Table of Contents
Definition / general | Essential features | Epidemiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Aqil B. Lymphoid aggregates (benign). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonemarrowlymphoidaggregates.html. Accessed May 11th, 2024.
Definition / general
- Benign lymphoid aggregates are composed predominantly of small lymphocytes
- Some benign lymphoid aggregates may have germinal centers made up of centrocytes and centroblasts
Essential features
- Presence of lymphoid aggregates in the bone marrow biopsy should be evaluated to exclude lymphoproliferative disorders / lymphoma
- Morphology is of paramount importance for the decision to perform ancillary tests
- Small size (< 600 μm), nonparatrabecular location, confined borders, paucity of B cells are usually supportive of benign lymphoid aggregates
- Ancillary modalities such as flow cytometry and molecular studies have their diagnostic limitations and should be taken into consideration when making a diagnosis
Epidemiology
- Benign lymphoid aggregates seen in only 1 - 2% of bone marrow biopsy specimens
- More frequently seen in autopsy specimens
Etiology
- Benign lymphoid aggregates are seen in association with the following (J Clin Pathol 1999;52:294, Virchows Arch A Pathol Anat Histopathol 1991;419:261, Leuk Res 2002;26:525, Am J Clin Pathol 1999;112:844, Eur Respir J 2009;34:405, Blood 2011;117:6438, Mod Pathol 2015;28:367, J Clin Pathol 1993;46:955, Br J Haematol 2016;172:923, Haematologica 2017;102:364)
| Advanced age | |
| Tobacco use | |
| Autoimmune diseases | Rheumatoid arthritis, systemic lupus erythematosus |
| Autoimmune lymphoproliferative syndrome with germline FAS mutation | |
| Inflammatory conditions | |
| Infectious diseases | HIV, hepatitis C virus, hepatitis B virus, mycobacteria, fungal or bacterial and cytomegalovirus infections |
| Myeloproliferative neoplasms | Polycythemia vera, primary myelofibrosis, systemic mastocytosis |
| Myelodysplastic syndromes | |
POEMS syndromes
TEMPI syndromes
| |
| Rituximab and chimeric antigen receptor T cells (CAR T) treatment | |
| Idiopathic hypereosinophilic syndrome |
Clinical features
- Usually, no prior history of lymphoproliferative disorder; however, even if there is a history, that does not necessarily signify the presence of lymphoid aggregates as malignant
- Mean age of presentation is in the sixth decade (Hum Pathol 2013;44:512)
- Incidence increases with age (Hum Pathol 2013;44:512)
Diagnosis
- Incidental finding on bone marrow examination
Prognostic factors
- In all ages, up to 33% of cases may have subsequent malignant lymphoid aggregates in bone marrow or other evidence of lymphoma or lymphoproliferative disorders (Blood 1974;43:389)
- If initial biopsy showed atypical lymphoid aggregates, then follow up with bone marrow biopsy should be suggested
Treatment
- No treatment for benign lymphoid aggregates
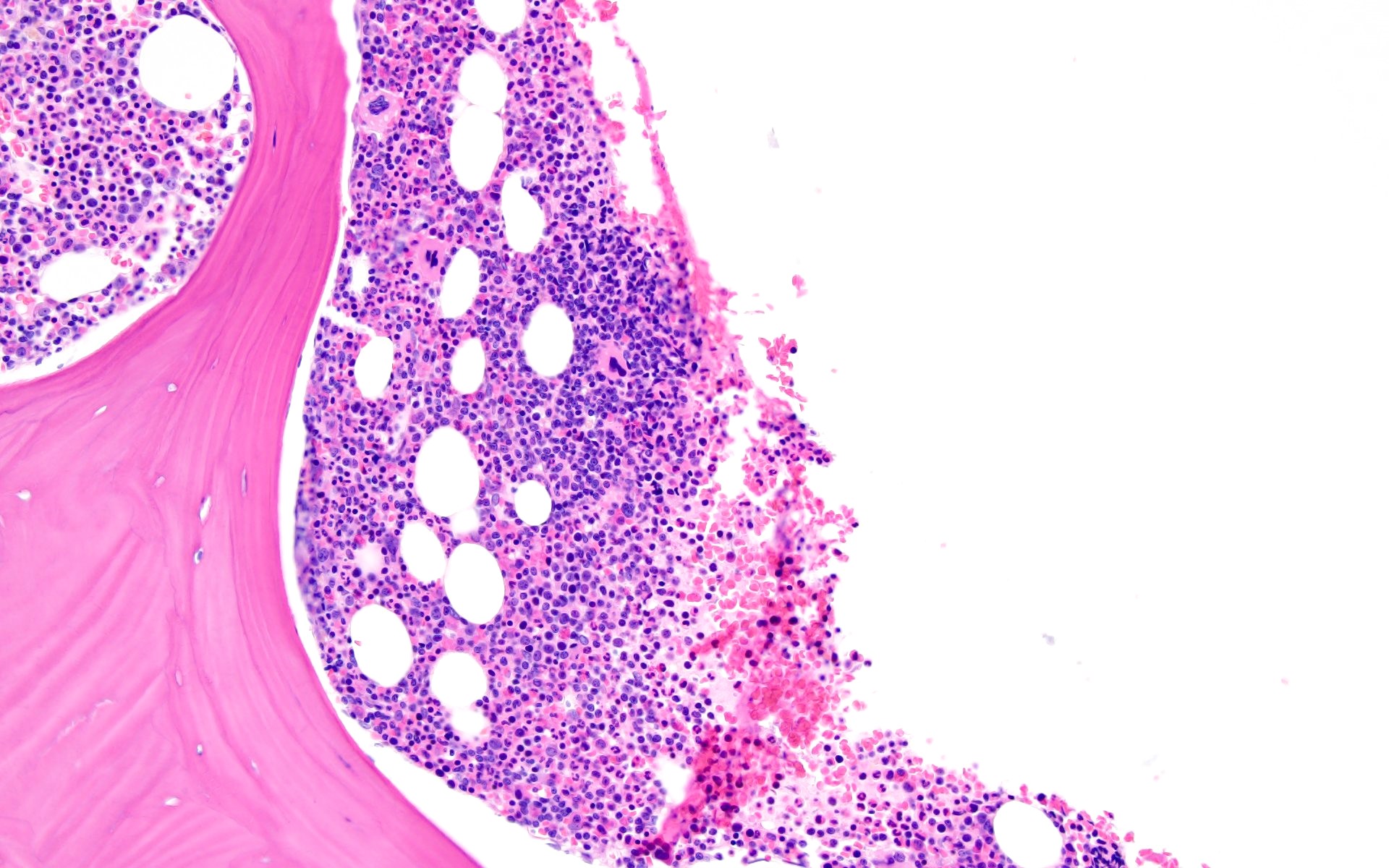
Microscopic (histologic) description
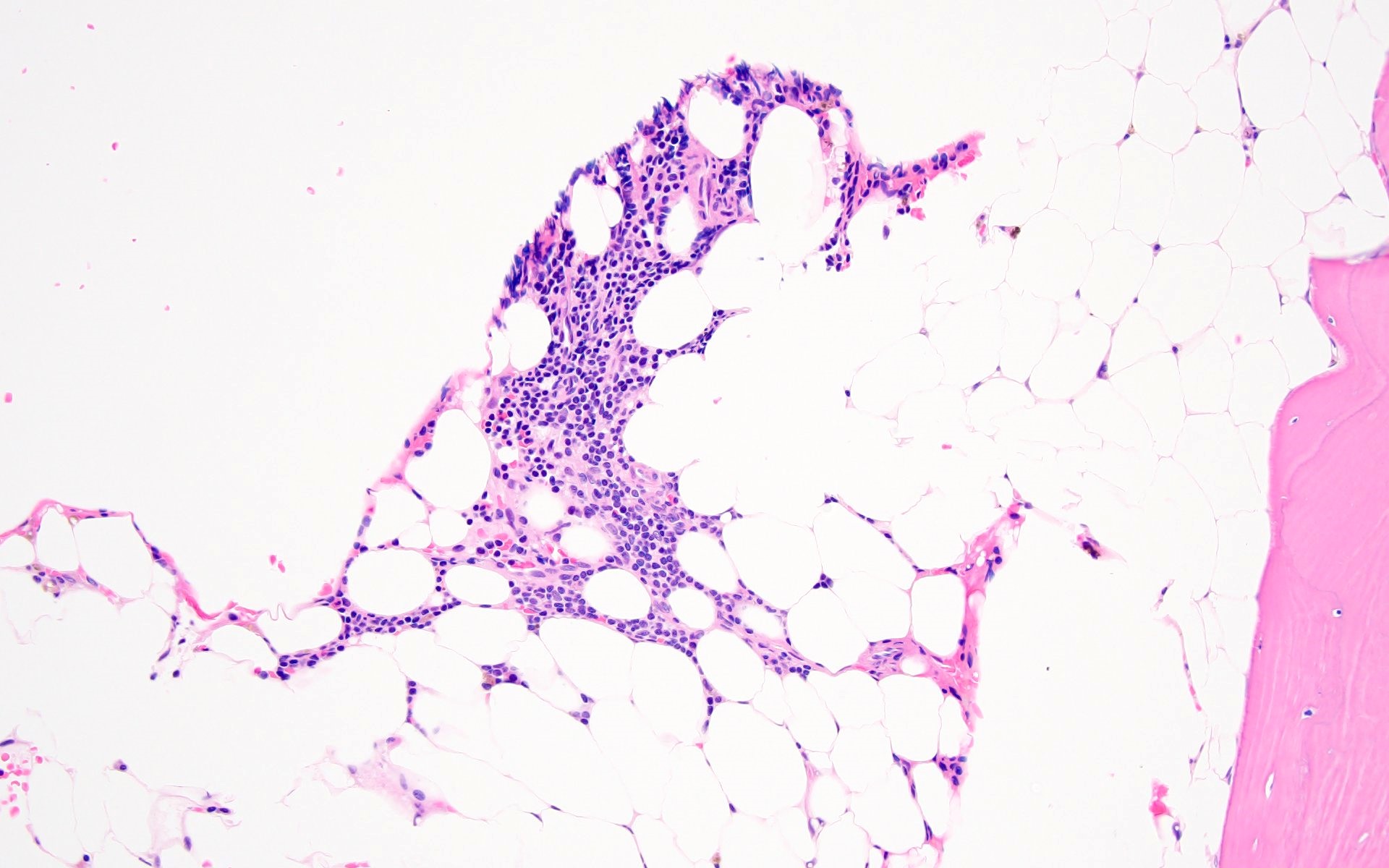
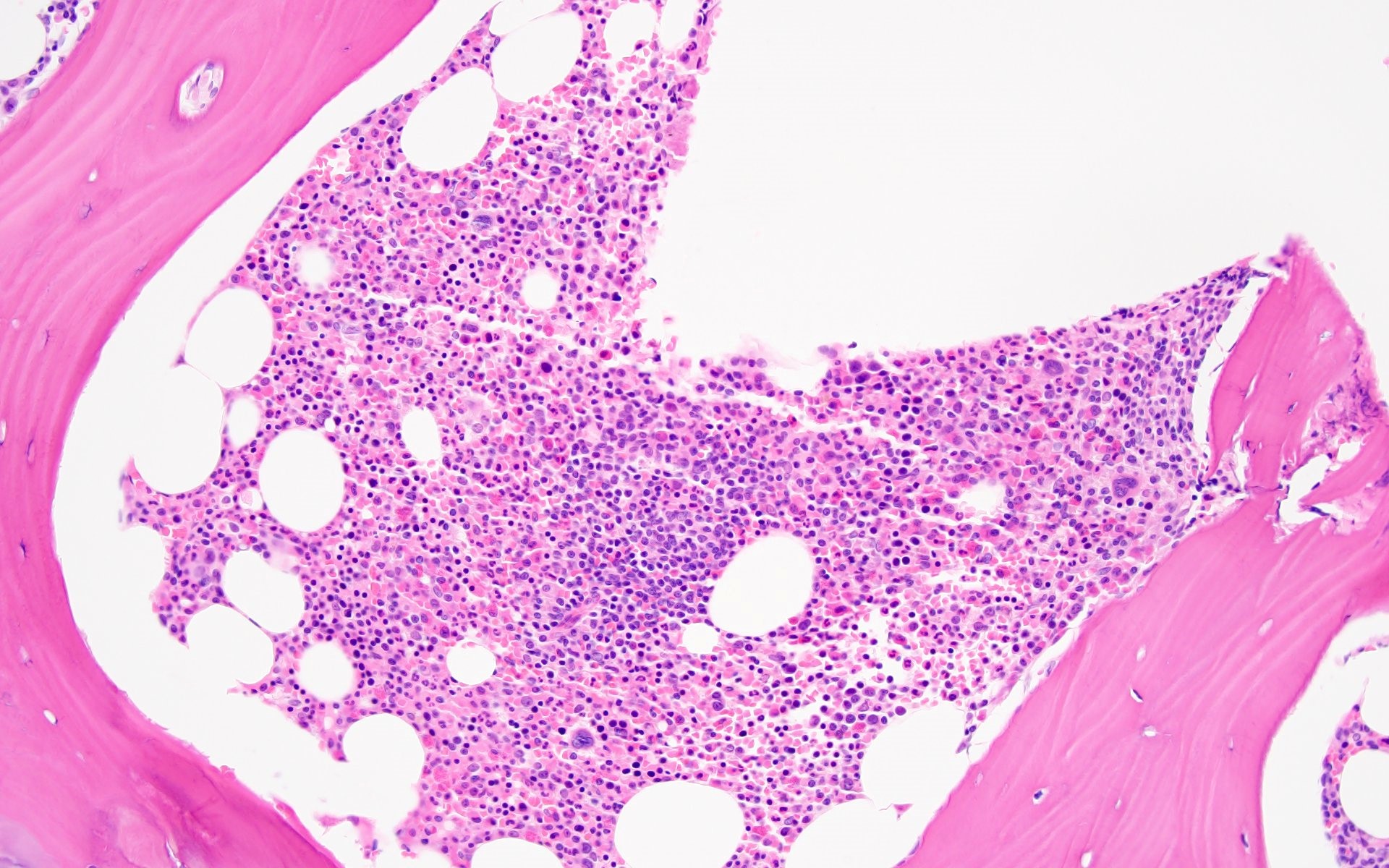
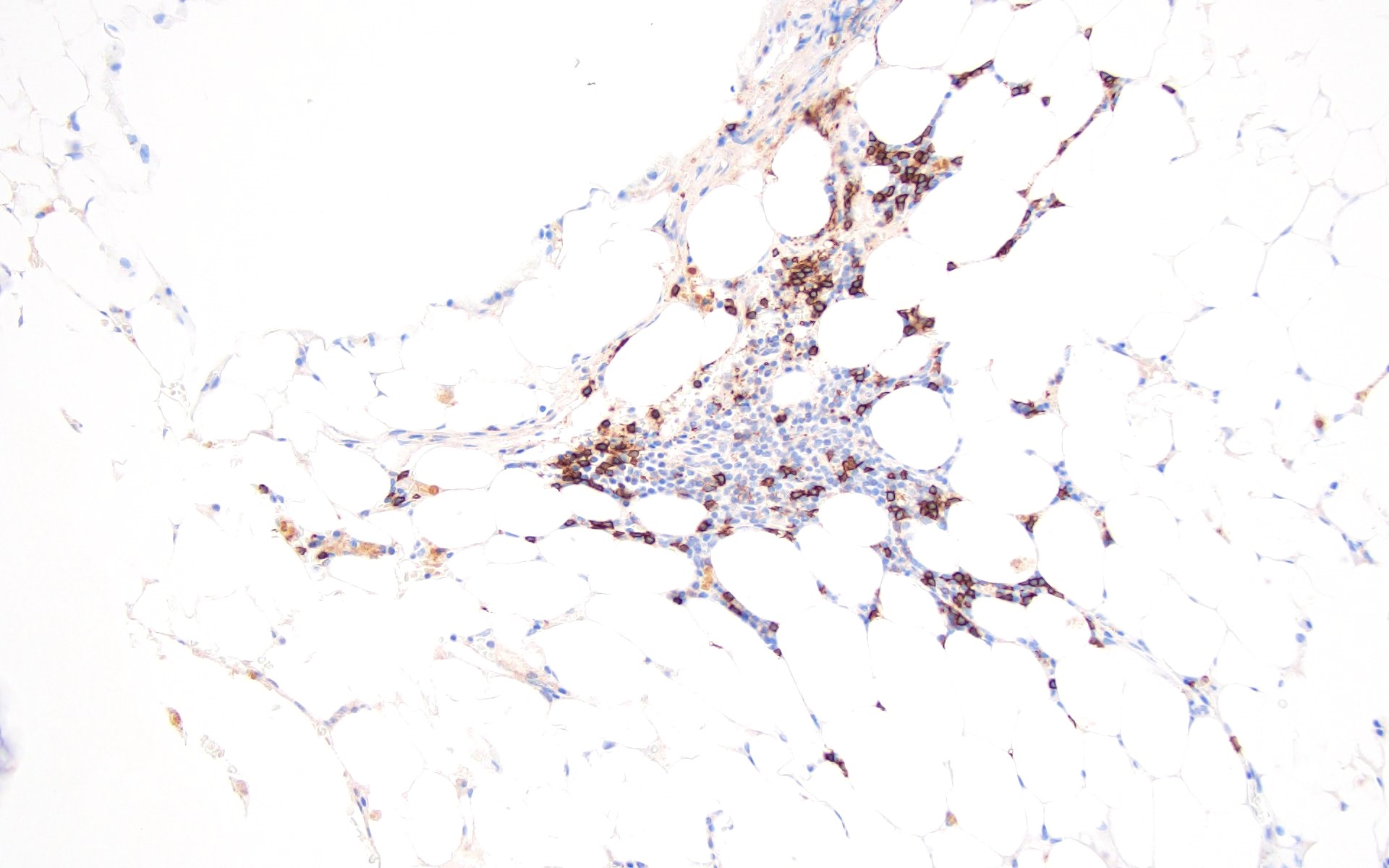
- Lymphoid aggregates are assessed based on the location (intertrabecular / paratrabecular), size and appearance of lymphocyte population
- Characteristics of benign lymphoid aggregates (J Clin Pathol 1999;52:294,
Virchows Arch A Pathol Anat Histopathol 1991;419:261,
J Pathol 1997;181:451,
J Pathol 1996;178:447)
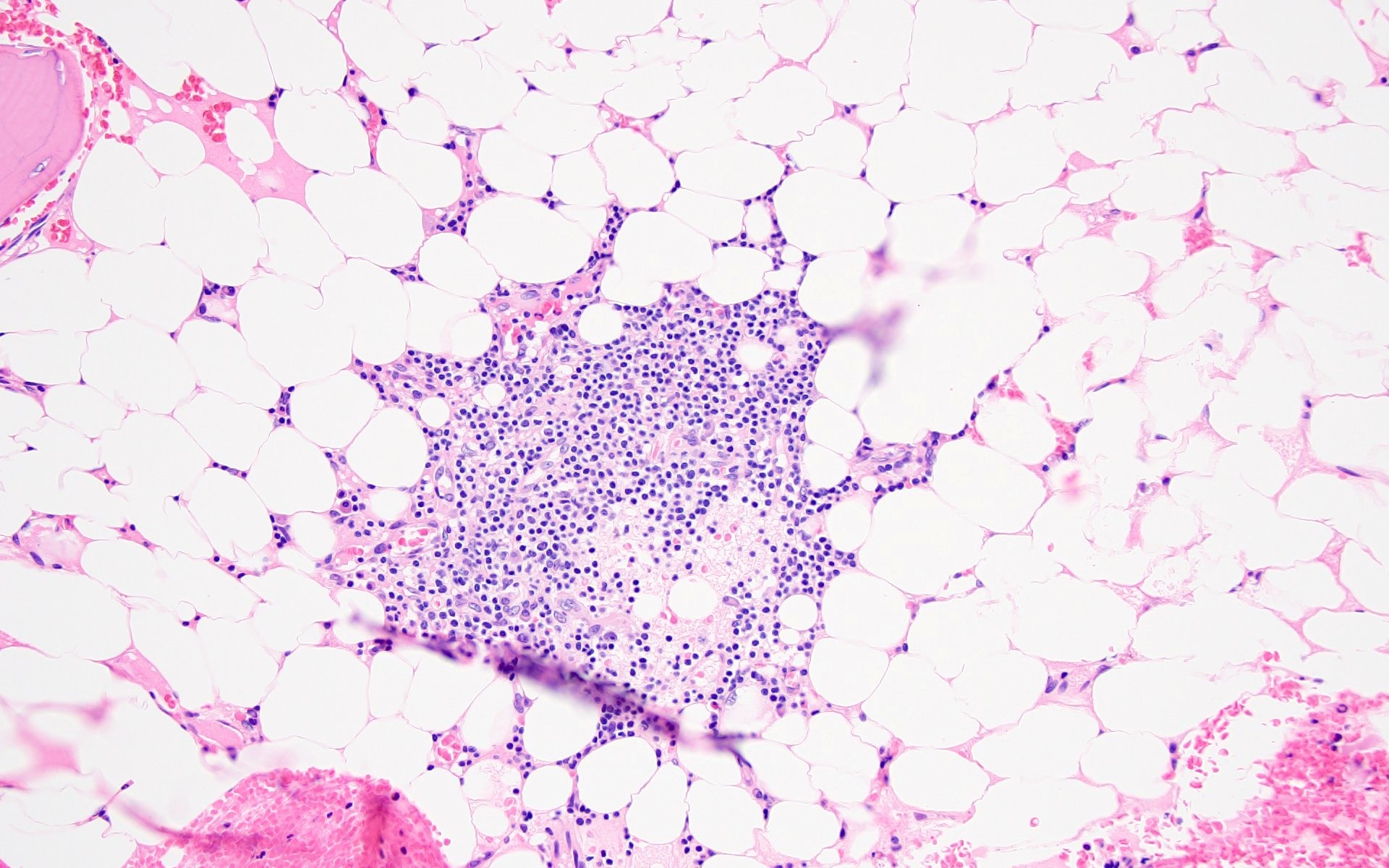
- Small size (< 600 μm)
- Uniform configuration
- Distinct outline
- Nonparatrabecular location
- Becomes smaller or disappears in deeper sections of the specimen
- Lack of cytologic atypia
- Negative for clonality (exception in autoimmune diseases)
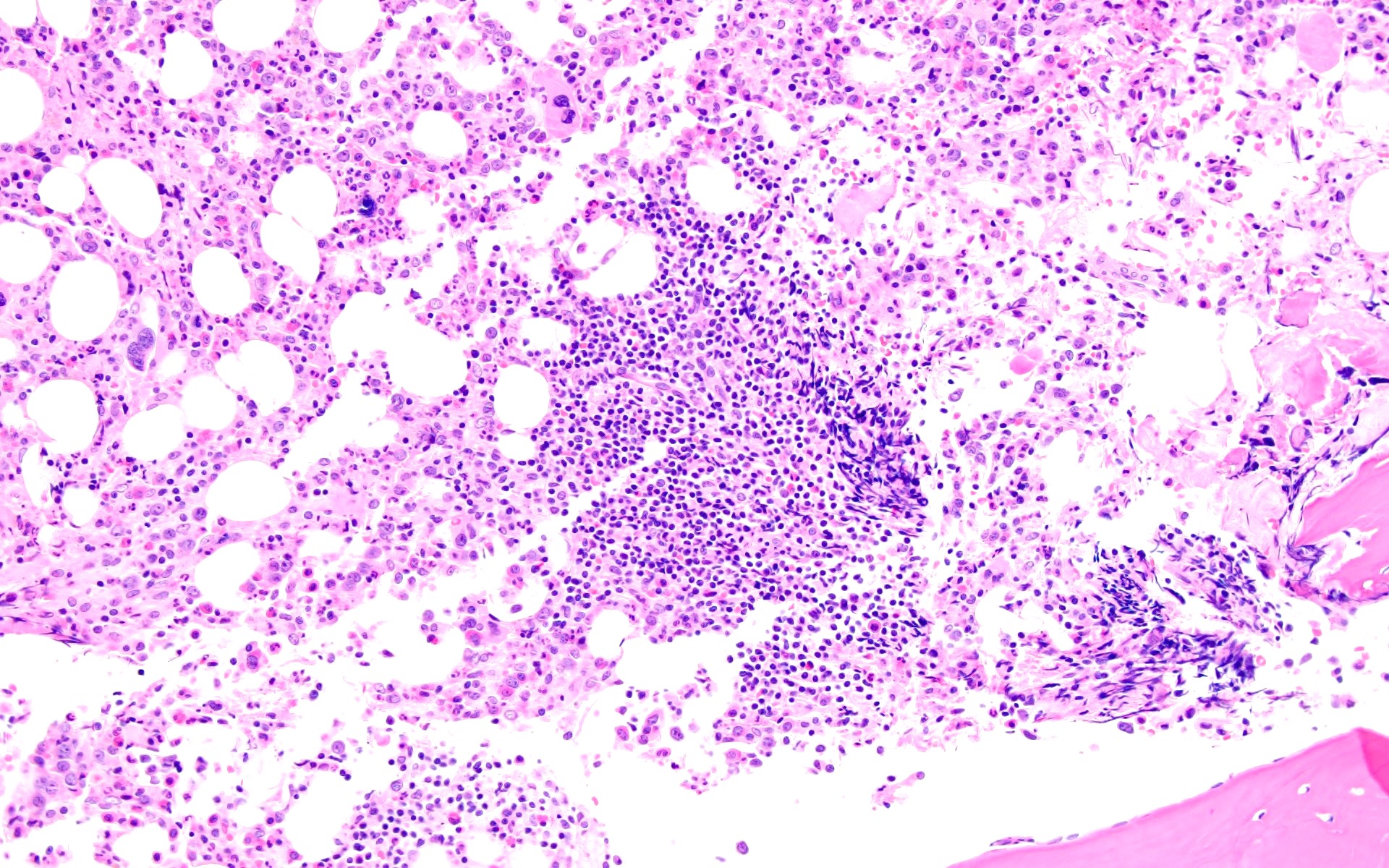
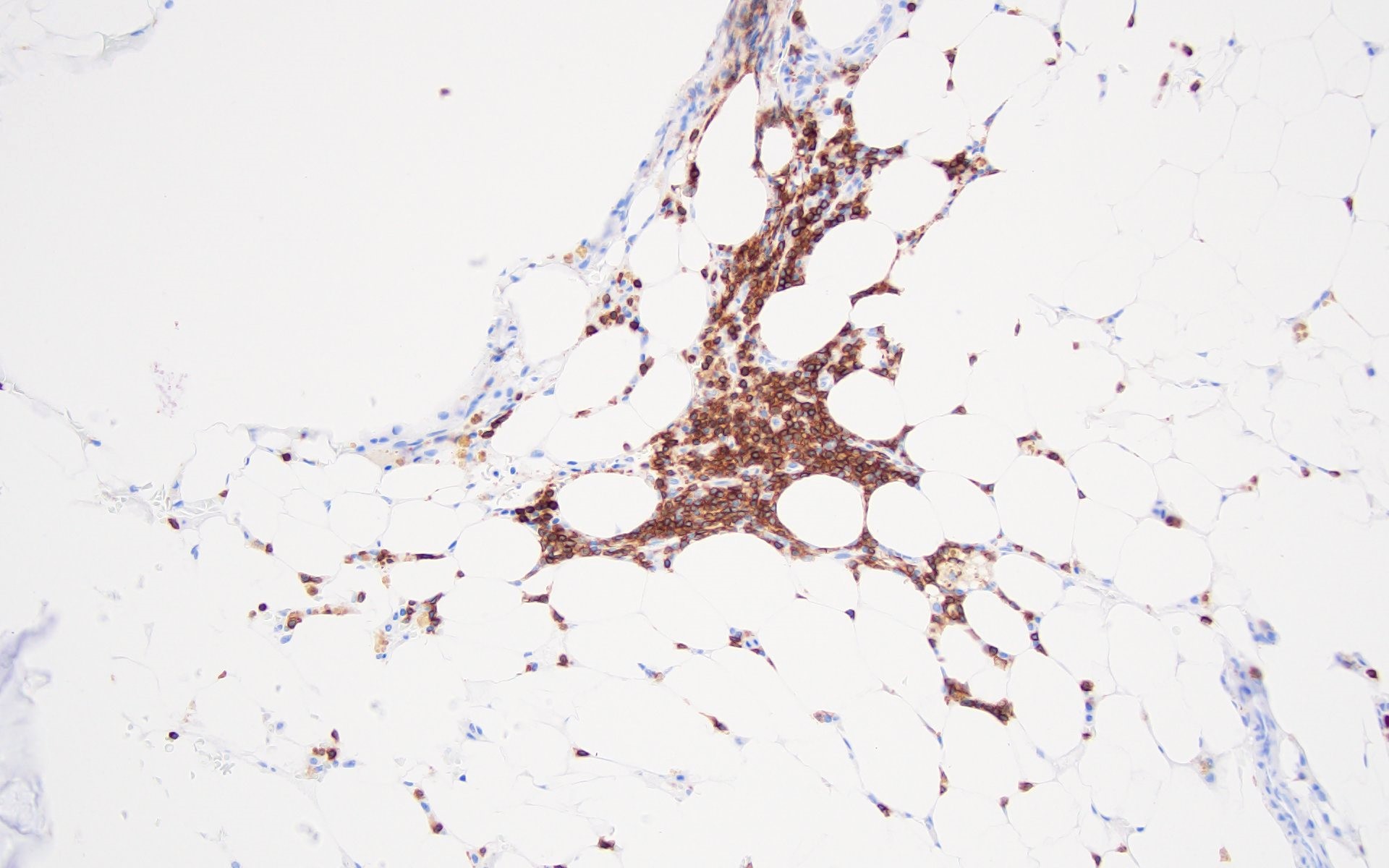
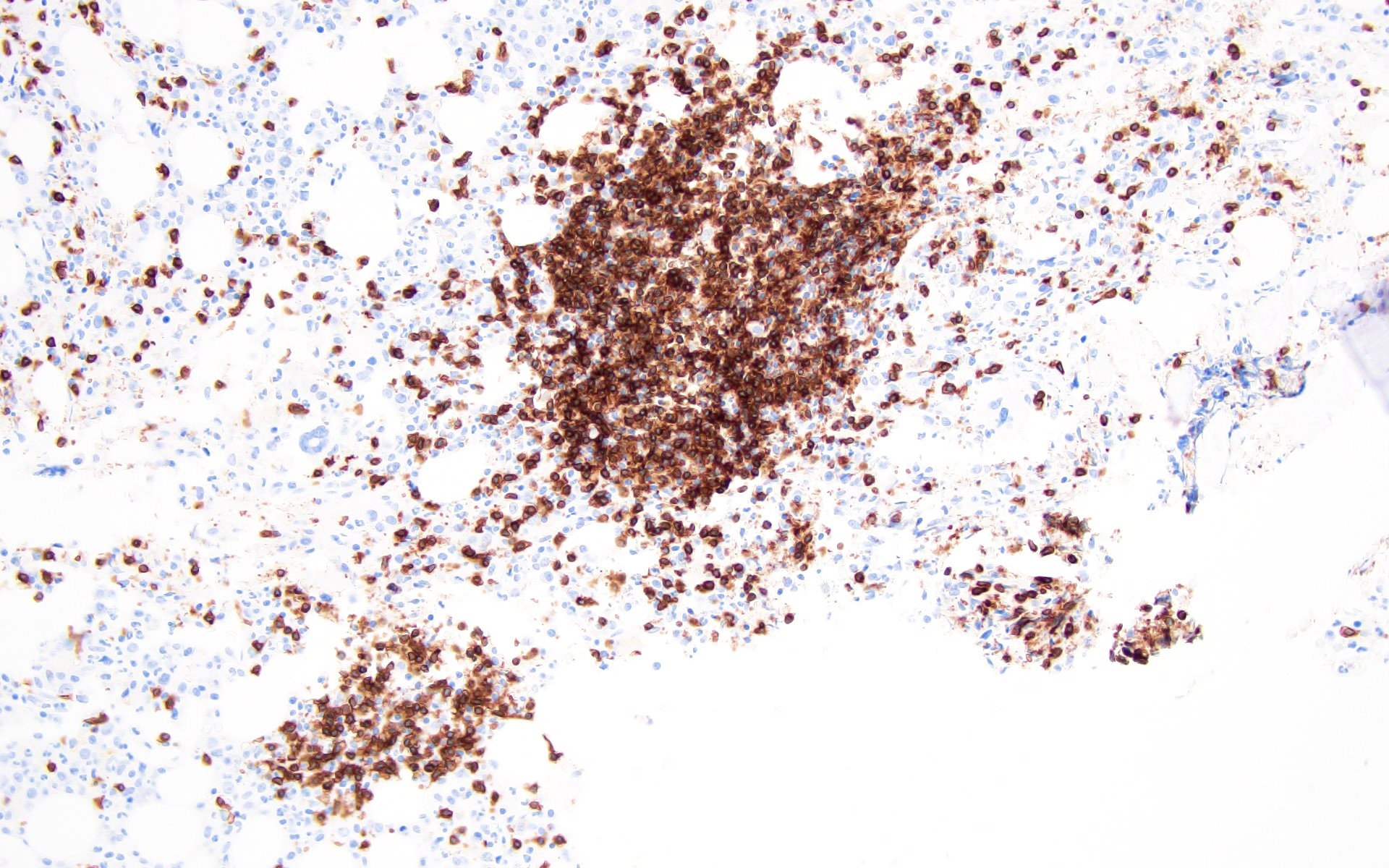
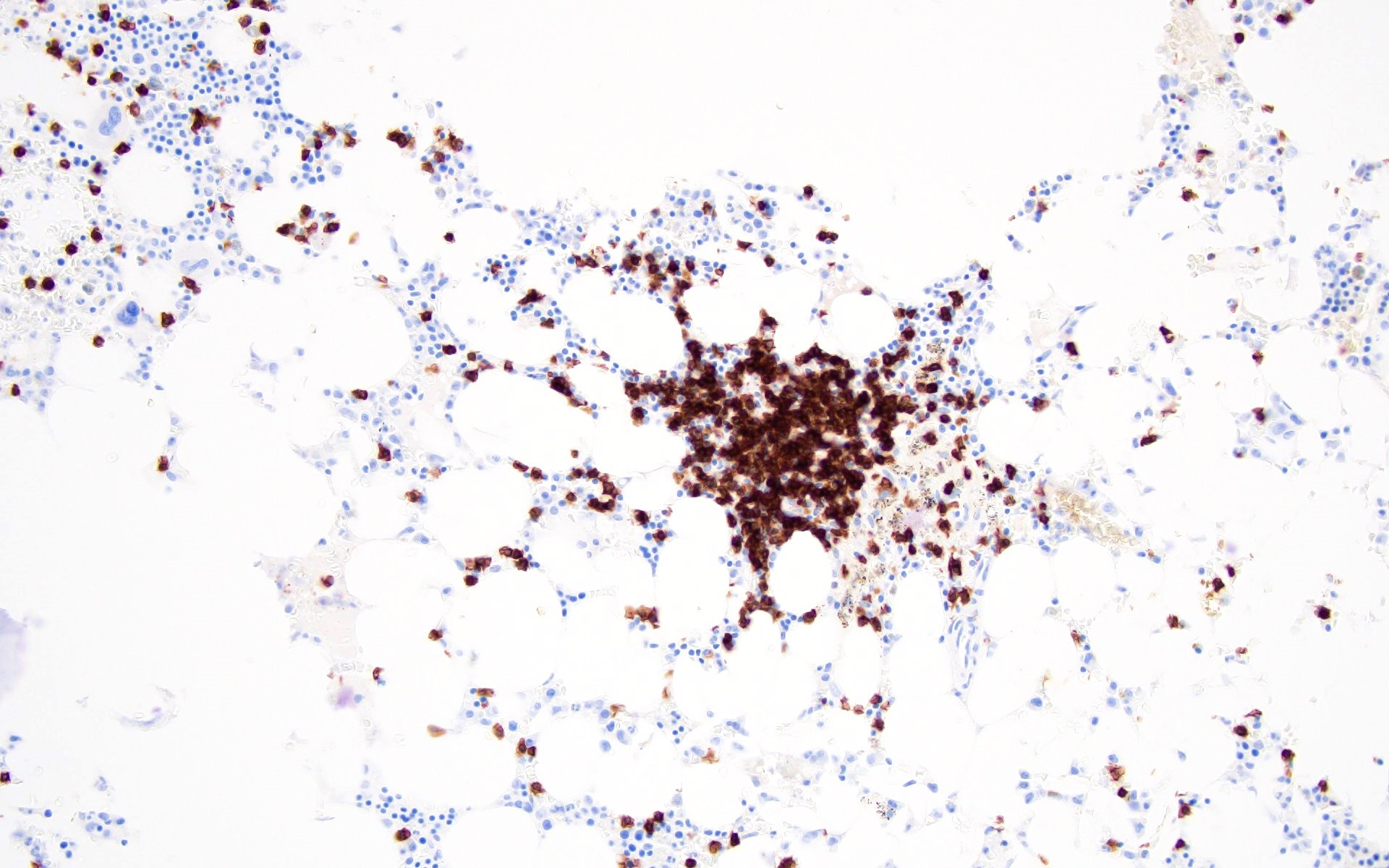
- 5 different patterns are described for the T cell and B cell distribution in the lymphoid aggregates (Hum Pathol 2013;44:512)
Patterns CD3+ T cells / CD20+ B cells 1 Predominantly T cells 2 Mixture of T and B cells, haphazard arrangement 3 T cell core surrounded by few B cells 4 B cell core surrounded by T cells 5 Predominantly composed of B cells
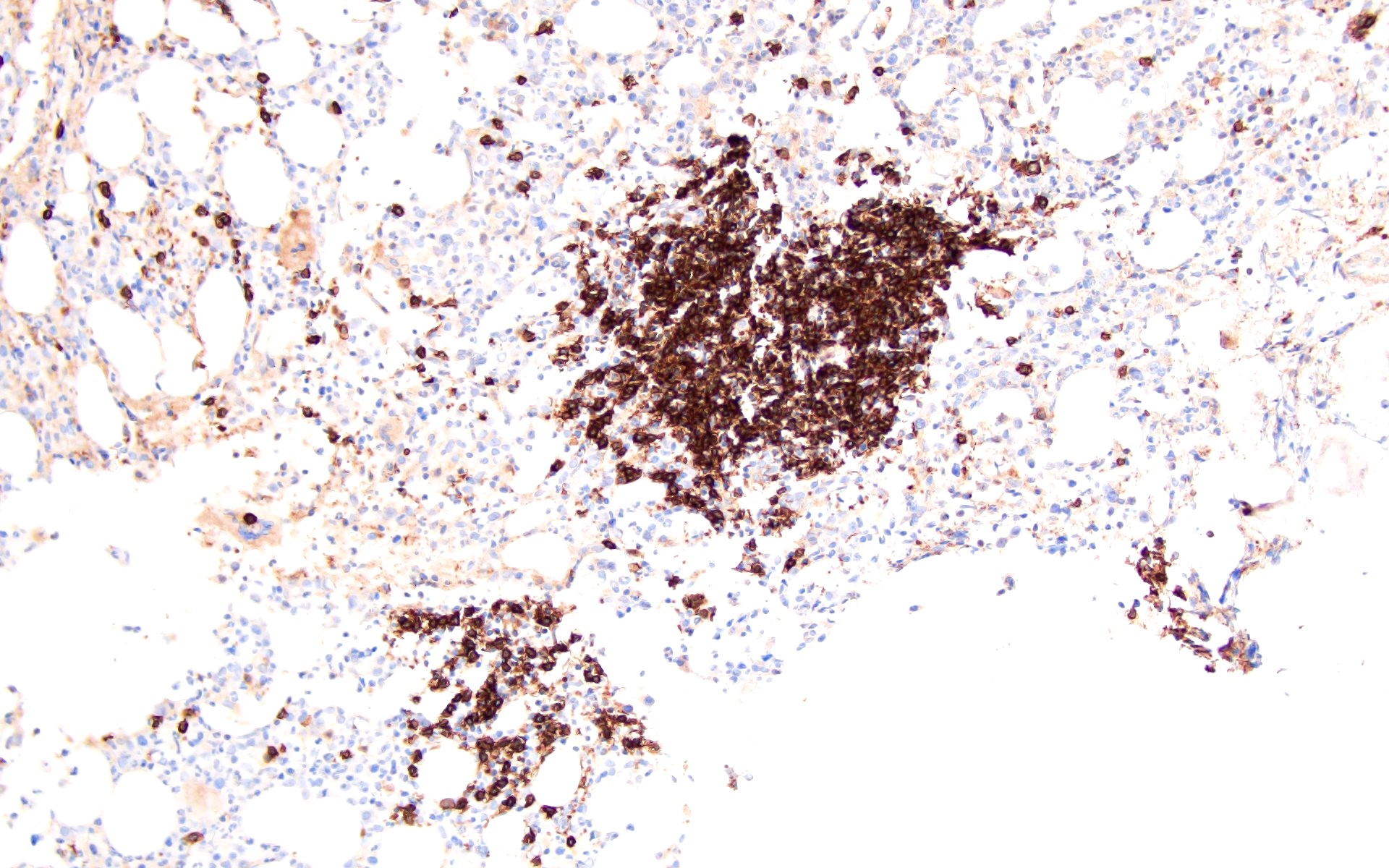
- Benign lymphoid aggregates show predominantly patterns 1 - 3 with rare cases of patterns 4 and 5
- Atypical features described in lymphoid aggregates include large size, infiltrative borders, paratrabecular location and predominance of B cells (patterns 4 and 5)
- Patterns 4 and 5 are seen most commonly in lymphomas, with the exception of reactive lymphoid aggregates with BCL6 positive germinal centers (Virchows Arch A Pathol Anat Histopathol 1987;411:543)
- Some of the benign lymphoid aggregates have characteristic morphologic findings based on the etiology (Pathologica 1995;87:640, Eur Respir J 2009;34:405,
Blood 2011;117:6438,
Mod Pathol 2015;28:367,
J Clin Pathol 1993;46:955,
Haematologica 2017;102:364,
Am J Clin Pathol 1999;112:844)
Etiology Lymphoid aggregate morphologic findings POEMS syndrome Composed of mixture of T and B cells,
surrounded by lambda / kappa light chain
restricted or polytypic plasma cellsIdiopathic hypereosinophilic syndrome T cell rich aggregates HIV Large poorly demarcated lymphoid aggregates with cytologic
atypia and histiocytic proliferationsAutoimmune lymphoproliferative
syndrome with germline FAS mutationT cell rich lymphoid aggregates with CD4- / CD8- T cells Rituximab treatment T cell rich lymphoid aggregates CD19 directed CAR T therapy T cell rich lymphoid aggregates with increased CD8+ T cells
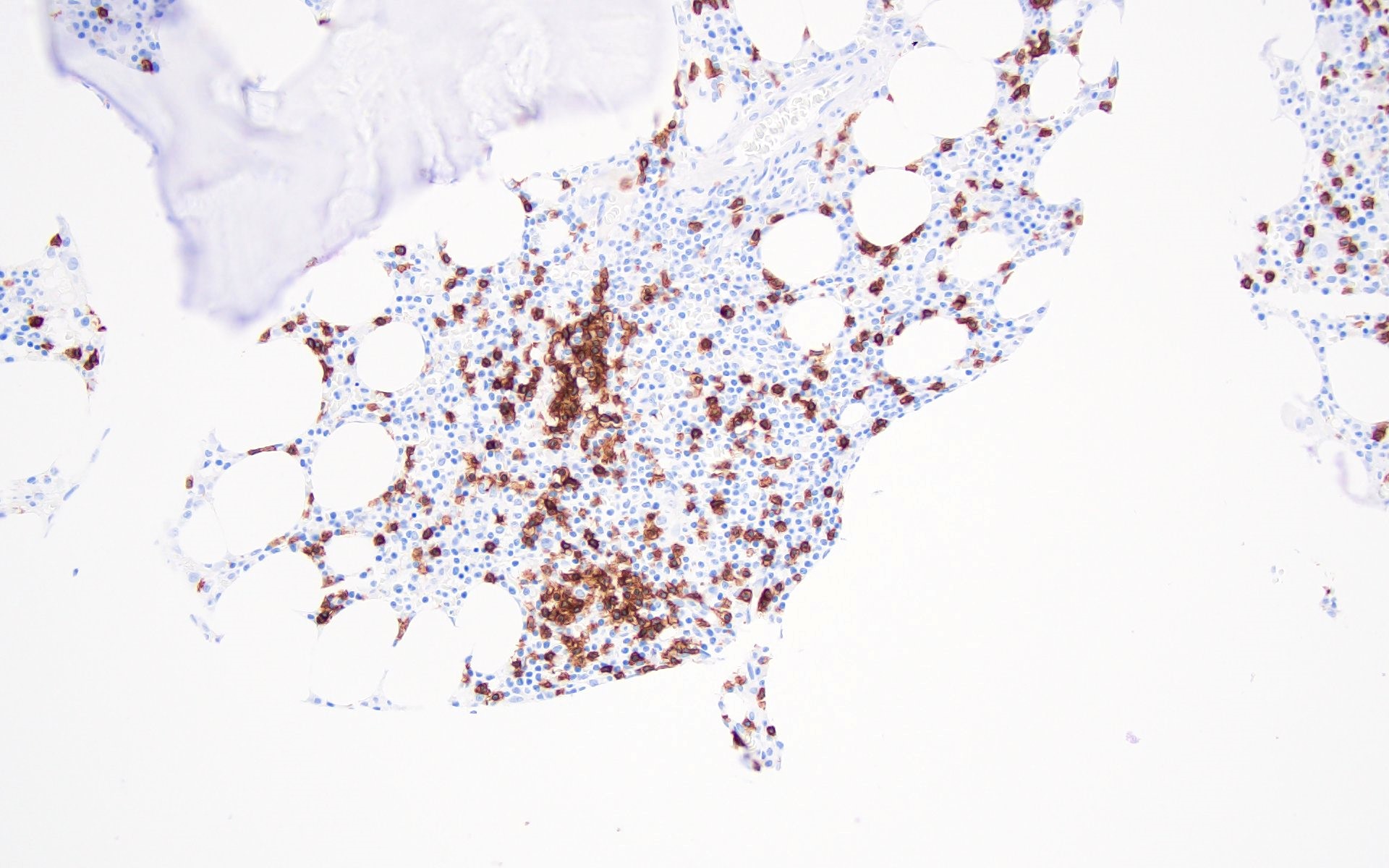
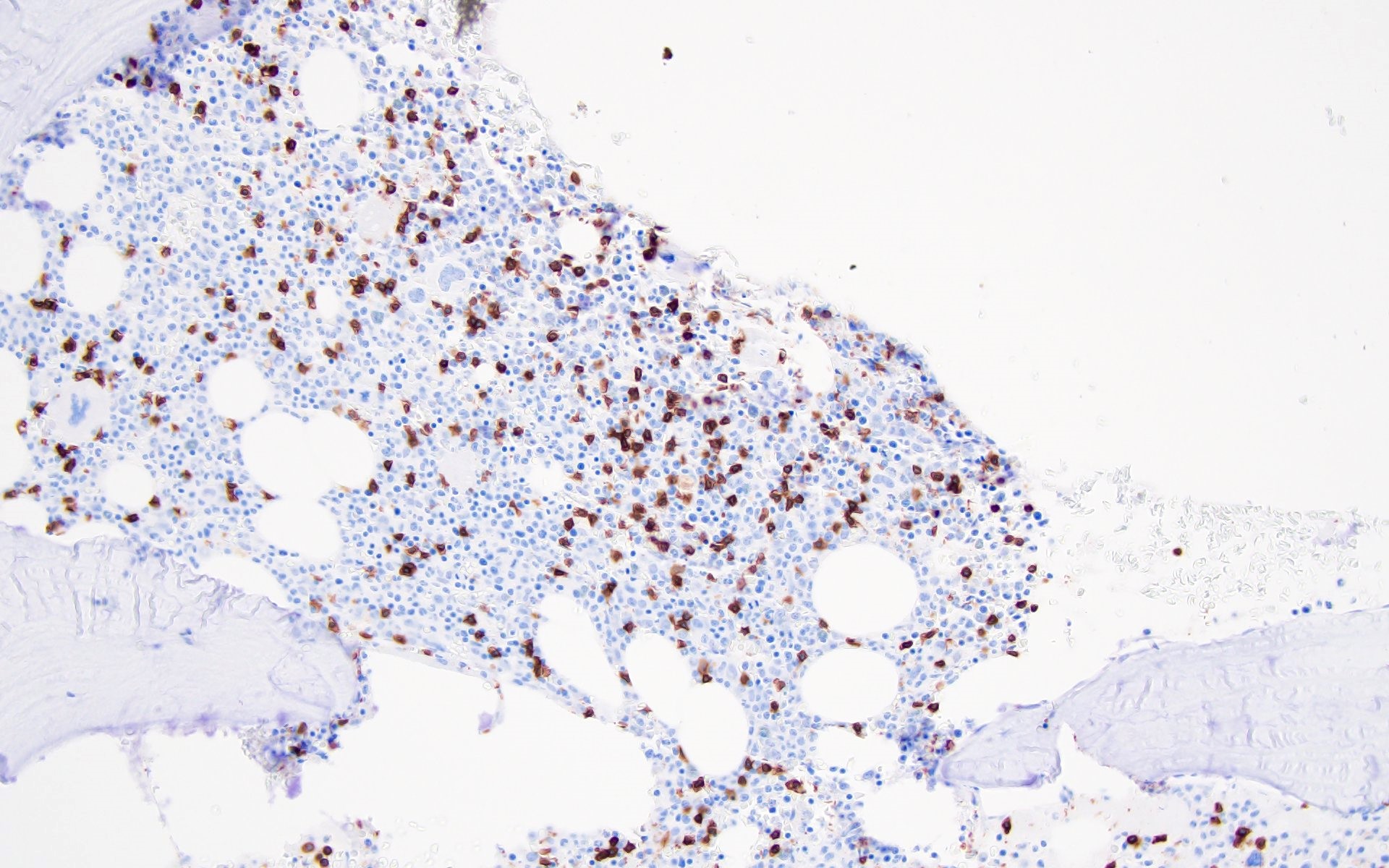
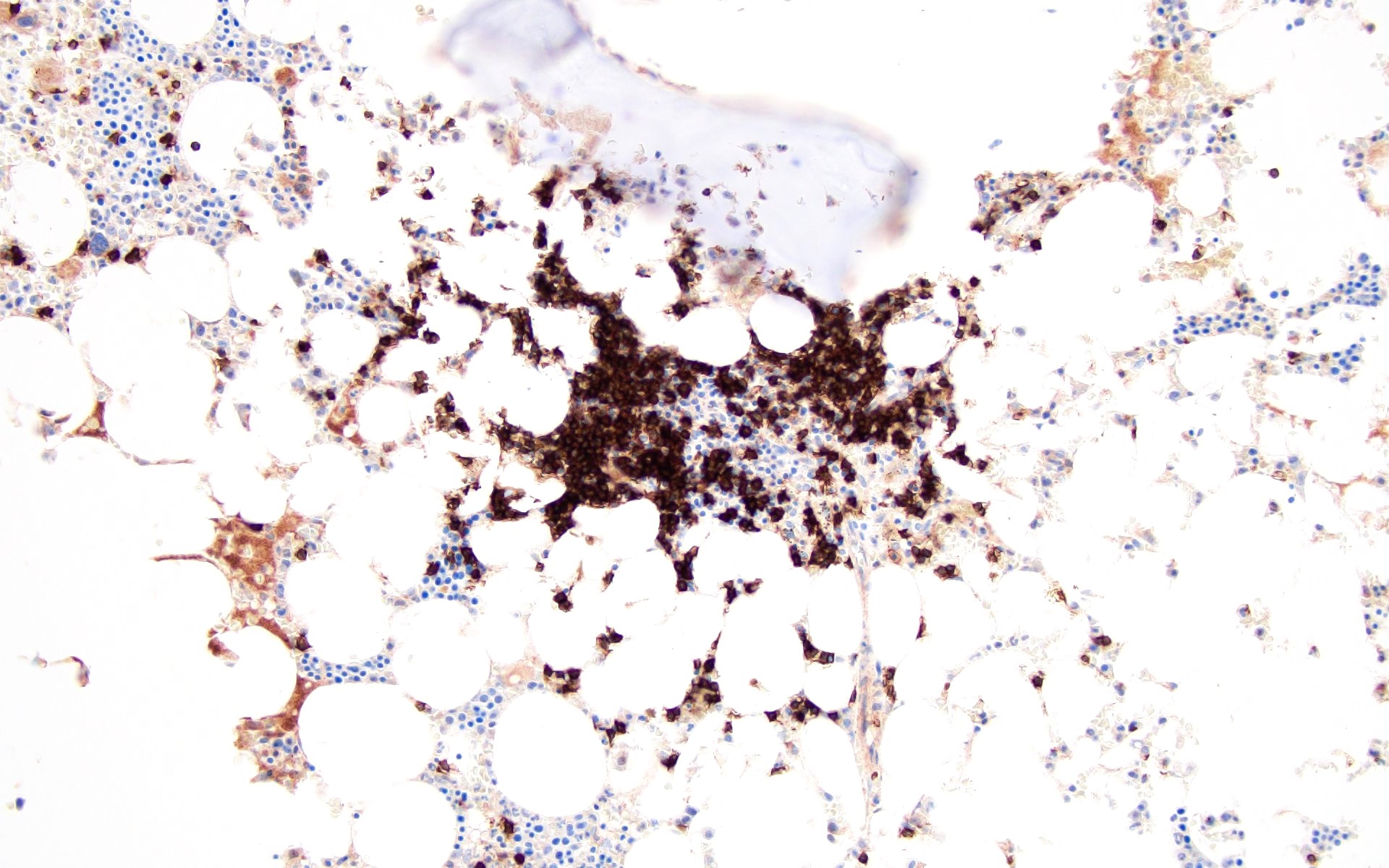
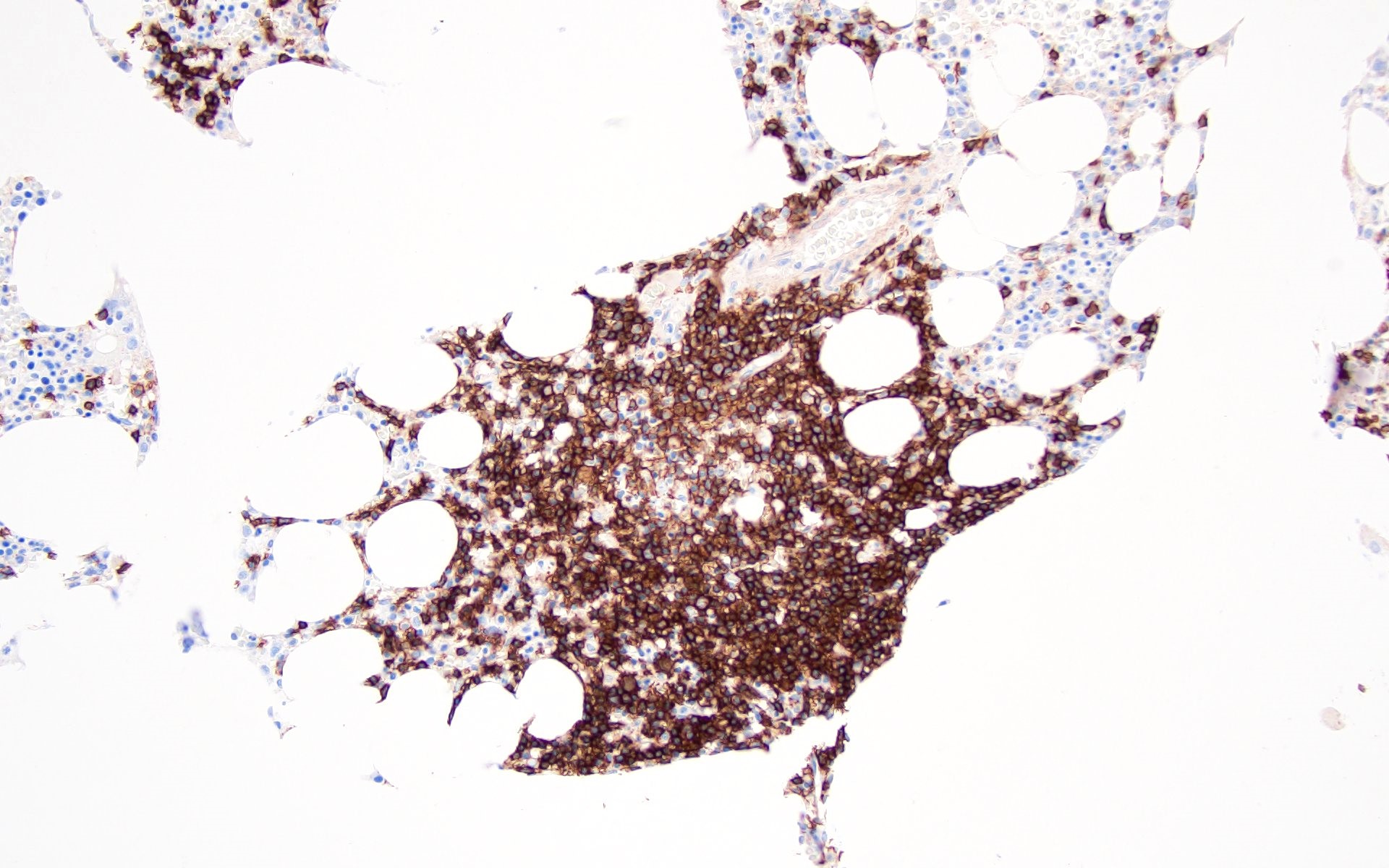
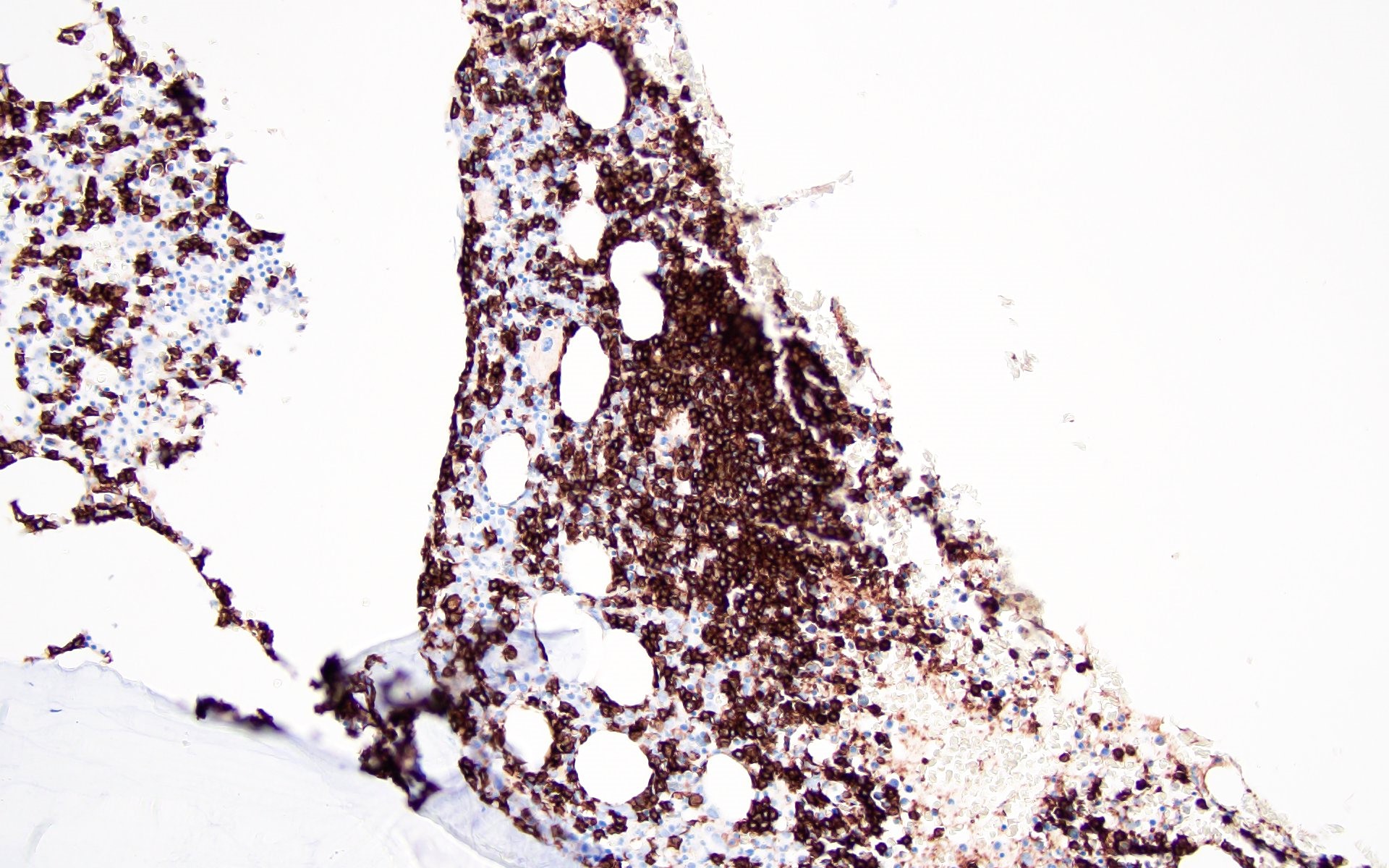
Microscopic (histologic) images
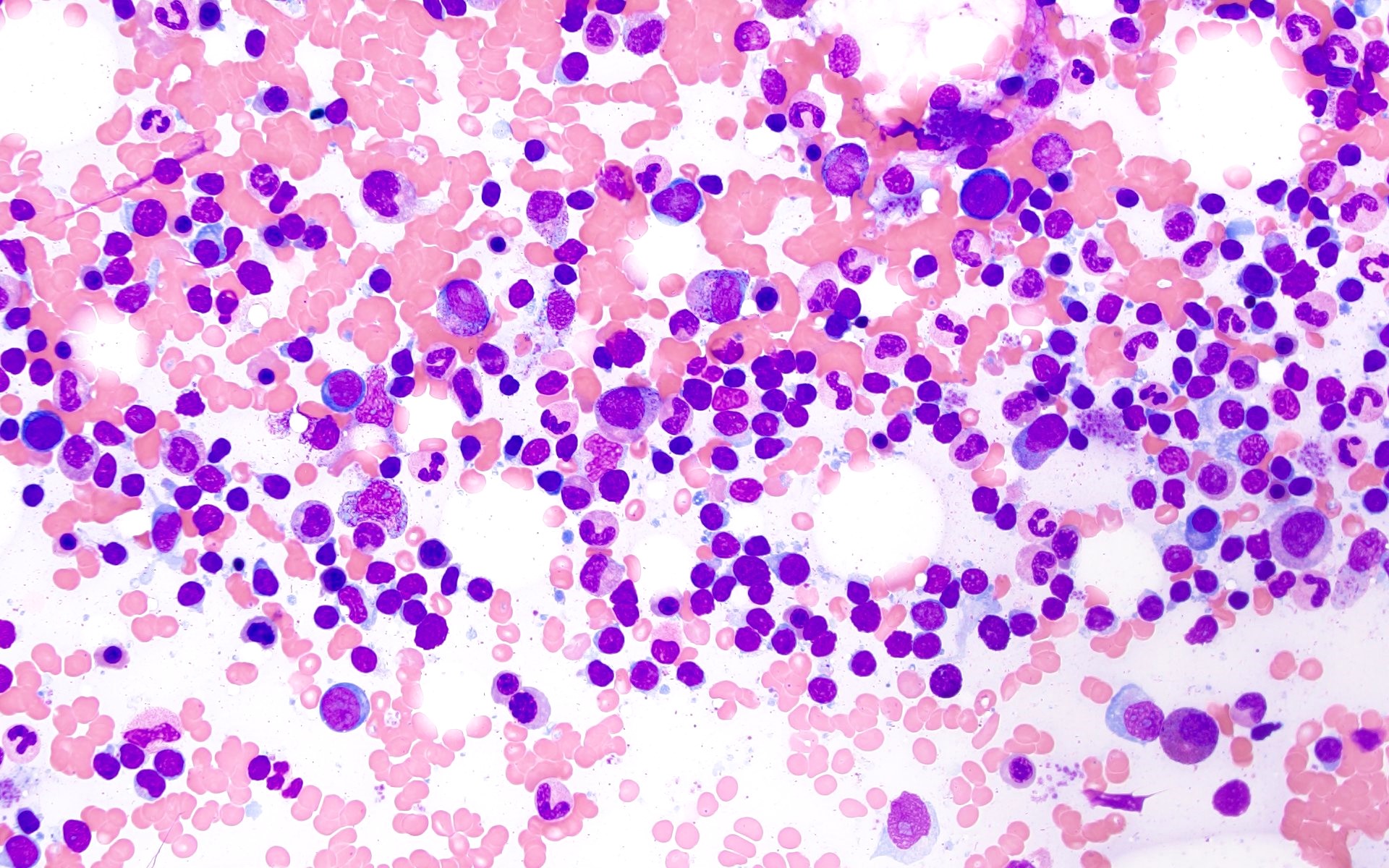
Cytology description
- Bone marrow aspirate may show lymphocytosis, consisting of small to medium sized, mature appearing lymphocytes without atypia
Negative stains
Flow cytometry description
- No monotypic B cell or phenotypically aberrant T cell populations identified
- Flow cytometry is used to assess the surrogate markers of clonality for B and T cells
- Kappa and lambda immunoglobulin light chains are evaluated for monotypic B cells, which includes kappa:lambda ratio > 3 or < 0.5
- Neoplastic B cells may also show lack of surface immunoglobulin light chains
- Abnormal T cell phenotype is described by abnormal expression patterns of T cell markers; for example, downregulation of surface CD3 expression, loss of CD7 or CD5 as well as a skewed CD4:CD8 ratio or expansion of double positive (CD4+ / CD8+) or double negative (CD4- / CD8-) populations
- Clonal T cell or NK cell populations can be evaluated by assessment of TCR Vβ or KIR repertoire, respectively
- TCR constant β chain 1 (TRBC1) expression is based on the expression of TCR β chain with either a constant region 1 or a constant region 2 (C1 or C2) on mature αβ T cells
- T cell clone is characterized by either a relative increase or a relative decrease in TRBC1+ T cells (Int J Mol Sci 2021;22:1817)
Molecular / cytogenetics description
- Molecular tests based on polymerase chain reaction (PCR) are used for detection of immunoglobulin heavy chain (IGH) and light chains or T cell receptor gene rearrangements to identify the clonal nature of lymphoid aggregates and are negative in benign lymphoid aggregates
- Cytogenetic analysis: normal karyotype and no abnormal FISH signals
Sample pathology report
- Peripheral blood, bone marrow aspirate and left posterior iliac crest, bone marrow core biopsy:
- Normocellular marrow (~30% cellular) with trilineage hematopoiesis and multiple benign lymphoid aggregates (see comment)
- Comment: Flow cytometric immunophenotyping performed on the bone marrow aspirate reveals a polytypic B cell population and a T cell population without evidence of immunophenotypic abnormality based on the markers assayed.
- Microscopic description
- Peripheral blood smear: normocytic normochromic red blood cells with polychromasia and mild anisopoikilocytosis
- Neutrophils are adequate with unremarkable morphology; platelets are adequate with unremarkable morphology
- Bone marrow aspirate smear: the myeloid and erythroid series show progressive maturation with unremarkable morphology
- No overt increase in blasts, lymphocytes or plasma cells noted; megakaryocytes are present with predominantly unremarkable morphology
- Bone marrow core biopsy (decalcified): the unilateral bone marrow core biopsy is normocellular for age (~50% cellular)
- The myeloid and erythroid series show progressive maturation
- Megakaryocytes are adequately present with unremarkable morphology
- Multiple interstitial lymphoid aggregates, which are composed predominantly of small lymphocytes, are noted
- Immunohistochemistry: CD3 and CD20 highlights mixture of interstitially scattered as well as aggregates of CD3+ T cells and CD20+ B cells, with T cell predominance
Differential diagnosis
- Persistent polyclonal B cell lymphocytosis:
- Rare condition of unknown etiology seen in young middle aged women who are usually smokers
- Mostly asymptomatic and are found to have absolute lymphocytosis, elevated serum IgM and binucleated lymphocytes
- Polyclonal B cells detected by flow cytometry
- Rare cases may have lymphadenopathy, hepatomegaly and splenomegaly
- Strong association with human leukocyte antigen DR7 and detection of translocation t(14;18) involving the BCL2 gene has been demonstrated in the literature
- Polymorphous reactive lymphoid hyperplasia:
- Characterized by the presence of interstitially increased lymphocytes or lymphoid aggregates in the bone marrow but it is usually focal, random and poorly circumscribed
- Lymphocytes are polymorphous, polytypic and are seen in the background containing plasma cells, immunoblasts, eosinophils and histiocytes
- Found in any age group and is mostly associated with underlying diseases, such as malignancies, postchemotherapy / stem cell transplant, infections and autoimmune disorders (Leuk Res 2013;37:1404)
- Systemic polyclonal B immunoblastic proliferation:
- Seen in middle aged to elderly population who present with fever, lymphadenopathy, hepatosplenomegaly and absolute lymphocytosis
- Peripheral blood shows circulating immunoblasts and plasmacytoid cells
- Bone marrow is hypercellular with extensive lymphocytic infiltration mimicking lymphoma
- No immunophenotypic abnormality is detected by flow cytometry
- No detection of IGH and TCR gene rearrangements by molecular studies (Cancer 1988;61:1350, Am J Clin Pathol 1992;98:222)
- Malignant lymphoid aggregates:
- Characteristic morphological findings include large / multiple lymphoid aggregates, paratrabecular localization, infiltrative border, distribution around large sinuses with increasing size on deeper sections
- Detection of clonality by flow cytometry and rearrangements by molecular studies
Board review style question #1
Board review style answer #1
A. Infiltrative border, cytologic atypia, B cell rich pattern. Malignant lymphoid aggregates usually have an infiltrative border, show cytologic atypia and are B cell rich (patterns 4 and 5). Answer B is incorrect because malignant lymphoid aggregates are composed predominantly of B cells. Answer C is incorrect because malignant lymphoid aggregates do not have a distinct border and are not usually T cell rich. Answer D is incorrect because malignant lymphoid aggregates demonstrate cytologic atypia and are usually large in size.
Comment Here
Reference: Lymphoid aggregates (benign)
Comment Here
Reference: Lymphoid aggregates (benign)
Board review style question #2
The benign lymphoid aggregate (LA) shows a germinal center composed of centrocytes and centoblasts along with follicular dendritic meshwork (CD21+) on bone marrow core biopsy. Which of the following would be the immunophenotypic profile of the LA?
- CD10+, BCL6+, BCL2+
- CD10+, BCL6+, BCL2-
- HGAL+, BCL6+, BCL2+
- LMO2+, CD10+, BCL2+
Board review style answer #2
B. CD10+, BCL6+, BCL2-. Benign lymphoid aggregates with a germinal center on the bone marrow core biopsy will be CD10+, BCL6+, BCL2-. CD10, BCL6, HGAL and LMO2 are germinal center markers and benign (normal) germinal centers are BCL2-, unlike malignant aggregates which are BCL2+. Answer A is incorrect because malignant lymphoid aggregates will be positive for germinal center markers (CD10+, BCL6+) and BCL2+. Answer C is incorrect because malignant lymphoid aggregates will be positive for germinal center markers (BCL6+, HGAL+) as well as BCL2+. Answer D is incorrect because malignant lymphoid aggregates will be positive for germinal center markers (CD10+, LMO2+) as well as BCL2+.
Comment Here
Reference: Lymphoid aggregates (benign)
Comment Here
Reference: Lymphoid aggregates (benign)