Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Dall C, Zynger DL. Cryptorchidism. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testiscryptorchidism.html. Accessed July 31st, 2025.
Definition / general
- Absence of one or both testes in the scrotum
- Most common congenital abnormality of the genitourinary tract (Transl Pediatr 2016;5:233)
- Associated with infertility and subfertility, testicular germ cell tumor, testicular torsion and inguinal hernia
Essential features
- Absence of one or both testes in the scrotum most commonly due to failure of descent into the scrotum during fetal development
- Increased risk of reduced fertility and testicular germ cell tumor
Terminology
- Cryptorchidism: absence of one or both testes in the scrotum
- Anorchia or vanishing testis syndrome: absence of one or both testes
- Orchiopexy or orchidopexy: procedure that tethers the testicle into the scrotum
- Ectopic testis: testis is situated away from normal path of descent; differs from undescended testicle
ICD coding
Epidemiology
- 1 - 4% in full term newborns of normal weight; decreases to 1% by the first year (Transl Pediatr 2016;5:233, Int J Urol 2021;28:882)
- Incidence varies by region with increased rates in United Kingdom, Denmark and Lithuania (Hum Reprod Update 2008;14:49)
Sites
- Undescended testicle may be located in the abdomen or inguinoscrotal region
Pathophysiology
- Testicular descent from initial position on abdominal wall is divided into 2 stages with abnormalities of migration thought to be associated with undescended testicle (Endocr Rev 2008;29:560)
- Transabdominal descent: the gubernaculum, a caudal ligament connecting the testicle to the internal ring, holds testicle near internal ring as abdominal cavity develops; insulin-like factor 3 (INSL3) and anti-Müllerian hormone dependent
- Inguinoscrotal descent: the gubernaculum shortens, pulling testicle through inguinal canal to position within scrotum; androgen dependent
- May be a component of testicular dysgenesis syndrome, which includes increased levels of testicular malignancy, poor semen quality and hypospadias
Etiology
- Numerous genes implicated; lack of a clear association in human studies suggests multifactorial causes
- More common in preterm (30%) and low birth weight infants (Transl Pediatr 2016;5:233, J Urol 1999;161:1606)
- Concordance in sibling studies (Fertil Steril 2010;93:124)
- Associated with and increased risk in certain chromosomal abnormalities and genetic syndromes, such as Klinefelter and Prader-Willi syndrome (Lancet 2004;364:273)
- Environmental factors likely play a role: diethylstilbestrol and pesticide exposure have been associated with increased rates; maternal and paternal smoking may increase risk (Mol Cell Endocrinol 2012;355:208, Pediatr Int 2020;62:1256, Med Sci Monit 2005;11:CR274)
Clinical features
- 80% of undescended testicles palpated within inguinal canal or high scrotal area
- 20% of undescended testicles not palpated
- 50% lie in abdomen, 50% are atrophic (Am Fam Physician 2000;62:2047)
- Associated with increased risk of testicular germ cell tumor
- Increasing risk of malignancy with delayed treatment (J Urol 2009;181:452)
- Relative risk of malignancy is 2 - 8x; higher risks associated with delayed repair, bilateral cryptorchidism, additional endocrinopathies, abnormal karyotype and intra-abdominal testes
- Seminoma is most common malignancy
Diagnosis
- Laparoscopy is gold standard in diagnosing a nonpalpable testis
- Ultrasound and other radiologic imaging are not sensitive in diagnosing a nonpalpable testis (Pediatrics 2011;127:119, Pediatrics 2013;131:e1908)
- Must exclude retractile testis, a testis that has descended into the scrotum but has been pulled superiorly by cremaster muscle
- In bilateral cryptorchidism, must exclude congenital adrenal hyperplasia and persistent Müllerian duct syndrome
Laboratory
- In cases of bilateral undescended testicles, hormonal studies (LH, FSH, Müllerian inhibiting substance [MIS] and testosterone) may support diagnosis of gonadal dysgenesis with abnormal hCG stimulation test (Am Fam Physician 2000;62:2037)
Radiology description
- Diagnostic imaging is not recommended in most cases (J Pediatr Surg 2011;46:2406)
Prognostic factors
- Delayed repair reduces fertility, which is worse with bilateral cryptorchidism
- Relative risk for testicular germ cell tumor is 2.2x with prepubertal repair versus 5.4x with postpubertal repair (N Engl J Med 2007;356:1835)
Case reports
- 1 year old boy with swelling of abdominal wall (Am J Case Rep 2020;21:e927495)
- 1 year old boy with persistent Müllerian duct syndrome and transverse testicular ectopia (BMJ Case Rep 2018;2018:bcr2017223994)
- 46 year old man with yolk sac tumor in cryptorchid testis (BMJ Case Rep 2019;12:e229541)
Treatment
- Orchiopexy may be performed at 6 - 18 months as it is unlikely that testicle will spontaneously descend after this time (J Pediatr Urol 2021;17:239)
- American Urological Association does not recommend hormonal therapy (hCG) to promote the descent of the undescended testicle due to low response rates (AUA: Evaluation and Treatment of Cryptorchidism [Accessed 19 November 2021])
Clinical images
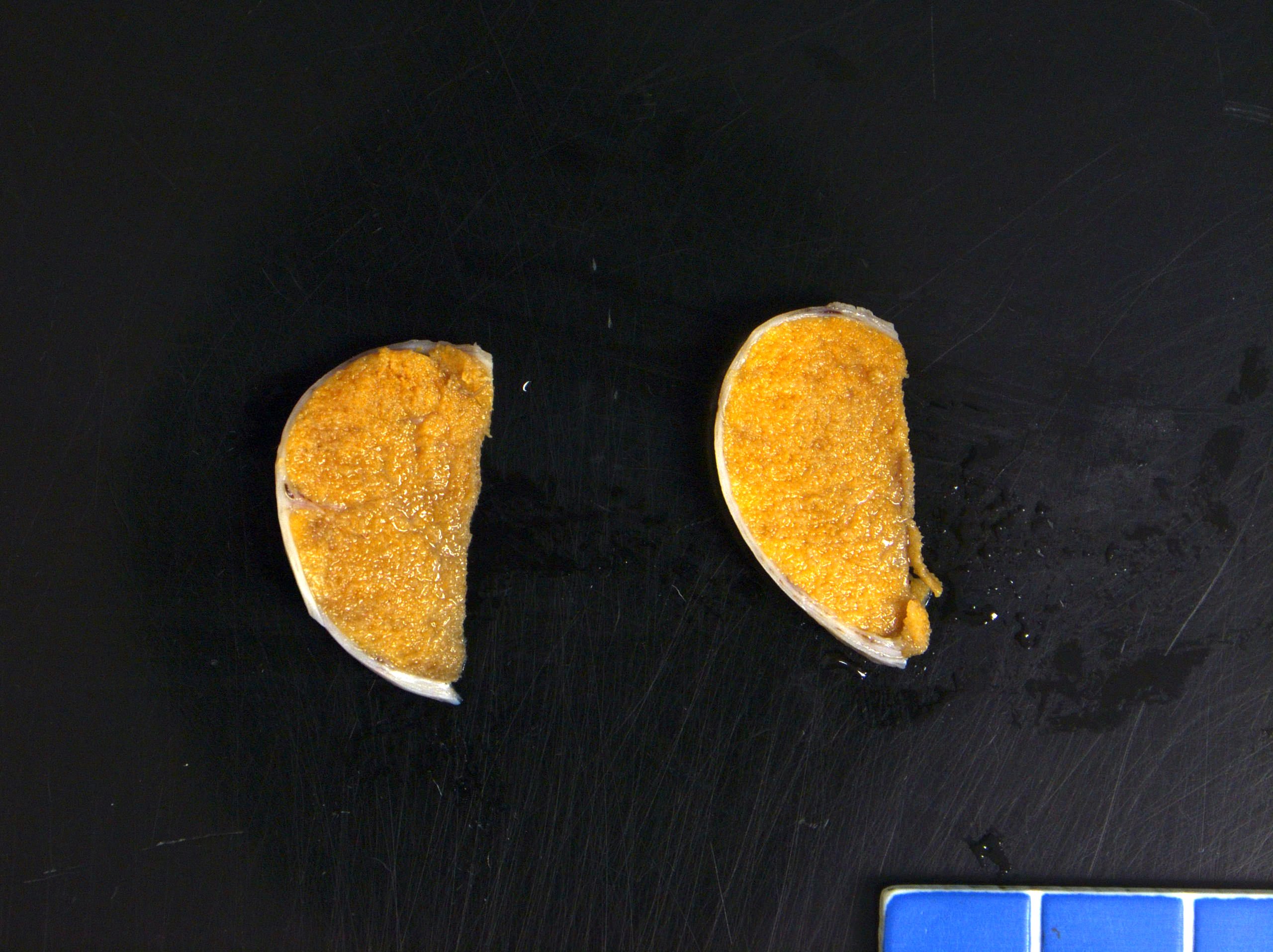
Gross description
- Smaller and atrophic compared to descended testis
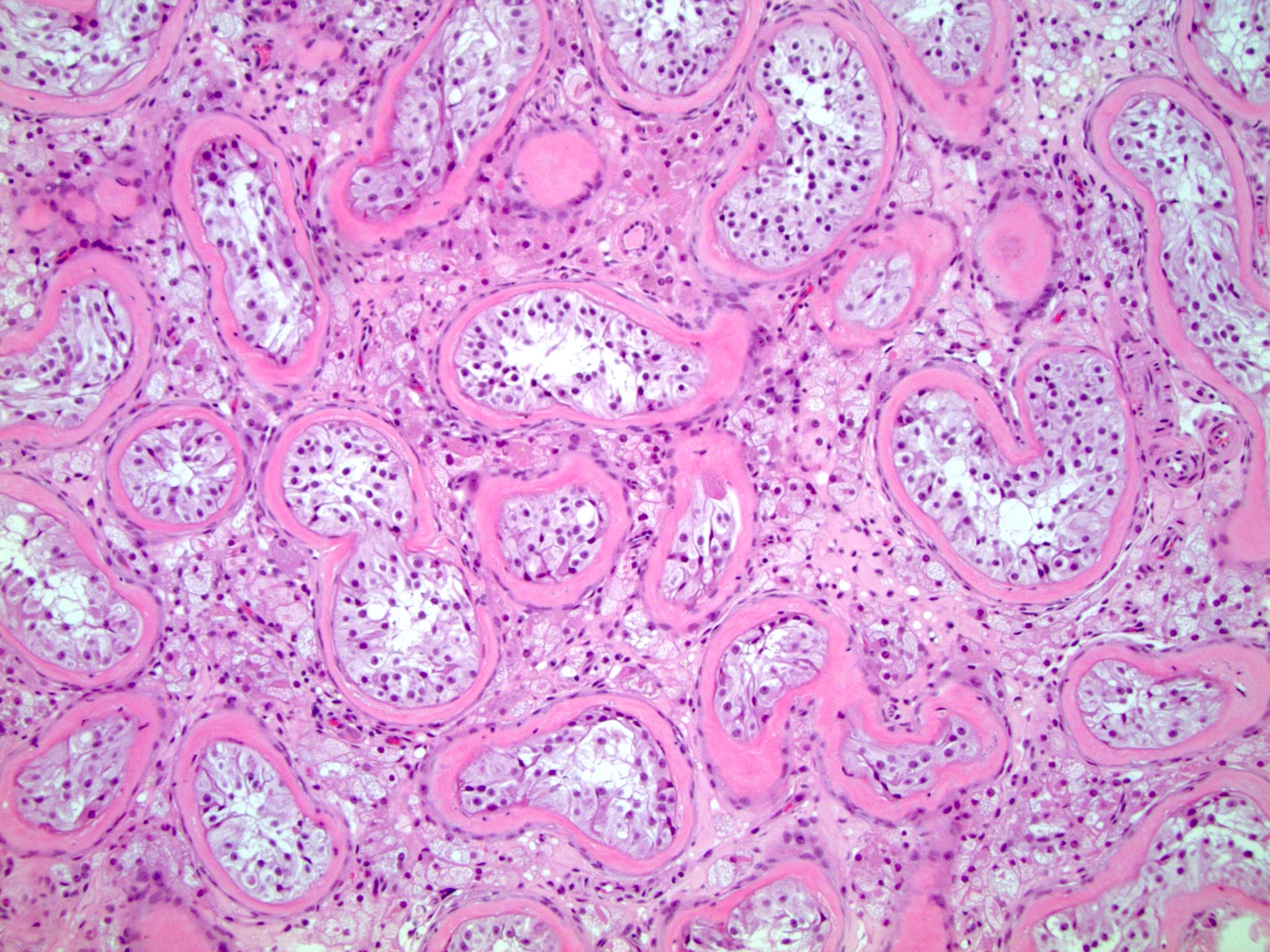
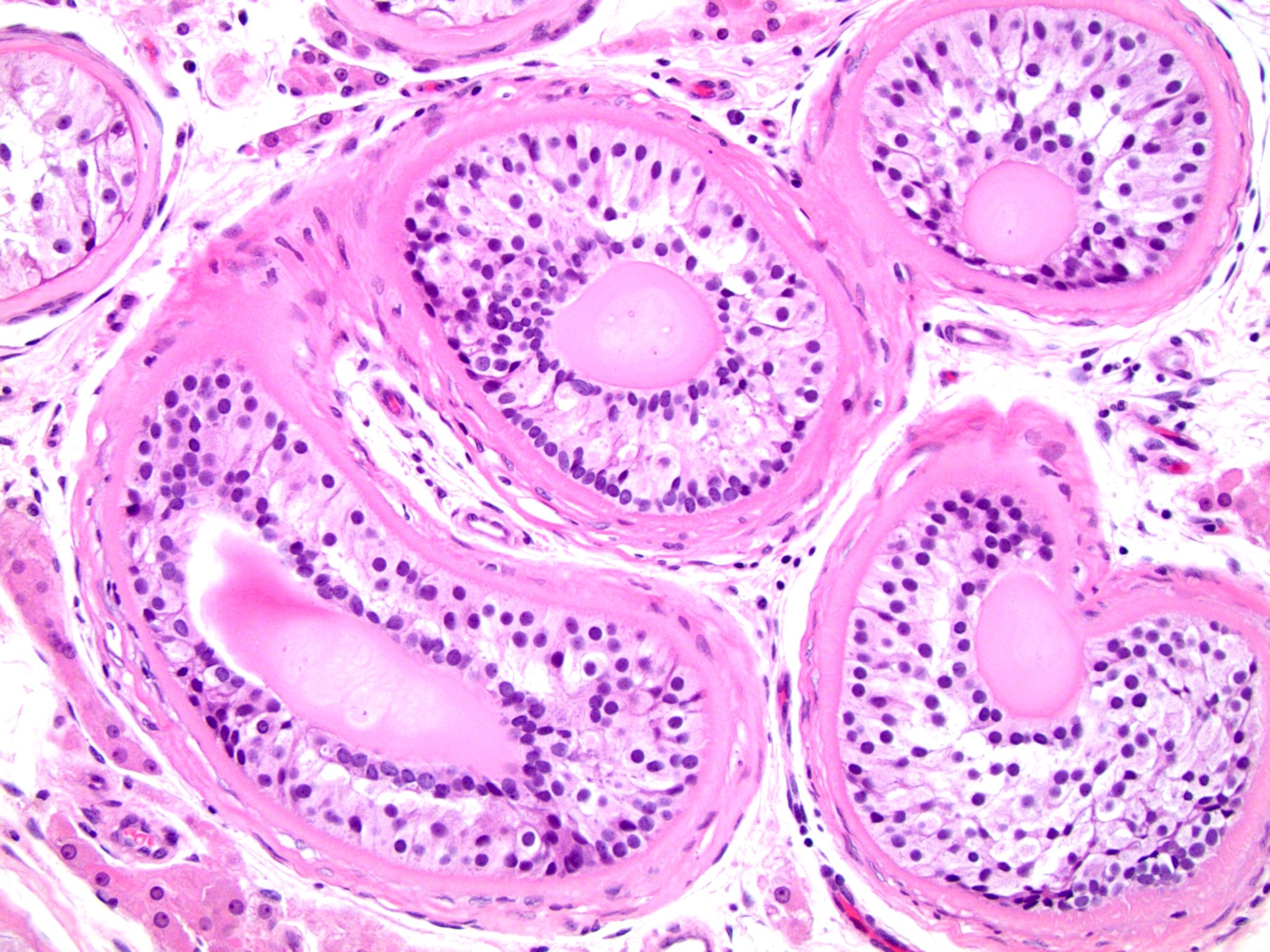
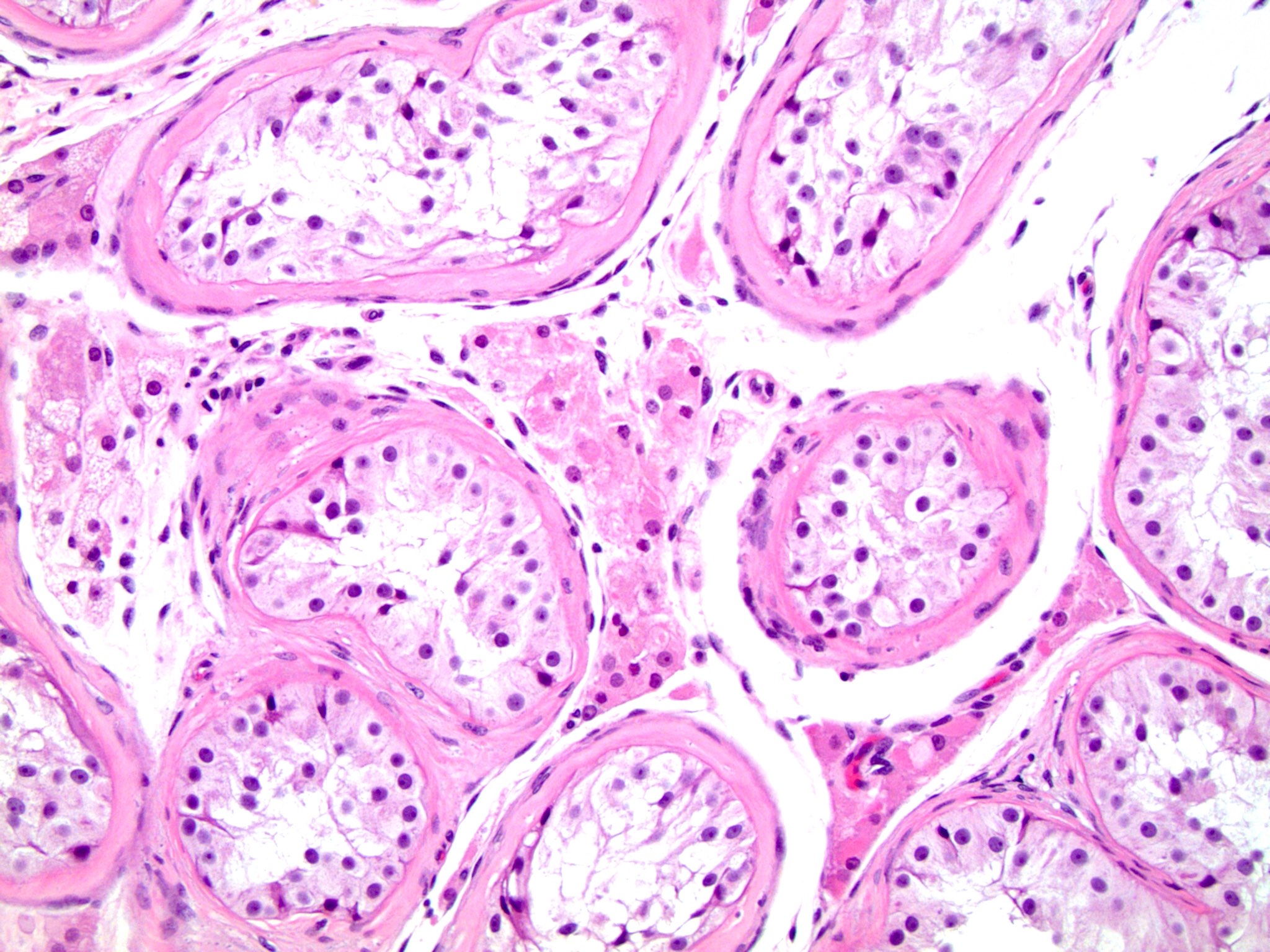
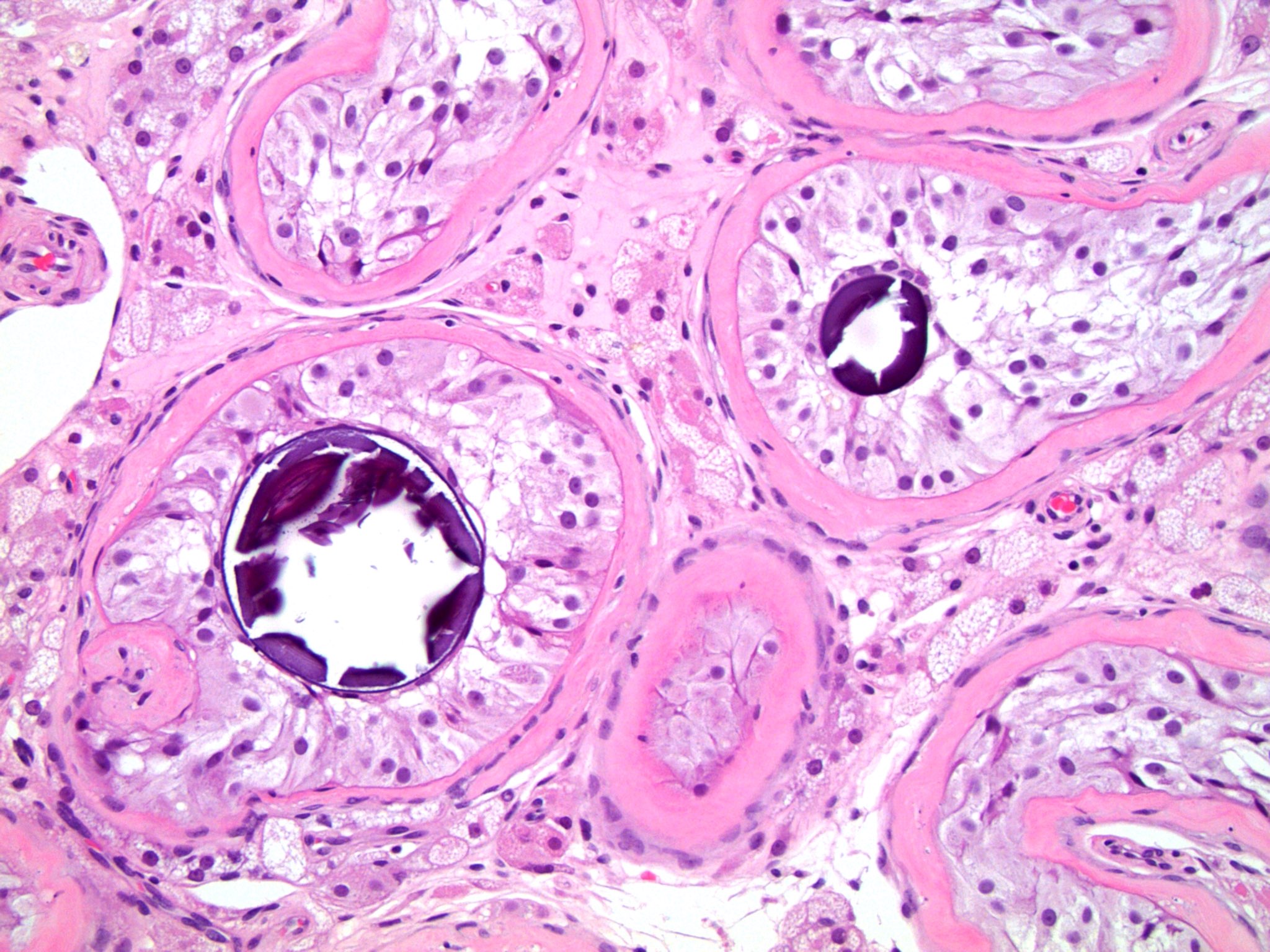
Microscopic (histologic) description
- Histopathologic differences become much more pronounced after 2 years of life and are increased with delayed orchiopexy (J Urol 2009;182:704)
- Peritubular fibrosis
- Seminiferous tubule atrophy
- Decreased / absent spermatogenesis
- Sertoli cells may demonstrate granular cell change with eosinophilic granular cytoplasmic lysosomes
- Sertoli cell only seminiferous tubules: tubules with only bland, monotonous pale cells with granular cytoplasm attached to the basement membrane; absent germ cells and no spermatogenesis
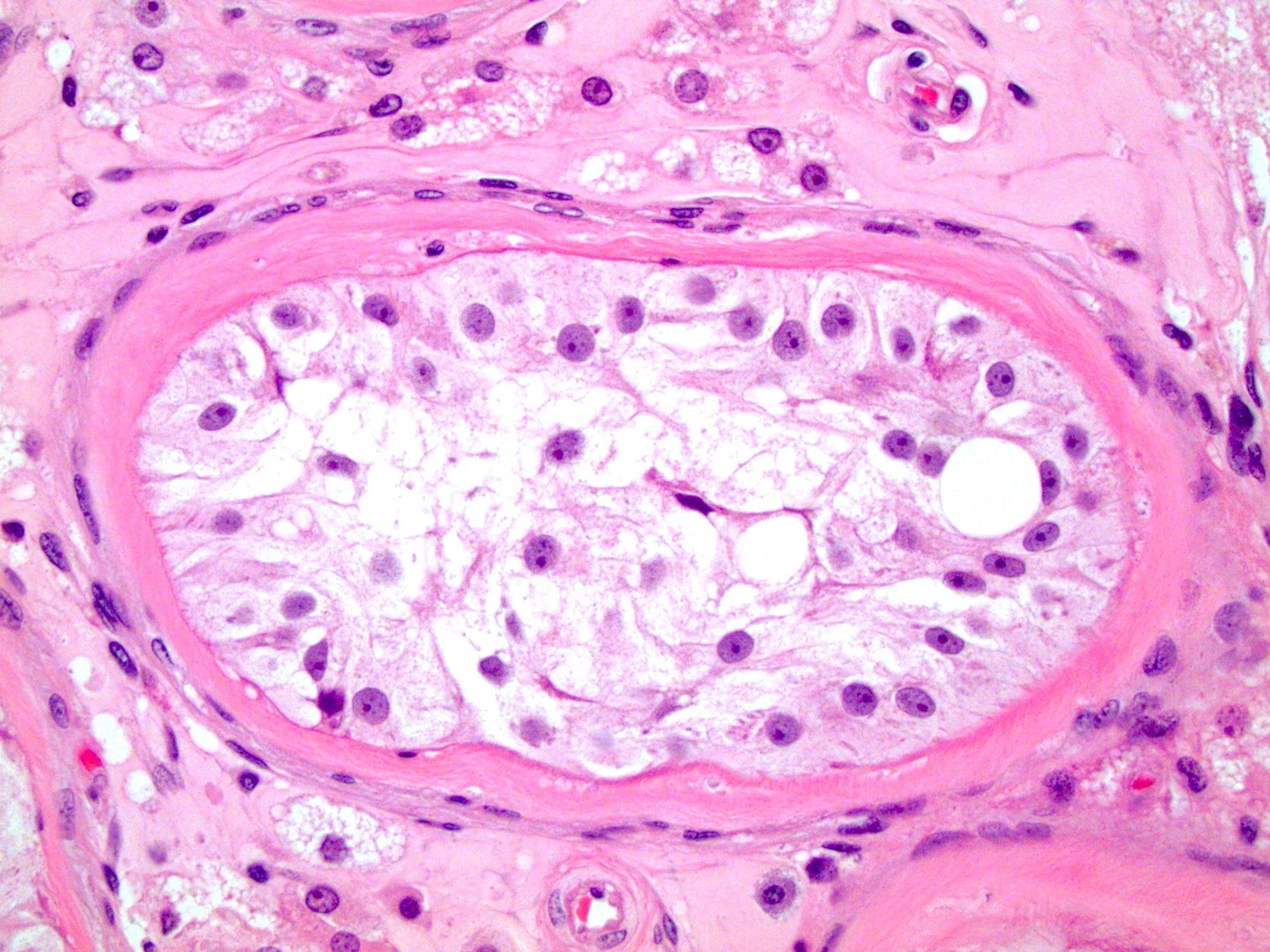
- Sertoli cell nodule: nodules composed of immature elongated Sertoli cells (Pick adenoma) may be present; can have central microliths
- Increased microliths within seminiferous tubules
- Retained Leydig cells give appearance of hyperplasia
- Evaluate for germ cell neoplasia in situ (GCNIS): large, pleomorphic, basally located cells within the seminiferous tubules may be present; use immunostains for confirmation
Microscopic (histologic) images
Cytology description
- Not used to evaluate a cryptorchid testis
Positive stains
- Germ cell neoplasia in situ (GCNIS) is positive for CD117 (KIT), PLAP, D2-40 and OCT 3/4 but these stains may be falsely positive in boys < 2 years old with cryptorchidism (J Urol 2014;191:1084)
Sample pathology report
- Ectopic testis, removal:
- Seminiferous tubules with Sertoli only tubules, peritubular fibrosis, no spermatogenesis and microliths consistent with cryptorchid testis
Differential diagnosis
Practice question #1
A 24 year old man with a history of untreated cryptorchidism presents with a painful abdominal mass. Pathology is most likely to be consistent with which of the following?
- Dermoid cyst
- Germ cell neoplasia in situ
- Mixed germ cell tumor
- Seminoma
- Sertoli cell tumor
Practice answer #1
D. Seminoma is the most common malignancy in the setting of cryptorchidism.
Comment Here
Reference: Cryptorchidism
Comment Here
Reference: Cryptorchidism
Practice question #2
What histological changes are most likely to be observed in a nonneoplastic cryptorchid testis?
- Atrophic seminiferous tubules, peritubular fibrosis and nodules of cells containing dark nucleoli and eosinophilic granular cytoplasm
- Bland appearing cysts lined with cuboidal epithelium and ciliated cells
- Cysts lined by squamous cells filled with keratin
- Glycogen rich cells with large, irregular nuclei arranged in sheets
- Rod-like cytoplasmic inclusions with a diffuse growth pattern and rare mitotic cells
Practice answer #2
A. Atrophic seminiferous tubules, peritubular fibrosis and nodules of cells containing dark nucleoli and eosinophilic granular cytoplasm are findings consistent with an undescended testicle. B is incorrect because these might be the findings associated with benign glands, such as those seen in endometriosis or endosalpingiosis. C is incorrect because this histology may be associated with teratoma. D is incorrect because these might be the findings of a seminoma, which are more common in undescended testicles. E is incorrect because Leydig cell tumors often contain Reinke crystals, described in this answer choice.
Comment Here
Reference: Cryptorchidism
Comment Here
Reference: Cryptorchidism