Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Magliocca K. Radicular (periapical) cyst. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillaperiapicalcyst.html. Accessed October 1st, 2025.
Definition / general
- Inflammatory type odontogenic cyst associated with the root of a nonviable (necrotic) tooth (PLoS One 2022;17:e0277387)
- Lined by nonkeratinized stratified squamous epithelium, derived from rests of Malassez
Essential features
- Located in the maxilla or mandible (Head Neck Pathol 2022;16:63)
- Must involve the root of a nonviable (necrotic) tooth
- Cystic strips of nondysplastic (para)keratinizing squamous epithelium
- Background stromal inflammation
Terminology
- Generally synonymous terms: radicular cyst, apical cyst, periapical cyst
- Radicular cyst: present in association with any portion of the tooth root
- Periapical cyst: present at the tooth root apex
- Lateral radicular cyst: present at the opening of lateral accessory root canals
- Residual cyst: radicular (periapical) cyst that persists after extraction of offending tooth (PLoS One 2020;15:e0244250)
- Dental implant associated cyst: likely best viewed as a subtype of residual cyst (PLoS One 2022;17:e0277387)
ICD coding
- ICD-11: DA09.8 - radicular cyst
Epidemiology
- Most common jaw cyst (PLoS One 2022;17:e0277387)
- Accounts for ~60% of all odontogenic cysts
- Most common in fourth and fifth decades but occurs over a wide age range
Sites
- Radicular cyst is associated with the root of a nonviable (necrotic) tooth within the maxilla or mandible
- Most common location: anterior maxilla
- Second most common location: posterior mandible (J Oral Pathol Med 2006;35:500, Head Neck 2012;34:852)
Pathophysiology
- Inflammation (usually associated with dental caries extending into the dental pulp or trauma) stimulates cells in the rests of Malassez
- Epithelial cells proliferate to form a cystic cavity
- Cystic cavity can enlarge secondary to
- Osmotic pressure
- Secondary infection and inflammation related to foreign material or bacteria
- Ongoing inflammation and proinflammatory cytokines (J Endod 2007;33:908)
Etiology
- Radicular (periapical) cyst is caused by inflammation at the apex of a nonviable (necrotic) tooth root (WHO)
Clinical features
- May be asymptomatic and incidentally discovered on radiographs taken for another purpose
- May have recent or remote history of tooth pain (WHO)
- Symptoms of pain and drainage if secondarily infected
- May be associated with parulis formation
- Reference: J Oral Pathol Med 2006;35:500
Diagnosis
- Lesion is intraosseous within the maxilla or mandible
- Lesion is associated with necrotic tooth root (radiographically or grossly)
- Histopathology is stratified squamous epithelium (nonspecific but in the context of the above parameters is compatible with radicular cyst)
Radiology description
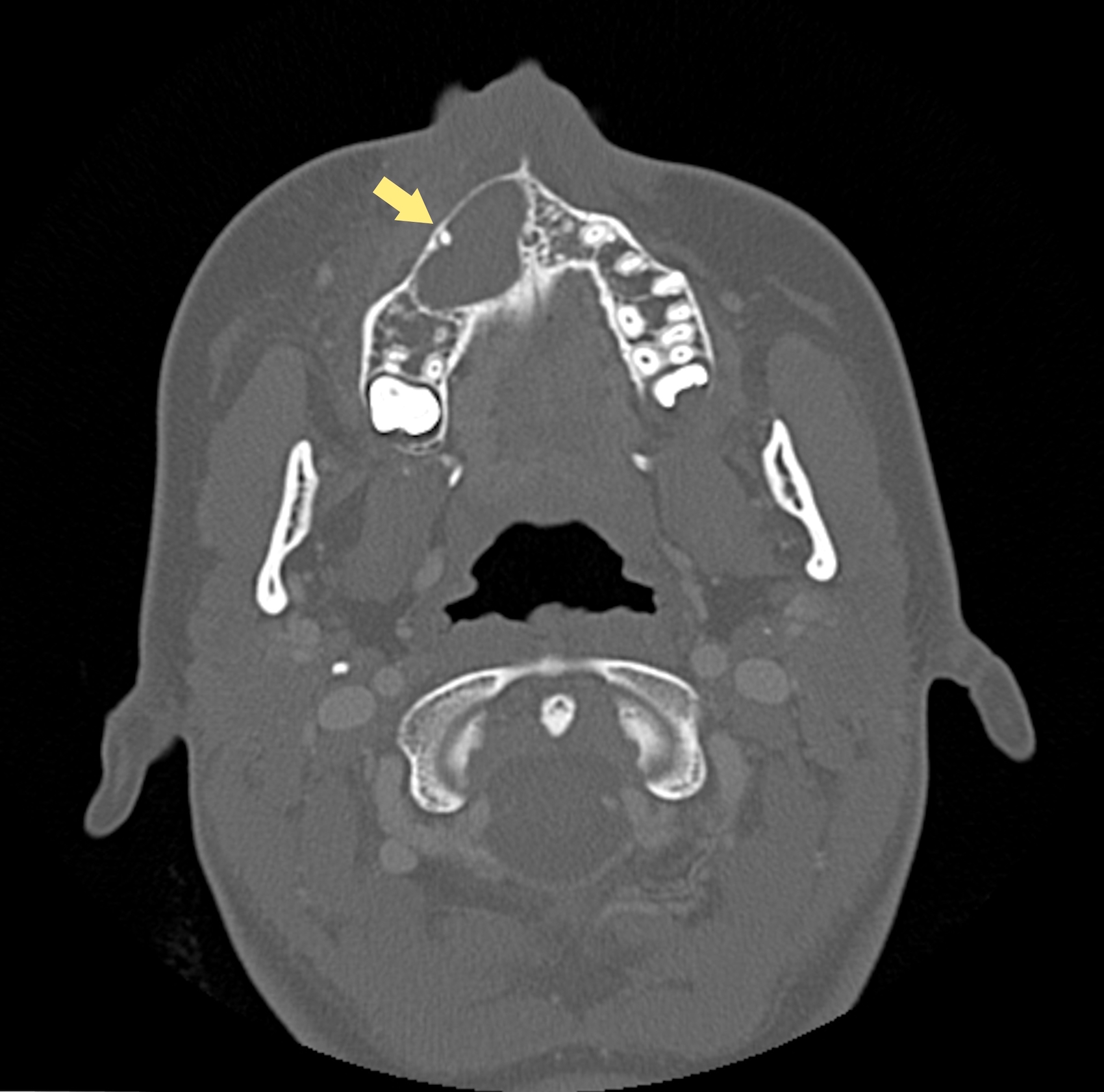
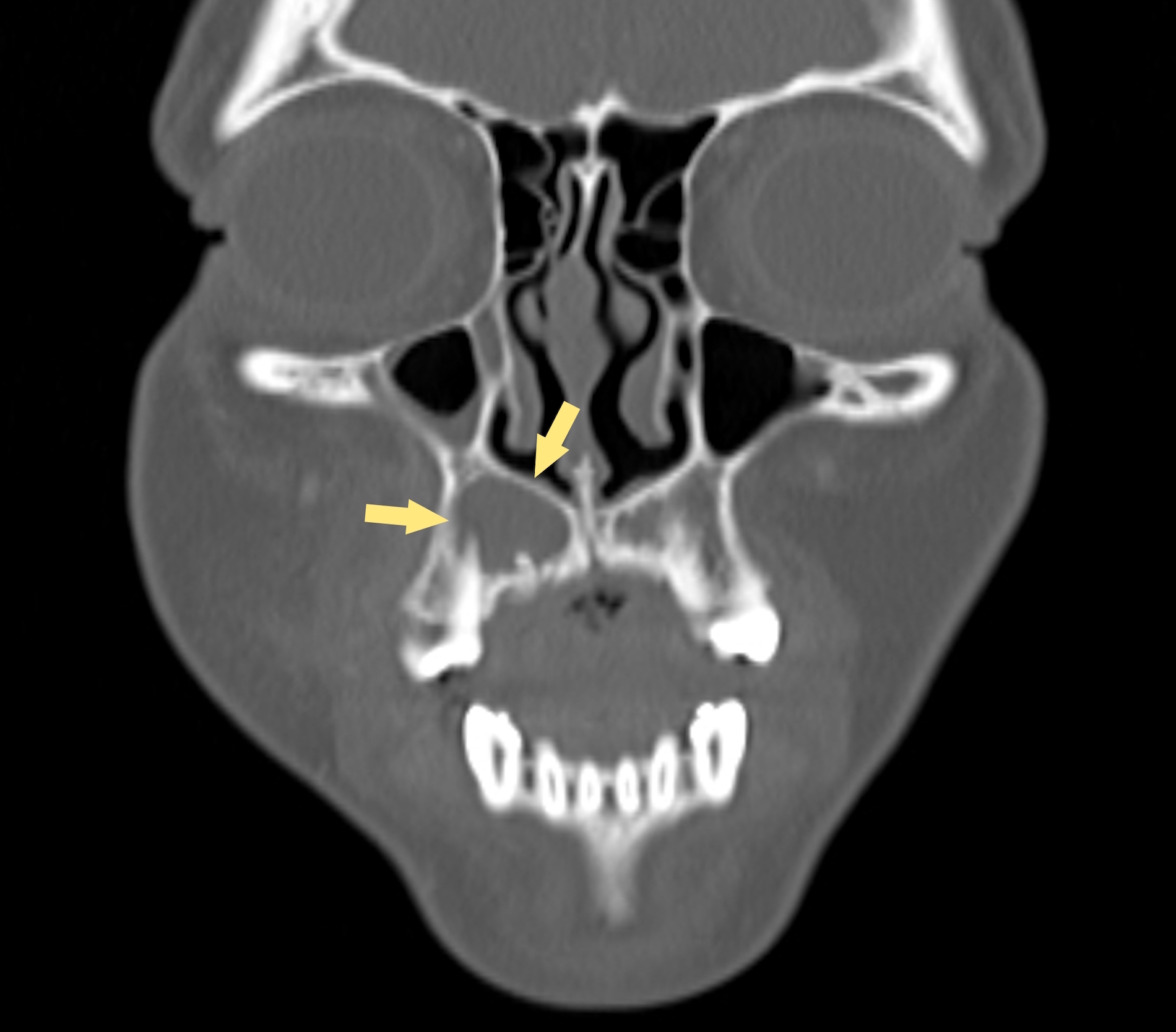
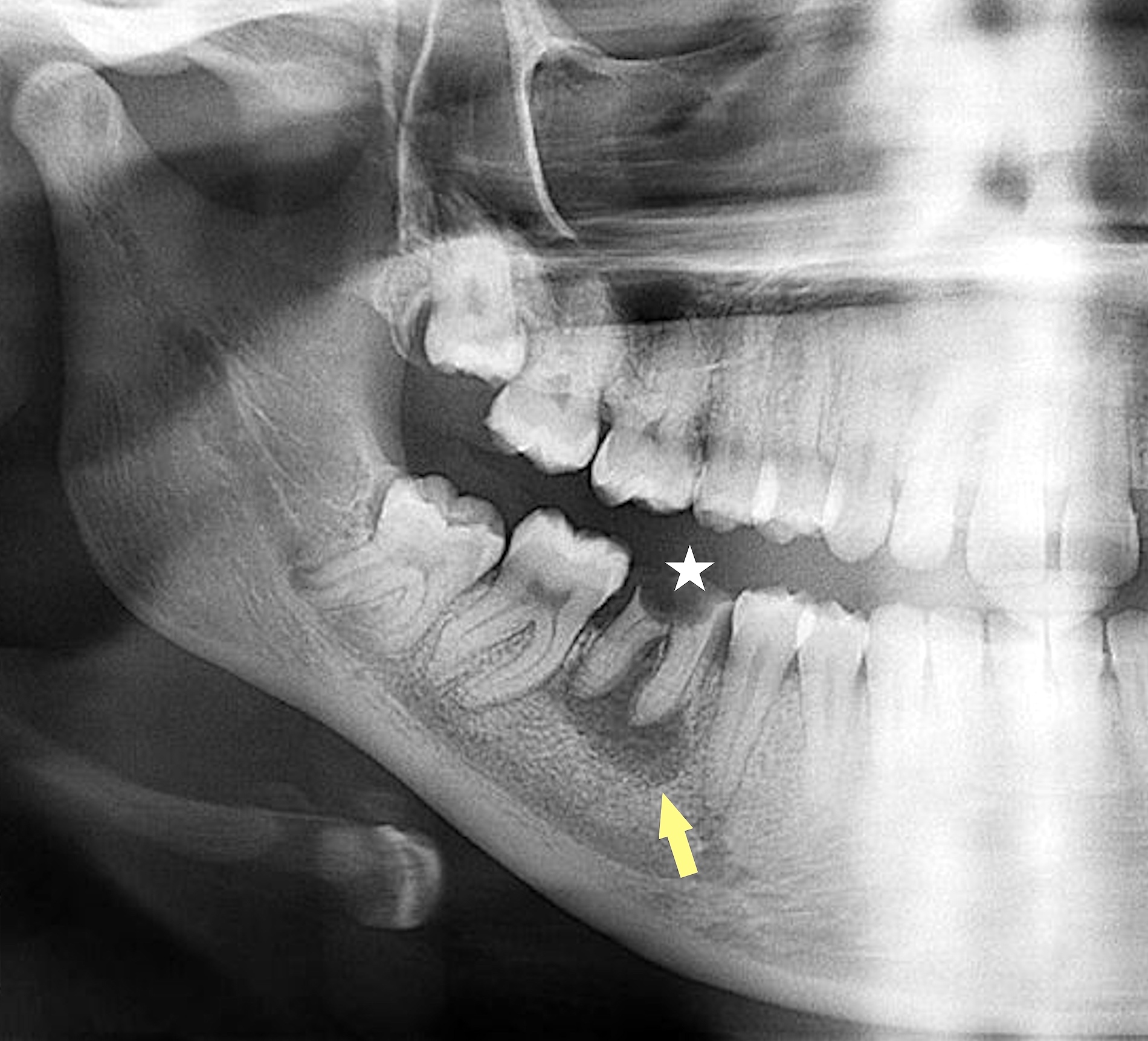
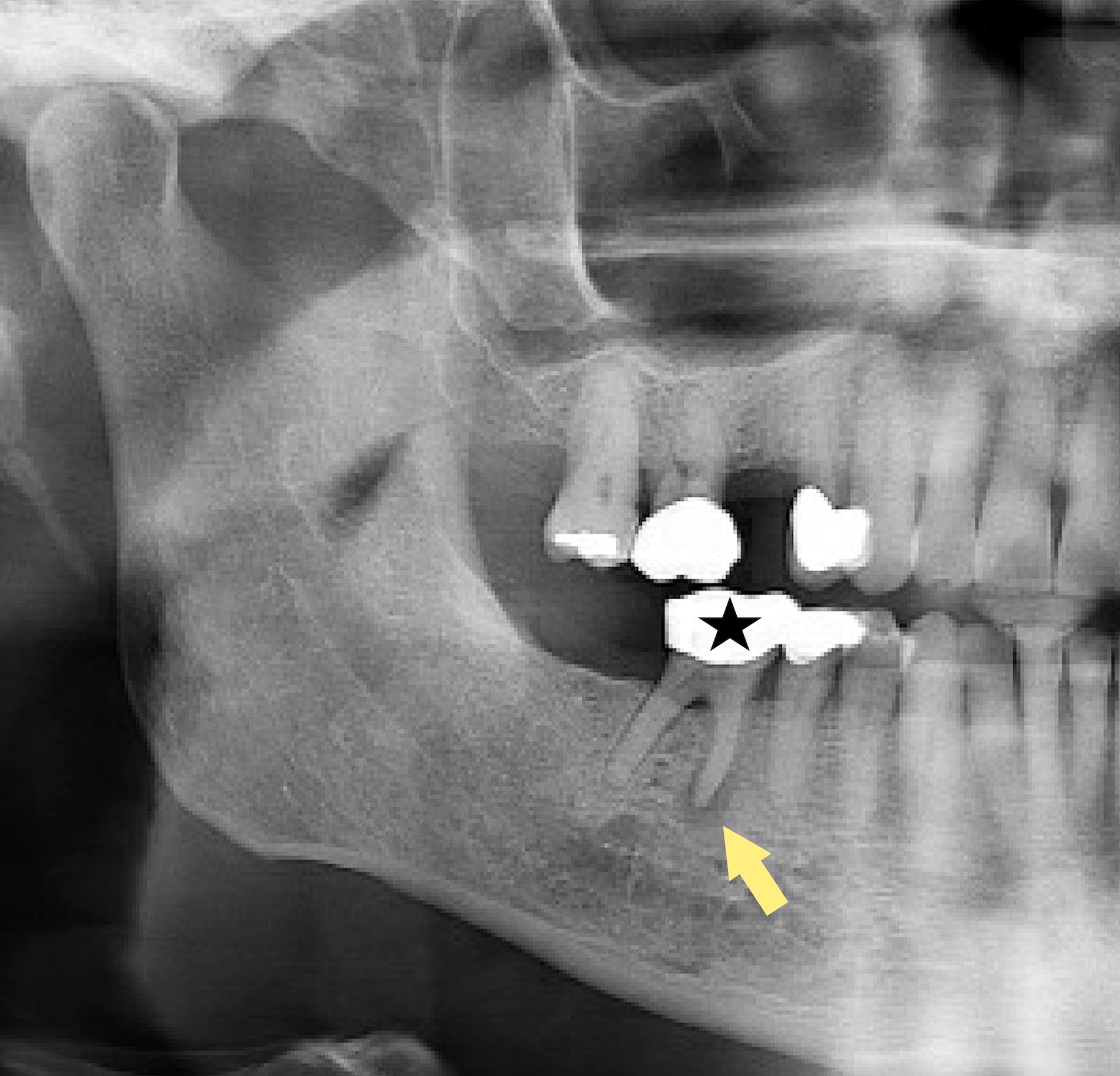
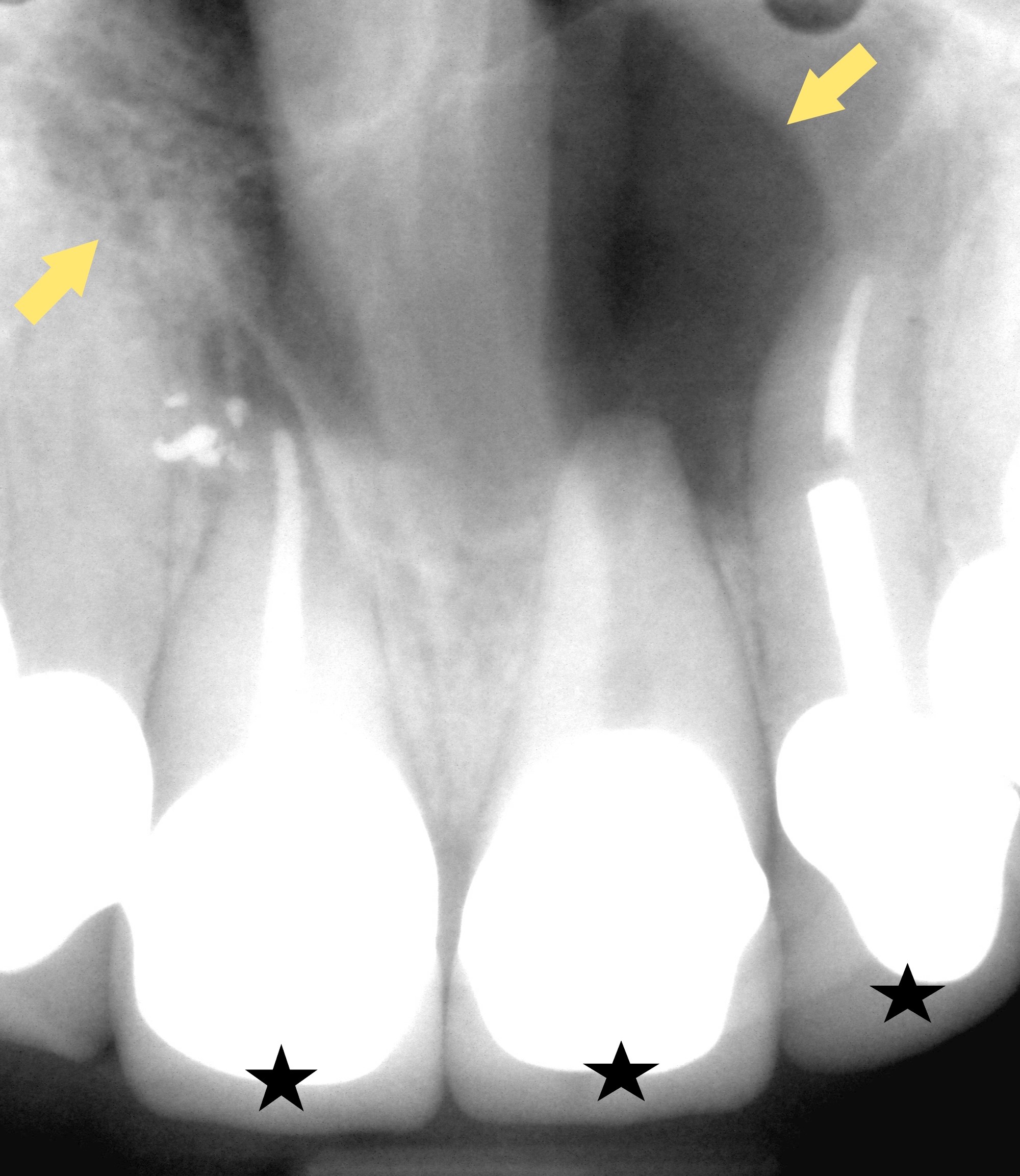
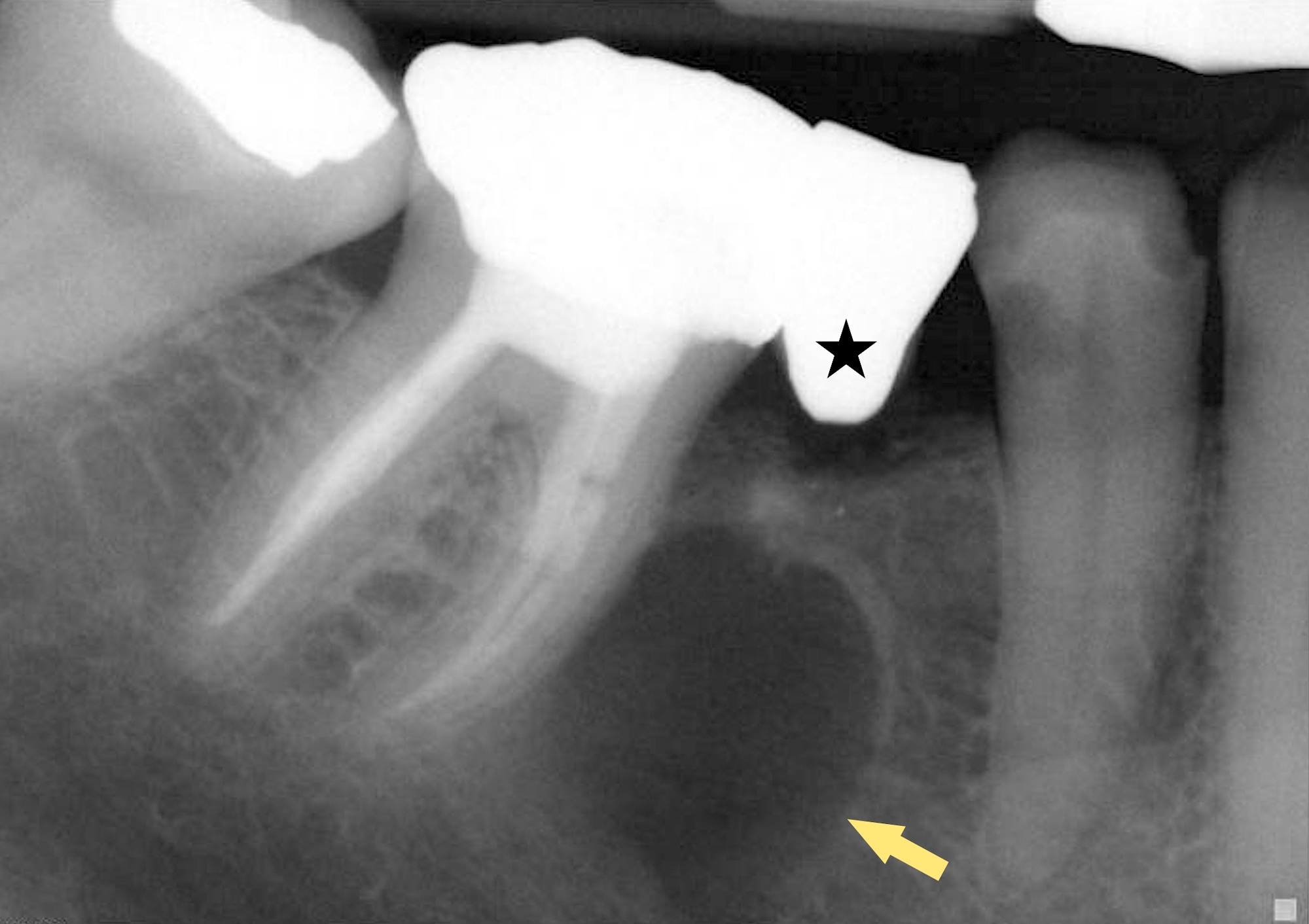
- Panoramic (panorex) radiograph, intraoral film or cross sectional imaging may be useful depending on cyst location, lesion size and the need to evaluate additional parameters (J Clin Med 2023;12:4647)
- Radiology is essential to identify landmarks and the extent of disease in the preoperative and follow up setting
- Round to oval radiolucency associated with the root of a nonviable (necrotic) tooth
- Can resorb or remodel the root of the tooth
Radiology images
Prognostic factors
- Overall prognosis is excellent once lesion is treated
- Recurrence rate low
Case reports
- 19 year old woman with bilateral radicular cysts (J Int Oral Health 2015;7:61)
- 47 year old woman with radicular cyst mimicking a nasopalatine duct cyst (J Endod 2020;46:1155)
- 49 year old woman with persistent pain in the left mandibular angle with limitations in mouth opening (Medicine (Baltimore) 2018;97:e13529)
Treatment
- Varies with age of patient, access to care and state or prognosis of the tooth
- In some patients, necrotic tooth pulp can be treated via root canal with the goal of inducing cyst involution (J Clin Med 2023;12:4647)
- In some patients with very large cysts or cysts that fail to involute after the above treatment, surgical management is likely required to treat the intraosseous cyst (J Clin Med 2023;12:4647)
- Any surgically removed material is submitted for pathologic examination (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:642)
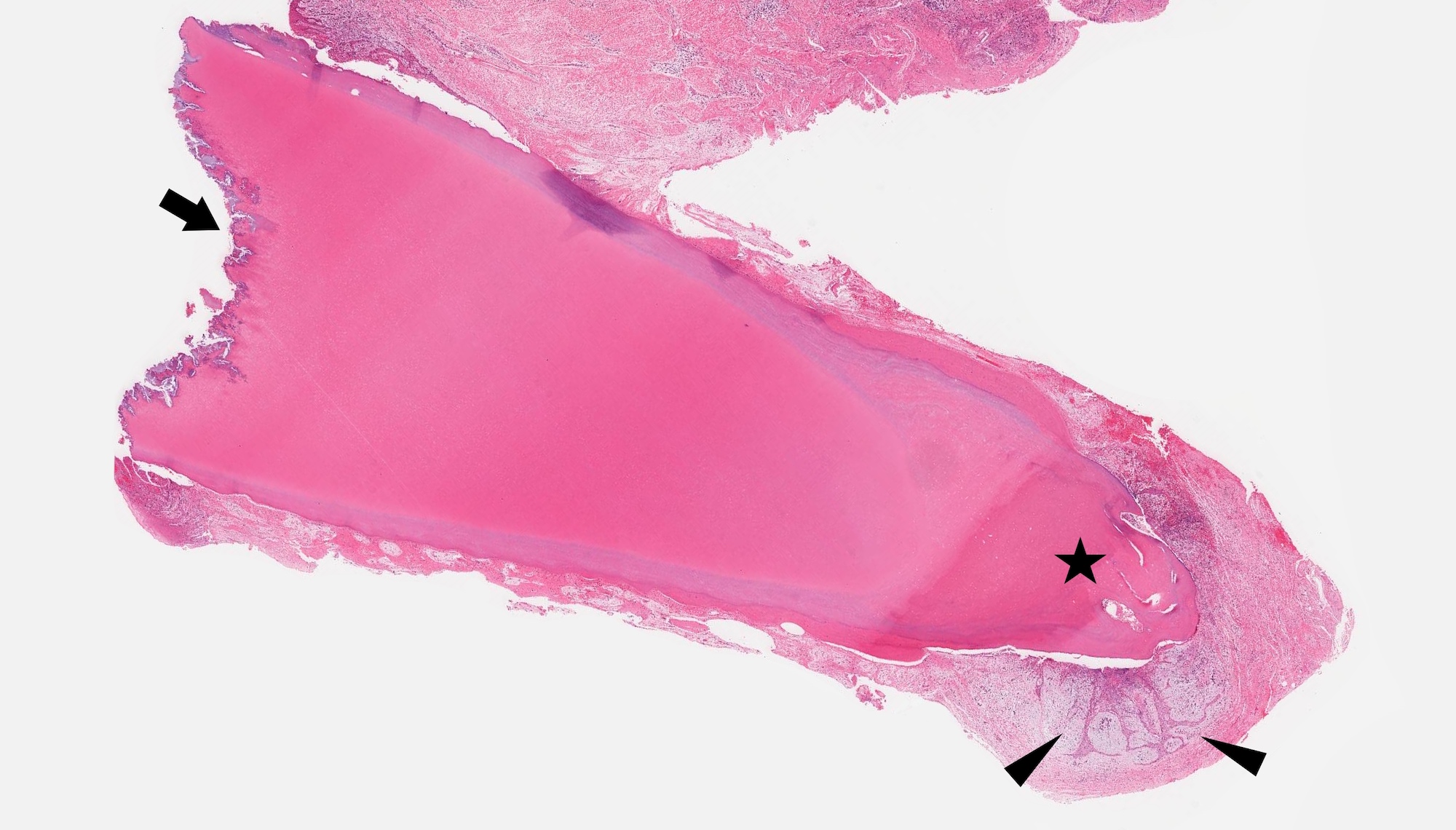
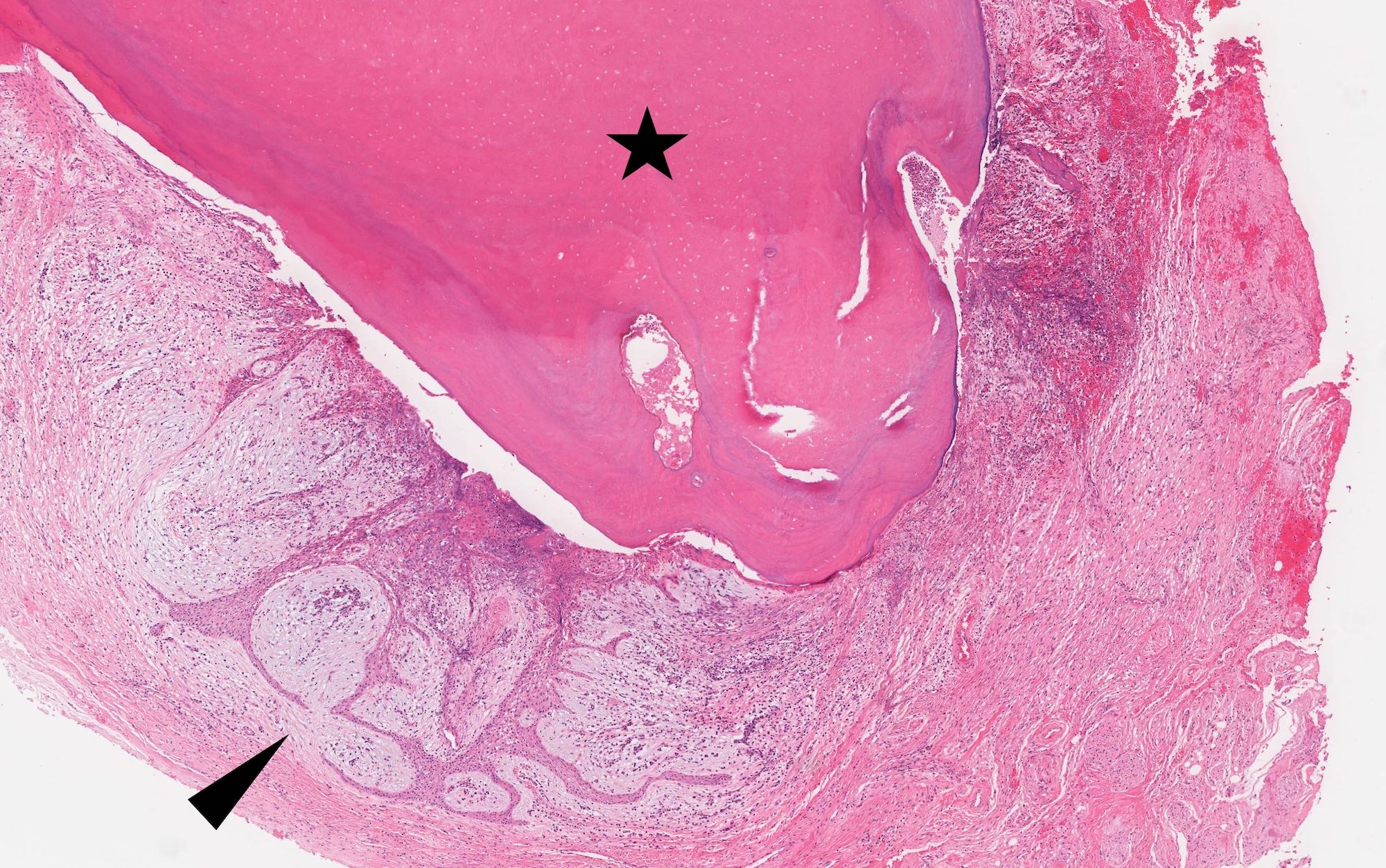
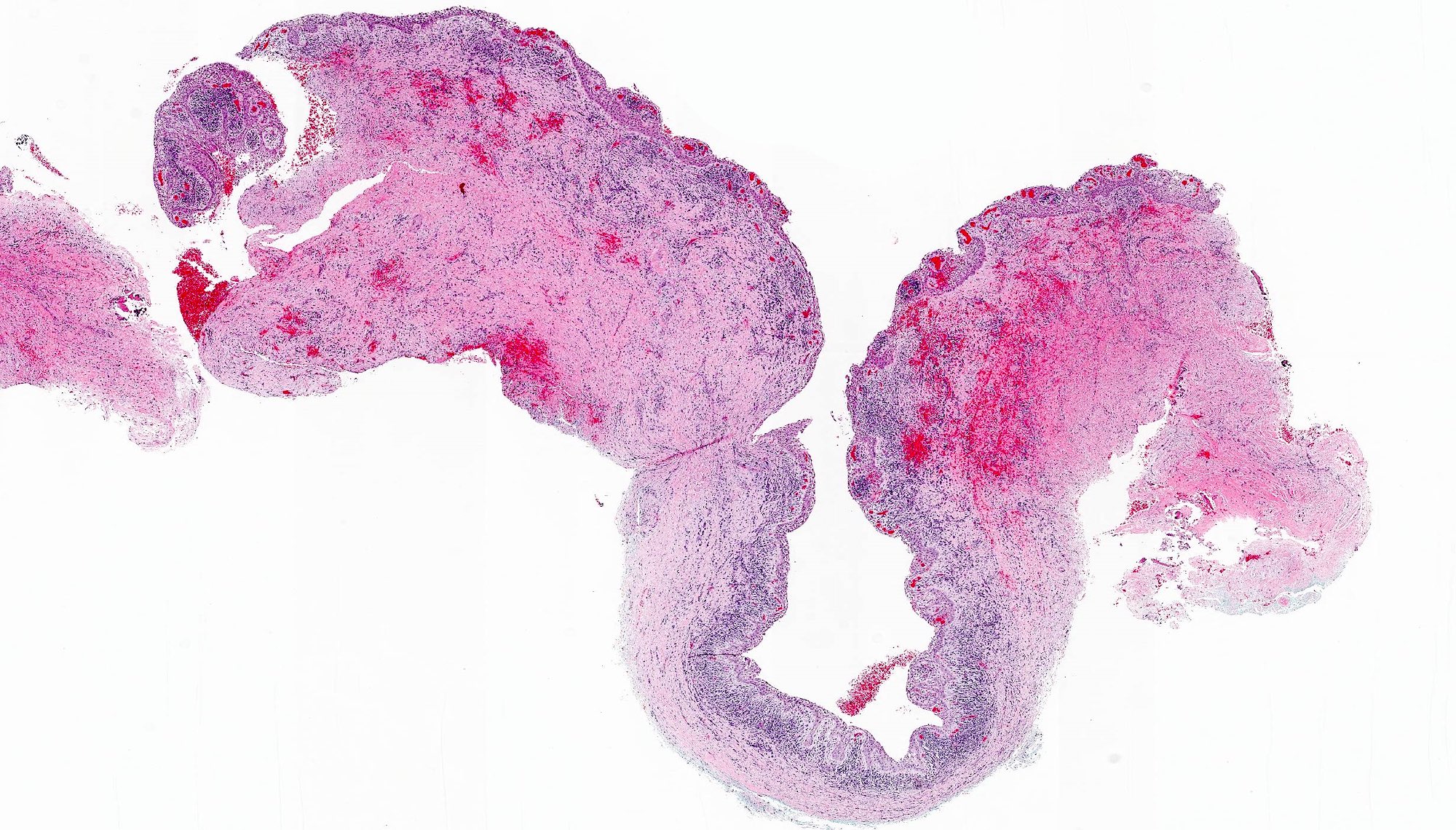
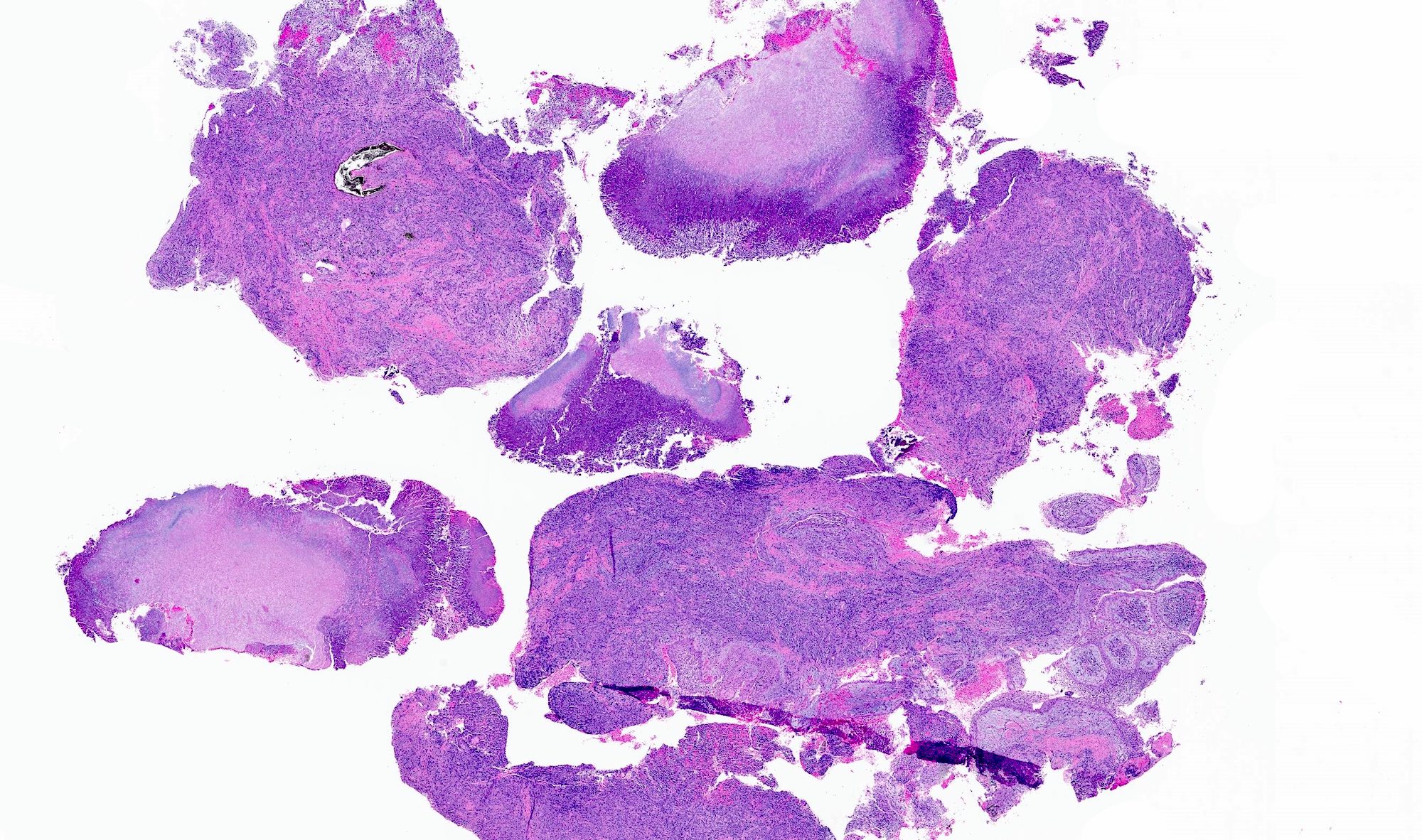
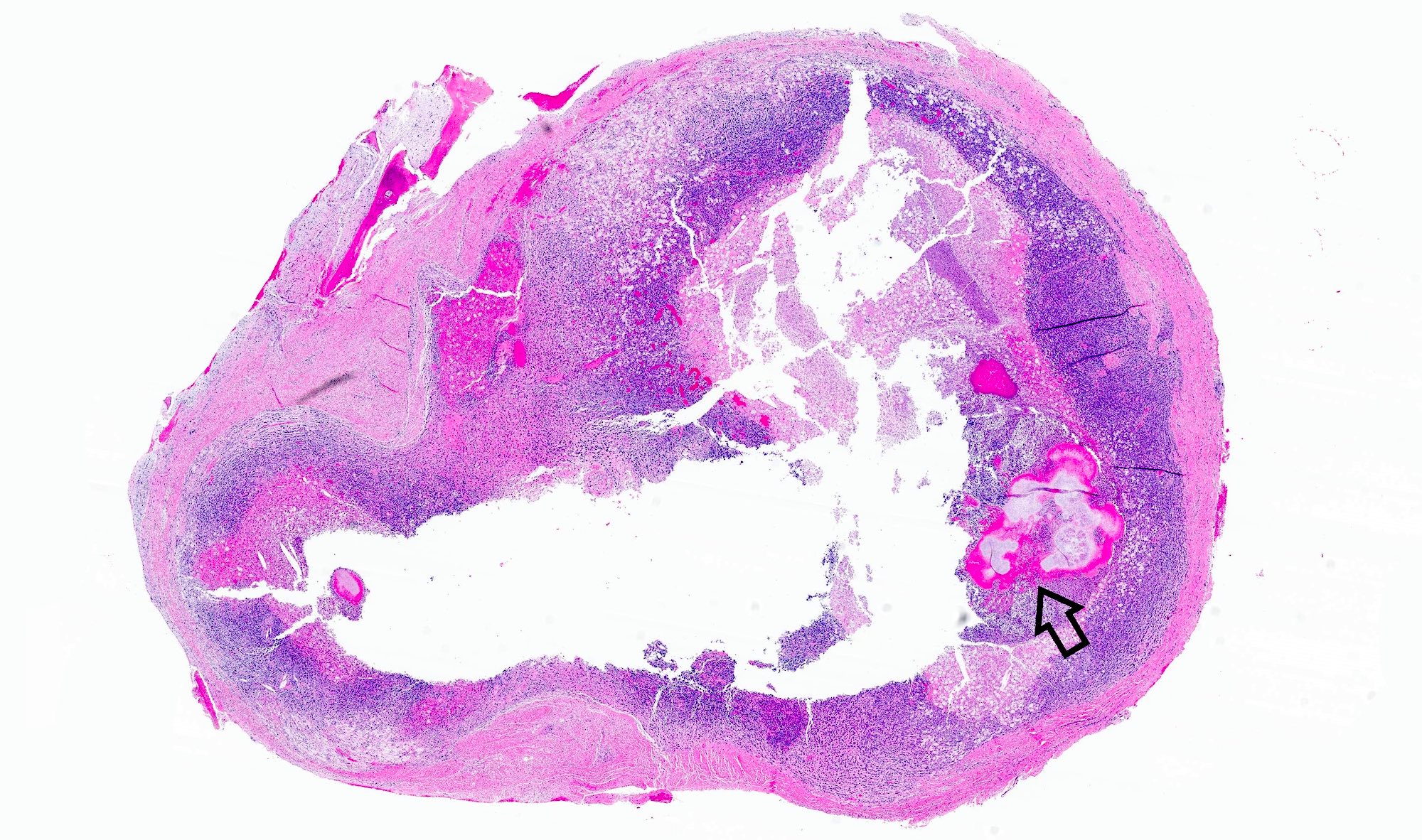
Gross description
- Surgical specimens usually consist of multiple, irregular tissue fragments
- Possible minute bone fragments
- All (nontooth) tissue should be submitted for histologic examination to definitively confirm the diagnosis
- Associated tooth received as specimen can be described grossly and supplemented with photographs where equipment is available
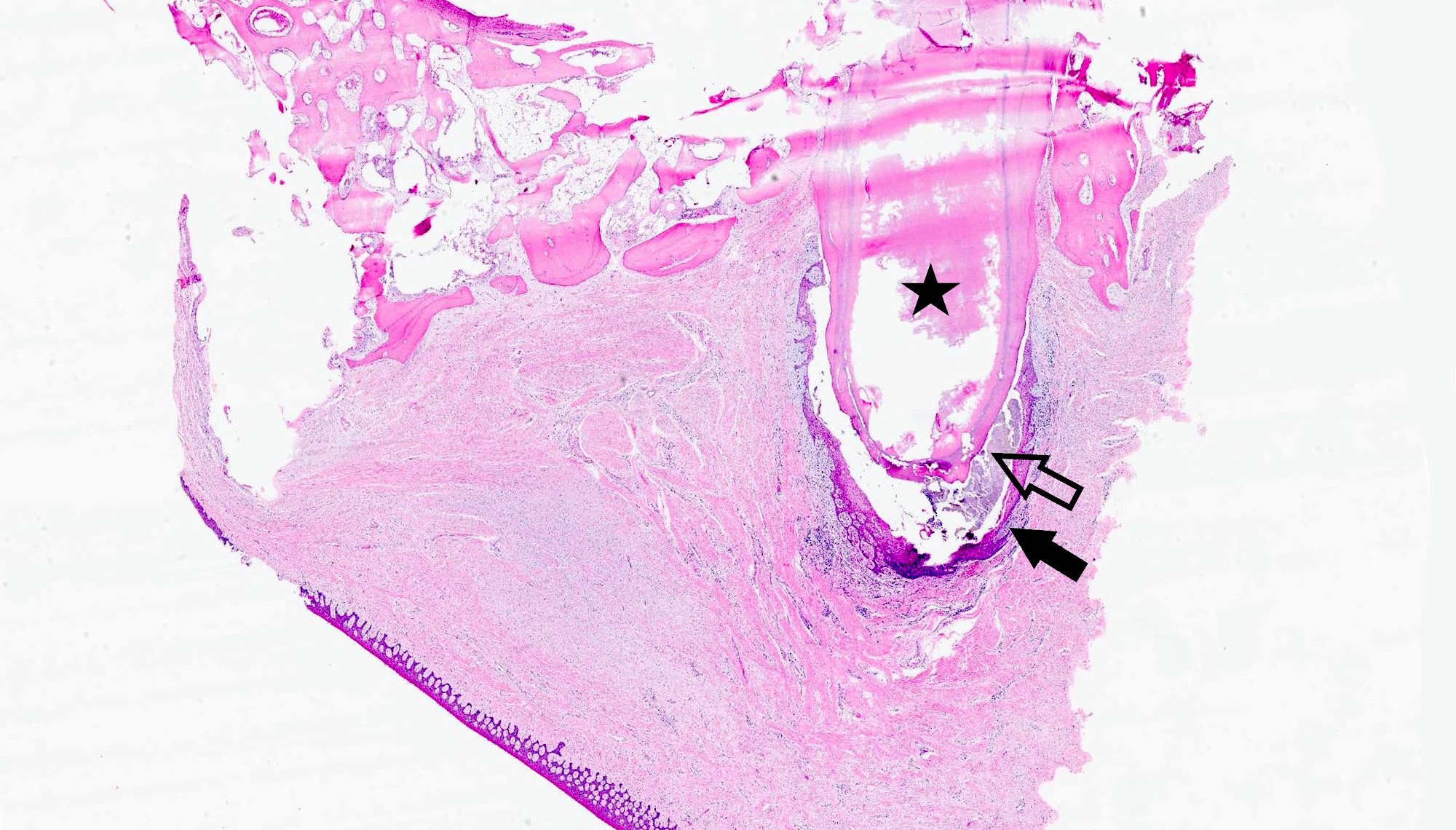
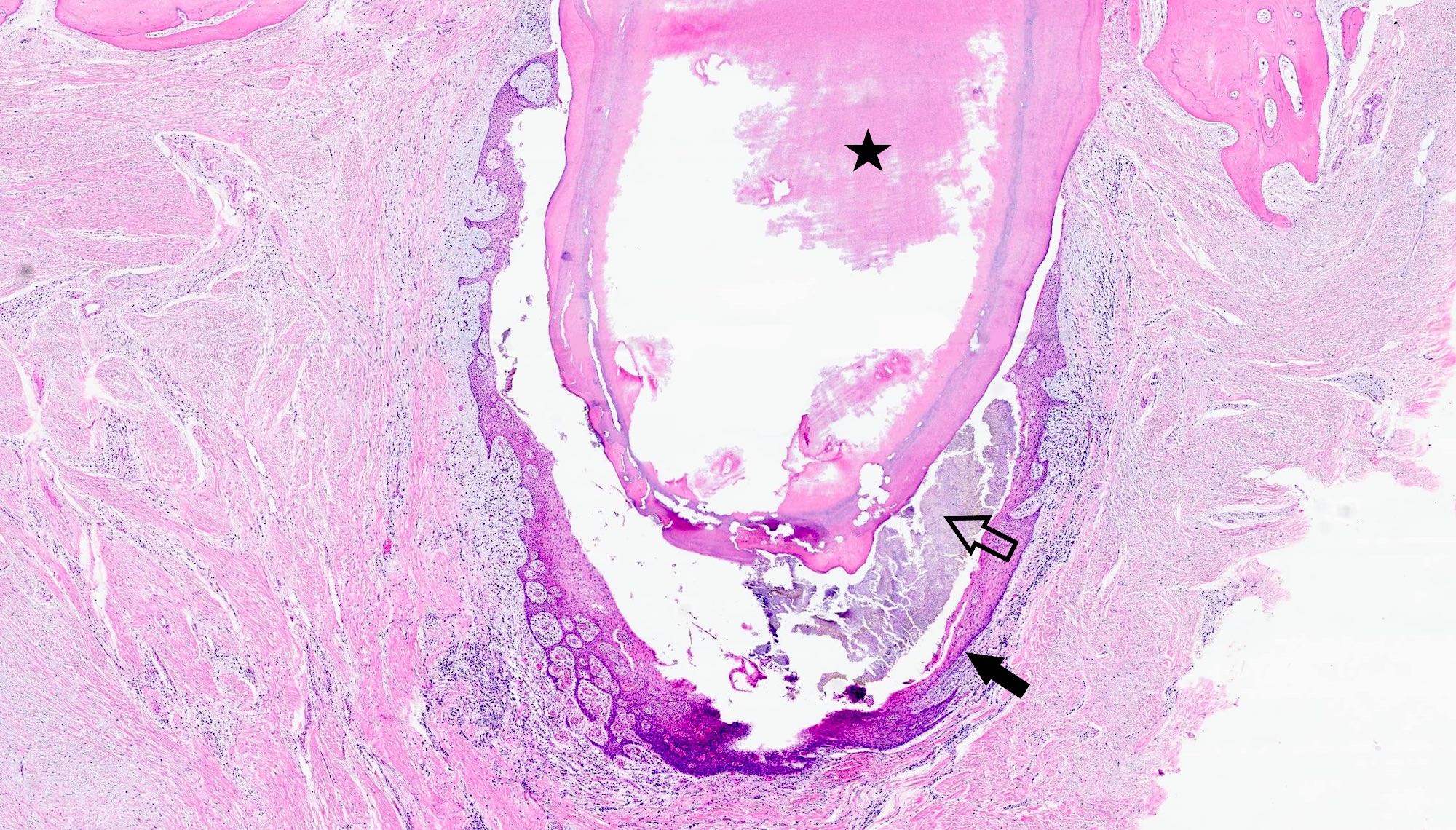
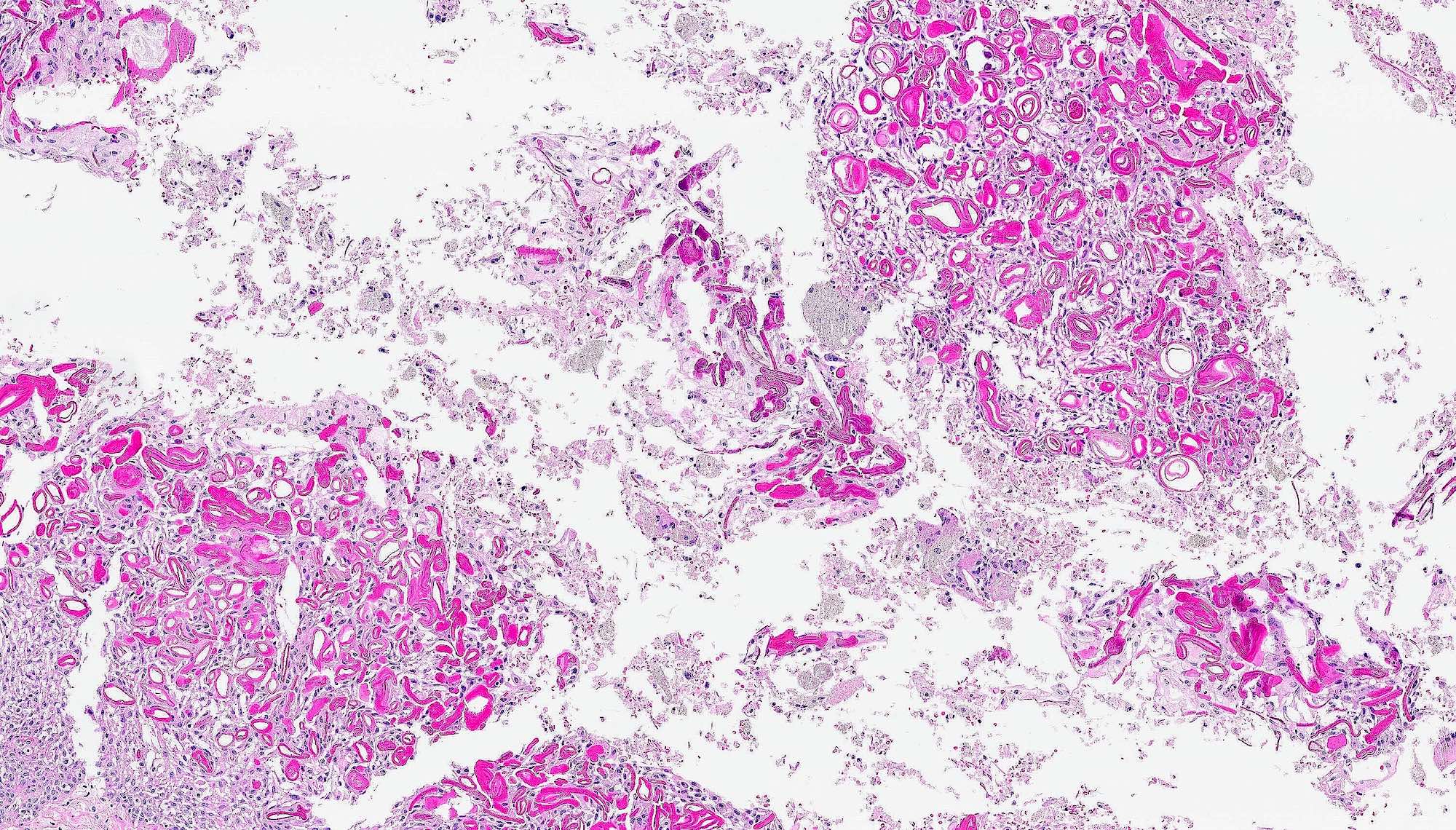
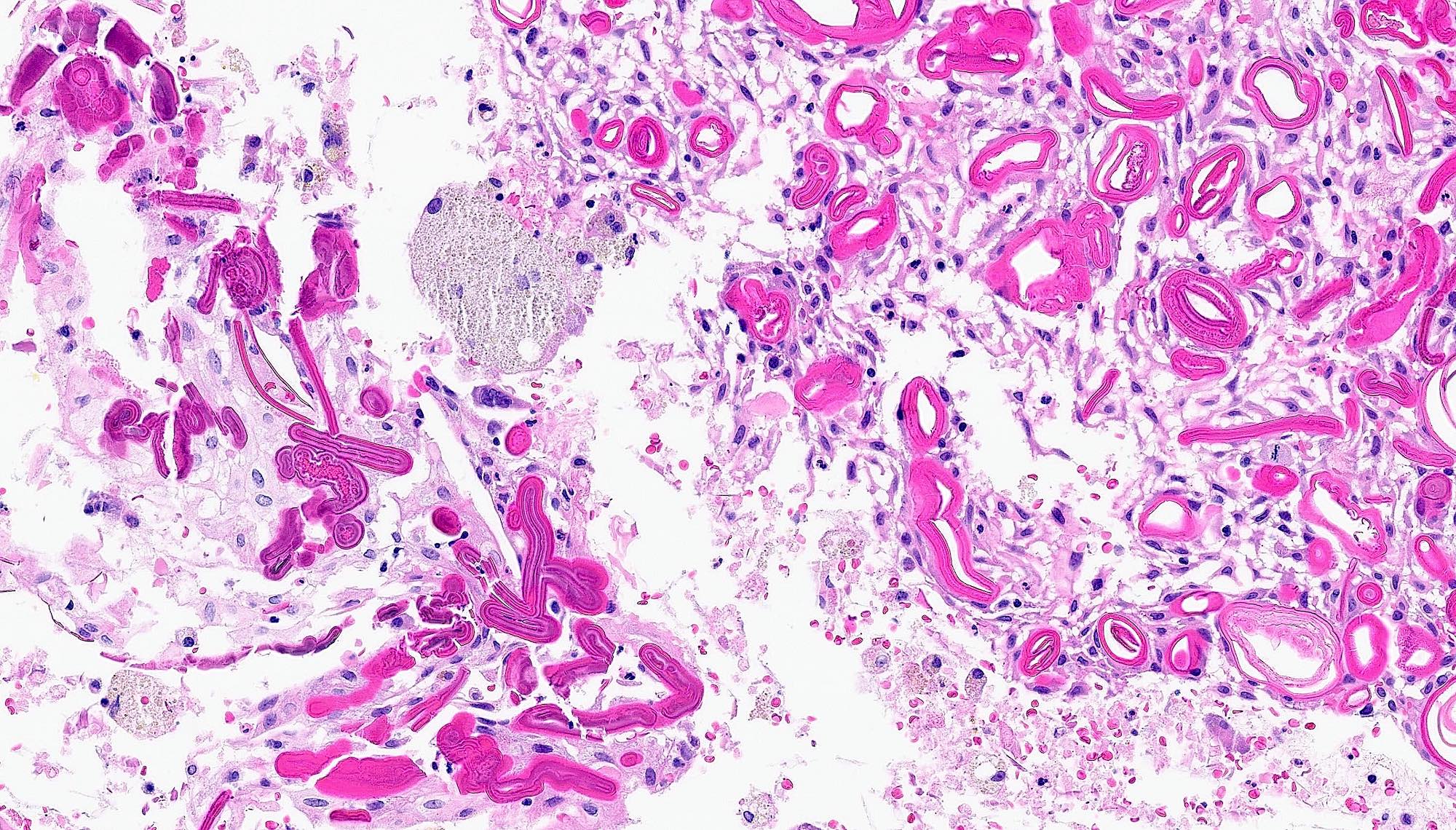
Frozen section description
- Multilayered stratified squamous epithelial lining
- Background fibrous and granulation tissue with acute or chronic inflammation
- Associated mineralized tissues (bone, tooth) may be present but technically difficult to section
- May have associated bacterial colonies present
Frozen section images
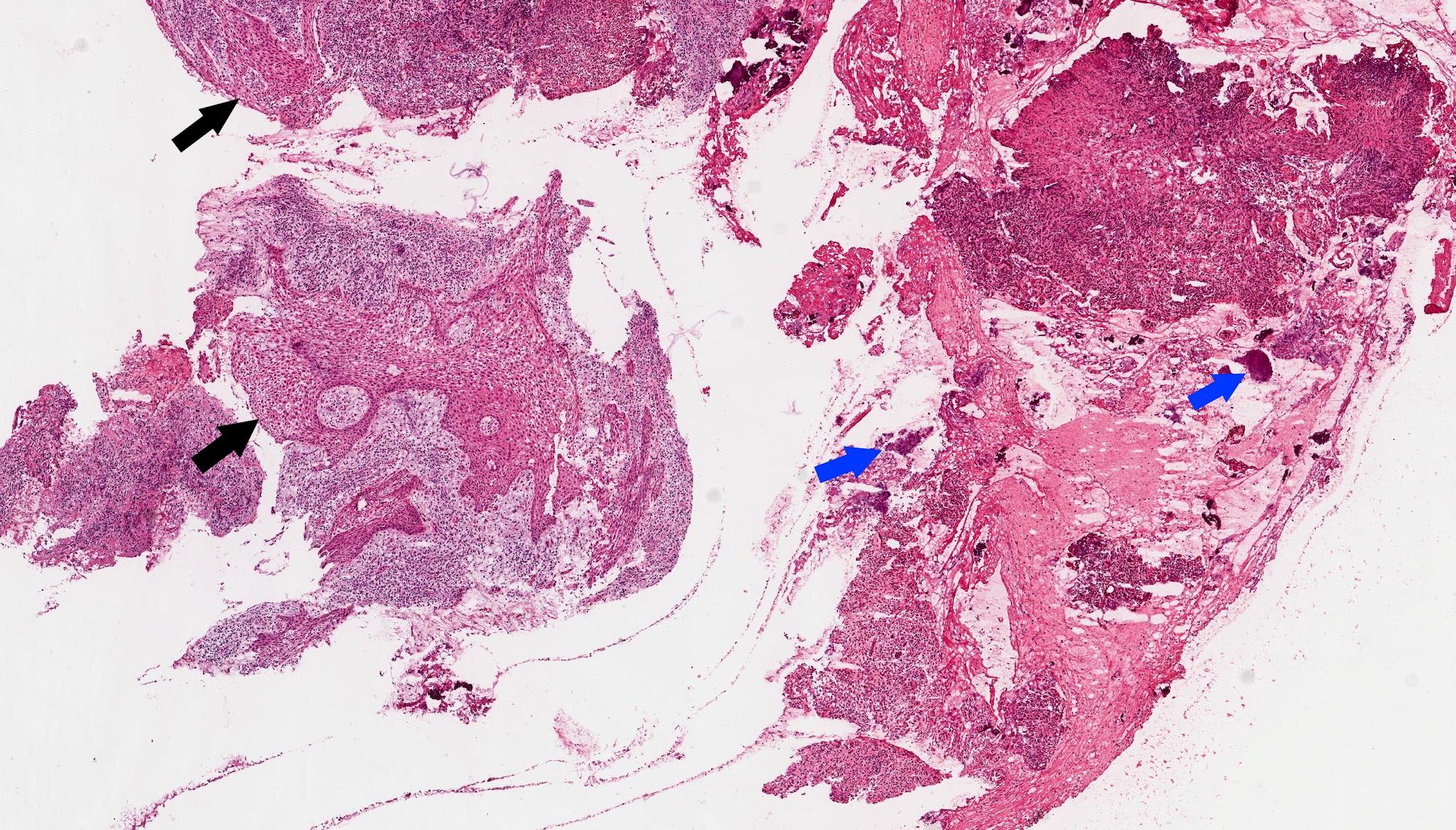
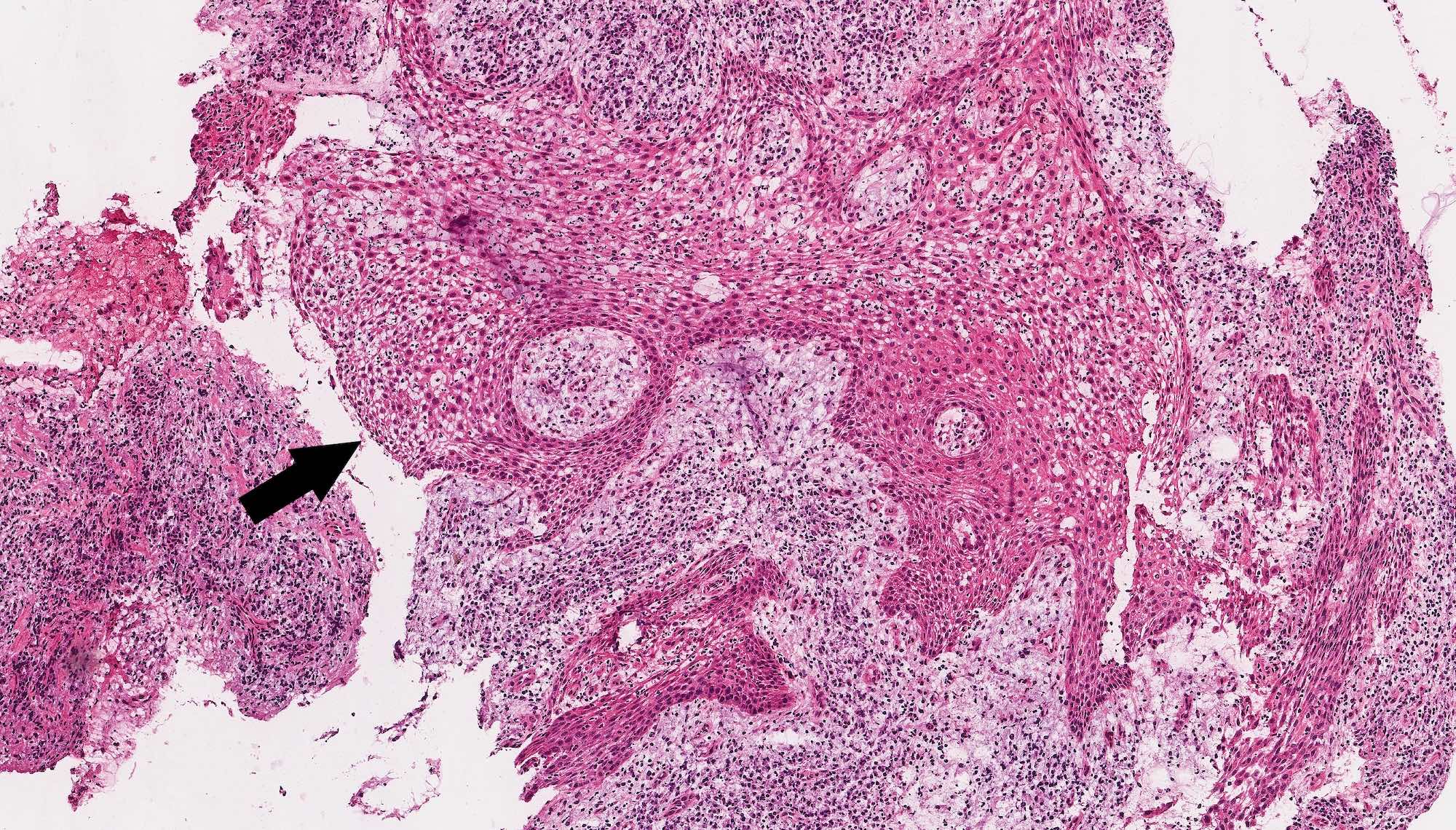
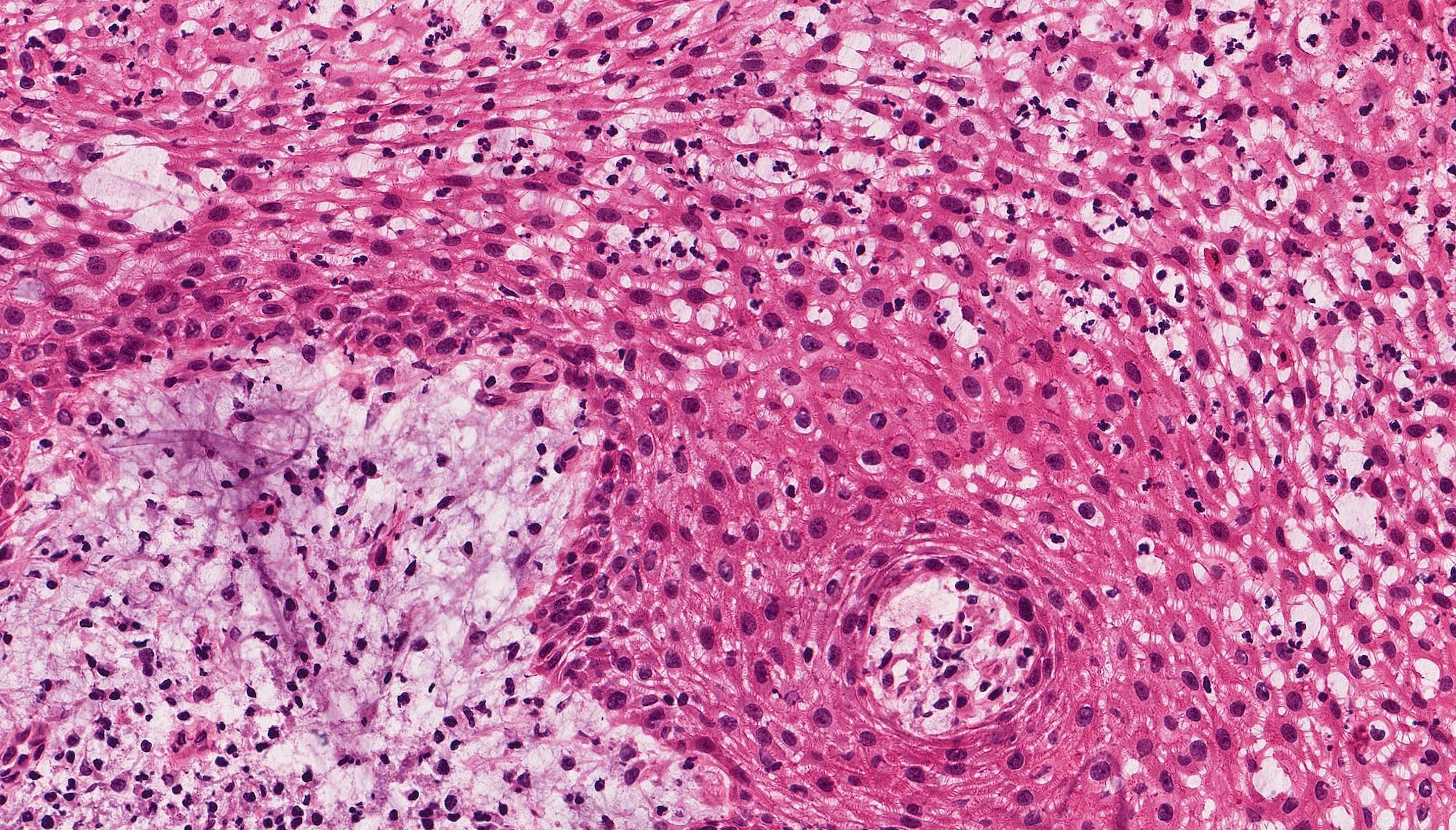
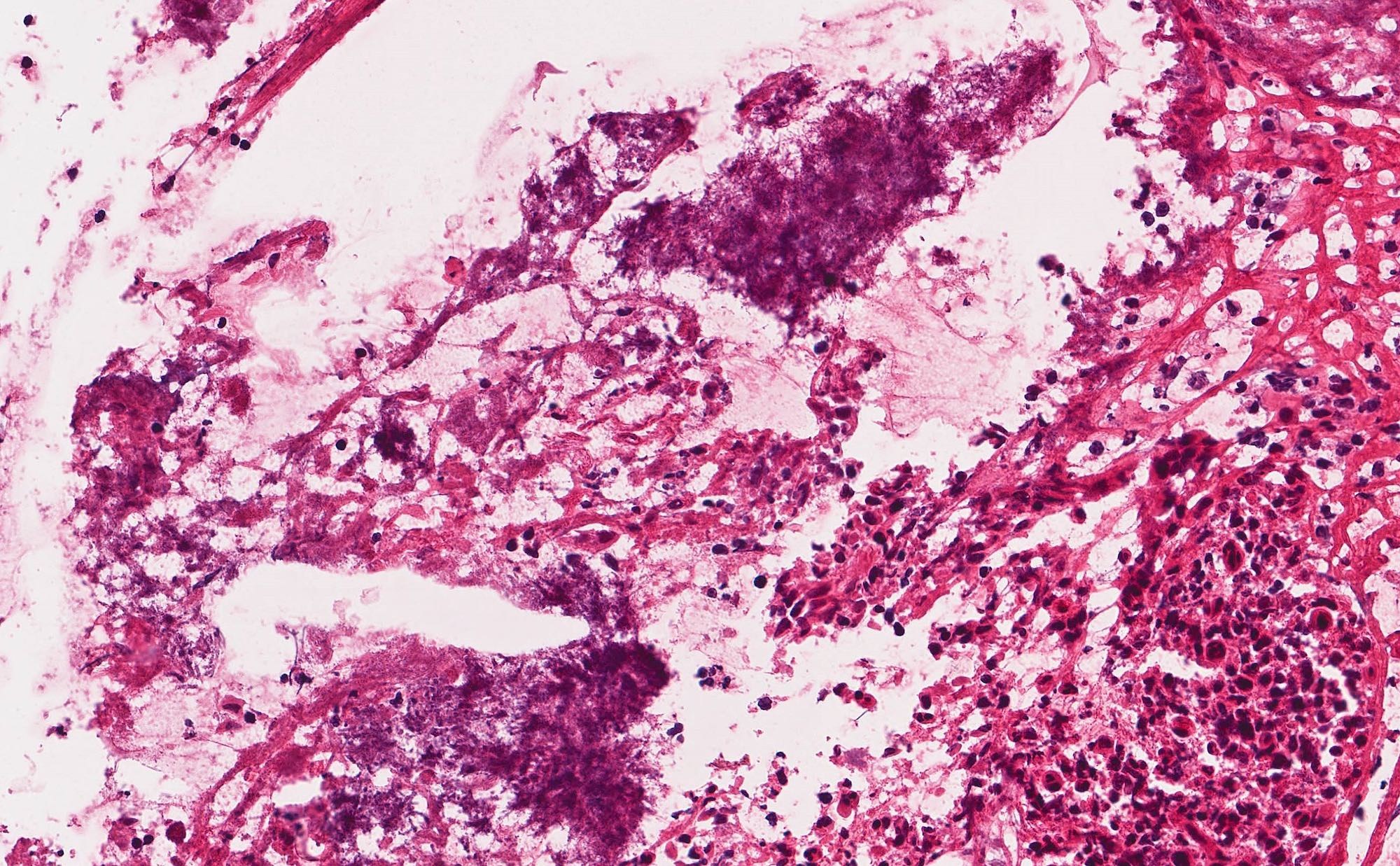
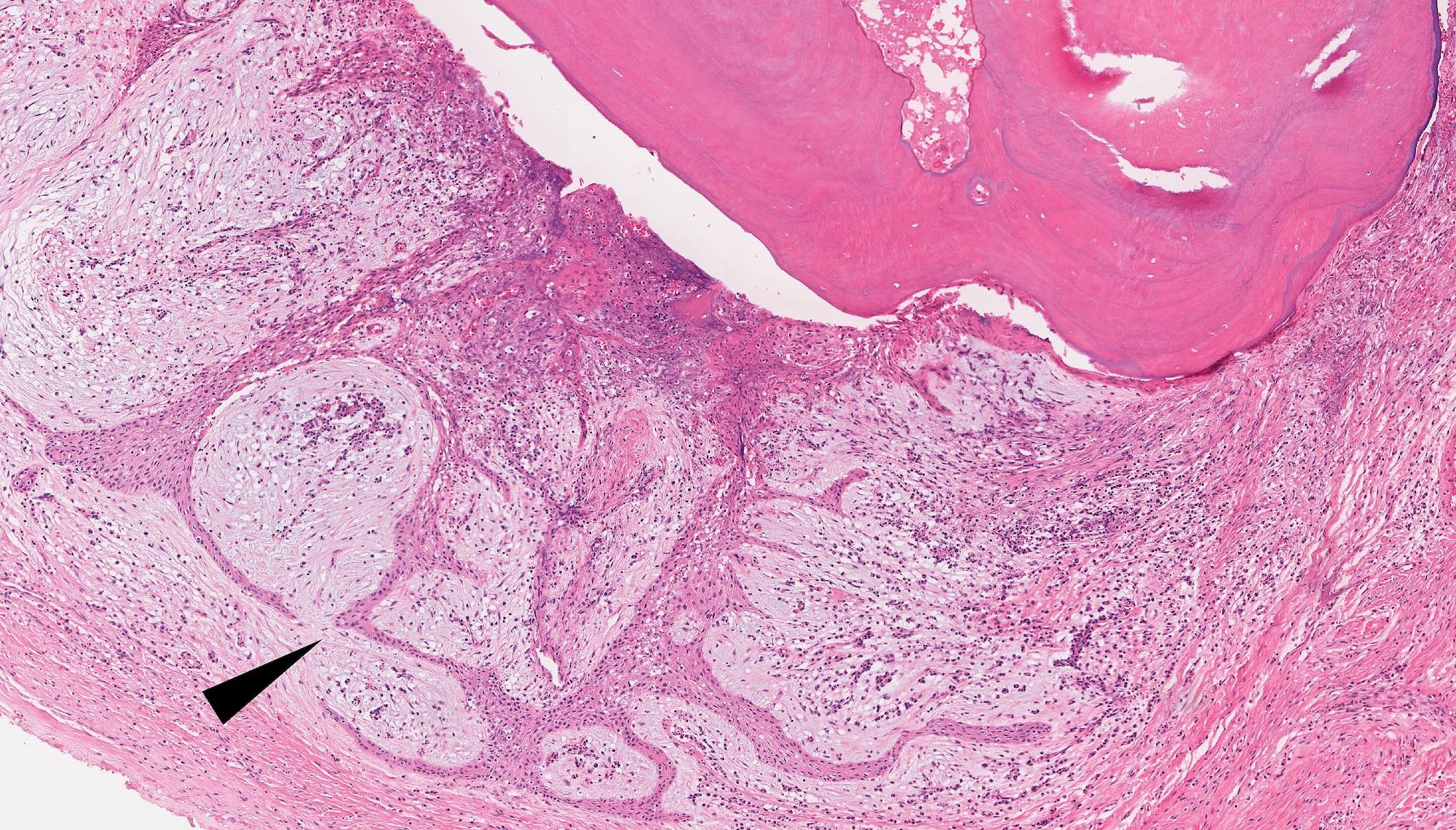
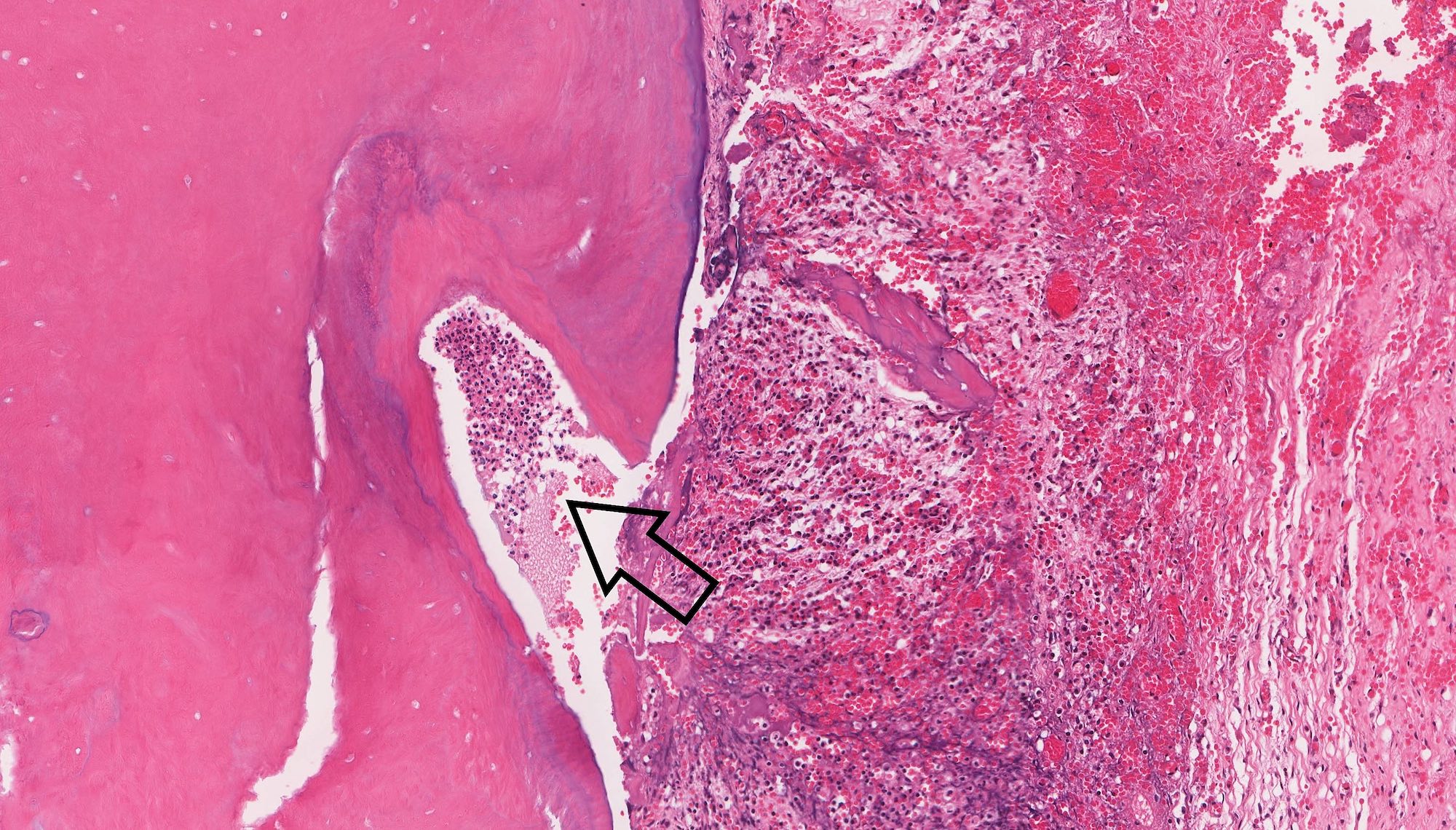
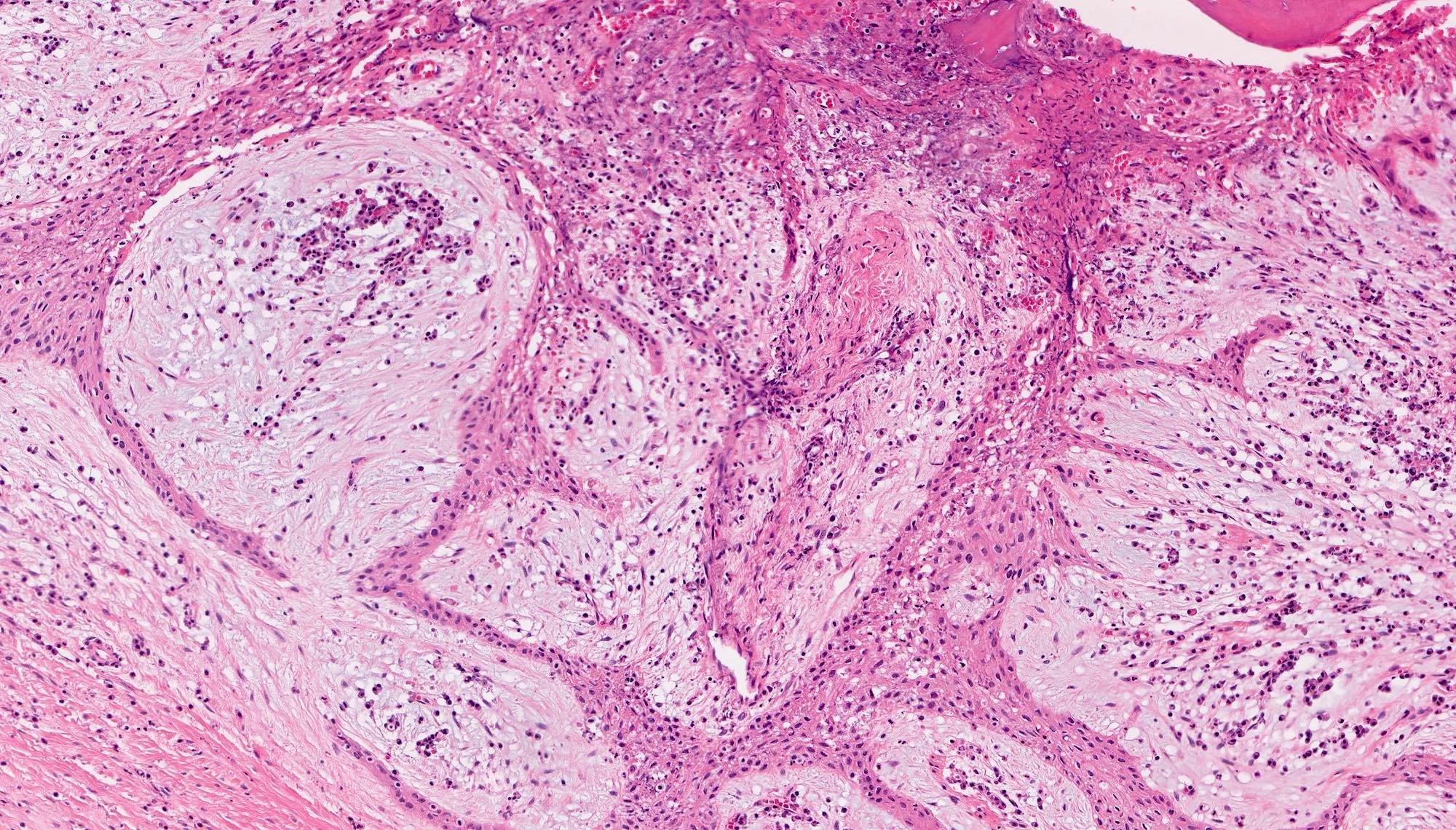
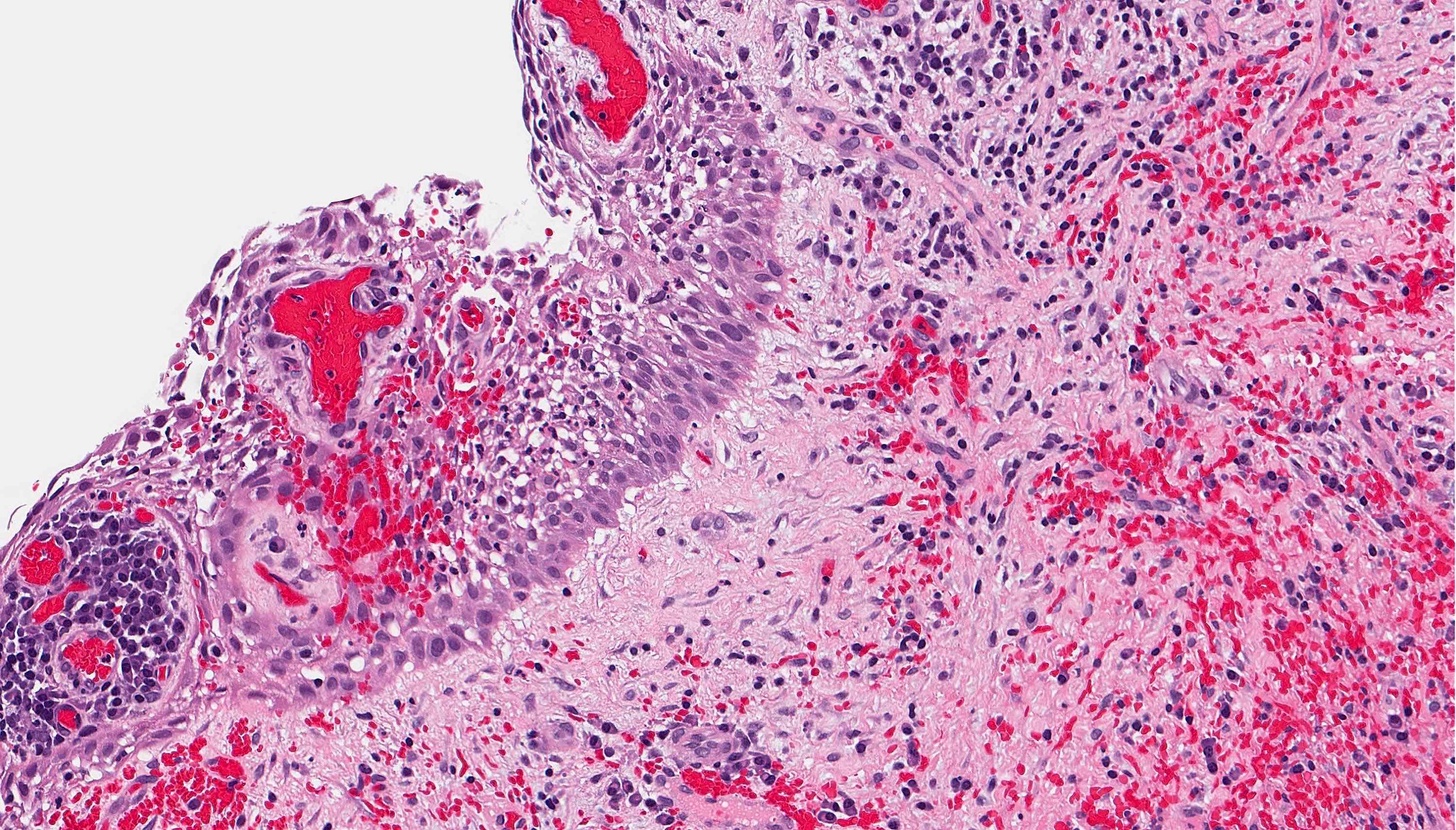
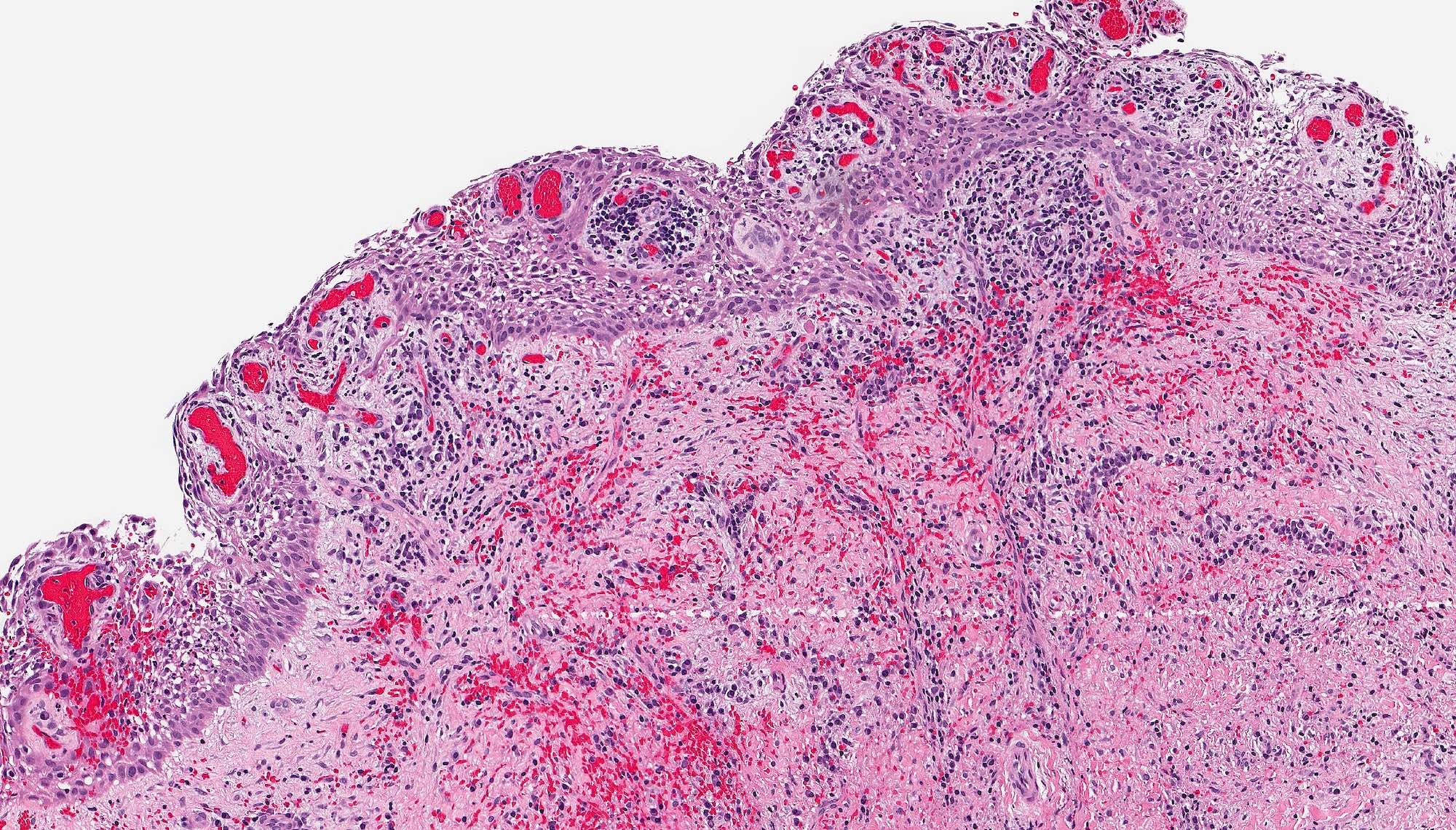
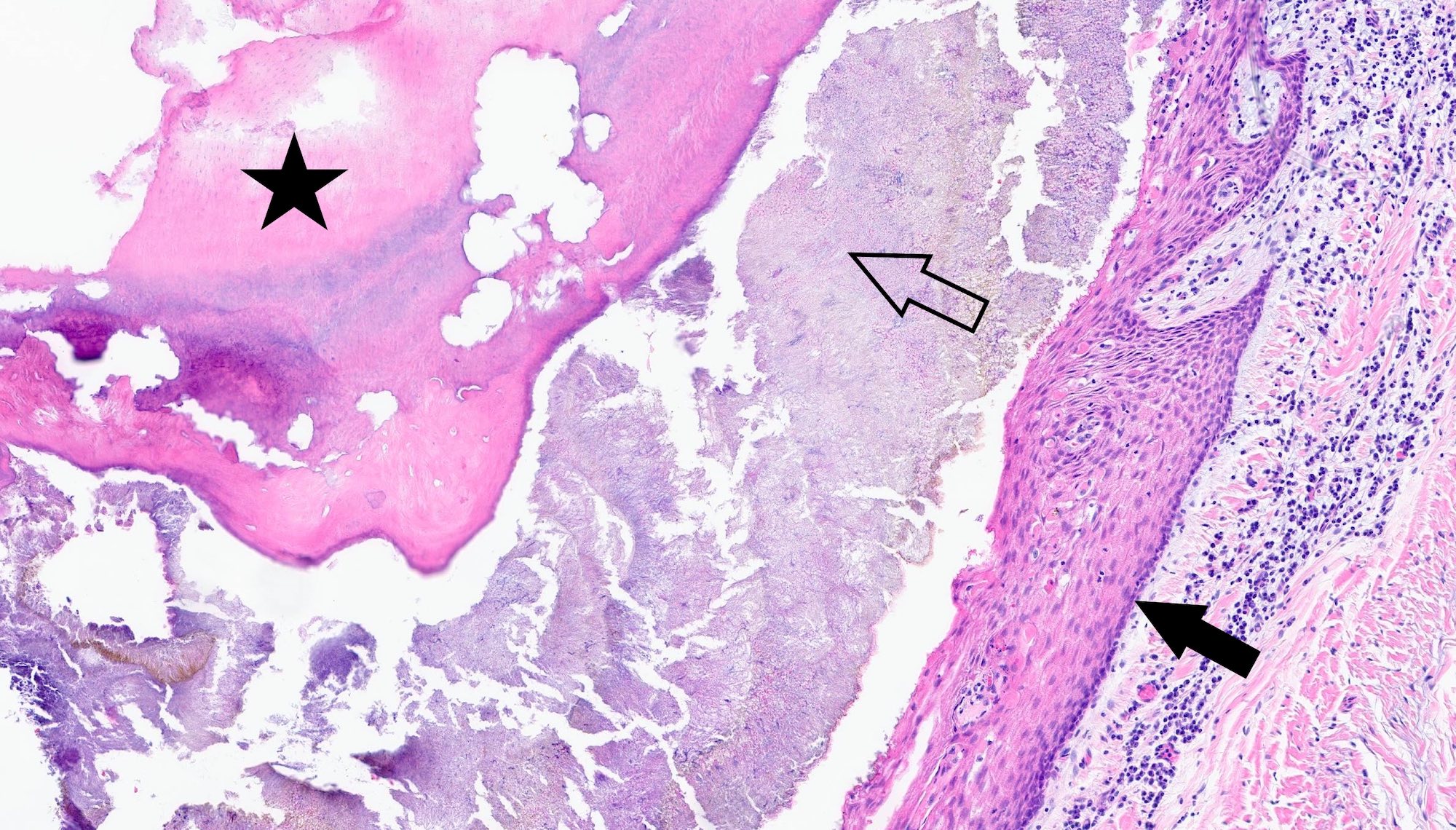
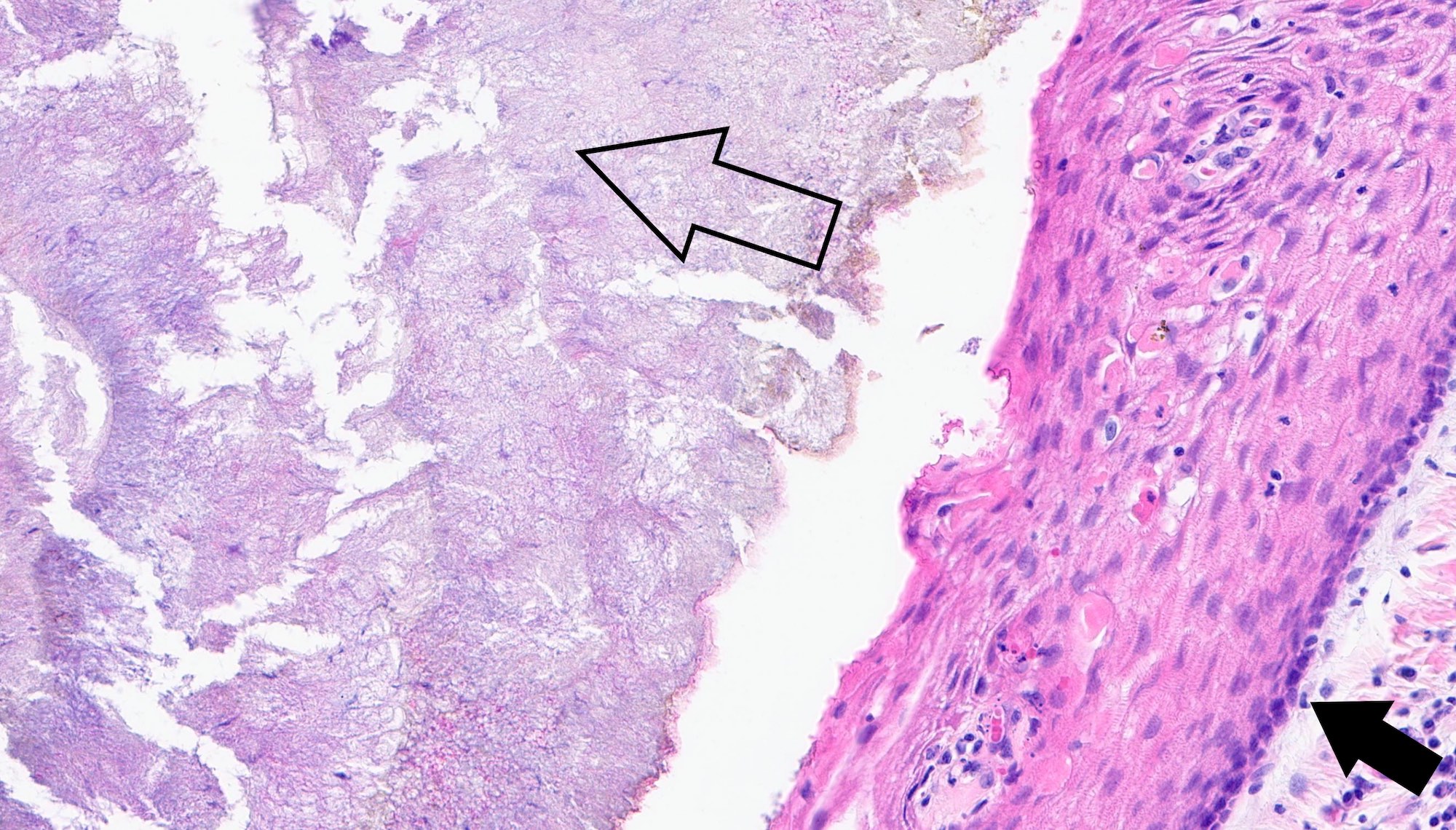
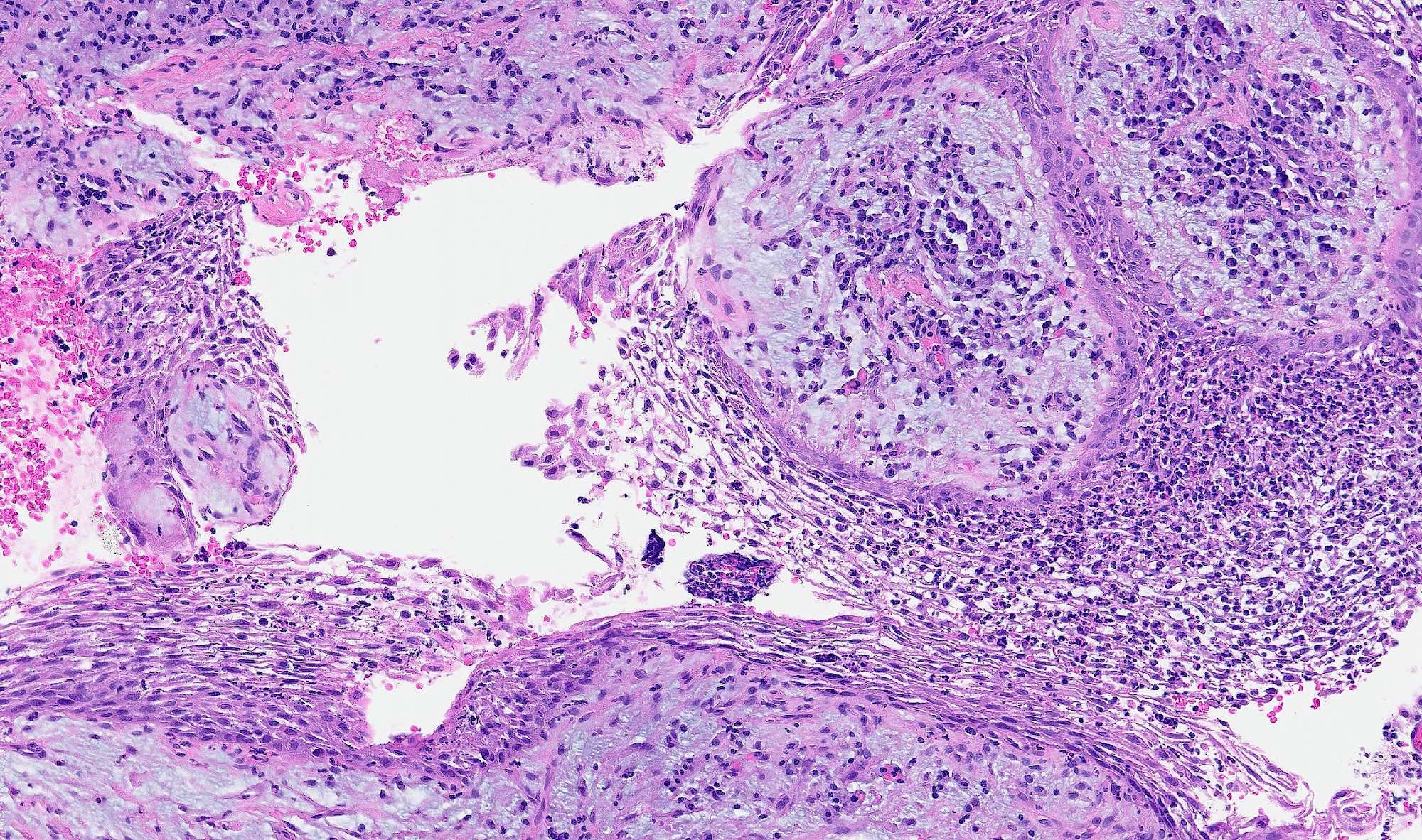
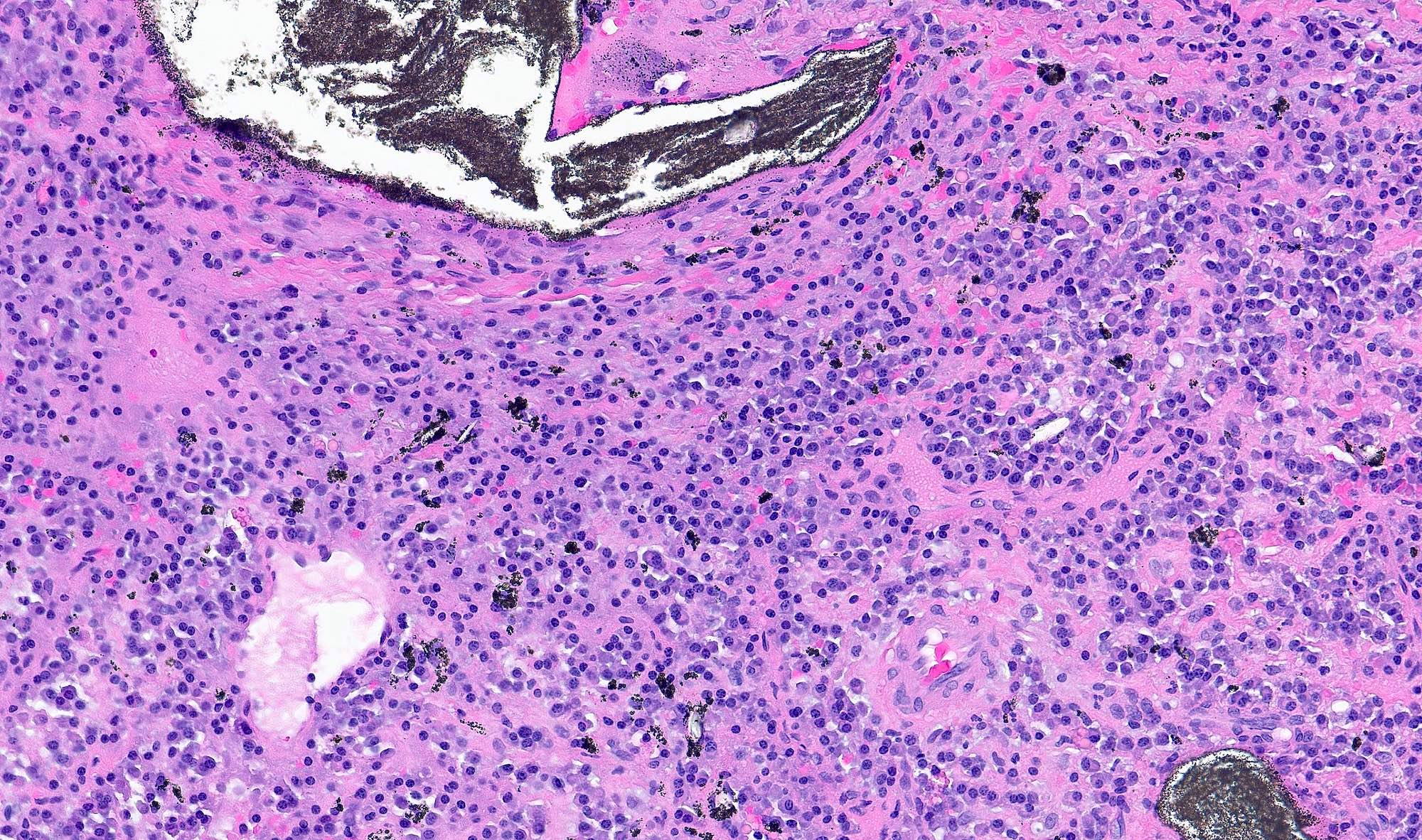
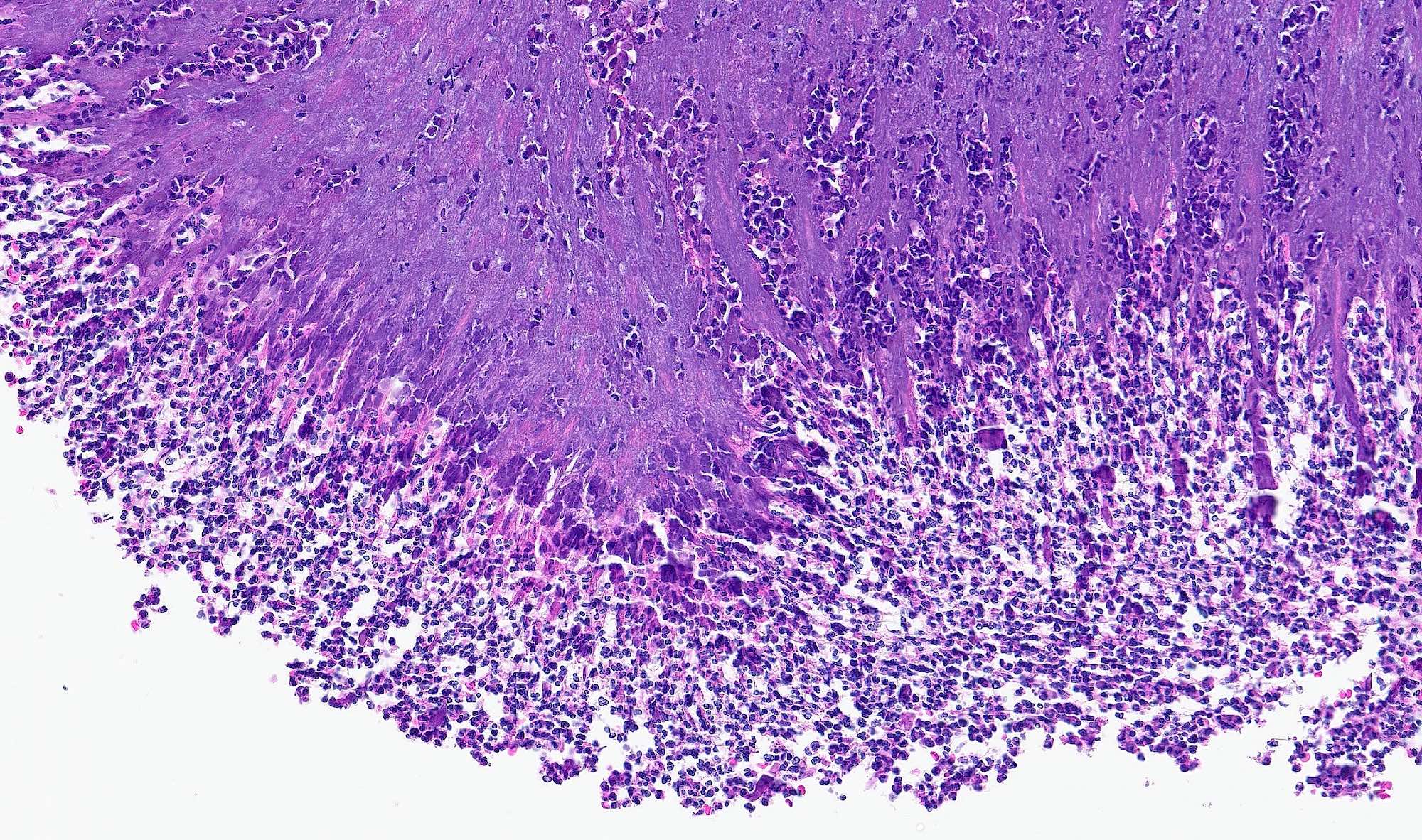
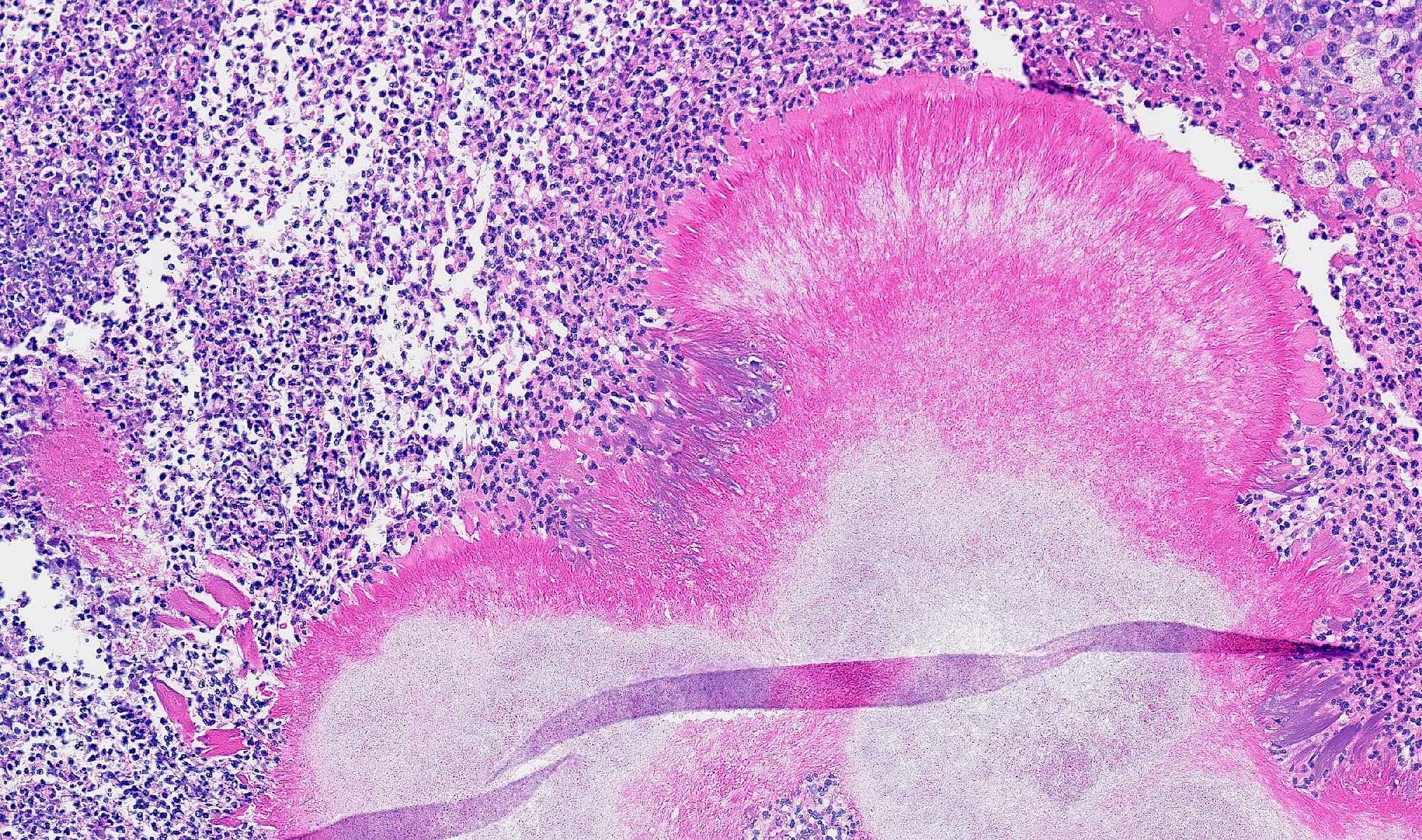
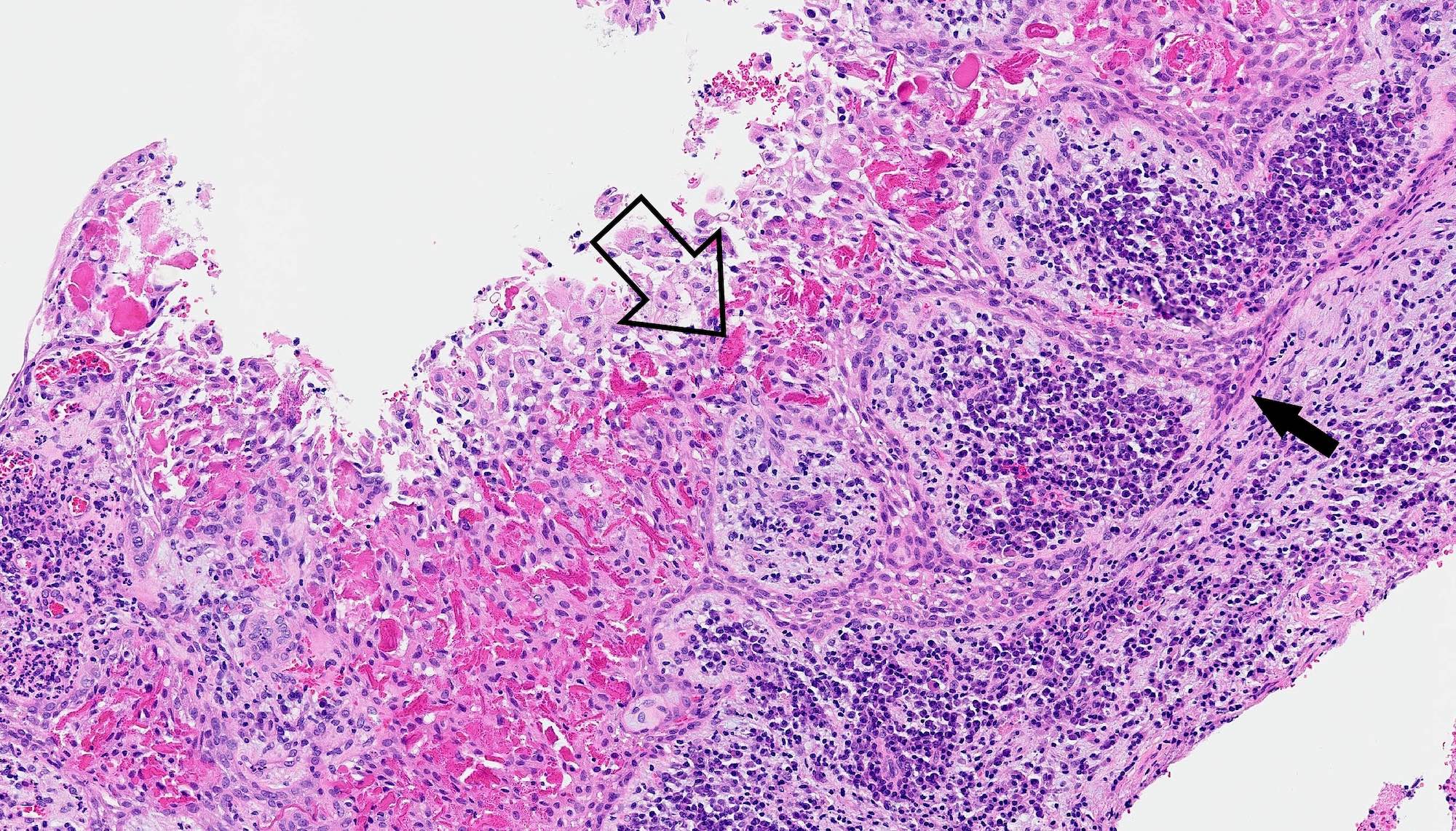
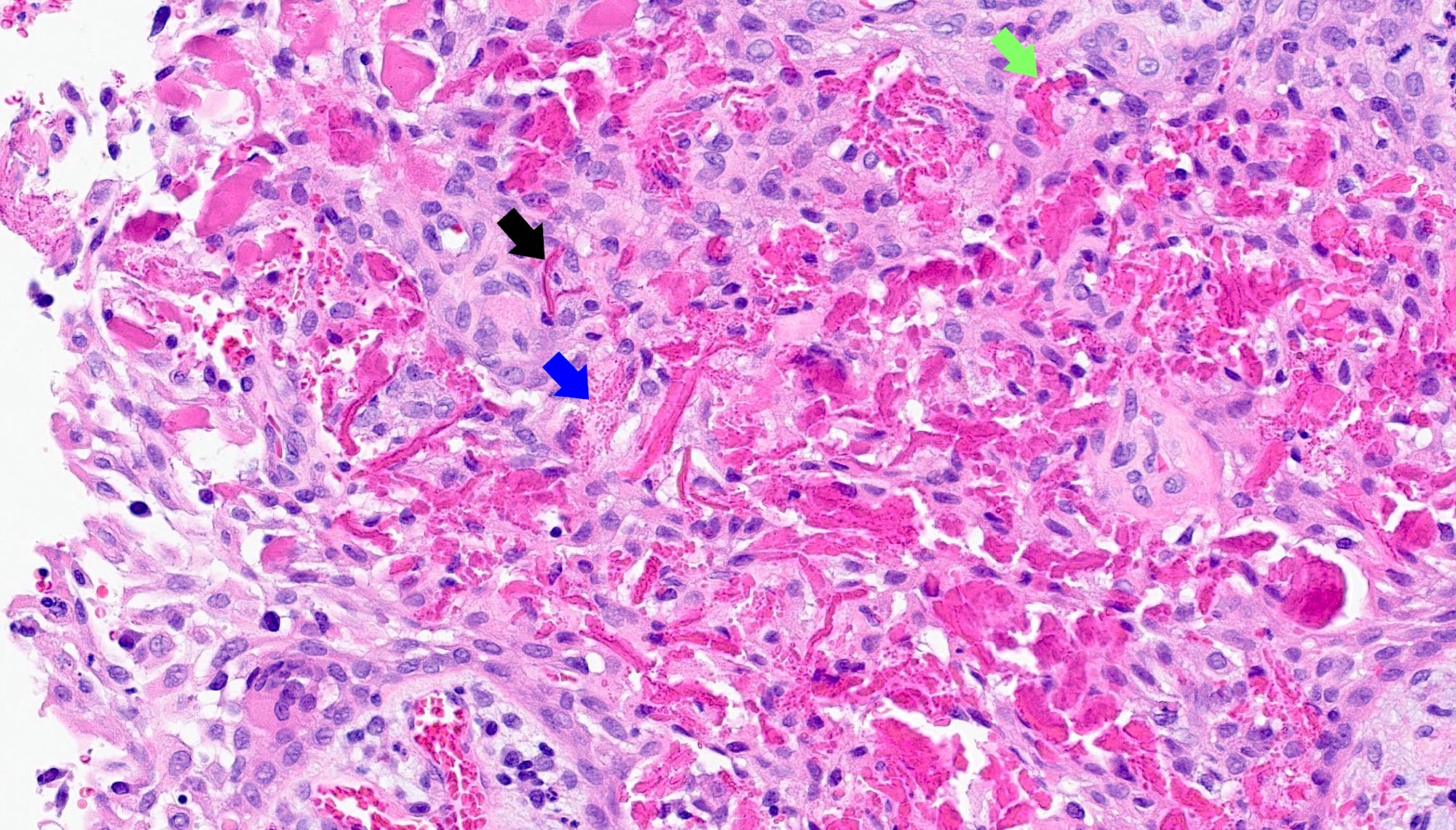
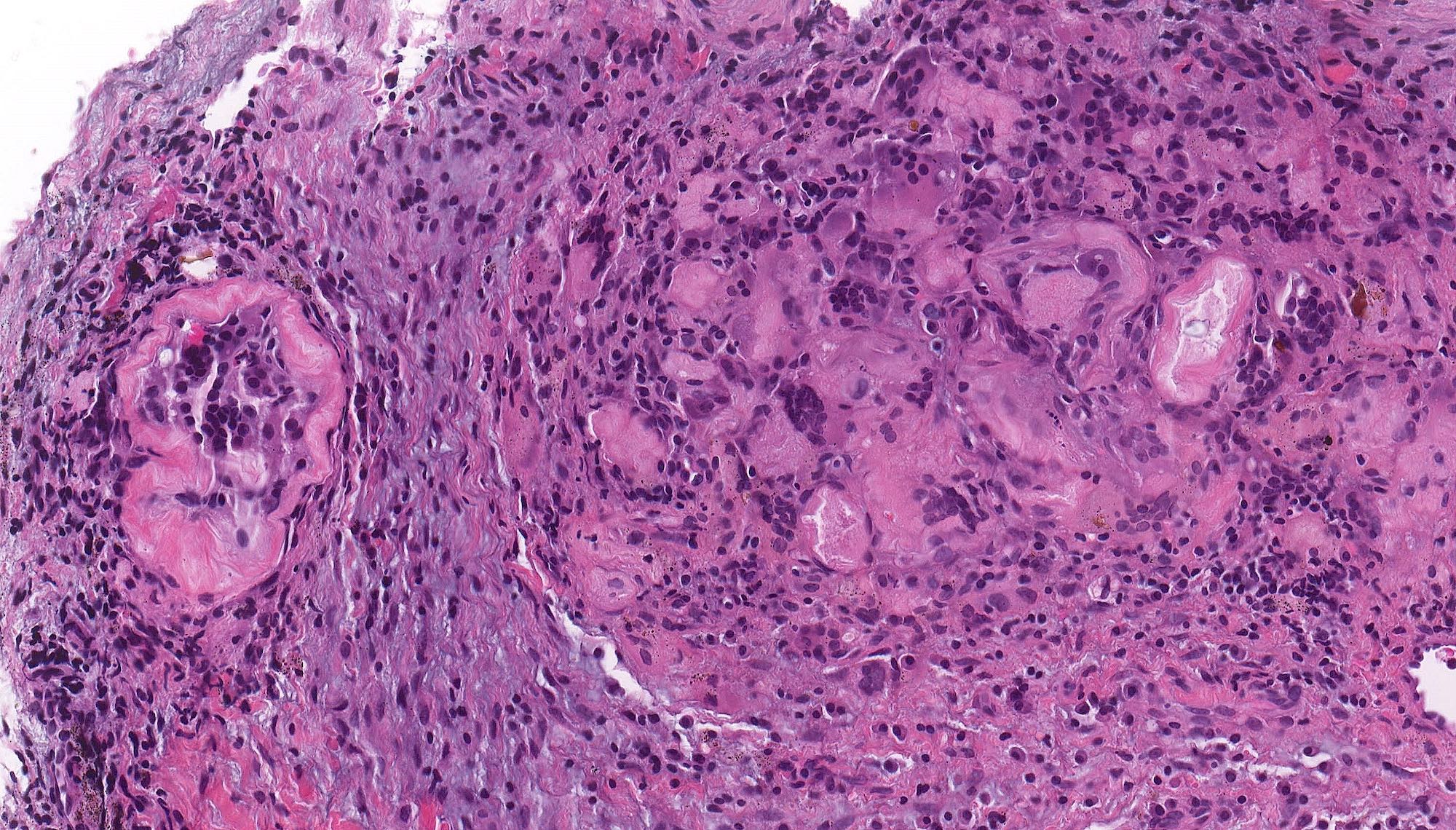
Microscopic (histologic) description
- Epithelial lining
- Lined by nonkeratinizing stratified squamous epithelium of variable thickness
- Architecturally creates an arcading pattern
- Can have limited areas of keratinization, goblet cells or scattered ciliated cells
- Rushton hyaline bodies can occur within the epithelium (not necessary for diagnosis, not specific to radicular cyst) (J Oral Maxillofac Pathol 2020;24:572)
- Fibrous capsule
- Varying thickness with acute or chronic inflammatory cells
- Plasma cells may be particularly prominent
- Foamy histiocytes may also be present
- Additional features possible (Kaohsiung J Med Sci 2018;34:249, Otolaryngol Head Neck Surg 2003;129:441)
- Cholesterol clefts
- Pulse granuloma
- Bacterial colonies
- Foreign material related to prior dental treatments
- Portions of bone, tooth or tooth root
- Regional odontogenic rests and neural tissue may be incorporated into biopsy tissue sample material by virtue of the curettage procedure
Microscopic (histologic) images
Contributed by Kelly Magliocca, D.D.S., M.P.H.
Positive stains
- No specific immunohistochemistry required for radicular cyst
- Squamous epithelium expected to be immunoreactive for cytokeratins, p63 and p40
Negative stains
- BRAF V600E
- Beta catenin nuclear staining
Sample pathology report
- Left mandible, biopsy:
- Intraosseous stratified squamous epithelial lined cyst, consistent with radicular cyst
Differential diagnosis
- Dentigerous cyst:
- Elongated clefts (spaces) in tissue remaining after cholesterol crystals dissolved in processing
- Clefts are associated with an adjacent or surrounding foreign body type giant cell reaction
- Rich granulation type inflammatory infiltrate, including hemosiderin laden macrophages
- Buccal bifurcation cyst:
- Polypoid chronic inflammation and granulation tissue only
- Lacking keratinizing squamous epithelial proliferation
- Lacking anucleate squames
- Microscopically some cases may be identical to cholesteatoma, though if middle ear is preserved, no middle ear mucosa will be seen microscopically
- Odontogenic keratocyst (inflamed):
- Uniform epithelial lining 6 - 8 cells thick; lacks rete ridges
- May have artifactual clefting between epithelium and underlying fibroconnective tissue
- Epithelium characterized by palisaded hyperchromatic basal cell layer comprised of cuboidal to columnar cells
- May have areas of budding growth from the basal cells
- Luminal surface has wavy (corrugated) parakeratotic epithelial cells
- Lumen may contain keratinaceous debris
- Squamous cell carcinoma:
- Lack of epithelial cell maturation or polarity, atypical mitosis, pleomorphism, dyskeratosis or individual cell keratinization
Additional references
Practice question #1
Practice answer #1
B. Association with nonviable (necrotic) tooth. Radicular cyst is seen in association with a nonviable (necrotic) tooth. Answer A is incorrect because association with an impacted tooth is a required element for dentigerous cyst. Answer C is incorrect because radicular cyst uncommonly occurs as a bilateral lesion. Answer D is incorrect because radicular cyst is located in association with teeth, within bone.
Comment Here
Reference: Radicular cyst
Comment Here
Reference: Radicular cyst
Practice question #2
Which of the following sites is most commonly involved by radicular cyst?
- Anterior mandible
- Anterior maxilla
- Maxillary sinus
- Posterior mandible
Practice answer #2
B. Anterior maxilla. Anterior maxilla is the most common site of involvement for radicular cyst. Answer A is incorrect because radicular cyst can involve the anterior mandible but is not the most common location. Answer C is incorrect because radicular cyst is unlikely to be centered in the maxillary sinus, unless the lesion secondarily extends into the sinus, which is uncommon. Answer D is incorrect because the posterior mandible is the second most common site for radicular cyst to occur.
Comment Here
Reference: Radicular cyst
Comment Here
Reference: Radicular cyst