Table of Contents
Definition / general | Essential features | Terminology | Physiology | Diagrams / tables | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kyle D, Schwartz L. Anatomy & histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusnormal.html. Accessed April 26th, 2024.
Definition / general
- Pear shaped organ which serves as physiologic site of implantation for fertilized egg and undergoes changes to support subsequent placental attachment and embryonic / fetal development
Essential features
- Mucosal component (endometrium) is hormonally responsive and undergoes physiologic and morphologic changes throughout the menstrual cycle
Terminology
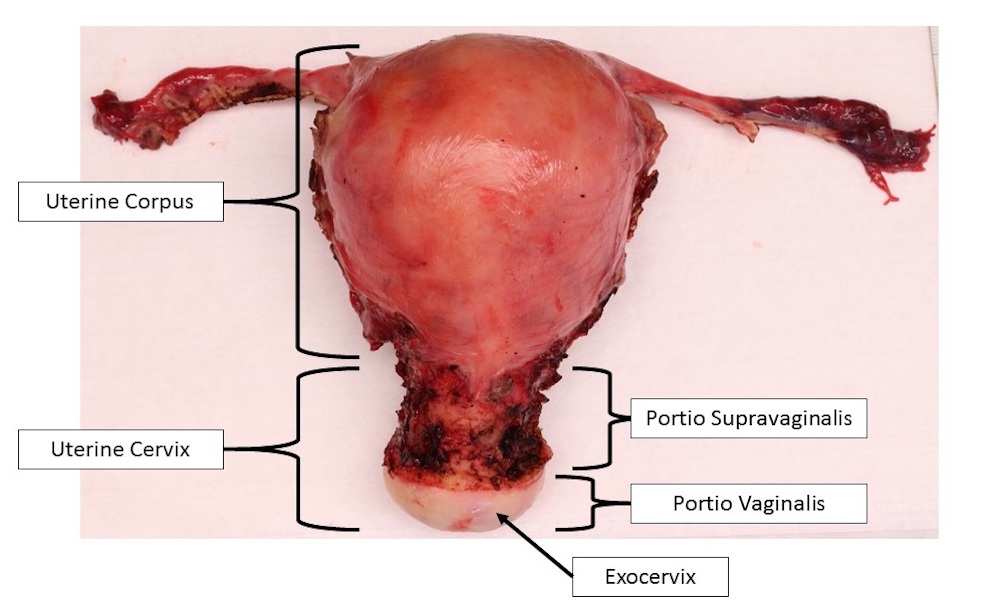
- Anatomic divisions
- Uterine corpus: main portion of the uterus comprising the upper two - thirds, which houses the endometrial lined cavity
- Uterine cervix: lower one - third of uterus, which attaches to vaginal canal; see Histology
- Fundus: domed superior portion of uterus located superior to points of fallopian tube insertion
- Cornua: lateral portions of uterine corpus; sites of fallopian tube insertion
- Isthmus (lower uterine segment): inferior portion of corpus, which connects to the cervix
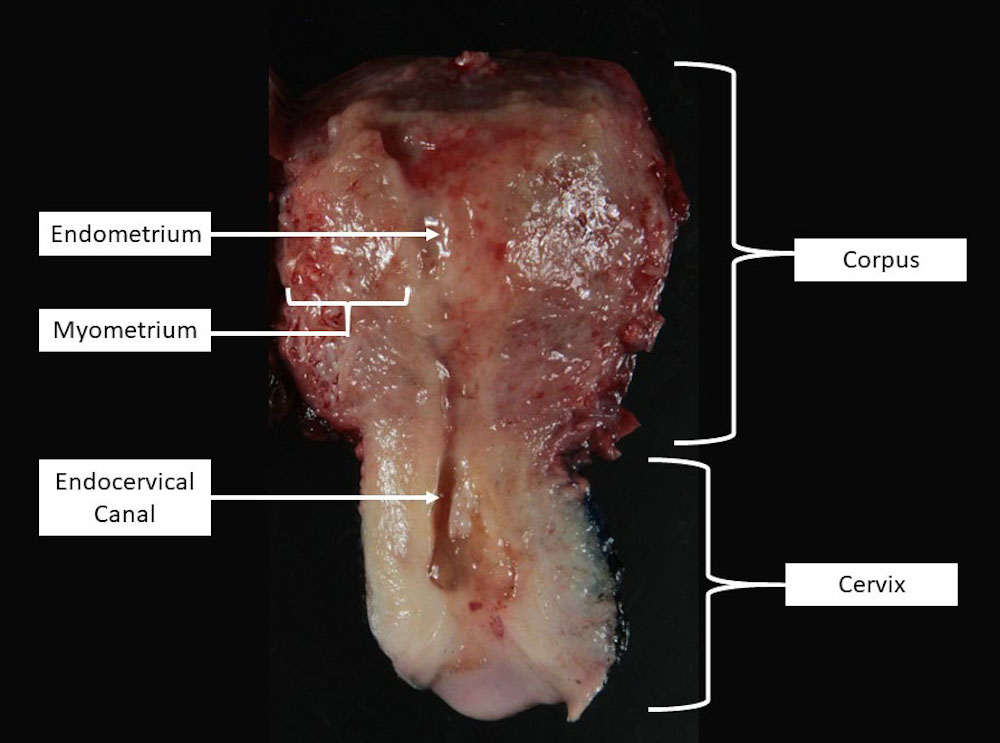
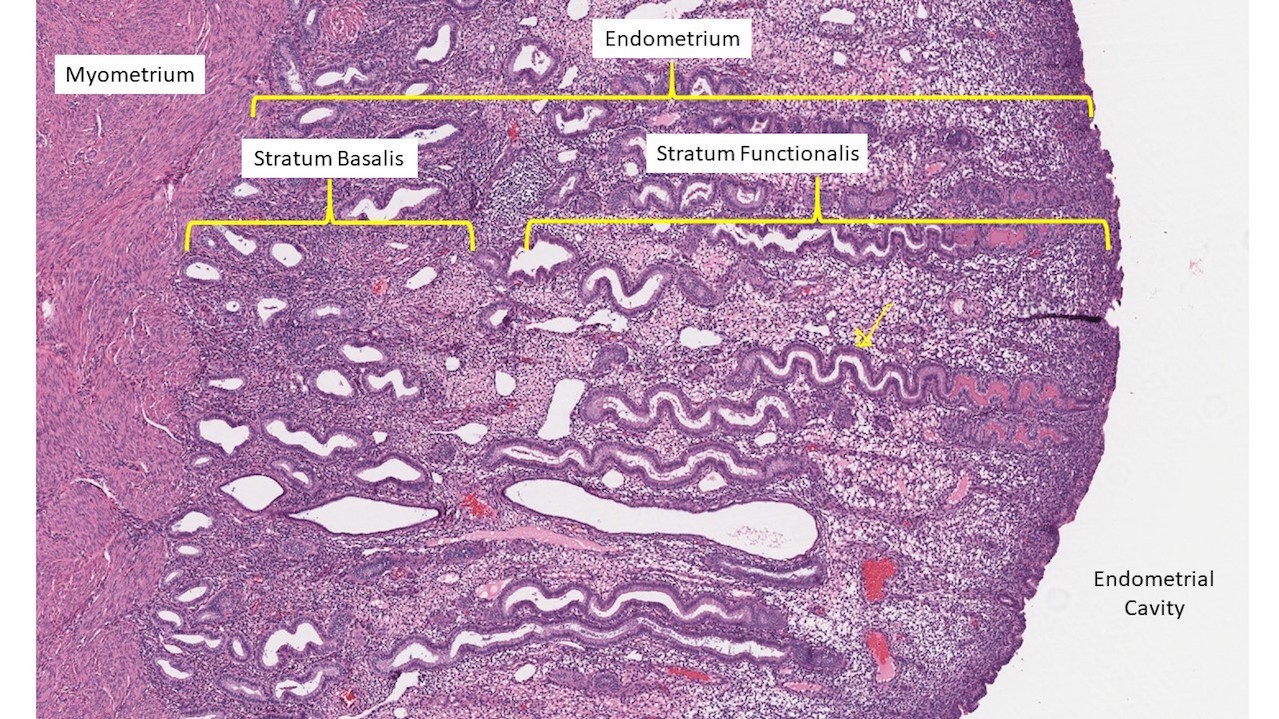
- Histologic divisions
- Endometrium: mucosal layer lining the uterine cavity composed of endometrial glands and specialized stroma; blood supplied by spiral arteries
- Stratum basalis: deep layer of endometrium, which is minimally hormone responsive and serves to replenish the stratum functionalis following menses
- Stratum functionalis: hormone responsive superficial layer of endometrium; undergoes functional and morphologic changes throughout menstrual cycle; shed during menses
- Myometrium: structural wall of uterus composed primarily of smooth muscle
- Serosa: thin, outermost layer of uterus consisting of loose connective tissue and mesothelium
- Endometrium: mucosal layer lining the uterine cavity composed of endometrial glands and specialized stroma; blood supplied by spiral arteries
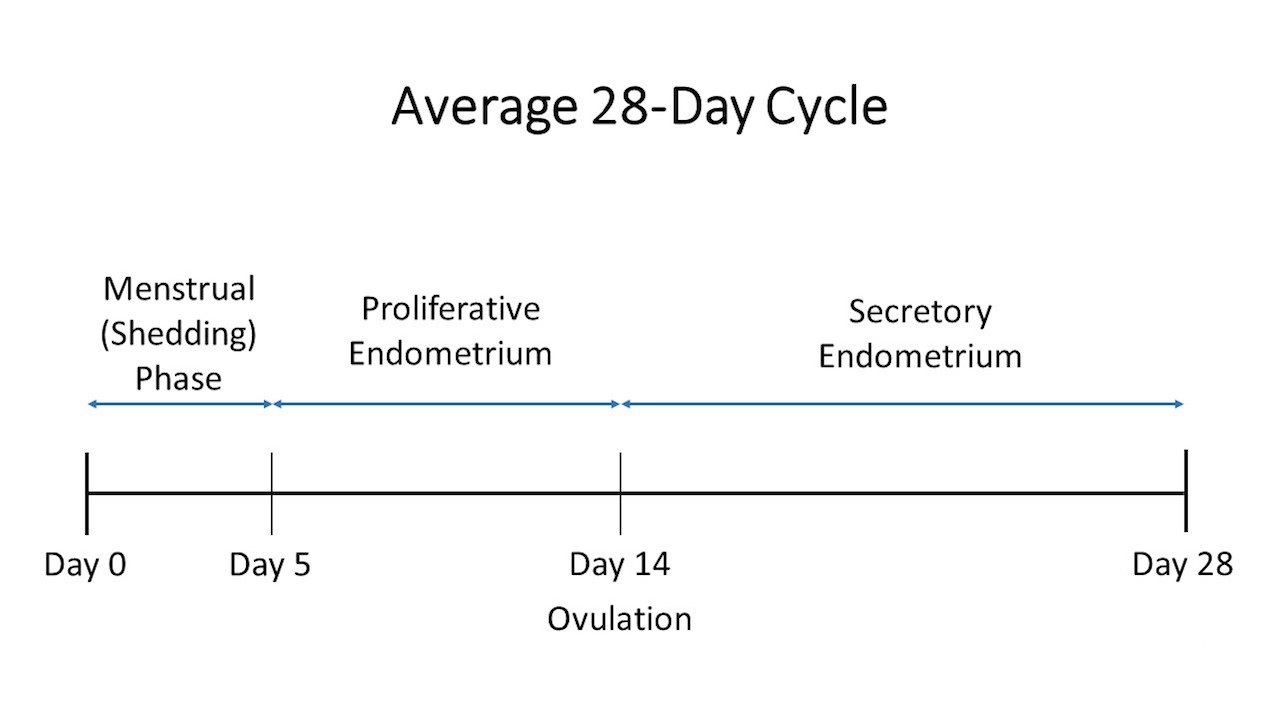
Physiology
- In infants and children, the endometrium is functionally inactive
- Menarche:
- First occurrence of menstruation (J Pediatr Adolesc Gynecol 2018;31:557)
- In gestational aged women, the endometrium undergoes hormonally driven changes throughout the menstrual cycle (Endotext: The Normal Menstrual Cycle and the Control of Ovulation [Accessed 11 June 2020])
- Menstrual phase (days 0 - 5):
- Estrogen and progestin levels fall in the absence of implantation of a fertilized egg, resulting in breakdown of endometrial stroma
- Stratum functionalis is shed; spiral arteries constrict to minimize blood loss
- Proliferative phase (days 6 - 14):
- Stratum functionalis is regenerated by cells from stratum basalis
- Primarily driven by increasing estrogen levels
- Corresponds to follicular phase of cycle in ovary
- Ends at approximately day 14 when ovulation occurs
- Secretory phase (days 15 - 28):
- Stratum functionalis undergoes changes to support implantation in the event of fertilization
- Glands become convoluted and endometrial cells increase glycogen stores
- Primarily driven by progestin
- Corresponds to luteal phase of cycle in ovary
- Menstrual phase (days 0 - 5):
- Following menopause, the endometrium becomes inactive and may eventually undergo atrophy
- Pregnancy changes
- Endometrium retains secretory phenotype and stroma becomes decidualized in response to progestins (detailed in Microscopic description section)
- Myometrium undergoes mechanoadaptation to allow distension and accommodation of developing fetus (J Cell Mol Med 2008;12:1360)
Gross description
- Pear shaped, smooth external surface
- Anatomic position within the pelvic cavity between the urinary bladder (anterior) and rectum (posterior)
- Anterior portion can be identified by a higher peritoneal reflection, due to location of the bladder in vivo (J Clin Pathol 1993;46:388)
- Hysterectomy specimens are often opened in the coronal plane by inserting a probe into the external cervical os and cutting along the probe to reveal the endometrial cavity
- Endometrial cavity is shaped like an inverted triangle when viewed in the coronal plane
Microscopic (histologic) description
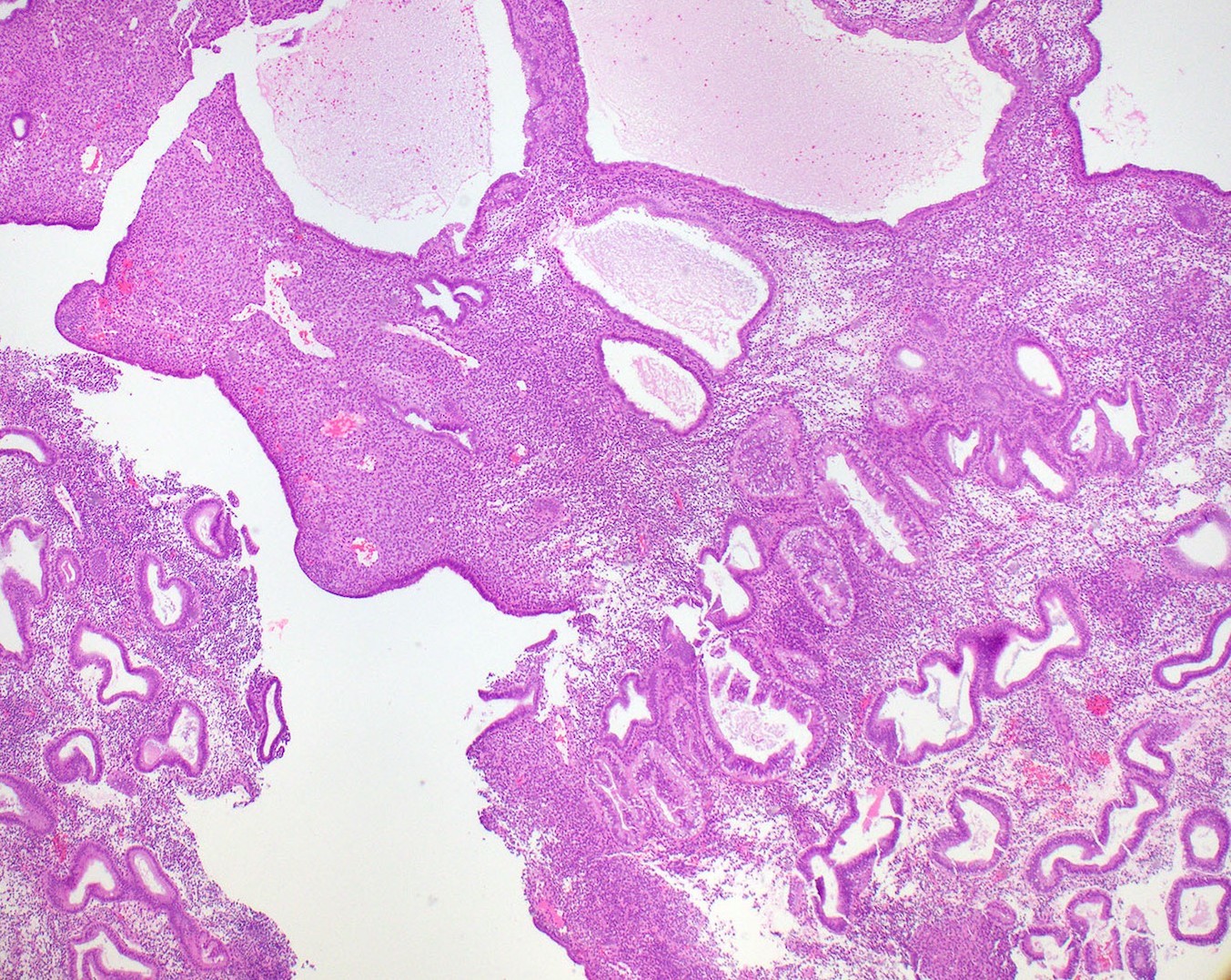
- Endometrium (Mod Pathol 2000;13:285)
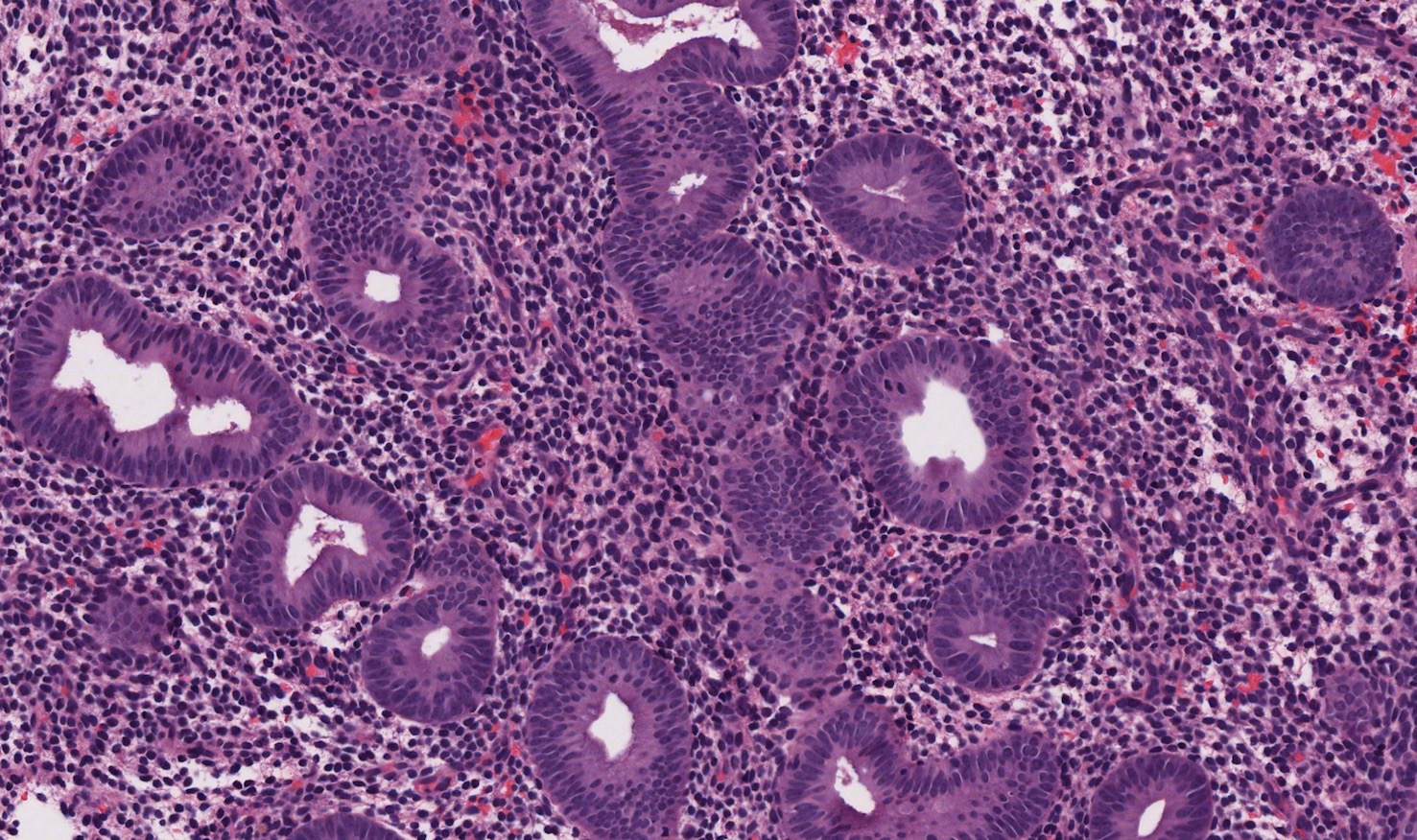
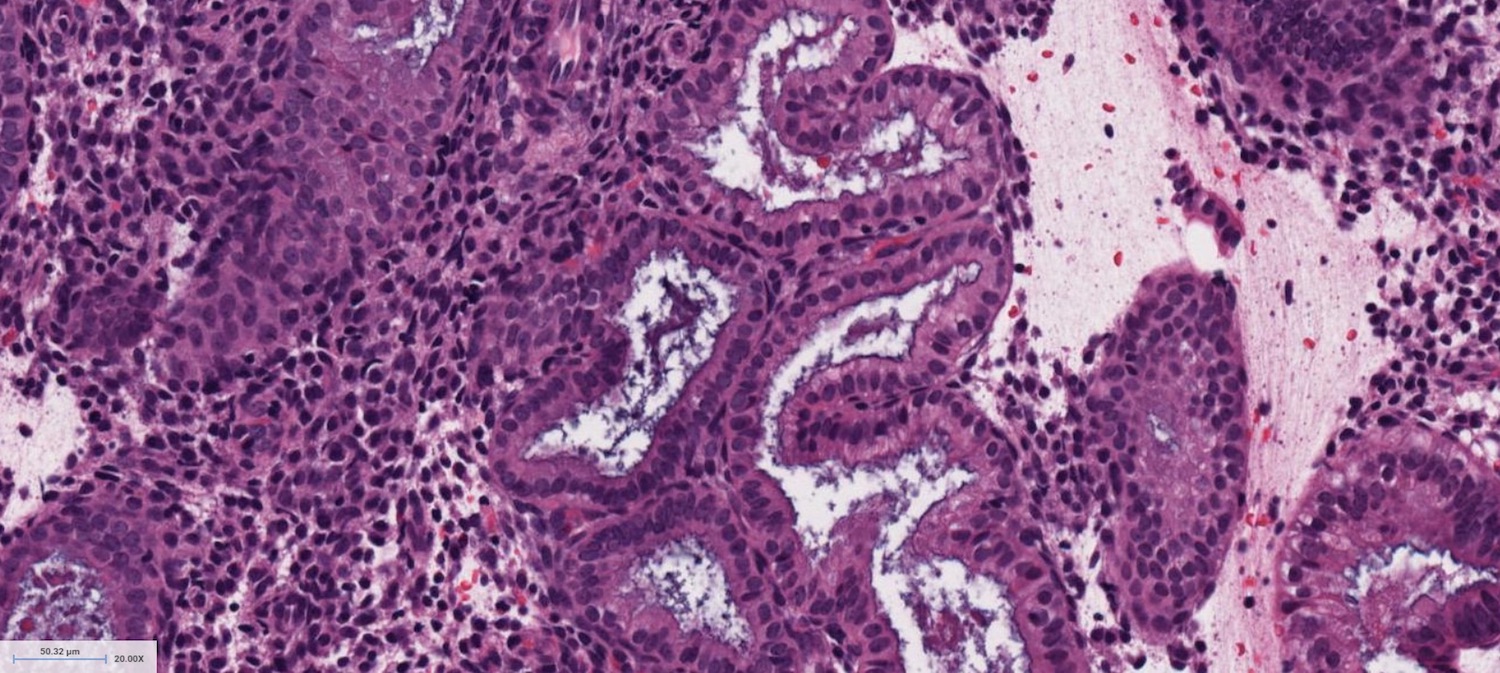
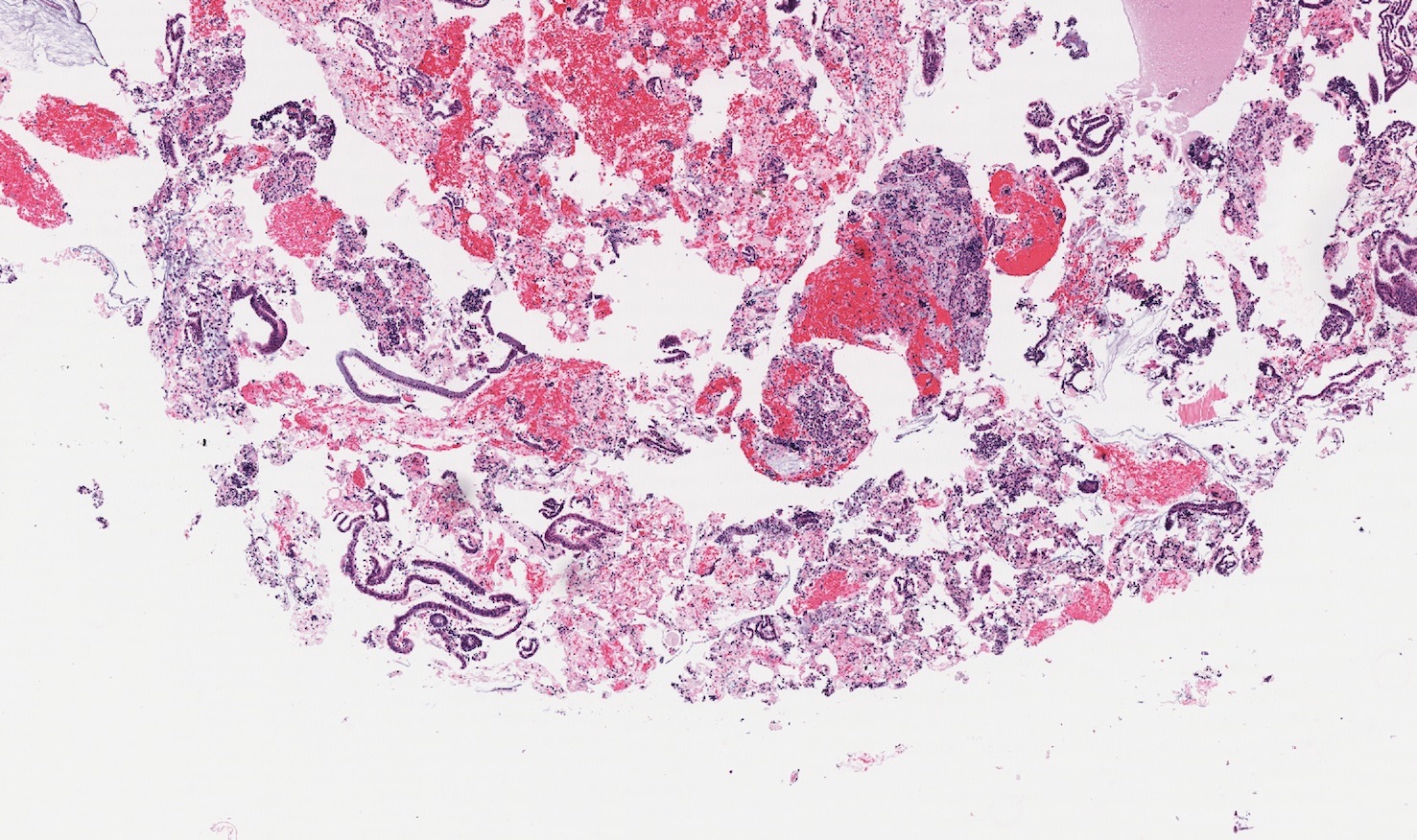
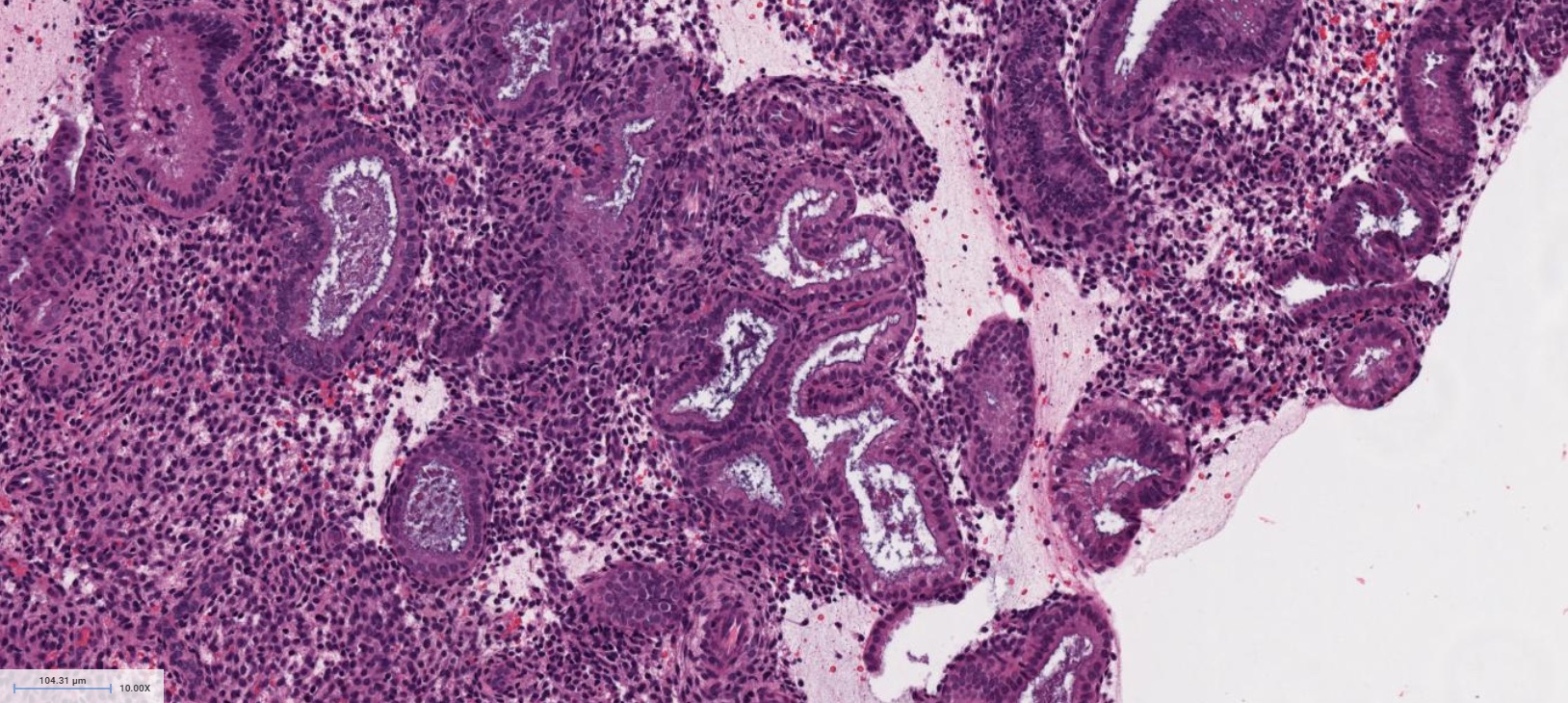
- Proliferative phase
- Cellular blue appearance at low power
- Round to tubular glands
- Even, regular spacing between glands
- Pseudostratified columnar cells in glands
- Numerous mitotic figures in glands and stroma
- Interval phase (Day 16)
- Partially developed subnuclear vacuoles
- Mitoses present, but not as numerous as in proliferative phase
- Less than 50% of cells in a gland with continuous and well developed subnuclear vacuoles
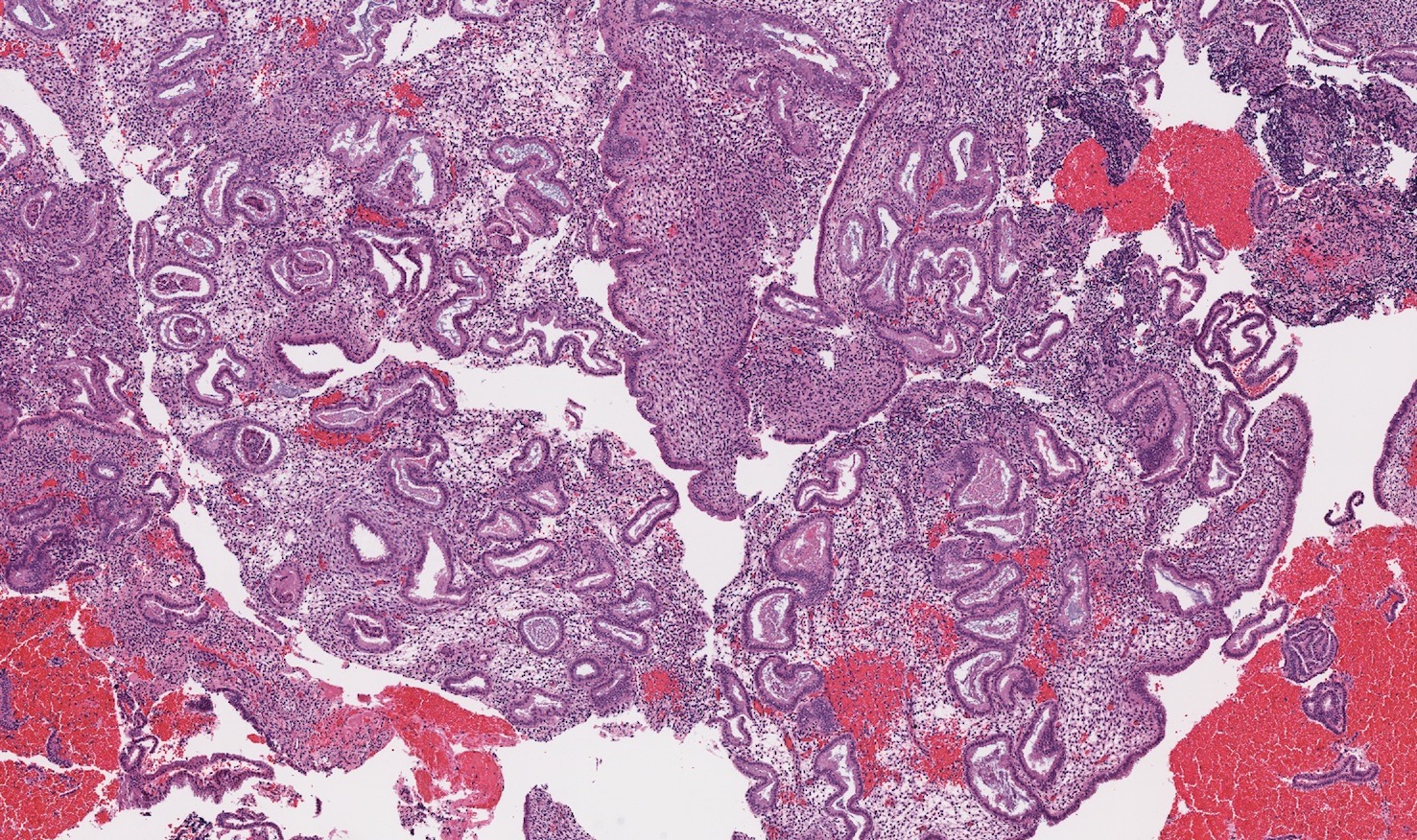
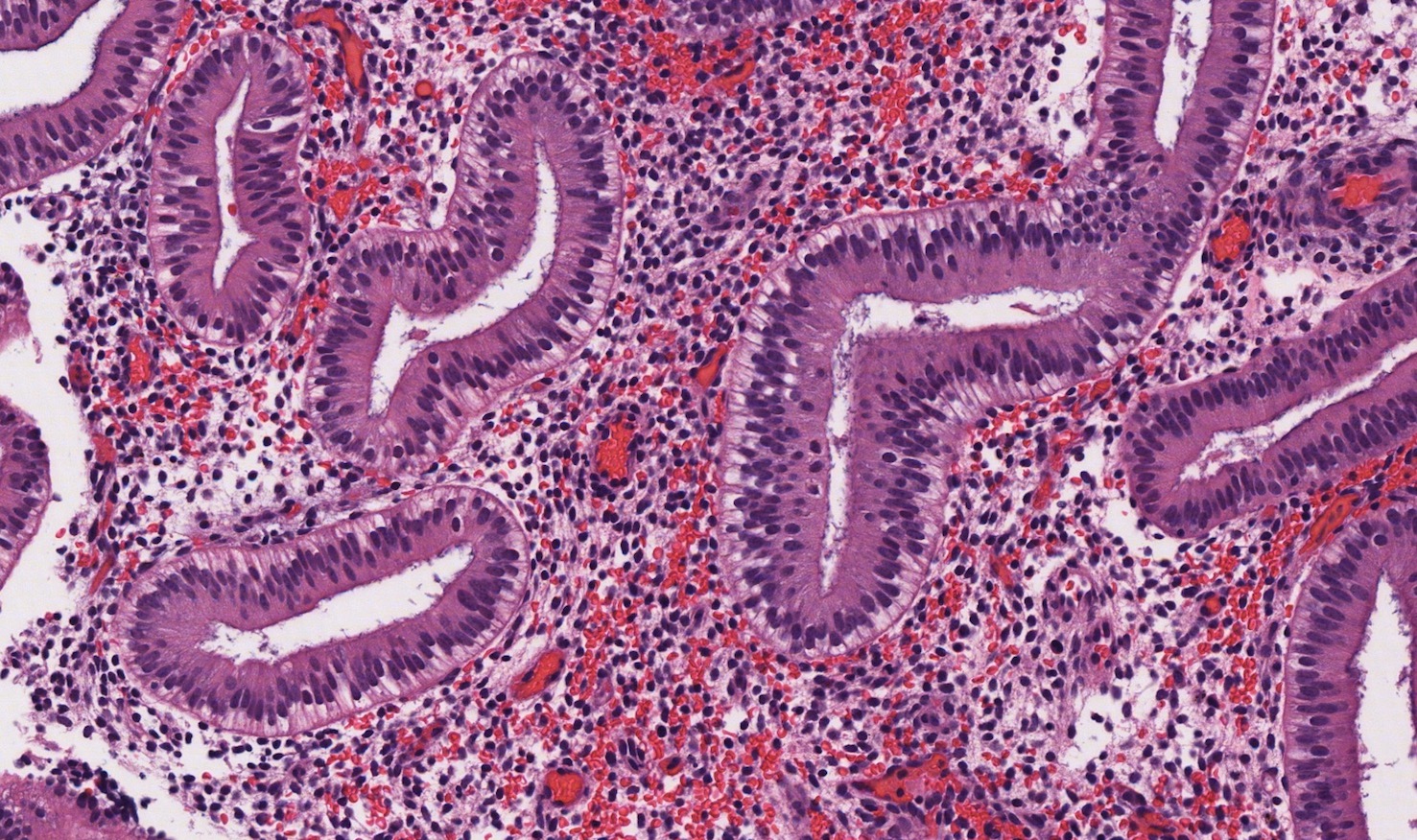
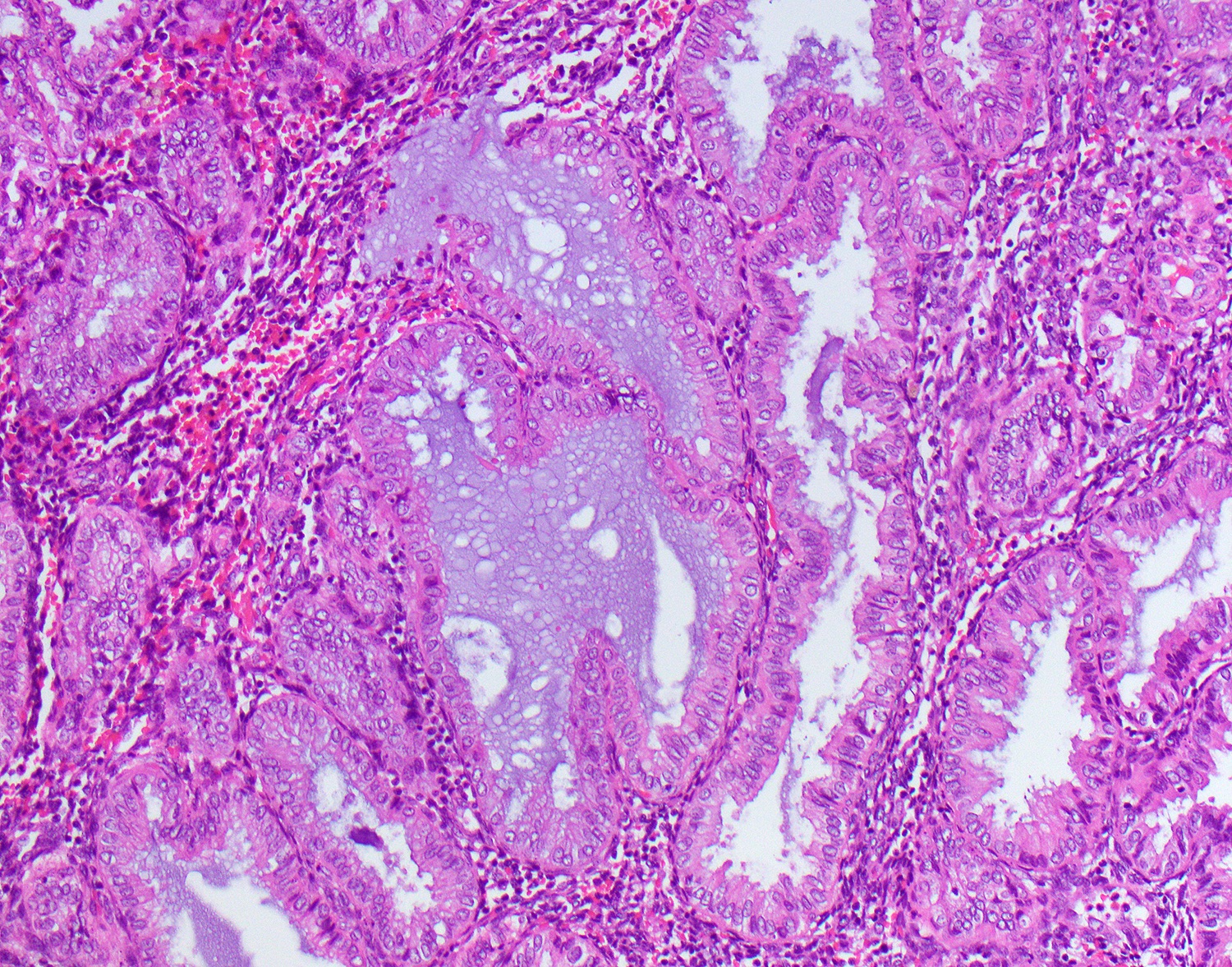
- Secretory phase
- Relatively pink appearance at low power
- Convoluted, irregularly shaped glands
- Single layer of columnar or cuboidal cells in glands
- Early secretory phase (Day 17 - 19)
- Day 17: Continuous and well developed subnuclear vacuoles in > 50% of a gland, rare mitoses
- Day 18: Sub- and supranuclear vacuoles (piano keys) with nuclei in the center of cell
- Day 19: Nuclei at base of cell, supranuclear vacuoles, start of luminal secretions
- Mid secretory phase (Day 20 - 22)
- Day 20: Maximal intraluminal secretions, stromal cells with hyperchromatic nuclei and high N:C ratio
- Day 21: Increased stromal edema
- Day 22: Peak stromal edema
- Late secretory phase (Day 23 - 27)
- Day 23: Predecidua surrounds spiral arterioles
- Day 24: Predecidua bridges multiple vessels
- Day 25: Thin band of predecidua beneath endometrial surface
- Day 26: Thick band of predecidua beneath surface
- Day 27: Abundant predecidua expanding downward from endometrial surface, increased number of stromal granulocytes
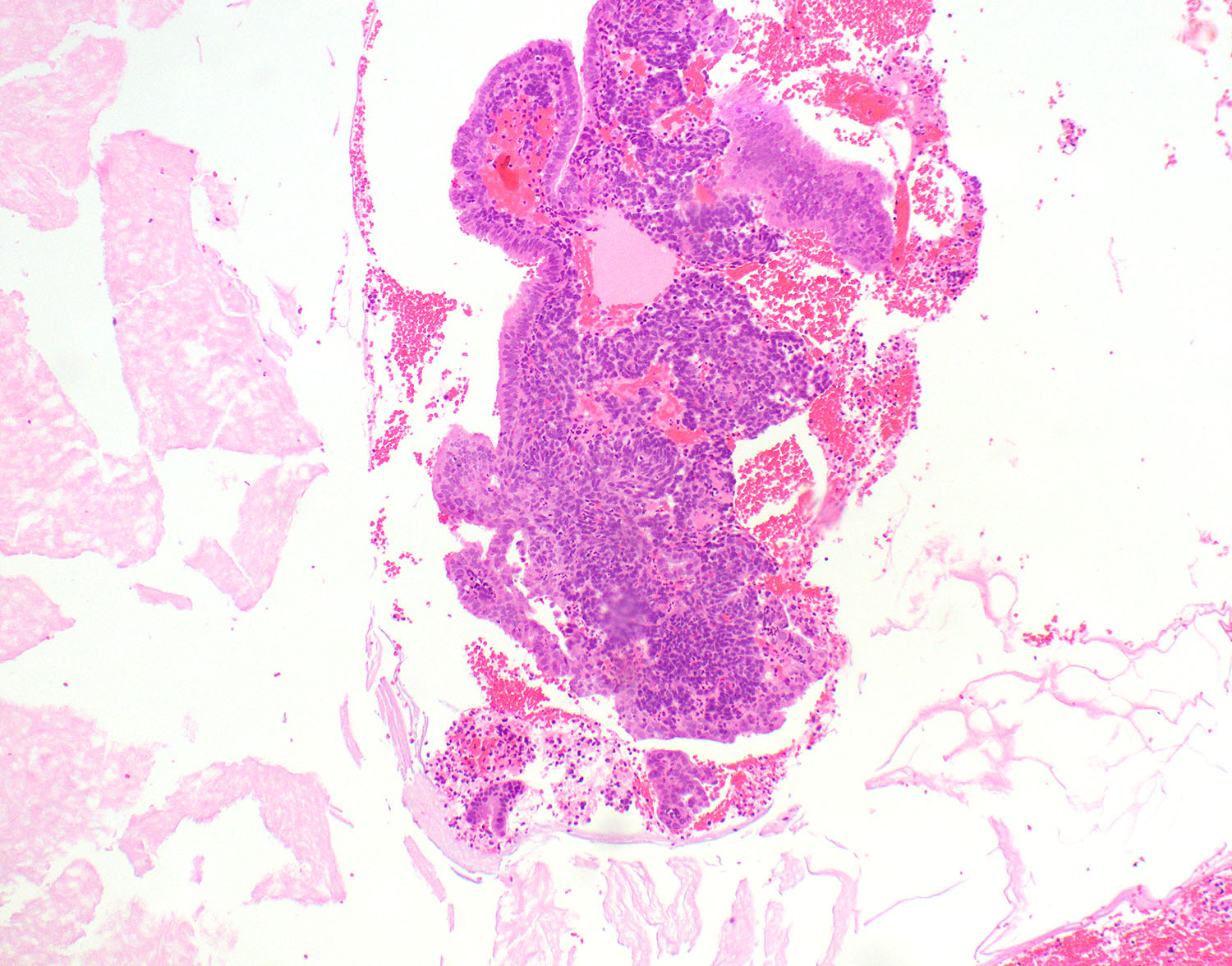
- Menstrual phase
- Endometrial stromal breakdown: dense round aggregates of stromal cells admixed with inflammatory cells and blood
- Papillary syncytial metaplasia is common, thought to be a reparative response
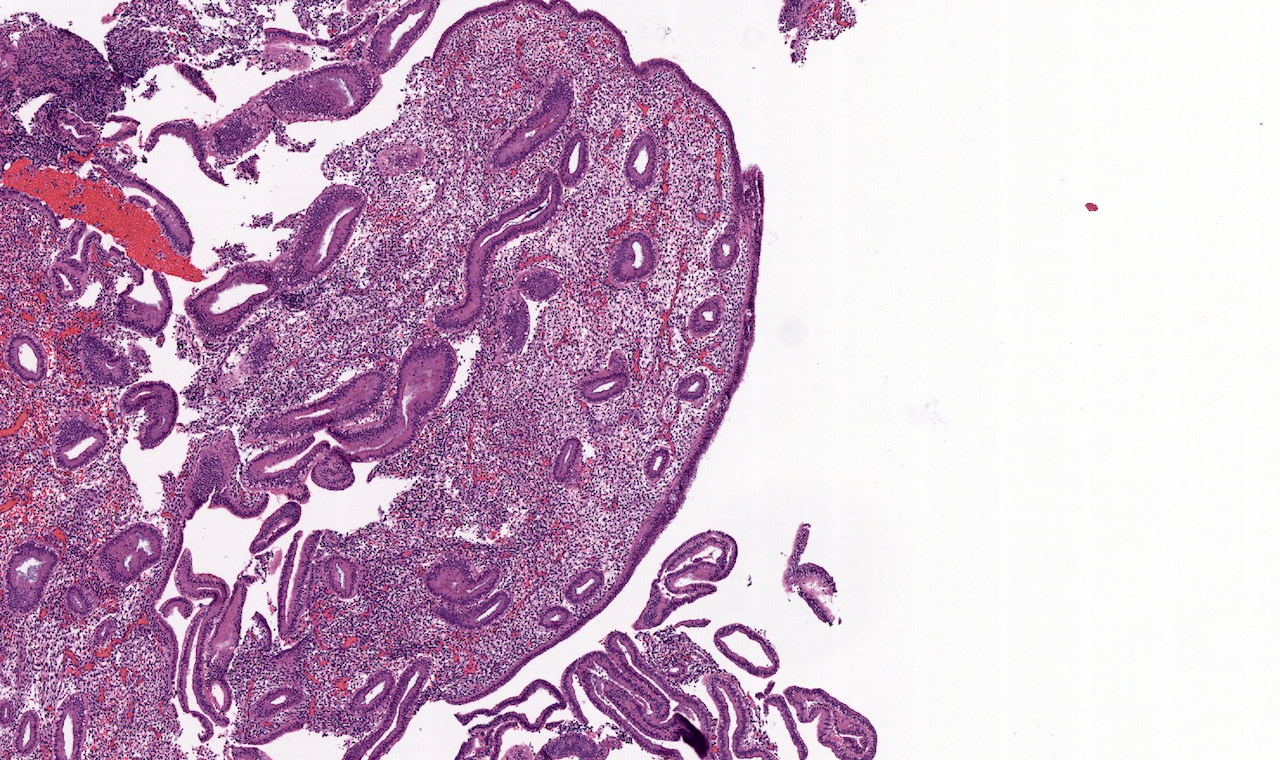
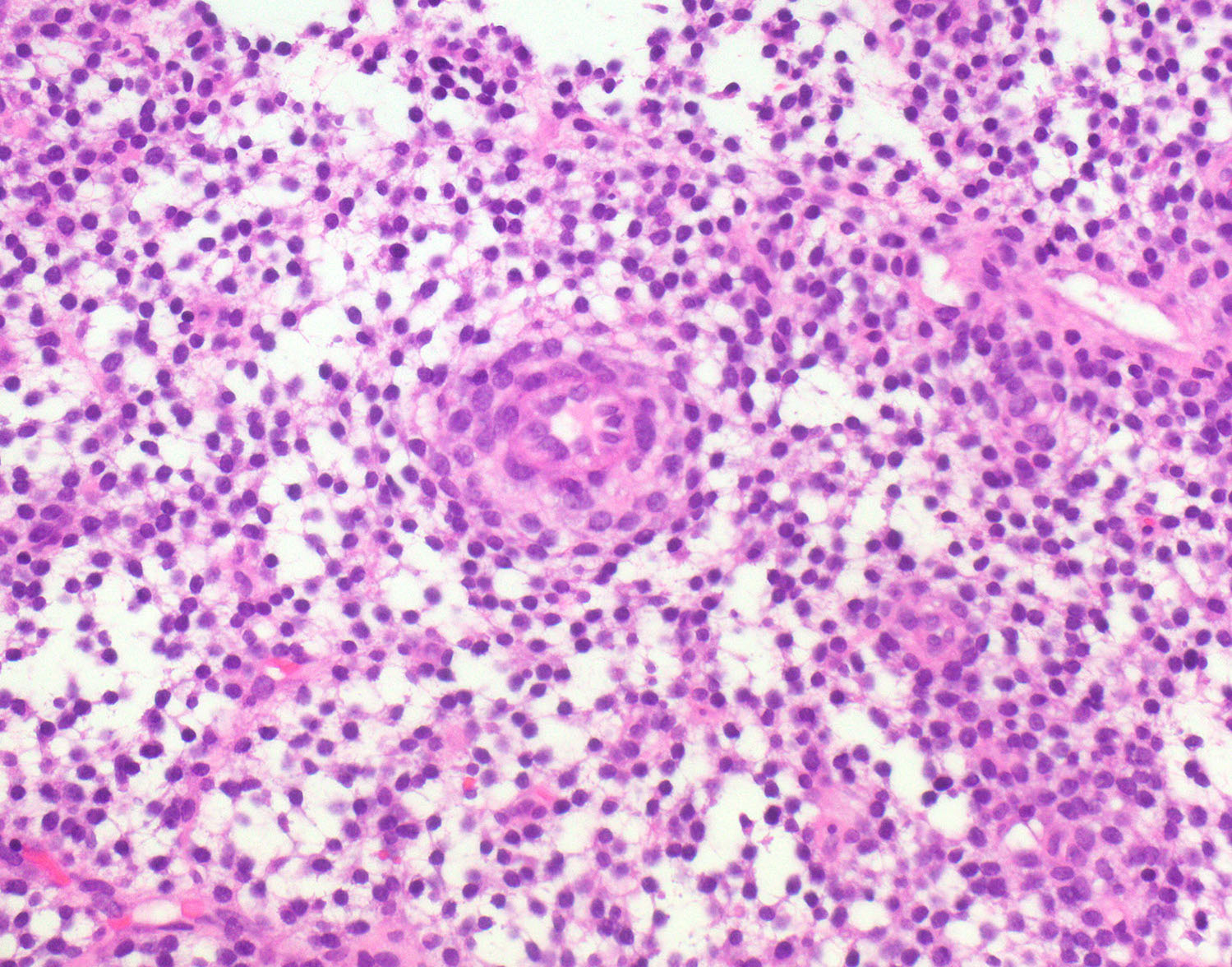
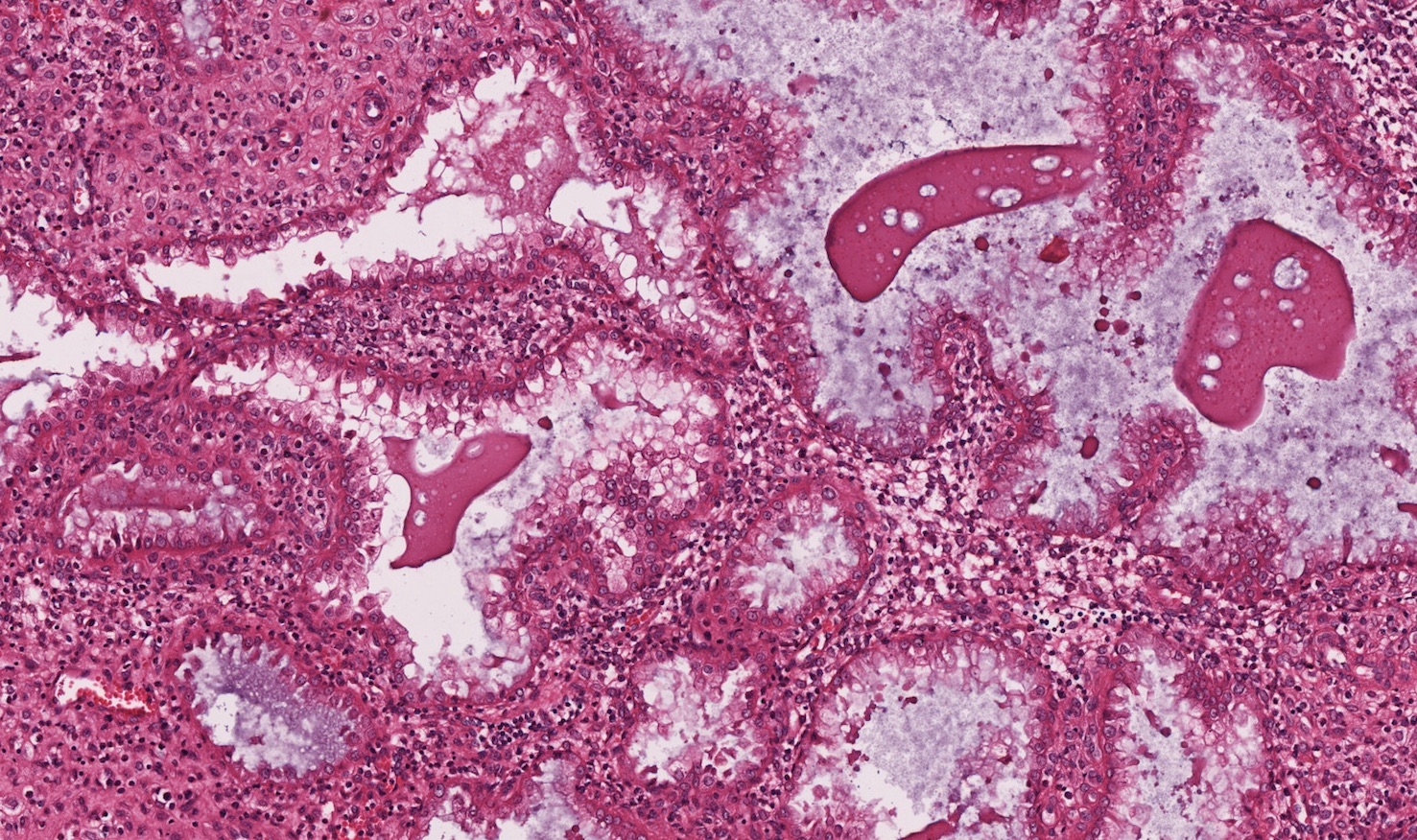
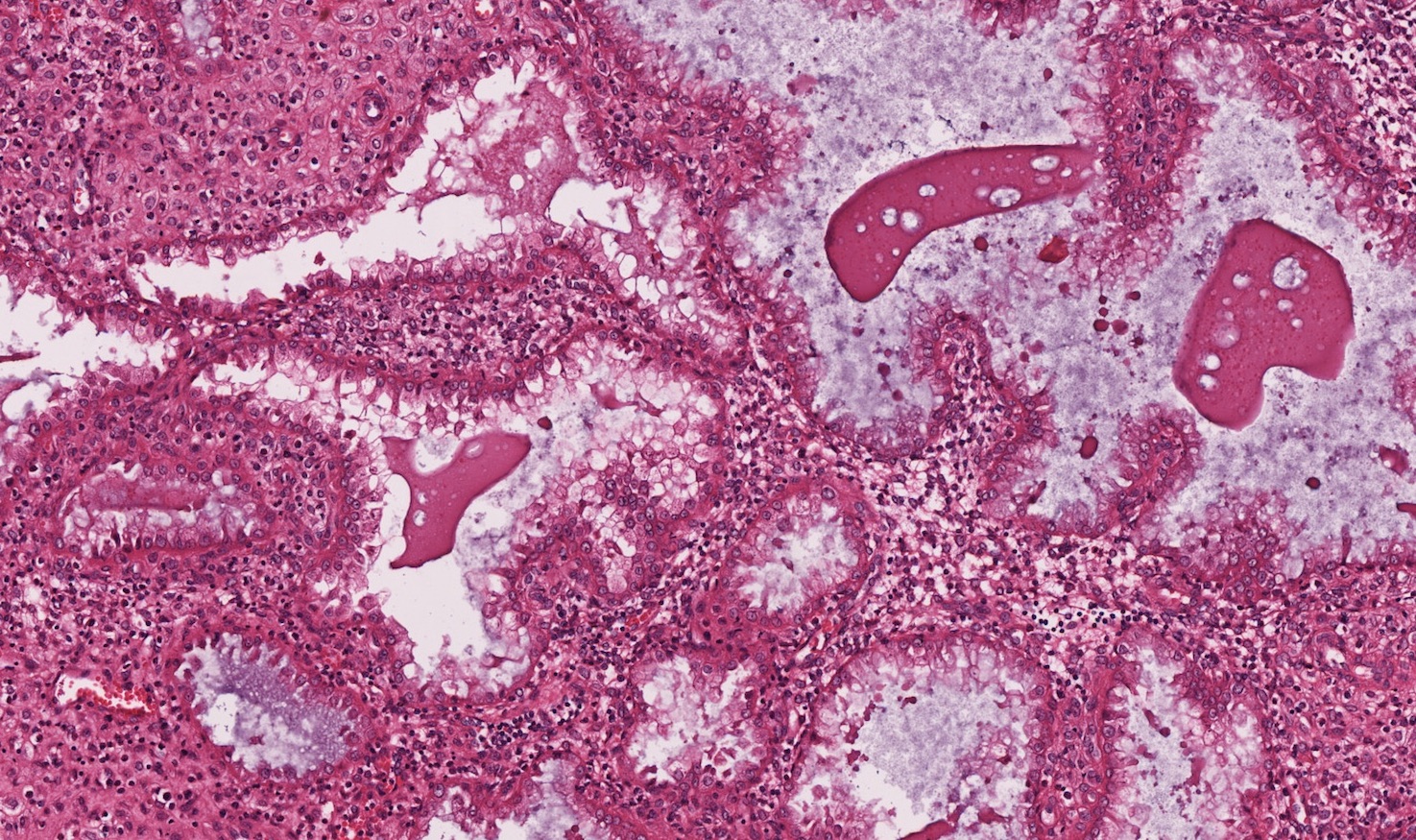
- Gestational changes
- Decidual change: stroma gains abundant eosinophilic cytoplasm, appears polygonal with distinct cell borders
- Arias-Stella reaction in glandular cells (Am J Case Rep 2012;13:271)
- Nuclear enlargement and hyperchromasia
- Abundant eosinophilic vacuolated cytoplasm
- Hobnail appearance with cells protruding into glandular lumen
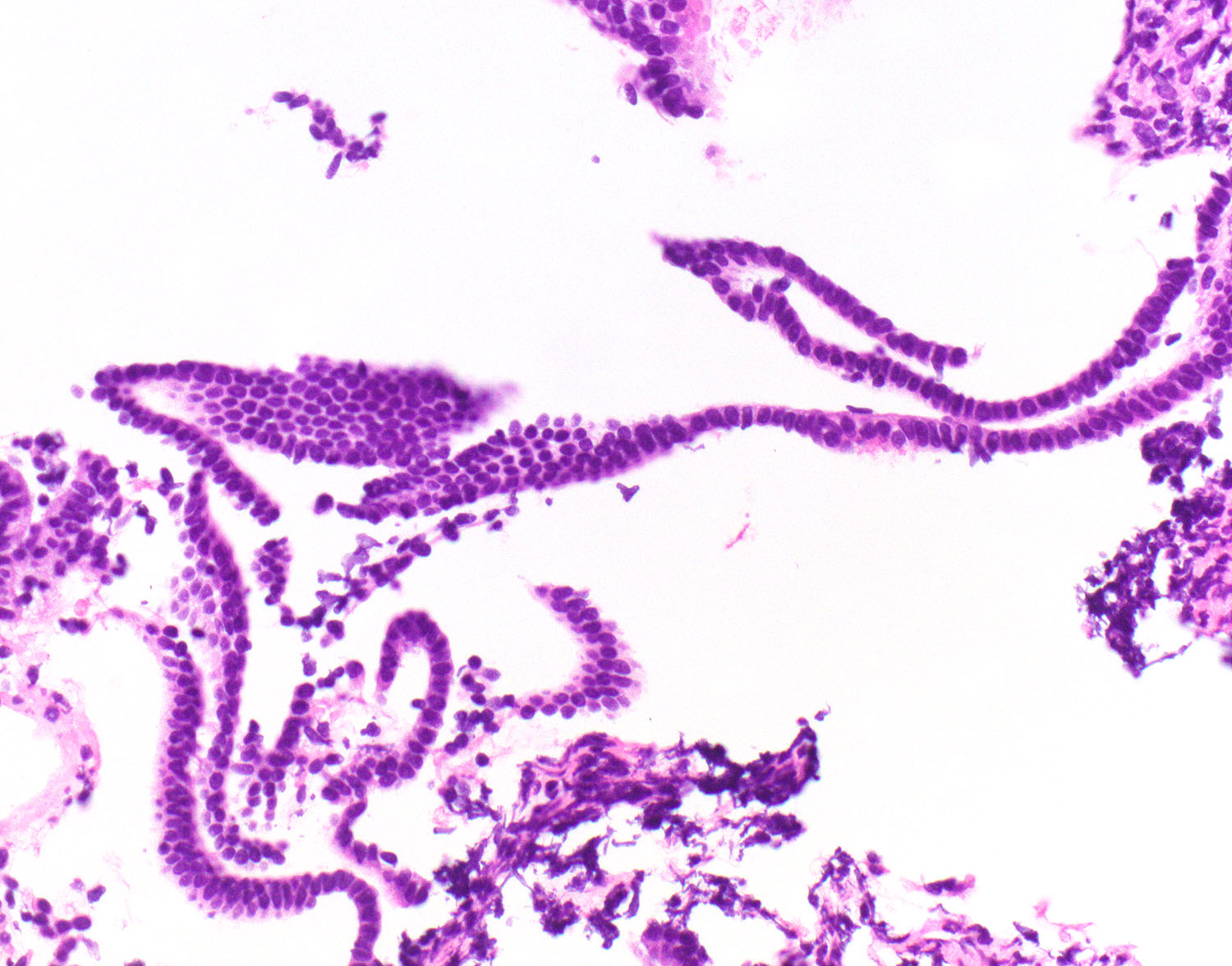
- Atrophy
- Common in postmenopausal women due to estrogen withdrawal
- Glands composed of inactive low columnar to cuboidal cells
- Glands often detached from stroma, forming hairpin structures
- May have cystic change
- Cystic atrophy is associated with postmenopausal tamoxifen for breast cancer (Am J Obstet Gynecol 1998;178:1145)
- Proliferative phase
- Myometrium
- Short fascicles of smooth muscle
- Large, thick walled blood vessels
Cytology description
- Refer to the following: Endometrial cells
Cytology images
- Refer to the following: Endometrial cells
Positive stains
Videos
Histology of benign cycling endometrium
Additional references
Board review style question #1
Board review style answer #1
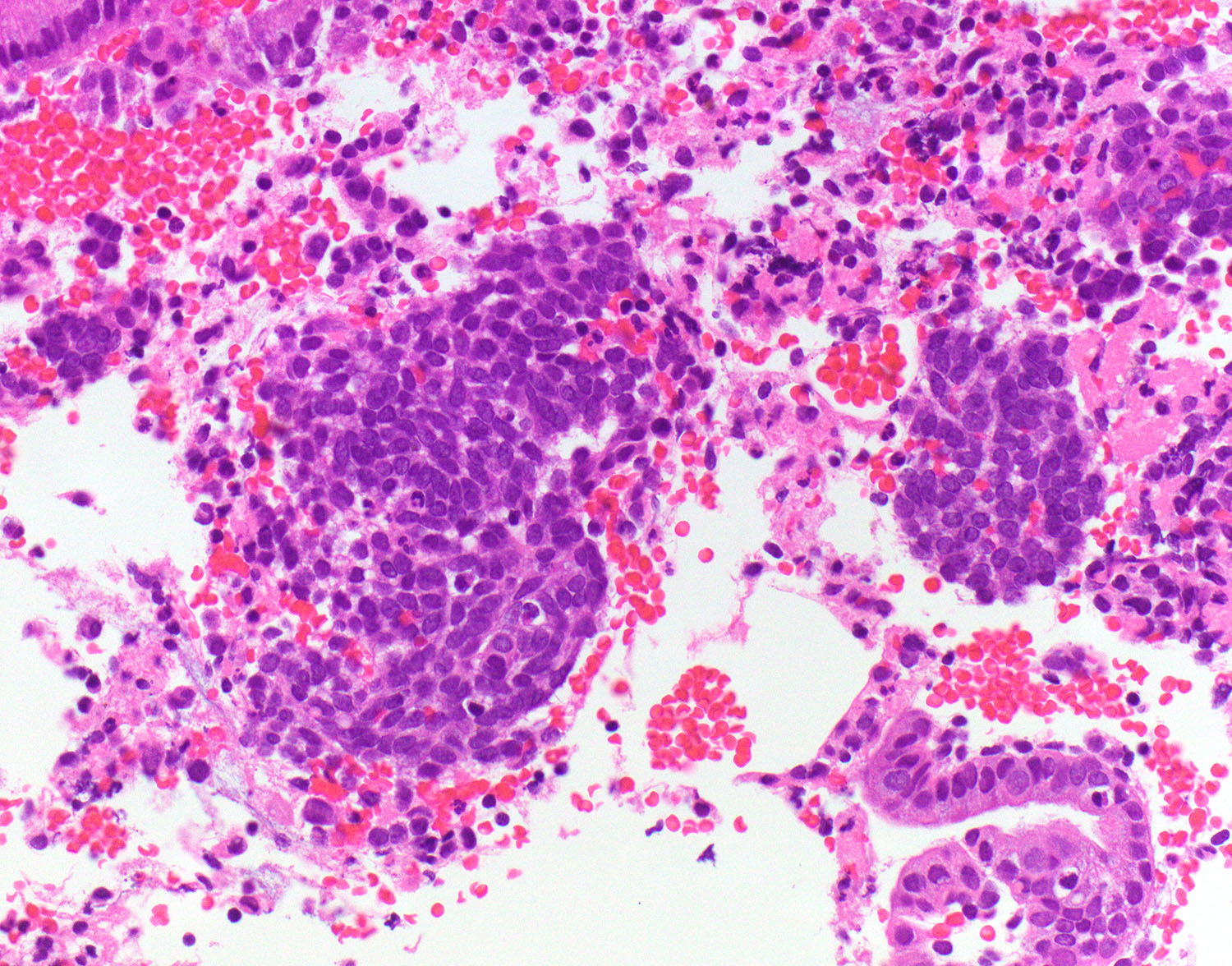
D. Secretory phase. The endometrial glands are lined by a single layer of low columnar cells with pink cytoplasm and prominent glandular secretions. There is predecidual change in the stroma.
Comment Here
Reference: Anatomy & histology
Comment Here
Reference: Anatomy & histology
Board review style question #2
Board review style answer #2
C. Pregnant woman. The image shows an example of gestational endometrium. There is decidual change in the stroma with abundant eosinophilic cytoplasm and polygonal cells with prominent cell borders. The glandular cells show Arias-Stella reaction.
Comment Here
Reference: Anatomy & histology
Comment Here
Reference: Anatomy & histology