Table of Contents
Definition / general | Essential features | Epidemiology | Diagrams / tables | Clinical features | Diagnosis | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Xu B. Adenoid cystic carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsadenoidcystic.html. Accessed May 19th, 2024.
Definition / general
- A carcinoma of primary salivary gland or minor salivary gland of upper aerodigestive tract characterized by its biphasic ductal and myoepithelial differentiation, tubular / cribriform / solid architecture (Head Neck 2017;39:456)
- May occur in major and minor salivary glands
- Among major salivary glands, the most commonly affected site is the parotid gland
- Minor salivary glands that may be affected include those of oral cavity, sinonasal tract, nasopharynx, oropharynx and trachea
Essential features
- Grows in tubular, cribriform, and/or solid patterns: solid pattern is associated with adverse outcome
- 60% - 90% carry MYB-NFIB or MYBL1-NFIB fusion
- Biphasic tumor showing ductal and myoepithelial differentiation
- Frequent perineural invasion
Epidemiology
- M=F (Head Neck 2017;39:456)
- Mean age 57 (Head Neck 2017;39:456)
Clinical features
- Characterized by a propensity of perineural invasion, high frequency of local and distant recurrence and poor long term prognosis (Eur J Cancer 2015;51:2768, Head Neck 2017;39:456, Braz J Otorhinolaryngol 2015;81:329, Head Neck 2014;36:998)
- 5 year overall survival 55 - 89%
- 15 year or 20 year survival is dismal, in the range of 20 - 40%
- Rates of local recurrence and distant metastasis are 16 - 67% and 8 - 46%
- Lung is most common site of distant metastasis (Head Neck 2017;39:456)
Diagnosis
- Diagnosis is based on tissue examination findings of typical histologic features or the presence of fusion involving MYB, MYBL1 or NFIB genes
Prognostic factors
- Independent prognostic predictors include AJCC TNM staging, margin status, high mitotic index (defined as ≥ 5 per 10 high power fields) and solid architecture (Am J Surg Pathol 2017;41:1422)
- Presence and percentage of solid architecture reflects clinical outcome and should be reported in the pathology report
- Some studies showed that the presence but not the percentage of solid growth is an independent predictor for adverse outcome (Am J Surg Pathol 2017;41:1422, Oral Surg Oral Med Oral Pathol Ora Radio 2013;115:368, Head Neck 2017;39:456)
- Other studies show that tumors with higher percentage of solid pattern, defined as 30% or more, are associated with increased risk of recurrence and decreased survival (Cancer 1984;54:1062, Cancer 1978;42:265)
- Based on the above data, 2 grading systems have been proposed (table)
- Current WHO classification does not endorse any specific grading system (IARC: WHO Classification of Head and Neck Tumours, 4th Edition, 2017)
- Other poor prognostic factors include female sex, older age, sinonasal location, lymphovascular invasion, high grade transformation and intraneural invasion
Perzin 1978 and Szanto 1984 Van Weert 2015, Zhang 2013 and Xu 2018 Grade 1 (low grade): no solid component Grade 1: no solid component Grade 2 (intermediate grade): 1 - 29% solid component Grade 2 (high grade): with solid component Grade 3 (high grade): ≥ 30% solid component
- Perzin 1978 (Cancer 1978;42:265) and Szanto 1984 (Cancer 1984;54:1062)
- Van Weert 2015 (Head Neck 2017;39:456), Zhang 2013 (Oral Surg Oral Med Oral Pathol Ora Radio 2013;115:368) and Xu 2018 (Am J Surg Pathol 2017;41:1422)
Case reports
- 27 year old woman with parotid adenoid cystic carcinoma and high grade transformation (Diagn Pathol 2013;8:113)
- 36 year old man with tracheal tumor: an autopsy case (Head Neck Pathol 2019;13:243)
- 39 year old woman with lacrimal gland tumor (Head Neck Pathol 2013;7:85)
- 70 year old woman with soft palate adenoid cystic carcinoma extending to bilateral orbits through perineural spread along cranial nerves (Digit J Ophthalmol 2018;24:1)
- 70 year old man with laryngeal tumor (Oncol Lett 2018;16:2783)
Treatment
- Complete surgical resection with appropriate margins is the mainstream treatment
- Most patients receive adjuvant radiation therapy given the high rate of local recurrence and dismal long term survival
- Chemotherapy for patients with distant metastasis
- Multiple clinical trials are ongoing investigating the effects of tyrosine kinase inhibitors, e.g. axitinib (Ann Oncol 2016;27:1902) and dovitinib (Clin Cancer Res 2017;23:4138)
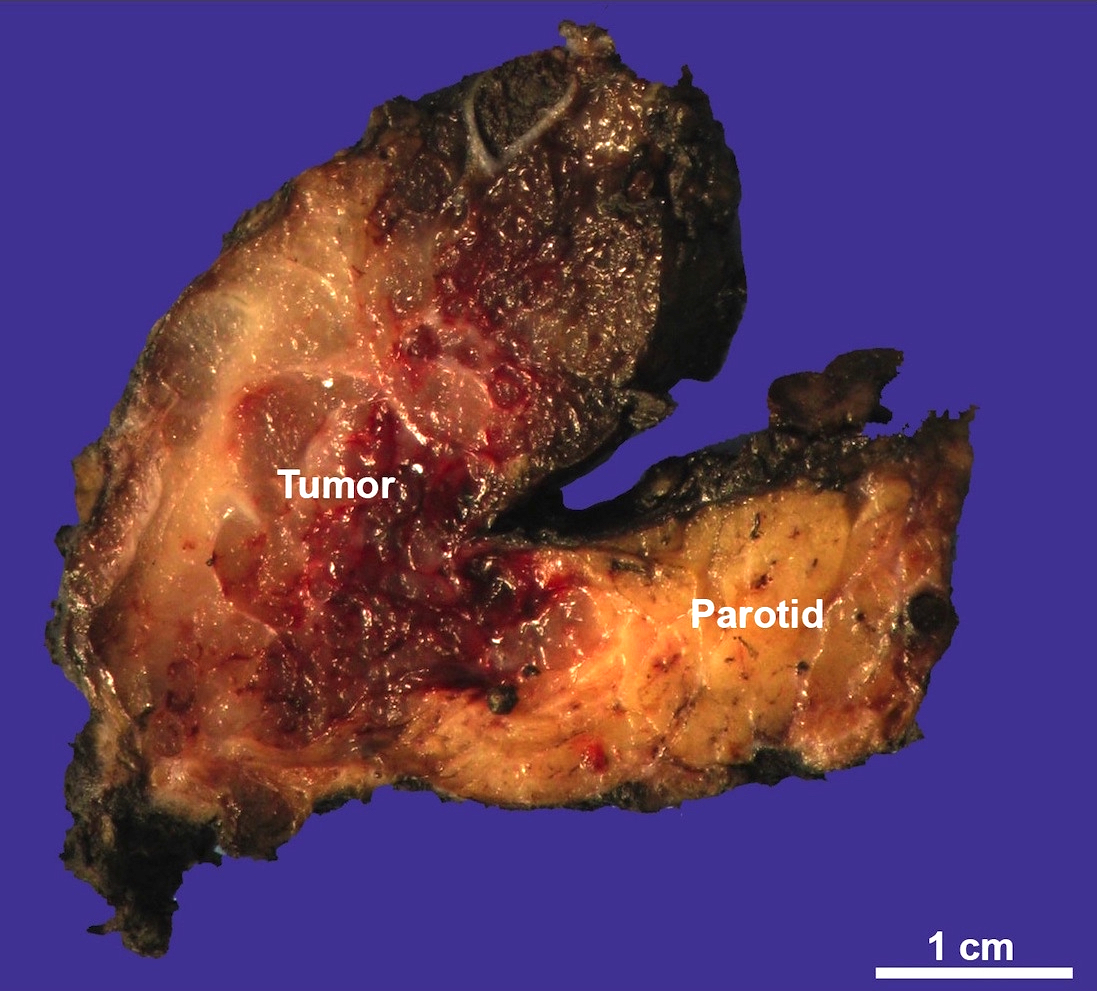
Gross description
- Infiltrative ill defined firm mass
Gross images
Frozen section description
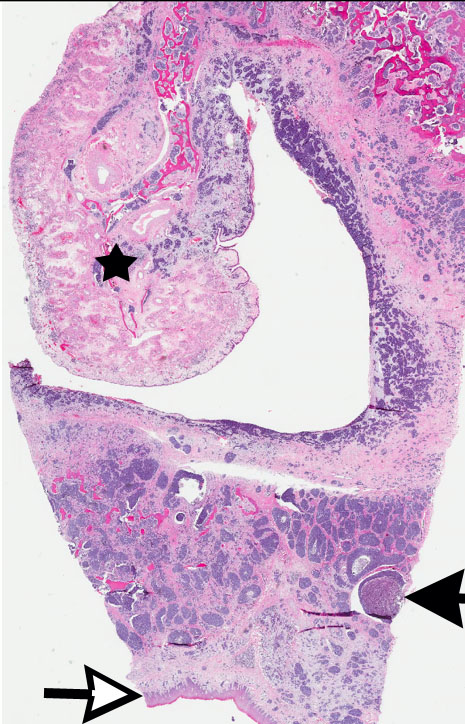
- Biphasic pattern of epithelial and myoepithelial cells and the typical tubular / cribriform / solid architecture are useful diagnostic cues
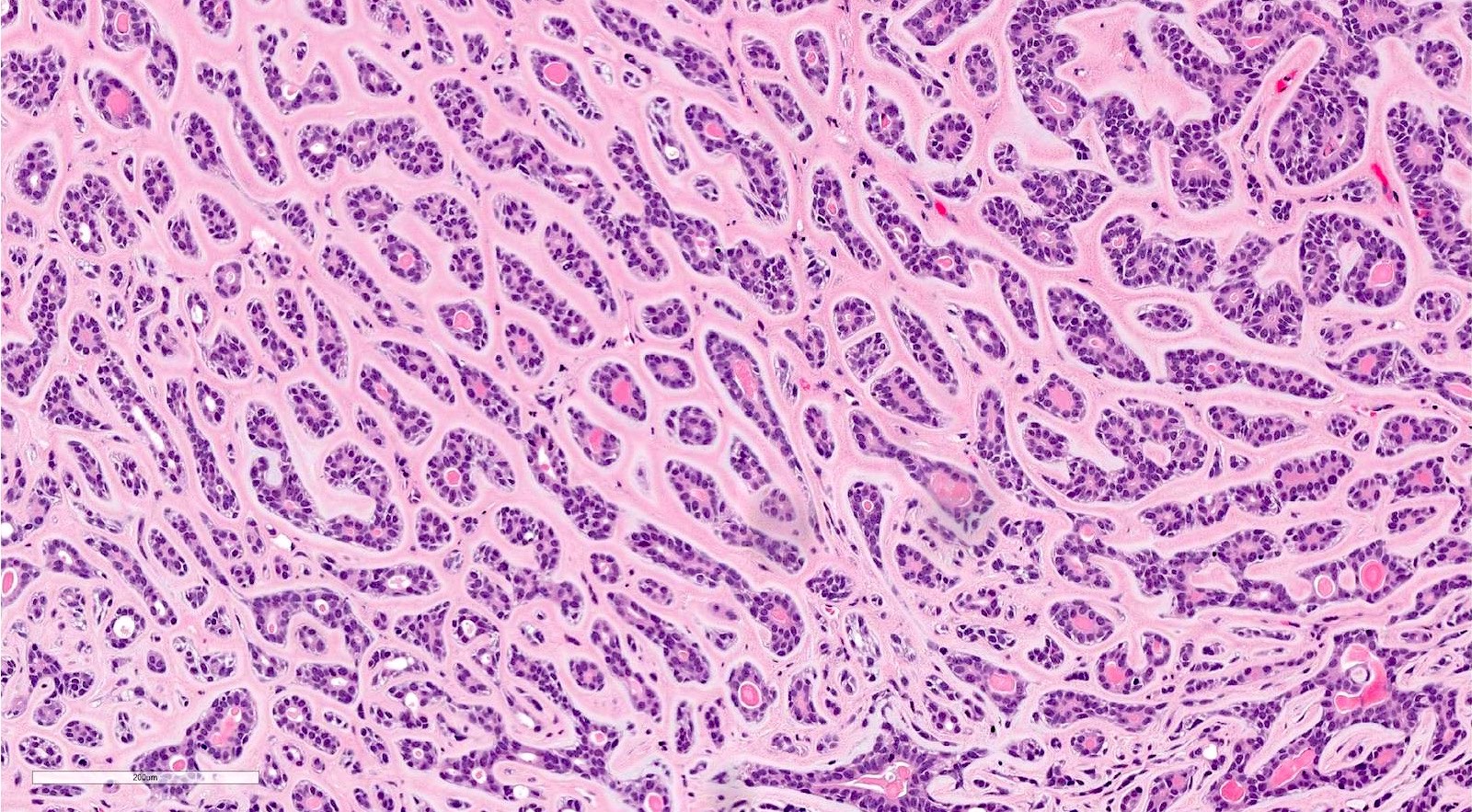
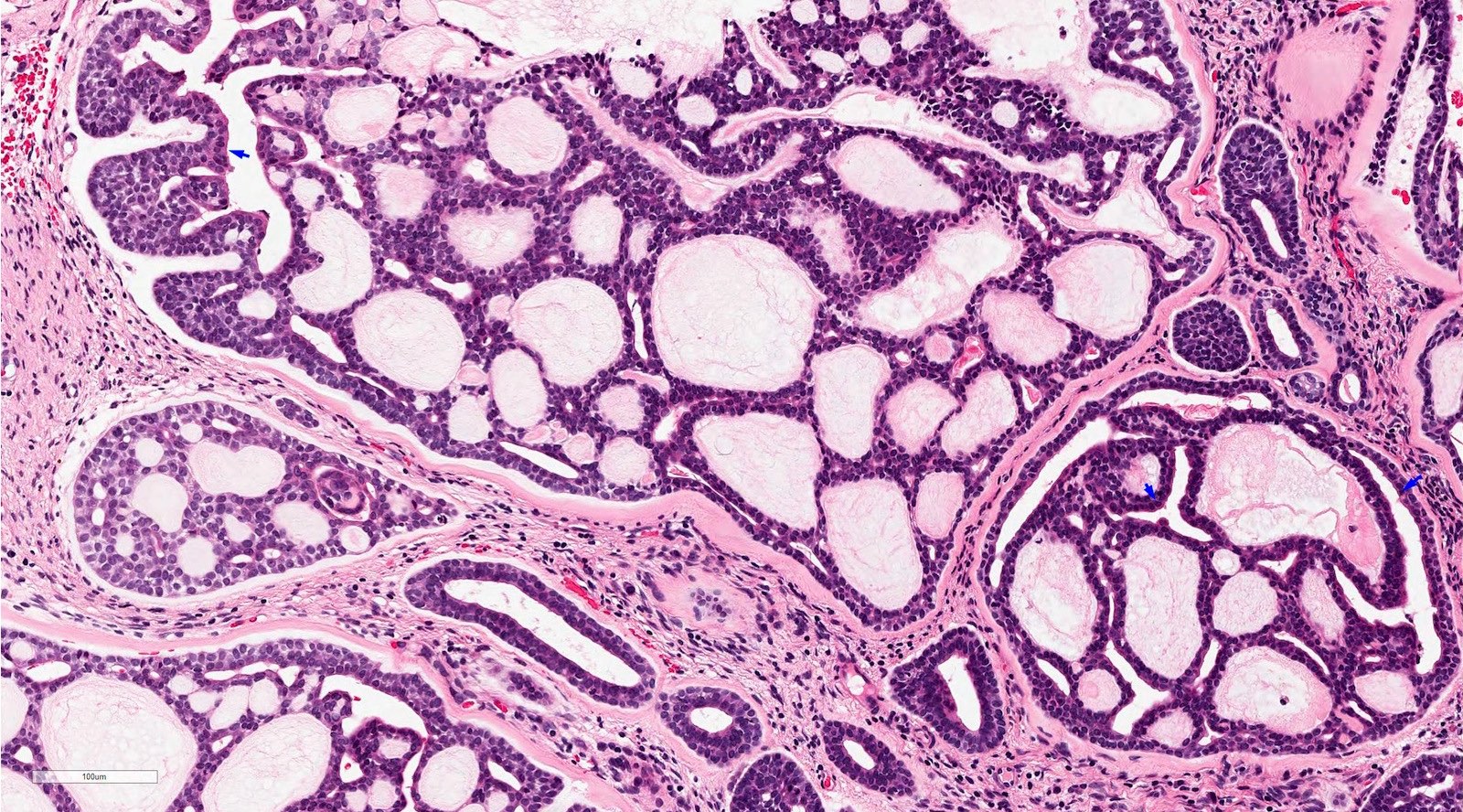
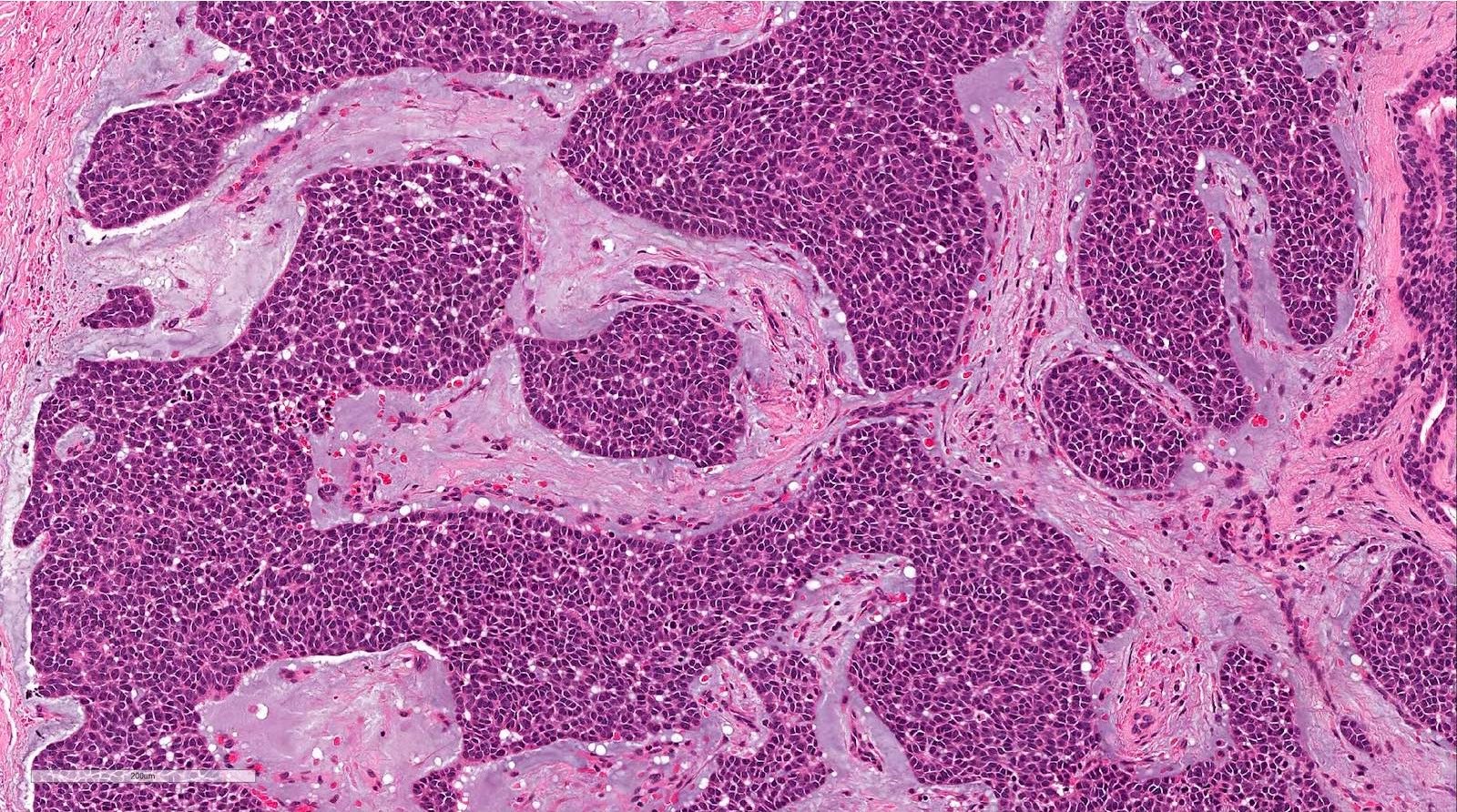
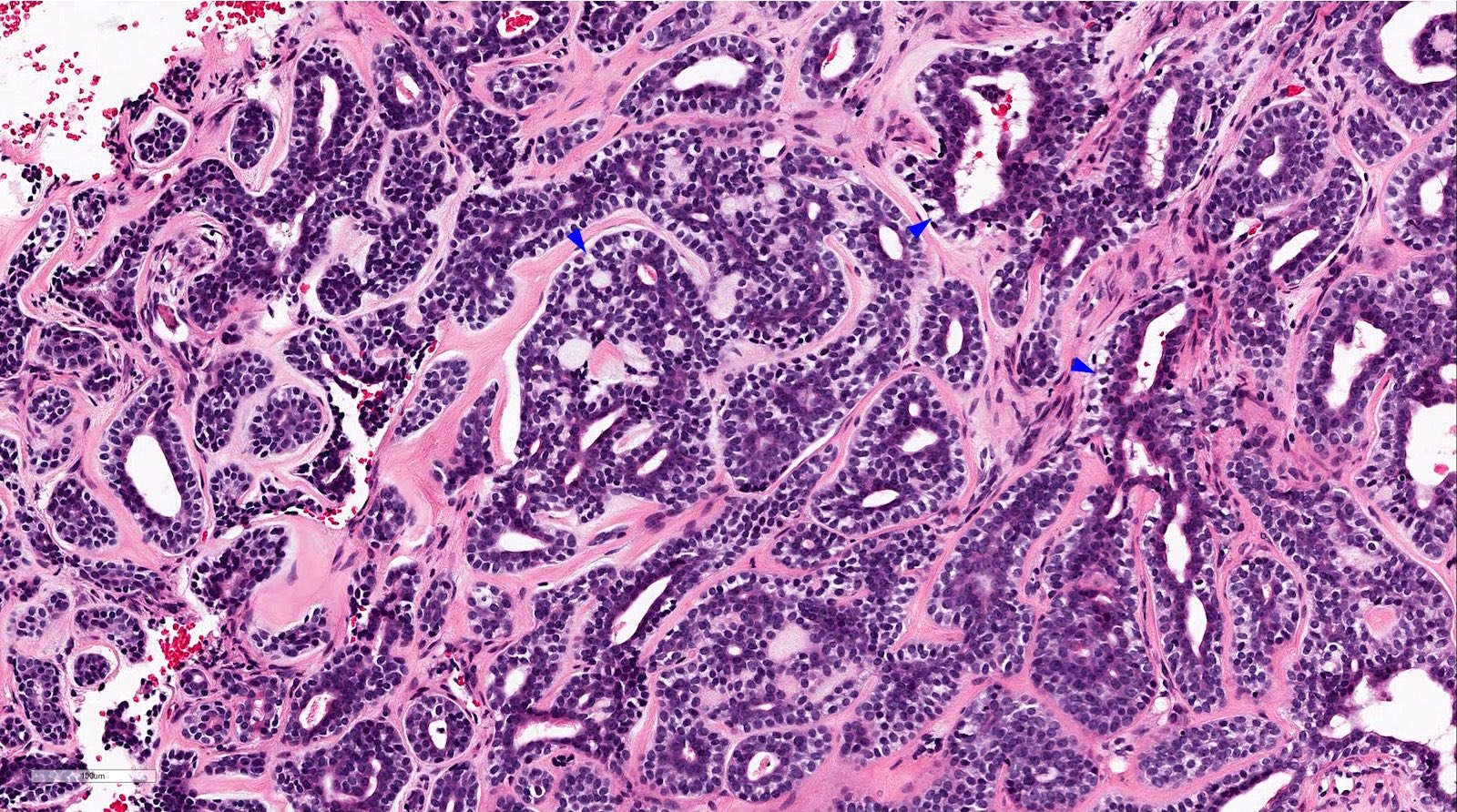
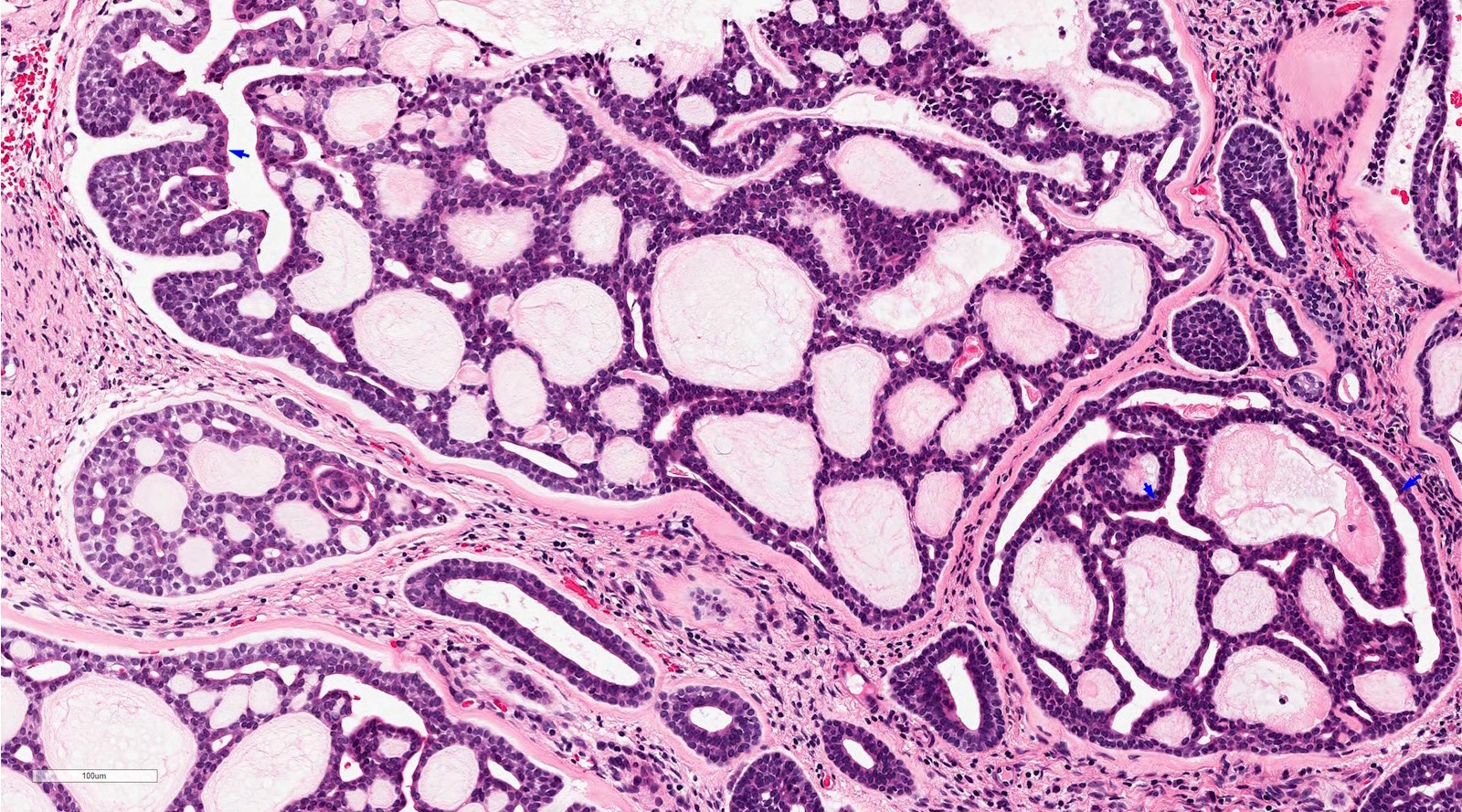
Microscopic (histologic) description
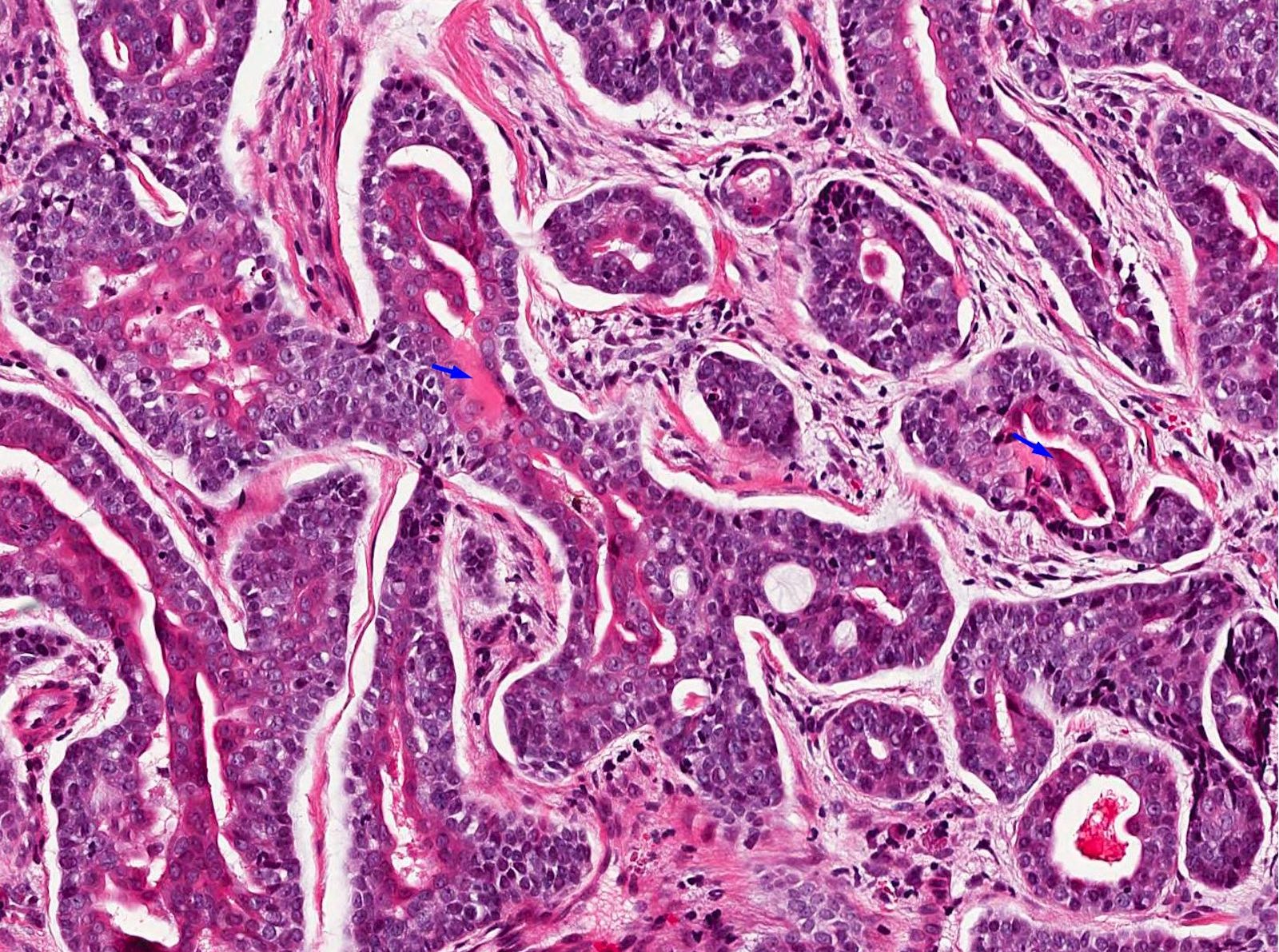
- Biphasic salivary gland tumor, composed of ductal and myoepithelial cells
- Myoepithelial cells have dark angulated nuclei and scanty cytoplasm, giving a basaloid appearance
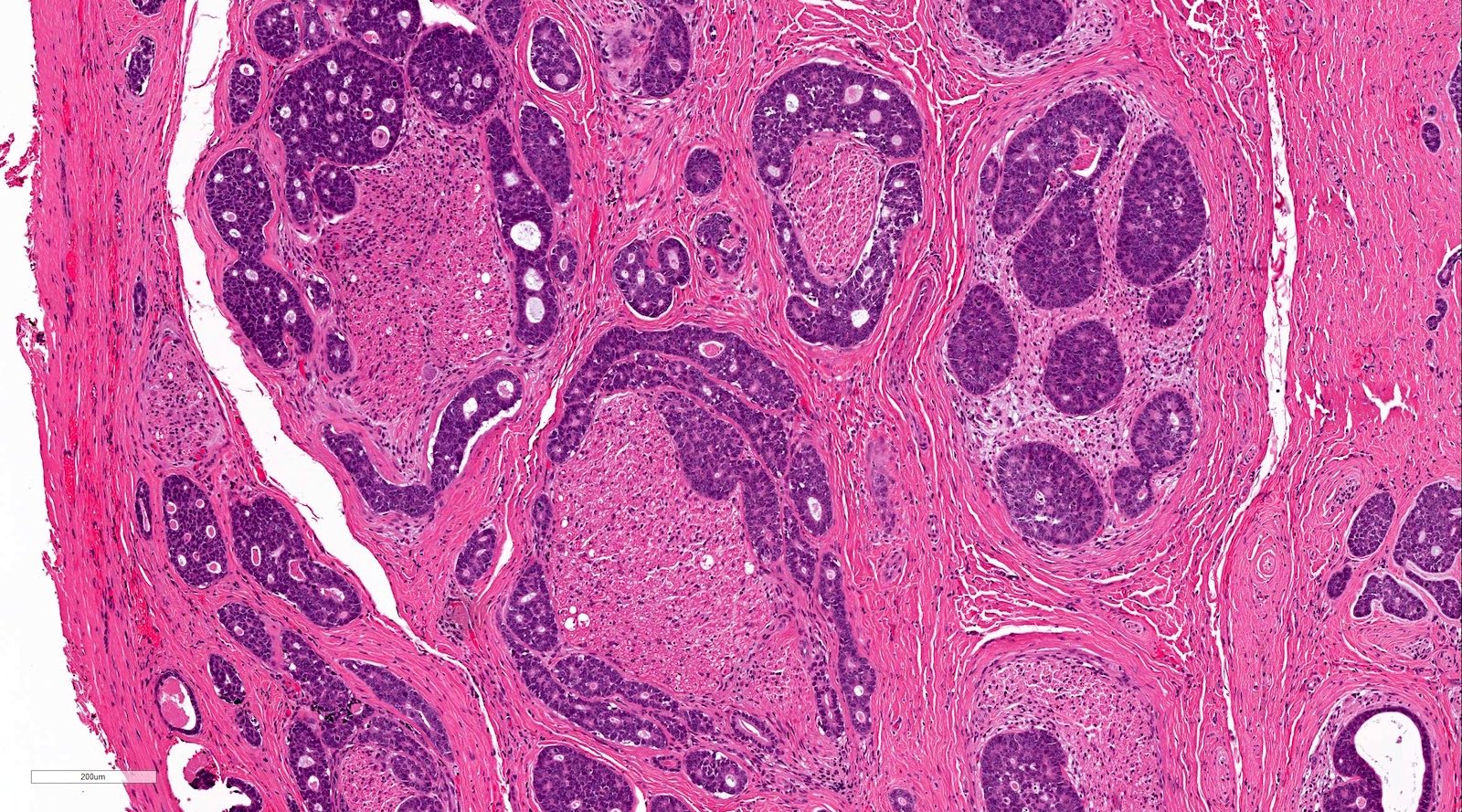
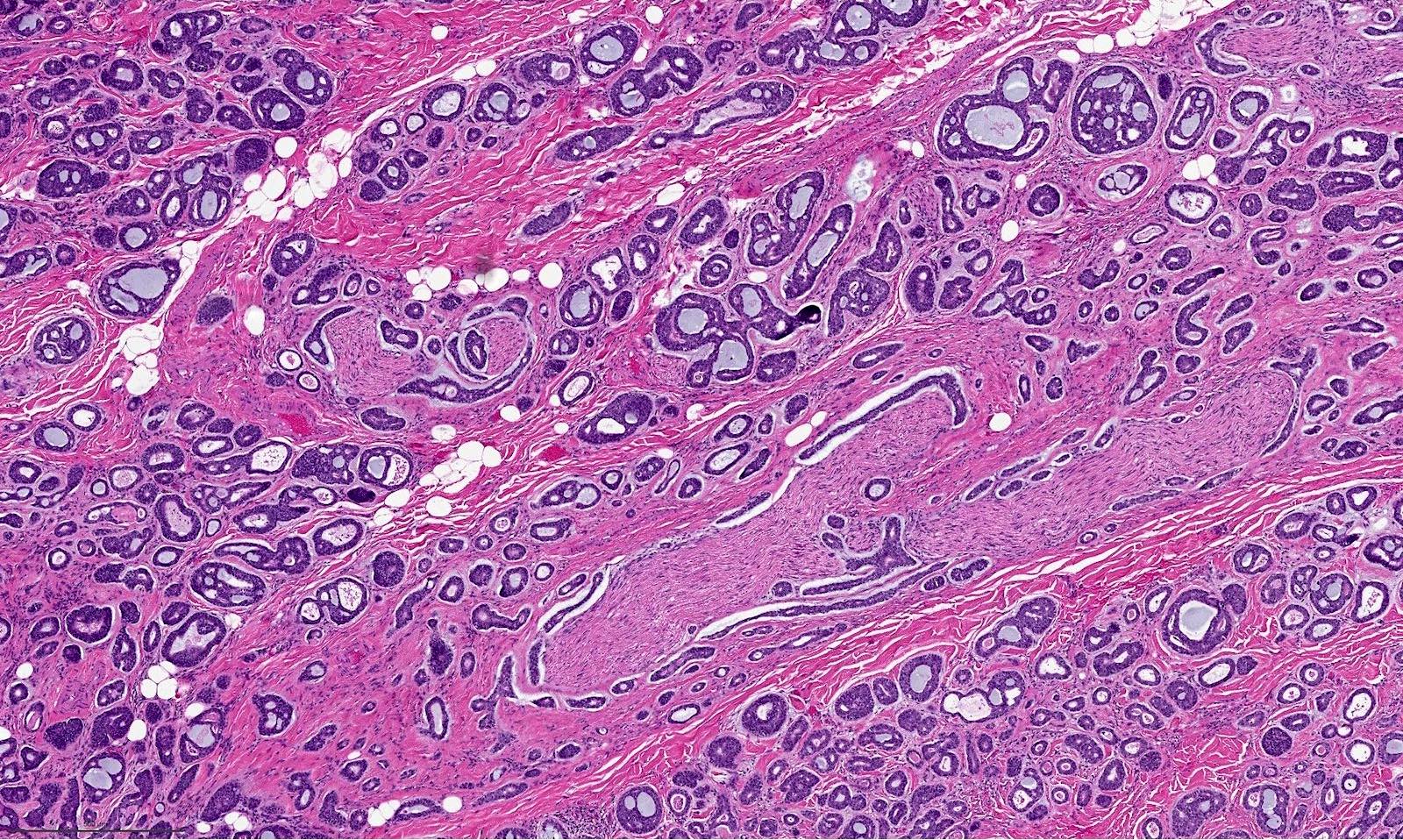
- Tubular, cribriform and solid architecture
- Tubular pattern contains simple tubules composed of inner ductal and outer myoepithelial cells
- Cribriform pattern is composed of predominantly myoepithelial cells with myxoid or hyalinized globules
- Scattered ductal elements may be seen within the cribriform area
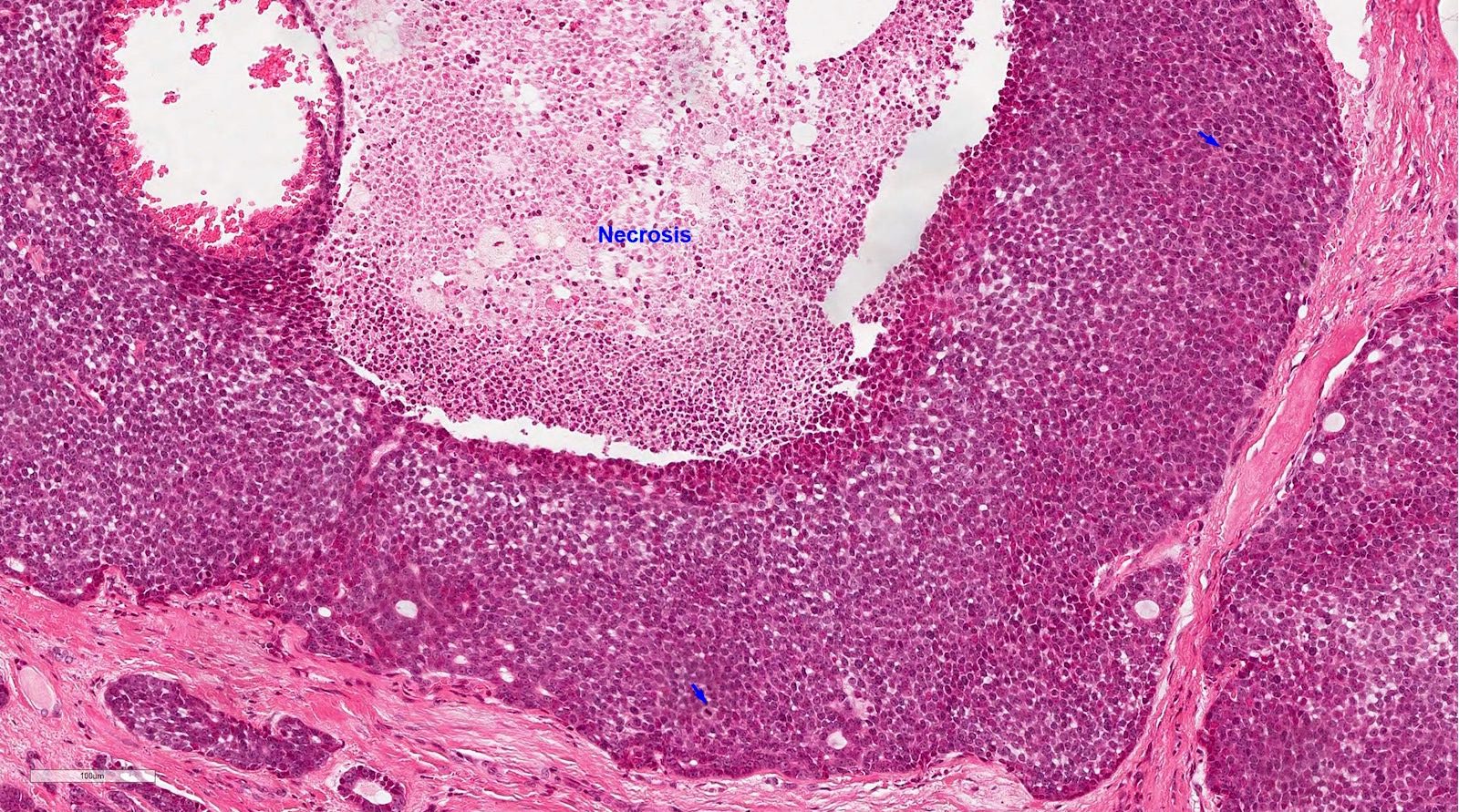
- Solid pattern is solid nests composed of sheets of basaloid cells
- Perineural invasion is frequent
- High grade transformation can be seen in a small number of cases, defined as comedo type tumor necrosis, frequent mitoses (often > 10 per 10 high power fields) and marked nuclear atypia; high grade transformation is associated with high risk of lymph node metastasis, distant metastasis and disease related death (Am J Surg Pathol 2007;31:1683)
- Other rare features that may present occasionally include:
- Focal squamous metaplasia / differentiation, especially in cases with high grade transformation (Am J Surg Pathol 2007;31:1683, Am J Surg Pathol 2017;41:1422)
- Areas in which myoepithelial cells show clear cell changes, resembling epithelial myoepithelial carcinoma (Am J Surg Pathol 2018;42:319)
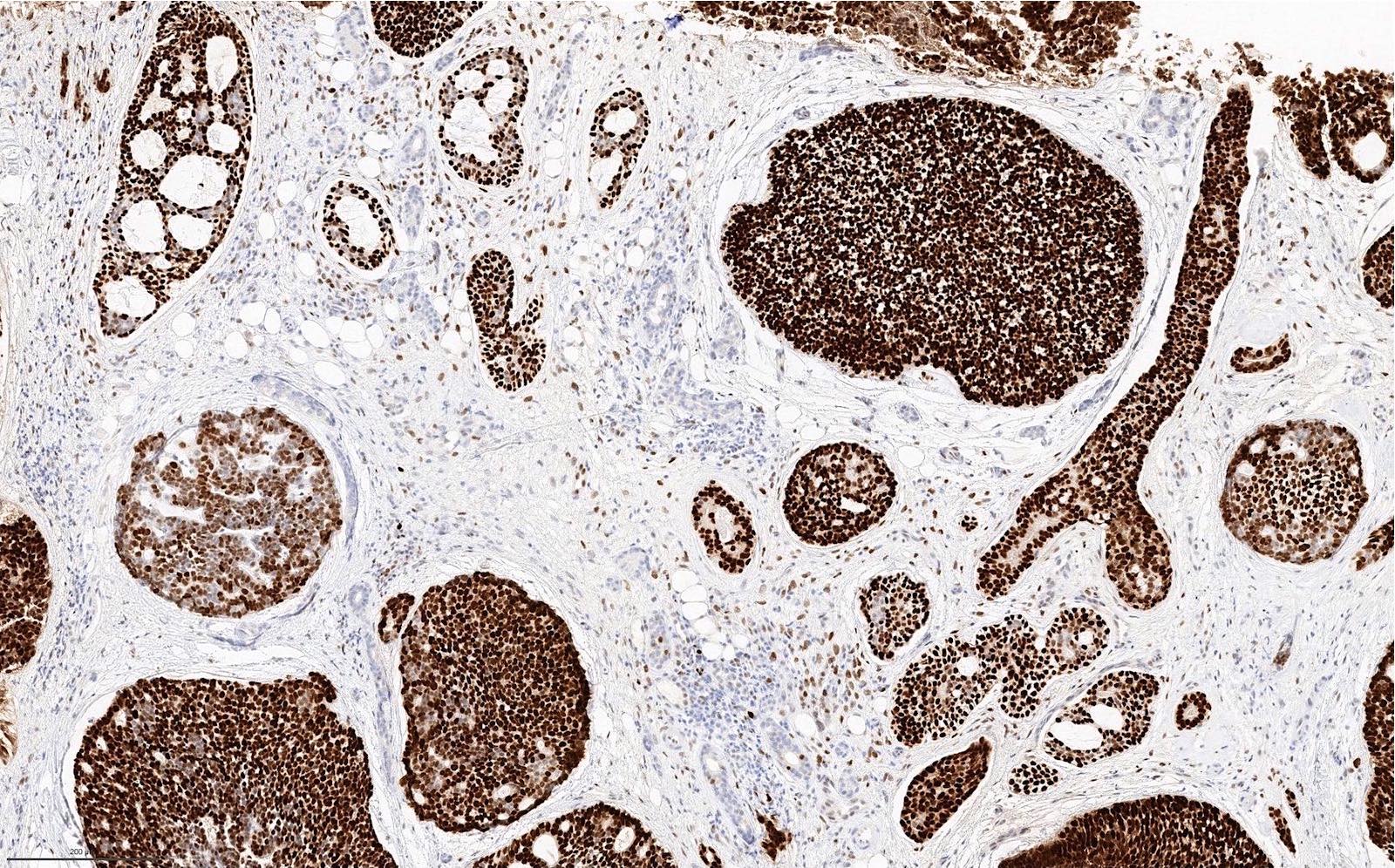
Microscopic (histologic) images
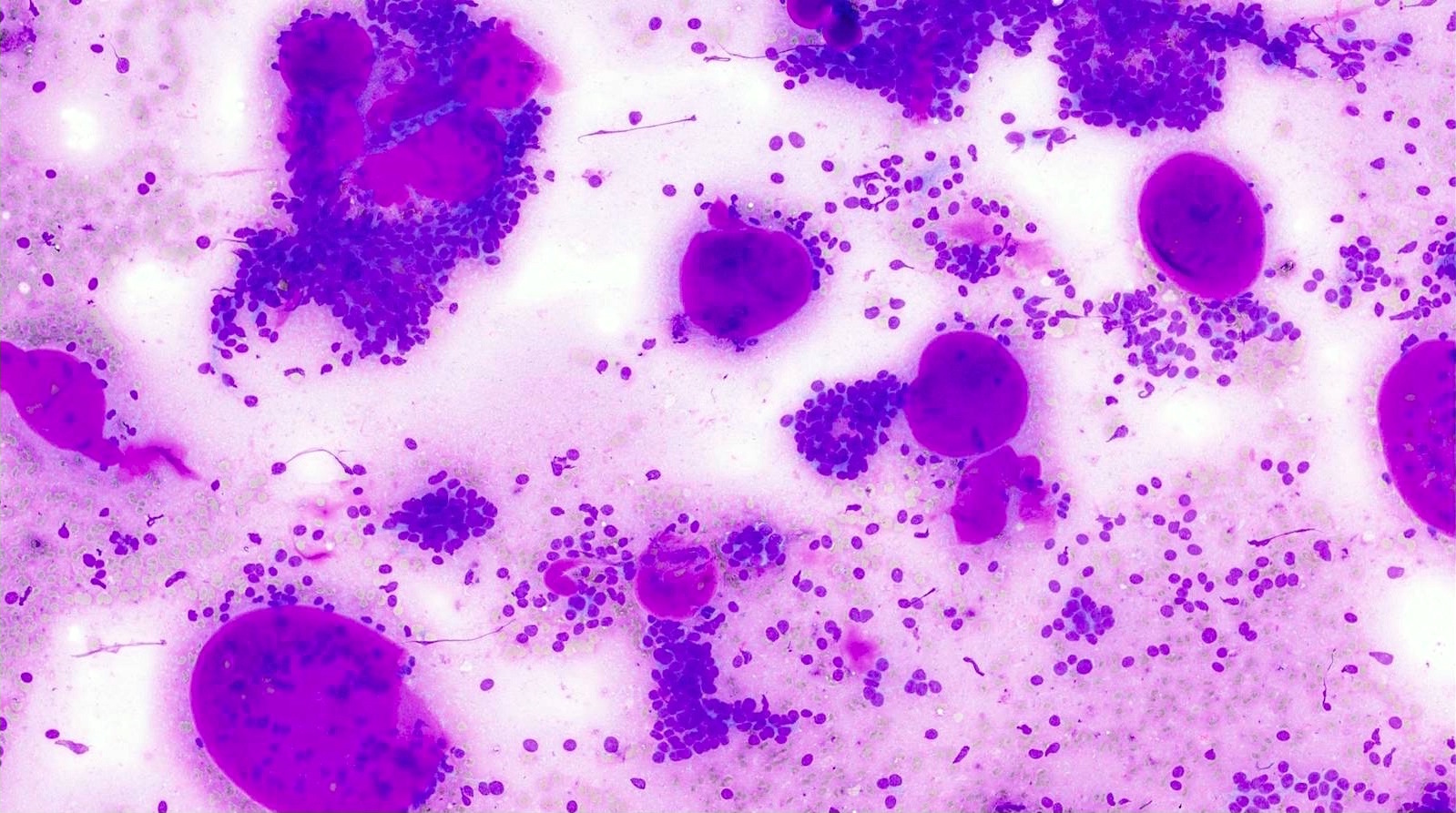
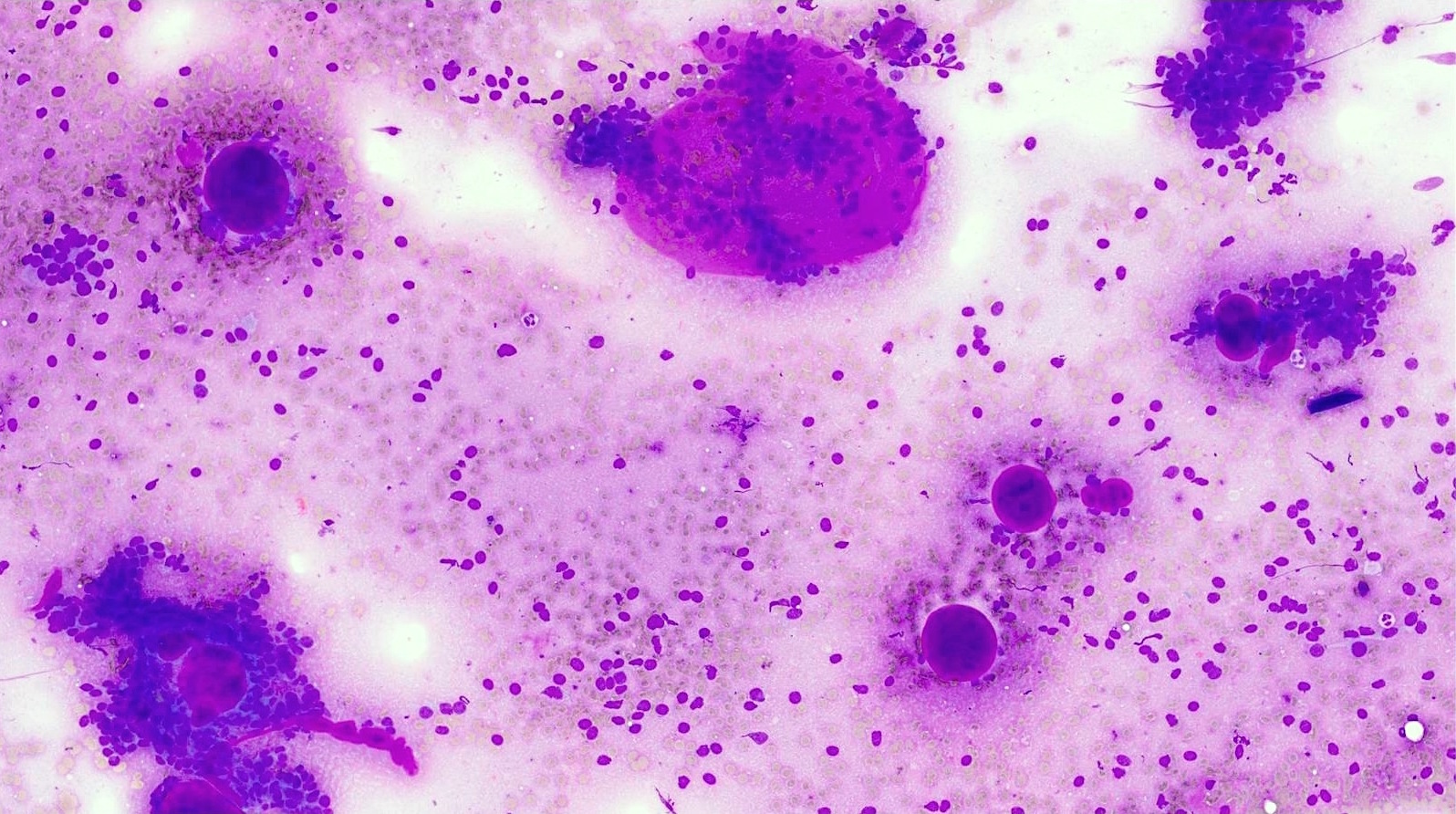
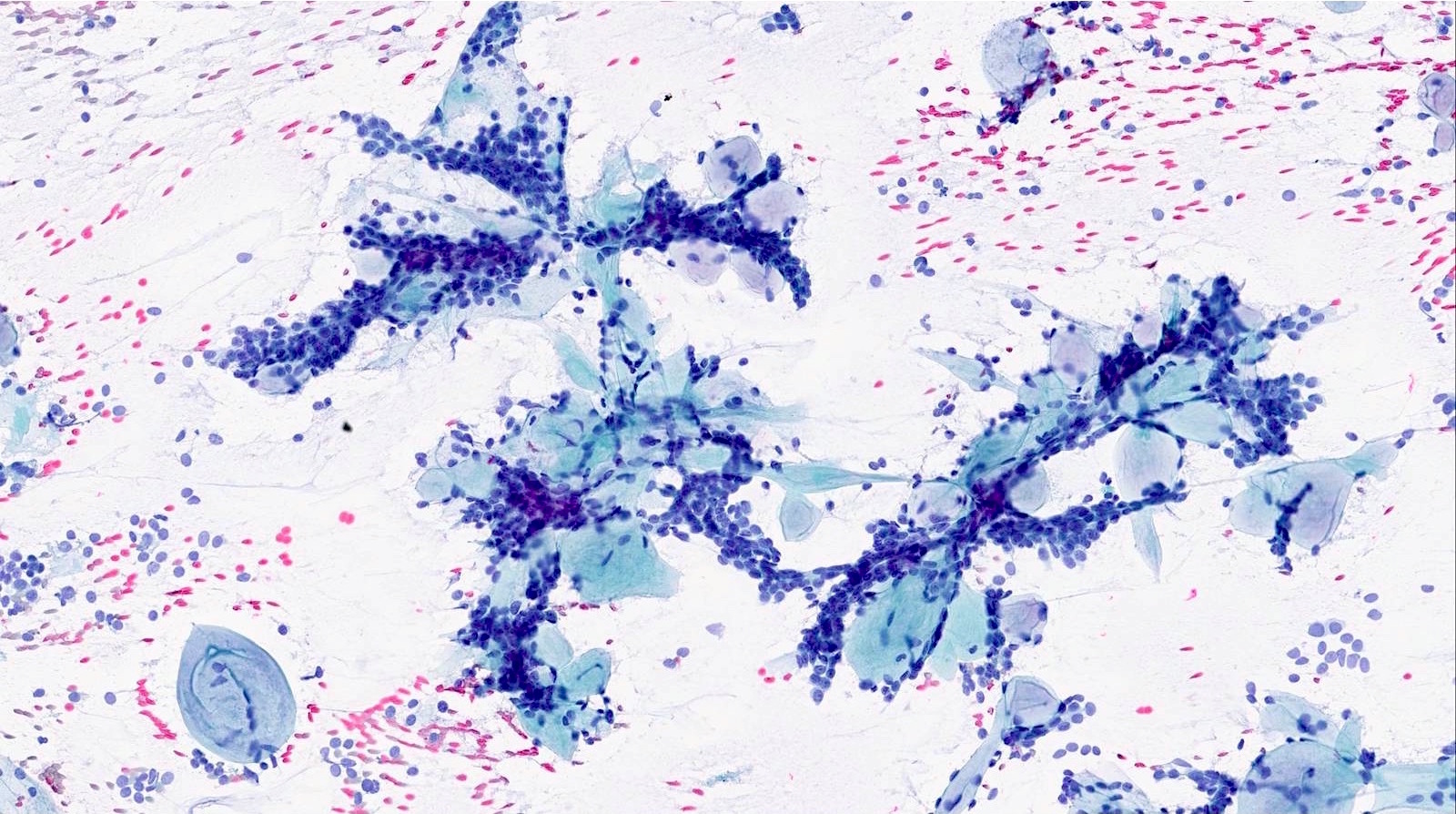
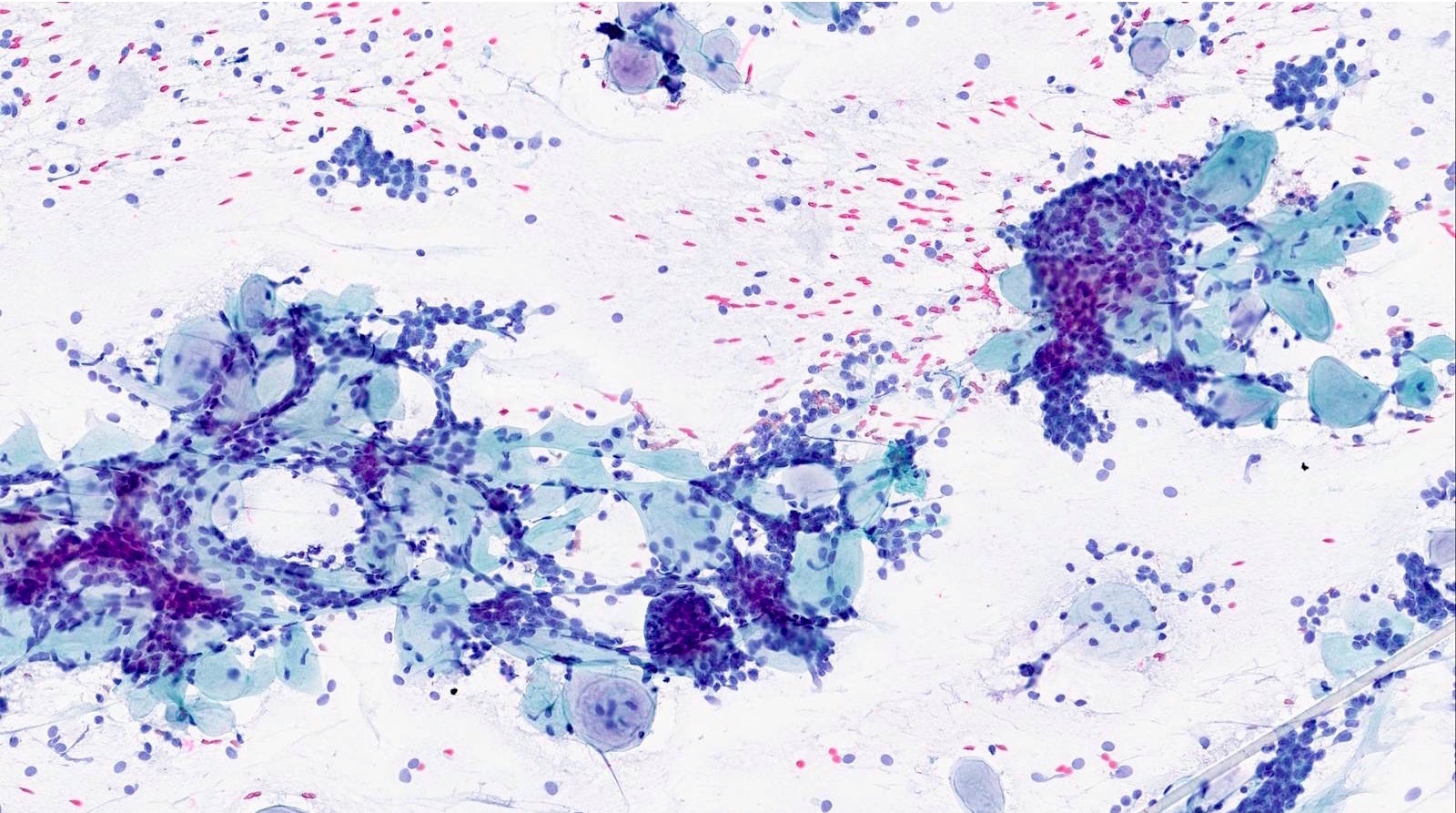
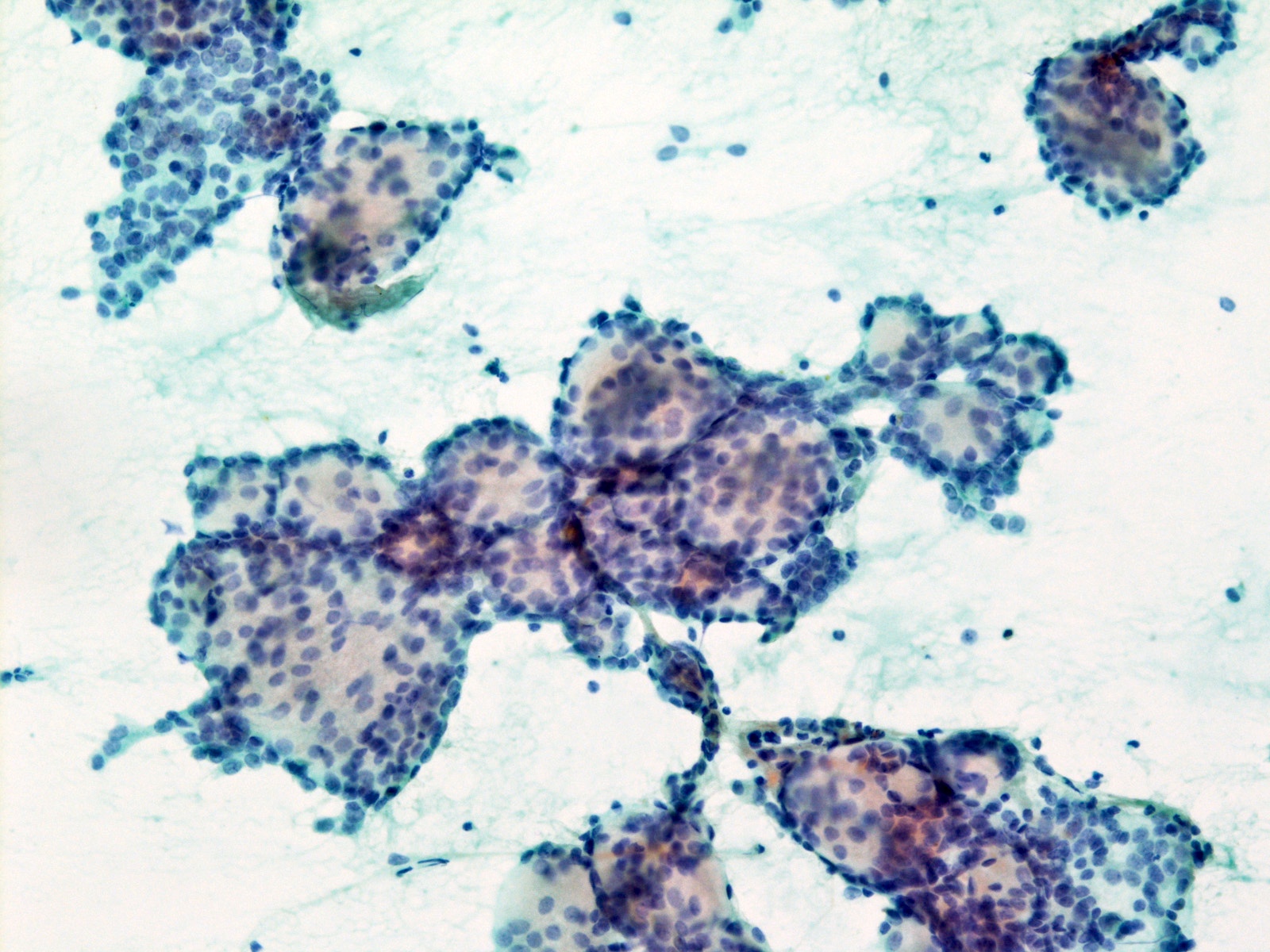
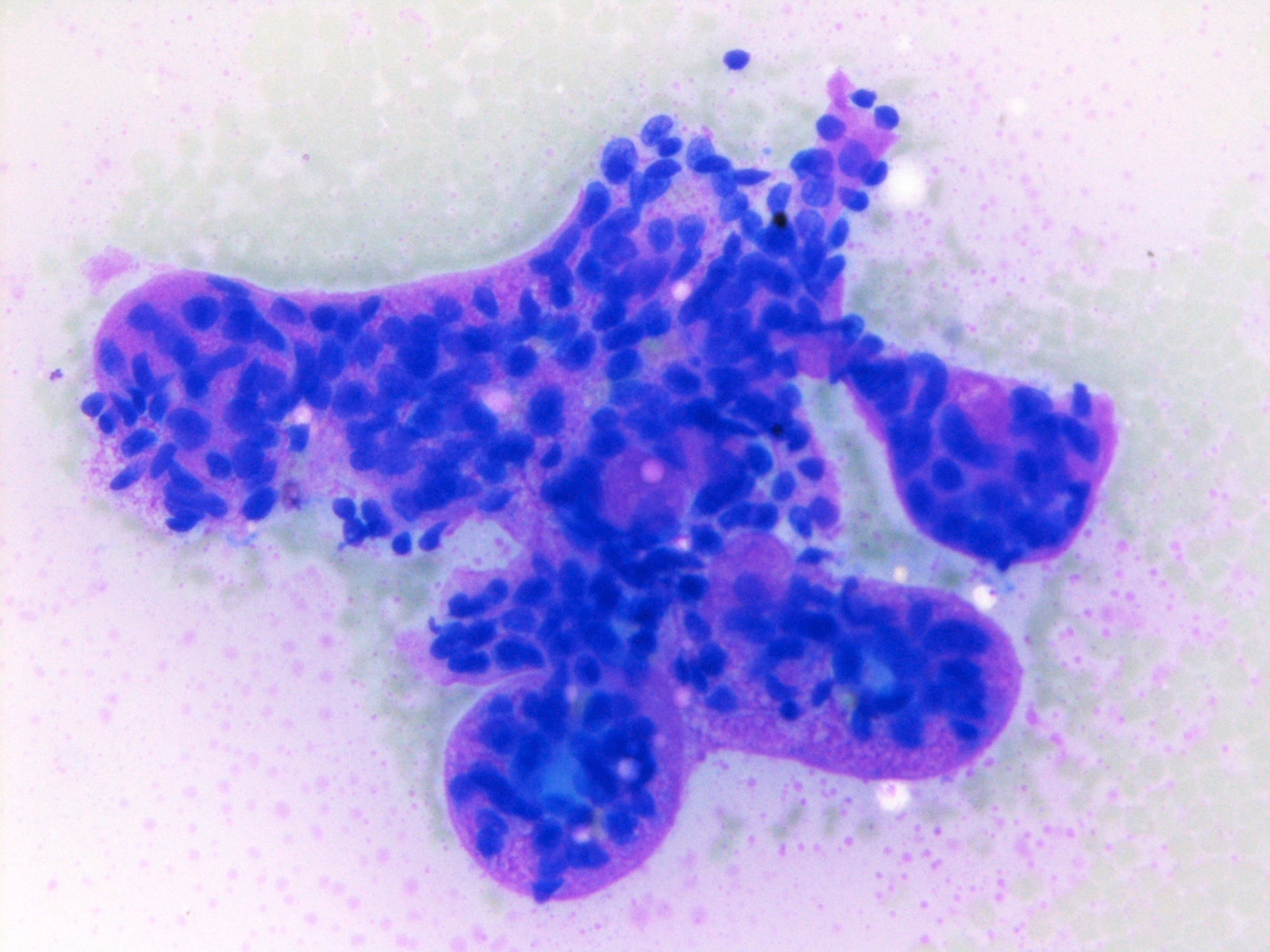
Cytology description
- Matrix containing and basaloid
- Diff-Quik stained smears: metachromatic matrix spheres with sharply defined border (hyaline globules) surrounded by basaloid tumor cells
- Uniform basaloid cells with scant cytoplasm, oval to angulated hyperchromatic nuclei and indistinct nucleoli
- Various architecture patterns, including microcystic, tubular and syncytial clusters
- Characteristic extracellular hyaline globules or cylinders of acellular metachromatic stroma with sharp borders best seen on Romanowsky type stain
- Marked cytologic atypia and necrosis in cases with high grade transformation
Cytology images
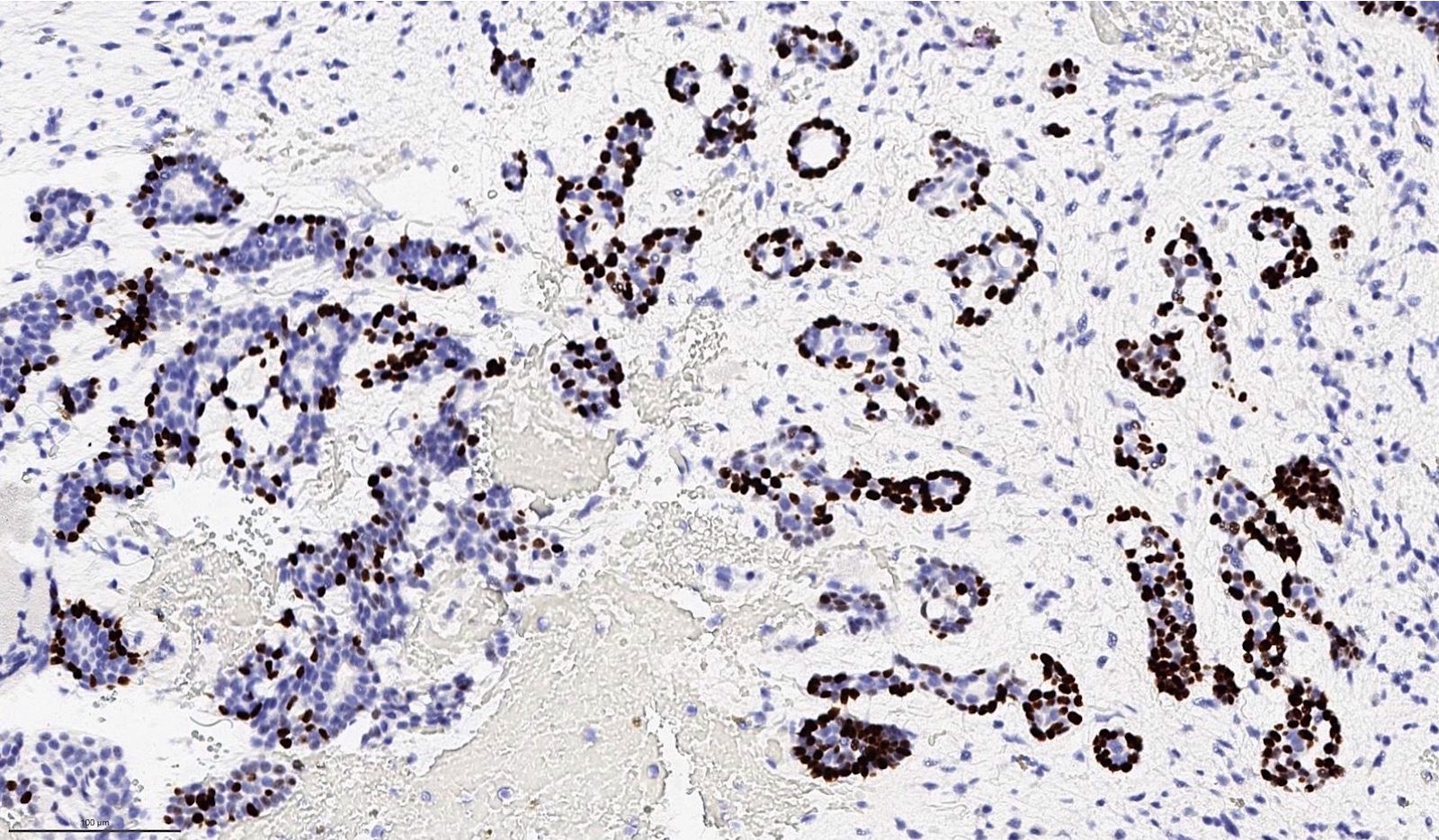
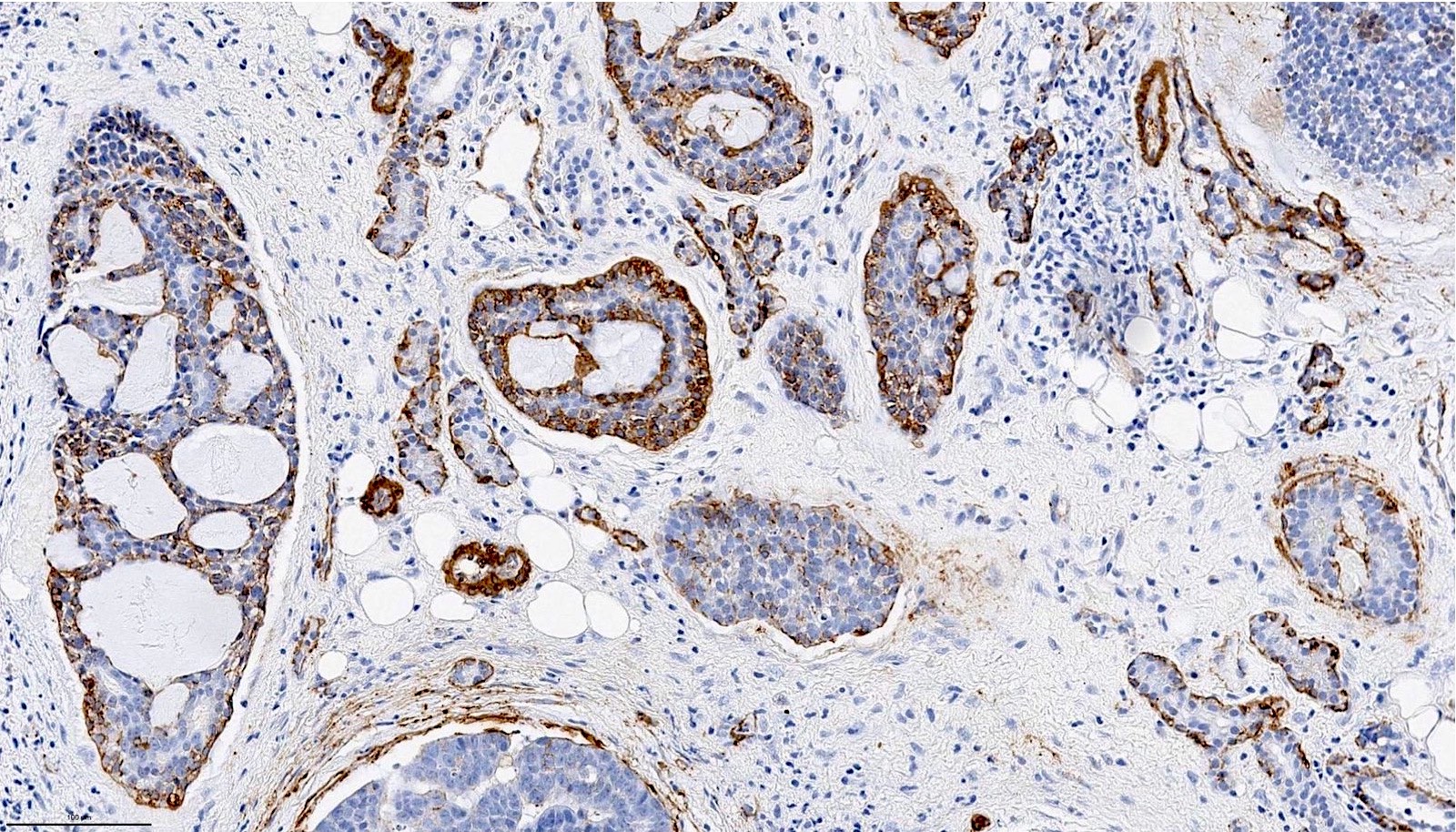
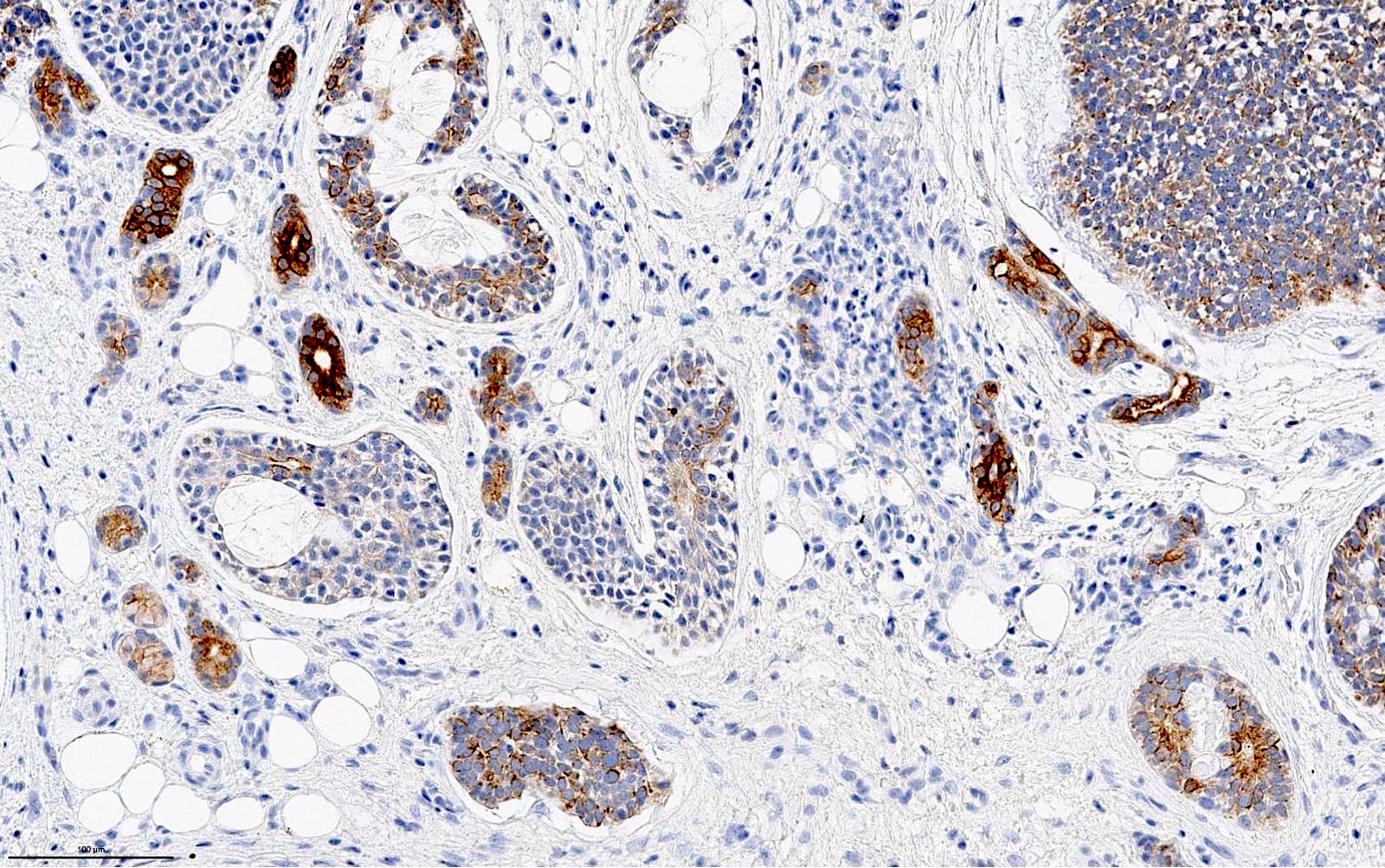
Positive stains
- Ductal component is typically positive for CK7 and CAM 5.2
- Myoepithelial component is positive for myoepithelial markers, e.g. SMA, S100, calponin, p40, p63, GFAP and cytokeratins
- Other positive stains: c-KIT (CD117)
- MYB overexpression is a sensitive but nonspecific immunomarker for adenoid cystic carcinoma (Am J Surg Pathol 2017;41:1422)
Molecular / cytogenetics description
- Absence of high risk HPV bby DNA or RNA in situ hybridization
- 60 - 90% have characteristic and diagnostic fusion involving MYB, MYBL1 or NFIB gene, the most common being t(6,9) MYB-NFIB fusion (Nat Genet 2013;45:791, Proc Natl Acad Sci U S A 2009;106:18740, Cancer Discov 2016;6:176)
- Additional mutations involving FGF-IGF-PI3K pathway (in 30%) and chromatin state regulators (e.g. SMARCA2, CREBBP and KDM6A) are reported (Nat Genet 2013;45:791)
- Although commonly overexpresses c-KIT by immunohistochemistry, it is not associated with c-KIT mutation
Sample pathology report
- Left parotid, parotidectomy:
- Adenoid cystic carcinoma, solid, cribriform and tubular pattern (see synoptic report)
- Comment: Solid component accounts for 20% of total tumor volume.
Differential diagnosis
- Epithelial myoepithelial carcinoma:
- Also biphasic with ductal and myoepithelial differentiation
- Typically contains compact branching tubules (adenoid cystic carcinoma contains simple tubules)
- Generally lacks cribriform growth pattern: if present, cribriform pattern is often very focal
- Papillocystic architecture may be seen (typically absent in adenoid cystic carcinoma)
- Contains clear myoepithelial cells (adenoid cystic carcinoma contains myoepithelial cells with dark angulated nuclei and scanty cytoplasm)
- Characterized by HRAS mutation; lacks fusions involving MYB, NFIB or MYBL1
- Basal cell adenocarcinoma:
- Also biphasic and basaloid
- Trabecular, tubular and solid growth and usually lacks cribriform growth (adenoid cystic carcinoma lacks trabecular growth)
- Prominent peripheral palisading and may contain areas with squamoid eddies
- Characterized by mutation of Wnt / beta catenin pathway leading to abnormal nuclear accumulation of beta catenin by immunohistochemistry; lacks fusions involving MYB, NFIB or MYBL1
- Polymorphous adenocarcinoma:
- Also may show tubular, cribriform and solid growth
- May have other growth patterns, e.g. single files, trabecular or papillary architecture
- Shows cytologic monotony with only one type of tumor cells
- Nuclei contain open chromatin resemble nuclei of papillary thyroid carcinoma
- Typically p63 positive / p40 negative, whereas adenoid cystic carcinoma is typically positive for both p63 and p40 (Am J Surg Pathol 2014;38:257)
- HPV related multiphenotypic sinonasal carcinoma:
- Also can affect sinonasal tract and show similar morphology and expression
- May have surface dysplasia
- Positive for high risk HPV; negative for MYB-NFIB fusion
- Squamous cell carcinoma:
- Basaloid squamous cell carcinoma and HPV+ oropharyngeal squamous cell carcinoma may contain adenoid cystic carcinoma-like areas
- Typically shows more pleomorphism, is negative for MYB-NFIB fusion, is diffusely positive for squamous markers (p40, p63 and CK5/6), is negative for myoepithelial markers (S100, calponin and SMA) and may be HPV+
Board review style question #1
- A parotid tumor is resected and the H&E is shown. Which of the following statements is true?
- It has an excellent prognosis with 5% risk of recurrence following complete resection of the primary tumor
- It is characterized by point mutation involving MYB gene
- Solid pattern is associated with adverse clinical outcome
- The most common site of this tumor is the parotid gland, followed by submandibular gland
Board review style answer #1
C. Solid pattern is associated with adverse clinical outcome
Comment Here
Reference: Adenoid cystic carcinoma
Comment Here
Reference: Adenoid cystic carcinoma
Board review style question #2
- What is the most common molecular alteration in adenoid cystic carcinoma?
- t(6,9) MYB-NFIB fusion
- t(11,19) MAML2-CRTC1 fusion
- t(12,15) ETV6-NTRK3 fusion
- t(12,22) ATF1-EWSR1 fusion
Board review style answer #2
Board review style question #3
Board review style answer #3
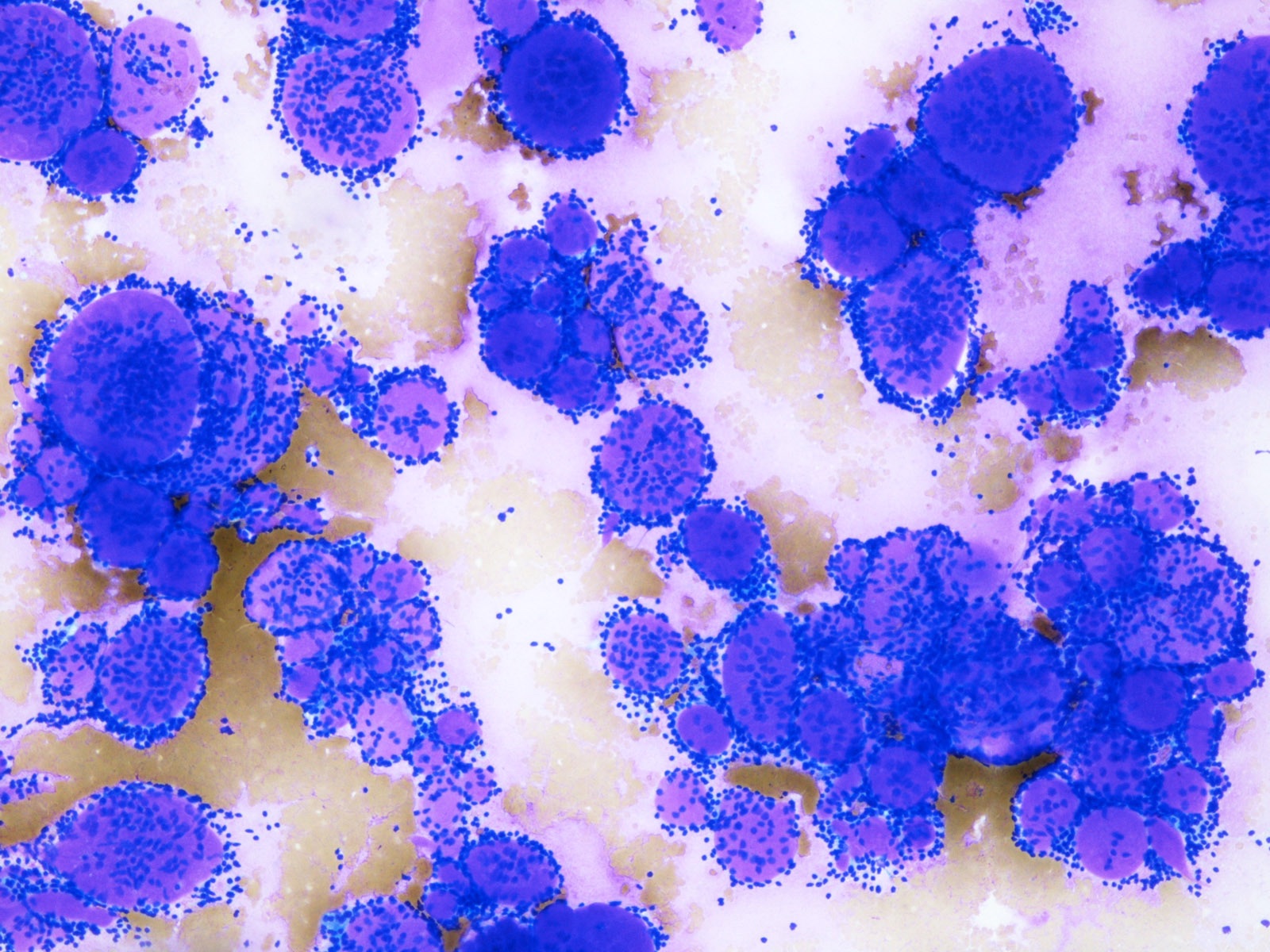
B. Adenoid cystic carcinoma
Basaloid tumor cells with prominent hyaline globules arranging in cribriform pattern are characteristic for an adenoid cystic carcinoma.
Comment Here
Reference: Adenoid cystic carcinoma
Basaloid tumor cells with prominent hyaline globules arranging in cribriform pattern are characteristic for an adenoid cystic carcinoma.
Comment Here
Reference: Adenoid cystic carcinoma