Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Yu YHS, Downes MR. Noninvasive papillary urothelial carcinoma high grade. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderhgpap.html. Accessed September 14th, 2025.
Definition / general
- Neoplastic proliferation of the urothelium with a papillary configuration and no invasion beyond the basement membrane
- Moderate to marked architectural and cytologic atypia
Essential features
- Noninvasive papillary urothelial neoplasm with moderate to marked cytoarchitectural abnormality
- Complex solid to fused papillary architecture, nuclear atypia, pleomorphism (may be focal), crowded and overlapping cells, brisk mitotic activity
- Immunohistochemistry not required for diagnosis
- Commonly presents with hematuria
- High rate of progression to invasion
Terminology
- Current 2016 WHO Classification: high grade
- Prior / older terminology - 1973 WHO classification: grade 2 and 3
- Overlap between WHO 1973 (grade 1, 2 and 3) and 2004 (low / high grade) nomenclatures
ICD coding
- ICD-O: 8130/2 - papillary transitional cell carcinoma, noninvasive
Epidemiology
- M:F = 6 - 8:1
- Median age: 70 years
Sites
- Most commonly found in posterior and lateral walls of bladder but may be found anywhere within urothelium
- 85% of urothelial neoplasms of renal pelvis are papillary and 66% of them are high grade (Mod Pathol 2005;18:11)
Pathophysiology
- Normal urothelium develops hyperplasia, dysplasia or carcinoma in situ as it acquires further genetic alterations: loss of chromosome 9, activating mutations in FGFR3 or RAS (Int J Clin Oncol 2008;13:287)
- Other mutations: PIK3CA, loss of 11p, CCND1, p53
Etiology
- Smoking (Int J Epidemiol 2016;45:857)
- Occupational exposure to chlorinated hydrocarbons, polycyclic aromatic hydrocarbons and aromatic amines (Eur Urol 2014;66:59)
- Arsenic exposure (Cancer Epidemiol Biomarkers Prev 2014;23:1529)
Clinical features
- Painless, intermittent hematuria
- Gross hematuria associated with more advanced pathologic stage (BJU Int 2016;117:783)
- Pure high grade carcinomas more aggressive than mixed high and low grade
- High rate of progression to invasive disease
Diagnosis
- Cystoscopy: exophytic lesion, solitary or multiple, with varying size
- Imaging: CT urography or ultrasound
- Urine cytology
Radiology description
- CT urography shows hydronephrosis and filling defects (Abdom Radiol (NY) 2018;43:663)
- Ultrasound can detect hydronephrosis and any intraluminal bladder masses
Prognostic factors
- WHO / ISUP histologic grade
- Nuclear anaplasia: decreased time to recurrence and progression
- Concomitant urothelial carcinoma in situ: higher recurrence rate
- Multifocal disease: higher disease associated mortality and progression
- High Ki67 poor prognosis (Int J Mol Sci 2018;19:2548)
- PTEN deletions: increased recurrence rate (Virchows Arch 2018;472:969)
- TP53 and RB alternations: adverse histopathological parameters (Anticancer Res 2018;38:3985)
Case reports
- 64 year old woman with high grade noninvasive papillary urothelial carcinoma develops Poncet disease (rare, nondestructive parainfective symmetric polyarthritis) after intravesical Bacillus Calmette-Guérin treatment (BMC Res Notes 2017;10:416)
- 69 year old woman with high grade noninvasive urothelial carcinoma of bladder later metastatic to uterus (Int J Gynecol Pathol 2017;36:493)
- 24 cases of noninvasive urothelial carcinoma of bladder with glandular differentiation (Am J Surg Pathol 2009;33:1241)
Treatment
- Surgical: transurethral resection of tumor
- Adjuvant therapy:
- Intravesical immunotherapy with Bacillus Calmette-Guérin
- Intravesical chemotherapy with thiotepa or mitomycin C
Gross description
- Exophytic single or multiple lesions with variation in size
- More likely nontranslucent and hyperemic than low grade lesions
Frozen section description
- Papillary architecture with nuclear pleomorphism, dyscohesion and mitotic activity
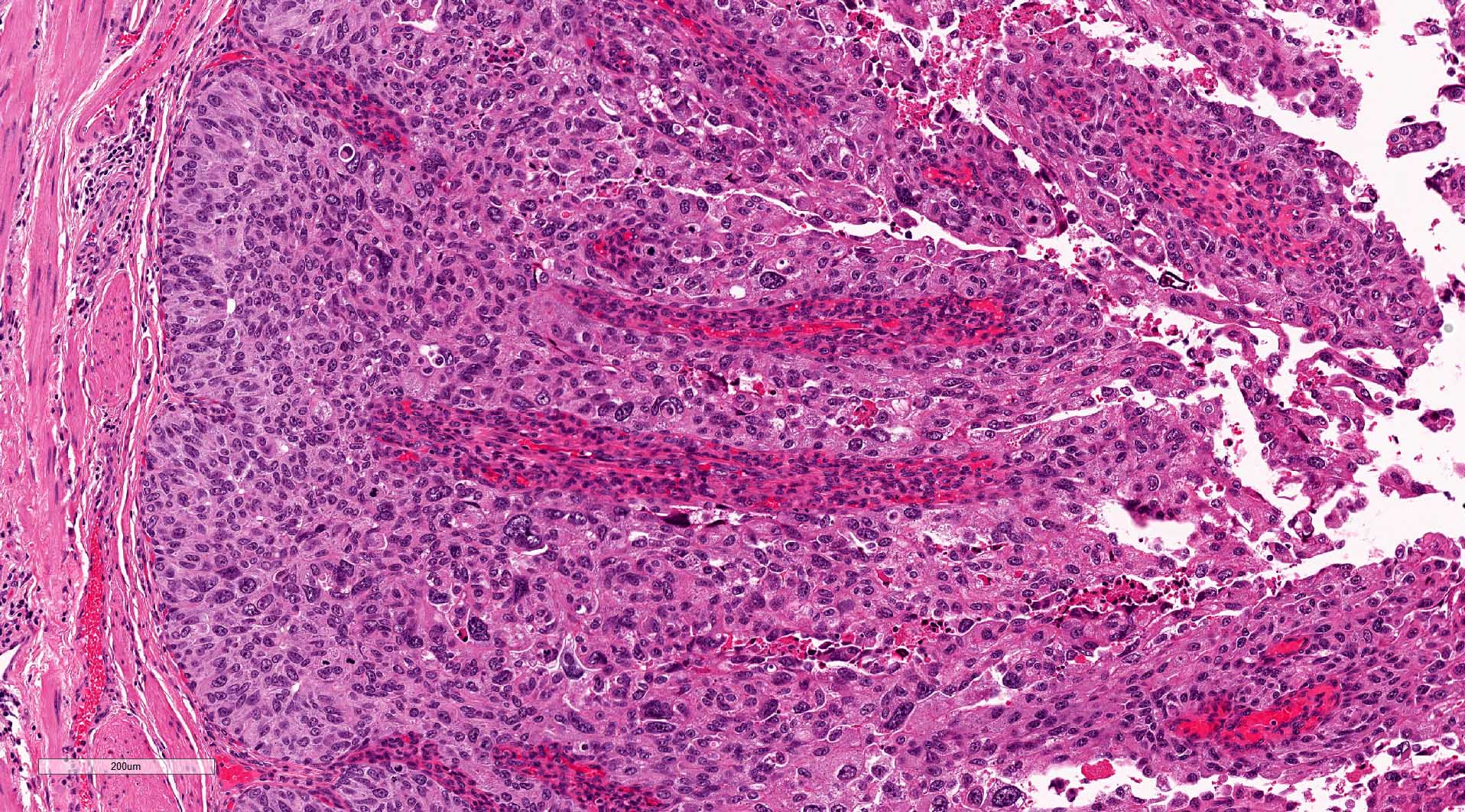
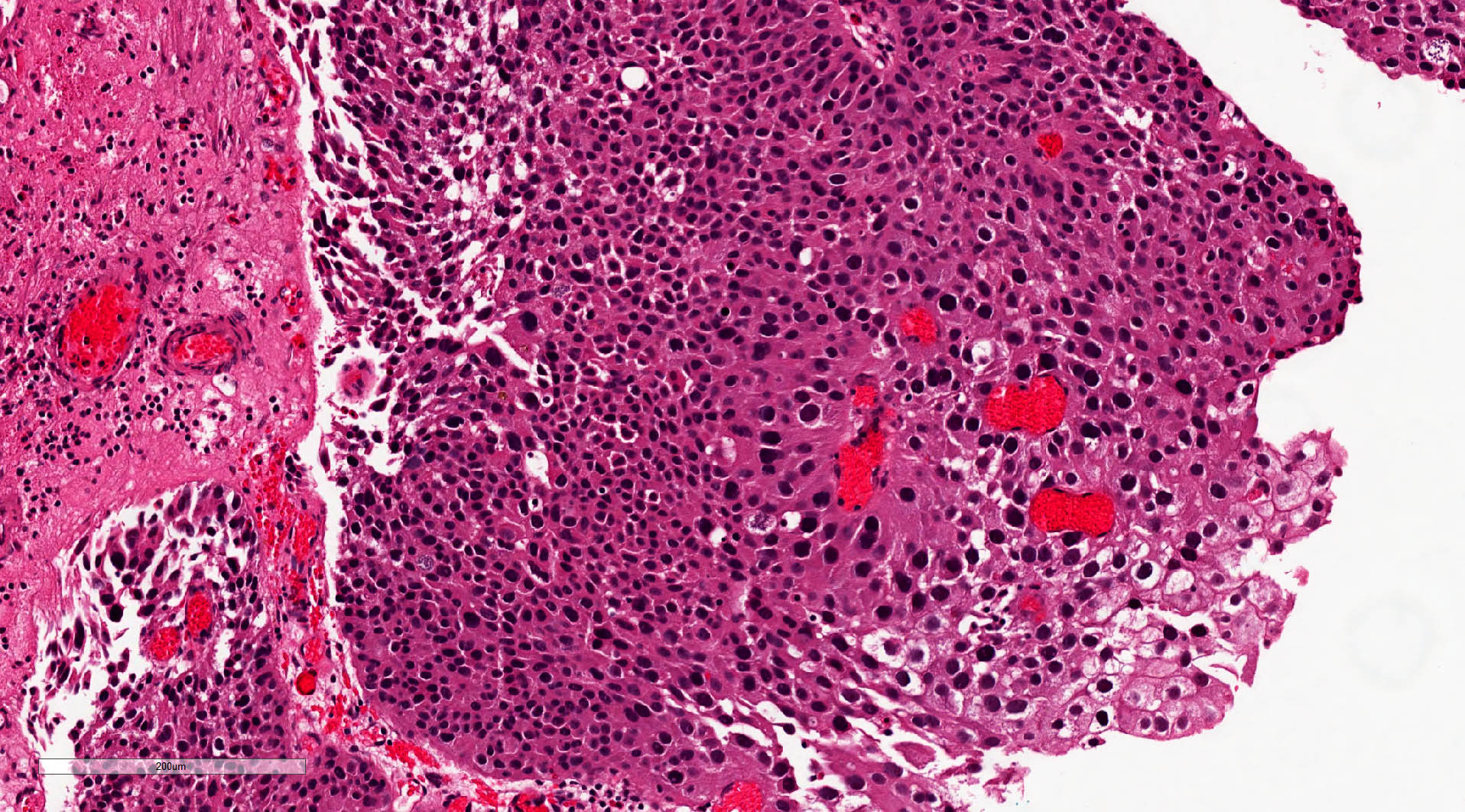
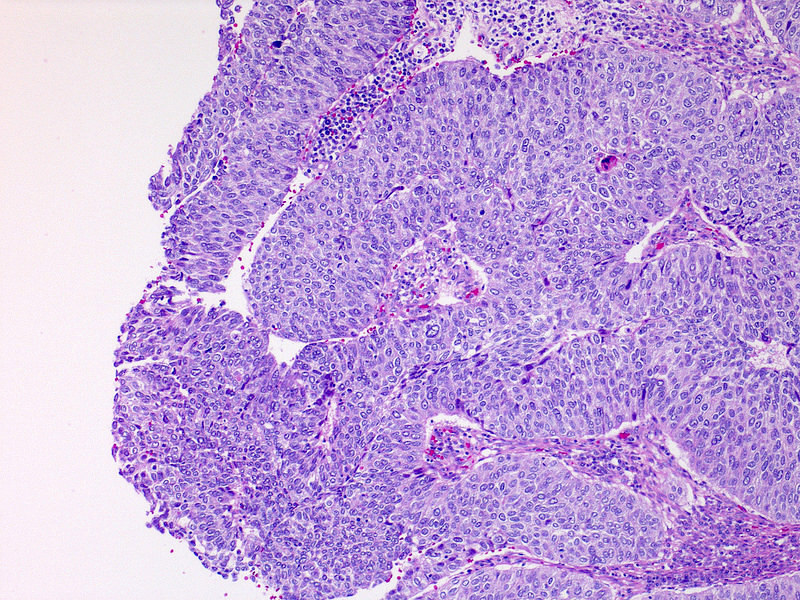
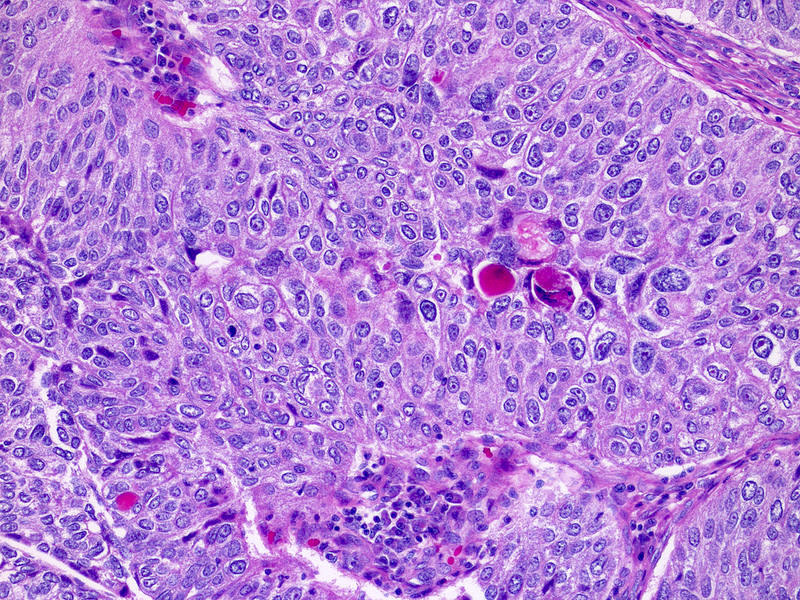
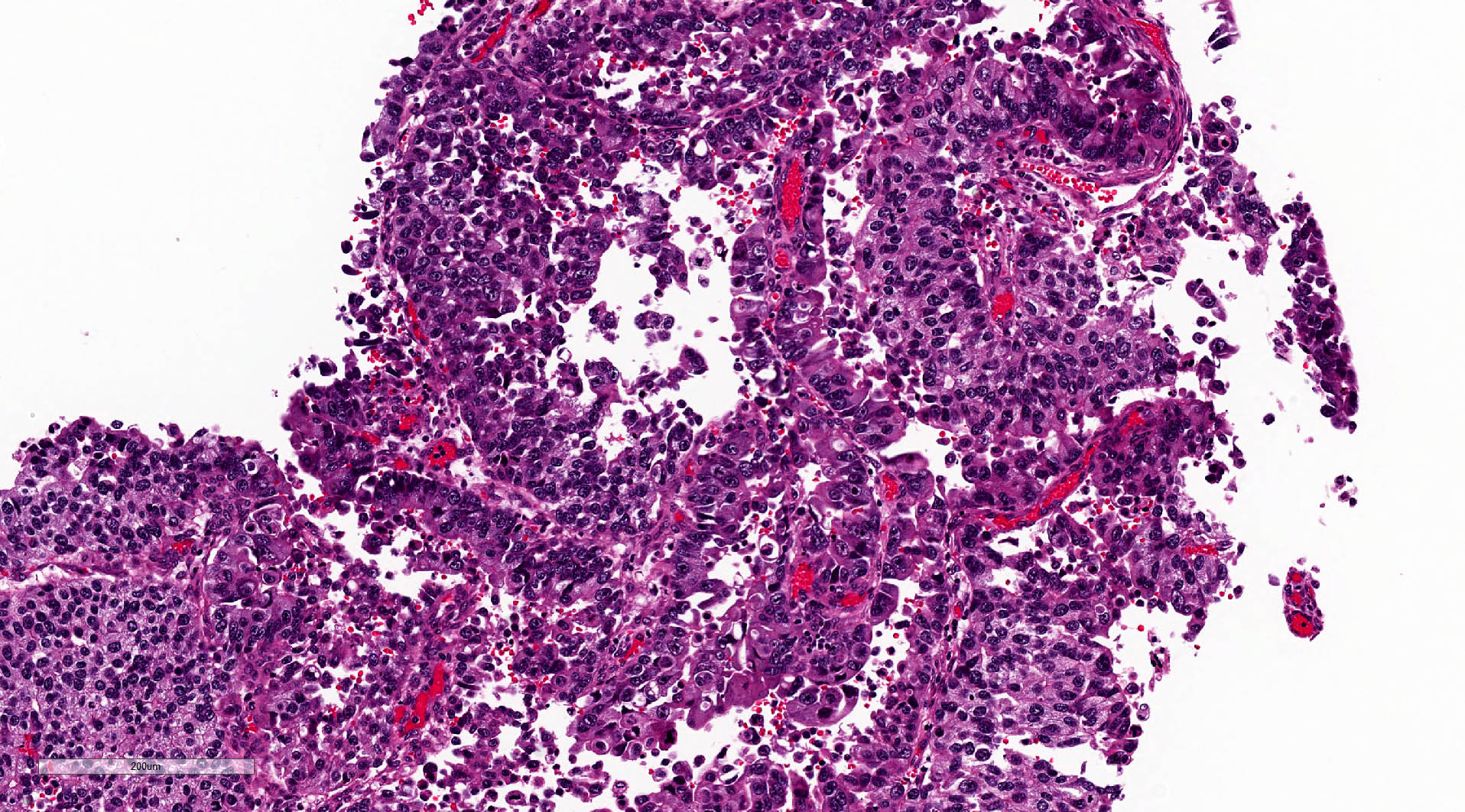
Microscopic (histologic) description
- Fibrovascular cores lined by neoplastic urothelium
- Complex, solid to fused papillae common
- Architectural disorder; nuclear pleomorphism readily visible at low and intermediate power
- Crowded overlapping cells, dyscohesion common and partial denudation
- Nucleomegaly present, irregular and clumped chromatin
- Frequent prominent nucleoli and mitoses (brisk and maybe atypical)
- Concomitant low grade carcinoma may be present
- Inverted growth pattern may coexist (both exophytic and endophytic growth)
- Reference: Mod Pathol 2009;22:S60
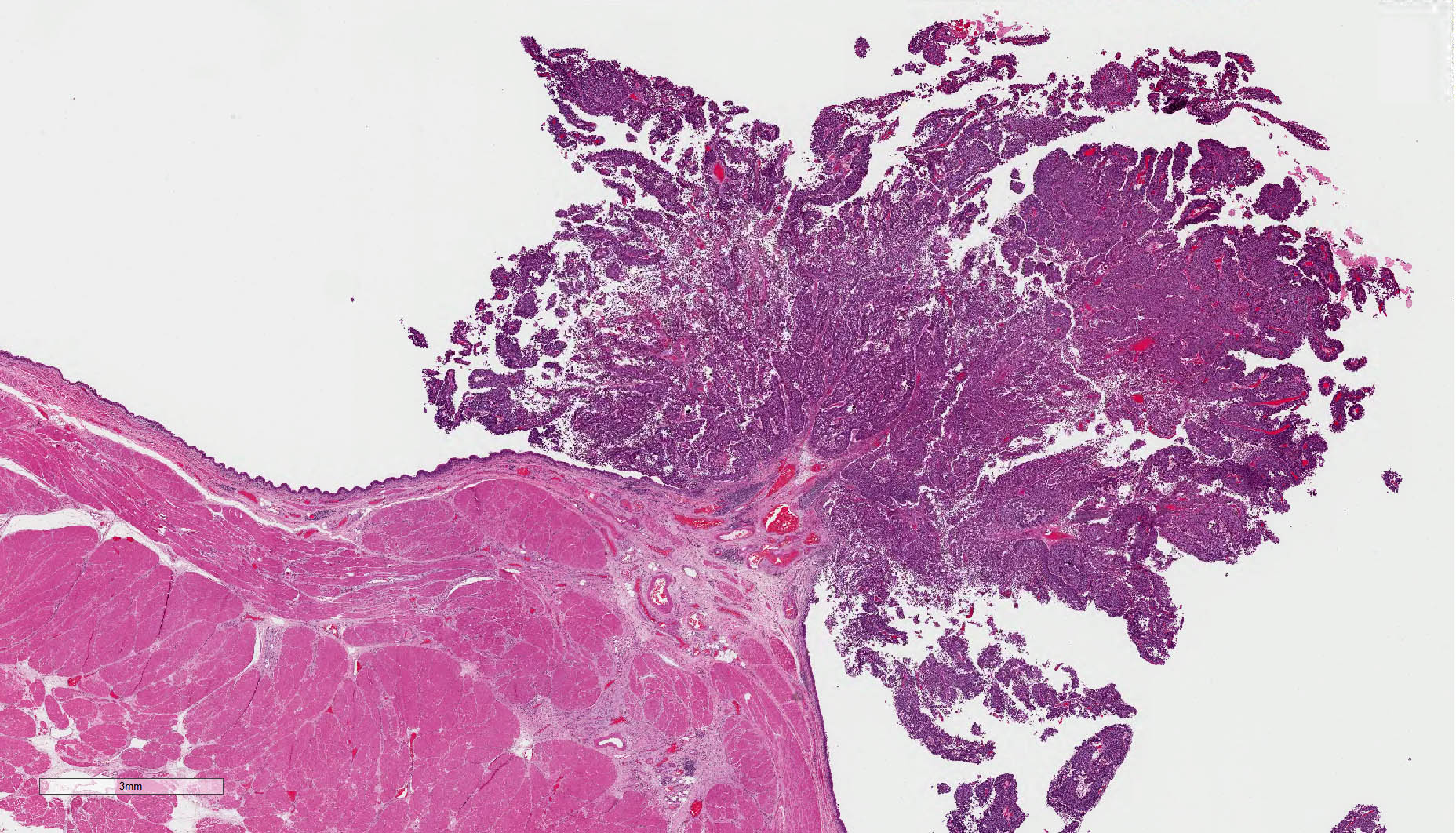
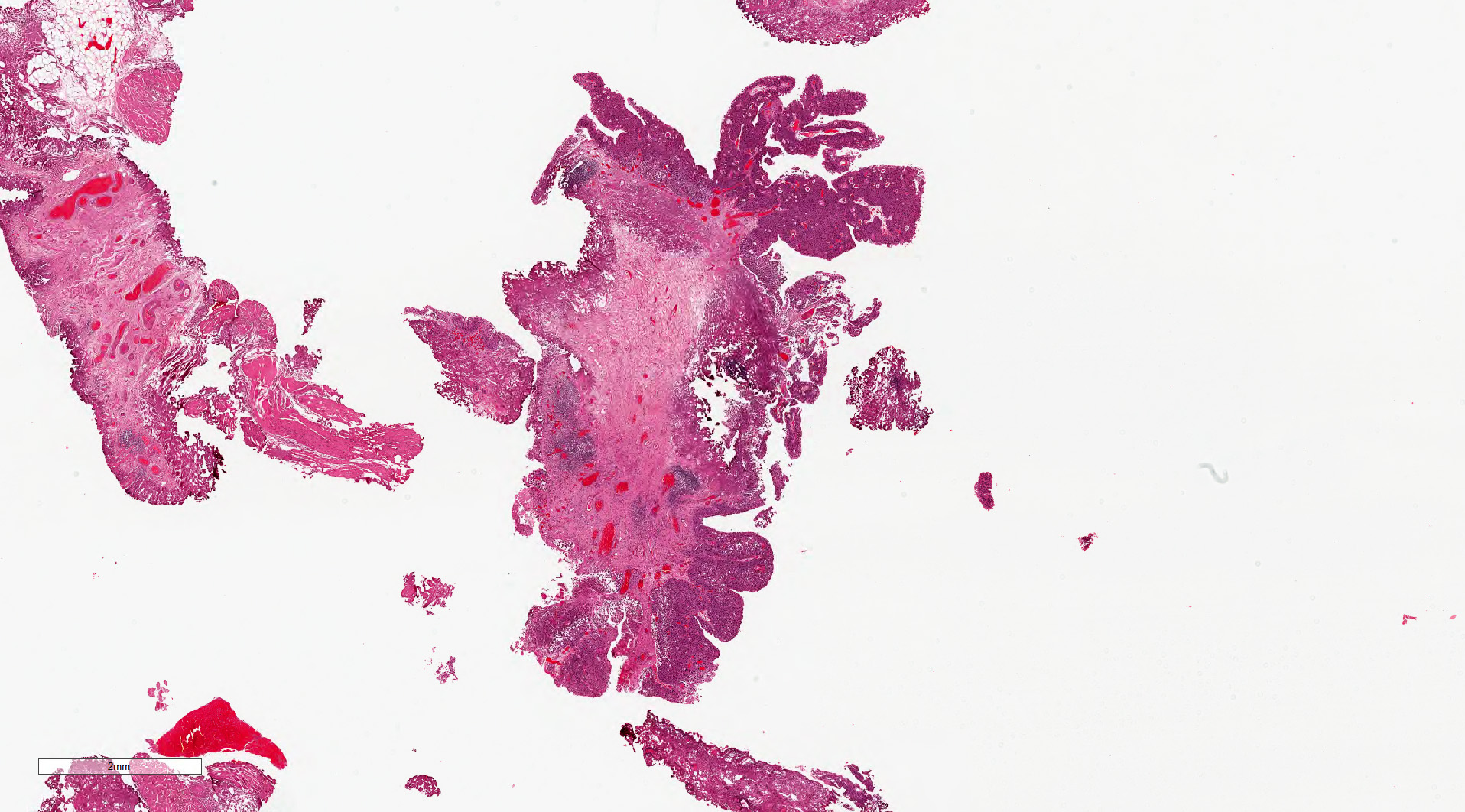
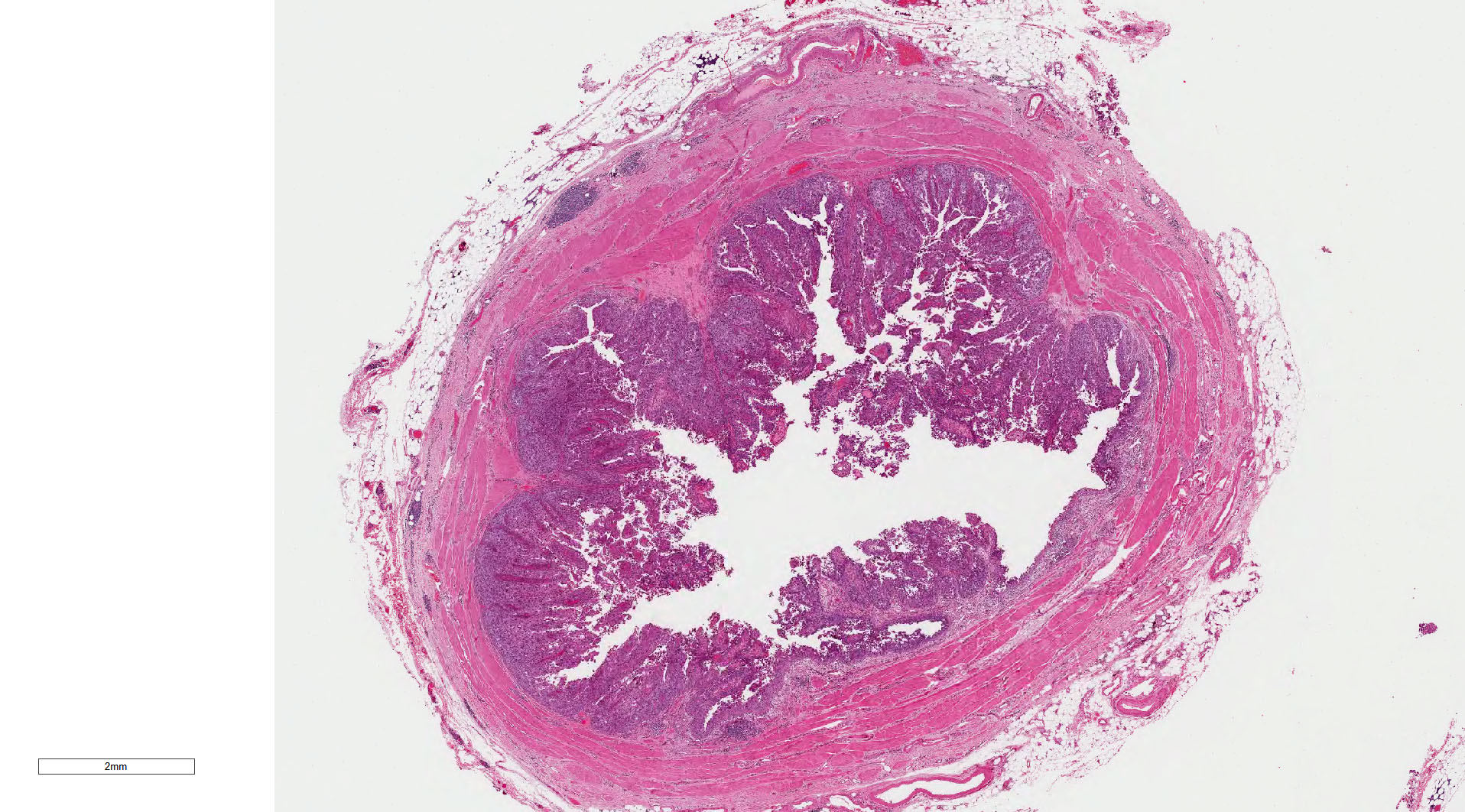
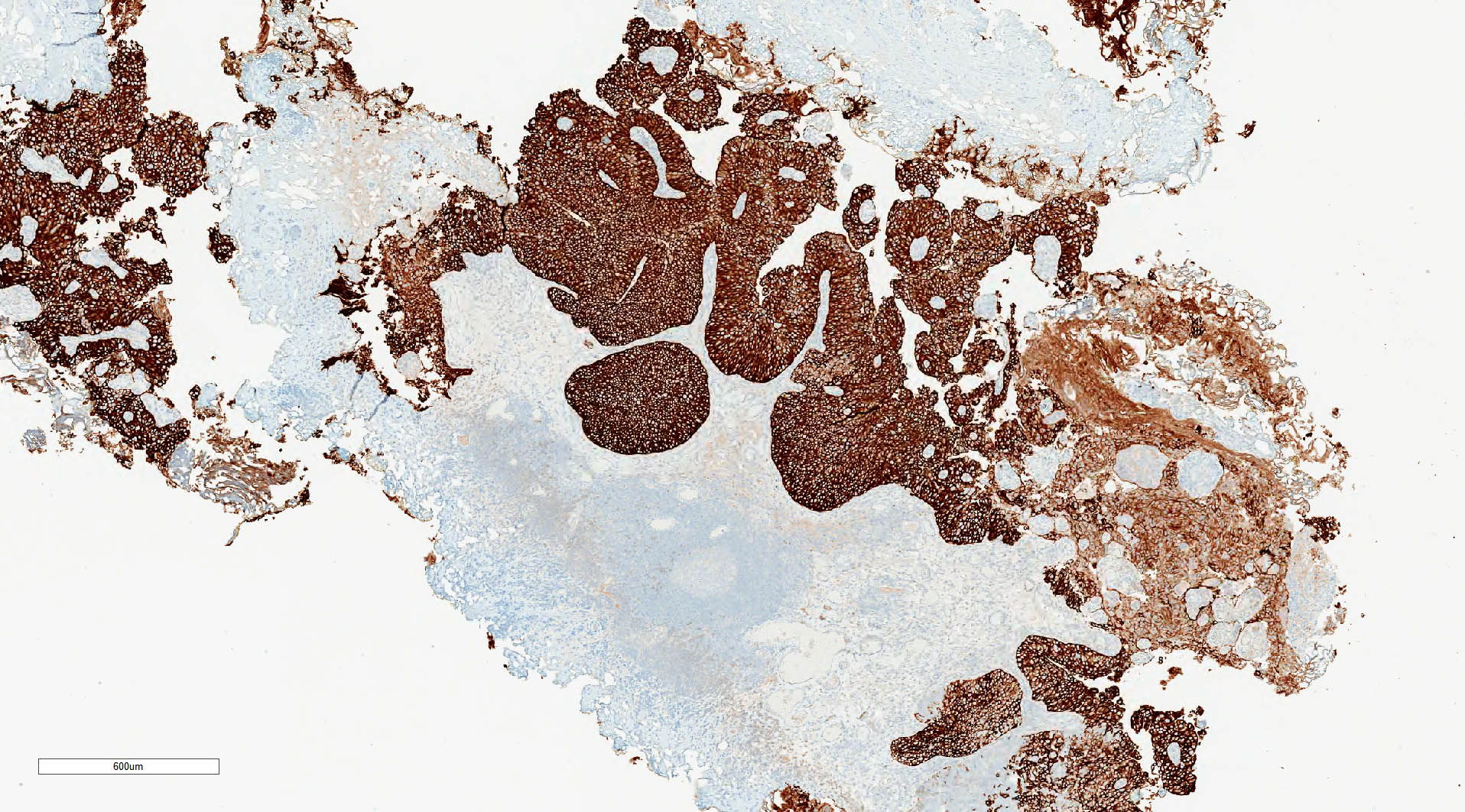
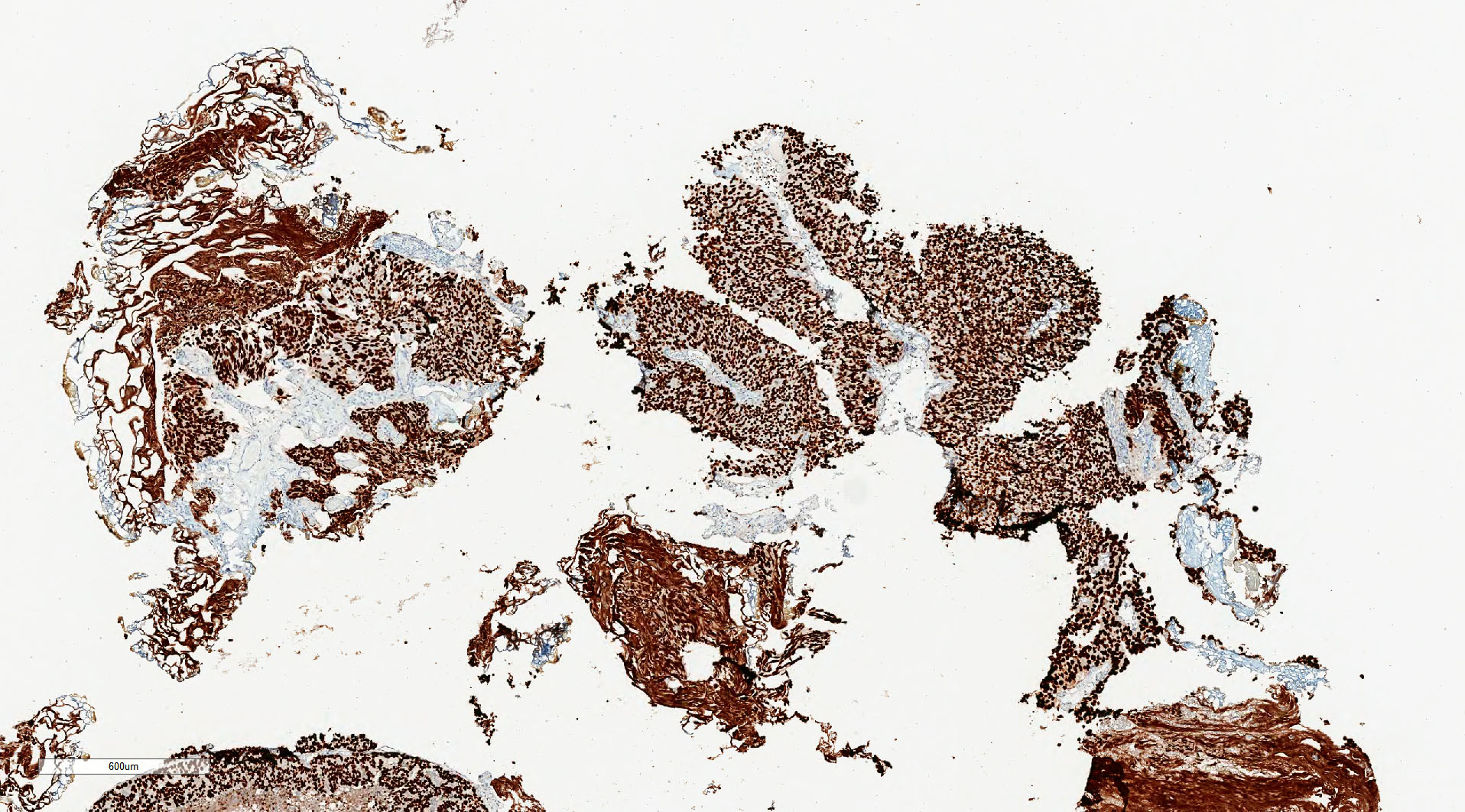
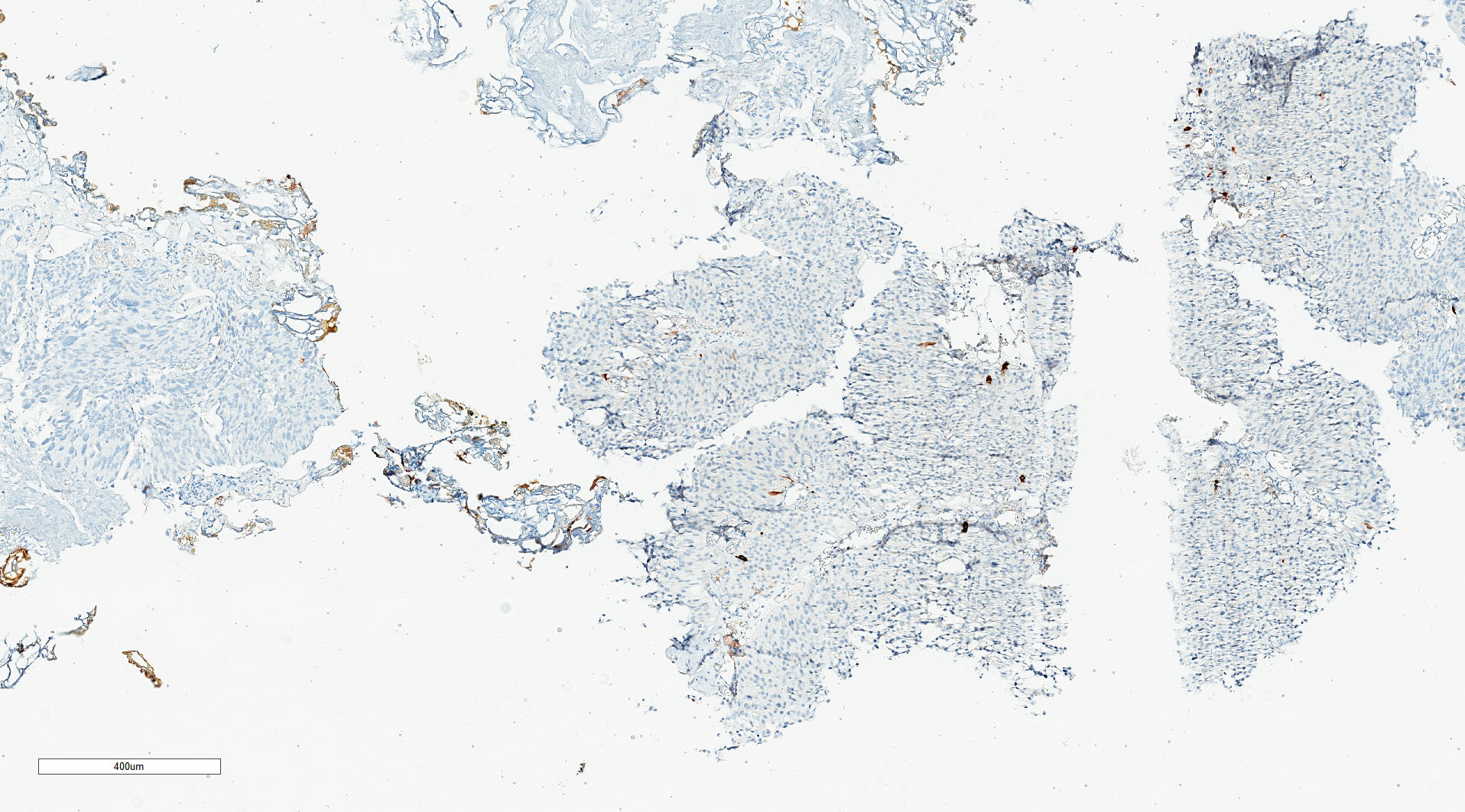
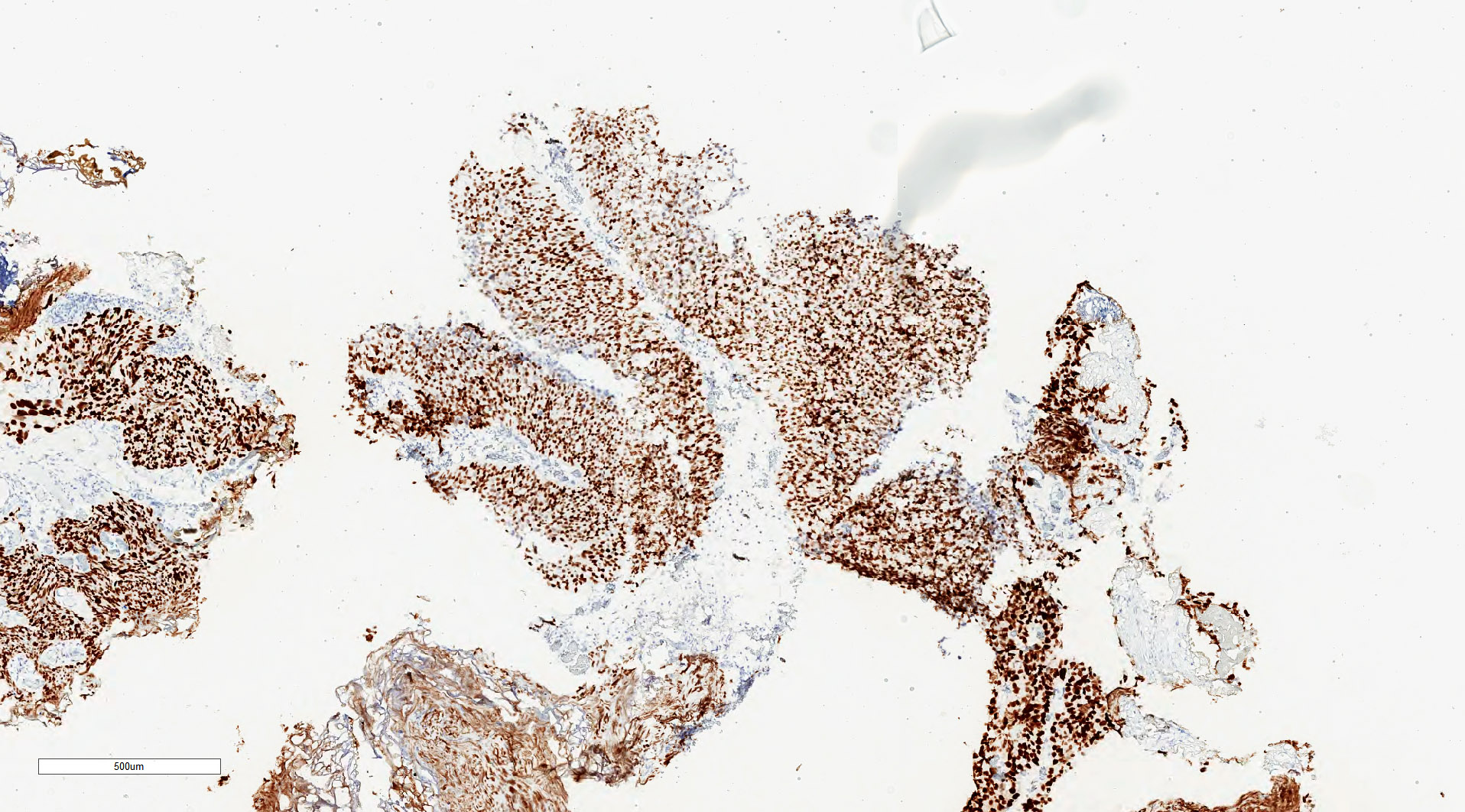
Microscopic (histologic) images
Contributed by Michelle R. Downes, M.D., Nicole K. Andeen, M.D. and Maria Tretiakova, M.D.
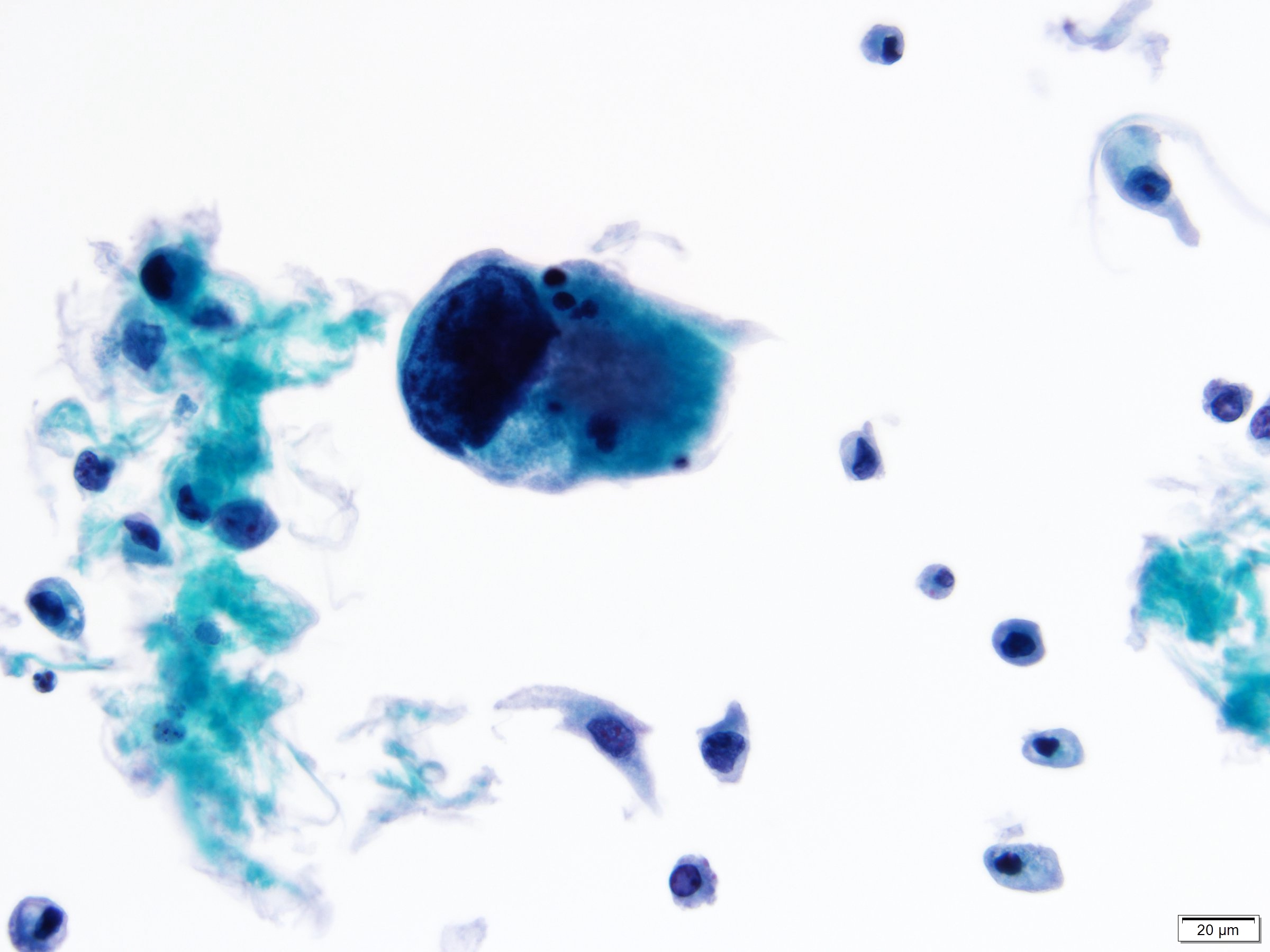
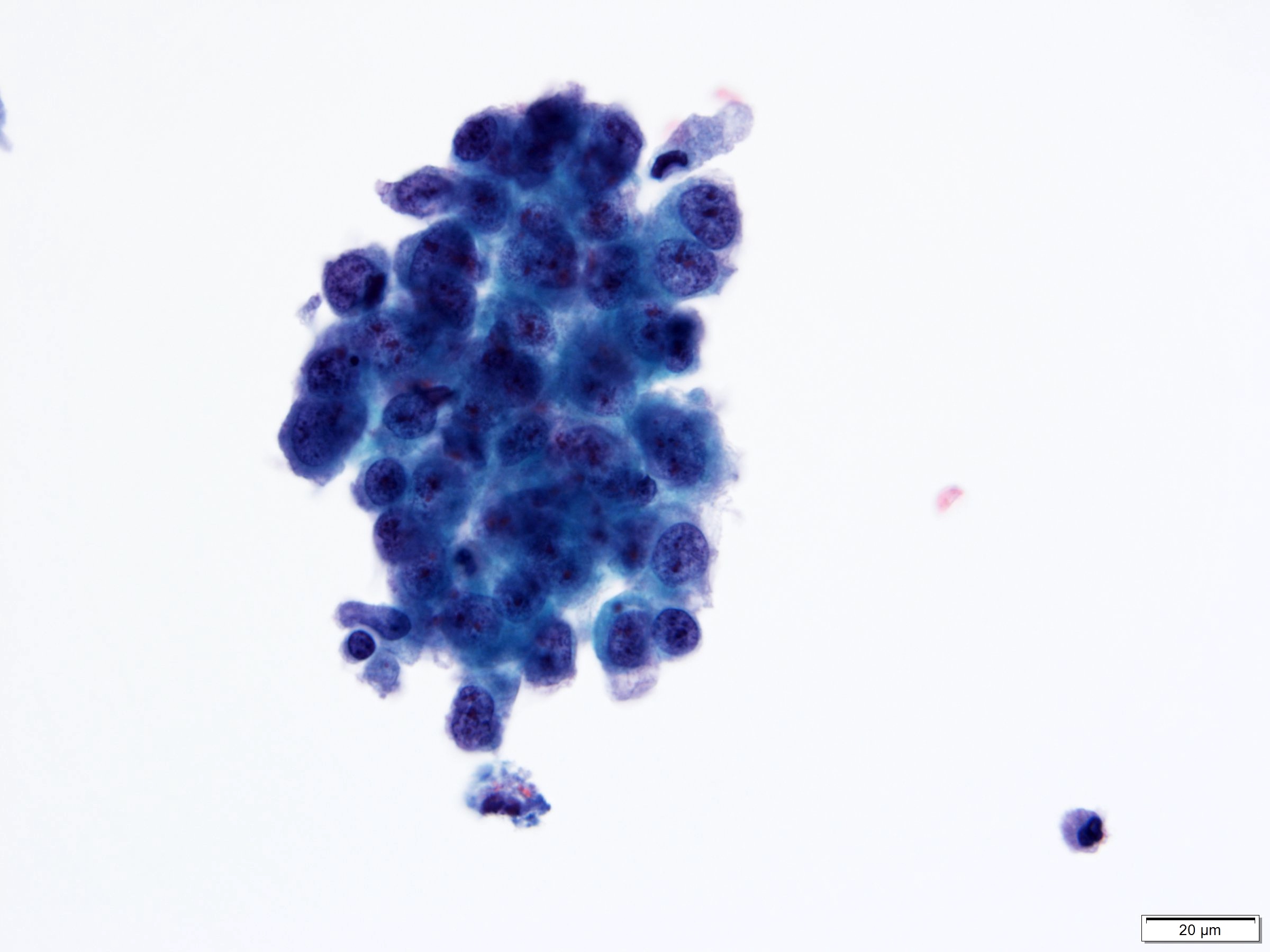
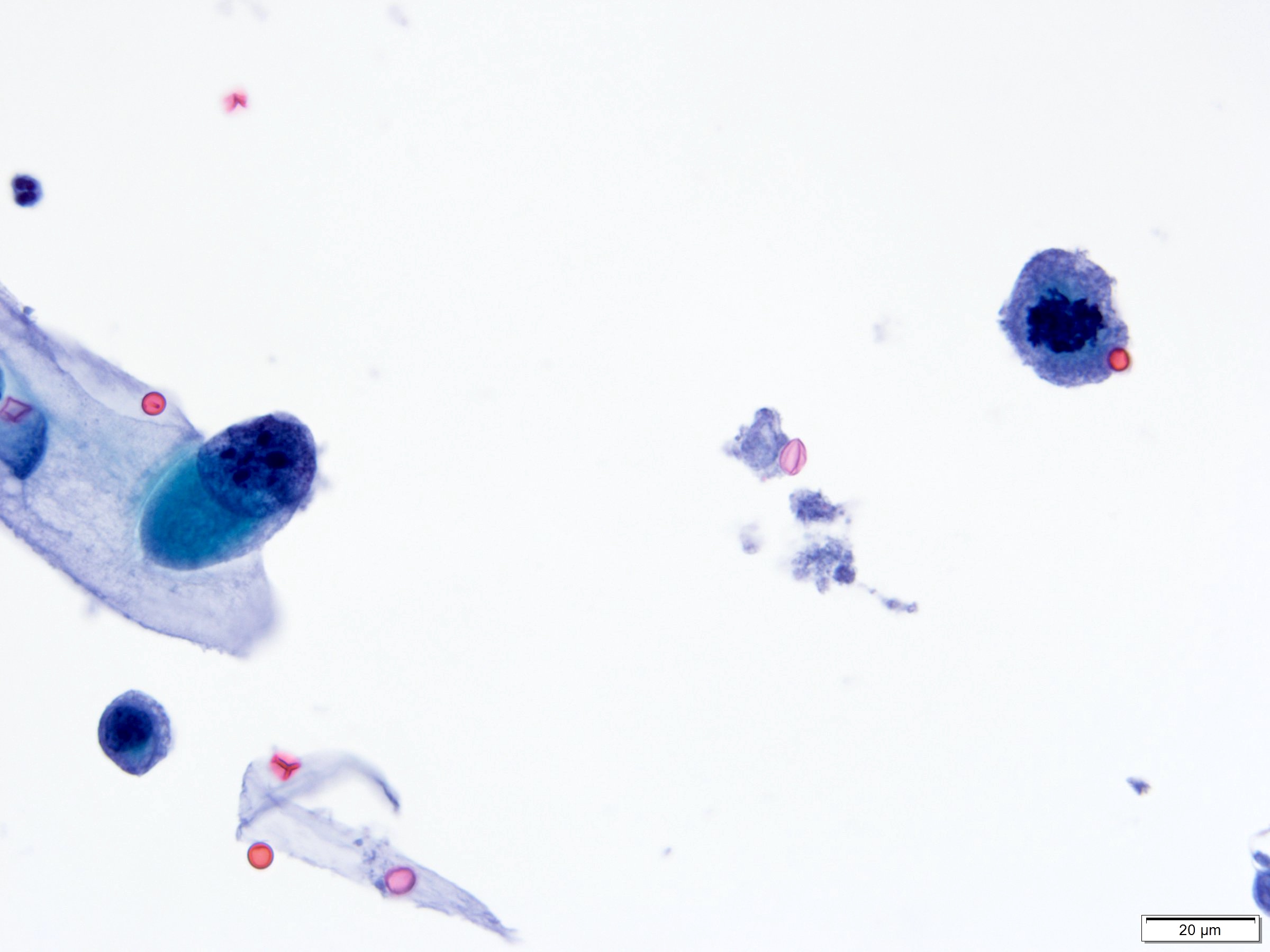
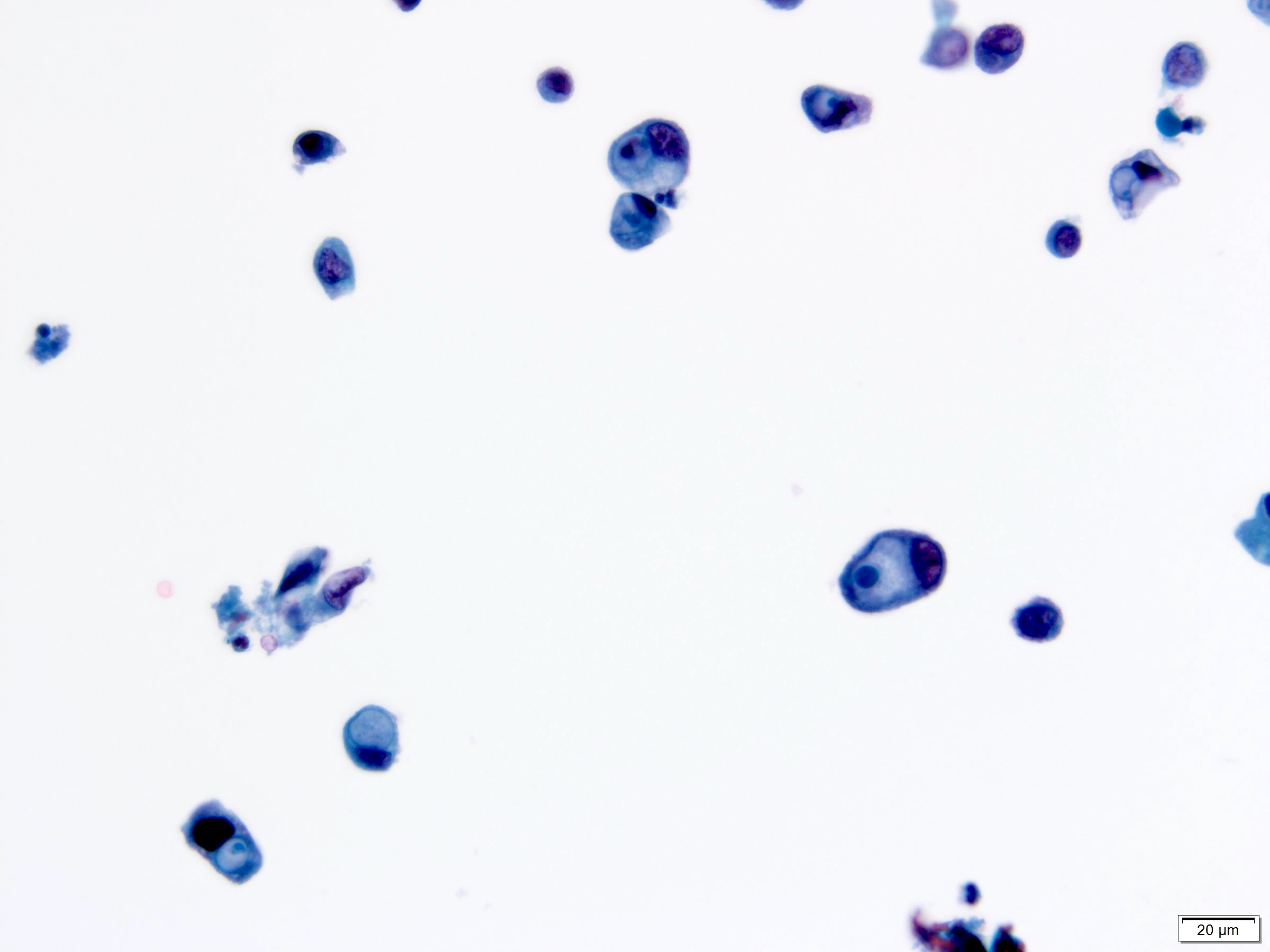
Cytology description
- Moderate / severe nuclear hyperchromasia, irregular nuclear membrane, coarse chromatin, nuclear/cytoplasmic ratio ≥ 0.7; mitoses and necrotic debris may be present
- Cytology cannot distinguish invasive from noninvasive high grade or carcinoma in situ
- Shows high sensitivity (up to 84%) for high grade tumors (Urol Oncol 2015;33:66.e25)
- Use of 2016 Paris Working Group Reporting system recommended (Acta Cytol 2016;60:185)
Cytology images
Positive stains
- GATA3, CK20, p63, CK5/6, high molecular weight cytokeratin, CK7
- Increased p53 and Ki67 expression more frequent than in low grade
- Reference: Am J Surg Pathol 2014;38:e20
Negative stains
- CK5/6 loss in subset (Int J Mol Sci 2019;20:570)
Electron microscopy description
- High grade papillary urothelial carcinoma shows focal loss of zonula occludens (tight junctions) and macula adherens (desmosomes) (Cancer 1971;27:71)
Molecular / cytogenetics description
- Genetic or epigenetic changes in TP53 gene or TP53 regulatory gene (CDKN2A or p16)
- Somatic mutations in TERT in 70 - 80% noninvasive urothelial carcinomas
- Mutations in PIK3CA (25% of cases), TSC1, HRAS, APC
- Epigenetic silencing of tumor suppressor genes via promoter hypermethylation): RUNX3, CDKN2A, MLH1, MGMT, VHL, DAPK, TBX2, TBX3, GATA2, ZIC4, GSTP1, CDH1 (Eur Urol 2012;61:1245, Nat Rev Urol 2013;10:327)
- MicroRNA alterations (J Pak Med Assoc 2018;68:759)
- Loss of chromosome 9
Videos
Urothelial carcinoma, papillary and invasive
Sample pathology report
- Bladder lesion, transurethral resection:
- Papillary urothelial carcinoma, high grade (grade 3/3 - WHO 1973)
- Noninvasive, pTa
- Muscularis propria sampled
- No lymphovascular invasion
- Negative for urothelial carcinoma in situ
Differential diagnosis
- Low grade urothelial carcinoma:
- Cells more uniform and appear orderly on low power
- Chromatin evenly distributed
- Mitoses may be present but usually confined to lower half of urothelium
- Prominent umbrella cells present
- Papillary polypoid cystitis:
- Broad based papillary fronds with edematous or fibrous stroma
- No complex branching papillary structures
- Reactive urothelial atypia may be present
- Papillary nephrogenic adenoma:
- Prostatic type polyp:
Additional references
Practice question #1
Which of the following is true about the noninvasive papillary bladder lesion in the above image?
- Immunohistochemistry is helpful for diagnosis
- Progression to invasive disease is rare
- Common presentation include dysuria, urgency, frequency
- Neoplastic cells dyscohesion and partial denudation of urothelium is rare
- Cytologic atypia, nuclear pleomorphism and loss of polarity are common
Practice answer #1
E. Cytologic atypia, nuclear pleomorphism and loss of polarity are common
Comment Here
Reference: Noninvasive papillary urothelial carcinoma high grade
Comment Here
Reference: Noninvasive papillary urothelial carcinoma high grade
Practice question #2
Which of the following molecular changes has been described in high grade noninvasive papillary urothelial carcinoma?
- TP53
- FGFR3
- STAG3
- Chromosome 11 point mutations
- Germline mutations in TERT promoter
Practice answer #2