Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Costa J, Croce S. Intravenous and diffuse leiomyomatosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusleiomyomaintravascular.html. Accessed May 13th, 2024.
Definition / general
- Intravenous leiomyomatosis
- Rare entity characterized by an intravenous proliferation of benign smooth muscle cells; may coexist with leiomyoma
- May present with pelvic and extrapelvic spread along venous vasculature
- Diffuse leiomyomatosis
- Rare entity characterized by a symmetrical uterine enlargement with innumerable poorly defined, confluent smooth muscle nodules that replace most of the myometrium
Essential features
- Intravenous leiomyomatosis
- Intravascular proliferation of tumor plugs composed by bland smooth muscle cells
- Most cases are confined to the uterus but may present with pelvic and extrapelvic extension through the venous circulatory system
- Clinical presentation is varied, nonspecific and dependent on tumor extension
- Despite being a benign tumor, it may cause remarkable systematic complications and has a relatively high risk of recurrence
- Diffuse leiomyomatosis
- Diffuse, symmetrical thickening of the myometrium with innumerous poorly defined, coalescent nodules of bland smooth muscle cells
- Clinical presentation is varied and nonspecific
- Benign tumor, patients usually do not experience recurrence
Terminology
- Intravenous leiomyomatosis: intravascular leiomyomatosis
- Diffuse leiomyomatosis: diffuse uterine leiomyomatosis
ICD coding
- Intravenous leiomyomatosis
- ICD-O: 8890/1 - intravenous leiomyomatosis
- ICD-11: 2E86.0 & XH60C2 - leiomyoma of uterus & intravascular leiomyomatosis
- Diffuse leiomyomatosis
Epidemiology
- Intravenous leiomyomatosis
- Rare; fewer than 400 cases have been reported in the English literature (Front Surg 2023;9:1020004, Int J Gynecol Pathol 2015;34:169, Pathol Res Pract 2018;214:871, Int J Gynecol Pathol 1994;13:1, Int J Gynecol Pathol 1987;6:331)
- Du et al. reported that intravenous leiomyomatosis comprised ~0.097% of all genital smooth muscle tumor cases in their hospital (Hum Pathol 2011;42:1240)
- Chen et al. reported that intravenous leiomyomatosis cases corresponded to 1.2% of all uterine leiomyomas diagnosed at their hospital (Front Surg 2023;9:1020004)
- Mean age of onset has been estimated between 45 and 47 years (J Obstet Gynaecol Res 2021;47:4357, Front Surg 2023;9:1020004)
- Most patients (estimated between 46.5 and 64%) have a history of uterine surgical procedures, such as cesarean section, myomectomy and hysterectomy (J Obstet Gynaecol Res 2021;47:4357)
- Diffuse leiomyomatosis
- Rare; < 50 sporadic cases have been reported in English literature (Cureus 2022;14:e29595)
- Frequently affects women between the third and fourth decades of life (Arch Gynecol Obstet 2014;290:815, Hum Pathol 2000;31:1429)
- Has been described in patients with hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome (Am J Surg Pathol 2019;43:1170, World J Clin Cases 2022;10:8797)
Sites
- Intravenous leiomyomatosis
- Marked variation reported in the literature in the sites of involvement and extension
- Most tumors present within the myometrium, with parauterine extension (mostly to the broad ligament) in a smaller number of cases (J Obstet Gynaecol Res 2021;47:4357, Medicine (Baltimore) 2021;100:e24228, Pathol Res Pract 2018;214:871)
- Pelvic and extrapelvic extension frequencies have been estimated at 28 - 71% and 0 - 7%, respectively (J Obstet Gynaecol Res 2021;47:4357, Medicine (Baltimore) 2021;100:e24228, Pathol Res Pract 2018;214:871, BMC Cancer 2016;16:73, Clin Radiol 2018;73:503.e1)
- Extension to the cardiac and pulmonary systems has been described
- Most cases are reported to spread unilaterally, with occasional bilateral spread
- Diffuse leiomyomatosis
- Most cases are confined to the uterus
- Cases associated with ovarian and parametrial involvement have been reported (Obstet Gynecol 2001;97:834)
Pathophysiology
- Intravenous leiomyomatosis
- Pathogenesis remains unknown; there are 2 main hypotheses
- Origin in a leiomyoma that invades the uterus or parauterine veins
- Intravenous leiomyomatosis cells exhibit estrogen and progesterone receptor positivity, unlike vascular endothelial and subendothelial cells, which express none or show patchy / weak staining (Medicine (Baltimore) 2021;100:e24228, BMC Cancer 2016;16:73, Pathol Res Pract 2018;214:871, Eur J Gynaecol Oncol 2004;25:362)
- Significant proportion of patients present with coexistent leiomyomas (~38.89 - 61.5% of cases) or a history of uterine surgery (Medicine (Baltimore) 2021;100:e24228, BMC Cancer 2016;16:73, Hum Pathol 2011;42:1240, Clin Radiol 2018;73:503.e1)
- These tumors do not show significant adhesion to the venous walls and the bases of implantation are connected with the myometrium (BMC Cancer 2016;16:73)
- Intravenous leiomyomatosis shares some cytogenetic and immunohistochemical features with uterine leiomyomas, such as balanced translocations t(12;14)(q14-15;q23-24) and HMGA2 expression (Mod Pathol 2016;29:500, Int J Gynecol Pathol 2015;34:169, Cancers (Basel) 2022;14:2907)
- Origin in the smooth muscle cells of the blood vessel walls, which proliferate and intrude into the venous lumen
- Significant proportion of cases are not associated with uterine leiomyomas (Pathol Res Pract 2018;214:871, Hum Pathol 2011;42:1240)
- Origin in a leiomyoma that invades the uterus or parauterine veins
- Pathogenesis remains unknown; there are 2 main hypotheses
- Diffuse leiomyomatosis
- Pathogenesis of diffuse leiomyomatosis is far from clear
- Some authors consider that diffuse leiomyomatosis may be originated from multiple leiomyomas in a hyperactive state, budding into each other and blending imperceptibly (World J Clin Cases 2022;10:8797, Hum Pathol 2000;31:1429)
Etiology
- Intravenous leiomyomatosis
- Some authors have suggested that vascular injury due to uterine surgery, venous stasis and elevated estrogen levels may play a role in the development (J Obstet Gynaecol Res 2021;47:4357, Medicine (Baltimore) 2021;100:e24228, BMC Cancer 2016;16:73, Hum Pathol 2011;42:1240, Clin Radiol 2018;73:503.e1)
- Diffuse leiomyomatosis
- Its etiology is still not completely understood; no specific risk factors reported in the literature (Cureus 2022;14:e29595)
Clinical features
- Intravenous leiomyomatosis
- Clinical manifestations are usually diverse, nonspecific and dependent on its location and extension
- According to one group of authors, clinically, intravenous leiomyomatosis can be divided into 4 stages (Medicine (Baltimore) 2016;95:e4902)
- Stage I: tumors invading the uterine vein and limited to the pelvis
- Stage II: tumors extending to the abdominal cavity but without involvement of the renal vein
- Stage III: tumors invading the renal vein and inferior vena cava and extending further up to the right atrium but without reaching the pulmonary arteries
- Stage IV: tumors reaching the pulmonary arteries or metastasizing to the lungs
- ~29.7% of patients reported in literature present in stages I / II and 65.6% in stages III / IV but patients with early lesions or asymptomatic patients may be underreported (Front Surg 2023;9:1020004)
- When confined to the uterus, most patients are asymptomatic (J Obstet Gynaecol Res 2021;47:4357 Mod Pathol 2016;29:500, Medicine (Baltimore) 2016;95:e4902)
- Some patients present with nonspecific symptoms suggestive of a pelvic mass and similar to uterine leiomyomas: hypermenorrhea, menostaxis, irregular vaginal bleeding, abdominal swelling or pelvic pain (J Obstet Gynaecol Res 2021;47:4357 Mod Pathol 2016;29:500, Medicine (Baltimore) 2016;95:e4902)
- Cases with extrapelvic extension may present with edema and heaviness of the lower extremities (J Obstet Gynaecol Res 2021;47:4357)
- In cases with cardiac and pulmonary extension, chest discomfort, dyspnea and syncope, congestive heart failure, pulmonary embolism and sudden death have been reported (J Obstet Gynaecol Res 2021;47:4357)
- Diffuse leiomyomatosis
- Clinical presentation is varied, nonspecific and often similar to the symptomatology of uterine leiomyomas
- Initial presenting symptoms include abnormal uterine bleeding, menorrhagia, dysmenorrhea, pelvic pain or abdominal swelling (World J Clin Cases 2022;10:8797, Cureus 2022;14:e29595)
- Unusual presentations have included a case of diffuse leiomyomatosis in a pregnant patient, associated with uterine rupture, fetal demise and benign metastasizing leiomyomas in the bone (Obstet Gynecol 2007;109:528, Indian J Pathol Microbiol 2012;55:585)
Diagnosis
- Intravenous leiomyomatosis
- Best methodology for diagnosis remains a topic of ongoing debate
- Typical imaging methods include ultrasonography, computerized tomography (CT) and magnetic resonance imaging (MRI)
- Preoperative misdiagnosis rate is exceptionally high due to the nonspecific clinical signs and symptoms and the difficulty in detection by current imaging techniques, especially in cases confined to the uterus (Radiol Case Rep 2022;17:4203, J Obstet Gynaecol Res 2021;47:4357)
- Ultrasonography may detect some cases of extrauterine extension and is important for the evaluation of intravascular and intracardiac lesions (Clin Radiol 2018;73:503.e1, Medicine (Baltimore) 2021;100:e24228, AJR Am J Roentgenol 2007;188:246)
- Contrast enhanced CT has the capacity to directly show the tumor size, location and extension pathway (Medicine (Baltimore) 2021;100:e24228, BMC Cancer 2016;16:73, Clin Radiol 2018;73:503.e1)
- MRI is useful for diagnostic imaging of the venous system; however, it is time consuming, has poor spatial resolution and is not suitable for patients carrying metal intrauterine devices or cardiac pacemakers (Clin Radiol 2018;73:503.e1)
- Diffuse leiomyomatosis
- Ultrasonography should be the first line imaging modality to assess the pelvic cavity and uterine disorders (Obstet Gynecol Clin North Am 2021;48:193)
- MRI is the optimal imaging technique due to its multiplanar imaging capabilities and excellent soft tissue contrast as well as its important roles in pretreatment mapping and differential diagnosis (Radiol Case Rep 2022;17:1536, Pediatr Radiol 2012;42:124, Eur Radiol 2018;28:3125, Obstet Gynecol Clin North Am 2021;48:193)
Radiology description
- Intravenous leiomyomatosis
- The most typical CT features of intravenous leiomyomatosis described are (Clin Radiol 2018;73:503.e1, BMC Cancer 2016;16:73)
- Continuous pelvic and intravenous masses, with heterogeneous enhancement and occasionally, presence of blood vessels in the lesion
- Lesions in the inferior vena cava that are continuous and shaped like sausages
- In cases with involvement of the right cardiac chambers, the cardiac imaging findings show a snake head or walking stick head appearance
- No invasion or adhesion to the vessel wall
- May present with calcifications
- Cases invading the inferior vena cava may have a characteristic feature on contrast enhancing CT and MRI: the growth pattern and the small vessels within the tumor create an appearance similar to a sieve on axial images and a luffa sponge on coronal images (Clin Radiol 2018;73:503.e1)
- The most typical CT features of intravenous leiomyomatosis described are (Clin Radiol 2018;73:503.e1, BMC Cancer 2016;16:73)
- Diffuse leiomyomatosis
- Imaging techniques reveal symmetrical and uniform enlargement of the uterus, with innumerable coalescing nodules of different sizes with indistinct borders in the myometrium (World J Clin Cases 2022;10:8797)
- Typical leiomyomas are well circumscribed masses with an asymmetrical involvement of the uterus and usually demonstrate low / intermediate signal intensity on T2 weighted images, which can be difficult to appreciate in diffuse leiomyomatosis (Radiol Case Rep 2022;17:1536, Eur Radiol 2018;28:3125)
Radiology images
Prognostic factors
- Intravenous leiomyomatosis
- Recurrence rate varies between 5.4 and 31% (J Obstet Gynaecol Res 2021;47:4357, Front Surg 2023;9:1020004)
- Regrowth of residual tumor has been reported in 16.6 - 30% of the patients (Pathol Res Pract 2018;214:871)
- Recurrence time ranges between 7 months and 15 years, with one study estimating a median recurrence time of 8.5 months (J Obstet Gynaecol Res 2021;47:4357, J Int Med Res 2020;48:300060519896887)
- 11 intravenous leiomyomatosis related deaths have been reported in literature, all of which were in stage III and IV (Front Surg 2023;9:1020004)
- Several factors have been associated with recurrence (albeit not consistently): younger age, large lesions (≥ 7 cm), extension to the broad ligament, type of surgical approach and incomplete resection (Medicine (Baltimore) 2021;100:e24228, J Obstet Gynaecol Res 2021;47:4357, Front Surg 2023;9:1020004)
- Early stage diagnosis and complete excision are critical for a good prognosis (Pathol Res Pract 2018;214:871)
- Excellent longterm survival after successful removal; most patients have an unremarkable clinical course with a relatively low risk of recurrence / distant metastasis (Mod Pathol 2016;29:500)
- Longterm follow up is necessary, to monitor for recurrence and observe the dynamic changes in residual lesions
- Follow up should include a systematic examination, regular ultrasound examinations of the pelvic region and the cardiovascular system and contrast enhanced CT or MRI, if necessary
- There is no consensus on the periodicity of the follow up, with some authors proposing a baseline CT 6 months after surgery and subsequently, every 2 - 5 years, while others recommend a more closely spaced surveillance regimen (every 3 months) (Medicine (Baltimore) 2021;100:e24228)
- Diffuse leiomyomatosis
- After hysterectomy and removal of any associated extrauterine lesions, patients usually do not experience recurrence (Radiol Case Rep 2022;17:1536, World J Clin Cases 2022;10:8797, Zhonghua Yi Xue Za Zhi 2020;100:2263)
- 2 cases of recurrence after conservative surgery have been reported (World J Clin Cases 2022;10:8797, Zhonghua Yi Xue Za Zhi 2020;100:2263)
- In the case of diffuse leiomyomatosis associated with benign metastasizing leiomyomas to the bone, the bone lesions regressed completely after hysterectomy (Obstet Gynecol 2007;109:528)
Case reports
- Intravenous leiomyomatosis
- 31 year old woman with a history of myomectomy presented with abnormal uterine bleeding, anemia and multiple uterine nodules (Radiol Case Rep 2022;17:4203)
- 49 year old woman presented with dyspnea, abdominal distension and a large uterine mass extending to the right parauterine veins, right ovarian vein and the inferior vena cava (Taiwan J Obstet Gynecol 2021;60:367)
- 52 year old woman presented with lower abdominal pain, a 270 mm uterine mass and a 78 x 47 mm mass in the right atrium (Diagn Pathol 2020;15:4)
- Diffuse leiomyomatosis
- 27 year old woman presented with heavy vaginal bleeding and a regularly enlarged uterus (World J Clin Cases 2022;10:8797)
- 36 year old woman presented with a 1 year history of lower abdominal discomfort and dysmenorrhea and a markedly enlarged uterus replaced by innumerable nodules (Radiol Case Rep 2022;17:1536)
- 38 year old nulliparous woman presented with abdominal distension and an enlarged uterus of size 250 x 200 x 130 mm (Cureus 2022;14:e29595)
Treatment
- Intravenous leiomyomatosis
- Surgery is the main treatment option (J Obstet Gynaecol Res 2021;47:4357, Medicine (Baltimore) 2021;100:e24228, J Int Med Res 2020;48:300060519896887, Front Surg 2023;9:1020004)
- Complete removal of the lesion is crucial to obtain a favorable prognosis
- Controversy surrounding the selection of the different surgical approaches
- Hysterectomy is recommended for most patients
- Bilateral oophorectomy has also been recommended for patients who are menopausal / perimenopausal or with extrauterine extension but recent studies questioned its usefulness
- Myomectomy has been proposed as an option for young women who wish to preserve fertility but it has been associated with an increased risk of recurrence
- Multidisciplinary surgical approach is required in cases of extrapelvic extension
- 1 stage or 2 stage surgery may be employed, depending on several factors, such as patient's tolerance and tumor extension
- Complete tumor resection is achieved in 56 - 92.1% of patients
- Use of postoperative hormone treatment is controversial (J Obstet Gynaecol Res 2021;47:4357, Medicine (Baltimore) 2021;100:e24228)
- Gonadotropin releasing hormone agonist was previously recommended as a postoperative approach to reducing the risk of recurrence in cases with preservation of both ovaries or impossibility of complete resection but recent studies have questioned its effectiveness
- Use of tamoxifen and aromatase inhibitors has also been reported
- Surgery is the main treatment option (J Obstet Gynaecol Res 2021;47:4357, Medicine (Baltimore) 2021;100:e24228, J Int Med Res 2020;48:300060519896887, Front Surg 2023;9:1020004)
- Diffuse leiomyomatosis
- Hysterectomy is the standard treatment of choice since hormone treatment frequently fails to control the symptoms
- Since most patients are of reproductive age, other strategies have also been studied (Radiol Case Rep 2022;17:1536, Zhonghua Yi Xue Za Zhi 2020;100:2263, J Vasc Interv Radiol 2003;14:643, Eur J Radiol 2012;81:2726, World J Clin Cases 2022;10:8797)
- Successful pregnancies have been reported in women treated with gonadotropin releasing hormone agonists or minimally invasive hysteroscopic myomectomy by removing submucosal leiomyomas
- Other treatment options include uterine artery embolization, high intensity focused ultrasound and sirolimus
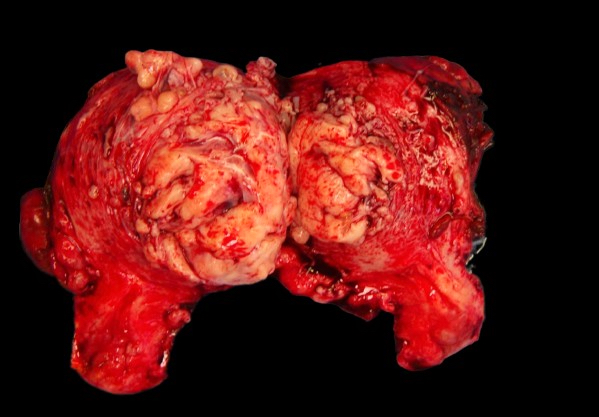
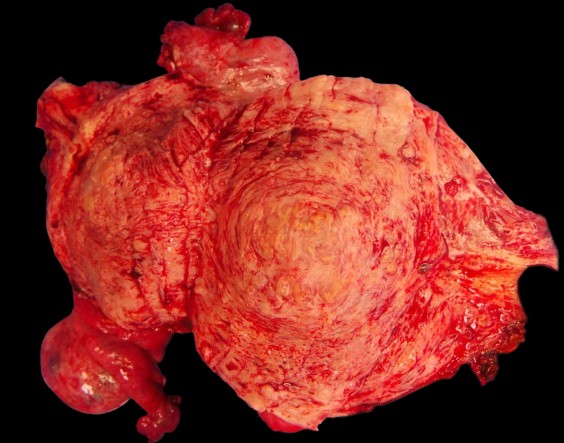
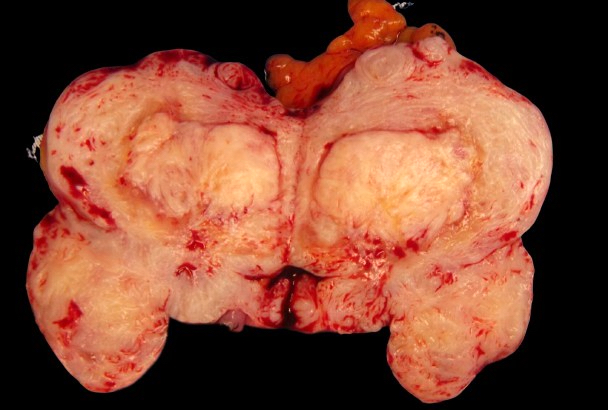
Gross description
- Intravenous leiomyomatosis
- Uterus appears enlarged, with multiple intramural masses, usually ranging between 5 and 130 mm in largest dimension (Pathol Res Pract 2018;214:871, Hum Pathol 2011;42:1240)
- These masses show a coiled or nodular growth within the myometrium, appearing as cord-like / worm-like plugs or lobulated structures (Pathol Res Pract 2018;214:871, Hum Pathol 2011;42:1240)
- Tumor plugs demonstrate a soft, spongy cut surface, with a grayish / pinkish white appearance and convoluted, irregular borders (Pathol Res Pract 2018;214:871, Hum Pathol 2011;42:1240, Cancer 1975;36:2164)
- Tumor can be entirely free floating within the vessel lumen or less commonly, it can have attachments to the vessel walls (Hum Pathol 2011;42:1240, Pathol Res Pract 2011;207:131)
- Gross examination is essential for identifying the tumor at earlier stages and avoiding a missed diagnosis (Hum Pathol 2011;42:1240, Int J Gynecol Pathol 2015;34:169, Medicine (Baltimore) 2021;100:e24228)
- Intravenous leiomyomatosis, in early stages, is easily overlooked by pathologists
- Careful examination of the sections of the external portion of the myometrium, broad ligament and the soft tissue on either side of the lower uterine segment, below the peritoneal reflection
- Intravenous leiomyomatosis may be obscured by large or multiple leiomyomas or adenomyosis
- Sampling should be concentrated on the peripheral aspects of mass lesions with adjacent vasculature and unremarkable smooth muscle
- Care should be taken to avoid extracting only the tumor plugs growing within the vessels and to avoid tumor retraction or protrusion from the vein, resulting in a missed diagnosis
- Diffuse leiomyomatosis
- Symmetrically enlarged uterus with a diffusely thickened myometrium, almost completely replaced by numerous poorly defined, confluent nodules, ranging from 2 to 50 mm (World J Clin Cases 2022;10:8797, Cureus 2022;14:e29595, Histopathology 1995;27:175)
Gross images
Contributed by Sabrina Croce, M.D., Ph.D.
Diffuse leiomyomatosis
Images hosted on other servers:
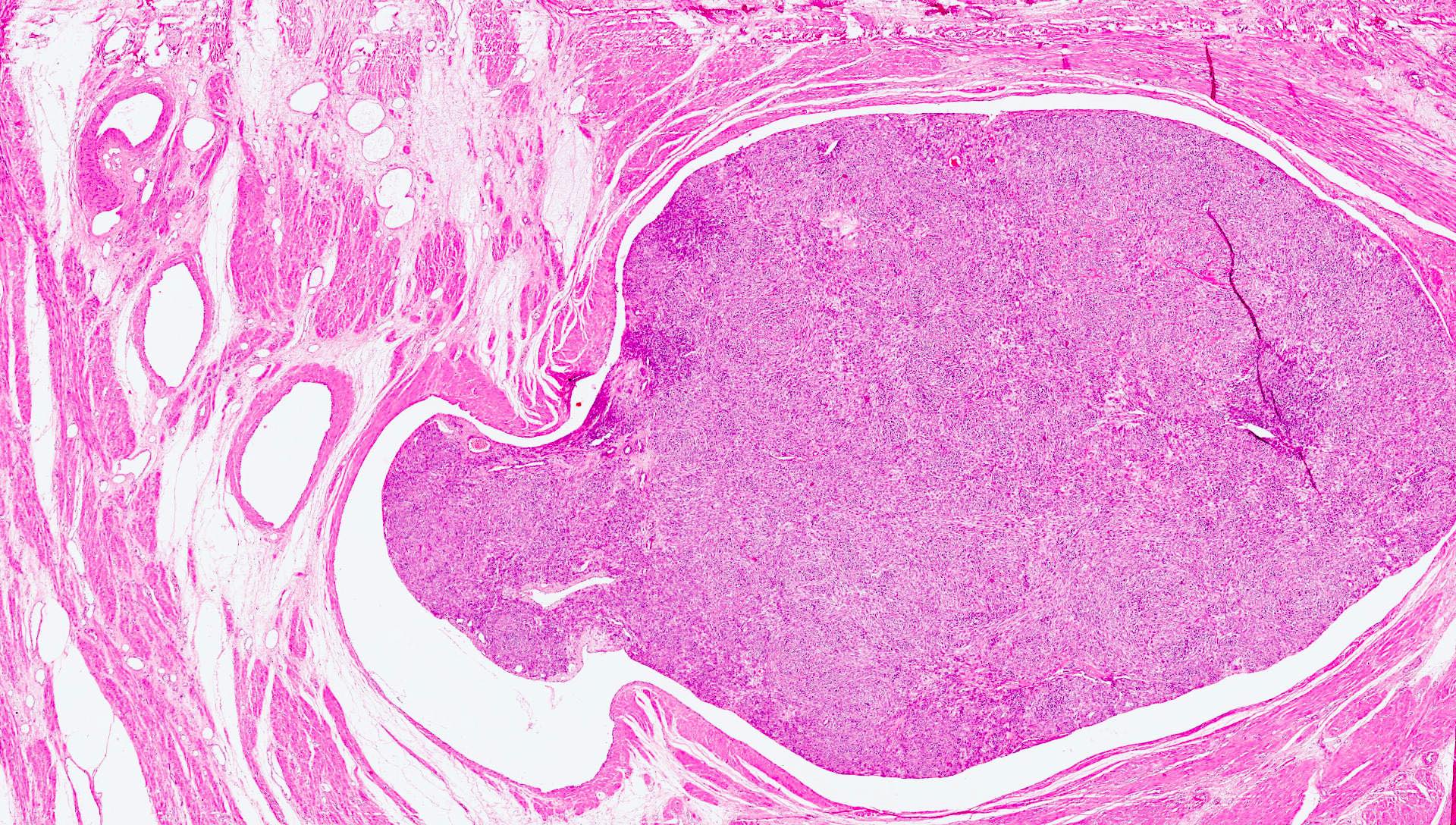
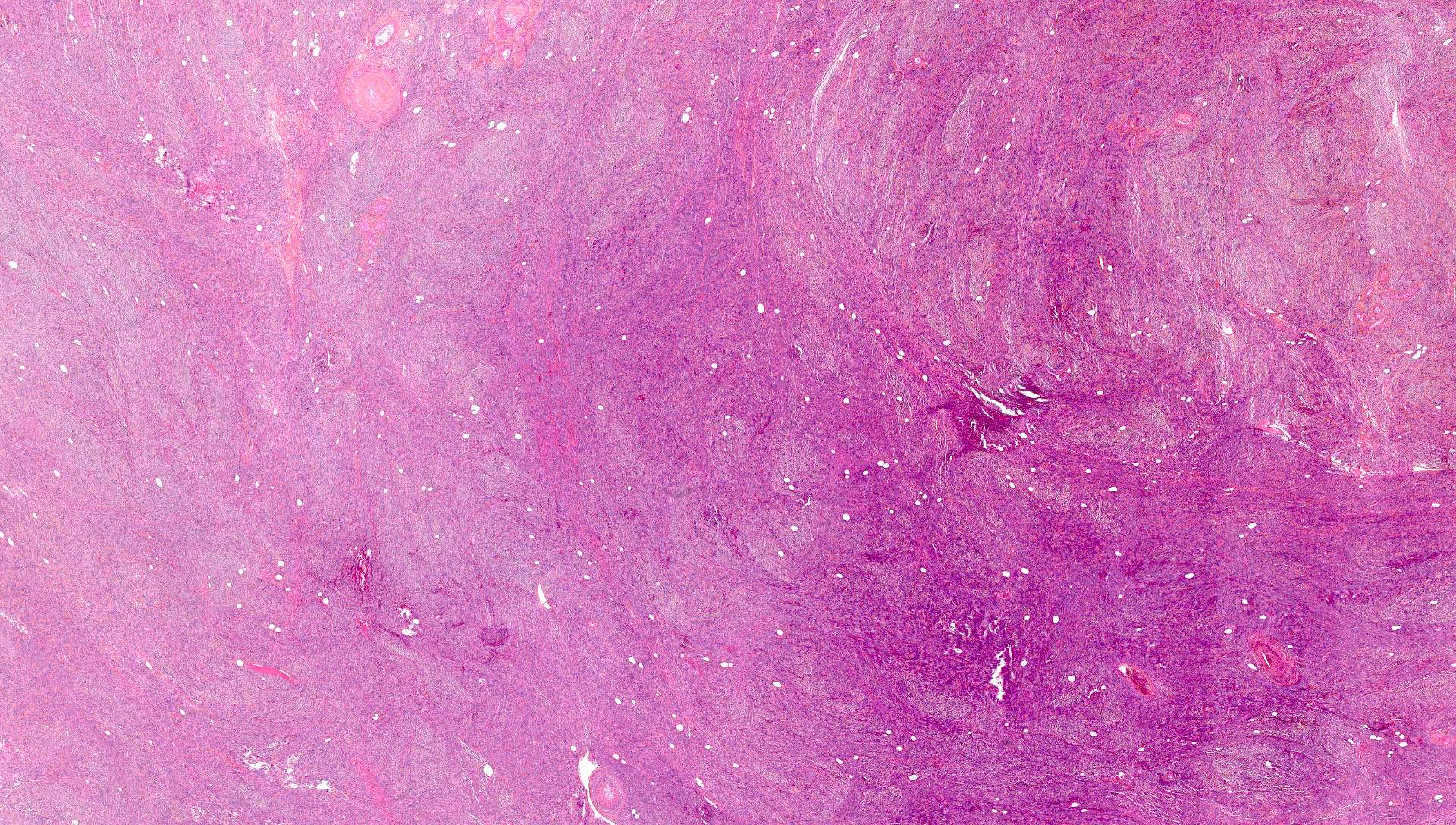
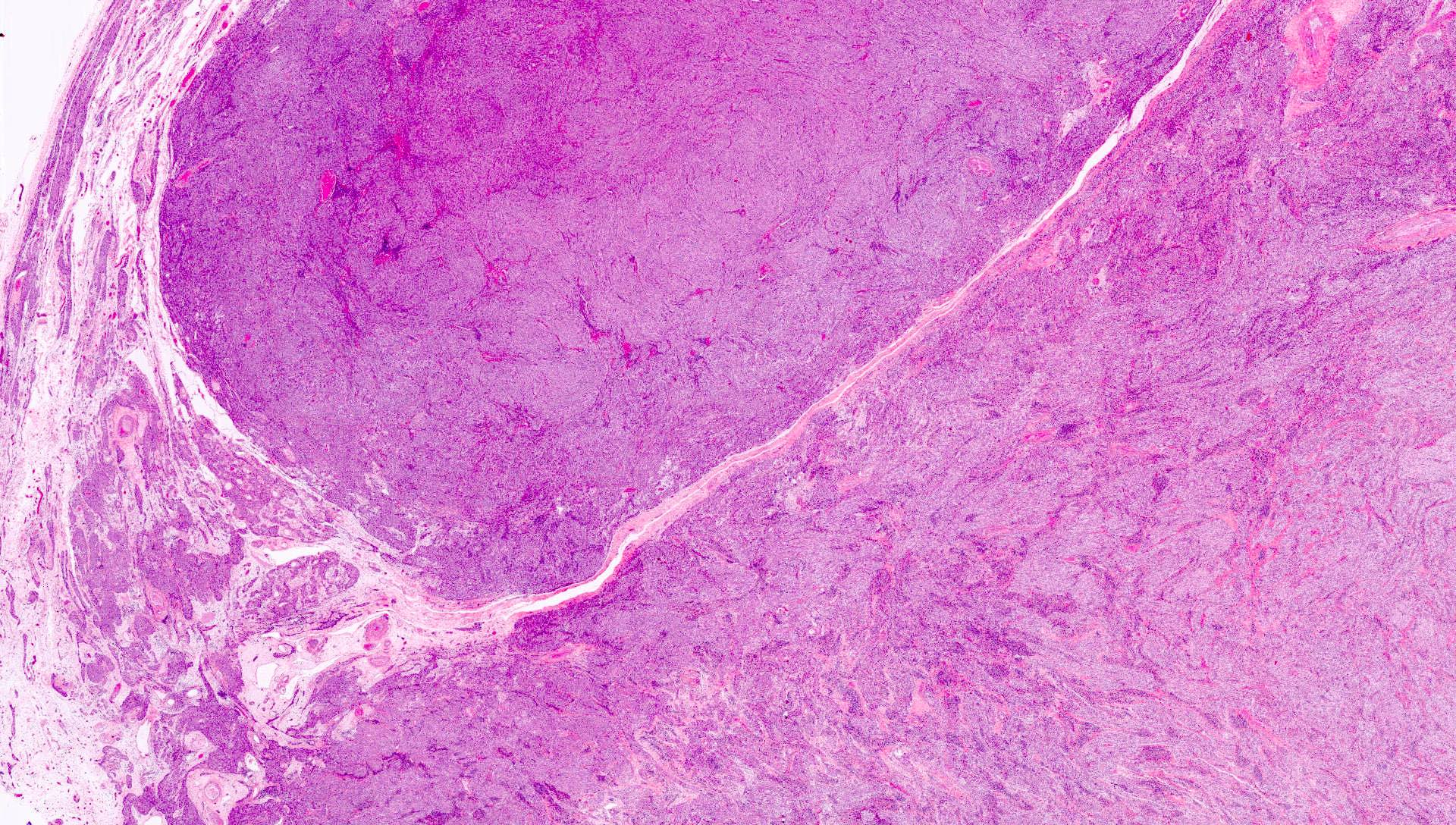
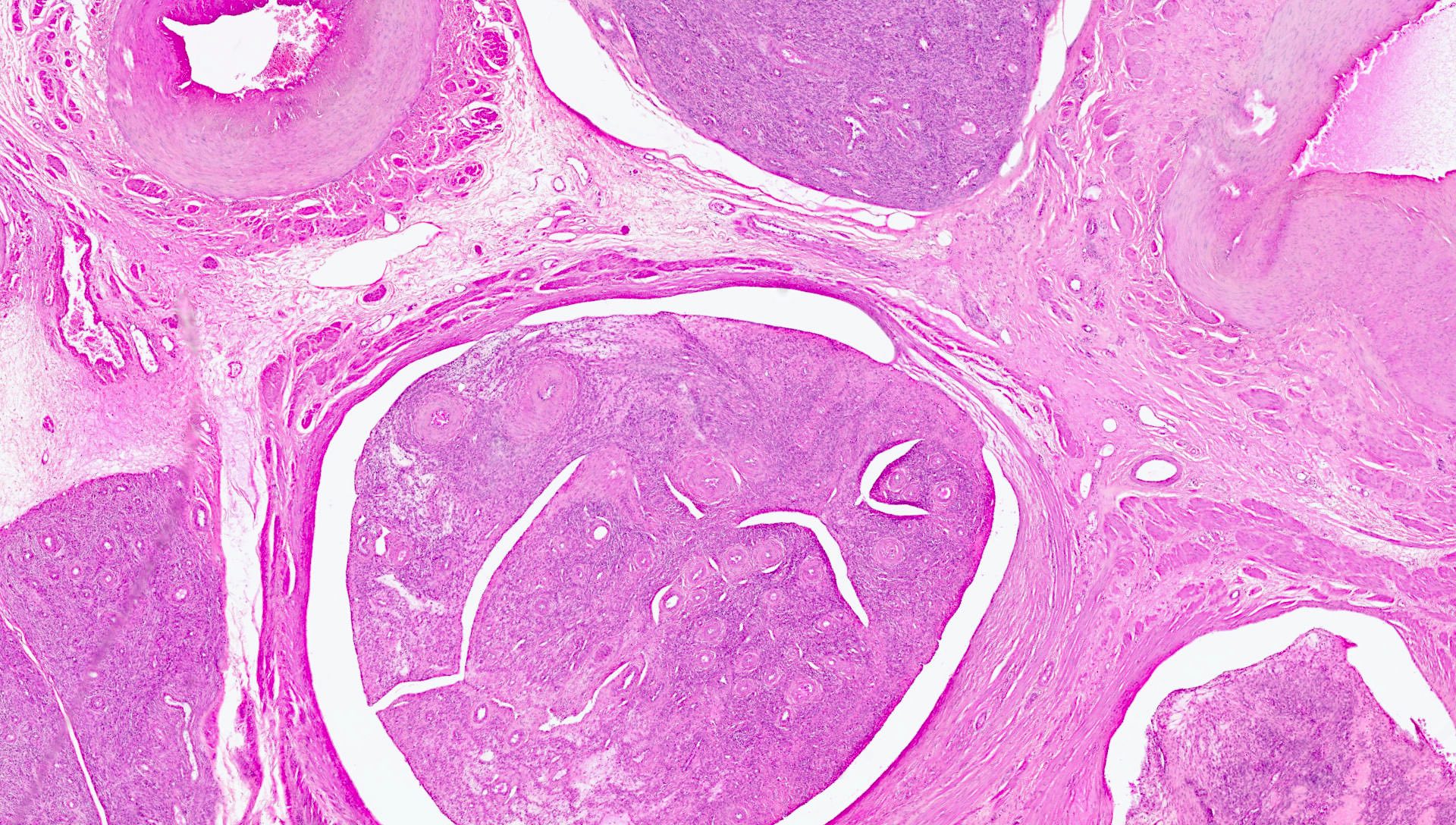
Microscopic (histologic) description
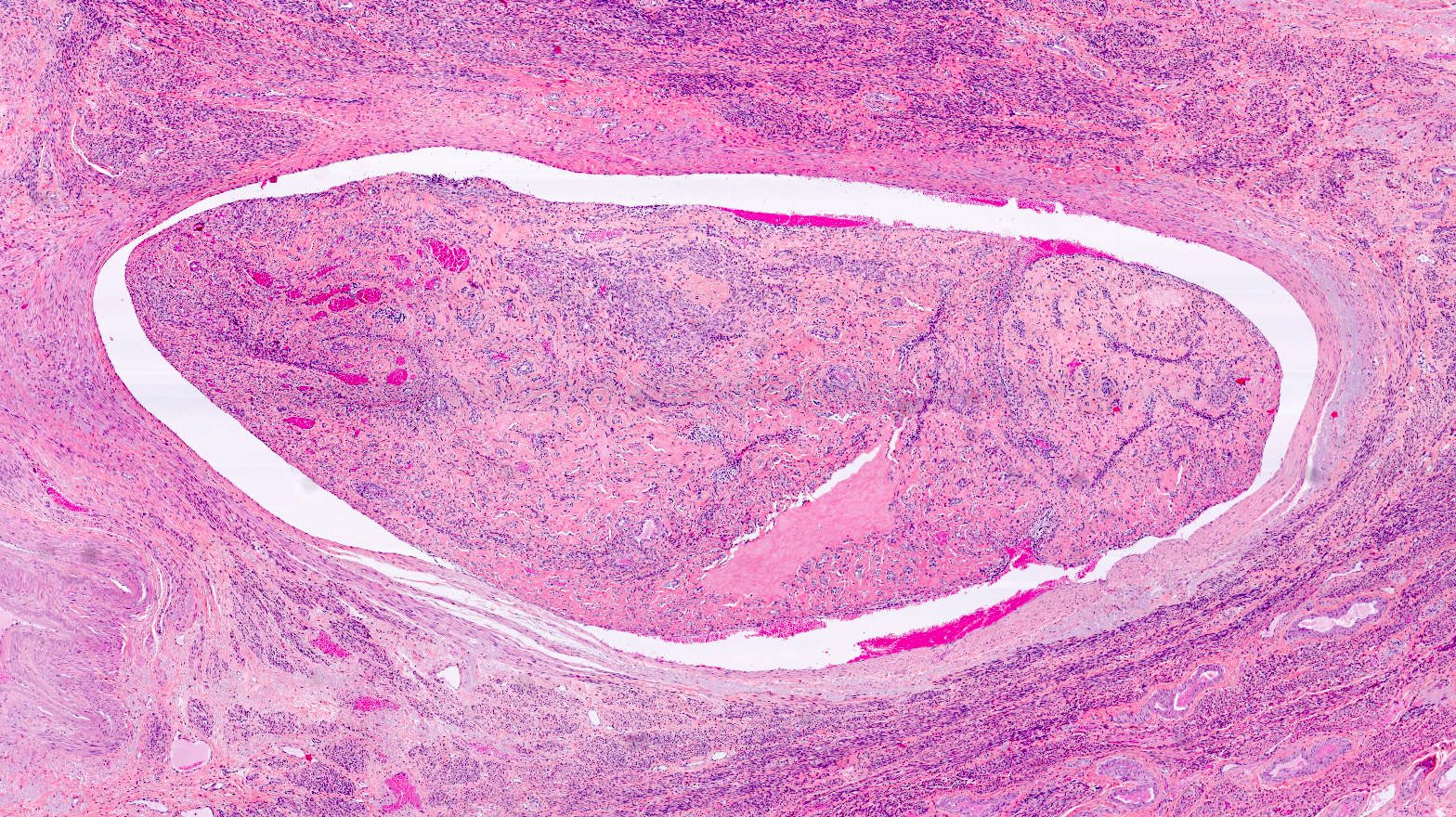
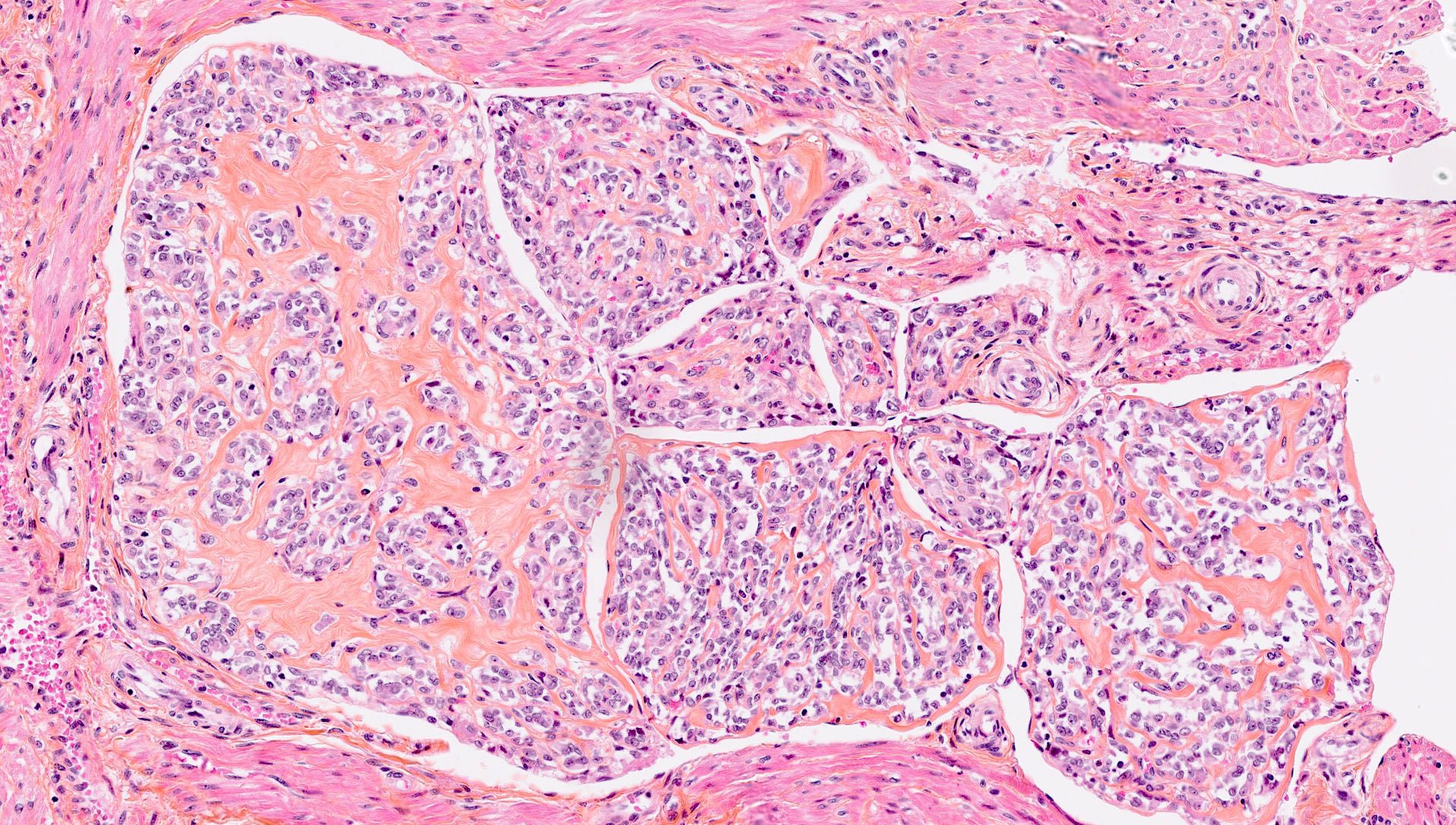
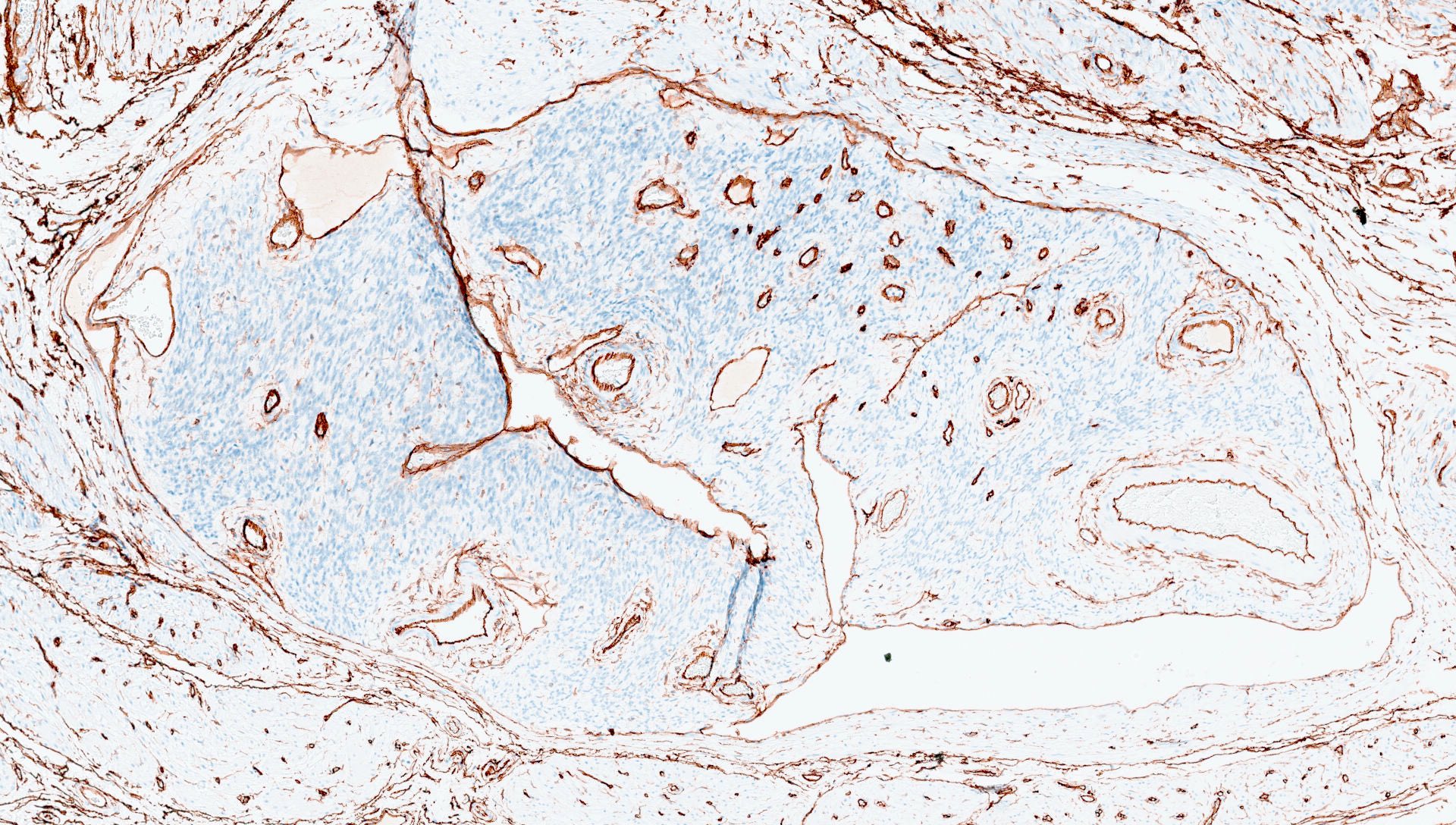
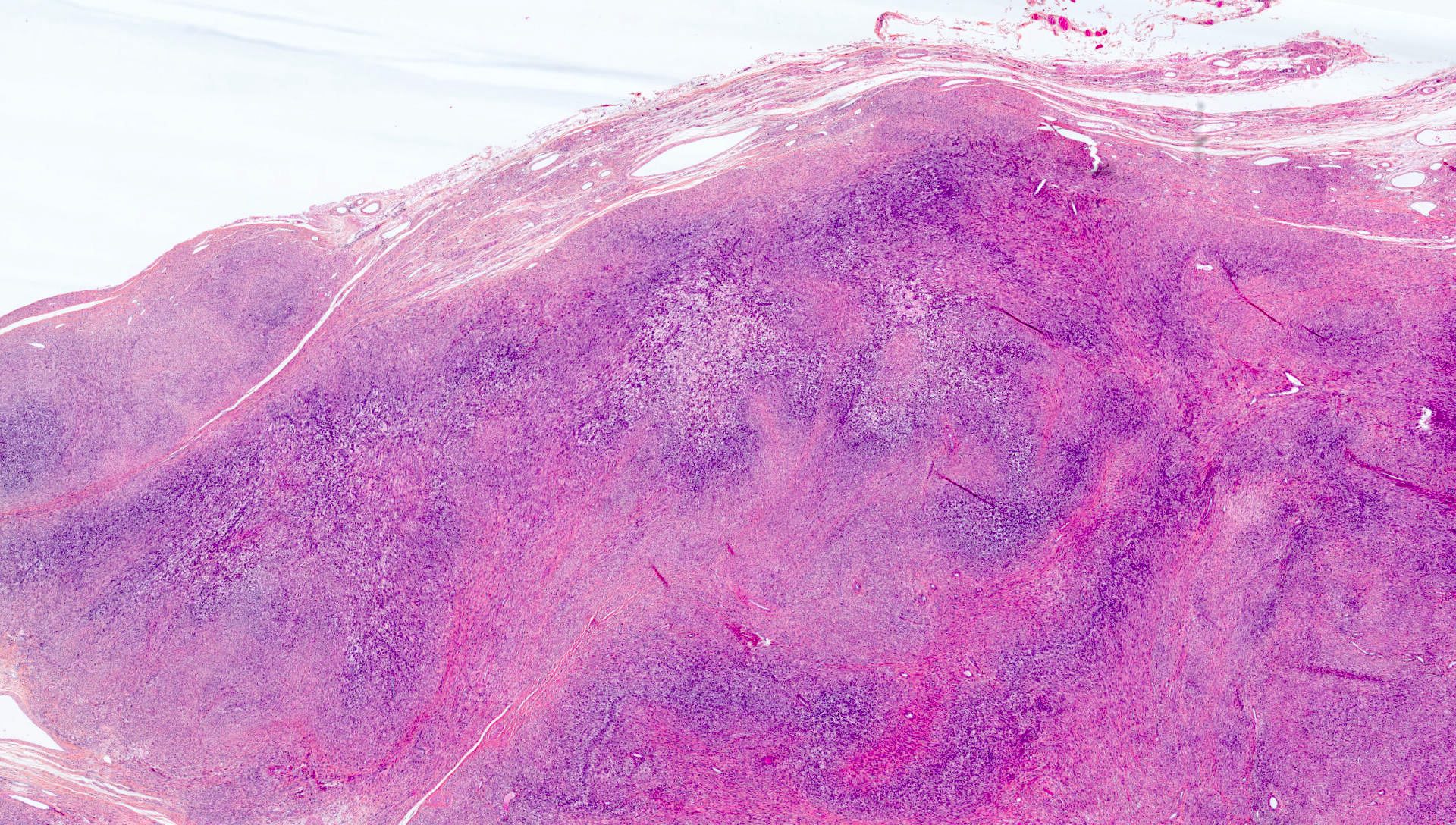
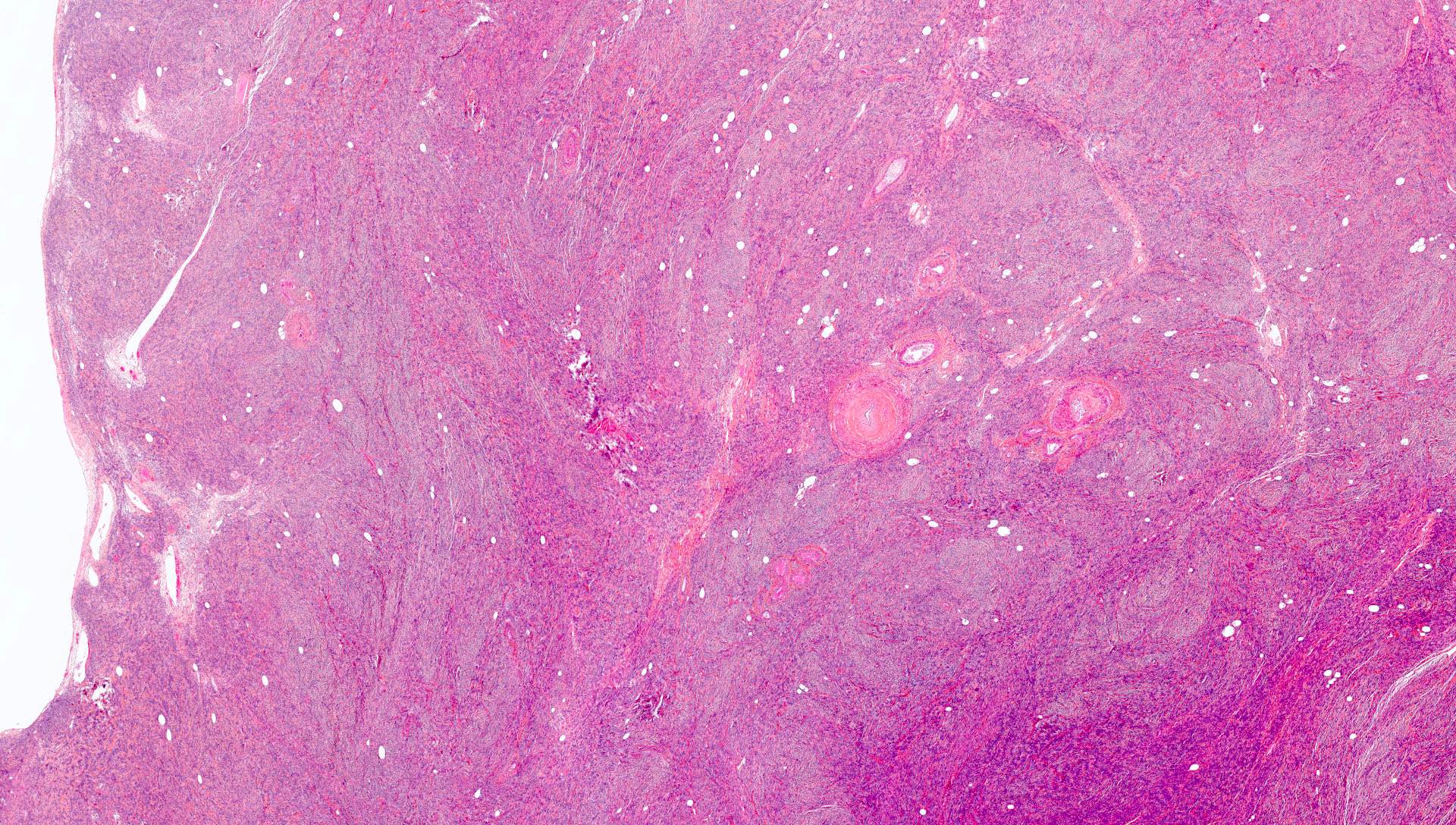
- Intravenous leiomyomatosis
- Nodules of smooth muscle cells growing in the venous lumina, lined by endothelial cells (Medicine (Baltimore) 2021;100:e24228)
- These nodules form polypoid protrusions that dilate the lumen and compress the vessel walls (Medicine (Baltimore) 2021;100:e24228)
- Attachment of the tumor on the vascular wall is infrequent but found in some cases (Pathol Res Pract 2018;214:871)
- Smooth muscle cells do not show cytologic atypia and are organized in fascicular, plexiform and storiform growth patterns
- Most cases show no or occasional mitotic figures (< 2/10 high power fields) (Pathol Res Pract 2018;214:871, Int J Gynecol Pathol 2015;34:169, Medicine (Baltimore) 2021;100:e24228, Am J Clin Pathol 2020;154:178)
- Some tumors contained numerous small, thick walled vessels (Pathol Res Pract 2018;214:871, Cancer 1975;36:2164)
- Hydropic degeneration (especially in young patients), hyaline and cystic degeneration and fibrosis have been described (Pathol Res Pract 2018;214:871, Medicine (Baltimore) 2021;100:e24228)
- Presence of a coexisting uterine leiomyoma has been estimated in 38.9 - 61.5% of cases; coexistence with adenomyosis has also been reported (Pathol Res Pract 2018;214:871, Hum Pathol 2011;42:1240)
- Cases containing admixed endometrial type glands or stroma (intravascular adenomyomatosis) have been reported (Hum Pathol 2022;120:18, Am J Surg Pathol 2013;37:1395)
- Several additional morphological variants have been reported (Hum Pathol 2011;42:1240, Pathol Res Pract 2011;207:131, Pathol Res Pract 2018;214:871, Hum Pathol 2022;120:18, Am J Surg Pathol 2013;37:1395)
- Cellular intravenous leiomyomatosis
- Epithelioid intravenous leiomyomatosis
- Myxoid intravenous leiomyomatosis
- Symplastic (bizarre nuclei) intravenous leiomyomatosis
- Intravenous leiomyomatosis with papillary-like contour
- Lipoleiomyomatous intravenous leiomyomatosis (intravenous lipoleiomyoma)
- Intravenous leiomyomatosis with plexiform features (intravenous adenomyomatosis)
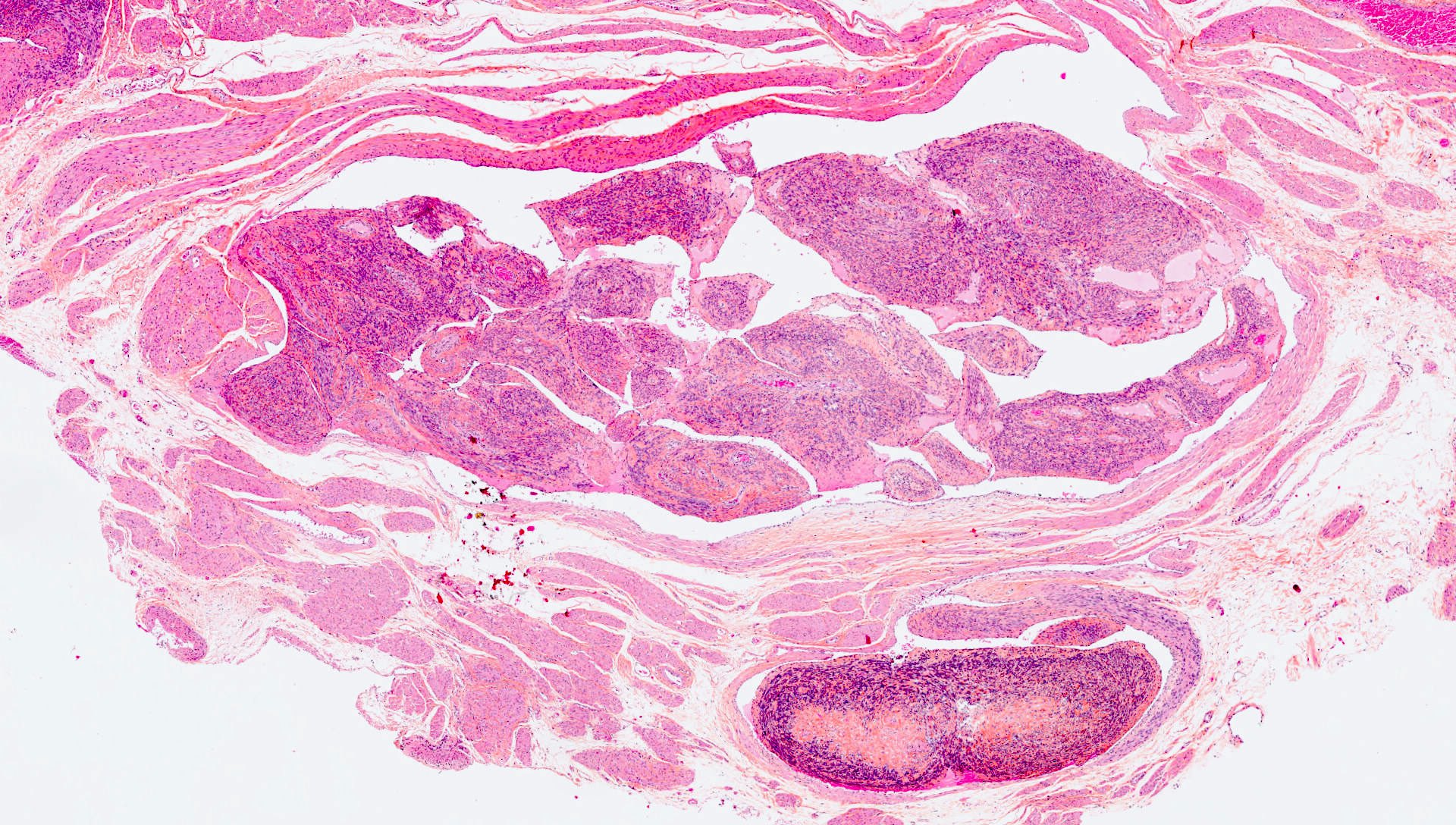
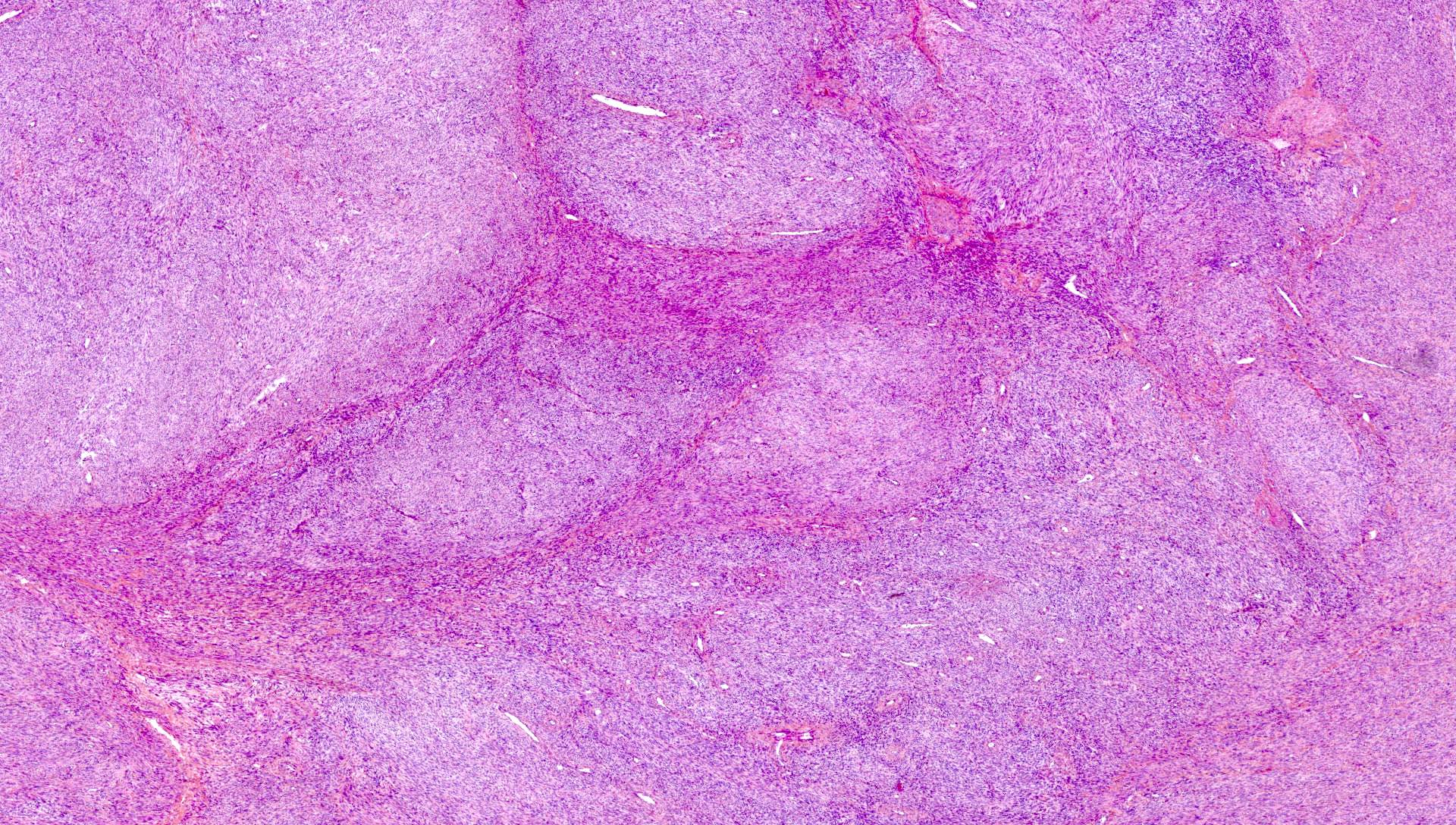
- Diffuse leiomyomatosis
- Replacement of the myometrium by innumerable poorly defined, confluent nodules, sometimes blending imperceptibly with the myometrium (Cureus 2022;14:e29595, Histopathology 1995;27:175)
- Some nodules within the proliferation may show more well defined contours
- No cytologic atypia and low mitotic activity (Cureus 2022;14:e29595, World J Clin Cases 2022;10:8797, Histopathology 1995;27:175)
- May show extensive plexiform morphology (Am J Clin Pathol 2020;154:178)
- Entrapped blood vessels may become distorted and elongated, mimicking intravenous leiomyomatosis; cases associated with intravenous leiomyomatosis have been described (Histopathology 1995;27:175)
Microscopic (histologic) images
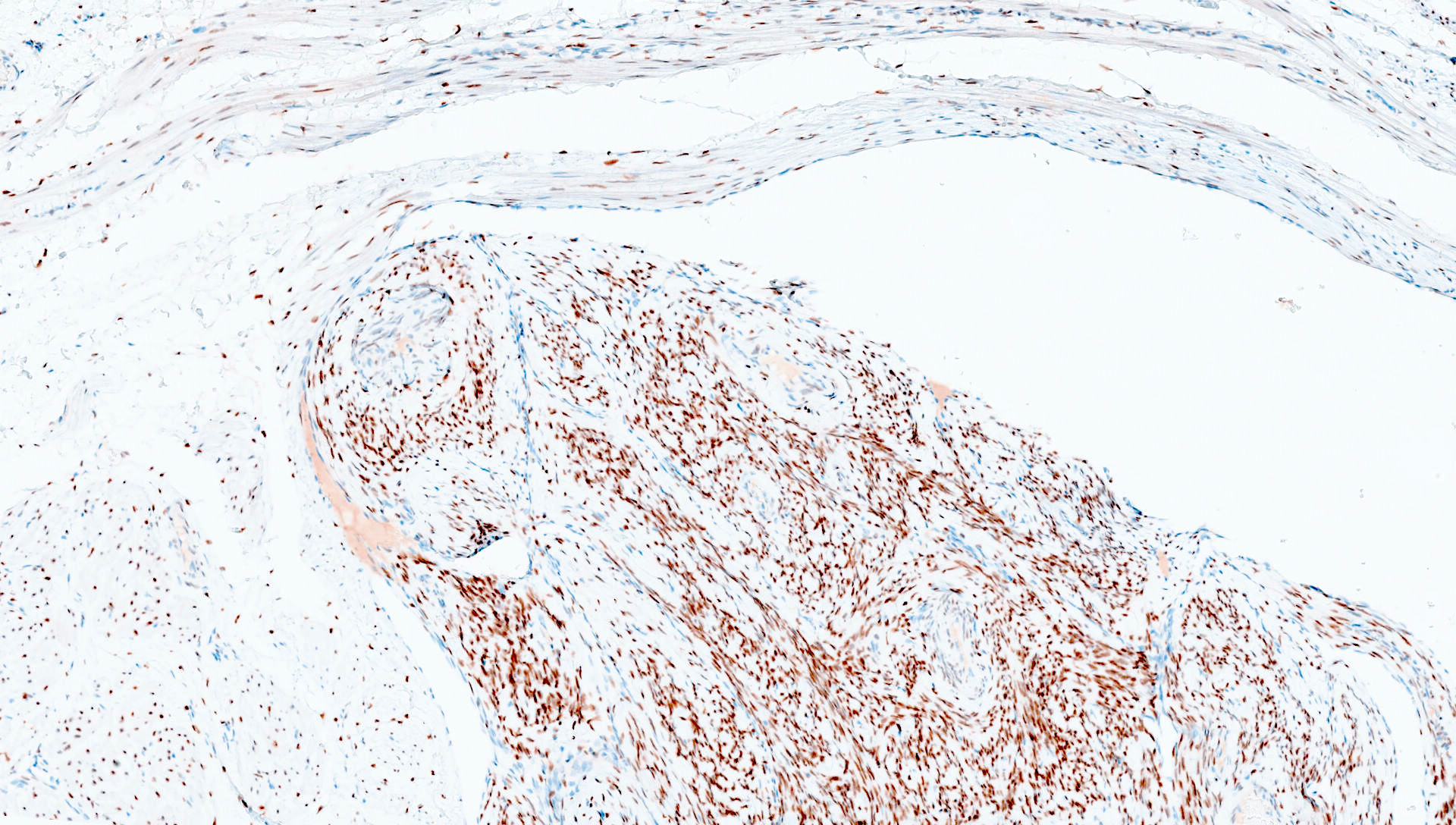
Positive stains
- Intravenous leiomyomatosis
- Desmin, caldesmon, smooth muscle actin and transgelin
- ER and PR (smooth muscle cells in the vascular wall are negative or weakly positive) (Pathol Res Pract 2018;214:871)
- CD10 (weakly positive in some cases and strongly positive in cases of intravascular adenomyomatosis) (Hum Pathol 2022;120:18)
- HMGA2 (58%) (Mod Pathol 2016;29:500)
- Ki67 ≤ 20%, with most cases presenting with scores of < 5% (Hum Pathol 2011;42:1240, Int J Gynecol Pathol 2015;34:169, Medicine (Baltimore) 2021;100:e24228, Front Surg 2023;9:1020004)
- Diffuse leiomyomatosis
- Desmin and smooth muscle actin
- ER and PR
- Ki67 low
Negative stains
Molecular / cytogenetics description
- Intravenous leiomyomatosis
- Some cases of intravenous leiomyomatosis demonstrate balanced translocations t(12;14)(q14-15;q23-24), commonly observed in uterine leiomyomas (Hum Pathol 2022;120:18, Mod Pathol 2016;29:500, Cancer Med 2020;9:4581)
- Breakpoint on 12q14-15 typically results in overexpression of HMGA2, as evidenced by high levels of HMGA2 staining
- HMGA2 overexpression and t(12;14)(q15;q24) likely have important roles in tumorigenesis but additional genetic alterations might explain the quasimalignant behavior of intravenous leiomyomatosis
- Recurrent 22q and 1p regional losses and 12q gains have been reported (Cancers (Basel) 2022;14:2907, Mod Pathol 2016;29:500, Int J Gynecol Pathol 2015;34:169)
- Unlike leiomyomas, MED12 mutations have been rarely reported in intravenous leiomyomatosis (Cancers (Basel) 2022;14:2907, Mod Pathol 2016;29:500, Int J Gynecol Pathol 2015;34:169)
- X chromosome inactivation analysis confirmed the monoclonal origin of intravenous leiomyomatosis (Mod Pathol 2002;15:351, Mod Pathol 2016;29:500)
- Comparative genomic hybridization analysis on a benign metastasizing leiomyoma of the lung and uterine intravenous leiomyomatosis suggested that these entities may represent different points from the same neoplastic continuum (Pathol Res Pract 2018;214:871, Mod Pathol 2002;15:351)
- RNA sequencing shows that intravenous leiomyomatosis appears to have higher expression of angiogenesis and antiapoptotic factors when compared to uterine leiomyomas (Cancer Med 2020;9:4581)
- These factors may be associated with the characteristic continuous extension growth and proliferation rate of intravenous leiomyomatosis
- Gene expression profile of intravenous leiomyomatosis is more complex than that of leiomyomas
- Comparative proteomic profiling study of intravenous leiomyomatosis and other smooth muscle tumors described the selective enrichment of coregulated splicing factors, which may be associated with distinct biological pathways (Cancers (Basel) 2022;14:2907)
- Some cases of intravenous leiomyomatosis demonstrate balanced translocations t(12;14)(q14-15;q23-24), commonly observed in uterine leiomyomas (Hum Pathol 2022;120:18, Mod Pathol 2016;29:500, Cancer Med 2020;9:4581)
- Diffuse leiomyomatosis
- X chromosome inactivation analysis of several nodules suggests a polyclonal origin (Hum Pathol 2000;31:1429)
Videos
Intravenous leiomyomatosis
Sample pathology report
- Uterus, hysterectomy:
- Intravenous leiomyomatosis (see comment)
- Comment: Microscopic examination reveals several tumor plugs inside dilated vessels. The tumor plugs are comprised of smooth muscle cells with a fascicular and plexiform architecture and are lined by endothelial cells. The mitotic activity is estimated at 2 mitoses/10 high power fields. No cytologic atypia or tumor cell necrosis is observed. The tumor plugs present with extension to the broad ligament vessels. Additionally, an intramural uterine leiomyoma is observed. Intravenous leiomyomatosis is a benign smooth muscle tumor, albeit with the potential for locoregional and distant recurrence. Clinical and imagiological correlation to determine the presence of intravenous extension beyond the uterus and broad ligament, as well as postoperative residual lesions, is advised. Close clinical follow up is recommended.
- Uterus, hysterectomy:
- Diffuse leiomyomatosis (see comment)
- Comment: Microscopic examination reveals numerous poorly circumscribed, coalescent nodules within the myometrium, composed of smooth muscle cells, organized into interlacing fascicles. The mitotic activity is estimated at 1 mitosis/10 high power fields. No cytologic atypia or tumor cell necrosis is observed. The morphology is consistent with diffuse leiomyomatosis.
Differential diagnosis
- Intravenous leiomyomatosis
- Uterine lymphangioleiomyomatosis:
- Rare, systemic disease
- Predominantly seen in young, reproductive age women
- Associated with TSC1 / TSC2 alterations and tuberous sclerosis complex
- Proliferation of bland spindle and epithelioid cells, along the lymphatic system
- Presence of variable positivity for HMB45 and MelanA (Am J Surg Pathol 2013;37:1395, Int J Gynecol Pathol 2020;39:227)
- Intimate association with the lymphatic system, not the venous system (Int J Gynecol Pathol 2020;39:227)
- Leiomyoma with vascular invasion:
- Presence of bulging or tumor plugs into blood vessels inside the confines of a leiomyoma, detected only under microscopic examination (Pathol Res Pract 2018;214:871, Cancer 1975;36:2164)
- No clinical significance and should not be diagnosed as intravenous leiomyomatosis (Hum Pathol 2011;42:1240)
- Dissecting (cotyledonoid) leiomyoma:
- Characterized by tongues and broad fascicles of smooth muscle cells, dissecting the myometrium
- May have varying degrees of hydropic change and numerous blood vessels (Hum Pathol 2011;42:1240)
- No atypia or necrosis
- No intravascular growth (Hum Pathol 2011;42:1240)
- Uterine leiomyosarcoma:
- Moderate / marked cytologic atypia, presence of tumor cell necrosis or numerous mitotic figures, including atypical mitosis
- Recurrences of intravenous leiomyomatosis may lead to suspicion of a missed diagnosis of a leiomyosarcoma
- Bland nuclear features, low mitotic activity and lack of tumor cell necrosis favor intravenous leiomyomatosis
- History of hysterectomy / myomectomies and histological review of previous uterine specimens (if possible) may also aid in the diagnosis
- Consultation services should be considered for difficult cases
- Low grade endometrial stromal sarcoma:
- Composed of cells resembling proliferative phase endometrium
- Infiltrative / permeative growth in the myometrium
- May be associated with lymphovascular invasion, with numerous intravascular tumor plugs, grossly detected
- Most cases show diffuse, strong expression of ER, PR, CD10 and IFITM1
- Immunohistochemical panel of at least 2 smooth muscle markers (desmin and caldesmon) and CD10 may be helpful in the differential diagnosis
- May show areas with smooth muscle differentiation, which may be positive for caldesmon, desmin, ER, PR and variably positive for CD10
- Searching for areas with the classical morphological and immunohistochemical features and molecular testing may aid in the diagnosis
- Differential diagnosis with intravenous leiomyomatosis may be challenging, especially with intravenous adenomyomatosis comprised only of endometrial stroma
- Uterine lymphangioleiomyomatosis:
- Diffuse leiomyomatosis
- Multiple leiomyomas:
- Asymmetrical involvement of the myometrium and sharp circumscription of the individual leiomyomas, unlike diffuse leiomyomatosis
- Intravascular leiomyomatosis:
- May also have a multinodular appearance
- Presence of coalescing nodules without associated intravascular involvement allows the diagnosis of diffuse leiomyomatosis
- Some cases of diffuse leiomyomatosis may present with concomitant intravenous leiomyomatosis
- Endometrial stromal sarcoma:
- Multinodular appearance and permeative growth may raise this differential diagnosis
- Morphological, immunohistochemical and molecular features allow for this diagnosis
- PEComatosis:
- Multiple PEComatous nodules in the uterus or other parts of the female genital tract, frequently associated with tuberous sclerosis complex (Surg Pathol Clin 2019;12:363)
- The few cases described presented with widespread, variably sized, discrete nodules (Diagn Pathol 2012;7:23)
- Expression of melanocytic markers (HMB45 or MelanA) and at least 1 smooth muscle marker (desmin, caldesmon or smooth muscle actin) (Surg Pathol Clin 2022;15:315)
- Multiple leiomyomas:
Additional references
- Zheng: Gynecologic and Obstetric Pathology, Volume 2, 1st Edition, 2019, Clement: Atlas of Gynecologic Surgical Pathology, 4th Edition, 2019, Oliva: Tumors of the Uterine Corpus and Trophoblastic Diseases, Series 4, 2019, Kurman: Blaustein's Pathology of the Female Genital Tract, 7th Edition, 2019, Surg Pathol Clin 2019;12:397
Board review style question #1
A 42 year old woman with metrorrhagia, abdominal pain and imaging findings suggestive of multiple leiomyomas was submitted to a hysterectomy. A representative microscopic image is shown above. Which of the following hypotheses is true?
- CD10 is consistently negative in these tumors
- High mitotic rates are frequently observed in these tumors
- These are benign tumors, without risk of spread beyond the uterus
- These lesions are associated with tuberous sclerosis complex
- These lesions may coexist with leiomyomas
Board review style answer #1
E. These lesions may coexist with leiomyomas. Presence of a coexisting uterine leiomyoma has been estimated to be 38.9 - 61.5% of cases. Answer D is incorrect because intravenous leiomyomatosis has not been associated with tuberous sclerosis complex, unlike lymphangioleiomyomatosis, an important differential diagnosis. Answer A is incorrect because CD10 is weakly positive in some cases and strongly positive in cases of intravascular adenomyomatosis. Answer B is incorrect because these tumors present with no or occasional mitotic figures (< 2/10 high power fields). Answer C is incorrect because intravenous leiomyomatosis is a benign tumor that may present with pelvic and extrapelvic spread along venous vasculature.
Comment Here
Reference: Intravenous and diffuse leiomyomatosis
Comment Here
Reference: Intravenous and diffuse leiomyomatosis
Board review style question #2
Which of the following observations is true regarding diffuse uterine leiomyomatosis?
- Cytologic atypia and high mitotic counts are typical of this tumor
- It is a benign condition with a relatively high risk of recurrence
- It is often characterized by an asymmetrical thickening of the myometrium
- Numerous well defined, confluent nodules are present in the myometrium
- X chromosome inactivation analysis suggests a polyclonal origin of the different nodules
Board review style answer #2
E. X chromosome inactivation analysis suggests a polyclonal origin of the different nodules. X chromosome inactivation analysis supports the hypothesis of an independent clonal origin of the different nodules (Hum Pathol 2000;31:1429). Answers C and D are incorrect because diffuse leiomyomatosis classically is characterized by a diffuse, symmetrical thickening of the myometrium with numerous poorly defined, confluent nodules. Answer B is incorrect because patients usually do not experience recurrence (only 2 cases of recurrence after conservative surgery have been reported). Answer A is incorrect because diffuse leiomyomatosis does not show significant cytologic atypia and only demonstrates low mitotic activity.
Comment Here
Reference: Intravenous and diffuse leiomyomatosis
Comment Here
Reference: Intravenous and diffuse leiomyomatosis