Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Vanderbeck K, Torres-Cabala CA. Acral melanoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticacrallentiginous.html. Accessed August 26th, 2025.
Definition / general
- Acral melanoma (AM): melanoma relating to or affecting the non-hair bearing / glabrous or volar skin of the soles, palms and digits as well as the nail apparatus
Essential features
- Occurs in nail apparatus as well as on volar surfaces of feet and hands (Cancer 1980;46:2492)
- Multiple histologic subtypes, including acral lentiginous melanoma (ALM) as well as other conventional histologic subtypes such as superficial spreading melanoma (SSM, also known as low cumulative sun damage [CSD] melanoma), nodular melanoma (NM) and desmoplastic melanoma
Terminology
- Acral lentiginous melanoma
- Nail apparatus melanoma
ICD coding
Epidemiology
- > 50% of cutaneous melanoma cases in East Asian countries (JAMA Dermatol 2013;149:1272)
- Most common type of melanoma in patients of Asian, Hispanic and African descent (BMC Cancer 2016;16:691, Arch Dermatol 2009;145:427, Mayo Clin Proc 2007;82:364)
- Subungual melanomas represent ~30% of acral melanomas (Ann Dermatol 2021;33:228, Br J Dermatol 2018;178:443)
- Rare; age adjusted incidence of 1.8 per million person years (Arch Dermatol 2009;145:427)
- Incidence is increased in older patients (mean age of onset: 63 years) (J Dermatol 2017;44:932, Br J Dermatol 2000;143:275, Arch Dermatol 2009;145:427)
Sites
- Palms, soles, digits, nail apparatus (Cancer 1980;46:2492)
- Weight bearing areas are most likely affected; heel more common than palm (N Engl J Med 2016;374:2404, Ann Dermatol 2021;33:228)
- Subungual melanoma: fingernails more common than toenails (Histopathology 2021;78:717, Ann Plast Surg 2013;71:346)
Pathophysiology
- Tumor mutation burden is decreased compared to other subtypes of melanoma while other structural aberrations, such as gene amplifications, are more commonly seen (N Engl J Med 2005;353:2135, JAAD Int 2020;1:135, Nature 2017;545:175)
- Documented amplifications include (J Natl Cancer Inst 2019;111:1068, Annu Rev Pathol 2014;9:239, Nature 2017;545:175, JAAD Int 2020;1:135)
- CCND1
- CDK4
- nTERT
- PAK1
- GAB2
- EP300
- YAP1
- MDM2 loci
- Mitogen activating protein kinase pathway (MAPK pathway) aberrations can be seen in some cases, specifically in BRAF, NRAS, KIT, NF1
- PTEN and CDKN2A deletions in ~25% of cases (Nature 2017;545:175)
- SPRED1 rearrangements in subungual melanomas are more common versus other locations (Nat Commun 2020;11:5259)
Etiology
- Trauma and physical stress play a potential role (Ann Dermatol 2021;33:228)
- Other factors including family history and ultraviolet (UV) radiation exposure are minimally involved (Genome Res 2017;27:524, Br J Dermatol 2006;155:561)
Clinical features
- Acral lentiginous melanoma is the most common subtype
- Typically starts as a pigmented macule and progresses to invasive melanoma over several months to years
- Subungual melanomas begin as a longitudinal discoloration referred to as longitudinal melanonychia, with progression to involve adjacent skin; clinical extension of pigmentation onto adjacent skin is called Hutchinson sign (Histopathology 2021;78:717, J Am Acad Dermatol 2015;73:213, J Natl Cancer Inst 2019;111:1068, N Engl J Med 2011;364:e38)
- Often advanced at diagnosis because hyperkeratotic epidermis overlies and hides primary lesion (J Am Acad Dermatol 2003;48:183)
- May evolve slowly over years; mean is 1 year to diagnosis (J Foot Ankle Res 2008;1:11)
- Rarely multiple (Dermatol Surg 2007;33:1)
- Median disease free survival is 10 years (Br J Dermatol 2006;155:561)
- Dermoscopy
- May have parallel ridge pattern (band-like pigmentation on ridges of skin markings is specific)
- Irregular pigmentation with variable shades (J Dermatol 2011;38:25)
Diagnosis
- Clinical presentation
- Definitive diagnosis is made on biopsy or excisional specimen through histologic examination
Prognostic factors
- Breslow thickness, ulceration, high mitotic rate, microsatellites (Br J Dermatol 2007;157:311)
- Positive sentinel lymph nodes are the most important factor for recurrence (Am J Surg 2012;204:874)
- Increased locoregional recurrence rate compared to other melanoma subtypes
- Worse survival rate than other melanoma subtypes (J Natl Compr Canc Netw 2014;12:1706)
Case reports
- 42 year old woman with lesion initially treated as plantar wart (Dermatol Online J 2006;12:3)
- 61 year old man with an amelanotic melanoma (Mol Clin Oncol 2020;13:59)
- 67 year old man with acral amelanotic melanoma with appearance of ulcer (Cureus 2022;14:e26615)
- 73 year old woman with acral melanoma clinically suspected of being mycotic intertrigo (Int Wound J 2020;17:1532)
- 74 year old man with in situ ALM which progressed to invasion (Ann Dermatol 2009;21:185)
- 84 year old man with ALM with multiple metastases to bone (Pan Afr Med J 2023;45:141)
Clinical images
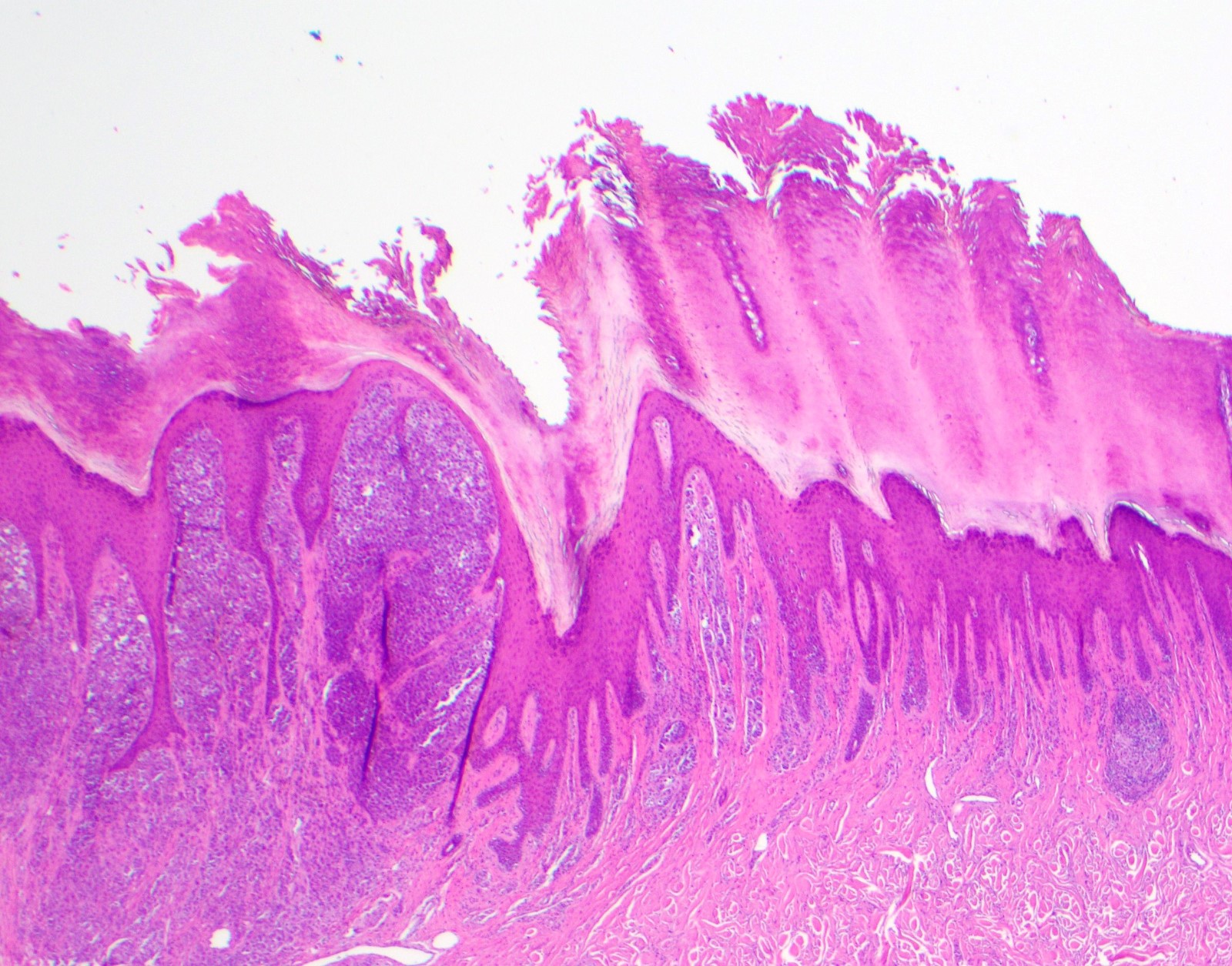
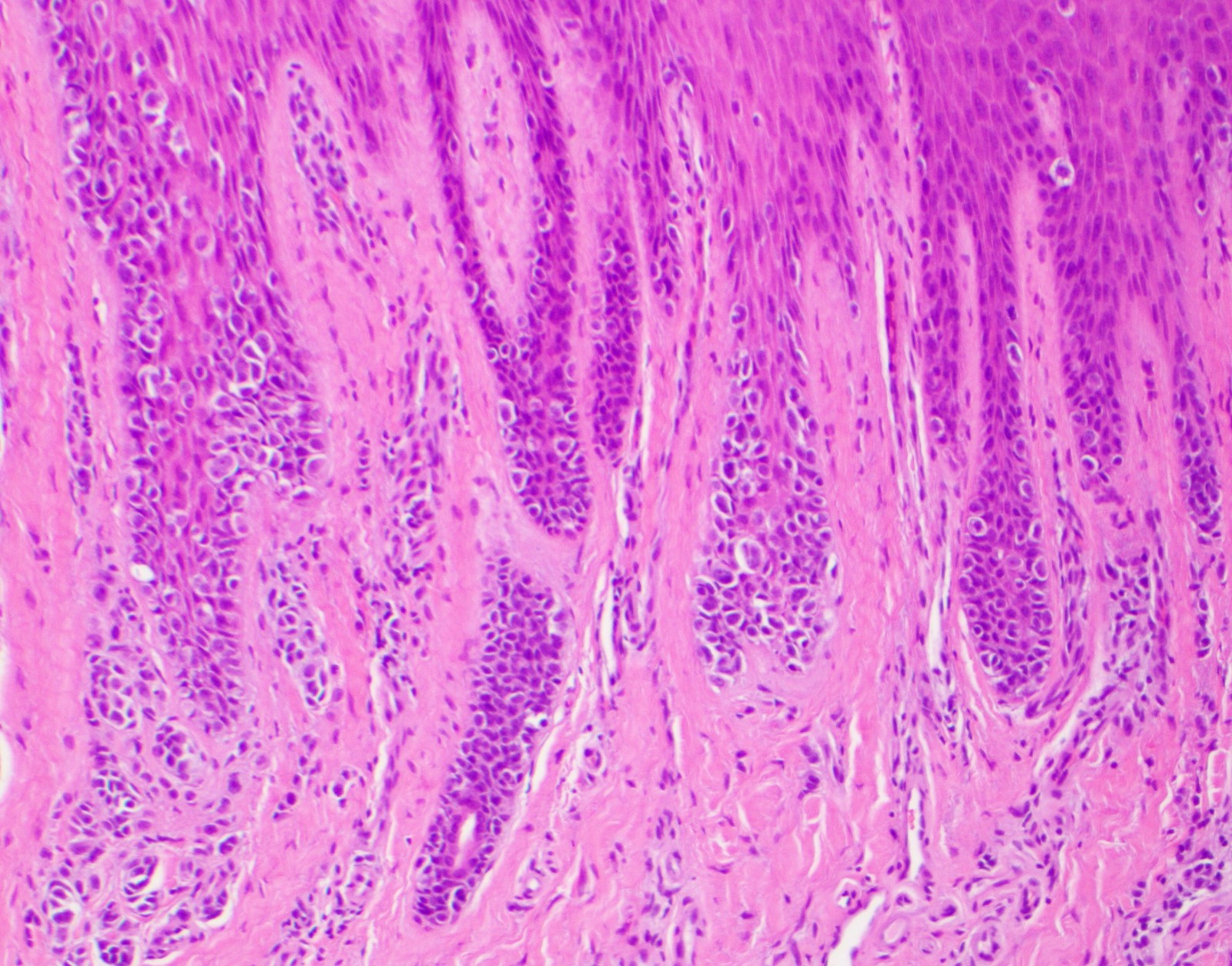
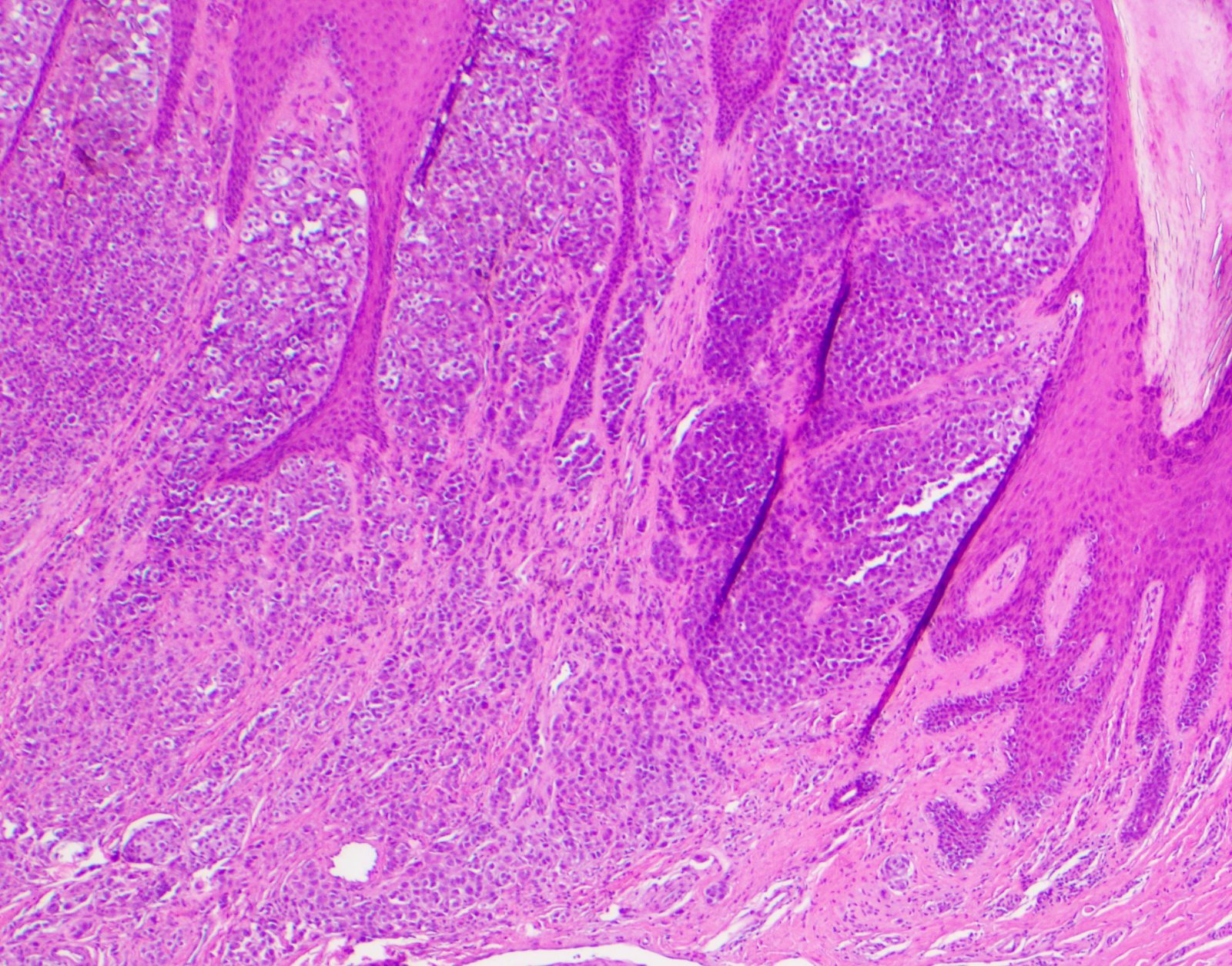
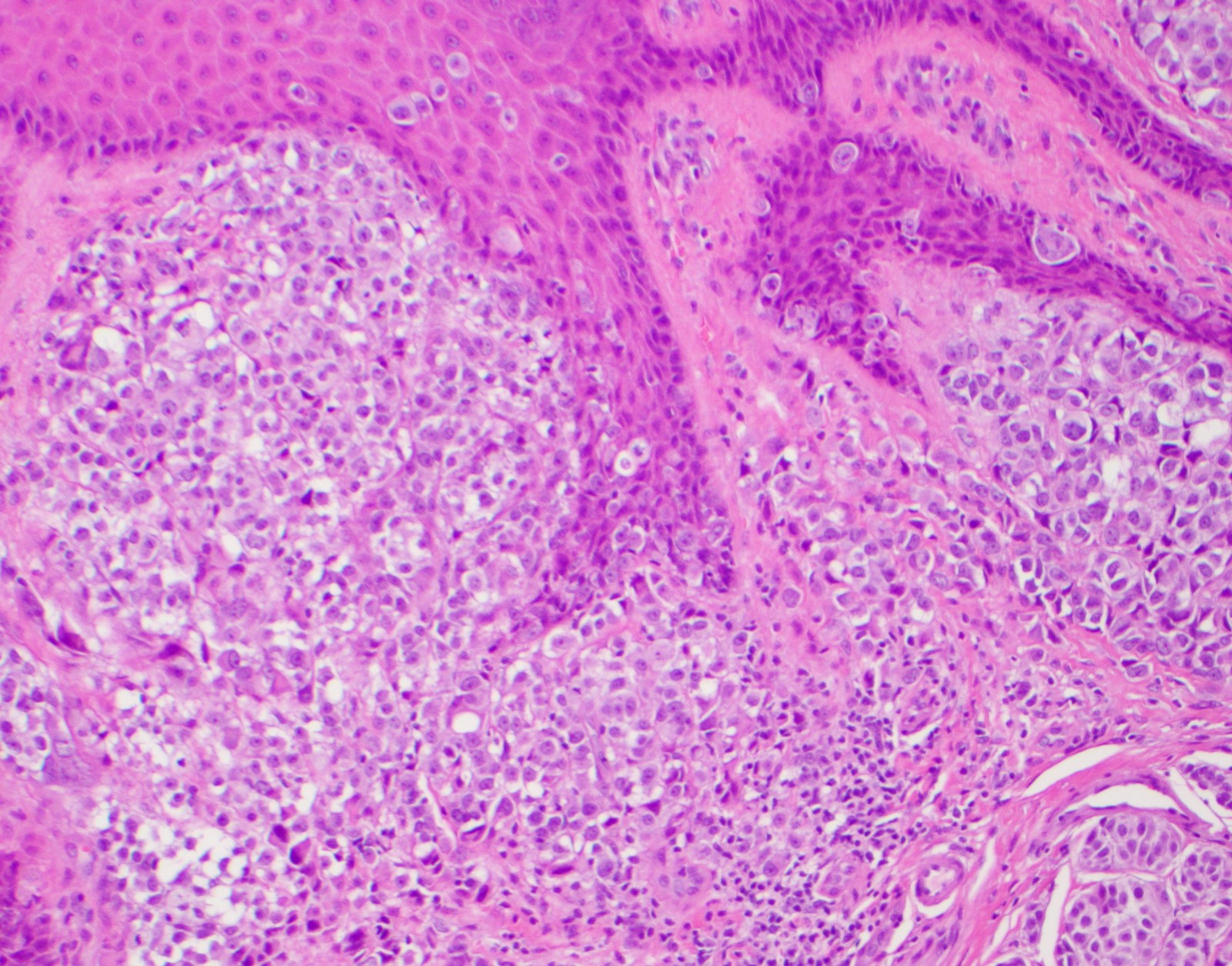
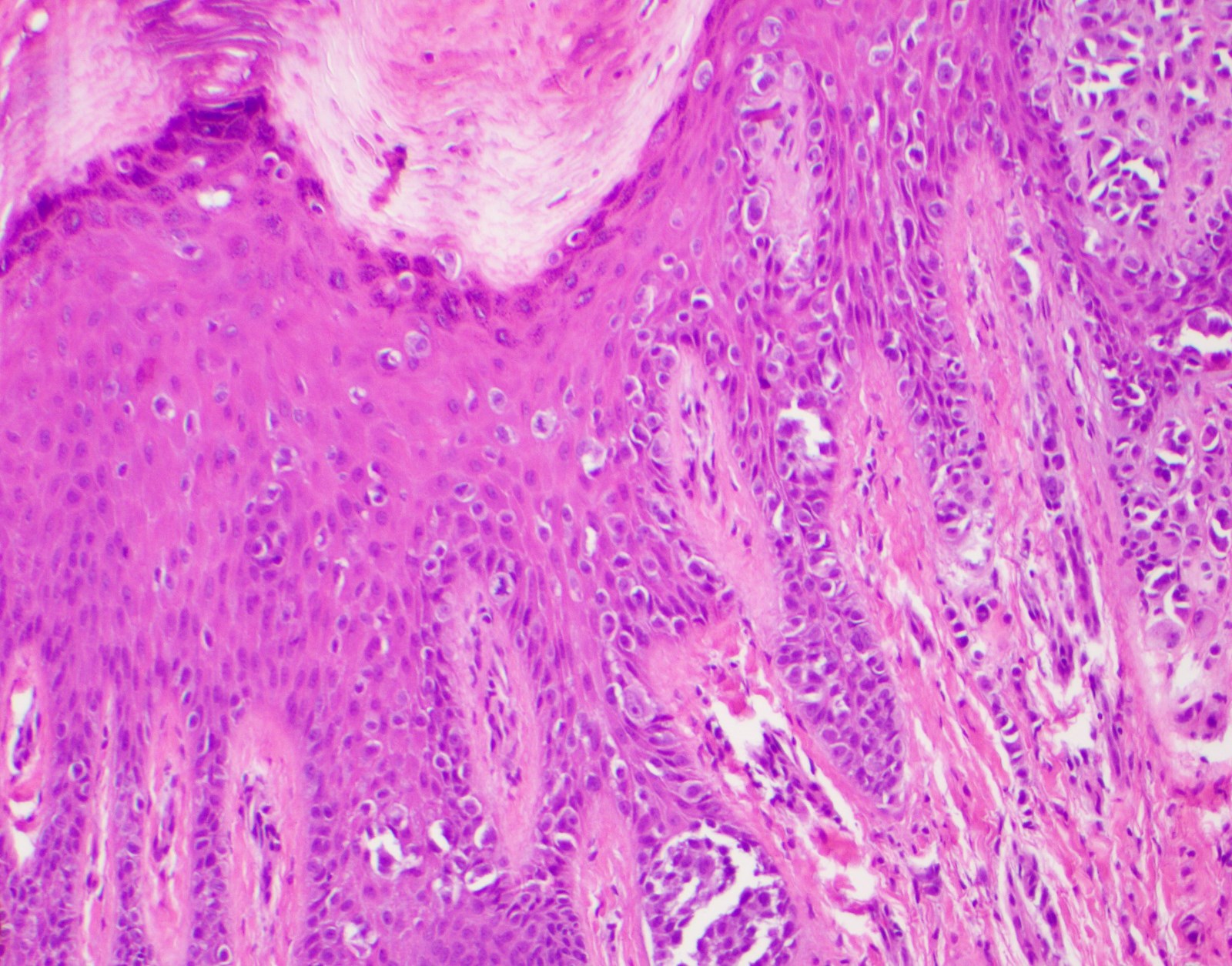
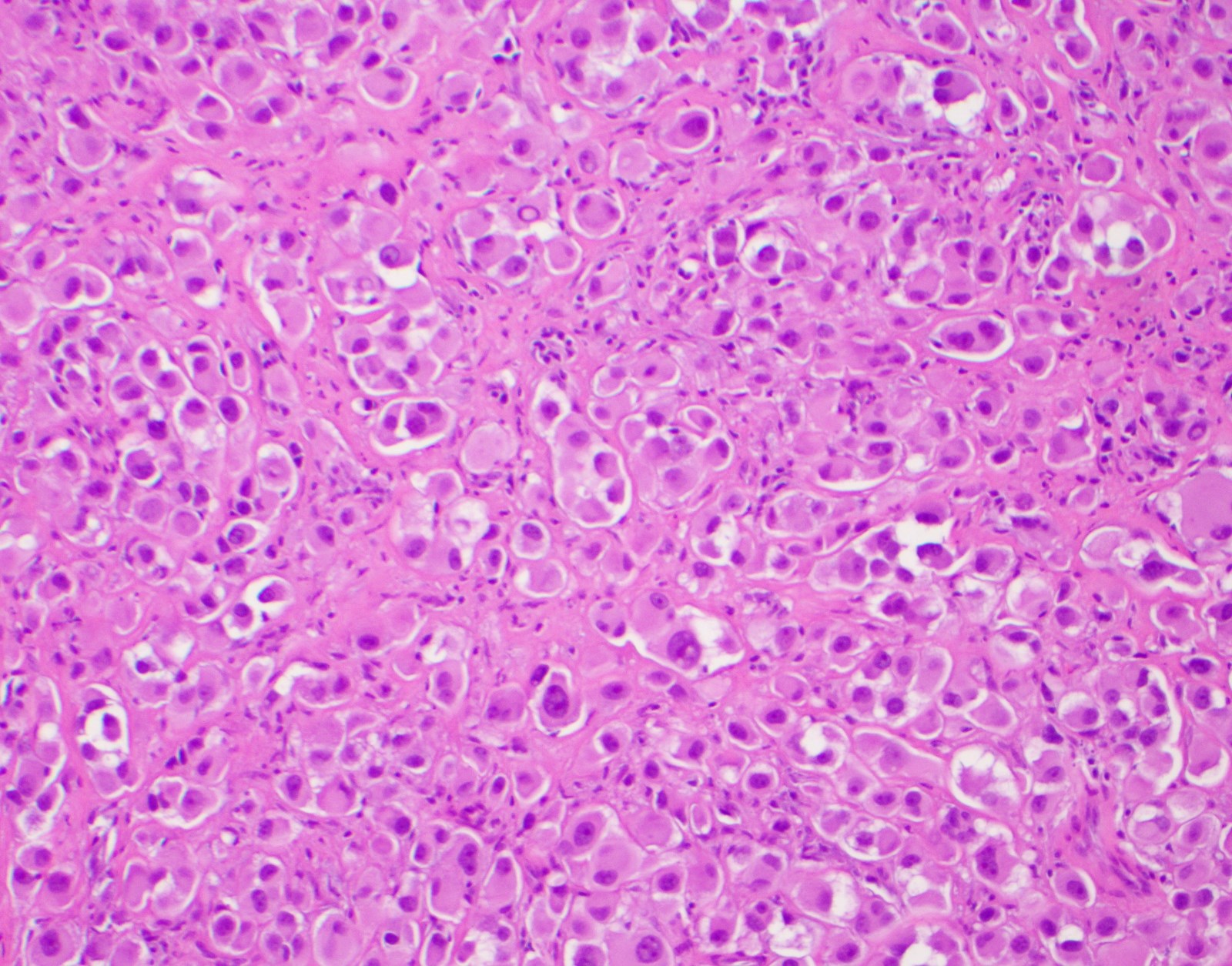
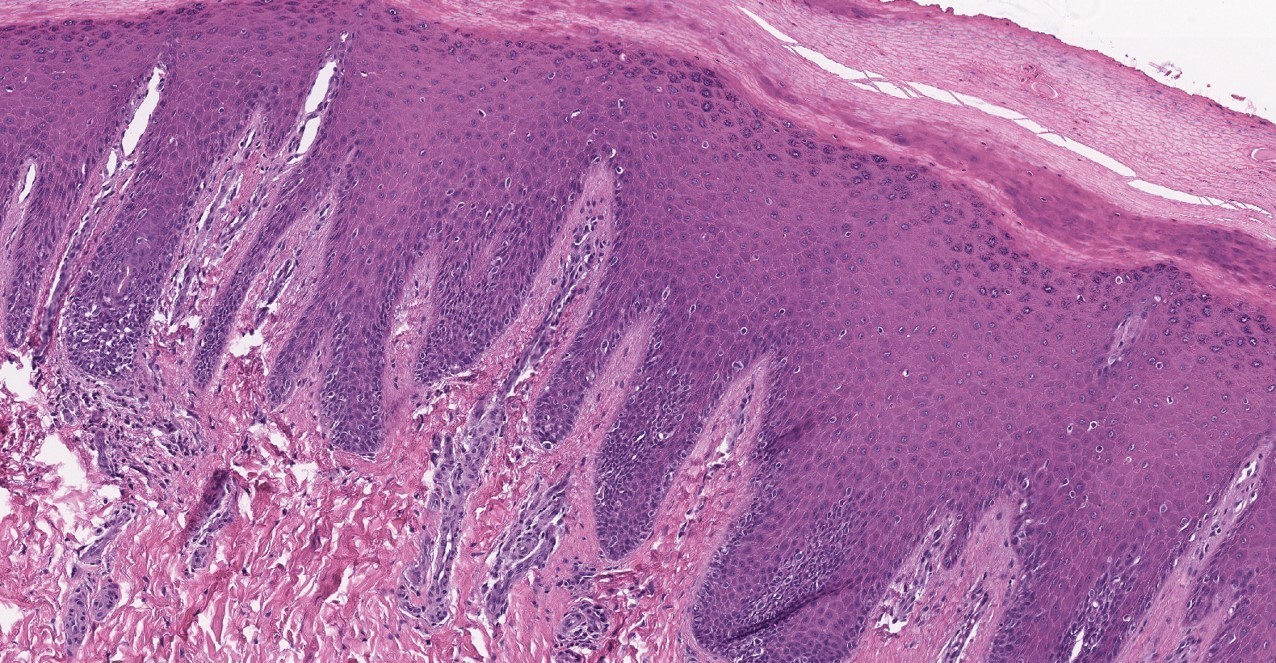
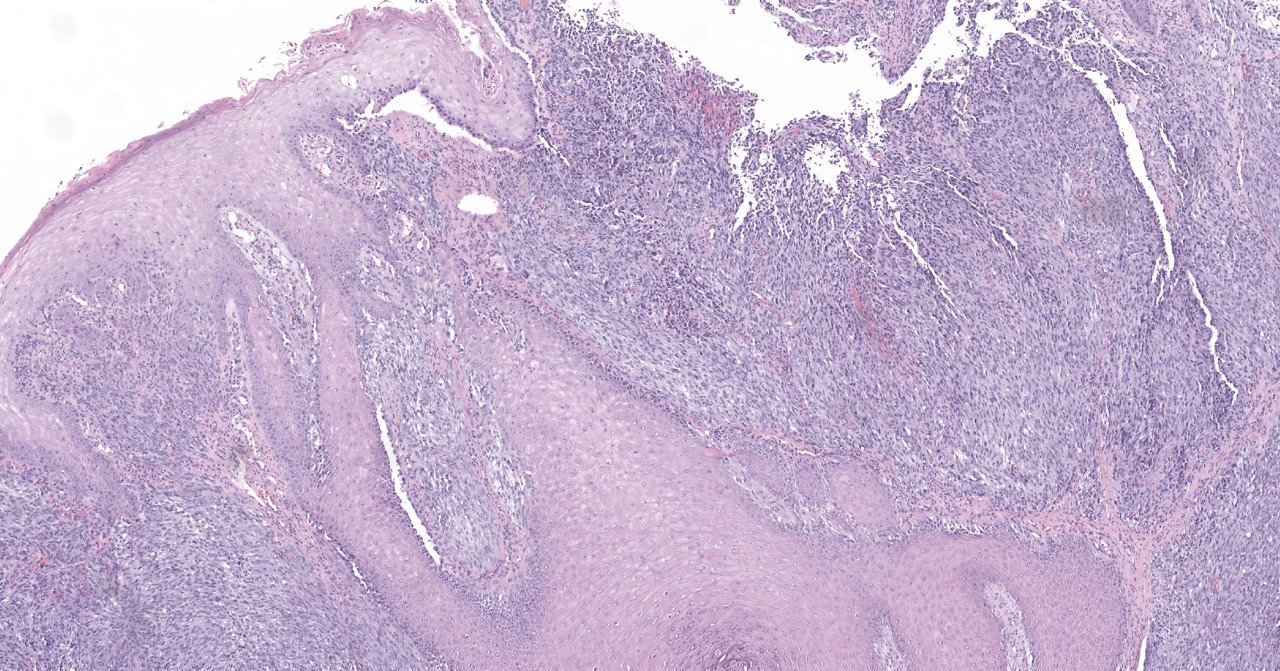
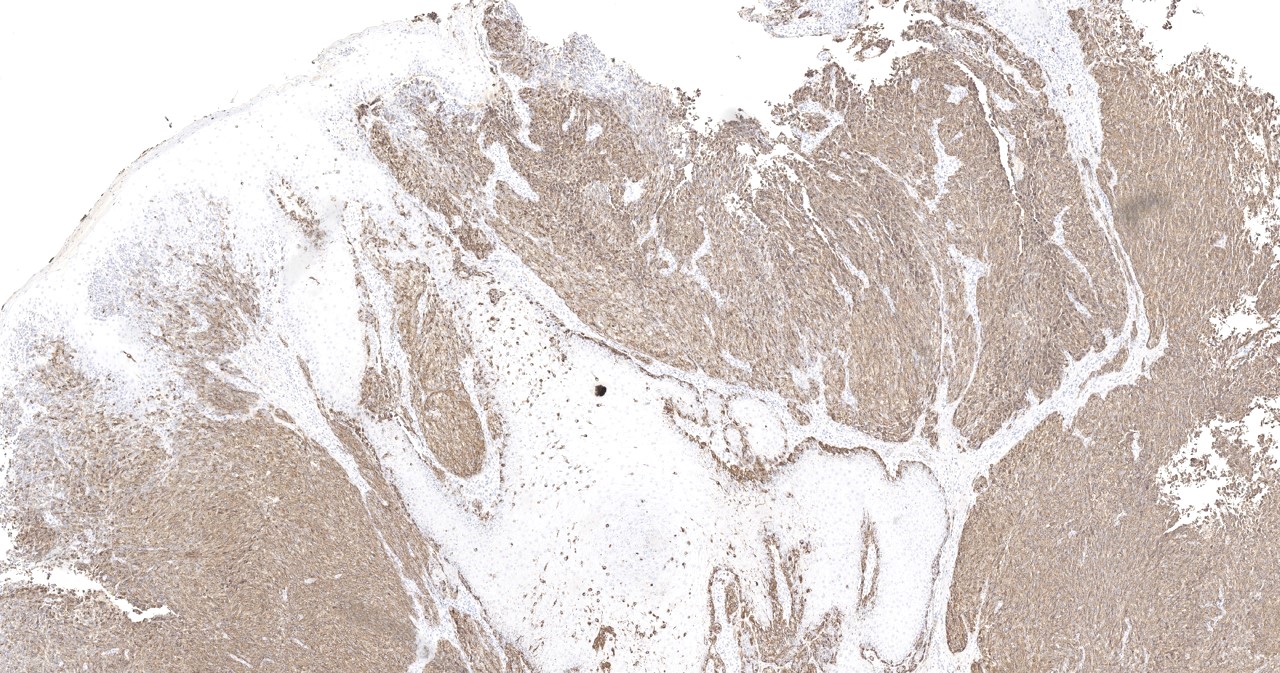
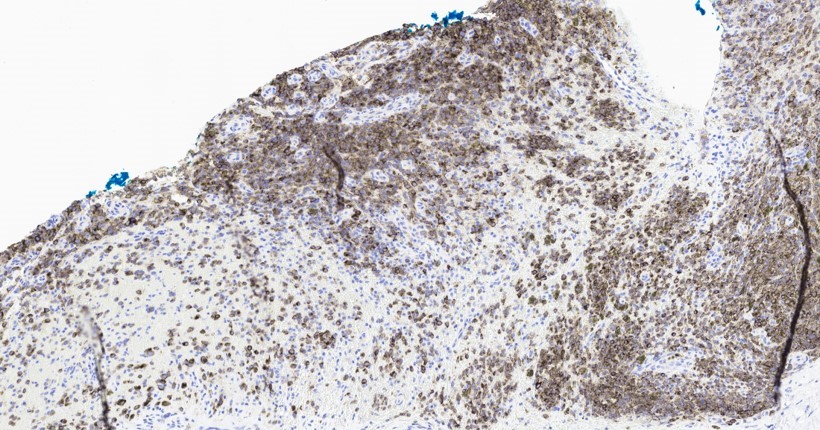
Microscopic (histologic) description
- Prominent acanthosis of epidermis with elongated rete ridges can be seen
- Pagetoid spread
- Atypical nuclei
- Increased N:C ratio
- Proliferation of melanocytes downward along eccrine ducts
- Consumption of epidermis present (attenuation of basal / suprabasal layers with rete ridge loss) (J Cutan Pathol 2012;39:577)
- Early lesions may show proliferation of solitary melanocytes in the epidermal rete ridge (crista profunda intermedia) underlying the ridge of the skin marking (Am J Dermatopathol 2006;28:21)
- Nail lesions show confluent stretches of solitary melanocytes, multinucleation, lichenoid inflammatory reaction and florid pagetoid spread (Am J Surg Pathol 2008;32:835)
- Heterologous osseocartilaginous differentiation seen more commonly in acral melanoma
- ALM is the most common histopathologic subtype, followed by NM and SSM (JAMA Dermatol 2013;149:1281, Sci Rep 2016;6:31432, Melanoma Res 2017;27:315)
- ALM
- ALM in situ demonstrates an increased number of irregularly distributed melanocytes at basal epidermis
- Variable cytologic atypia of melanocytes with hyperchromatic nuclei
- Prominent dendrites and confluent distribution of melanocytes
- Later vertical growth phase develops with invasion into dermis
- Melanocytes comprising the vertical growth phase are spindled (NF1 mutations) to epithelioid (BRAF mutations) (J Invest Dermatol 2018;138:933)
- Subungual melanoma: first demonstrates a mild proliferation of atypical melanocytes with hyperchromatic nuclei, increased N:C ratio and elongated dendrites (Am J Surg Pathol 2007;31:1902, J Dermatol 2008;35:695, J Cutan Pathol 2016;43:41)
- Important histologic features in subungual melanoma in situ include irregular and hyperchromatic nuclei and increased melanocyte count (Histopathology 2021;78:717)
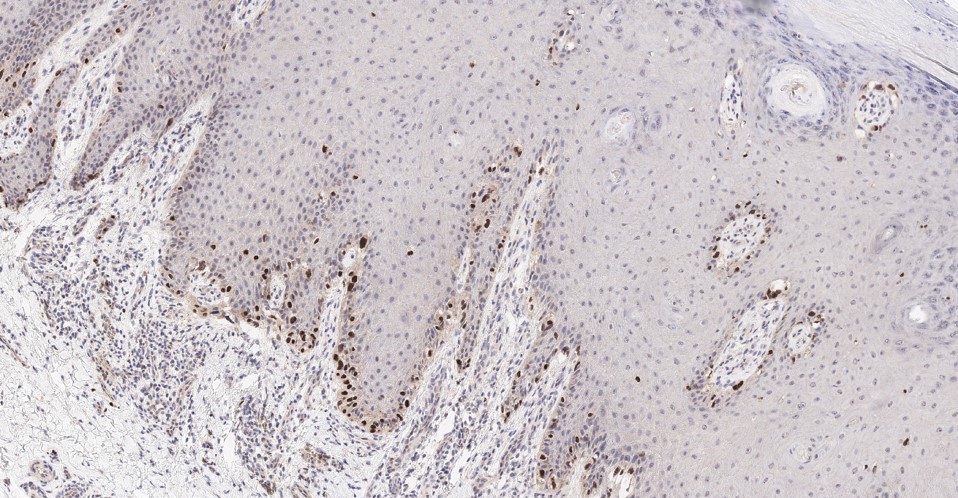
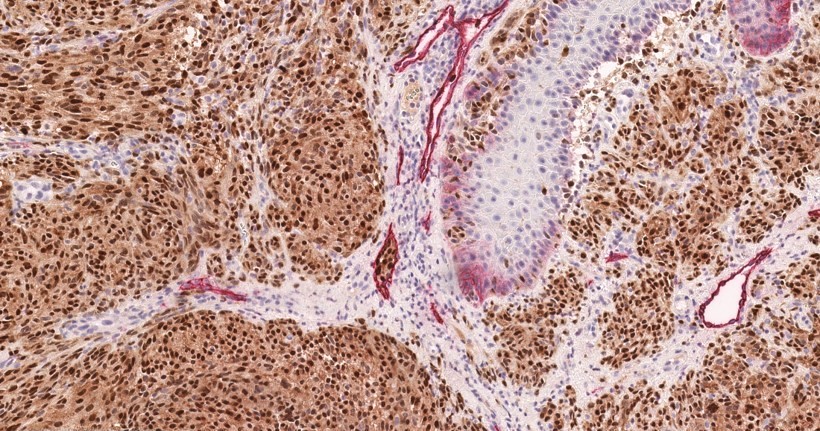
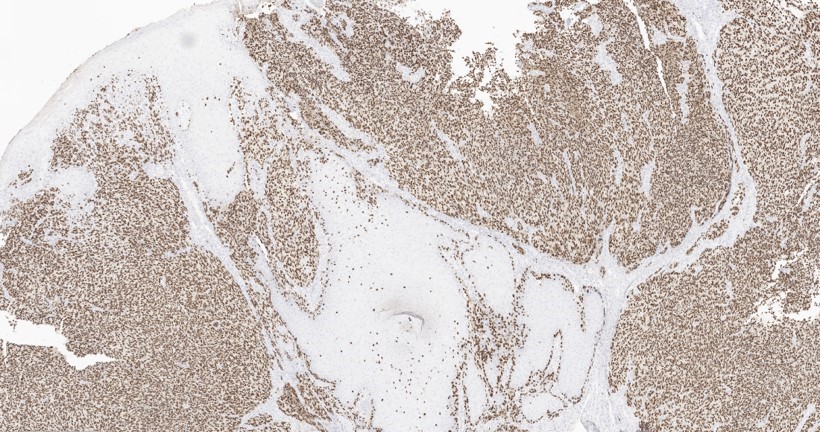
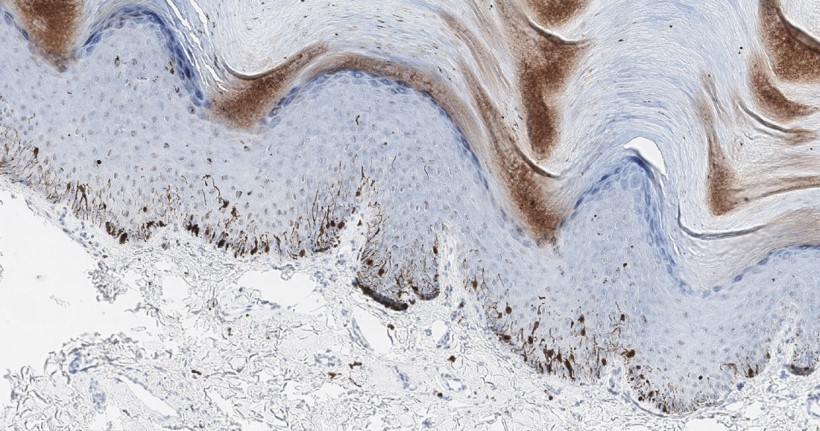
Microscopic (histologic) images
Contributed by Carlos A. Torres-Cabala, M.D.
Positive stains
- HMB45 (sometimes focal in amelanotic AM), useful to highlight long dendrites (Int J Dermatol 2003;42:123, J Am Acad Dermatol 2013;69:700)
- MelanA, SOX10, S100, MITF, PRAME (Hum Pathol 2022;120:9, J Cutan Pathol 2022;49:220, Am J Surg Pathol 2018;42:1456)
- Cyclin D1: if positive, it is supportive of melanoma
- Immunohistochemistry is not always required for diagnosis
Molecular / cytogenetics description
- BRAF p. V600E mutations predominate in patients of European descent (Exp Dermatol 2017;26:883)
- ALMs demonstrate frequent amplifications, deletions and structural rearrangement, yet mutational burden is low relative to other melanoma subtypes (N Engl J Med 2005;353:2135, Nature 2017;545:175)
- ALMs often demonstrate triple negative (BRAF, NRAS, KIT negative) pattern; ALMs generally develop from genetic amplifications de novo (Cancer Res 2000;60:1968)
- BRAF mutations are more common in low CSD / superficial spreading melanomas of acral sites; may be associated with pre-existing nevus (J Invest Dermatol 2018;138:933, JAMA Dermatol 2021;157:831)
- NRAS mutations are more common in nodular melanomas of acral sites (J Invest Dermatol 2018;138:933)
- Cyclin D1 protein expression, characterized via molecular studies (or immunohistochemistry) is associated with increased CCDN1 copy number in acral melanoma (Diagn Pathol 2021;16:60)
Sample pathology report
- Skin, right toe, punch biopsy:
- Invasive melanoma, acral lentiginous type (see comment)
- Tumor thickness (Breslow): at least 0.9 mm
- Clark level: at least IV
- Ulceration: present (0.2 mm width)
- Regression: not identified
- Mitotic count: 1/mm2
- Tumor infiltrating lymphocytes: present, nonbrisk
- Lymphovascular invasion: not identified
- Perineural invasion: not identified
- Tissue edges: melanoma present at deep and peripheral tissue edges
- Comment: Sections show skin and subcutis with a cellular and atypical compound melanocytic proliferation that extends to deep and peripheral tissue edges. Confluence of atypical melanocytes is appreciated at the dermoepidermal junction. Pagetoid spread is also readily seen. Cytologically, the melanocytes are epithelioid to spindled with abundant intracytoplasmic melanin pigment. These melanocytes have atypical and enlarged nuclei with readily identifiable mitotic figures within the dermal component. By immunohistochemistry, the tumor cells are positive for MelanA, HMB45, S100, SOX10 and PRAME. Overall, the findings are supportive of the above interpretation. Correlation with the subsequent excisional specimen is recommended for further definite staging information and classification.
Differential diagnosis
- Acral lentiginous melanocytic nevi:
- ALM and nevi with pagetoid scatter are difficult to differentiate
- Acral nevi:
- Melanocytes have less hyperchromatic and irregular nuclei
- Melanocytes appear smaller in acral nevi with mitotic activity rare or absent
- Inflammation and confluence of melanocytes at dermoepidermal junction are less common with acral nevi
- Patient demographics, including age, size, clinical appearance, dermoscopic impressions, are required for diagnosis
- In compound nevi, maturation of melanocytes is seen with descent
- Acral nevi tend to be negative for PRAME and, if compound, to show decreased expression of HMB45 and LEF1 with descent (Mod Pathol 2020;33:2067)
- Acral melanoma is more likely to be positive for cyclin D1 than acral nevi (Diagn Pathol 2021;16:60)
- Acral lentiginous nevus:
- Predominantly junctional growth pattern with melanocytes arranged in nests of single cells along basal layer of the epidermis, giving a lentiginous appearance
- Mild to moderate cytologic atypia; this cytologic atypia is less than that seen with ALM
- Some cases may demonstrate pagetoid spread (see MANIAC below); typically lack significant dermal involvement
- Compound acral nevus:
- Junctional component demonstrates melanocytes in nests and single cells along the basal layer of the epidermis with mild to moderate cytologic atypia; this cytologic atypia is less that that seen in acral melanoma
- Some cases may demonstrate pagetoid spread
- Dermal component demonstrates melanocytes in nests that are surrounded by fibroblasts and collagen fibers, typically without sclerosis, desmoplasia or significant inflammatory reaction (as in melanoma)
- Melanocytes demonstrate maturation with depth within the dermis
- Melanocytic acral nevus with intraepithelial ascent of cells, variant of acral nevus (MANIAC), also known as lentiginous nevus with upward migration of melanocytes:
- Defining feature of the variant is the presence of upward migration of melanocytes from the basal layer into the overlying epithelium
- Pagetoid spread is most often seen toward the center of the lesion
- This nevus otherwise demonstrates a predominantly junctional growth pattern with mild to moderate cytologic atypia; the cytologic atypia is typically less than that expected with ALM
- Dermal component can be seen in these nevi; if dermal component is present, maturation of melanocytes with depth is observed and mitotic activity is usually rare or absent (see compound acral nevus above)
- Other clinically relevant diagnostic considerations include the following
- Fibroma:
- Well circumscribed proliferation of spindled fibroblasts in collagenous stroma
- There is an absence of a melanocytic proliferation
- Fibroblasts are cytologically bland
- Subungual hematoma:
- Often demonstrate pigmentation clinically; examination demonstrates hemorrhage, hemosiderin, hemosiderin laden macrophages
- There is an absence of a melanocytic proliferation
- Verruca:
- Hyperkeratosis, epidermal hyperplasia, papillomatosis and hypergranulosis
- Koilocytic / viral cytopathic change appreciated within keratinocytes
- Dilated capillaries may also be seen within superficial dermis
- Squamous cell carcinoma:
- Atypical and invasive squamous proliferation with increased mitotic activity and cytologic atypia
- Pyogenic granuloma:
- Relatively bland vascular proliferation with superficial vessels
- Predominantly lobular configuration of vessels
- Overlying epidermal hyperplasia
- Lentigo:
- Increased (melanin) pigmentation within predominantly basal layer of epidermis without an increase in melanocytes
- Melanocytic proliferation appears absent
- Fibroma:
Additional references
Practice question #1
Practice answer #1
A. Acral melanoma. The images demonstrate an atypical compound melanocytic proliferation with a confluence of atypical melanocytes apparent at the dermoepidermal junction. Answer B is incorrect as the images lack benign features. The confluence of melanocytes, atypia of melanocytes with hyperchromatic, irregular and enlarged nuclei, increased N:C ratio and apparent mitotic figures are more in keeping with melanoma. Answer C is incorrect as the images do not show a wedge shaped melanocytic proliferation that is predominantly dermal. The images demonstrate marked cytologic and nuclear atypia as described that are more in keeping with melanoma versus deep penetrating nevus. Answer D is incorrect as the images demonstrate a melanocytic lesion and not a vascular lesion.
Comment Here
Reference: Acral melanoma
Comment Here
Reference: Acral melanoma
Practice question #2
What immunohistochemical profile would be expected in an acral lentiginous melanoma?
- MelanA-, SOX10+, S100+, PRAME+, HMB45+, cyclin D1-
- MelanA+, SOX10-, S100-, PRAME+, HMB45+, cyclin D1+
- MelanA+, SOX10+, S100+, PRAME-, HMB45+, cyclin D1+
- MelanA+, SOX10+, S100+, PRAME+, HMB45+, cyclin D1+
Practice answer #2
D. MelanA+, SOX10+, S100+, PRAME+, HMB45+, cyclin D1+. Via immunohistochemistry, acral lentiginous melanomas are positive for conventional melanoma markers including MelanA, SOX10, S100, PRAME and HMB45 as well as cyclin D1. Answers A, B and C are incorrect because acral lentiginous melanoma (ALM) is typically positive for all markers listed.
Comment Here
Reference: Acral melanoma
Comment Here
Reference: Acral melanoma