Table of Contents
Definition / general | Essential features | Terminology | Embryogenesis | Functional anatomy | Physiology | Diagrams / tables | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Paramaguru R, Ali RH. Histology-smooth muscle. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuesmoothmuscle.html. Accessed September 25th, 2025.
Definition / general
- Nonstriated muscle that serves diverse functions throughout the body and is responsible for involuntary movements
- 1 of 3 types of muscle tissue alongside cardiac and skeletal muscle
Essential features
- Smooth muscle is widely distributed throughout the body and serves diverse functions
- Physiologically divided into single unit and multi unit fibers
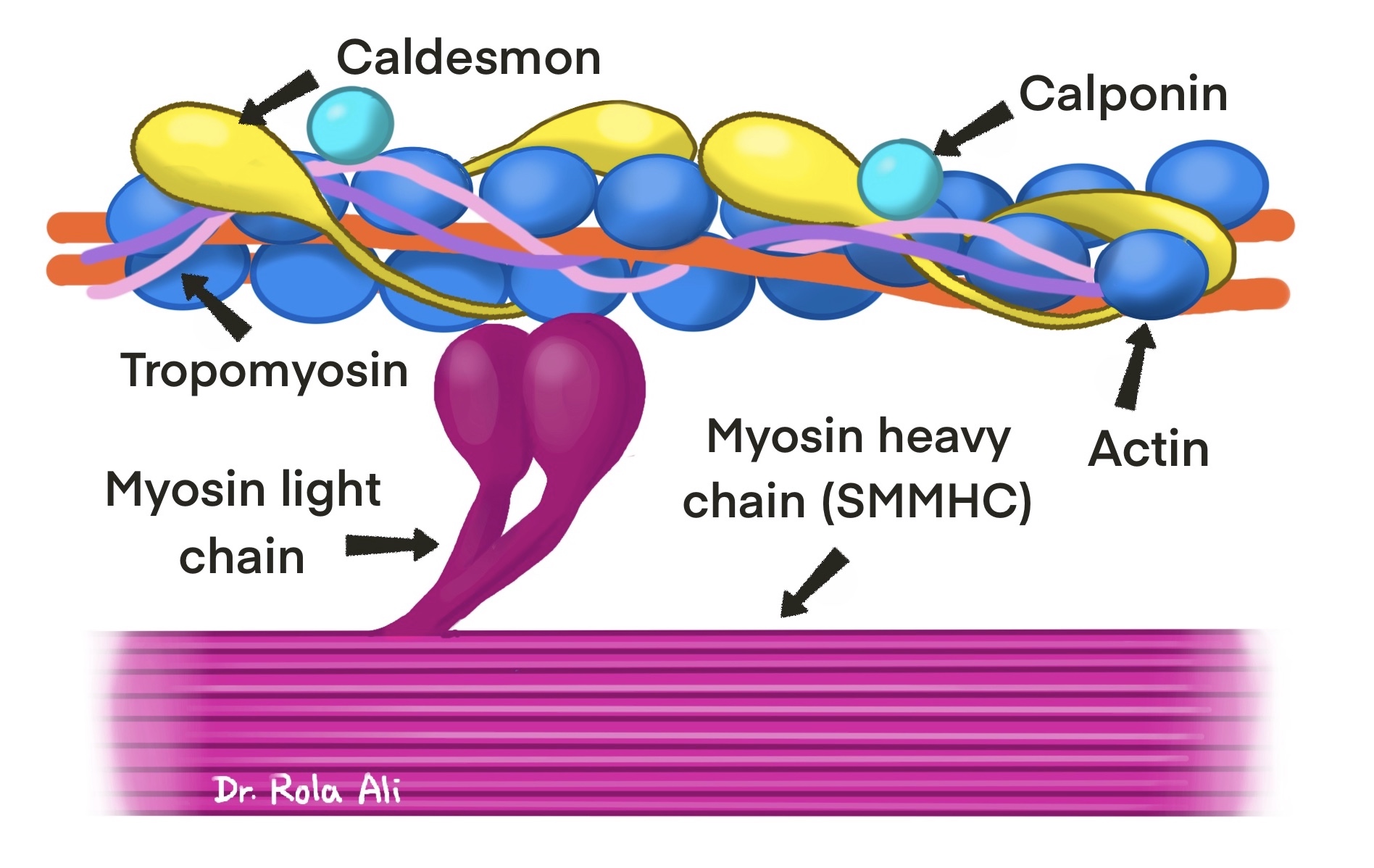
- Intracellular actin and myosin filaments generate contractile forces by a sliding filament mechanism
- Contractile filaments are not arranged into sarcomeres, thus giving it a nonstriated (smooth) appearance
- Awareness of the distribution of smooth muscle helps avoid microscopic misinterpretation
Terminology
- Synonyms: nonstriated muscle, involuntary muscle
- Smooth pertains to the lack of striations
- Muscle fiber is the basic functional unit (also known as myocyte, myofiber, muscle cell)
- Myofilaments are the contractile apparatus of smooth muscle cells consisting of thick myosin filaments and thin actin filaments along with regulatory proteins
Embryogenesis
- Smooth muscle is derived from mesoderm and neural crest cells
- Heterogeneity of smooth muscle origins in vascular development provides insights into the pathophysiology and site specific localization of some vascular disorders (e.g., atherosclerosis)
- References: StatPearls: Physiology, Smooth Muscle [Accessed 3 July 2023], Cell Mol Life Sci 2014;71:2271
Functional anatomy
- Smooth musculature is ubiquitous in viscera and blood vessels
- At certain sites, smooth and skeletal muscles come into contact coordinating the contractile force and direction with each other (e.g., esophagus, rectum and pelvic floor) (Anat Sci Int 2023;98:407)
- Muscle cell spatial arrangements (J Smooth Muscle Res 2021;57:19)
- Circumferential ring arrangement (e.g., arterioles)
- Less circumferential and not as tightly packed bundles (e.g., ureter, bile duct)
- Orthogonal layers (e.g., intestine, vas deferens, vessels)
- Cord-like (e.g., teniae coli)
- Bundles running seemingly in all directions (e.g., urinary bladder, myometrium)
- Laminar sheet (e.g., trachea)
- Short straight bundles (e.g., arrector pili)
- Contractile properties serve diverse functions based on
- Dimensions of the muscle fibers
- Spatial arrangement of the fibers (above)
- Types of stimuli
- Characteristics of innervation
- Types of intracellular filaments
- Thin actin, contractile function
- Thick myosin, contractile function
- Intermediate desmin and vimentin, maintain structure
- Visceral smooth muscle: gamma smooth muscle actin and desmin predominate
- Vascular smooth muscle: abundant alpha smooth muscle actin, vimentin > desmin (Proc Natl Acad Sci U S A 1981;78:298)
Skin
| Arrector pili muscles |
|
| Nipple |
|
| Scrotum |
|
| Vulva |
|
Eye
| Iris |
|
| Ciliary body |
|
| Müller muscle of eyelid |
|
| Orbit |
|
Cardiovascular
| Elastic arteries |
|
| Muscular arteries |
|
| Arterioles |
|
| Capillaries |
|
| Venules |
|
| Veins |
|
| Capillary pericytes |
|
| Lymphatics |
|
| Endocardium |
|
Lung
| Conducting airways |
|
| Respiratory airways |
|
Gastrointestinal
| Muscularis mucosae |
|
| Muscularis propria (externa) |
|
| Anal canal |
|
| Pelvic floor and perineum |
|
Biliary system
| Gallbladder |
|
| Extrahepatic biliary tract |
|
| Sphincter of Oddi |
|
Genitourinary
| Bladder |
|
| Ureter |
|
| Renal pelvis |
|
| Male ducts & seminal vesicles |
|
| Penis |
|
| Prostate |
|
| Urethra |
|
Female reproductive
| Uterus |
|
| Vagina |
|
| Fallopian tube |
|
| Ovary |
|
Physiology
- 2 major types of smooth muscle
- Single unit
- Hundreds to thousands of muscle fibers contract together as a single unit
- Action potential spreads through gap junctions between fibers
- Controlled by nervous and nonnervous stimuli
- Examples: walls of viscera such as gastrointestinal tract, blood vessels
- Multi unit
- Each fiber is innervated by a single nerve ending and operates independently for much finer control
- Controlled by nervous stimuli
- Examples: ciliary muscle of the eye, arrector pili muscles
- Single unit
- Types of stimuli
- Nervous: autonomic
- Nonnervous: hormones, local tissue chemical factors, stretch of the fibers (mechanical)
- Mechanism of contraction
- Initiated by an increase in intracellular Ca2+ ions upon stimulation (as in skeletal muscle)
- Mediated by actin myosin filament interaction (as in skeletal muscle)
- Does not involve troponin (unlike skeletal muscle)
- Source of Ca2+ ions
- Entry through channels in the caveolae of the cell membrane
- Release of sequestered Ca2+ from the sarcoplasmic (endoplasmic) reticulum
- Ca2+ binds to calmodulin (regulatory protein in place of troponin)
- Calmodulin calcium complex → activation of myosin light chain kinase (MLCK) → phosphorylation of myosin light chain → myosin actin interaction → contraction
- Some differences from skeletal muscle
- Involuntary contractions
- Prolonged and slower yet stronger contractions
- Less energy consumption
- Nervous and nonnervous stimuli
- References: Hall: Guyton and Hall Textbook of Medical Physiology, 13th Edition, 2015, StatPearls: Physiology, Smooth Muscle [Accessed 3 July 2023]
Diagrams / tables
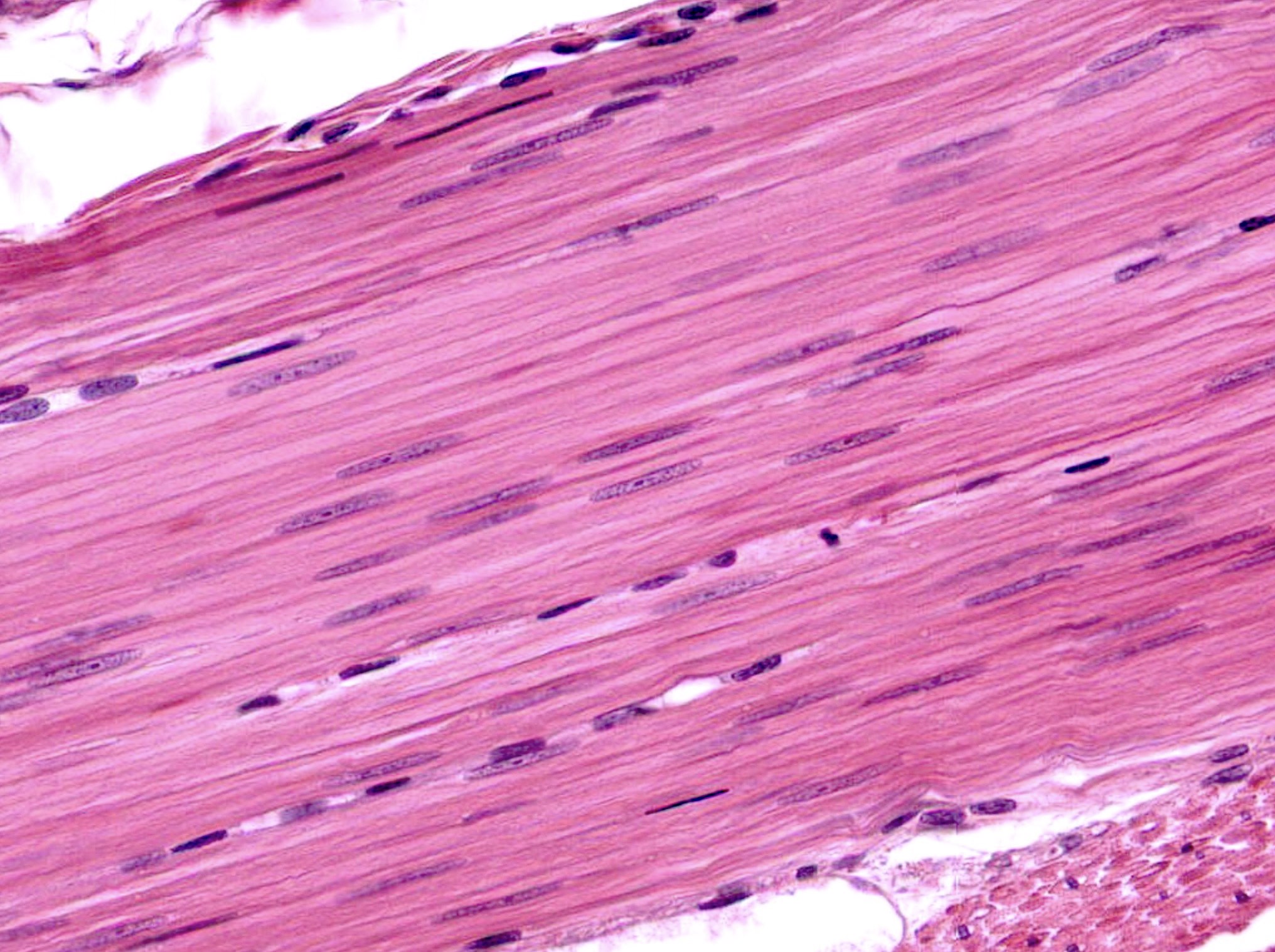
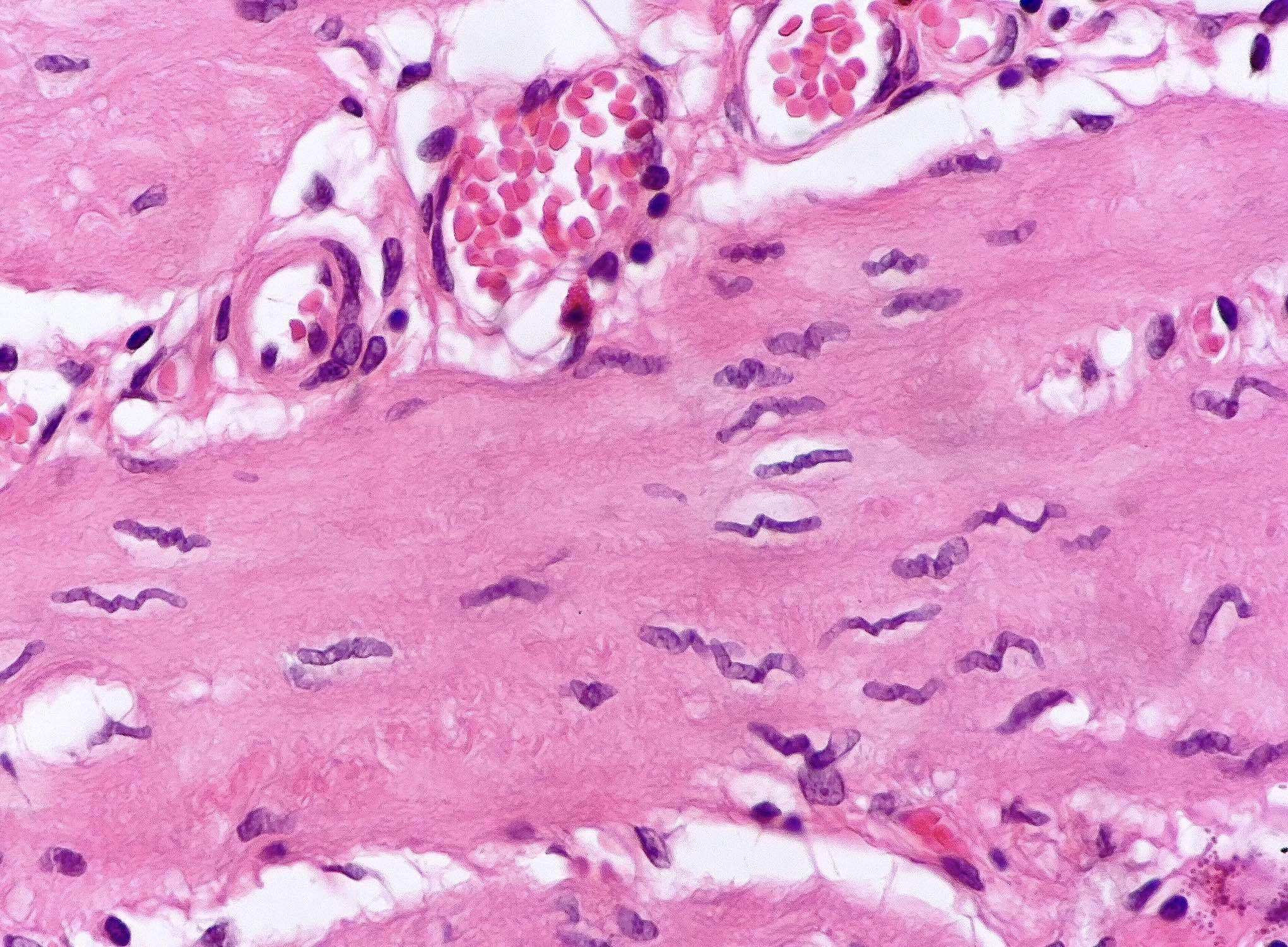
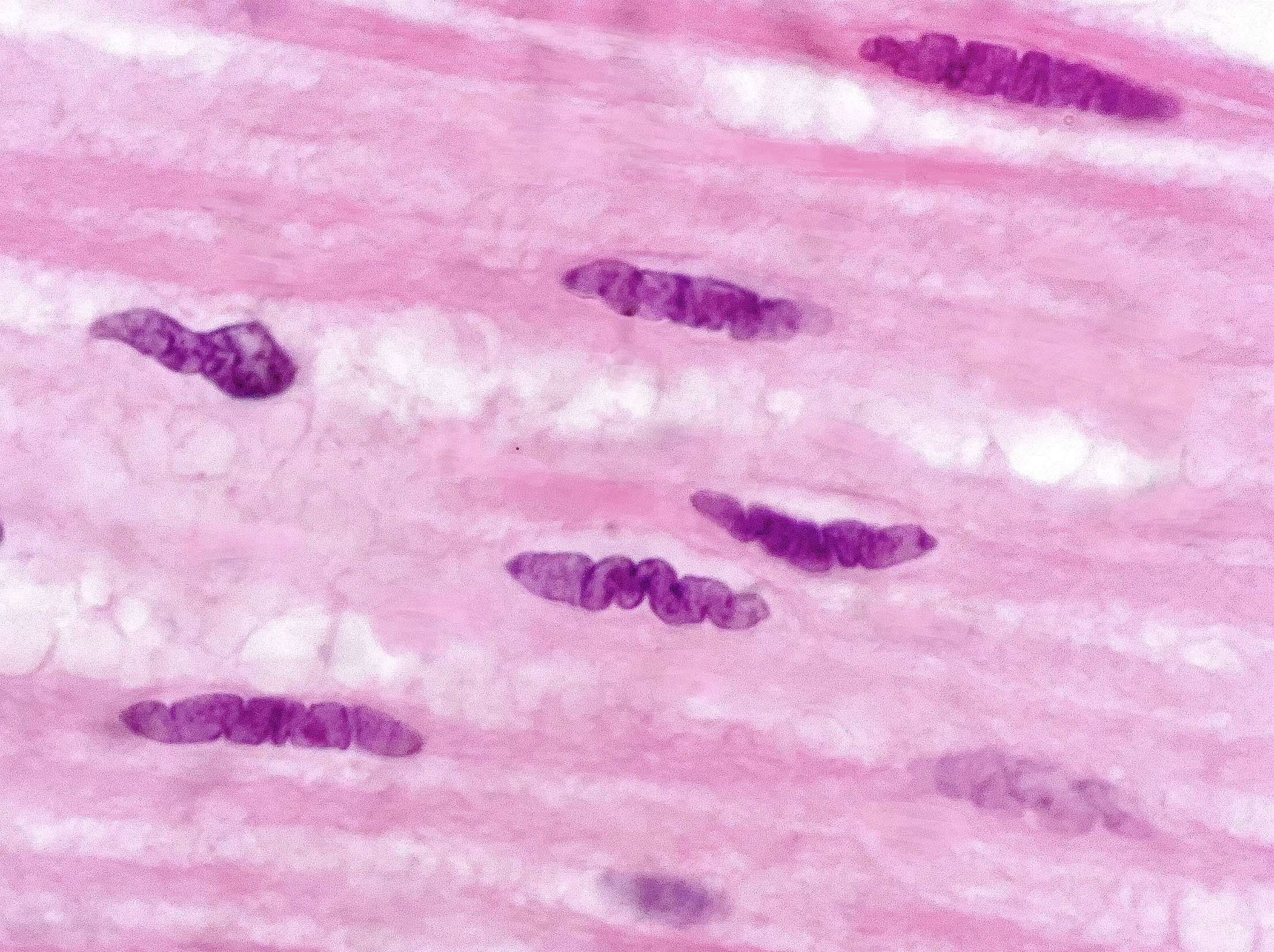
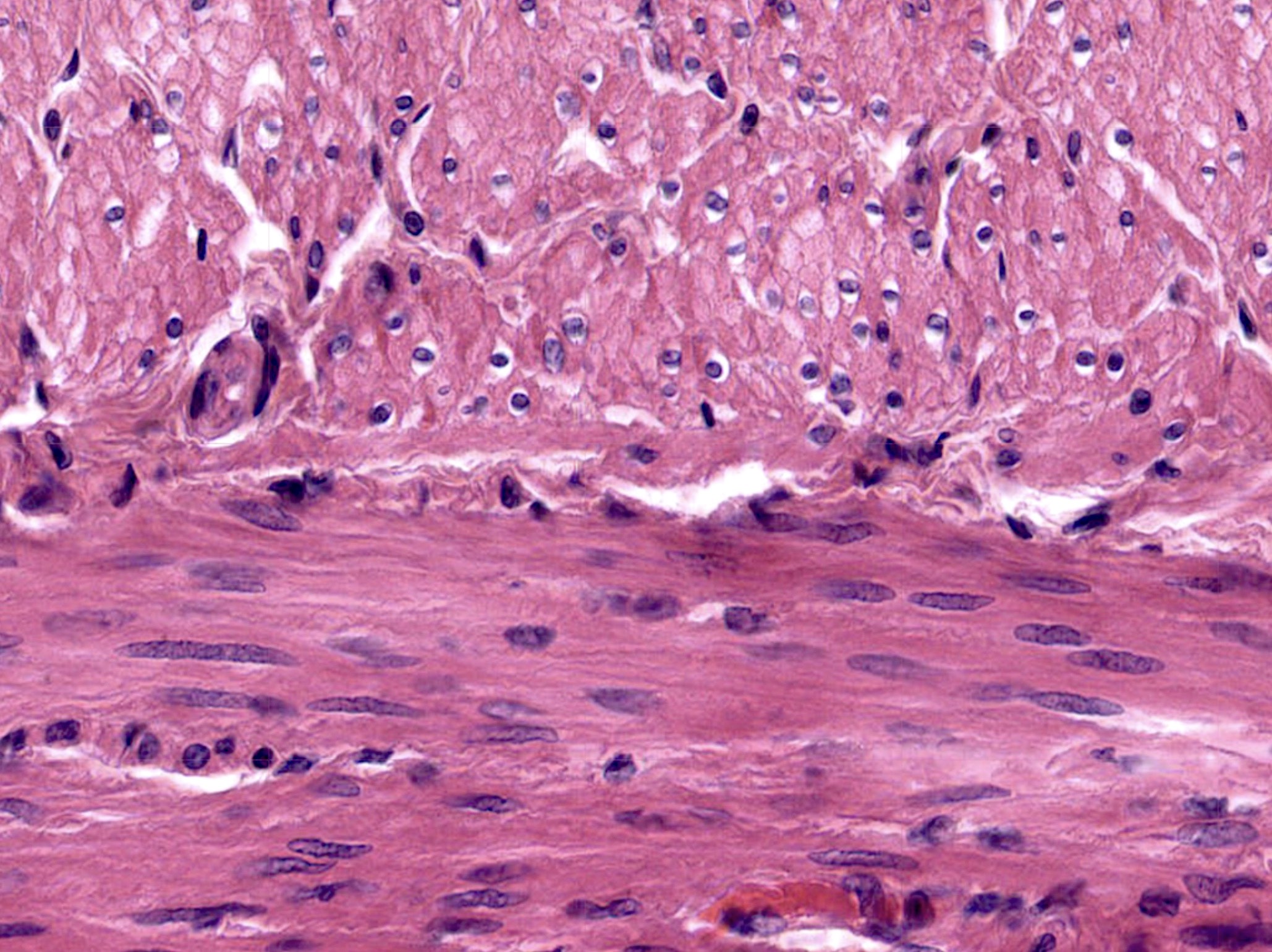
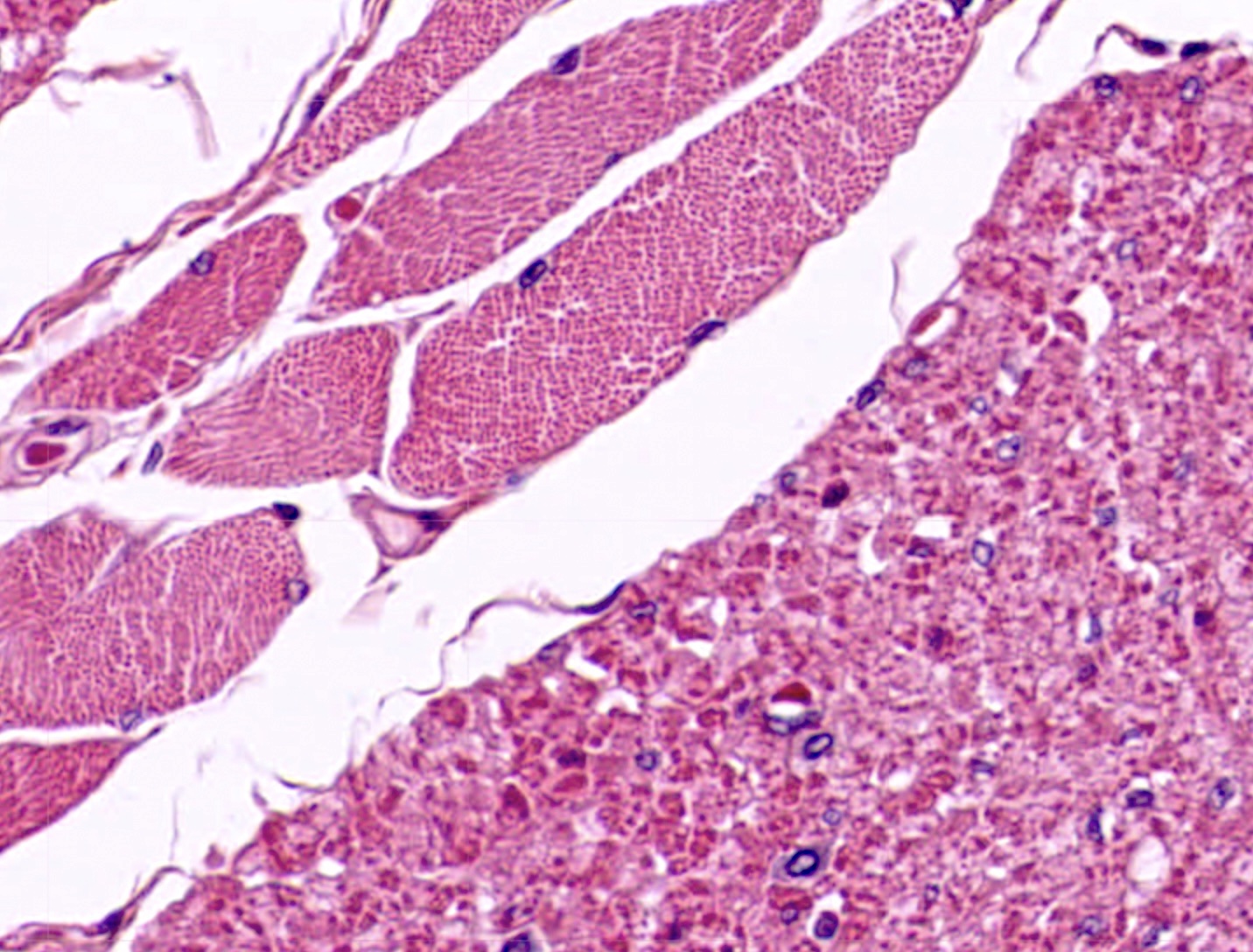
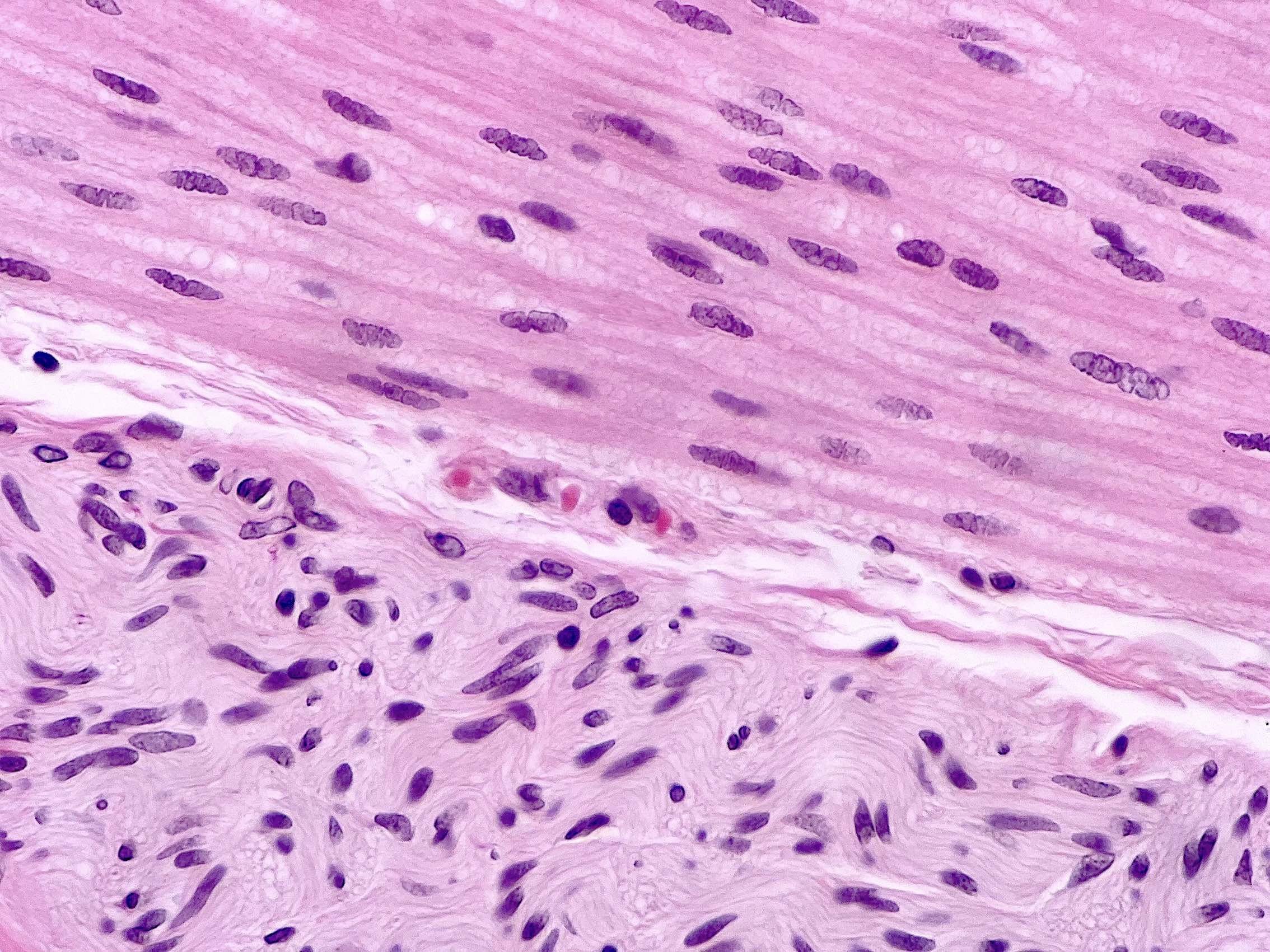
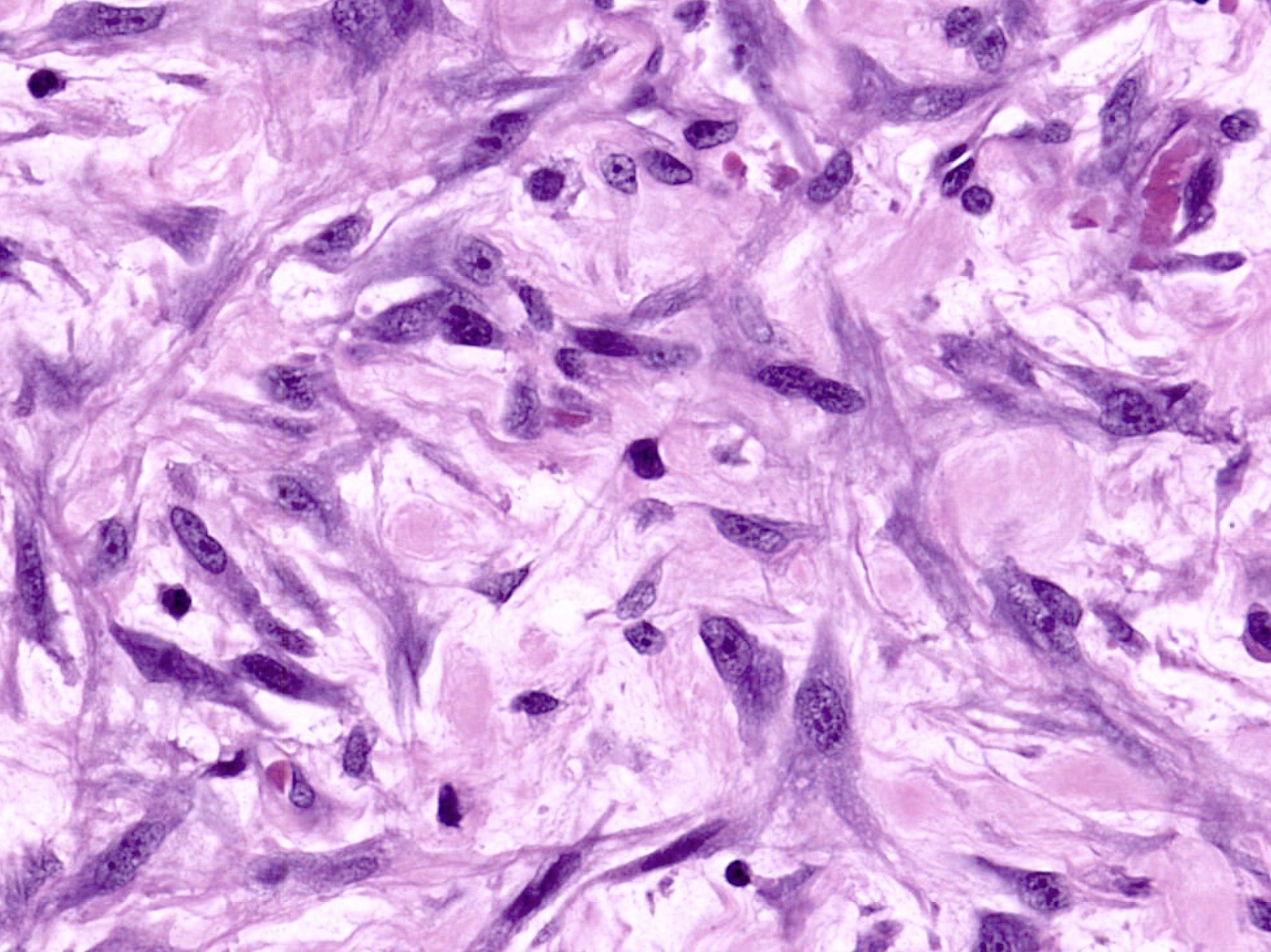
Microscopic (histologic) description
- Cell size: diameter between 1 - 5 μm and length between 20 - 500 μm (much smaller than skeletal muscle)
- Cell shape: spindle shaped or fusiform with tapered ends
- Cytoplasm: eosinophilic fibrillar with distinct cell borders and no cross striations
- Nucleus
- Central elongated cigar shaped nucleus with blunted ends
- Spiral corkscrew appearance in the contracted state
- Appear round on cross section
- Spindle cell mimics
- Fibroblasts in dense regular connective tissue
- Myofibroblasts: spindle to stellate, amphophilic cytoplasm, single elongated nucleus with 1 or 2 small nucleoli, collagen in between the cells
- Schwann cells: cells show slightly undulated buckled nuclei, often with 1 blunt and 1 pointed end, described as S shaped, serpentine, comma shaped, bullet shaped or boomerang-like
- Reference: Young: Wheater's Functional Histology, 6th Edition, 2013
Microscopic (histologic) images
Virtual slides
Positive stains
- Smooth muscle actin (SMA): diffuse cytoplasmic staining (as opposed to membranous tram track in myofibroblasts)
- Muscle specific actin (HHF35): panmuscle marker
- Desmin: panmuscle marker
- h-caldesmon: actin binding protein
- Calponin: actin binding protein
- Smooth muscle myosin heavy chain (SMMHC)
- Smoothelin: terminally differentiated smooth muscle cells (Am J Surg Pathol 2009;33:1795)
- Masson trichrome: smooth muscle stains red
Electron microscopy description
- Cytoplasm
- Filaments
- Thin (actin) and thick (myosin) filaments
- Intermediate filaments
- Dense bodies
- Electron opaque structures floating freely within the cytoplasm → analogous to Z lines of striated muscle anchoring actin and myosin
- Organelles
- Include sarcoplasmic reticulum, mitochondria and Golgi apparatus
- Filaments
- Cell membrane
- Membrane bound dense bodies
- Pinocytotic vesicles or caveolae → Ca2+ movement across the membrane
- Gap junctions → consist of connexins facilitating the transfer of metabolites, ions and signaling molecules
- References: Edwin: Methods in Pharmacology - Smooth Muscle, 1st Edition, 1975, Motta: Ultrastructure of Smooth Muscle, 1st Edition, 1990
Electron microscopy images
Videos
Smooth muscle versus myofibroblasts
Practice question #1
Practice answer #1
A. Cytoplasmic staining with h-caldesmon. Smooth muscle cells contain cytoplasmic caldesmon molecules bound to actin filaments. Answers B and E are incorrect because myogenin and MyoD1 both encode nuclear proteins expressed in skeletal muscle. Answer C is incorrect because membranous staining with smooth muscle actin is seen in myofibroblasts. Answer D is incorrect because S100 staining is seen in Schwann cells.
Comment Here
Reference: Histology-smooth muscle
Comment Here
Reference: Histology-smooth muscle
Practice question #2
Which of the following statements pertaining to the physiology of smooth muscle contraction is true?
- Actin filaments pull the Z lines inward in the contracted state
- Ca2+ binding to calmodulin stimulates myosin actin interaction
- Consumption of tremendous amounts of ATP is required
- Contraction is stimulated by somatic motor neurons
- Strong affinity of troponin for Ca2+ ions initiates contractions
Practice answer #2
B. Ca2+ binding to calmodulin stimulates myosin actin interaction. In smooth muscle, calmodulin acts in place of troponin. Answers A and C - E are incorrect because these statements are true for skeletal muscle.
Comment Here
Reference: Histology-smooth muscle
Comment Here
Reference: Histology-smooth muscle