Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Hedayat AF, Schwetye K. Primary angiitis of CNS. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnsprimaryangiitis.html. Accessed September 10th, 2025.
Definition / general
- Primary angiitis of the CNS (PACNS) is a rare and severe form of vasculitis of unknown cause limited to the brain, spinal cord and leptomeninges, resulting in inflammation of CNS vessels with subsequent cerebral ischemia and less frequently, hemorrhage (Acta Neuropathol 2012;123:759)
Essential features
- Primary angiitis of the central nervous system (PACNS) is a rare condition that is often misdiagnosed (Neurol Sci 2021;424:117422)
- Affects exclusively small and medium sized vessels of the central nervous system (Clin Exp Immunol 2014;175:419)
- Brain biopsy is essential to confirm the diagnosis (Arch Neurol 2009;66:704)
Terminology
- Synonyms: isolated angiitis of the CNS, primary CNS vasculitis
ICD coding
Epidemiology
- Prevalence is difficult to measure due to rarity and imprecise diagnostic criteria
- Incidence is estimated to be ~2.4 cases per 1,000,000 person years (Ann Neurol 2007;62:442)
- Similar frequency in male and female patients (Ann Neurol 2007;62:442)
- Initial symptoms at end of the fourth decade; ~50% of patients are 40 - 60 years old (J Neurol 1998;245:766)
- May occur at almost any age; uncommon in children (Curr Opin Rheumatol 2010;22:590)
- Mainly affects younger stroke patients lacking cerebrovascular risk factors (Clin Exp Immunol 2014;175:419)
- ~3 - 5% of cerebrovascular events that occur at < 50 years can be attributed to primary CNS vasculitis
Sites
- Brain and leptomeninges (Ann Neurol 2007;62:442)
- Spinal cord (Neurology 2008;70:2394)
Pathophysiology
- Not fully understood; very little is known about the pathogenesis (Acta Neuropathol 2012;123:759)
- Considerable research has centered on systemic vasculitides
- Both humoral and cellular immunological factors; these vary widely by subtype
- Antibodies are particularly relevant, especially in those affecting small vessels, either through a direct attack or through interaction with neutrophils
- Scant evidence for immune complexes or antibody associated mechanisms in PACNS
- Single case report describes predominant CD45R0+ T cell infiltration in and around small vessels, suggesting memory T cells play a role in the pathogenesis
- Suggests an antigen specific immune response in vessel walls
- Potentially triggered by pathogen derived antigens
- Exact triggers remain unknown (Eur Neurol 2001;45:184)
- Destructive vasculitic process with fibrinoid necrosis may severely weaken vessel walls
- Predisposes to blood vessel ruptures and aneurysmal dilatations
- Links necrotizing vasculitis with intracranial hemorrhage
- Ischemia appears to result from inflammation within the vascular walls
- Begins with obstruction of the vascular lumen, increased coagulability due to proinflammatory cytokine effect on endothelial cells and alterations in vasomotor tone
- Neurological findings due to ischemia and infarction or intracranial hemorrhage
Etiology
- Different clinical subsets of unknown etiology and pathogenesis (Acta Neuropathol 2012;123:759)
- Initial event that primes the inflammatory cells is unknown
- Final pathway of inflammation leads to occlusion of the involved blood vessel, thrombosis and ultimately ischemia and necrosis of the territories of the involved vessels
- Limited data suggest an association with systemic viral illnesses or a state of altered host defense and PACNS (Neurol Neuroimmunol Neuroinflamm 2021;8:e1093)
Clinical features
- Most common symptoms include headaches (63%) and focal / diffuse neurologic deficits (Ann Neurol 2007;62:442)
- Cognitive impairment is insidious; more acute alterations in consciousness or coma are very unusual (Ann Neurol 2007;62:442)
- Diagnosis is often delayed due to ambiguity of the symptoms; time from symptom onset to diagnosis is often up to 6 months
- Strokes or persistent neurologic deficits (40%) and transient ischemic attack (30 - 50%) are uncommon in the absence of headache or encephalopathy (Ann Neurol 2007;62:442)
- Seizures are more common in children; occurs in < 25% of adults
- Erythrocyte sedimentation rate (ESR) and C reactive protein (CRP) levels are more likely to be elevated in children and are usually normal in adults (elevated ESR in < 25%); symptoms or serologic markers of systemic inflammation are uncommon (Medicine (Baltimore) 1988;67:20, Ann Neurol 2007;62:442)
- Intracranial hemorrhage at the time of diagnosis (12%) (Arthritis Rheum 2011;63:3598)
- Although classically considered a small vessel vasculitis, symptoms related to large vessel disease, including aphasia (28%) and visual field deficits (21%), may occur
- Fevers, weight loss and night sweats in < 20% of patients (Medicine (Baltimore) 1988;67:20, Ann Neurol 2007;62:442)
- Symptoms suggestive of PACNS in patients that are < 30 years old or > 70 years old: consider other possible diagnoses
Diagnosis
- No consensus on diagnostic criteria for PACNS
- Most clinicians still use 1988 criteria (Calabrese and Mallek) (Medicine (Baltimore) 1988;67:20, Arch Neurol 2009;66:704)
- Clinical criteria: the patient has a history or clinical findings of an acquired neurological deficit, which remains unexplained after a vigorous diagnostic workup, including lumbar puncture and neuroimaging studies
- Imaging / histopathologic criteria: the patient demonstrates either classic angiographic findings or histopathologic features of angiitis within the CNS
- Criteria of exclusion: there is no evidence of systemic vasculitis or of any other condition to which the angiographic or pathologic features could be secondary
- To prevent misdiagnosis, particularly with the reversible cerebral vasoconstriction syndrome (RCVS), Birnbaum and Hellmann proposed new criteria (Arch Neurol 2009;66:704)
- Definite diagnosis when biopsy proven
- Probable diagnosis in the absence of tissue confirmation if there are high probability findings on an angiogram with abnormal findings on MRI and a cerebrospinal fluid (CSF) profile consistent with PACNS
Laboratory
- Blood tests in adults are generally normal, including acute phase reactants
- CSF analysis is abnormal in 80 - 90% of cases (Arch Neurol 2009;66:704)
- Protein levels in CSF are usually mildly increased but may differ in subsets of PACNS, as defined by caliber of vessels involved
- CSF white cell count is usually mildly increased
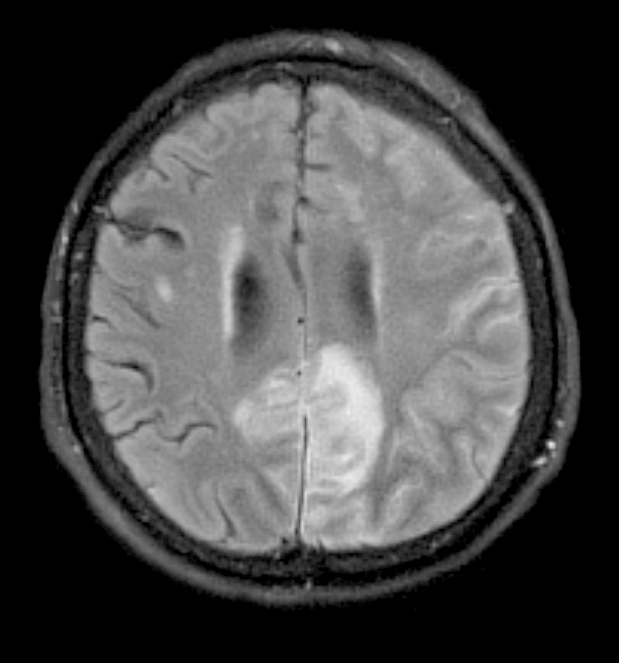
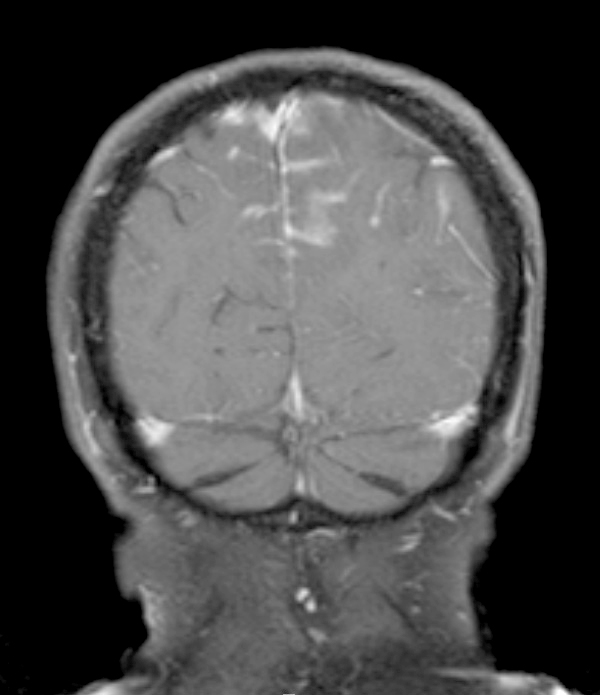
Radiology description
- Vascular irregularities, stenoses and occlusions occur in patterns atypical for atherosclerosis (Ther Adv Neurol Disord 2018;11:1756286418785071)
- Conventional angiography is gold standard but often negative
- Digital subtraction angiography (DSA) when clinical suspicion is high, regardless of magnetic resonance (MR) findings
- MR findings
- MR abnormality is variable (Stroke 2017;48:1248)
- Multifocal, deep, gray and subcortical white matter lesions (hypointense on T1WI and hyperintense on T2WI and FLAIR)
- Patchy enhancement in some cases
- MR angiography changes (beaded appearance) with larger caliber vessel involvement
Prognostic factors
- Expectation for recovery has improved with increasing identification of PACNS and appropriate use of immunosuppressive regimens (Stroke 2018;49:1946)
- Patients with recurrent infarcts and rapid progression are at an elevated risk for progression and require more aggressive treatment
- Identification of permanent deficits is paramount to prevent unwarranted escalations in therapy (Neurol Neuroimmunol Neuroinflamm 2024;11:e200262)
- Modified Rankin scores have commonly been used as response criteria (Arthritis Rheumatol 2014;66:1315)
Case reports
- 5 year old girl who was admitted because of an intermittent headache (Pediatr Investig 2022;6:140)
- 8 year old boy presented with 1 week of fever, headache, fatigue, unsteady gait, abdominal pain and vomiting (BMC Neurol 2023;23:57)
- 21 year old man presented with a 4 year history of progressive gait deterioration (J Neuroimmunol 2022;373:577991)
- 44 year old man presented with a 6 month history of bilateral headaches, cognitive decline, hypersomnolence and constitutional symptoms, including fevers and 20 kg of weight loss (Pathology 2023;55:547)
- 57 year old man presented with a 10 day history of transient episodes of tension headache with nausea, photophobia and aphasia (Mod Rheumatol Case Rep 2023;8:117)
- 62 year old, right handed man presented with sudden dysphasia, presumed due to stroke (SAGE Open Med Case Rep 2014;2:2050313X14559638)
Treatment
- Acute therapy (Arch Neurol 2009;66:704, Rheumatol Int 2024;44:211)
- Oral cyclophosphamide and corticosteroids (usually in the form of prednisone)
- If patient is in a life threatening state, corticosteroid therapy with methylprednisolone
- Maintenance therapy (Arch Neurol 2009;66:704, Rheumatol Int 2024;44:211)
- Azathioprine
- Methotrexate
- Mycophenolate mofetil
- Biological agents (Arch Neurol 2009;66:704, J Rheumatol 2013;40:2102, Rheumatol Int 2024;44:211)
- Rituximab
- TNFα blockers
- Infliximab
- Etanercept
Gross description
- May be minimal
- Multifocal strokes can be seen if there is large vessel involvement
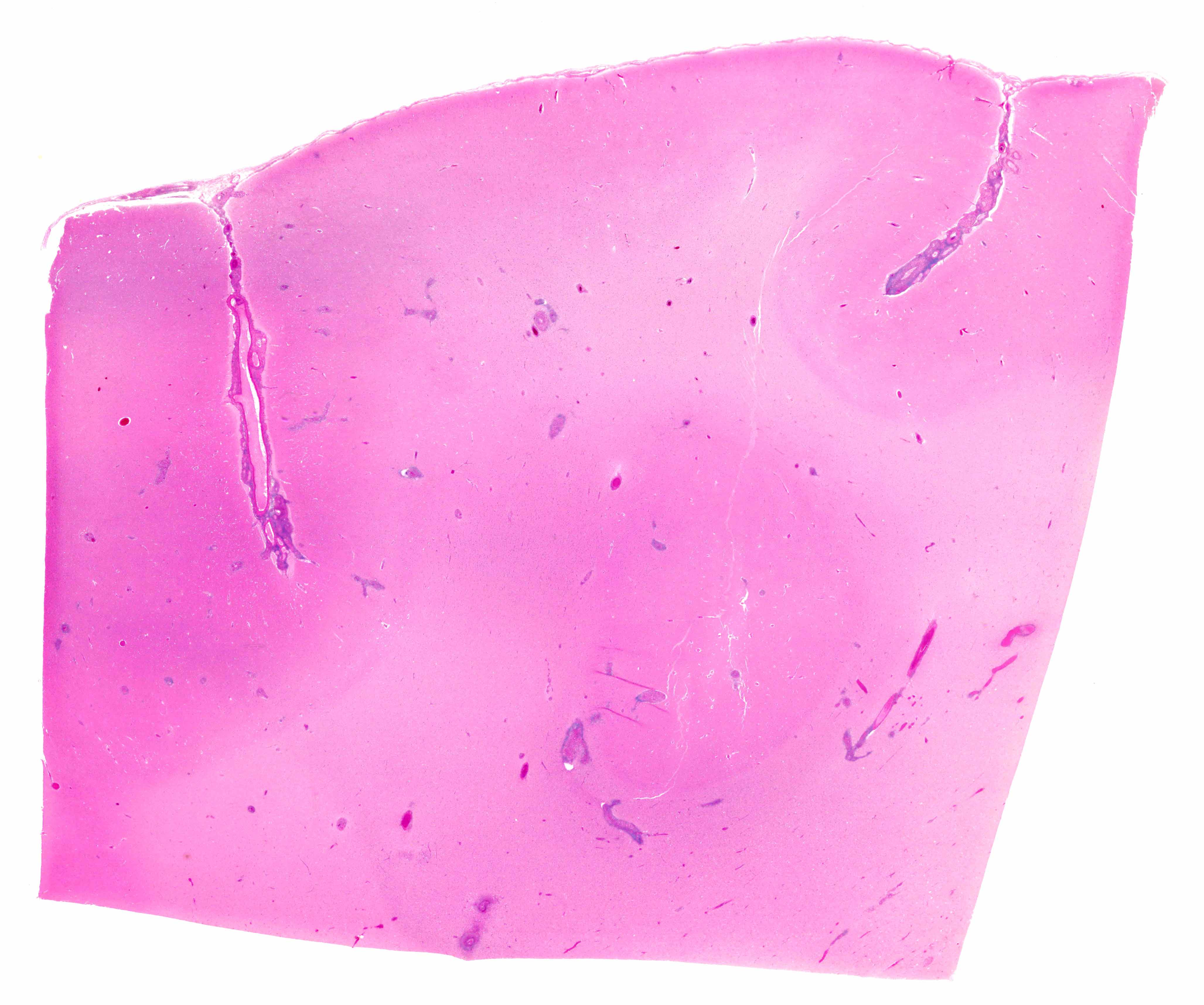
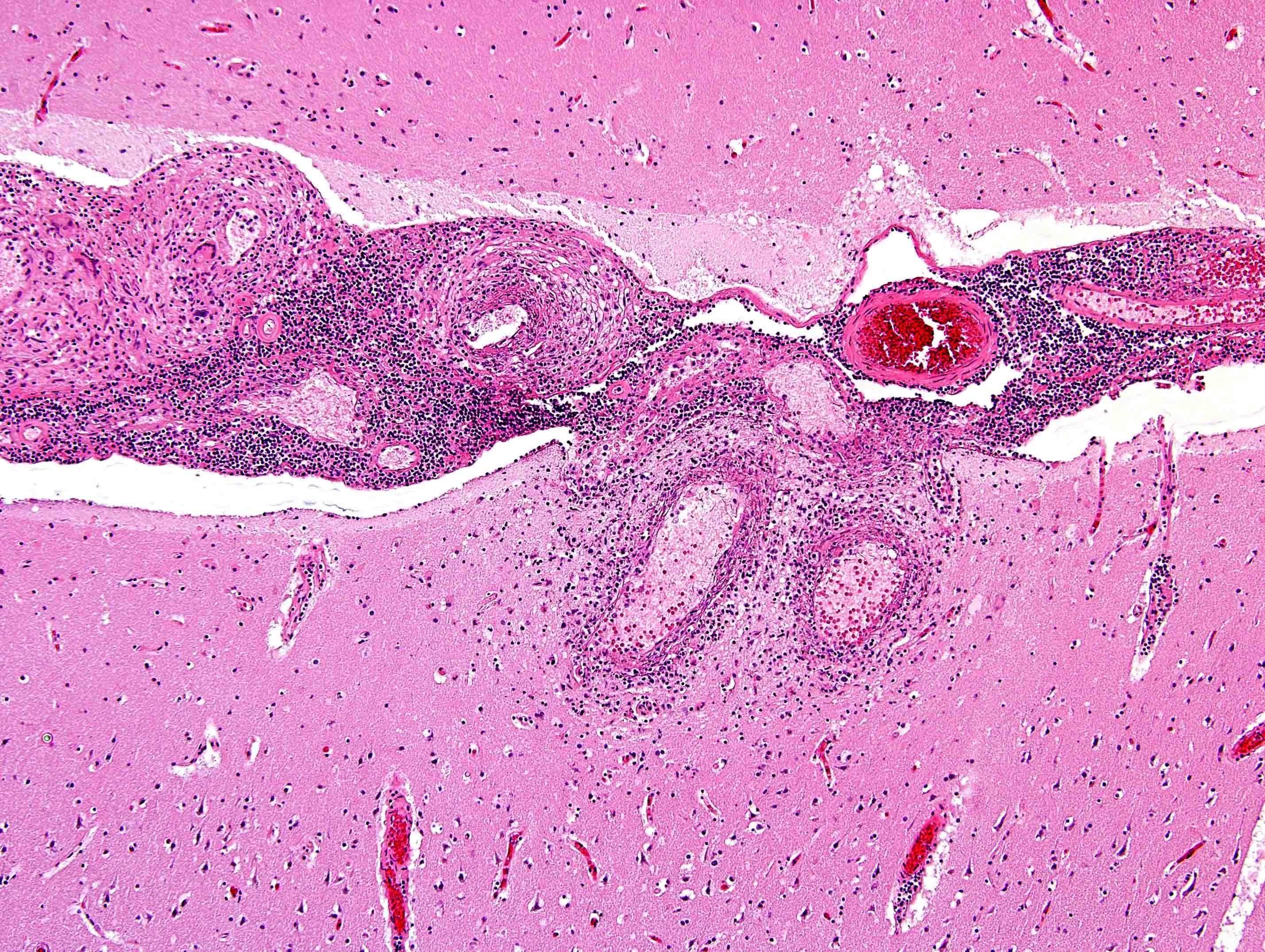
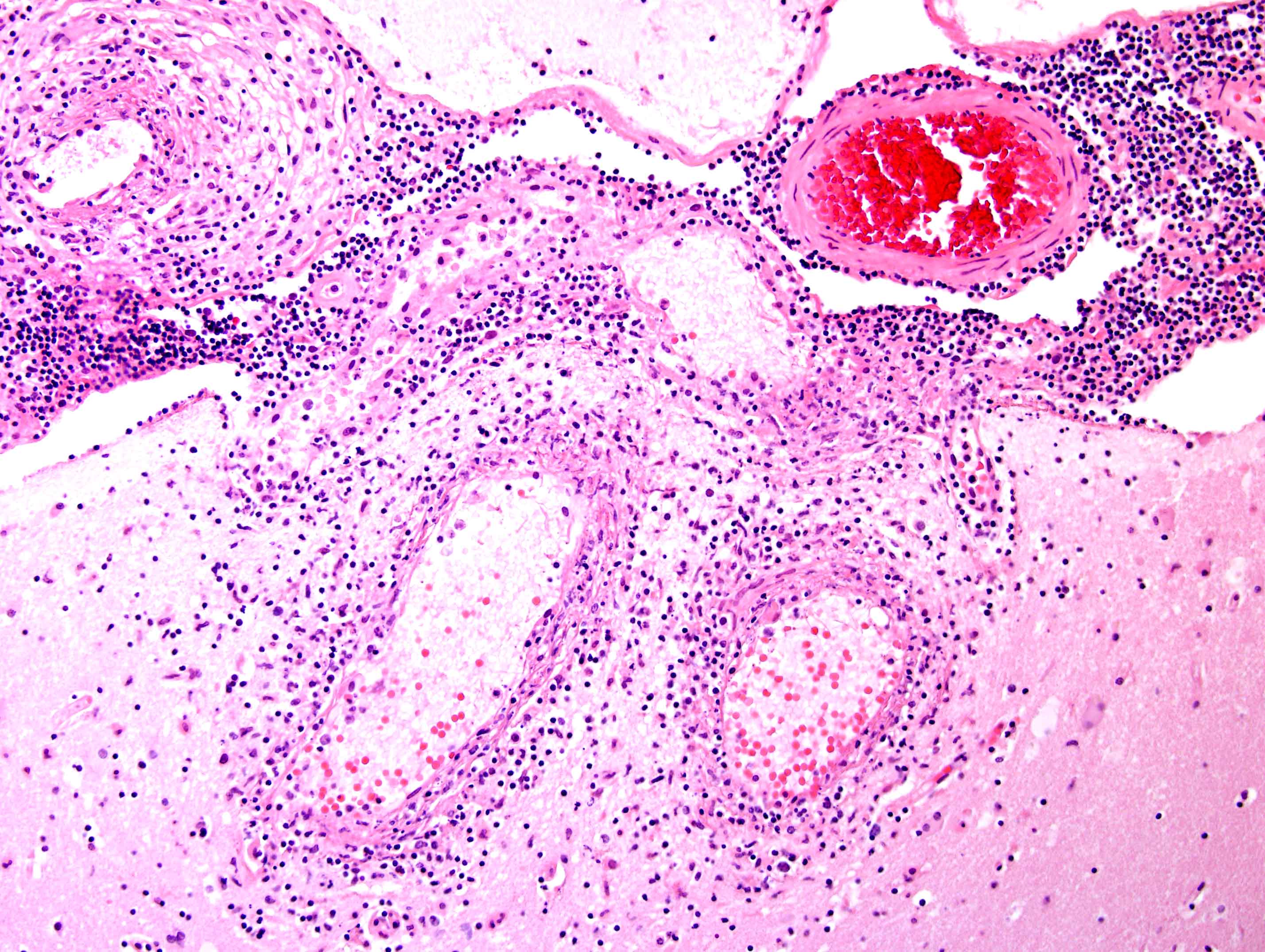
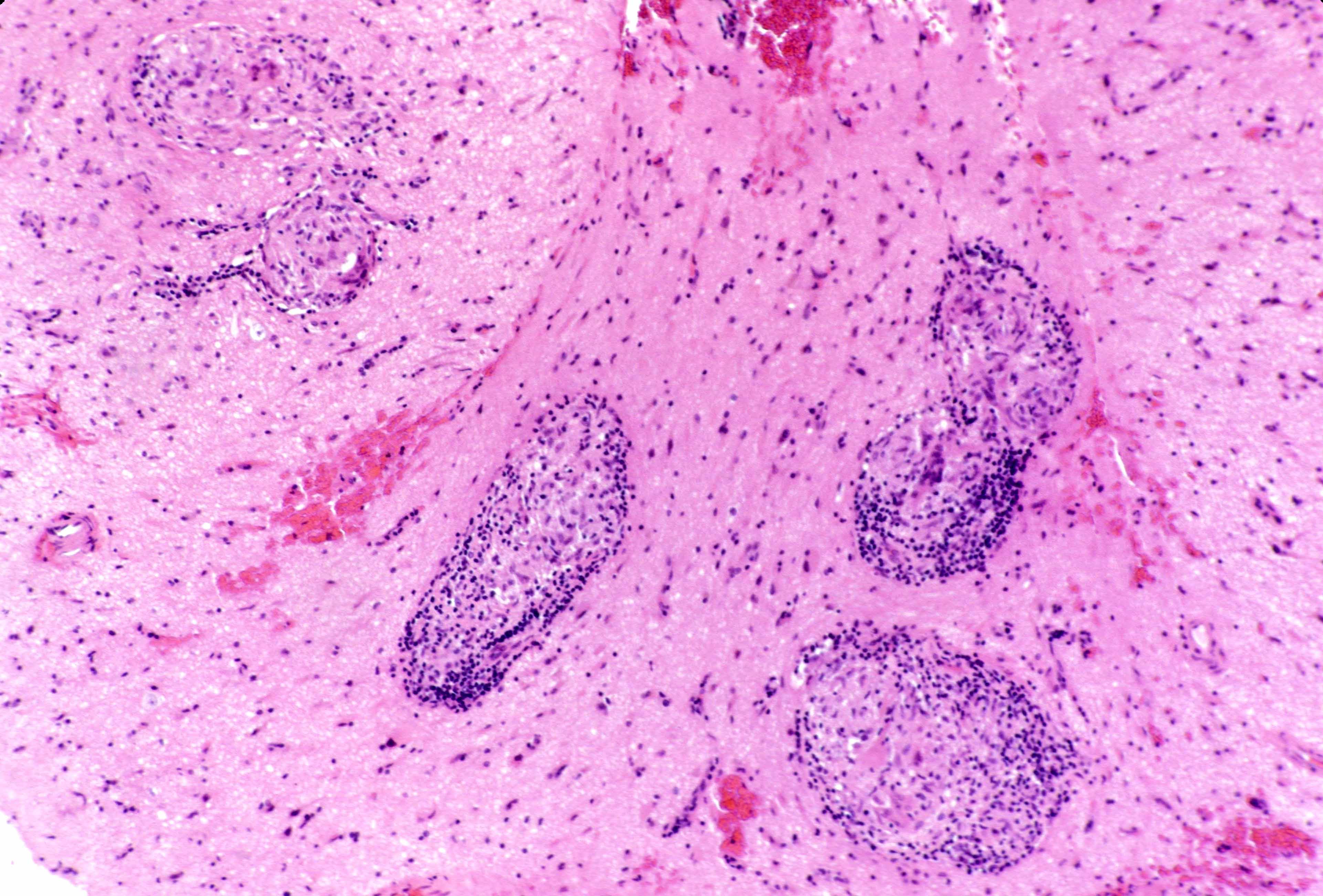
Microscopic (histologic) description
- Granulomatous form (granulomatous angiitis of nervous system)
- Most frequent subtype of PACNS
- Arteries and veins with angiocentric inflammation
- Mononuclear inflammatory infiltrates (histiocytes, lymphocytes, plasma cells, etc.)
- Both foreign body and Langerhans type multinucleated giant cells
- Amyloid beta related angiitis is a special type of granulomatous CNS vasculitis associated with cerebral amyloid angiopathy in older individuals
- Intimal proliferation (causing luminal narrowing, occlusion)
- Granulomas may appear parenchymal if narrowed vessel is not seen in the plane of section
- Lymphocytic form
- Difficult distinction from chronic inflammation in some cases; intense perivascular inflammation may be difficult to differentiate from true vascular wall involvement
- Intense perivascular inflammation may be difficult to differentiate from true vascular wall involvement
- Alternate diagnoses, such as viral encephalitis, should be excluded before diagnosis of PACNS is rendered
- Minimum of 2 layers of lymphocytes within or around vessel walls
- Lymphocytic form predominates in children
- No fibrinoid vascular necrosis
- Structural alterations of vessel walls, such as prominent endothelial cells, concentric and asymmetric vessel wall thickening, vessel wall distortion
- Acute necrotizing form
- Least frequent subtype of PACNS
- Associated intracranial hemorrhage in some cases
- Fibrinoid vascular necrosis in acute phases
- Morbidity and mortality not necessarily higher than in other forms of PACNS
- Need to exclude polyarteritis nodosa, other systemic vasculitis, drug related vasculitis
- Reference: Am J Surg Pathol 2009;33:35
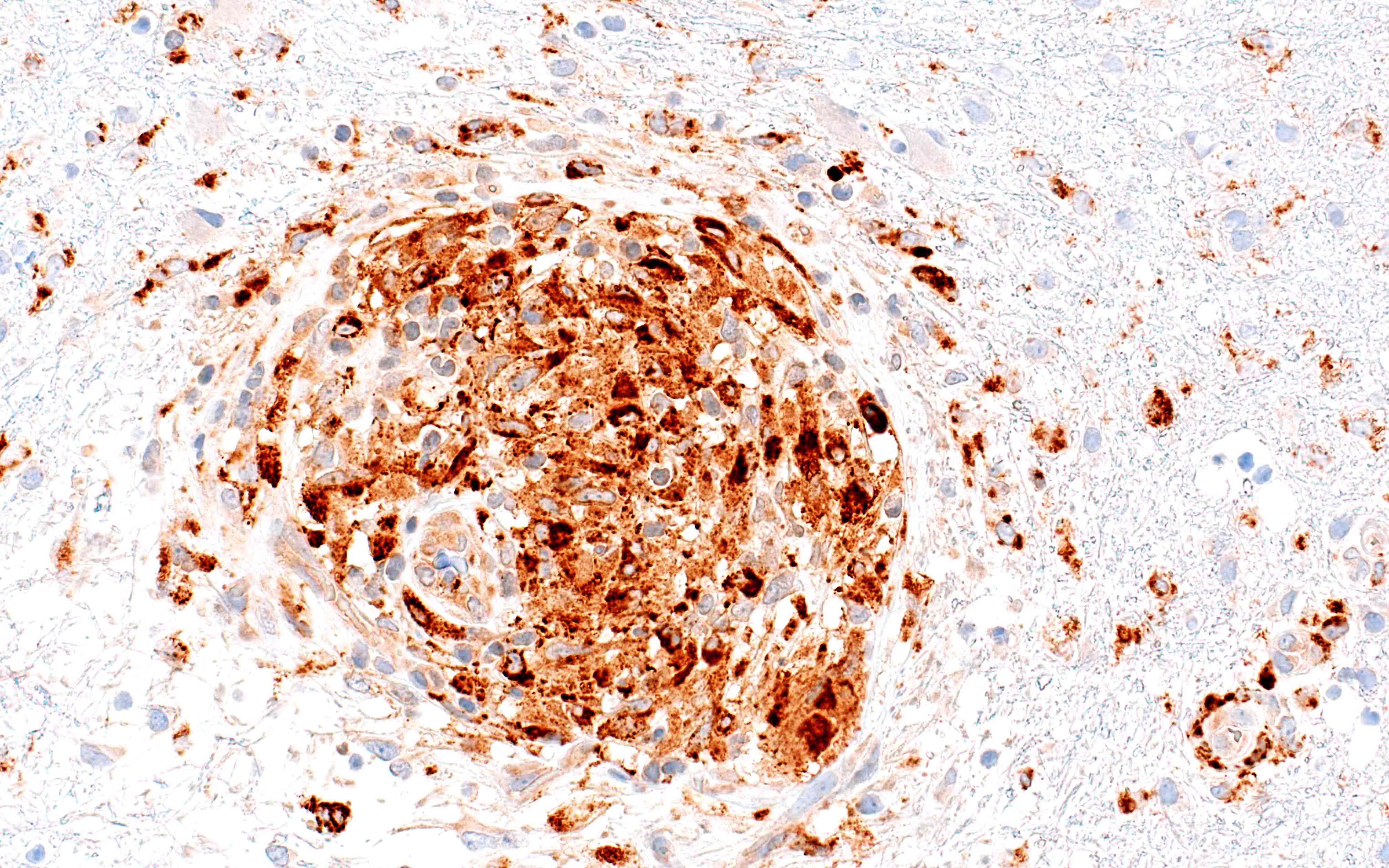
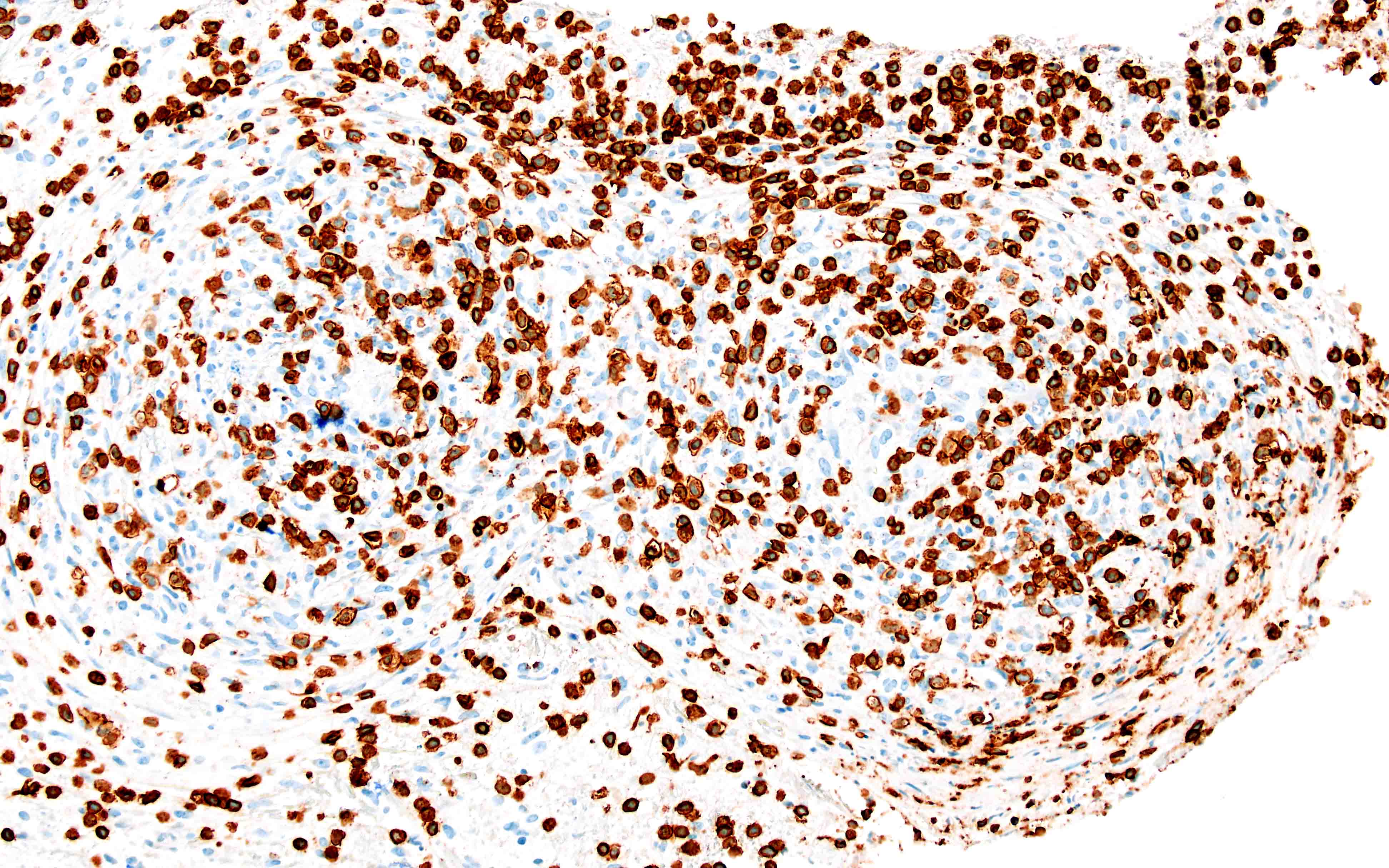
Microscopic (histologic) images
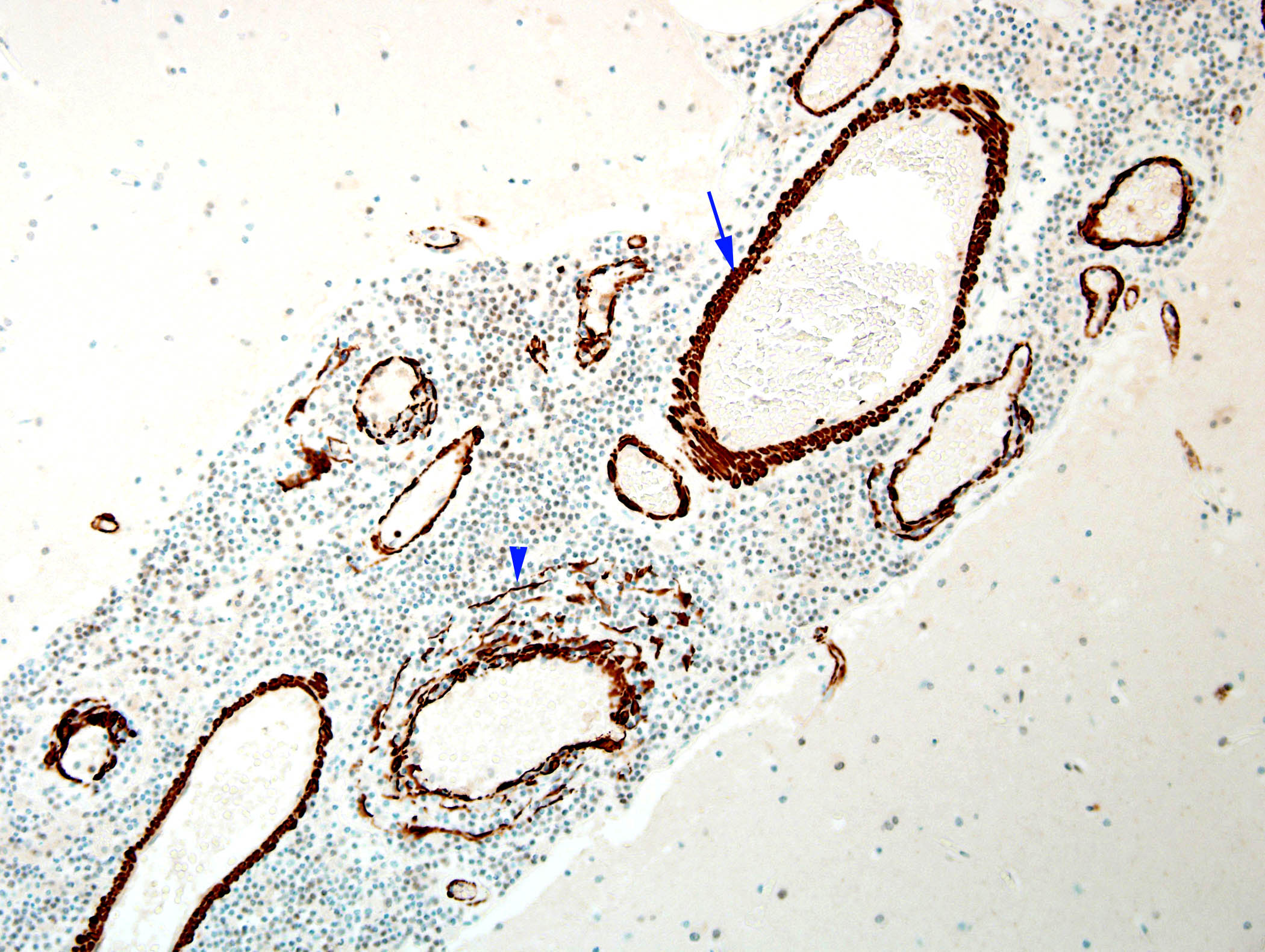
Positive stains
- CD3: marks T lymphocytes
- CD68: highlights macrophages
- SMA: highlights disrupted vessels
- Verhoeff-van Gieson (VVG)
- CD45RO: highlights memory T cells (Eur Neurol 2001;45:184)
Negative stains
- Congo red: negative for amyloid in typical PACNS, positive in amyloid beta related angiitis (Stroke 2024;55:e316)
- Acid fast bacteria (AFB) / Fite: negative for mycobacteria
- Grocott methenamine silver (GMS): negative for fungal organisms
- Periodic acid-Schiff (PAS): negative for fungal organisms and other periodic acid-Schiff positive substances (Am J Surg Pathol 2009;33:35)
- CD20: typically negative or low
Sample pathology report
- Brain, biopsy:
- Granulomatous vasculitis (see comment)
- Comment: H&E stained sections show mostly fragments of cortex with overlying meninges and scant subcortical white matter. Medium and small meningeal and parenchymal vessels, including Virchow-Robin spaces, have robust nonnecrotizing granulomatous inflammation comprising lymphohistiocytic cell aggregates and scattered multinucleated giant cells. No eosinophils are present. A subset of vessels shows complete to near complete luminal occlusion. The underlying cortex shows patchy microvacuolation, gliosis and increased number of microglia.
- Immunohistochemical and histochemical stains are performed on block A2 to characterize the lesion (single antibody stain procedures with appropriate controls). CD68 highlights abundant perivascular histiocytes / macrophages as well as robust microglial activation. CD3 labels abundant small perivascular T cells as well as scattered small parenchymal T cells. CD20 highlights small perivascular B cells, which are fewer in number than T cells but still significant. SMA highlights disrupted vessel walls. Elastic stain highlights very few vessels with preserved elastic laminae, indicating destruction in most others. GMS, PAS, AFB and Fite stains do not show any definitive fungal or mycobacterial organisms.
- The collective findings are consistent with granulomatous vasculitis. In the absence of systemic vasculitis or evidence of infection, the findings could be compatible with primary angiitis of the central nervous system. Further clinical correlation is essential.
Differential diagnosis
- Noninflammatory vasculopathies
- Reversible cerebral vasoconstriction syndrome (RCVS):
- Acute onset, thunderclap headache and focal presentation
- Patients younger than 40 years
- Vessels without inflammation
- Segmental narrowing and dilatation
- Stroke (SAGE Open Med Case Rep 2014;2:2050313X14559638):
- Amyloid angiopathy
- Older than 75 years old, especially when associated with lobar hemorrhages or a history of dementia
- Atherosclerosis:
- Intimal thickening and lipid laden macrophages
- Fibrous cap and calcification
- Narrowing of lumen without true vasculitis
- Neurofibromatosis:
- Dysplastic, tortuous vessels in association with neurofibromas
- Fragmented elastic lamina
- Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL):
- Granular osmiophilic material in vessel walls
- Thickened, hyalinized arterioles in white matter
- Mitochondrial encephalopathy with lactic acidosis and stroke-like syndromes (MELAS):
- Stroke-like lesions not confined to vascular territories
- Ragged red fibers in muscle biopsy (ancillary clue)
- Susac syndrome:
- Small vessel microangiopathy with endothelial cell injury
- Microinfarcts in corpus callosum and retina
- Moyamoya angiopathy:
- Intimal hyperplasia with smooth muscle proliferation
- Collateral vessel formation, mostly no vessel wall inflammation
- Hypercoagulable state
- Radiation vasculopathy:
- Fibrosis and hyalinization of vessel wall
- Endothelial atypia, luminal narrowing
- Reversible cerebral vasoconstriction syndrome (RCVS):
- Infections
- Emboli from subacute bacterial endocarditis:
- Septic thrombi in vessel lumen
- Vessel wall necrosis, neutrophilic infiltration
- Basilar meningitis caused by TB or fungal infection:
- Granulomatous inflammation with multinucleated giant cells (TB)
- Fungal organisms with vasculitic invasion and thrombosis
- Bacterial infection:
- Acute neutrophilic vasculitis with fibrinoid necrosis
- Septic thrombi possible
- Parainfection syndromes (e.g., acute disseminated encephalomyelitis):
- Acute neutrophilic vasculitis with fibrinoid necrosis
- Septic thrombi possible
- Emboli from subacute bacterial endocarditis:
- Demyelinating syndromes
- Multiple sclerosis (J Neuroimmunol 2022;373:577991):
- Perivenular demyelination
- Relative axonal preservation
- Macrophages with myelin debris
- Acute disseminated encephalomyelitis:
- Perivenous, confluent demyelination
- Abundant macrophages, lymphocytic perivascular infiltrates
- Multiple sclerosis (J Neuroimmunol 2022;373:577991):
- Sarcoidosis:
- Noncaseating granulomas in meninges or vessel wall
- Multinucleated giant cells, absence of necrosis
- Secondary CNS vasculitis affected as part of a primary systemic vasculitis
- Large vessel vasculitis (e.g., polyarteritis nodosa, Kawasaki disease):
- Transmural necrotizing inflammation of medium sized arteries
- Fibrinoid necrosis with mixed inflammatory infiltrates
- Small vessel vasculitis: ANCA associated (e.g., granulomatosis with polyangiitis, Churg-Strauss syndrome, microscopic polyangiitis):
- Necrotizing vasculitis of arterioles and venules
- Sparse immune complex deposition (pauci-immune)
- Granulomas in granulomatosis with polyangiitis and eosinophil rich infiltrates in Churg-Strauss syndrome
- Large vessel vasculitis (e.g., polyarteritis nodosa, Kawasaki disease):
- Malignant diseases
- Primary CNS lymphoma:
- Dense perivascular and angiocentric lymphoid infiltrates
- Monotonous atypical B cells
- Lymphomatoid granulomatosis:
- Angiocentric, angiodestructive infiltrates
- Polymorphous lymphoid population with necrosis
- Carcinomatous meningitis:
- Tumor cells infiltrating subarachnoid and perivascular spaces
- Often with mucin or gland formation (adenocarcinoma)
- Gliomatosis cerebri:
- Diffuse infiltration by glial cells without a discrete mass
- Preserved underlying architecture
- Intracranial tumor-like lesions (Pediatr Investig 2022;6:140)
- Primary CNS lymphoma:
- Comment (Arch Neurol 2009;66:704)
- In patients younger than 40 years, consider the diagnosis of RCVS, especially when associated with acute onset, thunderclap headache and focal presentation
- In patients older than 75 years, consider the diagnosis of amyloid angiopathy, especially when associated with lobar hemorrhages or a history of dementia
- In patients with clinical or radiographic signs of basilar inflammation, consider sarcoidosis, fungal infections or tuberculosis
- In patients with symptoms or serologic markers of systemic inflammation (e.g., elevated ESR, night sweats), consider infection, malignant neoplasm or secondary involvement of the CNS as part of a systemic vasculitis
- In the context of immunosuppression (including not only patients with human immunodeficiency virus but also patients with diabetes mellitus, significant alcohol consumption and a history of immunosuppression), strongly consider infection, including subacute bacterial endocarditis
Additional references
Practice question #1
Which diagnostic test is considered essential for confirming a diagnosis of primary angiitis of the central nervous system (PACNS)?
- Brain biopsy
- Cerebrospinal fluid (CSF) analysis
- Computed tomography (CT) angiography
- Magnetic resonance imaging (MRI)
- Positron emission tomography (PET) scan
Practice answer #1
A. Brain biopsy is considered essential for confirming the diagnosis of PACNS, which can reveal the presence of vasculitis affecting the small to medium sized blood vessels in the CNS (Arch Neurol 2009;66:704). Answer D is incorrect because while MRI is a critical tool for detecting abnormalities in the brain that may suggest PACNS, such as areas of inflammation, infarction or hemorrhage, it is not definitive for diagnosis and lacks the specificity provided by a biopsy. Answer B is incorrect because CSF analysis can show nonspecific signs of inflammation (such as elevated protein levels and pleocytosis) but these findings are not specific to PACNS and can be seen in various other CNS conditions. Answer C is incorrect because while CT angiography can help visualize larger vessel involvement and detect abnormalities (such as stenosis or aneurysms), PACNS typically affects smaller vessels that may not be well visualized by this modality. Answer E is incorrect because PET scans can provide information on metabolic activity and inflammation in the brain but these findings are not specific to PACNS and cannot definitively diagnose the condition.
Comment Here
Reference: Primary angiitis of CNS
Comment Here
Reference: Primary angiitis of CNS
Practice question #2
Practice answer #2
A. CD3, CD68, SMA, Verhoeff-van Gieson (VVG). CD3 and CD68 will highlight the cells that compose the majority of the inflammatory infiltrates disrupting vessel walls; SMA and VVG will highlight disruption of the smooth muscle and elastin layer components of the walls, respectively. Answers B, C and D are incorrect because they all include Luxol fast blue / PAS, which might serve to highlight loss of myelin; however, that is not necessarily a histopathologic feature of PACNS. Similarly, answers C and D include CD20 but not CD3. CD20 is typically negative or rare; it might be used to rule out a proliferative B cell process (such as lymphoma) but not without a paired CD3 immunostain. Finally, CD34 (answer C) is unlikely to be helpful in the diagnosis of vasculitis.
Comment Here
Reference: Primary angiitis of CNS
Comment Here
Reference: Primary angiitis of CNS