Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Asiry S, Rao RA. Mucoepidermoid carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsmec.html. Accessed October 5th, 2025.
Definition / general
- Malignant glandular epithelial neoplasm characterized by mucous, intermediate and epidermoid cells, with columnar, clear cell or oncocytoid features
Essential features
- Malignant epithelial neoplasm
- Characterized by mucous, intermediate and epidermoid cells, with columnar, clear cell or oncocytoid features
- Most common malignant salivary gland neoplasm in both adults and children
- Prognosis influenced by tumor stage, tumor site, surgical margins (WHO 2017)
- Associated with a specific translocation t(11;19)(q14-21;p12-13) with CRTC1(MECT1)-MAML2 fusion
Terminology
- Mucoepidermoid carcinoma (MEC)
- Not recommended: mucoepidermoid tumor
ICD coding
Epidemiology
- Most common malignant salivary gland tumor (adults and children) (Br J Oral Maxillofac Surg 2013;51:399)
- Represents 10 - 15% of all salivary gland tumors (Br J Oral Maxillofac Surg 2013;51:399)
- Adults: wide age range (15 - 86 years, median 49 years) (Am J Surg Pathol 2001;25:835)
- Children: 11 - 15 years (median 13 years) (Int J Pediatr Otorhinolaryngol 2019;120:93)
- F > M (slight predominance) (Br J Oral Maxillofac Surg 2013;51:399)
Sites
- Occurs in major and minor salivary glands (predominance of major > minor) (Eur J Surg Oncol 2021;47:1376)
- Major: parotid > submandibular > sublingual (Eur J Surg Oncol 2021;47:1376)
- Minor: palate, buccal mucosa, retromolar region (Indian J Pathol Microbiol 2018;61:397)
- Rarely occurs in sinonasal tract, nasopharynx, lungs and intraosseous mandible (Int Forum Allergy Rhinol 2019;9:1046, Expert Rev Respir Med 2018;12:249, Case Rep Dent 2018;2018:9348540)
Etiology
- Possible association with ionizing radiation (Indian J Pathol Microbiol 2018;61:397)
Clinical features
- In one study, 33% of patients are asymptomatic; however, varies with tumor site and size (J Stomatol Oral Maxillofac Surg 2020;121:713)
- Most common presentation is painless swelling with pressure and discomfort
- Can be variably fixed, rubbery or soft mass (J Stomatol Oral Maxillofac Surg 2020;121:713)
Diagnosis
- Preoperative assessment (radiology) may consist of:
- Ultrasonography (USG) for small tumors in major salivary glands
- Larger recurrent tumors: CT imaging for bone involvement, MRI for soft tissue delineation (Semin Radiat Oncol 2012;22:245)
- Evidence of (18)-fluorodeoxyglucose positron emission tomography CT in locoregionally advanced tumors (Nucl Med Commun 2013;34:211)
- Preoperative assessment (fine needle aspiration)
Radiology description
- Influenced by tumor size, location and possibly tumor grade
- Ultrasonography:
- Typically a well circumscribed hypoechoic lesion, with a partial or completely cystic appearance against a relatively hyperechoic normal parotid gland
- CT:
- Lower grade tumors are well circumscribed with cystic component (see Radiology images)
- Enhancing solid component and calcifications occasionally seen
- Higher grade tumors are solid and show poorly defined, infiltrative margins
- MRI:
- Low grade tumors are similar in appearance to a pleomorphic adenoma
- Higher grade tumors are solid, with a lower signal on T2 and poorly defined margins
- Reference: Radiopaedia: Mucoepidermoid Carcinoma of Salivary Glands [Accessed 8 January 2021]
Prognostic factors
- Adults:
- Excellent prognosis, with approximately 98.8% 5 year survival rate in low grade and 97.4% in intermediate grade tumors
- About 67% 5 year survival rate for high grade tumors
- Children:
- 5 year survival of 98%, as they predominantly present with low to intermediate grade tumors
- Negative prognostic variables
- Tumor arising in the submandibular gland: lymph node metastases common
- Positive surgical margins
- Extraparenchymal extension
- Nodal / distant metastases
- Increased expression of MUC1
- References: J Stomatol Oral Maxillofac Surg 2020;121:713, Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2016
Case reports
- 16 year old boy with a mandibular radiolucent lesion (Case Rep Dent 2018;2018:9348540)
- 36 year old man with a left parotid gland mass (Anticancer Res 2019;39:3213)
- 69 year old woman with a right submental mass (Eur Ann Otorhinolaryngol Head Neck Dis 2017;134:355)
Treatment
- Complete surgical resection
- Conservative approach for stage I and stage II tumors
- Wide excision with wide margin for high grade tumors or tumors with positive margins
- Neck lymph node dissection (depends on nodal status and histologic grade)
- Adjuvant radiotherapy and chemotherapy might be considered for higher grade tumors
- Reference: J Stomatol Oral Maxillofac Surg 2020;121:713
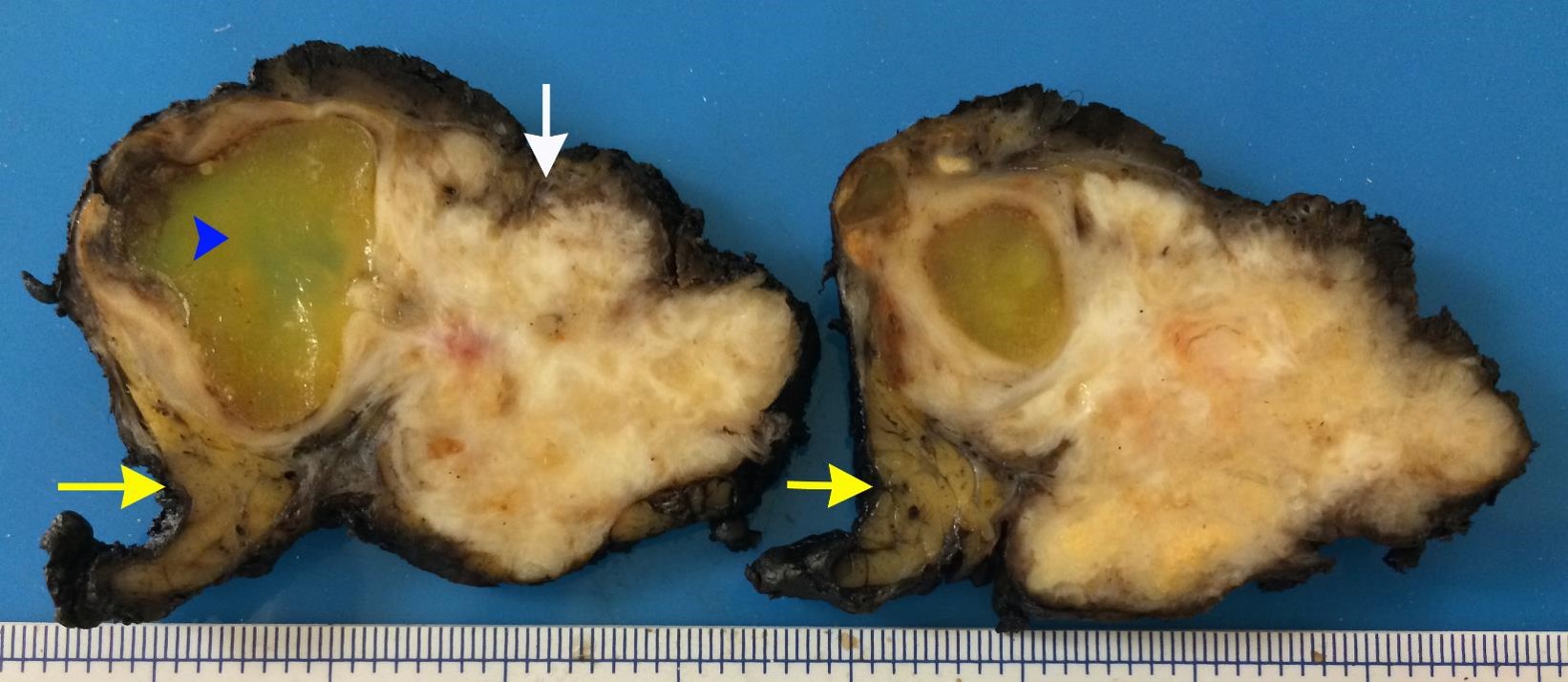
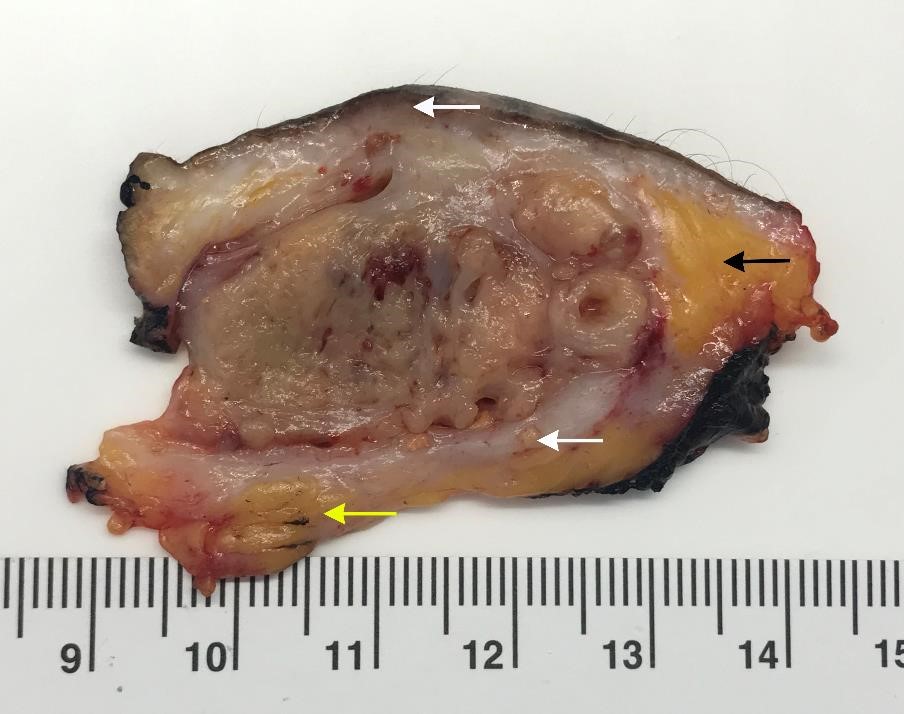
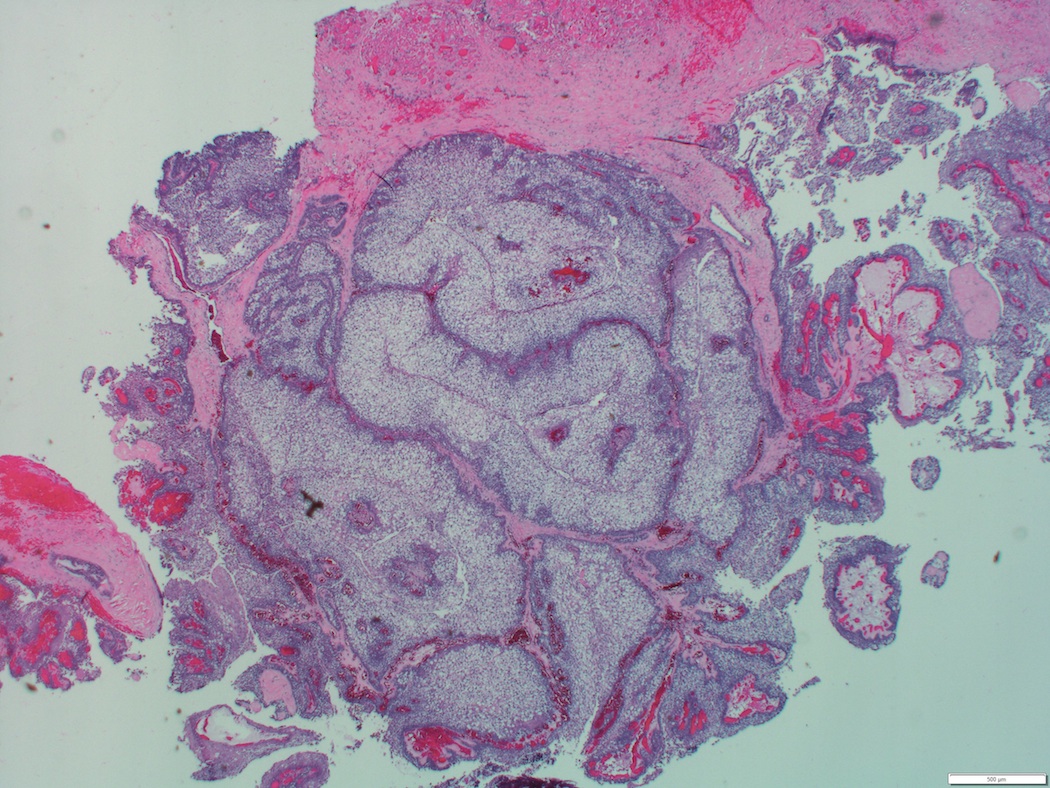
Gross description
- Incompletely encapsulated or unencapsulated
- Well circumscribed
- Low grade: often cystic
- High grade: often solid, necrotic, tan-pink
- References: J Stomatol Oral Maxillofac Surg 2020;121:713, Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2016
Frozen section description
- Higher grade tumors can be mistaken for squamous cell carcinoma, a pitfall (Cancer 2004;100:1876)
Frozen section images
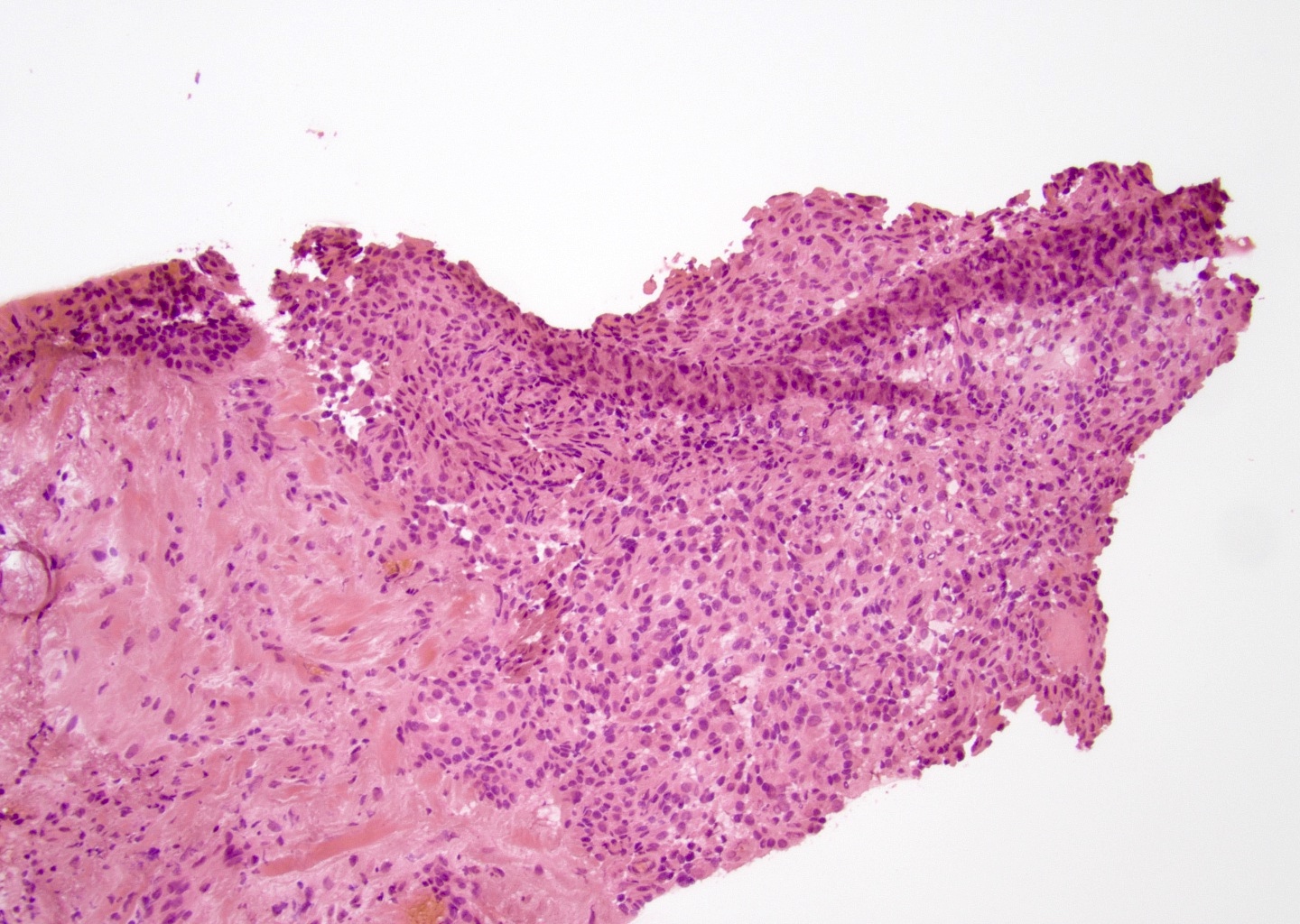
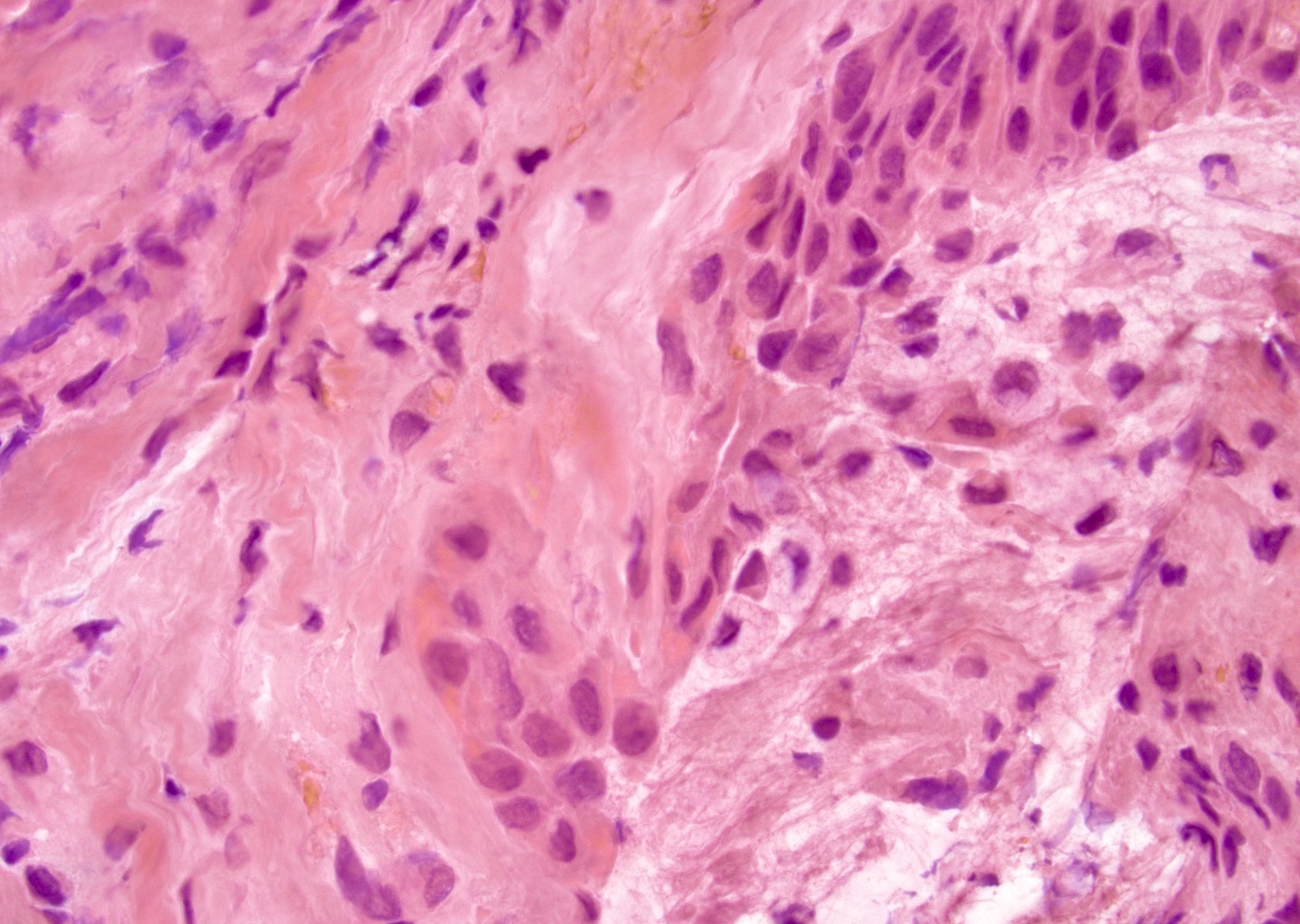
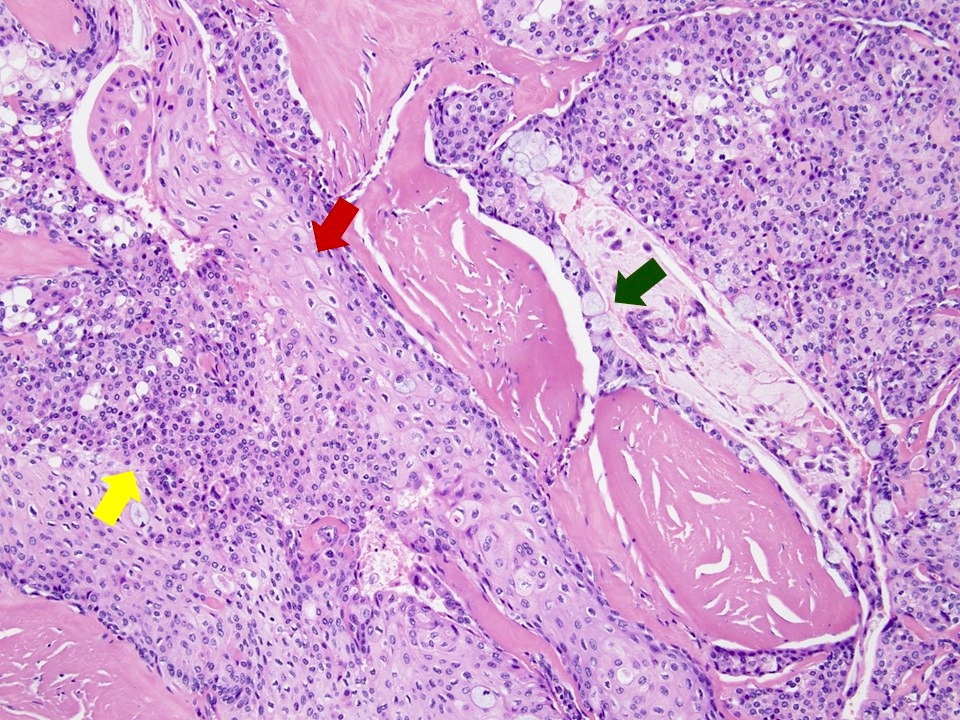
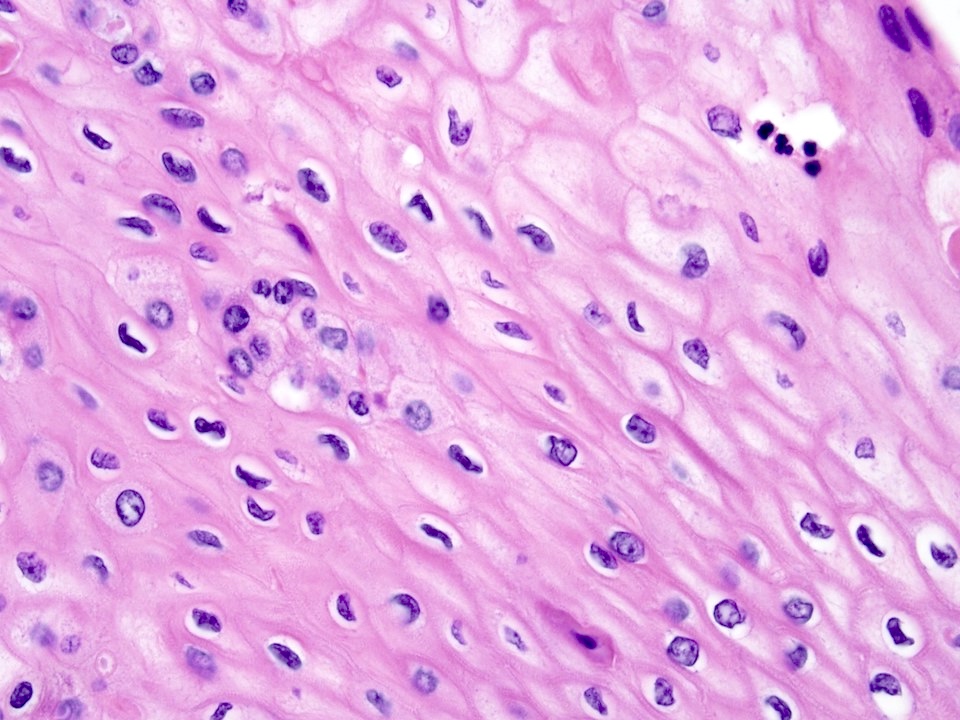
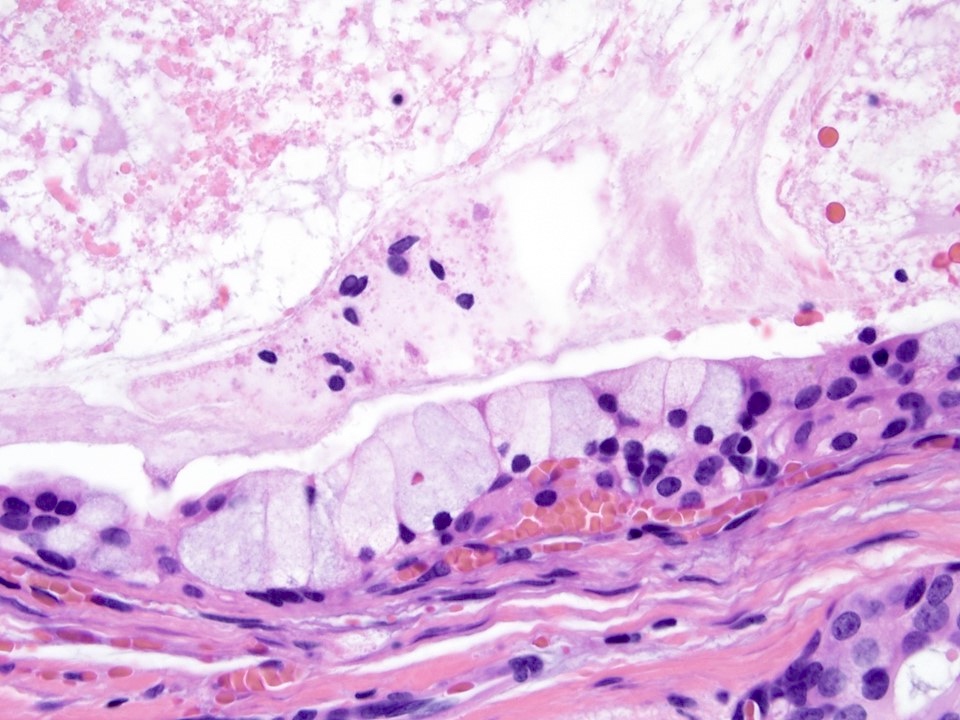
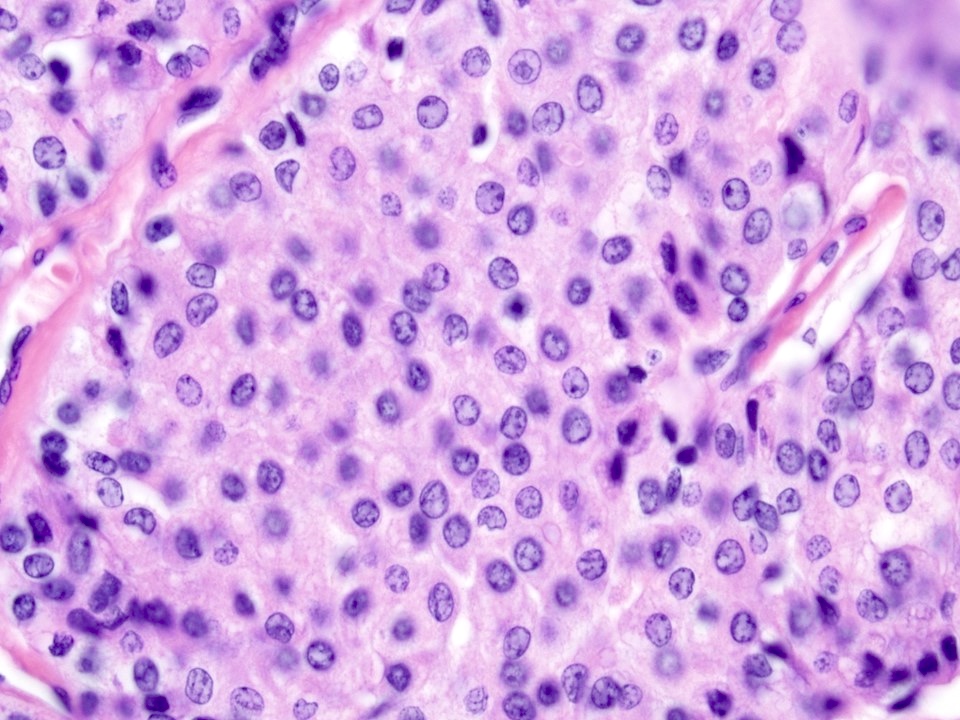
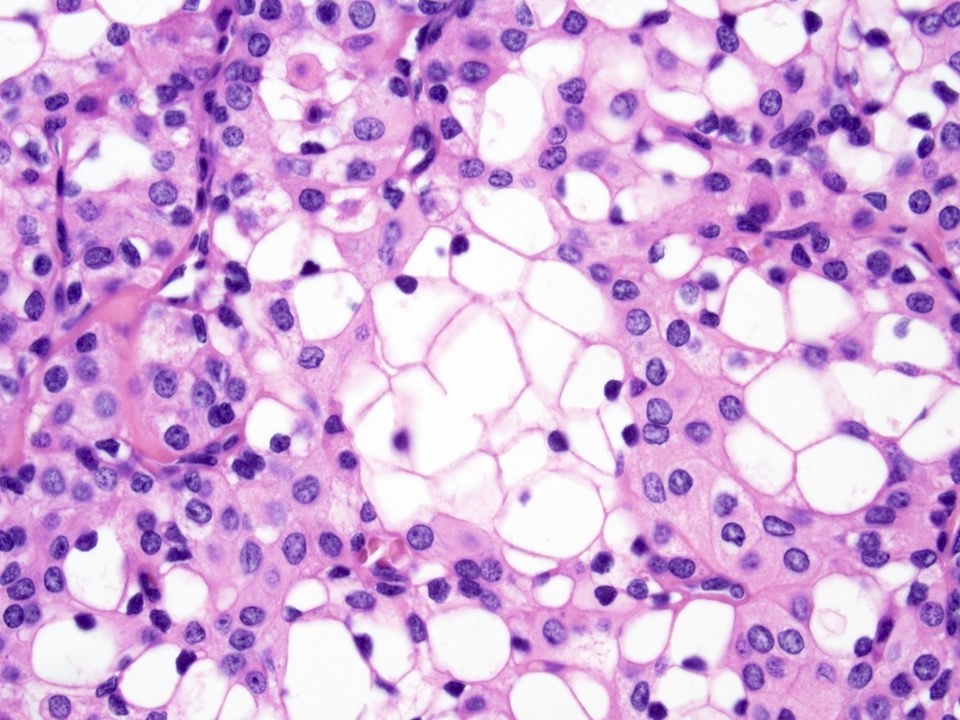
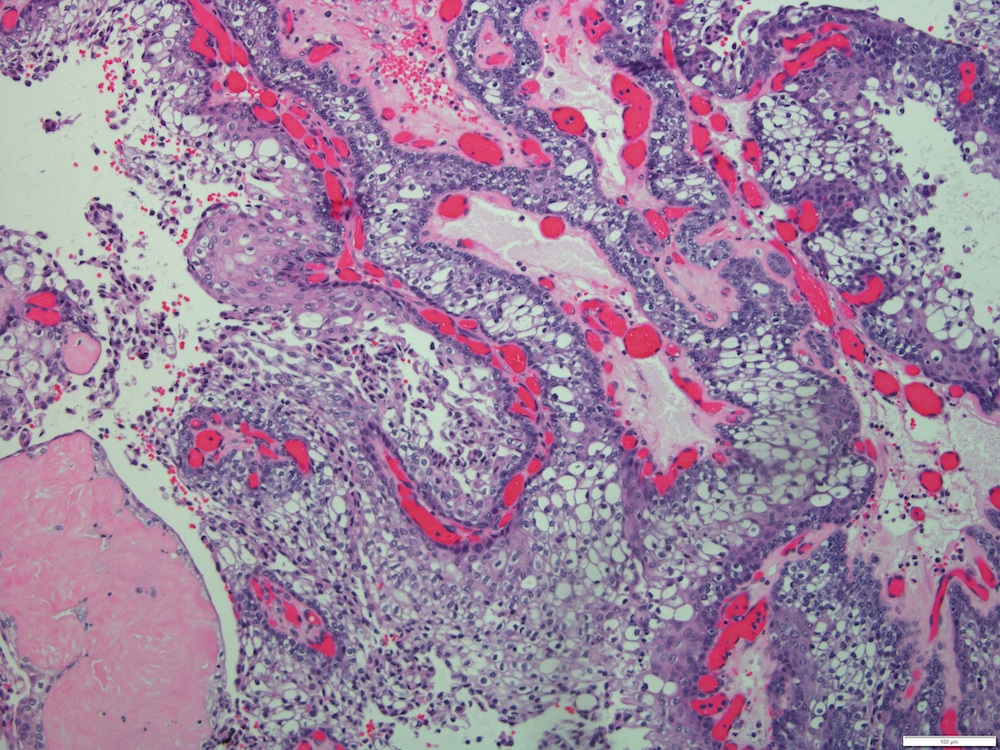
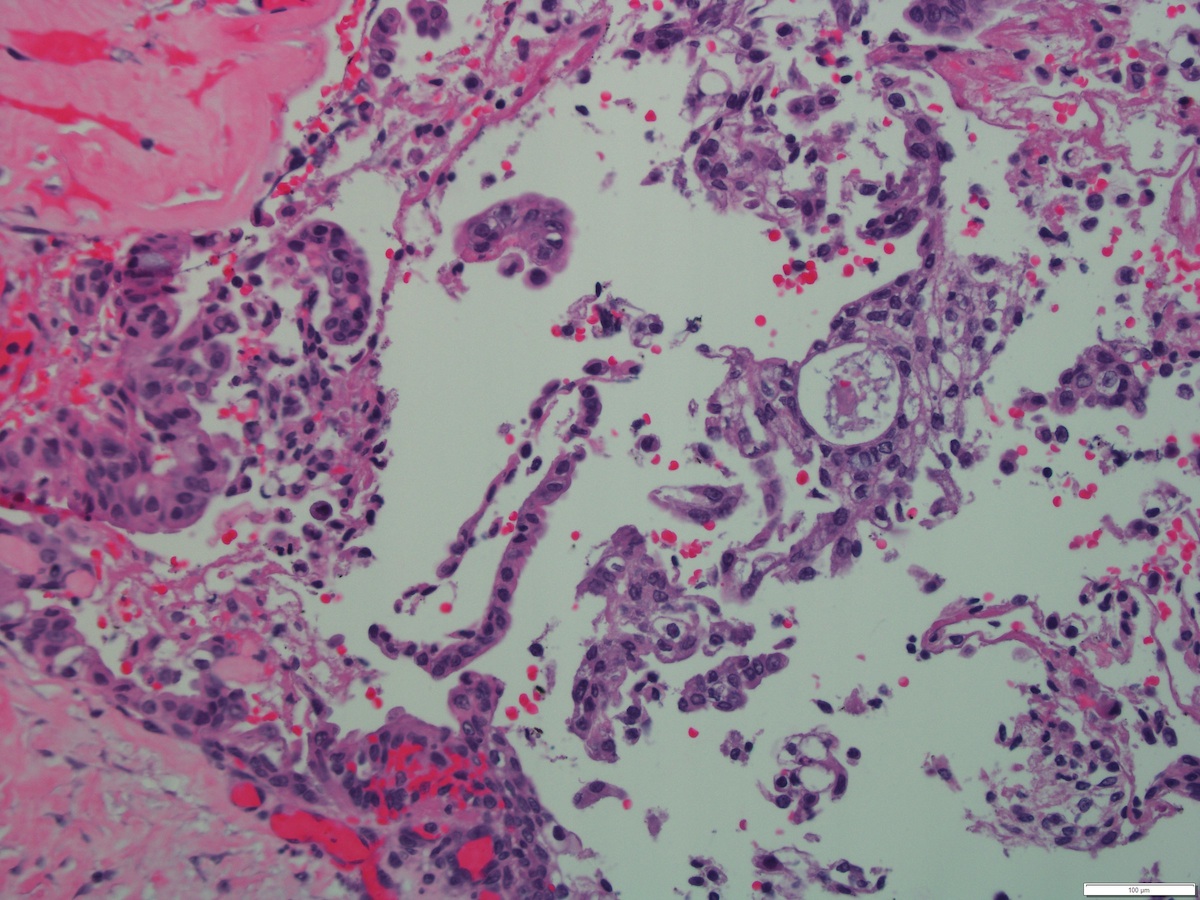
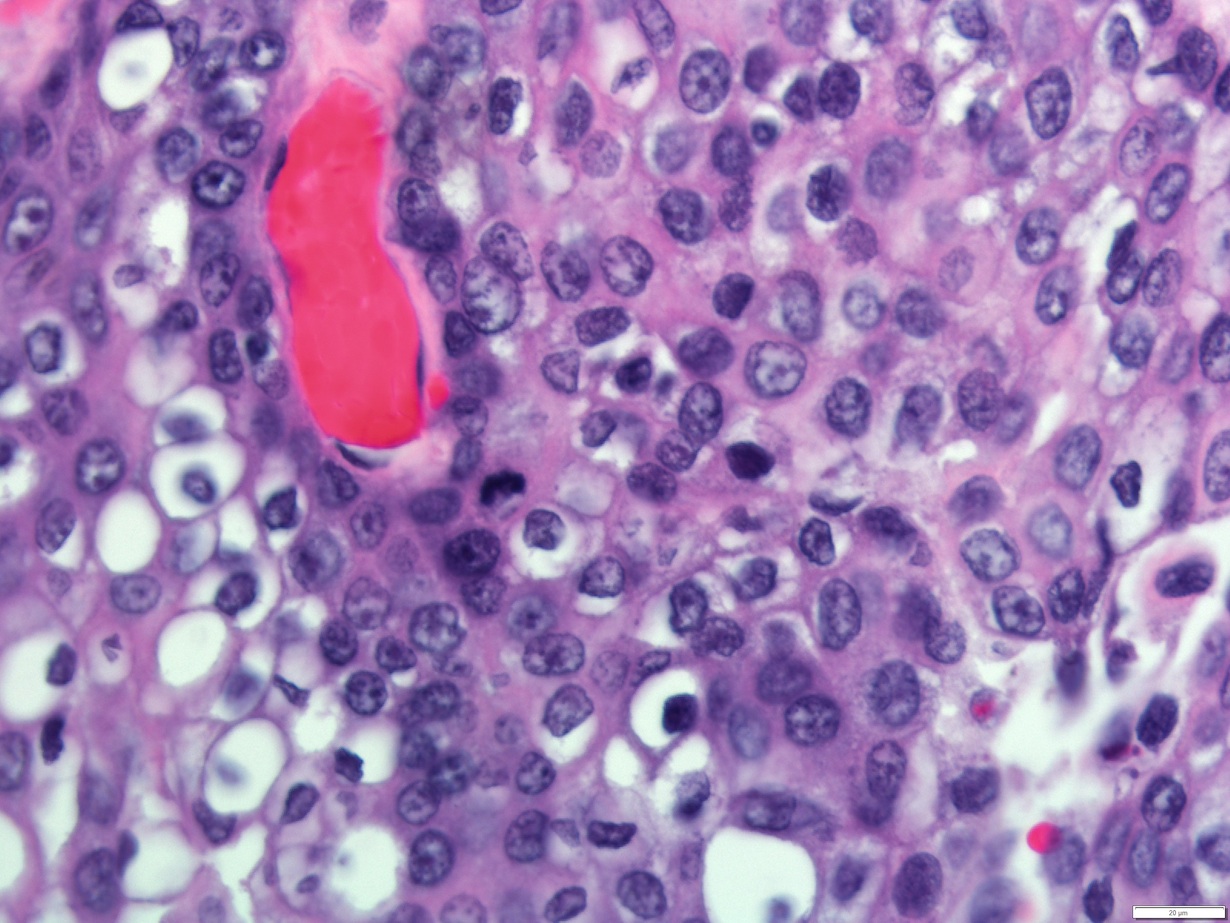
Microscopic (histologic) description
- Solid, cystic or mixed growth patterns
- Can show papillary or glandular growth pattern
- Areas suggesting a capsule can be seen in low grade mucoepidermoid carcinoma
- Varying proportions of epidermoid cells, intermediate cells and mucocytes
- Solid nests, sheets or cords of epidermoid cells
- Overt keratinization is rare
- Mucous cells embedded in epidermoid cell nests or lining cystic spaces
- Intermediate cells found within epidermoid cell nests or forming separate nests
- Background stromal sclerosis
- Luminal or extracellular pools of mucin may be present
- Mitosis, necrosis and pleomorphism more commonly seen in high grade tumors
- Limited number of mucocytes and cystic spaces in high grade tumors
- Perineural and lymphovascular invasion possible (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2016)
- Focal clear cell changes can occur due to accumulation of glycogen
- Histologic variants: clear cell, oncocytic, sclerosing, Warthin-like, ciliated, spindle cell and mucoacinar (Am J Surg Pathol 2015;39:1479, Am J Surg Pathol 2018;42:130, Int J Surg Pathol 2017;25:705, Am J Surg Pathol 2021;45:1028, Am J Surg Pathol 1999;23:523)
- Reference: J Stomatol Oral Maxillofac Surg 2020;121:713
Histopathologic grading:
- 4 histologic grading systems (2 quantitative and 2 qualitative)
- 2 different morphologic quantitative point systems, although histologic grading using any grading system appears to be inconsistent (Am J Surg Pathol 2019;43:885)
- Significant grading disparity between pathologists (Am J Surg Pathol 2019;43:885)
- Armed Forces Institute of Pathology (AFIP) grading scheme (quantitative) (Am J Surg Pathol 2019;43:885)
- Criteria:
- Intracystic component less than 20% (2)
- Neural invasion (2)
- Necrosis (3)
- 4 or more mitoses (3)
- Anaplasia (4)
- Grade:
- Low grade (0 - 4)
- Intermediate grade (5 - 6)
- High grade (7 or more)
- Criteria:
- Brandwein et al. grading scheme (quantitative) (Am J Surg Pathol 2001;25:835)
- Criteria:
- Intracystic component less than 25% (2)
- Tumor front invades in small nests and islands (2)
- Pronounced nuclear atypia (2)
- Lymphovascular invasion (3)
- Bony invasion (3)
- 4 or more mitoses (3)
- Perineural invasion (3)
- Necrosis (3)
- Grade:
- Low grade (0)
- Intermediate grade (2 - 3)
- High grade (4 or more)
- Criteria:
- Modified Healy grading system (qualitative)
- Low grade
- Macro and microcysts
- Rare intermediate cells
- Rare mitotic figures
- Absent or minimal nuclear pleomorphism
- Well circumscribed tumor with broad edges
- Extravasated mucin and fibrotic stroma present
- Intermediate grade
- Microcysts and solid component
- More intermediate cells
- Few mitotic figures
- Slight nuclear pleomorphism
- Uncircumscribed tumor
- Fibrotic stroma separating tumor nests
- High grade
- Predominantly solid, with or without microcysts
- Perineural invasion present
- Lymphovascular invasion present
- Surrounding soft tissue invasion present
- Many mitotic figures
- Nuclear pleomorphism, including presence of prominent nucleoli
- Predominance of intermediate cells
- Desmoplastic stoma
- Low grade
- Memorial Sloan Kettering Cancer Center (MSKCC) grading system (qualitative)
- Low grade
- Predominantly cystic growth pattern (> 80%)
- 0 - 1 mitotic figures/10 high power fields (HPF)
- Well circumscribed
- No necrosis
- Intermediate grade
- Predominantly solid growth pattern
- 2 - 3 mitotic figures/10 high power fields (HPF)
- Well circumscribed or infiltrative
- No necrosis
- High grade
- Any growth pattern but usually solid
- ≥ 4 mitotic figures/10 high power fields (HPF)
- Usually infiltrative
- Necrosis is present
- Low grade
Microscopic (histologic) images
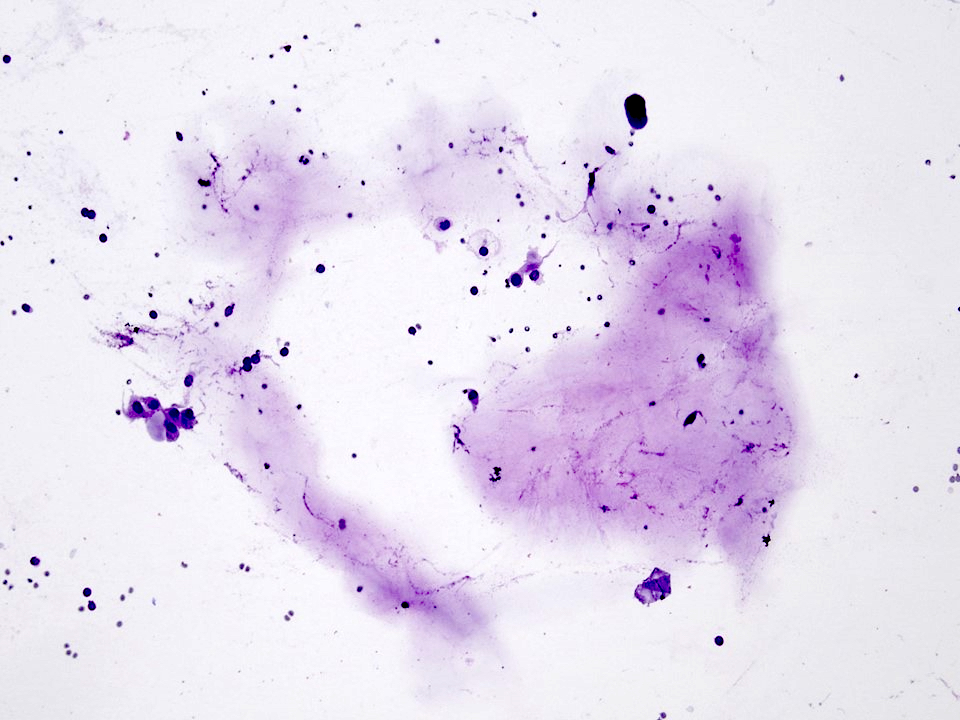
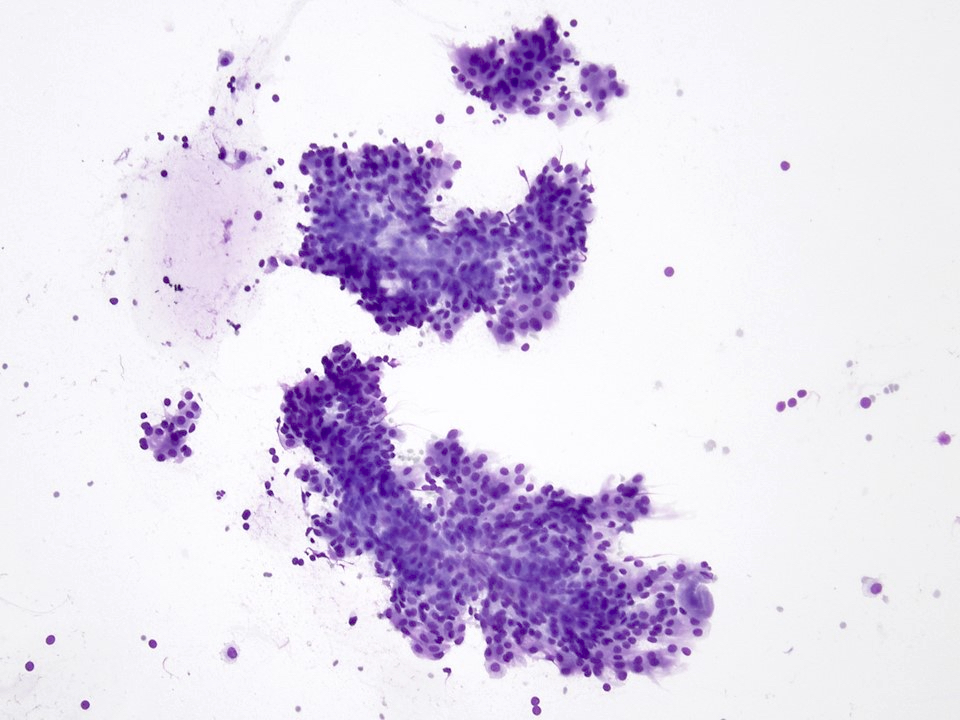
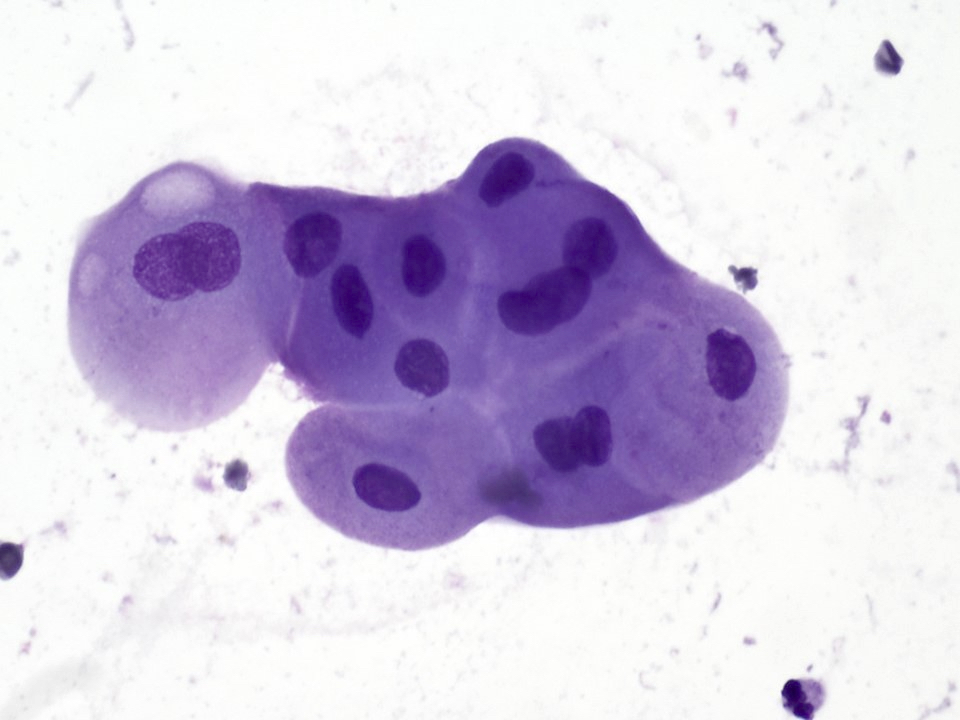
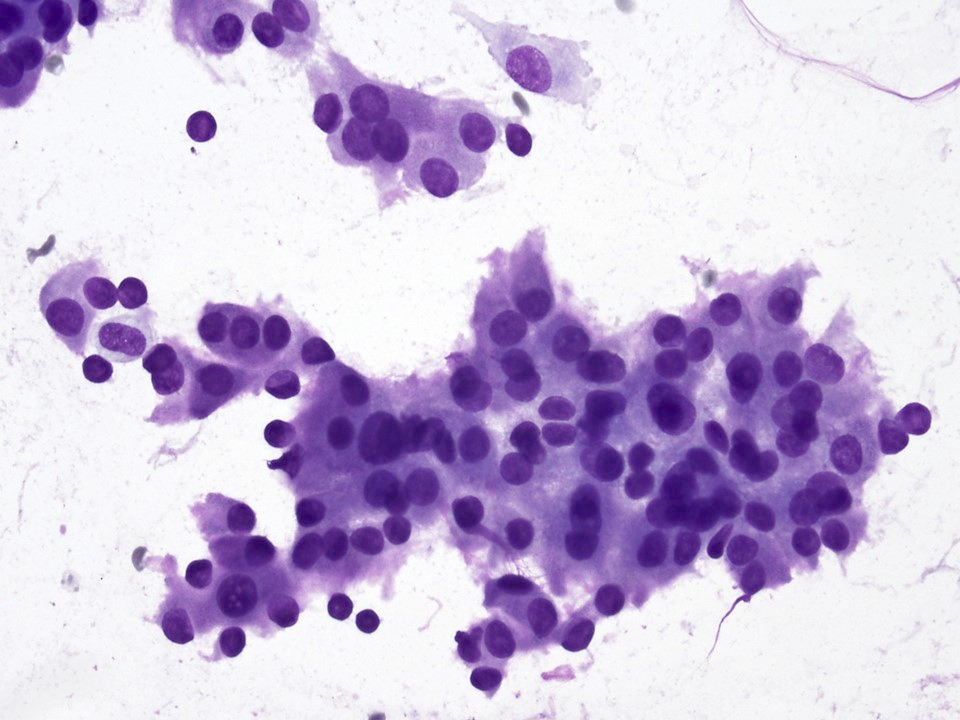
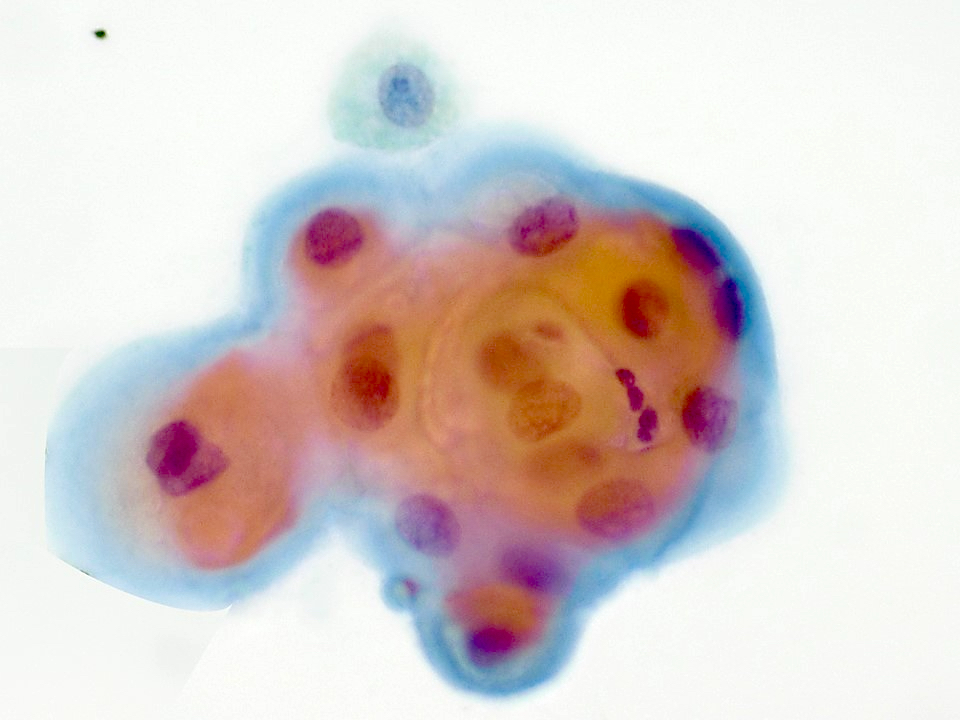
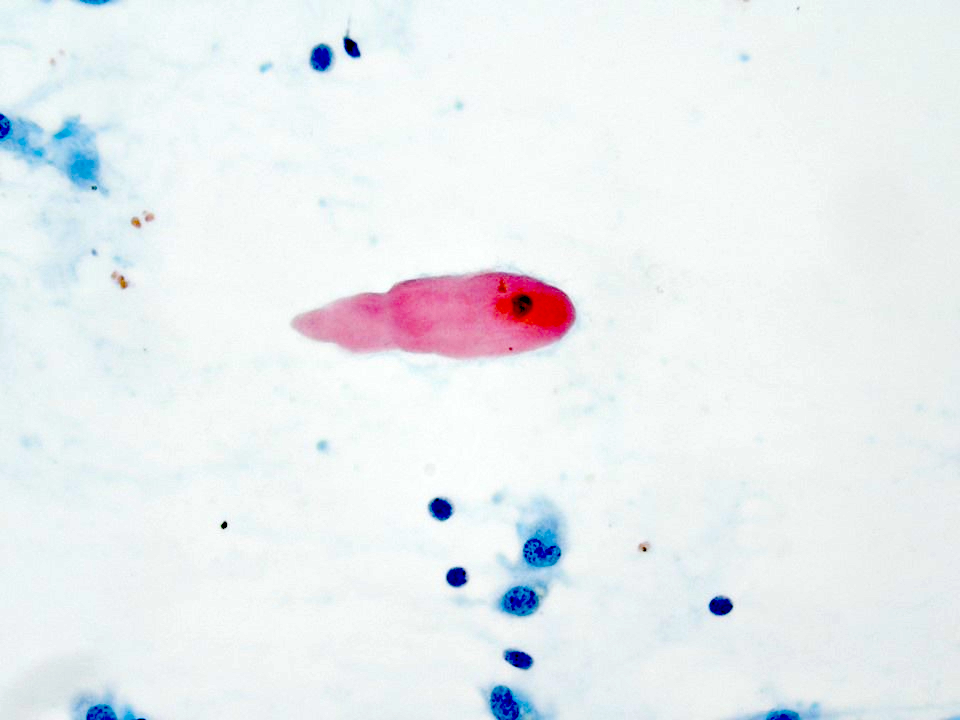
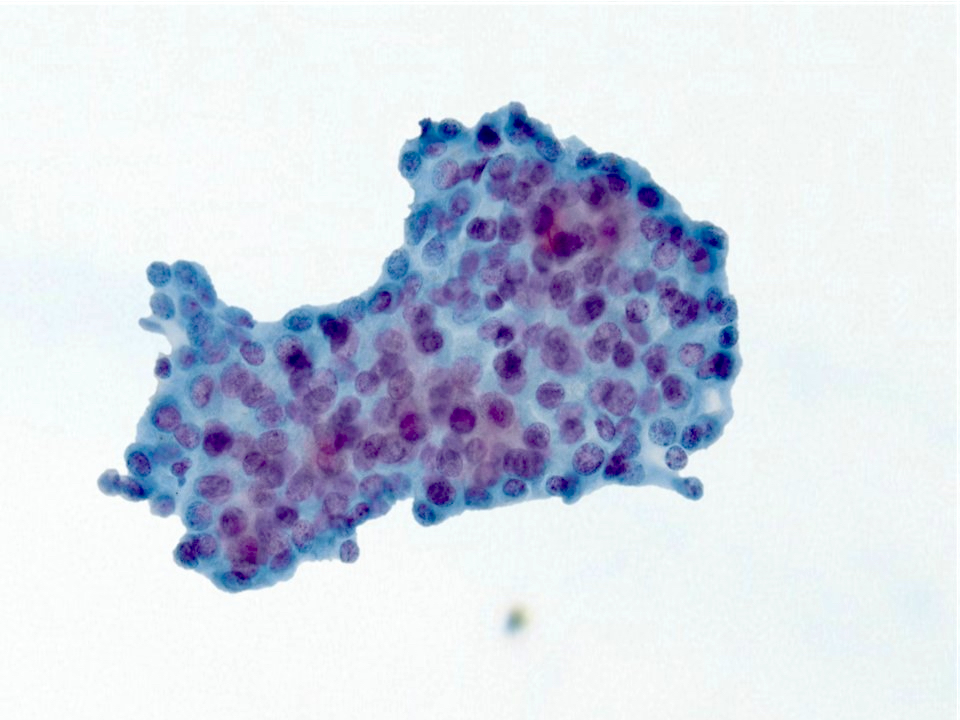
Cytology description
- Most often graded as low grade or high grade on FNA
- Low to intermediate grade:
- Can be acellular or hypocellular smears
- Extracellular mucin may be the prominent feature
- Cystic background
- Aggregates of epidermoid cells, intermediate cells and mucocytes
- Epidermoid cells appear as bland cohesive flat sheets with squamoid / dense cytoplasm and well defined cellular borders
- Predominantly mucus cells floating in extracellular mucin (low grade)
- No keratinization seen
- Lympocytes present in about 20% of cases and are abundant
- High grade:
- Highly cellular aspirates
- High grade nuclear features with pleomorphic nuclei, prominent nucleoli
- Intermediate cells and mucous cells are rare
- Increased mitosis
- Necrotic background
- References: J Clin Diagn Res 2017;11:ER04, Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 5th Edition, 2020
Cytology images
Positive stains
- Pancytokeratin, CK5/6, p63, p40, EMA, CK7, CK14
- Membrane bound mucins: MUC1, MUC2, MUC4, MUC5AC and MUC5B
- Mucocytes: mucin positive for mucicarmine and PASD (diastase resistant) stains
- Reference: J Stomatol Oral Maxillofac Surg 2020;121:713
Negative stains
- S100, GFAP, calponin, muscle specific actin, androgen receptor, HER2, DOG1, CK20 (Arch Pathol Lab Med 2015;139:55)
- SOX10: rare cases may be positive (Hum Pathol 2016;56:134)
- Mammaglobin: some cases may show positive cells (Hum Pathol 2016;56:134)
- GATA3: occasional cells may be positive (Hum Pathol 2016;56:134)
Electron microscopy description
- Epidermoid cells attached to each other with desmosomes and mucus cells showing mucous globules with stellate mucoid material (Oral Surg Oral Med Oral Pathol 1979;47:247)
Molecular / cytogenetics description
- t(11;19)(q14-21;p12-13) with CRTC1(MECT1)-MAML2 fusion (Nat Genet 2003;33:208)
- Present in 80% of mucoepidermoid carcinoma (Am J Surg Pathol 2016;40:1151)
- Low to intermediate grade (78%), high grade (84%) (Am J Surg Pathol 2016;40:1151)
- Detected by fluorescence in situ hybridization (FISH) or RT-PCR (Am J Surg Pathol 2019;43:885)
Sample pathology report
- Parotid gland, right, parotidectomy:
- Mucoepidermoid carcinoma, intermediate grade (2.3 cm)
- The tumor is confined to the parotid gland.
- No lymphovascular or perineural invasion is identified.
- Three lymph nodes, negative for carcinoma (0/3).
- Surgical margins negative for carcinoma.
- Carcinoma 0.3 cm of closest margin, medial.
- See synoptic report.
Differential diagnosis
- For low to intermediate grade tumors:
- Necrotizing sialometaplasia (Acta Otorrinolaringol Esp 2020;71:328):
- Lobular pattern, lacks cystic pattern, no intermediate cells
- Pleomorphic adenoma with squamous and mucinous cell metaplasia (J Oral Maxillofac Pathol 2018;22:S69):
- Composed of epithelial and myoepithelial cells and extracellular matrix material
- Warthin tumor with squamous metaplasia (J Med Case Rep 2019;13:12):
- Lacks the translocations seen in mucoepidermoid carcinoma
- Shows bilayered oncocytic epithelium
- Acinic cell carcinoma (Eur Arch Otorhinolaryngol 2016;273:3511):
- Mammary analogue secretory carcinoma (MASC) (Bosn J Basic Med Sci 2016;16:237):
- S100 positive
- Necrotizing sialometaplasia (Acta Otorrinolaringol Esp 2020;71:328):
- For high grade tumors:
- Squamous cell carcinoma (primary or secondary) (J Cancer Res Ther 2015;11:664):
- Shows keratinization and intercellular bridges
- Lacks intermediate cells and mucocytes
- Salivary duct carcinoma (Head Neck Pathol 2017;11:288):
- GATA3, HER2 and androgen receptor positive
- Shows a Roman bridge pattern, comedonecrosis
- Squamous cell carcinoma (primary or secondary) (J Cancer Res Ther 2015;11:664):
Additional references
Practice question #1
Which of the following is true about mucoepidermoid carcinoma?
- Associated with t(12;15)(p12;q25) and ETV6-NTRK3 gene fusion
- Highly associated with smoking
- Most common malignant salivary tumor in children
- Positive for HER2 and AR by immunohistochemistry
- Prognosis is poor regardlesss of histologic grade
Practice answer #1
C. Most common malignant salivary tumor in children
Comment Here
Reference: Mucoepidermoid carcinoma
Comment Here
Reference: Mucoepidermoid carcinoma
Practice question #2
Which of the following histologic features is more commonly seen in low to intermediate grade mucoepidermoid carcinoma?
- 4 or more mitoses
- Bone invasion
- Intracystic component more than 30%
- Necrosis
- Perineural invasion
Practice answer #2
Practice question #3
Practice answer #3