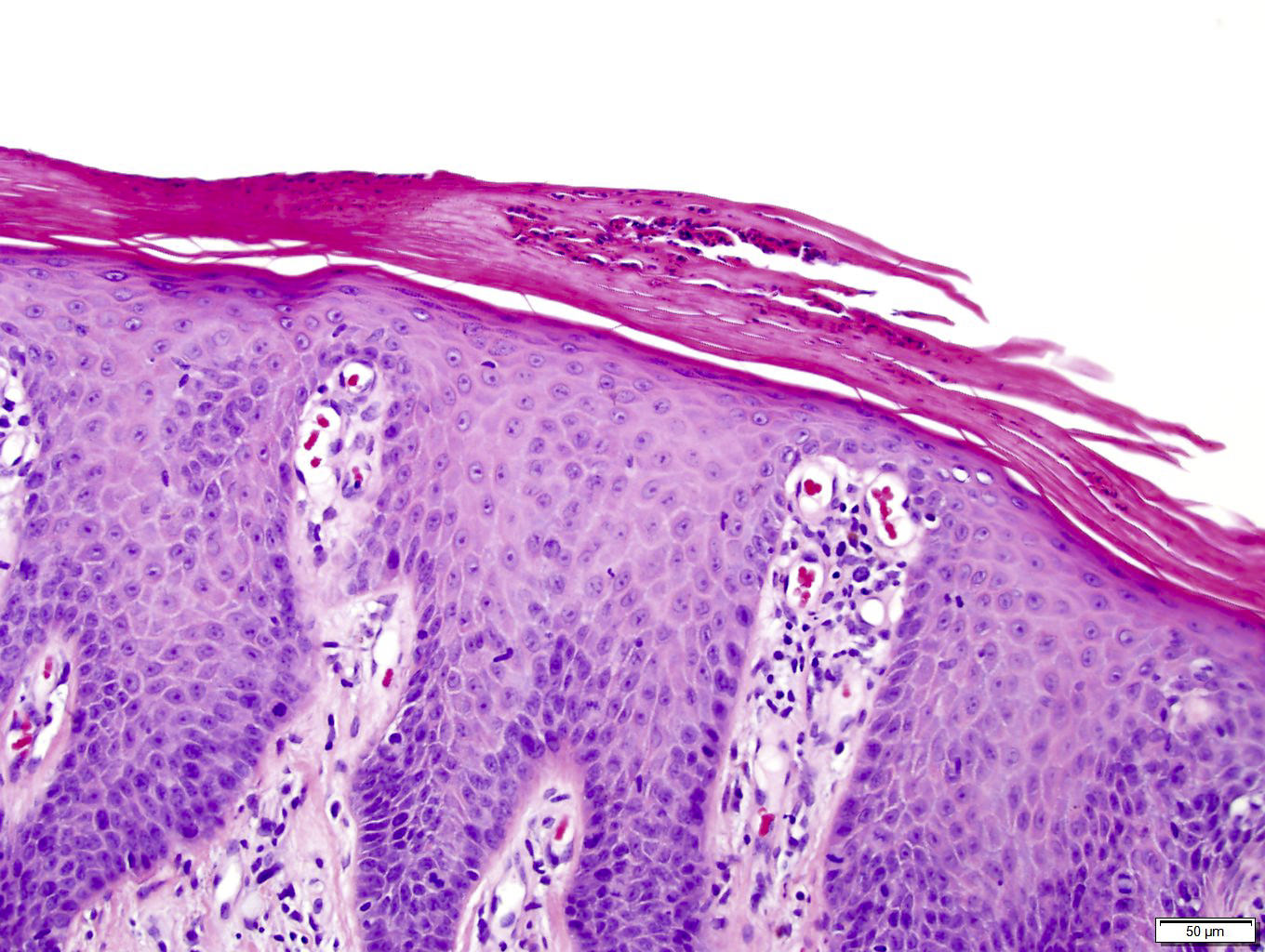
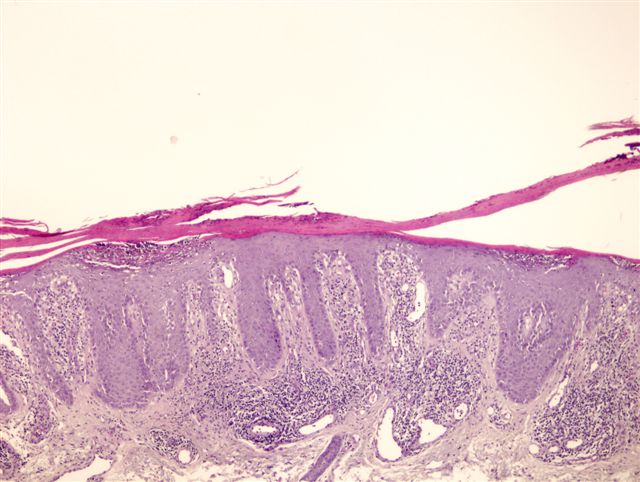
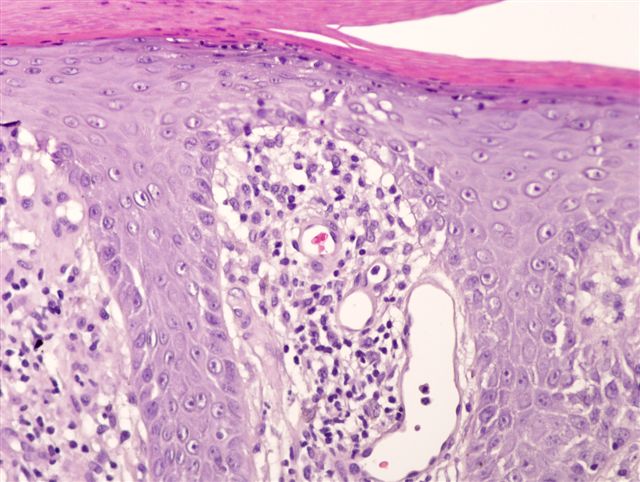
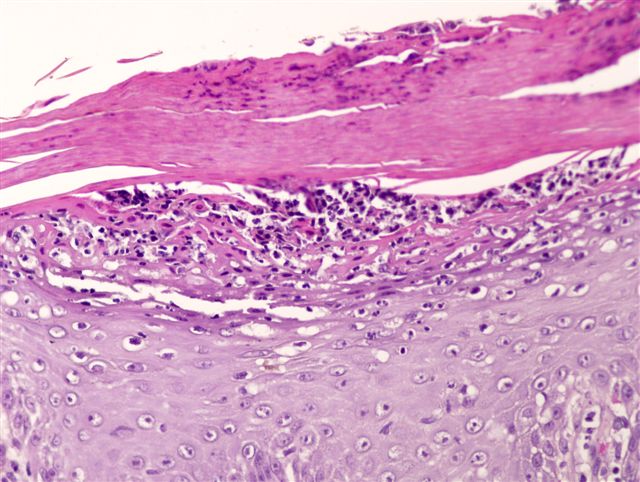
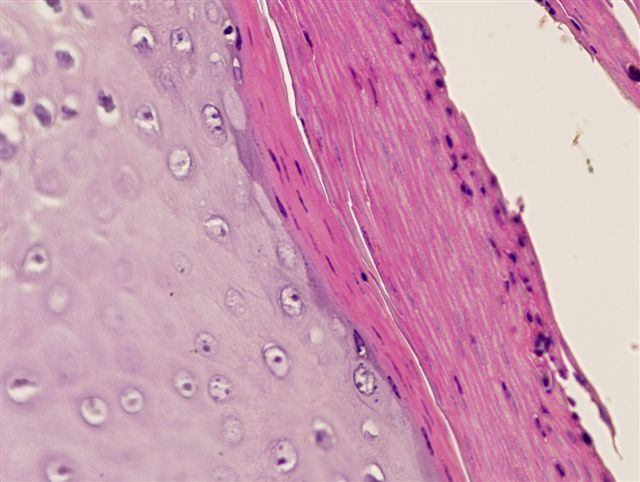
Microscopic (histologic) description
- Regular acanthosis, often with elongated rete (psoriasiform)
- Alternating zones of hypo and hypergranulosis in the epidermis
- Thinning of the suprapapillary plates
- Areas of parakeratosis in the stratum corneum with mounds of neutrophils (Munro microabscesses)
- Perivascular, predominantly lymphocytic infiltrate in the upper and middle portions of the dermis; few neutrophils or eosinophils may be seen
- Collections of neutrophils in the spinosum (spongiosiform pustules of Kogoj)
- Dilated and tortuous vessels in the dermal papillae
- Focal spongiosis may be present in the evolving lesions, intertriginous, acral and scalp variants
- Subcorneal pustules in the pustular forms of psoriasis
Microscopic (histologic) images
Immunofluorescence description
- Direct and indirect immunofluorescence are negative
Videos
Psoriasis: clinical presentation, histopathology and differential diagnosis
Sample pathology report
- Skin, biopsy:
- Psoriasiform dermatosis, suggestive for / consistent with psoriasis (see comment)
- Comment: Biopsy examination demonstrates a regular psoriasiform acanthosis of the epidermis. There is a mild inflammatory perivascular and interstitial infiltrate composed predominantly of lymphocytes. Thinning of suprapapillary plates, widened vessels in the superficial dermis and collections of neutrophils in the stratum corneum were noted. No fungal elements were identified with PAS stain.
- Overall, the histopathological features are consistent with psoriasis but only in appropriate clinical setting; psoriasiform drug eruptions may be indistinguishable.
Differential diagnosis
- Subacute spongiotic processes (atopic dermatitis, nummular dermatitis, contact dermatitis, dyshidrotic eczema):
- More prominent spongiosis
- Sometimes abundant eosinophils in the infiltrate
- Seborrheic dermatitis:
- Spongiosis, mounds of parakeratosis at the follicular ostia
- In some instances, differentiation is not possible
- Pityriasis rosea:
- Foci of spongiosis with small mounds of parakeratosis in the overlying stratum corneum
- Herald patch may have acanthosis
- Psoriasiform drug eruption:
- May be indistinguishable, greater number of eosinophils may be present
- Pityriasis rubra pilaris (Am J Dermatopathol 2019;41:37):
- Alternating areas of ortho and parakeratosis vertically and horizontally in the stratum corneum (checkerboard pattern)
- Acantholysis may be present
- Lichen simplex chronicus:
- Presence of vertical collagen bundles in the papillary dermis
- No significant parakeratosis and collections of neutrophils in the stratun corneum
- Inflammatory linear verrucous epidermal nevus (ILVEN):
- Vertically alternating areas of ortho and parakeratosis in the stratum corneum with orthokeratotic areas overlying epidermal hypergranulosis and parakeratosis overlying hypogranulosis
- No neutrophilic collections in the stratum corneum nor the epidermis
- Porokeratosis ptychotropica:
- Presence of cornoid lamellae and dyskeratotic cells
- Fungal infections:
- Nutritional dermatosis:
- May have variable findings
- In classical cases, a pallor of the superficial epidermis is seen
- Clear cell acanthoma:
- Usually a solitary lesion
- Sharp demarcation between normal epidermis and clear cell areas
- Pustular psoriasis:
- Acute generalized exanthematous pustulosis (AGEP):
- May have similar findings but with larger amount of eosinophils
- Bullous impetigo:
- May be very similar
- Clinical correlation is required
- Bacteria may be found in the intact bullas
- Pemphigus foliaceus or IgA pemphigus:
- May be indistinguishable
- Acantholytic cells may be present
- Direct immunofluorescence is required if suspected
- Acute generalized exanthematous pustulosis (AGEP):
- Mycosis fungoides:
- Epidermotropism, folliculotropism or syringotropism (tropism to eccrine glands)
- Lymphocytes display atypical features (irregular contours, hyperchromasia, sometimes enlarged, etc.)
- Presence of neutrophils in the stratum corneum is rare
- Presence of thickened collagen bundles in the superficial dermis
- Sezary syndrome:
- May be indistinguishable unless clear history and histopathological features of psoriasis are present
Practice question #1
What are the expected histopathological features of this condition?
- Regular psoriasiform acanthosis with subcorneal neutrophilic collections, PAS stain negative
- Regular psoriasiform acanthosis with subcorneal neutrophilic collections, PAS stain positive
- Irregular psoriasiform acanthosis with spongiosis
- Perifollicular pustules
- Intraepidermal bullae filled with neutrophils
Practice answer #1
A. The image demonstrates pustular psoriasis. Histopathological features of pustular psoriasis include regular psoriasiform acanthosis with subcorneal neutrophilic collections. PAS stain is negative. Positive PAS staining is seen in fungal infections (answer B). Spongiosis, although may be focally seen in psoriasis, is more typical for eczematous conditions (answer C). Pustules in pustular psoriasis are not perifollicular (answer D). Intraepidermal bullae are not seen in psoriasis (answer E).
Comment Here
Reference: Psoriasis
Comment Here
Reference: Psoriasis
Practice question #2
A patient was treated for onychomycosis with a systemic medication and developed a rash. Biopsy of the rash demonstrated regular psoriasiform acanthosis, parakeratosis with neutrophils in the stratum corneum, thinning of parapapillary plated with dilated vessels in the superficial dermis. What was the most likely medication causing this condition?
- Griseofulvin
- Voriconazole
- Terbinafine
- Itraconazole
- Fluconazole
Practice answer #2
C. The vignette describes psoriasis that started after administration of an oral antifungal agent. Terbinafine is known to exacerbate psoriasis. This side effect is not typical for griseofulvin (answer A) and azoles (voriconazole, itraconazole or fluconazole - answers B, D and E).
Comment Here
Reference: Psoriasis
Comment Here
Reference: Psoriasis
Practice question #3
What histopathological feature is helpful in differentiating psoriasis versus inflammatory linear verrucous epidermal nevus?
- Presence of spongiosis
- Presence of lichenoid infiltrate
- Presence of eosinophils in the inflammatory infiltrate
- Erythrocyte extravasates
- Alternating orthokeratosis with parakeratosis
Practice answer #3
E. Alternating orthokeratosis with parakeratosis is the most specific sign that helps to differentiate ILVEN with psoriasis. Focal areas of spongiosis and erythrocyte extravasates may be seen in both conditions but these features are not specific. Eosinophils and lichenoid infiltrate are not typical for ILVEN and psoriasis.
Comment Here
Reference: Psoriasis
Comment Here
Reference: Psoriasis