Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Smith MH. Calcifying epithelial odontogenic tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillacalcifyingepithelial.html. Accessed August 27th, 2025.
Definition / general
- Calcifying epithelial odontogenic tumor (CEOT) is a rare, benign odontogenic tumor characteristically containing amyloid
- Comprises 1% of all odontogenic tumors (Oral Surg Oral Med Oral Pathol Oral Radiol 2021;131:684)
Essential features
- Odontogenic tumor comprised of polyhedral epithelial cells characteristically containing amyloid and sometimes Liesegang rings
- Commonly mixed radiolucent / radiopaque lesion in the tooth bearing regions of the jaws
- 60% affect mandible
- Wide age range (4 - 90 years old) with no significant sex predilection
Terminology
- Also known as Pindborg tumor after the author who first published the best known, first paper in the English language literature in 1958, although the first description of the tumor was originally published by Heinz in 1932 (Cancer 1958;11:838, Head Neck Pathol 2019;13:485)
ICD coding
- ICD-10
- ICD-11
- 2E83.0 & XH4PT4 - benign osteogenic tumors of bone or articular cartilage of skull or face & calcifying epithelial odontogenic tumor
- 2E83.1 & XH4PT4 - benign osteogenic tumors of bone or articular cartilage of lower jaw & calcifying epithelial odontogenic tumor
Epidemiology
- No sex predilection
- Wide age range (4 - 90 years old) (Oral Dis 2019;25:192)
- Average age of 40 years
- Clear subtype appears to arise in a slightly older patient population and shows a female predominance
Sites
- Tooth bearing regions of the jaws
- 11% are peripheral (confined to the soft tissues of the jaws) (J Craniomaxillofac Surg 2017;45:1117)
- 60% are associated with unerupted tooth, often mandibular molar (Oral Surg Oral Med Oral Pathol Oral Radiol 2021;131:684)
- ~60% are in the mandible
Pathophysiology
- Pathogenesis is unknown
- Mutations have been reported, although they may not represent driver mutations (J Clin Pathol 2018;71:279, J Oral Pathol Med 2014;43:183, Oral Oncol 2010;46:387, Anticancer Res 2009;29:3065)
Etiology
- Unknown
Clinical features
- Slow growing, unilateral maxillary or mandibular swelling, often asymptomatic (Oral Surg Oral Med Oral Pathol Oral Radiol 2021;131:684)
- May be associated with unerupted tooth
Diagnosis
- Diagnosis is made on microscopic examination
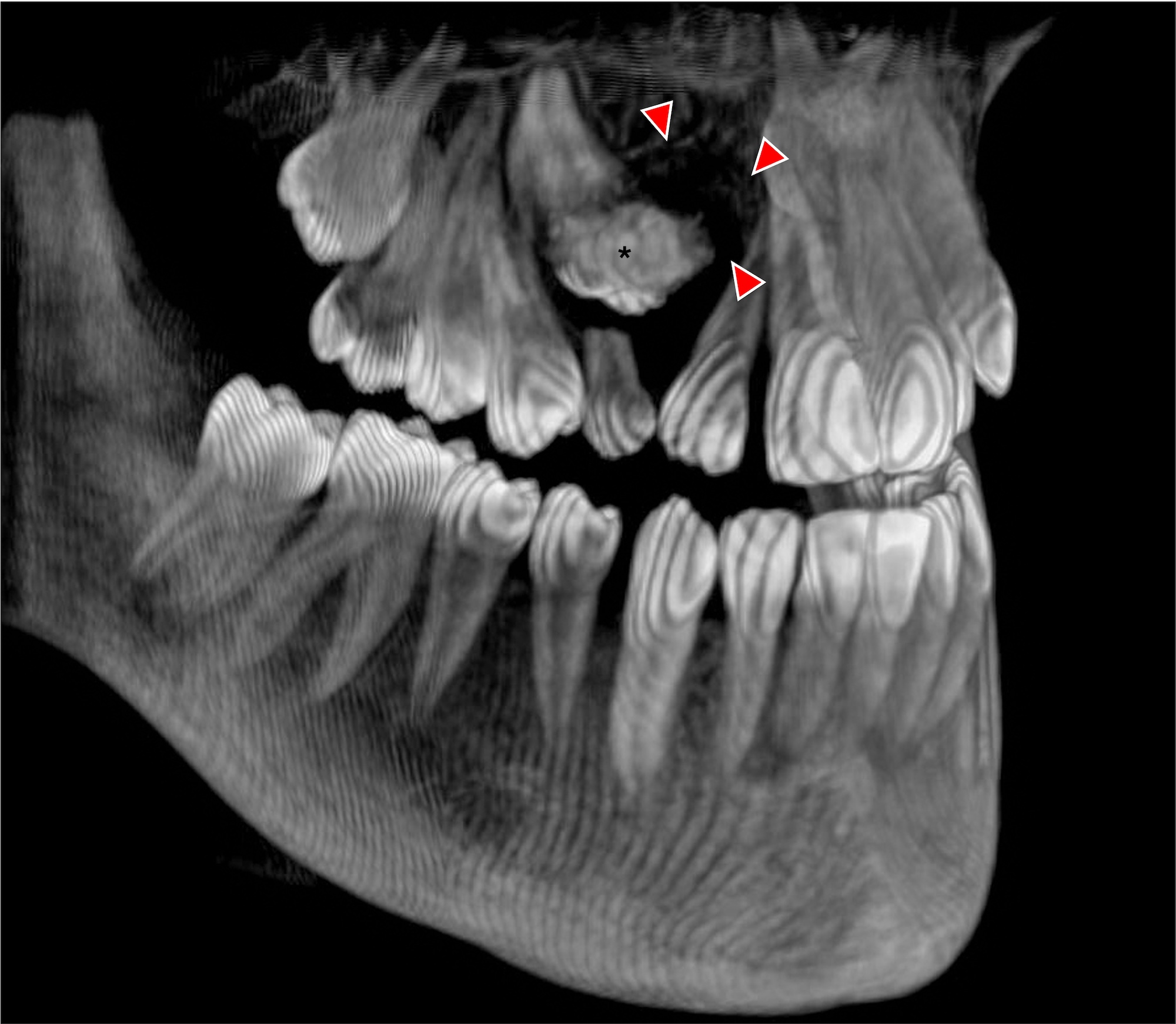
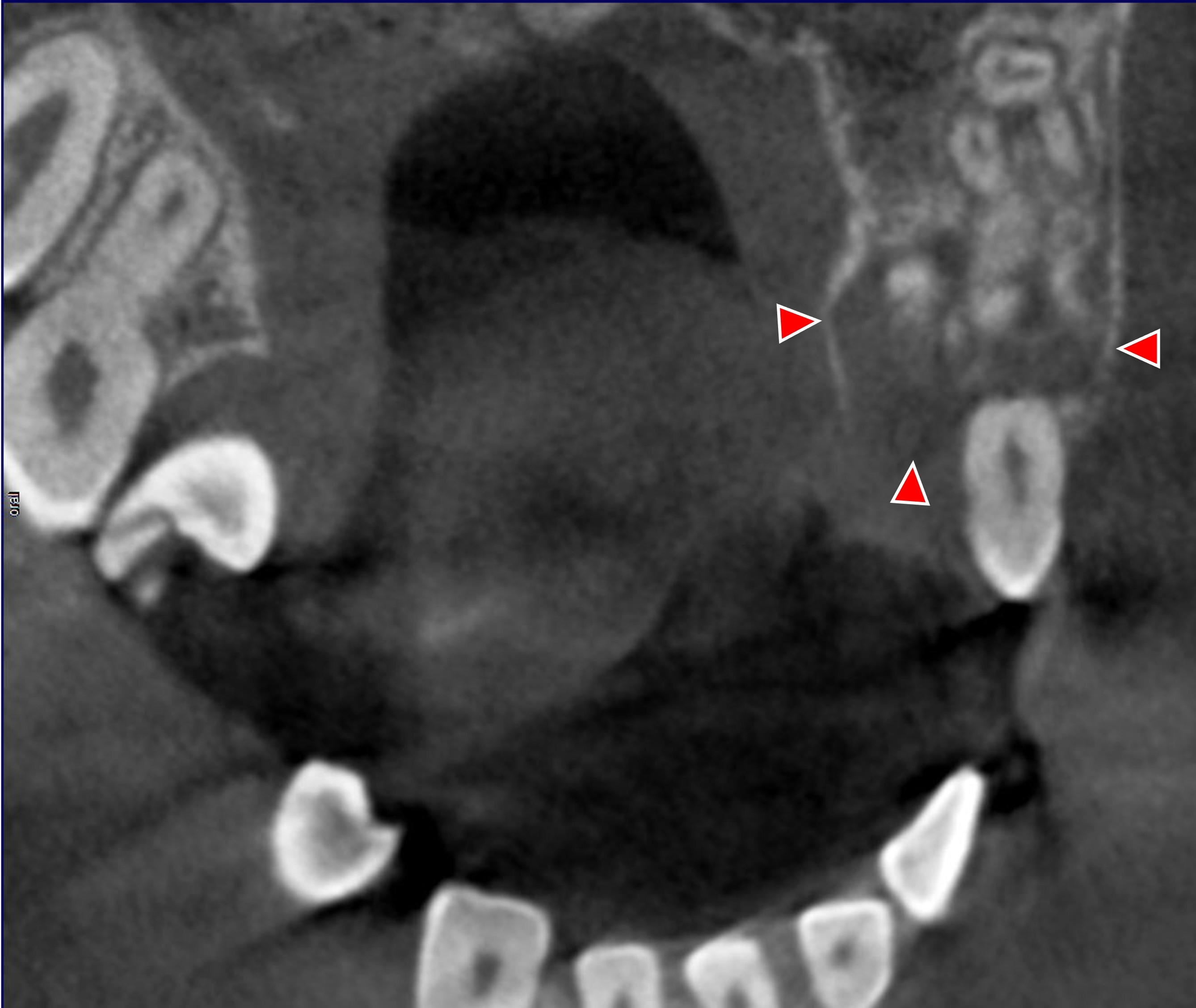
Radiology description
- Well defined radiolucent / radiopaque lesion, frequently associated with unerupted tooth (Oral Surg Oral Med Oral Pathol Oral Radiol 2021;131:684)
- Frequently unilocular, although 30% are multilocular
- May show cortical perforation (~50%) or root divergence
- Mostly hypointense on T1 weighted images and mixed hyperintense on T2 weighted images (Br J Oral Maxillofac Surg 2000;38:154)
- Radiographic differential diagnosis for a single, radiolucent lesion with variable amounts of opacities near the teeth may include an ameloblastic fibro-odontoma, adenomatoid odontogenic tumor, calcifying odontogenic cyst, developing odontoma, osseous dysplasia, ossifying fibroma, osteoblastoma / cementoblastoma
- Biopsy with microscopic examination differentiates CEOT from all of these entities
Radiology images
Prognostic factors
- Recurrence rates vary with treatment modality, with highest rates associated with curettage
- Overall recurrence rate is ~13%
- 25% of peripheral cases recurred after excision / curettage (J Craniomaxillofac Surg 2017;45:1117)
- Rare malignant transformation (Int J Oral Maxillofac Surg 2021;50:1540)
- Langerhans cell rich subtype of CEOT, regarded by many as representing the amyloid variant of odontogenic fibroma, has minimal to no risk of recurrence (Oral Surg Oral Med Oral Pathol Oral Radiol 2018;126:513, Head Neck Pathol 2023;17:313, Oral Surg Oral Med Oral Pathol Oral Radiol 2021;131:684)
Case reports
- 26 year old man with unilateral swelling (Int J Surg Case Rep 2019;57:197)
- 33 year old woman with maxillary tumor associated with supernumerary tooth (Autops Case Rep 2022;12:e2021358)
- 43 year old man with clear cell variant of CEOT (J Oral Maxillofac Pathol 2021;25:204)
- 53 year old man with mandibular mass with no resolution after implantation of iodine 125 particles (Heliyon 2023;9:e17087)
Treatment
- Treatment has varied from enucleation to conservative excision / curettage to segmental resection
- Conservative excision / curettage is considered inadequate treatment, with higher recurrence rates noted (Oral Surg Oral Med Oral Pathol Oral Radiol 2021;131:684)
Clinical images
Gross description
- Solid tan-white tumor
- May contain blood filled cystic cavities, variable amounts of calcified particles (Braz Dent J 2006;17:171)
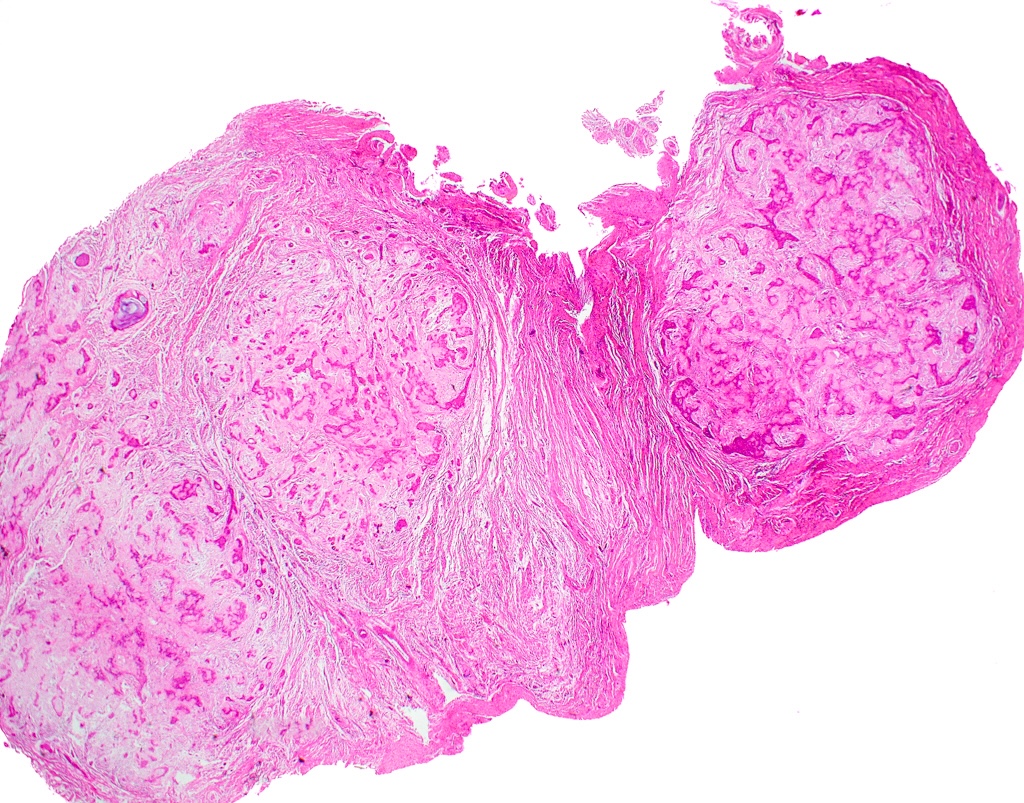
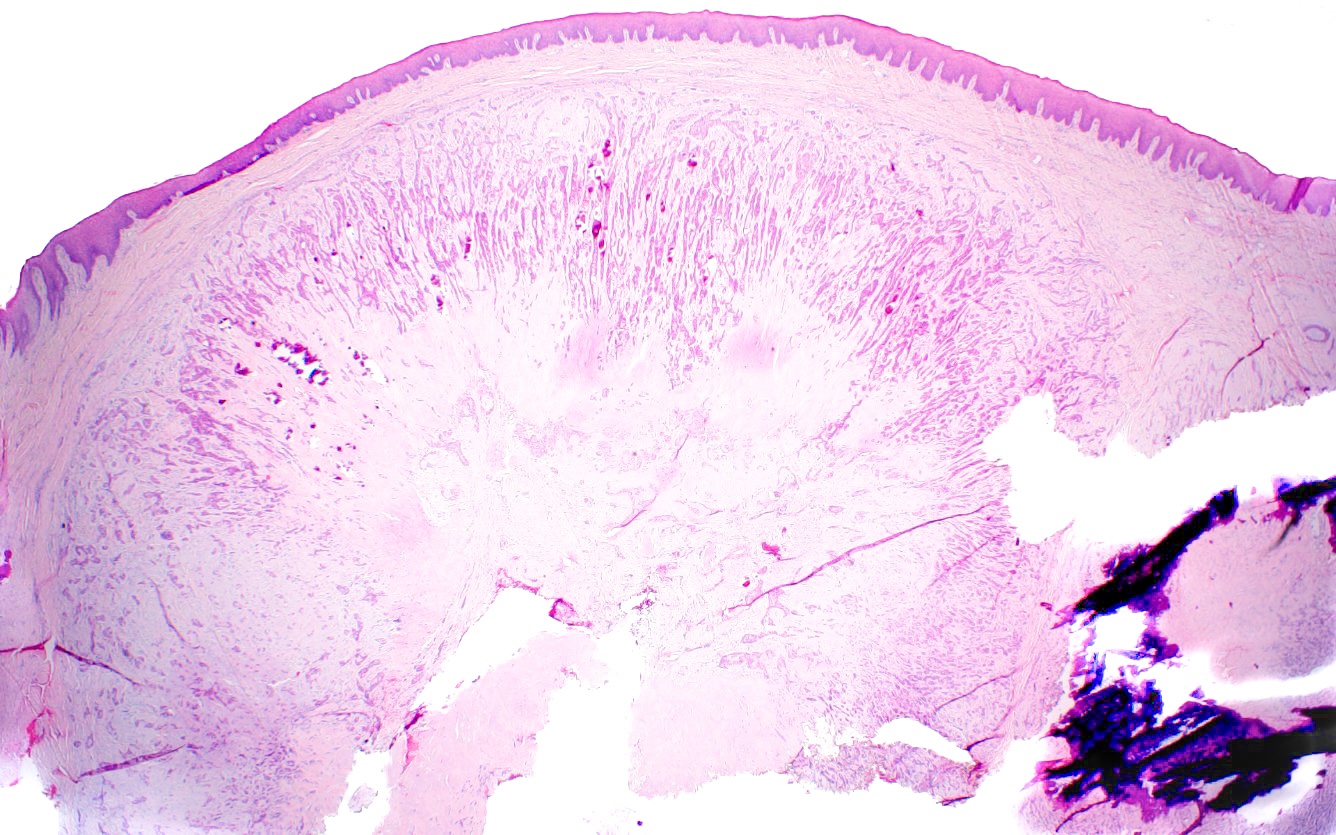
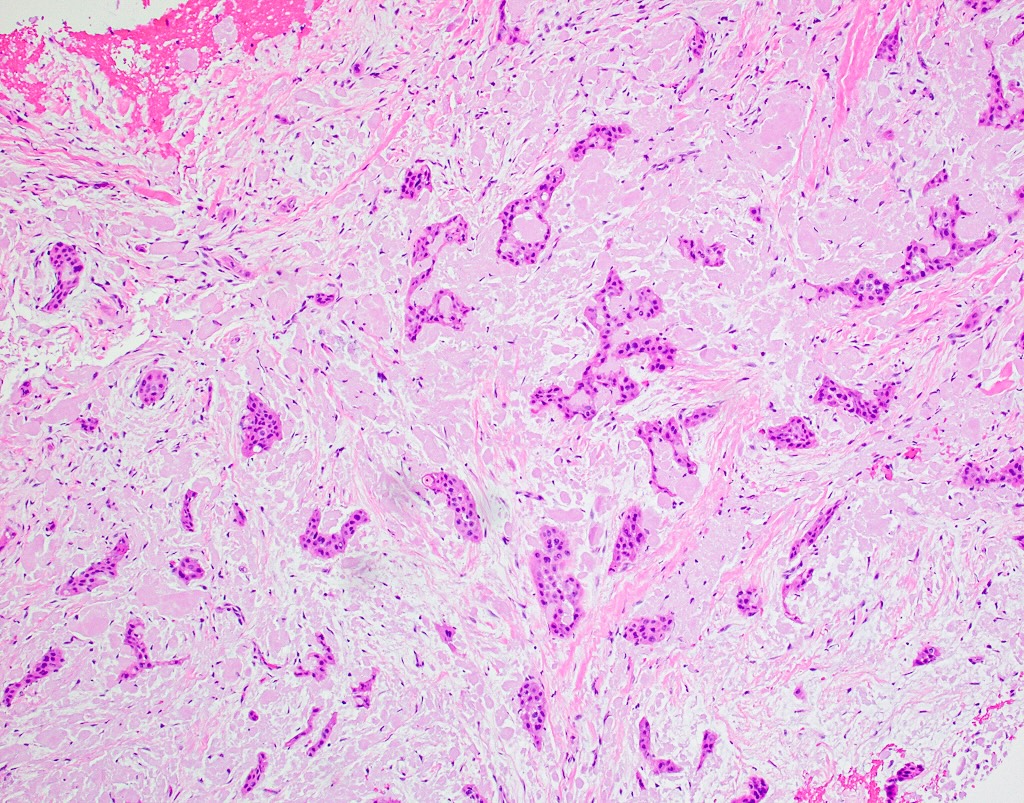
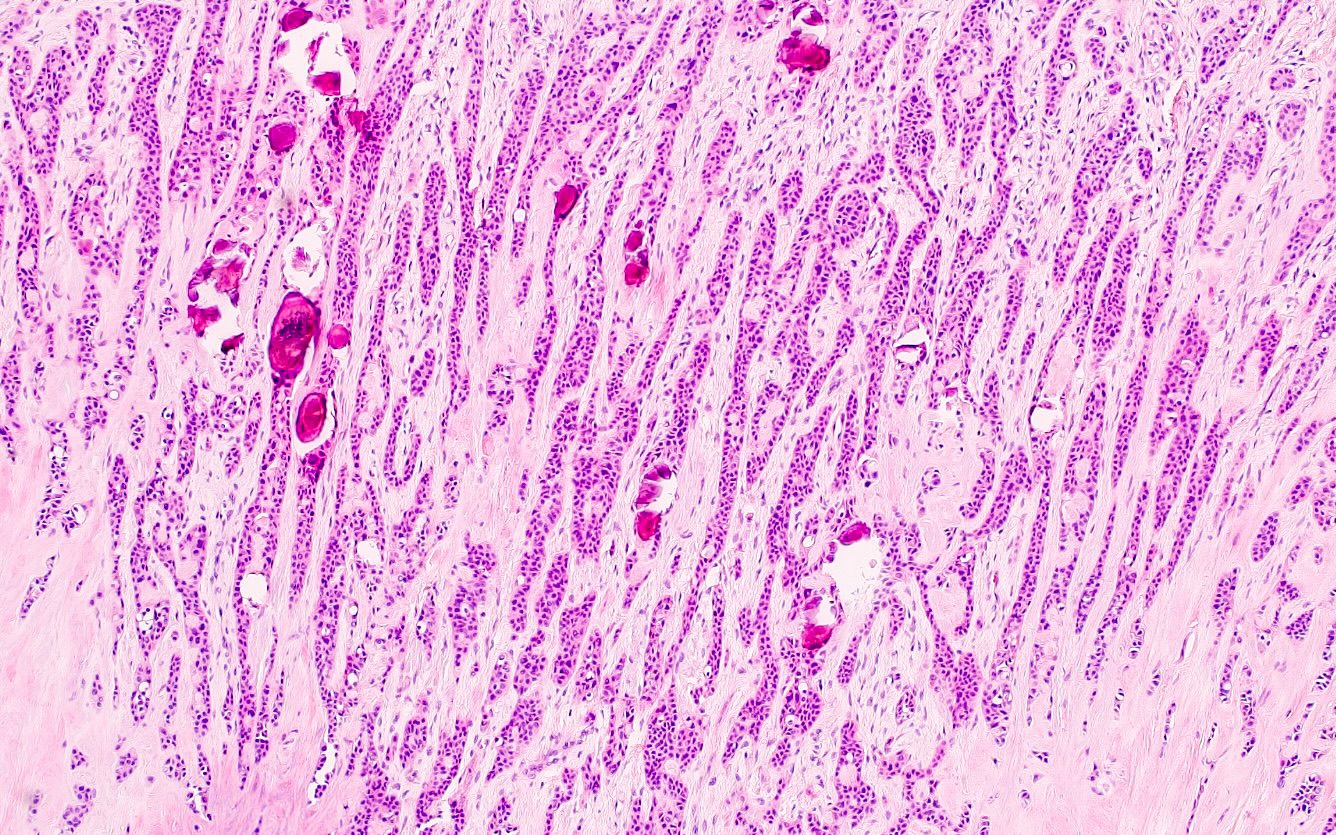
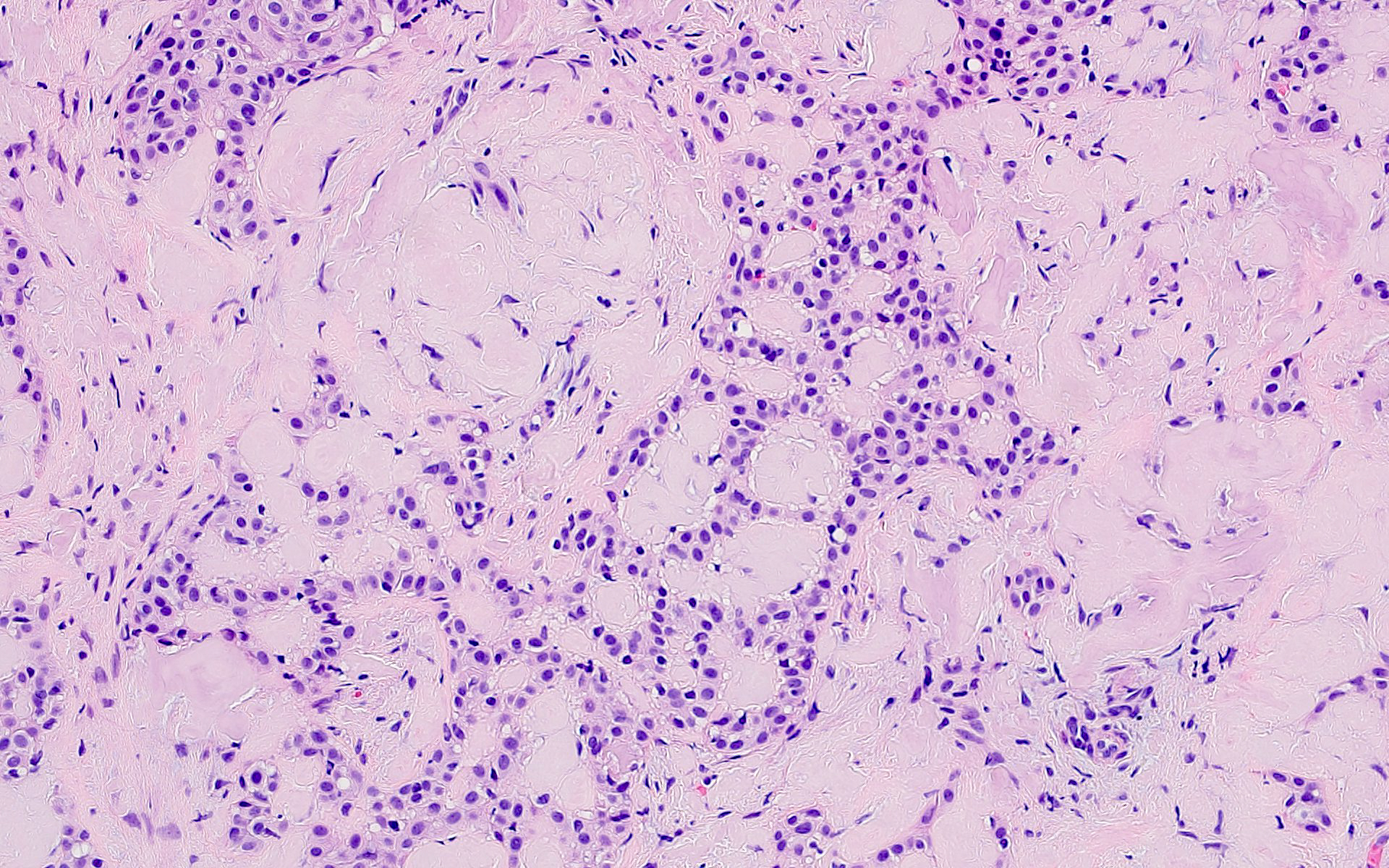
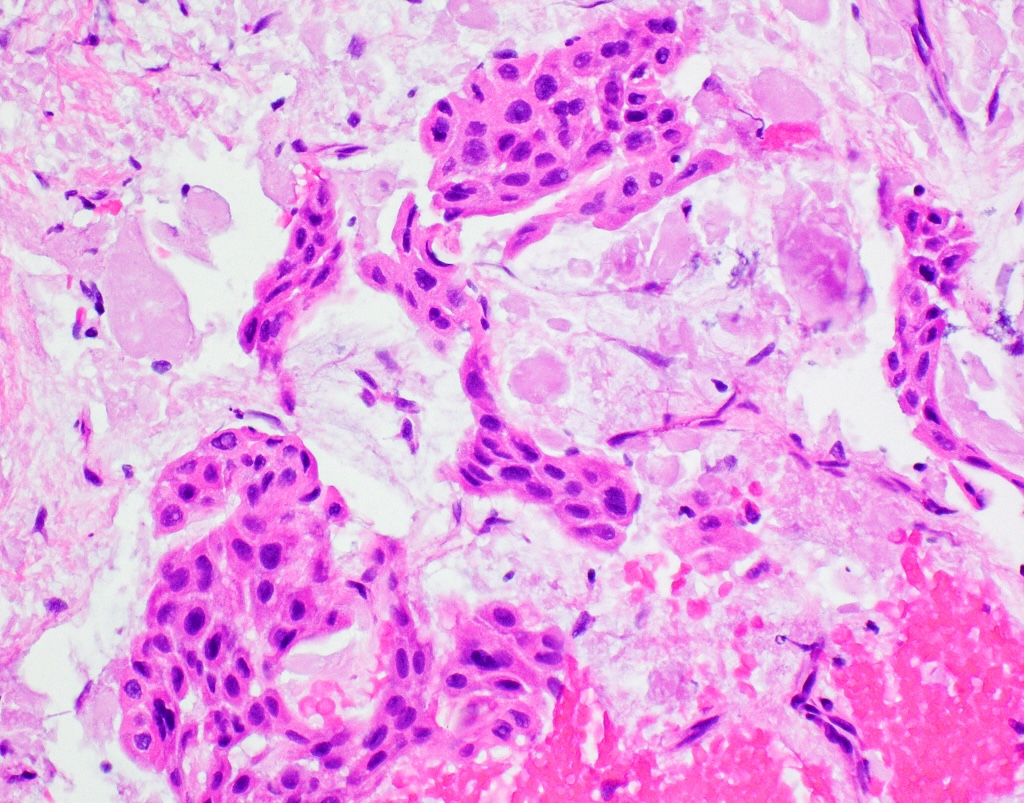
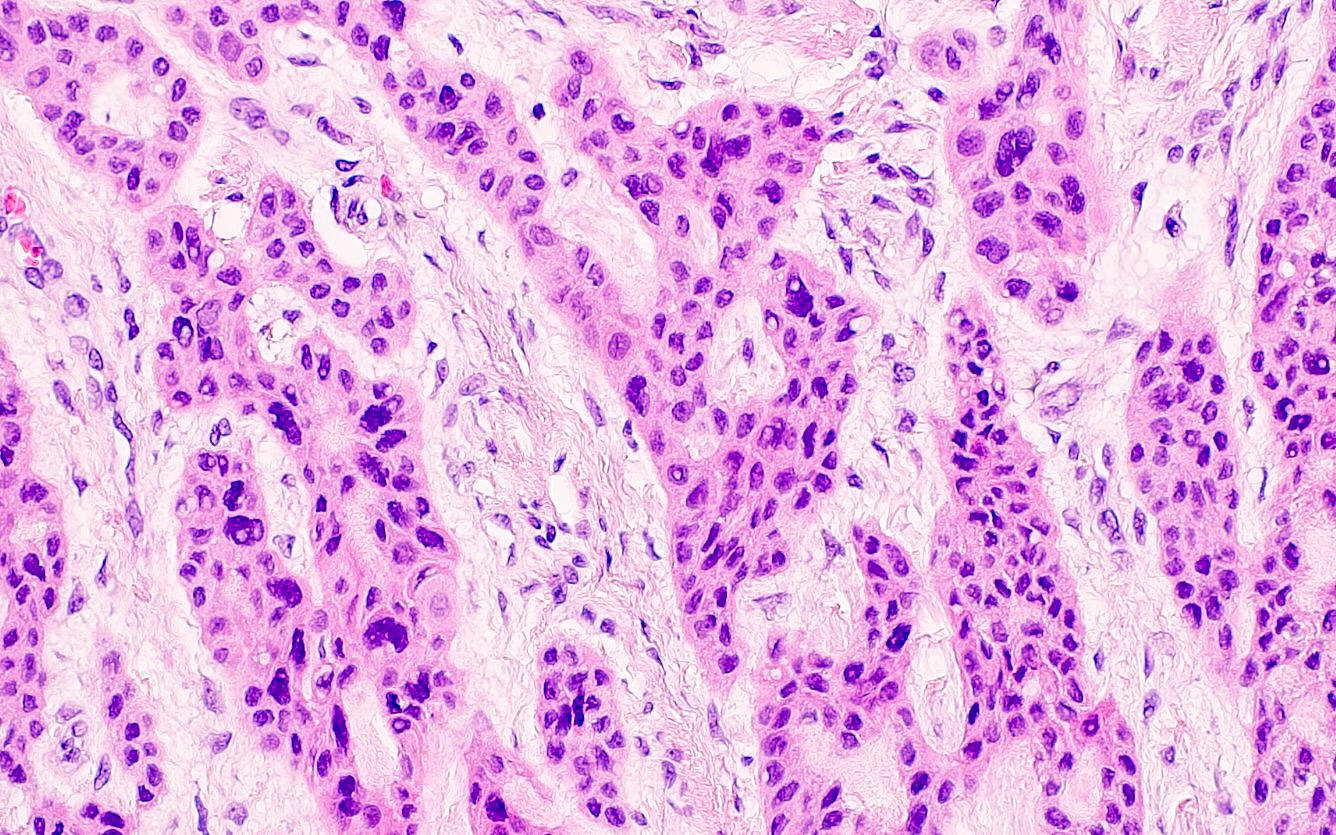
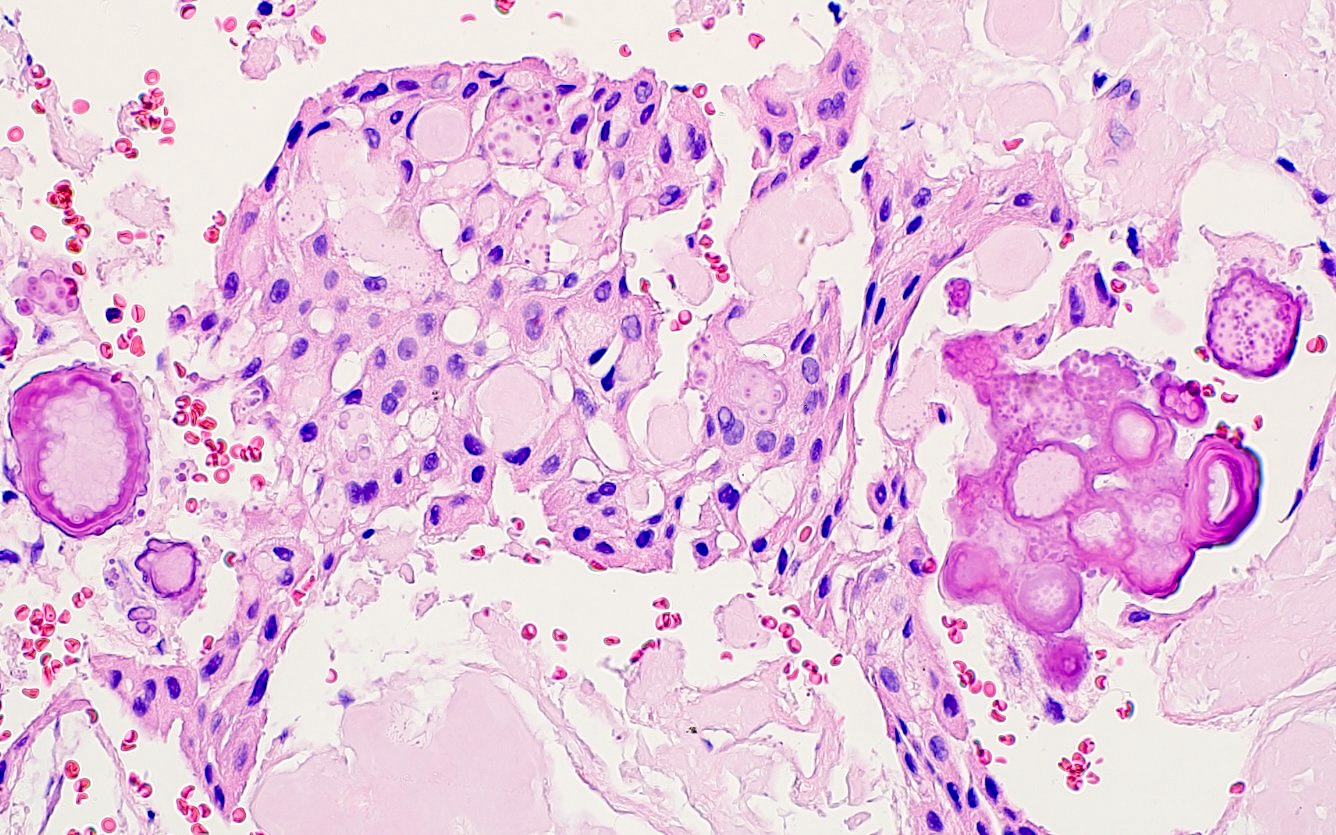
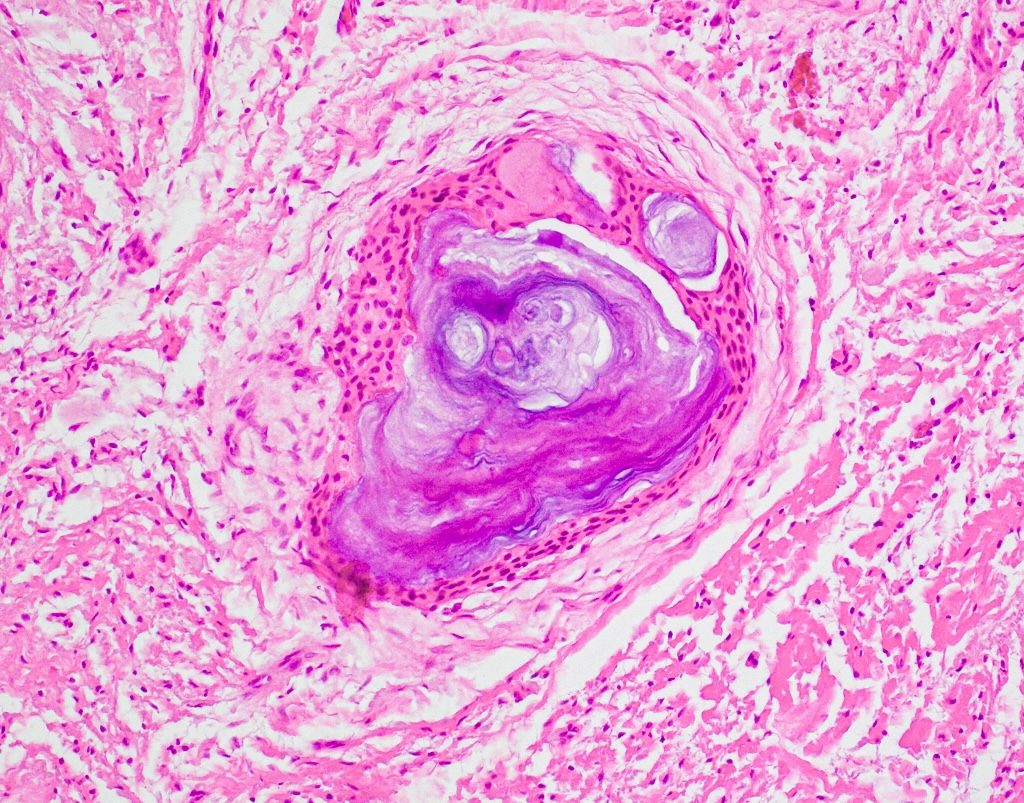
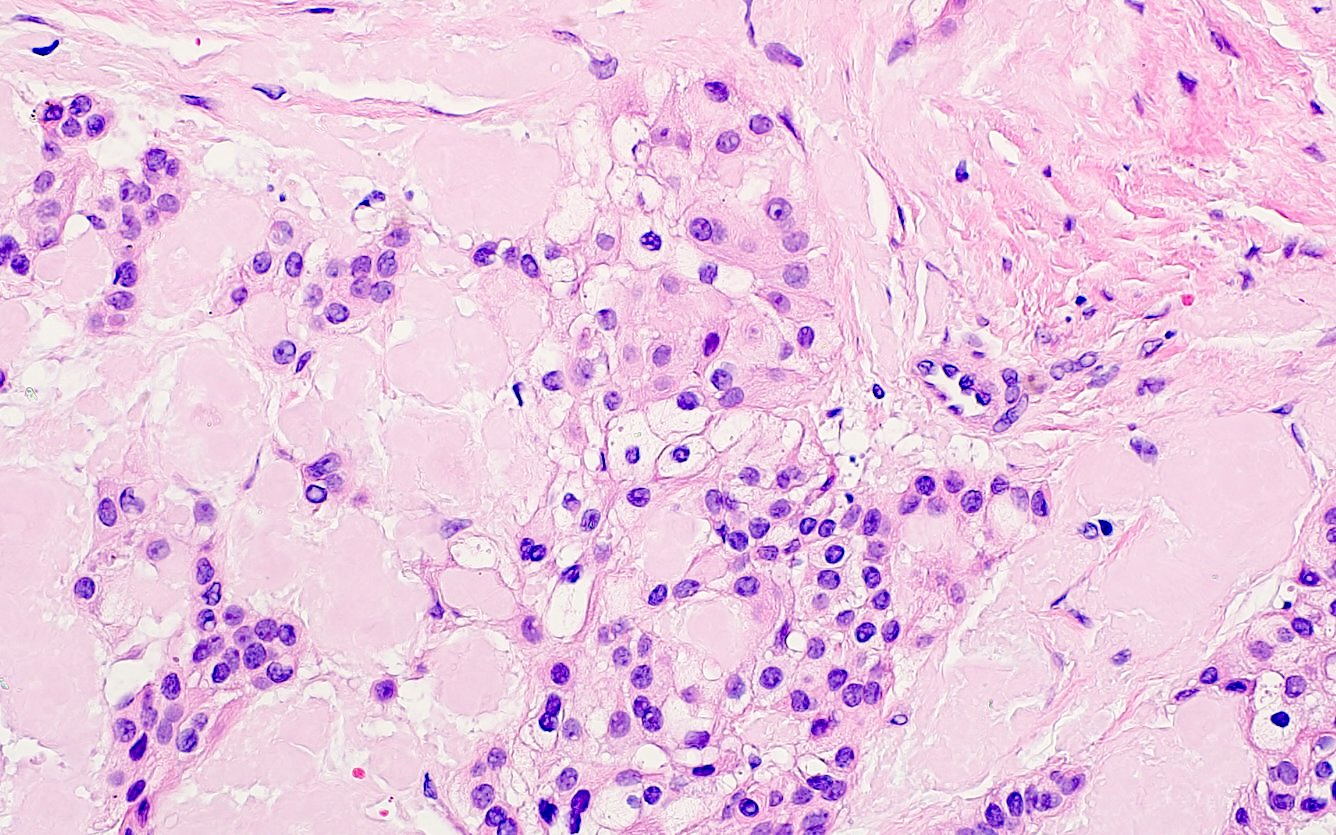
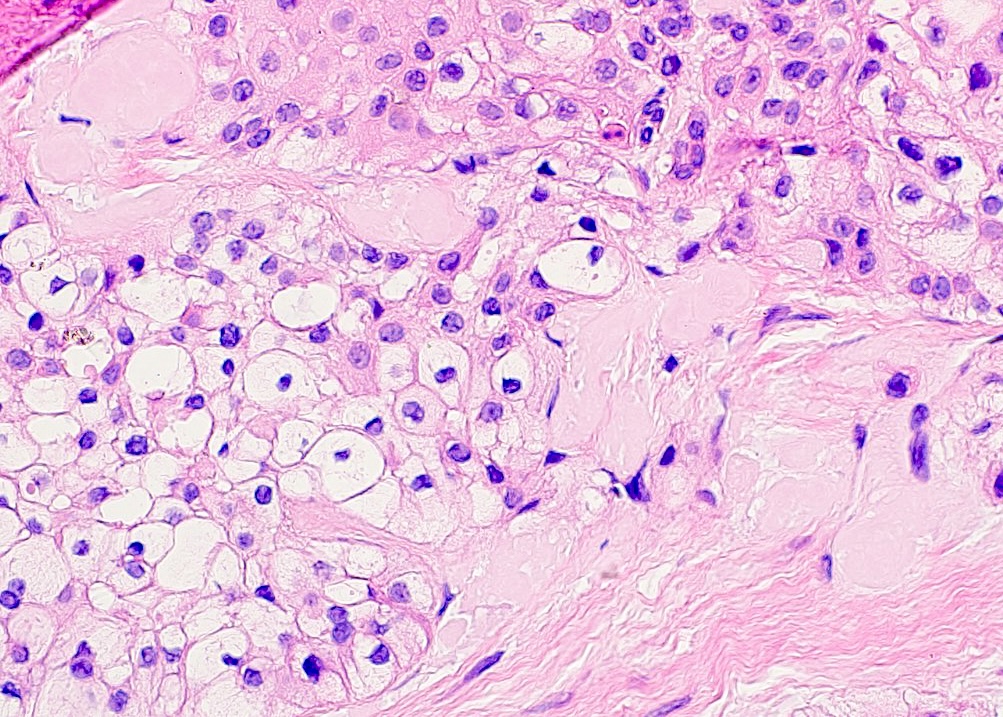
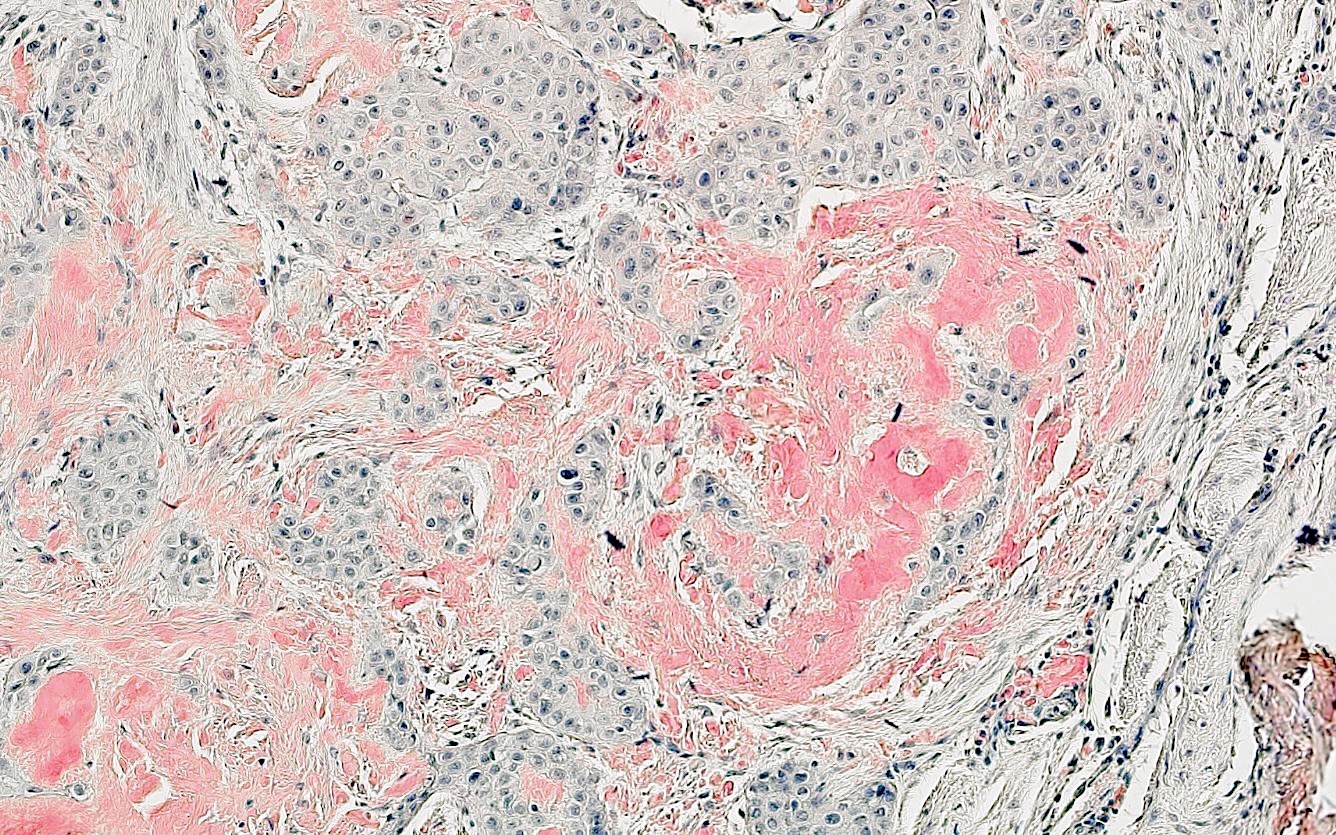
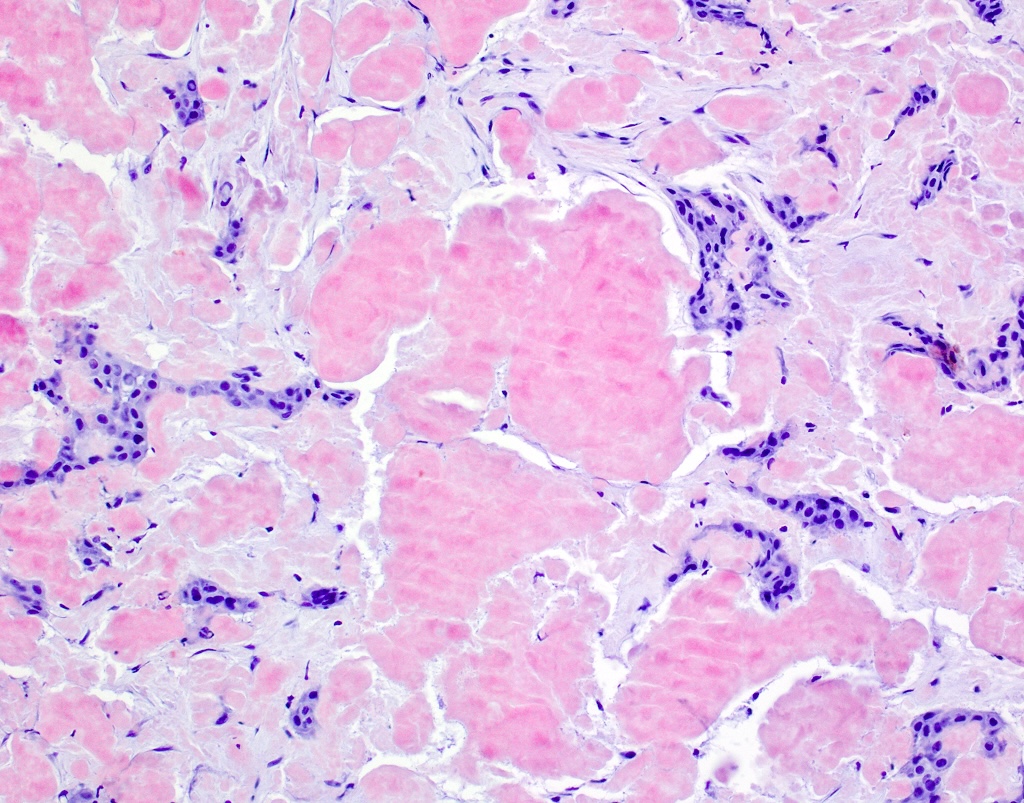
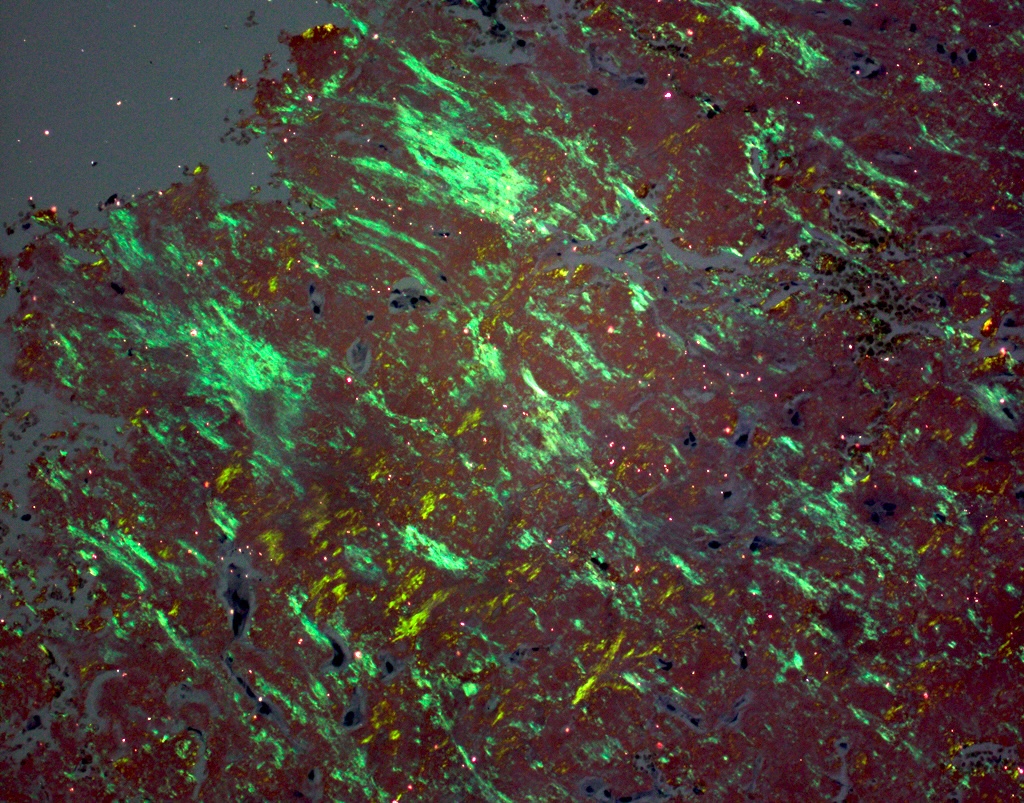
Microscopic (histologic) description
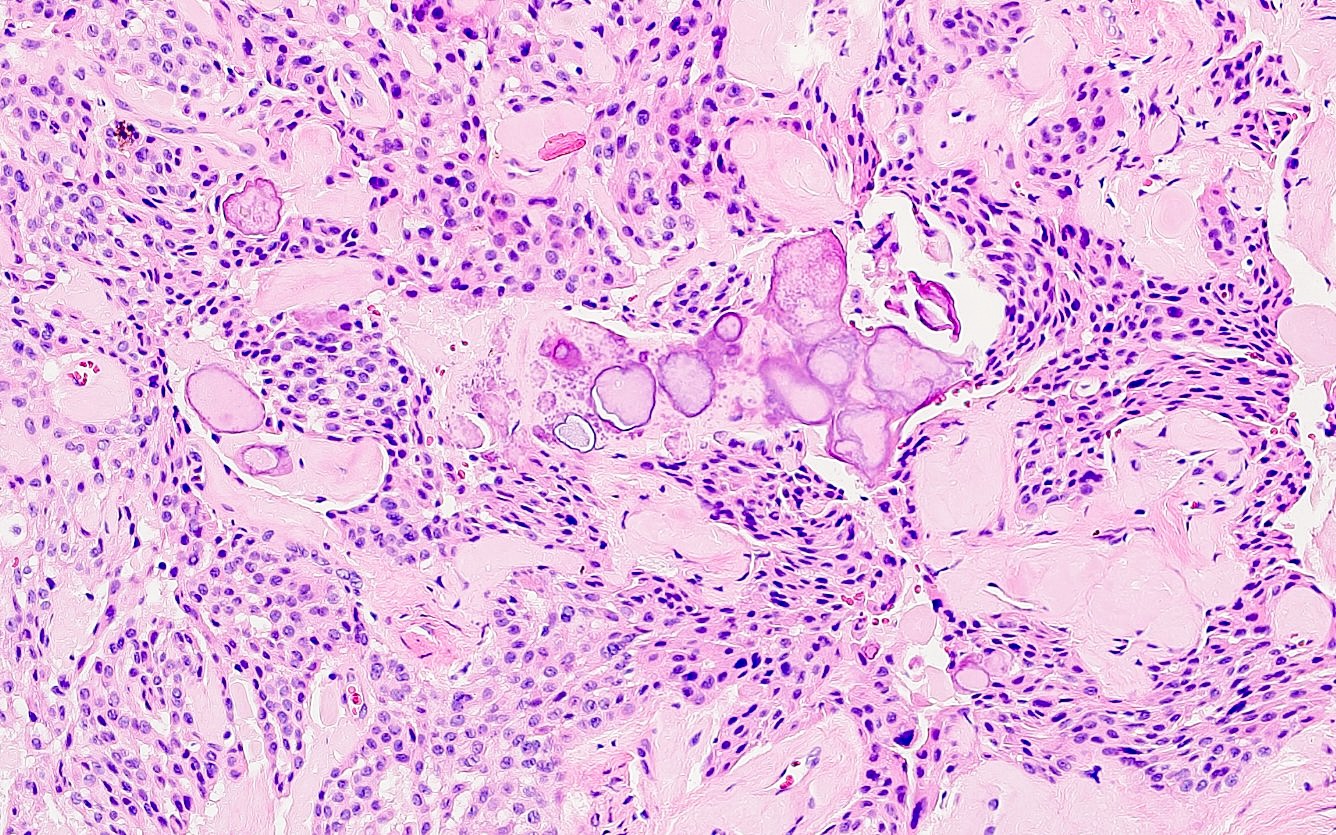
- Sheets, nests or cords of polyhedral cells often with nuclear pleomorphism
- Mitotic figures are rare or absent
- Nuclei may be hyperchromatic, angular or crinkled
- Distinct cell borders often with prominent intercellular bridges (prickles)
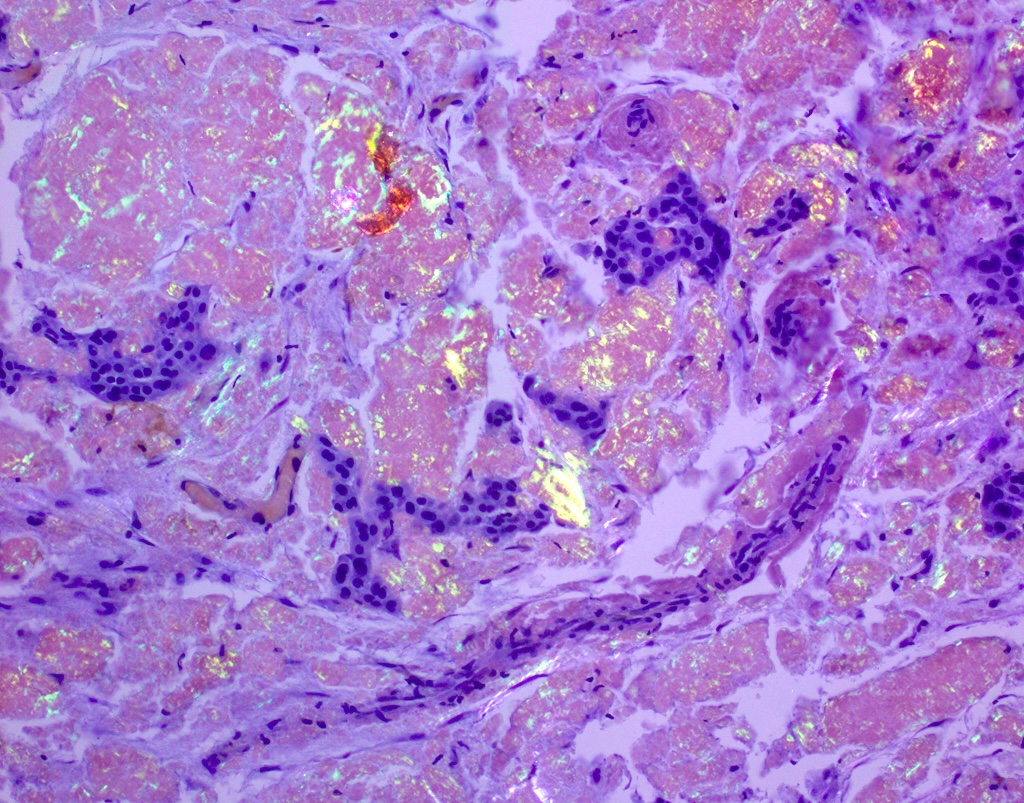
- Amorphous, congophilic eosinophilic amyloid
- Amyloid may calcify, forming masses or Liesegang rings (round basophilic calcifications with concentric laminations)
- Pseudoglandular structures and cystic spaces have been described (Head Neck Pathol 2018;12:598, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:773)
- Clear cell variant
- Clear cell variant shows focal to diffuse clear cells
- Noncalcifying / Langerhans cell rich variants
- Langerhans cell rich variant is an area of diagnostic uncertainty, with some suggesting that it represents an amyloid rich subtype of odontogenic fibroma and others suggesting it should be classified as a unique subtype of CEOT (Oral Surg Oral Med Oral Pathol Oral Radiol 2018;126:513, Head Neck Pathol 2023;17:313, Head Neck Pathol 2023;17:1011)
- At least 24 cases of combined adenomatoid odontogenic tumors - CEOT have been reported
- Clinically, these tumors behave indolently, similar to adenomatoid odontogenic tumors (Oral Surg Oral Med Oral Pathol 1983;55:487, Oral Oncol 1999;35:125)
Microscopic (histologic) images
Cytology description
- Clusters of round / polyhedral epithelial cells with numerous calcifications and amorphous eosinophilic, amyloid-like material (Acta Cytol 2005;49:533)
- May show pleomorphism (Acta Cytol 2006;50:545)
Positive stains
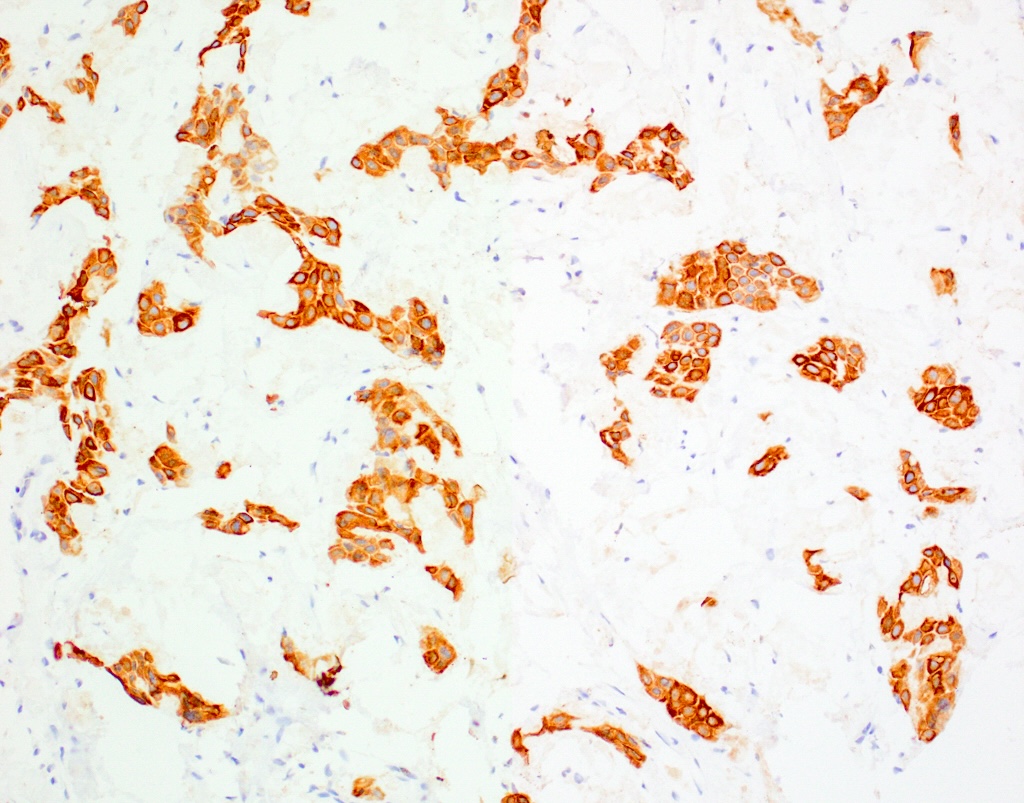
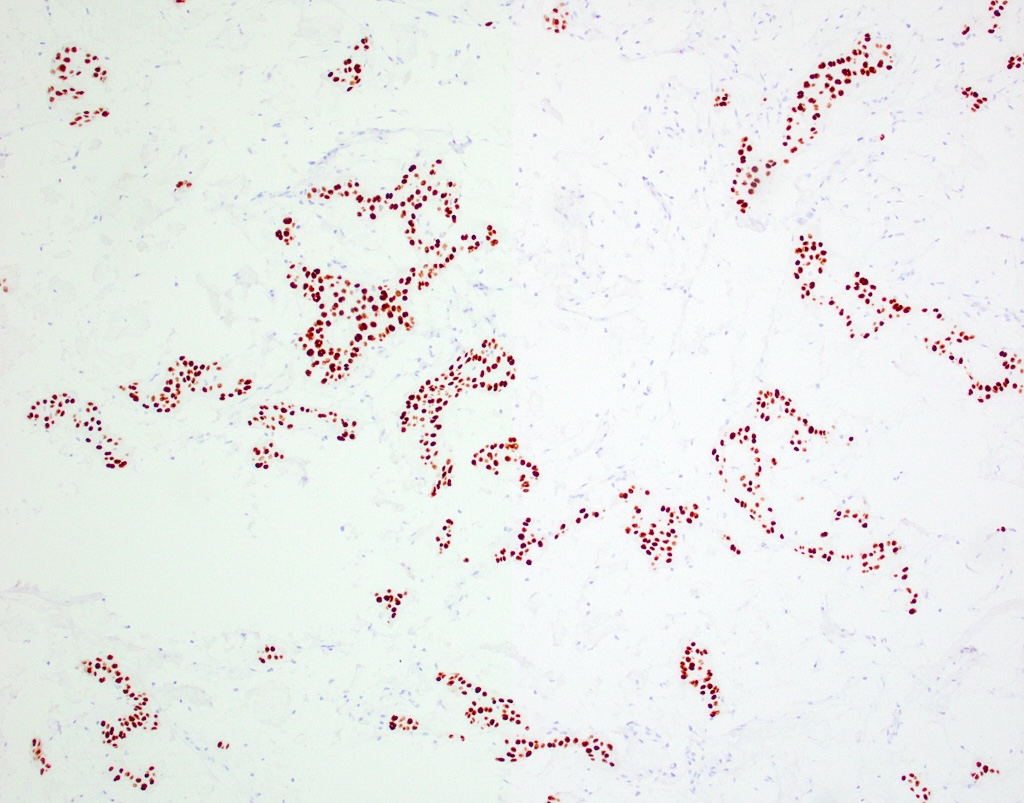
- Cytokeratins, CK5/6, p63, p40 (Korean J Pathol 2014;48:175)
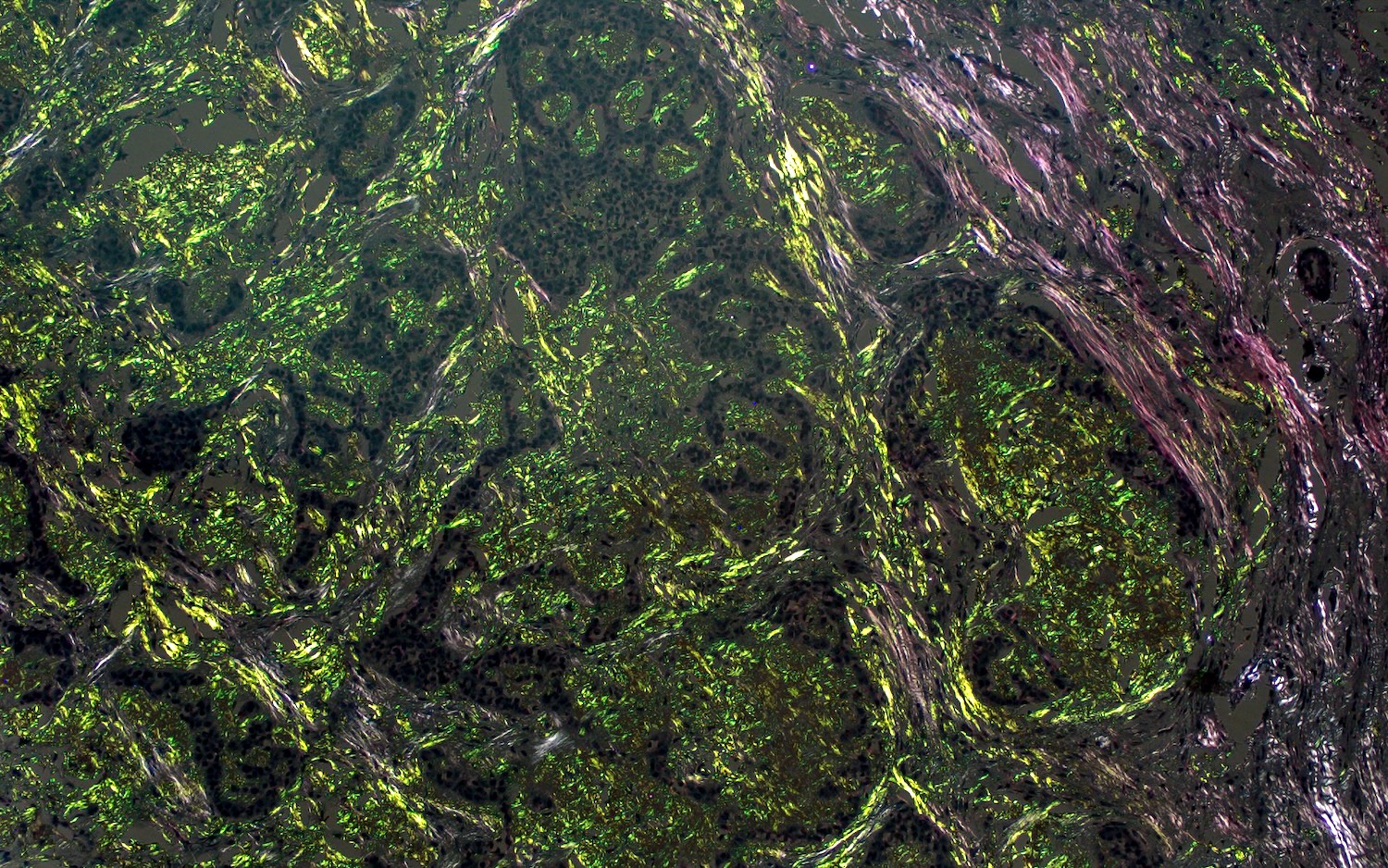
- Amyloid highlighted by Congo red with apple green birefringence
- Clear cell subtype has varying amounts of PAS positive, diastase labile accumulation
Molecular / cytogenetics description
- EWSR1 gene rearrangement is not found in CEOT, differentiating it from clear cell odontogenic carcinoma and hyalinizing clear cell carcinoma of salivary gland origin (Head Neck Pathol 2021;15:1391)
Videos
Clinical, radiographic, histological characteristics
Sample pathology report
- Mandible, incisional biopsy:
- Calcifying epithelial odontogenic tumor (see comment)
- Comment: Microscopic sections show a proliferation of islands and cords of polyhedral cells with prominent intercellular bridging and cellular pleomorphism. Mitotic figures are not readily identified. The epithelial cells are intermixed with basophilic concentric calcifications and globules of amyloid material which shows green birefringence upon polarization of the Congo red stained slide.
Differential diagnosis
- Microscopic differential diagnosis includes the following
- Central odontogenic fibroma, amyloid variant:
- Scattered small epithelial islands in a fibrous or fibromyxoid stroma with amyloid deposits
- Many believe that the Langerhans cell rich variant represents the amyloid rich subtype of odontogenic fibroma (Oral Surg Oral Med Oral Pathol Oral Radiol 2018;126:513, Head Neck Pathol 2023;17:313)
- Female predilection
- Anterior maxilla is most common location
- Clear cell odontogenic carcinoma:
- Polygonal cells with clear or faintly eosinophilic cytoplasm arranged into lobular sheets or nests
- May show zones of peripheral palisading
- Perineural invasion is noted in 33% of tumors
- EWSR1 gene rearrangement in 62.5% of cases (5 of 8) (Am J Surg Pathol 2013;37:1001)
- Hyalinizing clear cell carcinoma of salivary origin:
- Lacks large radiographic defect
- Clear or eosinophilic cells characterized by nests, cords or trabeculae with surrounding stroma ranging from densely hyalinized to desmoplastic or fibrocellular
- Prominent cellular atypia and increased mitotic figures are rare
- Perineural invasion in half of cases
- EWSR1 gene rearrangement in 92.3% of cases (12 of 13) (Am J Surg Pathol 2013;37:1001)
- Central mucoepidermoid carcinoma:
- Contains epidermoid, mucous and intermediate cells
- Mucocytes are positive with mucicarmine (J Oral Maxillofac Pathol 2021;25:204)
- May show MAML2 gene rearrangement
- Congo red negative
- Sclerosing odontogenic carcinoma:
- Poorly defined radiolucency
- Thin, single file cords, strands or nests of tumor cells set within a dense, fibrocollagenous sclerotic background stroma
- Perineural or intraneural invasion frequent
- Often with only minimal cellular atypia
- Locally aggressive
- Metastatic renal cell carcinoma:
- PAX8+
- May have known history of renal cell carcinoma
- Central odontogenic fibroma, amyloid variant:
Additional references
Practice question #1
A patient presents with a well defined radiolucency with speckled radiopacities in the posterior mandible. Biopsy reveals large islands of polyhedral cells intermixed with globules of amyloid which stain with Congo red. What is the diagnosis?
- Ameloblastoma
- Calcifying epithelial odontogenic tumor
- Calcifying odontogenic cyst
- Central mucoepidermoid carcinoma
Practice answer #1
B. Calcifying epithelial odontogenic tumor. It presents as a mixed radiolucent / radiopaque lesion with epithelial cells and amyloid material. Answer A is incorrect because ameloblastoma characteristically shows columnar cells, which exhibit peripheral palisading, reverse polarity and apical vacuolization. Answer C is incorrect because calcifying odontogenic cyst characteristically shows a cystic structure with ghost cells. Answer D is incorrect because central mucoepidermoid carcinoma demonstrates a proliferation of mucous cells, epidermoid cells and intermediate cells without the presence of congophilic amyloid.
Comment Here
Reference: Calcifying epithelial odontogenic tumor
Comment Here
Reference: Calcifying epithelial odontogenic tumor
Practice question #2
Which odontogenic tumor contains Congo red staining with green birefringence under polarized light? This tumor does not demonstrate EWSR1 rearrangements, differentiating it from other entities in the differential diagnosis.
- Ameloblastoma
- Calcifying epithelial odontogenic tumor
- Clear cell odontogenic carcinoma
- Gorlin cyst
Practice answer #2
B. Calcifying epithelial odontogenic tumor. It demonstrates islands, nests or cords of often pleomorphic appearing polyhedral cells intermixed with Congo red positive amyloid material. Answer A is incorrect because ameloblastoma is not positive for amyloid material upon staining with Congo red. Answer C is incorrect because clear cell odontogenic carcinoma frequently shows EWSR1 rearrangements. Answer D is incorrect because Gorlin cyst, often known as calcifying odontogenic cyst, is a cystic structure with ghost cells. Congo red positivity is not noted in calcifying odontogenic cysts.
Comment Here
Reference: Calcifying epithelial odontogenic tumor
Comment Here
Reference: Calcifying epithelial odontogenic tumor