- Medicolegal autopsy is supplemented by ancillary investigations to help determine or corroborate the cause of death (COD), manner of death (MOD) and to positively identify unknown deceased individuals
- Ancillary investigations include radiology, odontology, histology, microbiology, sexual assault kits, DNA testing and vitreous fluid analysis (Forensic Sci Int 2020;310:110235)
- Ancillary investigations supplement the anatomic findings identified during the autopsy
- Common types of ancillary investigations:
- Radiology
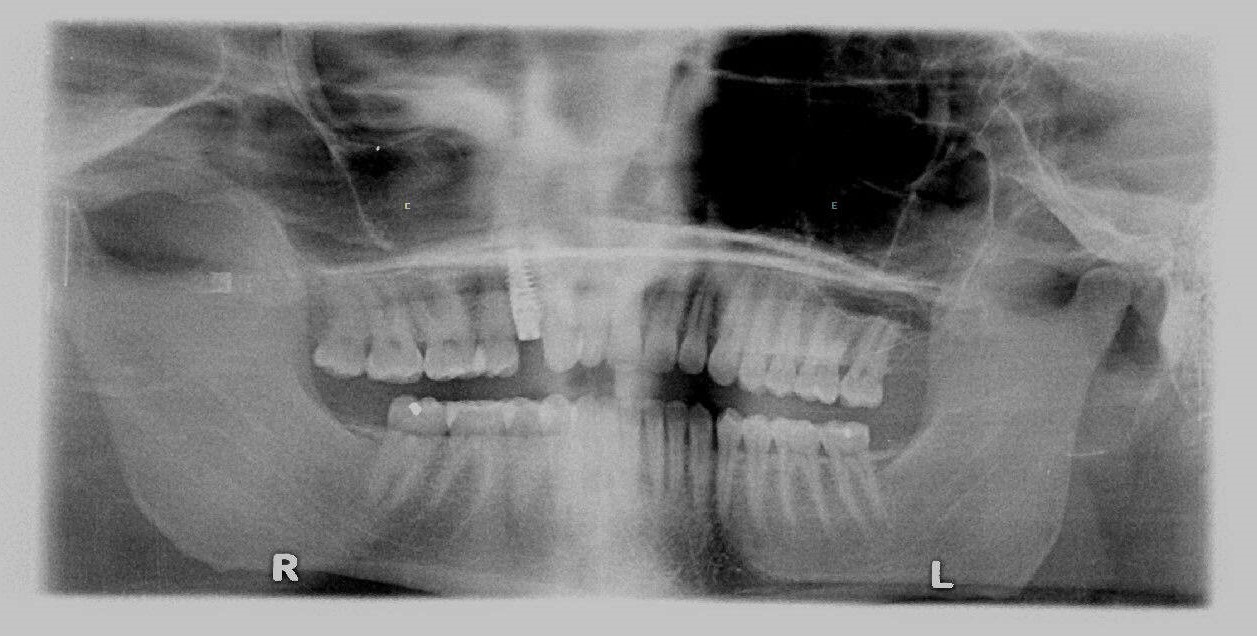
- Odontology
- Histology
- Microbiology
- Sexual assault kits
- DNA testing
- Vitreous fluid analysis
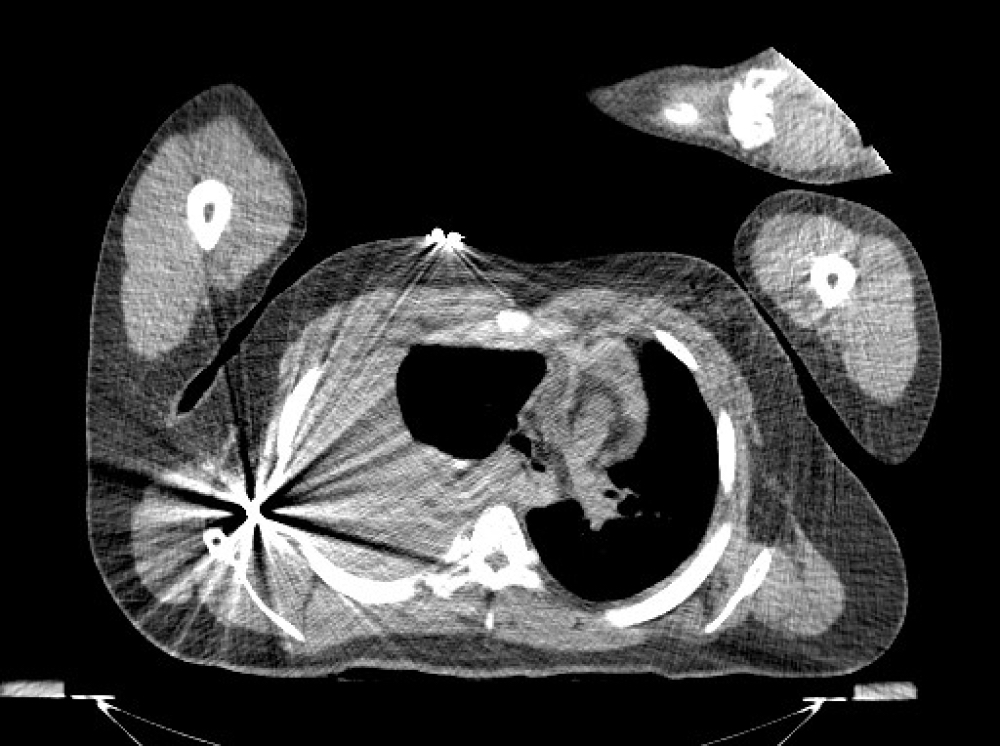
- To identify and document injuries, projectiles, projectile fragments in cases of homicide, incineration, motor vehicle accidents, infant deaths, decomposition or cases of suspicious circumstances (Forensic Sci Med Pathol 2014;10:583)
- Also to positively identify decedents
Methods:
- Conventional radiography, such as whole body Xray scanner (Int J Legal Med 2020;134:655)
- CT scan
- Radiography skeletal survey
- Adjunctive imaging, like fluoroscopy, MRI or CT angiogram, is case dependent
Case examples:
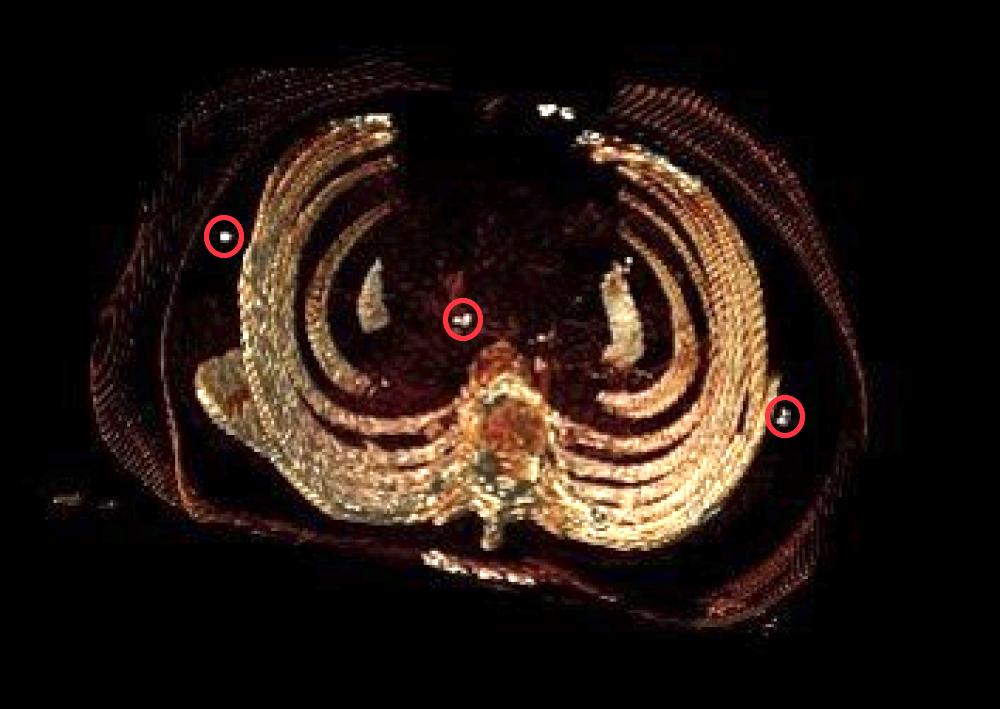
- Images are read by the medical examiner to aid in the gross examination (recovering projectiles or documenting fractures) or a formal consult is performed by a radiologist
- Conventional radiography is used to visualize the bones for fractures and lesions, age estimation and detect foreign bodies (projectiles or projectile fragments)
- Radiography skeletal survey and CT are utilized in child abuse (Forensic Sci Int 2006;164:131)
- MRI is good for visualizing soft tissue and helpful in blunt force trauma, like strangulation
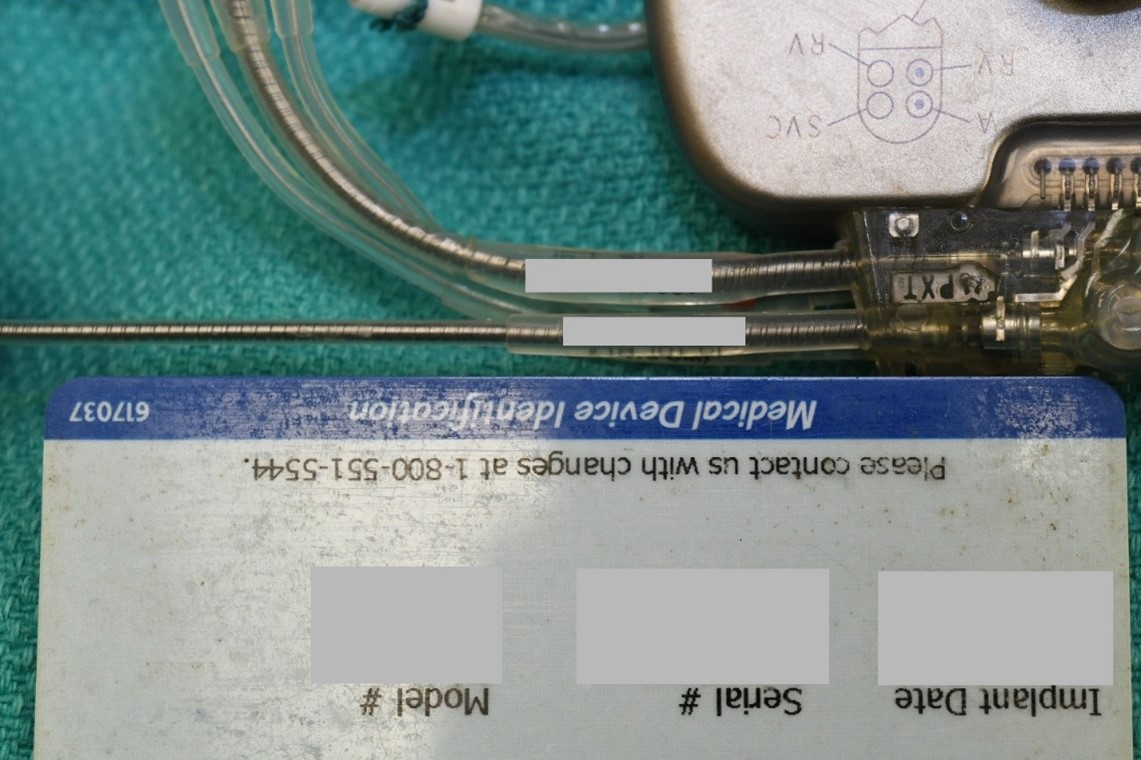
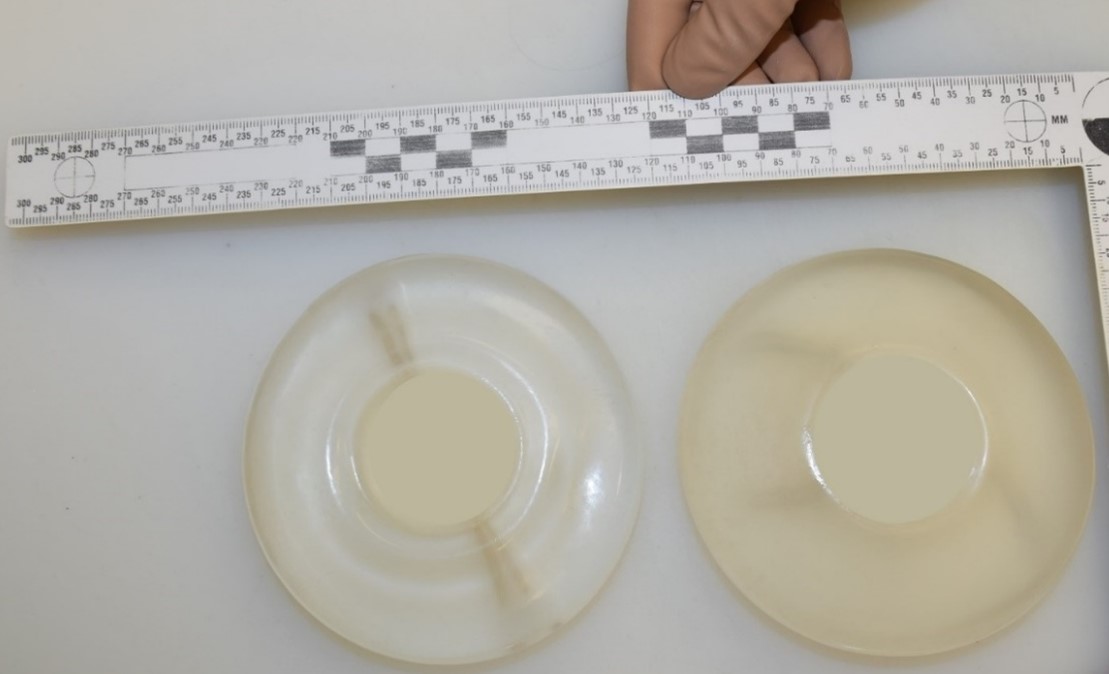
- Tentatively identified decedents with medical hardware on imaging and medical records to document the previous surgery (helps with positive ID)
Limitations:
- Conventional radiology and CT cannot accurately visualize soft tissue and the image quality is user dependent
Essential features:
- Postmortem radiology is used to identify and document projectiles, projectile fragments, motor vehicle accidents, infant deaths and decomposition
- Conventional radiology is performed to visualize bone fractures and detect foreign objects, like projectile or projectile fragments
- Radiograph skeletal survey is done in all cases of child abuse
Contributed by Allecia Wilson, M.D.
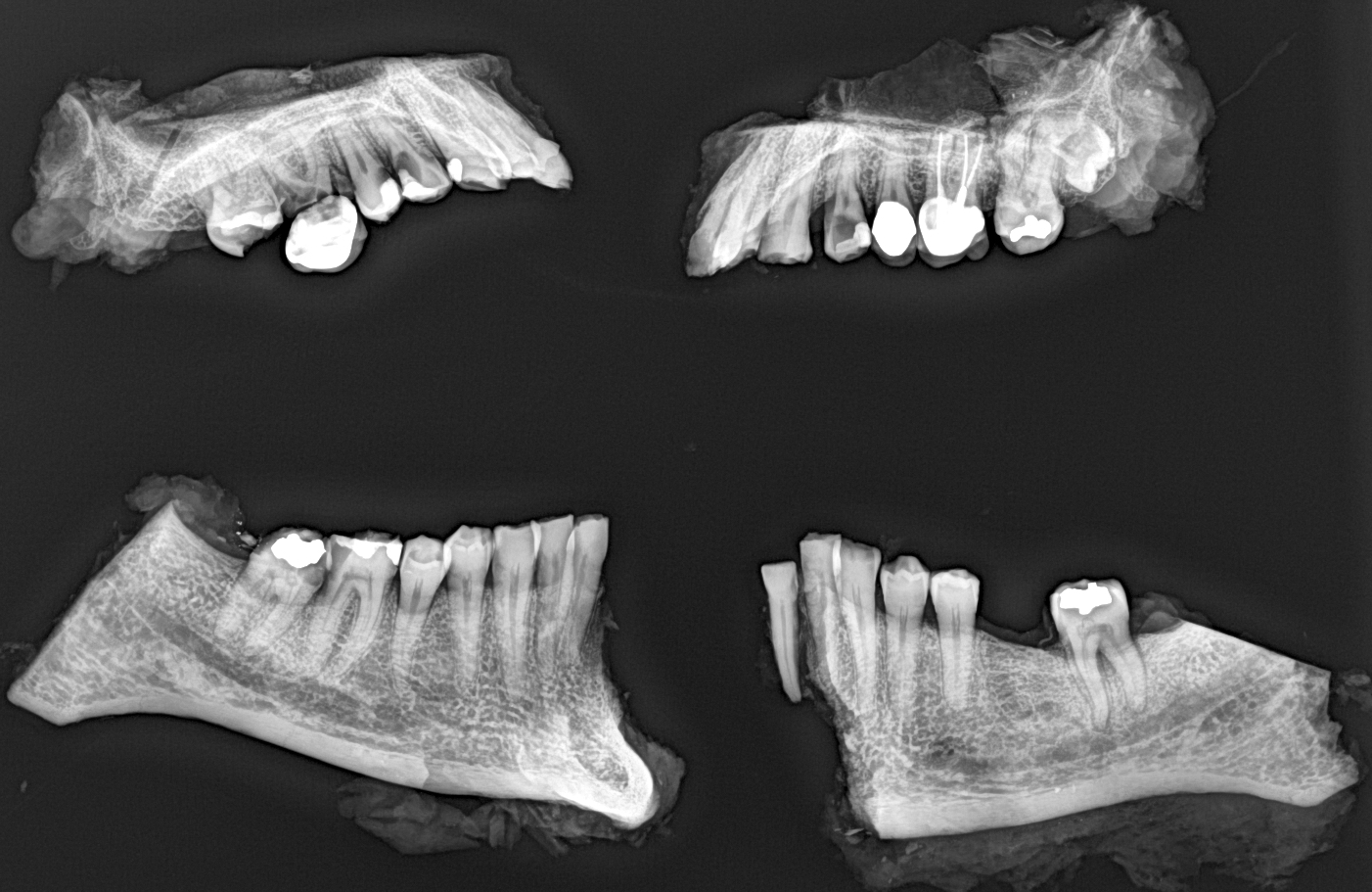
- To positively identify decedents when visual identification is not possible in cases such as incineration, decomposition, severe disfigurement, skeletonization and catastrophic events with multiple unidentified dead bodies, such as airline accidents, terrorist attacks and industrial accidents (StatPearls: Forensic Odontology [Accessed 3 June 2021])
How to perform:
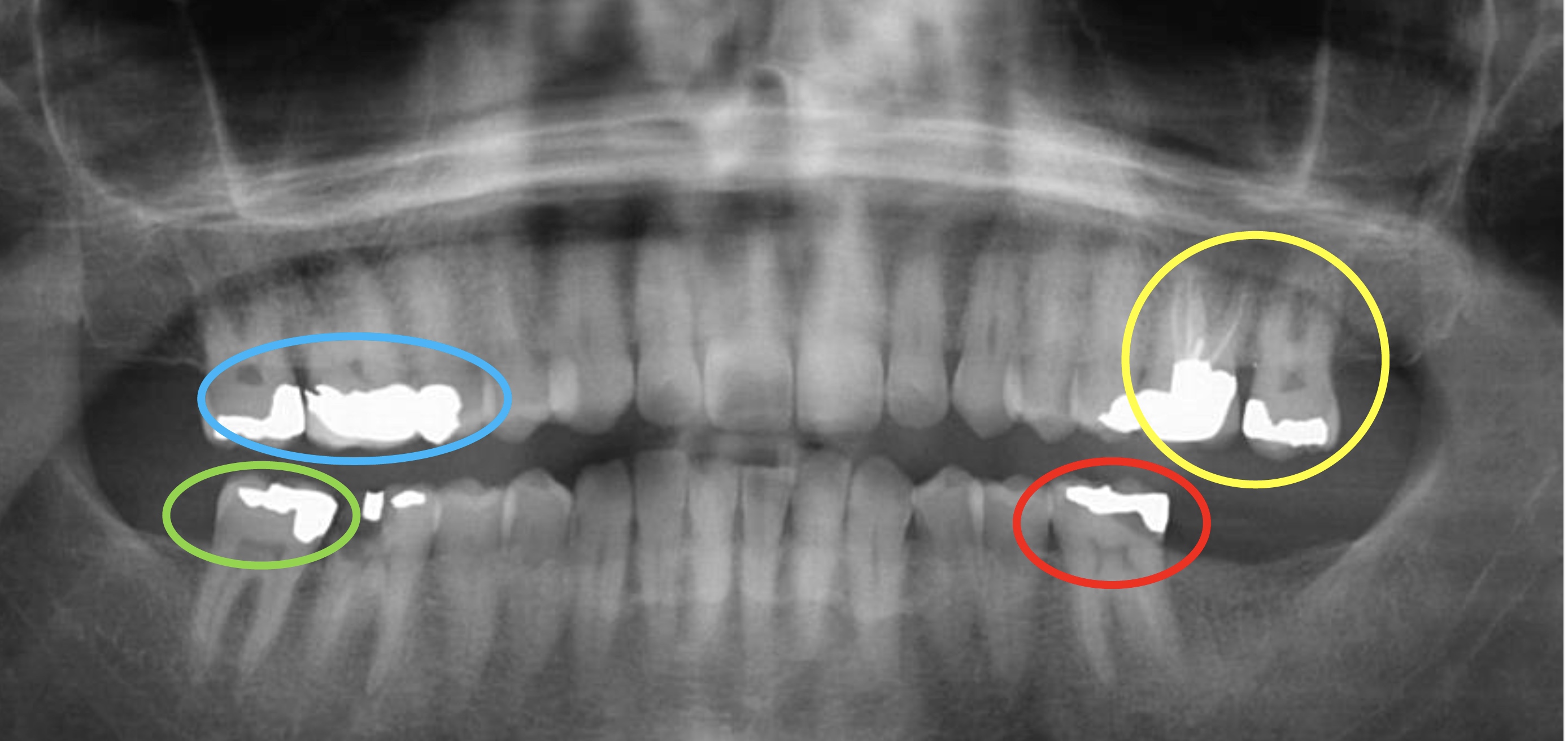
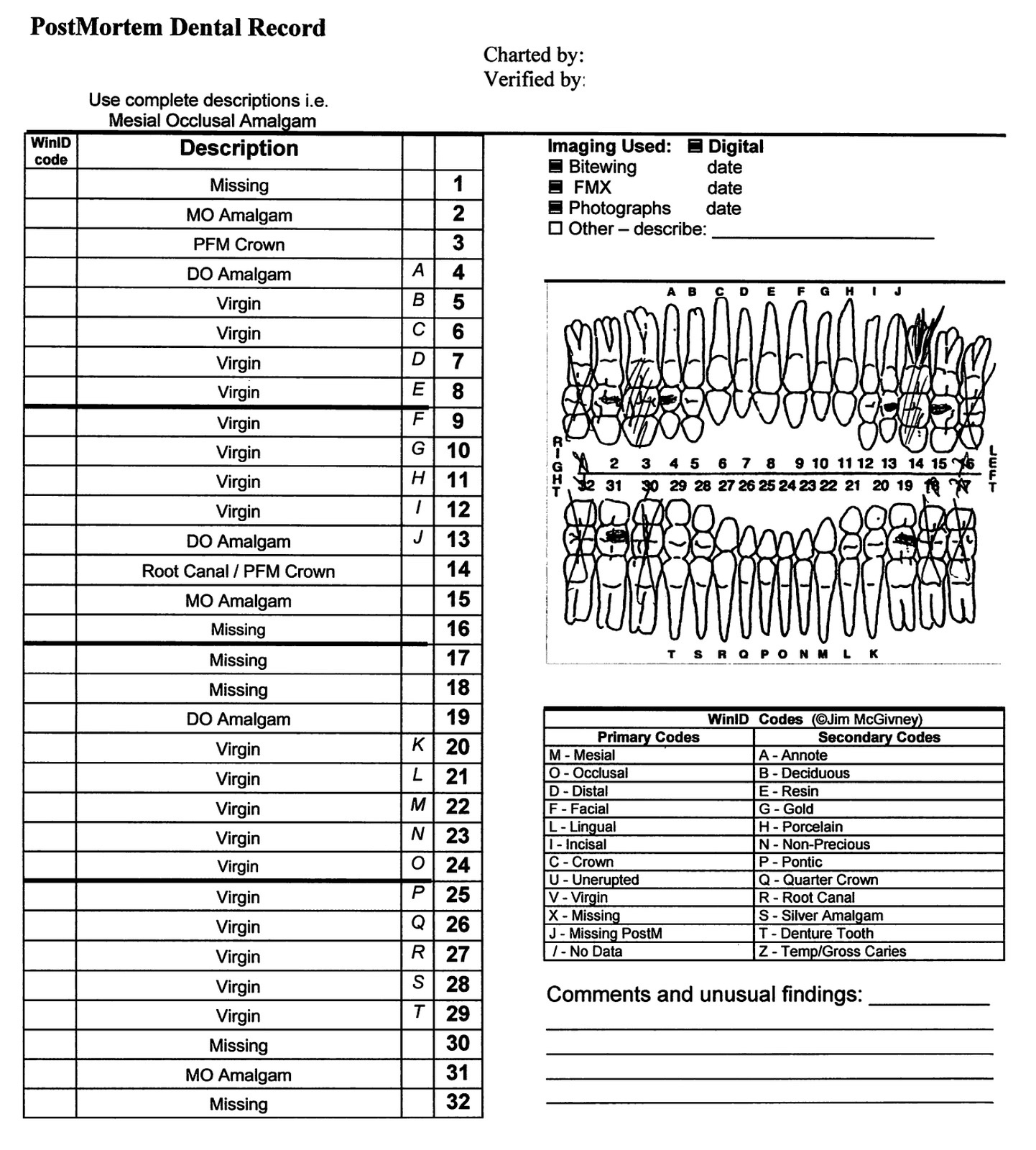
- Forensic dentist photographs the upper and lower teeth and performs a dental exam that includes teeth charting or a dentogram for location and type of teeth fractures, decay, fillings and prostheses
- Comparative analysis is done between the postmortem dental exam and antemortem dental records that include a dentogram and radiology (J Oral Maxillofac Pathol 2019;23:164)
Case examples:
- Antemortem radiology is more specific because fillings are unique to an individual and are stagnant over time, versus dental charting, which may be illegible or frequently change
- Presumptive identification of the decedent can be used to obtain antemortem dental records
- Presumptive identifications include tattoos, government identification and a patient's name on prescription medication or medical records, along with others
Limitations:
- Age dependent; pediatric cases are limited by their growth and development
- Challenging to perform on edentulous decedents or those with poor dentition
Essential features:
- Postmortem dentogram is performed and compared with antemortem dental records to positively identify an unknown decedent
- Antemortem radiology is best because fillings are unique to an individual and are stagnant over time
Contributed by Allecia Wilson, M.D.
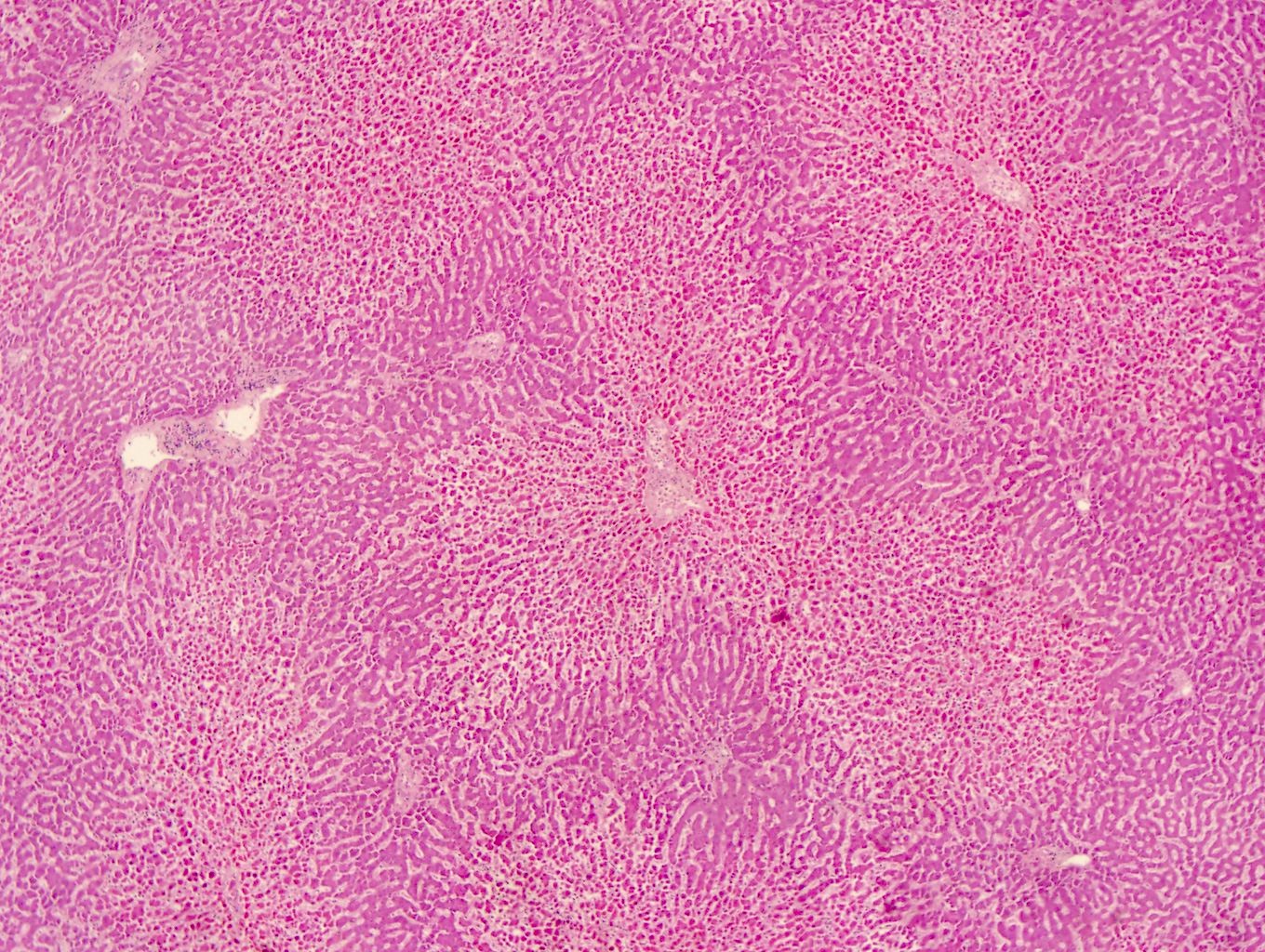
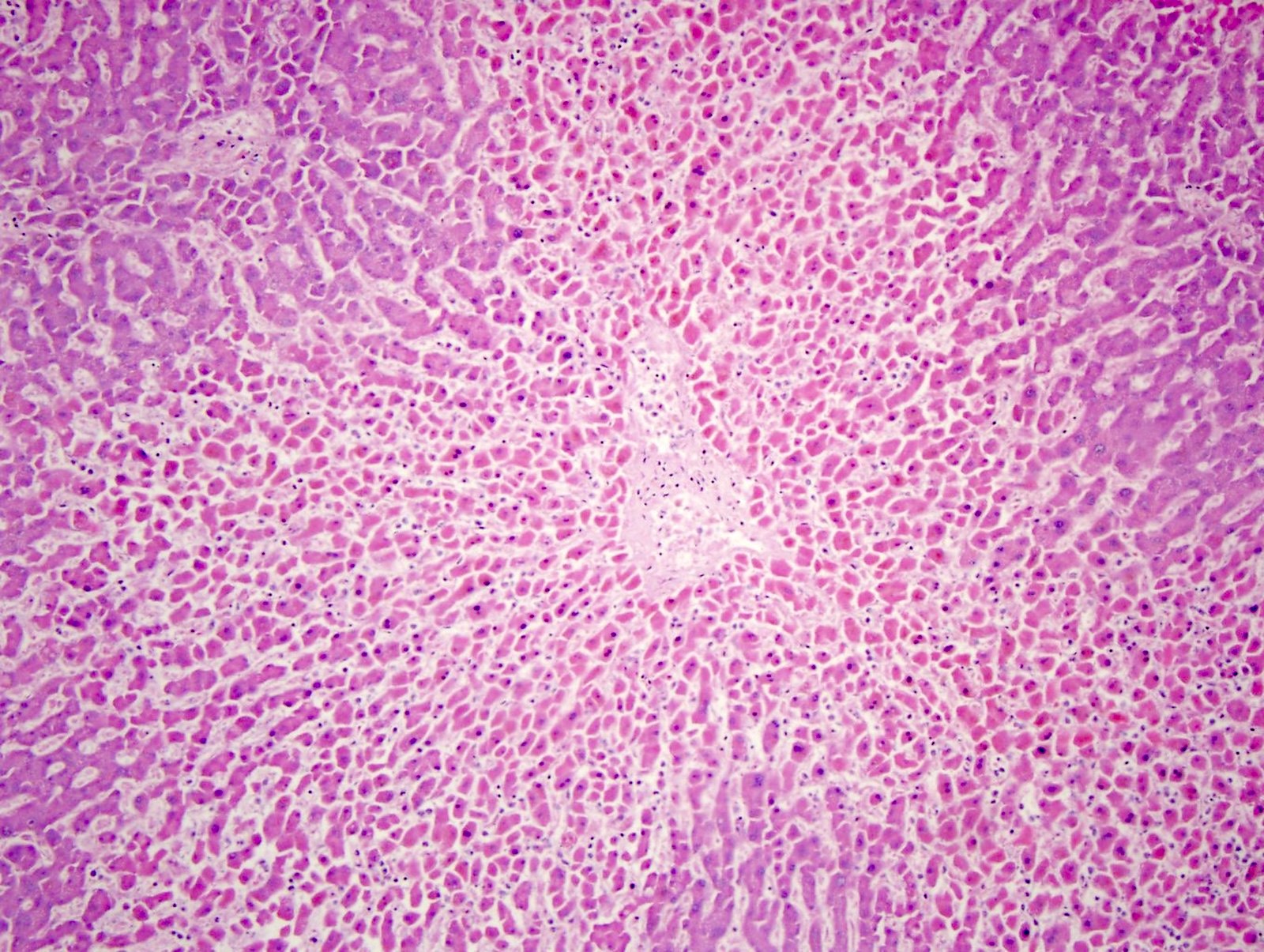
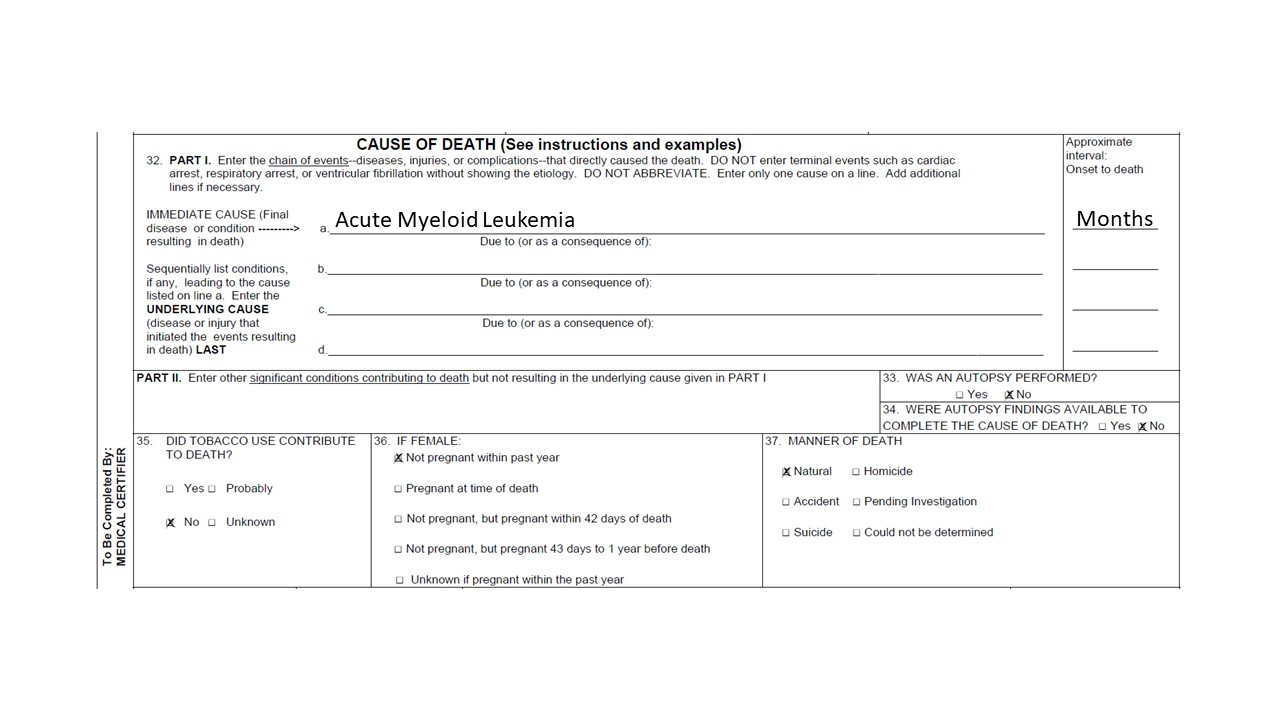
- To support or establish the COD and MOD
- Performed in cases of drug overdose, natural deaths, sudden unexplained death and all pediatric deaths
How to perform:
- Tissue sections are routinely taken from the heart, lungs, kidneys, liver and brain
- Tissue sections are processed and stained with H&E for standard histology
- Special stains can be performed, depending on the H&E
- Special stains include Masson trichrome for fibrosis, Prussian blue for hemosiderin, PAS or GMS for fungi, Gram stain for bacteria, Ziehl-Neelson for mycobacteria and Congo red for amyloid (Acad Forensic Pathol 2018;8:426)
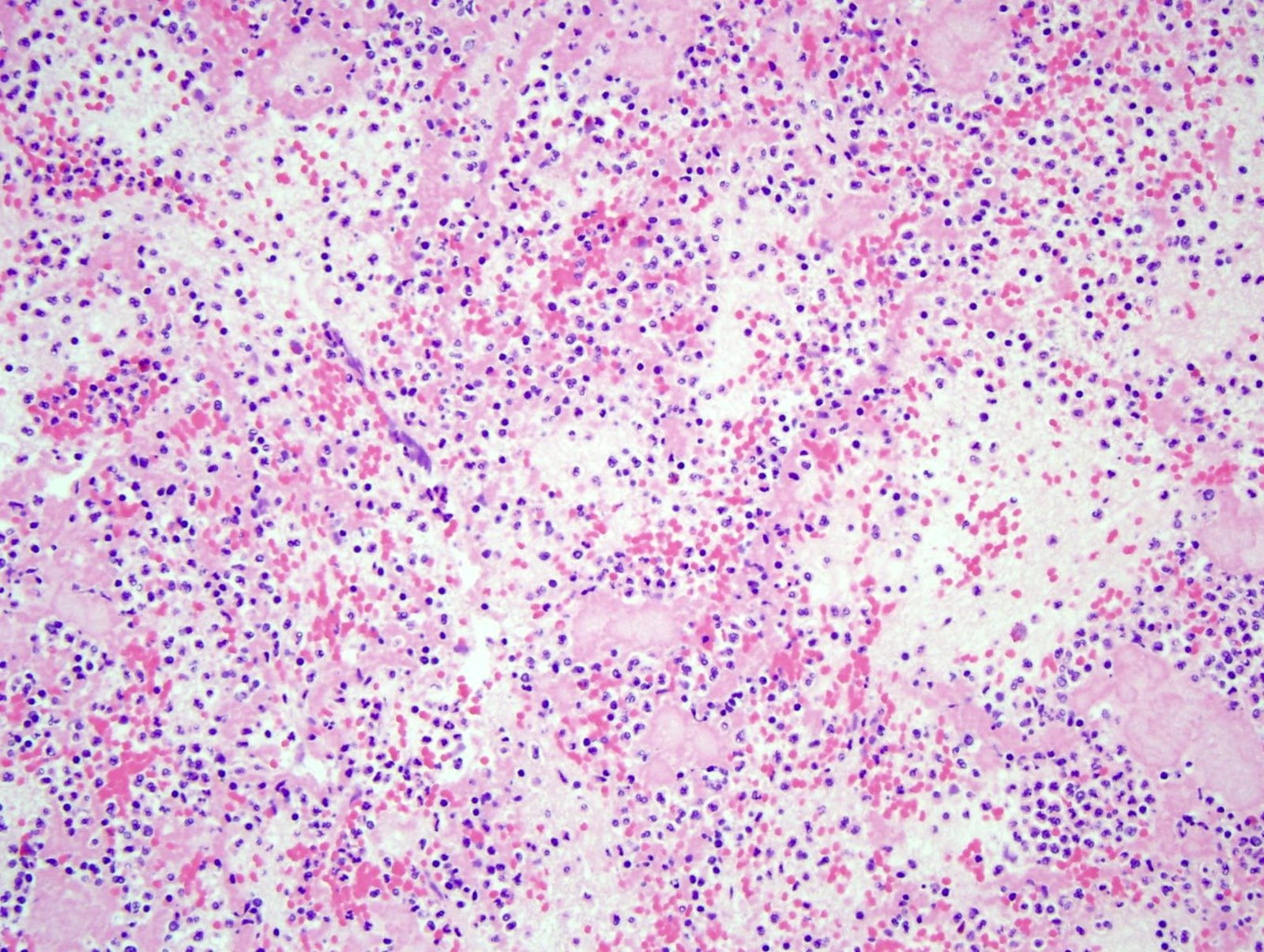
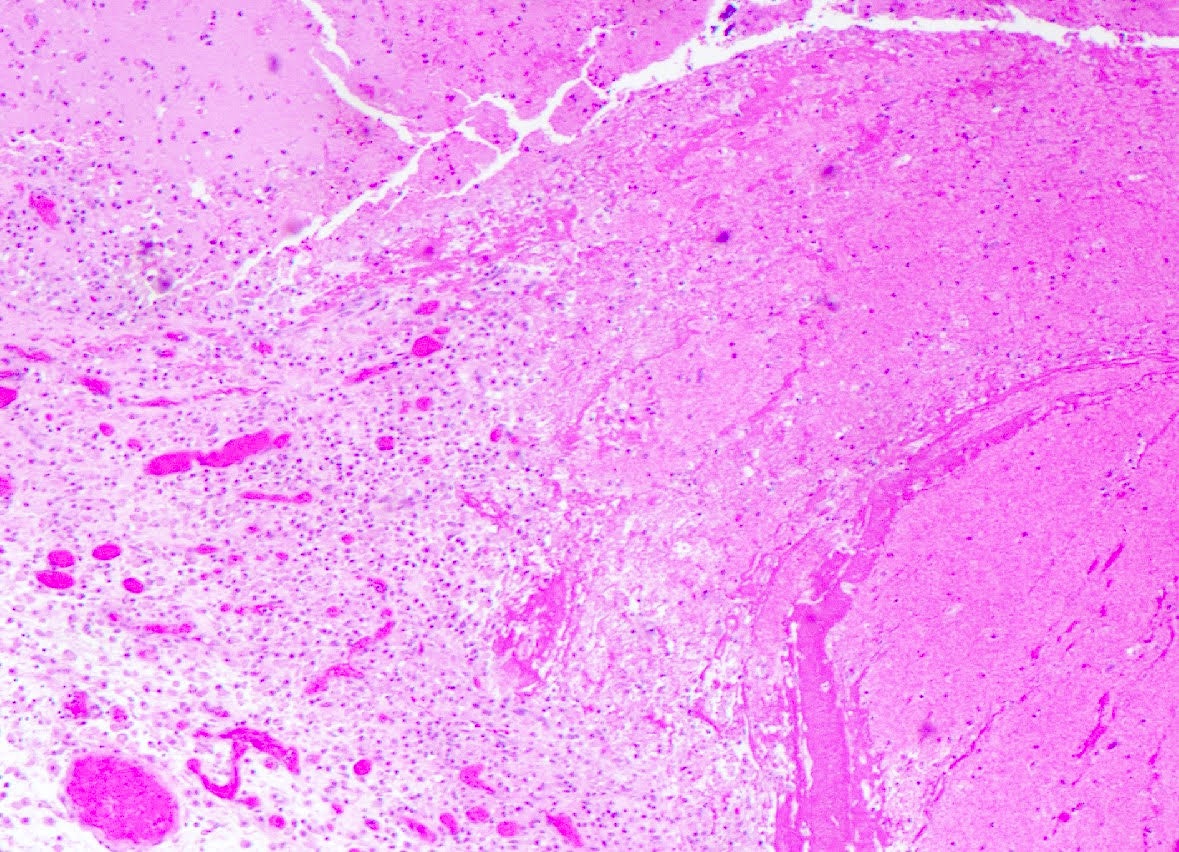
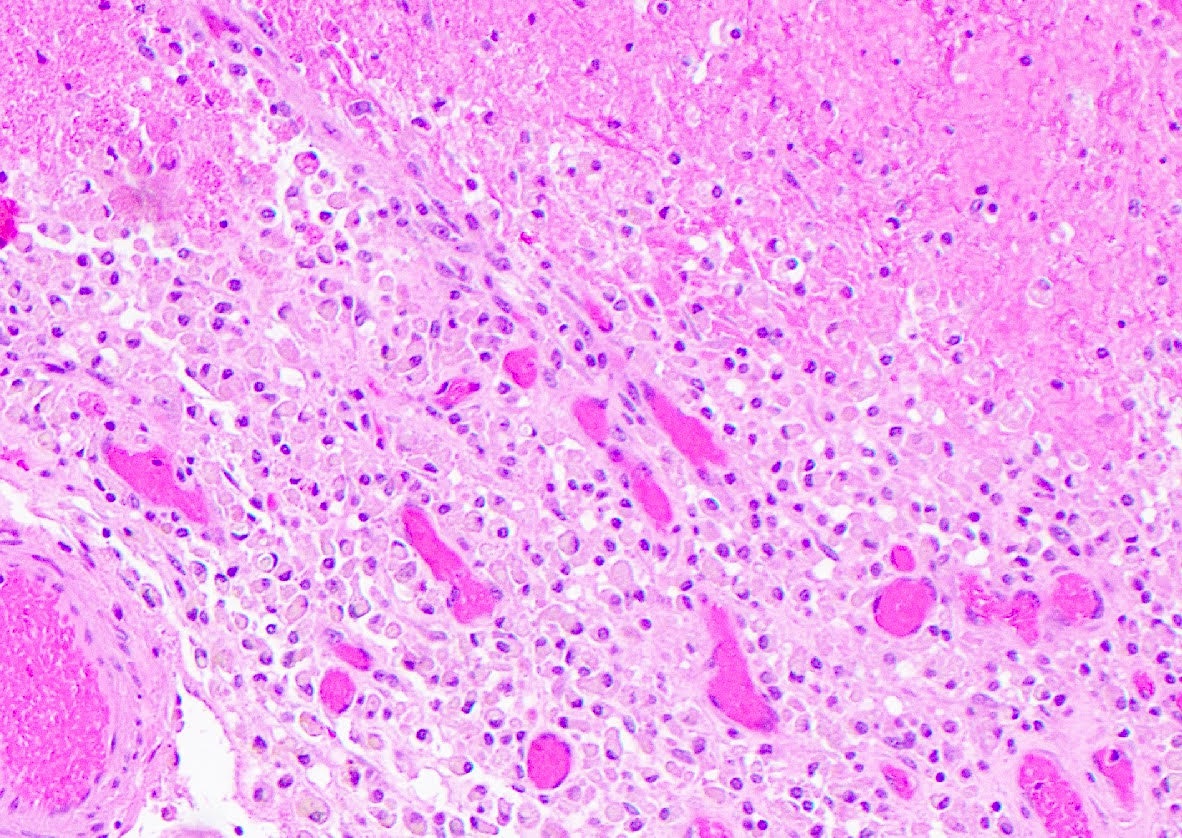
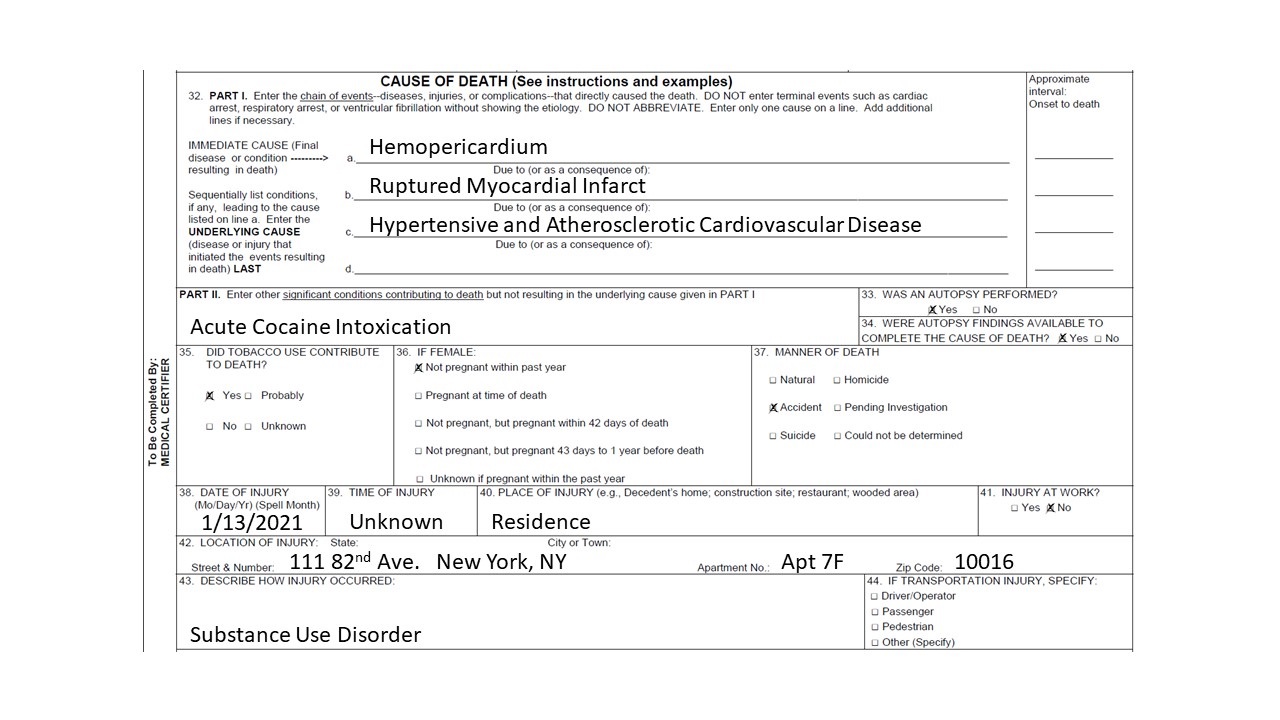
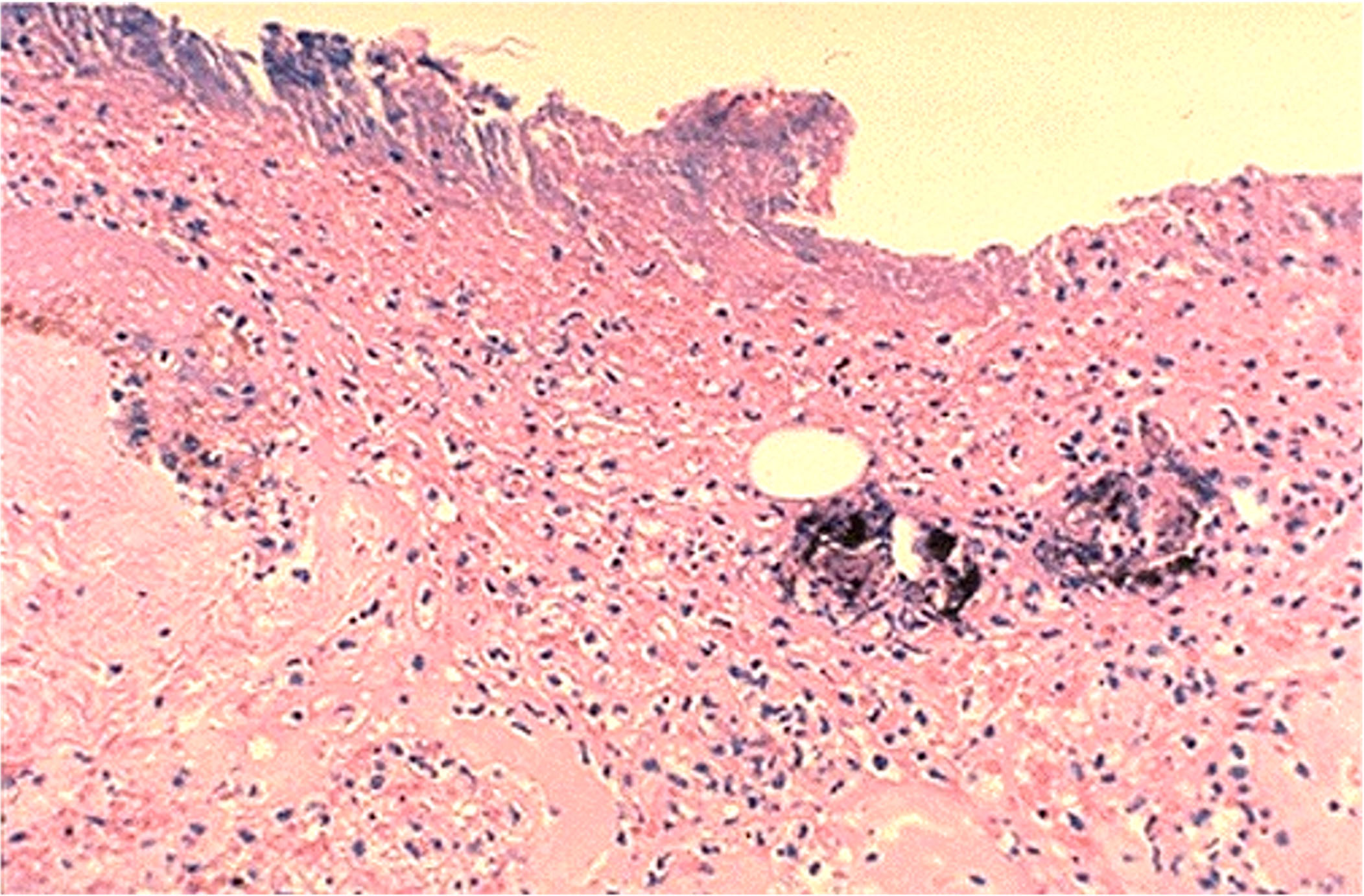
Case examples:
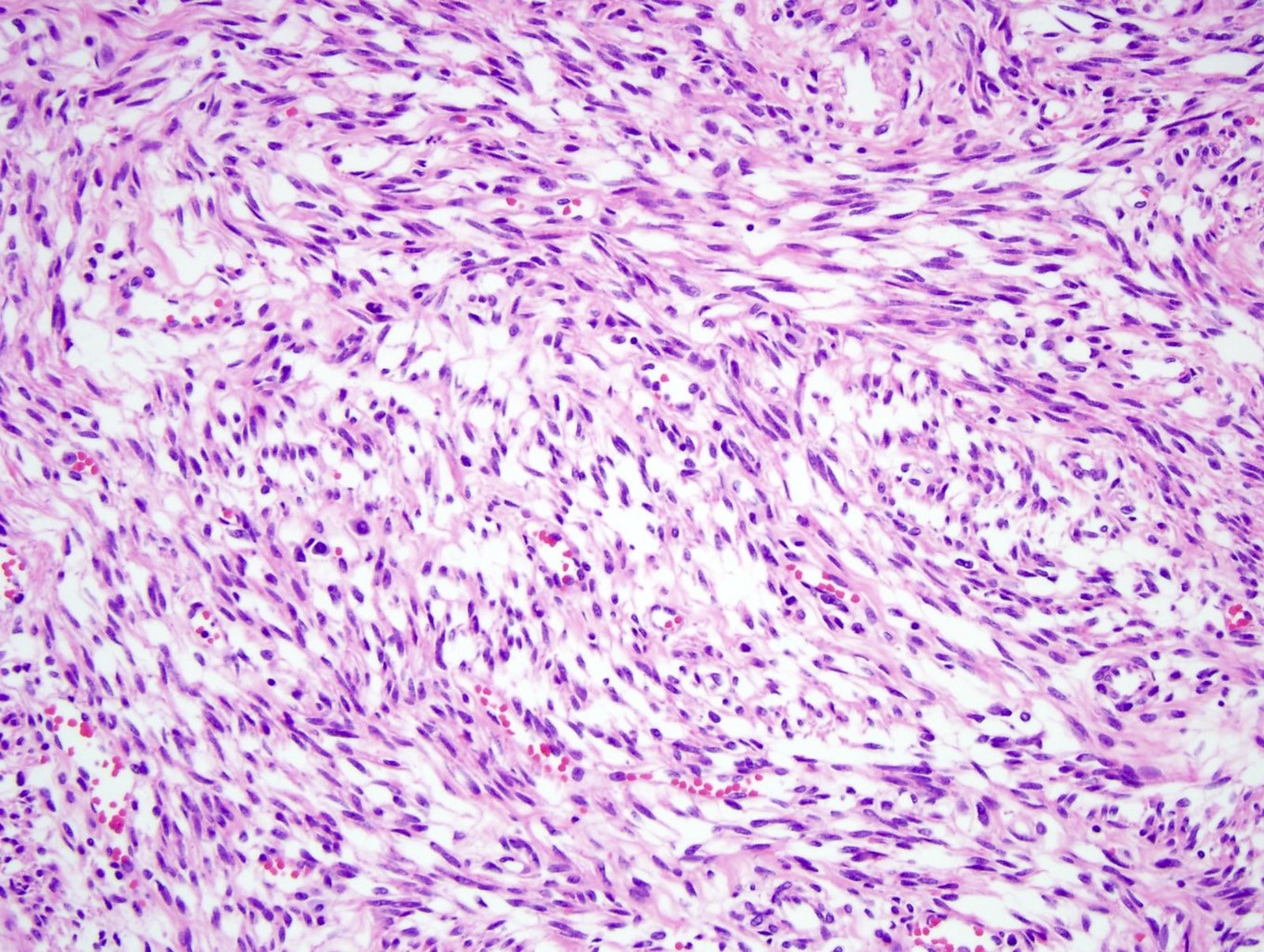
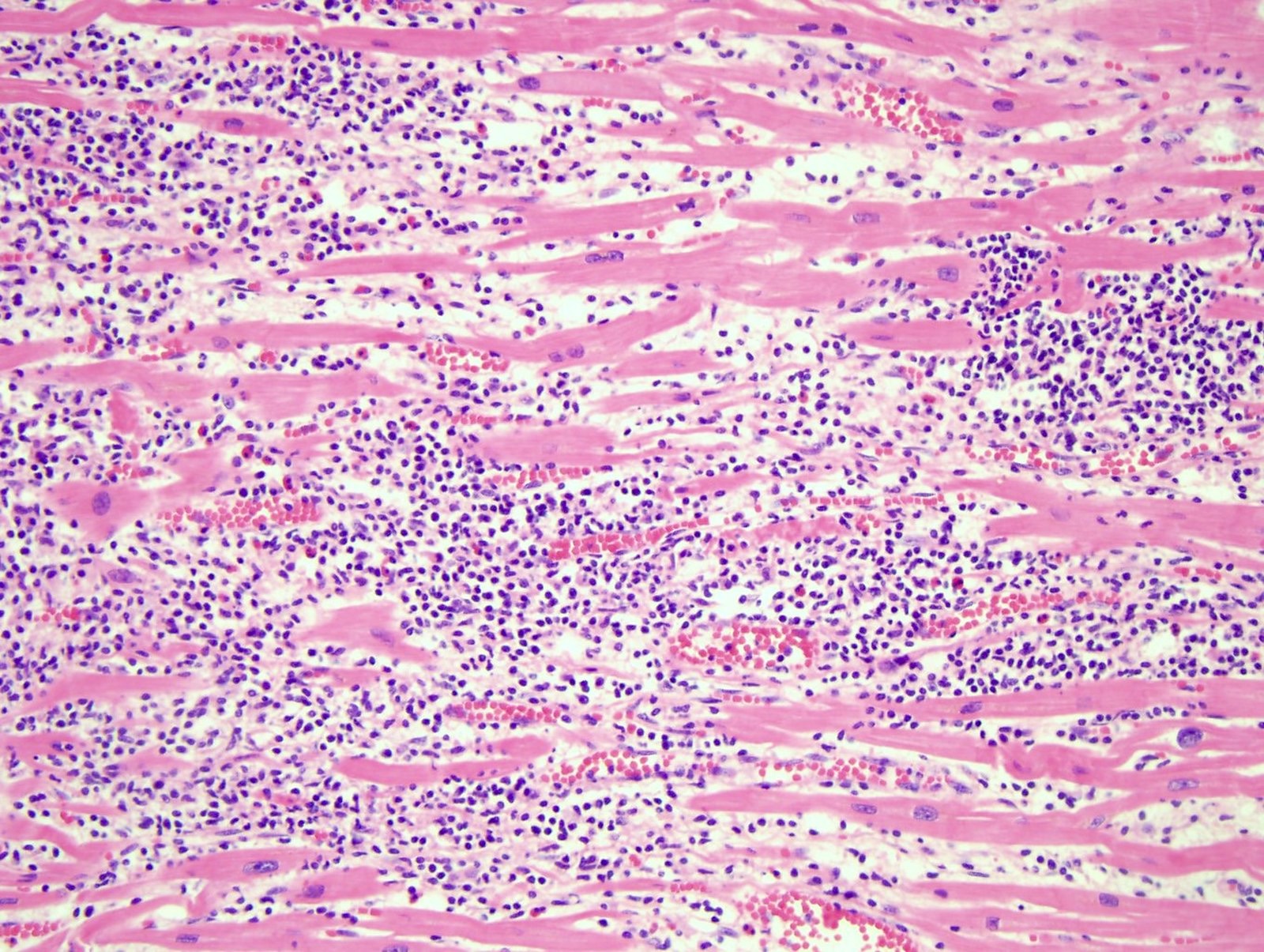
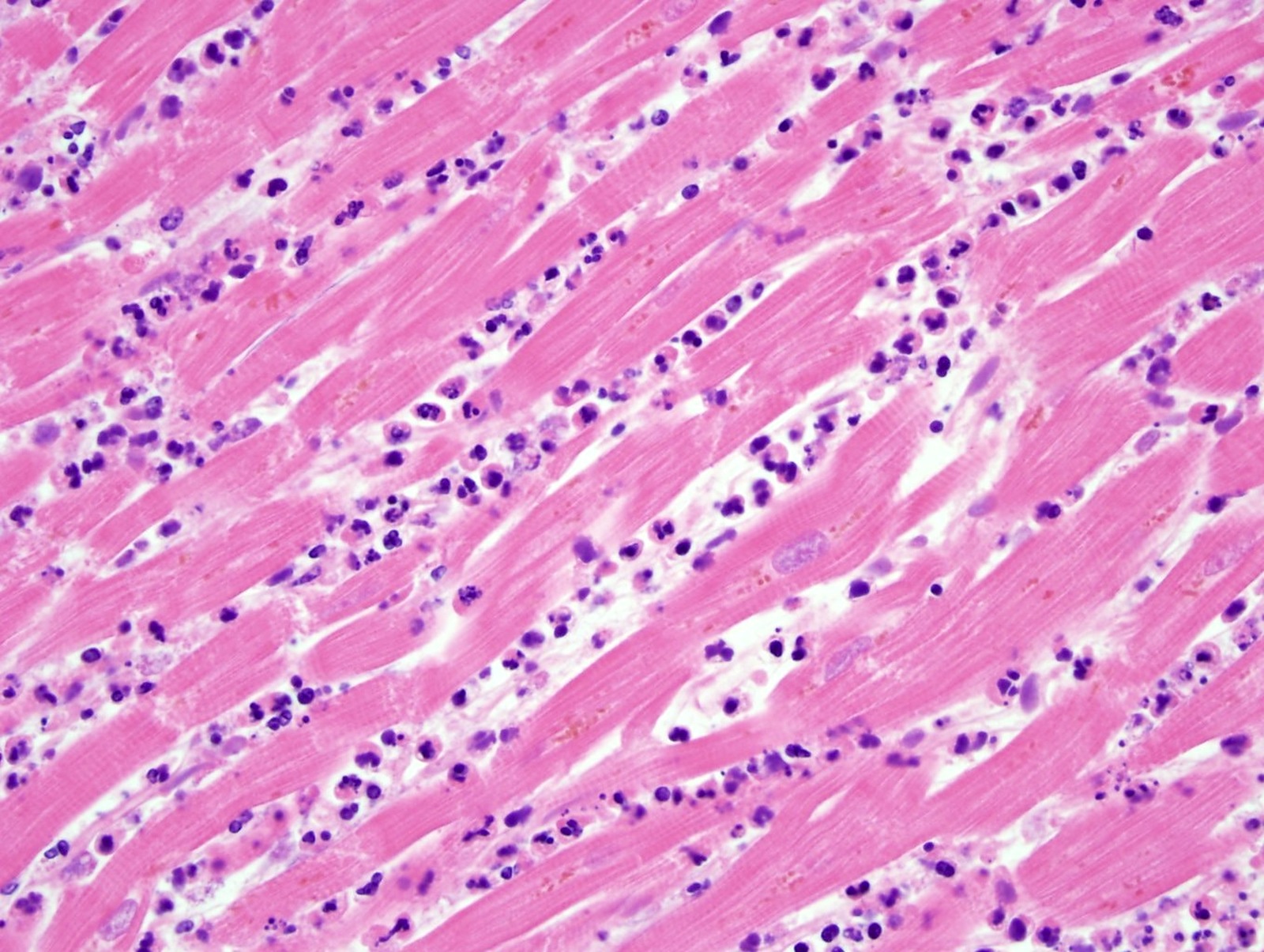
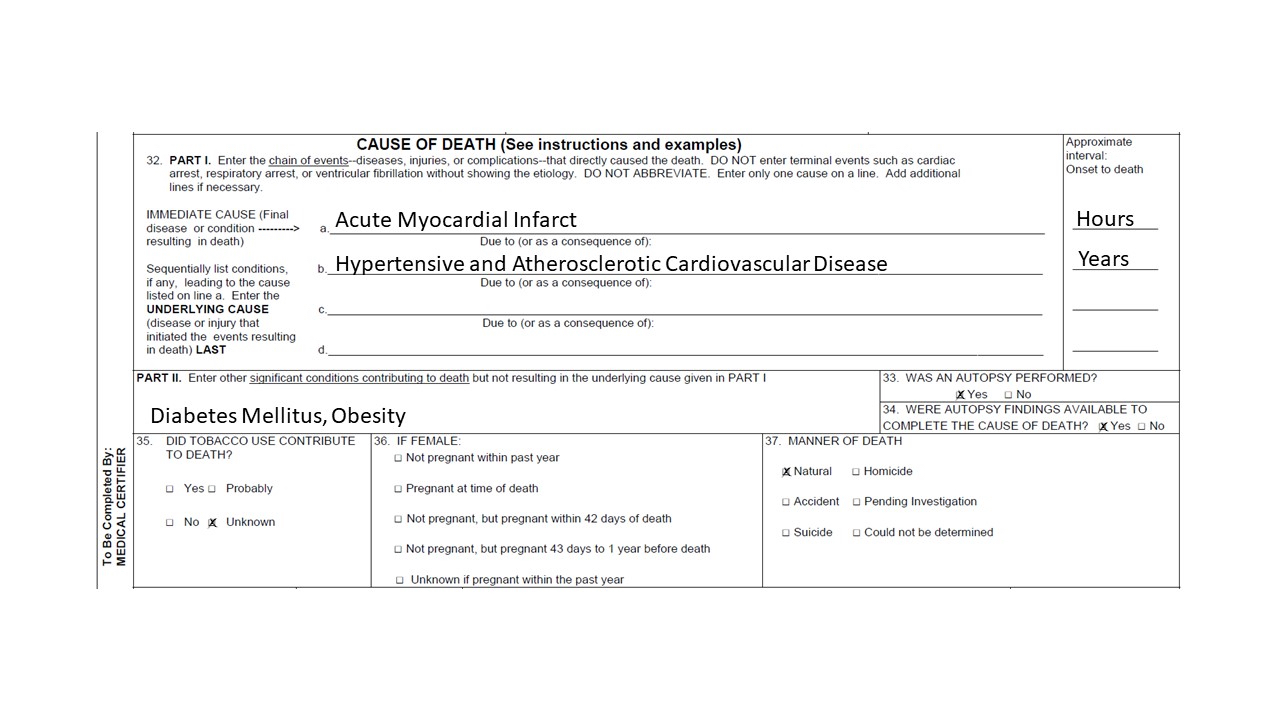
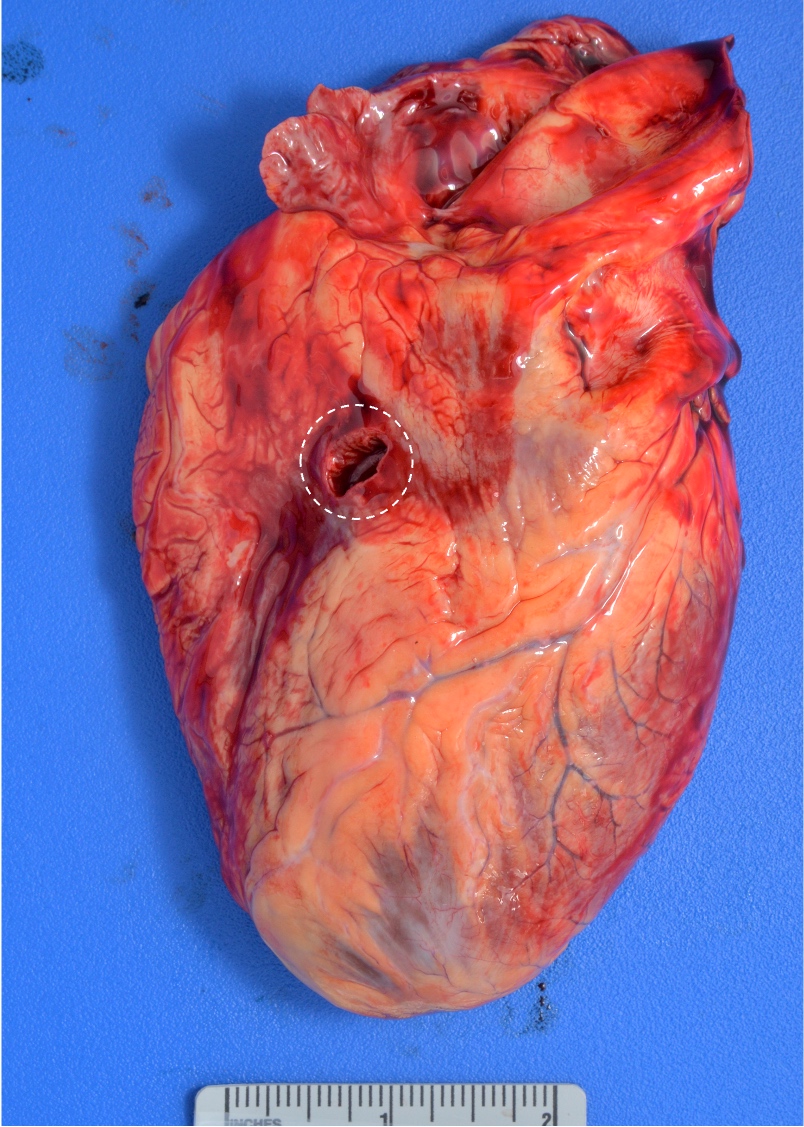
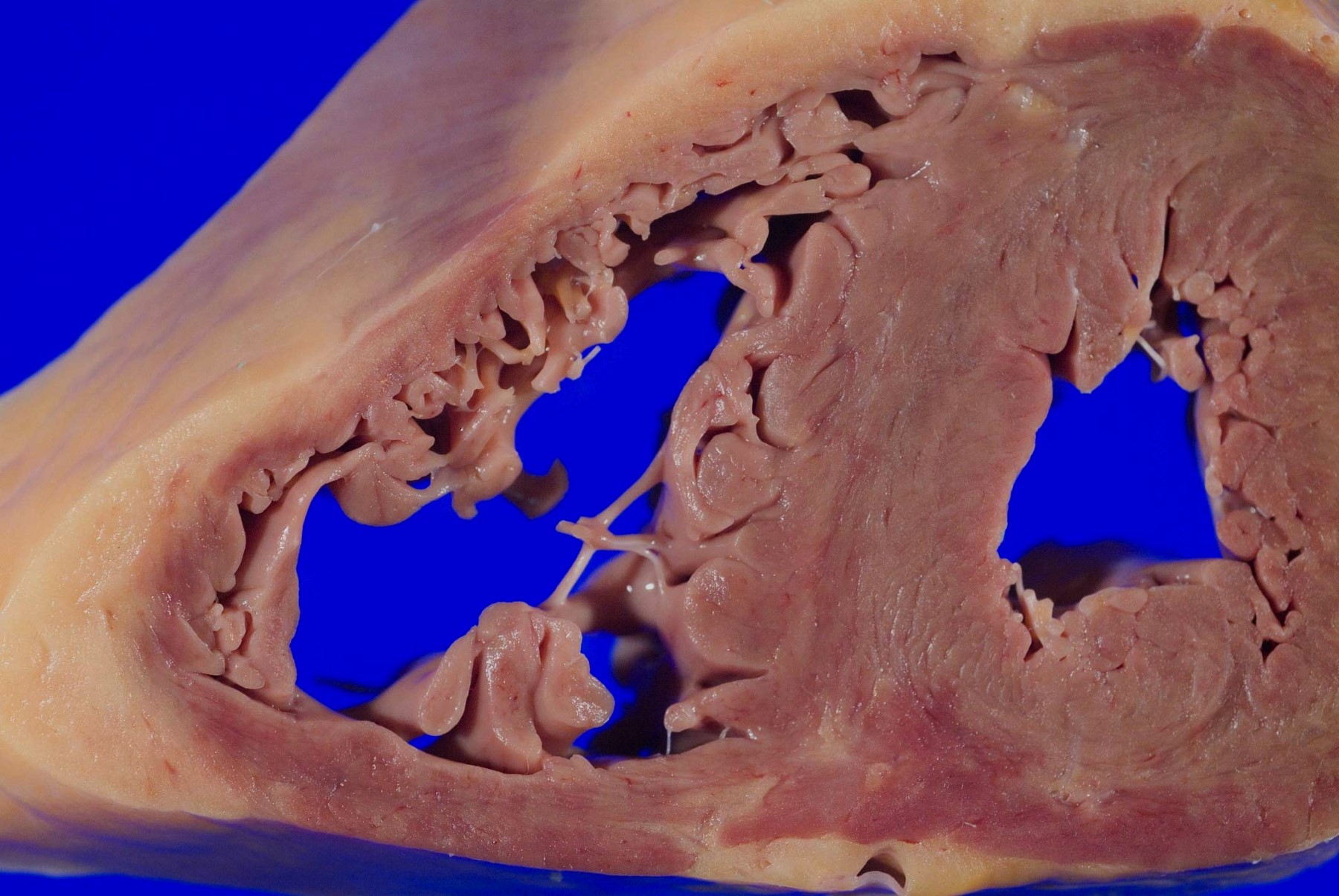
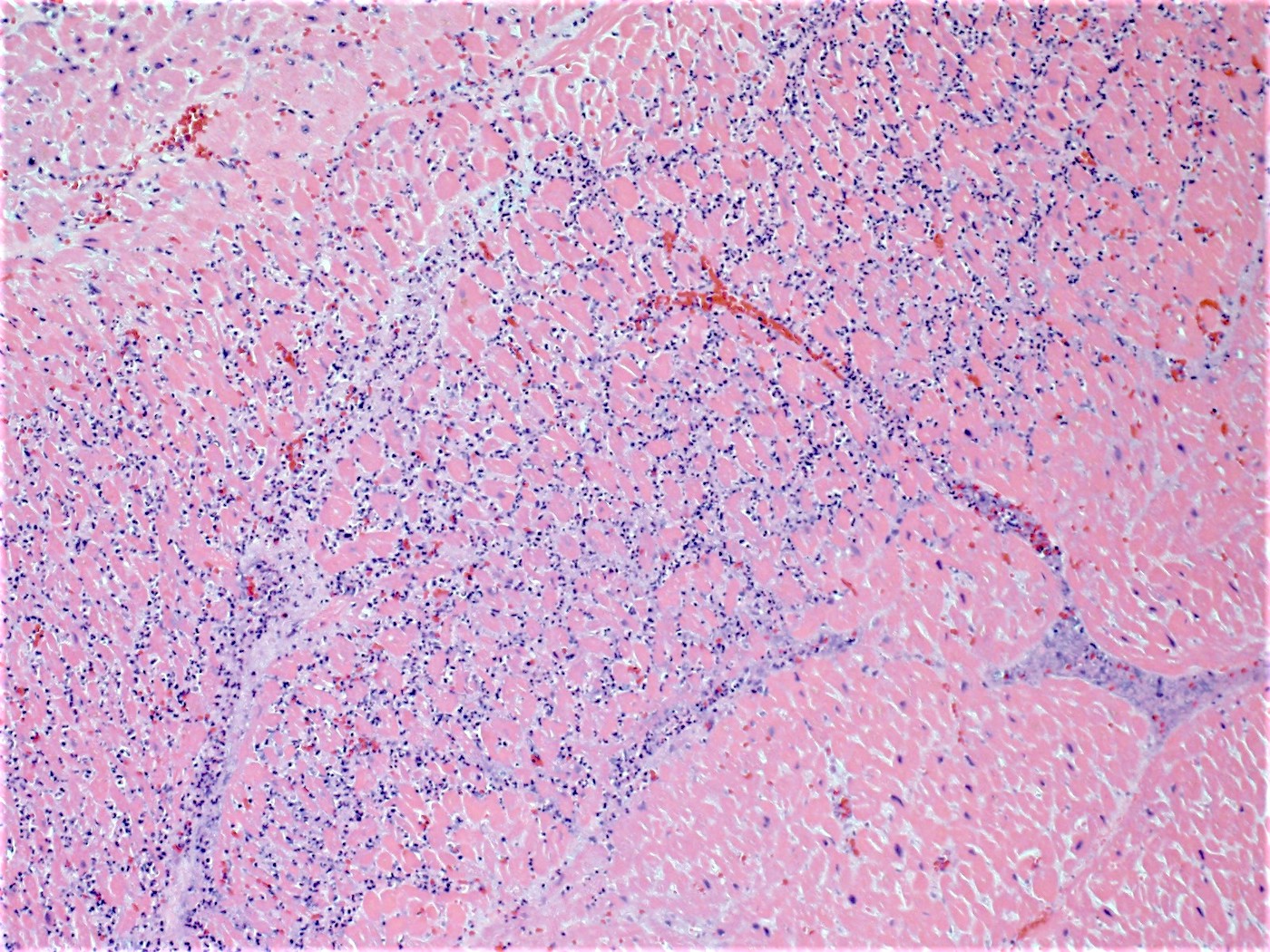
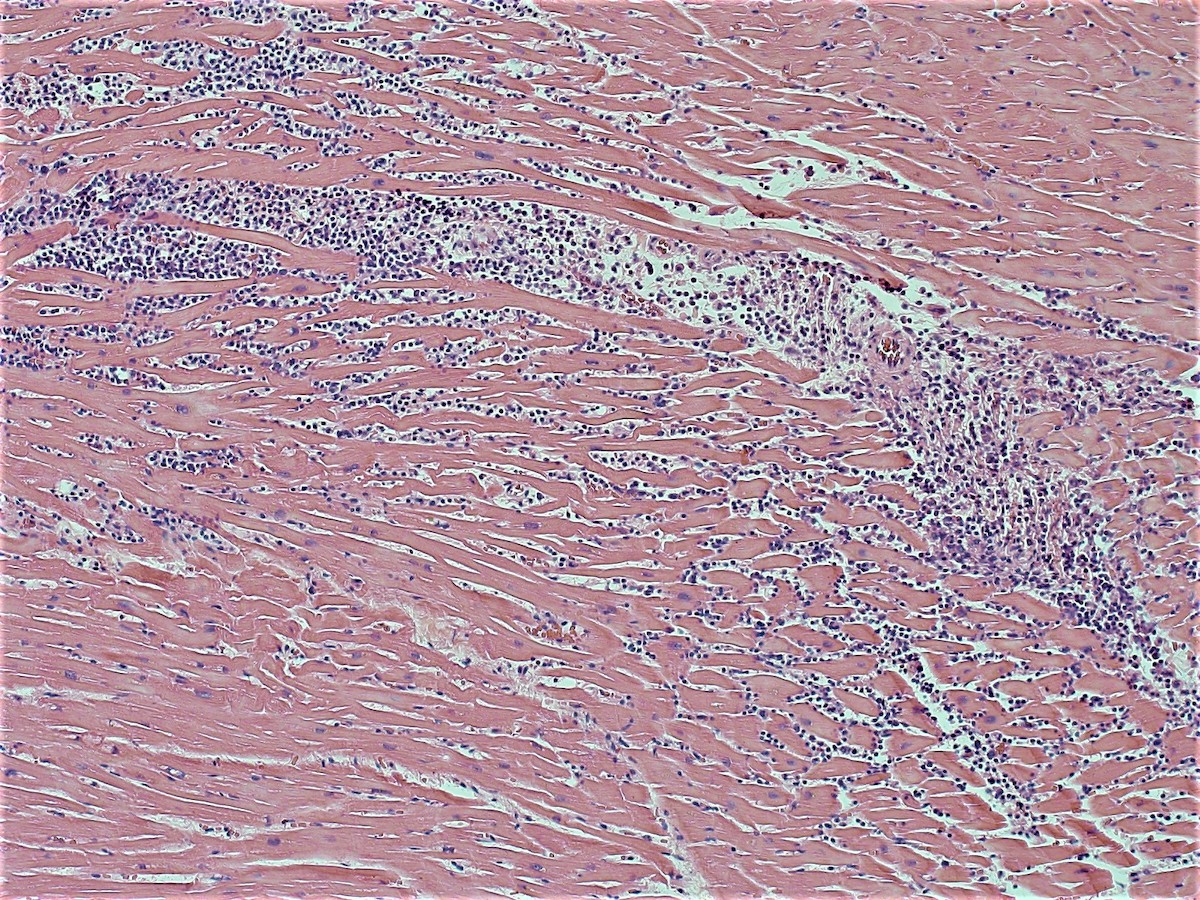
- Cardiac
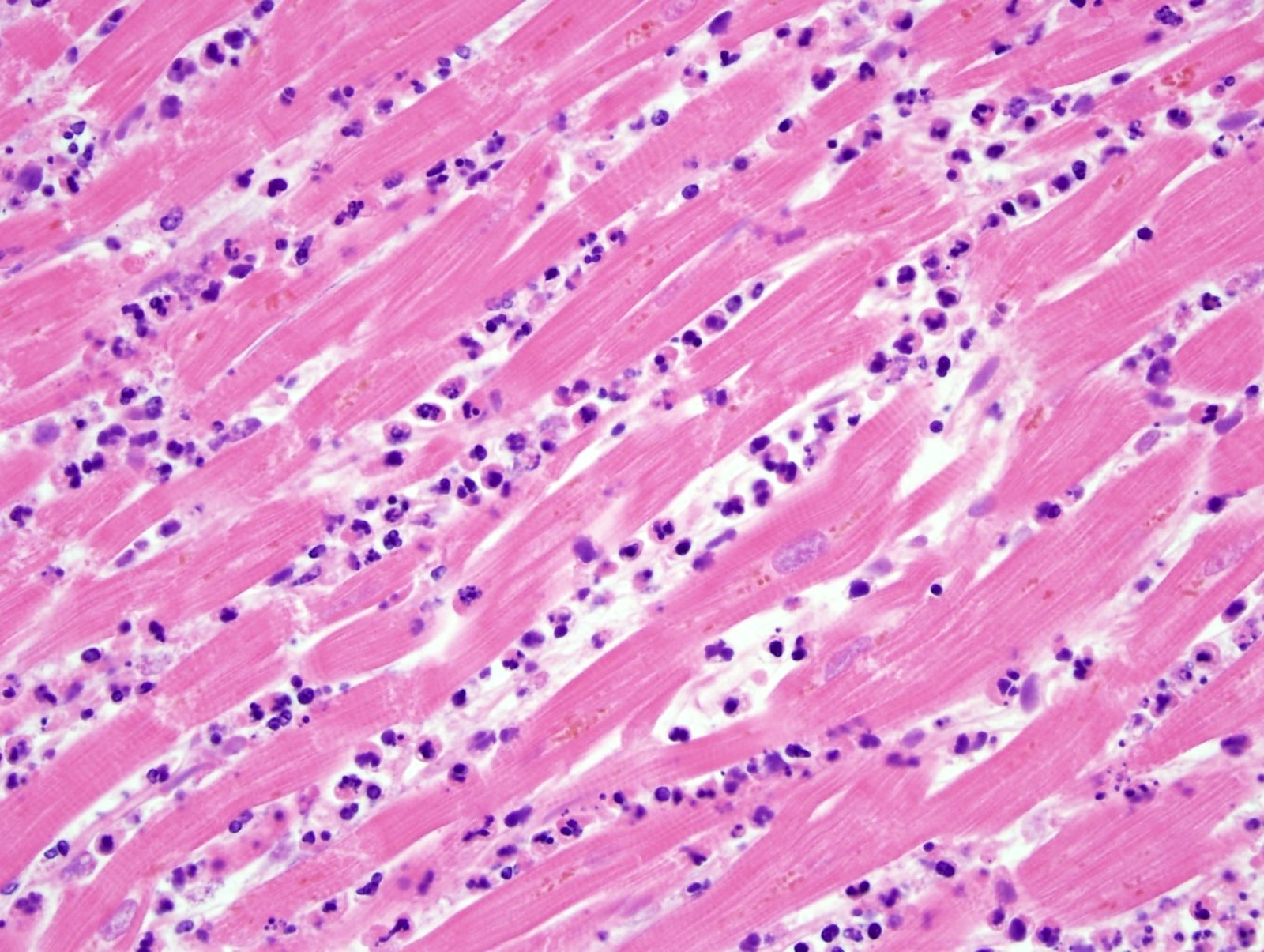
- Histology helps to date a myocardial infarction:
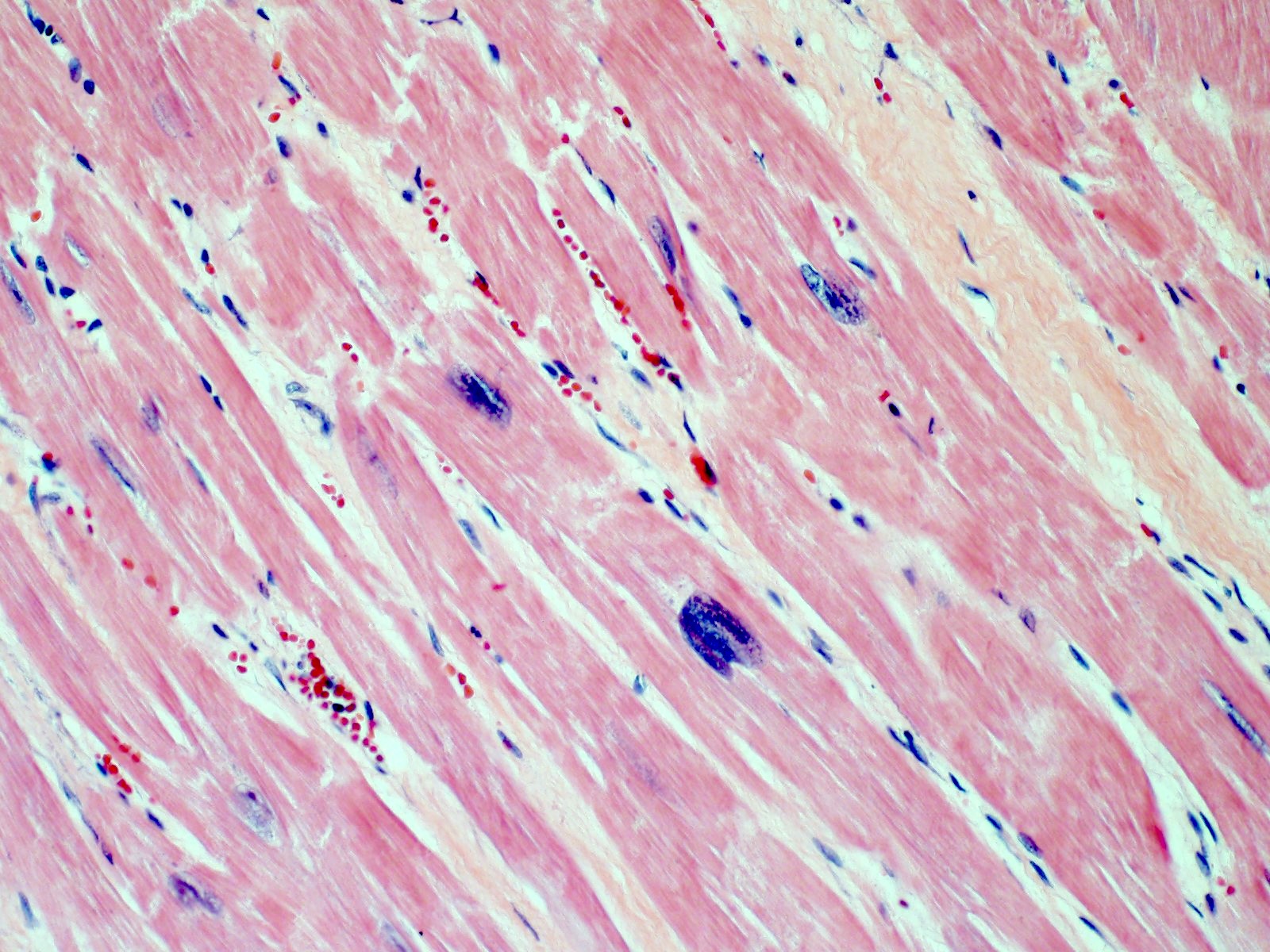
- Acute myocardial infarction > 4 hours = myocyte necrosis with polymorphonuclear neutrophils (PMNs)
- Subacute myocardial infarction > 3 days = hemosiderin laden macrophages and granulation tissue
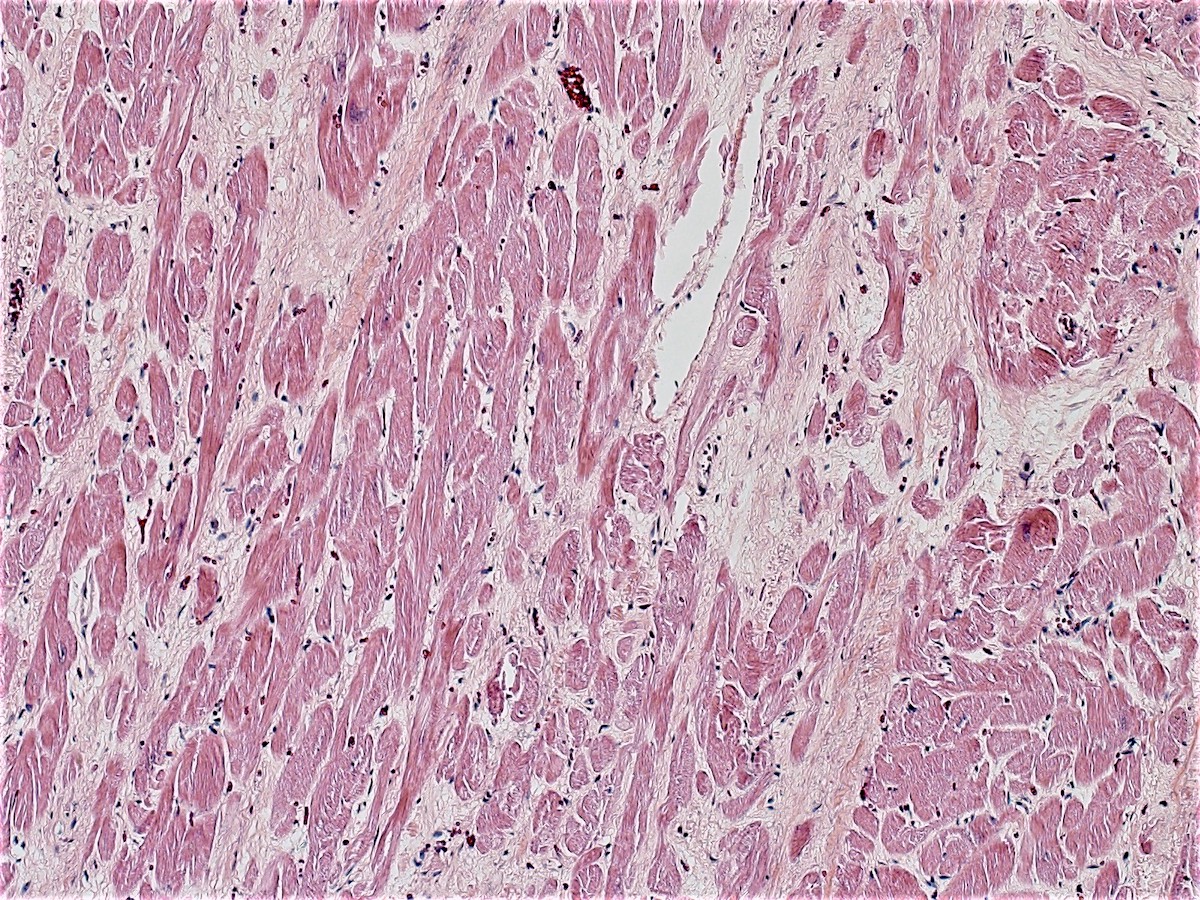
- Chronic myocardial infarction > 10 days = collagen deposition
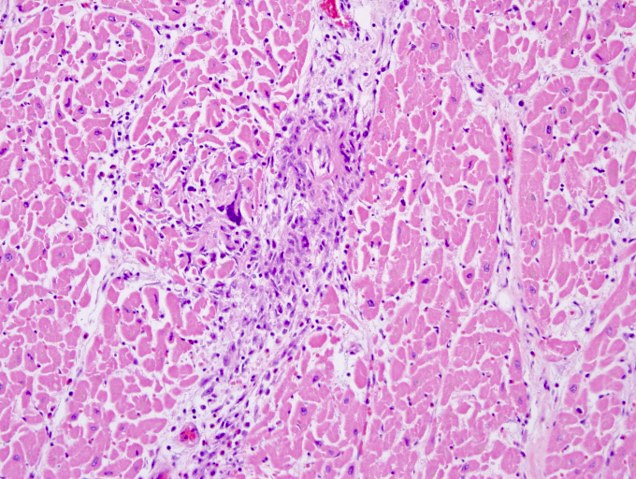
- Acute viral myocarditis shows a lymphocytic infiltration in the myocardium and myocardial necrosis (Forensic Pathology Reviews 2008;5:239)
- Histology helps to date a myocardial infarction:
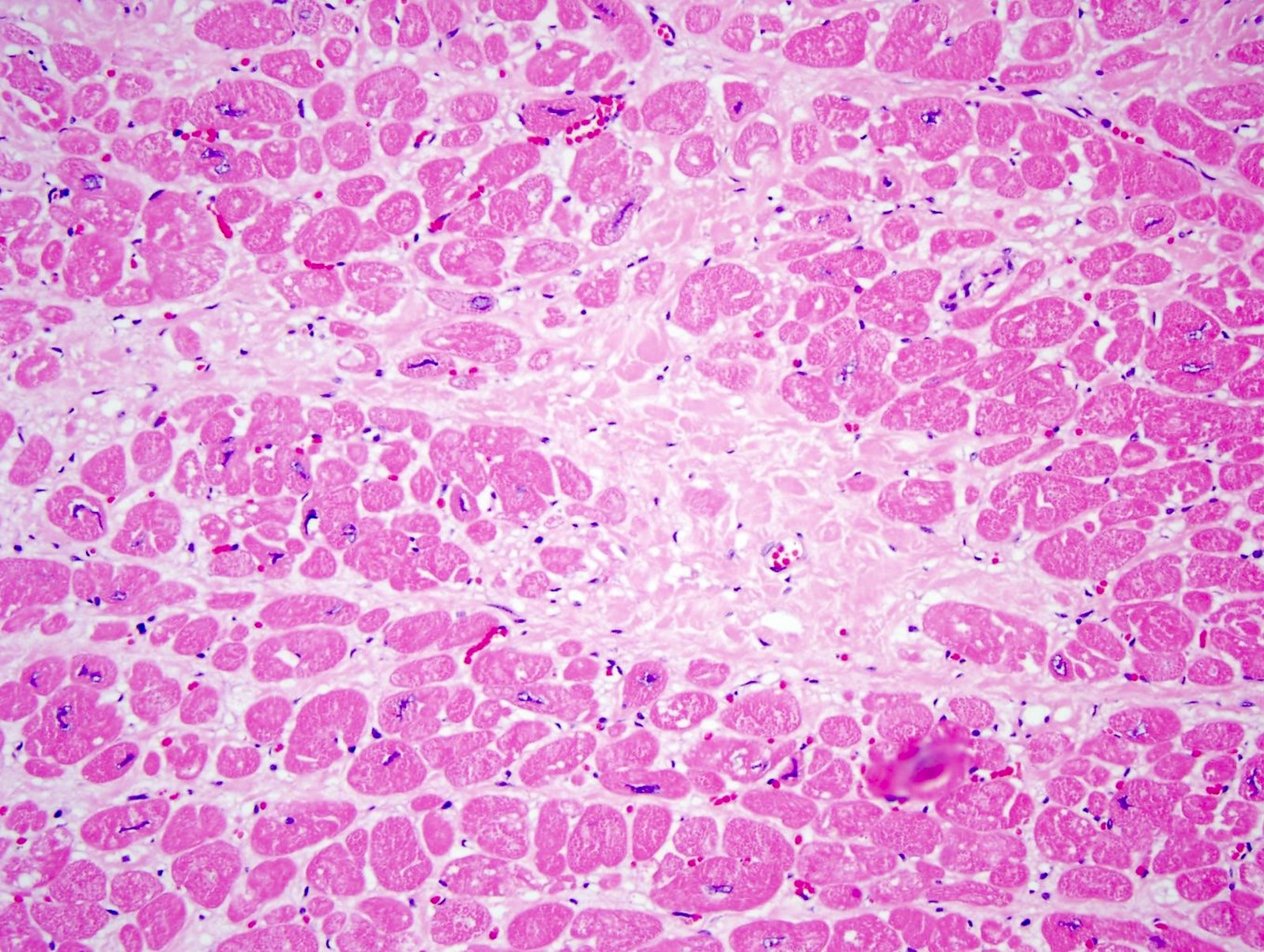
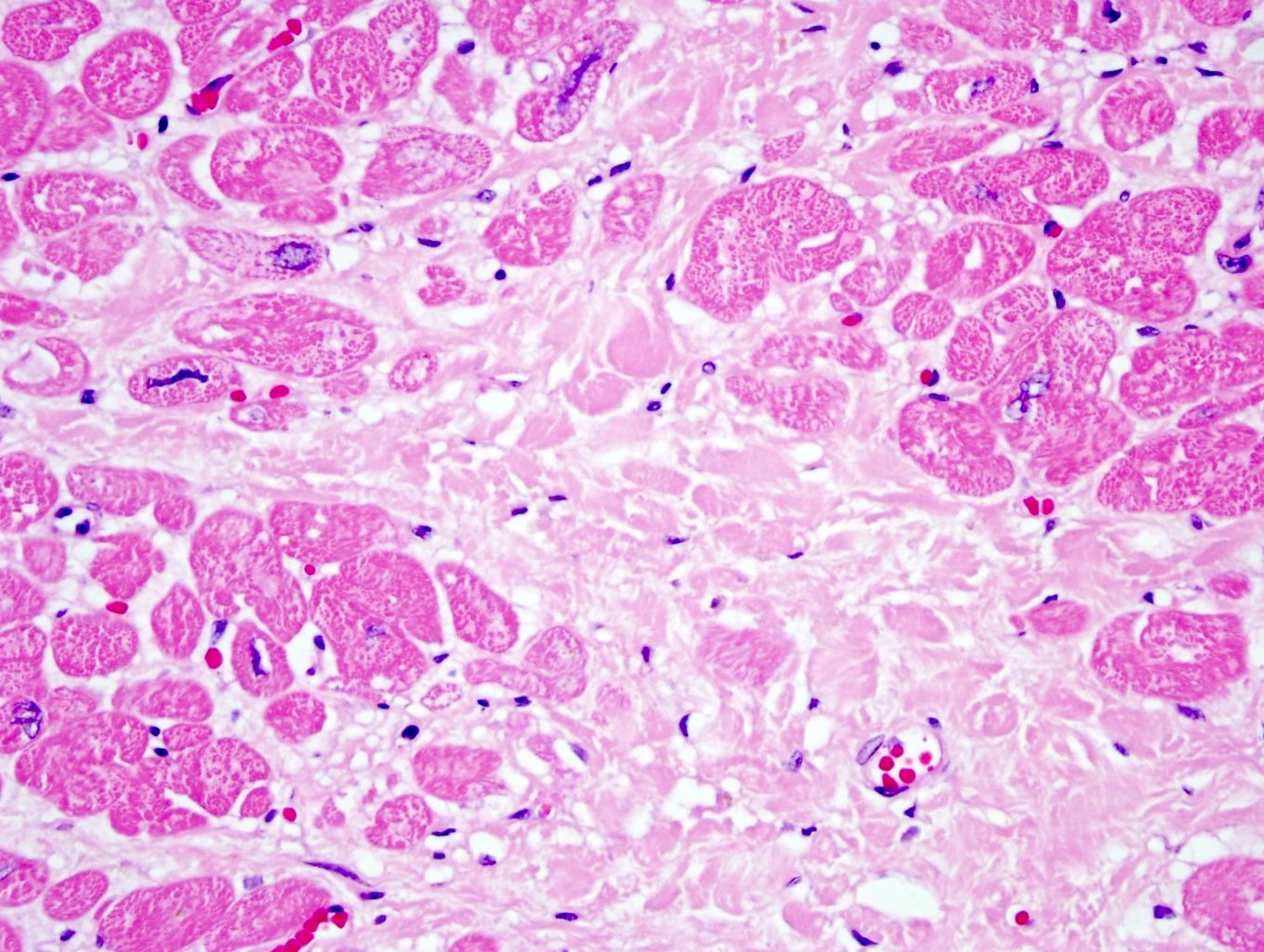
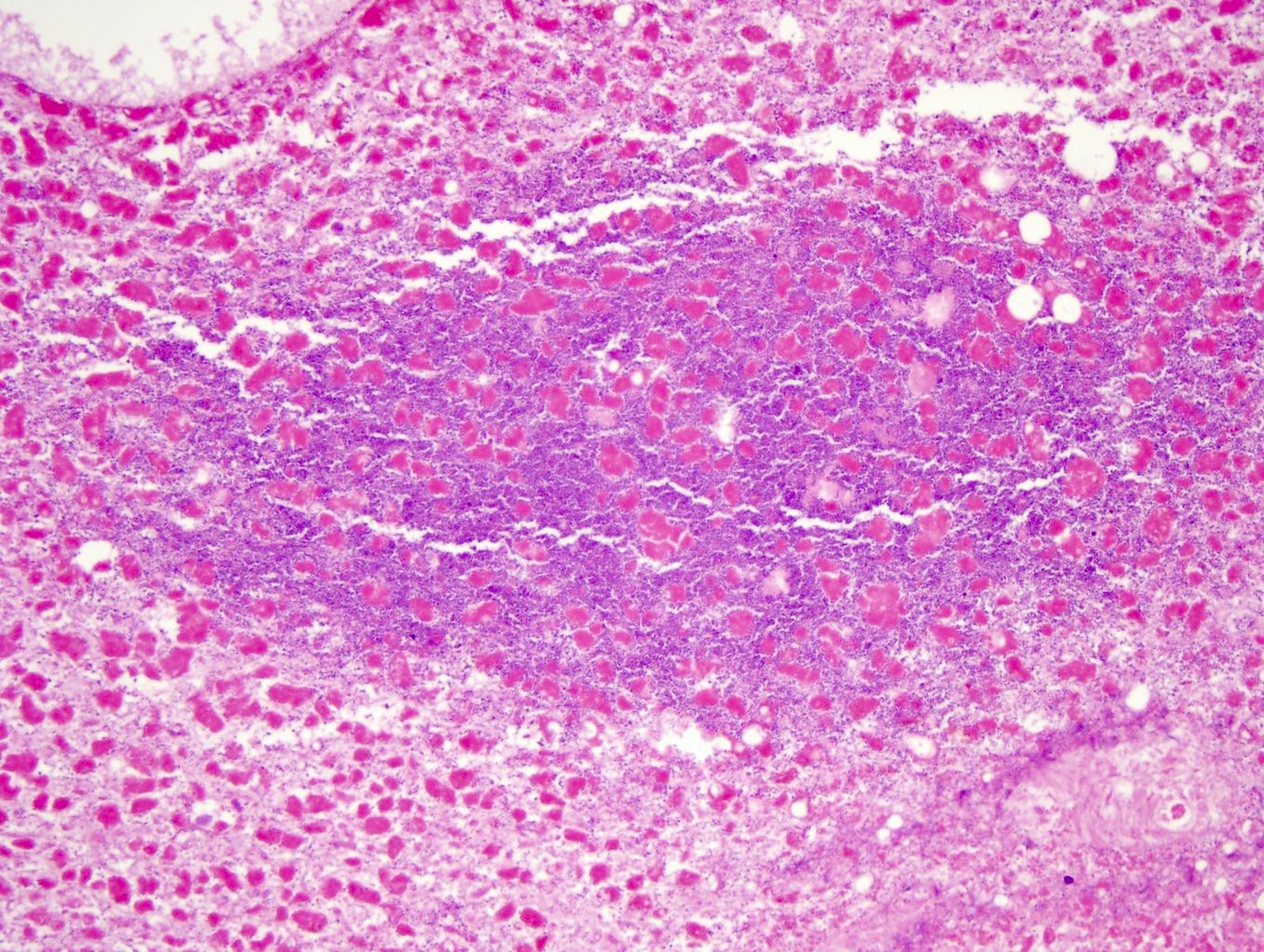
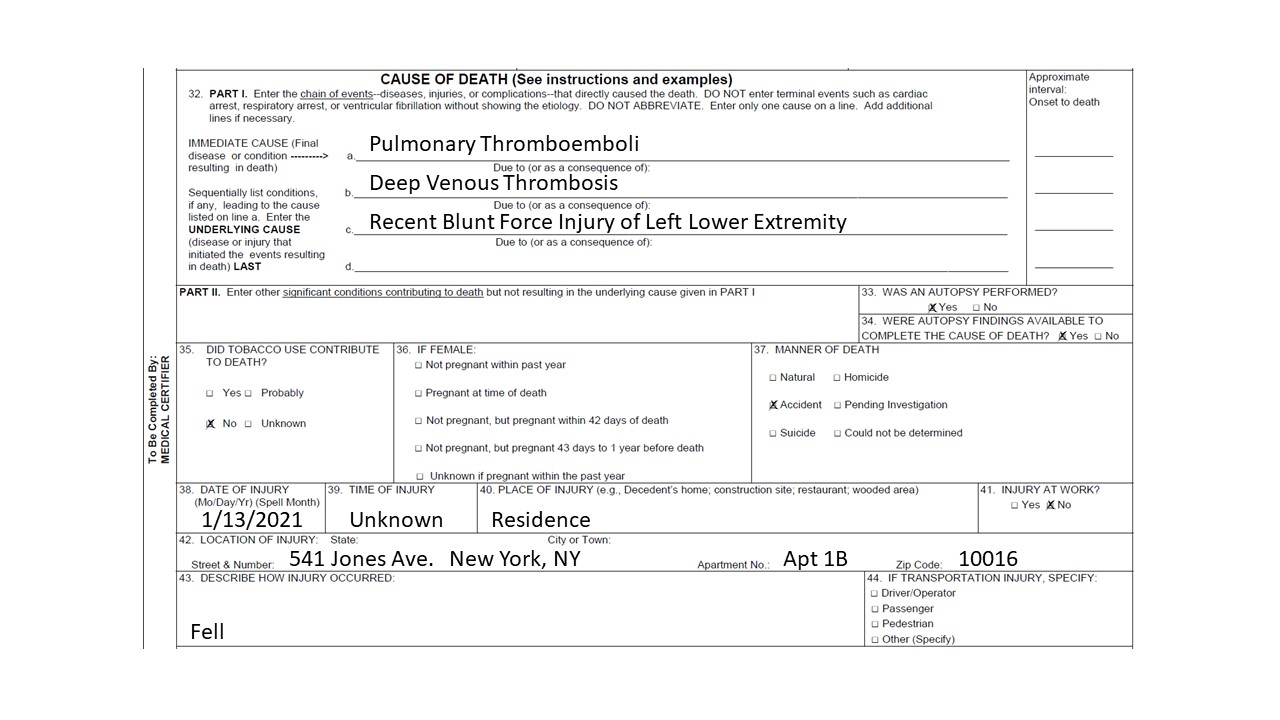
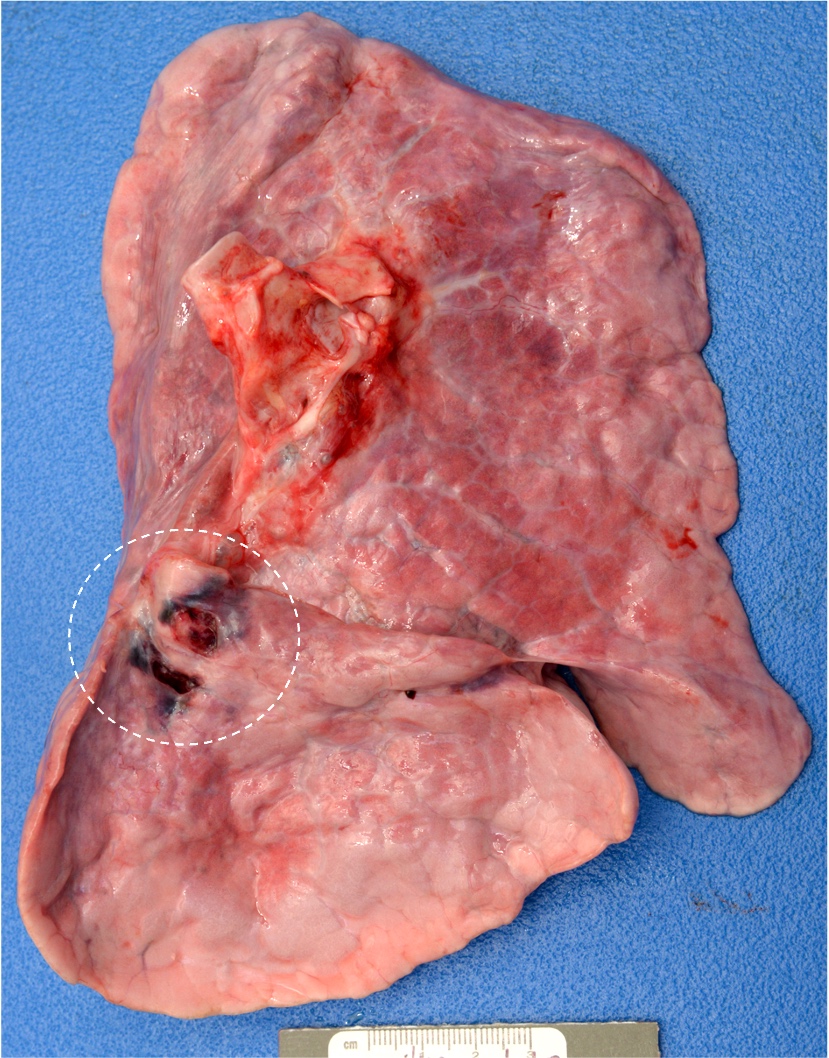
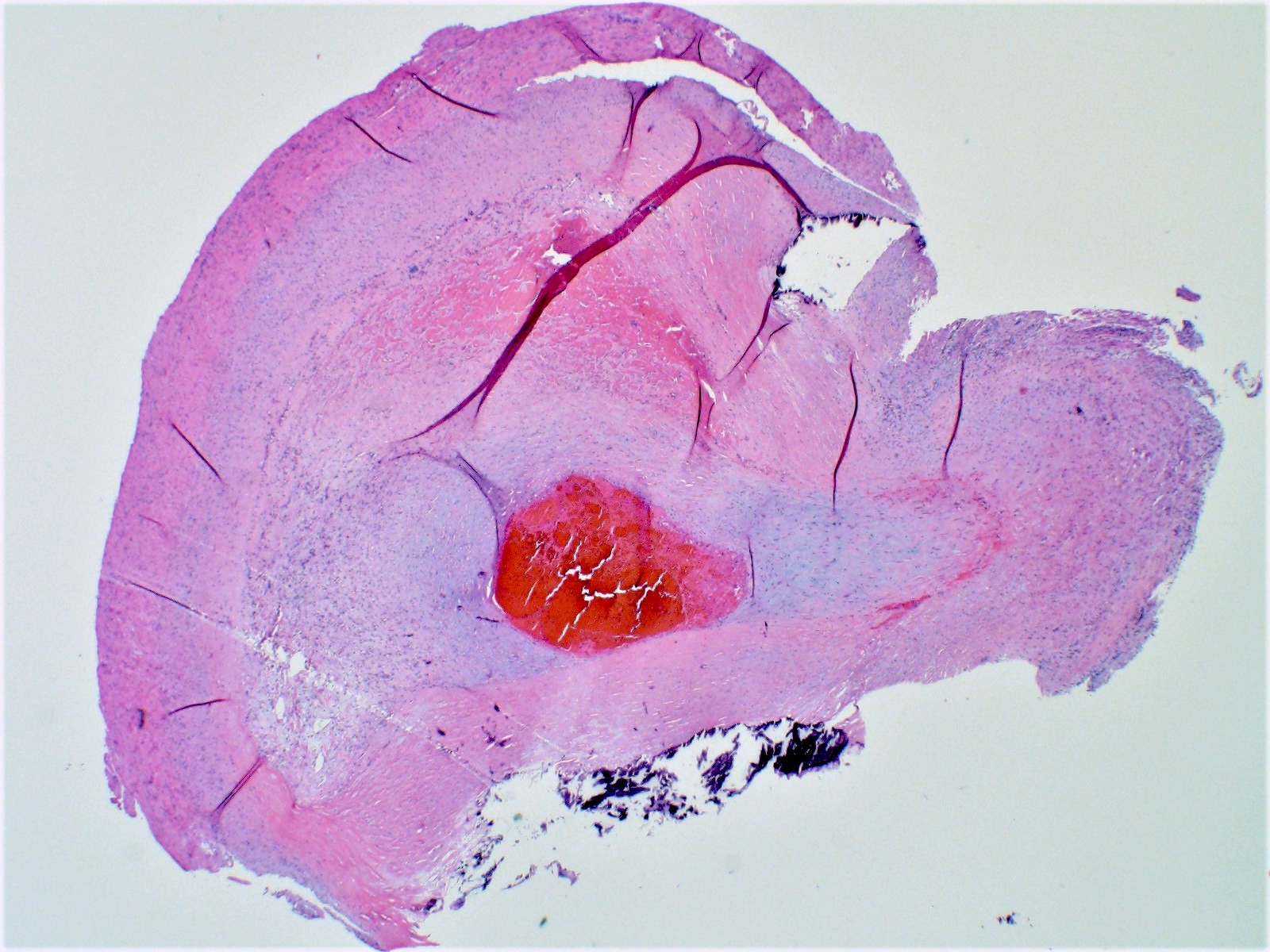
- Lungs
- Pulmonary embolism shows the layering of fibrin, platelets, RBCs and inflammatory cells, that differentiate it from a postmortem blood clot (Forensic Pathology Reviews 2008;5:239)
- Amniotic fluid in the pulmonary blood vessels is diagnostic for an amniotic fluid embolism
- Epithelial cells are highlighted with cytokeratin stains (AE1 / AE3, CAM5.2, CK7 and CK20) (Acad Forensic Pathol 2018;8:426)
- SARS-COVID-19 lung shows diffuse alveolar damages, cytological atypia of pneumocytes, syncytial change and giant cell formation; ISH for viral nuclear capsid antigen is positive in infected cells (Forensic Pathology Reviews 2008;5:239)
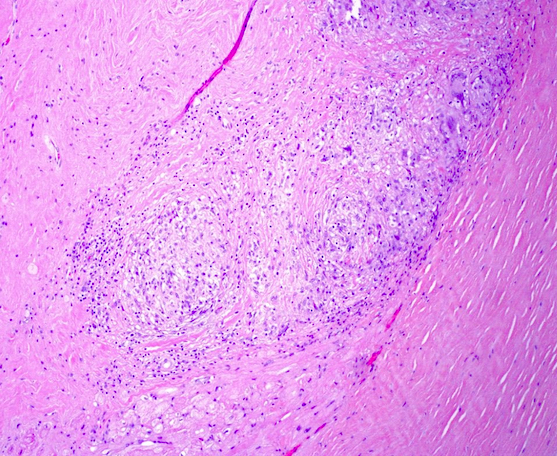
- Intravenous drug user (IVDU) has lung foreign body granuloma with polarizable material (made of talc, starch or other adulterants found injected in drugs like heroin, cocaine, amphetamines, etc.) (Forensic Pathology Reviews 2008;5:239)
- Liver
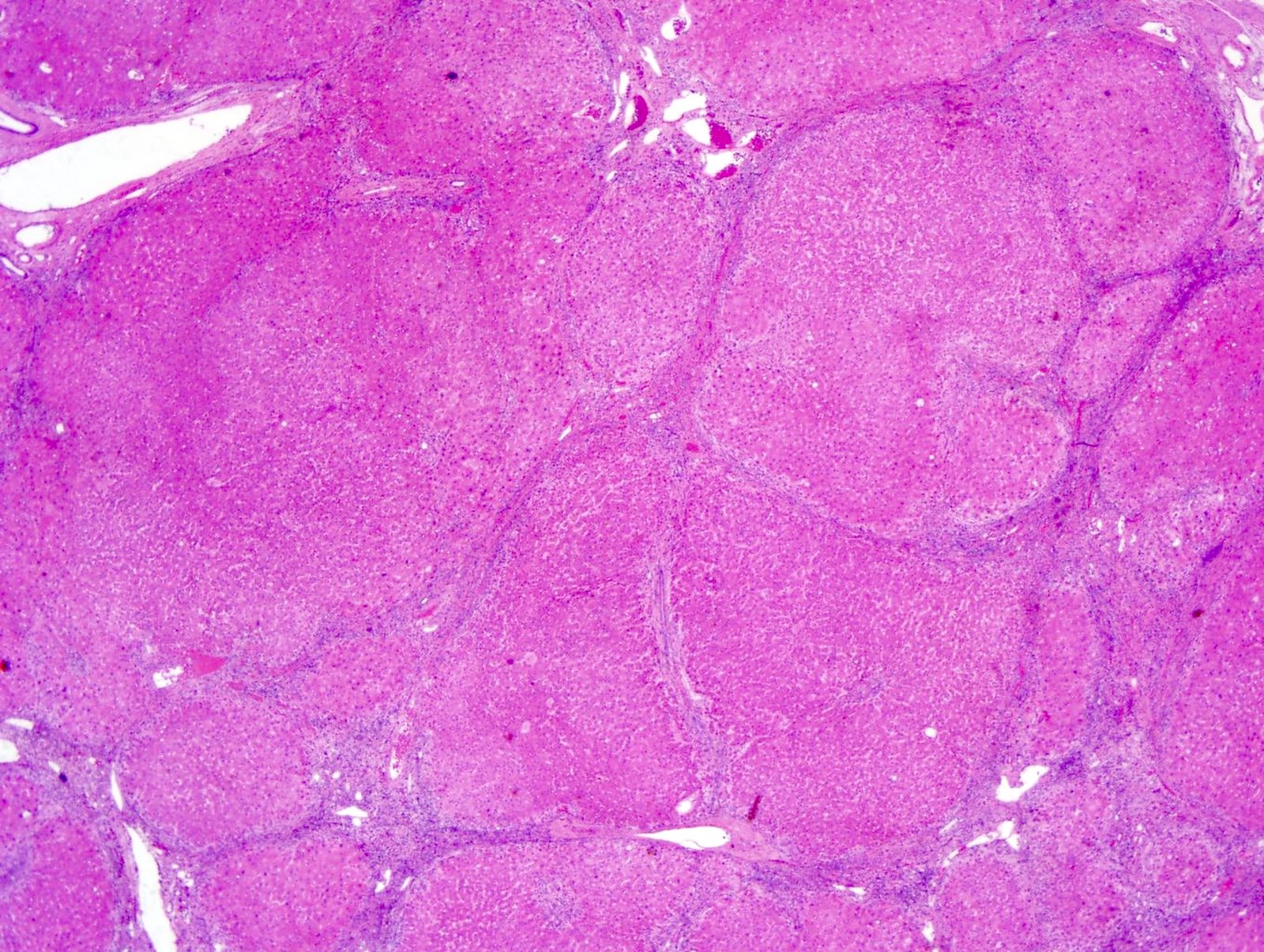
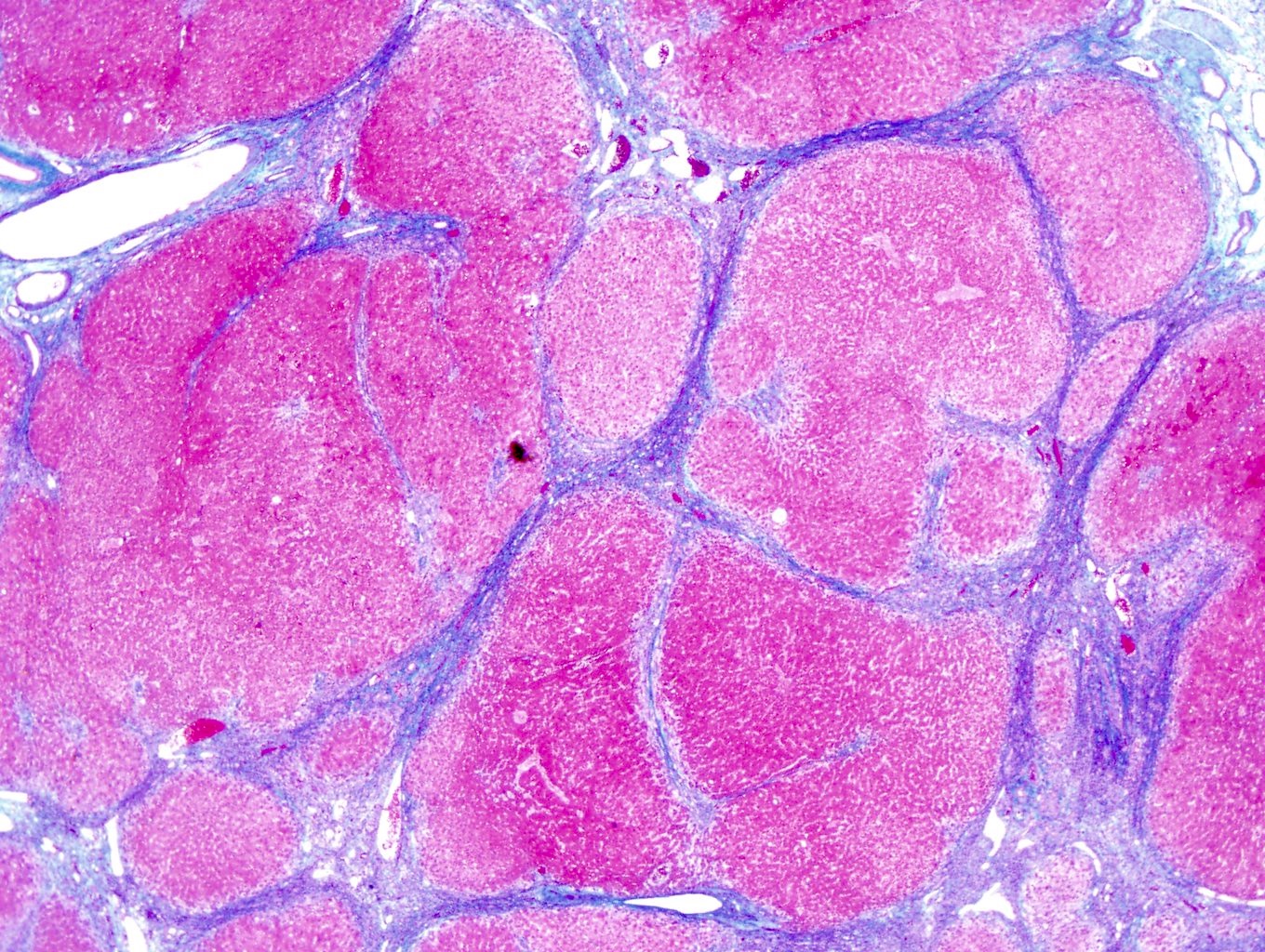
- Liver cirrhosis has regenerative nodules of hepatocytes surrounded by fibrous connective tissue that bridges between portal tracts; bridging fibrosis is highlighted by Masson trichrome
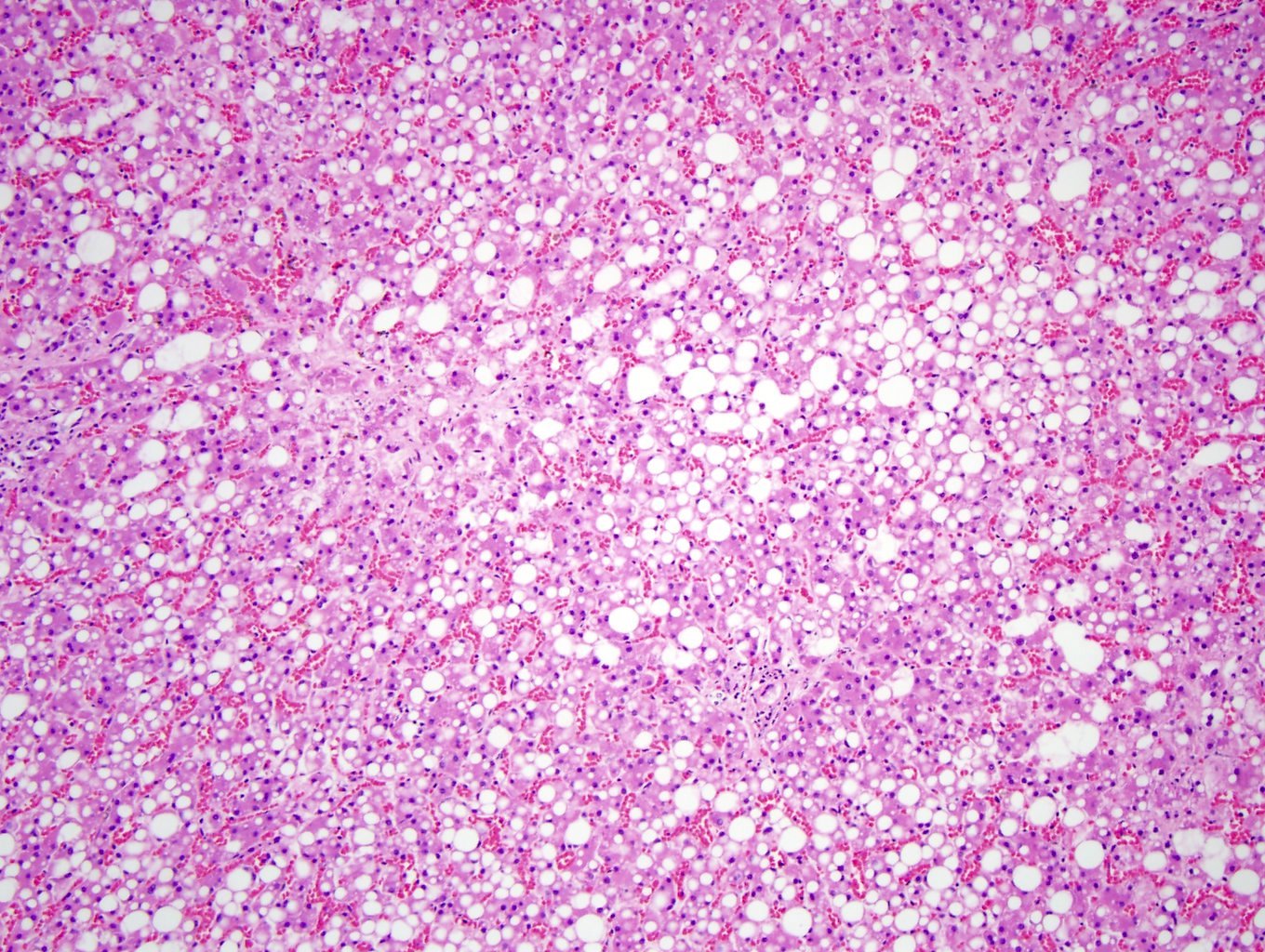
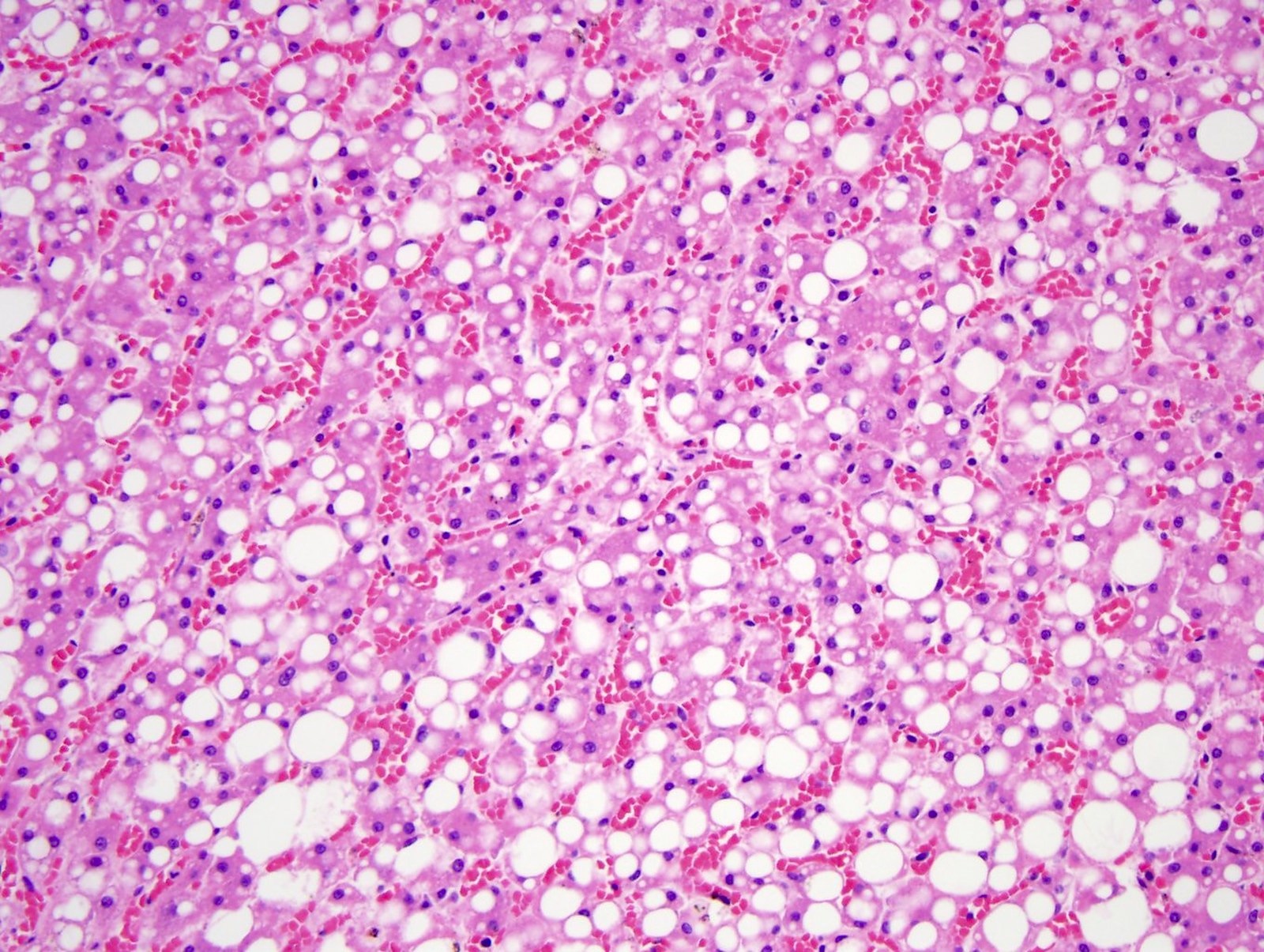
- In fatty liver disease, the hepatocytes have a large clear fat vacuole(s) in the cytoplasm pushing the nucleus to an eccentric location, consisting of steatosis
- In acetaminophen toxicity, there is centrilobular hepatic necrosis (zone 3) without acute inflammation (Forensic Pathology Reviews 2008;5:239)
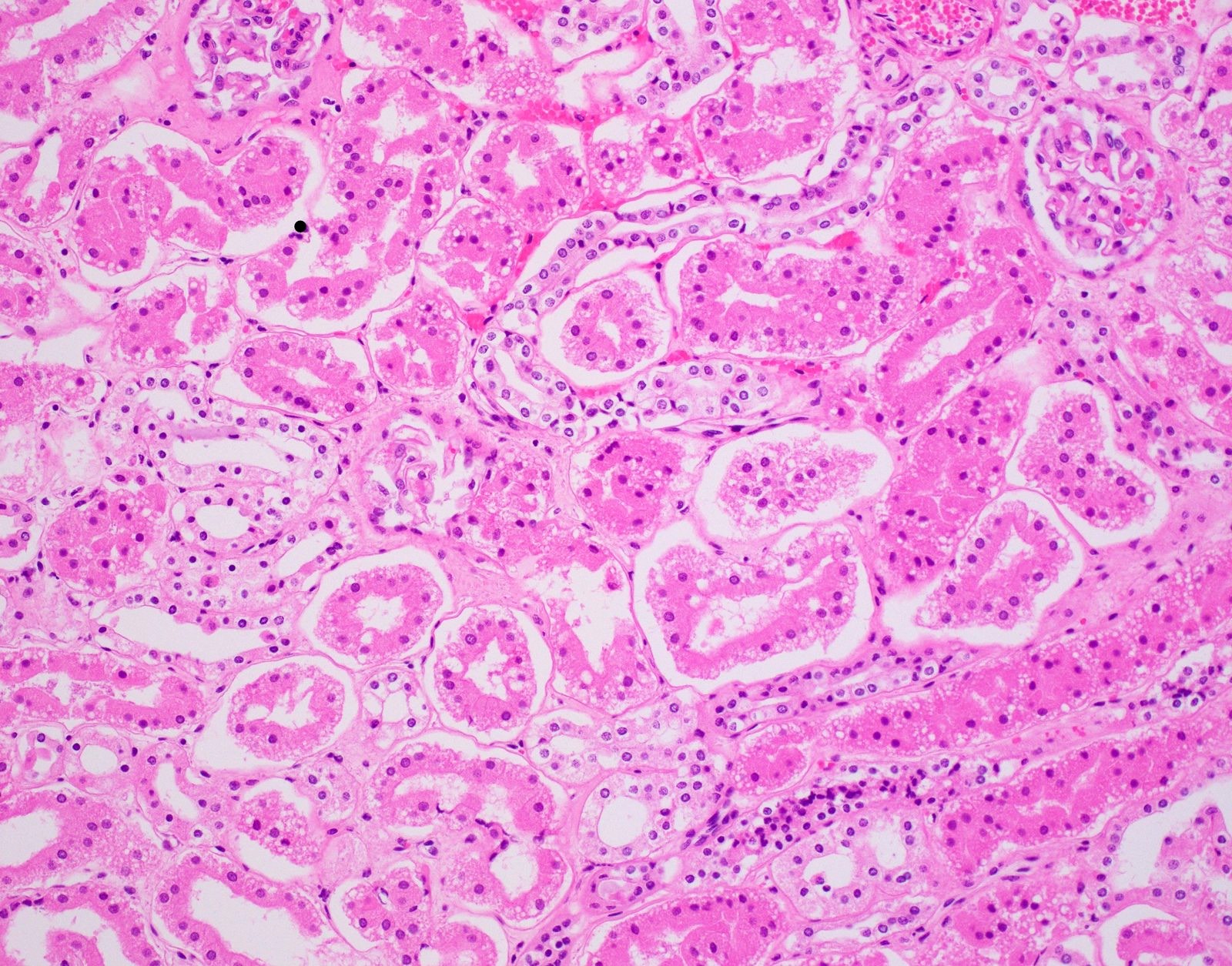
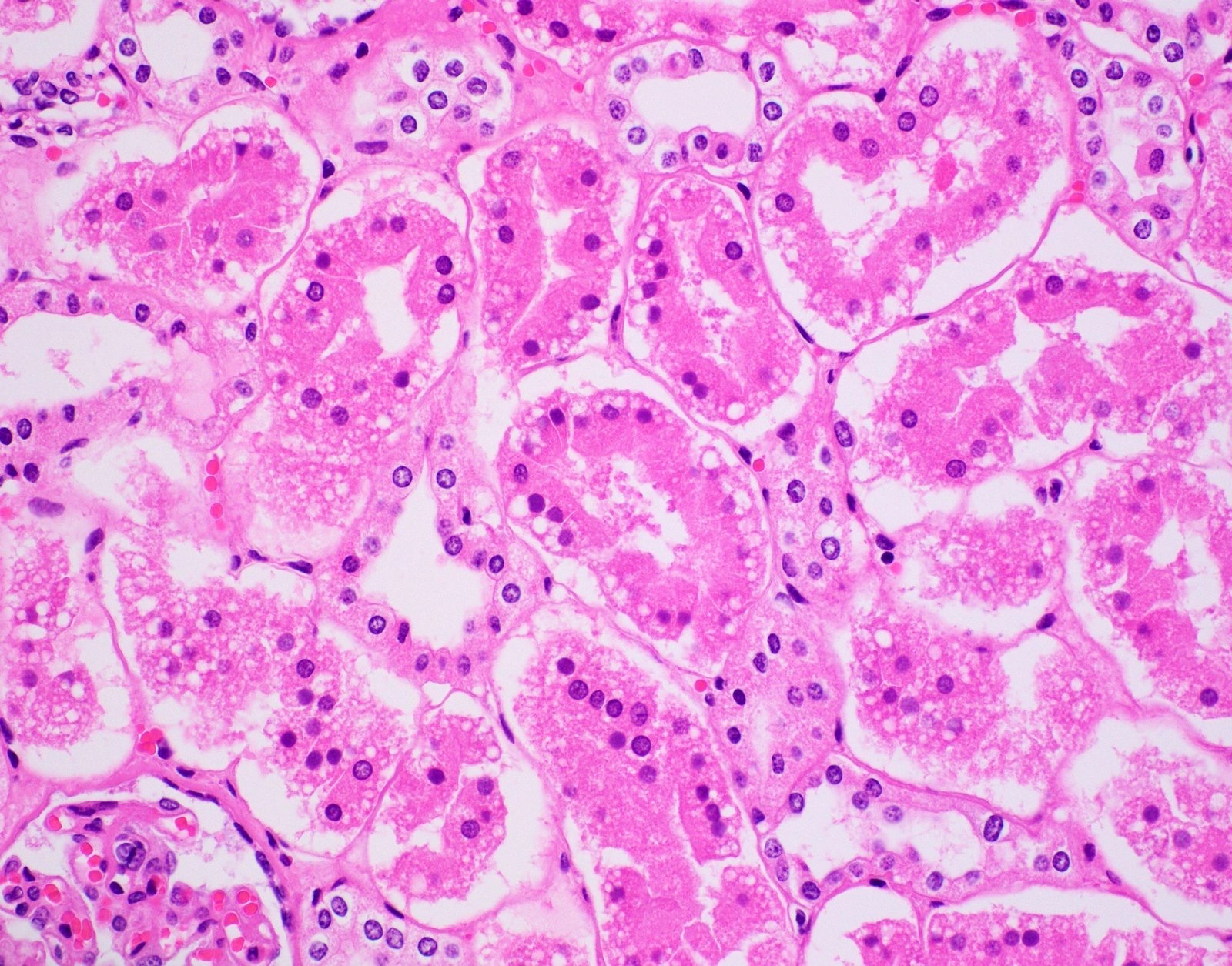
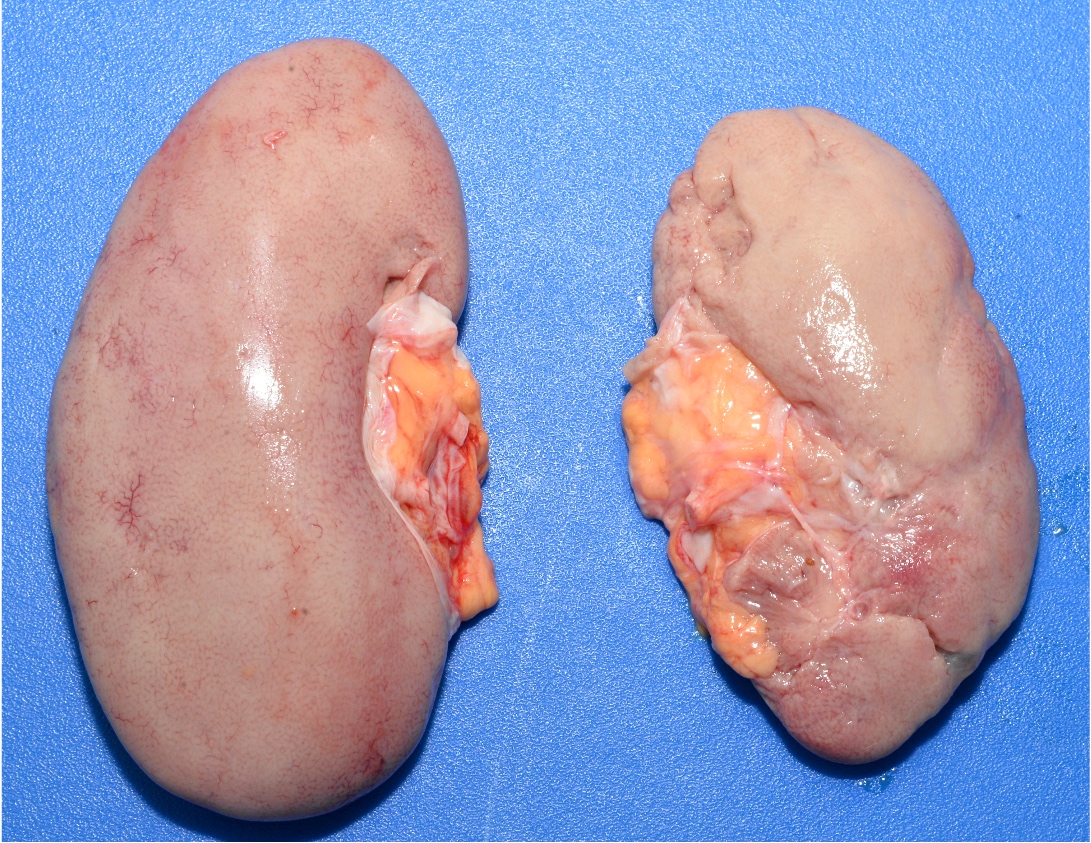
- Renal
- Ethylene glycol toxicity shows polarizable calcium oxalate crystals in degenerated renal tubules (also displays myocardial degeneration, bronchopneumonia and chemical meningoencephalitis) (Forensic Pathology Reviews 2008;5:239)
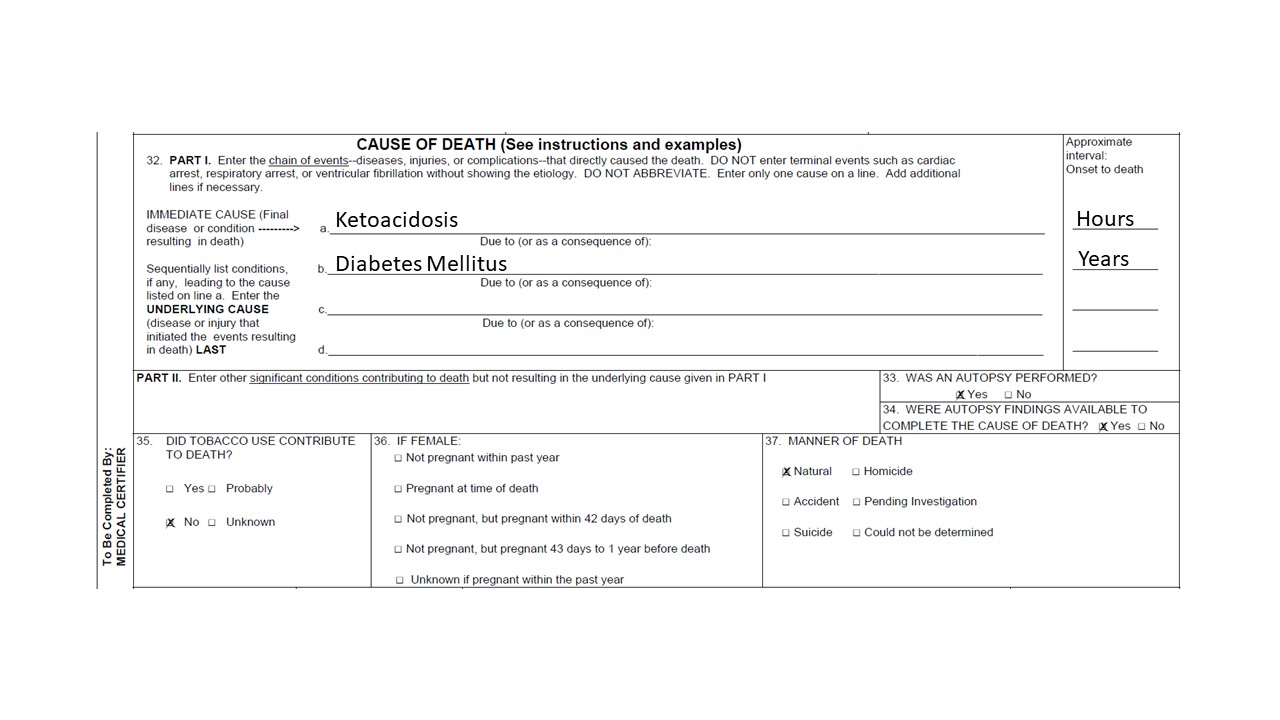
- Diabetic ketoacidosis (DKA) is supported by renal tubules showing Armanni-Ebstein lesions (PAS positive glycogenated cells) (Acad Forensic Pathol 2018;8:426)
- Brain
- Alzheimer disease shows gliosis and neuronal degeneration
- Bielschowsky silver stain highlights neuritic plaques and fibrillary tangles (Forensic Pathology Reviews 2008;5:239)
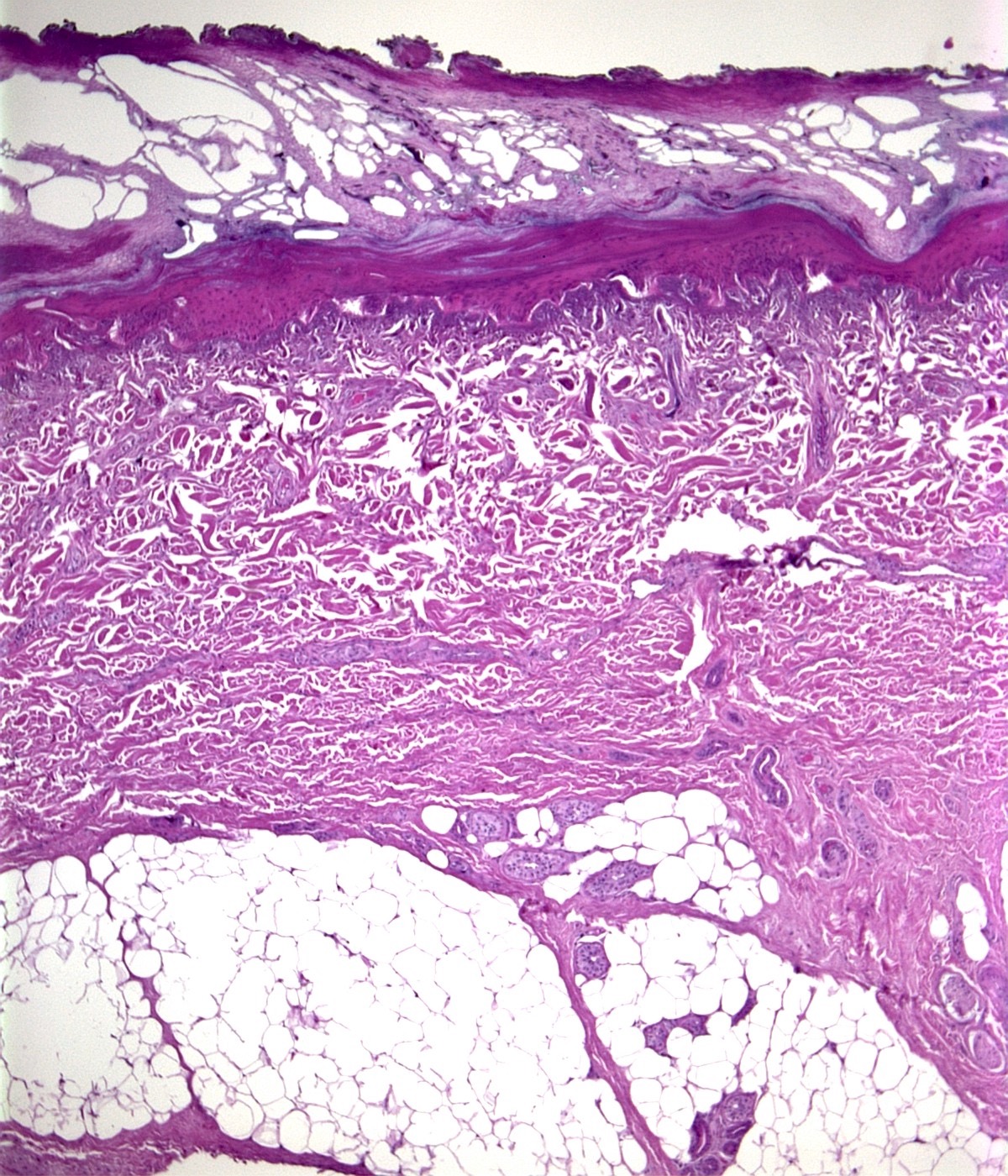
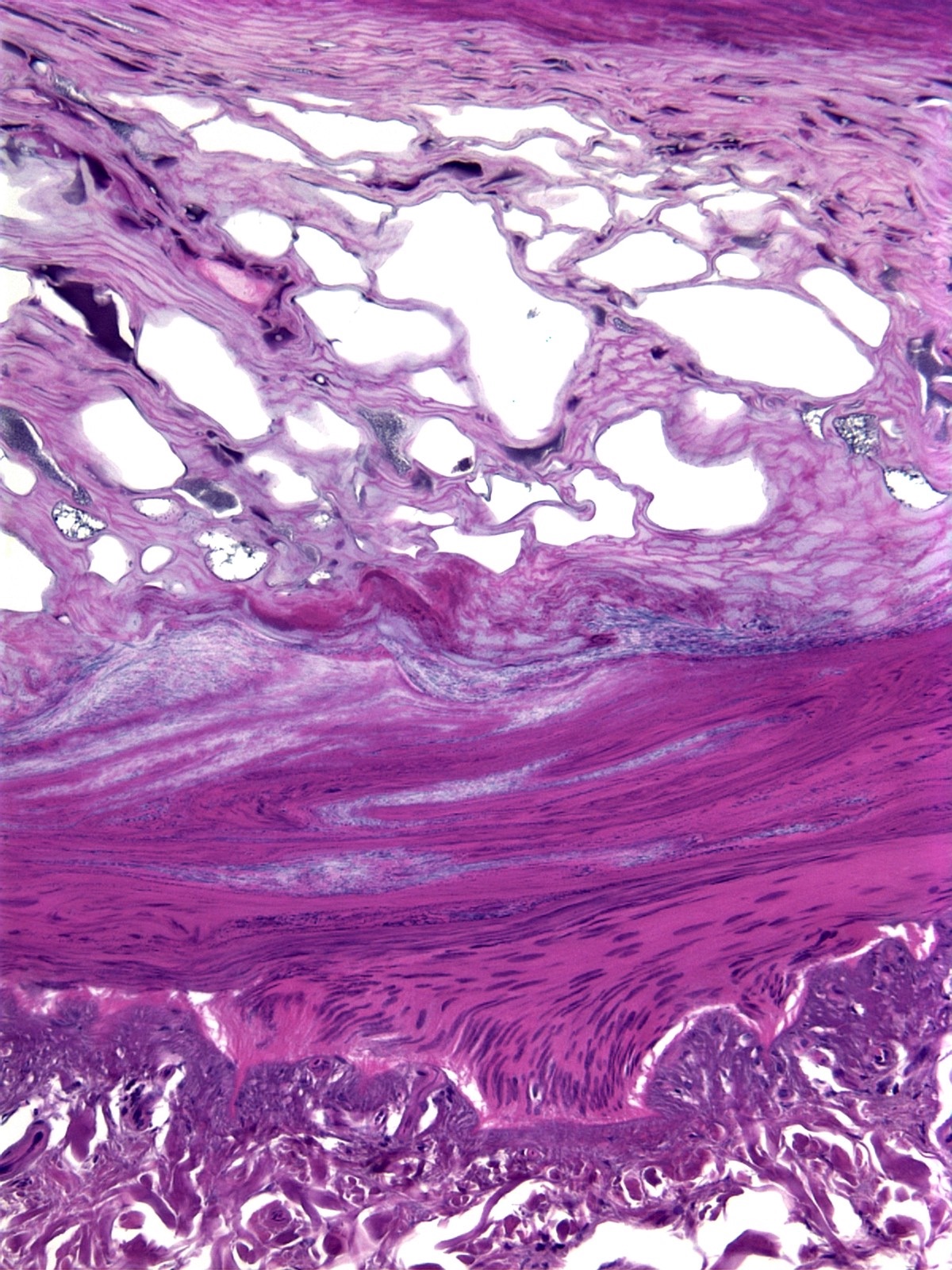
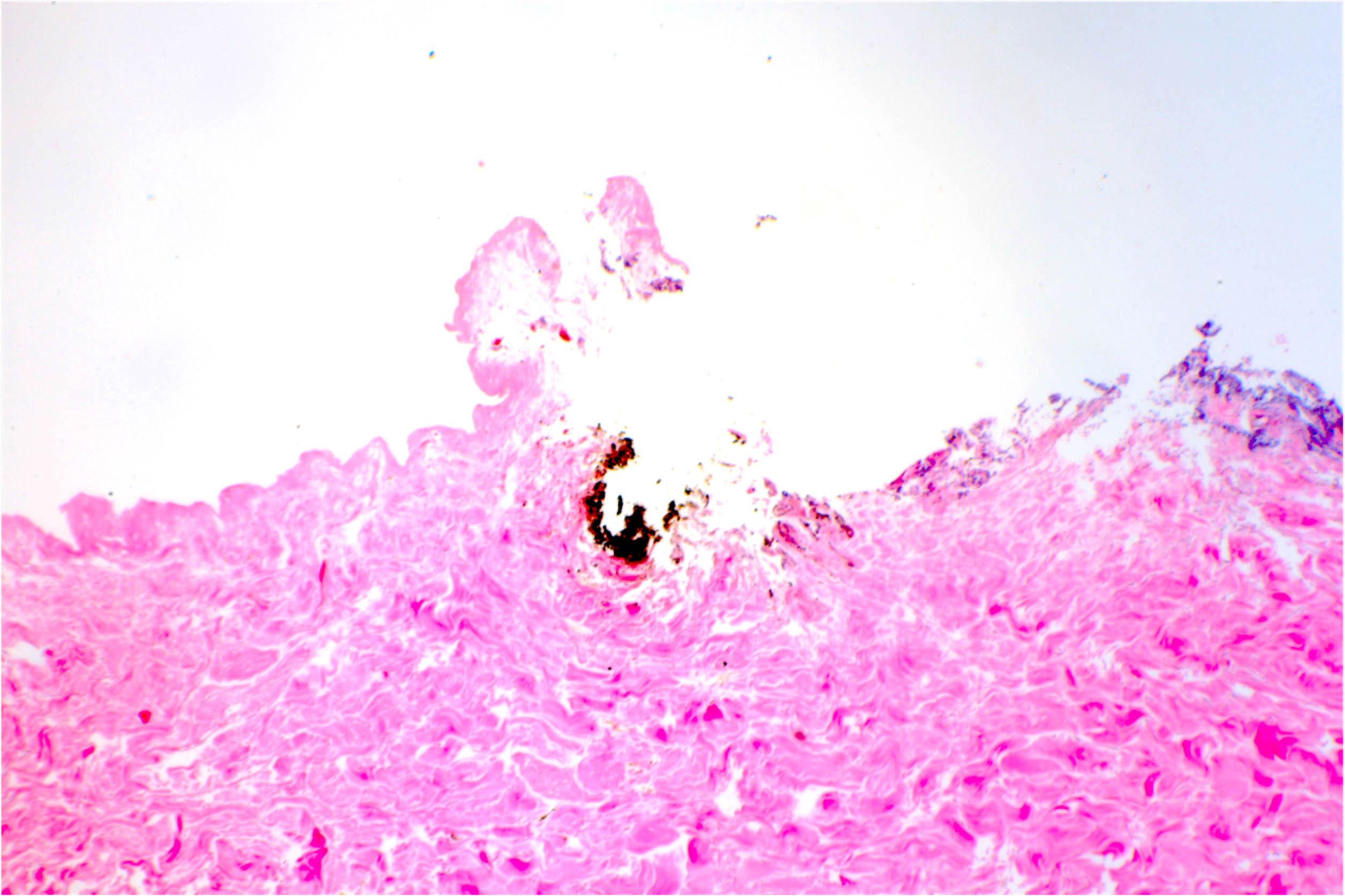
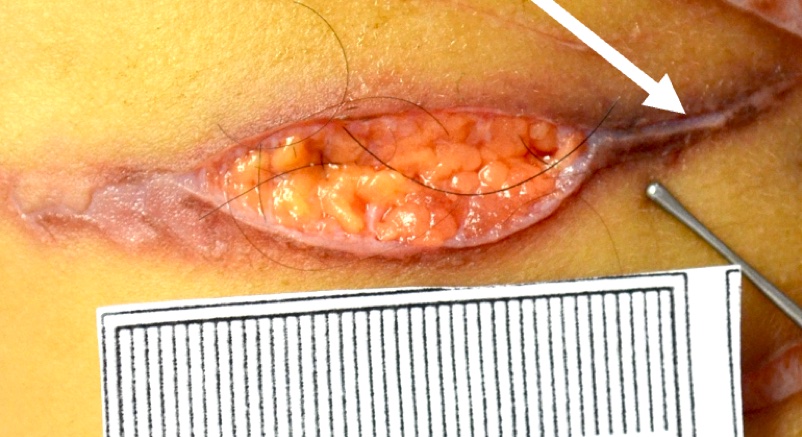
- Skin
- In electrocution, the thermal injury shows epithelial blister and streaming nuclei (Forensic Pathology Reviews 2008;5:239)
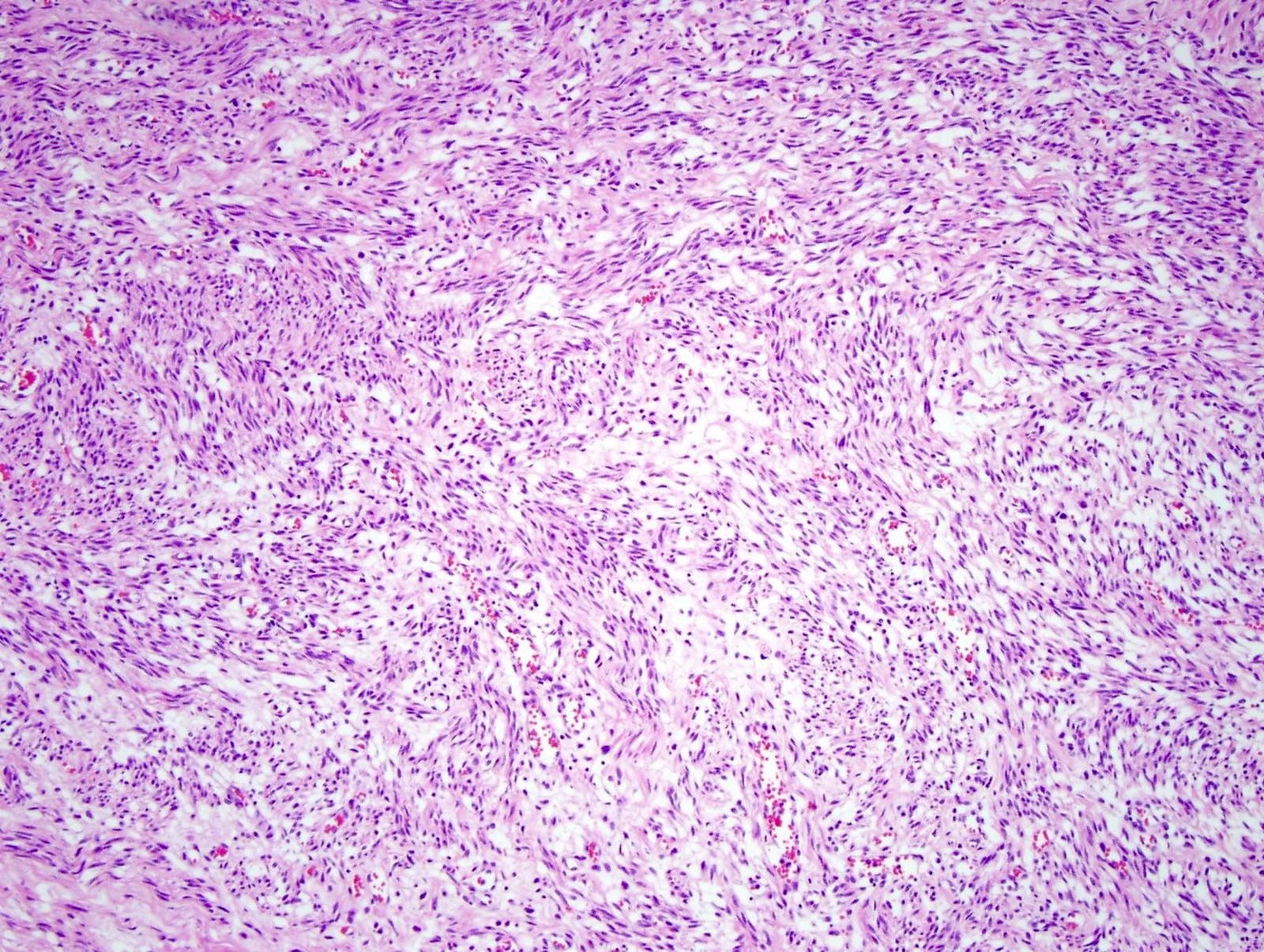
- Unknown lesions
- Unknown metastatic lesion (carcinoma, sarcoma, mesothelioma, melanoma or lymphoma) can be identified on histology (Forensic Pathology Reviews 2008;5:239)
Limitations:
- Postmortem enzymatic breakdown of tissue or autolysis can impede histologic diagnosis
- Putrefaction or tissue broken down by postmortem bacteria can impede histologic diagnosis
Essential features:
- Postmortem histology determines or supports COD in:
- Dating a myocardial infarction (> 4 hours = myocyte necrosis with PMNs, > 3 days = hemosiderin laden macrophages and granulation tissue and > 10 days = collagen deposition)
- Acute viral myocarditis (myocardial lymphocytic infiltration)
- Pulmonary embolism (layering of fibrin, platelets, RBCs and acute inflammation)
- Liver cirrhosis (bridging fibrosis highlighted with Masson trichrome)
- Acetaminophen toxicity in the liver has zone 3 necrosis without inflammation
- Diabetic ketoacidosis (Armanni-Ebstein lesions)
- Ethylene glycol toxicity (calcium oxalate crystals in renal tubules)
- Alzheimer disease (Bielschowsky silver stain highlights neuritic plaques and fibrillary tangles)
Contributed by Myra Khan, D.O., Michael Caplan, M.D. and Maria Westerhoff, M.D.
- Evidence of infection during autopsy and in all infant deaths
- Routine cultures are taken from the blood, nasal pharynx and lungs; spleen and liver can also be taken
- Tissue samples for microbiology are stored in sterile containers or bottles without additives, refrigerated until transport and sent to the microbiology laboratory 24 - 48 hours after the autopsy (Forensic Sci Med Pathol 2021;17:87)
How to perform:
- Nasal pharyngeal swabs
- Sterile nasopharyngeal swab, 1 for each nostril, is taken before opening the body cavity (Eur J Clin Microbiol Infect Dis 2015;34:1045)
- Swab is inserted until resistance is felt, ensuring the nasopharynx is adequately sampled with respiratory epithelium (N Engl J Med 2020;382:e76)
- Cultures
- When the body cavity is opened and before any dissection, the organ of interest is swabbed with iodine, a deep incision with a sterile blade is made and a sterile swab is taken and placed into a sterile container for cultures
- Cases of bacterial meningitis: sterile swabs of a brain are taken once the cranial cavity is opened
- Cases of sepsis or meningitis: culture spinal fluid
- Cases of endocarditis: culture heart valves
- When the body cavity is opened and before any dissection, the organ of interest is swabbed with iodine, a deep incision with a sterile blade is made and a sterile swab is taken and placed into a sterile container for cultures
- Blood cultures
- Before dissection, heart blood or spinal fluid can be taken by a sterile needle syringe for blood cultures
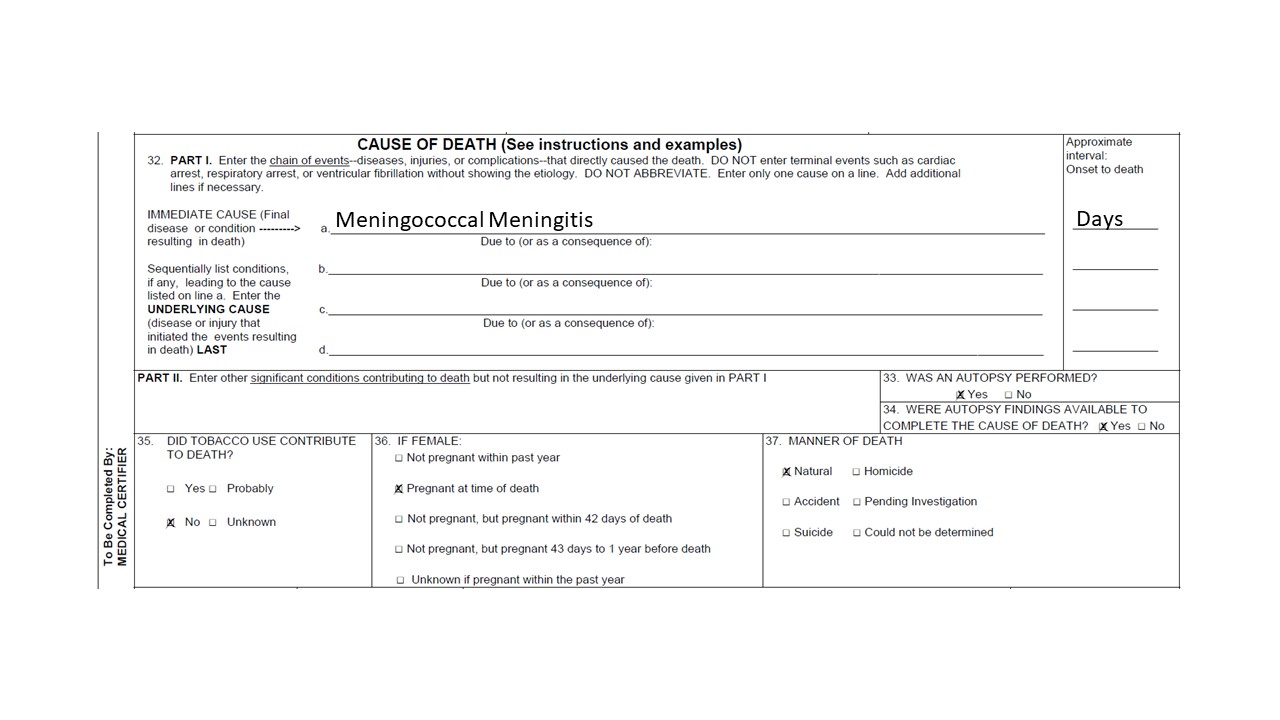
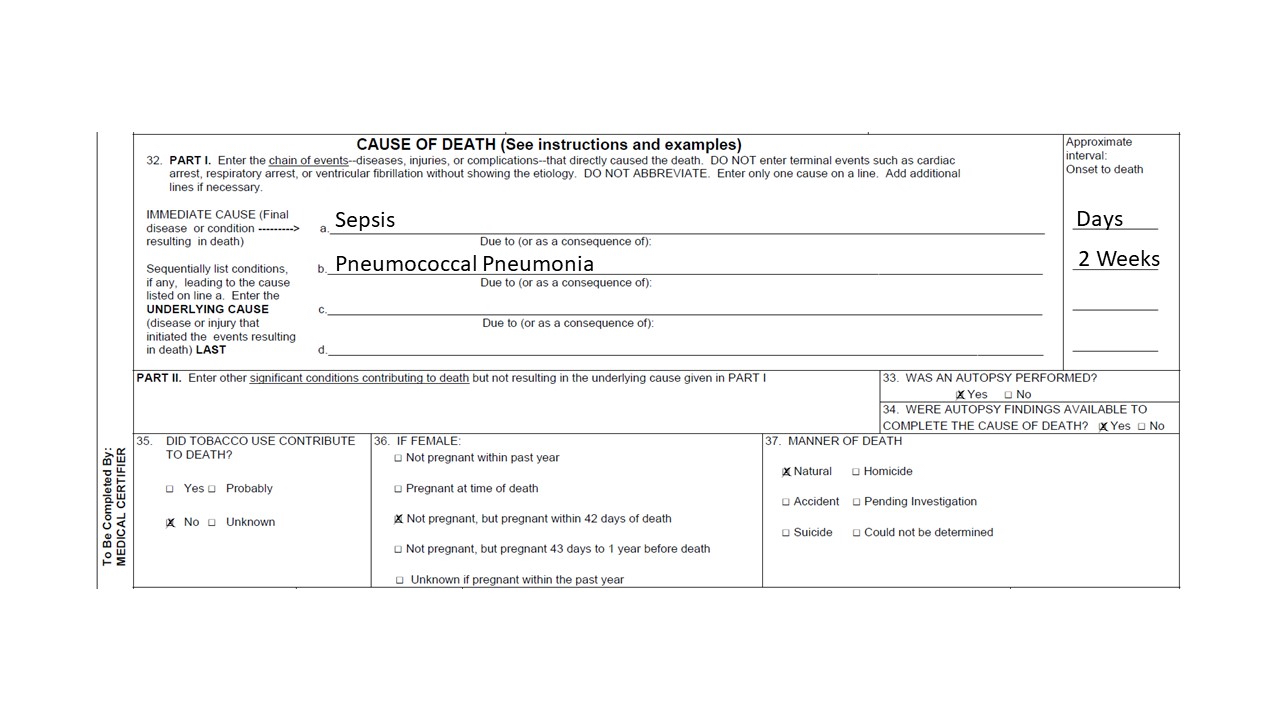
Case examples:
- Growth of a single microbial isolate is generally considered a true positive (Forensic Sci Med Pathol 2021;17:87)
- Isolation of a pathogenic organism from multiple sites at autopsy likely represents true antemortem bacteremia (Forensic Sci Med Pathol 2021;17:87)
- Growth of multiple endogenous commensal gut bacteria, such as Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Enterococcus spp., Clostridia and streptococci, are not pathogenic and considered postmortem bacterial translocation (Forensic Sci Med Pathol 2021;17:87)
- If there is concordance between the microbial growth, patient history, histology and possible imaging, it is reasonable to attribute the microorganism as a causative factor of death; if concordance is lacking, the microbiology findings represent contamination or postmortem bacterial growth (Forensic Sci Med Pathol 2021;17:87)
Limitations:
- Mixed growth represents sample contamination (Forensic Sci Med Pathol 2021;17:87)
- Microbial cultures are subject to postmortem bacterial overgrowth and can be a challenge to interpret
Essential features:
- Growth of a single microbe from multiple sites is consistent with antemortem bacteremia, along with concordance of patient history, histology or imaging
- Mixed microbial growth, especially of endogenous gut bacteria, supports postmortem bacterial overgrowth or contamination
Contributed by Michael Caplan, M.D.
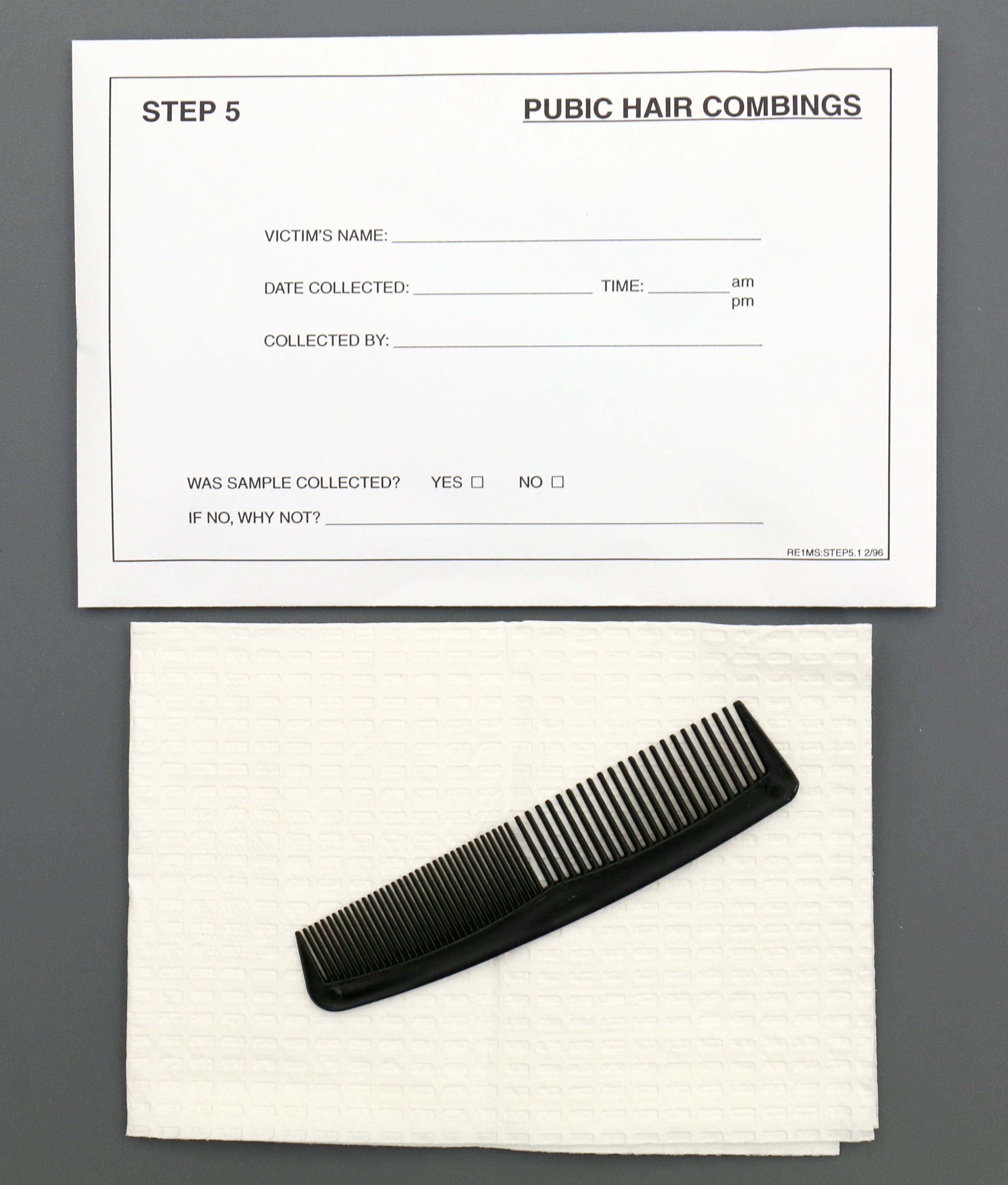
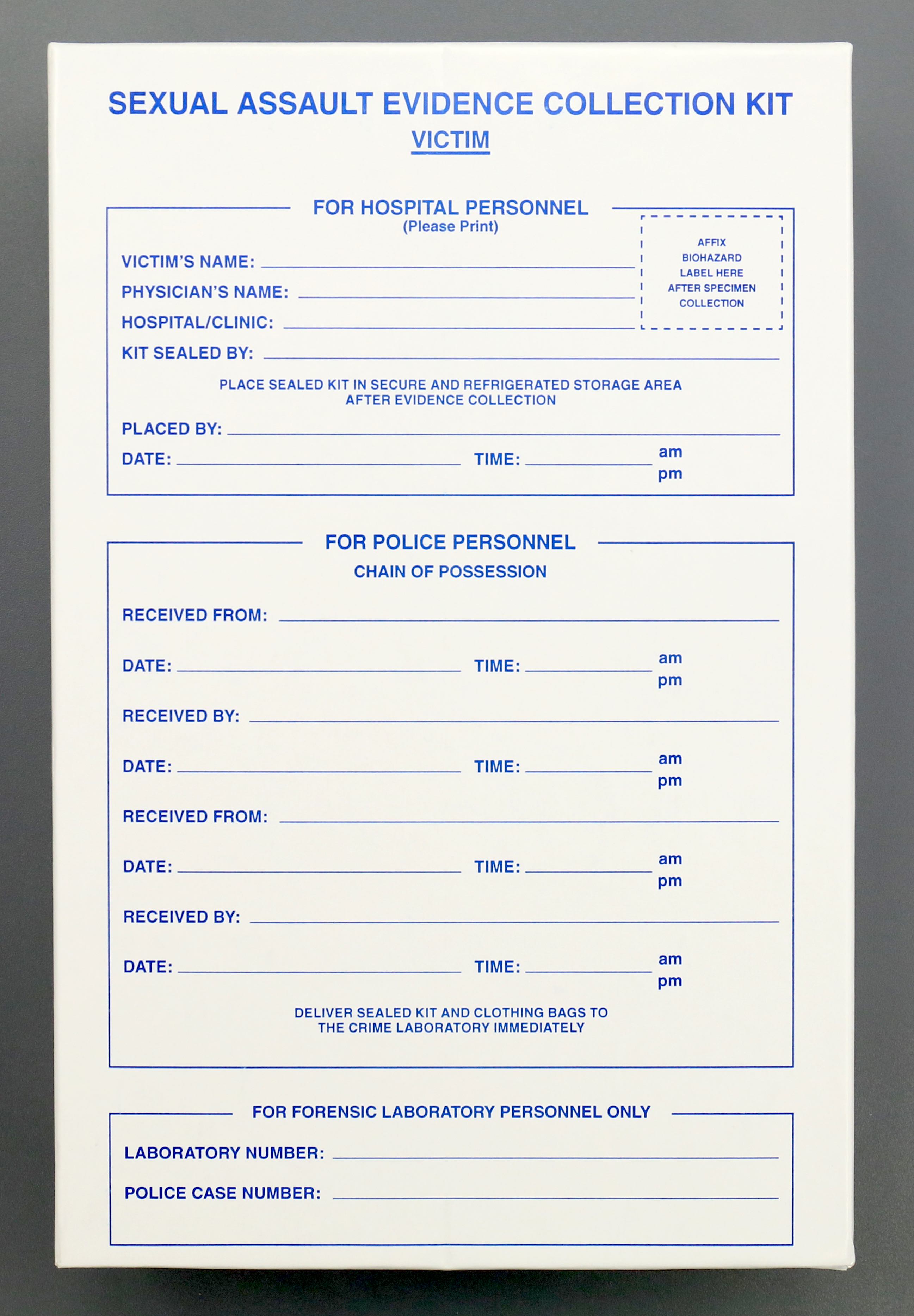
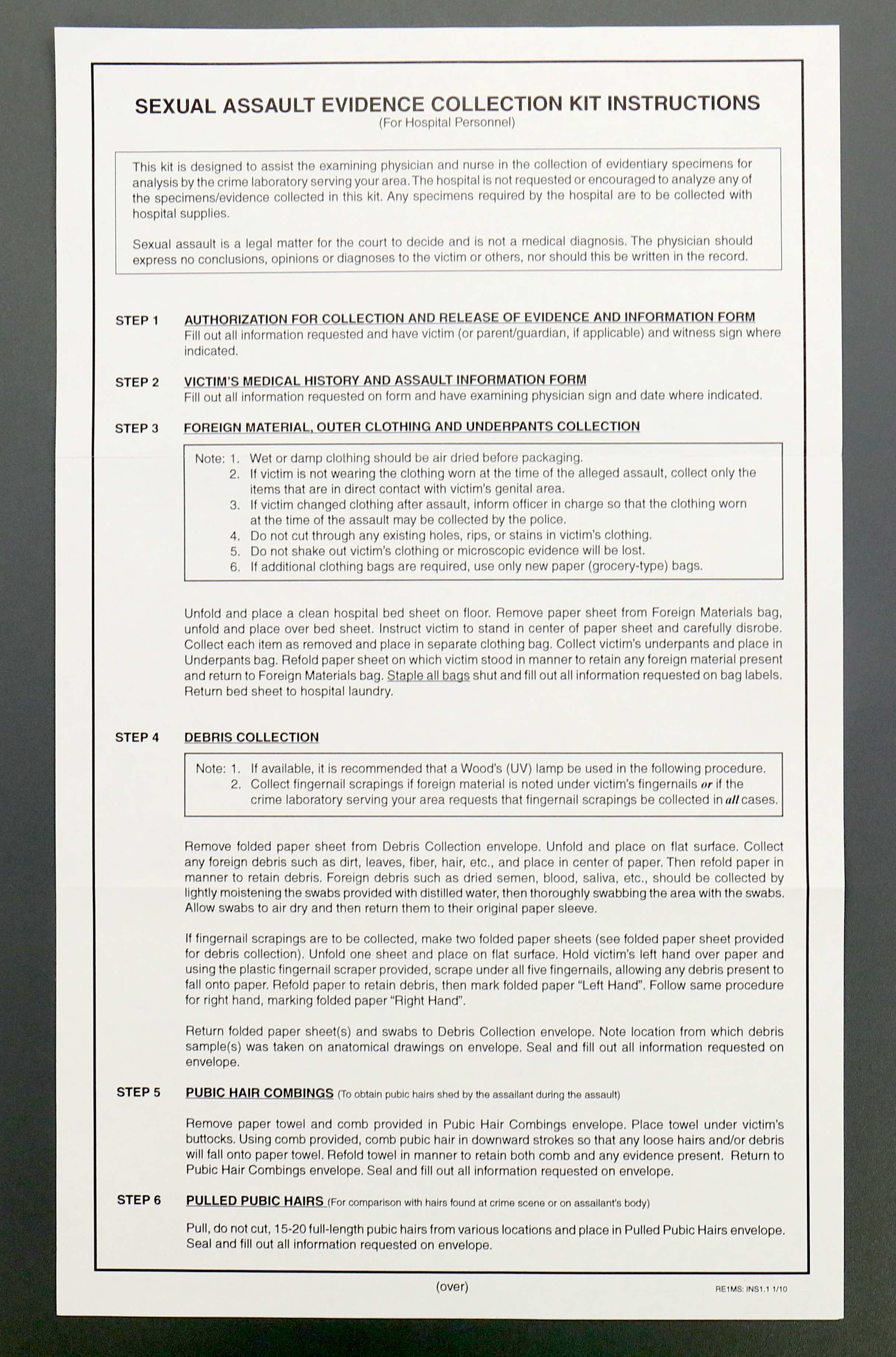
- All cases of sexual assault or suspected sexual assault, physical assault, strangulation, prostitution, if a decedent is found in a compromising position and physical trauma is identified in the genitalia at autopsy
How to perform:
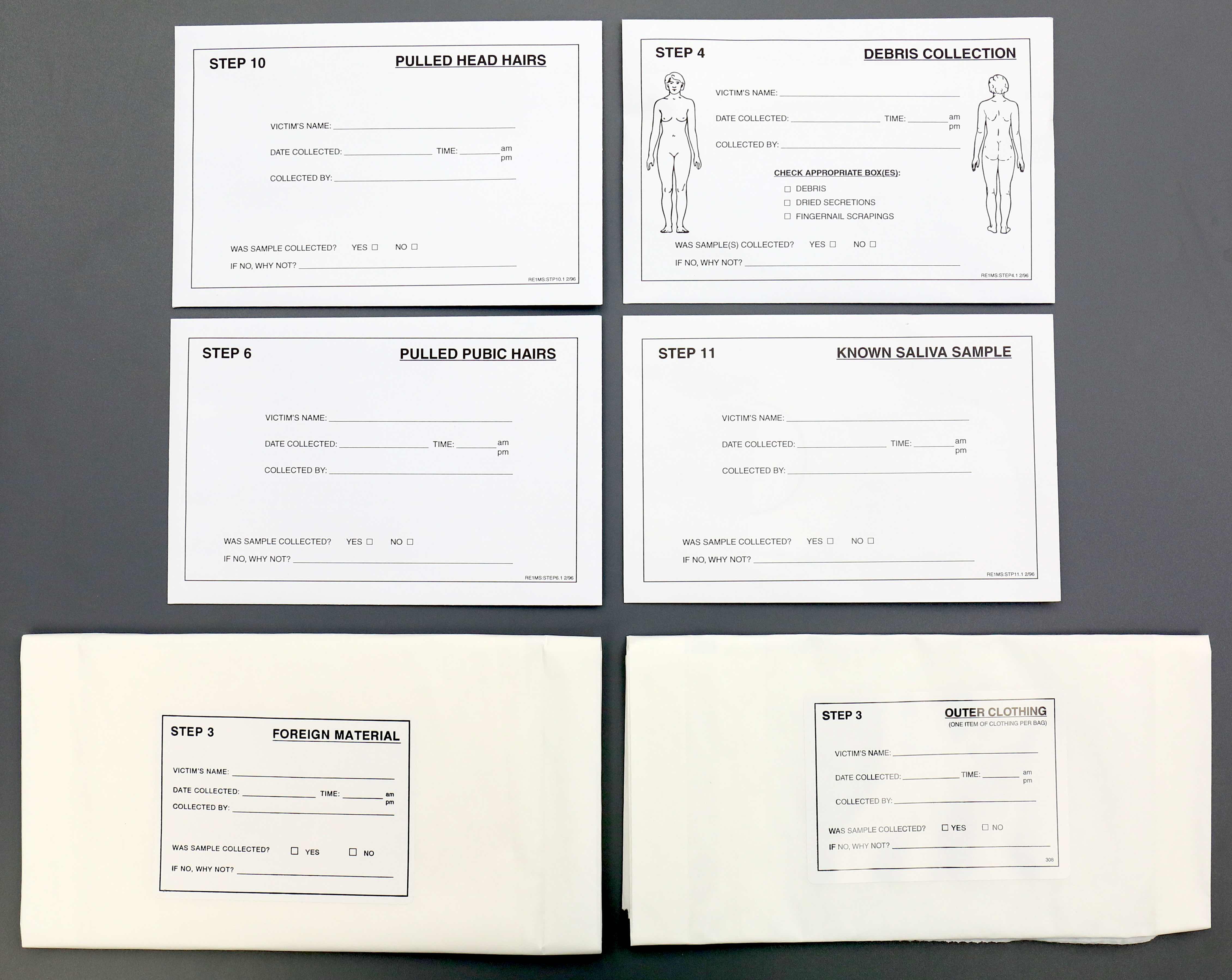
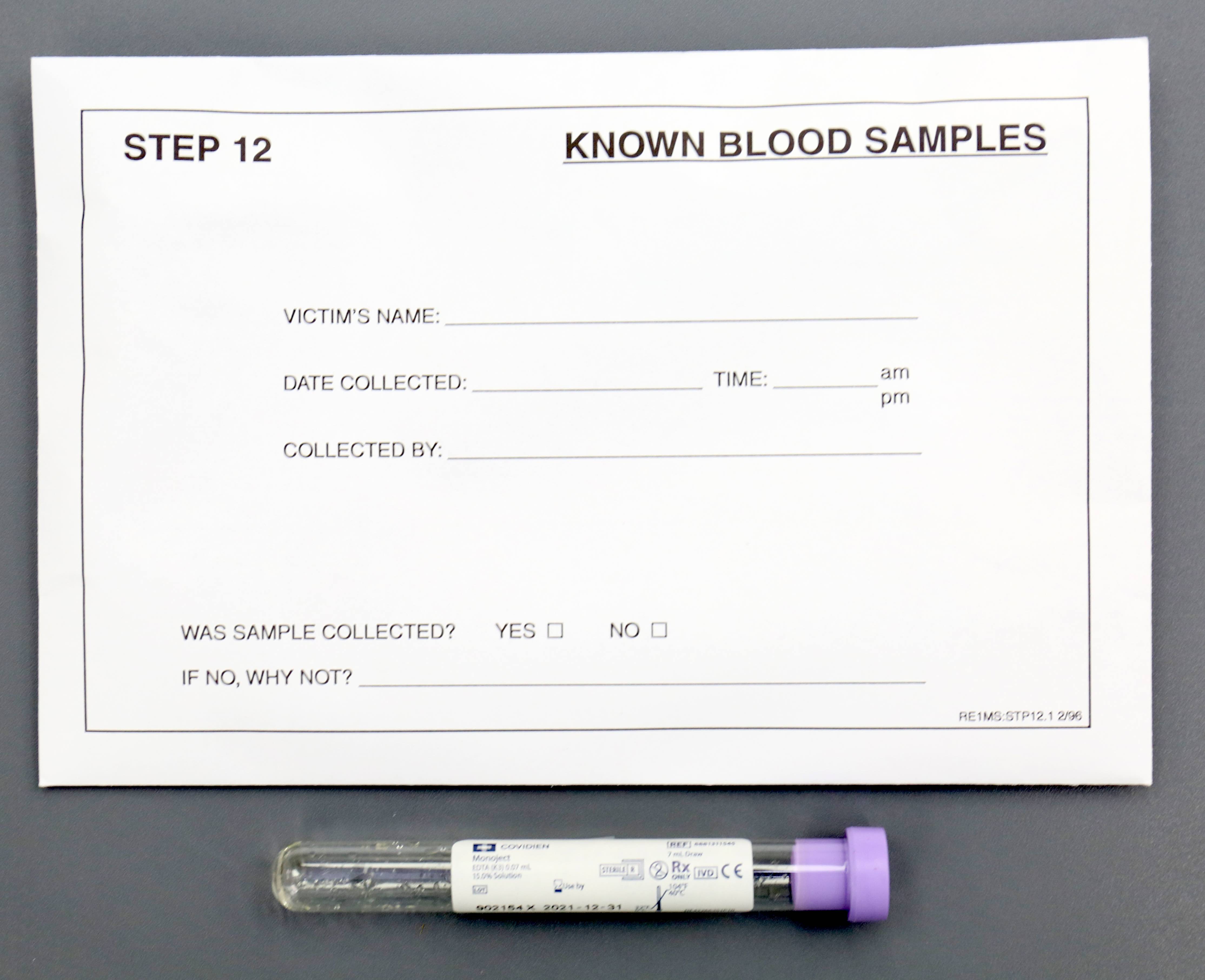
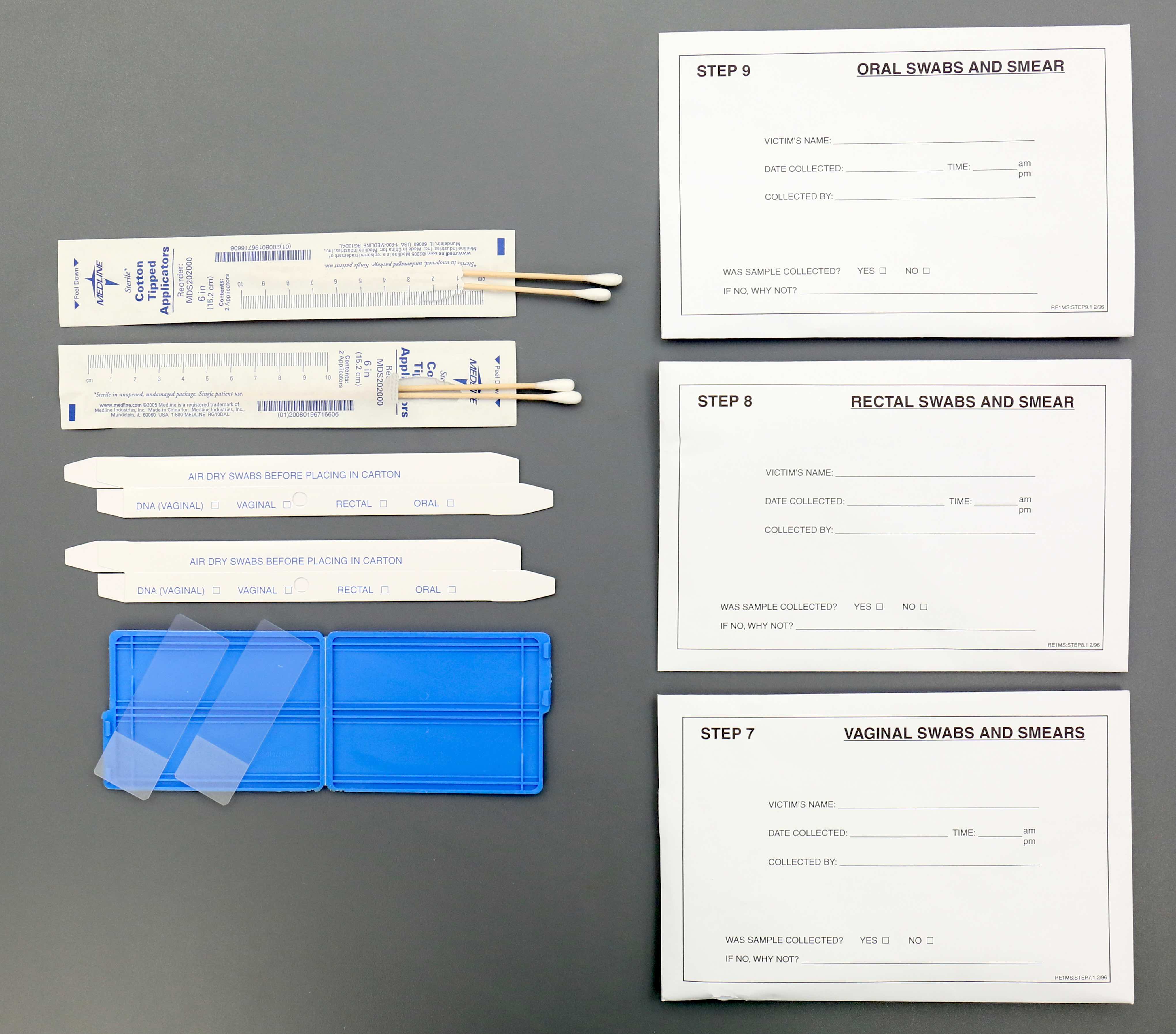
- Use a sexual assault kit that contains sterile saline, cotton tip swabs, a speculum, an anoscope, glass slides, envelopes, combs, self sealing bags and a white bedsheet
- Cotton tip swabs to collect DNA are first wet with sterile saline and 2 sets are swabbed to any area of the body (bite marks, breasts and around the neck); start from the top of the body and move down, air dry the swabs and place in the correctly labeled envelope
- Cervix, anal and rectal swabs are taken before vaginal swabs because fluid from the vagina drips down
- Speculum is inserted into the vagina to visualize the cervix and is swabbed
- Vaginal and cervical swabs are smeared on glass slides to visualize sperm; sperm can be recovered from the body days after death
- Anoscope is used to visualize the anus for trauma and swabbed
- Pubic and scalp hair is combed and pulled in different areas and each is placed in separate envelopes (labeled "pulled hair" and "combed hair"); combing allows the collection of foreign hairs and fibers
- Self sealing bags are used to collect and preserve evidence, like any clothing
- White bedsheet goes under the body to catch any missed evidence
Results:
- Swabs and other evidence collected are used for DNA analysis
- Even if no sperm are identified, chemical tests, like acid phosphatase, can be positive in absence of sperm (J Forensic Leg Med 2013;20:578)
Limitations:
- Decedent's body that is washed before the autopsy inhibits collection
- Improper order of evidence collection at autopsy
Essential features:
- Do not wash the body before evidence collection
- Take swabs of the cervix, anus and rectum because fluid from the vagina drips down the perineum and can contaminate results
- Vaginal and cervical slides can be made to look for sperm
- Comb and pull pubic and scalp hair in various locations and put it into separate envelopes to collect foreign hairs and fibers
Contributed by Myra Khan, D.O.
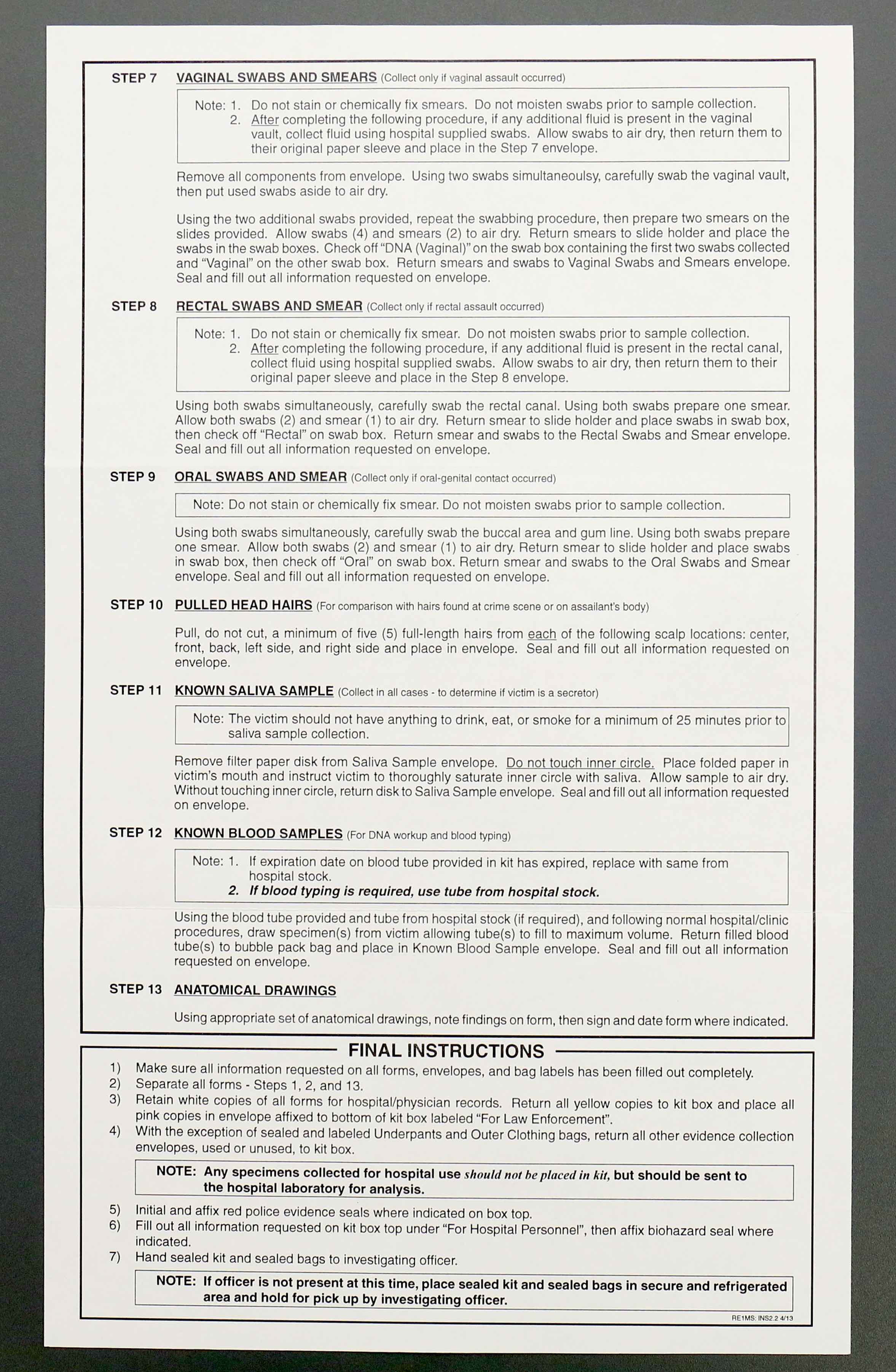
- To identify decedents, suspected cases of sexual assault, physical assault in which DNA could have been transferred between individuals and paternity testing
Specimens:
- Any tissue with nucleated cells, commonly semen and blood but also the follicle in pulled hair, saliva in bite marks, fingernail clippings and skeletal muscle
- In advanced decomposition, teeth, ribs and femurs are sufficient
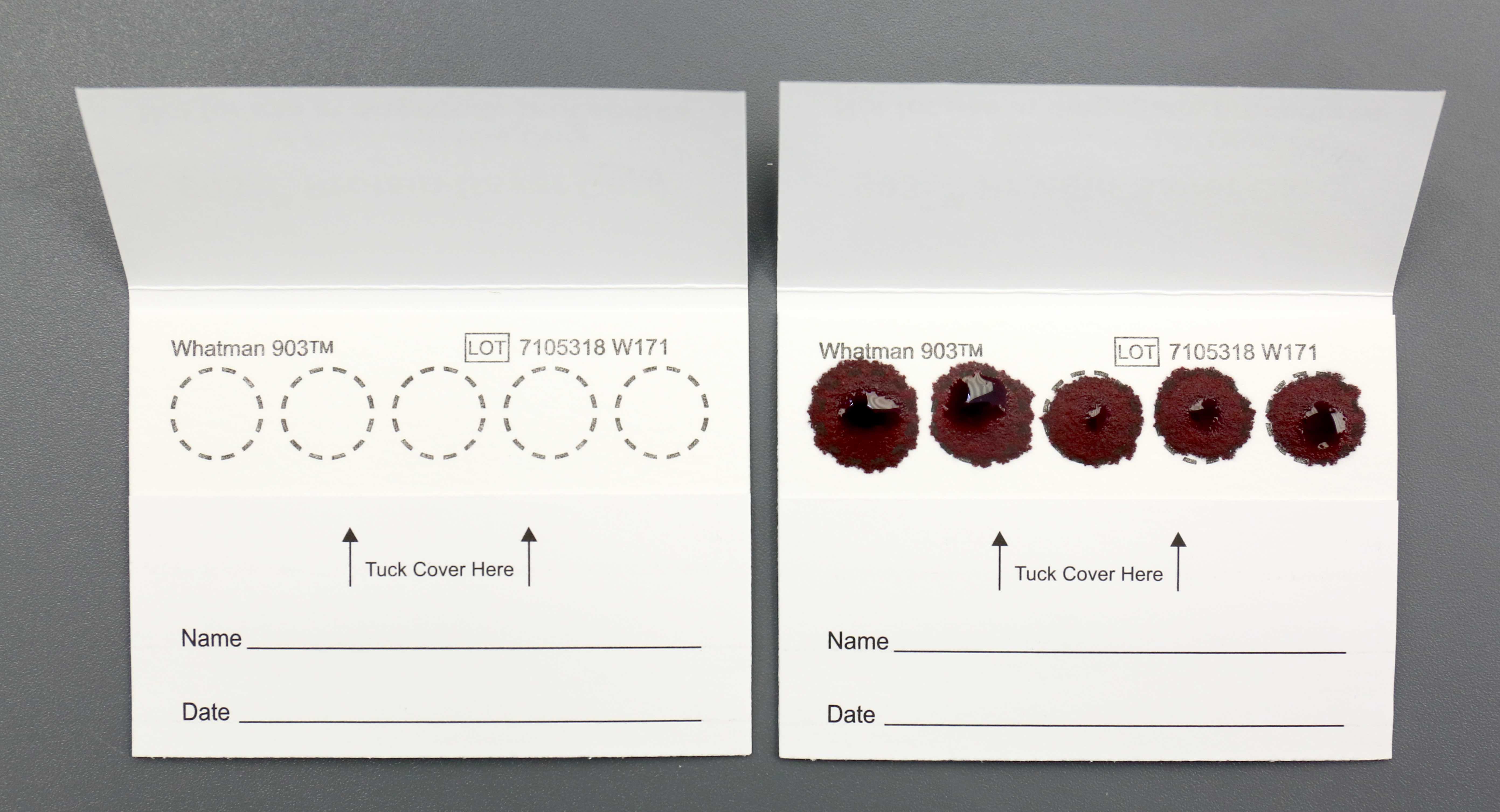
- Blood preserved on DNA spot cards
Methods:
- PCR:
- Amplifies short DNA sequences of specific alleles (Exp Mol Med 2001;33:101)
- Advantages: simple, short turnaround time and analyzes very small amounts of DNA (0.1 to 1.0 ng)
- Disadvantages: susceptible to contamination and PCR loci have few alleles it will recognize
- Short tandem repeats (STR):
- PCR used to identify DNA with high discriminatory power
- STR loci are repeating sequences of 2 - 6 base pairs that occur every 1 in 10,000 nucleotides and are unique to each individual
- In the U.S., 13 STR loci are used and the average random match probability is rarer than 1 in a trillion among unrelated people (Am J Hum Genet 1994;55:175)
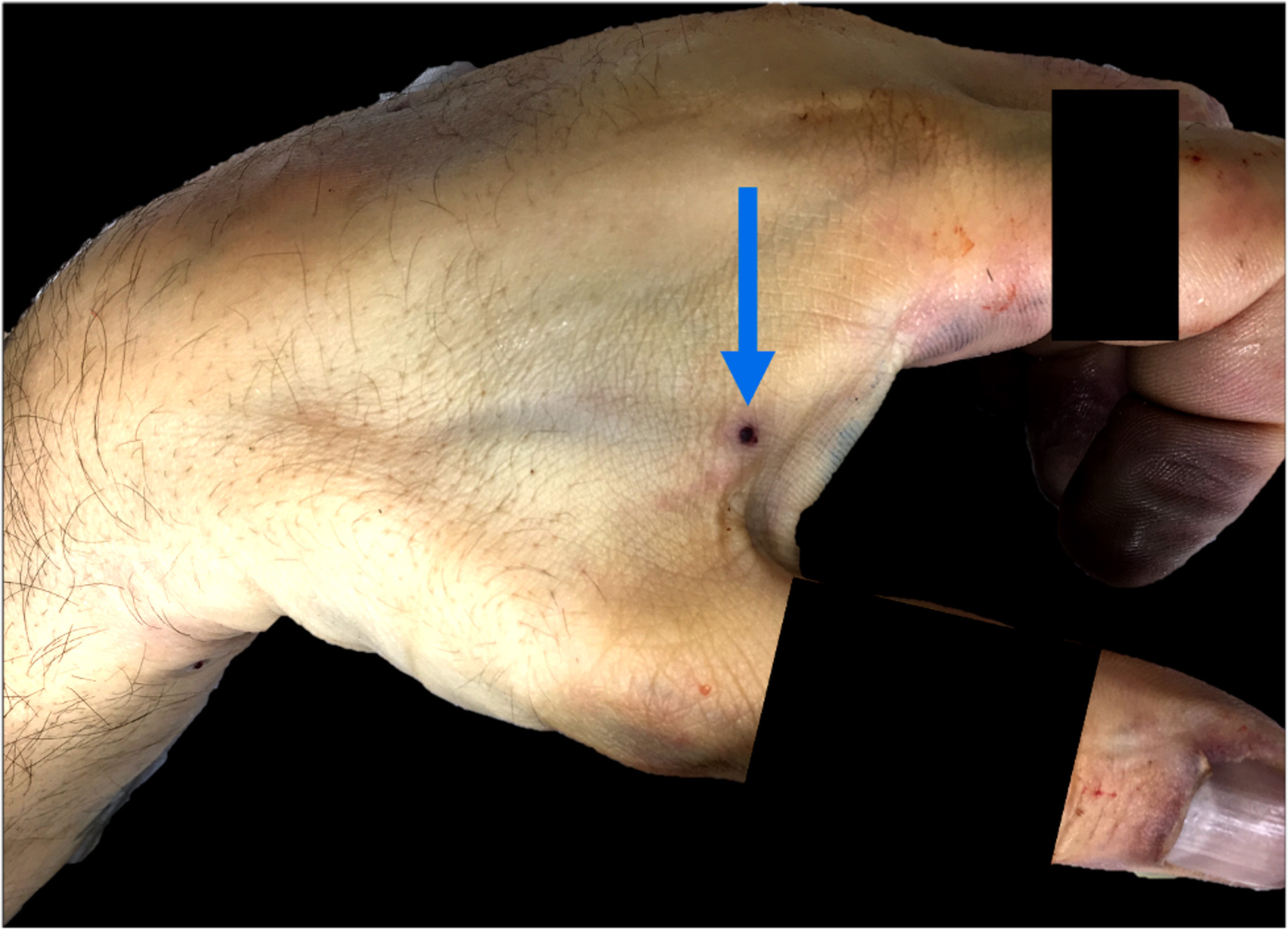
- Advantages: rapid and need small amount of DNA (like wiping from a full metal jacket penetrating a body)
- Mitochondrial DNA (mtDNA):
- Found in the cytoplasm and inherited maternally
- Siblings and maternal relatives have identical mtDNA
- Only used when biological material to be analyzed is scant or degraded (Cells 2019;8:100)
How to interpret:
- Insufficient amount of DNA means the specimen is inadequate in size, degraded or contaminated
- DNA profiles match, which can mean:
- Samples are from the same person
- Error in collection or at the lab occurred and the samples actually came from different people
- 2 individuals have the same DNA profile, such as identical twins
- Not enough tests were performed to differentiate between the 2 samples
- Different DNA profiles mean the DNA does not match the test subject
Limitations:
- In completely skeletonized decedent remains, it is challenging to collect adequate amounts of DNA
Essential features:
- DNA is collected at autopsy in the form of semen and blood
- Techniques for DNA identification are PCR, STR and mtDNA
- Even if DNA profiles match, caution should be maintained, as there may have been an error in collection or not enough tests performed to differentiate between the 2 samples
Contributed by Myra Khan, D.O.
A 55 year old woman presents to the emergency room with chest pain and is diagnosed with a myocardial infarction. Despite medical intervention, she dies and an autopsy is performed. Based on the histological image of the myocardium, what is the age of the myocardial infarct?
- Acute myocardial infarct
- Between a subacute and chronic / remote myocardial infarction
- Chronic / remote myocardial infarct
- Subacute myocardial infarct
A 65 year old alcoholic man is found dead on the sidewalk. At autopsy, a purulent abscess is identified in his right middle lung lobe and sterile cultures of the lung are taken. The cultures grow Klebsiella pneumoniae and the histological exam of the lungs is significant for acute pneumonia. Toxicology did not detect drugs of abuse. No other significant natural disease is identified. What is the cause of death?
- Acute alcohol intoxication
- Acute on chronic alcoholism
- Acute pneumonia
- Chronic alcoholism
- Asphyxia: generic term that indicates a condition resulting from an interference with respiration due to the lack of oxygen in the air or in the blood, a failure of cells to utilize oxygen or a failure of the body to eliminate carbon dioxide
- Body does not receive or utilize an adequate amount of oxygen
- Impairment of oxygen and carbon dioxide exchange
- Loss of consciousness and death result from progressive hypoxia / anoxia
- Numerous classifications are reported in the literature
- Types of asphyxia: suffocation (smothering, choking, confined space and vitiated atmosphere), strangulation (hanging, manual strangulation, ligature strangulation), mechanical (positional, compression), drowning, special types (autoerotic, incaprettamento, judicial hanging, mass suicide hanging)
- 3 main mechanisms: respiratory, vascular and nervous
- External findings are nonspecific but may support the diagnosis: ligature marks, petechiae, cyanosis
- Internal findings suggestive of asphyxia: hyoid and larynx injuries, neck muscles hemorrhage, visceral petechiae
- Numerous classifications are reported in the forensic literature (J Forensic Sci 2010;55:1259):
- A comprehensive classification of asphyxia in the forensic context includes:
- Suffocation: asphyxia due to the mechanical obstruction of the respiratory orifices or inadequate amount of oxygen in the environment (smothering, choking, confined spaces / vitiated atmosphere) (West J Emerg Med 2018;19:707)
- Strangulation: asphyxia due to external compression of the neck using the body's own weight or a force other than the body's weight (hanging, ligature strangulation, manual strangulation) (J Emerg Trauma Shock 2011;4:320)
- Mechanical asphyxia: asphyxia due to impaired breathing secondary to the body being in an unnatural position or severe compression to the neck, chest or other areas of the body that make respiration difficult or impossible (positional asphyxia, traumatic asphyxia, smothering, choking and strangulation)
- Drowning: asphyxia due to partial or complete submersion of the body in a liquid resulting in liquid inhalation, impairment of pulmonary exchanges and oxygen deprivation (Acad Forensic Pathol 2018;8:8)
- Special types: asphyxias that show combined or unusual mechanisms
- A comprehensive classification of asphyxia in the forensic context includes:
- Classically, asphyxia has been described as the result of the impairment of 3 components (single or combined) (J Forensic Sci 2010;55:1268)
- Respiratory: obstruction of the airways or impairment of respiration
- Usually, it is not the primary mechanism
- Results in progressive or sudden partial pressure of oxygen (PO2 - the amount of oxygen gas dissolved in the blood) reduction until it reaches levels that are incompatible with life
- Vascular: compression of the neck vessels
- Vascular mechanism is responsible for the rapid loss of consciousness
- Significant arterial blood flow reduction (carotid arteries account for approximately 67% of cerebral blood flow)
- Jugular vein compression resulting in stasis and congestion
- Nervous: the compression or stimulation of specific reflex areas of the neck may result in immediate death
- Carotid sinus: located at the base of the internal carotid artery just superior to the bifurcation of the internal carotid and external carotid; compression of the carotid sinus is a hypothesized cause of sudden death (J Forensic Sci 2013;58:1644)
- Vagus nerve: vagal stimulation is a known cause of potential life threatening cardiac events, including cardiac arrest and sudden death (Head Neck 2016;38:E2419, Heart 2011;97:623)
- Respiratory: obstruction of the airways or impairment of respiration
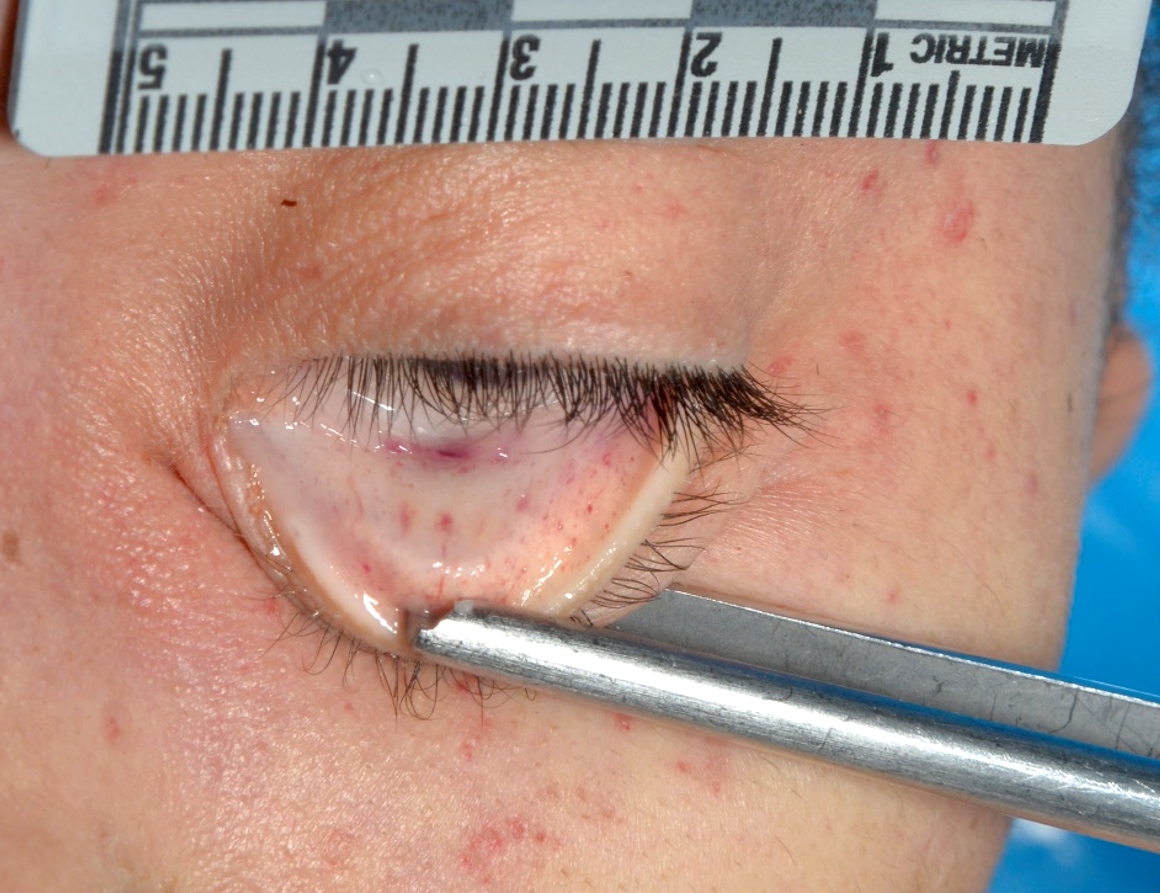
- External findings:
- Nonspecific but may support the diagnosis in the context of a thorough medicolegal investigation
- Ligature marks: marks made by any cord-like objects used for the purposes of strangulation
- Different patterns and features (see Strangulation)
- Petechiae: pinpoint hemorrhages frequently observed in asphyxia related deaths
- Caused by an acute rise in venous pressure, resulting in overdistension and rupture of thin walled vessels (Forensic Sci Int 2002;126:210, Am J Forensic Med Pathol 2011;32:378)
- Generally observed on the face and eyes but can also be seen on the chest or neck
- Conjunctiva is the most common location (Am J Forensic Med Pathol 1988;9:32)
- Overstretching of the eyelids may help in highlighting petechiae on their external surface
- Can also be found in other types of deaths (J Forensic Sci 2000;45:1274)
- Prone position of the body may result in petechiae formation due to hypostatic blood redistribution (Forensic Sci Med Pathol 2019;15:13)
- Cardiopulmonary resuscitation can result in artifactual conjunctival petechiae (J Forensic Leg Med 2010;17:87)
- Cyanosis: bluish discoloration of the skin
- From the Greek term κυανός, which means dark blue
- Depends on the absolute amount of reduced hemoglobin in the arterial blood
- Requires at least 5 g of reduced hemoglobin per 100 mL arterial blood (StatPearls: Central and Peripheral Cyanosis [Accessed 20 May 2022])
- In asphyxia with neck compression, cyanosis is typically observed on the face as a result of the jugular veins obstruction, which prevents adequate venous return from the cerebral circulation (J Forensic Sci 2015;60:1216)
- Postmortem lividity may mimic facial cyanosis if the victim was found in a prone position: let the body rest for 12 - 24 hours in a supine position to evaluate the attenuation of the lividity and distinguish it from real cyanosis (Am J Forensic Med Pathol 2019;40:129)
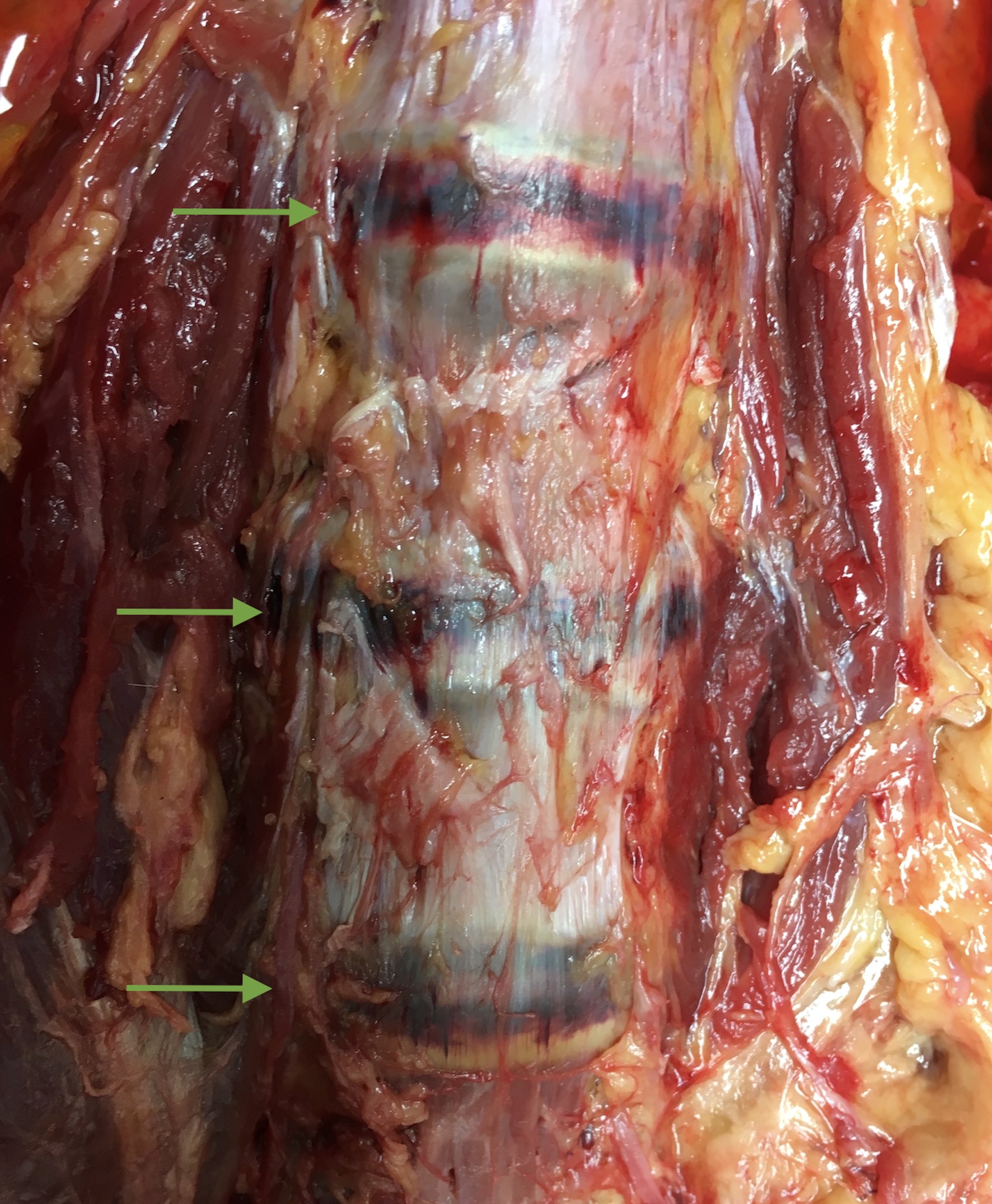
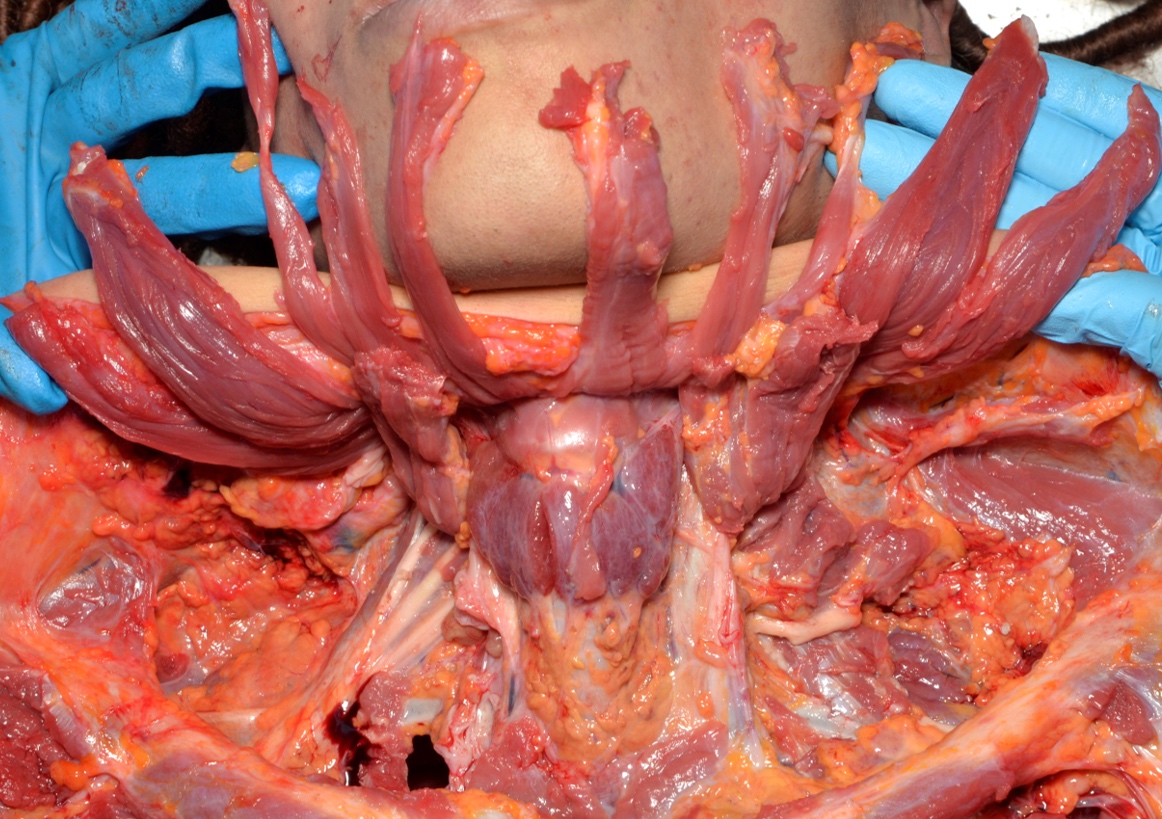
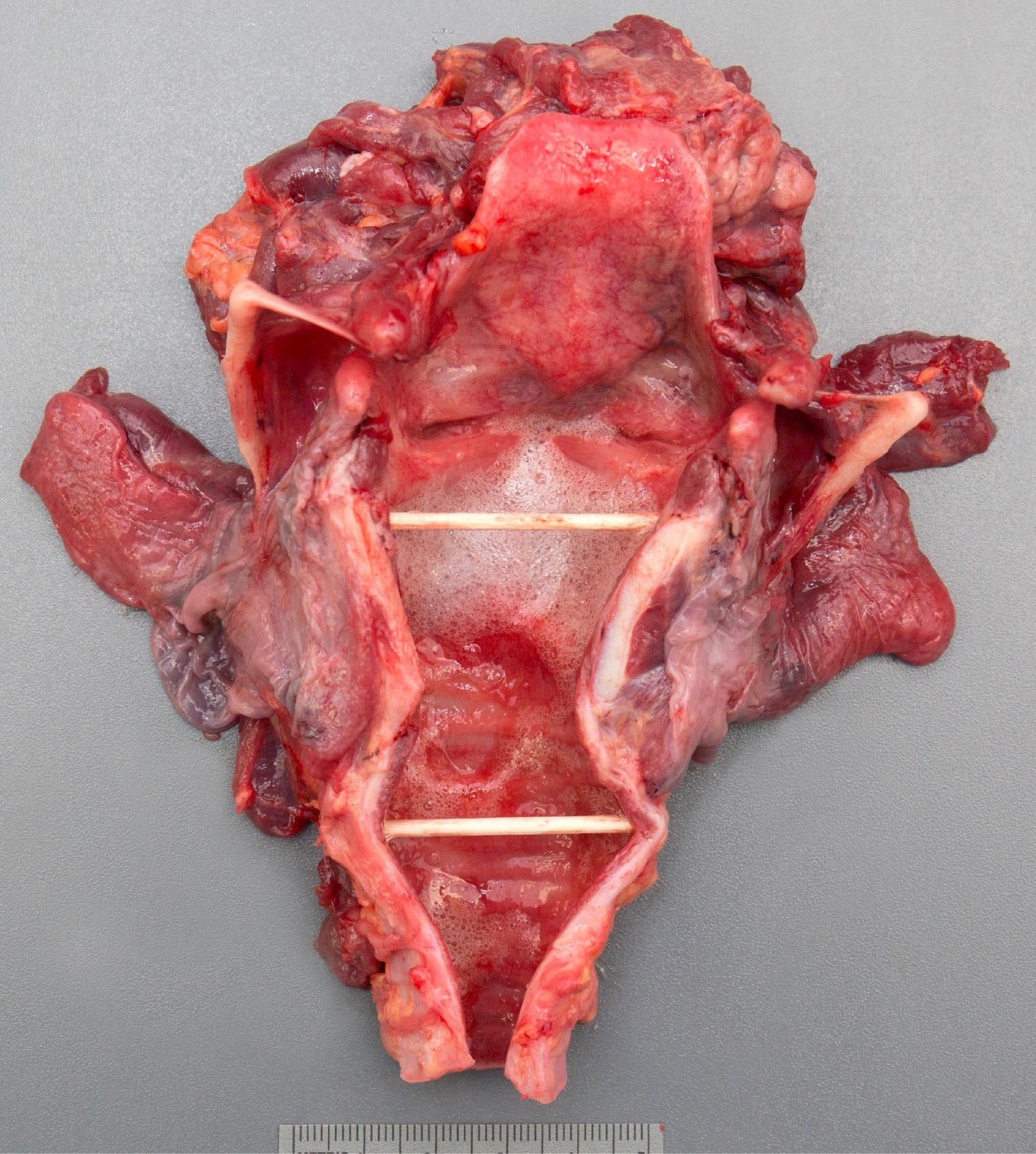
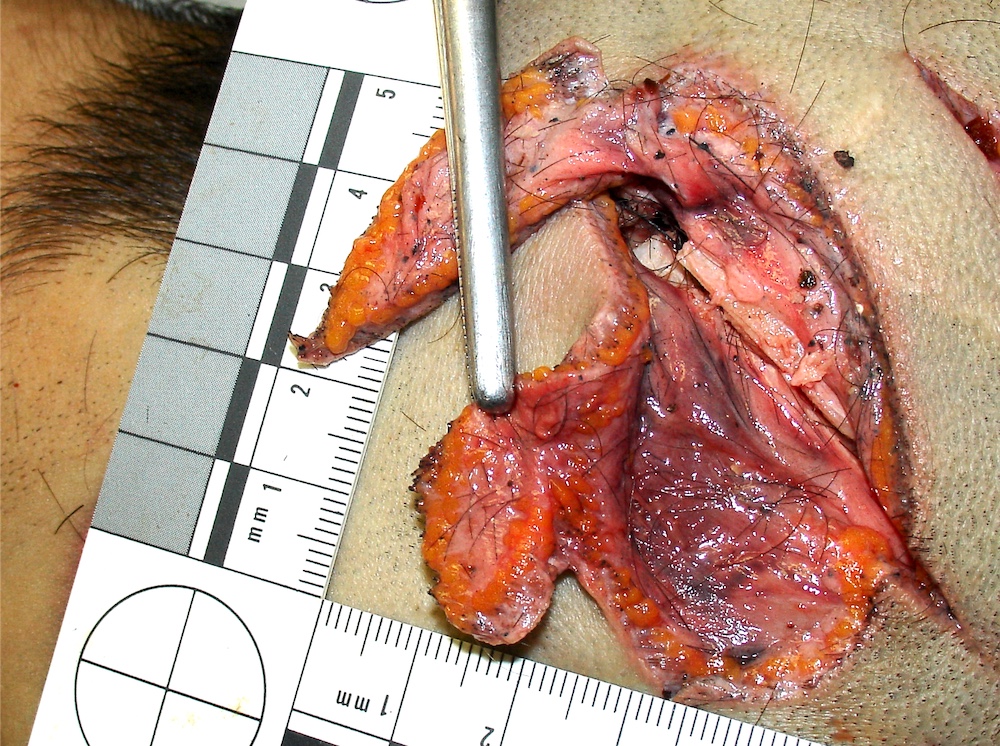
- Autopsy findings: neck injuries may be observed in asphyxias with neck compression mechanisms
- Layer by layer dissection of the anterior neck following vascular decompression of the neck is critical to evaluate the neck structures (Acad Forensic Pathol 2016;6:45)
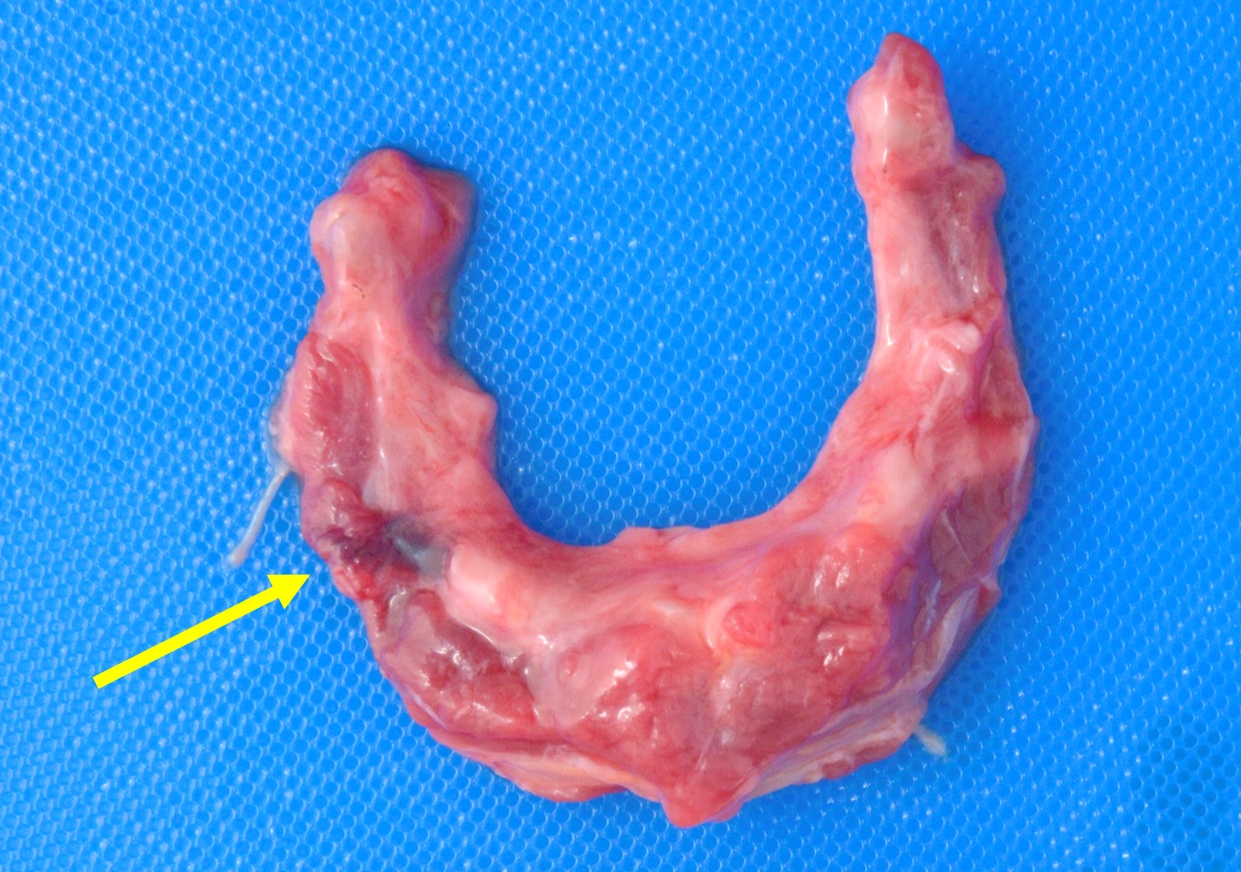
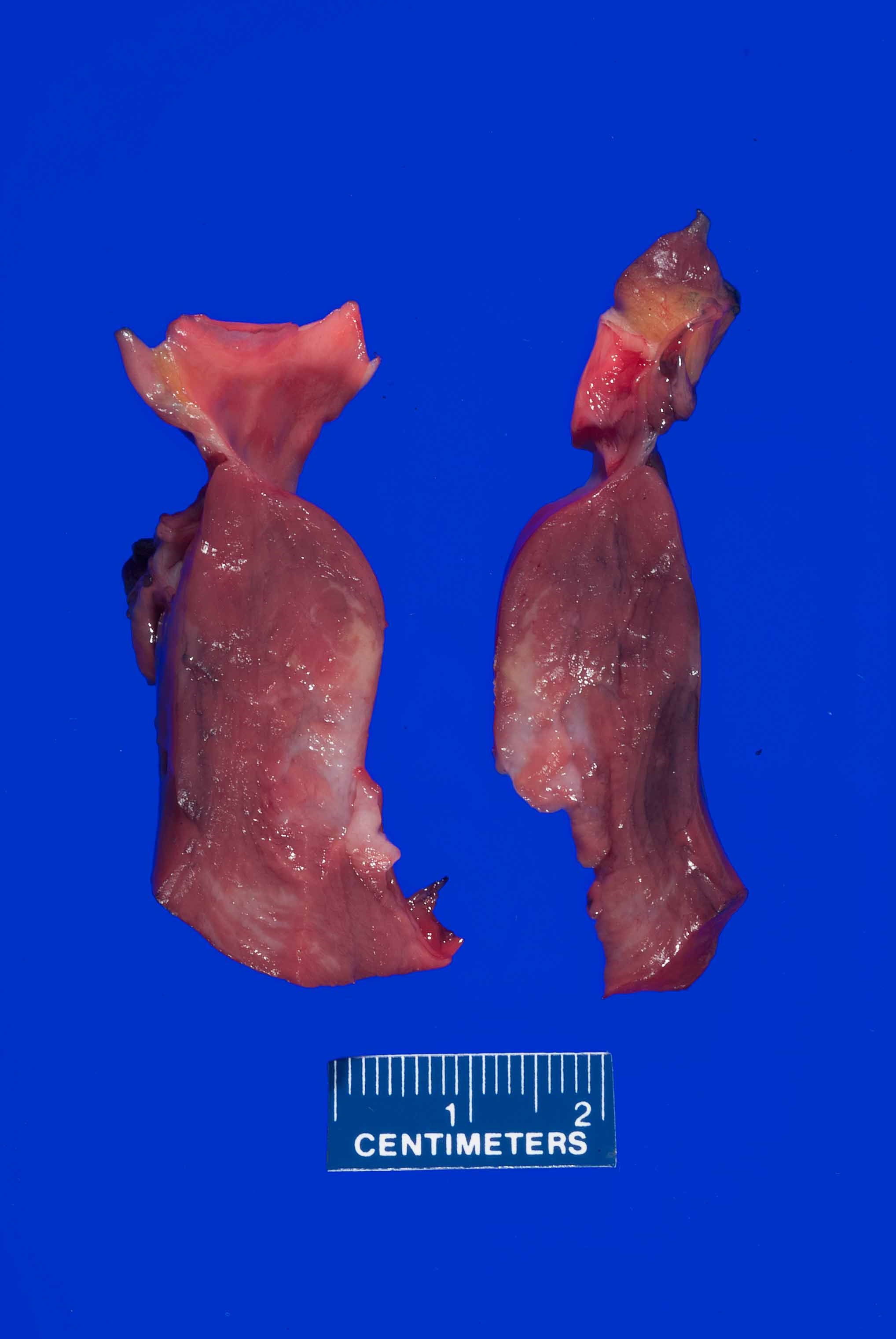
- Hyoid bone:
- U shaped bone located in the neck anteriorly between the mandible and the larynx
- More commonly injured in homicides (J Forensic Sci 1996;41:110)
- Fractures are more commonly observed in manual strangulation than in ligature strangulation (Leg Med (Tokyo) 2010;12:113)
- Less frequently injured in hanging than in strangulation; mostly observed in lateral hangings (Forensic Sci Int 2018;290:70, Journal of Indian Academy of Forensic Medicine 2005;27:149)
- The younger the individual, the greater the force required to fracture the hyoid bone (Forensic Sci Int 2013;228:47)
- Histology is rarely required but may help in identifying hyoid fractures in the absence of grossly visible hemorrhage (Forensic Sci Med Pathol 2012;8:307)
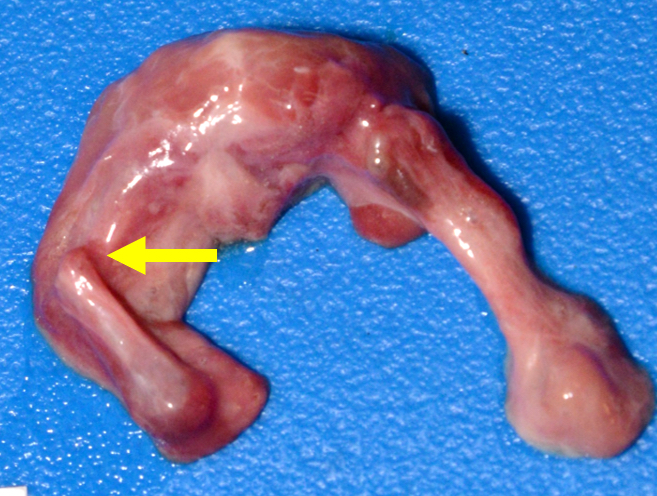
- Larynx (Acad Forensic Pathol 2016;6:486):
- Injuries generally seen in homicide by manual strangulation
- Less frequent in hanging
- May occur after an accidental fall or sport activities
- Possible injuries following resuscitation maneuvers (Am J Forensic Med Pathol 1999;20:31)
- Neck muscles:
- Muscles hemorrhage may be found in neck compressions
- It can be difficult to differentiate the hemorrhages associated with postmortem hypostasis from true bruising caused by strangulation (Am J Forensic Med Pathol 2009;30:322)
- Bodies found in the prone position typically show extensive lividity involving the face and neck, which may result in hypostatic hemorrhages within the soft tissues of the neck
- Hemorrhages may be the result of medical treatments or artifact due to resuscitation maneuvers (J Forensic Leg Med 2015;33:39)
- Visceral petechiae (subpleural or subepicardial) are not specific since they can be observed in asphyxia as well other conditions, such as sepsis and infections
- Congestion and edema:
- Can be seen in any autopsy (nonspecific)
- Due to obstructed venous return and subsequent tissues swelling
- Generally observed on the face, neck and chest organs
- Skin:
- Microscopic examination may be used to determine if a ligature mark on the neck was produced before death or postmortem (Am J Forensic Med Pathol 2017;38:211)
- Common findings: breaking, wrinkling and compression of skin along with micro hemorrhages and inflammatory changes in subcutaneous tissues (J Addict Depend 2016;2:1)
- Lungs:
- Acute pulmonary emphysema with septal rupture and hemorrhage, foreign bodies aspiration, congestion, interstitial and intra-alveolar edema, alveolar hemorrhage (Am J Forensic Med Pathol 2001;22:139, Int J Legal Med. 2016;130:1281)
- Broad spectrum of conditions
- Generally indicates a mechanical obstruction of the respiratory orifices or inadequate oxygen in the environment, resulting in the failure of oxygen to reach the blood
- Respiratory component is the primary mechanism involved in this type of asphyxia
Smothering
- Mechanical obstruction of the mouth and nose by hands, soft or hard material, or mobile solids able to block airflow
- Autopsy findings may be minimal or absent
- Homicide:
- Victims are usually elderly, children or debilitated subjects
- Requires a remarkable physical disproportion between the aggressor and the victim
- Usually committed by hands or other material (pillows, cloth, adhesive tape, etc.)
- Autopsy findings:
- Usually scarce
- Tears and lacerations of the labial, buccal and gingival mucosa
- Nasal bleeding and nasal bone fractures
- Facial abrasions
- Presence of facial injuries may indicate that the victim was alive and actively tried to resist the aggression
- If a pillow or a cloth is used, vital aspiration of fabric fibers may be proved at histology (Int J Legal Med 2009;123:517)
- Pediatric deaths:
- Usually no external signs due to the physical disproportion between aggressor and victim
- Difficult to prove
- Suicide:
- Less common than homicides
- Plastic bag suffocation is the main method of suicidal smothering (J Forensic Sci 2016;61:361)
- Head is inside a limited space
- During inspiration, the plastic bag adheres to the face, obstructing the mouth and nostrils
- There is a combined mechanism of mechanical obstruction and rapid oxygen depletion (see Vitiated atmosphere)
- Can be combined with inert gas inhalation
- Can be homicidal (when the victim is impaired)
- Can be accidental (children playing with plastic bags)
- Accident:
- Typically observed in children
- Investigation findings and clinical history typically support the diagnosis (Paediatr Child Health 2006;11:493)
- Rarely observed in adults (Med Sci Law 1992;32:68)
- Soft bedding: the infant's airway is obstructed by an adult mattress, blanket, pillow, couch cushion or other soft object in the immediate sleep environment (Pediatrics 2019;143:e20183408)
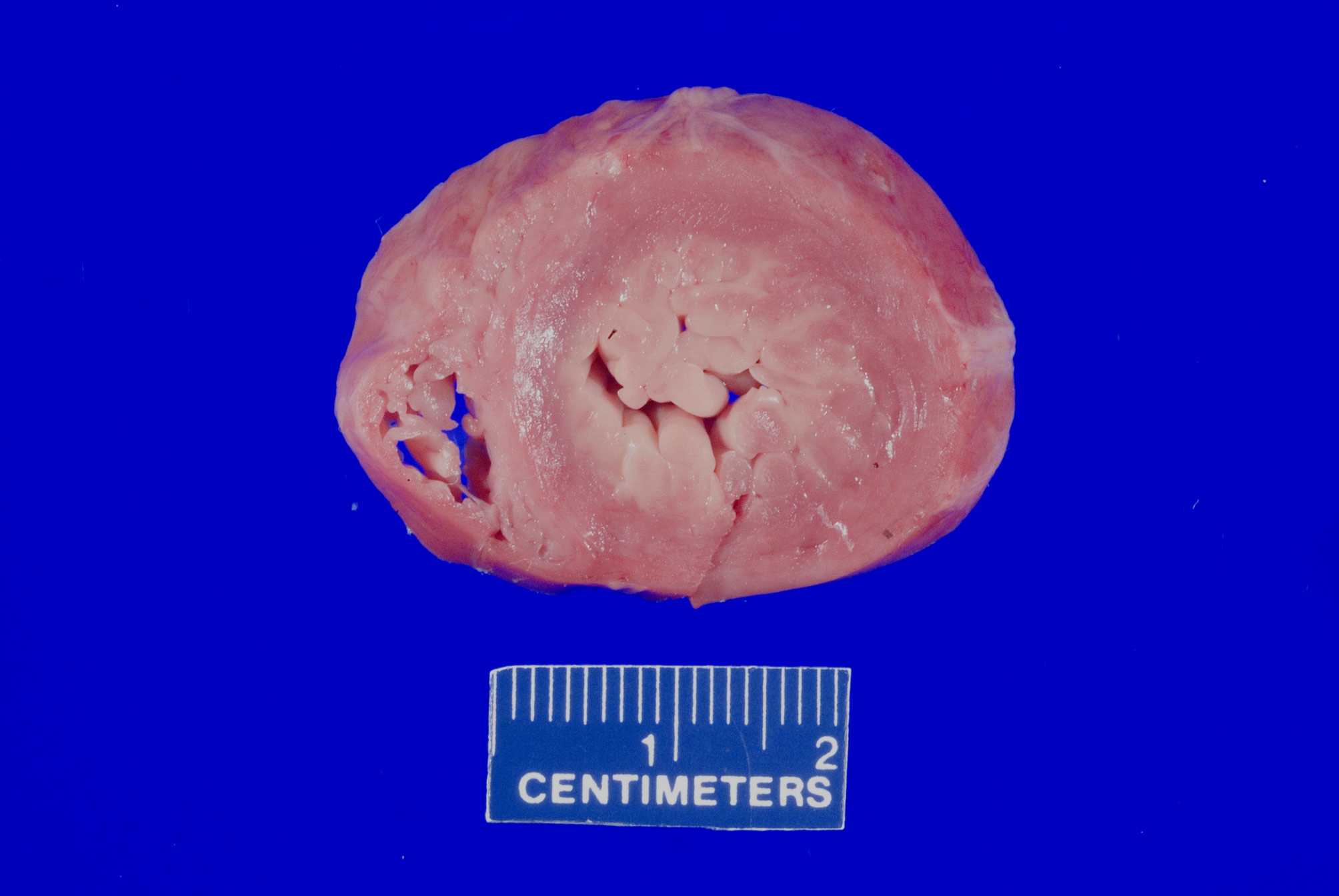
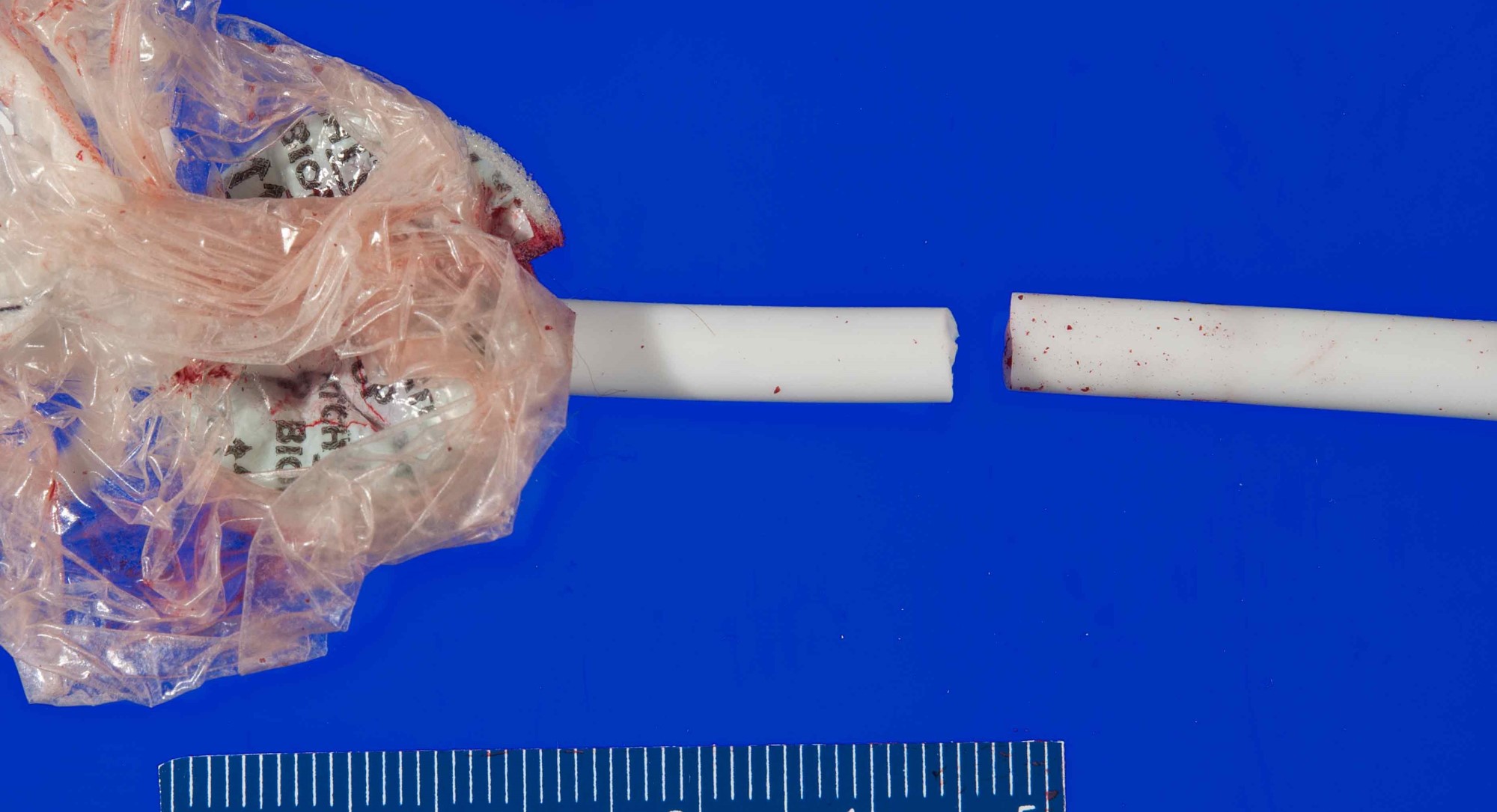
Choking
- Occlusion (partial or total) of the airways by foreign bodies, leading to respiratory blockage and potentially death
- Can be observed in any age category but typically in the elderly and children
- Diagnosis is usually suspected based on the clinical history
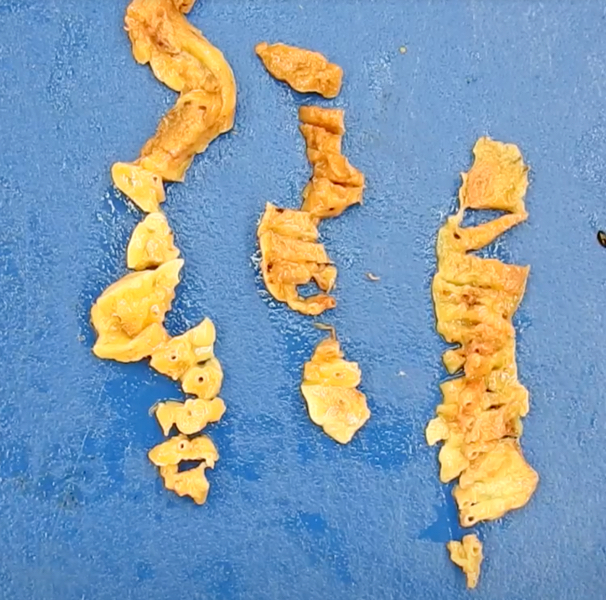
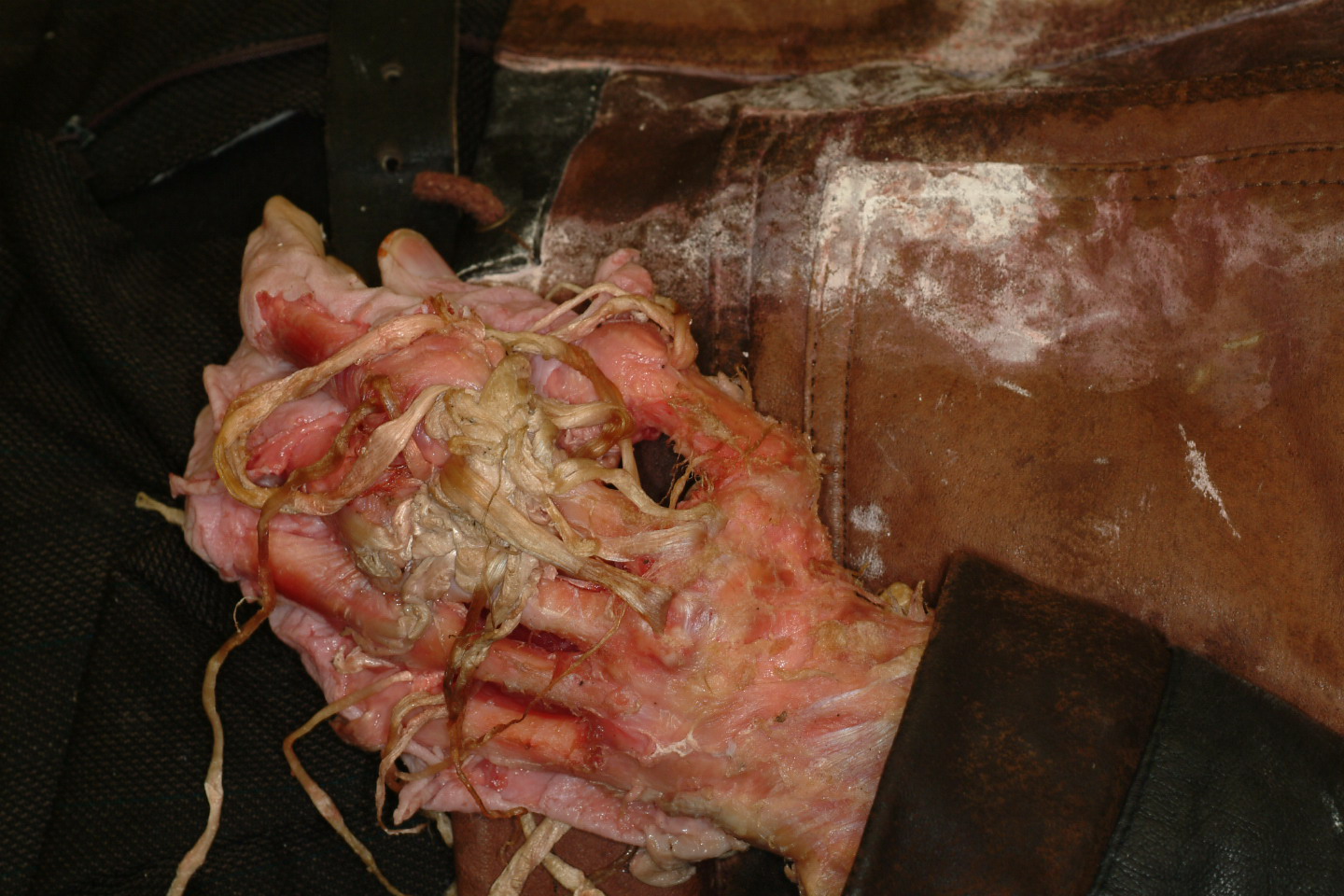
- Diagnosis is confirmed at autopsy when the airway is found occluded and the foreign body is retrieved
- Accident is the most common manner of death in choking
- Elderly: typically in subjects with poor dentition, neurologic deficit, swallowing problems or psychiatric disorders (J Forensic Sci 2007;52:176)
- Food is the most common foreign body
- Children: typically occurs while playing
- Multiple possible foreign bodies: food, toys, coins, batteries, etc. (Mo Med 2015;112:181)
- Alcohol and drugs may increase the risk of choking in otherwise healthy subjects (J Forensic Sci 2011;56:128)
- Ethanol inhibits the elicitation of the upper esophageal sphincter contractile reflex and reflexive pharyngeal swallow (Am J Gastroenterol 2009;104:2431)
- Café coronary syndrome: sudden collapse of apparently healthy subjects during meals in the absence of any sign of asphyxia, respiratory distress or neurological symptoms (Med Leg J 2021;89:264)
- Typically occurs when the subject swallows a food bolus (usually meat) larger than the esophagus can accept
- Victims are typically elderly with poor dentition and history of neurological or psychiatric disorders
- Due to the absence of choking symptoms, the death is commonly erroneously attributed to myocardial infarction
- Most fatal cases are unwitnessed
- Homicide is uncommon:
- Foreign body is forced into the victim's airway
- Can be mistaken for suicide or accident (Med Sci Law 1992;32:65)
- Suicide is uncommon:
- Can be suspected if the victim has a history of psychiatric disorder and previous suicide attempts (Clin Ter 2017;168:e293)
- Elderly: typically in subjects with poor dentition, neurologic deficit, swallowing problems or psychiatric disorders (J Forensic Sci 2007;52:176)
Confined space and vitiated atmosphere
- Confined space: asphyxia from oxygen deprivation (J Forensic Sci 2001;46:708)
- May be associated with heat stroke and positional asphyxia (J Forensic Leg Med 2015;34:139)
- Vitiated atmosphere: conditions in which there is air contamination or oxygen displacement / replacement / depletion by other gases (Forensic Sci Med Pathol 2019;15:646, Acad Forensic Pathol 2019;9:93)
- Oxygen may be reduced or eliminated from respired air by other gases
- Some gases are more rapidly absorbed by hemoglobin than oxygen
- Carbon dioxide: colorless gas with a faint sharp odor and a sour taste
- Replaces oxygen in the atmosphere causing hypoxia (Int J Emerg Med 2017;10:14, Acad Forensic Pathol 2019;9:93)
- Carbon monoxide: colorless, odorless and nonirritable gas (Toxicol Rep 2020;7:169)
- Has affinity for hemoglobin 200 - 300 times greater than oxygen
- Combines with hemoglobin to form carboxyhemoglobin, which has a characteristic pink color at autopsy when its saturation exceeds 30% (cherry red skin and lividity)
- Death is uncommon for carboxyhemoglobin concentrations
- Cyanide: colorless gas at higher temperatures with a bitter almond odor
- Produced by combustion of plastic
- Binds to the iron atom in mitochondrial cytochrome C oxidase and acts as an irreversible enzyme inhibitor (J Bioenerg Biomembr 2008;40:533)
- Prevents cellular respiration, leading to cellular hypoxia (Toxicol Res 2012;28:195)
- Hydrogen sulfide: colorless gas with a classic rotten egg odor
- Toxicity commonly results from occupational exposure (e.g., sewer gas exposure) (Am J Emerg Med 2008;26:518.e5)
- Inhibits mitochondrial cytochrome oxidase with subsequent arrest of aerobic metabolism (Toxicol Sci 2002;65:18)
- Neurotoxic (Biochem Pharmacol 2018;149:5)
- Nitrogen: odorless, colorless, tasteless and mostly inert diatomic gas
- Displacement of oxygen in the atmosphere (Am J Forensic Med Pathol 2008;29:235)
- Typically observed in accidental scuba diving related deaths (decompression injuries) (Hawaii J Med Public Health 2014;73:13)
- Suicides are described (Med Sci Law 2019;59:57)
- Decrease in atmospheric pressure results in reduced gas exchange in the lungs (StatPearls: Aerospace Pressure Effects [Accessed 20 May 2022])
- Increases in altitude result in decreasing total atmospheric pressure, which means the oxygen available for breathing is decreased as well
- Accident is the most common manner of death:
- Common causes: poorly functioning gas heating systems or furnaces, inhaled smoke from fires, motor vehicle exhaust fumes (J Forensic Leg Med 2017;48:23)
- Homicide is rare:
- May involve the use of toxic gases (Forensic Sci Med Pathol 2014;10:97)
- Suicide commonly due to carbon monoxide intoxication from car exhaust (Forensic Sci Int 2006;161:41)
- Carbon dioxide: colorless gas with a faint sharp odor and a sour taste
- Asphyxia due to an external compression of the neck
- Can be suicidal (body's own weight), accidental or homicidal (a force other than the body's weight)
Hanging
- Fatal compression of the neck by means of a ligature that is constricted by the weight of the body
- Full body weight is not needed to cause hanging
- 4 pounds of pressure is required to occlude jugular veins (preventing venous drainage of head) and 5 - 11 pounds to occlude carotid arteries
- Loss of consciousness occurs within 10 - 15 seconds; death within 3 - 5 minutes
- Amount of body weight changes based on body positions and different hanging types (J Forensic Sci 2010;55:1278)
- Amount of body weight needed to cause hanging can be roughly estimated (Forensic Sci Int 2001;123:172)
- Full body weight is not needed to cause hanging
- Types of hanging:
- Based on the degree of body suspension (J Emerg Trauma Shock 2011;4:320):
- Complete (suspension hanging): the whole body is suspended
- Partial (incomplete): the body is partially touching the ground
- Based on the location of the knot (Mymensingh Med J 2008;17:149):
- Typical hanging: the knot of the ligature should be at the nape of the neck and the point of suspension is in the occipital area
- Atypical hanging: the knot of the ligature at any site other than the nape of the neck
- Based on the degree of body suspension (J Emerg Trauma Shock 2011;4:320):
- Other terms related to hanging:
- Near hanging: when a subject survives a hanging injury long enough to reach the hospital (J Clin Diagn Res 2015;9:HC01)
- Anoxic brain injury is the most common complication (Am Surg 2019;85:549)
- Judicial hanging: modality of public execution for capital crimes
- Fractures of the cervical spine are common (e.g., hangman fracture) (Med Sci Law 2009;49:18)
- Near hanging: when a subject survives a hanging injury long enough to reach the hospital (J Clin Diagn Res 2015;9:HC01)
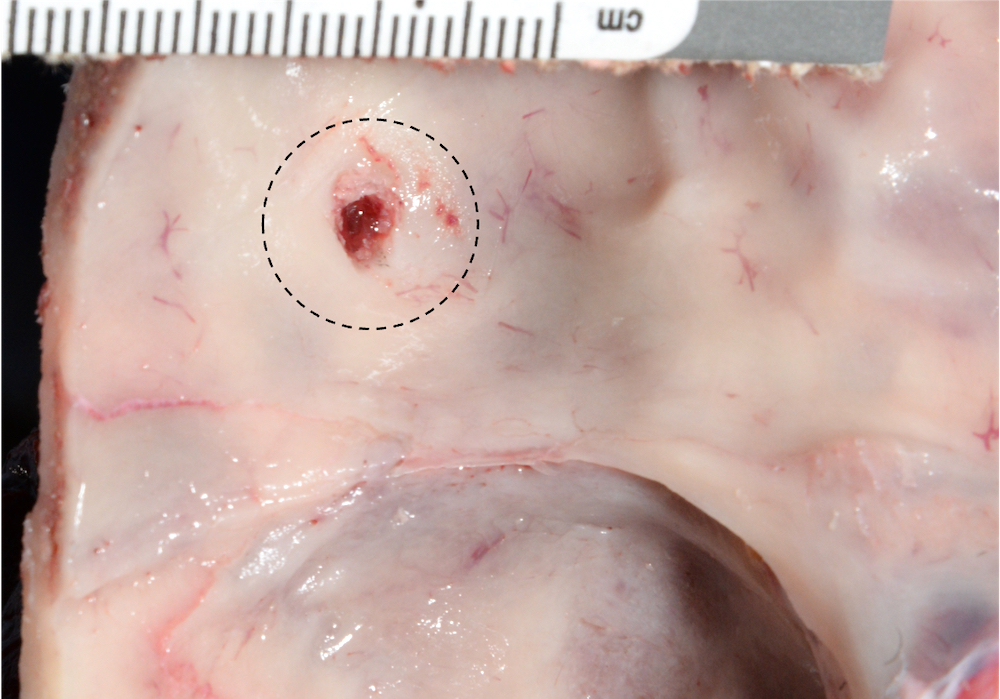
- Autopsy findings:
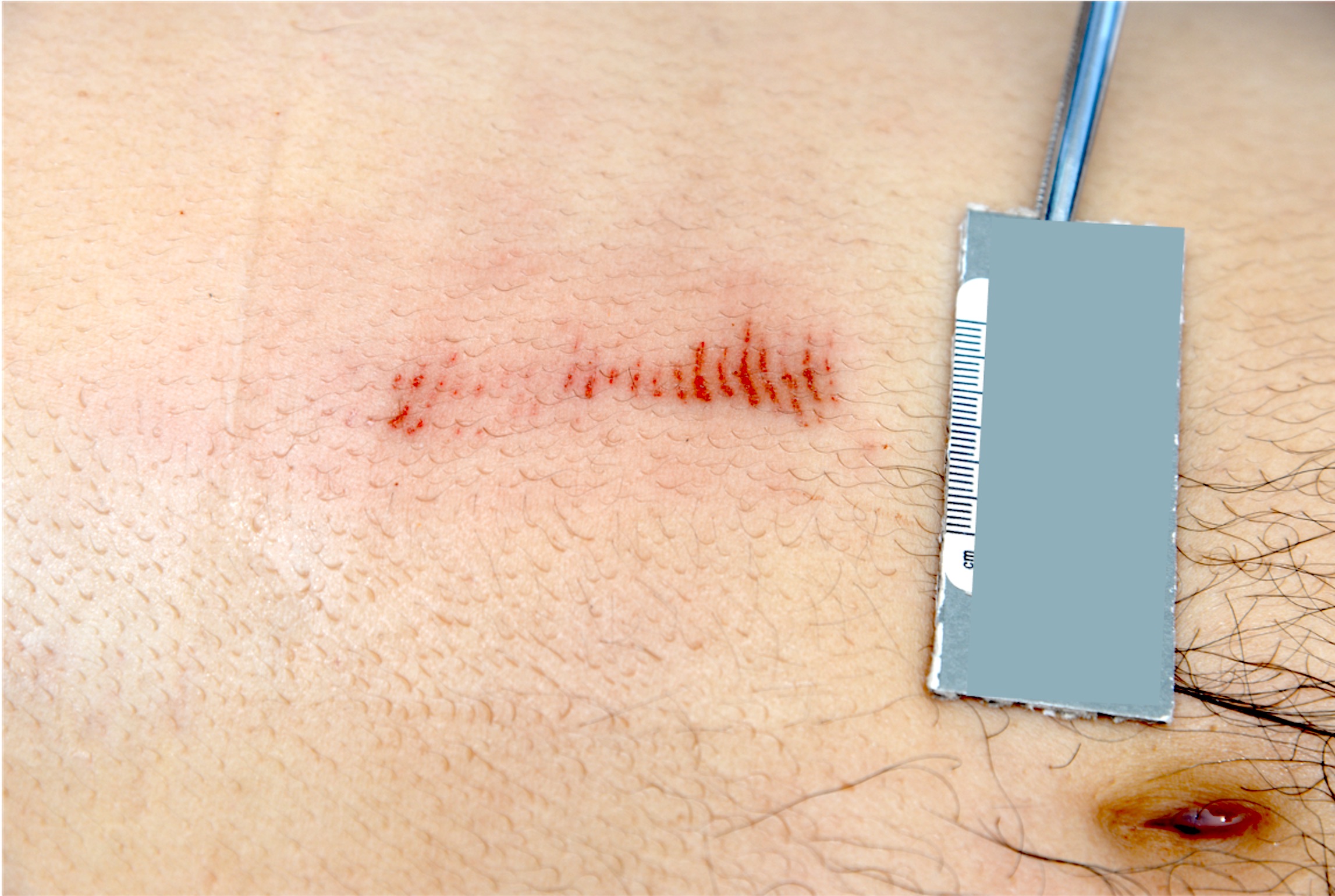
- Ligature mark: pressure abrasion that develops when there is a prolonged pressure on the skin surface, producing a dried, dark brown, parchment appearance (Egypt J Forensic Sci 2016;6:248)
- Typically is oblique and directed upwards (differential diagnosis with ligature strangulation where the mark is typically horizontal)
- Typically interrupted at the level of the knot, unless multiple loops around the neck are present
- Periligature injuries: additional injuries surrounding the primary ligature mark (J Clin Forensic Med 2003;10:255, J Forensic Leg Med 2014;22:80)
- Examples: rope burns and nail marks
- Facial congestion, cyanosis and petechiae
- Dribbling of saliva or seminal fluid
- Neck muscles hemorrhage and hyoid / larynx fractures uncommon
- Mostly seen in incomplete hanging (J Forensic Sci 2015;60:1216)
- Simon sign: hemorrhage into the anterior aspect of the intervertebral discs, usually at the level of the lumbar spine (Med Leg J 2022;90:52)
- Can be seen in other types of death (e.g., blunt force trauma)
- Amussat sign: transverse laceration of the carotid intima (J Forensic Sci 2011;56:132)
- Ligature mark: pressure abrasion that develops when there is a prolonged pressure on the skin surface, producing a dried, dark brown, parchment appearance (Egypt J Forensic Sci 2016;6:248)
- Suicide is the most common manner of death (Int J Epidemiol 2005;34:433)
- Accident is uncommon (Egypt J Forensic Sci 2016;6:310, J Clin Pathol Forensic Med 2014;5:1)
- Homicide is rare:
- Alleged suicide scene may cover homicide (Forensic Sci Int 2019 May;298:419)
- Victim is killed by other means with subsequent suspension of the body to simulate suicide (Leg Med (Tokyo) 2011;13:259)
- Alleged suicide scene may cover homicide (Forensic Sci Int 2019 May;298:419)
Manual strangulation
- Asphyxia mechanism in which the neck compression results from a pressure applied by hands, forearms or other limbs
- Independent from the victim's body weight
- May result in the compression of airway, vessels and nervous stimulation or a combination
- Some physical restraint mechanisms may result in manual strangulation injuries or death
- Choke hold: the pressure is applied to the anterior aspect of the neck, compressing the airway and blocking the air passage
- Carotid restraint: the forearm of the restrainer is flexed at the antecubital fossa over the anterior neck, compressing the carotid arteries on the lateral aspects of the neck, blocking the blood flow to the brain and causing rapid unconsciousness
- Banned by the majority of law enforcements since 1980s because it is considered unsafe (Am J Forensic Med Pathol 1982;3:253)
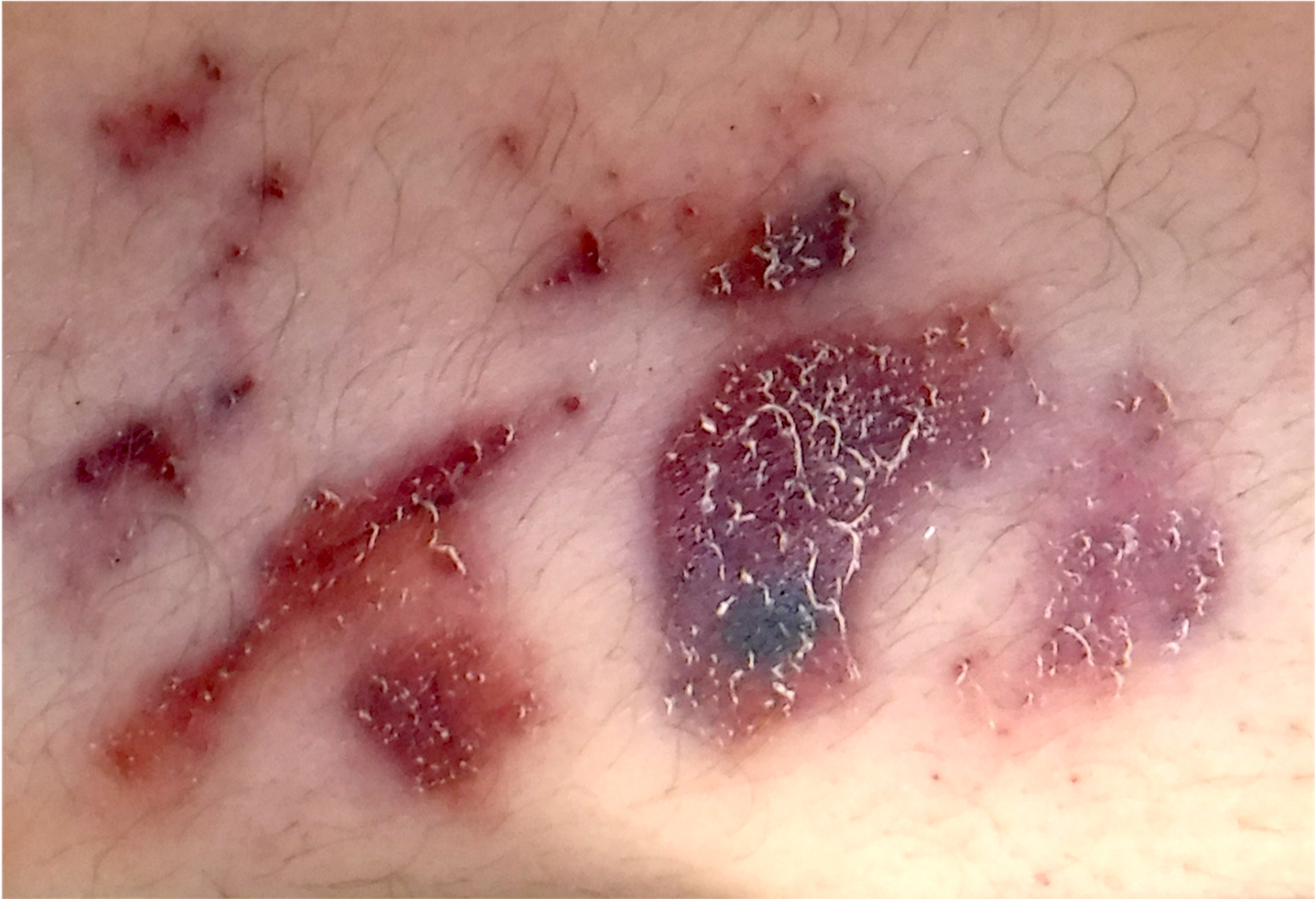
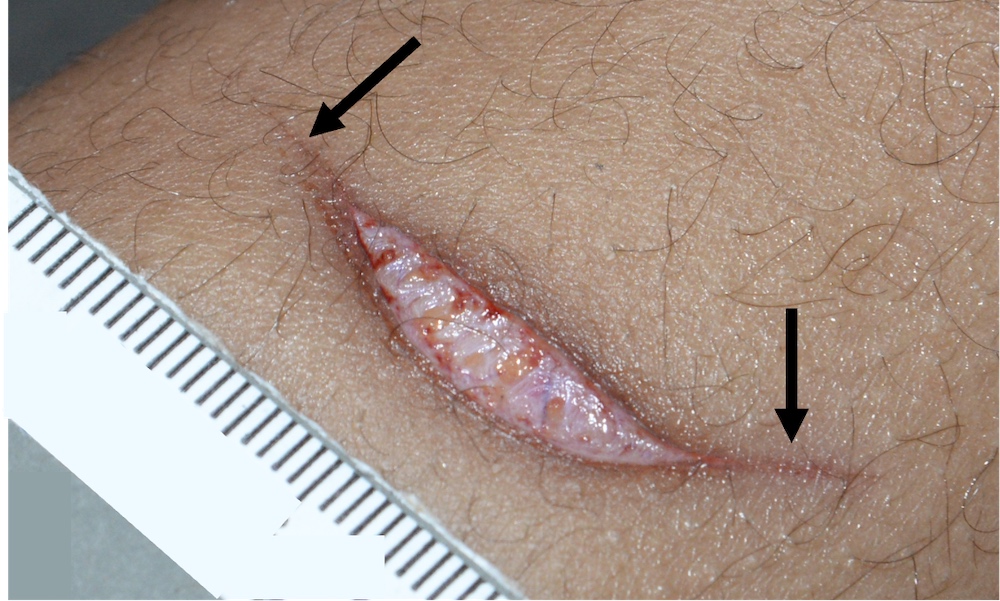
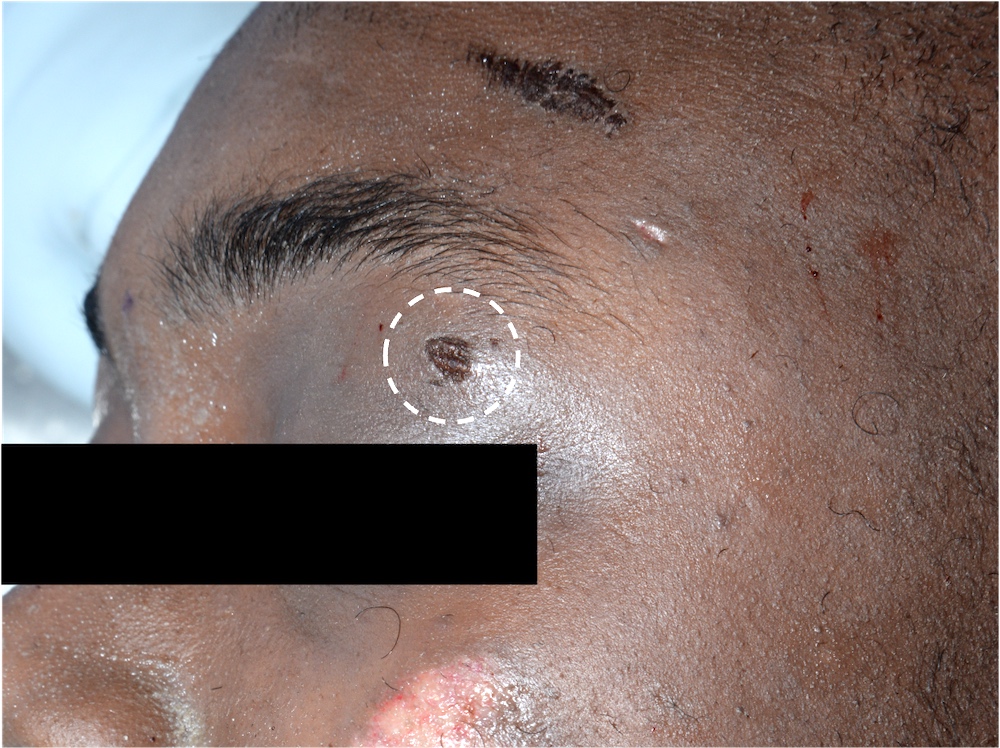
- Autopsy findings:
- Bruising due to neck compression by hands:
- Fingers: linear, parallel bruises connected to the fingerpad contusions due to the compression and sliding of the finger on the affected area
- Fingerpads: oval / round bruises of different sizes due to the compression by fingertips
- May be more prominent on one side of the neck but a single, larger, thumb-like bruise on the opposite side of the clustered fingertip contusions may also be present
- Abrasions due to fingernail scratches:
- There may be linear scratches if the fingernails are dragged down the skin or curved marks when the skin is just gripped
- Fingernail marks on the neck can also be self inflicted by victims in the attempt to extricate themselves from the offender or an intentional hanging
- Hyoid bone fractures, laryngeal cartilage fractures and neck soft tissue hemorrhages may occur
- Layer by layer neck dissection is mandatory
- Gross and microscopic examination of the carotid sinus area helps in ruling out deaths due to vagal inhibition
- Findings are not specific but the combination of subconjunctival petechial hemorrhages, hyoid - laryngeal injury and injury to the skin or soft tissues of the neck may support the diagnosis (Med Sci Law 2001;41:135)
- Bruising due to neck compression by hands:
- Delayed injuries or death may occur in survivors (Monaldi Arch Chest Dis 2009;71:132, Ann Otol Rhinol Laryngol 1989;98:824)
- Matching of hands and finger marks with neck injuries is hard and not reliable (J Forensic Sci 2006;51:381)
- Exclusively seen in homicides
- Usually results from a combination of manual and ligature neck compression
Ligature strangulation
- Asphyxia mechanisms in which the neck compression results from a pressure applied by any cord-like objects (rope, electric wires, etc.)
- Independent from the victim's body weight
- Ligature marks can be complete (full circumference of the neck) or incomplete (interrupted)
- Generally, the ligature mark is horizontal (Forensic Res Criminol Int J 2020;8:8)
- Exceptions:
- Relevant height discrepancy between offender and victim
- Victim is in recumbent posture (e.g., adult who kills a child)
- Victim is sitting and the assailant applied the ligature on the neck while standing behind
- Differential diagnosis with hanging, in which the mark is generally oblique and directed upwards
- Exceptions:
- Ligature marks may show a heterogeneous pattern due to several reasons (multiple loops around the neck, movements of the victim during strangulation, etc.)
- Autopsy findings (J Forensic Leg Med 2016;42:19):
- Ligature mark on the neck area
- Fingernail abrasions may be present
- Internal findings are the same as manual strangulation but are less frequent
- Facial congestion and cyanosis are more prominent than in manual strangulation
- Ligature strangulation mainly results in venous total occlusion rather than arterial compression
- Ligature mark on the neck area
- More common in homicides (Forensic Sci Int 2005;152:61)
- Suicides are occasionally described (Forensic Sci Med Pathol 2020;16:123, Forensic Sci Int 2020;2:100098, Am J Forensic Med Pathol 2009;30:369)
- Accidental ligature strangulation may occur, especially in children and adolescents (J Pediatr Neurosci 2011;6:164, J Clin Forensic Med 2006;13:148)
- Impaired breathing due to:
- Acquired body unnatural position (positional asphyxia)
- Severe compression to the neck or chest or other areas of the body that make the respiration difficult or impossible (traumatic or compressive asphyxia)
- Mechanical obstruction of the airways; includes smothering, choking and strangulation
Positional asphyxia
- Occurs when the victim is immobilized in a position which causes mechanical interference with pulmonary ventilation, leading to respiratory failure and death (Am J Forensic Med Pathol 2003;24:292)
- Scene investigation typically gives relevant clues to determine the cause and manner of death
- Prolonged head down position of the body interferes with respiration and blood circulation due to intra-abdominal organs compressing the diaphragm, causing increased intrathoracic pressure and compression of inferior vena cava (Forensic Sci Med Pathol 2008;4:51)
- Prolonged hyperflexion or hyperextension of the neck may result in airway obstruction (Am J Forensic Med Pathol 2011;32:31)
- Unnatural chest positions may interfere with the physiologic rib cage expansion and retraction, resulting in reduced gas exchange (Medicine (Baltimore) 2018;97:e11041)
- Hogtie position: the subject's wrists are handcuffed behind their back with ankles strapped and legs flexed back so the person is bent backwards
- Death may occur as a result of combined asphyxia, metabolic and cardiovascular changes (Med Sci Law 2021;61:215)
- Autopsy findings:
- If the positional asphyxia results from physical restraint, abrasions / bruises may be found at the level of compression
- Typically accidental (J Forensic Sci 2010;55:646)
- Homicides have been described (Rom J Leg Med 2014;22:229)
Compression asphyxia
- External pressure on the body prevents physiologic respiration
- Also called traumatic or crush asphyxia
- Usually due to external compression of chest / abdomen by heavy weight (Am J Forensic Med Pathol 2014;35:80)
- Commonly observed in soft drink vending machine tipping, motor vehicle accidents, cave related accidents and mass disasters (earthquake, collapsed buildings) (Lancet 2012;379:748)
- Primary mechanism of death is flail chest
- Adult male requires 2550 ± 250 N of chest applied distributed static force (260 ± 26 kg with earth gravity) or 4050 ± 320 N of dynamic force to cause flail chest from short term chest compression (Med Sci Law 2017;57:61)
- Frequently observed in children:
- Overlaying asphyxia: when a heavy sleeping adult may move on top of the infant, causing compression asphyxia (Am J Forensic Med Pathol 2001;22:155)
- Wedging: when the body is compressed between 2 firm surfaces, preventing breathing (Pediatrics 2019;143:e20183408)
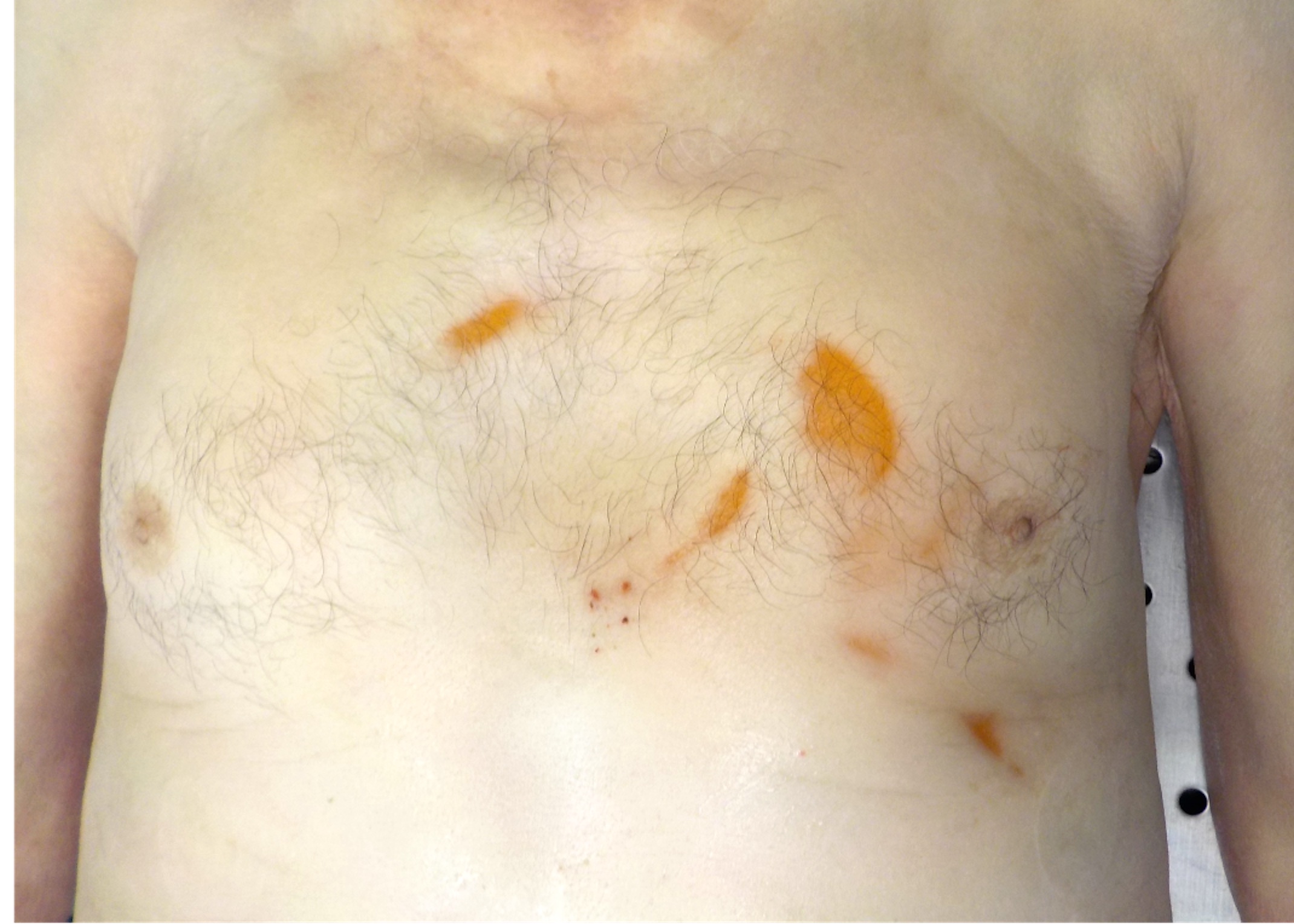
- Autopsy findings:
- Related to the thoracoabdominal compression, which results in venous hypertension in the valveless cervicofacial venous system (Int J Emerg Med 2010;3:379)
- Facial and conjunctiva severe congestion and cyanosis
- Conjunctival hemorrhage
- Facial and upper chest petechiae
- Heavy and dark red lungs with or without subpleural petechiae
- Hemorrhage in the soft tissues may be present
- Related to the thoracoabdominal compression, which results in venous hypertension in the valveless cervicofacial venous system (Int J Emerg Med 2010;3:379)
- Compression asphyxia is uncommon but accident is the most common manner of death
- Asphyxia due to partial or complete submersion of the body in a liquid, resulting in liquid inhalation, impairment of pulmonary exchanges and oxygen deprivation
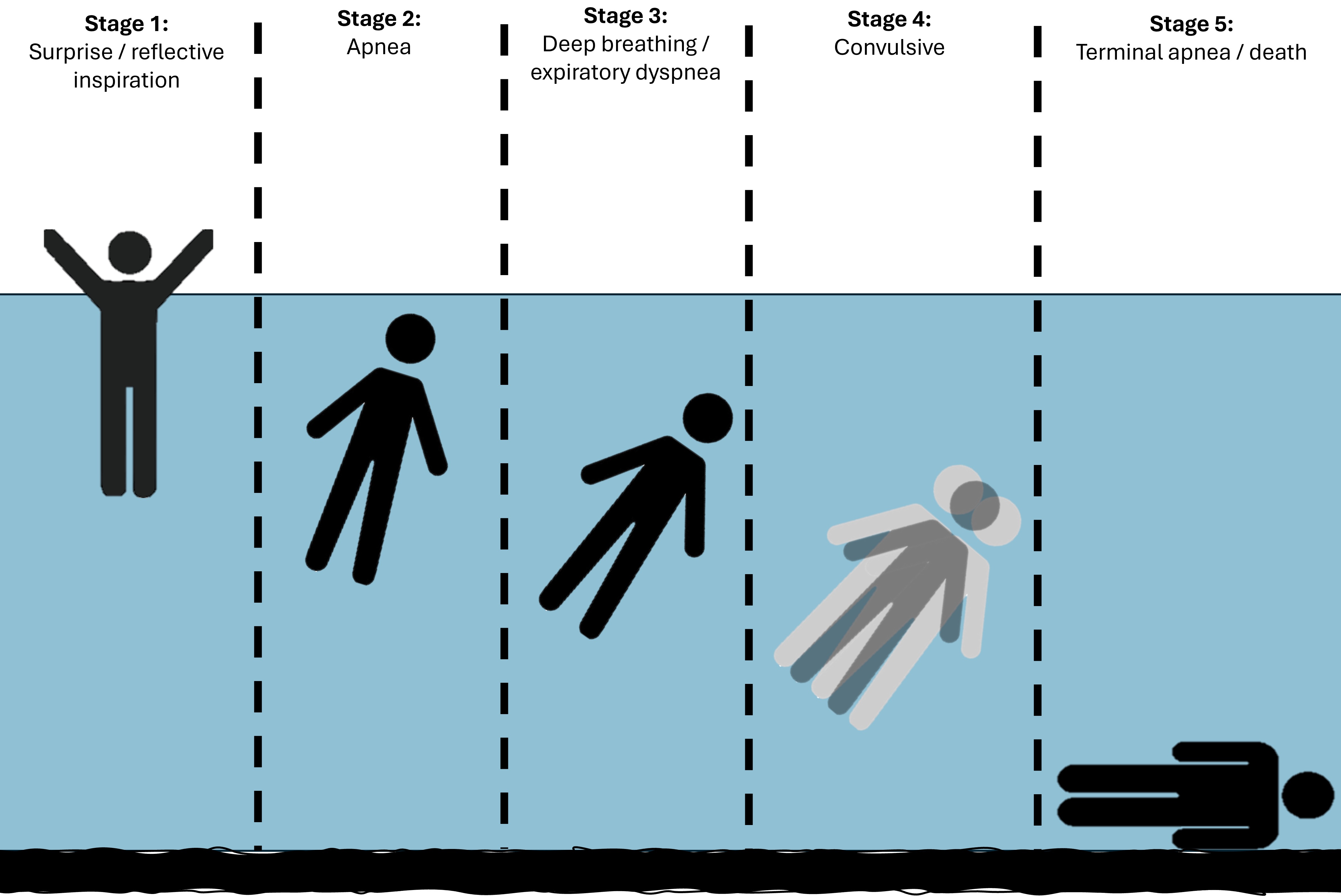
Stages of drowning (Int J Legal Med 2021;135:281)
- Stage 1: surprise / reflective inspiration
- Victim recognizes the risk and takes a deep breath to fill the lungs with as much air as possible
- Usually lasts a few seconds
- Stage 2: apnea
- Victim holds their breath in the attempt to not allow water to enter the airways
- Usually lasts less than 1 minute
- Stage 3: deep breathing / expiratory dyspnea
- Increasing hypoxia and hypercapnia, due to the apnea phase, leads to stimulation of the respiratory centers with expiratory dyspnea and rapid swallowing that allows water to enter the airway and GI tract
- Stage 4: convulsive
- Due to lack of oxygen, brain anoxia results in bradycardia, arrhythmias and convulsions
- Stage 5: terminal apnea / death
- Both breathing and circulation stop
Freshwater versus saltwater drowning
- Any difference in severity of fresh versus salt water drowning is unproven
- Freshwater drowning: hypotonic fresh water diffuses across the alveolar capillary membrane into the pulmonary microcirculation and then throughout the body, causing dilution of electrolytes and hemolysis (Pediatr Clin North Am 2001;48:627)
- Saltwater drowning: water dilutes alveolar surfactant; circulating plasma is drawn via osmosis into alveoli, resulting in hemoconcentration and increased blood electrolyte levels (Exp Ther Med 2017;13:2591)
Near drowning
- Survival after asphyxia due to submersion (Emerg Med (Fremantle) 2002;14:377)
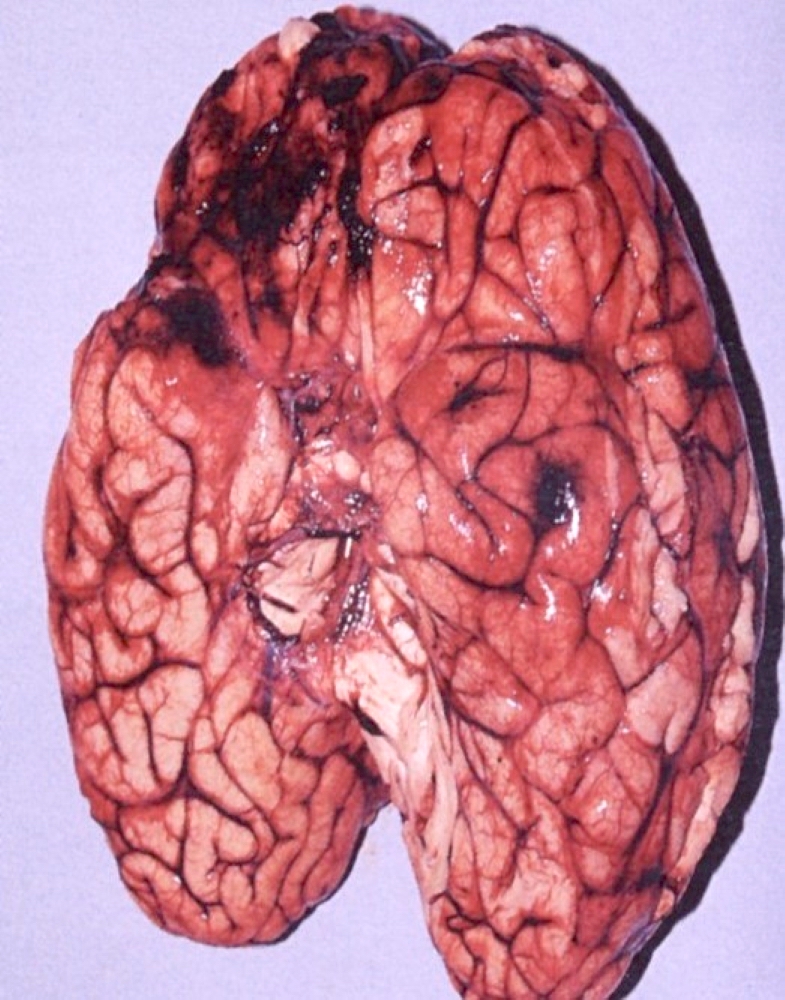
- Complications: pneumonia, pulmonary edema, hemoglobinuria, cardiac arrhythmia, fever, sepsis and sequelae of cerebral hypoxia; rapidly developing cerebral edema is a common mechanism of death (Int J Environ Res Public Health 2017;14:1402)
Cold shock
- Sudden skin cooling may result in a cold shock response characterized by peripheral vasoconstriction, hypertension, inspiratory gasp and hyperventilation with swimming inability and liquid aspiration (Int J Environ Res Public Health 2020;17:8984)
- Acute anxiety is an important risk factor for cold shock response (Front Psychol 2018;9:510)
Cold water immersion
- Complications arise based on the body temperature (Physiology (Bethesda) 2016;31:147):
- Body temperature below 35 °C leads to confusion, disorientation and decreased muscle coordination
- Body temperature below 33 °C leads to hypoventilation, bradycardia and irregular breathing
- Body temperature below 30 °C leads to stupor or unconsciousness and coma
- Body temperature below 28 °C leads to ventricular fibrillation
- Body temperature below 25 °C leads to cardiac arrest and death
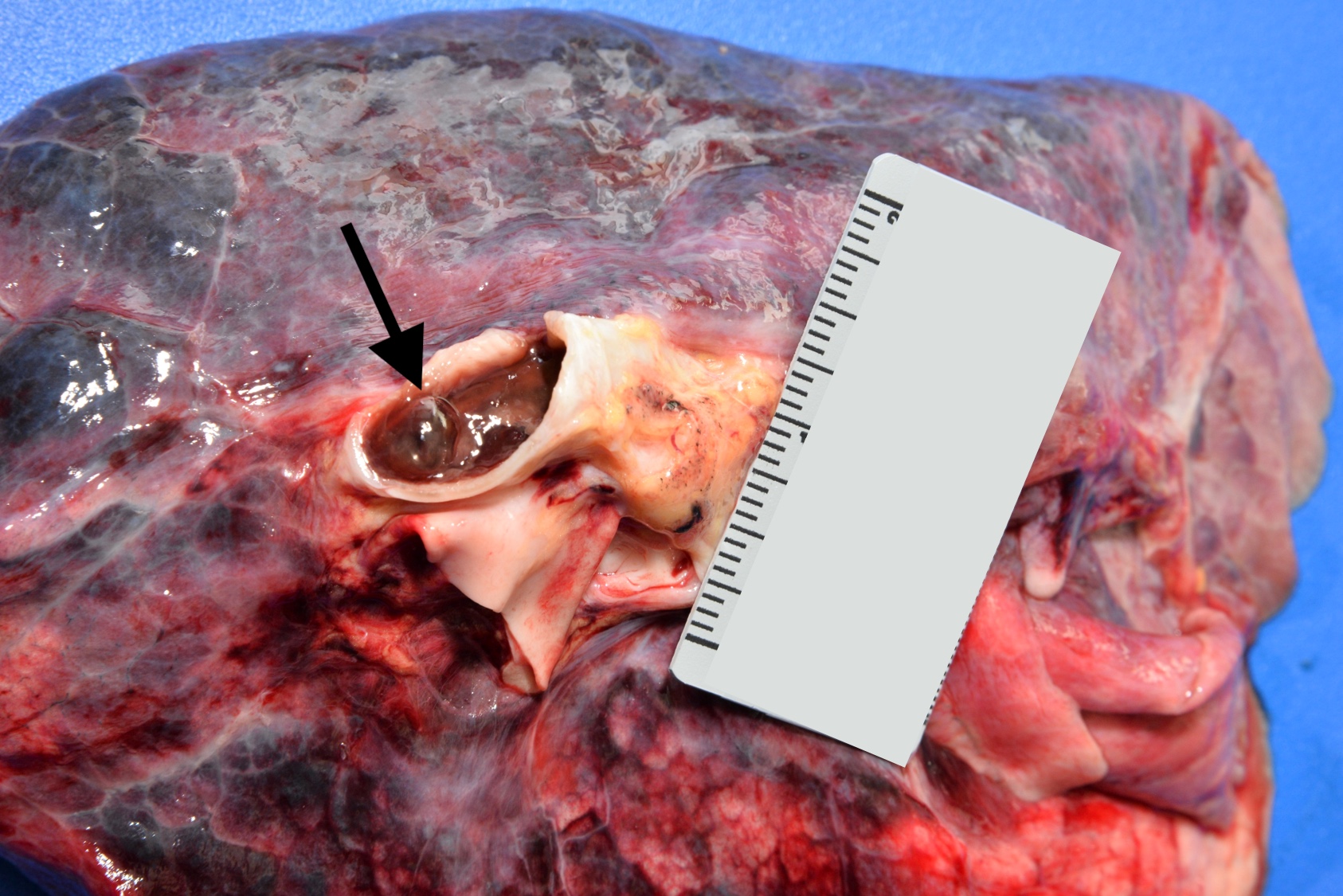
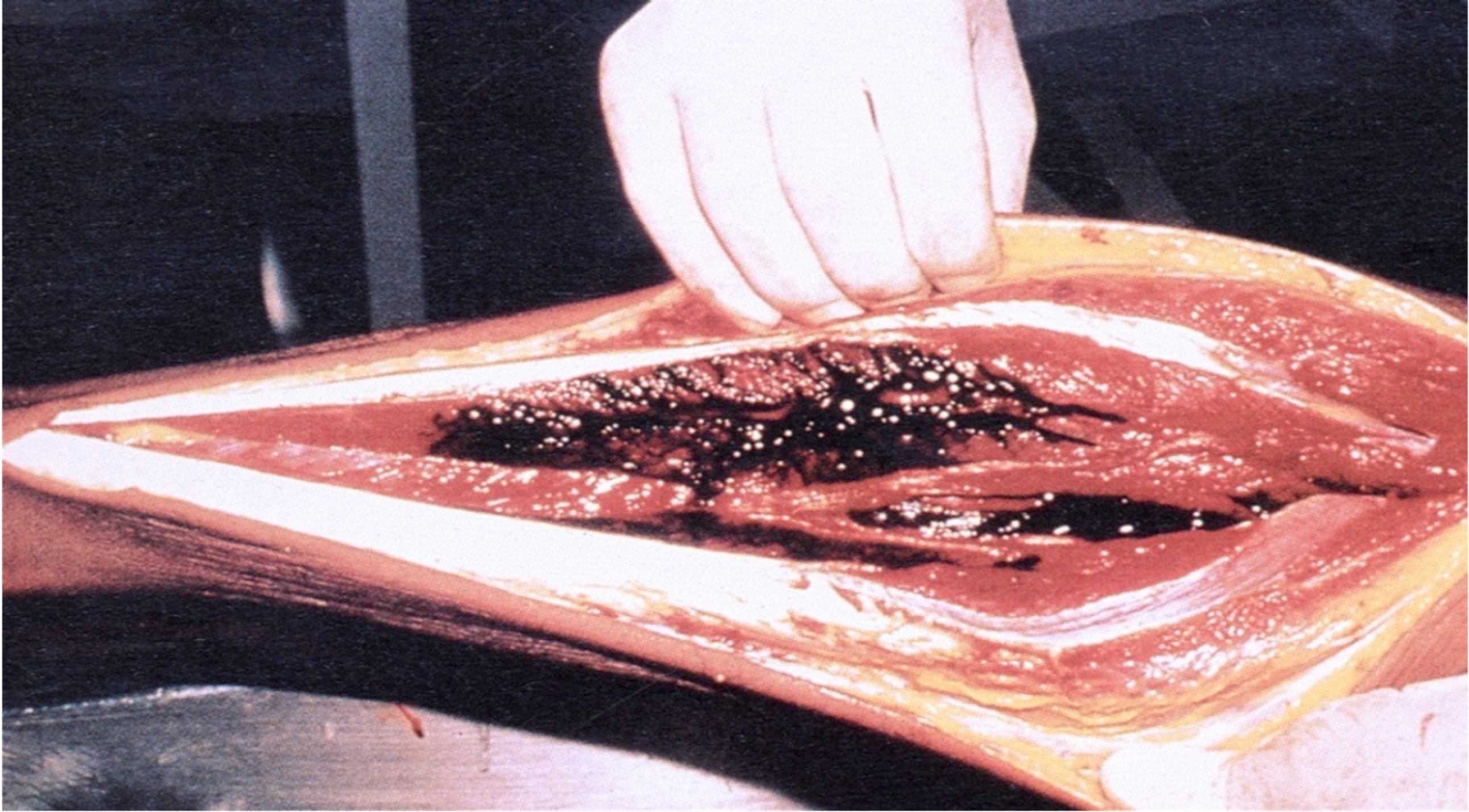
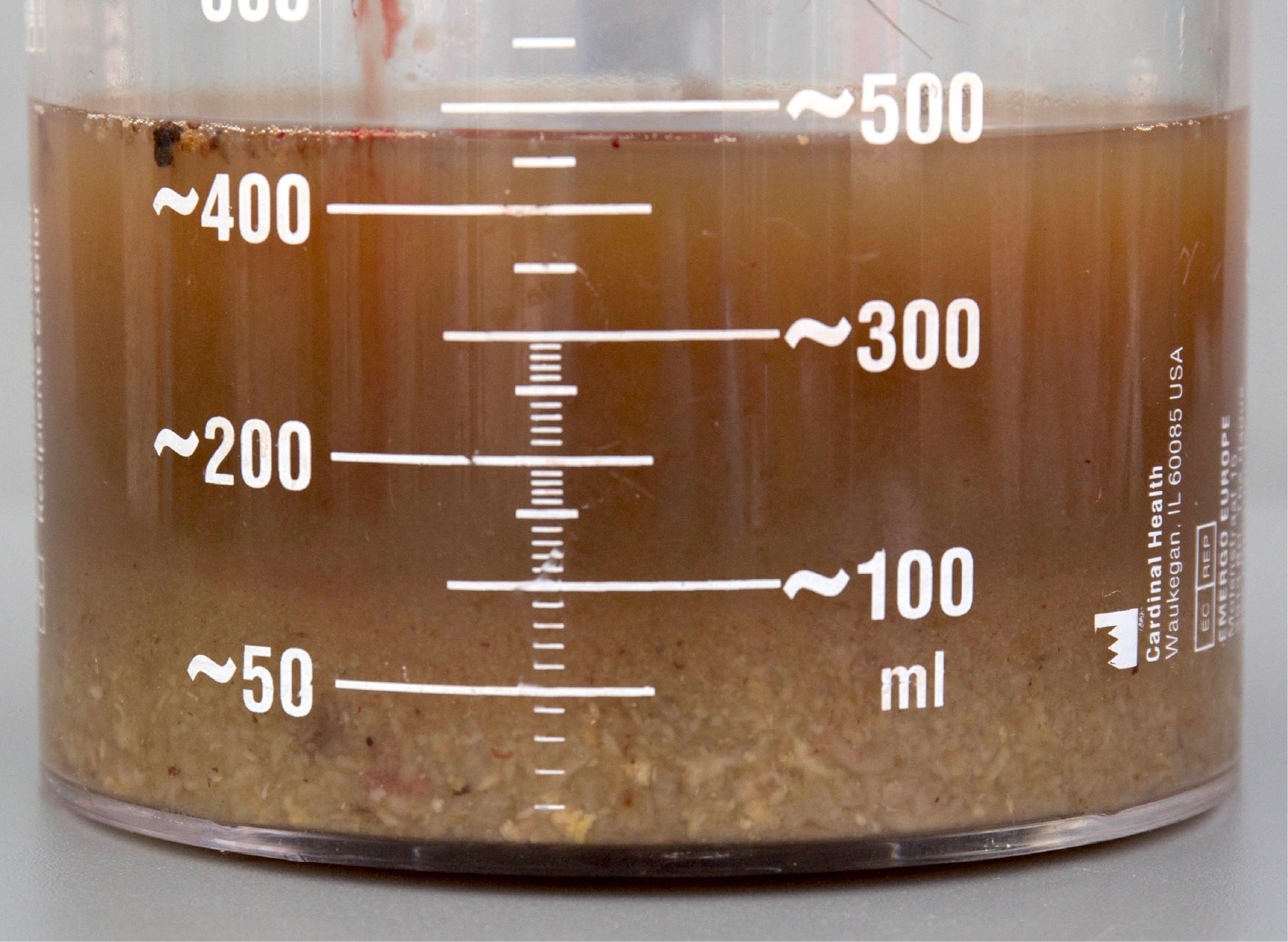
- Autopsy findings (Acad Forensic Pathol 2018;8:8):
- Drowning is a diagnosis of exclusion, based on ruling out all other causes of death via complete autopsy and toxicology
- May see bloody froth in the airway, water in the stomach, cerebral edema, petrous or mastoid hemorrhage
- Lung overinflation (emphysema aquosum) (Int J Legal Med 2021;135:281)
- Wrinkling of the skin, particularly involving the hands and feet (formerly called washerwoman changes) that develops when submerged in water for several hours; occurs regardless of whether the person died in the water (Acad Forensic Pathol 2016;6:19)
- Postmortem lacerations / abrasions due to scraping along rough surfaces in the water or animal activity should not be confused with antemortem trauma (J Forensic Leg Med 2019;66:79)
- Accident is common (Inj Prev 2015;21:e43):
- Psychotropic drugs and alcohol may contribute to fatal unintentional drownings (BMC Public Health 2017;17:388)
- Suicides have been reported (PLoS One 2020;15:e0231861)
- Homicides are uncommon (Forensic Sci Med Pathol 2019;15:233):
- Mostly involve children rather than adults
- Victim may be incapacitated by alcohol or drugs
- Undetermined is still one of the most common manners of death (Med Sci Law 2003;43:207)
- Unconfirmed tests for drowning:
- Diatoms (Int J Legal Med 2020;134:1037):
- Diatoms are microscopic algae present in bodies of water; theoretically should never be present in a human unless they inhaled water
- Best specimen for diatoms analysis is the bone marrow
- Validity questionable because diatoms are present in soil and atmosphere, and samples are easily contaminated
- Absence of diatoms does not rule out drowning
- Postmortem electrolytes:
- In saltwater drowning, Na and Cl concentrations in right and left heart blood should be widely different (Anesthesiology 1969;30:414)
- Invalid if individual survived for a period of time or had significant CPR
- Pleural effusion electrolyte analysis may be useful to distinguish between fresh and seawater drownings (J Forensic Leg Med 2009;16:321)
- Sphenoid sinus fluid (Forensic Sci Med Pathol 2013;9:177):
- Significant fluid in sphenoid sinuses (several milliliters) is suggestive of water aspiration; not a validated test
- Aortic intimal staining (Forensic Sci Med Pathol 2015;11:442):
- Arises from lysed erythrocytes staining the aorta, induced by hypotonic fluid entering the lungs during immersion
- Drowning index (Leg Med (Tokyo) 2010;12:68):
- Ratio of lung to spleen weight
- Drowning index of 14.1 is considered the cutoff point to diagnose actual drowning cases
- Limited to a postmortem interval of 2 weeks
- Diatoms (Int J Legal Med 2020;134:1037):
- Accidental deaths that occur during solitary sexual activity in which some type of apparatus is used to enhance sexual stimulation (Am J Forensic Med Pathol 2005;26:45)
- Not all autoerotic deaths are due to asphyxia
- To diagnose an autoerotic asphyxia, the following criteria must be satisfied:
- An asphyxia mechanism must be present
- By definition, the deaths must be accidental
- Pure autoerotic deaths require the victim to be alone (solitary: autoerotic comes from the Greek root auto, which means self or by itself)
- Escape mechanisms must be present but they do not necessarily need to be seen on the scene
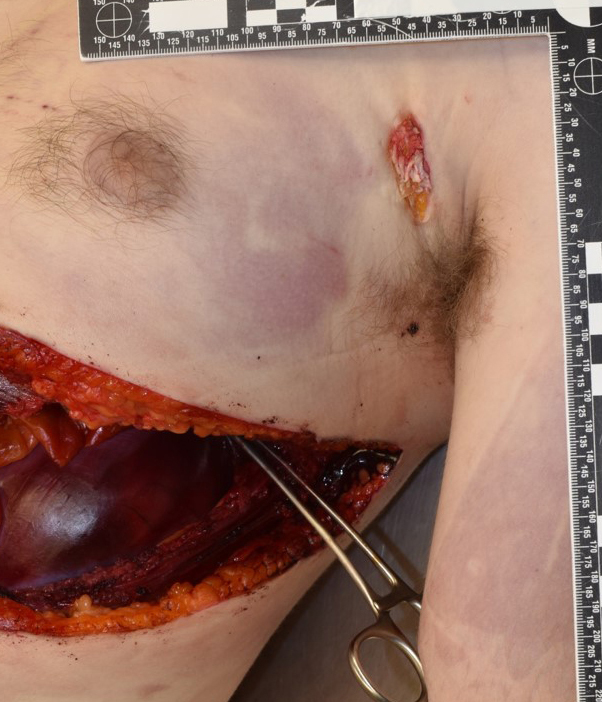
Incaprettamento
- Homicidal strangulation typical of the Italian Mafia in which the victim is obligated in a modified hogtie position with the wrists and ankles tethered together behind the victim's back, the body in the prone position and an additional ligature is encircling the neck and attached to the bindings of the extremities (Am J Forensic Med Pathol 2003;24:51)
Judicial hanging
- Modality of public execution for capital crimes (see Hanging)
Mass suicides by hanging
- Several people commit suicide together led by a charismatic leader with strong religious beliefs or loyalties (Indian J Psychol Med 2018;40:108)
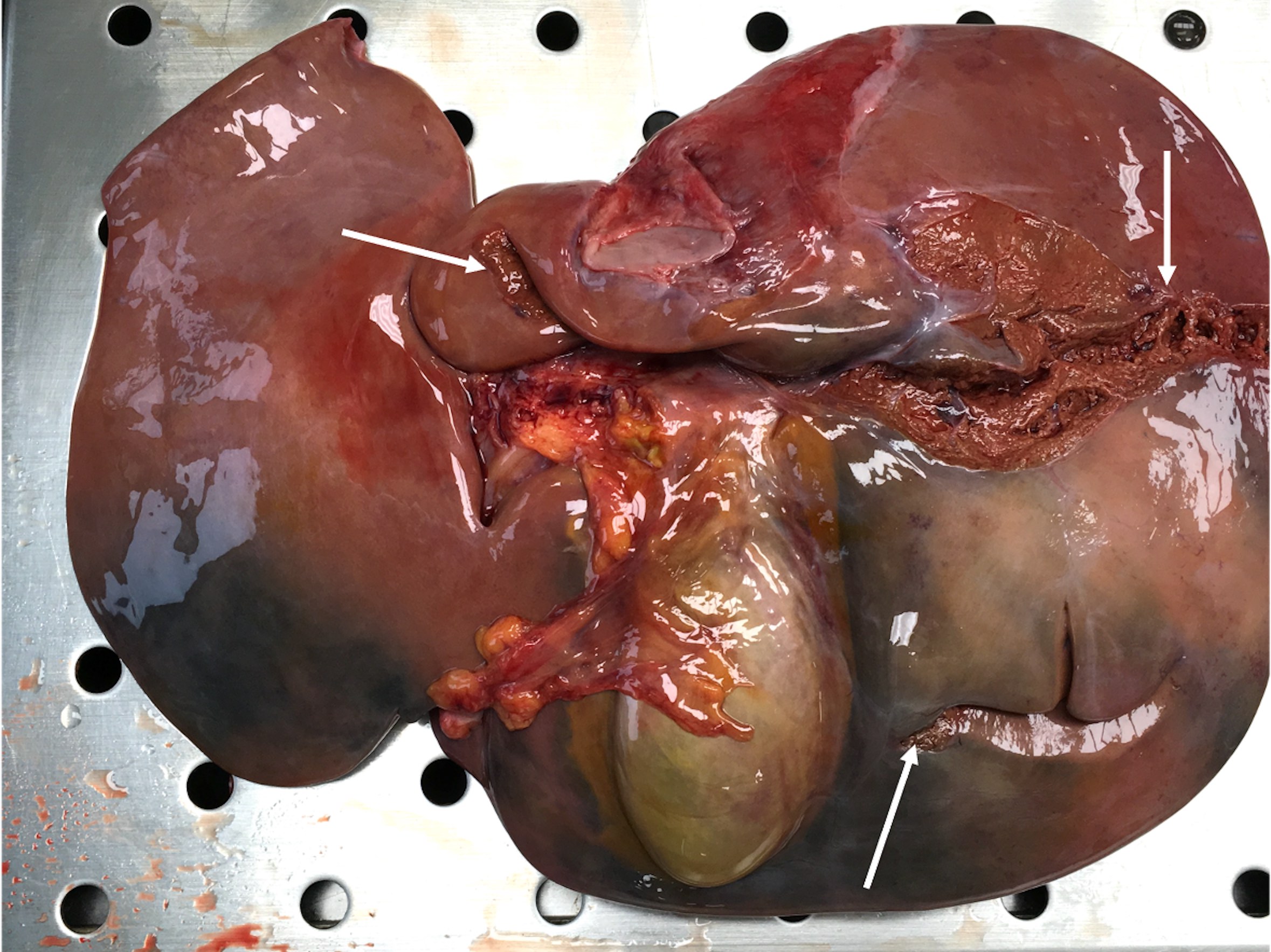
- 2 year old girl died of pacifier aspiration (Forensic Sci Int 2004;141:73)
- 46 year old man trapped between the rims of an automatically closing door of a supermarket (Arch Med Sadowej Kryminol 2006;56:61)
- 48 year old man found dead with a ligature around neck and another around the feet (J Forensic Leg Med 2012;19:434)
- 55 year old man who died from fatal asphyxia caused by a thyroglossal cyst (J Clin Forensic Med 2006;13:349)
- 74 year old man killed by a combination of ligature strangulation, traumatic asphyxia and smothering by plastic bag (Int J Appl Basic Med Res 2015;5:61)
- 75 year old man with poor dentition suddenly collapsed while drinking water (Med Leg J 2021;89:264)
Contributed by Lorenzo Gitto, M.D., Ponni Arunkumar, M.D. and the Cook County Medical Examiner's Office
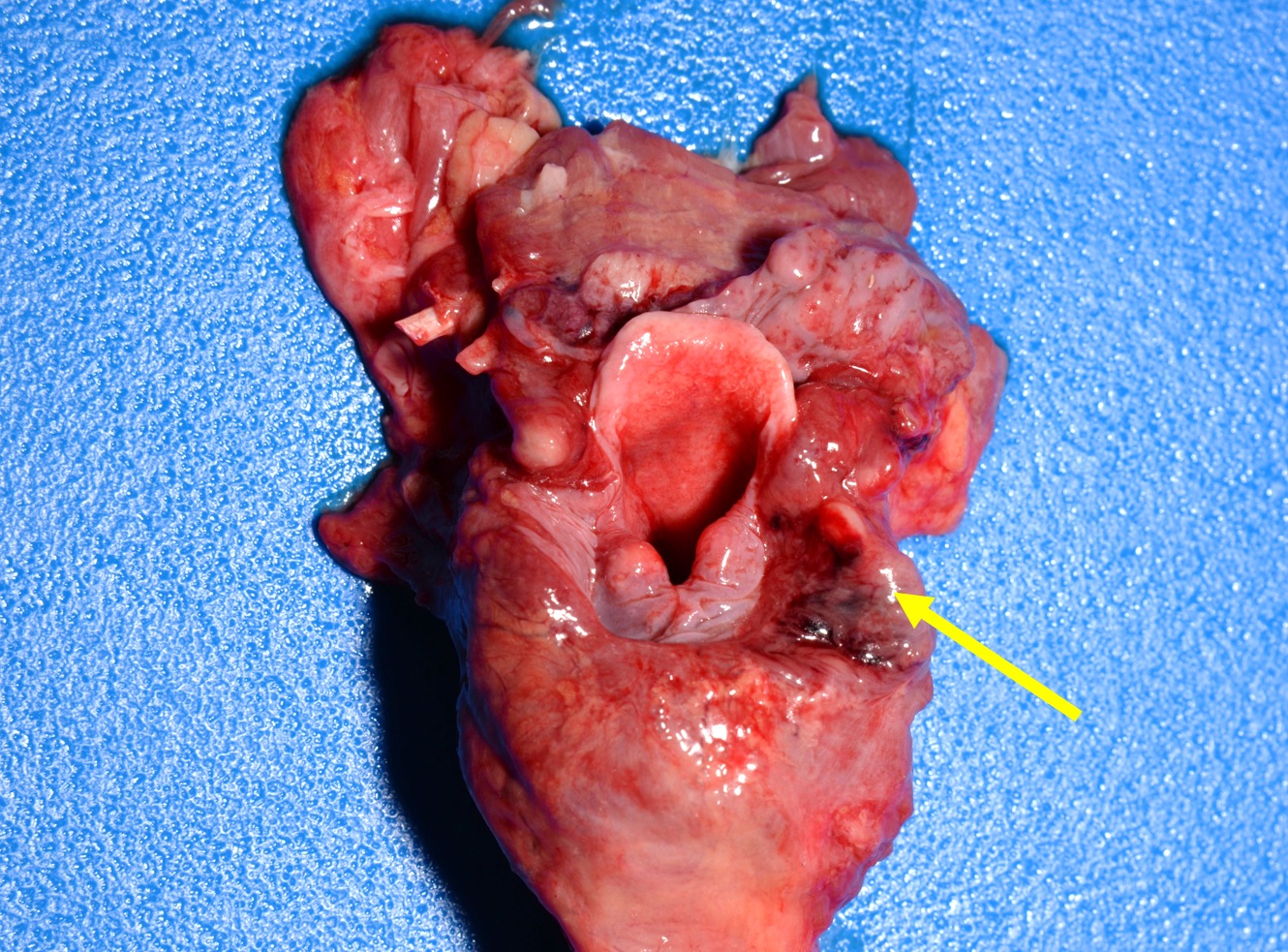
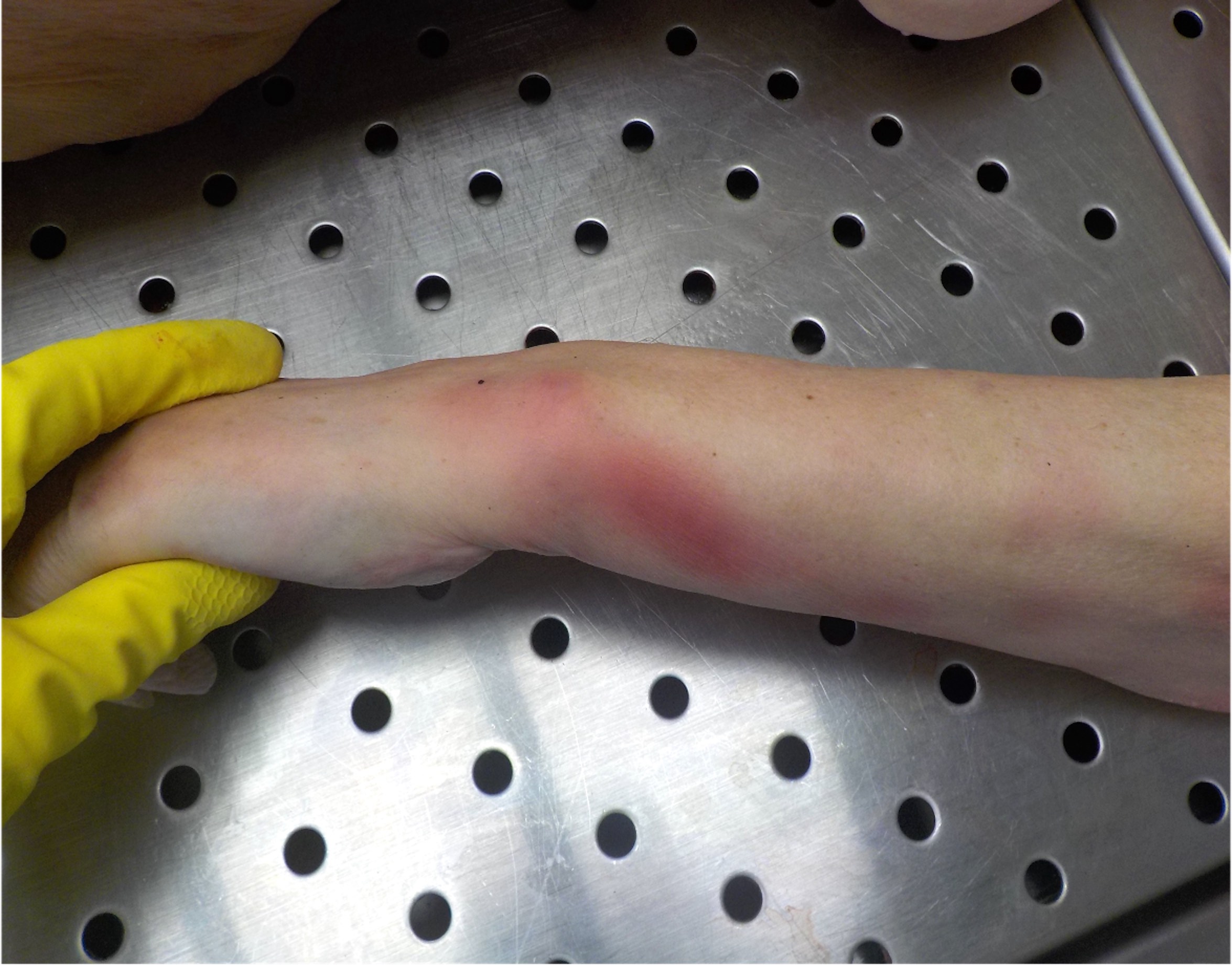
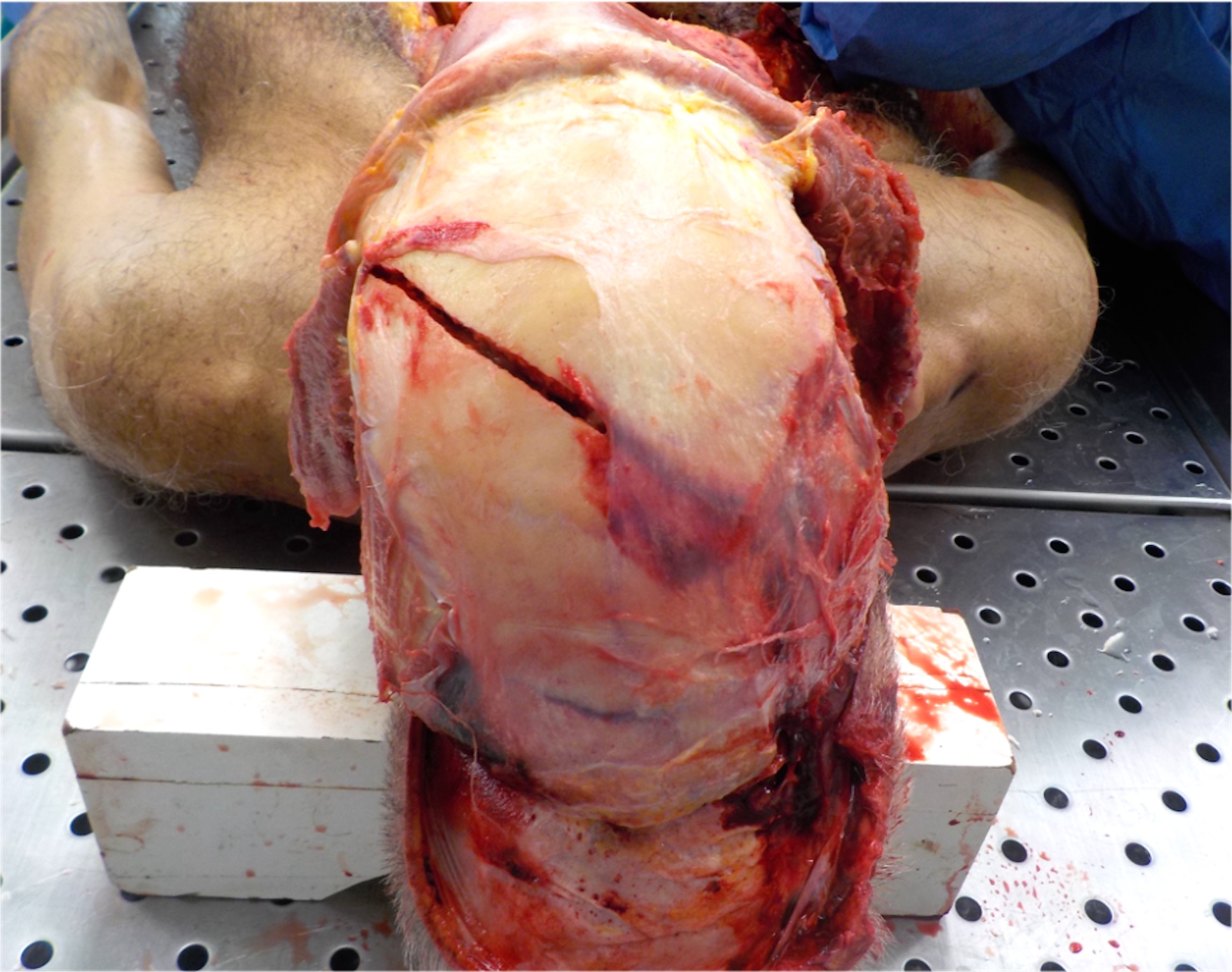
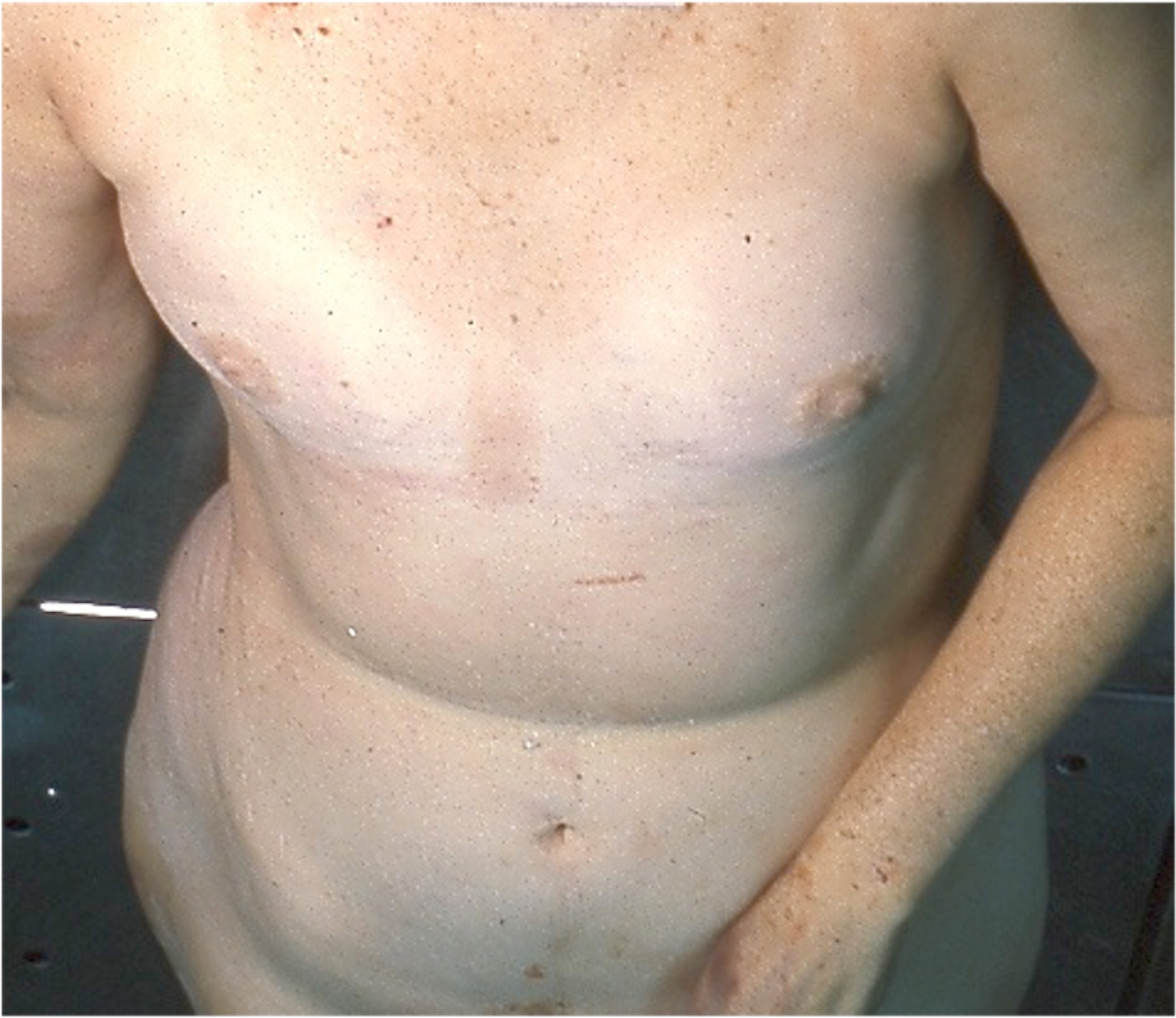
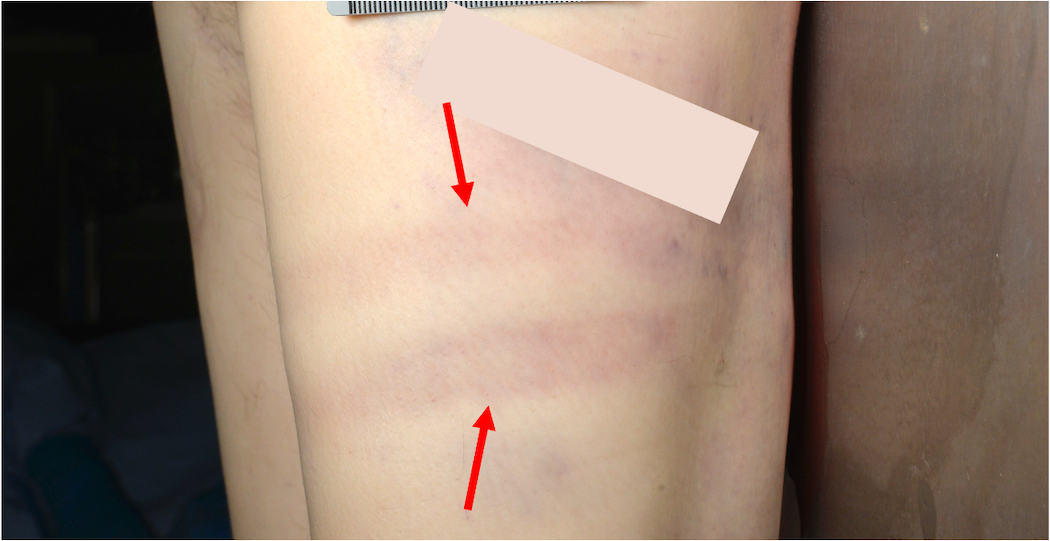
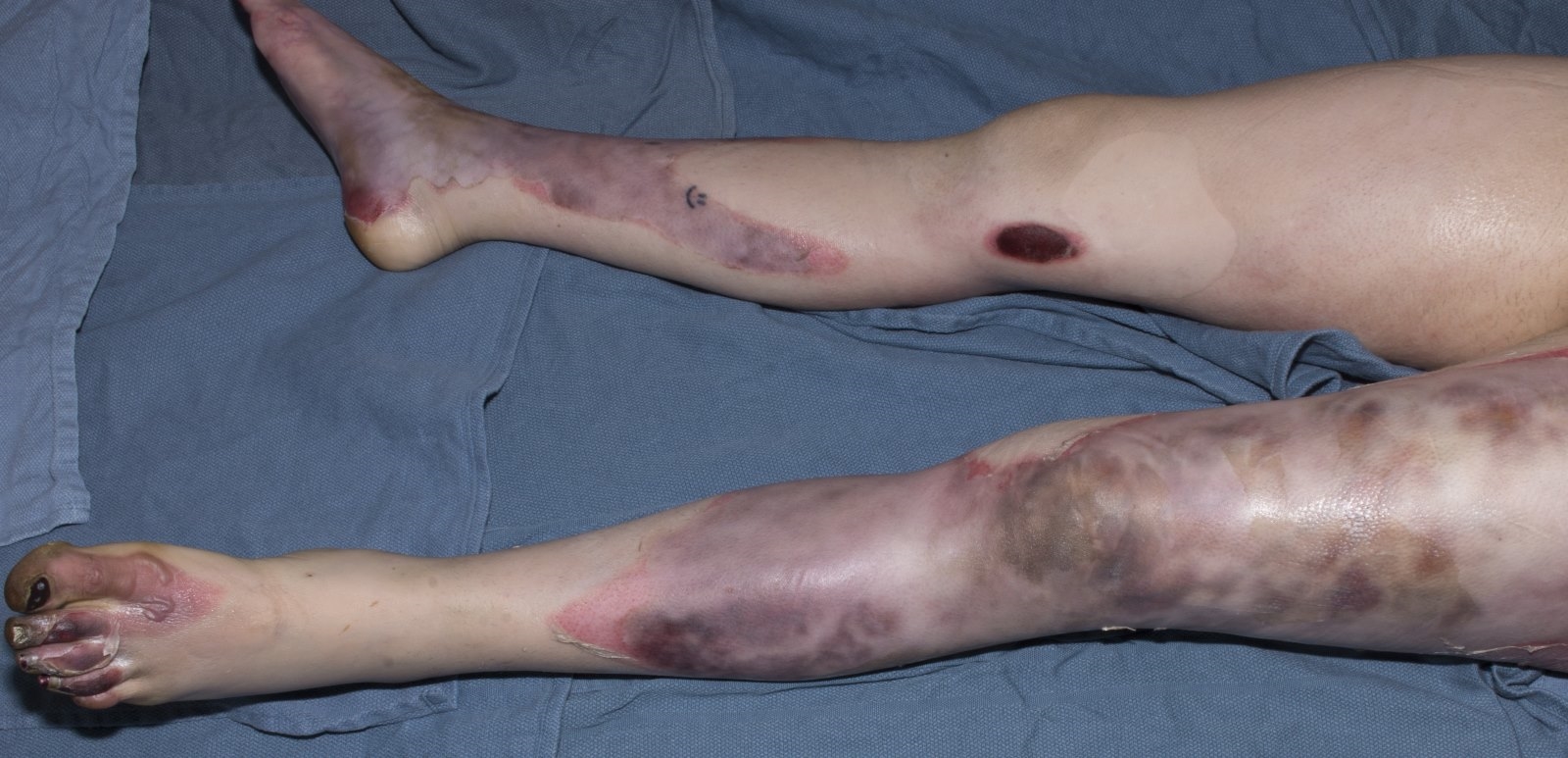
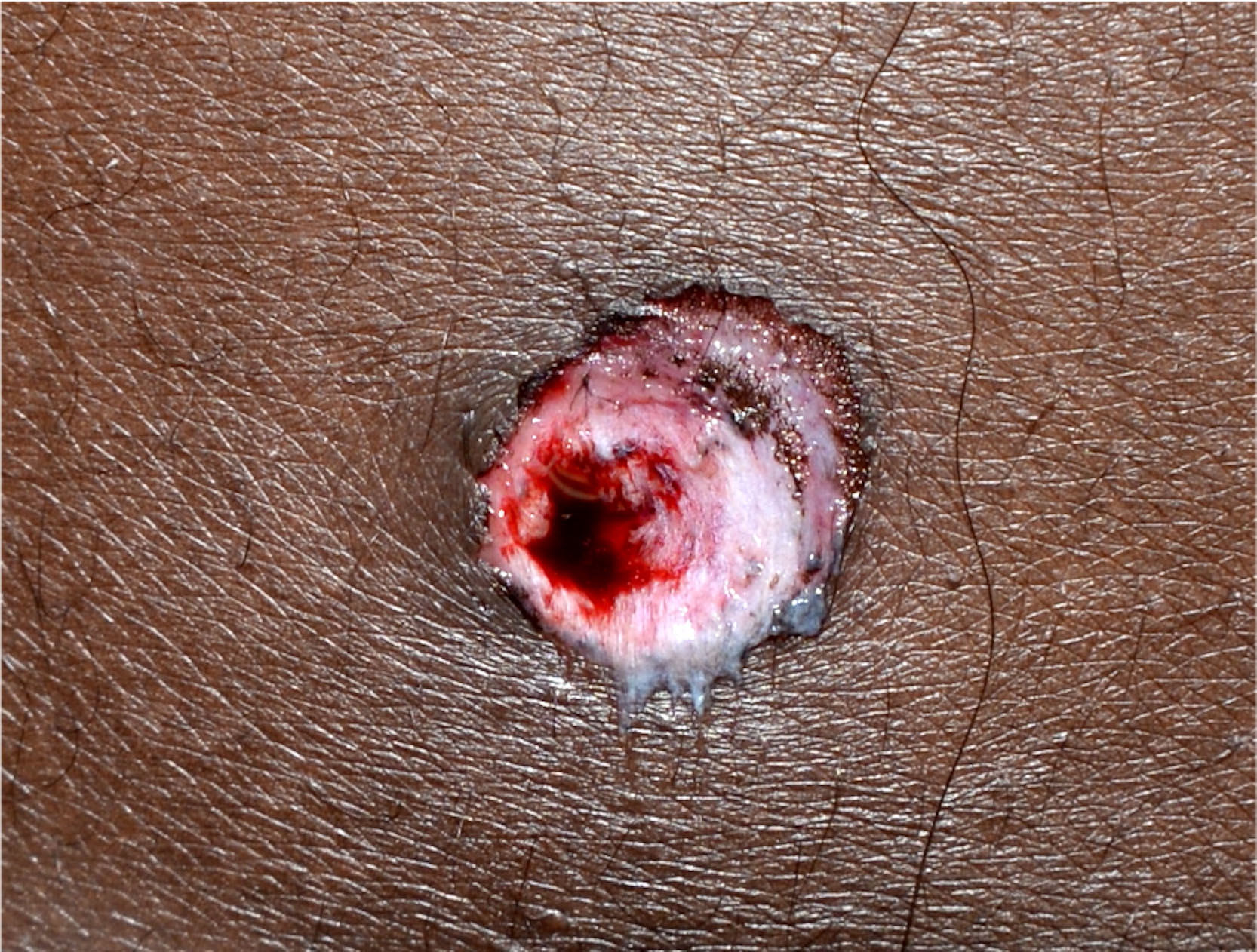
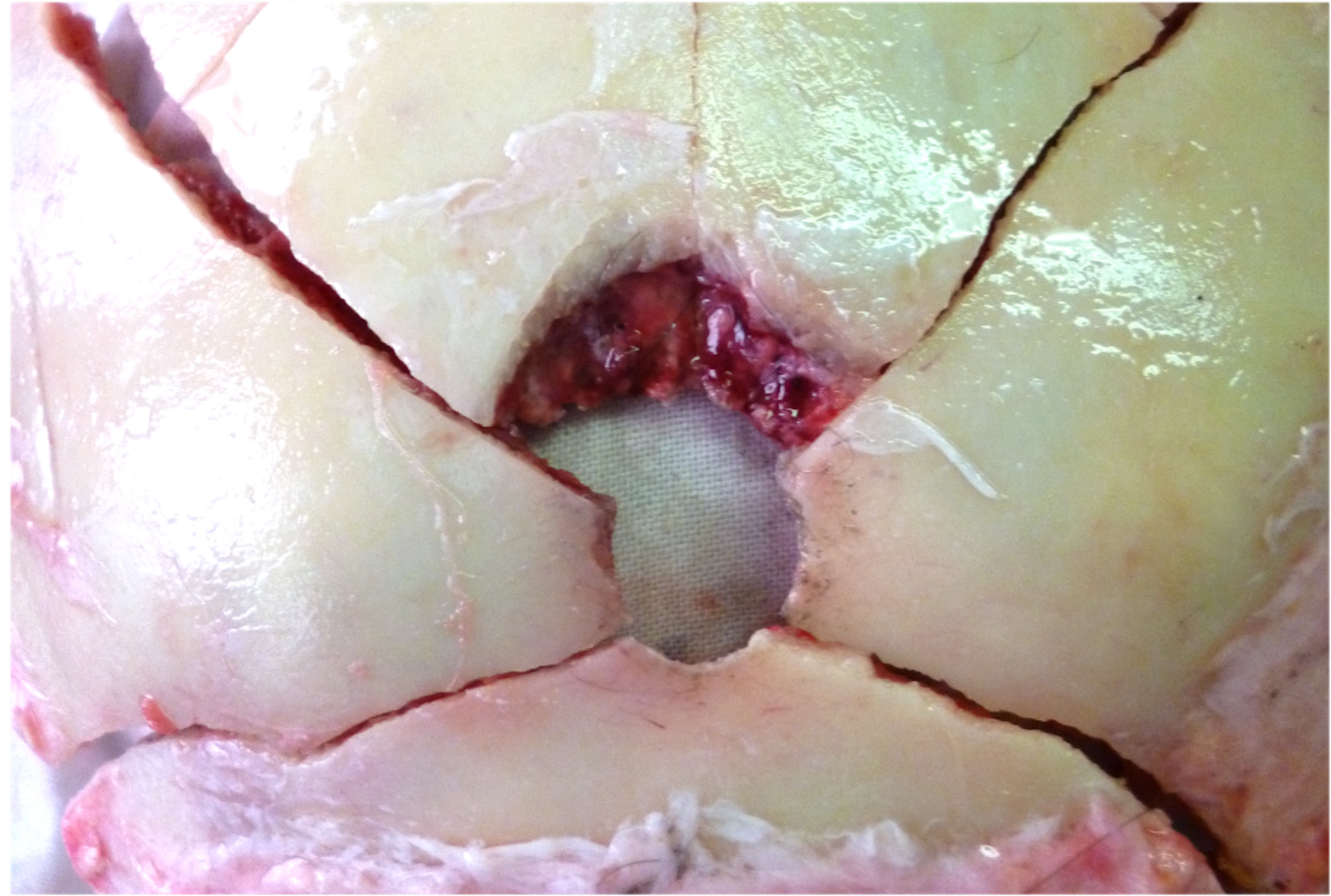
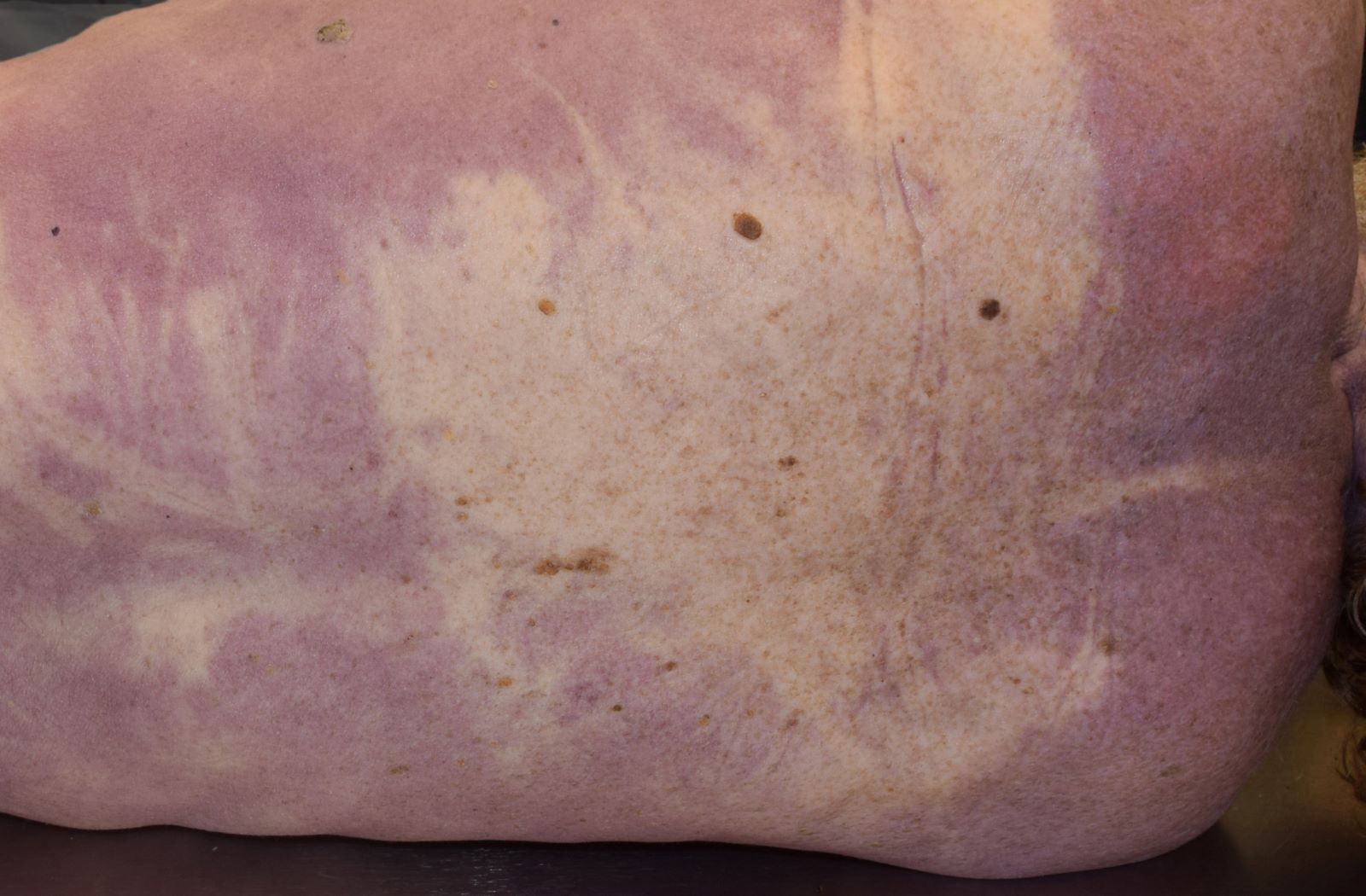
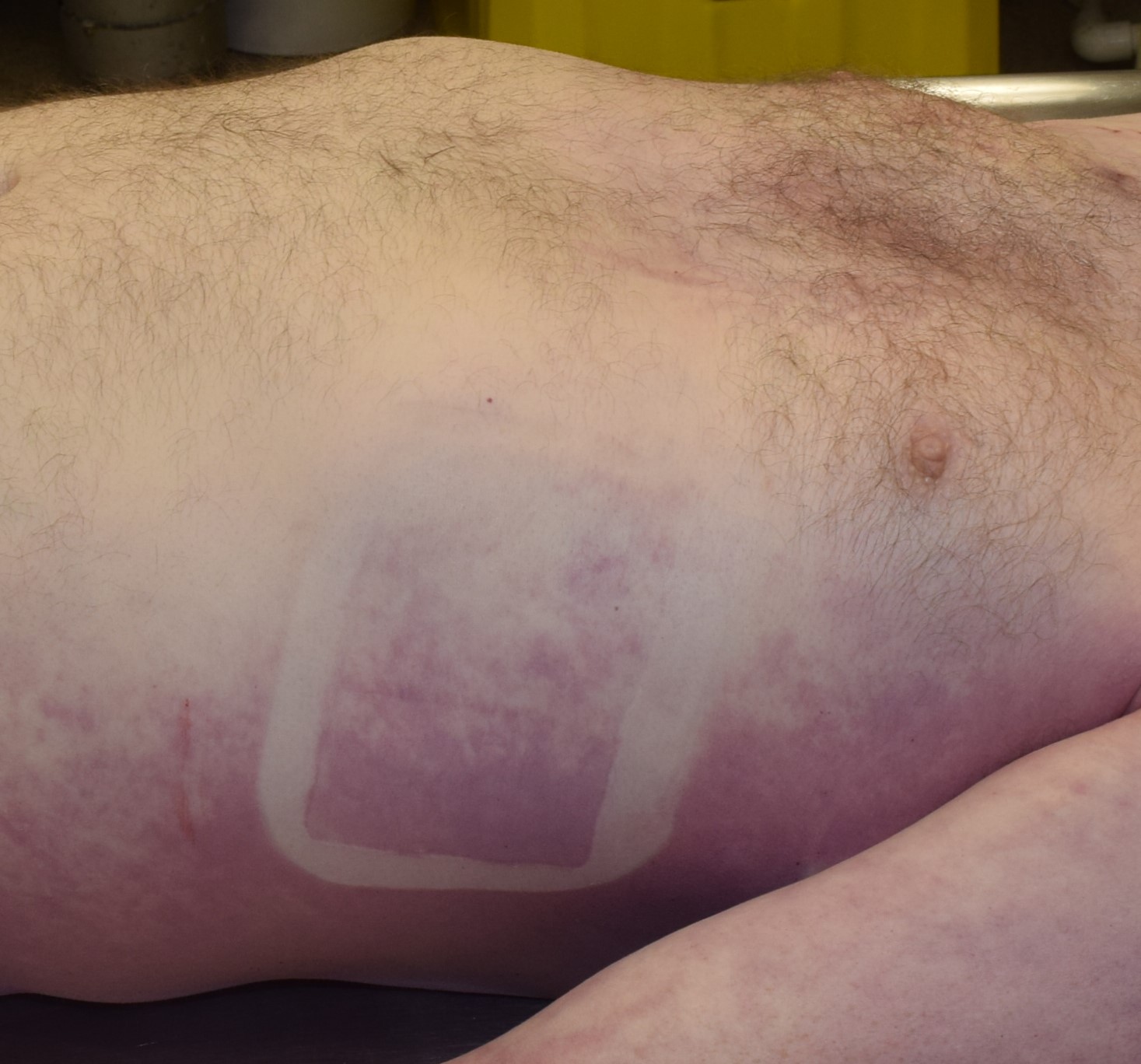
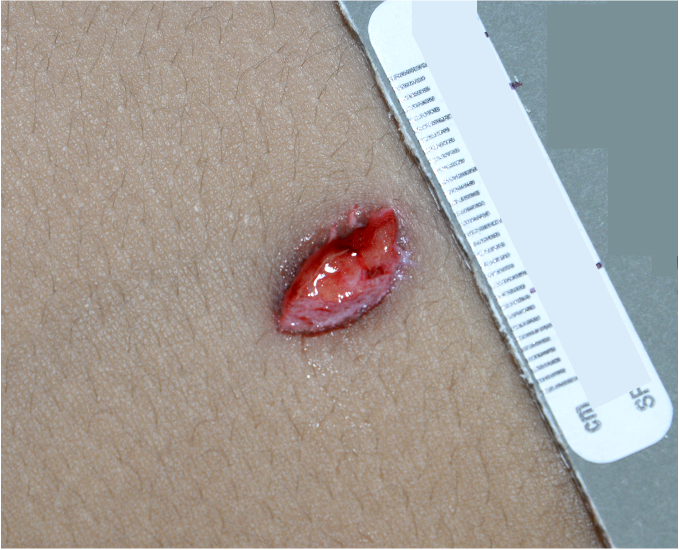
A 27 year old woman is found dead on a riverbank. The body is fully dressed and the clothes are soaked and soiled. Investigations did not reveal evidence of foul play. The external examination findings are shown in the image and an irregular 1.4 x 1.3 cm laceration of the left frontal areas without hemorrhage of the soft tissues. Autopsy is negative except for a 30% obstruction of the left descending coronary artery. Toxicology analysis shows a blood ethanol concentration consistent with alcohol intoxication. What additional findings would support the suspected cause of death?
- Lung hyperinflation and water in the sphenoid sinus
- Multiple skin injuries on the anterior and lateral aspects of the neck
- Round bruises on the anterior aspect of the thighs
- Presence of a horizontal abrasion mark on the neck
- Conjunctival petechiae
Multiple skin injuries on the anterior and lateral aspects of the neck (answer B) may suggest manual strangulation. In this case, the external examination showed only a laceration on the left frontal area, consistent with the body scraping along rough surfaces in the water or animal activity. Round bruises on the anterior aspect of the thighs (answer C) may suggest sexual assault; there was no investigative evidence of assault in this case and the foam from the airways would be an uncommon finding. A horizontal abrasion mark on the neck (answer D) may suggest homicidal strangulation. Facial congestion, cyanosis and petechiae and neck skin injuries are generally present, while foam from the airways would be an uncommon finding. Petechiae (answer E) is a nonspecific finding that can be virtually observed in all types of asphyxia and other types of deaths.
Comment Here
Reference: Asphyxia
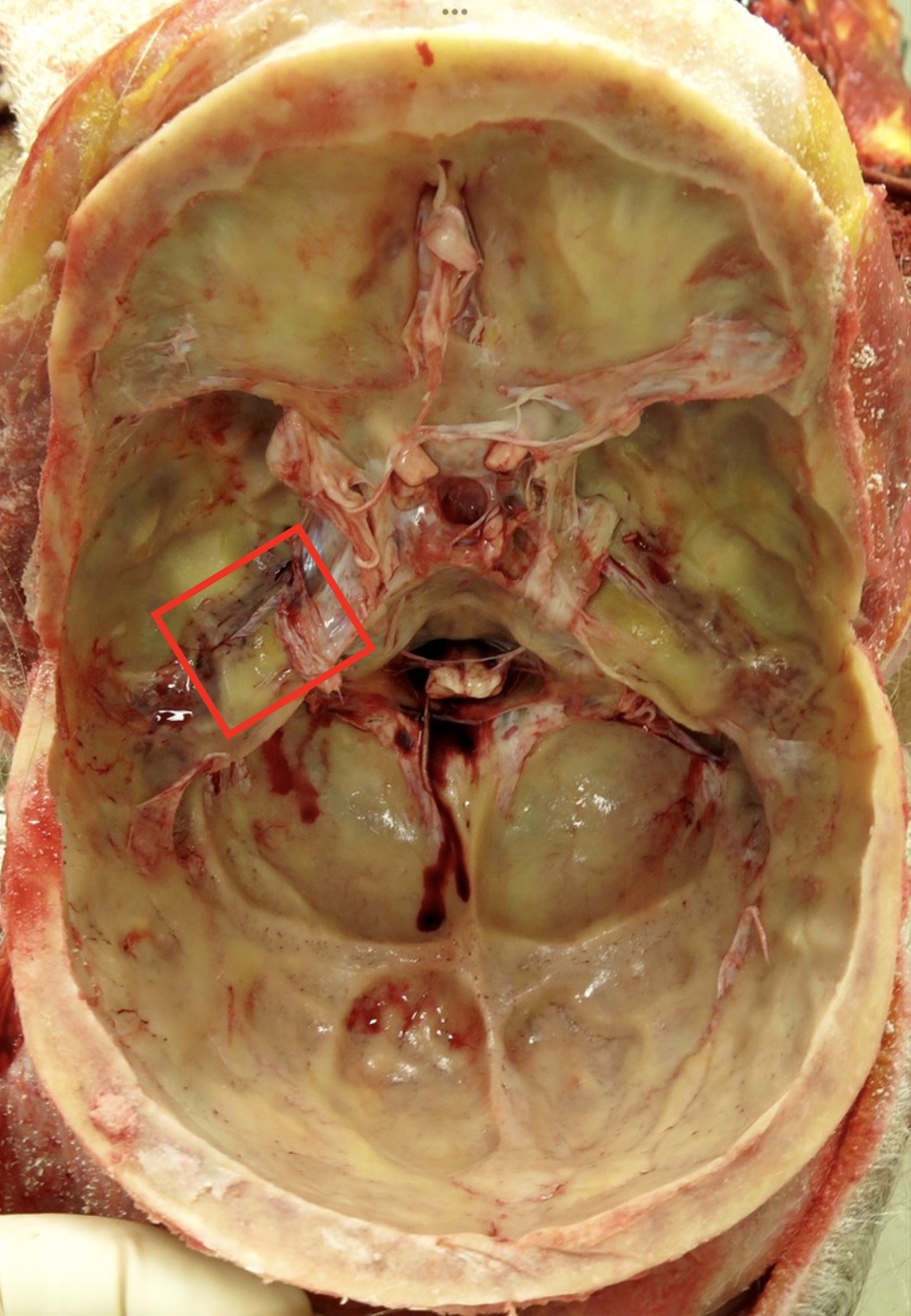
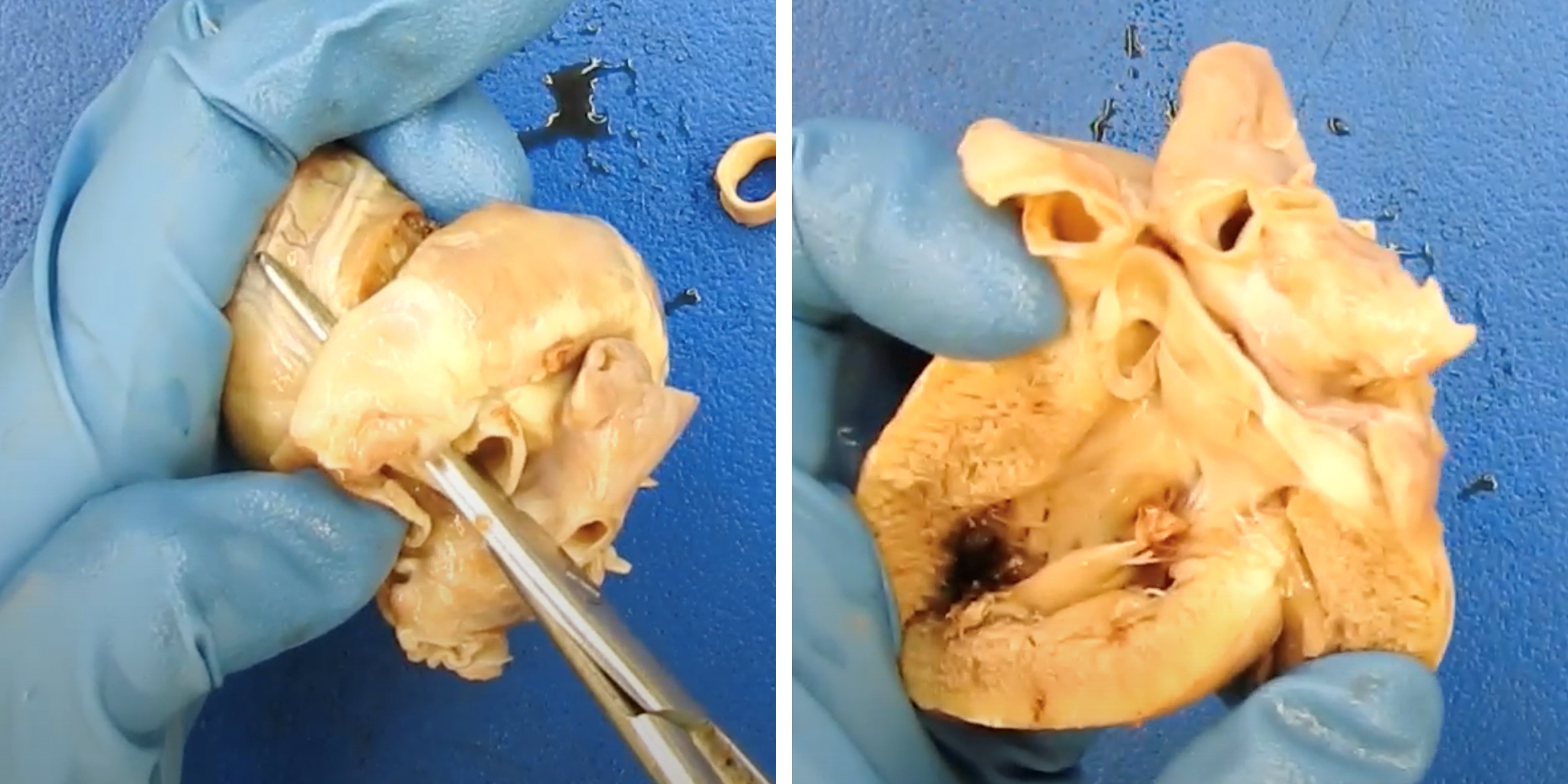
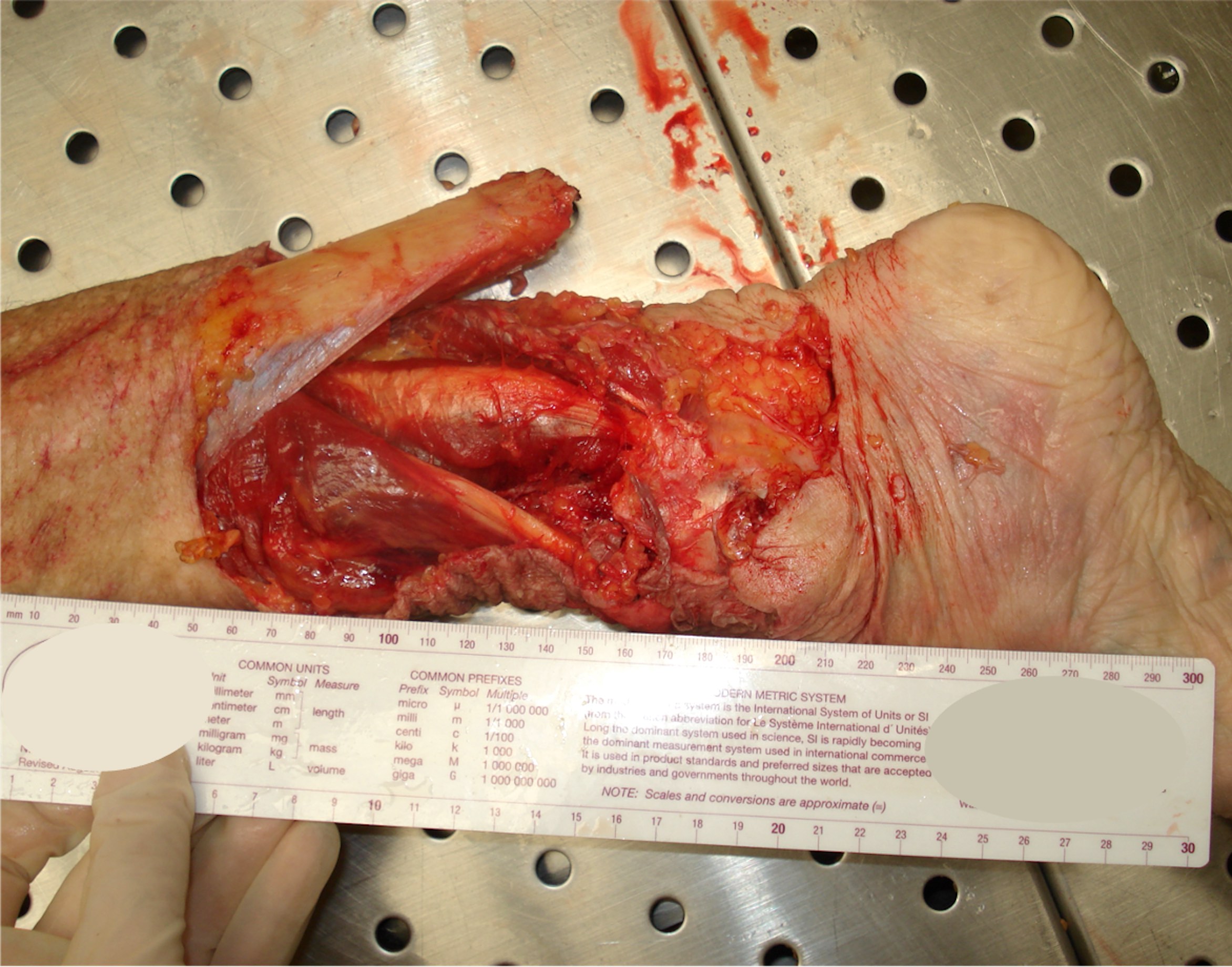
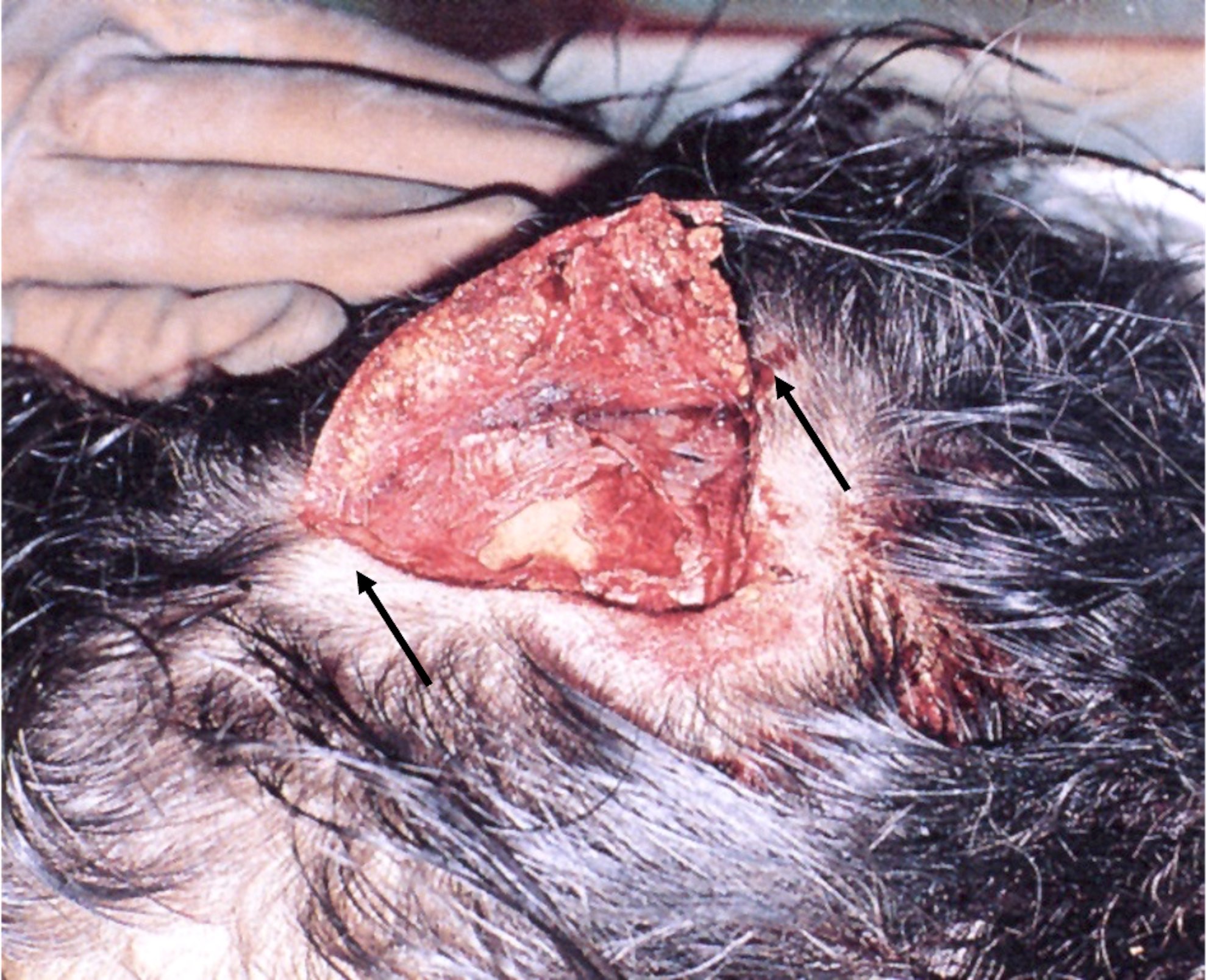
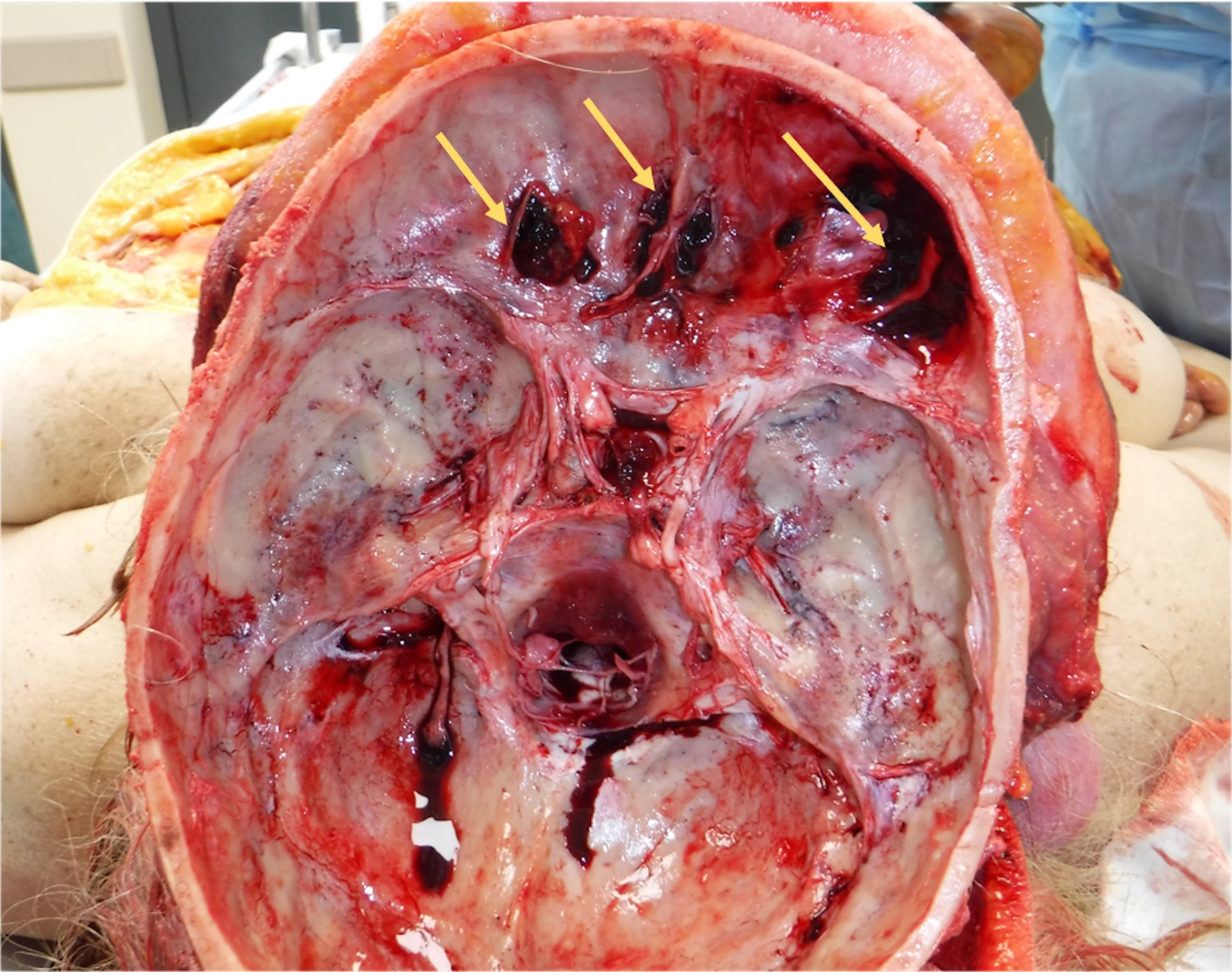
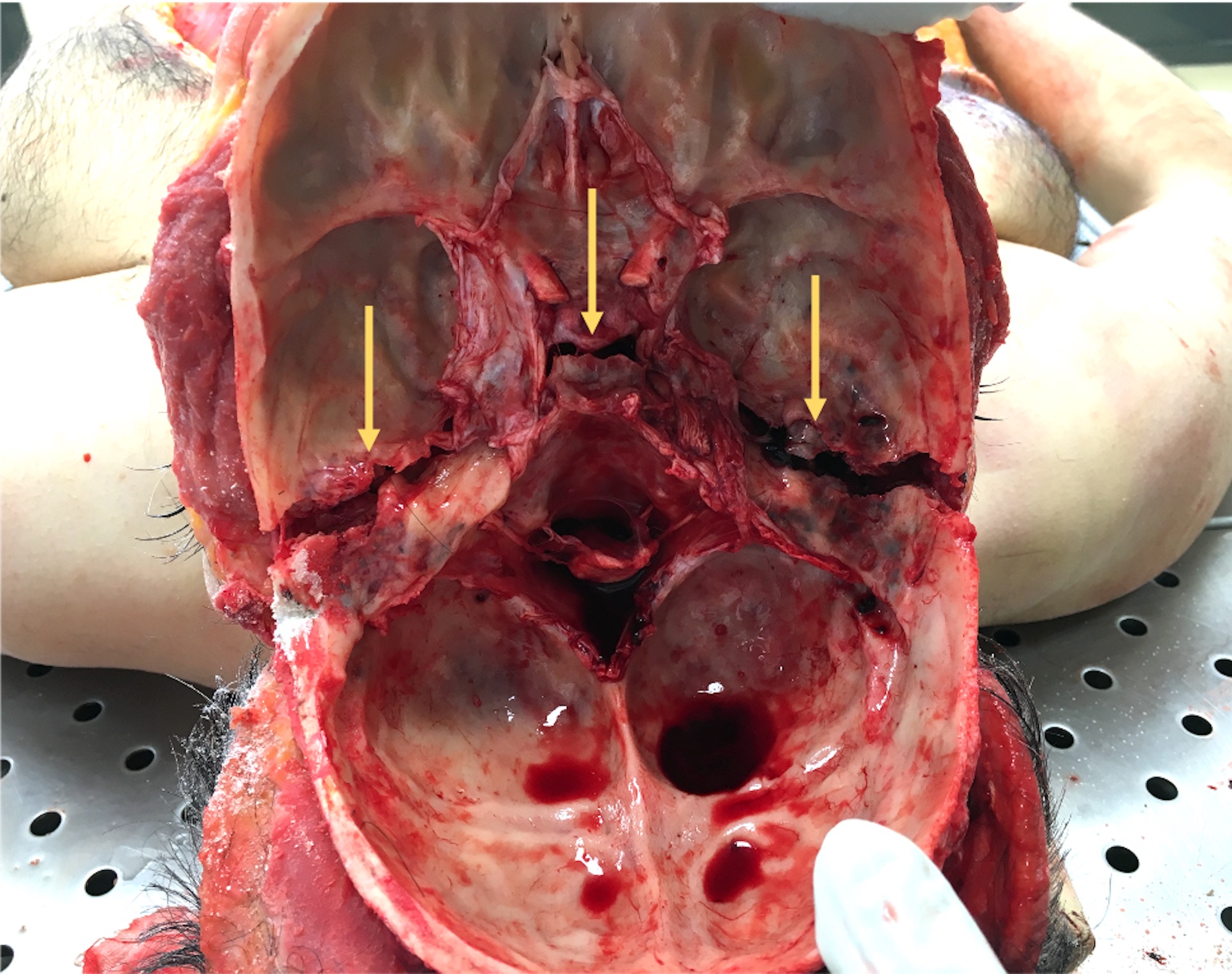
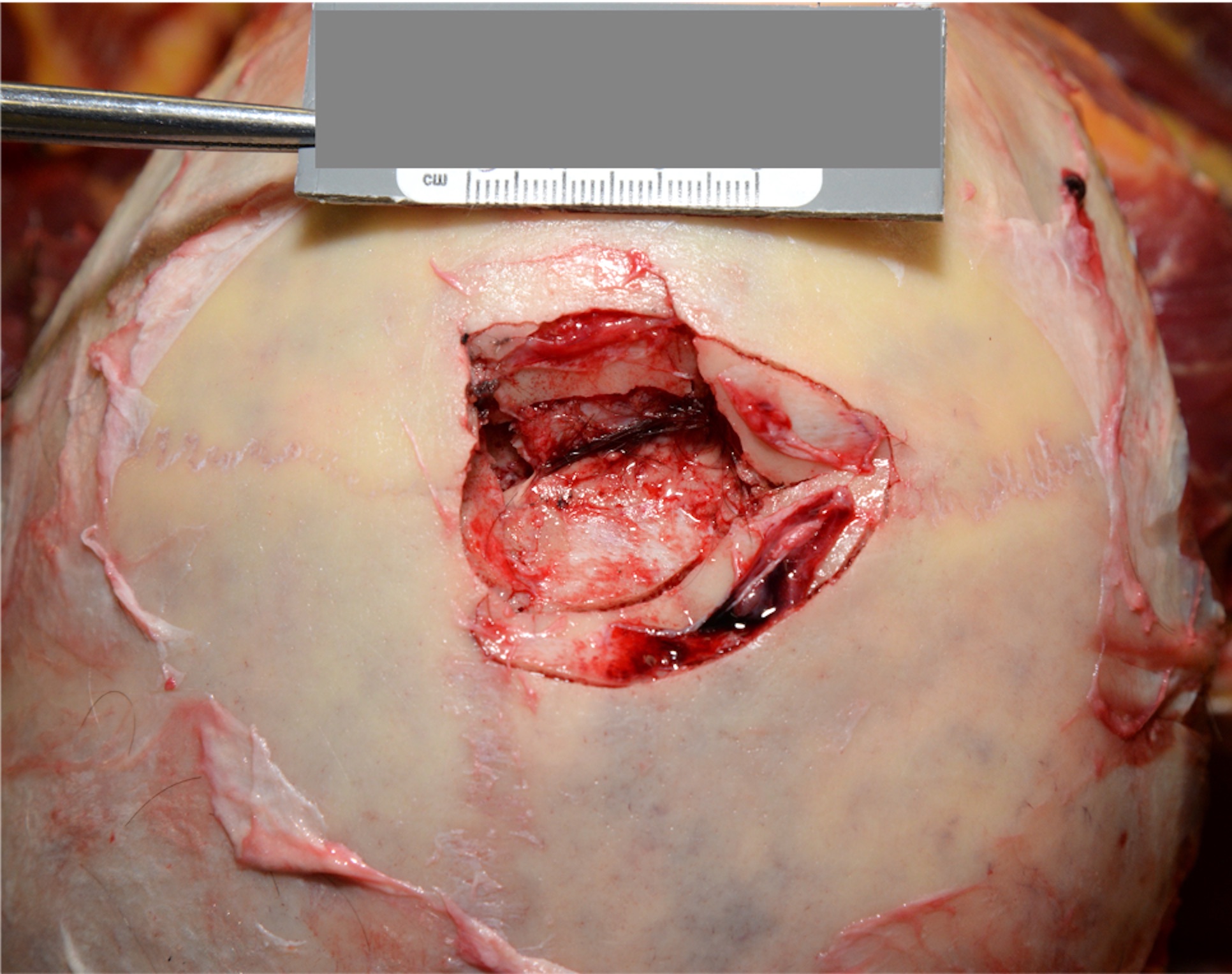
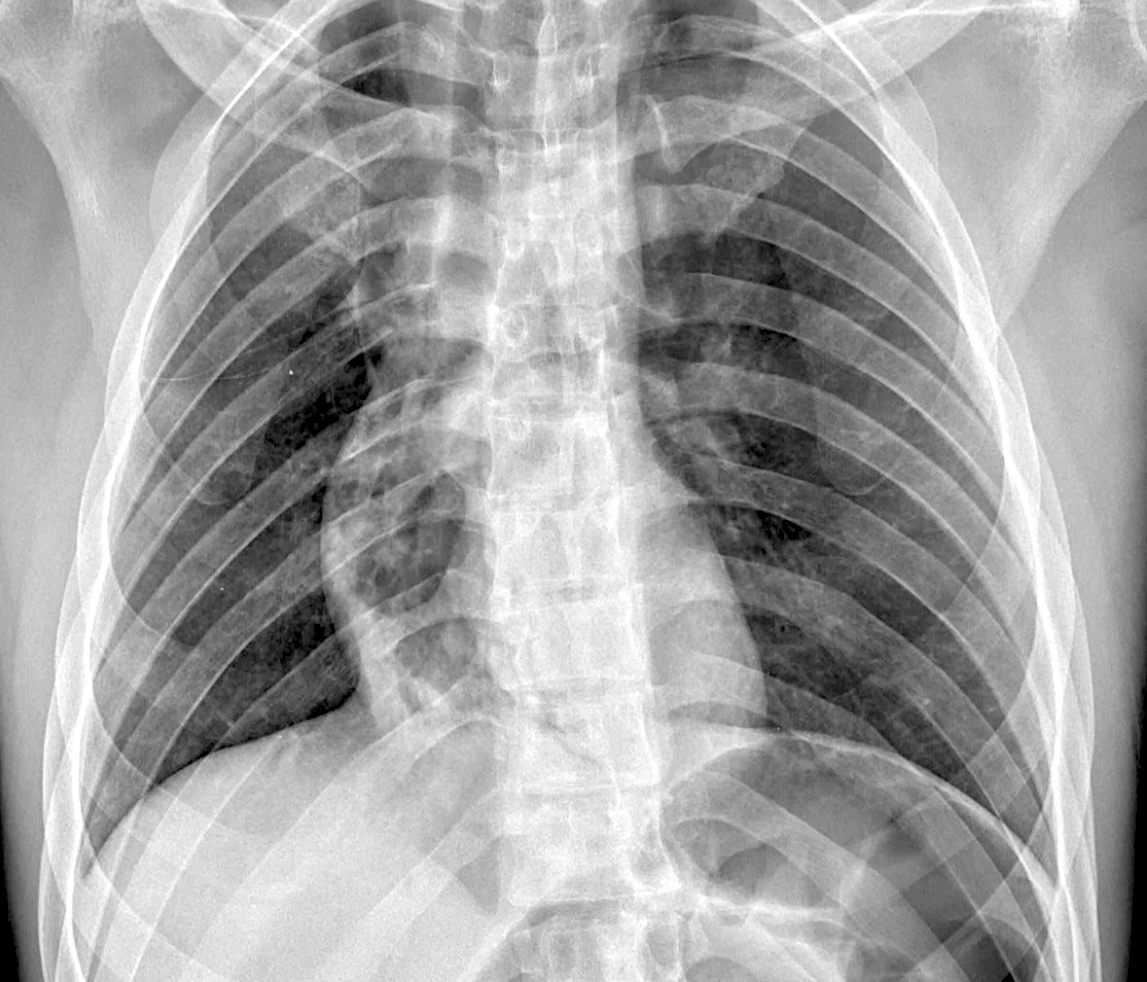
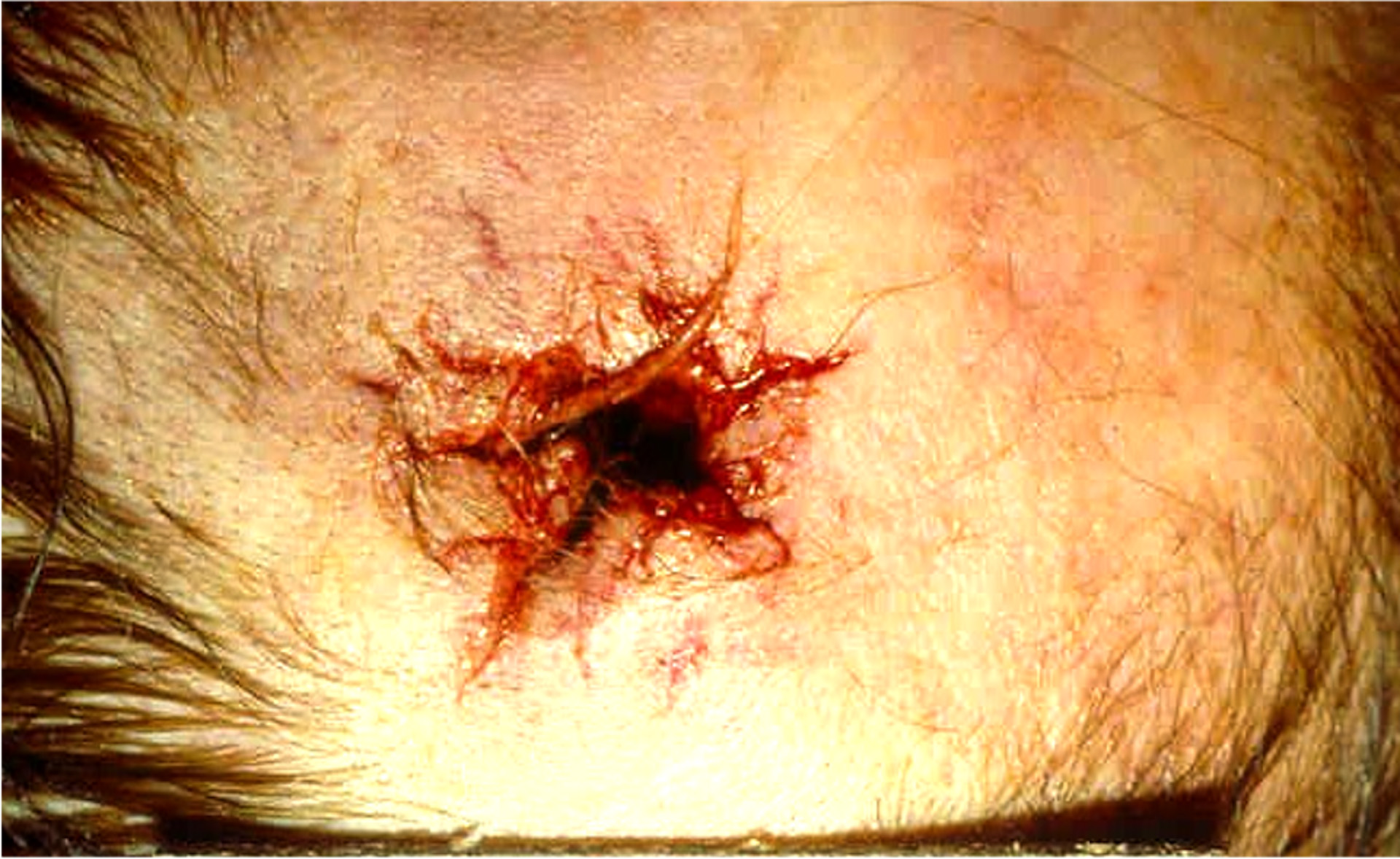
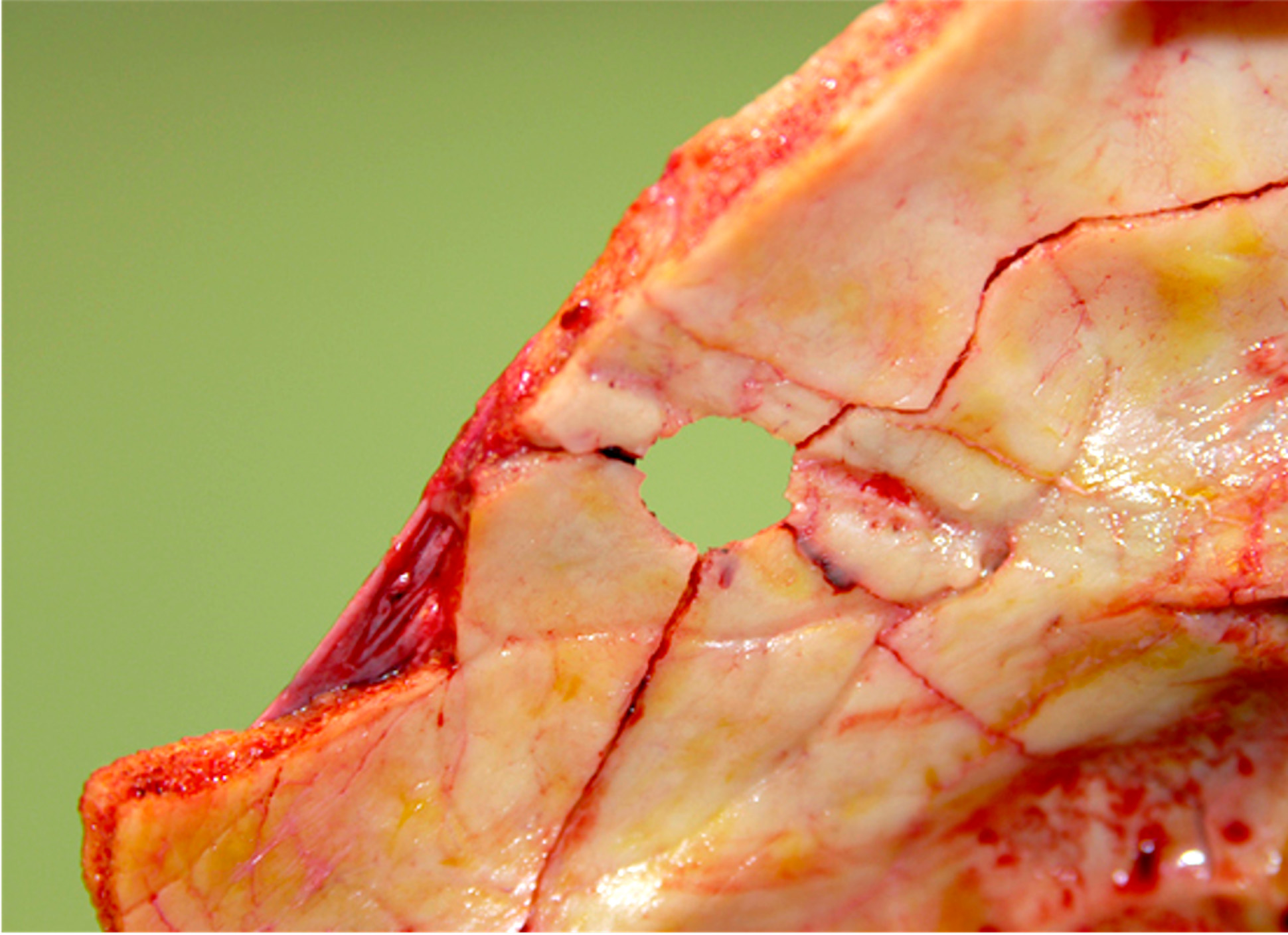
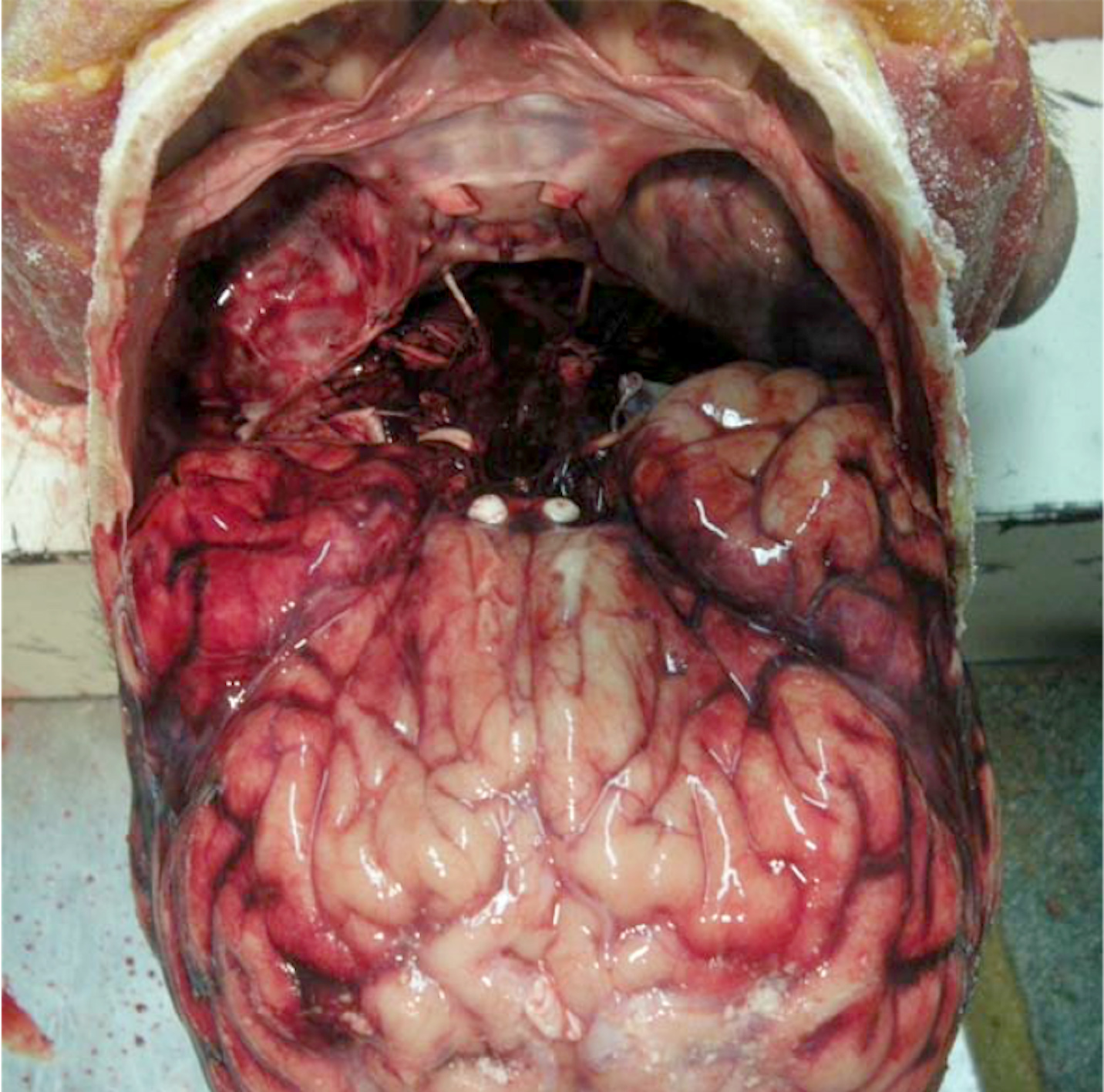
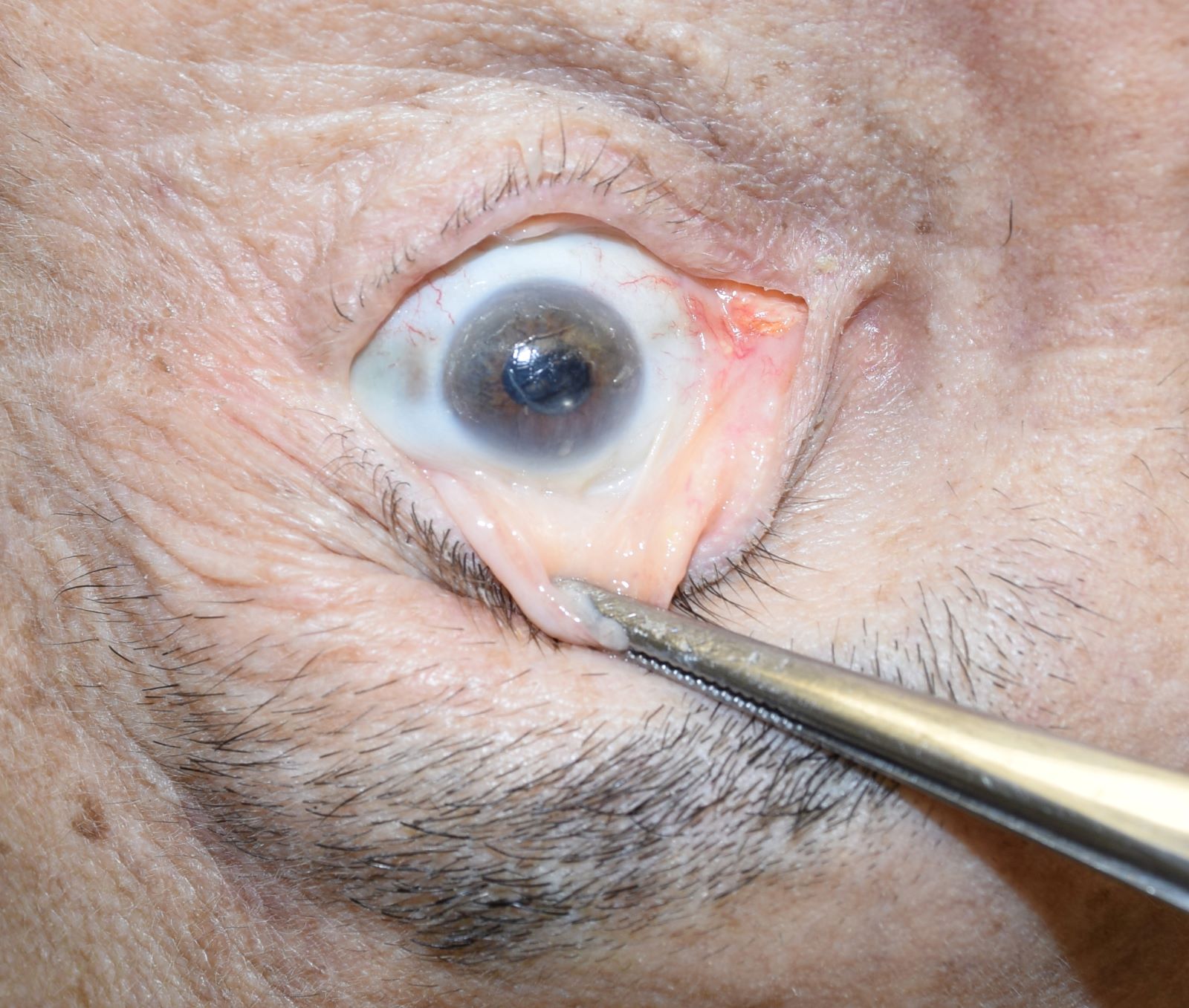
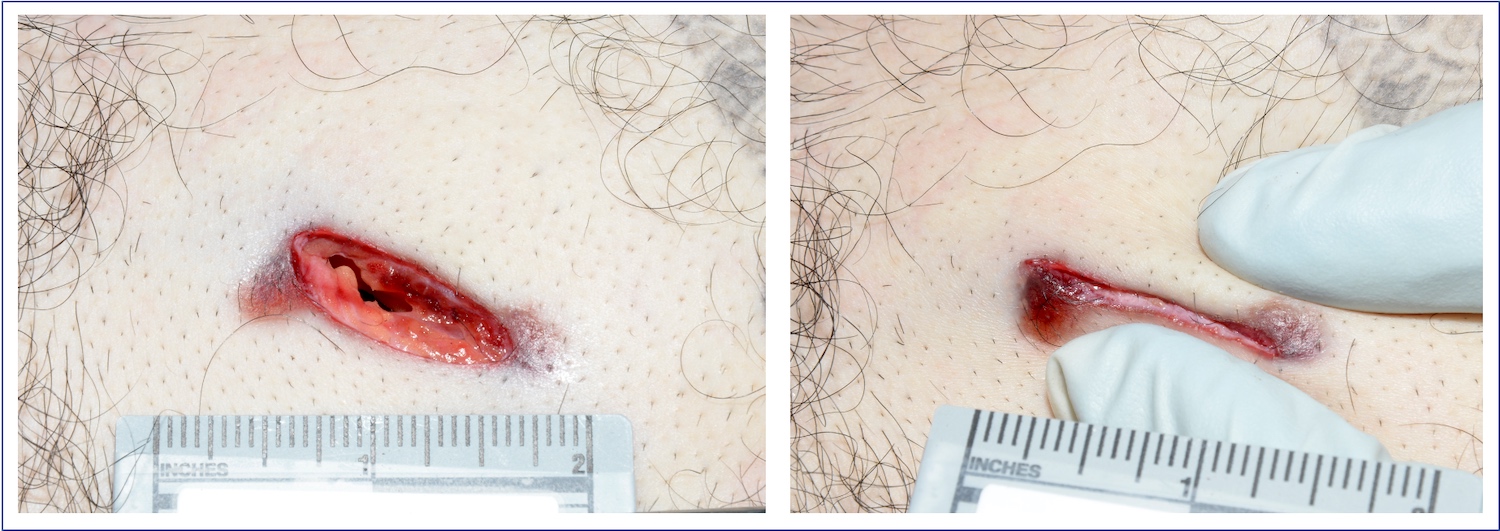
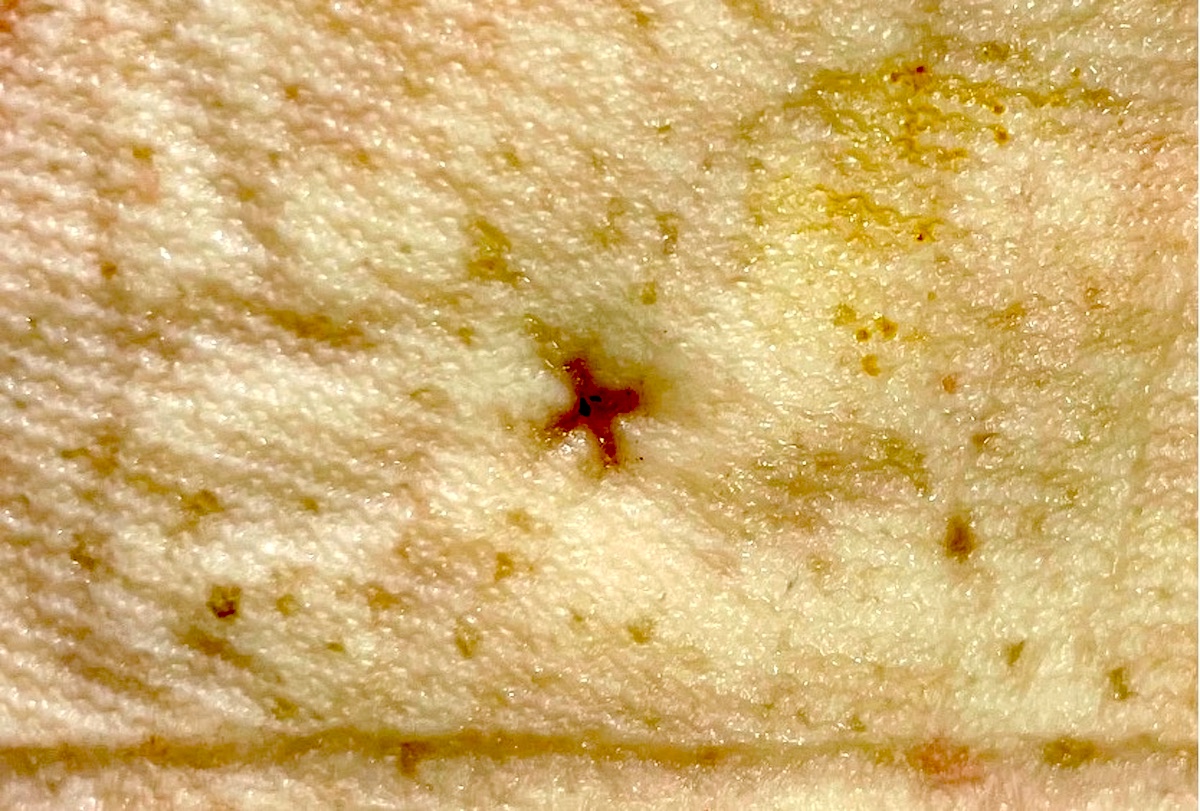
A 73 year old man is found dead in his apartment. Autopsy reveals multiple neck bruises and abrasions as well as the finding shown in the image. Assuming that the death results from an asphyxia mechanism, what is the most likely manner of death?
- Manual strangulation
- Hanging
- Drowning
- Homicide
- Suicide
Manual strangulation, hanging and drowning (answers A, B and C) are specific types of asphyxia and represent causes of death, not manners of death. Larynx and hyoid injuries are less common in suicide (answer E). Moreover, suicide by manual strangulation is not possible.
Comment Here
Reference: Asphyxia
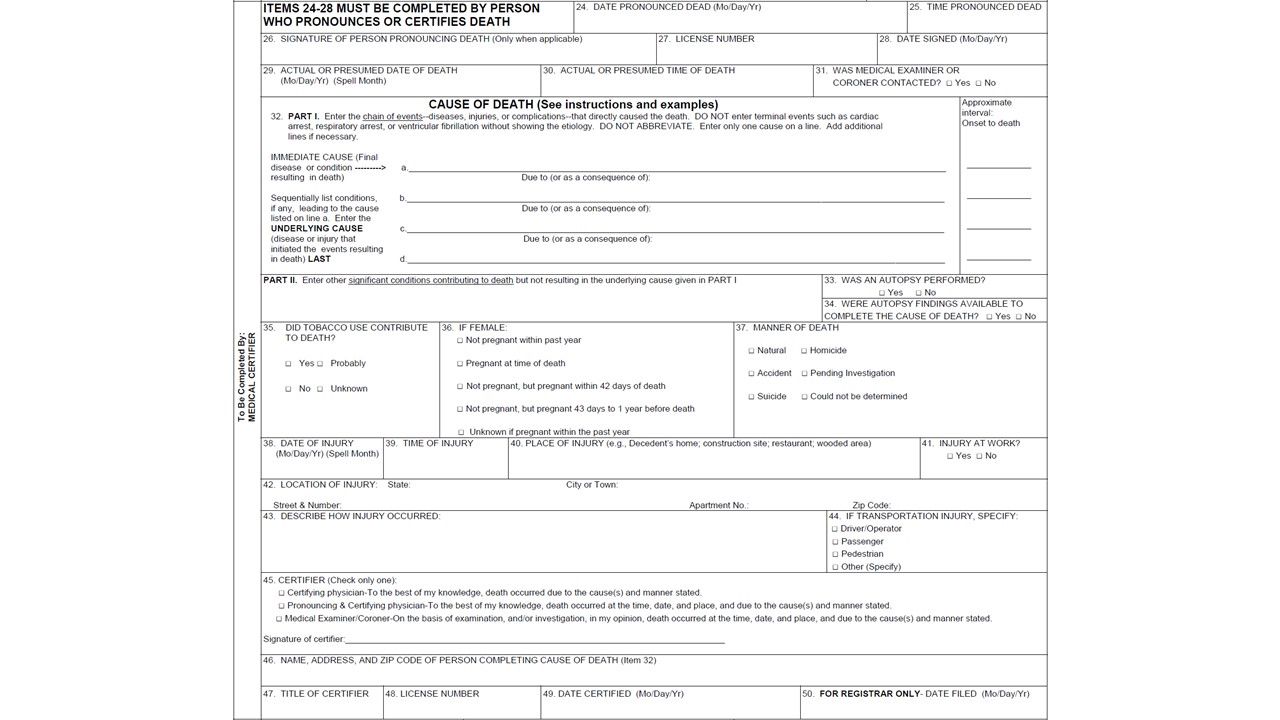
- Completing a forensic autopsy report is an art in itself
- Everything, including the decedent's demographics, circumstances of death, external examination, clothing / personal effects, medical intervention, radiographic imaging, evidence of injury, internal examination, microscopic examination, specific organ system pathology consultation, final autopsy diagnosis, and opinion sections should complement one another in a cohesive manner
- No two autopsy reports are the same; keep an open mind for each case
- If using a template, take care to make the appropriate changes to suit each case
- Cause of death (COD) is usually straightforward, but the manner of death (MOD) and mechanism of death tend to be more challenging
- Forensic autopsies emphasize identification of deceased, time of death, proper handling of evidence, recognition of injuries and pathological conditions that may be relevant to the court case
- For homicide court cases, an autopsy report is only one piece of the pie
- Law enforcement investigators, attorneys, forensic science experts (e.g., trace evidence, fingerprints) and other expert witnesses will fill in the rest
- Depending on the jurisdiction, the cover page of a forensic autopsy report includes: demographics of the decedent, circumstances of death, identification, cause of death and manner of death
- Having an autopsy report with an undetermined cause and undetermined manner of death (undetermined / undetermined) is very rare; only if all evidence at autopsy is inconclusive
- Frequency of undetermined cases: not more than 1% - 2% of all autopsy cases done by a forensic pathologist in one year
- Conduct "VIP" / high profile cases as if you would routinely perform like any other case to avoid unnecessary mistakes
- Depending on the case, high profile or difficult autopsies should be checked by another forensic pathologist for accuracy
- FP should be board certified in at least anatomic and forensic pathology for competency measures
- Decedent: person who died (a legal term)
- Include full name, autopsy number, social security number, age, date of birth, date of death, date of autopsy performed, place of death and date of autopsy report completed
- Events that occurred prior to the person's death, such as when last seen alive, prior hospitalizations, and pertinent positive / negative evidence to support COD / MOD
- Antemortem / postmortem fingerprint, dental, radiographs or DNA comparison is objective evidence and is added to evidence from pictures, driver license or other unique identifiers (e.g., tattoos or amputations)
- Drowning, gunshot wound to the chest, acute myocardial infarction, multidrug toxicity (overdose), undetermined, etc.
- Accident, homicide, natural, suicide or undetermined
- Circumstances of death need to be reported by the forensic pathologist (FP) based on information provided by law enforcement personnel who are familiar with the death scene
- Depending on the case, the FP can obtain crucial information at the death scene or by a phone call to law enforcement investigators
- Asking specific questions related to the case will help provide clues to Cause / Manner of Death (COD / MOD)
- Specific questions related to the decedent's past (medical history, recent surgeries, state of mental health, drug / alcohol abuse, etc.) may reduce the need to perform a complete autopsy when only toxicology analysis is required to determine COD / MOD
- Overall: state body weight, height, age, body temperature, rigor and lividity
- Head / neck: describe hair color, facial hair, eye color, oral cavity, ear canals, nose, lips and teeth
- Torso: describe chest, abdomen, back, anus and genitalia
- Extremities: describe upper / lower limbs and fingernails / toenails
- Miscellaneous: describe tattoos, ID tags, medical / surgical intervention, etc.
- Clothing: describe any defects to support cause of death (COD)
- Body surface: state anything to suggest evidence of cause of death, such as gunshot wounds, blunt trauma, sharp force injury, illicit drug residue, anasarca, obesity, emaciation, sexual assault
- General:
- Organs need to be weighed
- All lesions need to be measured in 3 dimensions, if possible
- Evidence of Injury does not need to be repeated in each organ system; a statement such as "see 'evidence of injury' above" will suffice
- Natural causes of death are usually found in this section of the autopsy report: body cavities, head / CNS / neck, cardiovascular system, respiratory system, hepatobiliary system, gastrointestinal system, genitourinary system, lymphorecticular system, endocrine system, and musculoskeletal system
- Body cavities: state any abnormal pericardial, thoracic or abdominal fluid acumination
- Head / CNS / neck: look for lesions involving the scalp, calvarium, dura mater, falx cerebri, leptomeninges, cerebral hemispheres, gyri / sulci, cut sections of brain, brain stem, cranial nerves, major blood vessels, CSF, cerebellum, atlanto-occipital joint, thyroid cartilage, hyoid bone, larynx, tongue, etc.
- Cardiovascular system: epicardial surface, coronary arteries (distribution, patency versus occlusion, and wall thickness), myocardium (LV / RV / septum) thickness, valves, endocardium, aorta, renal vessels, mesenteric vessels, etc.
- Respiratory system: upper airway, mucosa, pleural surfaces, pulmonary parenchyma, vasculature, etc.
- Hepatobiliary system: hepatic capsule, liver parenchyma / vasculature, gall bladder serosa / mucosa, etc.
- Gastrointestinal system: esophagus, gastric mucosa, small bowel, colon, appendix, pancreas, etc.
- Genitourinary system: renal capsule(s), cortical surface(s), cortical / medullary parenchyma, bladder, male organs (testes, prostate), female organs (ovaries, uterus), etc.
- Lymphorecticular system: splenic capsule, splenic parenchyma, regional lymph nodes, etc.
- Endocrine system: pituitary gland, thyroid gland, adrenal glands, etc.
- Musculoskeletal system: muscle and bone structures
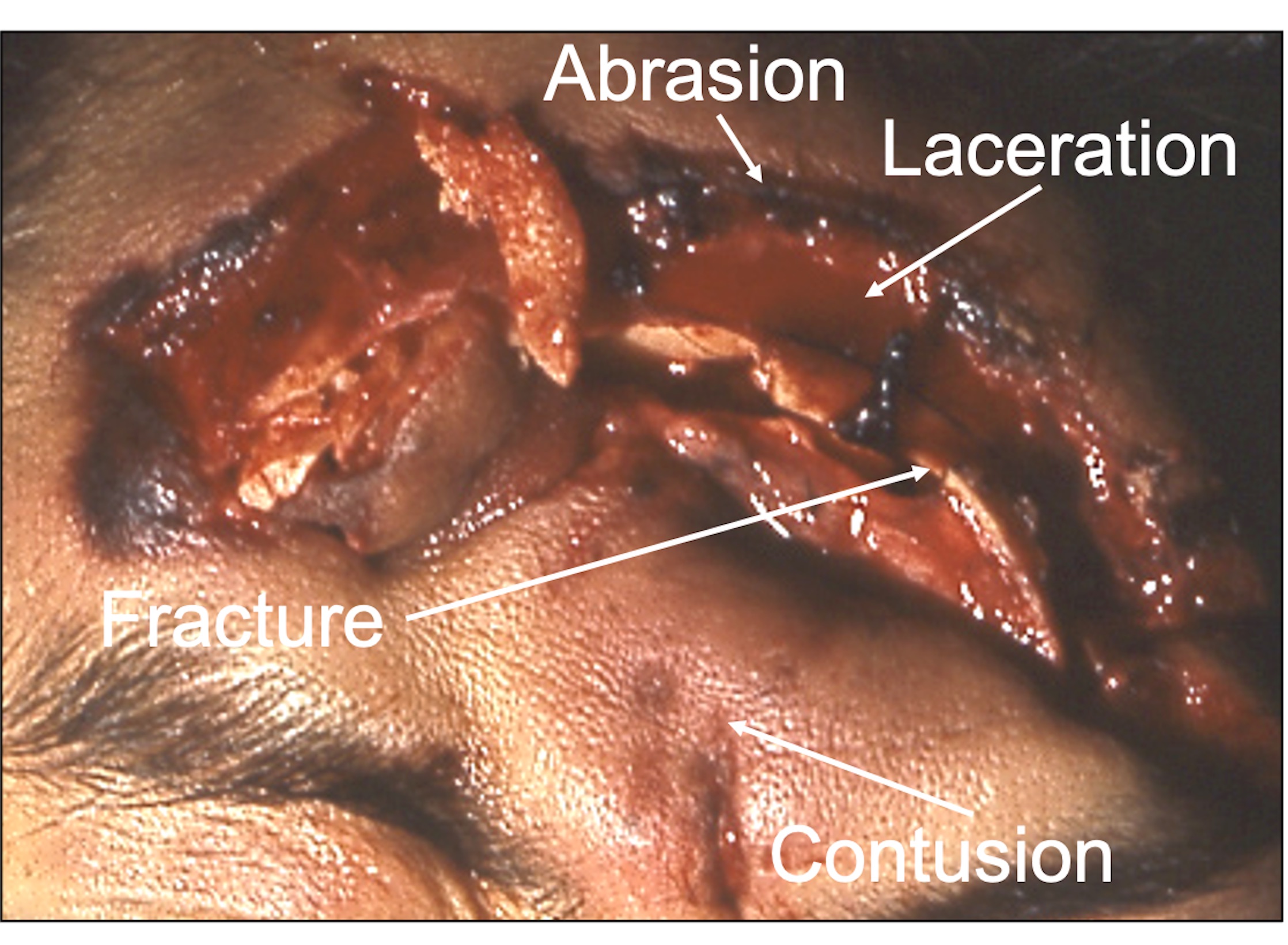
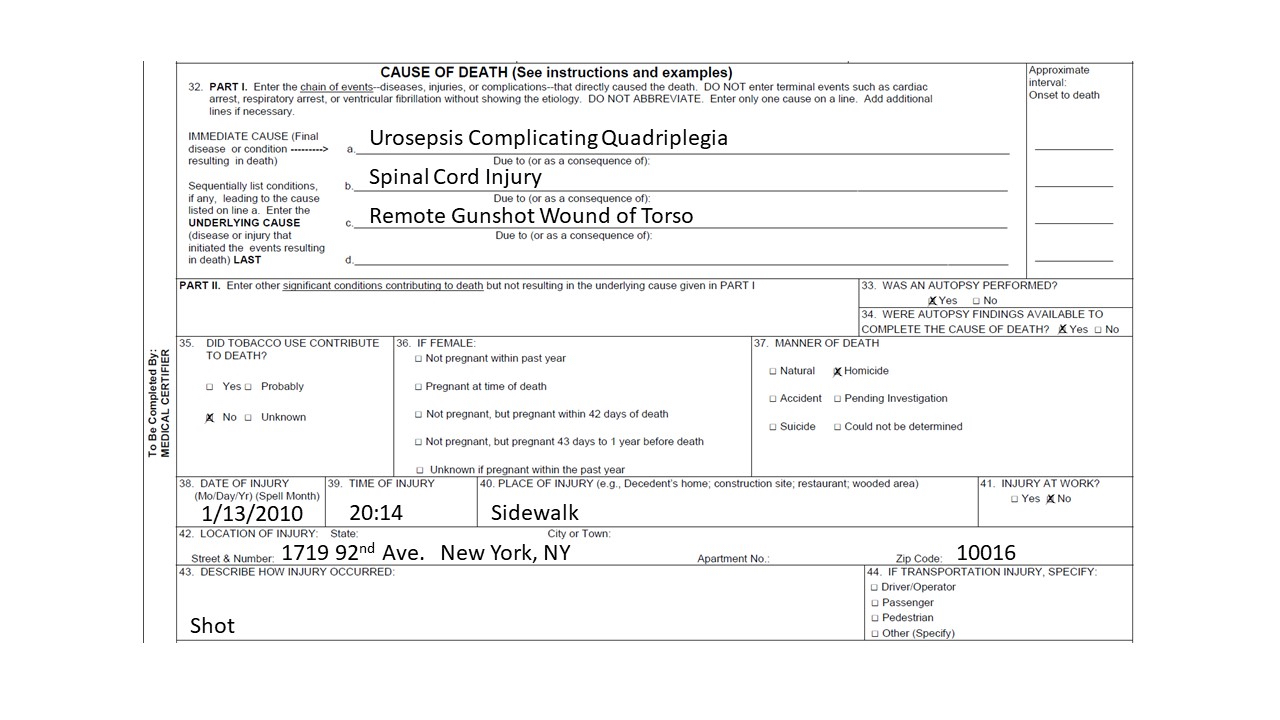
- This section usually contains both external and internal descriptions of injury
- Gunshot wounds (GSW): list each GSW trajectory separately, determine how many entry (penetrating) / exit (perforation) wounds, range of fire, soot / stippling, trajectory, recovery of projectile(s), state in proper order of anatomic landmarks injured by each GSW, hemorrhage, etc.
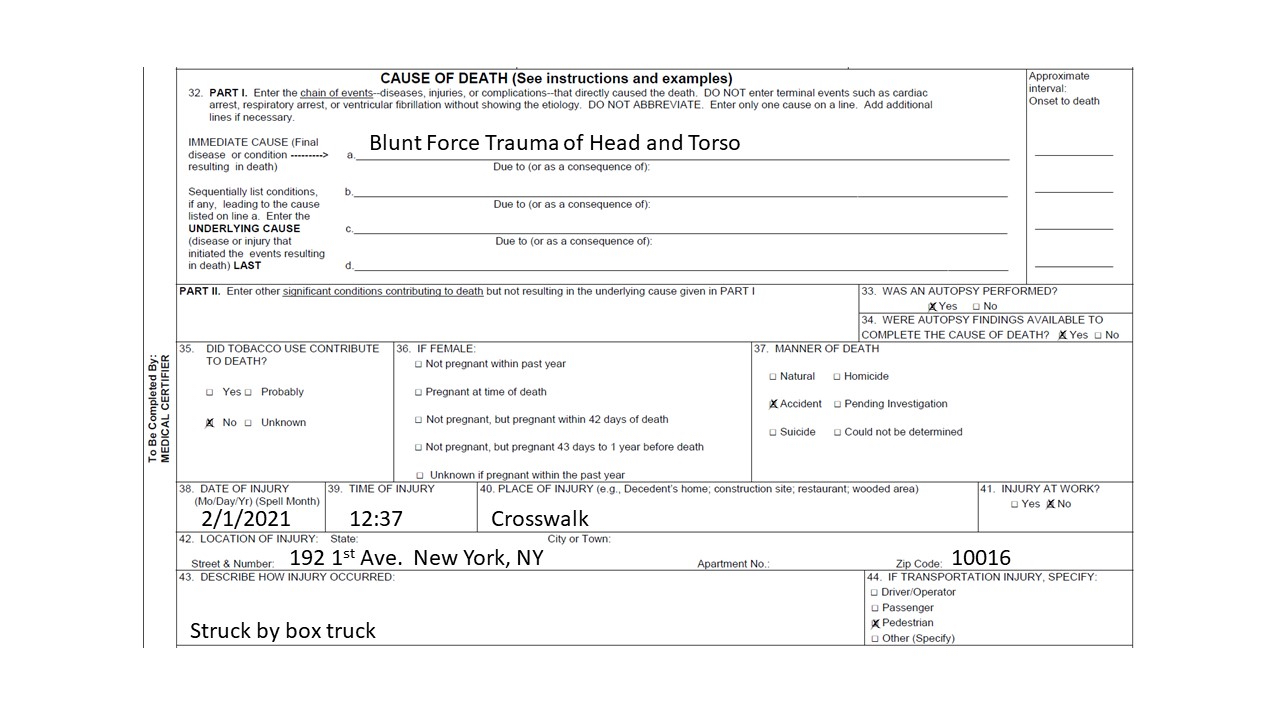
- Blunt force injuries from motor vehicle accident (MVA): trace evidence collected on body (e.g., paint chips or glass), pattern contusions / abrasions, fractures, lacerations, avulsions, hemorrhage, etc.
- Stab wounds: cuts, incisions, defense wounds, determine the knife's sharp verses blunt end in each skin wound, depth of wound, organs affected, hemorrhage, etc.
- Additional injuries: minor lesions that are attributed by the mechanism or cause of death
- Useful for documenting natural disease or gross lesions histologically (e.g., gunpowder residue)
- Describe what is seen microscopically; do not state diagnosis in this section
- This section may include neuropathology or cardiovascular consultation reports, toxicology reports, autopsy attendance roster, etc.
- Spinal cord (2 - 3 levels), medulla, pons, midbrain, cerebellum, hypothalamus, basal ganglia, hippocampus, thalamus, parietal cortex, occipital cortex, cingulate gyrus, superior temporal gyrus, paracentral cortex and pituitary
- The scalp and skull are entered in a standard biparietal, postauricular manner
- The dura is intact and the sagittal sinus is patent
- The prefixation brain weight is __ grams
- The formalin fixed brain weights __ grams
- The cerebral and cerebellar hemispheres are symmetrical with no masses, areas of discoloration or gross lesions identified
- There is no evidence of midline shift
- There is no uncal, subfalcine or tonsillar softening or grooving
- The sulci / gyri are unremarkable, with no atrophy identified
- The leptomeninges are thin, translucent and without hemorrhage
- The circle of Willis is intact, with no atherosclerotic plaque
- Coronal sections of the cerebral hemispheres show well delineated gray and white matter structures
- The ventricles are symmetric and not dilated
- Distal blood vessels are unremarkable
- Axial sections of the midbrain, pons and medulla are symmetrical with well delineated gray and white matter structures
- The substantia nigra and locus ceruleus are well pigmented
- The aqueduct and fourth ventricle are unremarkable
- Parasagittal sections of the cerebellum show well delineated white and gray matter structures with prominent folia
- The pituitary is removed from the sella and is grossly unremarkable
- The spinal cord is removed by an anterior approach
- Axial sections of the spinal cord are symmetric with well delineated gray and white matter
- The spinal cord shows...
- The midbrain, pons and medulla show mild neuronal loss and gliosis consistent with the patient's age
- The cerebellum, basal ganglia and thalamus are unremarkable
- The hippocampus shows no senile plaques or neurofibrillary tangles
- The cerebral neocortex is unremarkable
- Autopsy techniques refer to the manner in which an autopsy is performed in order to assess the body externally and internally to identify the cause and circumstances of death
- Techniques vary based on the training and experiences of the autopsy practitioner and the particulars of the case
- Incisions must provide ready access to the site of interest while offering an opportunity for excellent reconstruction
- General methods of autopsy vary and may include the removal of organs individually or en masse with subsequent dissection
- Specific dissections may be required depending on the circumstances of death and autopsy findings; techniques vary by autopsy practitioner and some cases may benefit from subspecialist referral
- Postmortem examination techniques
- Prior to autopsy
- Follow local standards regarding patient identification and written consent by first of kin (for clinical autopsy)
- Full 3 cavity examination
- Limited to particular areas
- External / noninvasive only (which may allow radiology and taking of samples via a needle)
- Summarize information as available regarding the circumstances of death, if known, including any past medical, occupational and social history, in order to determine the autopsy techniques most likely to yield answers
- Determine if the presence of police or other specialists (e.g., forensic dentists) is needed
- Determine whether radiology will assist the autopsy (Forensic Sci Res 2022;7:385)
- Follow local standards regarding patient identification and written consent by first of kin (for clinical autopsy)
- Complete external examination
- Primary skin incisions
- Anterior body wall incisions
- Y shaped: most common and with excellent reconstruction results
- T shaped
- I shaped or vertical
- Scalp
- Coronal incision in an adult provides ready access for the removal of the crown with excellent reconstruction results as it is behind the hairline
- Anterior body wall incisions
- General autopsy methods
- Letulle
- Organs removed en mass and subsequently dissected
- Best for observing the pathological and anatomical relationships of structures
- Produces a large, bulky mass with which to work
- In brief
- After opening the body, remove the distal duodenum to the rectum and dissect the pelvic organs away from the body wall
- Transect the iliac vessels
- Free the diaphragm then the retroperitoneal organs (bluntly dissect and pull the kidneys forward) from the body wall around each side to the vertebra
- Free the neck structures anterior to the cervical vertebrae moving upward to stop once the tongue is free
- Use the tongue (being wary of damaging the larynx) to strip the organs downward off the vertebrae anteriorly to remove the organs en masse
- Organs are then usually examined sequentially from the posterior aspect
- Ghon
- Organs removed as organ blocks and subsequently dissected
- Thoracic, coeliac, intestines and urogenital system blocks
- In brief
- Free the tongue as described for Letulle and strip the organs downward off the vertebrae anteriorly stopping at the lower esophagus
- Transect the esophagus and descending aorta at this level and remove the thoracic block
- Tie and cut the duodenal / jejunal junction then the rectum
- Work from one end of the bowel to the other, cutting across the mesentery close to the bowel wall to remove the intestines en bloc
- Remove the rest of the abdominal organs with a method similar to Letulle
- Virchow
- Organs removed from the body and inspected one by one (Virchow: Post-Mortem Examinations, With Especial Reference To Medico-Legal Practice, 1880)
- In brief
- After opening the body, inspect the abdominal contents and the pleural cavities
- Open the pericardium and remove the heart, followed by each lung
- Assess the neck (pharynx, larynx, parathyroid glands, thyroid gland) and remaining organs in the thorax (predominantly the esophagus)
- Move to the abdomen and remove the spleen, intestines, liver and pancreas
- Open the stomach in situ
- Remove the kidneys and adrenal glands from the retroperitoneum, tracing the ureters to the bladder
- Remove the pelvic organs
- Inspect and open the large arteries and veins in the abdomen and pelvis
- Rokitanksy
- Debated as to the exact original technique
- Organs inspected and incised in situ
- Considered to provide less information
- Of benefit if there is a highly transmissible disease
- In reality, each autopsy practitioner performs their own modified autopsy technique depending on their training, experiences and the particulars of the case
- All autopsies require thorough documentation of positive findings and relevant negative findings including the taking of photographs (with visible identifiers and scale)
- Letulle
- After autopsy
- Consider further investigations
- Histology
- Blood spot card (previously known as a Guthrie card)
- Biochemistry
- Microbiology
- Virology
- Toxicology
- Genetics
- Other
- Summarize information to determine the provisional cause of death
- Compile histology and other investigation results into final report, completed at a later date
- Consider further investigations
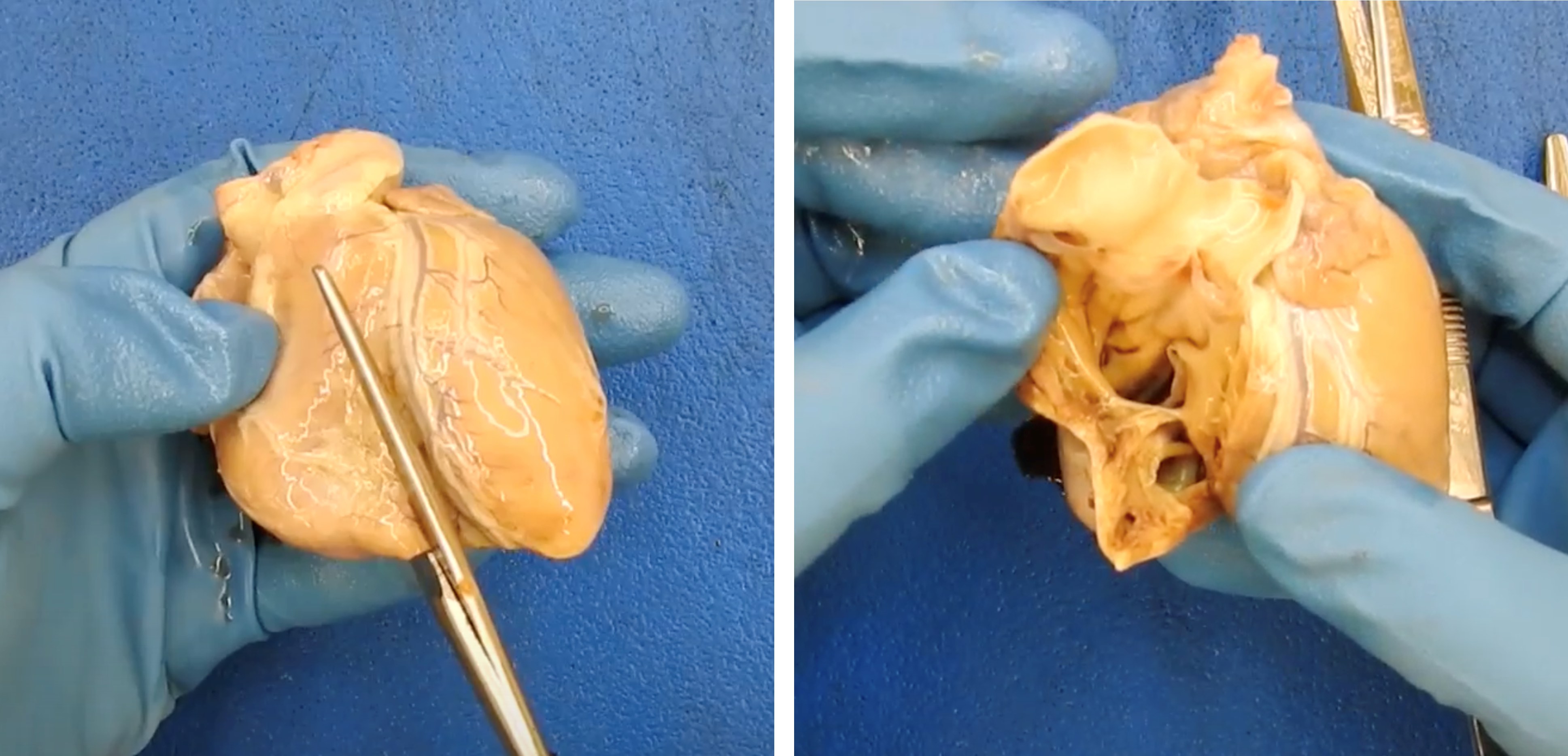
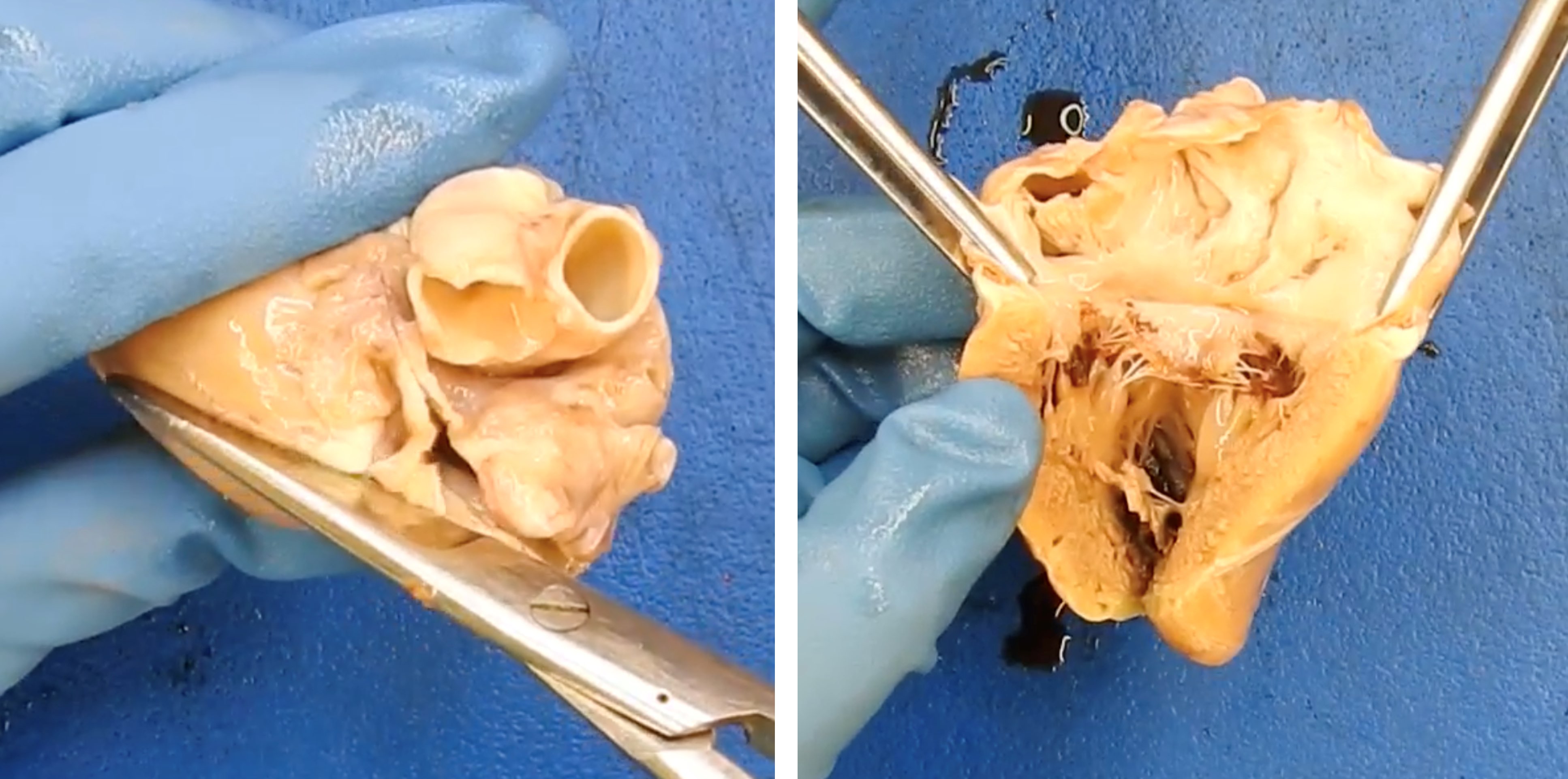
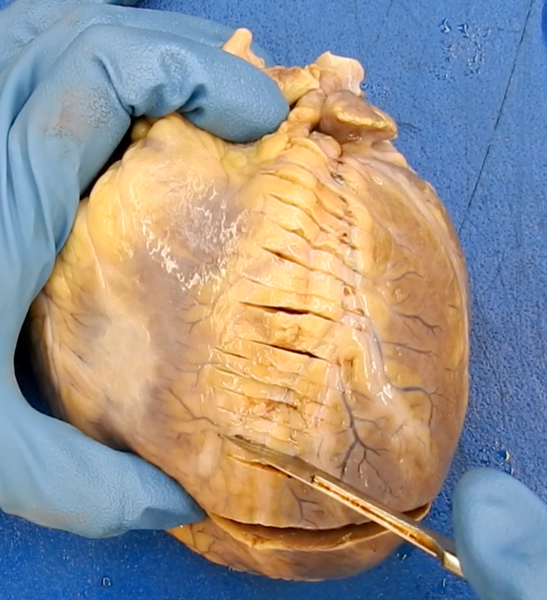
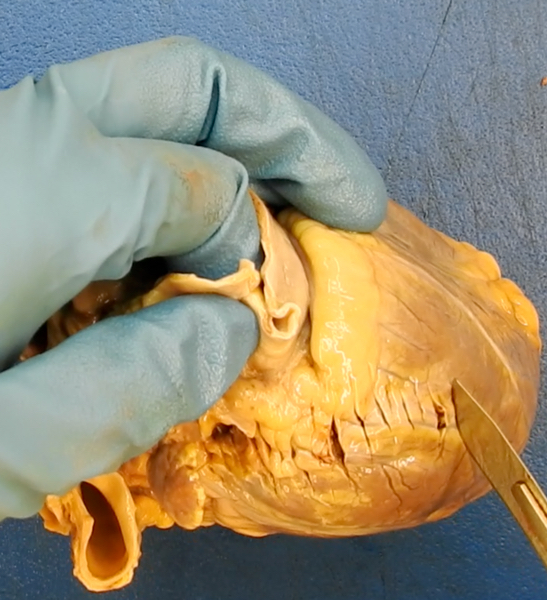
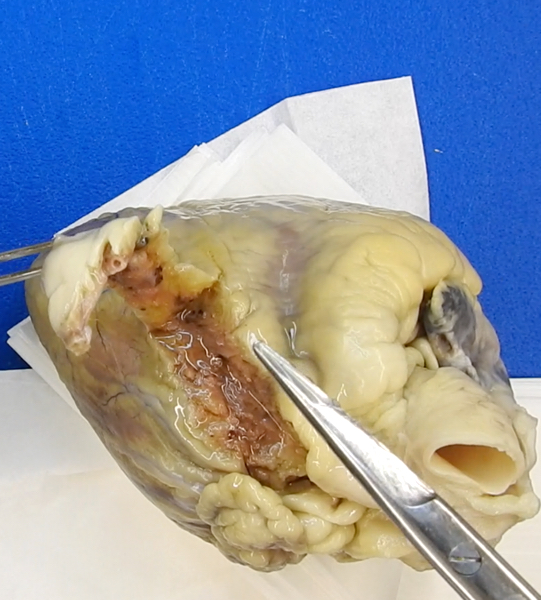
- See Forensic heart dissection
- Standard line of flow
- Indicated in all autopsies due to the prevalence of cardiac causes of sudden natural death in all ages and to rule out its contribution in unnatural deaths
- Heart is usually separated from the body at the level of the transverse pericardial sinus allowing for several centimeters of aorta and pulmonary artery above the respective valves and intact atria; care must be taken to assess for major aberrant anatomy when separating the heart from the body
- Several methods exist for organ dissection, most commonly the major named coronary arteries are first assessed for aberrant anatomy and disease
- Arteries can be opened longitudinally or transversely, the latter being regarded as more accurate
- Assessment frequently requires decalcification, which can be completed on already sectioned arteries or on a whole artery (later sectioned)
- Next, the ventricles are sliced perpendicular to the interventricular septum (IVS) from the apex to the level of the midpapillary muscle
- Right atrium is opened and inspected by cutting between the superior and inferior vena cava
- Cut is made opposite the septum from the atrium, through the tricuspid valve and through the right ventricle
- Cut is made on the anterior surface of the heart through the pulmonary valve
- On the left side of the heart, the atrium is opened by cutting between 2 pulmonary veins
- Cut is made opposite the septum from the atrium, through the mitral valve and through the left ventricle
- Cut is made on the anterior surface through the aortic valve to inspect the valve and coronary ostia
- Measurements should include at a minimum the weight of the heart in total, size of each chamber, thickness of each wall and valve orifice
- Fulton technique is used for assessing ventricular hypertrophy and involves separating the left ventricle (including the IVS) from the right ventricle and weighing them separately to calculate a ratio, with 2.3 - 3.3:1 (LV:RV) being considered normal (Br Heart J 1952;14:413)
- Postsurgery (coronary artery bypass grafting [CABG], valve replacement, ascending aorta repair / replacement)
- Assessment is often made much more difficult by fibrous adhesions around the heart and metal stents
- Rarely, postmortem coronary angiography prior to autopsy may be indicated and compared to antemortem angiography
- If the surgery is recent or likely to be involved in the cause of death, it is critical to receive clinical notes including any operation reports
- With CABG, it is essential to study both the native and grafted vessels for patency and check the ostia
- Following valvular surgery, it is important to note the type of valve prosthesis as well as assess for any paravalvular leak, signs of thrombi or vegetations, degradation of the cusps or position of the components such that function would be affected
- Safe implantable cardioverter defibrillator (ICD) removal
- Consideration should be given for the removal of the device in a manner that avoids electric shock to the mortuary staff but enables data to be collected that may assist in determining the cause of death (J Forensic Sci 2022;67:1924, Circulation 2018;137:2730)
- Most mortuaries will have local management protocols available for safe removal; optimally, the device should be electronically inactivated by transcutaneous programming but this requires a device specific programmer
- ICD magnet placed over the device generator will disable all antitachycardia therapies as well as prevent electrical noise from being recorded by the device; if neither is available and delaying the autopsy is impossible, 2 layers of rubber or plastic gloves have been shown to provide sufficient protection in laboratory models (Europace 2009;11:1317)
- Once deactivated, free the generator from its subcutaneous pocket (identified by the scar from insertion) and use a wrench to unscrew the leads; this deactivates the ICD, which can then be sent to a cardiac physiologist for assessment
- Cardiac conduction system
- Indicated for deaths considered compatible with sudden cardiac death where no other cardiac cause has been identified
- Most commonly, the region of the atrioventricular node is dissected and assessed microscopically; the node is removed by opening the right atrium and ventricle and cutting out a square of tissue of the interatrial and IVS between the foramen ovale and coronary sinus, including the anterior leaflet of the tricuspid valve
- Sinoatrial node is less often dissected; the node is removed by opening the posterior surface of the superior vena cava (SVC) and cutting out a square of tissue around the junction of the SVC and the base of the right atrial appendage
- Consider involving a cardiac pathology specialist when complex cardiac problems are anticipated; they may prefer the heart fixed and sent whole or advise on additional investigations prior to review
- Fixed versus unfixed
- Advantage of not fixing the brain prior to examination is that the return of the complete body is not delayed; a fixed brain provides the ability to complete an examination in finer detail with better photography and histology (including immunohistochemistry), which allows for better specialist neuropathological outcomes
- Weight should be taken and excess blood removed prior to fixation
- There are many methods to fix the brain
- It can be suspended upside down in a large bucket of 10% buffered formalin for at least 4 weeks; suspension methods include resting in a hairnet or with the basilar artery tied with string to the handles of the bucket
- Formalin should be intermittently replaced (an example routine would be after ~3 days, then every week); high strength formalin (37%) can be used
- Short fixation period (1 - 4 days) may be useful in some circumstances as a compromise (J Clin Pathol 2013;66:50, J Clin Pathol 2006;59:393)
- Special techniques and protective equipment are required for any brain that could harbor prion disease; mostly done in specialty departments with their own strict management protocol to reduce the risk of transmission to staff (J Clin Pathol 1993;46:193)
- Autopsy is still essential despite some value in postmortem radiology (PLoS One 2018;13:e0201434)
- In brief
- For routine work, the brain is removed from the skull, then the cerebellum and brain stem are separated from the cerebrum at the level of the midbrain
- Cerebellum is sectioned through the vermis then separated from the brain stem through the cerebellar peduncles
- Cerebellum is sectioned radially and the brain stem cranial to caudal
- Cerebrum is serially sliced into ~10 mm thick slices from anterior to posterior
- All slices are laid out in sequence for careful cleaning and then close inspection as abnormalities can be subtle
- Dissection of the arteries of the base of the brain
- Indicated for subarachnoid hemorrhage to identify aneurysm
- After the cerebellum and brain stem have been separated, the vessels of the circle of Willis and tributaries are lifted from the surface and penetrating small arteries are transected; leaving the transection of the most peripheral branches until all the central dissection is completed provides traction for easier dissection
- Removal of the brain and spinal cord in continuity
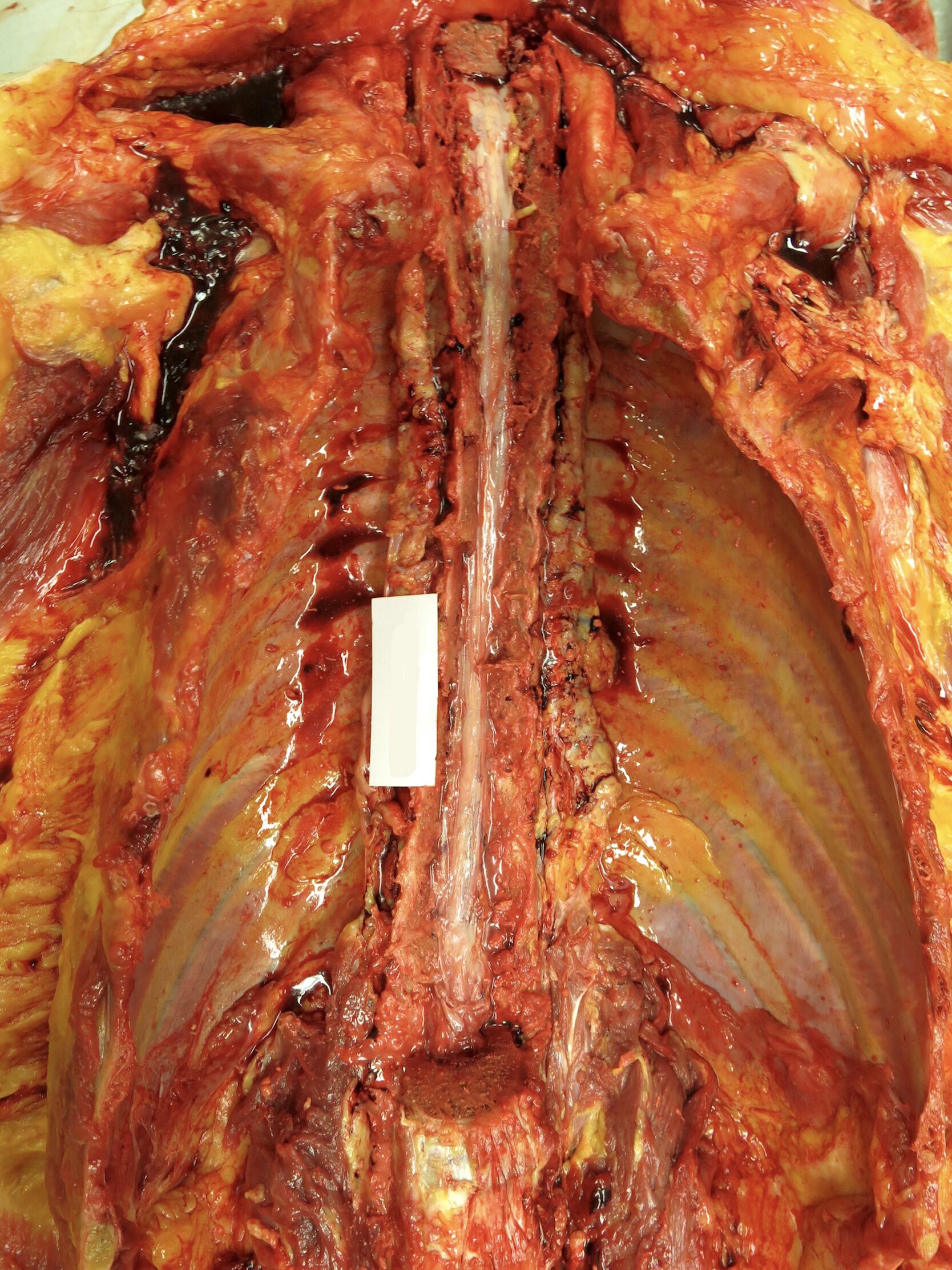
- Posterior incision is made from the occiput to the coccyx and soft tissue is dissected away from the bone
- Oscillating saw divides both laminae throughout the spine and the posterior column of the spine is lifted
- Dura is opened to expose the spinal cord, which is then dissected free from its nerve roots
- Once the brain has been exposed in the usual manner, a wedge of occipital bone must be removed in order to free the cerebellum from its dura, after which the spinal cord can be delivered upward through the foramen magnum
- If only partial examination of the spinal cord is required or for other reasons, an anterior approach is performed, the spinal column can be accessed anteriorly after organ removal (see Clinical images and Gross images)
- Oscillating saw divides the pedicles of the vertebrae on both sides and the anterior column of the spine is lifted
- Dura is either opened to expose the spinal cord or left intact and removed with the spinal cord, which is then dissected free from its nerve roots and removed from the spinal canal
- If the spinal cord taken is longer than several vertebrae, it is best fixed suspended by its caudal end to prevent it from curling
- See Gross images
- Indicated for circumstances of death suggestive of arterial injury, such as relatively minor neck trauma (e.g., sport, osteopathic manipulation, low speed motor vehicle incident, fall from standing height, unilateral blunt force injury to the mandible) with delayed sudden death or stroke symptoms prior to death
- Consider postmortem angiography as a guide to a site of suspicion or as an alternative to dissection (Forensic Sci Med Pathol 2023;19:135)
- Dissection can involve removal of the entire cervical spine en bloc with subsequent fixation and decalcification before examination or in situ identification of the artery as it traverses from its origin in the thorax, through the lateral pedicles of the inferior cervical spine to the posterior elements more superiorly
- This latter dissection requires significant time and skill and has a high rate of iatrogenic injury; access is gained through a posterior neck dissection as detailed below (J Clin Pathol 2006;59:1000, J Forensic Sci 2012;57:212)
- Indicated for investigation of trauma, origin of pulmonary embolus, upper limb venous obstruction or vasculitis
- SVC can be identified where it enters the right atrium once the breastplate has been removed; from here, the subclavian veins and internal jugular veins (IJV) can be traced and if indicated, opened longitudinally along their course
- Alternatively, the IJV can be identified at the time of neck dissection running in the carotid sheath (that also contains the vagus nerve and carotid artery)
- Indicated for investigation of trauma, origin of pulmonary embolus, lower limb venous obstruction or vasculitis
- Measure the widest part of both calves as part of external examination
- Several methods exist; one approach is made through a long vertical incision following the medial border of the tibia
- This incision is continued medially and horizontally at the level of the popliteal fossa superiorly and Achilles tendon inferiorly
- Skin and subcutaneous tissue is reflected
- Exposed calf muscle is removed and serially sectioned in the transverse plane to demonstrate the deep veins in cross section (Ann Vasc Dis 2016;9:15)
- Simpler method involves a transverse incision in the popliteal fossae, which can expose the veins in cross section; by milking the blood from the calf, any clots can be identified
- Large veins in the pelvis can be identified once the abdominal and pelvic organs have been removed; the common iliac vein will have been transected and the large veins can be opened longitudinally along their course both within the pelvis (internal iliac vein) and at their entry point through the femoral canal (external iliac vein)
- Most commonly indicated in pediatric nonaccidental injury cases (Leg Med (Tokyo) 2003;5:S288)
- Do not aspirate vitreous humor prior to examination as the retina may be damaged
- Several methods exist
- One approach is to remove a flap of bone from the anterior cranial fossa with an oscillating saw; the orbital contents are carefully separated from the surrounding bone circumferentially both anteriorly to meet the conjunctiva and posteriorly to include the optic nerve
- Further dissection of the eye is best done after fixation in formalin (at least 48 hours is usually recommended)
- See Clinical images
- Most commonly indicated for systemic sepsis of unknown cause
- Methods range from simple (but destructive) removal of the bone overlying the middle ear (tegmen tympani) to en bloc removal of the middle ear requiring decalcification prior to sectioning with an oscillating saw
- One example is Cobbler's Cut technique (J Forensics Res 2014;5:2)
- For the simplest method, once the brain has been removed and dura stripped from the middle cranial fossa, chip the bone overlying the middle ear off with a chisel; the area of interest is located posterior and lateral to the foramen spinosum (transmits the middle meningeal artery) and anterior to the ridge of the petrous temporal bone
- This will provide access to sample any fluid for microbiology but fine anatomical detail will be lost
- See Clinical images
- Each part of a postmortem should be considered as essential to justify its intrusiveness; therefore, one must weigh the value of facial dissection versus the ability to reconstruct the face or compromise the embalmer's ability to access facial vessels, especially given the value of postmortem radiology
- Most commonly indicated for assessing trauma to the face
- Standard Y incision of the anterior body can be used by continuing to reflect the skin and subcutaneous tissue with the skin carefully reflected upward, exposing the face; alternatively, a high Y incision can be used
- Depending on the level of inspection required, examination can be limited to the bones of the jaw and facial skeleton, leaving the oral mucosa attached and without breaching the oral cavity; alternatively, it can be extended further upward (including the removal of the eyes in continuity allowing for examination of the bony eye sockets) if necessary
- Complete after brain and thoracic organs have been removed to reduce pressure within blood vessels that may lead to artefactual bleeding within tissues (Acad Forensic Pathol 2016;6:45)
- Anterior approach is commonly done in daily practice to assess injury to the neck structures, including if sustained pressure to the neck as a cause of or contributor to death (see Asphyxia)
- Similar to facial dissection, the standard Y incision of the anterior can be utilized by continuing to reflect the skin and subcutaneous tissue upward, exposing the neck; alternatively, a high Y incision can be used
- Then, each layer of muscles (platysma, then sternocleidomastoid, then the strap muscles) is separated at their caudal attachments and reflected upward for assessment
- IJV and common carotid arteries can then be opened longitudinally to assess for intimal tears
- Tongue and neck are then removed en bloc for further dissection
- Precervical fascia and underlying cervical spine can now be seen and any abnormalities are exposed
- Tissue bloc is further assessed on the bench by opening the cervical esophagus posteriorly, separating the thyroid for further sectioning, completely separating and stripping the hyoid bone for close inspection (and photography) and opening the larynx
- Document (including photographs) any surface or tissue hemorrhage, deformation or fractures in any structures; the interpretation of possible injuries can be controversial and should be approached with caution (Acad Forensic Pathol 2016;6:45)
- Posterior approach is used to document injury to the soft tissues of the back of the neck including subcutaneous bruising or to access to the vertebral arteries in the upper cervical vertebrae (as described above); several methods exist (Kitulwatte: Dissection Technique of the Posterior Neck and Vertebral Arteries [Accessed 16 June 2023])
- One approach is with an inverted T incision with the horizontal aspect extending over the scapula
- After the skin and subcutaneous tissue are reflected, the muscle groups can be reflected laterally; these muscles are typically divided into superficial (trapezius), intermediate (splenius capitis, splenius cervicis and semispinalis capitis) and deep (deep paraspinal and deep subcapital muscles) groups
- Once removed, the extracranial vertebral artery and spinous processes of the atlas and axis will be seen along with the important atlantoaxial and atlantooccipital ligaments
- See Clinical images
- Usually well visualized on postmortem radiology (Leg Med (Tokyo) 2016;18:25)
- Once the subcutaneous tissues have been reflected from the anterior thorax, create a pool of water inside the pocket formed between the reflected tissues and lateral chest wall
- Insert an instrument underneath the water surface between the ribs and into the pleural space; if gas is released under pressure, a pneumothorax could be considered
- In the setting of a limited postmortem, a needle thoracostomy is performed similarly to those done with live patients (a large needle attached to a 50 mL syringe partially filled with water and aspirated in the second intercostal space midclavicular line in a supine patient) and could yield evidence for the presence of a pneumothorax
- Decomposition can produce gas in the chest so care must be taken in the interpretation of gas released in this setting
- Findings should be considered along with other signs of clinically significant pneumothorax, such as circumstances of death and other autopsy findings including mediastinal shift, hemithorax volume changes and lung bullae
- Indicated for pulmonary barotrauma / cerebral artery gas embolism (PBT / CAGE) diving fatality where there has been a rapid ascent and rapid loss of consciousness after resurfacing; venous air embolism may occur secondary to trauma, iatrogenic causes (intravenous lines, cardiopulmonary bypass, neurosurgery or gas assisted surgery or endoscopy), childbirth, abortion or rarely from criminal intervention
- For a diving fatality, postmortem imaging must be completed within 8 hours of death due to decomposition or off gassing
- Off gassing is where nitrogen that has been absorbed into the tissues with diving forms bubbles in the tissues and vessels if the diver ascends rapidly and dies or dies on the bottom and is rapidly brought to the surface
- This will result in gas artifact that is difficult to differentiate from pulmonary barotrauma and cerebral air gas embolism as a cause of death (J Clin Pathol 2006;59:489)
- For demonstration of gas in the heart, the anterior pericardium is carefully opened and the pericardial space is filled with water; the right and left ventricles are penetrated under the water's surface to assess for the presence of gas
- In order to be sure not to disturb the great vessels, the upper third of the sternum can be left intact until the testing is completed (Ulus Travma Acil Cerrahi Derg 2019;25:311)
- Significant venous air embolism is ~100 - 250 mL but is much less when arterial
- Demonstration of gas in the cerebral circulation is best seen with postmortem radiology prior to dissection as artefactual introduction of gas into the cerebral vessels is common
- Bubbles within the vessels of the circle of Willis and deep arteries of the brain might provide evidence for nonartefactual cerebral gas if the brain has been removed after careful clamping of both of the internal carotid and vertebral arteries; however, this is fraught with difficulty and should be interpreted with caution (Am J Forensic Med Pathol 2018;39:61)
- Gas can be produced during tissue decomposition, so care must be taken with the interpretation of gas in this setting
- Indicated for checking the patency of the biliary system in the setting of malignancy, systemic sepsis, trauma or after adjacent abdominal surgery
- Several methods exist
- Can be dissected with the organs in situ or from the posterior aspect after the abdominal organs have been removed as a block
- One approach identifies the ampulla of Vater in the duodenum, which is then probed and opened longitudinally to its insertion into the gallbladder and common bile duct
- May be aided by the cannulation of the biliary system and injection of dye (such as methylene blue) or with the assistance of a suitably experienced surgeon
- Commonly indicated in cases of homicide for evidence of blunt force injury to determine age of injuries as circumstances of death
- Possible bruising should be sampled for histology to confirm
- Reflection may be done in layers, with sequential reflection of the skin, fat and muscles
- Routine anterior body incision will enable assessment of the anterior trunk
- Posterior trunk can be dissected through a midline posterior longitudinal incision, which can be carried over the back of the buttocks if limb examination is also required
- Limbs should have a longitudinal incision on the posterior surface for best reconstruction results (Forensic Sci Int 2018;284:85)
- Photography of bruising may be enhanced with ultraviolet light
- Curved skin incision is made around the area with the needle puncture mark and the skin and subcutaneous fat are reflected to demonstrate the underlying vessel
- In some cases, the puncture mark is obvious (marks may be hidden by cigarette burns or tattoos) and macroscopic assessment of the perivascular tissues for fibrosis can be made
- Cross sections of the vessel and adjacent soft tissue can be submitted for histology and surrounding subcutaneous tissues sent for toxicological testing
- If sending tissue for toxicology, control specimens should be taken from the opposite side of the body and sent in a separate container
- See Clinical images
- Consider involving the local jurisdiction specialist in sexual assault to attend the autopsy to assist with interpretation of possible injuries and the taking of samples
- Prior to any instrumentation or dissection any samples needed for evidentiary purposes (sexual fluids or DNA) must be taken to avoid potential contamination (Acad Forensic Pathol 2018;8:912)
- Lithotomy position may assist in examination and dissection
- Speculum examination is completed as per the local jurisdiction protocols for sexual assault and is similar to that completed on a live victim
- Several methods exist for the dissection of the vagina / rectum
- Traditionally, the routine anterior body incision is continued inferiorly to pass over the pubic symphysis and surround the vagina / rectum
- Pubic bones are sawed through ~5 cm on either side of the pubic symphysis and the tissues are separated away from the inner surface of the pelvic brim until the pelvic contents can be removed en bloc
- Tissue is fixed in formalin before dividing in the sagittal plane for assessment of the vagina / rectum
- This pelvic exenteration is disfiguring and consideration should be given to less invasive approaches where possible
- Less destructive technique involves making an elliptical incision around the external genitalia, meeting anteriorly to the clitoral hood anteriorly and posteriorly to the anus posteriorly, extending laterally at approximately the level of the labia majora
- This incision is continued into the deep pelvic tissues, following the contours of the inner aspect of the pelvis, to eventually communicate with the abdominal cavity; the entire tissue block including anus to rectum and vagina to uterus and ovaries can then be removed
- Lateral incisions from the anus to the cut end of the rectal stump and from the vagina, through the cervix and through the uterus can then be made and the entirety of the genital tract examined for injury
- Bladder is also opened and inspected
Opening of the skull and removal of the brain
Removal of the orbital contents
Full body autopsy, including the brain, with modified Virchows technique
Simple method to check patency of the biliary system
Dissection of the heart (after separation from the body)
Comment Here
Reference: Autopsy techniques
- 20 mL of air removed from the right ventricle can be considered as definitely causing death
- Any bubbles within the circle of Willis can be considered as definitely causing death
- Consideration of the interval between death and postmortem is unimportant
- For a diving fatality, postmortem imaging must be completed as soon as possible but definitely within 8 hours
Comment Here
Reference: Autopsy techniques
- Heart dissection is a medical procedure whereby a pathologist examines and dissects the heart of a deceased individual to determine the cause of death or any underlying heart conditions
- Cardiovascular disease accounts for most natural deaths in the medical examiner / coroner's office
- Multiple heart dissection techniques exist
- Each dissection technique allows for examination of specific heart regions or disease
- Short axis: the heart is dissected into thin slices perpendicular to its long axis, allowing for a detailed examination of the cross sectional anatomy of the heart
- Blood flow (or inflow - outflow): the heart is dissected following the path of blood
- 4 chambers: the heart is dissected to expose its 4 chambers
- Base of the heart: the heart is dissected to expose the valve plane
- Initial dissection: separate the aorta and pulmonary artery from the other vessels at the base of the heart, cutting the intervening connective tissue
- Right atrium: cut anteriorly from the inferior vena cava (IVC) opening to the tip of the right atrial appendage
- Alternatively, dissect along the posterior atrial wall between the IVC and superior vena cava (SVC)
- Both methods will allow for preservation of the sinoatrial node that lies on the lateral margin of the junction of the SVC with the right atrium and the atrial appendage along the crista terminalis (sulcus terminalis - terminal groove) (see image 1)
- Right ventricle: place the scissors or blade within the right atrial cavity and move through the tricuspid valve; keep the blade along the right ventricle's lateral margin (free wall) and make a single, continuous dissection to the cardiac apex (see image 2)
- Right ventricle outflow tract: once the right ventricular cavity is opened, extend the dissection from the apex upwards through the pulmonary outflow tract (pulmonary conus, valve and artery)
- Placing the scissors or the blade parallel to the interventricular (IV) septum will decrease the chance of cutting through one of the cusps of the pulmonary valve (see image 3)
- Left atrium: an easy way to open the left atrium is by dissecting between the pulmonary veins' orifices
- If the pulmonary veins need to be spared, make a hole in the left atrial appendage and extend the dissection to the orifice of the pulmonary veins (see image 4)
- Left ventricle: place the scissors or blade within the left atrial cavity and move through the mitral valve; keep the blade along the lateral margin of the left ventricle and make a single, continuous dissection to the cardiac apex (see image 5)
- Left ventricle outflow tract: once the left ventricular cavity is opened, the dissection needs to be extended along the IV septum between the apex and the aortic valve (AV)
- If the AV cusps are not relevant in the specific case, placing the scissors or the blade perpendicular to the IV septum will decrease the chance of cutting through one of the AV cusps
- If the AV cusps need to be spared, the safest way is to check them from the aortic root by cutting the aorta up to ~0.5 - 1 cm above the AV plane
- When the AV cusps are exposed, place the scissors between the cusps and make a dissection in the direction of the IV septum (see image 6)
- This dissection can be extended from the AV plane to the apex
- Alternatively, after a dedicated dissection has secured the cusps, the left ventricle outflow tract can be opened by dissecting from the apex toward the AV, joining the previous AV dissection
- Final dissections: once all chambers of the heart are opened, the right and left ventricles wall can be sliced by partial thickness sections from the endocardial surface, to allow examination of the myocardium
- Papillary muscle should be dissected to assess for any abnormalities
- Most common heart dissection technique used in forensic autopsies
- Initial dissection: multiple transverse cuts are performed, 0.8 - 1.5 cm thick from the cardiac apex to the base, parallel to the atrioventricular groove (which demarcates the borders of the underlying atria from the ventricles) (see image 1)
- Dissection should be stopped just below the apical papillary muscles to preserve the valve
- Heart should be kept as still as possible to avoid irregular sections or dissection artifacts; placing a paper towel beneath the organ may help
- Slices can then be placed on the board and examined (see image 2)
- Remaining specimen: once the transverse sections have been made, the heart can be dissected following the blood flow method described above
- Initial dissection: dissect the ventricles following the short axis method described above
- Right atrium: place the scissors into the IVC and dissect along the free wall of the right atrium to the tip of the right atrial appendage and the upper aspect of the atrial septum adjacent to the ascending aorta; leave ~1.0 cm distance from the tricuspid valve plane
- Left atrium: locate the coronary sinus ostium and dissect from the right atrium along the outer wall of the coronary sinus in the left atrioventricular groove
- Once the left atrium free wall is reached, extend the dissection from the lower aspect of the atrial septum to the level of the left atrial appendage and the upper border of the atrial septum, meeting the previous dissection from the right atrium
- Dissect through the atrial septum to remove both atria
- Aorta and pulmonary artery: transect the great vessels at the level of the valve commissures
- Trim the soft tissues as needed to expose the aortic and pulmonary valves
- If the left circumflex (LCX) and the right coronary arteries have not yet been examined, it is not possible to dissect them easily
- Initial dissection: the heart is placed with the anterior aspect facing the operator; the first cut can be done in 2 ways using a long blade sharp knife
- First way: dissect from the heart base to the apex
- Using the fingers through the atrial cavities and atrioventricular valves (mitral and tricuspid), to locate and palpate left and right free ventricular walls
- Superficial cuts can be made on the external aspect of the organ at the level of the left and right ventricular walls as a guide
- Place the blade between these 2 cuts (or approximately in the middle of the right and left ventricular walls)
- Place the free hand palm on the anterior aspect of the heart and make a single, continuous cut moving from the base to the apex, dissecting the right ventricle, the left ventricle and the IV septum
- Second way: dissect from the heart apex to the base
- Starting from the cardiac apex, the dissection is extended along the acute margin of the right ventricle, the obtuse margin of the right ventricle and the IV septum
- During the dissection, the operator can check if the cut is oriented in the right direction
- First way: dissect from the heart base to the apex
- Remaining specimen: once the heart is bisected into 2 halves, all 4 chambers should be visible; the remaining unopened portions (bilateral ventricular outflow tracts) can be opened following the blood flow method described above
- Most common coronary dissection technique
- Locate the coronary arteries on the epicardial surface
- Separate the aorta and pulmonary artery from the other vessels at the base of the heart, cutting the intervening connective tissue to locate the left common coronary artery (see image 1)
- Make an initial transverse section at the left common coronary origin level
- Then move distally to find the vessel bifurcation
- Follow the left anterior descending (LAD) coronary artery path, making serial 0.3 cm thick cuts perpendicular to the main axis of the vessels, up to the most distal part (see image 2)
- After examining the LAD coronary artery, move back to the left common coronary artery bifurcation and follow the LCX coronary artery, which travels laterally just below the left atrial appendage
- If needed, the soft tissue below the left atrial appendage can be superficially trimmed to allow a more accessible examination of the LCX coronary artery
- Follow the LCX coronary artery path, making serial 0.3 cm thick cuts perpendicular to the main axis of the vessels, up to the most distal part (see image 3)
- Place the heart with the anterior aspect facing the operator and the apex facing inferiorly
- Rotate the heart ~45 degrees counterclockwise and make a straight cut at the level of the adipose tissue surrounding the lateral ascending aorta
- This should expose the right coronary artery, which travels just below the right atrial appendage
- Follow the right coronary artery path, making serial 0.3 cm thick cuts perpendicular to the main axis of the vessels, up to the most distal part (see image 4)
Longitudinal dissection
- Can be done in young subjects when there are no concerns for coronary diseases
- Serial sectioning is still the preferred method
- Locate the coronary arteries' ostia at the level of the aortic valve
- Using dedicated vascular coronary scissors, place the blunt tip within the ostium and the sharp tip outside the vessel and extend the dissection as distally as possible
- If stenosis or atherosclerotic plaques are encountered during the dissection, do not push the blunt tip forward to avoid creating artifacts or removing potential plaques or thrombi
- Instead, stop the longitudinal dissection and perform a local serial section to evaluate the grade of lumen stenosis
Removal of the coronary arteries from the heart
- Useful in case of severely atherosclerotic and calcified vessels
- Rarely necessary in the forensic setting
- This method will produce artifacts to the epicardial surface of the heart, which are expected and cannot be avoided
- Using scissors with blunt tips, make a small cut just beneath the origin of the left anterior coronary artery (see image 1)
- From there, dissect along the posterior aspect of the vessel, following its pathway up to the most distal part (see image 2)
- If a tract of the coronary artery is accidentally transected, proceed with an extra deeper cut along the posterior aspect of the vessel
- Use the same technique to remove the LCX and the right coronary arteries (see images 3 - 4)
- Once the coronary arteries have been removed, they can be placed on the board (see image 5)
- Serial transverse sections at 2 - 3 mm intervals are made to evaluate for lumen stenosis, thrombosis or other abnormalities (see image 6)
- Dissect the heart after formalin fixation using the 4 chamber technique; in case of pathologic findings, consider further testing
- Dissect the heart after formalin fixation using the base of the heart method technique; in case of pathologic findings, consider further testing
- Dissect the heart after formalin fixation using the short axis technique; no other tests are needed
- Dissect the heart fresh following the blood flow; no other tests are needed
- Dissect the heart fresh using the 4 chamber technique; in case of pathologic findings, consider further testing
Comment Here
Reference: Forensic heart dissection
- Do not perform an autopsy, collect blood samples during the external examination and run an expanded toxicology panel; once you get the results, you can sign out the case accordingly
- Perform the autopsy and save the heart in formalin for examination once fixed; run genetic tests and expanded toxicology
- Perform the autopsy, dissect the coronary arteries using the serial sectioning method and run expanded toxicology
- Perform the autopsy; since he is young and has no history of coronary disease, dissect the coronary artery using the longitudinal dissection method and run expanded toxicology
- Sign out the case as probably cocaine and amphetamine toxicity and accident
Comment Here
Reference: Forensic heart dissection
- Blunt object: an object that has a wide, dull or convex surface with rounded edges or corners; does not possess any pointed or sharp edges
- Blunt force injuries: produced by blunt objects due to different possible mechanisms
- Moving blunt object impacting against a resting body
- Moving body impacting against a resting blunt object
- Moving body and a moving blunt object collide
- Body is trapped between 2 surfaces
- Many different objects can produce blunt force injuries
- Different objects may create similar injuries, so caution is needed when attributing a specific injury to a particular weapon or object
- Specific determination of the age of blunt force injuries is currently not reliable
- Distinguishing between antemortem and postmortem blunt force injuries is mandatory
- Resuscitation injuries can produce blunt force injuries and must be differentiated at the postmortem examination
- Kinetic energy:
- Energy possessed by an object due to its motion
- Function of the object's mass (M) and its velocity (V)
- KE = 1/2 MV2
- Impact dynamics:
- Impact refers to the physical force that develops during blunt trauma
- Elastic impact: after the impact, an object bounces, preserving its kinetic energy
- Plastic impact: kinetic energy is entirely or partially transferred to the body, leading to wound development; the vast majority of blunt force injuries have a plastic impact dynamic
- Inertia:
- Property of a body to resist changes in velocity
- If velocity changes suddenly (e.g. acceleration / deceleration), there will be a more severe effect on the affected body
- Impacting surface features: blunt force injury's appearance depends on the composition, size and shape of the impacting object or surface (Postepy Dermatol Alergol 2013;30:302)
- Tissue properties:
- Elasticity and plasticity play an essential role in determining the wound features
- Allow for deformation in response to an applied force
- After deformation, elastic tissue can drive passive recoil and return to its initial state after the force's termination
- When the force exceeds the tissue resistance, then a wound occurs
- Size of the involved area:
- Large body areas will disperse more energy, lessening the injury to the tissue
- Focal or curved areas concentrate the energy from the impact on a limited area, resulting in more severe damage
- Chronology of the impact:
- Slow, gradual forces cause a progressive compression and the energy can be slowly absorbed, resulting in minor damage
- Rapid or sudden forces result in a rapid transfer of energy to the body, frequently exceeding tissue resistance and producing more severe injuries
- Energy transfer: injuries can develop in body areas far from the point of impact due to the transfer of energy within the body (e.g. ring fracture of the skull in a subject who falls from a height and hits the ground with the sacrum)
- Skin injury consisting of the traumatic removal or detachment of the epidermis due to friction (shearing) or pressure (crushing) mechanisms
- Tangential abrasions: a lateral rubbing mechanism that scrapes off the superficial layers of the skin; epidermal shreds (skin tags) can be present and may suggest the impact's direction, although this phenomenon does not always occur
- Linear abrasions: caused by a sliding movement of a narrow object on the skin, which results in superficial epidermis denudation; typical examples are fingernail abrasions that can be observed in manual or ligature strangulations (Am J Forensic Med Pathol 1981;2:45, J Clin Forensic Med 2003;10:255)
- Brush abrasions: caused by the body's frictional movements against a wide, rough surface or object, leading to scraping of the epidermis; usually wider at the starting point and narrower at the end (e.g. "road rash" in traffic accidents) (J Clin Forensic Med 2003;10:255)
- Compression abrasions: direct pressure from a blunt object together with slight rubbing movements produce skin and epidermal crushing
- Patterned abrasions: these injuries show a distinct pattern that may reflect the shape of the impacting blunt object; frequently observed in tortures (Forensic Sci Int 2018;284:85)
- Typically occur when the force is applied at or near perpendicular to the skin surface and can be classified as:
- Impact abrasions: occur when a force is applied suddenly or rapidly and perpendicular to the skin, pushing and crushing it on a body surface
- Pressure abrasions: occur when there is a slow, prolonged compression of the skin by a blunt object, which results in a dried, parchment-like abrasion (e.g. hanging mark)
- Typically occur when the force is applied at or near perpendicular to the skin surface and can be classified as:
- Nonpatterned abrasions: abrasions that don't resemble the producing object
- Patterned abrasions: these injuries show a distinct pattern that may reflect the shape of the impacting blunt object; frequently observed in tortures (Forensic Sci Int 2018;284:85)
- Differential diagnosis in abrasions:
- Antemortem abrasions (with survival interval):
- Usually dark red or red, covered with a dark scab and showing signs of healing
- Inflammatory cell infiltration, evidence of hemorrhage or granulation tissue are histologic signs of vitality (Clin Dermatol 2007;25:39)
- Postmortem abrasions:
- Several mechanisms can produce abrasions in the postmortem period (autopsy procedures, insect activity, body dragging on a rough surface, etc.)
- Usually orange-yellow or brown with a parchment appearance (J Forensic Leg Med 2014;26:10, Am J Forensic Med Pathol 2009;30:84)
- Antemortem abrasions (with survival interval):
- Dating of abrasion: despite recent research describing possible morphological features to establish an abrasion's age, it is extremely difficult to reach reliable conclusions based on the morphology of the injury (Am J Forensic Med Pathol 2017;38:167)
- A contusion results from crushing or tearing of the dermis and subcutaneous tissues without breaking of the skin; the applied force causes blood vessel rupture, leading to variable bleeding in the subcutaneous space
- Locations: contusions can develop on the body surface as well as on internal organs
- Terms:
- Contusion: lesion that can happen anywhere in the body
- Bruise: lesion visible on the skin surface
- Ecchymosis: lesion resulting from nontraumatic bleeding, such as medical therapy (e.g. intravenous injection) or senile ecchymoses
- Petechia: small, pinpoint hemorrhage due to acute rise in venous pressure (congestion) leading to capillary rupture (e.g. from asphyxia)
- Hematoma: large collection of extravasated blood (e.g. from traffic accident)
- Patterned contusions:
- Linear contusions: when a rectangular shaped object strikes the body
- Tram-like or railway line contusions: when a cylindrical or rod-like object hits the body, the blood accumulates laterally to the point of impact, creating an injury that appears pale in the center, lined by 2 linear, parallel bruises on each side (Forensic Sci Med Pathol 2017;13:508)
- Loop contusions: when a cable or cord-like item strikes the body, frequently seen in child abuse (Paediatr Child Health 2013;18:433)
- Fingertip contusions: a cluster of small round bruises, approximately 1 cm in diameter, develops when the offender grips a victim's body area vigorously
- Most frequently involved body area is the neck
- Sometimes, a single, larger, oval or round bruise on the opposite side of the clustered fingertip contusions may also be present (thumb-like bruise) (Pediatr Emerg Care 2019 Jan 7 [Epub ahead of print])
- Intradermal contusions: when an object with grooves or ridges hits the skin, producing an injury limited to the subepidermal layer (e.g. tire marks, shoe marks) (J Forensic Sci 2007;52:1050, Forensic Sci Int 2020;2:521)
- Suction contusions: confluence of multiple petechiae in a circumscribed area due to a vacuum-like mechanism, which leads to capillary rupture and blood leakage in a circumscribed body area (Oral Implantol (Rome) 2016;8:68)
- Coup / contrecoup contusions: contusions that develop at the point of impact (coup) and on the side opposite the impacted area (contrecoup); typically observed on the brain (Neurocrit Care 2004;1:385)
- Human bites: typical bruise resulting from human bites shows 2 opposing arches separated by a central pale, uninvolved area with possible associated abrasions and lacerations (J Forensic Odontostomatol 2014;32:1)
- Dating of bruises:
- Red blood cells and hemoglobin degradation lead to pigment formation and chromatic changes of the bruise, generally from red / purple to green to yellow-brown
- Chromatic changes have been studied to estimate the age of the bruise
- Consistent gross or histological dating of contusion is not reliable
- With the current knowledge, it is reasonable to state that a yellow colored bruise may have been produced > 18 hours before the examination
- Absence of yellow color does not mean < 18 hours
- Recommended to describe them just as recent or old (Forensic Sci Med Pathol 2007;3:241)
- Differential diagnosis in contusions:
- Antemortem contusions: contusions are a vital phenomenon; can affect any body area, are usually unilateral and asymmetrical, are commonly associated with tissue swelling, show different colors in the same subject, do not become pale on digital pressure and show a cellular reaction microscopically
- Livor mortis: lividity is usually bilateral and symmetrical, uniform in color, shows pallor on digital pressure (if recent), is preferentially located in the dependent portions of the body with no cellular reaction at the microscopic examination (Am J Forensic Med Pathol 1998;19:46)
- Tardieu spots: small postmortem hemorrhages that develop in areas of intense lividity (also called hypostatic hemorrhages) (Am J Forensic Med Pathol 2009;30:322)
- Laceration occurs when a blunt force causes skin compression, crushing and splitting; lacerations frequently occur on the skin overlying bony prominences but can also affect the internal organs, leaving the skin intact
- Hallmark: presence of tissue bridges in the depth of the wound is the pathognomonic feature for lacerations; also helps to distinguish them from an incised wound (sharp force injury)
- Edges: laceration edges are usually jagged; abrasions, bruising and crushing of the margin are frequently observed
- Types of lacerations:
- Tear lacerations:Â classic form of laceration occurring when a blunt force impact rips and tears the skin and the subcutaneous tissues
- Split lacerations: compression of the skin between blunt object and bone
- Stretch lacerations: blunt trauma that causes an overstretching of the skin until it ruptures
- Crush lacerations: blunt trauma that causes grinding and compression of the skin and soft tissue, resulting in possible amputation
- Degloving injury: blunt mechanism that occurs when the skin and subcutaneous tissues are trapped between 2 hard surfaces and are suddenly pulled at the moment of the impact, resulting in minimal to extensive loss of skin and soft tissues (Rom J Leg Med 2013;21:165)
- Avulsions: violent blunt trauma that tears away the tissues from their attachments
- Direction of the impact: sometimes the presence of an abrasion surrounding a laceration may suggest the direction of the impact; abrasion is usually wider at the point of impact
- Undermining: impact is over the bone, resulting in a clean separation of the skin from the underlying bone in the direction of the application of force
- Dating of lacerations: estimation of the age of a laceration is not reliable
- Differential diagnosis:
- Incised wounds: sharp object (such as a knife) produces incised wounds (or cuts) that are typically longer than deeper due to the blade's sharpness and the sharp force related mechanism of injury; incised wounds lack tissue bridges; edges are usually sharply demarcated
- Bone lesions that occur when the intensity of the blunt force exceeds the bone resistance
- Types of fractures (Acad Forensic Pathol 2016;6:463):
- Traumatic:Â typical fractures due to a blunt force trauma
- Pathologic: fractures due to a pathologic condition (e.g. osteoporosis, bone metastasis, etc.)
- Direct: fractures that occur at the point of impact
- Indirect: fractures that occur away from the point of impact due to energy transfer
- Open (compound): direct communication between the fracture and the external environment
- Closed:Â the fracture lies underneath intact skin
- Complete:Â the bone is separated into 2 or multiple parts
- Incomplete:Â the bone cracks but does not separate
- Biomechanisms of fracture:
- Long bones:
- Compression:Â leads to an internal shortening of the bone
- Traction:Â when a tension force pulls the bone apart
- Shear: when a force acts parallel to the bone, resulting in a fracture parallel to the force's direction
- Torsion (spiral):Â when the bone is twisted; typically observed in child abuse (tibial fractures)
- Bending:Â when the bone is compressed on one side on its axis, creating tension on the opposite side
- Skull: following a blunt force injury to the head, the area of impact temporarily bends inward while there is a compensatory distortion of surrounding areas; when the intensity of the impact exceeds the skull resistance, fractures develop
- Linear:Â usually resulting from the impact of the head against a large surface; can develop on the cranial vault or on the bases and can be single or multiple, sometimes intersecting
- Depressed:Â break of the bone, which is pushed inward at the point of impact, producing a permanent focal depression of the skull; usually results from a blunt object with a limited surface striking the head (e.g. hammer) (Med Sci Law 2015;55:44)
- Ring:Â fracture encircling the foramen magnum resulting from the transmission of energy over the bone from the impact point to a distant site
- Diastatic: fracture involves and separates the cranial sutures (common in children)
- Combined:Â combination of the mechanisms described above
- Long bones:
- Basilar skull fractures: delayed bruises may follow cranial base fractures but they should not be considered definitive evidence of a specific cranial base fracture
- Anterior cranial fossa fracture:Â conjunctival, palpebral or periorbital bruises (raccoon eyes) with or without liquorrhea or bleeding from the nose (J Neurosci Rural Pract 2018;9:370)
- Middle cranial fossa fracture:Â bruising visible behind and below the ear at the mastoid process (Battle sign) or bleeding from the ear (StatPearls: Battle Sign [Accessed 8 February 2021])
- Posterior cranial fossa fracture:Â Battle sign or pharyngeal bruises / hematomas
- Commotio cordis: cardiac concussion in which a blunt impact to the precordium leads to a cardiac rhythm disorder in the absence of structural heart damage (Leg Med (Tokyo) 2019;38:73, Med Sci Law 2017;57:146)
- Acceleration / deceleration injuries:
- Typically observed in motor vehicle collisions
- Rapid deceleration results in differential movements among adjacent structures, resulting in the tearing of visceral organs, ligaments and vascular pedicles
- Internal organs are also crushed between the anterior abdominal wall and the spine or posterior chest, leading to severe parenchymal lacerations
- Blast injuries (Philos Trans R Soc Lond B Biol Sci 2011;366:144):
- Typically observed in explosions
- Following the detonation, a shock wave (blast or pressure wave) propagates radially from the original point, acting as a blunt force when interacting with the body
- Lungs, middle ear (barotrauma), gastrointestinal tract and bones are the most affected body areas
- Chop lacerations:
- Injuries that show both blunt and sharp force trauma features
- Produced by a heavy blunt object with a sharp edge (e.g. cleaver)
- Typically show abraded and bruised edges with a clean separation of the margins and no tissue bridges
- Resuscitation injuries: cardiopulmonary resuscitation (CPR) or other procedures may result in physical injuries that can be hard to interpret during autopsy (J Forensic Leg Med 2015;33:39)
- Commonly observed injuries are:
- Bruises and abrasions on the scalp and face (e.g. use of a mask for resuscitation, intubation attempts, pinching of the nose during mouth to mouth resuscitations, etc.)
- Bruise and abrasions on the precordial region or the central chest area due to external compressions during cardiopulmonary resuscitation
- Rib and sternum fractures and soft tissue hemorrhages are commonly associated
- Laceration of the heart, lungs, pleura and pericardial sac may result from rib fractures
- Electrical burns from defibrillation, in the form of a rectangular, parchment-like, yellow-orange abrasion on the anterior chest
- Retinal hemorrhages have been rarely described in children following cardiopulmonary resuscitation (J Forensic Sci 2017;62:107)
- Commonly observed injuries are:
- 4 month old boy with a patterned abrasion of uncertain etiology (Forensic Sci Med Pathol 2009;5:324)
- 49 year old woman with diaphragm laceration due to cardiopulmonary resuscitation (J Forensic Sci 2016;61:1135)
- 90 year old man with an atypical patterned bruise on the forearm (Forensic Sci Med Pathol 2014;10:637)
- 92 year old man with a simple depressed skull fracture (Med Sci Law 2015;55:44)
- Severe degloving injury of the foot (Rom J Leg Med 2013;21:165)
- 3 cases of commotio cordis (Int J Legal Med 2005;119:88)
Contributed by Lorenzo Gitto, M.D., Robert Stoppacher, M.D., Serenella Serinelli M.D., Ponni Arunkumar, M.D. and Luigi Bonaccorso, M.D.
Comment Here
Reference: Blunt force injuries
Comment Here
Reference: Blunt force injuries
Comment Here
Reference: Blunt force injuries
- Focal injuries to the brain occurring at locations where brain tissue directly impacts against the inner skull / bony protuberances
- Bleeding is a result of the damage to the small caliber blood vessels (Handb Clin Neurol 2015;127:45)
- Contusions are observed where there is direct impact of brain against bony surfaces of the inner aspect of skull
- Can bleed into the cerebrospinal fluid (CSF), causing subarachnoid hemorrhage
- Coup contusion: contusion occurring at site of impact
- Contrecoup contusion: contusion at site separate from impact site
- Generally related to differential movement of brain within the skull, leading to contusion at areas of bony prominences
- Regions with highest frequency of contusions: orbital frontal, frontal and temporal poles, cortex near the Sylvian fissure
- More prevalent in males with ratios from 1.5:1 to 2.5:1 across the world (J Med Life 2015;8:272)
- Highest rate occurs between the ages of 15 - 24 years (PLoS One 2020;15:e0229489)
- 20 - 30% of the elderly who fall suffer moderate to severe injuries besides contusions and traumatic brain injury (WHO: Falls [Accessed 22 November 2022])
- A blow is defined as an impact to a head by a load delivered by a hard object
- Several classes are defined based on kinetic energy and the inertia (or movement) of the involved head:
- Blows producing small amounts of energy that slightly rotate the head
- Examples include lightweight objects such as stones
- Produce abrasions or lacerations of the scalp with or without subgaleal hemorrhage; no fractures or brain injury (J Neurotrauma 2012;29:19)
- Blows that produce more kinetic energy and approach the head at an equal or greater speed (Front Neurol 2015;6:89, StatPearls: Blunt Force Trauma [Accessed 3 March 2023])
- Examples include hollow steel pipes, police night sticks, beer bottles
- Deform the skull, which moves / impacts the brain underneath the impact site
- Single (or multiple) cone shaped lesions beneath the impact site, with the base at the skull and apex within brain parenchyma
- May present as a superficial lesion confined to the cortex or as a deeper lesion with more extensive hemorrhage
- Blows that happen in the course of falling (StatPearls: Blunt Force Trauma [Accessed 3 March 2023])
- Examples include striking the head on a table edge
- May show scalp abrasion or laceration, subgaleal hematoma and contusions, with or without skull fractures
- Hard to interpret without sufficient background information
- Blows with momentum greater than the inertia of the head (Front Neurol 2015;6:89)
- Examples include weighted pipes, two by fours, metallic baton, heavy duty flashlight, baseball bat
- Forces produced by the impact to the head approximate those of falls
- They deform the skull with or without fractures and may produce coup and contrecoup contusions or contrecoup contusions only
- May be difficult to interpret and should be interpreted within the context of witness accounts and scene inspection
- Blows where the velocity and mass of the object are much greater than the head or the fixed head is struck with an object with a much greater momentum
- Skull is shattered without any significant contusions
- Rare instances where the brain is thrown from the skull while still intact
- Miscellaneous
- Blows at the top of the head
- No surface contusions
- Produce pattern of internal cerebral trauma
- Acceleration type of injury to the centroaxial region of the brain within an enclosed cranium (Handb Clin Neurol 2015;127:45)
- Tangential blows to the head
- Blows at the mandibular condyles
- These lesions involve inner cerebral contusions to the corpus callosum, white matter hemorrhages, avulsions of the choroid plexus and hemorrhages into the tela choroidea
- Blows at the top of the head
- Blows producing small amounts of energy that slightly rotate the head
Brain contusions due to falls
- Tend to produce a contrecoup contusion, as the brain is in motion and then abruptly stops in the course of the fall
- Falls that impact the occiput of the head will have contrecoup contusions at the base of the skull (J Med Case Rep 2018;12:166)
- If impact is on the lateral side of the head, the contusion may be seen on the opposite surface but the impact site will most likely be cushioned by the shoulders so as to decrease its intensity
- Frontal impact contrecoup are uncommon (J Neurotrauma 2016;33:1034)
- Front of the cranium absorbs the energy produced by the impact → no dissipation of energy into the brain parenchyma
- Motor vehicle accident victims that are driven into windshields of their cars will most likely use their hands to protect themselves as a reflex, thus cushioning the impact
- Lateral falls will be cushioned by the shoulders absorbing all the energy
- Falls that impact the inferior portion of head (e.g., mandible), may produce contrecoup contusions at the vertex of the brain (Radiographics 2019;39:1571)
Gliding contusions
- Hemorrhagic lesions within parasagittal white matter in superior cerebral areas; frequently bilateral
- Accompany traumatic axonal injury (Arch Pathol Lab Med 1986;110:485, Front Neurol 2016;7:178)
Fracture contusions (Curr Neuropharmacol 2020;18:538)
- Fracture line produced by an impact injury can rub against the underlying brain parenchyma causing a contusion
- Typically associated with basilar skull fracture
Theories that explain the formation of contrecoup contusions
- Vibration theory (J Neurotrauma 2005;22:845)
- Impact to the skull creates vibrations that travel throughout the brain
- These vibratory waves hit the skull on the other side with a large magnitude, fracturing the skull and damaging the brain
- Transmitted force wave theory
- Wave generated by the impact can be strong enough to produce a vacuum at the impact point, leading to disruption of blood vessels, damage to the brain parenchyma and the contrecoup phenomenon (Arch Surg 1965;90:157)
- Brain displacement theory (Neurocrit Care 2004;1:385)
- Brain is mobile within the skull and thus its own momentum can lead to tearing of the brain from its own attachments thus causing damage
- Skull deformation theory (Nihon Hoigaku Zasshi 1993;47:387)
- Combination of brain displacement and skull deformation results in the brain being contused
- Pressure gradient theory
- Movement between the brain and a skull produces intracranial cavitation due to focal, nonuniform pressure gradient (Nihon Hoigaku Zasshi 1993;47:387)
- Rotational shear force theory
- Rapid rotations of the head generate shear forces throughout the brain and therefore have high potential to cause shear force induced brain tissue damage (Clin Sports Med 2011;30:19)
Dating contusions (Open Access Maced J Med Sci 2017;5:813)
- Early reactions
- Edema
- Starts within minutes of injury
- Increases within hours and plateaus over days
- Disappears within 6 days (Vet Pathol 2016;53:962)
- Hemorrhage
- Microscopically starts and expands within hours around perivascular areas
- Maximal accumulation is reached within 24 hours
- Intact red blood cells remain viable for 5 - 6 months postinjury (Forensic Sci Med Pathol 2008;4:187)
- Polymorphonuclear leukocytes
- Starts within hours of the injury
- May be visible for up to a month postinjury, with or without infection
- Degenerating neurons (Toxicol Pathol 2011;39:22)
- Appear within 2 hours
- Characteristic red neurons (= shrinkage, eosinophilic cytoplasm, pyknosis)
- Not very prominent neuronophagia (phagocytosis of dying neurons by microglial cells) may remain in the lesion
- Edema
- Macrophages and scavenger cells
- Start within 24 hours postinjury, plateau at 7 - 14 days and then decrease
- Become distended with fatty granules due to phagocytosis of red cells and degenerate cellular material
- Hemosiderin and siderophages
- Hemosiderin laden macrophages appear as early as 5 days postinjury and may last for years
- Due to iron containing residue of hemoglobin from degenerate red blood cells
- Hematoidin pigment
- Yellow-orange crystallized bilirubin derived from hemoglobin breakdown
- Appears 10 - 12 days postinjury
- Absorbed within a few months due to its high solubility
- May persist for years within hemorrhagic lesions (Blood 2014;124:2158)
- Intermediate and late reactions
- Vascular reactions (J Neuropathol Exp Neurol 1999;58:153)
- Angiogenesis starts 5 - 7 days postinjury and plateaus at 3 weeks
- Residual tissue is made up of a mixture of small and sclerotic vessels
- Astrocytic reaction
- Protoplasmic astroglial proliferation starts 4 - 5 days postinjury
- Fibrillary astroglial proliferation starts 7 - 10 days postinjury
- Eventually forms a glial scar (a focus of increased proliferation of glial cells)
- Believed to be a type of reactive gliosis to restore the blood brain barrier
- Vascular reactions (J Neuropathol Exp Neurol 1999;58:153)
- Collagen production and fibrosis (Stem Cell Res Ther 2014;5:122)
- Rarely occurs in the CNS as a reparative mechanism unless the injury occurred at the cortical surface or when many small vessels are involved
- Fibroblasts appear within a week and can persist for months and years
- Microscopically the lesion ultimately resembles an old infarct
- CT imaging (J Stroke 2017;19:11)
- Small foci of petechial hyperdensity involving the gray matter and subcortical white matter
- Large cortical or subcortical bleed
- Coup contusions (J Emerg Trauma Shock 2018;11:205)
- Classically, are found over the cerebral or cerebellar hemispheric surfaces, especially the gyral crests
- Earliest manifestation is a focal discoloration or bruise on the surface of the cortex, appearing as a cone with its base at the gray matter and fading into the white matter
- With the passage of time contusions undergo reparative changes, sometimes with parenchymal collapse and gliosis
- Contrecoup contusions (Pediatr Radiol 2014;44:S632)
- Occur at surface of gyri and spare the sulci
- Occur at sites distant from initial impact to the head (most frequently in orbitofrontal or temporal tip regions)
- Like coup contusions, they undergo reparative changes and parenchymal collapse / gliosis as time passes
- Older contusions have a sunken tan-brown lesion with a serpentine appearance that follows the crests of the gyri
- Differentiated from infarcts based on the following:
- They do not follow a particular vascular distribution
- Brain will adhere to dura if contusion is extensive or has been surgically manipulated
- Underlying white matter might show demyelination and pallor
- Gliding contusions
- Intraparenchymal hemorrhages within parasagittal cerebral white matter, typically with accompanying traumatic axonal injury (Arch Pathol Lab Med 1986;110:485)
- Fracture contusions
- Appear more like lacerations
- They follow fracture lines
- May involve multiple gyri
- Can be associated with abscess if the fracture passed through a paranasal sinus
- Appear more like lacerations
- Contusional tears (Curr Neuropharmacol 2020;18:538)
- Mostly seen in infants
- Infant's brain is largely made of water and encased within a malleable nonossified cranium
- Does not develop contusions but rather necrosis and hemorrhage in the subcortical matter, that might be mistaken for congenital cysts or artifacts
- Produces a slit-like lesion underneath the vertex of brain
- Mostly seen in infants
- Blow contusions that indent the skull might deform the underlying brain cortex, deep into the sulci instead of superficially on the gyri
- These blows are uncommon and mostly seen when a hammer is used to strike the head or in crush scenarios
- Contrecoup contusions produced by falls are almost always accompanied by coexisting injuries due to shearing and torsional forces (e.g., inner cerebral trauma, traumatic axonal injury) and subdural or epidural hemorrhages (Neurocrit Care 2004;1:385)
- Contusional tears can be a potential marker of nonaccidental trauma / child abuse or when an adult crushes a child during a fall (AJNR Am J Neuroradiol 2016;37:163)
The image shown above is that of a traumatic brain injury. Which of the following statements is true in reference to the lesions present?
- They always result in loss of consciousness
- They are most likely the direct result of a skull fracture
- They are the result of the differential movement of the brain inside of the skull in acceleration / deceleration head injury
- They are the result of uncal herniation
- They could never have resulted from closed head injury alone
Comment Here
Reference: Brain contusions
- 18 year old man who was struck in the head with a baseball bat
- 30 year old man with a history of trisomy 21
- 44 year old woman who struck her head on a tree while skiing and was lucid for 30 minutes before collapsing
- 55 year old man who fell off a ladder, striking the occipital skull
- 80 year old woman with progressive memory decline over the past 10 years who recently fell out of bed at a nursing home
Comment Here
Reference: Brain contusions
- Cause of death: natural disease or injury that led to physiologic changes resulting in death
- Acute event (e.g., motor vehicle collision, gunshot wound to the head, sudden death in previously healthy individuals)
- Chronic event (e.g., complications related to atherosclerotic cardiovascular disease, malignancy, etc.)
- Manner of death: circumstances surrounding death (how the death came about / how the injury or disease leads to death)
- Mainly based on scene investigation, interviews with next of kin, review of medical history / records, autopsy and ancillary studies (studies (toxicology, histopathology, vitreous chemistry, microbiology, etc.)
- Mechanism of death: immediate physiologic derangement resulting in death (e.g., hemorrhage, sepsis, asphyxia), which is not etiologically specific
- Accurate and timely determination of the cause and manner of death are important for many reasons, including for the benefit of the decedent's family, vital statistics, public health implications and the medicolegal system
- Cause of death (COD) is the natural disease or injury that led to physiologic changes resulting in death
- Manner of death (MOD) is the classification / categorization used for how the death came about
- MOD commonly has 5 categories:
- Natural
- Homicide
- Suicide
- Accident
- Undetermined
- Some jurisdictions have an additional MOD: therapeutic complication
- Medical examiner cases can also be pending further studies
- MOD commonly has 5 categories:
- Mechanism of death is the immediate physiologic derangement resulting in death (e.g. hemorrhage, sepsis, asphyxia), which is not etiologically specific
- COD and MOD are determined based on the circumstances of the death, examination of the body and ancillary studies as appropriate
- Accurate and timely determination of the cause and manner of death are important for many reasons, including for the benefit of the decedent's family, vital statistics, public health implications and the medicolegal system
- Medicolegal manner of death "homicide" stated on the death certificate has no direct bearing on criminal prosecution or insurance settlements
- Homicide and murder have not the same meaning
- "Murder" is used in criminal law matters but cannot be used as a manner of death
- While all murders are homicides, not all homicides are murders
- Death certificates serve as legal documentation that death occurred and in aggregate, provide mortality statistics for public health purposes, which influences allocation of funding for research and public health initiatives
- Must be a direct, continuous sequence of events unbroken by any efficient intervening cause and without which the end result would not have occurred
- Must be an etiologically specific disease or injury
- Following terminology must be distinguished (BMC Health Serv Res 2007;7:183):
- Immediate cause of death: final disease or condition that leads to death
- Underlying / proximate cause of death: other conditions that precede and initiated the train of morbid events that ultimately culminate in the immediate cause of death
- Intervening cause: any condition that interrupts or exacerbates the chain of proximate causation
- Contributing factors to death: other conditions that play a role in the death process but are not the primary cause of death
- Autopsy is an essential tool to identify the cause and manner of death correctly (Am J Forensic Med Pathol 2003;24:313)
- Clinical autopsy (hospital autopsy): performed to diagnose the disease which led to a natural death (Med J Armed Forces India 2005;61:258)
- Medicolegal (forensics) autopsy: performed to provide information about the identity, cause of death, time of death, circumstances of death, etc. to support the law enforcing agencies to solve a possible crime (Med J Armed Forces India 2005;61:258)
- Classification / categorization used for how the death came about; a judgment based on the examination and circumstances surrounding the fatal event (J Med Toxicol 2017;13:111)
- In most jurisdictions, 5 categories are used:
- Natural: due entirely (or nearly so) to natural disease processes
- Homicide: due to a volitional act of another person with the intent to cause fear, harm or death and some negligent acts, even when a person did not intend to cause harm
- Examples of negligent acts designated homicide: caretaker leaves illicit drug on a table which a toddler consumes and dies from an overdose; intoxicated adult falls asleep on top of an infant, resulting in asphyxiation of the child
- Homicidal manner does not indicate a criminal homicide, which is determined by the legal process and not by the certifier of death
- Suicide: due to injury that occurred with the intent to induce self harm or cause one's own death
- Accident: due to injury when there is no evidence of intent to harm
- Undetermined: inadequate information regarding the circumstances of death to determine manner
- Example: individual found unconscious with large subdural hemorrhage; in the absence of information on the events leading up to death, it may not be possible to determine if the hemorrhage is due to accidental fall, homicidal violence, etc.
- Medical examiner cases can also be pending (pending further studies), while the results of special studies such as toxicology, histology, medical record review or police investigation are being performed
- When death is due to a combination of natural and unnatural events, preference is generally given to the unnatural cause
- Example: a man suffers a myocardial infarct while swimming in the ocean, loses consciousness and drowns; the manner of death is ruled accidental, as he may have survived if the fatal myocardial infarct had occurred on land
- "But for" principle asks the question: "But for the inciting injury (or event), would the decedent still be alive?"
- In most jurisdictions, deaths due to motor vehicle collisions are considered accidental in manner
- While acute alcohol or drug toxicity is considered an accidental death, deaths due to consequences of chronic substance abuse (hepatic cirrhosis due to ethanol abuse, endocarditis secondary to IV drug use) are conventionally considered natural in manner
- Acute intoxications may also be seen in suicides (Am J Public Health 2017;107:1233, J Forensic Sci 2016;61:661)
- Based on the investigations and medical history of the victim
- History of psychiatric disorder, previous suicide attempts or recent emotional trauma is commonly present
- Acute intoxications may also be seen in suicides (Am J Public Health 2017;107:1233, J Forensic Sci 2016;61:661)
- Deaths due to improper use of medical devices or improper therapy (e.g. malfunctioning morphine drip, incorrectly calculating dosage and administering 100 times the dose of a medication, resulting in death) are considered accidental
- Therapeutic complication (TC): refers to deaths caused by predictable complications of appropriate therapeutic procedures (J Forensic Sci 2006;51:1127)
- Some jurisdictions (New York City) have this additional manner of death
- TC differs from accident; accident would apply for grossly inappropriate therapy or unanticipated complications that should not have occurred
- In jurisdictions that do not have TC as a manner of death, deaths due to complications of medical therapy that are reasonably expectable (e.g. neutropenia due to chemotherapy, digoxin toxicity) are considered natural
- Medicolegal classification of the manner of death is mainly for statistical purposes
- Manner of death stated on the death certificate has no direct bearing on criminal prosecution or insurance settlements
- Defined as the immediate physiologic derangement resulting in death (StatPearls: Death Certification [Accessed 25 February 2019, Indiana Coroners' Association: Cause of Death and the Death Certificate [Accessed 3 March 2021])
- Particular mechanisms of death can be produced by a variety of different causes of death and are never etiologically specific
- Examples: hemorrhage, cardiac arrhythmia, cerebral hypoxia, sepsis, asphyxiation, disseminated intravascular coagulation (DIC)
- Mechanism of death is usually not specific to the condition that led to death
- Example: hemorrhage can be associated with natural (e.g., metastatic disease) or traumatic causes (e.g., gunshot wound to the chest)
- Circumstances of the death:
- Scene investigation (J Med Toxicol 2017;13:111, Am J Forensic Med Pathol 2020;41:152, Acad Forensic Pathol 2018;8:119)
- Interviews with next of kin
- Review of relevant medical history and medical records
- Evaluation for evidence of natural disease and injuries (acute and remote)
- May consist of external examination of the body or external and internal examination of the body (autopsy) (J Med Toxicol 2017;13:111)
- Dissection and evaluation of organs
- Photographic documentation
- Ancillary studies
- Purpose
- To legally document that death occurred (Clin Med Res 2015;13:74)
- To provide mortality statistics for public health purposes, which influences allocation of funding for research and public health initiatives
- Certifier of death
- Physician, medical examiner or coroner who completes the cause of death section on the death certificate, including information regarding the circumstances of death
- Cause of death and circumstances represent the certifier's opinion
- Not legally binding and can be changed if new information regarding the death is introduced
- How to complete the death certificate
- Cause of death should always be listed
- If an acute mechanism of death is known, this can be stated in the first line of part I, with the underlying cause of death listed in the second or third line of part I, as appropriate
- Conditions which contributed to the death but are separate from those in part I can be included in part II
- Incorrect cause of death: respiratory arrest
- Correct cause of death: respiratory arrest due to pneumococcal pneumonia; or complications of pneumococcal pneumonia; or pneumococcal pneumonia
- Manner: natural
- Incorrect cause of death: cardiac arrest
- Correct cause of death: acute myocardial infarct complicating hypertensive and atherosclerotic cardiovascular disease
- Manner: natural
- Incorrect cause of death: cardiac arrest
- Correct cause of death: acute myocardial infarct complicating hypertensive and atherosclerotic cardiovascular disease
- Contributing condition: acute cocaine intoxication
- Manner: accident (substance use disorder)
- Incorrect cause of death: bowel obstruction
- Correct cause of death: bowel obstruction due to metastatic colonic adenocarcinoma
- Manner: natural
- Incorrect cause of death: bowel obstruction
- Correct cause of death: bowel obstruction due to adhesions complicating exploratory laparotomy for gunshot wound of torso
- Manner: homicide (shot by other)
- Incorrect cause of death: cirrhosis
- Correct cause of death: hepatic cirrhosis complicating chronic alcohol use disorder
- Manner: natural
- Incorrect cause of death: anoxic encephalopathy
- Correct cause of death: anoxic encephalopathy complicating acute intoxication by the combined effects of heroin, fentanyl and ethanol
- Manner: accident (substance use disorder)
- Incorrect cause of death: urosepsis
- Correct cause of death: urosepsis complicating quadriplegia due to spinal cord injury from remote gunshot wound of torso
- Manner: homicide (shot by other)
- References: CDC: Physicians' Handbook on Medical Certification of Death [Accessed 25 February 2021], CDC: Improving Cause of Death Reporting [Accessed 25 February 2021], Indiana Coroners' Association: Cause of Death and the Death Certificate [Accessed 3 March 2021]
What is the manner of death in this case?
- Accident
- Homicide
- Natural
- Suicide
Comment Here
Reference: Cause, manner, mechanism of death & death certificate
What is the manner of death in this case?
- Accident
- Homicide
- Natural
- Suicide
Comment Here
Reference: Cause, manner, mechanism of death & death certificate
- Drowning: respiratory impairment (asphyxia) due to inhalation of water following submersion in liquid (Acad Forensic Pathol 2018;8:8, J Forensic Leg Med 2019;66:79)
- Implies an air - liquid interface at the opening of the airway that prevents the individual from inhaling air
- Effects of drowning dependent on many factors including age and health of victim and environmental circumstances (e.g., temperature, composition of water, etc.)
- Definitions vary with context (Circulation 2003;108:2565)
- End point variations: immediate death, delayed death or survival
- For the purposes of forensic pathology, the definition of drowning includes an endpoint of death
- Death cases that should be categorized as drownings
- Individual dies due to drowning while submerged
- Individual is rescued and resuscitated but dies due to drowning related sequelae
- Most common cause of death in resuscitated drowning victims is posthypoxic encephalopathy
- Other sequelae that may lead to death include acute respiratory distress syndrome (ARDS), multiorgan system failure due to global ischemia, sepsis due to aspiration pneumonia or nosocomial infections
- Drowning: submersion in liquid leading to respiratory impairment and death
- Deaths categorized as drownings: person dies while submerged or dies of submersion sequelae after resuscitation
- Circumstances of drowning critical for determination of cause and manner of death
- Nonspecific autopsy findings; drowning is usually a diagnosis of exclusion
- Submersion can alter the evolution of usual postmortem changes
- Various terminology related to drowning may be found in the literature; use of these terms may vary
- Dry drowning: sometimes used to describe delayed drowning deaths (i.e., person inhales water, is resuscitated and dies after)
- Near drowning: sometimes used to refer to an individual submersed who is resuscitated and survives > 24 hours
- Complications: pneumonia, pulmonary edema, hemoglobinuria, cardiac arrhythmia, fever, sepsis and sequelae of cerebral hypoxia; rapidly developing cerebral edema is a common mechanism of death (Int J Environ Res Public Health 2017;14:1402)
- > 230,000 annual drowning deaths worldwide
- Third leading cause of unintentional injury death worldwide
- > 4,000 annual drowning deaths in the United States
- Risk factors
- Male sex (M:F = 2:1)
- Young age (more prevalent in ages 1 - 24; highest in ages 1 - 4)
- Age > 85 years
- Lower socioeconomic status
- Intoxication (drug and alcohol)
- Reference: WHO: Drowning [Accessed 17 January 2024]
- Stage 1: surprise / reflective inspiration
- Victim recognizes risk and inhales deeply to fill lungs with as much air as possible
- Usually lasts a few seconds
- Stage 2: apnea
- Victim holds breath in attempt to not allow water to enter airways
- Usually lasts less than 1 minute
- Stage 3: deep breathing / expiratory dyspnea
- Increasing hypoxia and hypercapnia as a result of apnea lead to respiratory stimulation with expiratory dyspnea and rapid swallowing, resulting in entry of water into airway and gastrointestinal (GI) tract
- Stage 4: convulsive
- Anoxic brain injury results in bradycardia, arrhythmia and convulsion
- Stage 5: terminal apnea / death
- Anoxic brain injury becomes irreversible and breathing and circulation cease
- Dependent on person's age and temperature of water
- Case reports of survival following prolonged submersion in cold water versus retrospective analysis of near drownings (JAMA 1988;260:377, Resuscitation 2002;52:247)
- Submersion time thought to be best prognostic factor
- Anoxic brain injury becomes irreversible and breathing and circulation cease
- References: Int J Legal Med 2021;135:281, Med J Aust 1985;142:586
- Drowning physiology involves 2 events
- Immersion (above water)
- Cardiorespiratory responses to temperature changes (see below)
- Can culminate in a collapse followed by submersion
- Submersion (underwater)
- Inhalation of water → vagal reflex → increased airway resistance and pulmonary vasoconstriction → decreased lung compliance and pulmonary hypertension → severe ventilation perfusion mismatch (JAMA 1986;256:75)
- Extrapulmonary sequelae may include hemolysis or electrolyte disturbances (see Freshwater versus saltwater drowning below)
- Immersion (above water)
- Diving reflex: cold water submersion causing bradycardia and vasoconstriction in peripheral vascular beds to shunt blood to brain and heart
- May be present in children and contribute to higher survival rates in younger ages
- Reflexive peripheral vasoconstriction varies with vascular gene expression (Am J Physiol Heart Circ Physiol 2017;312:H622)
- Cold shock
- Immediate exposure of the body to cold water (usually after body immersion)
- Sudden skin cooling may result in a cold shock response characterized by peripheral vasoconstriction, hypertension, inspiratory gasp and hyperventilation with swimming inability and liquid aspiration (Int J Environ Res Public Health 2020;17:8984)
- Acute anxiety is an important risk factor for cold shock response (Front Psychol 2018;9:510)
- Complications according to body temperature
- Below 35 °C (95 °F) leads to confusion, disorientation and decreased muscle coordination
- Below 33 °C (~91 °F) leads to hypoventilation, bradycardia and irregular breathing
- Below 30 °C (86 °F) leads to stupor or unconsciousness and coma
- Below 28 °C (~82 °F) leads to ventricular fibrillation
- Below 25 °C (77 °F) leads to cardiac arrest and death
- Reference: Physiology (Bethesda) 2016;31:147
- Differences in survivability after inhalation of fresh versus salt water unproven
- Freshwater denatures alveolar surfactant and passes to bloodstream → hemodilution → disruption of osmotic gradient → hemolysis (Pediatr Clin North Am 2001;48:627)
- Freshwater frequently defined as salinity < 1% (e.g., most rivers, lakes, ponds, pools, bathtubs, etc.)
- Saltwater dilutes surfactant → intravascular water is drawn into alveoli → hemoconcentration → electrolyte disturbances (Exp Ther Med 2017;13:2591)
- Saltwater most commonly refers to ocean water and includes some lakes
- Reference: Eur Radiol 2016;26:1186
- External examination
- Inspection of clothing, if present, for condition, defects, debris
- Artifacts in clothing condition may be present if caught on rocks, brush or other objects in water
- Cutaneous changes of immersion (washerwoman hands and feet): wrinkling and pallor of skin
- Cutis anserina (goose flesh): rigor of arrector pili muscles
- Variable injuries
- Blunt force most common, abrasions and lacerations also possible
- May occur before submersion, on impact with water or during submersion
- Consider topography, presence of manmade objects in water, velocity of currents (postmortem abrasions exaggerated in rapid current), depth of water
- Resuscitative injuries
- Inspect carefully for suspicious injuries (e.g., stab wounds)
- Froth in mouth or nose (foam cone)
- Signs of animal predation, if applicable
- Inspection of clothing, if present, for condition, defects, debris
- Internal examination
- Froth / foam in airways
- Watery gastric contents with fluid - fluid level
- Water in respiratory tract (often minimal)
- Watery sphenoid contents
- Debris in respiratory tract or gastrointestinal tract (e.g., silt, dirt, vegetation)
- Neck muscle hemorrhage can be present
- May result from violent neck movements during the process of drowning (Am J Forensic Med Pathol 1998;19:223)
- Can be a sign of excessive neck extension at convulsion stage (Int J Legal Med 2021;135:281)
- Does not necessarily indicate neck compression or inflicted trauma
- Scleral hemorrhage can be present
- Drowning related elevation in central venous pressure can be communicated to head through valveless veins of the neck (J Forensic Sci 2011;56:522)
- Any barotrauma findings
- References: Acad Forensic Pathol 2018;8:8, Forensic Sci 1972;1:397
- Usual postmortem changes still occur in drowning cases
- Livor and rigor mortis
- Skin discoloration and sloughing
- Marbling
- Purge fluid
- Bloating
- Bloating will cause body to float (if not tethered or weighted down)
- Body usually arrives to surface in prone position with face submerged and extremities hanging downward (drowning position)
- Regions above water surface may dry out and mummify
- Anterior lividity if body in drowning position
- Decomposition changes may occur at different pace than on land
- Dependent on water factors (temperature, salinity, currents, bacteria present)
- Fly larvae not present under water; may be present if there are body surfaces exposed to air
- Saltwater bacterial content typically lower → slower decomposition
- Onset and disappearance of livor and rigor may be accelerated or slowed based on water temperature
- Adipocere: yellow to brown waxy material comprising long chain fatty acids
- Formed in moist environments, can occur with submersed bodies
- Usually occurs over long postmortem interval (months)
- May present as white spots on mucosal surfaces of organs
- Reference: Acad Forensic Pathol 2016;6:19
- Drowning is a diagnosis of exclusion
- Not widely used, sensitive / specific, validated testing available (research ongoing)
- Characterization of drowning deaths involves routine ancillary testing (to rule out other causes of death or contributory factors), including
- Drug toxicology
- Carbon monoxide testing
- Tests discussed in the literature, used variably in forensic examination
- Paranasal (sphenoid, maxillary, frontal) sinus fluid
- Nonspecific
- Some evidence of association of drowning with larger fluid volume in paranasal sinuses versus other causes of death (Eur Radiol 2016;26:1186)
- Can be assessed visually or with postmortem computed tomography (CT) scanning (J Forensic Radiol Imag 2015;3:111)
- With or without sediment
- Forensic limnology
- Diatom test: identification of unicellular algae found in all bodies of water (Forensic Sci Res 2020;5:98)
- If present in the body, may suggest drowning
- If absent, does not rule out drowning
- Diatoms are very ubiquitous and have been documented in nondrownings
- May involve diatom species classification
- If present in the body, may suggest drowning
- Diatom test: identification of unicellular algae found in all bodies of water (Forensic Sci Res 2020;5:98)
- Gettler chloride test
- Used in context of suspected drowning for confirmation of saltwater versus freshwater
- Blood analyzed from right and left heart, chloride levels compared
- If chloride level higher on right than left, thought to indicate saltwater drowning
- If chloride level higher on the left than right, thought to indicate freshwater drowning
- Unreliable and not widely used
- Forensic anthropology / taphonomy
- Becomes critical if body is skeletonized due to aquatic animal predation
- Skeletonization can occur rapidly if carnivorous aquatic species present
- Paranasal (sphenoid, maxillary, frontal) sinus fluid
- Not all bodies recovered from water have cause of death attributed to drowning
- Must consider death due to natural disease, weather and temperature, drug intoxication, electrical hazards or other causes
- If death due to natural disease, must consider whether the disease would have caused death if event occurred outside of water
- Example: catastrophic brainstem hemorrhage would cause death in water or on dry land (water would not play a role, usually not ruled as drowning) versus a seizure in water may cause drowning but the seizure would not necessarily lead to death if it occurred on dry land (usually ruled as drowning)
- Drowning largely considered a diagnosis of exclusion
- Must consider death due to natural disease, weather and temperature, drug intoxication, electrical hazards or other causes
- Manner of death in drowning not always accidental
- Attention must be paid to evidence as to how and why the person was submersed and whether there was attempt to self extricate
- Manner may be accidental, homicide or suicide
- If the event is unwitnessed, there are conflicting statements or simply there is not enough information on the circumstances of the event, the manner of death should remain undetermined (Med Sci Law 2003;43:207)
- Accurate determination of cause and manner of death requires coordinated efforts between law enforcement, medicolegal investigators, first responders and forensic pathologists
- Reference: Forensic Sci Int 2006;163:1
- Standard scene investigation and documentation elements apply to cases of suspected drowning
- Body location, position and temperature
- Identification and medical history of decedent
- Resuscitation efforts
- Witness statements
- Photographs
- Special considerations for investigation of suspected drowning scenes
- Water and surrounding environment conditions
- Efforts to recover body from water
- Collection of water sample
- Collection of any gear associated with the decedent (e.g., life vests, breathing apparatuses used for snorkeling or diving, etc.)
- Inspection of any vehicles or vessels that may be involved (e.g., boats, rafts, jet skis, etc.)
- Collection of ancillary testing materials, where applicable
- Entomology
- Botany
- References: Wagner: Death Scene Investigation - A Field Guide, 1st Edition, 2008, Spitz: Spitz and Fisher's Medicolegal Investigation of Death - Guidelines for the Application of Pathology to Crime Investigation, 5th Edition, 2020
- Drowning can occur in any collection of liquid or water sufficient enough to cover the mouth and nose
- Sinks or basins, bathtubs, pools, hot tubs, sewage tanks, etc.
- Must modify scene investigation based on water involved
- Examination of surrounding areas (e.g., counters, floors) for wetness
- Temperature of home or building (if indoors)
- Temperature of bath water
- Very hot water may indicate intentional scalding
- Cold water may indicate delayed activation of emergency services
- Temperature of pool or hot tub water, documentation of temperature control apparatuses
- Collection of water if not drained by associates of decedent or first responders
- Example: analysis of water from bathtub for soap at a scene where a parent claims to have been bathing an infant or toddler
- Depth of water and presence of any identifiable substance (e.g., soap, mildew, blood, urine)
- Presence of other objects
- Expected objects (e.g., towels in a bathroom, pool toys in a pool, etc.)
- Unexpected objects (e.g., cleaning supplies open and recently used, possibly indicating attempted clean up of scene)
- Presence of electrical hazards (e.g., hair dryer in bathroom)
- Documentation of layout of home or other involved buildings
- References: Wagner: Death Scene Investigation - A Field Guide, 1st Edition, 2008, Spitz: Spitz and Fisher's Medicolegal Investigation of Death - Guidelines for the Application of Pathology to Crime Investigation, 5th Edition, 2020
- 18 month old child drowns in home swimming pool (Med Sci Law 2015;55:304)
- 5 year old daughter and 30 year old father drown in sea during homicide / suicide (J Forensic Sci 2014;59:1432)
- 8 year old girl dies by manual strangulation in connection with drowning (Forensic Sci Med Pathol 2019;15:233)
- 26 year old man drowns in private pool (Forensic Sci Int 2021;3:100189)
- 31 year old woman drowns in a well (Am J Forensic Med Pathol 2018;39:27)
- 37 year old woman drowns in a Jacuzzi (Med Leg J 2016;84:159)
- 55 year old man dies after being beaten and thrown into sea (Forensic Sci Med Pathol 2019;15:233)
A 51 year old man is discovered deceased, floating face down in a lake where he is known by friends to swim recreationally. He is wearing only swim trunks. He was observed by a passing jogger to be swimming back and forth in regular laps from one side of the lake to the other. This observation was made about 30 minutes before he was discovered floating face down. He also spoke to his sister on the phone the day before and is reported by her to have been in good spirits. The decedent's medical history includes hypertension, depression and seizure disorder. He is known to struggle with medication compliance but is prescribed medications for each of these conditions. He is not married and has one adult child in good health. He is a former smoker. The lake water is found to be clear, still and 77 °F (25 °C). The lake is within walking distance to the decedent's home in northern Florida and only the jogging path is nearby. A pair of tennis shoes are found neatly placed on the shore. Investigators have found no signs of foul play. The above examination finding was discovered at autopsy. Drug and alcohol toxicity panels are negative. What is the most likely cause and manner of death?
- Cardiac arrhythmia, natural
- Drowning, accidental
- Drowning, suicide
- Myocardial infarction, natural
- Myocardial infarction with rupture, natural
Comment Here
Reference: Drowning
- Bathtub
- Lake
- Ocean
- Standing outdoor water (e.g., bucket of water near a home or school)
- Swimming pool
Comment Here
Reference: Drowning
- Death due to exogenous environmental factors, exposure or injury
- May be due to natural phenomena, unintentional human exposure or intentional human intervention
- Burn injury severity can vary significantly depending on a number of intrinsic and external factors and may result in immediate or delayed death
- Careful examination is required to determine antemortem thermal injuries from postmortem thermal artifacts
- Electrical injuries may present with minimal external signs and require careful scene investigation
- Hypothermia and hyperthermia have no specific postmortem findings and diagnosis may be dependent on investigation, supportive findings and lack of another cause of death
- Immediate or delayed death due to exposure to an electrical current
- Transmission of energy dictated by Ohm's law (BMJ 2017;357:j1418)
- I = V/R
- Current (I): measure of flow of energy through an object / circuit
- Voltage (V): unit charge of the source (dependent on the electrical source)
- Common household voltage in the United States ranges from 120 to 240 volts
- Lightning voltage can be into the tens of millions of volts or higher
- Resistance (R): resistance of the object / circuit
- Resistance can be increased (less transmission) by wearing protective equipment
- Resistance can be decreased (more transmission) with increased surface area of contact or exposure to wet skin / clothing
- 2 types of electrical current may be encountered, which may cause distinctly different findings (StatPearls: Electrical Injuries [Accessed 16 February 2024], Forensic Sci Med Pathol 2023;19:91)
- Alternating current (AC)
- Most common form of electricity in standard applications (household products, most industrial machinery and power lines)
- Low voltage electrocution (
- Most commonly used home electrical devices
- May have little to no external injury (requires careful external examination and scene investigation)
- Gross findings: may leave burns at the entry and exit site
- High voltage electrocution (> 1000 volts)
- Some industrial equipment and power lines are common sources
- May have enough energy to arc (jump) from the source to the victim
- Gross findings: often significant burn / charring at sites of entry and exit
- Alternating current (AC)
- Direct current (DC)
- More rarely encountered (lightning is most common source)
- May have little to no external signs of injury or significant burns / charring
- Ferning pattern of Lichtenberg figures may be seen on the skin surface
- Force generated during a lightning strike may throw the victim a significant distance and cause damage to clothing or nearby objects
- In the correct circumstances, the scene may appear akin to a motor vehicle striking a pedestrian
- May also cause secondary blunt injuries if the victim strikes other objects
- Lightning strikes can and do occur at the border of storms or during storm development and no rain or other evidence of a storm may be present during investigation
- Nuclear streaming / palisading within the epidermis
- Separation of the layers of the epidermis or between the epidermis and dermis
- Immediate (can be seen in all types of electrical injury): cardiac arrhythmias
- Delayed and indirect (generally high voltage injuries)
- End organ damage (along path of current)
- Secondary blunt injuries
- Complications of external and internal burn injury
- May be the key to determining electrocution as the cause of death
- Disconnect concerning products / power sources
- It may be necessary to have a certified electrical expert inspect the suspected product / connections
- Careful examination of clothing and other objects in the vicinity may help detect subtle electrical entry / exit sites at autopsy
- Manner of death is related to the underlying source of the electrical injury
- Manner of death in the vast majority of cases is an accident
- Work related deaths must be reported so that workers' death benefits can provide financial support for their family
- Very rarely do electrical injuries occur in homicides or suicides (scene investigation will help identify these cases)
A bystander noticed a damaged bicycle sitting on the side of a rural highway; the bicycle belonged to a 63 year old neighbor who often rides in the area for exercise. The bystander searched the area and found the neighbor collapsed ~15 feet from the roadway without apparent external injuries. The ground was dry and there had been no recent rain in the area. During investigation, the decedent's hat was found near the bicycle, as seen in the image above. What is the most likely cause of the decedent's death?
- Arrhythmia due to lightning strike
- Blunt force injuries from a hit and run motor vehicle collision
- Carbon monoxide inhalation
- Gunshot wound to the head
- Myocardial infarction due to coronary artery disease
Answer B is incorrect because of the lack of external evidence of trauma and no mention of vehicle parts or other signs of collision near the bicycle. Autopsy would be helpful to exclude occult injuries from a motor vehicle strike. Answer C is incorrect because carbon monoxide inhalation is extremely unlikely in an outside environment in the absence of an obvious source. Answer D is incorrect because there is no external trauma to the body and no blood or other evidence of a gunshot on the hat. Answer E is incorrect because a myocardial infarction due to coronary artery disease would not explain the damage to the bicycle or the hat.
Comment Here
Reference: Environmental deaths
- Antemortem injuries
- Postmortem amputation due to body entrapment for extrication
- Postmortem dismemberment in attempt to hide homicide
- Postmortem thermal amputation and tissue loss
- Remote antemortem amputation
Answer A is incorrect because of the absence of hemorrhage or other signs of vital response to injury, which are often seen if the body is not largely consumed by thermal changes. Answer B is incorrect because postmortem amputation for extrication purposes would result in clean margins of tissue without thermal changes. Answer C is incorrect because postmortem dismemberment with secondary burning would lead to atypical patterns of thermal changes and likely other evidence of trauma from the homicidal violence. Answer E is incorrect because antemortem amputation is unlikely to impact all 4 limbs and the margins would be clean and well healed. Antemortem amputation may help to explain the absence of a single or more limbs without significant thermal changes in some circumstances.
Comment Here
Reference: Environmental deaths
- Forensic entomology is the study of insects / arthropods pertaining to its applications to medicolegal and criminal death investigations
- Predictable sequence of insect colonization on a decomposing body is known as insect succession (PLoS One 2018;13:e0195785)
- Insect succession depends on whether physical obstructions to oviposition are present and if conditions are suitable for oviposition (PLoS One 2018;13:e0195785)
- Insect succession patterns, developmental age of immature insects and environmental data are used to estimate the postmortem interval (Forensic Sci Int 2011;211:67)
- Blow flies are regarded as the primary and most accurate forensic indicators of time of death (J Med Entomol 1991;28:565)
- Larval stages of flies are called maggots
- Maggot movement through bodily fluids, especially prior to pupation, adult fly meal regurgitation and adult fly waste products may confound bloodstain pattern interpretation at the crime scene or during autopsy (Forensic Sci Int 2003;137:152)
- Uses:
- Substantiate cases of neglect (Forensic Sci Int 2001;120:155, Forensic Sci Int 2004;146:S195)
- Alternative sample for toxicology (J Forensic Leg Med 2019;67:28)
- Alternative sample for human DNA identification (J Forensic Sci 2001;46:685)
- Detect postmortem relocation (PeerJ 2017;5:e3506)
- Correlation of period of insect activity with a postmortem interval (PLoS One 2018;13:e0195785, Int J Legal Med 2007;121:90)
- Tissue destruction and lesions caused by postmortem insect feeding activity may resemble or obscure antemortem injuries (Int J Legal Med 2019;133:307)
- Insect feeding activity may begin in the antemortem phase and continue postmortem, especially in cases of neglect and abuse (Forensic Sci Int 2001;120:155, Forensic Sci Int 2004;146:S195)
- Antemortem feeding (myiasis) may be a contributor to the cause of death as opposed to a postmortem artifact (J Forensic Sci 2002;47:542)
- Tissue sampling of candidate postmortem artifacts for histology is useful to confirm the postmortem nature of the lesion (Int J Legal Med 2019;133:307)
- Not all forensically important insects wait until death to feed (Forensic Sci Int 2004;146:S195)
- Medical conditions and wounds can produce chemoattractants and provide substrates for necrophagous insects to feed (e.g. diabetes, ulcers, sores, wounds) (J Forensic Sci 2002;47:542)
- Larval myiasis can be fatal (Forensic Sci Int 2004;146:S195)
- While a low number of maggots can be used therapeutically to debride wounds, a large enough maggot mass can damage and destroy healthy tissue through buildup of larval waste products and secondary invaders in the form of predators, which may introduce harmful microorganisms into the wound site (Trends Parasitol 2001;17:176)
- Some fly species have larva that may opportunistically switch to feeding on living tissue to overcome feeding competition within a large enough maggot mass (Forensic Sci Int 2004;146:S195)
- Indicator of neglect or abuse
- Usual movement by living organisms and changing environmental conditions deters fly progeny deposition (Forensic Sci Int 2004;146:S195)
- Incapacitated individuals are unable to interrupt fly activity, allowing surface deposition of fly egg or larva (Forensic Sci Int 2004;146:S195)
- Exposed body fluids and waste products are powerful chemoattractants for several species of flies (Forensic Sci Int 2001;120:155)
- Indicator of caregiver neglect (Forensic Sci Int 2001;120:155)
- Consumption of maggot infected foods may cause gastrointestinal symptoms and oral or anal infestation, described as accidental myiasis (pseudomyiasis) (Forensic Sci Int 2001;120:155)
- Significant as a sign of negligence by caregiver (Forensic Sci Int 2001;120:155)
- Complicates the use of the period of insect activity in the calculation of a postmortem interval (Forensic Sci Int 2004;146:S195)
- Insect feeding activity can modify decomposition process
- Activity and metabolism in a maggot mass create heat (up to 25 °C above ambient air temperatures), accelerating both the decomposition process and the rate of feeding activity (J Med Entomol 1991;28:565)
- Insect activity is temperature dependent; warmer temperatures increase rate of tissue consumption (J Med Entomol 1991;28:565)
- Maggots release digestive enzymes, contributing to rapid localized breakdown of cadaveric tissue (Acta Trop 2013;128:686)
- A heavy maggot load can counteract the preservative effects of refrigeration prior to autopsy; thus, a timely postmortem examination is advised (Int J Legal Med 2007;121:90)
- Effects on skin and other soft tissue:
- Ants feed on superficial layers of skin, leaving lesions characterized by orange-pink to yellow, diffusely scattered and shallow points of erosion, scalloped areas of skin loss and linear trails with absence of bleeding, known as parchmenting (Forensic Sci Med Pathol 2005;1:37, Int J Legal Med 2019;133:307)
- Usually resembles abrasions, cigarette or strong acid scars (Int J Legal Med 2019;133:307)
- May resemble marks from ligature strangulation when feeding activity obstructed by collar lines of shirts or pullovers (Forensic Sci Med Pathol 2005;1:37)
- Useful as a marker of clothing and body position due to ants' inability to feed underneath parts pressed against the ground or clothing (Forensic Sci Med Pathol 2005;1:37)
- Ants feeding on areas of lividity may show significant postmortem seepage of blood resembling antemortem injury (Int J Legal Med 2019;133:307)
- Histological examination of the ant feeding artifacts demonstrates absence of the epidermis only without hemorrhage (Int J Legal Med 2019;133:307)
- Beetles tend to feed at the edges of wounds and tunnels within skin and connective tissue late in decomposition; this is capable of masking antemortem wounds while producing patterned depressions that can grossly mimic imprint marks from blunt trauma by objects (Int J Legal Med 2019;133:307, J Forensic Leg Med 2015;36:22)
- Beetle frass (waste) appears as whitish ribbons (Int J Legal Med 2019;133:307)
- Cockroach feeding artifacts may be misinterpreted as burn marks due to the small round shapes (Int J Legal Med 2019;133:307)
- Ants feed on superficial layers of skin, leaving lesions characterized by orange-pink to yellow, diffusely scattered and shallow points of erosion, scalloped areas of skin loss and linear trails with absence of bleeding, known as parchmenting (Forensic Sci Med Pathol 2005;1:37, Int J Legal Med 2019;133:307)
- Effects on bone:
- Beetles, moth larvae, wasps and termites can bore into bone and create microscopically visible, star shaped patterns and linear etchings, replicating the damage caused by bullets (Int J Legal Med 2019;133:307)
- Effects on hair:
- Beetles and caterpillars produce concave lesions attributed to gnawing activity, visible under scanning electron microscopy when compared with lesions with regular edges made by sharp force trauma (Int J Legal Med 2019;133:307, Forensic Sci Med Pathol 2015;11:104)
- A multidisciplinary approach is recommended in death investigation; collection of insect evidence and workup is best conducted in collaboration with forensic entomology technicians or forensic entomologists (Int J Legal Med 2019;133:307)
- American Board of Forensic Entomology and the Entomology Society of America offer a publicly accessible directory of active, board certified entomologists (American Board of Forensic Entomology: Members [Accessed 17 November 2020], Entomology Society of America: Rosters [Accessed 17 November 2020])
- European Association for Forensic Entomology offers a public directory of active, Europe based forensic entomologist members and international associate members on their website (European Association for Forensic Entomology: Home [Accessed 17 November 2020], Int J Legal Med 2007;121:90)
- If the forensic pathologist wishes to identify specimens on their own, Rivers and Dahlem (2014) recommends Borror and Delong's Introduction to the Study of Insects by Johnson and Triplehorn (2004) for identification to order and family level (Rivers: The Science of Forensic Entomology, 1st Edition, 2014, Johnson: Borror and Delong's Introduction to the Study of Insects, 7th Edition, 2004)
- If the forensic pathologist only requires definitive specimen identification by a systematic expert, especially if the findings will be used in court, then payment should be offered to the expert; Rivers and Dahlem (2014) suggests a payment of $55 per single identification as a good starting point and increasing depending on whether DNA based identification is necessary and the condition of the specimen
- Systematic experts employed in a public service position (such as research entomologists at a local museum of natural history) may also be readily available for identification services (Rivers: The Science of Forensic Entomology, 1st Edition, 2014)
- In lieu of trained personnel, a thorough investigation and presentation of entomological evidence is still possible when following published guidelines
- Best practice in forensic entomology - standards and guidelines by Amendt et al. is a resource developed by the European Association for Forensic Entomology (EAFE) for practical guidance in collection, preservation and documentation of insect evidence in medicolegal death investigations (Int J Legal Med 2007;121:90)
- At the scene:
- Complete photograph documentation and scene description should include body position, clothing, doors, windows and light positions to identify entry / exit points for insects and possible hiding places for pupating maggots (Int J Legal Med 2019;133:307)
- The ambient temperature and humidity should be noted; this data is best when taken at the scene in addition to noting recent local weather station data (Int J Legal Med 2007;121:90)
- The temperature of any maggot mass, if present, should be noted (Int J Legal Med 2007;121:90)
- Collection of the insect evidence is best taken at the scene; always check the corpse and the surroundings for entomological evidence (Int J Legal Med 2007;121:90)
- It is strongly recommended to collect entomological evidence from the surrounding area before the removal of the remains and under the remains immediately after removal (Int J Legal Med 2007;121:90)
- Example sampling sites may include natural orifices, traumatic wounds, pleats of clothes, pockets, carpet and windowsills (Int J Legal Med 2007;121:90)
- Collect living and dead specimens of every shape and size and sample flying insects, if present, with an insect net (Int J Legal Med 2007;121:90)
- At the autopsy:
- Inspect and sample the insects from within the body bag, clothing and body (Int J Legal Med 2007;121:90)
- Compare clothing and position from the scene with lividity and site of injuries (Int J Legal Med 2019;133:307)
- Sampling of suspected postmortem artifact for histological review is useful to confirm the postmortem nature of the lesion, notably the absence of congestion, inflammatory reaction and fibrin deposition (Int J Legal Med 2019;133:307)
- Preserving insect evidence:
- Store dead specimens immediately in 70 - 95% ethanol and avoid formalin / formaldehyde use, as insect specimens are less well preserved for morphological and molecular identification (Int J Legal Med 2007;121:90)
- Recommended guidelines by the EAFE for storing living specimen varies by life stage and investigational goals (Int J Legal Med 2007;121:90)
- Place eggs on moistened tissue paper within aerated vials that do not allow the escape of newly hatched larvae for transfer to an expert for rearing within 24 hours; otherwise immediate killing and preservation of all egg specimens by placing them in 70 - 95% ethanol is recommended (Int J Legal Med 2007;121:90)
- Store larva in vials lined with coarse sawdust in a controlled humidity and temperature environment, preferably 2 - 6 °C for transfer to an expert for rearing within 24 hours; otherwise larval specimens should be quickly killed by 30 seconds of immersion in very hot but not boiling water (> 80 °C) and placed in a vial with 70 - 95% alcohol to best preserve morphological features (Int J Legal Med 2007;121:90)
- Store pupae in vials with airflow under controlled temperatures and humidity, preferably 2 - 6 °C (Int J Legal Med 2007;121:90)
- Preserve adults by freezing at -20 °C for 1 hour, then store in 70 - 95% alcohol or alternatively pinned to simplify identification (Int J Legal Med 2007;121:90)
- Insect remnants, such as empty puparia and frass, can be stored under completely dry conditions in vials or in 70 - 95% ethanol (Int J Legal Med 2007;121:90)
- EAFE standards recommends the killing of all sampled specimens when the use of insects is ambiguous at the time of collection or when rearing is impossible (Int J Legal Med 2007;121:90)
- Submitting evidence for identification:
- Rivers and Dahlem (2014) recommends the United States Postal Service when shipping within the United States and caution when packing specimen for shipment (Rivers: The Science of Forensic Entomology, 1st Edition, 2014)
- To legally send biological specimens internationally, authorization by the United States Fish and Wildlife Service is required (Rivers: The Science of Forensic Entomology, 1st Edition, 2014)
- Use in toxicology workup:
- Insect specimens may be used as a source of reliable toxicology samples in cases of severe decomposition and where conventional tissue or fluid samples are no longer available (J Forensic Leg Med 2019;67:28)
- Chitin, the chemical which makes up the insect cuticle, accumulates and forms highly stable bonds with many drugs and toxic substances; puparial casings, which are rich in chitin, may be used in place of hair in toxicology assays in specific preparations (J Forensic Leg Med 2019;67:28)
- Insect growth, morphology and activity can be modified by ingestion of trace amounts of drugs or toxic substances found in cadaveric tissue, complicating the calculation of the postmortem interval (J Forensic Leg Med 2019;67:28)
- Use in identification of human DNA:
- Mitochondrial DNA sequences have been retrieved from the dissected gut of a maggot that fed on human tissue (J Forensic Sci 2001;46:685)
External examination of a decedent reveals a multifocal, orange-pink, linear lesion along the shirt collar. No petechial conjunctival hemorrhage is noted. Anterior neck dissection reveals no area of hemorrhage in the underlying soft tissue and the hyoid is intact. Microscopic examination of the lesion demonstrates absence of the epidermis without hemorrhage. What is the most likely cause of the lesion?
- Decomposition
- Excoriation
- Postmortem ant feeding
- Strangulation by shirt collar
Comment Here
Reference: Forensic entomology
Comment Here
Reference: Forensic entomology
- Noninvasive or minimally invasive techniques used to supplement postmortem examination
- Postmortem radiography is an effective and efficient supplement to autopsy
- Postmortem Xray is the most prevalent modality used in the United States
- Computed tomography has multiple utilities in postmortem examination
- Identification of remains can be accomplished through multiple imaging means
- Postmortem radiology is a powerful tool that complements full postmortem examinations but cannot replace them
- Forensic / postmortem imaging
- Forensic / postmortem radiography
- Virtopsy
- Wilhelm Conrad Röntgen discovered the Xray in 1895
- First use in forensic medicine was in the United Kingdom in 1896 (Am J Forensic Med Pathol 1984;5:53)
- By the early 1900s, Xray techniques for forensic examination became widely adopted throughout the world
- First reported application of postmortem computed tomography was in 1977 (Z Rechtsmed 1977;80:227)
- Advanced imaging techniques have been adopted more slowly but are becoming more commonplace throughout the world
- Imaging has been suggested as a potential replacement to autopsy (Lancet 2012;379:136)
- Postmortem imaging is often technically superior to antemortem imaging due to lack of motion artifacts and the ability to increase the time of exposure and radiation dose
- When performing postmortem imaging, try to remove as much foreign material from the deceased and imaging area as possible to prevent overlay and artifacts
- Generally interpreted by pathologists; radiologists may be retained as consultants by some institutions
- Specific training programs in forensic radiology have become available through the years (Clin Radiol 2008;63:1189)
- Also known as radiograph or roentgenogram
- 2 dimensional image created by electromagnetic radiation (Xrays) interacting with structures of various densities between a radiation source and detector
- Projectional technique: objects closer to the detector appear smaller than same sized objects farther from the detector; unreliable at determining the size of findings
- Requires at least 2 views for localization
- Most utilized modality in the United States
- Widely available, low cost and most familiar for most pathologists
- Requires less technical skill to capture and interpret than other modalities
- Most useful for differentiating high contrast structures (bone, metallic foreign bodies, etc.) (Forensic Sci Int 1982;19:263)
- May also be useful in detecting large fluid or air collections (pneumothorax, pneumoperitoneum, etc.)
- Poor at detecting soft tissue changes
- Full postmortem radiographic examinations (skeletal survey) are standard of care in pediatric autopsies to exclude occult injuries or natural disease processes
- 3 dimensional image created by multiple electromagnetic radiation sources interacting with structures of various densities and multiple detectors (Acad Radiol 2019;26:820)
- Allows for multiple planes of view utilizing a single scan
- Can accurately determine the size of findings or relationships between landmarks
- Adjusting the window (scope of densities viewed) can allow for better differentiation of specific types of tissues (i.e., bone, lung, brain, soft tissue, etc.)
- Can also allow for 3 dimensional reconstruction
- Metallic objects can interfere with scanning (metallic streak artifact)
- More widely used in Europe, Australia and Asia than the United States
- Since it is noninvasive, it may be more acceptable to religious / cultural groups that object to postmortem examinations
- Better than Xray at detecting most traumatic injuries and air or fluid collections (J Geriatr Cardiol 2014;11:363, J Forens Radiol Imaging 2015;3:91)
- Useful in asphyxia and gunshot wound related deaths (Leg Med (Tokyo) 2014;16:364, Leg Med (Tokyo) 2014;16:357)
- Detailed visualization of the larynx and hyoid bone
- Bullets / fragments location; bone fragments directed toward the bullet direction
- Poor at detecting soft tissue and intra-abdominal pathologies / injuries
- Virtopsy has been suggested as an alternative to postmortem examination (Leg Med (Tokyo) 2007;9:100)
- Complete external and internal imaging of the body with contrast
- Limited sampling can be utilized for histologic or microbiologic specimens
- Significant limitations when compared with traditional autopsy
- Most people agree that a hybrid approach with postmortem CT and traditional postmortem examination is superior to either technique alone (J Forensic Sci 2023;68:524)
- Significant postmortem artifacts may occur, especially with decompositional changes or heavily refrigerated individuals
- 3 dimensional image created by the interaction of magnetic and ultrasonic waves with various tissues and organs through a series of emitters and detectors
- Different phases can be utilized to detect different organs and structures (Br J Radiol 2014;87:20130567)
- More detailed images than any of the other modalities and smaller scale resolution
- Superior to other modalities for detecting soft tissue findings
- Not widely available in most areas and largely used as a research modality
- Takes longer than other modalities, which limits use
- Time to image an individual body segment is often greater than the time it would take to perform a full postmortem examination
- Metallic objects (projectiles or surgical implants) may be at risk of moving due to high power magnetic fields
- Significant postmortem artifacts may occur with even mild decompositional changes or any degree of postmortem refrigeration
- 2 or 3 dimensional image created by the interaction of ultrasonic waves and tissues based on the rates of transmission, reflection and deflection between the source / detector probe
- Not widely available and utilized mostly as a research modality (Int J Legal Med 2021;135:2363)
- Requires additional training in operation and interpretation, which is not widely available outside of radiology training
- Good at detecting air and fluid collections or areas of largely differing density
- May be used to target areas of interest in limited dissection sampling
- Significant postmortem artifacts may occur, especially with decompositional changes or heavily refrigerated individuals
- Postmortem angiography can be used with Xray, CT or MRI modalities (AJR Am J Roentgenol 2007;188:832)
- Isolated vessel angiography can be used to identify injuries (such as vertebral artery dissections or sharp / projectile injuries in the extremities)
- Segment of vessel can be isolated using clamps and contrast can be injected into the segment to look for extravasation or luminal irregularity
- Whole body angiography can be used for better quality imaging
- Requires washout of clot and a reperfusion pump
- If contrast is introduced at too high of pressure, it may result in rupture of blood vessels and artifactual extravasation of contrast
- Traditional dissection may still be needed in cases with subtle or no findings when they are suspected
- Postmortem imaging is very frequently used as a means of identification in persons that are not visually identifiable (decomposition, thermal changes, mass disasters, etc.) (Forensic Sci Res 2022;7:385)
- Requires comparison of antemortem images with postmortem images
- Cannot use a written report for comparison purposes
- Having antemortem images available prior to examination can help limit the number of postmortem images needed and may guide positioning of the body to obtain correct orientation
- Features useful in postmortem identification
- Unique anatomic findings
- Frontal sinus pattern (only in skeletally mature individuals; generally > 18 - 20 years of age)
- Skeletal abnormalities (i.e., fused ribs, cervical ribs, unfused vertebrae, etc.)
- Degenerative changes (i.e., osteophytic lipping, degenerative joint changes, diffuse idiopathic skeletal hyperostosis, etc.)
- Dystrophic calcifications
- Remote injuries with healing (i.e., fracture callus)
- Medical implants
- Orthopedic hardware
- Implanted medical devices
- Surgical clips / staples
- Dental radiographs (J Pharm Bioallied Sci 2015;7:S260)
- Dental implants / fillings
- Dental root morphology
- Unique bone features
- Unique anatomic findings
- May also be useful to exclude individuals
- Identification should not be based on a single unique feature but instead on an aggregate of multiple distinct features (Am J Forensic Med Pathol 2016;37:86)
Comment Here
Reference: Forensic radiology
- Accurate measurement of findings
- Angiography
- Detection of air and fluid collections
- Detection of metallic foreign bodies
- Detection of soft tissue injuries
Comment Here
Reference: Forensic radiology
- Forensic toxicology is the science that deals with the harmful effect of chemicals on the human body and the use of toxicology for the purpose of law (Clin Lab Med 2016;36:753)
- A drug is any substance which has a physiological effect when ingested or otherwise introduced into the body
- Drug intoxication is one of the most common nonnatural causes of death
- Toxicology results shall be interpreted in the context of a thorough medicolegal investigation
- Autopsy findings are generally nonspecific
- Toxicology can give information about toxic chemical levels that may have contributed to death
- Postmortem redistribution is a process in which drugs are redistributed into the blood from solid organs such as the lungs, liver and myocardium, and may affect the interpretation of substance levels
- Most common samples collected at autopsy are urine, blood, vitreous, gastric content and liver
- Prescribed medications: pharmaceutical drugs that require a medical prescription to be dispensed
- Over the counter medications: pharmaceutical drugs that can be obtained without a prescription
- Recreational drugs: legal and illegal substances used without medical supervision and taken for enjoyment or leisure purposes
- Drug levels
- Therapeutic / nontoxic: drug concentration that is usually expected to achieve the desired therapeutic effect or that does not cause damage to the body
- Toxic: drug concentration that can cause damage to the body but is not enough to cause death
- Lethal: minimum amount of a drug that is supposed to cause death
- Lethal levels may vary among individuals, and toxicological results need to be considered in the context of other investigative and autopsy evidence
- Screening test: a qualitative (presumptive) test that indicates intentional or unintentional exposure to a specific substance
- Involves the postmortem redistribution of drugs into the blood from adjacent solid organs with high drug concentrations, such as lungs, liver and myocardium, affecting the interpretation of substance concentration in the blood after death (Clin Toxicol (Phila) 2005;43:235)
- Blood sample from a peripheral site (e.g., femoral) less likely to be affected than that from a central site (torso)
- The greater the interval between death and sample collection, the more pronounced is the postmortem redistribution phenomenon (Forensic Sci Int 2012;219:265)
- Multiple factors determine the postmortem redistribution phenomenon
- Cell death: cessation of aerobic respiration and promotion of anaerobic metabolism, loss of structural integrity, enzymatic leakage into the cytoplasm with progressive degradation of cellular components and leakage in the extracellular space (Toxicol Pathol 2007;35:495)
- Decomposition: drugs are metabolized by microorganisms (Forensic Sci Med Pathol 2012;8:373)
- Passive diffusion from the stomach: if drug or alcohol is present in the stomach at the time of death, postmortem diffusion to the adjacent pericardial sac can occur (Am J Forensic Med Pathol 1996;17:1, Am J Forensic Med Pathol 1995;16:89)
- Substance properties: characteristics such as volume of distribution, lipophilicity and pKa are important factors related to specific drug postmortem redistribution (J Med Toxicol 2017;13:111)
- Body position after death: may explain differences in body concentrations from different sampling sites (e.g., regurgitation of gastric content into the airway) (Anal Toxicol 2003;27:533)
- Quality and quantity of the sample determine the reliability of the toxicological analysis
- Samples should be collected as soon as possible after death (Forensic Sci Res 2017;1:42)
- Not possible in most cases
- Body refrigeration helps in minimizing the postmortem processes
- Hospital samples may be available
- Most common postmortem samples and collection methods:
- Femoral blood (Toxicol Mech Methods 2010;20:363)
- Generally by blind puncture on the groin area or local dissection
- Considered the most reliable specimen for postmortem analysis
- Urine (Can Fam Physician 2013;59:50)
- Suprapubic puncture or by catheter if external examination only
- Bladder focal dissection in situ and urine collection if autopsy
- Vitreous
- Puncture and aspiration of gelatinous contents of the posterior chamber of the eye (Acad Forensic Pathol 2016;6:12)
- Gastric content
- Collect the content in a proper container from the esophagus or cut a small hole in the gastric wall
- Record the amount of gastric content
- Check for the presence of pills or foreign bodies
- If no gastric content is present, a sample of the gastric wall should be collected
- Liver
- Major metabolic organ
- Collect samples after evisceration
- Femoral blood (Toxicol Mech Methods 2010;20:363)
- Less common or special postmortem specimens (Forensic Sci Res 2017;1:42)
- Other organs: usually collected to search for specific substances or if other samples are not available
- Lung: volatile compounds (Forensic Sci Res 2017;2:192)
- Spleen: analysis of compounds that bind to hemoglobin, such as carbon monoxide and cyanide (Forensic Sci Int 2018;291:94)
- Brain: especially for substances acting on the central nervous system (J Anal Toxicol 2015;39:137)
- Bile: qualitative analysis, if urine is not present (screening purposes) (Acad Forensic Pathol 2018;8:324)
- Muscle: reliable specimen in case of advanced decomposition, charred bodies, exhumation and exsanguination (Forensic Sci Int 2021;325:110901)
- Hair: chronic substance abuse (Curr Pharm Des 2017;23:5480)
- Cavity blood / fluids: if other body fluids are not available
- Blood clots: fire related deaths when blood is not available
- Fly larvae (maggots) (J Forensic Leg Med 2019;67:28)
- Entomotoxicology: the study of the usefulness of insects as alternative toxicological samples
- Reliable toxicological specimen in case of advanced decomposition, when conventional samples are not available
- Mostly for qualitative analyses
- Other organs: usually collected to search for specific substances or if other samples are not available
- Sealed in proper containers
- Should be labeled with the following information:
- Subject identification
- Collector identification
- Type of specimen
- Collection site
- Amount
- Date
- Short term: keep at 4 °C
- Long term: keep at -20 °C to -80 °C
- Hair samples: room temperature
- Reference: Forensic Sci Res 2017;1:42
- Tests used for presumptive and confirmatory analyses of substances in the specimens collected during autopsy
- Screening tests
- Presumptive or qualitative
- Urine is the most commonly used specimen for screening tests
- Indicates intentional or unintentional exposure to a specific substance
- Need to be confirmed by more accurate analyses
- Urine dipstick (Harm Reduct J 2017;14:52)
- Very easy to use, quick to check and relatively inexpensive
- Includes numerous drug panels (opiates, benzodiazepines, methadone, cocaine, amphetamines, methamphetamines, marijuana [THC], phencyclidine, tricyclic antidepressant [TCA], barbiturates)
- Have limits of detection, below which a substance cannot be detected
- Possible false positive due to substance cross reactions
- Confirmatory tests
- Quantitative analyses
- Necessary to correlate the analyte concentration with the presumed effect on the body
- Blood is the most commonly used specimen for confirmatory tests
- In the absence of blood, vitreous is the next preferred sample
- Mass spectrometry, coupled either to gas chromatography or liquid chromatography (Harm Reduct J 2017;14:52)
- Expensive (machine and consumable materials)
- Requires intermediate level of expertise
- Can identify virtually any substance
- Provides information about the molecular mass and isotopic abundance of elements
- Only a very small sample size is required
- Tested samples are generally destroyed by the testing process (with few exceptions)
- Quantitative analyses
- Category: opioid, CNS depressant
- Metabolism:
- Rapidly (t1/2: 2 - 6 min) metabolized into 6-monoacetylmorphine (MAM) - in vivo or in vitro
- Slower (t1/2: 6 - 25 min) metabolism into morphine
- Will generally be detected as morphine in postmortem toxicology
- Mechanism of death: respiratory depression (StatPearls: Heroin Toxicity [Accessed 24 February 2022], Br J Anaesth 2008;100:747)
- Binds to and activates specific receptors in the brain:
- Mu: stimulation causes respiratory depression, analgesia (supraspinal and peripheral) and euphoria
- Kappa: analgesic effects, disassociation, hallucinations and dysphoria
- Delta: analgesic effects, modulate mu receptors and are thought to influence mood
- Tolerance to respiratory depression is less than complete and may be slower than tolerance to euphoria and other effects
- Produce inhibition at the chemoreceptors via mu opioid receptors and in the medulla via mu and delta receptors causing respiratory depression
- Binds to and activates specific receptors in the brain:
- Best samples at autopsy
- Urine (screening)
- Blood (quantification)
- Vitreous humor (extended window of detection for 6-acetylmorphine [6AM]) (Forensic Sci Int 2013;226:152, J Forensic Sci 2020;65:570)
- Autopsy findings
- Needle marks
- Local dissection of the skin may show underlying soft tissue hemorrhage in doubtful cases
- Pulmonary edema
- Association with endocarditis (from use of unclean needles)
- Septic emboli can travel to diverse regions of the body
- Needle marks
- Histopathology findings
- No specific histologic findings
- Toxicology (Forensic Sci Int 2012;215:18, Pharmazie 2003;58:447)
- Therapeutic levels (for morphine)
- 10 mg IV dose = plasma concentration 0.01 - 0.1 mg/L
- Lethal levels (heavily dependent on decedents history of use)
- Morphine: 0.04 - 5.5 mg/L
- 6-MAM: 0.01 median; 0.06 mg/L (97th percentile) (blood)
- Therapeutic levels (for morphine)
Cocaine
- Category: CNS stimulant
- Metabolism: rapidly (t1/2: 0.7 - 1.5 h) metabolized into benzoylecgonine
- When coadministered with alcohol = cocaethylene (produced in the liver whether cocaine and alcohol are both metabolized)
- Mechanism of death: arrhythmias and cardiotoxic effects
- Binds to and activates specific receptors
- Stimulation of adrenergic receptors: vasoconstriction in both cardiac and peripheral vasculature, tachycardia
- Inhibition of CNS serotonin and dopamine: euphoria and addictive effects
- Sodium (Na+) channel blockade - slow Na+ current in cardiac myocytes and local anesthetic properties
- Increases cardiac rate, blood pressure and cardiac contractility (all of which increase myocardial oxygen demand), while causing vasoconstriction, platelet adherence, thrombus formation and coronary spasm (all of which simultaneously decreases oxygen supply), resulting in myocardial ischemia and infarction (Cureus 2021;13:e14594)
- Effect on Na+ channels lead to prolongation of QRS complex, which is arrhythmogenic
- Binds to and activates specific receptors
- Best samples at autopsy
- Urine (screening)
- Blood (quantification)
- Vitreous (for screening) (J Anal Toxicol 2000;24:59)
- Autopsy findings (possible but not required)
- Myocardial infarction
- Spontaneous coronary artery dissection is a potential complication of cocaine use (Cardiovasc Pathol 2001;10:141)
- Cerebrovascular accidents
- Myocardial infarction
- Histopathology findings (possible but not required)
- Myocarditis
- Contraction band necrosis
- Alveolar hemorrhages from airway injury (if smoked)
- Eosinophilic pneumonia (if smoked)
- Overall ischemia related changes (from vasoconstriction / thrombus formation)
- Toxicology
- Cocaine may exhibit postmortem redistribution
- Lethal levels (Am J Forensic Med Pathol 2011;32:71)
- Cocaine: 0.01 - 78 mg/L
- Benzoylecgonine: 0.02 - 90 mg/L
- Dependent on dose, method of administration, period of survival and combination with other substances
Methamphetamine / amphetamine
- Category: CNS stimulant
- Metabolism: amphetamine
- Mechanism of death: cardiovascular complications
- Interacts with monoamine transport proteins in the CNS to enhance the release and prevent reuptake and degradation of monoamine neurotransmitters such as serotonin, dopamine and norepinephrine (Front Neuroanat 2019;13:48)
- Results in a surge of adrenergic stimulation
- Stimulated alpha and beta adrenergic receptors produce hypertension, tachycardia, hyperthermia and vasospasm that can lead to multiple cardiovascular complications, including cardiac arrhythmias, acute coronary syndrome and cerebrovascular accidents
- Best samples at autopsy
- Urine (screening)
- Blood (quantification)
- Autopsy findings
- Needle marks
- Local dissection of the skin may show underlying soft tissue hemorrhage in doubtful cases
- Myocardial infarction
- Complications from increased blood pressure
- Cerebrovascular pathology (especially hemorrhagic strokes and aneurysm ruptures)
- Aortic rupture
- Needle marks
- Histopathology findings (Addiction 2008;103:1353)
- Cardiovascular pathology
- Cardiomegaly, hypertrophy, atherosclerosis, ischemic heart disease, etc.
- Methamphetamine use may cause the premature and accelerated development of cardiovascular disease and exacerbate pre-existing pathology
- Cardiovascular pathology
- Toxicology (Forensic Sci Int 2007;170:163, CUNY Academic Works: Investigation of Postmortem Methamphetamine Cases Submitted to the New York City Office of Chief Medical Examiner [Accessed 25 February 2022], J Occup Environ Med 2002;44:435)
- May exhibit postmortem redistribution
- Therapeutic levels
- Amphetamine: 0.02 - 0.1 mg/L
- Toxic levels
- Amphetamine: > 0.2 mg/L
- Lethal levels
- Amphetamine: 0.24 - 11 mg/L
- Methamphetamine: 0.02 - 15 mg/L
- Other
- Illicit methamphetamine will consist of a racemic mixture (d and l enantiomers)
- Certain inhalers, decongestants and prescription drugs can metabolize or contain a specific enantiomer of methamphetamine and since standard confirmatory assays are unable to differentiate between the 2 chiral molecules, postmortem toxicology results will show up as methamphetamine (J Occup Environ Med 2002;44:435)
- Common examples include Vicks inhalers, selegiline, famprofazone
Ethanol (EtOH)
- Category: CNS depressant
- Metabolism: primarily metabolized in the liver (by alcohol dehydrogenase) into acetaldehyde
- Mechanism of death:
- Acute ethanol intoxication: respiratory depression (J Intensive Care Med 2004;19:183)
- Binds to GABA and glycine receptors: potentiating release of inhibitory neurotransmitters
- Interacts with N-methyl-D-aspartate (NMDA) receptors: inhibiting glutamate release (primary CNS excitatory neurotransmitter)
- Directly suppresses the respiratory center in the medulla oblongata (dose dependent), leading to respiratory depression
- Induces metabolic abnormalities: including lactic acidosis, hypoglycemia, hypokalemia, hypomagnesemia, hypocalcemia and hypophosphatemia, which can lead to atrial and ventricular tachydysrhythmias, metabolic (keto) acidosis and seizures
- Chronic ethanolism - complications of chronic liver disease
- Chronic ethanol use is known to induce many neuroadaptive changes in the CNS involving both glutamatergic and GABAergic synaptic transmission
- Number of GABA receptors increases, as well as the function of NMDARs and in NMDAR mediated glutamatergic synaptic transmission, requiring more and more alcohol to create the same level of inhibition
- Increased ethanol consumption levels lead to increased hepatotoxicity, mediated through metabolism to acetaldehyde, a well known hepatotoxic molecule (Clin Liver Dis 2019;23:71)
- Ketoacidosis can also develop in chronic alcoholics with poor nutritional intake
- High levels of ketone bodies in body fluids, namely acetone, acetoacetate and particularly b-hydroxybutyrate
- Most ultimately succumb to systemic complications of chronic liver disease
- Withdrawal (StatPearls: Delirium Tremens [Accessed 25 February 2022])
- After discontinuation of chronic alcohol consumption, there is loss of the GABA inhibitory effect with potentiation of NMDA excitatory effects, leading to CNS hyperstimulation
- Delirium tremens is the most severe form, leading to significant autonomic dysfunction and vital sign abnormalities that can result in cardiovascular collapse and seizures
- Acute ethanol intoxication: respiratory depression (J Intensive Care Med 2004;19:183)
- Best samples at autopsy
- Urine (screening)
- Blood (quantification)
- Vitreous (more stable in decomposing or embalmed bodies) (Forensic Sci Int 2007;165:10)
- Autopsy findings
- Acute ethanol intoxication
- Acute pancreatitis
- Pulmonary edema
- May have no specific findings
- Chronic ethanolism
- Hepatic steatosis / cirrhosis
- Dilated cardiomyopathy
- Ascites
- Jaundice
- Ecchymosis
- Lower extremity edema
- Cerebellar vermis atrophy
- Atrophy / infarction of mammillary bodies (Wernicke-Korsakoff syndrome)
- Acute ethanol intoxication
- Histopathology findings
- Acute ethanol intoxication
- Acute hepatitis / pancreatitis
- Pulmonary edema
- Central pontine demyelination (can be seen with rapid correction of hyponatremia during attempted resuscitation of decedents that die after presenting to the emergency department)
- Chronic ethanolism
- Cirrhosis - hepatic nodular fibrosis
- Macrovesicular steatosis
- Periportal chronic inflammation
- Atrophy / infarction of mammillary bodies (Wernicke-Korsakoff syndrome)
- Acute ethanol intoxication
- Toxicology - all levels heavily dependent on tolerance
- Does not exhibit significant postmortem redistribution
- Therapeutic levels
- 100 - 150 mg/dL
- Ensures saturation of alcohol dehydrogenase in ethylene glycol and methanol poisonings in order to prevent conversion into toxic metabolites (formic acid or formate anions) (Clin Toxicol (Phila) 2015;53:797)
- Toxic levels (Eur J Intern Med 2008;19:561)
- > 50 mg/dL
- Lethal levels (Leg Med (Tokyo) 2013;15:122, Forensic Sci Int 2003;135:206)
- Acute ethanol toxicity: 74 - 680 mg/dL (mean: 364 mg/dL)
- Other
- Alcohol can be endogenously produced in decomposing bodies from microbial activity and fermentation of glucose (Forensic Sci Int 2007;165:10)
- Low concentrations (usually < 30 mg/dL)
- Supporting evidence of alcohol in urine and vitreous humor proves useful for comparison in such cases
- Ethanol > 10 mg/dl in blood or in chest fluid but < 10 mg/dl in vitreous or urine should be considered as endogenous production (Leg Med (Tokyo) 2013;15:122, J Forensic Sci 1982;27:549)
Fentanyl
- Category: synthetic opioid, CNS depressant
- Metabolism: norfentanyl
- Mechanism of death: respiratory depression (Br J Anaesth 2008;100:747)
- Binds to and activates specific receptors in the brain:
- Mu: stimulation causes respiratory depression, analgesia (supraspinal and peripheral) and euphoria
- Kappa: analgesic effects, disassociation, hallucinations and dysphoria
- Delta: analgesic effects, modulate mu receptors and are thought to influence mood
- Fentanyl rapidly crosses the blood brain barrier, resulting in greater analgesic potency than natural opioids
- Street heroin is often contaminated with unknown amounts of fentanyl, making it dangerous to unsuspecting users
- Fundamental drive to breathe is generated in the brainstem and modulated by inputs from the cortex, brainstem and peripheral (carotid and aortic bodies) chemoreceptors that sense changes in the chemical constituents of blood
- Inhibition of the chemoreceptors, via mu opioid receptors and in the medulla via mu and delta receptors, causes respiratory depression
- Binds to and activates specific receptors in the brain:
- Best samples at autopsy
- Screening
- Urine
- Vitreous humor
- Brain tissue (high affinity / higher than circulating levels) (Forensic Sci Int 2019;305:109999)
- Blood (currently preferred)
- Liver tissue
- Higher levels but less prone to postmortem redistribution (Clin Biochem 2013;46:598)
- Screening
- Autopsy findings
- Needle marks
- Local dissection of the skin may show underlying soft tissue hemorrhage in doubtful cases
- Pulmonary edema / congestion
- Needle marks
- Histopathology findings
- Pulmonary edema / congestion
- Toxicology
- May exhibit postmortem redistribution
- Therapeutic levels (Drugs 2017;77:747)
- Opioid naïve patients experience rapid and effective analgesia at minimum plasma concentrations between 0.6 - 1.5 μg/L
- Used for pain control, primarily in postsurgical and cancer patients
- Toxic levels
- Blood: 3 - 20 μg/L
- Liver: 23 - 56 μg/kg (Clin Biochem 2013;46:598)
- Lethal levels
- Blood: 3 - 383 μg/L (mean 25 μg/L) (J Anal Toxicol 2006;30:603)
- Liver: > 56 μg/kg (Clin Biochem 2013;46:598)
- Collect blood and liver samples to run toxicology studies before signing out the case
- Rib fractures are evidence of blunt force trauma; stop the examination and contact the medical examiner's office
- Document all the findings and sign out the case as a natural death
- Take a photo of the pills found in the gastric content, collect them with blood and liver samples and contact the medical examiner's office
- Document all the findings and contact the medical examiner's office
Comment Here
Reference: Forensic toxicology
- Accidental air embolism following intravenous drug injection
- Acute subarachnoid hemorrhage
- Benzodiazepines toxicity
- Cocaine intoxication
- Opiate overdose
Comment Here
Reference: Forensic toxicology
- Gunshot wounds occur when a bullet hits the body, producing injuries
- One of the most common causes of death and injury
- Severity of injuries depends on multiple factors, including the type of weapon and bullet and the affected body area
- May result in severe tissue and organ damage with sudden incapacitation, profuse bleeding, fractures and death
- Determining the range of fire is one of the most critical parts of the forensic pathologist activity; secondary effects of the discharge surrounding the entrance wound (muzzle imprint, soot deposition, stippling or blackening of the skin edges) can help estimate the firing range
- Entrance wounds can be round, oval or irregular (atypical); an abrasion ring is almost always present
- Exit wounds are usually irregular and there is no abrasion ring in the vast majority of cases; there are no secondary effects of the discharge
- Wound mechanism and injury severity are mostly related to the kinetic energy transferred by the bullet to the tissues with the development of 2 cavities within the body: the permanent and temporary cavities
- At autopsy, it is essential to provide proper documentation (by photographs and body diagrams) of the gunshot wound's features
- Science that pertains to firearms and bullets; can further be classified as:
- Internal ballistics: what happens within the firearm from the deflagration to the exit of the bullet from the barrel
- External ballistics: the behavior of the bullet while traveling from the firearm to the final target
- Terminal ballistics: what happens when the bullet hits the final target; if the final target is a biological one, the term wound ballistics is used (Eur J Trauma Emerg Surg 2017;43:579)
- Firearms of forensic interest can be generally classified as:
- Handguns (pistols and revolvers)
- Long guns (shotguns and rifles)
- Rifled: the barrel contains spiral lands and grooves into the inside of the barrel that grips the bullet as it exits the firearm, providing spin and stabilization along its path
- Smoothbore: the barrel is not rifled; typically found in shotguns
- Low velocity: usually fires at less than 1,000 ft/sec (Bull Emerg Trauma 2016;4:65)
- High velocity: usually fires at more than 1,000 ft/sec (Bull Emerg Trauma 2016;4:65)
- During its travel, the bullet is subject to rotational forces causing:
- Yawing: oscillation of the bullet along its longitudinal axis (Forensic Sci Med Pathol 2009;5:204)
- Tumbling: bullet loses its gyroscopic stability, presenting a continually changing surface to the direction of motion (Forensic Sci Med Pathol 2009;5:204)
- Precession: rotation of the bullet around the center of mass (Forensic Sciences Research 2020;5:1)
- Nutation: circular movement of the tip of the bullet (Forensic Sciences Research 2020;5:1)
- When the bullet hits the biological target, it transfers its energy to the body, resulting in injuries
- Kinetic energy: the energy possessed by an object due to its motion; a function of the object's mass (M) and velocity (V): KE = 1/2 MV2
- While the bullet's mass plays an important role in gunshot wounds, the most critical variable is the bullet velocity; doubling the velocity will quadruple the kinetic energy
- Types of gunshot wounds:
- Penetrating wounds: the bullet enters the body but does not exit
- Perforating wounds: the bullet enters and exits the body
- Re-entry wounds: the bullet passes through a body segment, exits and re-enters the body (Int J Legal Med 2009;123:419)
- Graze / tangential wounds: the bullet strikes the skin at a shallow angle, producing a superficial wound (Acad Forensic Pathol 2016;6:291)
- Entrance wounds: point where the bullet enters the biological target
- General features:
- Abrasion ring: a reddish brown abrasion on the skin surrounding the gunshot wound of entrance
- Greasy rim or bullet wipe is a dirt collar due to the lubricant carried on the bullet
- Inverted edges: due to the bullet movement inside the body
- Smaller than bullet caliber (usually): due to the elastic recoil of the affected tissues
- Shape
- Round (circular) shape: suggests a perpendicular discharge with respect to the skin
- Oval shape: suggests an acute angle of fire with respect to the skin
- Atypical or irregular shape: indicates loss of stability of the bullet before hitting the target or hard contact gunshot wounds to the skin overlying bone (i.e. skull) (Am J Forensic Med Pathol 2012;33:250)
- Range of fire: determination by estimating the distance from the muzzle of the weapon to the target; specific findings on the skin (secondary effects of the discharge) surrounding the entrance wound can help determine the range of fire
- Thermal effect: due to the gas and flame produced by the deflagration; flames cause searing of the skin and regional hairs
- Soot deposition: due to the carbon produced by combustion of the gunpowder that exits the barrel and deposits on the skin surrounding the entrance wound; can be wiped out by cleaning the body
- Stippling (or powder tattooing): red to orange or brownish punctate abrasions surrounding the entrance wounds as a result of pieces of gunpowder expelled from the barrel and striking the skin; can't be wiped out by cleaning the body
- Pseudostippling: punctate abrasion due to fragmented bullets or fragments of a damaged intermediate target interposed between the firearm and the target (Am J Forensic Med Pathol 2003;24:243)
- Contact wounds: firearm is in contact with the target at the time of discharge
- Loose contact: circular wound with blackened, seared skin margins
- Hard contact: gas expansion within the subcutaneous tissues may result in a muzzle imprint (abrasion resembling the shape of the muzzle = Werkgartner mark) or in an irregular, stellate appearance with a central defect and radiating lacerations (typically seen in gunshot wounds to the head) (Arch Kriminol 2009;224:145)
- Near contact wounds: firearm is not in contact with the target but is held a very short distance from it (usually < 1 cm)
- Entrance wound may show soot deposition and burn / seared edges; small amount of powder stippling can be present (Forensic Sci Int 2003;138:68)
- Intermediate range: distance between the firearm and the target increases but is still short enough to allow secondary effects of the discharge; distance depends on firearm type (usually from a few centimeters up to several feet)
- Hallmark is the presence of stippling (or powder tattooing) on the skin surrounding the entry wound (Arch Pathol Lab Med 2006;130:1283)
- Greater distance = larger area of stippling but its density will decrease
- Distant range: firearm is at a distance (many feet) from the target so there will be only the gunshot wound of entrance due to the mechanical action of the bullet
- There must be no stippling
- Usually round or oval, depending on the angle of discharge
- If there is an intermediate target between the firearm and the target, close or intermediate gunshot wounds can be confused with distant ones
- In the absence of reliable evidence of a distant range gunshot wound, it is preferable to classify it as an indeterminate range
- General features:
- Wound channel: path of the bullet within the body; after hitting the target, the bullet releases its energy to the body and creates 2 cavities (J Trauma 1985;25:522)
- Permanent cavity: primary wound channel caused by the tissue damage due to the bullet passage through the body; the final injury that can be observed at autopsy
- Temporary cavity: while the bullet travels through the body, the permanent cavity is stretched, causing progressive pulsations and contractions
- Energy is transferred to the surrounding tissues, causing damage even far from the primary bullet path
- After a variable amount of time, the temporary cavity collapses into the permanent cavity due to the elastic recoil of the biological tissues
- Temporary cavities are not identifiable at autopsy but effects can be observed on tissues and organs surrounding the permanent cavity
- Exit wounds: point where the bullet leaves the body
- Generally, an exit gunshot wound is more irregular in shape than entry wound
- Skin is perforated from the inside out, causing eversion of skin tags and protrusion of tissue from the defect
- Exit wounds do not show soot deposition, muzzle imprint, stippling or blackening of the skin edges
- Can be slit-like lesions that can mimic a stab wound
- Shored exit wound is one in which the skin is in contact with another object when the bullet exits (a belt, a wall, etc.); this causes an irregular area of abrasion on the skin, which can be confused with the abrasion ring of an entrance wound (Am J Forensic Med Pathol 2000;21:220)
- When a shotgun is fired, a compact mass of shot or pellets emerges from the muzzle; dispersion is directly related to the distance increase
- Shotguns are usually smoothbore and fire pellets
- Most common shotgun pellets:
- Birdshots: smallest type of shotgun pellets; small, metal spheres
- Buckshot: larger metal spheres, giving greater weight and force to each pellet
- Some shotguns are rifled and fire slugs
- Slug: single, large projectile with high energy and penetration ability (Rom J Leg Med 2014;22:237)
- Entrance wounds (Am J Forensic Med Pathol 2007;28:99)
- Contact range: up to a few feet, the entrance wound is a single, round defect because the pellets penetrate the target as a single mass; soot deposition can be present, usually in a greater amount than the one produced by handguns
- Near contact: soot deposition, searing, reddish brown rim or skin blistering; wound is still round and regular
- Short distance: at a range of 3 - 4 feet, the pellets begin to spread out before reaching the body, producing one large entry wound that shows serrated or crenated edges (scalloping or rathole appearance)
- Intermediate to distant range: as the range increases, the central defect becomes smaller and is surrounded by several satellite pellet holes, which increase with the increasing distance; when the shotgun is far enough from the target, there will be no central defect but just pellet holes
- Wound channel
- Shape of the pellets does not allow for their stabilization, resulting in lower penetration ability
- In distant shotgun wounds, most of the damage is due to the permanent cavity, while there is a negligible secondary cavity effect
- In contact shotgun wounds, the secondary cavity effect is significant (i.e. intraoral shotgun wound)
- Exit wounds
- Shotguns firing pellets rarely produce exit wounds and mostly when fired at contact or short distance
- Slugs frequently produce exit wounds, since they are comparable to high velocity missiles with high penetration ability
- Generally used in the military field
- High velocity missiles: the secondary cavity effect accounts for the vast majority of the damage (J Trauma Acute Care Surg 2019;87:690)
- In contact wounds of the head with centerfire rifles, there is massive tissue destruction of the skin, skull and brain with a heterogenous pattern of entrance and exit wounds (Leg Med (Tokyo) 2016;23:10)
- Full metal jacketed bullets produce less tissue damage and tend to travel through the body undeformed
- Semijacketed ammunition creates the classic lead snowstorm appearance on Xray due to the peeling back of the jacket as it travels through the body, releasing numerous, small lead fragments
- In perforating gunshot wounds to the head, entrance and exit wounds show a typical feature called beveling, distinguishing between entrance and exit
- Beveling is a sort of cone shaped bone erosion in the direction of the bullet path through the cranial vault
- Entrance wounds can be round / oval or stellate in shape and show an internal beveling (bone erosion in the inner part of the bony table) (J Forensic Sci 1991;36:1592)
- Exit wounds are usually irregular and show an external beveling (bone erosion on the outer part of the bony table)
- Fragments of bone travel in the direction of the bullet path through the cranial vault
- In the skull, gunshot wounds often produce numerous fractures due to rapidly increasing pressure as the bullet travels through the skull
- Gunshot wounds to other flat bones can produce similar effects
- Keyhole lesion: a single bone defect that shows both entrance and exit wound morphologies due to a bullet that strikes the skull at a shallow angle (Australian Journal of Forensic Sciences 2014;46:258)
- Distinguishing between entrance and exit wounds and determining the direction of fire can be challenging
- Even if the bullet does not penetrate into the cranial cavity, its energy is still transferred to the bone and central nervous system, resulting in fractures and severe damage
- Scene investigation
- Before examining the body, observe, take photographs and document the environment
- Avoid any unnecessary procedures that can alter the scene or the body
- Search for a suicide note, medications and the weapon on the scene (Am J Forensic Med Pathol 1999;20:1)
- Analyze the blood spatter: passive stains, transfer stains or impact stains can give clues about the dynamic of the event (Data Brief 2018;22:269)
- Postmortem imaging
- Usually performed before the autopsy to detect and locate potential bullets or their fragments
- At least an Xray study should be performed in every gunshot wound death, since bullets or fragments need to be collected at the time of autopsy
- Postmortem computer tomography (virtopsy) gives more accurate information about the location of the bullet / fragments, providing a 3D view of the body; also allows for software manipulation of the CT scans (taking measurement, adding virtual probes, 3D reconstruction or other tools) (Leg Med (Tokyo) 2014;16:357)
- External examination and autopsy
- It is essential to provide a proper documentation (by photographs and body diagrams) and description of the following (Arch Pathol Lab Med 2006;130:1283):
- Body conditions before any alteration
- Clothes
- Entrance wound, wound channel and exit wound features
- Direction of fire: give 3 directions according to the main body axis (left / right, front / back and top / bottom)
- Any possible bullet or bullet fragments that are recovered within the body: the location must be reported and the bullet should not be recovered using metal forceps or other metal tools to avoid creating artificial marks on its surface
- Extremities: a small, linear abrasion / bruise can be present on the interdigital groove between the thumb and index finger (Felc mark), which can be due to the pinching of the skin between the sliding barrel and the handgrip; may suggest that the subject fired the shot
- It is essential to provide a proper documentation (by photographs and body diagrams) and description of the following (Arch Pathol Lab Med 2006;130:1283):
- Microscopic examination
- Rarely needed (Am J Forensic Med Pathol 2012;33:231)
- Used to distinguish between the entrance and exit gunshot wounds in unclear cases
- Entrance wound: cell compression, nuclear streaming, epidermis and dermal thermal injury with coagulative necrosis of keratinocytes, dermoepidermal disjunction, hemorrhage (a sign of vitality); gunshot residues can be observed as a black granular material progressively decreasing from the entrance to the exit wound (Am J Dermatopathol 2016;38:566)
- Exit wound: fragments of bone, adipose tissue and muscle can be found, oriented toward the exit (J Forensic Leg Med 2014;25:49)
- Manner of death determination
- Suicide note, history of mental illness and weapon on the scene support suicide; however, an offender can place the weapon in the victim's hand or close to the body to simulate suicide (J Clin Diagn Res 2017;11:HD01)
- Multiple gunshot wounds generally support homicide; however, the subject may retain a certain amount of ability to act after multiple gunshot wounds (even when the head is involved) if targets of immediate incapacitation are spared (J Forensic Sci 2015;60:1373)
- Accidental fatal gunshot wounds are rare
- 14 year old boy with tandem bullet wounds (Acad Forensic Pathol 2016;6:130)
- 28 year old man with atypical exit shotgun wound (Forensic Sci Int 2017;275:e1)
- 63 year old man suffers homicide by intraoral gunshot wound (Forensic Sci Med Pathol 2011;7:209)
- 2 cases of tandem bullets (Am J Forensic Med Pathol 2019;40:262)
- Suicide by 8 gunshot wounds to the head (J Forensic Sci 2015;60:1373)
- Bullet embolism (J Forensic Leg Med 2016;42:33)
Contributed by Lorenzo Gitto, M.D. and Robert Stoppacher, M.D.
- DiMaio: Gunshot Wounds - Practical Aspects of Firearms, Ballistics, and Forensic Techniques, 3rd Edition, 2015, Knight: Knight's Forensic Pathology, 4th Edition, 2015, Brooks: Ryan's Ballistic Trauma - A Practical Guide, 3rd Edition, 2011, Dolinak: Forensic Pathology - Principles and Practice, 1st Edition, 2005, Spitz: Spitz and Fisher's Medicolegal Investigation of Death, 4th Edition, 2005
- Caliber of the bullet
- Kinetic energy of the bullet
- Location of the injury
- Shape of the bullet
- Weight of the bullet
The weight and the velocity of the bullet are the most critical variable in determining the amount of kinetic energy. Doubling the mass doubles the energy, while doubling the velocity quadruples it. However, the wound's ultimate extent and severity are determined by the kinetic energy released to the body at the moment of the impact. The higher the kinetic energy transferred to the tissues, the greater the temporary cavity size is and the most severe is the resulting injury. The wound's morphology and size (especially on the bone) may give information about the bullet caliber and shape but caution is recommended in any attempt to determine precise bullet caliber from the wound examination alone. Gunshot wounds can show different features based on the affected body area but their severity is still mainly due to the amount of energy transmitted to the body.
Comment Here
Reference: Gunshot wounds
The finding above is observed at the autopsy of a 34 year old Caucasian man. Which of the following is correct regarding this gunshot wound?
- Its morphological features are indicative of an exit gunshot wound
- It results from a bullet fired from a long distance at an acute angle of fire with respect to the skin
- There was an intermediate target between the muzzle of the firearm and the body
- This wound typically occurs in hard contact gunshots to the head
- Weapon was not in contact with the target but was held a very short distance from it
Hard contact gunshot wounds to specific body areas may result in a peculiar patterned injury, called muzzle imprint, surrounding the central defect. When the weapon is pressed firmly and fired against a body area covered only by a thin layer of skin and subcutaneous tissue overlying the bone (such as the head), the gases produced by the detonation enter the body together with the bullet. The gases accumulate between the skin and the bone, causing a sudden expansion of the subcutaneous tissues. The skin is forced to balloon outward and push against the weapon muzzle, producing a typical abrasion / bruise that resembles the muzzle's shape. When the expansion exceeds skin elasticity and resistance, it will tear, resulting in an entrance gunshot wound with a stellate or irregular appearance.
Comment Here
Reference: Gunshot wounds
- Process that involves analyzing and constructing hypotheses of the identity of human remains and reconciling the information collected using several lines of evidence by comparing antemortem and postmortem data (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- Scientific / comparative methods of identification:
- Fingerprint comparison
- Comparative dental radiography
- Surgical hardware and implants (with unique numbers)
- Radiographic comparison
- Deoxyribonucleic acid (DNA)
- Nonscientific methods of identification:
- Circumstantial evidence:
- Jewelry
- Clothing
- Eyeglasses found on body
- Location of the body (residence, car registered to an individual)
- Dentures
- Medical alert bracelets
- Papers or identification cards found with the body
- Visual identification
- Distinctive marks:
- Tattoos
- Scars
- Piercings
- Birthmarks
- Other cutaneous lesions
- Physical attributes:
- Biological sex
- Apparent age
- Apparent ethnicity
- Body length
- Body weight
- Acquired and congenital anomalies
- Prior surgeries or medical procedures
- Head hair color (caution: can be dyed)
- In skeletal remains, a biological profile needs to be completed by an anthropologist
- Circumstantial evidence:
- Disaster victim identification process:
- Phase 1: scene (processing human remains and property at the disaster site)
- Phase 2: postmortem (detailed examination of human remains in mortuary)
- Phase 3: antemortem (collection of missing person data from various sources)
- Phase 4: reconciliation (matching postmortem and antemortem data)
- Mass disaster identification
- Mass casualty identification
- Identification is paramount in death investigation systems
- Those that have died in the community and enter the death investigation system are often unknown to the coroner or medical examiner that is investigating their death; the coroner or medical examiner must therefore rely on other means to determine identification
- The integrative process of identification begins at the death scene where human remains are discovered; the location, wallet containing official identification cards, physical appearance can be used to formulate a hypothesis of identity (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- All information should be documented and recovered from the scene before it is lost and the surrounding location changed forever (ICRC: Forensic Identification of Human Remains [Accessed 6 October 2022])
- It is imperative that confirmation bias be recognized and mitigated to avoid misidentification
- Identification should be supported by lines of evidence based on technical opinion or the decision of experts (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- Description of the method used for identification must be documented (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Identification is positive if achieved when the consistency of individualizing traits and lack of excluding discrepancies is sufficient to conclude that the individual in question is the expected person (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- The opinion of multiple experts may be required; these may include forensic pathologists, forensic anthropologists, law enforcement, radiologists, forensic dentists and forensic biologists (ICRC: Forensic Identification of Human Remains [Accessed 6 October 2022])
- Established procedures exist for identification of the deceased and are classified into scientific and nonscientific methods (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Comparative fingerprint analysis, comparative dental analysis and DNA analysis are the most reliable identifiers; however, nonscientific identifiers such as physical attributes, distinctive marks, medical findings, medical records and circumstantial evidence are usually the starting place in identification and are often used in conjunction with or to complement the primary identifier (Forensic Sci Criminol 2016;1:1)
- All lines of evidence are important and need to be considered; however, not all lines of evidence carry the same weight (i.e., hair color consistency but fingerprint incompatibility) (ICRC: Forensic Identification of Human Remains [Accessed 6 October 2022])
- To avoid preanalytical errors, it is the pathologist's responsibility to ensure that proper tagging of the body has occurred prior to commencing the autopsy (DiMaio: Handbook of Forensic Pathology, 2nd Edition, 2006)
- Every unidentified individual should be assigned a unique alphanumeric identifier to ensure that all individuals involved are referring to the correct case (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- During the autopsy, physical characteristics, clothing and personal belongings should be documented and photographed (ICRC: Forensic Identification of Human Remains [Accessed 6 October 2022])
- Review missing person data reports, including information collected from multiple sources containing the physical and medical profiles and circumstantial information related to their disappearance (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Families should be notified regarding identification of their loved ones before the public and media (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Body should not be released for burial until all attempts at identification have been exhausted (ICRC: Forensic Identification of Human Remains [Accessed 6 October 2022])
- After exhaustive comparison and investigation, it may be impossible to confirm the identity of human remains (ICRC: Forensic Identification of Human Remains [Accessed 6 October 2022])
- Identification of unknown deceased and human remains is critical for ethical, legal and humanitarian reasons
- Identify deceased individuals and notify families
- Establish identification for legal and statistical reasons
- Administrative record of an individual's death (death certificate and official records)
- Record of identity for ceremonial and burial practices
- To allow for legal proceedings
- Reference: INTERPOL: Disaster Victim Identification (DVI) [Accessed 6 October 2022]
- Circumstantial evidence:
- Items, personal effects or the location associated with a deceased individual (Forensic Sci Int Synerg 2021;3:100154)
- Jewelry
- Clothing
- Eyeglasses found on body
- Location of the body (residence, car registered to an individual)
- Dentures
- Medical alert bracelets
- Papers, identification cards found with the body
- Family members and friends are excellent resources (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- Limitation:
- Personal effects can be variably present
- Circumstantial evidence should be interpreted in the appropriate context (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
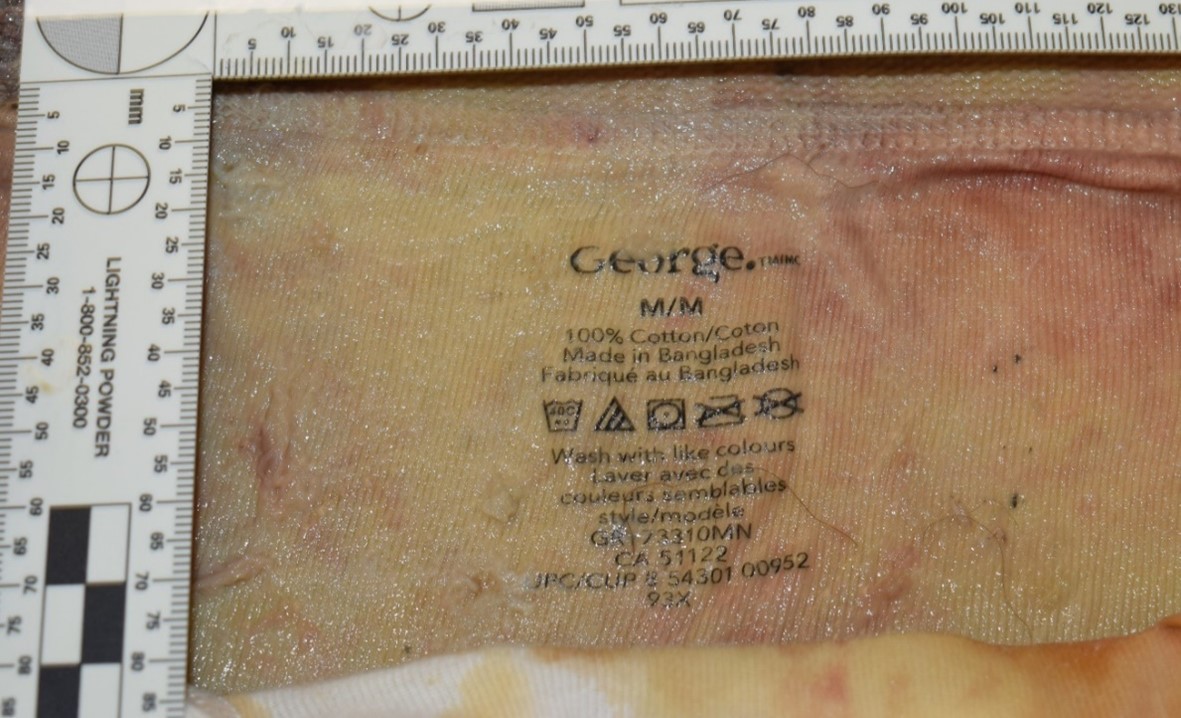
Clothing on the decedent
can function as means
to collect evidence of
identification of the decedent
- Items, personal effects or the location associated with a deceased individual (Forensic Sci Int Synerg 2021;3:100154)
- Visual identification:
- Visual confirmation of the identity of the deceased individuals by a living human, such as a relative or friend (Forensic Sci Int Synerg 2021;3:100154)
- Limitation:
- Alteration in physical features caused by death (e.g., postmortem changes such as corneal clouding, postmortem hypostasis, pallor and muscle flaccidity) may be profound and can lead to doubt for family and friends making visual identifications (J Forensic Sci 2018;63:662)
- Injury, decomposition, coupled with the emotional state of the deceased's friends or relatives may lead to misidentification (J Forensic Sci 2018;63:662)
- Distinctive marks:
- Record of distinctive findings recorded at time of autopsy and compared to antemortem records (J Forensic Radiol Imaging 2015:3:29)
- Process:
- Visual recognition of distinctive marks, including
- Tattoos
- Scars
- Piercings
- Birthmarks
- Other cutaneous lesions
- Skeletal or joint abnormalities
- Amputations
- Visual recognition of distinctive marks, including
- Limitation:
- Comparison to known characteristics of an individual from numerous sources, including medical records, licensing information, police records, etc. (J Forensic Radiol Imaging 2015:3:29)
- Decomposition and maggot activity can obscure marks such as scars and tattoos (Forensic Sci Int 2012;222:394.e1)
- Removal of skin slippage from putrefactive decomposition may reveal an underlying tattoo (Forensic Sci Int 2012;222:394.e1)
- Infrared photography and ultraviolet light may be used to highlight tattoos that are otherwise not visible due to mummification or decomposition (Acad Forensic Pathol 2016;6:338)
- Distinctive marks and physical attributes can lead to tentative or presumed identification (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])

Right axillary freckling and café au lait
spot is associated with neurofibromatosis,
which is often a hereditary condition
that can be used in identification
- Physical attributes:
- Comparison of physical attributes used to establish identification, leading to tentative or presumed identification (Acad Forensic Pathol 2016;6:361)
- Process:
- Record of physical attributes at time of autopsy, compared to antemortem records (Am J Forensic Med Pathol 2006;27:200)
- Photographs of the face and body, using a scale with the unique case number, documents and preserves the appearance at the time of identification (Am J Forensic Med Pathol 2006;27:200)
- Physical attributes used for identification:
- Biological sex
- Apparent age
- Apparent ethnicity
- Body length
- Body weight
- Acquired and congenital anomalies
- Prior surgeries or medical procedures
- Head hair color (caution: can be dyed)
- In skeletal remains, a biological profile needs to be completed by an anthropologist
- Limitation:
- Some surgeries and medical procedures are more common in a population (i.e., appendectomy, as compared to a pancreaticoduodenectomy); in the proper context, a pancreaticoduodenectomy would carry a higher discriminatory value
- Comparison to known characteristics of an individual including medical records, government issued photo identification, etc. (Acad Forensic Pathol 2016;6:361)
- Scientific means is the ideal method for identifying the deceased
- There are 5 means to perform scientific identification through a comparison of the antemortem to postmortem record:
- Fingerprints
- Dental
- Surgical numbers on surgical hardware
- Radiology
- DNA
- Expertise in different fields is required to perform the comparison of the postmortem to antemortem record; both forensic pathologists and their pathology assistants arrange and facilitate the acquisition of the postmortem record for the experts
- There are 5 means to perform scientific identification through a comparison of the antemortem to postmortem record:
- Fingerprint comparison:
- System of identification based on the classification and comparison of finger ridge patterns and minutiae (Forensic Sci Res 2018;4:293)
- Process:
- The science of fingerprints, their classification, retrieval from records and methods of recording typically lie in the domain of police procedure
- The forensic pathologist's role is to facilitate the process of obtaining the postmortem fingerprints
- Fingerprints are unique (no 2 fingerprints have been found to be identical, including among monozygotic twins, who share the same DNA) (Forensic Sci Res 2018;4:293)
- To establish identity based on fingerprints, an antemortem record must exist for the deceased to serve as a comparison
- Fingerprints can be uploaded into databases such as the Automated Fingerprint Identification System (AFIS) for comparison, which does not require a tentative identification for comparison (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Skin from a decomposed body may detach in a glove-like fashion, which can be slipped over the hand of an investigator so that classifiable prints can be made (S Afr Med J 2005;95:665)
- It is unnecessary to amputate fingers to obtain fingerprints
- In case of diffuse rigidity or charring, a local dissection of the tendons at the base of the hands will help opening the fingers to obtain fingerprints
- Mummified tissue may need to be rehydrated to obtain fingerprints (Acad Forensic Pathol 2016;6:338)
- If the epidermis is missing from the fingers, it may be possible to obtain classifiable prints from the finger pads (Am J Forensic Med Pathol 2006;27:200)
- Limitations:
- Fingerprints can be affected by multiple factors including postmortem decomposition, chemicals and immersion changes, altering the fingerprint quality and comparison ability (Forensic Sci Res 2018;4:293)
- In homicides, fingers can be cut out by the offender(s) to avoid fingerprinting
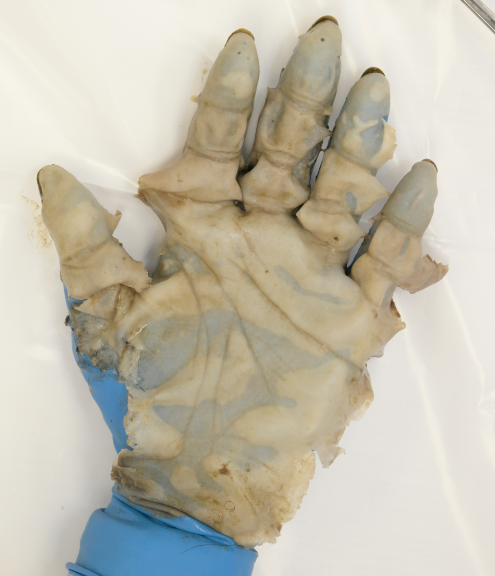
Skin from a decomposed body which
detached in a glove-like fashion is placed
over the hand of an investigator;
fingerprint impressions can then be made
- Comparative dental radiography:
- System of identification based on dental characteristics and features (Forensic Sci Res 2018;4:303)
- Process:
- Positive identification can often be established based on dental fillings, bony structures of the jaw, roots of teeth and sinuses, as these are unique to individuals (J Forensic Radiol Imaging 2015:3:29)
- Examination of the dentition of the deceased may give information as to the age, nutrition and hygiene, which can be clues to identity (Open Dent J 2015;9:250)
- Determination of age is evaluated based on crown and root development and eruption (Open Dent J 2015;9:250)
- Identification via dental records is performed in conjunction with a forensic odontologist (dentist with forensic training) or an oral pathologist (J Forensic Radiol Imaging 2015:3:29)
- Interpretation:
- Antemortem record must be available for comparison to postmortem records as no central database exists (Acad Forensic Pathol 2016;6:361)
- Dentition of all unidentified human remains should be charted and radiographed and a tooth extracted for DNA sampling if no other DNA sample is available (J Forensic Radiol Imaging 2015:3:29)

Comparative dental radiography on the
left is the antmortem radiograph and on
the right is the postmortem radiograph;
the dental implant is apparent in both
- Surgical hardware and implants:
- Devices found at the postmortem examination that can be compared with antemortem medical records (Forensic Sci Res 2018;4:303)
- Process:
- Implanted devices can have unique serial numbers or lot numbers (i.e., specific to a group of implanted devices manufactured at the same time) (Forensic Sci Res 2018;4:303)
- Radiographs:
- System of identification based on antemortem radiological comparison to postmortem radiographs (Acad Forensic Pathol 2016;6:361)
- Limitation:
- Antemortem record must exist and be locatable for comparison to postmortem records (Acta Stomatol Croat 2017;51:227)
- Interpretation:
- Individual bones may possess distinctive markings or characteristics (cranial sinuses, prior orthopedic procedures, healed fractures, etc.) (Acad Forensic Pathol 2016;6:361)
- Consultations with radiologists or anthropologists may be required (Acta Stomatol Croat 2017;51:227)
- Antemortem radiographs may have been performed at multiple institutions or in different film formats, making collection difficult (J Forensic Radiol Imaging 2015:3:29)
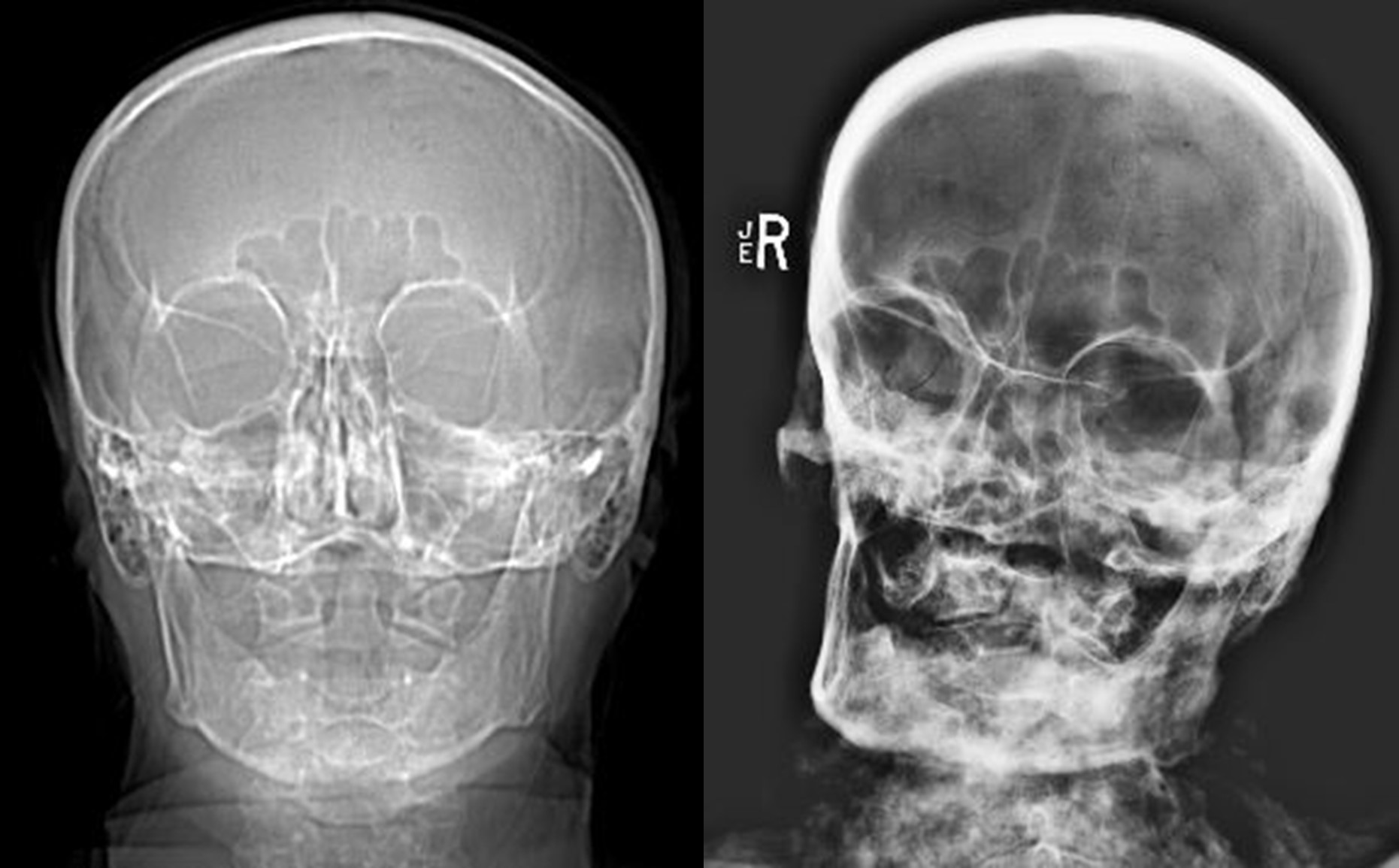
Comparative radiography on the
left is the antmortem radiograph
and on the right is
the postmortem radiograph
Postmortem shoulder radiograph with
evidence of surgical hardware that
can be used to make an identification
if antemortem radiographs are available
- Deoxyribonucleic acid (DNA):
- System of identification based on antemortem DNA comparison to postmortem DNA (J Forensic Radiol Imaging 2015:3:29)
- Process:
- DNA is a proven source for identification as the genetic information contained in a cell can connect biological relatives (J Appl Genet 2012;53:41)
- Identification of human remains by DNA is possible because of multiple alleles and DNA regions that can be amplified and used to compare genetic patterns (J Appl Genet 2012;53:41)
- DNA methods for identification require a sample from human remains to be compared to the biological sample of the closest living relative
- DNA matching to biological relatives is the only method for primary identification that is independent of direct comparison, unlike other forms of scientific identification (J Appl Genet 2012;53:41)
- Common foci that are examined include: short tandem repeat (STR), mitochondrial DNA (mtDNA) and Y chromosome (J Appl Genet 2012;53:41)
- Routine postmortem samples should be collected and stored for all cases as future DNA analysis may be required (Am J Forensic Med Pathol 2006;27:200)
- DNA samples collected for identification purposes must be correctly labeled, sealed, handled, stored and traceable through a proper chain of custody to avoid contamination (ICRC: Forensic Identification of Human Remains [Accessed 6 October 2022])
- Postmortem samples include (Forensic Sci Res 2018;4:51)
- Whole blood, fluid or tissues
- Buccal swab if not too decomposed or if taphonomy impairs collection
- Bone window ideally from an intact weight bearing bone (i.e., femur) as the dense cortical portion of lower limb bones tend to yield more consistently reliable DNA profiles compared to less dense spongy bone
- Limitations:
- Success depends on the ability to obtain a sufficient quality and quantity of DNA from the remains and the availability and willingness of family members to provide a DNA sample for the purpose of identification (J Appl Genet 2012;53:41)
- Degradation of the postmortem sample, absence of nucleated cells and DNA extraction difficulties may be due to taphonomic and putrefactive changes that inhibit PCR techniques (J Appl Genet 2012;53:41)
- Biological sample for DNA identification from biological relatives must be obtained with informed consent (J Appl Genet 2012;53:41)
- A routinely obtained DNA sample can be compared with surgical specimens from the decedent, if they exist (Am J Forensic Med Pathol 2006;27:200)
- Paraffin embedded tissue from prior surgical procedures can be a source of antemortem DNA (Leg Med (Tokyo) 2005;7:230)
- DNA is identical for monozygotic twins (Forensic Sci Res 2018;4:303)
- Siblings of the same biological sex cannot be differentiated based on DNA alone if the comparative reference sample is from a biological relative; other primary and secondary lines of evidence would be required
- Dental pulp tissue is often used as a source of DNA from severely decomposed and skeletal remains; however, dentition will need to be charted and radiographed prior to extraction (Int J Forensic Odontol 2017;2:43)
- In burned bodies or decomposed bodies, bone is often collected as a source of DNA (Forensic Sci Res 2018;4:303)
- It is imperative that all attempts have been made to acquire a genetic profile prior to release of the body; multiple samples may need to be collected to obtain a DNA profile (Forensic Sci Int 2018;289:253)
- Prior to disposition of unidentified bodies (Am J Forensic Med Pathol 2006;27:200):
- Perform a forensic autopsy
- Obtain radiographs
- Chart and radiograph dentition
- Document (including photos) clothing (with details of brand tag and size) and personal effects
- Collect DNA sample for archiving
- Collect blood in fresh bodies
- Collect bone (commonly femur) in severely decomposed bodies
- Request consultations, if required
- Anthropology
- Radiology
- Identification of skeletal remains:
- Background:
- First determine if the remains are indeed bone (Acad Forensic Pathol 2016;6:361)
- Subsequently determine if the bones are human or nonhuman, the minimum number of individuals present, the biological profile for each set of human remains and collect a DNA sample (Acad Forensic Pathol 2016;6:361)
- Fragmented human remains may be easily confused with animal bones, as well as long animal bones may be confused with human ones (Acad Forensic Pathol 2016;6:361)
- Expertise of a forensic anthropologist / archeologist is required (Acad Forensic Pathol 2016;6:361)
- Scientific means of identification (Acad Forensic Pathol 2016;6:361):
- DNA
- Radiographic comparison studies: antemortem and postmortem
- Surgical serial numbers
- Nonscientific means of identification (Acad Forensic Pathol 2016;6:361):
- Facial reconstruction (sketch, clay or computer): tentative identification of remains and subsequent positive identification if antemortem records can be obtained (Acad Forensic Pathol 2016;6:361)
- Photo superimposition: technique in which a life photograph of a missing person is superimposed on a photograph of the unidentified skull or the skull itself, using video equipment (Acad Forensic Pathol 2016;6:361)
- Careful detail of clothing including sizes, brand names, type of clothing (Forensic Sci Res 2018;4:293)
- Biological sex, ethnicity, approximate age range, osseous injuries, congenital osseus anomalies and antemortem stature determination based on standard anthropometrical techniques (Acad Forensic Pathol 2016;6:361)
- Background:
- Background:
- Any incident resulting in more decedents to be recovered and examined than can be managed by the local jurisdiction's medical examiner or coroner (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Disaster victim identification forms part of the emergency response following a disaster and involves a multidisciplinary team with a command and organizational structure that must be implemented to ensure effective coordination of a disaster response (INTERPOL: Disaster Victim Identification (DVI) [Accessed 6 October 2022])
- Concept of the search universe can be highlighted in DVI:
- Open search universe: scene with an unknown number of registered individuals (i.e., explosions in public areas)
- There is typically no early registered list to assess for possible missing persons (Forensic Sci Res 2018;4:303)
- Requires development of a list of missing person reports, typically from families and friends (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Closed search universe: scene with a well known or presumptive number of individuals (i.e., airline crashes and train derailments with passenger manifests) (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Open search universe: scene with an unknown number of registered individuals (i.e., explosions in public areas)
- Multiple fatalities that arise in a disaster can be criminal or noncriminal (Leg Med (Tokyo) 2005;7:230)
- Identification of victims in disasters is one of the most important tasks of investigators (J Appl Genet 2012;53:41)
- Once an appraisal of the situation is obtained, operational units should be formed to conduct disaster response activities (INTERPOL: Disaster Victim Identification (DVI) [Accessed 6 October 2022])
- Human remains must be scientifically identified and returned to family members expediently (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Preliminary actions and context analysis steps of the search process are essential (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- A system of organizing, recording and storing identification information and personal effects is imperative (J Appl Genet 2012;53:41)
- Gathering of antemortem data can be very time consuming and collection of current and accurate data can be challenging (NAME: Standard Operating Procedures for Mass Fatality Management 2010 [Accessed 6 October 2022])
- Disaster victim identification is often hindered by fragmentation of remains, heat damage, decomposition and comingling of remains; identification of a small part of the recovered remains can be enough to identify a person (J Appl Genet 2012;53:41)
- Unless there is reliable evidence, the fate of an individual is uncertain and it should not be assumed that they are deceased as not all missing persons are necessarily deceased (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- There may be a lack of medical or dental records as some populations may have limited or no access to certain health care services; records may also have been destroyed or may be of poor quality (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- Integrated reconciliation of information is the final step with the aim of establishing compatibility or discrepancy and is carried out by an identification coordinator with multidisciplinary support to avoid confirmation bias (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- Poor coordination, management, insufficient collection of information and improper labeling can all lead to misidentification (ICRC: The Forensic Human Identification Process - An Integrated Approach [Accessed 6 October 2022])
- Jurisdictional, legal, religious and cultural considerations must be respected and adhered to (INTERPOL: Disaster Victim Identification (DVI) [Accessed 6 October 2022])
- Disaster victim identification strategy development factors (INTERPOL: Disaster Victim Identification (DVI) [Accessed 6 October 2022]):
- Existing legislation, regulations and procedures
- Local capacity and expertise
- Infrastructure and equipment
- Family / community needs
- Disaster victim identification process
- Phase 1: scene (processing human remains and property at the disaster site)
- Secure scene and ensure it is treated as a crime scene until trained examiners arrive
- Render the scene safe prior to examination (i.e., live explosives)
- Photograph, record, label, collect
- Document with standard forms / methods
- Tag human remains with a unique alphanumeric identifier
- Phase 2: postmortem (detailed examination of human remains in mortuary)
- Accession, process, examine and sort human remains at the mortuary
- Photography, fingerprinting, radiology, odontology, DNA sampling, postmortem examinations
- Examine, document and store personal property
- Phase 3: antemortem (collection of missing person data from various sources)
- Interview families, relatives or friends to obtain sufficient data
- Physical descriptions, jewelry, clothing, etc.
- Secure antemortem data (dental radiographs, medical imaging, fingerprints, DNA)
- Phase 2 and 3 can occur concurrently
- Interview families, relatives or friends to obtain sufficient data
- Phase 4: reconciliation (comparing postmortem and antemortem data)
- Identity is determined if multiple lines of evidence show consistency and compatibility, lack discrepancies and features allow for differentiation from other candidates (Forensic Sci Int Synerg 2021;3:100154)
- Serious discrepancies lead to exclusion of an individual as the source of the human remains (Forensic Sci Int Synerg 2021;3:100154)
- When information analysis is not sufficient to conclude with certainty in favor of one possibility or another, the case file is listed as inconclusive and the investigation should be expanded (Forensic Sci Int Synerg 2021;3:100154)
- Visual identification can be very unreliable and should not be considered alone
- Assessment of reconciliation files needs to consider the reliability of evidence to conclude positive identity; the case file is then presented to an authority that has overall responsibility for the identification of the deceased (i.e., coroner, medical examiner)
- If identification is accepted, a death certificate confirming identity and cause of death is issued; once release is granted, arrangements can be made for repatriation of remains to the family
Lines of evidence used for reconciliationMissing Person Unidentified Person Location last seen Location found Date last seen Date found Biological profile Biological profile Dental comparison Dental comparison Fingerprint records Fingerprint records DNA sample DNA sample Clothing and personal effects Clothing and personal effects Health conditions Medical findings
- Identity is determined if multiple lines of evidence show consistency and compatibility, lack discrepancies and features allow for differentiation from other candidates (Forensic Sci Int Synerg 2021;3:100154)
- Outcomes of the reconciliation process:
- Identification
- Exclusion
- Inconclusive
- Causes of misidentification:
- Lack of rigorous procedures
- Overreliance on a single identification technique
- Inadequate recovery of human remains
- Inadequate interpretation
- Lack of chain of custody
- Lack of adequately trained personnel
- Lack of quality control and quality assurance mechanisms
- Confirmation bias
- External pressure to complete an identification without following accepted procedures
- Phase 1: scene (processing human remains and property at the disaster site)
The antemortem image shown above is acquired from an unidentified individual. What is true about dental radiographs in the context of forensic identification?
- A central database exists to compare postmortem records to antemortem records
- If dental fillings and implants are present they can be compared to antemortem records
- It is not advisable to routinely perform dental radiographs of unidentified individuals
- There is no association between age and crown and root development
Comment Here
Reference: Forensic identification
- Dental enamel is a reliable source of DNA in this scenario
- DNA from a biological relative will not be able to differentiate between the brothers
- DNA from buccal swabs is the best source of DNA in burned bodies
- mtDNA should be used to differentiate between the brothers
Comment Here
Reference: Forensic identification
What is true about the forensic identification method shown above?
- Finger pads don't contain ridge detail or minutiae
- Fingerprints cannot be used to distinguish between identical twins
- If the skin is detached it can still potentially be slipped over the hand of an investigator in a glove-like fashion to obtain fingerprints
- Postmortem decomposition has no effect on fingerprint quality
Comment Here
Reference: Forensic identification
- Term currently favored by many forensic pathologists / pediatricians to replace Sudden Infant Death Syndrome (SIDS)
- Defined as sudden, unexpected death of an otherwise healthy infant, less than 1 year of age, in which scene investigation, clinical history and complete postmortem evaluation fail to determine a cause of death
- Diagnosis of exclusion, and likely represents a group of as yet unidentifiable natural causes of sudden death (i.e. congenital cardiac arrhythmia, occult infection, etc)
- Risk factors: prematurity, male gender, poor socioeconomic status, colder climate, maternal smoking or illicit drug, young maternal age (less than 20 years old)
- Death usually occurs during sleep
- No specific autopsy findings; may see thymic / pleural / epicardial petechiae, pulmonary congestion, sparse pulmonary inflammation
- Natural causes of death that may at first appear to be SUID: myocarditis, respiratory infection, cardiac channelopathies, meningitis, gastroenteritis, inborn errors of metabolism
- Accidental causes of death that may at first appear to be SUID: asphyxia (overlay in shared bed or poor bedding material), poisoning
- Neonaticide: the deliberate killing of an infant
- Mother is most common perpetrator
- Usually death via asphyxia (e.g. smothering) or environmental exposure (due to abandonment)
- With newborns, mother may claim child was stillborn; air in lungs indicates child was breathing prior to death
- Hydrostatic test: lungs are placed in a container of water; if they float, they are presumably filled with air, suggesting the child was breathing prior to death
- False positive hydrostatic test with attempted resuscitation or decomposition; false negatives can also occur
- Child homicide
- In first year of life, most homicidal deaths are due to head trauma
- In second year of life, head trauma and abdominal trauma are both common
- Battered child syndrome: multiple bruises, abrasions and boney fractures of various ages; this category also included neglected children suffering from malnutrition
- Other causes of death include thermal injury due to scalding, smothering (autopsy usually negative)
- Shaken baby syndrome: controversial cause of death due to violent shaking of infant with subdural or subarachnoid hemorrhage and retinal hemorrhages
- Many believe shaking alone cannot produce significant injuries and death, and most of these infants actually suffered from blunt force trauma
- Postmortem changes refers to a continuum of changes that occur in a dead body following death; these changes include livor mortis, rigor mortis, decomposition and taphonomy (StatPearls: Evaluation of Postmortem Changes [Accessed 1 July 2020])
- Given the postmortem changes and the rate of change are influenced by many variables, it is not possible to reliably estimate an accurate postmortem interval or time since death based solely on postmortem changes; time intervals given below are dependent on the circumstances and the reference (Forensic Sci Int 2018;283:180)
- Artifact is any change produced in the body after death or during resuscitation that may lead to misinterpretation of relevant antemortem findings; postmortem changes may mimic injuries, obscure and hinder interpretation of antemortem findings (Rutty: Essentials of Autopsy Practice - Advances, Updates and Emerging Technologies, 2014)
- Body undergoes decompositional changes after death; typically, this process is composed of 2 parallel processes: autolysis and putrefaction (StatPearls: Evaluation of Postmortem Changes [Accessed 1 July 2020])
- To aid in differentiating antemortem injury from a postmortem artifact is the presence of a vital reaction; this is characterized by an inflammatory response or significant bleeding, however, using the presence of bleeding as a finding of a vital reaction can be limited in areas of livor mortis (Forensic Sci Int 2004;144:221)
- Major factors that influence decomposition (Forensic Sci Int 2011;204:34):
- Temperature
- Moisture
- Access for bugs and animals
- Injuries
- Illness
- Body habitus
- Clothing
- General classifications of decomposition (StatPearls: Postmortem Changes [Accessed 1 July 2020]):
- Putrefaction
- Mummification
- Adipocere
- Maceration
- Definition:
- Postmortem stiffening or rigidity of the body due to depletion of ATP and accumulation of lactic acid; in a dead body, the glycogen stores are rapidly depleted, preventing the energy dependent breakage of sarcomere contraction (J Physiol 1947;106:177)
- Process:
- This is a transient postmortem change (Forensic Sci Int 2004;140:79)
- In general, there is an initial flaccid interval that is followed by a gradual stiffening of the body, which then eventually disappears (Forensic Sci Int 2004;140:79)
- This onset, peak and dissipation of rigor mortis is a temperature dependent process (i.e. onset and dissipation will be faster in warmer temperatures and delayed by colder temperatures) (Leg Med (Tokyo) 2013;15:293)
- In addition, antemortem physical exertion will influence the rate of onset (Forensic Sci Int 1983;22:1)
- Typically, rigor mortis may begin within a couple of hours after death and occurs in all muscle groups but is initially notable in the small muscles (i.e. jaw) followed by larger muscle groups (i.e. legs) (Forensic Sci Int 1978;12:97)
- Rigor mortis will be fully fixed after approximately 6 - 12 hours and will maintain the position of the body when fully fixed, unless sufficient pressure is applied that breaks the rigor mortis leaving the joint easily moveable (Br Med J 1950;2:304, J Pak Med Assoc 1998;48:49)
- Once rigor mortis is fixed and then broken, it will not return (Forensic Sci Int 2008;176:157)
- Rigor mortis dissipates after approximately 36 - 48 hours (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Interpretation and artifact:
- Quality (i.e. strength) of rigor mortis and position of the body should be noted at the scene due to the transient nature and ability to break rigor mortis (Int J Appl Basic Med Res 2011;1:120)
- Rigor mortis can indicate the position of the body at the scene; inappropriate or antigravitational rigor mortis can indicate that a body has been moved once rigor mortis has been fully fixed and the body is discovered prior to full dissipation of rigor mortis (Int J Appl Basic Med Res 2011;1:120)
- Rigor mortis may not be readily apparent in decedents with low muscle mass (i.e. elderly and infants) (Exp Appl Acarol 2009;49:21)
- So called cadaveric spasm, described as near instantaneous onset of rigor mortis at time of death, is rare; it is postulated that this occurs in extreme physical or emotional situations (Forensic Sci Med Pathol 2013;9:244, Forensic Sci Med Pathol 2013;9:249)
- Extreme temperatures may mimic rigor mortis due to freezing or heat induced protein denaturation (Int J Emerg Med 2018;11:46)
- Body site specific artifacts (Shkrum: Forensic Pathology of Trauma, 2007):
- Skin: cutis anserinus (goosebumps) - rigor mortis of the erector pilae muscles
- Pupil inequality: rigor mortis of the ciliary muscles
- Semen deposition: may indicate postmortem rigor mortis of seminal vesicles
- Widening of the anal orifice: resolution of rigor mortis
Contributed by Karissa French, M.Res., M.D. and Rebekah Jacques, M.H.Sc., M.D.
- Definition:
- Gravity dependent accumulation (pooling) of blood in the skin and organs creating a purple-red discoloration (Forensic Sci Med Pathol 2016;12:451)
- Also known as lividity, postmortem hypostasis, dependent lividity (Forensic Sci Med Pathol 2016;12:451)
- Process:
- Following the cessation of circulation there is settling of blood in the dependent parts of the body, which distributes in the body in a gravity dependent manner (Exp Appl Acarol 2009;49:21)
- Livor mortis is evident as deep purple-red discoloration in the skin and internal organs (Forensic Sci Med Pathol 2016;12:451)
- Blanching occurs in gravity dependent areas of the body that come into contact with firm surfaces (i.e. floor, tight clothing); livor mortis is spared in these areas due to localized pressure preventing blood from entering the skin (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Blanching can also occur with pressure in nonfixed areas of lividity; this force displaces the pooled blood but the pooled blood will return following the removal of pressure, such as pressing your thumb to an area of lividity to test if it is fixed (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Livor mortis will eventually become fixed in several hours (approximately 8 - 12 hours or so) and lose its ability to become blanchable; this is due to breakdown of red blood cells and vessels (Z Rechtsmed 1984;93:283)
- Fixation of lividity does not occur all at once (Saukko: Knight's Forensic Pathology, 4th Edition, 2015)
- Interpretation and artifact:
- Distribution depends on body position and can indicate that the body has been moved
- A distribution of livor mortis which does not correspond to the position of the body is an indication of a prior different position of the body (Forensic Sci Med Pathol 2016;12:451)
- Dual distribution of livor mortis occurs when the body is moved so that new areas of the body are now dependent (Forensic Sci Med Pathol 2016;12:451)
- Misinterpreted as disease: internal organs are also affected by livor mortis, for example (Vet Pathol 2016;53:929):
- Myocardium: misinterpreted as a myocardial infarction
- Meninges: misinterpreted as subarachnoid hemorrhage
- Lungs: misinterpreted as pneumonia
- Misinterpreted as injury or obscure injuries, for example (Saukko: Knight's Forensic Pathology, 4th Edition, 2015):
- Bruises in areas of lividity may be difficult to identify (StatPearls: Evaluation of Postmortem Changes [Accessed 1 July 2020]):
- Unfixed lividity: apply pressure to identify if blanches; bruises don’t blanch
- Fixed lividity: incision may be helpful to demonstrate lack of subcutaneous hemorrhage; histology may assist if inflammatory reaction present
- Hypostatic hemorrhages or hemorrhagic lividity
- Blood vessels may rupture and cause areas of hemorrhage; these are limited to areas of livor mortis (Forensic Sci Med Pathol 2012;8:330, Am J Forensic Med Pathol 2009;30:322)
- To avoid livor mortis associated artifacts, bodies should be stored and transported face up (J Pak Med Assoc 1998;48:49)
- Color and character of livor mortis may aid in suggesting a cause or mechanism of death:
- Cherry red: carbon monoxide toxicity, hypothermia, cyanide toxicity or artifact of mortuary refrigeration (Forensic Sci Int 1999;99:149)
- Brown: primary or secondary methemoglobinemia (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Yellow-brown: phosphorus toxicity (Shkrum: Forensic Pathology of Trauma, 2007):
- Diminished lividity: death is associated with substantial blood loss (Forensic Sci Med Pathol 2018;14:57)
- Ventral lividity with blanching of the anterior neck: may indicate positional asphyxia (Am J Forensic Med Pathol 1992;13:101)
- Bruises in areas of lividity may be difficult to identify (StatPearls: Evaluation of Postmortem Changes [Accessed 1 July 2020]):
- Distribution depends on body position and can indicate that the body has been moved
Contributed by Karissa French, M.Res., M.D. and Rebekah Jacques, M.H.Sc., M.D.
- After death, the skin and mucosal membranes may desiccate resulting in a change in color and character of these tissues (Forensic Sci Med Pathol 2012;8:330)
- Tache noir: horizontal linear scleral blackening along the equator of the globe of the eye; the sclera is exposed to drying when the eyelids are incompletely shut; tache noir is often initially red in appearance and over time becomes black (Forensic Sci Med Pathol 2012;8:330)
- Lips, tip of tongue and scrotum darken with postmortem drying (Forensic Sci Int 2018;283:180)
Contributed by Karissa French, M.Res., M.D. and Rebekah Jacques, M.H.Sc., M.D.
- Definition: the process by which organic matter is broken down into simpler forms of matter
- Different organs break down at different rates (Forensic Sci Int 2012;222:162)
- Type and rate of decomposition is environment dependent (Exp Appl Acarol 2009;49:21)
- Skeletonization is the final common result (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Dead body can have different types of decomposition occurring in different areas of the body (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Atypical localized accelerated decomposition may indicate injury (Forensic Sci Int 2016;261:93)
- Autolysis:
- Aseptic breakdown of tissues caused by the release of intracellular enzymes; degradation of a substance by chemical or physical processes (i.e. hydrolysis) (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Changes in pH cause cells to lose structural integrity, leading to release of enzymes (Forensic Sci Int 2015;253:136)
- Putrefaction decomposition:
- Typical environment: hot and humid (Int J Legal Med 2018;132:301)
- Most common form of decomposition is composed of liquid (i.e. purge) and gaseous transformation of tissues and organs by local and hematogenous spread of intestinal bacteria and other microorganisms (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Fermentation process causes softening and liquefaction of the soft tissues by transforming carbohydrates, lipids and proteins into organic acids and gases (Forensic Sci Med Pathol 2013;9:135)
- Modifying factors: ambient temperatures, bacteremia, defects exposing body cavities, prone body position, clothing, fever, elevated BMI / body habitus, certain drugs, submersion in water, burial (Forensic Sci Int 2013;231:257)
- First sign: green discoloration of the abdomen in the right lower quadrant due to the proximity of the cecum to the skin (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Characterized by:
- Skin discoloration: green, deep red and black (Acad Forensic Pathol 2016;6:19)
- Marbling: venous distribution in the skin due to proliferation of bacteria within superficial veins (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Bloating: gaseous distension leads to expulsion of sanguineous fluid from mouth and nose (i.e. purge fluid) (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Skin slippage and epidermal blistering: peeling of the epidermis in a glove and stocking fashion of the hands and feet, respectively; the hair and nails detach (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Artifact:
- Purge fluid is commonly misinterpreted as antemortem hemorrhage (Am J Forensic Med Pathol 2008;29:145)
- Differentiate purge from antemortem trauma:
- No trauma
- No source of bleeding present
- Putrefactive decompositional bloating present
- Differentiate purge from antemortem trauma:
- Gastromalacia / esophagomalacia: mimics a perforated ulcer; distention from gas and softening of the gastrointestinal tract may cause an artefactual rupture; histology shows no features of an ulcer (Am J Forensic Med Pathol 2006;27:61)
- Decompositional fluid in the chest cavities: low volumes of red-brown fluid mimic hemothoraces (Acad Forensic Pathol 2016;6:19)
- Breakdown of the pancreas: mimics hemorrhagic pancreatitis (Forensic Sci Int 2012;222:162)
- Purge fluid is commonly misinterpreted as antemortem hemorrhage (Am J Forensic Med Pathol 2008;29:145)
- Mummification decomposition:
- Typical environment: hot and dry (J Bone Joint Surg Br 1991;73:969)
- A form of decomposition that typically results in desiccation of the tissues and inhibits bacterial overgrowth (Forensic Sci Int 2019;303:109948)
- Differs from ritual mummification, which is an embalming technique that utilizes salt based chemicals and resins as was done in ancient Egypt (Anat Rec (Hoboken) 2015;298:974)
- Can also occur in cold environments (Am J Phys Anthropol 2007;Suppl 45:162)
- Wounds may be preserved (Forensic Sci Int 2018;286:31)
- Adipocere formation (saponification):
- Typical environment: damp and free of oxygen (Leg Med (Tokyo) 2016;18:49)
- Also known as grave wax (Forensic Sci Int 2011;208:167)
- Wax-like organic substance formed by the anaerobic bacterial hydrolysis of fat to oleic, palmitic and stearic acids (Forensic Sci Int 2013;226:301)
- Occurs in cold, humid and anaerobic environments (ie. wet ground, bottom of a lake) but internal body water content may be enough for hydrolysis to occur (Naturwissenschaften 2003;90:291)
- After months or years may become brittle / chalky (Leg Med (Tokyo) 2016;18:49)
- Tends to develop on the cheeks, orbits, chest, abdominal wall and buttocks (StatPearls: Evaluation of Postmortem Changes [Accessed 1 July 2020])
- Can form visibly any time between 3 weeks and 3 months and is often mixed with other forms of decomposition (StatPearls: Evaluation of Postmortem Changes [Accessed 1 July 2020])
- Surface adipocere formation may maintain the features of the face and preserve the features of wounds (Forensic Sci Int 2011;208:167, Leg Med (Tokyo) 2016;18:49)
- Maceration:
- Term also used for the aseptic autolysis of the stillborn fetus (StatPearls: Postmortem Changes [Accessed 1 July 2020])
- Softening and breakdown of tissues due to prolonged exposure to a moist / liquid environment (J Wound Care 2017;26:159)
- Features: skin slippage, softening and darkening of the tissues and organs with hemosiderin staining, loosening of the joints (J Clin Pathol 1971;24:159)
Contributed by Karissa French, M.Res., M.D., Rebekah Jacques, M.H.Sc., M.D. and Michael Shkrum M.D.
- Definition: environmental influences on the body after death, including but not limited to insect activity, postmortem animal predation and human intervention
- Bodies discovered in water:
- Cool water will slow putrefaction, however, once the body is removed from the water, putrefaction may undergo an accelerated course (Acad Forensic Pathol 2016;6:19)
- Over time, the skin becomes wrinkled (immersion changes), edematous and eventually the epidermis will slough off (Z Rechtsmed 1984;92:277)
- Over time, gas formation causes floating of the body with the extremities and head in a dependent position; this may result in postmortem abrasions as the hands scrape against the rocky / sandy bottom of the body of water (Acad Forensic Pathol 2016;6:19)
- Small aquatic fish may leave irregularly shaped postmortem abrasions while large aquatic animals such as sharks and crocodiles may amputate whole limbs (Am J Forensic Med Pathol 2002;23:238)
- Postmortem animal predation:
- Knowledge of the scene and of local fauna is vital for differentiating traumatic lesions from postmortem animal predation (Am J Forensic Med Pathol 2002;23:238)
- Mammals:
- Domestic dogs and cats can cause postmortem damage in uncovered areas of the body, commonly the face and hands; unlikely to tear clothing or perforate body cavities (Forensic Sci Med Pathol 2011;7:344)
- If the body is unclad, the genitals may be involved, raising the suspicion for sexual trauma (Med Sci Law 2002;42:269)
- Rodents will initially create shallow crater-like wounds with finely scalloped edges in exposed areas; prolonged exposure will lead to total skeletonization; the bones will have distinct double furrows from gnawing activity (Int J Legal Med 1999;112:115)
- Margins of tissue loss are free of hemorrhage (Forensic Sci Med Pathol 2011;7:309)
- Animal scavengers may disarticulate a body and scatter the remains (Forensic Sci Int 2018;290:29)
- Birds:
- Triangle to hourglass shaped punctures, preferentially in the exposed skin and eyes (J Forensic Sci 2004;49:592)
- Strips of soft tissues leaving exposed frayed tendons (J Forensic Sci 2004;49:592)
- Insects:
- Forensic entomologists may be involved and use insect evidence to determine time of death as successive waves of insects colonize and mature (Forensic Sci Int 2001;120:132)
- Insect activity in regions of intense lividity may produce some bleeding (Int J Legal Med 2019;133:307)
- Flies: the most common insect encountered (Am J Forensic Med Pathol 2002;23:238)
- Fly eggs are laid in naturally occurring orifices (i.e. mouth, nose, eyes, genitals, anus) and antemortem wounds; preferential colonization of non-natural occurring orifices should be examined for evidence of trauma (Int J Legal Med 2019;133:307)
- Eggs hatch into maggots (fly larvae) and have proteolytic enzymes that allow them to destroy tissue and burrow into the body; this may mimic injury but also distort and obscure the presence and features of antemortem injuries (Int J Legal Med 2019;133:307)
- Metabolism associated heat of the maggot mass will speed up local decomposition (Int J Legal Med 2019;133:307)
- Ants: have a predilection for skin, causing irregularly shaped clusters with scalloped edges; this finding may be misinterpreted as antemortem abrasions (Am J Forensic Med Pathol 2009;30:84)
- Cockroaches: cause shallow, rounded lesions which mimic antemortem burns (Int J Legal Med 2019;133:307)
- Resuscitation related artifacts:
- General:
- Information on the resuscitation status and the types of interventions, including bystander resuscitation, should be considered prior to commencing the external examination (Leg Med (Tokyo) 2007;9:94)
- Cardiopulmonary resuscitation often involves multiple needle punctures, placement of an oral endotracheal tube, chest compressions and defibrillation (J Forensic Leg Med 2015;33:39)
- Needle punctures may occur in multiple areas; to differentiate from antemortem intravenous drug injection requires details from the paramedic and clinical record (J Forensic Leg Med 2015;33:39)
- Resuscitation related artifacts involving the face and neck:
- Oxygen face mask can cause perioral and nose abrasions (J Forensic Leg Med 2015;33:39)
- Head tilt / chin lift to open the decedent’s airway may result in abrasions of the face and chin area due to the healthcare worker’s fingernails (J Forensic Leg Med 2015;33:39)
- Insertion of an oral endotracheal tube or oropharyngeal airway may cause bruises and abrasions of the lips and oral mucosa; in particular, laryngoscopy may cause damage to the teeth and uvula (Leg Med (Tokyo) 2007;9:94)
- Obstructing objects within the oral cavity or oropharynx may be removed during resuscitation (Med Sci Law 1988;28:200)
- Neck braces may cause abrasions and hemorrhage into the strap muscles of the neck (J Forensic Leg Med 2019;66:95)
- Resuscitation related artifacts involving the torso:
- Chest compressions may cause precordial bruises and abrasions as well as fractures of the sternum, anterior and anterolateral ribs; histology may reveal fat and bone marrow pulmonary emboli as a result; in addition, the fractured ribs can lacerate the internal organs such as the heart, lungs, spleen and liver resulting in hemothorax and hemoperitoneum (Leg Med (Tokyo) 2007;9:94, Am J Emerg Med 2018;36:838)
- Defibrillators may leave abrasions when they come in contact with the skin (J Forensic Leg Med 2015;33:39)
- Thoracostomies can be interpreted as sharp force injury or may alter a pre-existing injury (J Thorac Dis 2019;11:S186)
- Abdominal pressure during chest compressions may result in regurgitation of gastric contents mimicking aspiration (Am J Med 2000;108:144S)
- General:
- Organ and tissue donation related artifacts:
- Whole organs (heart, lungs, liver, kidneys, pancreas and adrenals) and tissues (skin, corneas / eyes, long bones, heart valves) may be procured for donation (J Transpl Coord 1999;9:73)
- Donations may deplete the intravascular blood volume; request samples of blood to be taken at the time of organ donation and most tissue types of tissue donation; in addition, organ donors often have antemortem hospital blood samples and investigations which should be noted and seized for toxicology (Am J Forensic Med Pathol 2007;28:202)
- Review surgical notes may be of some value in interpreting postsurgical changes (Am J Forensic Med Pathol 1994;15:192)
- Skin donation often leaves wide, clean edged, even depth, rectangular abrasions (Am J Forensic Med Pathol 1994;15:192)
- Eye donation may cause periorbital bruising (Am J Forensic Med Pathol 1994;15:192)
- Obscure the cause of death: donation of the heart and lungs may involve the aorta and pulmonary vessels; surgical team should document and avoid altering area of prior aortic dissection or laceration; in addition, if a thromboembolus in the pulmonary vasculature is present at the time of donation this requires documentation and pathological evaluation (Am J Forensic Med Pathol 2010;31:113)
- Autopsy related artifacts:
- Autopsy is an innately destructive process and can cause artifacts (Saukko: Knight's Forensic Pathology, 4th Edition, 2015)
- Fracture of the cornua (horns) of the hyoid bone and thyroid cartilage can occur during removal of the neck structures; postmortem fractures of the cornua are free of hemorrhages; careful in situ dissection of the cornua can avoid this (Med Sci Law 2011;51:109)
- Prinsloo-Gordon hemorrhages: artefactual extravasation of blood into the tissues of the neck, most commonly seen on the posterior pharyngeal wall; removal of the brain and thoracoabdominal organs prior to neck dissection could help to minimize potential confusion with external neck compression (Acad Forensic Pathol 2016;6:45)
- Base of skull fracture out of context: this fracture commonly occurs when a focal area of the inner table of the skull has not been completely cut with the oscillating saw and the key is used to pry the calvarium from the base of skull; a snap (i.e fracture) may be heard when the key fractures the base of skull (J Pak Med Assoc 1998;48:49)
- Vitreous fluid sampling may cause scleral hemorrhage (DiMaio: Handbook of Forensic Pathology, 2nd Edition, 2006)
- Funerary artifacts:
- General: Funerary practices are used to disinfect, preserve and alter the dead body to make it presentable for viewing (Am J Forensic Med Pathol 1994;15:122)
- Preparing a body for a funeral includes (Am J Forensic Med Pathol 1994;15:122):
- Changing the clothing, hair and applying make up
- Shaving, which may cause skin abrasions
- Restraints may be used to position the body and may mimic ligature marks
- Mouth may be sutured closed or wired at the maxilla
- Corneal caps inserted in the eyes to hold the eyelids in place
- Embalming: those commonly encountered at the autopsy are arterial and cavity embalming
- Arterial embalming is injecting embalming fluid into the vasculature, typically done through the neck, arms and legs which may cause dissection (Med Sci Law 1992;32:58)
- Cavity embalming involves inserting a trochar into the abdominal cavity and using this opening to create multiple punctures into the organs before filling the cavity with embalming fluid
- Artifacts and other associated findings:
- Some embalming fluid contains red dye which causes a false pink color similar to carbon monoxide poisoning (Med Leg Bull 1984;33:1)
- Diminished intravascular blood volume due to its to removal from the embalming process (Am J Forensic Med Pathol 1994;15:122)
- Trochar puncture sites may cause aortic dissection (J Forensic Sci 2016;61:S246)
- Areas of postmortem clots are not macroscopically distinguished from thromobembolus
- Bruising (Am J Forensic Med Pathol 1994;15:122):
- May become enhanced by blood being forced into these areas by the pressure of the embalming fluid
- Exaggerate mild injury
- Create the appearance of bruising where there was no antemortem trauma, this may happen in the embalming fluid injection site
- Undertaker’s fracture: fracture of the lower cervical spine (typically C6 - C7) during body transport or organ removal (Eur J Forensic Sci 2016;3:202)
- Toxicological analysis, if performed, must be interpreted with caution and ideally in conjunction with the embalming fluid used (Forensic Sci Int 2013;233:312)
Contributed by Karissa French, M.Res., M.D. and Rebekah Jacques, M.H.Sc., M.D.
Comment Here
Reference: Postmortem changes
Comment Here
Reference: Postmortem changes
- Sharp force injuries: injuries produced by sharp objects
- Sharp object: an object that has a sharp edge or pointed extremity
- Numerous objects can produce sharp force injuries; knives are the most commonly used weapons (Int J Legal Med 2000;113:259, J Forensic Sci 2020;65:833)
- Typical knife contains:
- Handle: the portion that can be gripped; it can be used as a blunt force weapon, producing patterned injuries
- Guard (or finger guard): a metal bar at right angles between the blade and the hilt; the guard may include the quillon, protuberances extending perpendicularly to the long axis of the knife that stop the fingers from sliding forward onto the knife blade and cutting edge; the quillon may produce patterned skin injuries (Italian Journal of Legal Medicine 2012;1:4)
- Blade: can have a plain edge or serrated edge with rounded or pointed extremity and a single or double edge
- Atypical sharp and pointed objects that can be used to produce sharp force injuries include but are not limited to scissors, screwdrivers, fragments of glass (e.g. broken bottleneck or glasses), forks, ice picks, etc. (Forensic Sci Int 2001;123:135)
- Typical knife contains:
- Numerous objects can produce sharp force injuries; knives are the most commonly used weapons (Int J Legal Med 2000;113:259, J Forensic Sci 2020;65:833)
- Sharp force wounds typically show cleanly divided edges and may involve different types of tissue with the same contact
- Depth of the wound track relative to the length of the cutaneous wound distinguishes a stab from an incision
- Sharp force injuries can be subcategorized as follows:
- Incised wounds
- Stab wounds
- Chop wounds
- Atypical wounds (atypical weapons, combined incised and stab wounds)
- Incised wounds are typically superficial and longer than they are deep
- Incised wounds must be distinguished from laceration: tissue bridges are the hallmark of laceration
- Stab wounds generally are deeper than their cutaneous length
- Chop wounds are produced by heavy, relatively blunt objects with at least 1 sharp edge
- Number and location of the wounds can give clues regarding the manner of death
- Multiple deep stab wounds are generally seen in homicides
- Progressively deeper wounds with a single fatal stab wound are typically seen in suicides
- Accidental fatal sharp force deaths are rarely described
- Also called cuts or slashes
- Surgical incision is a typical example of an incised wound
- Wounds caused by sharp objects that contain a blade with at least 1 sharp edge (knives, razors, swords, etc.)
- Produced by a tangential movement of the blade to the skin
- Typically, wounds are superficial and longer than they are deep
- In most cases, incised wounds tend to be deeper at the point of the first contact with the skin (entrance) and become progressively more superficial as the wound approaches the distal end (exit)
- Wounds show clear separation of the injured and uninjured tissues
- Tissue bridges absent in the center of the wound (BMC Med Imaging 2012;12:32)
- Tissue bridging is caused by incomplete separation of stronger tissue elements, such as blood vessels and nerves
- Critical feature to differentiate incised wounds from laceration (tear in tissue caused by blunt trauma, e.g. tearing or crushing)
- Based on the depth of penetration and the energy applied to the blade, there may be different wounds:
- Abrasions: though typically produced by blunt objects, when the blade affects the superficial layer of the skin involving just the epidermis, it may leave superficial linear scratches (abrasions)
- Cuts: the blade penetrates deeper, resulting in skin and soft tissue splitting
- Mutilations: the blade is used vigorously on protruding body areas, resulting in their complete detachment
- Wound tails: tails are superficial, linear scratches localized at the level of the wound's extremities that are due to the blade movement on the skin; as a general rule, the tail is shorter and deeper at the entrance point (entrance tail) where there is higher pressure applied to the blade; it is longer and more superficial at the exit point (exit tail) as the blade progressively rises from the skin, decreasing the pressure toward the end
- Tails may give information about the direction in which an incised wound was inflicted; associated skin and soft tissue injuries or clothing defects need to be considered to evaluate the direction
- Tails can be absent
- Entrance tail can be absent if the applied pressure is too vigorous, causing skin separation without scratching
- Exit tail may be absent or shorter than the entrance tail when the affected body area is convex: the involved surface escapes the sliding action of the cutting edge
- If the skin surface is not flat but folded (hands, knuckles, breast, etc.), a single cut can determine more than 1 wound (wrinkle wounds); the sharp edge of the object moves from crest to crest, leaving intact skin between the incised wounds
- Incised wounds are rarely fatal but can be life threatening if they affect body areas with superficial major blood vessels, such as the neck and the wrist
- Also called puncture wounds
- Wounds caused by a sharp pointed object that enters the body during a more or less perpendicular movement
- Penetration mechanism is the critical feature of stab wounds
- Penetration is related to pressure (P), which is the force (F) applied perpendicular to a surface per unit area (A)
- P = F/A
- Penetration is related to pressure (P), which is the force (F) applied perpendicular to a surface per unit area (A)
- Stab wounds are typically deeper than their cutaneous length (Med Sci Law 1994;34:67)
- Sharp pointed objects penetrate the body producing:
- Entrance wound: may show additional injuries due to the blunt mechanism of the knife's handle or guard (patterned injuries, abrasions, bruises, etc.)
- Wound track, usually with a dead end
- Rarely, an exit wound; for example, stab wounds to the upper extremities or high energy stab wounds (e.g. arrows)
- No tissue bridges are present in the center of the wound
- Critical feature to differentiate stab wounds from laceration
- When the knife is twisted into the body before withdrawal, there may be peculiar wound shapes: V, L, Y or irregular
- Imprint abrasions from the handle can be present (handle's mark) (Italian Journal of Legal Medicine 2012;1:4)
- Indicates that the entire blade penetrated the body
- Requires vigorous pressure
- Mixed injuries showing both patterns of sharp and blunt force injuries (J Clin Forensic Med 1999;6:24)
- Produced by various objects that are generally heavy, relatively blunt and with at least 1 sharp edge
- Chop wound appearance:
- Clean center due to the action of the sharp edge of the object on the tissues
- Margins are less clean and regular than classic sharp force injuries due to:
- Increased weight and thickness of the blade
- Decreased sharpness of the blade
- Bruising, abrasions and crushing are usually present surrounding the center of the wound
- Significant weight of the weapon allows for a high energy pressure mechanism that results in a cut of the tissues together with evidence of bruising, abrasion and crushing
- Wound depth is usually variable due to the irregular penetration of the blade
- No wound tails are typically observed due to the primary pressure mechanism
- Chop wound mechanism involves high energy forces:
- Skin and soft tissues are usually lacerated
- Fractures may be observed
- When the head is involved, a typical linear dent is observed on the external surface of the cranium due to the action of the heavy blade
- If the force exceeds the elastic threshold of the cranium, then fractures develop
- When the extremities are involved, partial or full amputations may occur
- Typical chop wounds (J Forensic Sci 2001;46:228):
- Axes: crushing, fragmenting wounds with fractures
- Cleavers: clean, narrow wounds without fractures at the entry site
- Machetes: wider, less clean wounds with small fragments of bone at the entry site and fractures in the bed of the cut
- Atypical chop wounds:
- Boat propellers: typically observed in bodies found in water
- Characteristic large, parallel wounds, variable in depth, usually set a few centimeters apart and showing a sliced nature (J Forensic Sci 2000;45:917)
- Evidence of hemorrhage within the soft tissues surrounding the wound is highly indicative of an antemortem injury
- Absence of hemorrhage within the soft tissues surrounding the wound does not exclude an antemortem injury
- Prolonged immersion in water washes away the blood from the soft tissues
- Tangential cuts may result in partial or complete skin and soft tissue flap wounds
- Boat propellers: typically observed in bodies found in water
- Scissors (J Am Acad Dermatol 2020 Sep 15 [Epub ahead of print]):
- Closed pair of scissors usually produce a singular skin wound with a triangular, rhomboid or Z shape
- Open scissors usually produce 2 separate stabs wounds separated by a bridge of intact skin
- Broken glass (Med Leg J 2019;87:196, Med Sci Law 2005;45:81):
- Broken bottleneck or glass injuries may resemble the shape and diameter of the object; 1 or more glass spikes can produce multiple stab wounds connected by a circular or superficial semicircular cut
- Screwdrivers (J Forensic Sci 2007;52:1243):
- Cross shaped tip screwdrivers generally result in wounds showing 4 equally spaced cuts, resembling the cross shape of the tip
- Flathead screwdrivers generally result in wounds showing a rectangular morphology, resembling the flat end of the tip
- Ice pick (J Forensic Leg Med 2013;20:803):
- Purely pointed with no or very limited sharp surface
- Mechanism of injury is related to its high penetration ability
- Resulting wounds are usually small, round or slit-like; their diameter may vary based on the depth of penetration of the object
- May grossly resemble a mole
- Forks (Int J Image Graph Signal Process 2018;10:1):
- Kitchen forks generally cause 4 circular defects separated by a short distance, corresponding to the fork prongs
- Barbecue forks with 2 or 3 prongs generally cause groups of 2 or 3 wounds, with regular or irregular unremarkable skin between the wounds based on the angle of penetration
- Before manipulating the body, it is critical to take photographs of the body as it is received
- Medical interventions may alter the shape and size of the wound
- Clothing must be examined thoroughly to compare the number, size and location of tissue defects to the wounds observed on the body
- Anatomical location of the wounds must be described
- Location can give clues regarding the manner of death
- Number of wounds:
- Wounds can be described singularly or in clusters, depending on the case
- Each wound or cluster should be sequentially numbered
- Size and shape of wounds:
- Wound margins can be more or less apposed, resulting in size and shape artifacts
- Due to the skin and soft tissue elasticity and the direction of fibroelastic fibers (Langer lines or Langer lines of skin tension)
- Wound edges should always be gently apposed to evaluate the length and the shape of the lesion better
- Wound margins can be more or less apposed, resulting in size and shape artifacts
- Wound's path and direction:
- Always remember that stabbing deaths are dynamic rather than static situations
- Direction of the thrust is based both on the skin wound feature and the wound track
- Must be determined during the internal examination
- Involved organs must be included in the report
- Always remember that stabbing deaths are dynamic rather than static situations
- Depth of the wounds:
- Due to the soft tissue elasticity, the wound depth does not necessarily represent the length of the blade
- Vigorous stab can indent the body surface (i.e. abdomen) and compress the soft tissues allowing the blade to reach deep tissues and organs at a greater distance than the blade length
- Suggested to describe the maximal depth, as recorded during the autopsy (e.g. "The wound depth is not less than…†or “The wound depth is approximately...â€)
- Due to the soft tissue elasticity, the wound depth does not necessarily represent the length of the blade
- Internal organs:
- Direct evidence of stab wounds can be observed in the involved organs (e.g. heart, lungs, liver)
- Due to the respiratory phases, the lung can show injuries that are longer or shorter than the actual blade length
- During inspiration, the lung expands and comes close to the chest wall, thus becoming easier to be involved by the stab wound
- During the exhalation, the contraction of lung brings it away from the chest wall, making it harder to be reached by the blade
- Direct evidence of stab wounds can be observed in the involved organs (e.g. heart, lungs, liver)
- Evaluation of blood loss following sharp force trauma is suggested (Int J Legal Med 2020;134:1123)
- Signs of severe blood loss include extreme paleness of the internal organs, even if they are not directly involved (e.g. kidneys)
- Sometimes bleeding is not extensive and death is due to vascular injury complications (e.g. air embolism to the heart)
- Radiology studies can be helpful in sharp force traumas (Acta Radiol 2010;51:92)
- Postmortem Xrays or computed tomography may show (Leg Med (Tokyo) 2009;11:4):
- Retained weapons or their fragments
- Allow for collection as evidence
- Help in preventing autopsy operators from accidental injuries
- Pneumothorax
- Air embolism
- Additional autopsy techniques are required to confirm
- Retained weapons or their fragments
- Homicidal sharp force injuries:
- No specific anatomical location (random)
- Usually, numerous deep wounds
- Mostly stab wounds (Forensic Sci Med Pathol 2018;14:295)
- Additional injuries are often present:
- Defense injuries (J Forensic Leg Med 2012;19:207)
- Active: on the palms of the hand in the attempt of the victim to grab the blade
- Passive: on the dorsal or anterior aspects of the forearm or hands in the attempt of the victims to protect themselves from the blade
- Clothes are typically involved
- Suicidal sharp force injuries:
- Typical location
- Wrist
- Neck
- Thorax
- Only accessible areas of the body are involved
- Posterior aspects are virtually never involved
- Mostly incised wounds
- If present, usually 1 deep stab wound
- Rarely a few stab wounds can be present
- Hesitation marks are typically observed (J Forensic Sci 2016;61:1515)
- Typically, linear, parallel, superficial incised wounds involving the upper extremities
- Hesitation stab wound can also be observed, especially on the chest; typically, there are progressively deeper stab wounds and a single stab wound penetrating into the chest wall, hitting an internal organ
- Remote hesitation marks are usually in the form of linear, parallel scars
- No additional injuries are present
- No defense injuries
- Clothes generally are not involved
- Victims tend to remove clothes to be sure that they will cut / stab the right anatomical location
- Typical location
- Accidental sharp force injuries:
- Rarely described (Am J Forensic Med Pathol 2001;22:358)
- Rarely reported in the literature (Arch Kriminol 2011;228:108)
- Hard to demonstrate
- Only a comprehensive medicolegal death investigation helps determine the manner of death
- Fixation of the blade, meaning that the knife is securely gripped and held firmly, seems the primary factor in determining accidental stabbing fatalities
- Common defense theory in court is about the possibility of the victim running or falling onto a knife and sustaining a stab wound
- Rarely described (Am J Forensic Med Pathol 2001;22:358)
- Frequently asked question to the forensic pathologist in stab wound deaths
- Knight found that the velocity and sharpness of the blade are critical factors in consideration of the amount of force needed to cause any given stab wound (Forensic Sci 1975;6:249)
- Green found that the skin was the most resistant tissue to penetration (J Forensic Sci Soc 1978;18:161)
- Clothing increased the force required to produce a stab wound
- O'Callaghan confirmed that the skin was the most resistant tissue to penetration (Forensic Sci Int 1999;104:173)
- Gitto et al. performed a study on cadaveric chest tissues (skin and soft tissue, cartilage and bone) using 3 different types of blades (Am J For Med Path 2021 May 4 [Epub Ahead of Print])
- Skin is the most resistant tissue encountered by the blade
- Maximum peak force of 261 N has been recorded to penetrate the chest tissues
- Serrated edge blades showed difficulties in penetrating chest bones and cartilage compared with the plain edge blades
- 21 year old man who died due to accidental femoral vessels injuries by a broken glass (Med Leg J 2019;87:196)
- 24 year old man who committed suicide by a transcranial stab wound (Am J Forensic Med Pathol 2008;29:268)
- 42 year old man who committed suicide by more than 90 stab wounds (Int J Legal Med 2001;115:167)
- 45 year old man who committed suicide by an atypical cut throat injury (J Forensic Leg Med 2009;16:492)
- 45 year old man killed with a dessert spoon (For Sci Int Rep 2020;100094)
- 59 year old woman died due to accidental impalement by a broken rose bush (Am J Forensic Med Pathol 2018;39:341)
Contributed by Lorenzo Gitto, M.D., Ponni Arunkumar, M.D., Luigi Bonaccorso, M.D. and the Cook County Medical Examiner's Office
Comment Here
Reference: Sharp force injuries
Comment Here
Reference: Sharp force injuries
- Spinal cord injuries may lead to disruption to the axonal tracts running the length of the cord, leading to loss of function and increased rates of mortality and morbidity
- Clinical symptom complex relates directly to the level and severity of cord injury
- Traumatic injury to the spinal cord may take the form of localized compression, contusion, laceration, hemorrhage, flexion / extension injury or even direct penetrating injury from a knife or bullet
- Vertebral fractures and dislocations of the vertebral column may result in concomitant spinal cord injury
- Globally, between 250,000 and 500,000 patients each year sustain spinal cord injuries (J Spinal Cord Med 2016;39:493)
- In the United States, there are 17,000 new cases of spinal cord injury annually
- Males between the ages of 16 to 30 years are the most prone (Hodler: Diseases of the Brain, Head and Neck, Spine 2020-2023, 1st Edition, 2020)
- 38% of new spinal cord injury cases yearly are due to motor vehicle accidents, followed by falls at 30%, violent encounters at 13%, sports injuries at 9% and iatrogenesis at 5% (J Spinal Cord Med 2016;39:493)
- Cervical cord injuries may result from whiplash type injuries, including in the context of shaking of infants
- Up to 67% of spinal cord injuries are cervical, with ~25% thoracic and 10% involving lumbar cord
- Injury to the upper cervical spine and cord
- Anteroposterior shear force or rotational force → disruption of the transverse ligament of C1 → atlantoaxial subluxation with or without odontoid fracture and no cord injury (J Am Acad Orthop Surg 2002;10:271)
- Compressive vertex impacts (falls) → compression fracture of the anterior and posterior arches of C1 with lateral displacement of the fragments to C2 without cord injury (J Athl Train 2012;47:489)
- Forcible hyperextension of the neck (judicial hangings or motor vehicle accidents) → fracture of pedicles of C2 → anterior dislocation of C2 or C3 with or without odontoid fracture
- Ring fractures (J Korean Neurosurg Soc 2014;56:534)
- Occur at the base of the skull leading to separation of the foramen magnum from the skull
- The spine pushes against the base of the skull leading to pontomedullary junction lacerations
- Caused by substantial blunt force trauma (e.g., motor vehicle collision) and commonly associated with temporal bone fracture
- Causes of death include dislocation of the atlanto-occipital junction, hemorrhage in the pons and brainstem injury
- Injury to the middle and lower cervical spine (C4 - C8)
- Most common type of nonfatal spinal cord injury
- More severe than upper cervical spine injuries
- Spinal ligamentous injury is always present
- Hyperflexion injuries (blows to the back, shallow water diving, vehicle rollover) → teardrop fracture (pinching off of the anterior part of the vertebral body and backward displacement of posterior part into the spinal canal and cord) (Asian Spine J 2009;3:73)
- Combination of rotational movements (automobile accident) → subluxation and spinal canal impingement
- One of the most immediate factors determining survival rate is respiratory control (Spine (Phila Pa 1976) 2001;26:S27, Front Neurol 2019;10:282)
- Injury at C4 or higher → loss of phrenic nerve control over diaphragm → total dependence on accessory muscles
- Other existing conditions like organ failure, shock lung, air embolism or hemothorax might overwhelm the lungs, leading to death
- Quadriplegia may ensue if injury is above level of emergence of the brachial plexus roots
- Paraplegia may ensue if injury is below level of emergence of brachial plexus roots (T1 or T2)
- Injury below C4 → bladder and bowel function disability → recurrent and chronic cystitis and pyelonephritis
- Injury at C4 or higher → loss of phrenic nerve control over diaphragm → total dependence on accessory muscles
- Spinal cord injury without radiographic abnormality (SCIWORA) (Adv Orthop 2018;2018:7060654)
- An entity based on clinical signs of posttraumatic spinal cord injury without evidence of fracture or malalignment on imaging
- MRI is now a preferable modality because of its superior ability to identify soft tissue lesions that may not be visualized in plain radiographs or CT
- Mostly seen in children rather than adults, due to increased head to body ratio and immaturity of neck musculature
- 2 hit hypothesis: initial hyperextension or hyperflexion of the neck leads to a subsequent secondary insult that worsens the cellular reaction to the primary injury
- Craniocerebral trauma (J Neurosurg 1971;34:603)
- Spinal cord injuries occurring in conjunction with brain trauma resulting in sudden death
- Mostly high cervical spinal cord trauma with pontomedullary or brain stem injury
- Spinal cord injuries occurring in conjunction with brain trauma resulting in sudden death
- Injury to the thoracic spine
- Upper thoracic: higher resistance to injury due to the rib cage and costovertebral ligaments → greater force required
- Lower thoracic: vulnerable to rotational and flexion force injuries due to higher flexibility and lack of stability of lateral ribs
- Injury to the lumbar and lumbosacral spine
- Compression injuries with burst fractures (breaks of vertebra in multiple directions) are common
- Sitting position injuries, such as in airplane crashes (Korean J Neurotrauma 2015;11:195)
- Common to have fractures in this location related to osteoporosis and metastatic disease (pathologic fractures)
- Soft tissue disruption and hemorrhage are common findings at the site of bone fracture or ligament tears
- Grossly evident damage to the cord may take the form of indentation and edema to hemorrhage or disruption (Hodler: Diseases of the Brain, Head and Neck, Spine 2020-2023, 2020)
- Acute fatal cases of craniospinal trauma → look for perivascular petechial intramedullary hemorrhages with an otherwise normal look to the spinal cord (Radiopaedia: Traumatic Spinal Cord Injury [Accessed 11 April 2023])
- Assessment of spine / spinal cord injury may require removing the affected portion of the vertebral column en bloc to preserve anatomic relationships (J Orthop Sci 2006;11:3)
| Time and course of injury | |
| Time interval (postinjury) | Microscopic findings |
| 0 - 1 hours | Minimal to no changes |
| 4 hours | Central necrosis |
| 8 - 24 hours | Necrosis starts spreading peripherally |
| Within 24 hours | Polymorphonuclear cells dominate |
| Within 1 month | Macrophages dominate |
| Months to years | Residual cystic lesion with variable amount of neovascularization and gliosis |
- Acute spinal cord injury will show a mixture of edema, axonal spheroids, hemorrhage and infarct
- As time passes, the area of damage will expand with progressive cavitation and subsequent tract degeneration
- High mental and emotional burden on victims of disabling spinal cord injury → depression and suicide are among the most common complications of spinal cord injury (J Spinal Cord Med 2007;30:S76)
- Circumstances in which legal issues can arise include spinal injuries after chiropractic management, in suspected child abuse cases, complications of spinal surgery and in sports and training (World Neurosurg 2021;149:e108, Int J Legal Med 2021;135:1481)
- Filum terminale
- Lumbar cord
- Mid to lower cervical cord
- Thoracic cord
- Upper cervical cord
Injuries to the upper cervical cord are less common due in part to more space around the cord in this region, as well as restriction of motion by the transverse ligament of the atlas. The thoracic rib cage and costovertebral ligaments provide added stability to the thoracic spine. The lumbar region would be more prone to injury due to less lateral stability and more flexibility than the thoracic region, though still is less susceptible to injury than the mid / lower cervical region. The filum terminale is a fibrous band connecting the lower end of the cord (conus medullaris) to the posterior coccyx and not typically injured without disruption / injury of adjoining structures.
Comment Here
Reference: Spine and spinal cord traumatic injury
- Unexpected death of an individual not attributable to extracardiac causes within 1 hour of symptom onset or within 24 hours of last being known in good health (if death is unwitnessed) (Intern Med J 2019;49:826)
- Some definitions extend the time range with symptom onset up to 24 hours without diagnosed cardiac conditions within that time frame
- Sudden cardiac death is the unexpected death of an individual from apparent cardiac causes without symptoms or within 1 hour of symptom onset
- Careful gross and microscopic examination is essential to rule out identifiable causes of sudden cardiac death
- A negative autopsy without observable gross or microscopic findings should warrant additional testing, including genetic testing, especially if there is a history of sudden cardiac death in the family
- ICD-10:
- I46.1 - sudden cardiac death, so described
- Other cardiovascular disorders:
- I10-16 - hypertensive diseases
- I20-25 - ischemic heart diseases
- I33 - acute and subacute endocarditis
- I34 - nonrheumatic mitral valve disorders
- I35 - nonrheumatic aortic valve disorders
- I36 - nonrheumatic tricuspid valve disorders
- I37 - nonrheumatic pulmonary valve disorders
- I38 - endocarditis, valve not specified
- I40 - acute myocarditis
- I42 - cardiomyopathy
- I44 - atrioventricular and left bundle branch block
- I45 - other conduction disorders
- I5A - nonischemic myocardial injury (nontraumatic)
- Most common causes of sudden cardiac death vary by age:
- Under the age of 35: most common etiologies include congenital anomalies, heritable disorders and idiopathic causes (Circulation 2016;133:1006)
- Over the age of 35: most common etiology is atherosclerotic cardiovascular disease and its sequela (Circ Res 2015;116:1887)
- Atherosclerotic and hypertensive cardiovascular disorders:
- Coronary artery atherosclerosis (most common cause over age 35):
- Approximately 75 - 90% of all sudden deaths due to natural disease among those 35 - 64 years of age
- Associated with hypertension and diabetes mellitus
- Accelerated atherosclerosis is associated with stimulant drug use (especially cocaine), particularly in males less than 35 years of age and premenopausal women (Atherosclerosis 2017;262:154)
- Accelerated atherosclerosis in younger persons may be associated with genetic disorders related to lipid and triglyceride metabolism (Cardiol Clin 2015;33:267)
- May have significant impact on primary family members
- Gross findings:
- Myocardium may demonstrate either ventricular dilation or hypertrophy in chronic disease
- Coronary luminal stenosis may be concentric or eccentric (it is unclear if either type has an increased risk of adverse events); a variety of grading systems are used and are up to practitioner preferences
- Some pathologists use numeric values to indicate degree of stenosis (i.e., 10%, 50%, etc.)
- Some pathologists use a qualitative scale (i.e., mild, moderate, severe, occlusive, etc.)
- Generally, the greater degree of luminal stenosis, the higher the risk of cardiac event
- Coronary calcifications should be noted as rigidity of the vascular wall may increase the risk of cardiac events even absent atherosclerosis (Int J Cardiol Heart Vasc 2016;14:41)
- Early infarcts may show no changes
- Nitroblue tetrazolium staining may be used to help accentuate early infarcts (Br J Exp Pathol 1978;59:254)
- Acute and subacute infarcts may demonstrate pale discoloration or hemorrhage
- Marked softening of the myocardium may be present in subacute infarcts
- Subacute infarcts (typically 3 - 7 days) may evolve into ventricular rupture with development of hemopericardium and cardiac tamponade
- Remote infarcts will be pale, fibrous and often with thinning of the myocardium
- Compensatory hypertrophy may be present in the viable myocardium
- Microscopic findings:
- Myocyte abnormalities cannot be detected by routine histologic staining for 4 - 6 hours after myocardial infarction
- People dying rapidly of myocardial infarctions may have no myocyte abnormalities (such as by ischemia induced dysrhythmia / arrhythmia)
- Early changes are nonspecific and may include cytoplasmic hypereosinophilia, myofiber irregularities and edema
- Contraction band necrosis is evidence of irreversible ischemic change as the sarcomeric proteins begin to break down
- Coagulative necrosis begins within 24 hours after the ischemic event associated with hemorrhage, neutrophilic infiltrates and continuing myocyte changes (include nuclear pyknosis and dropout)
- Subacute infarcts evolve with macrophage infiltration and necrosis; fibroblasts will also begin infiltrating
- Remote infarcts / chronic ischemic change associated with cardiac myocyte drop out and resultant interstitial fibrosis and fibroblast proliferation (varying depending on length of time and chronicity of ischemia)
- May also see hemosiderin laden macrophages
- Cross sections of involved coronary arteries should be taken to determine if a clot is postmortem or antemortem
- Ruptured fibrous capsule or hemorrhage within the wall of a vessel indicate acute plaque rupture
- Myocyte abnormalities cannot be detected by routine histologic staining for 4 - 6 hours after myocardial infarction
- Hypertensive cardiomyopathy:
- Can present as a chronic disease process (heart failure) or sudden cardiac death (via dysrhythmia / arrhythmia)
- Gross findings:
- Most commonly concentric (less commonly eccentric) thickening of the left ventricular wall without outflow tract obstruction
- End stage hypertensive damage may result in dilation and thinning of the ventricular walls
- Microscopic findings:
- Enlarged nuclei with squaring of the nuclear edges (aka boxcar nuclei); enlarged myofiber diameter (Am Heart J 2009;158:799)
- Coronary artery atherosclerosis (most common cause over age 35):
- Aortic abnormalities:
- Aortic aneurysm and dissection:
- Risk factors include hypertension, hyperlipidemia, tobacco smoking and male gender
- Unruptured aneurysm can lead to vascular compromise in downstream body areas or compression of adjacent structures
- Ruptured aneurysm can lead to rapid exsanguination
- Congenital aortic stricture (coarctation) and post valvular stenosis:
- Can lead to hypertensive complications upstream of the site of narrowing and hypotensive complications downstream from the site of narrowing
- May be associated with other vascular or congenital abnormalities
- Infective complications of the aorta:
- Syphilis is the most commonly associated agent; rare in the United States due to the availability of treatments
- Aortic aneurysm and dissection:
- Coronary artery abnormalities:
- Anomalous coronary arteries
- Coronary arterial arteritis and aneurysm
- Fibromuscular dysplasia
- Other nonischemic coronary artery disorder
- Myocardial bridging (intramural coronary artery) (J Invasive Cardiol 2015;27:521)
- Controversial cause of sudden cardiac death
- Proposed mechanism is that myocardial contraction causes constriction of the intraluminal segment, resulting in reversible ischemia
- Cardiomyopathies:
- Myocardial dysfunction due to primary myocardial disease or secondary to systemic disease or treatment of systemic disease (such as cardiotoxic chemotherapeutic agents)
- Primary or secondary dilated cardiomyopathy
- Hypertrophic (and obstructive) cardiomyopathy
- Restrictive cardiomyopathy
- Arrhythmogenic right ventricular cardiomyopathy / dysplasia
- Takotsubo cardiomyopathy
- Inflammatory conditions of the endocardium, myocardium and pericardium:
- Infective endocarditis
- Noninfective endocarditis
- Infective myocarditis
- Noninfective myocarditis
- Noninfective pericarditis
- Noninfectious disorders of the heart valves:
- Primary disorders may be due to congenital abnormalities or due to cardiac flow abnormalities
- Mitral valve prolapse (Echocardiography 2019;36:1549)
- Prevalence of 2 - 3% in general population (Circulation 2019;140:952)
- May be associated with Marfan syndrome or other genetic connective tissue disorders
- Gross findings: enlarged, ballooning of the mitral valve leaflets
- Microscopy: myxoid degeneration of the central spongiosa of the valve leaflet (due to buildup of acid mucopolysaccharides)
- Can be seen in cases of sudden death, though controversial if it is causative or coincidental
- Bicuspid aortic valve and other congenital valvular abnormalities (Development 2020;147:dev183020)
- Predisposed to accelerated valvular degeneration due to flow abnormalities around the affected valves
- Degenerative valve disease (including valvular stenosis and regurgitation)
- Physiologic abnormalities of valve function, often associated with valvular sclerosis and changes to the papillary musculature and chordae tendineae
- Degree of functional impairment should be based on antemortem studies
- Morphologic changes do not always accurately depict the degree of physiologic impairment due to compensatory mechanisms during life
- See related topic (Degenerative valve disease)
- Mitral valve prolapse (Echocardiography 2019;36:1549)
- Secondary valvular disorders are most commonly associated with inflammatory and postinfective causes
- Rheumatic heart disease
- Immune complex mediated damage to the cardiac valves after Group A streptococcal infection (most commonly mitral) (Clin Microbiol Rev 2014;27:264)
- Generally considered rare due to the use of antibiotics to treat streptococcal infection
- More commonly seen in elderly patients
- Connective tissue disorders
- Drug induced valvular injury
- Prosthetic heart valves
- Rheumatic heart disease
- Primary disorders may be due to congenital abnormalities or due to cardiac flow abnormalities
- Congenital heart disease:
- Primary cardiovascular disorders are the most common congenital disorders, affecting ~0.08% of live births (Circ Res 2017;120:908)
- Complications of congenital heart defects vary widely from asymptomatic to severe and life threatening
- Asymptomatic, undiagnosed cardiac defects can progress to life threatening disease if not treated
- All disorders arise from abnormal embryogenesis and development
- See related topic (Heart - embryology)
- Disorders can include atrial septal defects, ventricular septal defects, outflow tract abnormalities and abnormalities of the great vessels
- See related topics (Tetralogy of Fallot and VACTERL association)
- Neoplastic lesions:
- Primary and secondary cardiac neoplasms are exceedingly rare entities (Curr Treat Options Oncol 2019;20:66)
- Death can occur due to a variety of mechanisms including cardiac flow obstruction, heart failure and conduction abnormalities resulting in arrhythmia
- See related topics under benign and malignant tumor headings (Heart)
- Primary and secondary cardiac neoplasms are exceedingly rare entities (Curr Treat Options Oncol 2019;20:66)
- Disorders of the conduction system:
- Conduction system is comprised of specialized fibers allowing for the rapid passage of electrical signals through the heart in a synchronized manner
- Primary or secondary abnormalities of these specialized fibers may result in asynchronous transmission and the development of dysrhythmias and arrhythmia (Circulation 2011;123:904)
- Nearly all disorders of conduction will have no gross anatomic findings at the time of autopsy unless due to prior injury or secondary to other disease process
- Functional (primary) disturbances include channelopathies (such as Long QT syndrome), pre-excitation syndromes, sick sinus syndrome, vagal inhibition and spontaneous idiopathic dysrhythmias associated with excitation (either physical or emotional excitation)
- Structural disturbance (primary or secondary) include Lev’s disease, collagen vascular disorders with cardiac involvement and infiltrative involvement of systemic disease (hemochromatosis, amyloidosis, etc.)
- Microscopy may reveal no abnormalities, nonspecific fibrosis or discrete lesions
- If conduction studies are indicated at the time of autopsy, specialized dissection methods should be undertaken and planned for prior to examination (Anat Sci Educ 2009;2:78)
- Careful and extensive sampling may be indicated
- In cases of negative autopsy, testing for genetic mutations which can lead to cardiac dysrhythmias may be indicated (Trends Cardiovasc Med 2017;27:207)
- Testing availability and appropriate samples vary by laboratory; confirm with your preferred testing provider prior to examination
- Medical records will be useful in determining if prior events occurred, what their triggers may be and what work up was conducted (especially for individuals with vagal or excitation type events)
- Conduction system is comprised of specialized fibers allowing for the rapid passage of electrical signals through the heart in a synchronized manner
- 21 year old man with sudden cardiac death due to left ventricular noncompaction, arrhythmogenic right ventricular cardiomyopathy and acute myocardial infarction (Egypt Heart J 2017;69:157)
- 24 year old man with sudden cardiac death due to acute myocardial infarction in the setting of anabolic steroid abuse (Forensic Sci Res 2019;4:267)
- 35 year old man with sudden cardiac death due to tuberculosis (Breathe (Sheff) 2015;11:67)
- 37 year old man with sudden cardiac death due to stellate ganglionitis (Auton Neurosci 2021;234:102837)
- 58 year old man with sudden cardiac death due to cardiac involvement by lymphoma (J Formos Med Assoc 2018;117:939)
- Cardiac examination should include weight with excess valvular tissue removed
- Note any external features, including general size and shape of the heart, areas of discoloration or defects
- Coronary arteries and their major branches should be identified and sectioned at 3 mm intervals along their course (Virchows Arch 2017;471:691)
- Note any stenosis, calcification, perivascular hemorrhage, thrombus or dissection
- Note areas of myocardial bridging including length of the involved segment
- If coronary artery bypass grafts are present, note the origins, anastomotic site, course and patency
- Serially section the ventricles in a plane parallel to the base of the heart, from apex to base at 1 cm intervals until approximately 2 cm from the atrioventricular valves (Cardiovasc Pathol 2012;21:2)
- Measure the thicknesses of the left ventricular free wall, interventricular septum and right ventricular free wall, excluding the papillary muscles
- Note areas of discoloration, fibrosis or areas of thinning
- Note the distribution and pattern of epicardial fat, especially in the right ventricle
- Note the thickness and areas of discoloration of the epicardium
- Cardiac valves should be inspected for abnormalities prior to sectioning; note areas of obstruction, stenosis or other abnormalities
- Open the heart by following the direction of blood flow
- Posterior incision of the right atrium to right ventricle through the tricuspid valve
- Anterior incision of the right ventricle to the pulmonary artery through the pulmonic valve
- Posterior incision of the left atrium to the left ventricle through the mitral valve
- Anterior incision of the left ventricle to the aorta through the aortic valve
- Measure the circumference of the cardiac valves
- Note any areas of thickening, vegetations, chordae tendineae and papillary muscles
- If prosthetic valves are present note the type of valve, if it is appropriately seated / attached and any abnormalities of the valve or artificial surfaces
- Section the remaining myocardium to include the conduction system
- Microscopic sections should be taken of areas of interest
- The conduction system, including the SA and AV nodes, should be sampled in otherwise negative autopsies
- Connolly: Autopsy Pathology: A Manual and Atlas, 3rd Edition, 2015, DiMaio: Forensic Pathology, 2nd Edition, 2001, Dolinak: Forensic Pathology - Principles and Practice, 1st Edition, 2005, Miller: Diagnostic Pathology - Cardiovascular, 2nd Edition, 2018, Spitz: Spitz and Fisher's Medicolegal Investigation of Death - Guidelines for the Application of Pathology to Crime Investigation, 4th Edition, 2005
A 75 year old woman is consented for a hospital autopsy. Her past medical history is significant for hypertension, hyperlipidemia and congestive heart failure. At autopsy, the findings shown above are identified in the mitral valve. Remote infection with which organism is most likely to have precipitated these findings?
- Coxsackie virus A and B
- Enterococci
- Group A streptococci
- Staphylococcus aureus
- Trypanosoma cruzi
Comment Here
Reference: Sudden cardiac death
- 1 day
- 3 - 7 days
- 1 weeks
- 3 - 7 weeks
- 1 year
Comment Here
Reference: Sudden cardiac death
- In outline form, the FAD summarizes the pertinent autopsy findings, categories may include: Cause of Death / COD (natural or unnatural), natural diseases or pre-existing conditions, evidence of medical / surgical therapy, postmortem changes, identifying body marks, and toxicology
- Complications of hemorrhagic stroke, drowning, asphyxia by hanging, etc.
- State any additional microscopic diagnoses here
- Hypertension, hypercholesterolemia, type II diabetes, etc.
- Cardiac pacemaker, internal fixation of left tibia, CABG, etc.
- Decomposition, marbling, skin slippage, etc.
- Tattoos on the arms, forearms, right calf, etc.
- Can be broken down by volatiles (ethanol in blood and vitreous fluid) and drugs (medications or illicit drugs found in blood or urine)
- Probably the most important section of the autopsy report that will be read by lawyers, judges, law enforcement, insurance companies, lay public, and most importantly the decedent's family members
- A well written and thought out opinion may reduce the need for the pathologist to be summoned to testify in a courtroom
- An opinion section links the COD with MOD and describes all pertinent findings in paragraph form
- The opinion section needs to be precise, factual, logical
- Depending on the complexity of the case, an opinion section may be a few short sentences or several pages
- Deaths which occur due to complications of medical treatment
- Not limited to people dying in a hospital setting
- Medications and medically administered solutions are an important and significant source of morbidity and mortality
- If a medical device is used in patient care, it should be investigated as a cause or contributor to death
- Most procedure related deaths occur due to the underlying natural disease or injury which made the procedure necessary
- Comorbidities and social factors should be considered when determining the impact that medical treatment had on the cause and manner of death
- Manner of death classification with therapy related deaths is complex and should weigh a variety of factors, including what direct impacts (if any) the treatment had on morbidity and mortality
- A variety of medications and medically prepared solutions can result in complications which may cause or contribute to death
- Likelihood of reactions or interactions between medications increases significantly with an increasing number of administered agents (Expert Opin Drug Saf 2014;13:57)
- Medication reactions can occur even at the recommended dosages and frequency:
- Hypotension (i.e. antihypertensives)
- Hyper / hypoglycemia (i.e. antidiabetics)
- Electrolyte abnormalities (i.e. antihypertensives, replacement supplements, overhydration)
- Dysrhythmias (i.e. digitalis)
- Idiopathic reactions (i.e. serotonin syndrome, neuroleptic malignant syndrome)
- Paradoxical reactions (i.e. antidepressants, benzodiazepines)
- Acute and delayed allergic reactions (i.e. monoclonal antibodies)
- Anaphylaxis (i.e. penicillin)
- Chronic systemic or organ specific toxicities:
- Most common with chemotherapeutic or immunomodulatory therapies
- Cardiac toxicity
- Hepatic toxicity
- Bone marrow suppression (i.e. ineffective hematopoiesis, infection)
- Secondary neoplasia
- Radiology contrast material:
- Most reactions occur with iodinated contrast
- Rare reactions have been reported with gadolinium contrast (CNS Drugs 2018;32:229)
- Barium and other orally introduced contrast material can lead to a variety of complications but these are rarely fatal on their own
- Blood products / apheresis:
- Blood products are not benign and can result in a variety of reactions that cause or contribute to death
- Any reaction believed to have caused or contributed to death must be reported to the FDA
- Acute / delayed hemolytic reactions
- Allergic / anaphylactic reactions
- Transfusion related acute lung injury (TRALI)
- Transfusion associated cardiac overload (TACO)
- Especially in persons with underlying cardiac / renal conditions
- Sepsis / transfusion associated infectious disease transmission
- Electrolyte abnormalities (i.e. hyperkalemia with massive transfusion protocols, hypocalcemia from citrate toxicity)
- Resuscitation fluids:
- Hyper / hypotonic fluids can lead to significant electrolyte abnormalities, especially in patients on NPO (nothing by mouth) diet
- Isotonic fluids, especially at large doses (such as intraoperative irrigation), can result in significant electrolyte and physiologic abnormalities
- Sudden corrections of electrolyte abnormalities can result in death (i.e. central pontine myelinolysis)
- Important measures to review include fluid inputs, urine outputs and antemortem / postmortem electrolyte measurements
- Medication and dosage errors:
- More common for patients residing in facilities (inpatient, long and short term) versus outpatients
- Medication administration logs can be helpful in determining under / overdosage
- If medications are available, check pill counts and descriptions against bottle
- Pill identifier websites are available at no cost to providers
- If a medication or dosage error is suspected and antemortem blood samples are available, obtain them for possible toxicology testing (the closest after the administration time preferred)
- Some genetic testing is available for persons believed to be hypermetabolizers or poor metabolizers
- Both implanted and external medical devices may result in complications that cause or contribute to death
- Intubation / rescue airways / tracheostomy tube:
- Pneumothorax
- Laryngeal, tracheal or esophageal trauma
- Intubation of the esophagus / mainstem bronchus
- Attempted intubation with impaction of foreign body
- Dislodgement or occlusion
- Orogastric tubes
- Craniofacial trauma (i.e. malplacement into the cranial vault)
- Foley catheters
- Infection
- Bladder perforation
- Vascular catheters
- Hemorrhage
- Infection
- Thromboembolism
- Arteriovenous fistulization
- Implanted medical devices
- Orthopedic hardware: infection, bony fracture, hardware failure
- Pacemaker / implanted defibrillators: erroneous or repeated discharge, lead displacement, battery failure
- May require interrogation of the device
- Nerve stimulators: lead displacement
- External ventricular assist devices: pump failure, hemorrhage, thromboembolism
- Tissue expanders / implants: infection, chemical injury, foreign body reaction
- Medical synthetic implants (i.e. mesh): infection, scarring
- Device embolization (i.e. catheter tip embolization, IVC filter dislodgement)
- Catheter failure (i.e. hemorrhage, air embolism)
- External equipment failure
- Ventilators
- Medication administration pumps
- Cardiac bypass pumps
- Any medical equipment suspected to have been involved in a patient's injury or death should be removed from use and investigated
- Manufacturer or appropriate engineer may need to examine the device to determine safety prior to continued use (maintain the device as is until it can be examined)
- Radiation can cause a variety of acute and delayed complications
- Radiation induced necrosis (i.e. wound dehiscence, infection)
- Radiation fibrosis / scarring (i.e. mediastinal fibrosis, bowel / bladder obstruction)
- Secondary malignancy (i.e. angiosarcoma)
- Vast majority of deaths during medical procedures occur as a direct result of the underlying natural disease process or injury which required the treatment
- Some state and local statutes require medicolegal investigation of all deaths occurring during medical procedures or under anesthesia; this does not always necessitate an autopsy
- Severe underlying natural disease is another common cause of death (i.e. myocardial infarction due to severe coronary artery disease during a surgical procedure)
- Procedural safety has greatly improved in recent years due to mandatory safety checklists and a time out process conducted just before the start of an invasive procedure (AORN J 2019;109:P5)
- All procedures carry inherent risks, which are often modified by the severity of disease or injury, underlying comorbidities (i.e. hypertension, diabetes mellitus) and social factors (i.e. tobacco, alcohol, drug use)
- Surgical procedures are commonly assigned a risk score which takes into account risk factors and the likelihood of significant morbidity or mortality due to the procedure
- Emergent procedures (conditions requiring treatment due to risk of severe morbidity and mortality)
- Consent is often implied or signed by a surrogate due to severity of illness / injury
- Risks of morbidity or mortality due to untreated injury / illness are greater than that of the procedure
- Traumatic injuries (i.e. gunshot wounds, stab wounds, blunt injuries, burns)
- Medical emergencies (ruptured vascular aneurysms, cerebrovascular events, gastrointestinal tract perforation)
- Consent is often implied or signed by a surrogate due to severity of illness / injury
- Nonemergent / elective procedures (conditions which require treatment but are typically stable)
- Require informed consent with understanding of known procedural risks
- Not all elective procedures are low risk and often carry an associated risk score
- Orthopedic joint replacements (i.e. bone marrow embolization, infection)
- Cancer resections
- Vascular surgeries (i.e. stable vascular aneurysms, asymptomatic endarterectomy)
- Routine maintenance procedures (tonsillectomy, cholecystectomy, skin excisions)
- Cosmetic procedures
- While generally considered to be low risk; individual tolerances and comorbidities vary
- Under normal circumstances death should not occur
- Nonreconstructive plastic surgical procedures
- Liposuction (i.e. adipose or air embolization, infection)
- Filler / dermal subcutaneous injections (i.e. filler embolization, infection)
- Botox injection (i.e. systemic botulinum toxicity via vascular injection)
- While generally considered to be low risk; individual tolerances and comorbidities vary
- Dental procedures
- Generally considered low risk but comorbidities can increase the risk of adverse events
- Anesthetic and medication overdoses have been reported (J Forensic Sci 1989;34:377)
- Bacteremia, sepsis and infective endocarditis can occur
- Deaths under anesthesia
- Type of anesthesia (general versus local)
- While local anesthetics are generally considered safer, their use can still result in death (i.e. vascular injection leading to dysrhythmia)
- Types of inhaled anesthetics (i.e. wrong type / dosage of gas, incorrectly filled tanks, pressure valve failure resulting in pneumothorax)
- Length of time under anesthesia (longer times significantly increase risk)
- Underlying genetic conditions predisposing to reactions (i.e. malignant hyperthermia)
- Type of anesthesia (general versus local)
- Remember that medication errors can also occur during procedures
- Deaths which occur during the course of medical treatment or procedures without identifiable cause
- Extensive, thorough medical record review can be helpful in excluding potential causes of death
- If the survival interval between the inciting event and death is long, extensive review of medical records might be the only way to determine what occurred (or did not occur)
- Often require an autopsy to eliminate occult drug toxicity, injury or natural disease
- If no anatomic or toxicologic cause of death can be determined by autopsy, additional factors which should be considered / excluded:
- Electrolyte abnormalities (i.e. hyper / hypokalemia, hyper / hypocalcemia)
- Hyper / hypoglycemia
- Idiopathic medication reactions / interactions
- Physiologic reactions (i.e. vasospasm, vasovagal mediated bradycardia, idiopathic dysrhythmias, hyper / hypotension)
- Despite safeguards, a variety of medical errors can occur during treatment
- Some errors are harmless and have no effect on the subsequent treatment course
- Some errors are harmful and can result in varying degrees of morbidity or mortality
- In general, known and expected complications of a procedure are not considered medical misadventures (i.e. infection, expected hemorrhage)
- Physicians and literature originating in the specialty (or specialties) of question are the best sources of knowledge for appropriate evidence based treatments and expected outcomes
- Medical misadventures are those injuries or outcomes which are not expected (i.e. vascular injury unrelated to the anticipated procedure site, ligation of the incorrect vascular supply, incorrect line placement without verification, wrong patient / wrong procedure)
- They do not imply medical incompetence or negligence
- They do not imply negligence
- They do not imply an unavoidable error occurred
- Every effort should be made to identify the source of the unexpected outcome and complicating factors which may have contributed (i.e. atypical anatomy, distortion due to prior procedures)
- Report language should only reflect factual findings
- Judgment of error should be reserved for appropriate legal / review body
- Subject matter experts in the field of practice are better versed than the pathologist at determining what are / are not appropriate treatments or complications
- Do not use malpractice or similar terminology, which should be part of a legal / review body determination
- Comorbidities often potentiate or adversely impact medical complications
- An increasing number of comorbidities significantly increases the risk that an individual will suffer complications during medical treatment and increases the likelihood of severe complications
- Chronic obstructive pulmonary disease / asthma / reactive airway disease (i.e. increased risk of pulmonary failure, prolonged intubation, pneumonia)
- Diabetes mellitus (i.e. poor wound healing, infection)
- Hypertensive and atherosclerotic cardiovascular diseases (i.e. poor wound healing, vascular complications)
- Dementia (i.e. aspiration)
- Some jurisdictions use a separate classification for most accidental or natural complications of medical treatment: therapeutic complication (J Forensic Sci 2006;51:1127)
- If death is directly related to underlying natural disease without contribution by medical treatment
- Manner is natural
- If death is related to the underlying injury without contribution by medical treatment
- Manner is determined by the cause of the injury: accident, homicide, suicide (and potentially undetermined)
- If death is due to a known and expected complication of therapy for a natural disease
- Manner is natural
- If death is due to use of inappropriate, defective or malfunctioning medical equipment / devices; and there is no evidence that the equipment was tampered with to result in malfunction
- Manner is accident
- If death is due to grossly negligent medical care without evidence of volitional act to cause harm or death
- Manner is accident
- This does not preclude the possibility of legal liability or actions by a medical board
- If death is due to a volitional act to cause harm or death (i.e. administration of large doses of opiate medications to cause cardiorespiratory arrest)
- Manner is homicide
- Law enforcement investigation will reveal additional information to support the manner in these cases
- Oftentimes caregivers that repeatedly cause harm to patients follow repeated patterns which may be revealed by thorough investigation (i.e. ICU nurse that has more cardiopulmonary arrests on their shifts than any other nurse due to smothering patients to create attention for themselves)
- If death is due to an undesirable or unexpected outcome of a diagnostic or therapeutic procedure and the circumstances are determined to be outside the realm of reasonably acceptable risk and expected outcome
- Manner is accident
- If death occurs in high risk surgical patients undergoing (or after) high risk procedures for natural disease (i.e. coronary bypass grafting due to coronary artery disease without procedural complications)
- Manner is natural
- If the death is due to undetermined causes (regardless of expected outcomes)
- Manner is undetermined
- There are a variety of gray zones and disagreements with some of the above classifications; however, these are the generally accepted classifications agreed upon by the National Association of Medical Examiners (NAME)
- For additional information about the nuances of death certification, please reference:
- DiMaio: Forensic Pathology, 2nd Edition, 2001, Dolinak: Forensic Pathology - Principles and Practice, 1st Edition, 2005, Froede: Handbook of Forensic Pathology, 2nd Edition, 2003, Spitz: Spitz and Fisher's Medicolegal Investigation of Death - Guidelines for the Application of Pathology to Crime Investigation, 4th Edition, 2005
- Accident
- Homicide
- Natural
- Suicide
- Undetermined
Ruptured abdominal aortic aneurysms carry a high mortality rate regardless of operative treatment. There is no evidence to support that the surgical procedure caused or contributed to death and thus the underlying natural disease is the cause of death. Therefore, the manner of death is best classified as natural.
Comment Here
Reference: Therapy related deaths
- Accident
- Homicide
- Natural
- Suicide
- Undetermined
This individual has a significant past medical history, develops sepsis and suffers a significant medical complication during treatment. Both the sepsis and medical complication are a result of needed treatment for the initial gunshot wounds. Therefore, the gunshot wounds (though not independently lethal) are the proximate cause of death. The manner of death is best classified as homicide. Her significant medical complications and natural disease would be appropriate to list under other significant contributing factors if they were felt to be contributory.
Comment Here
Reference: Therapy related deaths
- Most common (80%); occurs when two vehicles collide head on, or when a single vehicle hits a stationary object head on
- Vehicle occupants continue moving forward due to kinetic energy; impacting the windshield and dashboard
- Drivers show trauma of the anterior head due to impact with windshield or visor; may show skull fractures, atlantooccipital dislocation, neck fractures, diffuse axonal injury
- Drivers may have chest injuries due to impact with the steering wheel, with sternal and rib fractures, pulmonary contusions and lacerations (due to rib fractures), cardiac laceration / contusion, aortic dissection, hepatic and splenic lacerations
- May show pattern impact injury of the steering wheel
- Drivers may show wrist or forearm fractures if hands were positioned on wheel at time of impact
- Drivers may have patellar or femoral fractures due to impact with dashboard; or ankle fractures
- "Dicing injuries" to the left face and left arm: small abrasions / lacerations on driver due to shattering of the driver side window
- Front seat passengers: injuries similar to driver, but no steering wheel impact
- Dicing injuries of the right face and right arm due to shattering of passenger side window
- Unrestrained rear passengers may be thrown to front compartment of vehicle
Side impact:
- Usually due to one vehicle impacting the side of another vehicle
- All injuries seen in frontal impact collisions can occur
- Injuries should be more severe on side of impact; individuals on impacted side should have more severe injuries than those on the opposite side
Rear impact:
- May cause "acceleration" injuries (e.g. whiplash) which tend to be less severe
Rollover:
- Tend to be more severe; many different injury patterns can occur
- May cause traumatic asphyxia if individual is ejected and becomes trapped beneath vehicle
- May see pattern injury from seatbelts; pattern should correspond to position of individual in car (e.g. driver vs. passenger)
- Seatbelts can produce mesenteric, omental, or bowel contusions / lacerations
- Vehicle directly collides with fixed object or another vehicle
- No signs of braking at scene
- Decedent may have history of suicidal ideation or suicide attempts
- Vehicle speed: high speed impact may cause pedestrian to be thrown over vehicle
- Braking may result in pedestrian being "picked up" by vehicle or being thrown forward
- Type of vehicle: larger vehicles that hit pedestrian above their center of gravity tend to knock them down rather than pick them up
- Size / age of pedestrian: impact below pedestrian’s center of gravity causes them to be lifted and thrown
Injuries sustained by pedestrians:
- Tire / tread marks: on skin or clothing; can link pedestrian to vehicle
- Pattern injuries: in addition to tire marks, can include impressions of bumper, headlights, or other parts of vehicle; can be used to link pedestrian to vehicle
- Bumper fractures: occur when bumper strikes pedestrian's lower extremities; may not be associated with overlying cutaneous injury
- Measure distance from heel to estimate bumper height
- Contusion pockets: collections of blood in subcutaneous tissue or muscle; due to impact with hood or bumper
- "Stretch" lacerations of inguinal folds: due to overstretching of body at hip joint; appear yellow and dry
- Suicidal pedestrian deaths: need witness information and decedent history of suicidal ideation to corroborate
- Head trauma: most common lethal injury; may occur even in individuals wearing a helmet
- Basilar skull fracture is most common
- Motorcycle passengers tend to fall backwards, producing lacerations and fractures of posterior head
- Brush abrasions ("road rash") on exposed skin
- Traumatic asphyxia: may occur if motorcycle lands on individual
- Most bicycle accidents produce only minor trauma
- Degree of injury is largely related to speed of the impact
- Bicycle spoke injury: occurs when leg or foot passes through wheel spokes; causes crushing / avulsion of soft tissues; more common in children
- Toxicology of driver, passenger, and pedestrian, to include carbon monoxide for vehicle occupants
- Trace evidence: hair, blood, clothing fibers, glass chips, or paint chips can be used to link a car to a pedestrian death, or to determine a person's position in vehicle
- Subgroup of traumatic brain injury caused by angular or rotational acceleration / deceleration of the head, leading to a pattern of widespread injury to neurons, specifically to their axons (Trends Neurosci 2016;39:311)
- Acceleration / deceleration in the coronal plane in particular is associated with shearing force injuries
- Subdural hematoma (via tearing of bridging veins)
- Traumatic axonal injury
- Spectrum of injury ranges from subclinical to that of severe diffuse damage resulting in persistent vegetative state and death
- Axonal injury (traumatic or otherwise) can only be directly diagnosed by microscopic examination; axonal swellings / retraction balls (also known as spheroids) are characteristic of axonal injury
- Lesions of traumatic axonal injury most frequent in parasagittal white matter, corpus callosum, dorsolateral rostral brainstem
- B amyloid precursor protein (APP) immunostain is helpful for detection of axonal damage
- Axonal injury is a nonspecific term
- May be focal or diffuse (diffuse axonal injury [DAI])
- May be traumatic or nontraumatic etiology (especially secondary to hypoxic / ischemic injury)
- Traumatic axonal injury (TAI): axonal injury with trauma as the underlying etiology
- May be focal or diffuse
- TAI occurs with high frequency in the context of motor vehicle accidents; only in ~10% of fall injuries
- Head trauma victims who die with TAI tend to have a lower incidence of lucid interval, skull fracture, contusive injury or intracranial hematoma compared to those with fatal head injury without TAI (Ann Neurol 1982;12:557)
- Morphological manifestation of a traumatic brain injury typically due to strain or shearing force (Acta Neuropathol 2002;104:79)
- Axonal swellings are the result of axonal transport leading to accumulation of material (including heat shock protein, amyloid precursor protein) proximal to the site of axonal tear / axotomy (Exp Neurol 2012;233:364)
- Pathologic grading system for the severity of TAI has been previously proposed (Ann Neurol 1982;12:557, Histopathology 1989;15:49, PLoS One 2015;10:e0122329)
- Grade 1: axonal swellings seen only microscopically with no obvious macroscopic lesions are clinically associated with mild or moderate posttraumatic coma
- Grade 2: axonal swellings and macroscopic focal lesions in the corpus callosum are associated with moderate posttraumatic coma and severe disability
- Grade 3: axonal swellings, macroscopic focal lesions in both corpus callosum and brainstem are associated experimentally with the poorest outcome
- Correlation with clinical presentation and outcomes is unclear (J Forensic Leg Med 2017:48:35)
- Absence of validation in substantial human studies to directly correlate MRI findings with histopathologic findings complicates the interpretation of the TAI grade in clinical practice (Acta Neurochir (Wien) 2021;163:31)
- In diffuse axonal injuries, it is not only the magnitude of acceleration but also the time over which the acceleration occurs that produces the injury (DiMaio: Forensic Pathology, 2nd Edition, 2001)
- Diffuse vascular injury (J Forensic Sci 2003;48:626)
- Often accompanies moderate to severe TAI; it is likely that vascular damage is secondary to the same deformative forces
- Diffuse petechial hemorrhages may also be the result of fat emboli to the CNS
- Macroscopic findings (Int J Curr Res 2017;9:48426, Sud Med Ekspert 2022;65:24)
- Grossly evident lesions may accompany more severe injuries with TAI, including
- Petechial or more confluent hemorrhagic lesions in deep white matter structures like the corpus callosum, internal capsule and superior cerebellar peduncles
- Gliding contusions of frontal lobe white matter
- Deep cerebral hemorrhages of the basal ganglia
- Cerebral surface contusions or other hemorrhages (epidural / subdural / subarachnoid) are often not present
- Grossly evident lesions may accompany more severe injuries with TAI, including
- Diffuse vascular injury (J Forensic Sci 2003;48:626)
- Typically multiple petechial hemorrhages in the centrum ovale region of the frontal lobe or other regions where TAI is frequent
- Microscopic findings
- Histologic examination is needed for detection of TAI; it does not by itself result in grossly evident lesions
- Histologic findings are dependent upon survival time postinjury
- Sampling of regions including cerebral parasagittal white matter, corpus callosum, other long tracts (internal capsule, etc.) and brainstem should be performed in all cases where TAI suspected
- Shortly after traumatic brain injury, there is often a notable, singular swelling known as an axonal bulb (previously termed a retraction ball), which is indicative of probable complete axonal disconnection (Exp Neurol 2013;246:35)
- Amyloid precursor protein axonal accumulations may be detected within a few hours of injury, well before axonal spheroids would be visible by routine stains (Leg Med (Tokyo) 2009:11:S171)
- β amyloid precursor protein (APP) is the gold standard to detect axonal injury (J Lab Physicians 2023;15:399)
- By 24 hours, axonal spheroids visible by H&E stained sections
- Focal increase in calcium concentration in an axon precedes and can result in the development of axonal spheroids (Trends Neurosci 2016;39:311)
- Spheroids may persist for 1 - 2 months and may be highlighted by silver stains or immunostains for neurofilament or APP
- At 2 weeks postinjury, microglial clusters become evident in damaged areas; these may persist for multiple months (Neural Plast 2021;2021:5554824)
- Wallerian degeneration with fiber tract degeneration will occur over months and years postinjury (Curr Opin Neurol 2019;32:786)
- Differentiation of TAI from axonal injury secondary to ischemia may be difficult (Jenny: Child Abuse and Neglect - Diagnosis, Treatment and Evidence, 1st Edition, 2010)
- Features that favor the latter include microscopic evidence of necrotic neurons and geographic accumulations of APP
- Findings of widely scattered APP staining, APP staining in caudal brainstem and lesions of vascular injury in the corpus callosum or dorsolateral brainstem would favor TAI
- Note that both of these processes can co-occur
A 35 year old woman was brought to the emergency room after a high speed automobile accident. She was found unresponsive at the scene, with little external evidence of trauma. Severe brain injury was suspected. She was pronounced dead upon arrival at the ER. Autopsy revealed petechial hemorrhages within the corpus callosum and superior cerebellar peduncles. What other finding is most likely to be encountered in this patient?
- Diffuse axonal injury
- Diffuse subarachnoid hemorrhage
- Epidural hematoma
- Skull fracture
- Subdural hematoma
Comment Here
Reference: Traumatic axonal injury
- Biochemical analysis of body fluids (blood, urine, cerebrospinal fluid and vitreous humor) to measure endogenous constituents in dead bodies helps determine the cause of death
- Postmortem chemistry has become an important ancillary procedure for the forensic pathologist (Am J Forensic Med Pathol 1993;14:91)
- Specimens must be collected, labeled, stored and analyzed under established, standardized conditions (Connolly: Autopsy Pathology: A Manual and Atlas, 3rd Edition, 2015)
- Peripheral venous / arterial specimens best approximate antemortem values
- For toxicology, recommended to use femoral or subclavian vessels, via percutaneous collection with large bore needle and syringe
- 40 - 50 mL required
- Place portion in fluoride preservative and portion in anticoagulant
Vitreous Humor
- Most frequently used specimen for postmortem analysis
- Isolated and protected by the orbit, less subject to putrefaction than blood
- Not subject to diffusion of drugs and alcohols from the stomach
- Also free of erythrocytes
- Collect with small syringe attached to an 18 gauge needle, using gentle suction to remove all vitreous (2 - 5 mL in adult, 1 mL in newborn)
- Fluid from each eye is stored separately
Synovial Fluid
- Rarely used as substitute for vitreous humor
- About 1 mL can be aspirated from each knee joint
Urine
- Collect with large bore needle attached to syringe once bladder is exposed at autopsy or by urethral catherization before autopsy
Cerebrospinal Fluid
- Aspirated from cisterna magnum with needle, by standard percutaneous posterior lumbar puncture
- Aspirate through the spinal foramina after organ evisceration or by inserting a needle into a lateral ventricle after removing the skull cap, reflecting the dura and separating the cerebral hemispheres
Bile
- Rarely used
- Aspirate from gallbladder or directly from common bile duct in patients status post cholecystectomy
Gastric Contents
- Rinse external stomach with water
- Puncture stomach wall and pour stomach contents into bag
Hair
- Hair should be obtained by pulling to include hair roots
- Adequate sample is 0.5 g for DNA analysis, up to 10 g for analysis of heavy metals
- Tie together while maintaining orientation of hair roots
Fingernails
- Acquired by clipping or removing the entire nail
Fibroblasts for Tissue Culture
- Can be used for karyotyping, metabolic assays, enzyme assays and diagnostic ultrastructural studies
- Collect from skin, fascia, lung, diaphragm, muscle and cartilage
- Samples are placed in sterile tube containing culture medium (RPMI or MEM)
Tissue
- Liver, brain, kidney, cardiac muscle, skeletal muscle and peripheral nerve can be used for metabolic studies and nucleic acid analysis
- Should be obtained shortly after death and frozen rapidly in liquid nitrogen or dry ice and stored at -70°C
-
Diabetic ketoacidosis
- Vitreous glucose concentration (> 200 mg/dL or > 11.1 mmol/L) is the most reliable marker
- Also reliable are ketone bodies, urine glucose and glycated hemoglobin
- Increased postmortem serum and vitreous urea nitrogen levels (> 40 mg/dL)
- Increased vitreous sodium (> 155 mEq/L) and chloride levels (> 135 mEq/L)
- Normal postmortem serum and vitreous creatinine levels
- Pituitary, adrenal cortical and a few other hormone concentrations will reflect antemortem levels
- Epinephrine and insulin levels are unstable postmortem
- Mast cell granules contain proteases such as tryptase and chymase which are degranulated during anaphylactic reactions
- Hypothermia results in an increase in ketone bodies in the blood and urine
- Alcohol consumption inhibits ketogenesis
- There is an inverse statistically significant relationship between ketone body blood levels and ethanol levels (Connolly: Autopsy Pathology: A Manual and Atlas, 3rd Edition, 2015)
- Serum procalcitonin increases (> 100 ng/ml) in severe systemic bacterial infections
- Acute phase proteins and cytokines can be used in postmortem chemistry similarly to clinical practice
- Serum and urine neopterin is increased in cases of fatal bacterial and viral infections
- Hypoglycemia cannot be reliably tested
- Ratio of insulin to C peptide can be used
- Aminotransferases are not reliable postmortem
- Albumin-globulin ratio is reliable
- Decreased sodium and chloride concentrations
- Increased potassium concentrations (> 20 mEq/L)
- Increased thyroglobulin and T3 concentrations in postmortem serum from heart blood
Dehydration
Endocrine Disorders
Anaphylaxis
Hypothermia
Sepsis
Insulin Overdose
Liver Disease
Decomposition
Incomplete suspension / manual strangulation
- Alcohol misuse: carbohydrate deficient transferrin, ethyl glucuronide, ethyl sulphate
- Anaphylaxis: tryptase, chymase
- Cardiac function: atrial natriuretic peptide, brain natriuretic peptide, myocardial ischemia (troponin I, troponin T, myosin, myoglobin, creatine kinase and creatine kinase MB)
- Electrolytes: sodium, chloride, calcium, magnesium, strontium
- Glucose metabolism: glucose, glycated hemoglobin, ketone bodies, insulin, peptide C
- Liver function: total cholesterol, total bilirubin, total protein
- Renal function: urea nitrogen, creatinine, uric acid
- Sepsis/Inflammation/Infection: procalcitonin, acute phase proteins and cytokines, neopterin
- Hormones: adrenocorticotropic hormone; thyroid stimulating hormone / thyroglobulin / thyroid hormones; catecholamines; cortisol; chorionic gonadotropin; erythropoietin ; chromogranin A; S100B; serotonin, myoglobin
- Postmortem chemistry is a critical ancillary procedure for the forensic pathologist
- The number of analytes currently being evaluated includes many biological fluids in addition to blood
- Consultation with forensic toxicologists is essential to determine the cause and manner of death in questionable cases
- Biochemical analytes provide useful information in deaths when autopsy findings are nonspecific or no apparent causes of death are identified
- Circumstantial data and medical history can give information on whether vitreous chemistry analysis is required or not
- Vitreous glucose is the most reliable marker of antemortem hyperglycemia
- Vitreous potassium concentration more than 15 mmol/L suggests postmortem decomposition and the other analytes should be considered with caution
- Acetone, isopropyl alcohol and β hydroxybutyrate are useful markers of ketoacidosis
- β hydroxybutyrate is a suggested marker of hypothermia
- Serum tryptase and immunoglobulin E are useful markers of anaphylaxis
- Vitreous humor
- Collected by direct gentle needle aspiration from each eye, using a syringe inserted in the outer corner until the tip is placed centrally in the globe (Arch Med Sadowej Kryminol 2017;67:201)
- Less subject to putrefaction than blood, not subject to diffusion of microbes and xenobiotics from the central body cavities (Forensic Sci Int 2009;192:78)
- Recommended quantity: all available (2 - 5 mL in adults, 1 mL in newborns)
- Generally collected in a red top tube with no preservatives
- Quick rise of the vitreous potassium after death prevents determination of antemortem potassium status
- Vitreous potassium concentration more than 15 mmol/L suggests postmortem decomposition
- Remaining analytes should be considered with caution
- Blood
- Cardiac blood is useful for qualitative / screening analyses
- Generally collected from the right chambers of the heart
- Collected in a gray top tube (preservative: sodium fluoride)
- Recommended quantities: heart blood 25 mL
- Peripheral blood is the matrix of choice for quantitative analysis
- Generally collected from the inferior vena cava or femoral vein (Toxicol Rev 2005;24:63)
- Collected in a gray top tube (preservative: sodium fluoride)
- Recommended quantities: peripheral blood 10 mL from a ligated femoral vein / up to 50 mL if part of the blood is drawn from the inferior vena cava
- Cardiac blood is useful for qualitative / screening analyses
- Urine
- Used for qualitative screening
- Gives information on recent drug use but not on acute toxicity (Ther Drug Monit 2002;24:199)
- Collected by a needle aspiration from lower abdominal wall above the pubic symphysis or by urethral catheterization (if external examination only) or directly from the bladder (if internal examination)
- Collected in a plastic tube with no preservatives
- Recommended quantity: all available up to 50 mL
- Used for qualitative screening
- Tissues
- Mostly liver for biochemical purposes
- Skeletal muscle can be collected in case of advanced decomposition
- Spleen can be used for carbon monoxide analysis when blood is unavailable
- Collected in a container with no preservatives
- Recommended quantity: 30 - 50 g
- Hair
- Information on chronic exposure to drugs (Forensic Sci Int 1993;63:19)
- Obtained by pulling to include hair roots
- Tied tightly together with ligature to maintain orientation
- Axillary, pubic, arms or beard hair if head hair unavailable or unsuitable
- Recommended quantity: 50 g
- Cerebrospinal fluid
- Qualitative analysis
- Can be used for postmortem microbiology analysis (J Family Med Prim Care 2023;12:1893)
- Collected through percutaneous suboccipital / lumbar puncture before the internal examination
- Alternatively aspirated from the posterior fossa / lateral ventricles after the brain's removal
- Recommended quantity: all available up to 10 mL
- Collected in a plain universal tube / container with no preservatives
- Bile (Acad Forensic Pathol 2018;8:324)
- For qualitative screening and to determine what drugs an individual used or was exposed to prior to death
- Collected by aspiration from gallbladder or directly from common bile duct if cholecystectomy was performed
- Always obtained before eviscerating the liver to avoid contamination
- Recommended quantity: all available up to 10 mL
- Synovial fluid (Am J Forensic Med Pathol 2014;35:154)
- Collected from each uninjured joint cavity by lateral puncture of the bursa sac under the patella
- Recommended quantity: all available (1 - 2 mL by each knee joint)
- Substitute for vitreous humor, if not available
- Pericardial fluid
- Collected through a syringe (no needle) from the pericardial cavity
- Recommended quantity: all available (5 - 20 mL)
- Reference: Forensic Sci Res 2017;1:42
- Disorders of glucose metabolism
- Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are acute metabolic complications of diabetes mellitus
- Distinguish between diabetic and alcoholic ketoacidosis can be challenging
- Most useful biochemical analytes (Croat Med J 2015;56:181)
- Vitreous glucose: most reliable indicator of antemortem hyperglycemia (DKA, HHS)
- Blood glycated hemoglobin HbA1c: marker of long term (8 - 12 weeks) antemortem blood glucose control (DKA, HHS)
- Blood / vitreous / pericardial fluid β hydroxybutyrate (3HB) and acetone: 3HB is a better postmortem indicator of ketoacidosis (pathologically significant levels > 2500 μmol/L); elevated acetone levels indicate the need for 3HB measurement (Alcohol Alcohol 2014;49:271)
- Serum / vitreous / pericardial fluid urea nitrogen, creatinine, urate; vitreous sodium and chloride: increased urea nitrogen, urate, sodium and chloride with normal creatinine indicate volume depletion (DKA, HHS)
- Vitreous lactate: increased levels possibly due to underlying complications such as sepsis, pneumonia related hypoxia, severe hepatic disorders (J Forensic Sci 2004;49:371)
- Blood / vitreous carbohydrate deficient transferrin (CDT): marker of chronic heavy ethanol consumption
- Blood prealbumin and albumin: estimation of undernourishment
- Other analytes
- Urine glucose: use as a confirmatory test only after analysis of the other markers of hyperglycemia (DKA, HHS)
- Blood / vitreous isopropyl alcohol: unspecific marker of ketoacidosis (DKA, AKA, ALA)
- Blood / vitreous fructosamine: marker of 1 - 3 weeks glycemic control but large deviation from living subjects (DKA, HHS) (Int J Legal Med 1999;112:275)
- Vitreous ethyl glucuronide and ethyl sulphate: rarely used to distinguish ethanol ingestion from postmortem formation
- C reactive protein and proinflammatory cytokines: increased levels even without signs of underlying infections (DKA, AKA)
- Dehydration
- Vitreous sodium, chloride, urea and creatinine are usually increased in cases of hypernatremic dehydration
- Vitreous sodium and chloride are decreased in hyponatremic dehydration
- Vitreous urea and creatinine are increased when the dehydration is isonatremic
- Reference values should be considered with care because they are very narrow
- Postmortem diagnosis should rely on toxicological results and autopsy findings (sunken eyes, tinting of skin, poor skin turgor) (Forensic Sci Int 2005;155:1)
- Insulin toxicity related deaths
- Challenging to prove
- Reported among both diabetic and nondiabetic individuals
- Scene investigation and a comprehensive medical record review are essential to suspect and determine the contributory role of insulin to death (Acad Forensic Pathol 2016;6:174)
- Most useful biochemical analytes (Acad Forensic Pathol 2016;6:174)
- Serum insulin: measured on peripheral blood
- Serum C peptide: connecting peptide of A and B chains of proinsulin; suppressed levels with elevated insulin levels in exogenous insulin administration
- Freezing the samples as soon as possible is required to avoid the rapid degradation of insulin at room temperature
- Long hypoglycemic coma allows for metabolism and elimination of the insulin before dearth
- Immunohistochemical detection of insulin at the injection site may be helpful
- Anaphylaxis
- Acute immunologic multiorgan (cutaneous, gastrointestinal, respiratory, cardiovascular) response following the exposure to an antigen
- Common stimuli include insects, food, medications and radiocontrast media
- Frequent lack of autopsy findings of airway obstruction (laryngeal / epiglottic edema, mucus plugging in the bronchi) due to rapidly developing shock (Forensic Sci Med Pathol 2017;13:269)
- Biochemical testing should be based on circumstances of the death and the individual's medical history
- Most useful biochemical analytes
- Serum β tryptase: neutral protease released following mast cells IgE induced degranulation; sampling from femoral vein to avoid confounding effect of resuscitation induced tryptase release from the heart (Forensic Sci Int 2020;314:110415)
- Serum immunoglobulin E (IgE) levels: markers of atopic disposition (total IgE) and prior sensitization (specific IgE; only if the offending antigen is known / suspected)
- Other analytes
- Chymase: mast cells derived neutral protease; positive correlation with tryptase levels
- Histamine: amine stored in the secretory granules of mast cells; too rapid degradation, unreliable postmortem marker
- Hypothermia
- Core body temperature at / below 35 degrees C
- No pathognomonic signs at autopsy (diagnosis of exclusion)
- Most useful analytes
- Blood / vitreous / pericardial fluid / urine / cerebrospinal fluid β hydroxybutyrate (3HB) and acetone: there is an inverse statistically significant relationship between ketone body levels in various fluids and ethanol blood levels (Int J Legal Med 2014;128:607)
- Blood / vitreous / pericardial fluid / urine / cerebrospinal fluid isopropyl alcohol: nonpecific marker of ketoacidosis
- Serum / urine cortisol, urine catecholamines: increased levels may support the diagnosis but normal levels do not exclude it (Clin Chem Lab Med 2018;56:1819)
- Ethanol is the most commonly detected drug and can accelerate body cooling, preventing morphologic and biochemical changes from occurring
- Drowning
- Death caused by submersion in a liquid
- No pathognomonic autopsy findings (diagnosis of exclusion)
- Circumstances of the event are critical to determine cause and manner of death
- Suggested analytes
- Vitreous sodium and serum chloride: hemodilution (low sodium) with left heart blood chloride right heart blood chloride in salt water drowning
- Serum and pericardial fluid calcium and magnesium: increased levels in both peripheral and central blood reported in saltwater drowning
- Serum strontium: increased levels in central blood from left ventricle reported in saltwater and freshwater drownings (Forensic Sci Int 2012;214:159)
- Sepsis
- Systemic inflammatory response syndrome triggered by an infection, leading to acute organ dysfunction (severe sepsis) and perfusion abnormalities due to either refractory hypotension or hyperlactatemia (septic shock)
- Nonspecific and often controversial autopsy findings
- Most useful analytes (Croat Med J 2014;55:103)
- Serum procalcitonin (PCT): long half life (25 - 30 hours); very stable even at room temperature; increased levels in severe systemic bacterial, parasitic or fungal infections (Forensic Sci Int 2007;165:155)
- Serum / liver C reactive protein and serum proinflammatory cytokines: increased levels in acute phase response to inflammatory tissue injury
- Other analytes
- Serum interleukin-2 receptor (sIL-2R): marker of lymphocyte activation
- Serum lipopolysaccharide binding protein: opsonin
- Serum / urine neopterin: produced upon IFNγ stimulation; elevated concentrations in viral, bacterial, protozoic, parasitic or fungal systemic infections
- Renal function
- Serum / vitreous / pericardial fluid urea nitrogen, urate and creatinine, vitreous sodium and chloride are reliable markers
- Useful in cases of neglect (increased urea nitrogen, urate, sodium and chloride with normal creatinine), salt poisoning (rapid onset of hypernatremia and hyperchloremia) and water intoxication (marked hyponatremia and hypochloremia) (J Clin Pathol 2003;56:803)
- Liver function
- Total cholesterol, low serum proteins with inversion of albumin:globulin ratio, high serum bilirubin, abnormal levels of bile and urobilinogen are reliable indicators of advanced liver disease (J Forensic Leg Med 2008;15:312)
- Cardiac function
- Atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP): increased levels in pericardial fluid reported in chronic congestive heart disease cases (Int J Legal Med 2007;121:28)
- Troponin I (cTnI), troponin T (cTnT) and creatin kinase (CKMB): in cases of myocardial ischemia, cTnI and cTnT increase depends on the severity of myocardial damage at the time of death
- Hormones
- ACTH (adrenocorticotropic hormone), TSH (thyroid stimulating hormone): low levels in cerebrospinal fluid observed in cases of prolonged hypothermia (Forensic Sci Int 2008;179:147, Am J Forensic Med Pathol 2001;22:78)
- Chromogranin A: low serum and high cerebrospinal fluid levels described in cases of fatal hypothermia (Int J Legal Med 2011;125:11)
- TG (thyroglobulin), T3 (triiodothyronine): increased central blood levels reported in cases of incomplete suspension and manual strangulation (Forensic Sci Int 1997;90:165)
- HCG (chorionic gonadotropin): positive in pregnant women (serum, vitreous, bile) and postmortem levels corresponding to antemortem levels in deaths by choriocarcinoma or related tumors (J Forensic Sci 2010;55:792)
- EPO (erythropoietin): survival time dependent postmortem serum elevation within 6 hours in deaths due to acute massive hemorrhage (Int J Legal Med 2008;122:481)
- 5-HT (serotonin): some authors observed elevated levels in deaths due to sedative / hypnotic drug intoxication and hyperthermia (Forensic Sci Int 2004;142:211)
- Miscellanea
- S100B: marker of astrocyte injury in cases of hypoxic cerebral damage due to mechanical asphyxia (Leg Med (Tokyo) 2006;8:71)
- Myoglobin: elevated levels reported in cases of massive skeletal muscle damage (heat stroke, fatal burns, convulsive disorders, muscle hyperactivity) (Forensic Sci Int 2001;115:183)
- Sudden unexpected death in infancy and childhood: skin sample for fibroblast culture and biochemical analysis on urine (if present), blood and bile spots on Guthrie card for inherited metabolic disorders; muscle biopsy if history is suggestive of mitochondrial disorder (Leg Med (Tokyo) 2009;11:S36)
- Postmortem interval estimation: numerous analytes have been proposed but none are currently validated
- 31 year old man with a history of type 1 diabetes mellitus and diabetic ketoacidosis (J Forensic Leg Med 2019;63:34)
- 38 year old man and two 58 year old men with anaphylaxis due to bee stings (Forensic Sci Med Pathol 2016;12:81)
- 54 year old man with psychiatric history and fatal water intoxication (Int J Legal Med 2018;132:173)
- Inferior vena cava blood
- β hydroxybutyric acid: > 1200 mcg/mL
- Ethanol: 78 mg/dL
- Isopropanol: 6.6 mg/dL
- Acetone: 42 mg/dL
- Caffeine: presump pos
- Vitreous
- Creatinine: 0.875 mg/dL
- Sodium: 143 mmol/L
- Potassium: 14.3 mmol/L
- Chloride: 118 mmol/L
- Glucose: 327 mg/dL
- Urea nitrogen: 27 mg/dL
The cause of death and manner of death are best certified as which of the following?
- Alcoholic ketoacidosis - natural
- Chronic alcoholism- natural
- Diabetic ketoacidosis - natural
- Ethanol toxicity - accident
- Multifactorial ketoacidosis - natural
Answer D is incorrect because the concentration of alcohol in peripheral blood is not enough to cause acute toxicity, even if there is a history of recent consumption of large quantities of ethanol. Answers A and C are incorrect because there is no reliable way to distinguish between alcoholic and diabetic ketoacidosis since both conditions can lead to it. Answer B is incorrect because even if there is liver steatosis, suggesting chronic ethanol use, the high levels of ketones are consistent with ketoacidosis.
Comment Here
Reference: Vitreous analysis (postmortem chemistry)
- Liver tissue is the best specimen for quantitative analyses
- The absence or presence of glucose in vitreous fluid is of no significance
- The color of the vitreous fluid is suspicious for trauma to the eye; a more detailed inspection is required
- The potassium concentration in vitreous fluid
- The sodium concentration in vitreous fluid
Answer B is incorrect because glucose concentration is a useful marker of diabetes or a hyperglycemic state. Answer A is incorrect because the best and most reliable postmortem specimen for quantitative analysis is peripheral blood. Answer C is incorrect because while in a fresh body, a red tinged vitreous fluid may suggest local trauma or sampling artifact; in a decomposed body, a darker color in the absence of clear evidence of injury should be considered a postmortem artifact. Answer E is incorrect because the sodium concentration in vitreous fluid is a useful marker of dehydration; however, its concentration should be considered after determining the potassium concentration.
Comment Here
Reference: Vitreous analysis (postmortem chemistry)
Find related Pathology books: forensic, autopsy, pediatric