Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Peripheral smear description | Peripheral smear images | Positive stains | Negative stains | Flow cytometry description | Flow cytometry images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Shi M, Jevremovic D. T cell large granular lymphocytic leukemia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonBtLGL.html. Accessed May 13th, 2024.
Definition / general
- A chronic T cell lymphoproliferative disorder characterized by a clonal proliferation of mature cytotoxic T cells without an identified cause
- Patients commonly present with cytopenia(s) and eventually require treatment
Essential features
- Indolent clonal proliferation of mature cytotoxic T cells
- Neutropenia or anemia
- Associated with autoimmune disorders
- Commonly CD8+ T cells coexpressing NK cell associated markers
- Characteristic intrasinusoidal involvement in bone marrow, spleen and liver
- Approximately half of the patients carry a STAT3 / STAT5b mutation
Terminology
- T cell large granular lymphocytosis; T cell lymphoproliferative disease of granular lymphocytes
ICD coding
Epidemiology
- 2 - 5% of mature lymphocytic leukemias
- M = F
- Commonly occurs in elderly individuals with a median age of 60 years (Blood 2017;129:1082)
Sites
- Peripheral blood, bone marrow, spleen, liver
Pathophysiology
- Oligoclonal expansion of cytotoxic large granular T cells in response to antigen stimulation
- Subsequent clonal proliferation of large granular T cells due to constitutive upregulation of cellular survival signals or downregulation of apoptotic pathways via a secondary event
- STAT3 / STAT5b mutation as a secondary event (N Engl J Med 2012;366:1905, Blood 2012;120:3048)
- Other secondary events include resistance to Fas / FasL mediated cell death, increased cell survival by interleukin 15 and platelet derived growth factor and activation of NFkB pathway (Blood 2018;131:2803)
- Neutropenia and anemia are caused by direct cytotoxicity from the clonal T cells
Etiology
- Chronic antigen exposure from autoimmune disorders such as rheumatoid arthritis and Sjögren syndrome
- Chronic antigen exposure due to viral infection such as human T lymphotropic virus
Clinical features
- Approximately 70% of patients have neutropenia or anemia
- Approximately 30% of patients are asymptomatic but regular complete blood count reveals lymphocytosis and cytopenia(s) (Blood 2017;129:1082)
- Splenomegaly in approximately 30% of patients
- Approximately 30% of patients carry autoimmune disorders with rheumatoid arthritis being by far the most common (Blood 2017;129:1082)
- Could be associated with other hematologic malignancies such as B cell lymphoma, myelodysplastic syndrome and aplastic anemia
Diagnosis
- Persistent (more than 6 months) increase in the number of peripheral blood large granular lymphocytes, usually 2-20 x 10⁹
- Distinct T cell population with coexpression of one or more NK cell associated antigens (CD16, CD56 or CD57) and decreased CD2, CD5 or CD7 expression
- Proof of T cell clonality by a molecular or flow cytometry study
- Intrasinusoidal cytotoxic T cell infiltrates in bone marrow, spleen or liver (Blood 2002;99:268)
- STAT3 or STAT5b mutation (N Engl J Med 2012;366:1905, Blood 2012;120:3048)
Laboratory
- Variable lymphocytosis (Blood 2017;129:1082)
- Neutropenia occurs in approximately 85% of patients, anemia in 50% with pure red cell aplasia in 10% and thrombocytopenia in < 25%
- Rheumatoid factor and antinuclear antibodies could be positive
Radiology description
- Splenomegaly in 30% of patients (Blood. 2017;129:1082)
- Hepatomegaly < 30% of patients
- Rarely lymphadenopathy
Prognostic factors
- Overall an indolent disease
- Deaths infrequently occur because of infections related to severe neutropenia
- STAT3 / STAT5b mutations may adversely impact overall survival (Leukemia 2019 Nov 18 [Epub ahead of print], Blood 2013;121:4541)
Case reports
- 16 year old boy developed donor derived T cell large granular lymphocytic leukemia after hematopoietic stem cell transplant (J Natl Compr Canc Netw 2016;14:939)
- 54 year old man with giant intracytoplasmic inclusion in T cell large granular lymphocytic leukemia cells (Blood 2019;134:492)
- 55 year old woman suffered from panuveitis caused by T cell large granular lymphocytic leukemia (Ocul Immunol Inflamm 2019:1)
- 57 year old woman with immunoglobulin heavy chain amyloidosis (Am J Case Rep 2019;20:43)
- 65 year old man developed late graft rejection by recipient origin T cell large granular lymphocytic leukemia (Transplant Proc 2016;48:3222)
Treatment
- The majority of patients eventually require treatment because of severe or symptomatic neutropenia or anemia
- No standard therapy established
- Immunosuppressive therapy (methotrexate, cyclophosphamide or cyclosporine) as initial agents
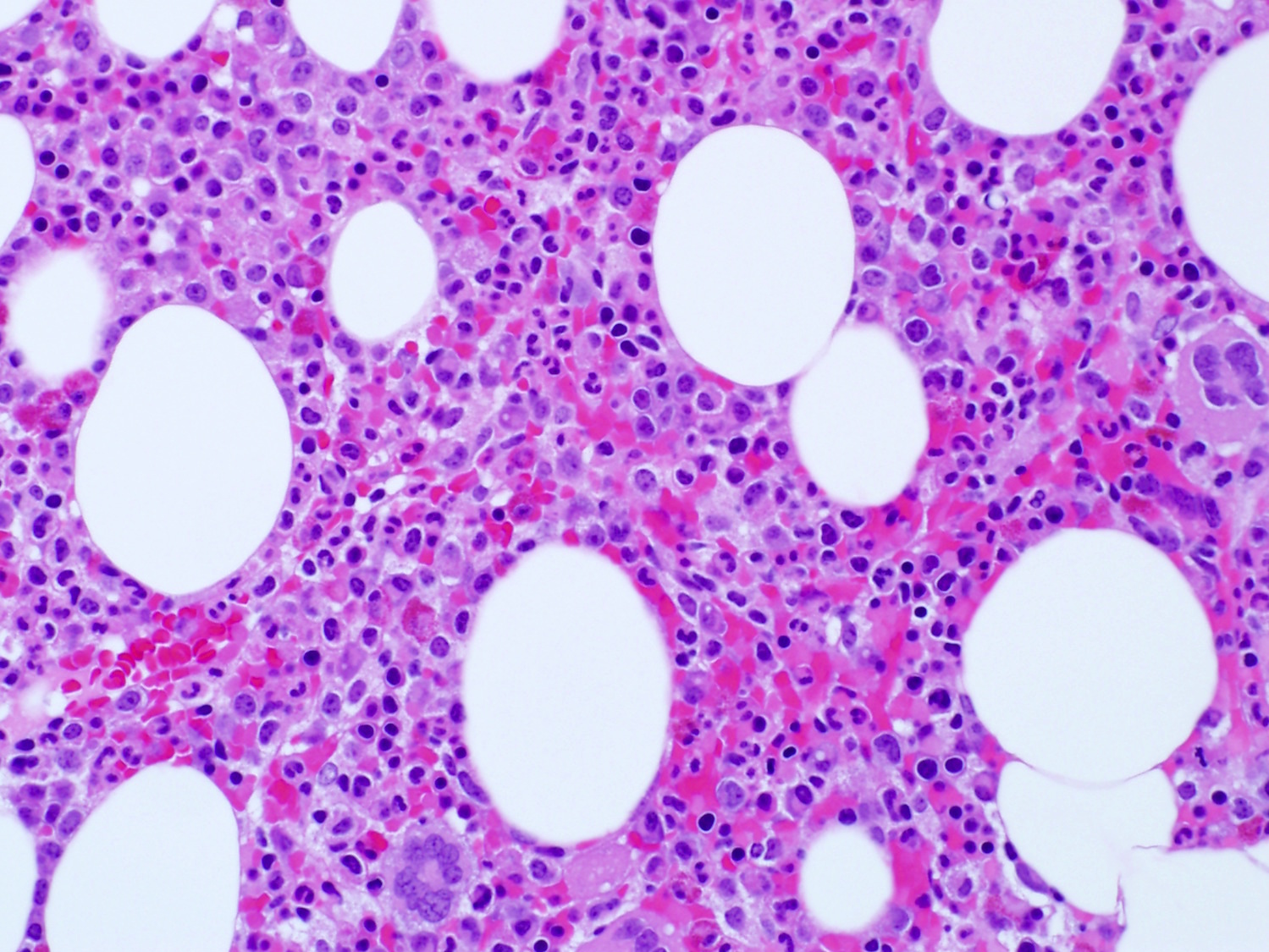
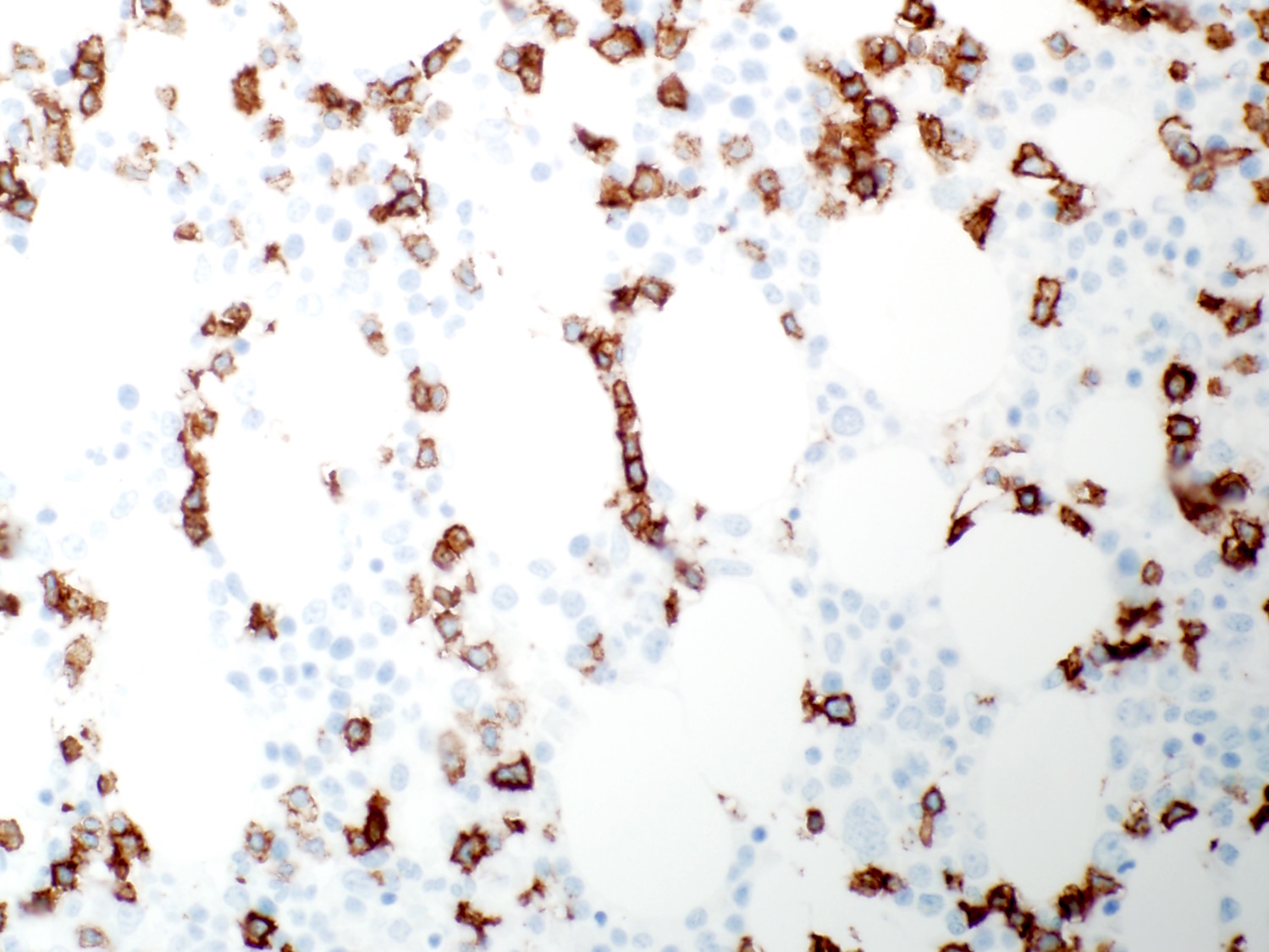
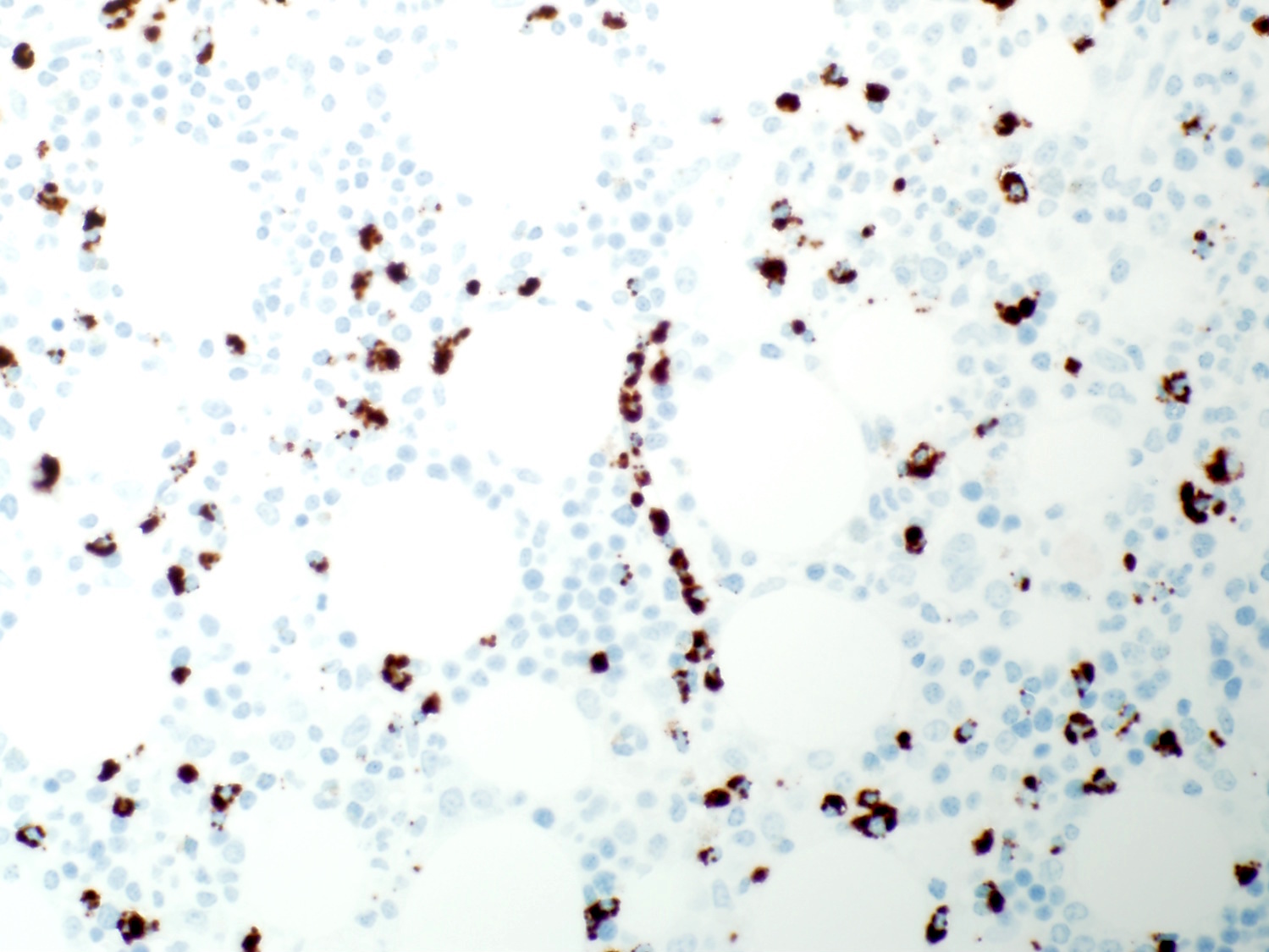
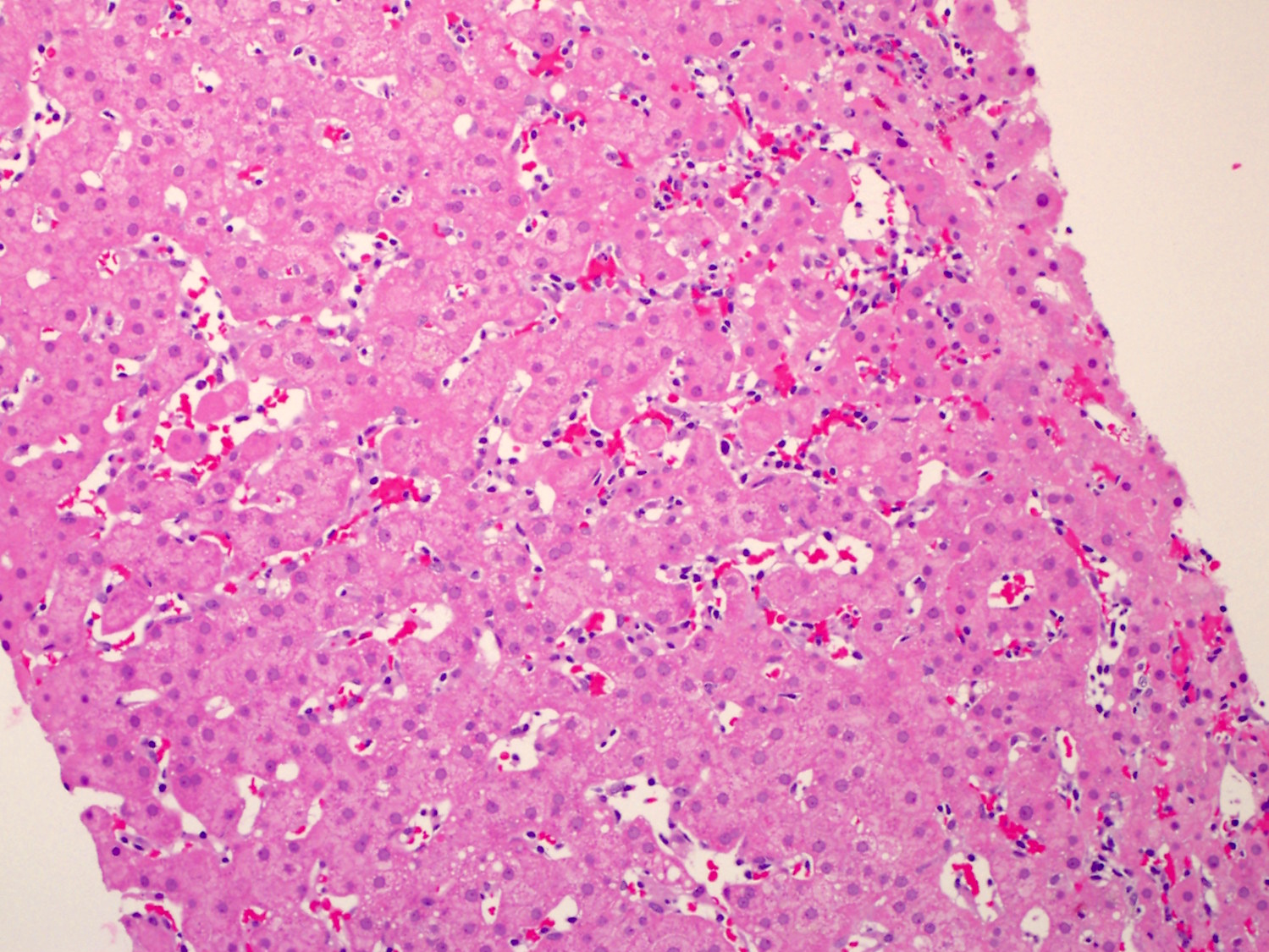
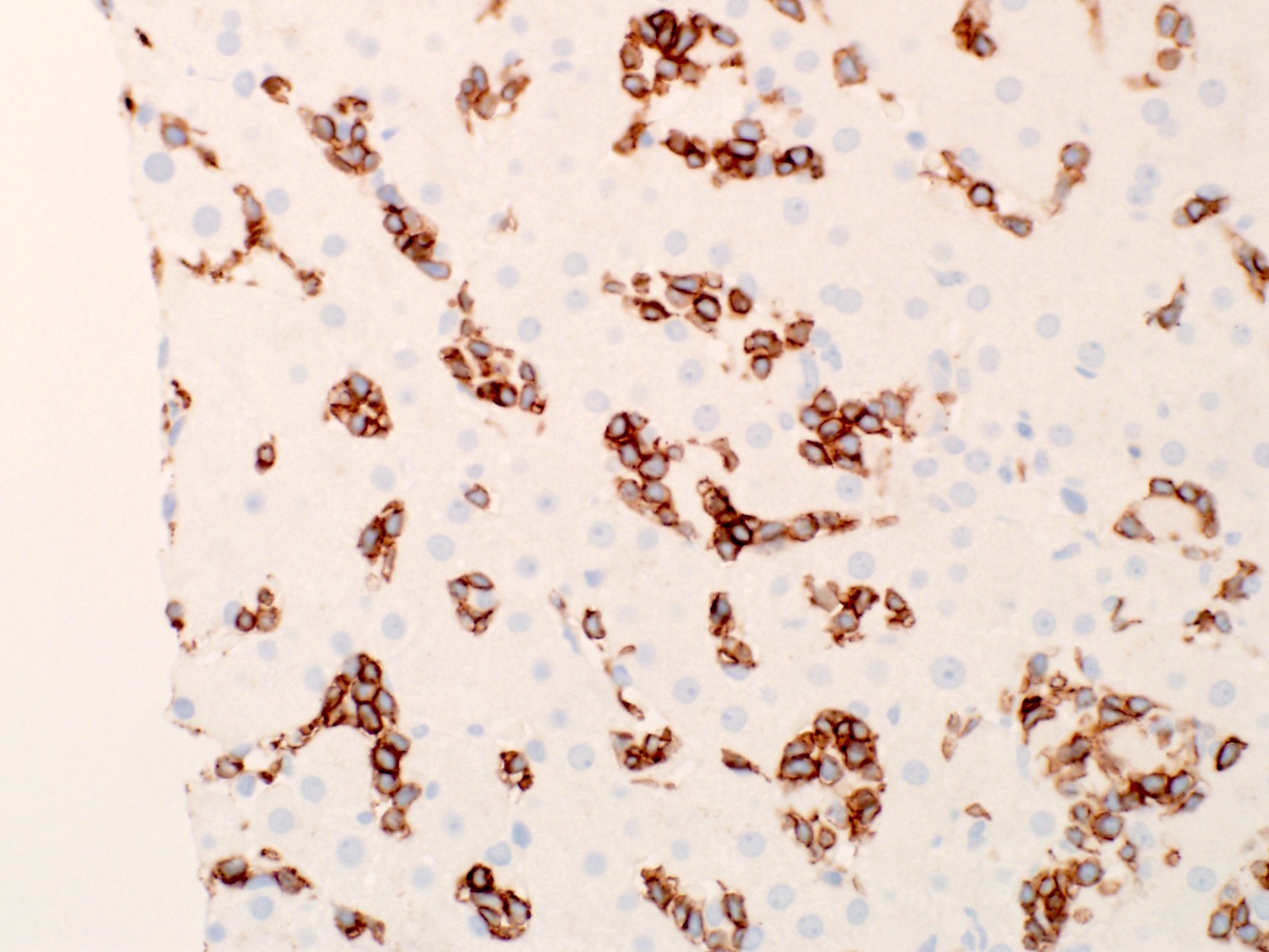
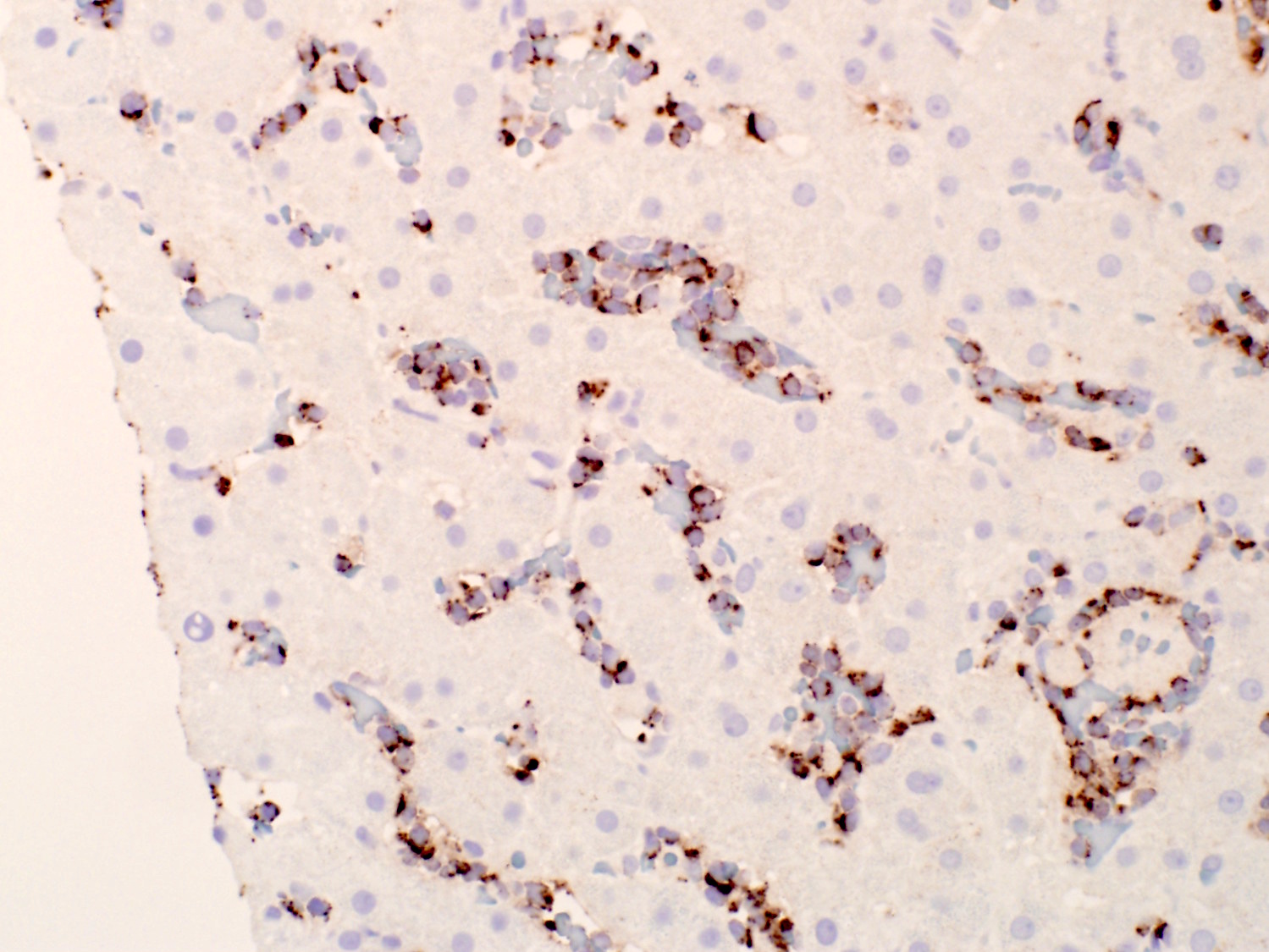
Microscopic (histologic) description
- Bone marrow biopsy does not show apparent abnormal lymphocytic infiltrates by hematoxylin and eosin stain; immunohistochemical studies reveal the characteristic linear / intrasinusoidal distribution of cytotoxic T cells (Blood 2002;99:268)
- Spleen biopsy demonstrates linear arrays of cytotoxic T cells in the sinusoids and red pulp cords
- Liver biopsy reveals linear arrays of cytotoxic T cells in the sinusoids
Microscopic (histologic) images
Contributed by Min Shi, M.D., Ph.D. and Dragan Jevremovic, M.D., Ph.D.
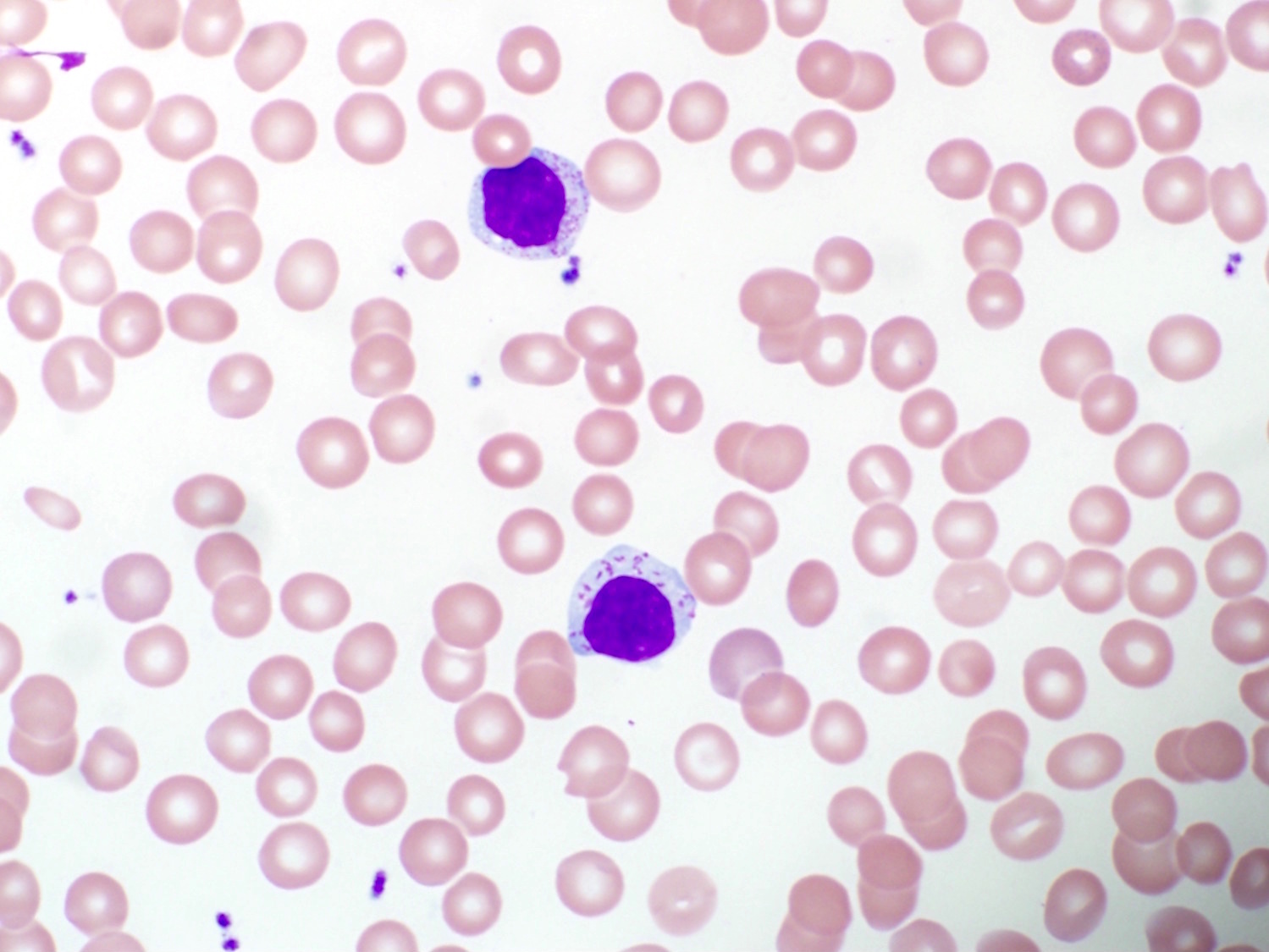
Peripheral smear description
- Increased lymphocytes containing small to intermediate sized reticulated nuclei and fine to coarse azurophilic cytoplasmic granules
Peripheral smear images
Positive stains
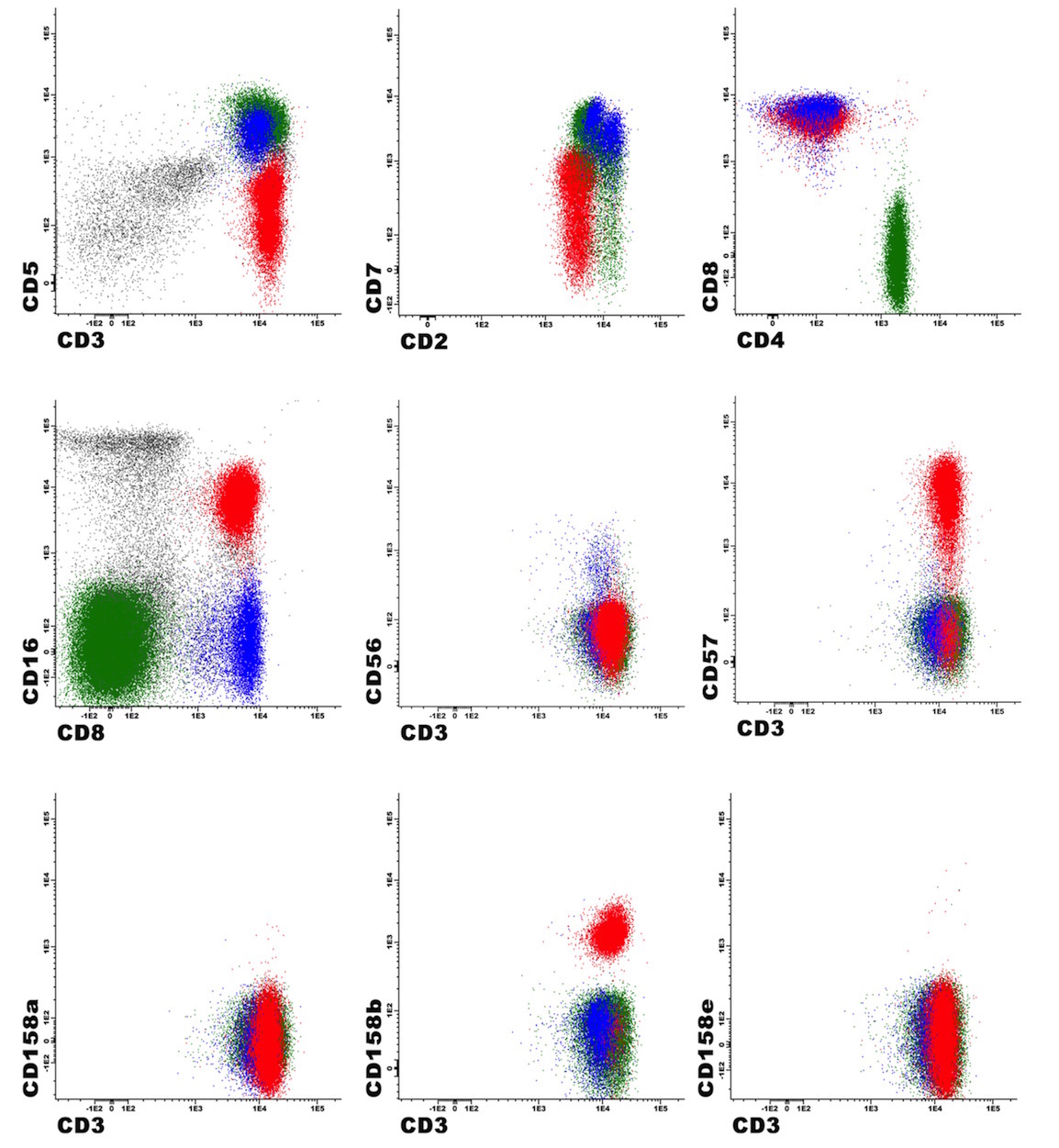
Flow cytometry description
- Mature CD3 positive T cells, usually coexpress NK cell associated markers (CD16 and CD57), with variable expression of other pan T cell markers such as CD2, CD5, CD7; 25% of cases are KIR restricted
- CD4- CD8+ T cell type being the most common, followed by TCRγδ+ T cell type, CD4+ CD8- T cell type, TCRαβ+ CD4- CD8- T cell type and rarely mixed phenotype (Hum Pathol 2018;81:96)
Flow cytometry images
Molecular / cytogenetics description
- Clonal T cell receptor (TCR) gene rearrangements
- STAT3 mutation in 40 - 50% of T cell large granular lymphocytic leukemia (N Engl J Med 2012;366:1905, Blood 2012;120:3048)
- STAT5b mutation in 2% of T cell large granular lymphocytic leukemia (Blood 2013;121:4541)
- No specific cytogenetic abnormalities
Sample pathology report
- Peripheral blood, bone marrow aspirate and biopsy, iliac crest:
- T cell large granular lymphocytic leukemia involving 15% marrow cellularity with normal trilineage hematopoiesis
- Peripheral blood smear: neutropenia; absolute lymphocytosis with increased large granular cells
- Bone marrow aspirate and biopsy: adequate quality; normal M:E ratio; slightly hypercellular marrow with left shift granulopoiesis, otherwise normal hematopoiesis; slight interstitial lymphocytic infiltrates of small lymphocytes
- Flow cytometric immunophenotyping: distinct T cell population (70% of gated lymphoid events, 30% of total analyzed events) with expression of CD2, CD3, CD5 (dim), CD7 (dim), CD8, CD16, CD57, CD94 (partial), CD158b (restricted); they do not express CD4, CD56, CD158a, CD158e, NKG2A and TCR gamma / delta
- Molecular study for TCR gene rearrangement: positive for clonal TCR gene rearrangement
Differential diagnosis
- Reactive T cell expansion:
- Clinical presentation (viral infection or an autoimmune disorder)
- Polyclonal
- No linear arrays of cytotoxic T cells in the bone marrow
- Chronic lymphoproliferative disorder of NK cells:
- Peripheral T cell lymphoma:
- Aggressive clinical presentation (B symptoms, lymphadenopathy)
- Neoplastic cells have very irregular nuclear contours
- Loss of pan T cell markers
- Hepatosplenic T cell lymphoma:
- Aggressive clinical presentation
- TCRγδ+, TIA1+, perforin-, granzyme B-
- Isochromosome 7q
Board review style question #1
What is the most common immunphenotype of T cell large granular lymphocytic leukemia?
- CD2+ CD3- CD4- CD5- CD7+ CD8+ CD16+ CD56- CD57+
- CD2+ CD3+ CD4- CD5- CD7+ CD8+ CD16+ CD56- CD57+
- CD2+ CD3+ CD4+ CD5- CD7+ CD8+ CD16+ CD56- CD57+
- CD2- CD3+ CD4- CD5- CD7+ CD8+ CD16- CD56- CD57-
- CD2+ CD3- CD4- CD5- CD7+ CD8- CD16- CD56+ CD57-
Board review style answer #1
B. The most common immunophenotype of T cell large granular lymphocytic leukemia is that of mature CD3+ CD8+ T cells expressing NK cell associated markers such as CD16 and CD57 and variable pan T cell marker lost. A) Typical chronic lymphoproliferative disorder of NK cells immunophenotype. C) Rare T cell large granular lymphocytic leukemia immunophenotype. D) Peripheral T cell lymphoma immunophenotype without NK cell associated marker expression. E) Aggressive NK cell leukemia immunophenotype.
Comment Here
Reference: T cell large granular lymphocytic leukemia
Comment Here
Reference: T cell large granular lymphocytic leukemia
Board review style question #2
- Which genetic abnormality is most commonly identified in T cell large granular lymphocytic leukemia?
- STAT5b mutation
- NOTCH mutation
- TP53 mutation
- STAT3 mutation
- TCL1A rearrangement
Board review style answer #2
D. STAT3 mutation is the most common genetic mutation in T cell large granular lymphocytic leukemia which results in constitutive activation of JAK / STAT3 pathway and drives proliferation and survival of neoplastic cells.
Comment Here
Reference: T cell large granular lymphocytic leukemia
Comment Here
Reference: T cell large granular lymphocytic leukemia