Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Busca A, Parra-Herran C. Teratoma-immature. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorteratomaimmature.html. Accessed September 24th, 2025.
Definition / general
- A malignant germ cell tumor consisting of a teratoma containing variable amounts of immature tissue (typically primitive neuroectodermal)
Essential features
- Malignant germ cell tumor of the ovary composed of cells from the 3 germ layers and containing variable amounts of mature and immature tissue
- Affects mostly young females < 20 years old
- Grossly solid ovarian tumor mass with necrosis and hemorrhage on cut sections
- Grading is based on the amount of immature neuroepithelium
- Can have associated nodal or peritoneal gliomatosis (presence of mature neural tissue), which increases risk of recurrence
- Grading and stage are the most important factors for prognosis and prognosis is greatly improved after chemotherapy
Terminology
- Immature teratoma
ICD coding
- ICD-O: 9080/3 - teratoma, malignant, NOS
Epidemiology
- Immature teratomas constitute about a third of malignant germ cell tumors (Cancer 1976;37:2359, Obstet Gynecol 2006;107:1075)
- Mean age at diagnosis is 20.6; only 4 of 244 patients with immature teratoma were older than 40 (Int J Gynecol Pathol 1994;13:283)
Sites
- Ovary
Pathophysiology
- Abnormal differentiation of fetal germ cells
- 2 pathogenetic models for ovarian teratomas, similar to their testicular counterparts
- Pure mature and immature teratomas are not derived from transformed ovarian germ cells
- Teratomatous components of mixed germ cell tumors derived from their associated nonteratomatous components
- Pure mature and immature teratomas do not have i(12p) or 12p amplification, abnormalities that are identified in both teratomatous and nonteratomatous components of mixed germ cell tumors; this supports a different pathogenesis for pure versus mixed tumors (Mod Pathol 2006;19:766)
- 25% of cases with immature teratoma have peritoneal implants composed of mature glial tissue (gliomatosis peritonei); this phenomenon is thought to arise from metaplasia of submesothelial cells in response to growth factors secreted by the ovarian tumor, rather than a true metastatic process (Hum Pathol 1976;7:625, Hum Pathol 2004;35:685, Int J Gynecol Cancer 2015;25:244, Mod Pathol 2015;28:1613)
- Rarely, mature glial tissue is also present in lymph nodes (nodal gliomatosis), usually with associated gliomatosis peritonei
- Prognosis is good and the presence of nodal gliomatosis does not warrant chemotherapy (J Ovarian Res 2016;9:45, Mod Pathol 2015;28:1613)
Etiology
- No known causative agents
Clinical features
- Associated with symptoms of rapidly growing abdominal mass, pain, distention and torsion
- Growing teratoma syndrome: immature teratoma status postneoadjuvant chemotherapy consists of persistent or enlarging ovarian tumor with normalization of serum markers
- Thought to represent conversion of deposits of immature teratoma into mature teratoma as a result of chemotherapy (chemotherapeutic retroconversion) (Int J Gynecol Pathol 2015;34:465, Medicine (Baltimore) 2016;95:e2647)
- Histologic examination shows only mature teratoma
Diagnosis
- A combination of clinical, radiological and laboratory findings: rapidly enlarging adnexal mass in a young patient with mildly elevated alpha fetoprotein (AFP) and typical radiological findings raises the possibility of immature teratoma
- Requires histological examination for confirmation of diagnosis and grading
- Reference: Int J Gynecol Pathol 1994;13:283
Laboratory
- Low level increase of AFP
- High levels of AFP suggest the presence of a yolk sac tumor component (mixed germ cell tumor)
Radiology description
- On CT imaging, the solid component appears large and irregular, with coarse calcifications and small foci of fat scattered throughout the lesion rather than localized, as seen in dermoid cyst (J Med Imaging Radiat Oncol 2009;53:480, Eur J Radiol 2009;72:454)
Prognostic factors
- Older age at diagnosis, higher stage and grade confer worse prognosis but overall improved after chemotherapy, with 72% survival for stage IV disease (Gynecol Oncol 2016;142:261, Gynecol Oncol 2016;142:446)
- Grade is the most important risk factor for relapse across all age groups
- In a study of 98 pediatric patients and 81 adult patients, there were no relapses in grade 1 patients, irrespective of stage or age; only 1 adult patient with a grade 2 tumor relapsed (Cancer 2016;122:230)
- In patients with grade 3 tumors, recurrence rate was 21% in the pediatric cohort and 20% in the adult cohort and was significantly associated with stage (Cancer 2016;122:230)
- Higher risk of recurrence with presence of gliomatosis peritonei or lymph node gliomatosis but similar overall survival (Virchows Arch 2012;461:299, J Ovarian Res 2016;9:45)
Case reports
- 5 year old girl with ruptured immature teratoma at initial presentation (IJAR 2017;5:1811)
- 12 year old girl with grade 1 immature teratoma in the left ovary that presented as growing teratoma syndrome of the ovary (Medicine (Baltimore) 2020;99:e22297)
- 12 year old monozygotic twin girls with simultaneous presentation of ovarian mature and immature teratomas (Case Rep Obstet Gynecol 2017;2017:5810515)
- 13 year old girl with growing teratoma syndrome after treatment for immature teratoma (J Obstet Gynaecol India 2017;67:295)
- 31 year old woman with immature teratoma in pregnancy (Open Access Maced J Med Sci 2019;7:1016)
- 46 year old woman presented with simultaneous immature teratoma in the endometrium and mature teratomas in the ovary associated with gliomatosis peritonei (Int J Gynecol Pathol 2017;36:222)
Treatment
- Surgery plus chemotherapy for grade 2 or 3 lesions in adult women (Cancer 2016;122:230, Gynecol Oncol 2011;123:50)
- Patients with stage I, grade 1 tumors can be followed by surveillance (Gynecol Oncol 2011;123:50)
- Primarily surgical treatment for pediatric population (J Clin Oncol 2008;26:3590)
Gross description
- Usually unilateral ovarian masses with a mean size of 16 cm (range: 5 - 42 cm) (Int J Gynecol Pathol 1994;13:283)
- Solid with cystic areas or mostly solid; hemorrhage and necrosis on cut sections
- Contralateral ovary with mature teratoma in 9% of cases
Frozen section description
- Extensive sampling may be needed to include areas of immature teratoma at the time of frozen section in cases where a preoperative diagnosis of immature teratoma is suspected; sample nodular, soft appearing and mass forming areas
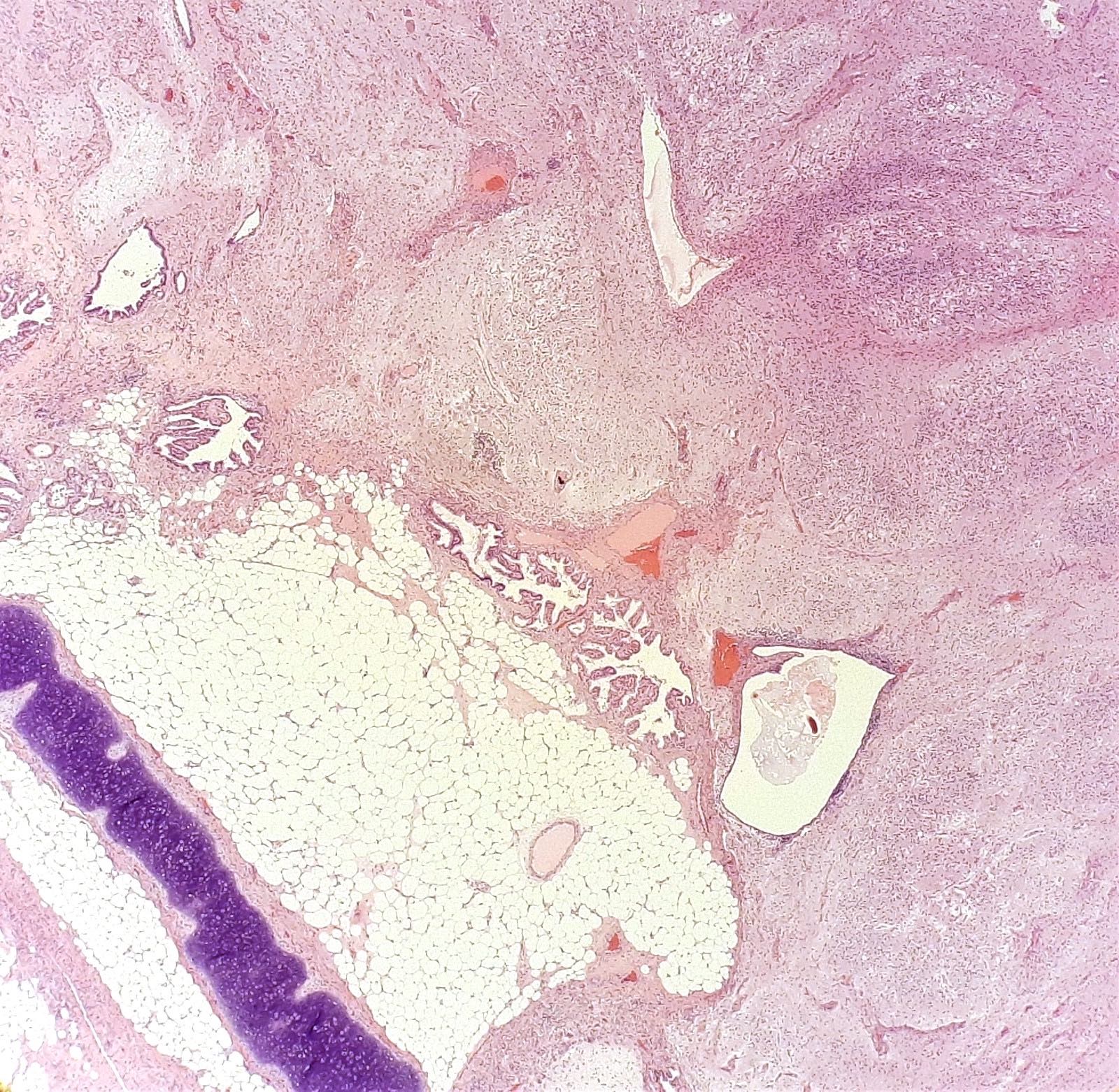
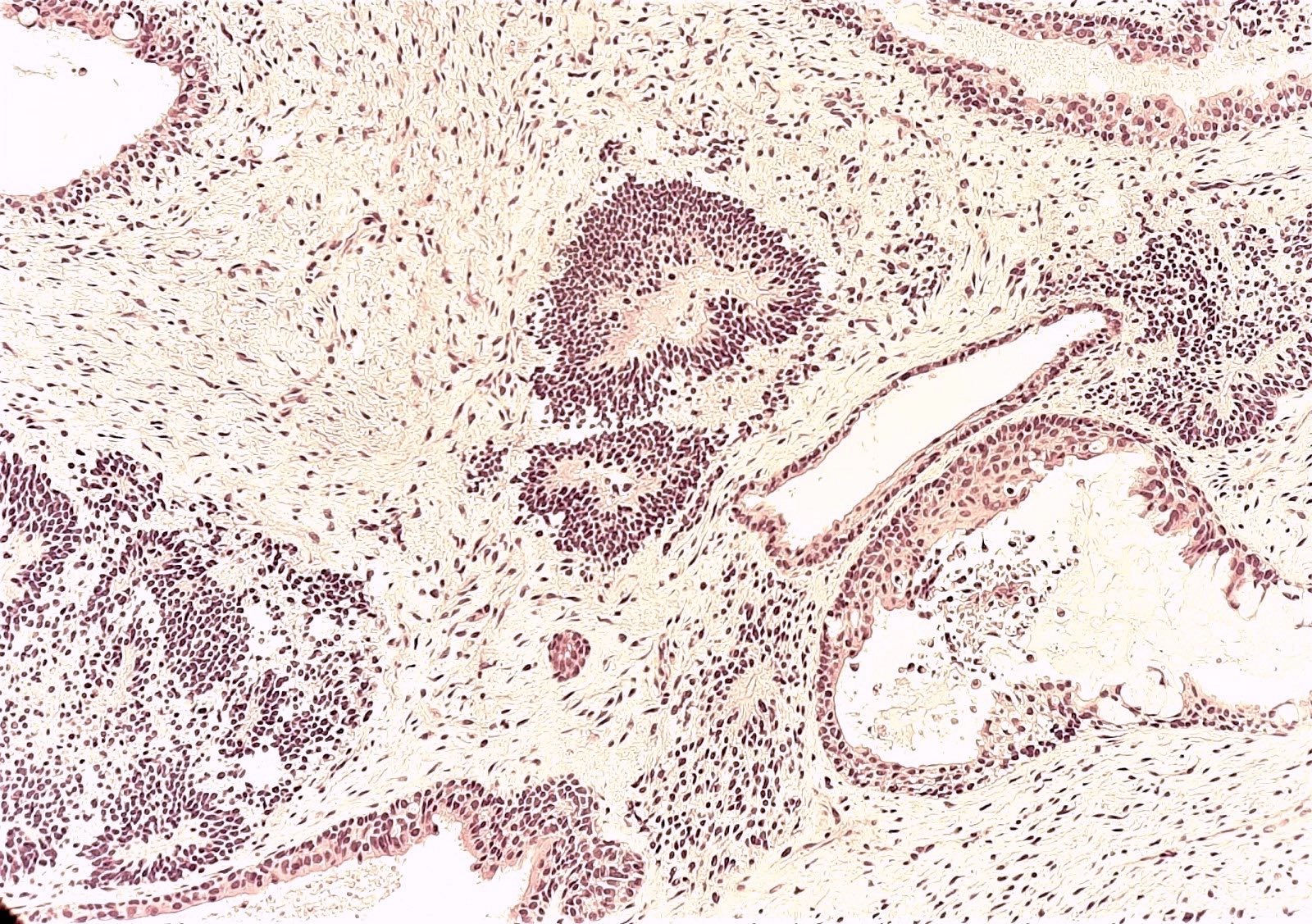
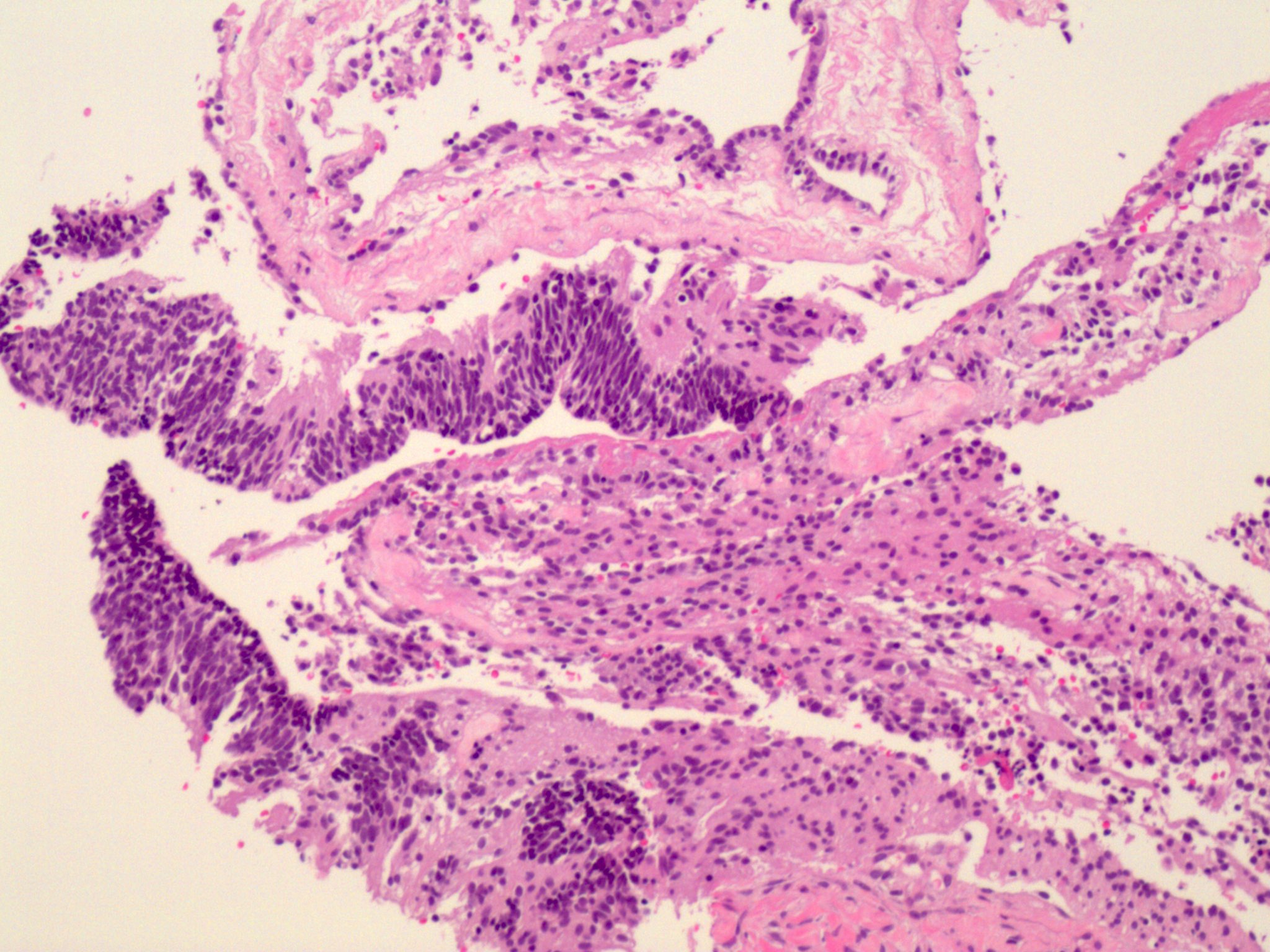
Microscopic (histologic) description
- Variable amounts of mature elements from all 3 germ layers, admixed with immature elements, mostly neuroectodermal
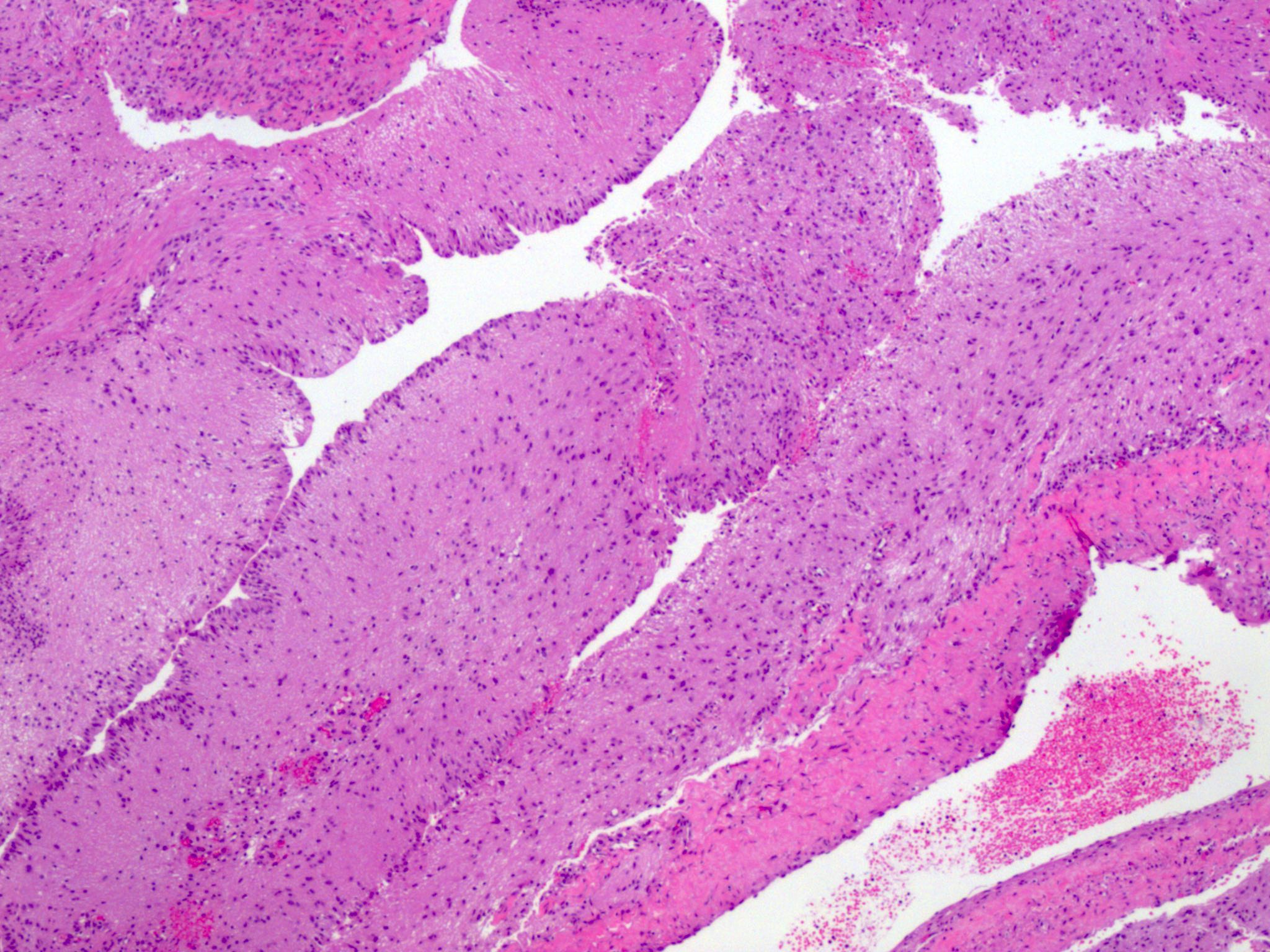
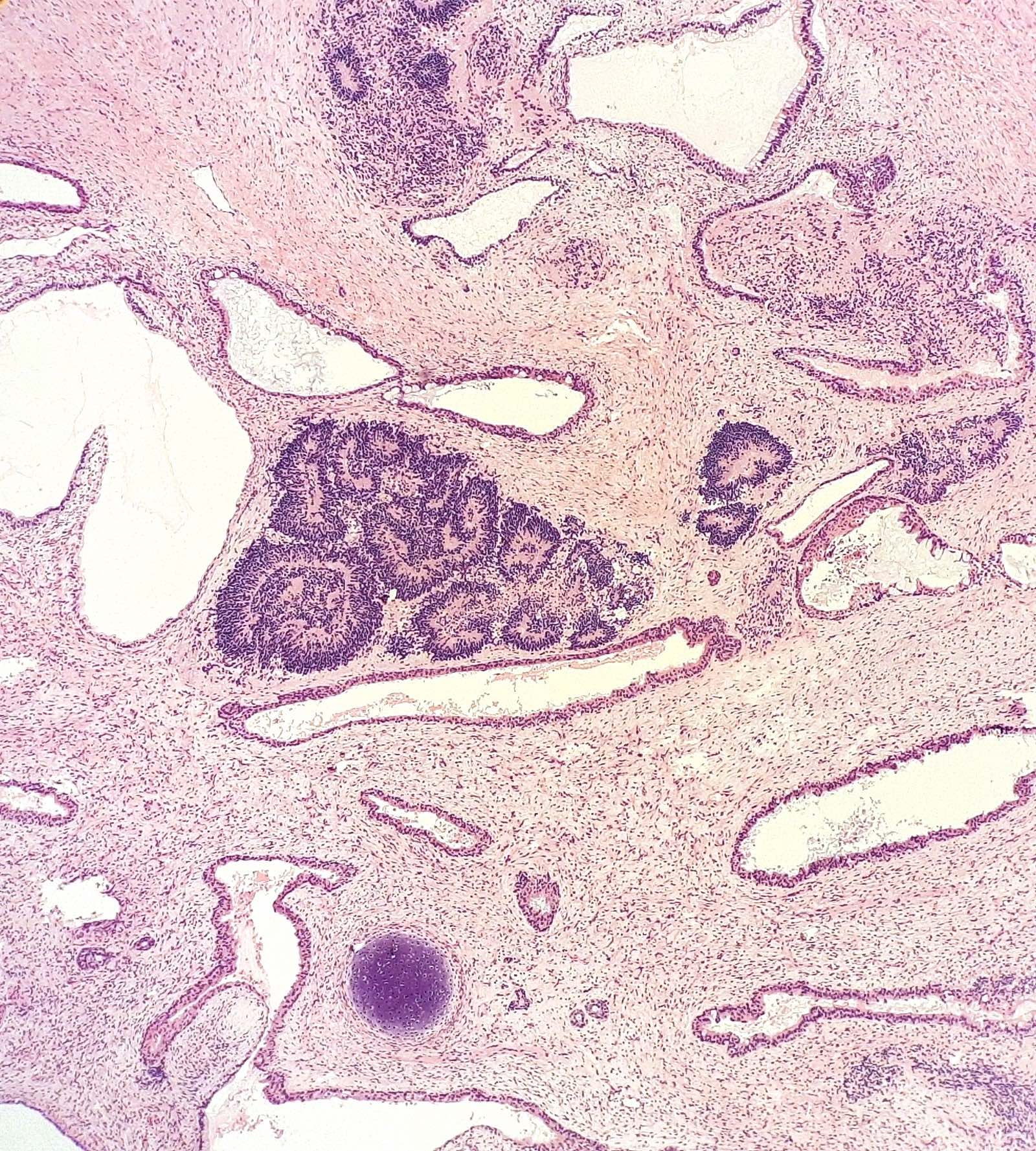
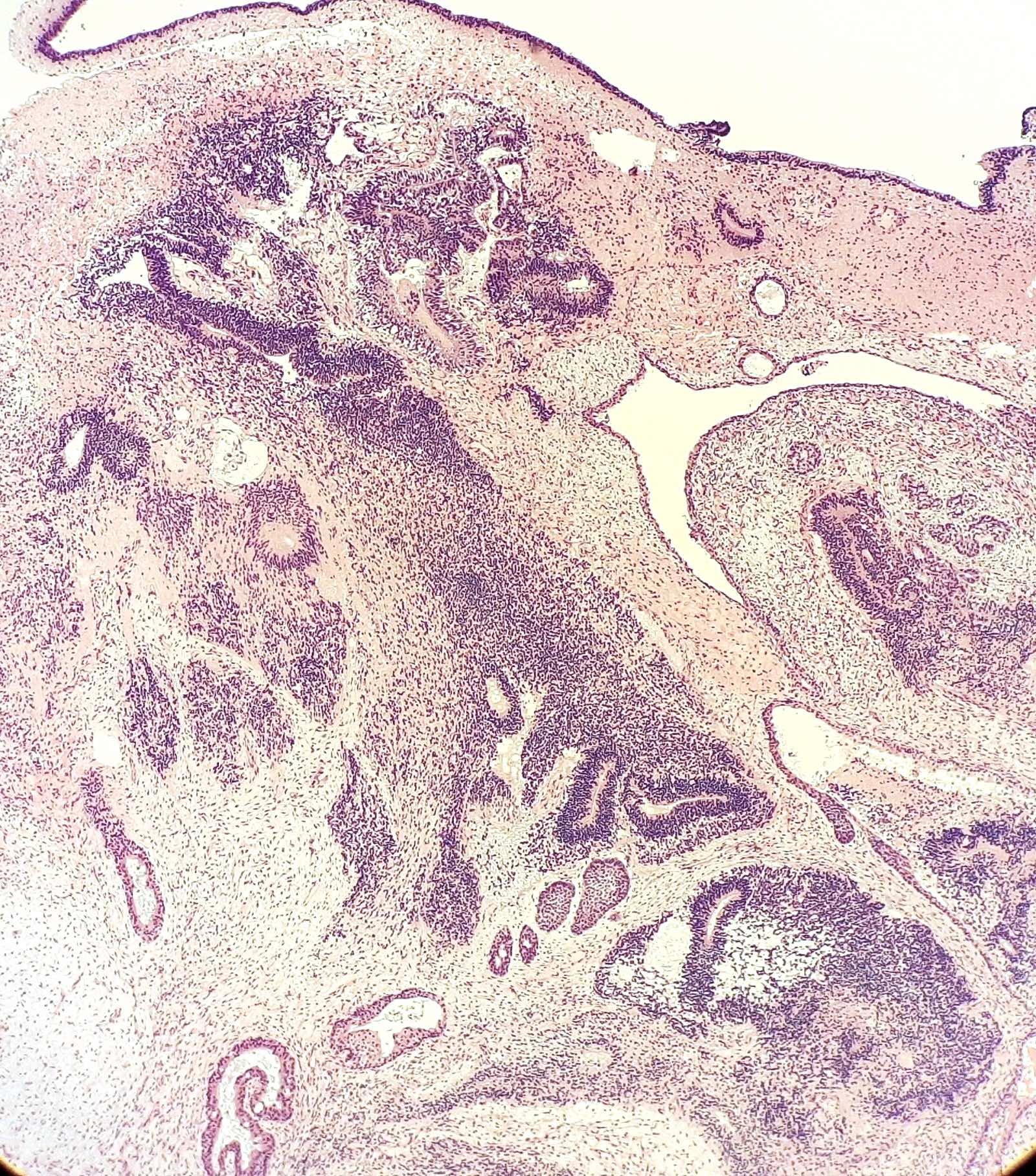
- Immature neuroepithelium
- Immature neuroepithelium can be spindled (sarcomatoid) or with rosette, pseudorosette and primitive tubule formation; the latter is easier to recognize
- Cells appear primitive with scant cytoplasm, hyperchromatic nuclei and frequent mitoses, which helps differentiate the immature elements from mature brain tissue
- Only immature neuroepithelium is used for grading, so it is important to recognize as such on histological slides
- Grading is based on the number of low power microscopic fields containing aggregated amounts of immature neuroepithelium in any one slide
- Original grading system (Cancer 1976;37:2359)
- Grade 1: ≤ 1 low power field (using a 4x power objective, which when using a 10x eyepiece, leads to a 40x magnification) in any slide
- Grade 2: > 1 but ≤ 3 low power fields in any slide
- Grade 3: > 3 low power fields in any slide
- Grade 2 and 3 tumors are considered high grade, therefore the updated grading system is 2 tiered, with improved reproducibility (Int J Gynecol Pathol 1994;13:283)
- Low grade: ≤ 1 low power field (using a 4x power objective, which when using a 10x eyepiece, leads to a 40x magnification) in any slide
- High grade: > 1 low power field in any slide
- Neural tissue can have a prominent associated benign vascular proliferation with Wagner-Meissner-like corpuscles, which should not be interpreted as an immature component (Int J Gynecol Pathol 2002;21:16, Int J Surg Pathol 2008;16:320)
- Fetal cartilage can be present and is not considered an immature element
- Small foci of yolk sac tumor or embryonal carcinoma (< 3 mm) can be seen in immature teratomas without changing prognosis; however, presence of any yolk sac or embryonal carcinoma component changes the classification to a mixed germ cell tumor (Int J Gynecol Pathol 1994;13:283, Cancer 1976;37:2359)
- Peritoneal and nodal gliomatosis nodules consist of mature glial tissue, considered grade 0 for grading purposes; thorough sampling is required to identify immature tissue (metastatic immature teratoma component), which has a worse prognosis
Microscopic (histologic) images
Cytology description
- Immature elements are rarely observed in ascites (Diagn Cytopathol 2005;33:39)
Positive stains
- Immunohistochemistry has limited role in diagnosis of immature teratoma
- Immature neuroepithelium
- S100, GFAP, NSE (does not differentiate between mature and immature components)
- OCT4 and PAX6 (OCT4 preferentially expressed in immature neural tissue of advanced stage immature teratomas) (Am J Surg Pathol 2010;34:1842)
- SALL4, SOX2, glypican 3 (Hum Pathol 2010;41:716, Histopathology 2011;58:312)
- Gliomatosis peritonei: SOX2+ (Mod Pathol 2015;28:1613)
Negative stains
- Gliomatosis peritonei: OCT4- / NANOG- (Mod Pathol 2015;28:1613)
- Neuroepithelium is negative for CD30, alpha fetoprotein (AFP), keratin, PAX8
Molecular / cytogenetics description
- i(12p) and 12p amplification is present in immature teratomatous components of mixed germ cell tumors but not in pure immature teratomas (Mod Pathol 2006;19:766)
Sample pathology report
- Left ovary, oophorectomy:
- Immature teratoma (see synoptic report)
- Tumor grade: 1 (low grade)
- Tumor size: 16 cm
- Ovarian surface involvement: present
- Immature teratoma (see synoptic report)
Differential diagnosis
- Mature cystic teratoma with mature neural elements:
- Predominantly cystic appearance grossly
- Neural elements are mature
- Microscopic foci of immature elements do not warrant a diagnosis of immature teratoma (Int J Gynecol Pathol 1987;6:203)
- Mature solid teratoma:
- Grossly similar
- Composed exclusively of mature elements
- Very rare, requires very rigorous sampling to rule out an immature component (Gynecol Oncol 1989;33:212)
- Carcinosarcoma:
- Usually postmenopausal women
- Mixed malignant epithelial and mesenchymal components, usually high grade
- Mesenchymal component is frequently chondrosarcoma (no fetal cartilage)
- Rare cases of ovarian carcinosarcoma with neuroectodermal differentiation have been reported (teratoid carcinosarcoma) (J Obstet Gynaecol Res 2010;36:907, Case Rep Oncol 2019;12:241)
- Mixed germ cell tumor:
- Extensive sampling is required to rule out another germ cell component (usually yolk sac tumor or embryonal carcinoma)
Additional references
Practice question #1
Which of the following is true about gliomatosis peritonei found in ovarian immature teratoma?
- Considered a metaplastic rather than a true metastatic process
- Consists of immature glial tissue
- Has no impact on prognosis of immature teratoma
- Is used for grading of the immature teratoma
Practice answer #1
A. Considered a metaplastic rather than a true metastatic process. The current understanding of gliomatosis is as a metaplastic rather than a true metastatic process. Answer B is incorrect because gliomatosis consists of mature neural tissue. Answer C is incorrect because presence of gliomatosis has been linked with increased risk of recurrence. Answer D is incorrect because only immature neuroepithelium component is used for grading.
Comment Here
Reference: Teratoma - immature
Comment Here
Reference: Teratoma - immature
Practice question #2
Which of the following is true about grading of immature teratoma of the ovary?
- Both grade 1 and grade 2 tumors are considered low grade in the 2 tier classification system
- Grade does not impact prognosis
- Presence of immature elements in more than 1 low power field is in keeping with high grade
- Takes into account all histologic types of immature tissue
Practice answer #2
C. Presence of immature elements in more than 1 low power field is in keeping with high grade in the 2 tier classification system. Answer B is incorrect because higher grade correlates with worse prognosis. Answer A is incorrect because grade 2 tumors are considered high grade in the 2 tier classification system. Answer D is incorrect because only immature neuroepithelium component is used for grading.
Comment Here
Reference: Teratoma - immature
Comment Here
Reference: Teratoma - immature