Table of Contents
Definition / general | Essential features | Clinical features | Diagnosis | Case reports | Cytology description | Cytology images | Management | Sample cytology report | Videos | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Suzuki A. Suspicious for malignancy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidsuspicious.html. Accessed September 4th, 2025.
Definition / general
- Bethesda category V suspicious for malignancy (SM) is used when some cytologic features are strongly suspected of malignancy but are not sufficient for a conclusive diagnosis (Thyroid 2017;27:1341)
- Higher suspicion of malignancy than atypia of undetermined significance (AUS) but lower suspicion than malignant
- Exceptions: follicular and oncocytic carcinomas
Essential features
- Molecular testing with mutation panels may be useful, particularly for potential cases of noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP)
- Purpose of separating suspicious for malignancy from malignant is to preserve the very high positive predictive value of the malignant category without compromising the overall sensitivity of fine needle cytology aspiration
- Used when cytology is strongly suspected of malignancy but is not sufficient for a conclusive diagnosis
- Frequency: 1.0 - 6.3%; resection rate: 70%
- Risk of malignancy: 74% (67 - 83%) (NIFTP = malignant), 65% (NIFTP ≠ malignant)
- Most common histological diagnosis is papillary thyroid carcinoma (PTC) (Acta Cytol 2014;58:15)
Clinical features
- Frequency: 3% (Ali: The Bethesda System for Reporting Thyroid Cytopathology - Definitions, Criteria and Explanatory Notes, 3rd Edition, 2023)
- Resection rate: 70% (Cancer Cytopathol 2020;128:238)
- Risk of malignancy: 74% (NIFTP = malignant), 65% (NIFTP ≠ malignant) (Cancer Cytopathol 2020;128:238, Ali: The Bethesda System for Reporting Thyroid Cytopathology - Definitions, Criteria and Explanatory Notes, 3rd Edition, 2023)
- Suspicious for malignancy interpretation allows for more conservative management options (e.g., lobectomy)
Diagnosis
- Aspirates where malignancy is suspected but cannot be determined due to
- Suboptimal sampling
- Poor cellular preservation
- Unusual variant of neoplasm
- Overlapping cytological features with other thyroid lesions
- Excluded from this category
- Specimens suspicious for a follicular or oncocytic neoplasm (see Follicular neoplasm and Follicular neoplasm / oncocytic follicular neoplasm)
- Unequivocally malignant aspirates (see Malignant)
- Specimens with a minor degree of atypia, primarily cytologic or architectural (see Atypia of undetermined significance)
- Most cases of follicular variant of papillary thyroid carcinoma and NIFTP are diagnosed cytologically as either suspicious for malignancy, follicular neoplasm or atypia of undetermined significance
- Rapid on site evaluation (ROSE) adds value to the FNA procedure by reducing the number of suspicious cases
- Frozen section has limited utility for suspicious for malignancy nodules (Thyroid 2002;12:619)
Case reports
- 18 year old woman with thyroid schwannoma (Medicine (Baltimore) 2021;100:e25517)
- 55 year old man with colon cancer metastasis within a NIFTP that was cytologically suspected of papillary thyroid carcinoma (Head Neck Pathol 2020;14:833)
- 58 year old woman with mammary analogue secretory carcinoma of the thyroid that was cytologically suspected of papillary thyroid carcinoma (Int J Surg Pathol 2018;26:459)
- 63 year old man with follicular variant of papillary thyroid carcinoma that presented as a toxic nodule and was cytologically suspected of follicular variant of papillary thyroid carcinoma (Clin Nucl Med 2010;35:770)
- 63 year old woman with hyalinizing trabecular tumor that was cytologically suspected of hyalinizing trabecular tumor (J Pathol Transl Med 2018;52:252)
- 71 year old man with mixed medullary and follicular cell carcinoma of the thyroid that was cytologically suspected of thyroid carcinoma (Med Sci Monit 2008;14:CS31)
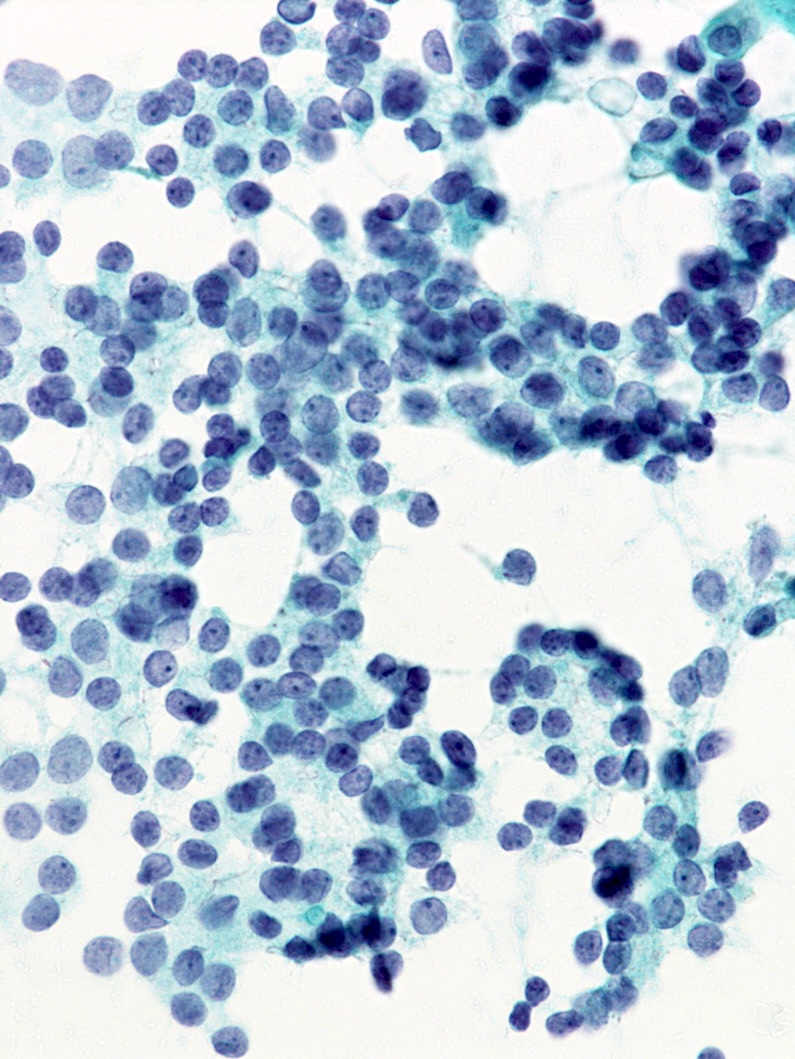
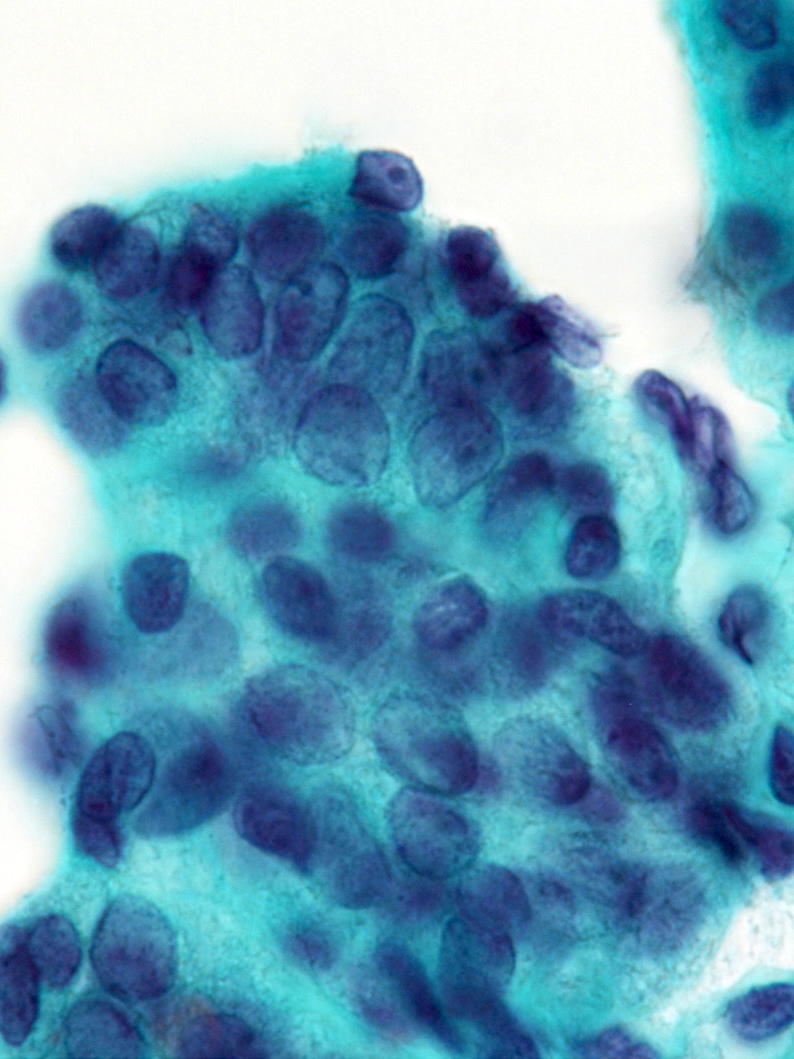
Cytology description
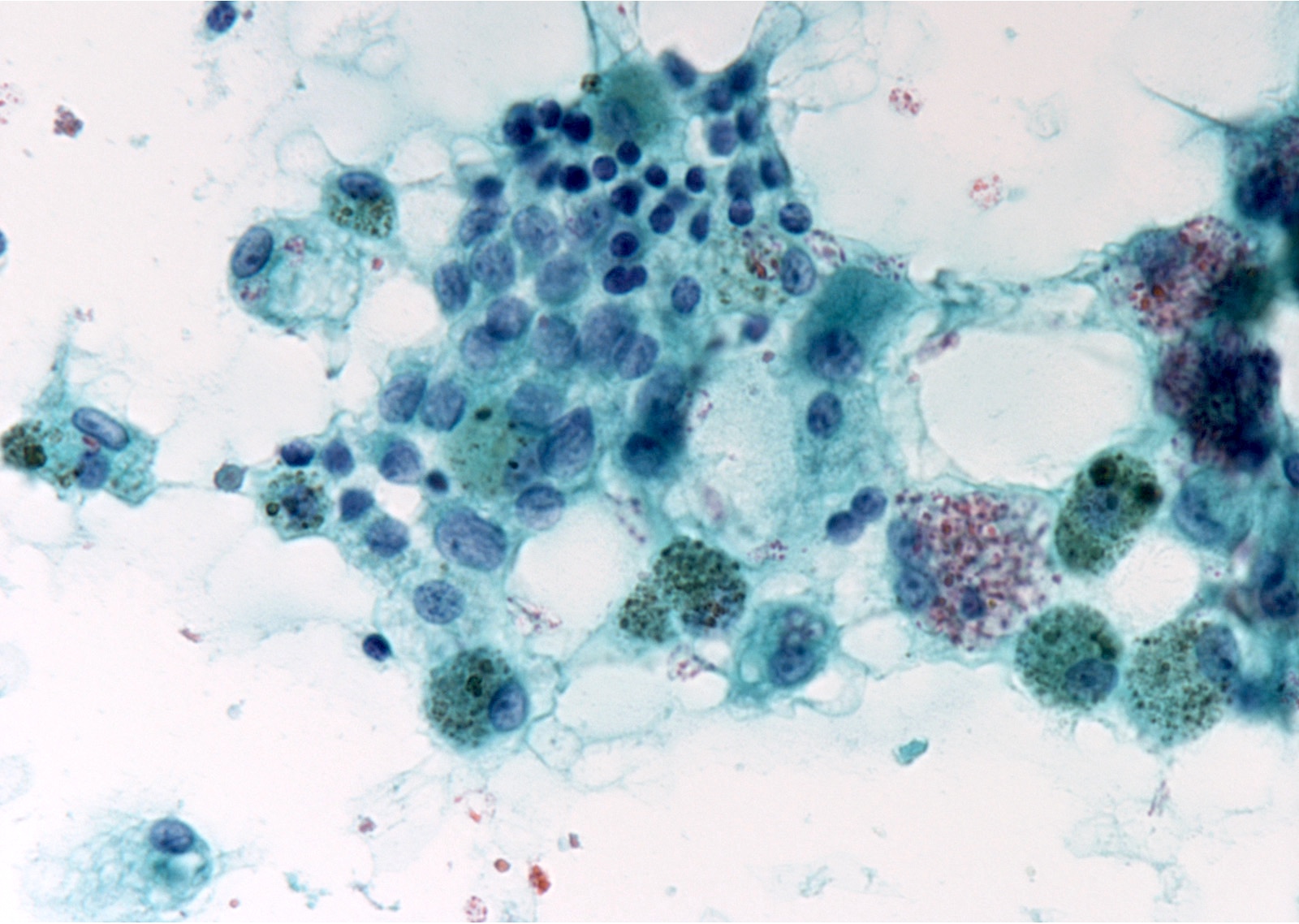
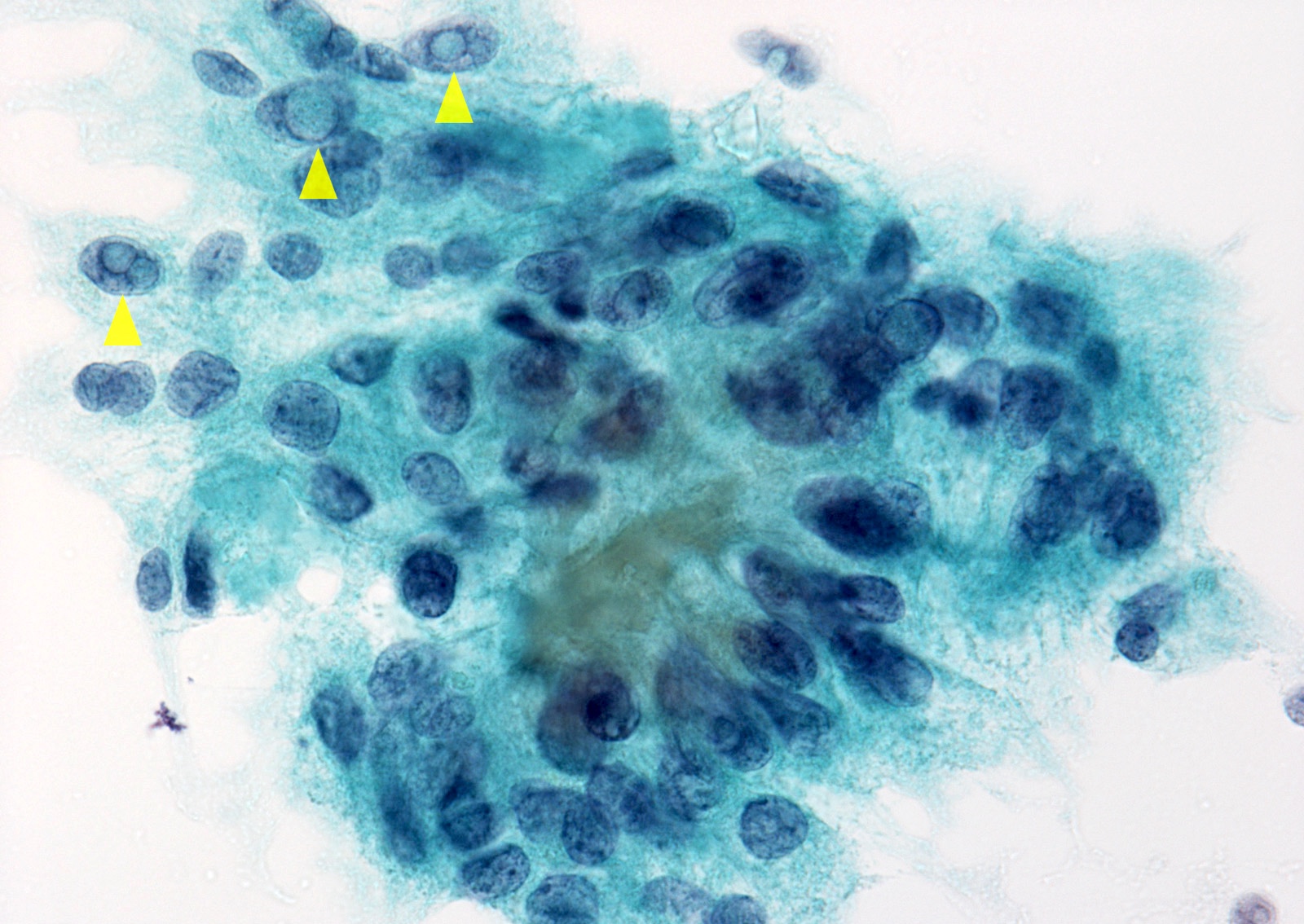
- Suspicious for papillary thyroid carcinoma
- Patchy nuclear changes: moderate to high cellularity with nuclei that show enlargement, pallor, grooves, irregularity or molding but lack nuclear pseudoinclusions, psammoma bodies and papillary architecture
- Mimicked by several benign conditions
- Incomplete nuclear changes: nuclei that show enlargement with mild pallor and grooves, absence of nuclear irregularity, nuclear molding, nuclear pseudoinclusions, psammoma bodies and papillary architecture
- NTRK rearranged papillary thyroid carcinoma often demonstrates intermediate nuclear features
- Sparsely cellular specimen: poor cellularity, presence of many findings suggesting papillary thyroid carcinoma
- Cystic degeneration: cystic degeneration based on foamy histiocytes, scattered clusters of follicular cells with the nuclei showing enlargement, pallor, grooves, absence of nuclear pseudoinclusions, psammoma bodies and papillary architecture, large, atypical, histiocytoid cells with enlarged nuclei and without abundant vacuolated cytoplasm (Ali: The Bethesda System for Reporting Thyroid Cytopathology - Definitions, Criteria and Explanatory Notes, 3rd Edition, 2023)
- Patchy nuclear changes: moderate to high cellularity with nuclei that show enlargement, pallor, grooves, irregularity or molding but lack nuclear pseudoinclusions, psammoma bodies and papillary architecture
- Suspicious for papillary thyroid carcinoma
- Follicular variant: moderate to high cellularity, follicular arrangements, presence of many findings suggesting papillary thyroid carcinoma
- Suspicious for medullary thyroid carcinoma
- Sparse or moderate cellularity
- Monomorphic population of isolated small or medium sized cells with a high N:C ratio
- Nuclei are eccentrically located, with smudged chromatin
- Small fragments of amorphous material
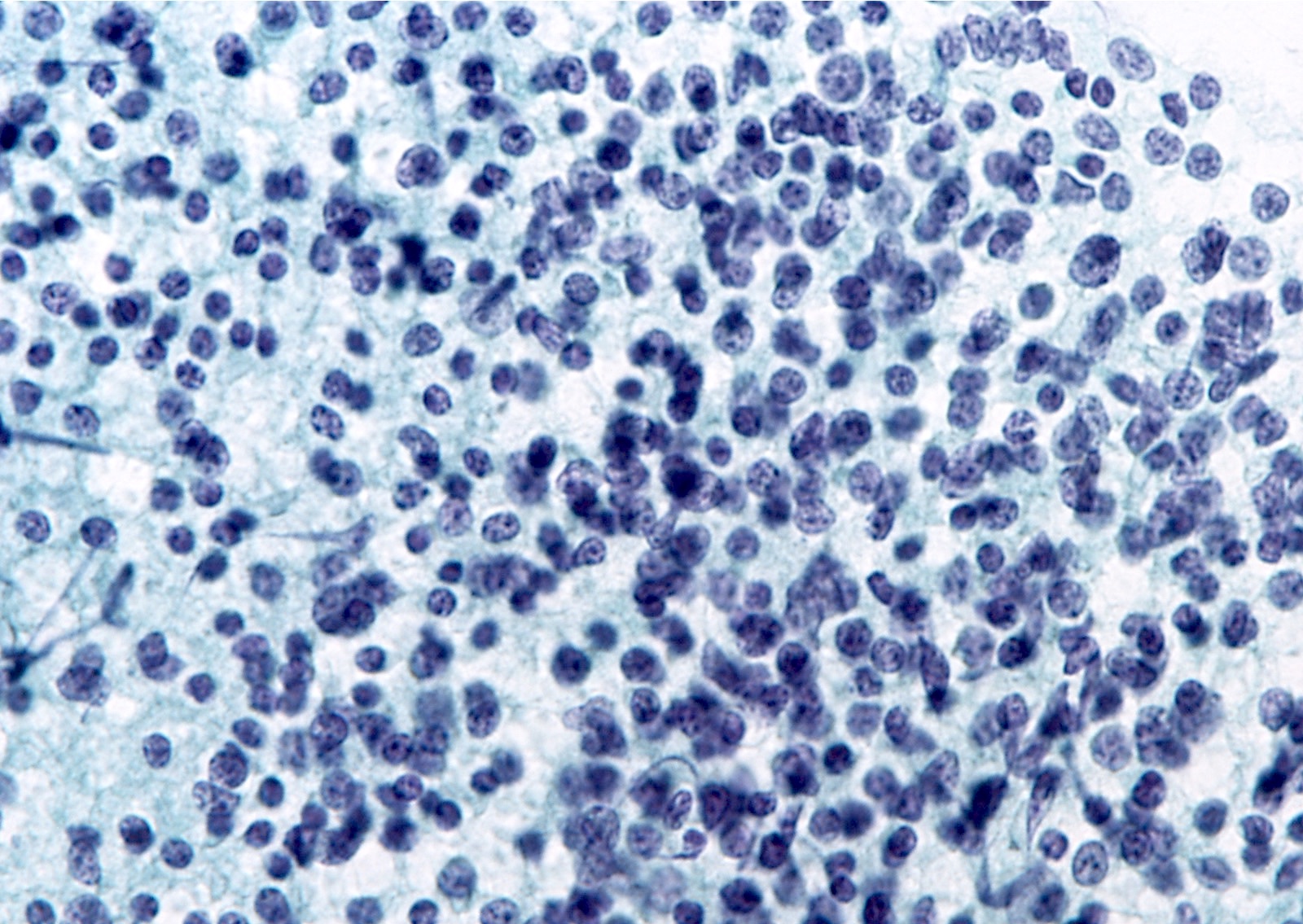
- Suspicious for lymphoma
- Numerous monomorphic small to intermediate sized lymphoid cells
- Sparsely cellular and contains atypical lymphoid cells
- Suspicious for malignancy, not otherwise specified
- Other primary thyroid malignancies like anaplastic carcinoma and poorly differentiated carcinoma
- Suboptimal cellularity or preservation can lead to uncertainty and result in a suspicious for malignancy interpretation
Cytology images
Management
- Usually surgical management similar to that of malignant nodules (Thyroid 2016;26:1)
- In suspicious for papillary thyroid carcinoma cases with low risk features (≤ 1 cm, without extrathyroidal extension and clinical metastasis), active surveillance is an option (Thyroid 2018;28:23)
- 7 gene molecular panel (including BRAF, RAS, RET::PTC, PAX8::PPARγ) test would guide the surgical management (Thyroid 2015;25:760)
- Positive: initial oncologic thyroidectomy
- Negative: at least a diagnostic lobectomy
- Active surveillance is an option for low risk papillary microcarcinoma (Thyroid 2016;26:1)
- For suspicious for medullary thyroid carcinoma
- Measuring serum calcitonin level or calcitonin immunostaining is recommended (Endocr J 2017;64:1099)
- For suspicious for lymphoma
- Repeat fine needle aspiration to obtain cells for flow cytometry (Endocr J 2017;64:859, Endocr J 2019;66:1083)
Sample cytology report
- Thyroid, ultrasound guided FNA:
- Suspicious for malignancy (papillary thyroid carcinoma) (see comment)
- Comment: A few follicular cells showing nuclear enlargement, pale and powdery chromatin and nuclear grooves are present.
- Thyroid, ultrasound guided FNA:
- Suspicious for malignancy (medullary thyroid carcinoma) (see comment)
- Comment: Correlation with serum calcitonin level or immunostaining might be helpful for definitive diagnosis if clinically indicated.
- Thyroid, ultrasound guided FNA:
- Suspicious for malignancy (lymphoma) (see comment)
- Comment: Reaspiration for flow cytometry might be helpful to better characterize the lymphocyte population if clinically indicated.
Videos
Head and tail of the Bethesda system for thyroid
Thyroid cytology - Bethesda classification
How to observe thyroid FNA
Differential diagnosis
- Noninvasive follicular thyroid neoplasm with papillary-like nuclear features:
- Microfollicular architecture with minimal nuclear features of papillary thyroid carcinoma, absence of nuclear pseudoinclusions, papillae or psammoma bodies
- Impossible to distinguish from invasive follicular variant of papillary thyroid carcinoma by fine needle aspiration alone
- Hyalinizing trabecular tumor:
- Trabecular growth pattern of the cells with nuclear grooves and abundant nuclear pseudoinclusions, intratrabecular hyaline material
- MIB1 membranous positivity is useful to distinguish from papillary thyroid carcinoma (Am J Surg Pathol 2000;24:575)
- Chronic thyroiditis (versus papillary thyroid carcinoma):
- Nuclear changes of follicular cells with focal enlargement, grooves, prominent nucleoli and chromatin clearing in the lymphocytic background
- Abundance of lymphocytes and plasma cells does not exclude the possibility of a coexisting papillary thyroid carcinoma (Acta Cytol 2012;56:352)
- Chronic thyroiditis (versus MALT lymphoma):
- Numerous lymphocytes, few follicular cells
- Difficult to distinguish from MALT lymphoma without immunophenotyping by flow cytometry
- Benign cyst:
- Elongated cells with pale chromatin, nuclear grooves and relatively large nucleoli
- Spindle shaped morphology of the cell and nucleus, reminiscent of reparative epithelium in cervical Pap smears
Practice question #1
Practice answer #1
C. Follicular variant of papillary thyroid carcinoma. Follicular cells appear as a microfollicular pattern. A few follicular cells showing nuclear enlargement, pale and powdery chromatin and nuclear grooves are present. Answer A is incorrect because tumor cells show follicular pattern without papillary pattern. Answers B, D and E are incorrect because tumor cells show nuclear findings characteristic of papillary thyroid carcinoma (powdery chromatin, grooves).
Comment Here
Reference: Suspicious for malignancy
Comment Here
Reference: Suspicious for malignancy
Practice question #2
What is the most common histological equivalent of suspicious for malignancy aspirate of thyroid?
- Anaplastic thyroid carcinoma
- Follicular carcinoma
- Medullary thyroid carcinoma
- Papillary thyroid carcinoma
- Poorly differentiated thyroid carcinoma
Practice answer #2
D. Papillary thyroid carcinoma. > 85% of suspicious for malignancy cases are papillary thyroid carcinoma. Answers A, C and E are incorrect because they are all rare tumors and therefore have low percentages in this category. Answer B is incorrect because follicular carcinoma is classified as follicular neoplasm by cytology.
Comment Here
Reference: Suspicious for malignancy
Comment Here
Reference: Suspicious for malignancy