Table of Contents
Definition / general | Epidemiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Do HK. Histoplasma capsulatum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorfungihistoplasma.html. Accessed August 24th, 2025.
Definition / general
- Infection is caused by inhalation of airborne spores of Histoplasma capsulatum, a dimorphic saprophytic fungus found in soil contaminated with bird or bat feces
Epidemiology
- Highest incidence is in North America, particularly in the central states along the Mississippi River basin
- Histoplasma is endemic to Southeast U.S. (80% of this population may have positive intradermal histoplasmin skin test), Mexico, Africa, Asia
- Transmission of disease is by inhalation of spores that can be found in feces of bats, starlings (type of bird) and chickens; causes a primary pulmonary pneumonia
Clinical features
- There are several clinical manifestations of histoplasmosis:
- Acute pulmonary histoplasmosis: almost 90% patients have no symptoms
- Chronic pulmonary histoplasmosis: occurs mostly in patients with underlying lung disease
- Progressive disseminated histoplasmosis: occurs mostly in immunosuppressed patients
- Ocular histoplasmosis syndrome: eye disease, occurs in 1 - 10% of the patients
- Cutaneous histoplasmosis: erythema nodosum or erythema multiforme
- Pneumonia is self-limited in immunocompetent patients, but disseminates in immunocompromised (very young, very old, HIV+) to liver, spleen, bone marrow, nodes, lung, rarely to skin
- Disseminated disease: strongly associated with AIDS; patients have fever, weight loss, splenomegaly; variable cutaneous lesions
- Cutaneous lesions are nodules, papules, ulcers; less commonly macules, pustules or vesicles
Diagnosis
- Culture shows tan-white-brown wooly mold at 25 - 30 °C on Sabouraud dextrose agar
- Organisms have delicate, septate hyphae, 1 - 2 microns thick, with large rough walled macroconidia 5 - 15 microns
- Reverts to yeast at 37 °C on sheep blood agar
- Yeast is 2 - 4 microns, budding, single nuclei, round / oval with thin rigid walls
Case reports
- 5 year old healthy child with atypical variant causing disseminated cutaneous disease (Rev Inst Med trop S Paulo;1999:41:195)
- 27 year old woman with multiple cutaneous lesions (Arch Pathol Lab Med 2004;128:e15)
- 33 year old HIV+ man with recurrent disseminated disease (Arch Pathol Lab Med 2001;125:571)
Treatment
- Most with minimal disease require no treatment
- Moderate to severe cases require antifungal drugs, usually Itraconazole x 9 months in immunocompetent patients, Itraconzazole followed by IV amphotericin B in immunosuppressed patients
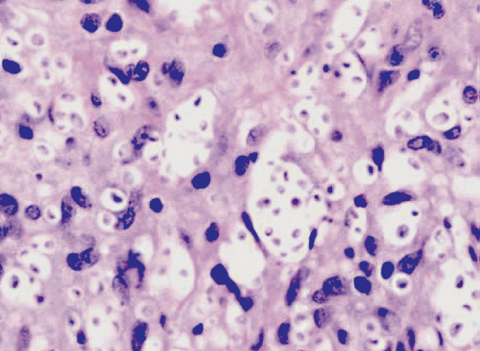
Microscopic (histologic) description
- Isolated intracellular organisms and large aggregates surrounded by chronic inflammatory cells and fibroblasts (but no neutrophils or eosinophils); also epithelioid granulomas with variable caseation
- May be narrow based budding of spores
Microscopic (histologic) images
Molecular / cytogenetics description
- PCR probes are now available
- Best diagnostic test is the urinary ELISA
Differential diagnosis
- Aspergillosis
- Blastomycosis
- Carcinoid lung tumors
- Chlamydial pneumonia
- Coccidioidomycosis
- Legionella pneumonia
- Lymphoma
- Mycoplasma pneumonia
- Pancoast tumor (tumors at extreme apex of either lung in the superior sulcus)
- Pneumocystis carinii
- Pneumonia - bacterial, fungal or viral
- Sarcoidosis
- Tuberculosis
Additional references