Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Gagné A, Joubert P. Typical carcinoid tumor / neuroendocrine tumor, grade 1. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumorcarcinoid.html. Accessed September 1st, 2025.
Definition / general
- Pulmonary carcinoids are well differentiated neoplasms, with neuroendocrine differentiation further divided into typical and atypical carcinoids (neuroendocrine tumors grade 1 and 2)
- Classification is based on mitotic count per 2 mm2 and the presence / absence of necrosis (Ki67 proliferative index is currently not recommended to distinguish between typical and atypical carcinoids)
Essential features
- Typical carcinoids are classified according to a mitotic count < 2 per 2 mm2, the absence of necrosis and a tumor size > 0.5 cm
- Histologic features include neuroendocrine growth pattern and monotonous tumor cells with salt and pepper chromatin and inconspicuous nucleoli and moderate to abundant eosinophilic cytoplasm
- Treatment is based on surgical resection; prognosis is excellent
Terminology
- Not recommended: well differentiated lung neuroendocrine tumor
- G1 - G3 neuroendocrine neoplasm classification is not currently applied to pulmonary carcinoids (Mod Pathol 2018;31:1770)
- Neuroendocrine tumor (NET) terminology has been added, according to the unifying nomenclature proposed by the WHO classification of tumors group
ICD coding
- ICD-O: 8240/3 - typical carcinoid
- ICD-10: D3A.090 - benign carcinoid tumor of the bronchus and lung
- ICD-11: 2C25.4 & XH9LV8 - carcinoid or other malignant neuroendocrine neoplasms of bronchus or lung & neuroendocrine tumor, grade 1
Epidemiology
- < 1% of all lung cancers and 2% of resected lung tumors (Histopathology 2018;72:142)
- Usually adults but also most common lung tumor of children (Cancer 2008;113:5)
- More frequent
- Patients aged < 60 years
- Female
- Caucasian
- Risk factors
- Family history
- Mutation in MEN1 gene
- Unrelated to smoking (Arch Pathol Lab Med 2010;134:1628)
Sites
- Anywhere from the trachea to the distal bronchioles
- Central airways (85%), mostly main and lobar bronchi > peripheral airways (15%) (Cancer 2008;113:5)
- Central
- Most common type; usually slow growing and associated with obstruction, infection, hemorrhage
- 5% metastasize, usually to regional lymph nodes
- Rarely distant osteoblastic metastases to bone
- 10 year survival: 70%
- Cytology (bronchoalveolar lavage [BAL] and brushings) often negative since tumor is covered by mucosa
- Peripheral
- Arise in peripheral lung, often beneath the pleura
- Usually asymptomatic and incidental
- Excellent prognosis
- Rare nodal metastases are usually cured by excision
Etiology
- Unclear
- May arise in the context of diffuse idiopathic pulmonary neuroendocrine cell hyperplasia and tumorlets
- No relation to high grade pulmonary neuroendocrine carcinoma (Mod Pathol 2018;31:1770)
Clinical features
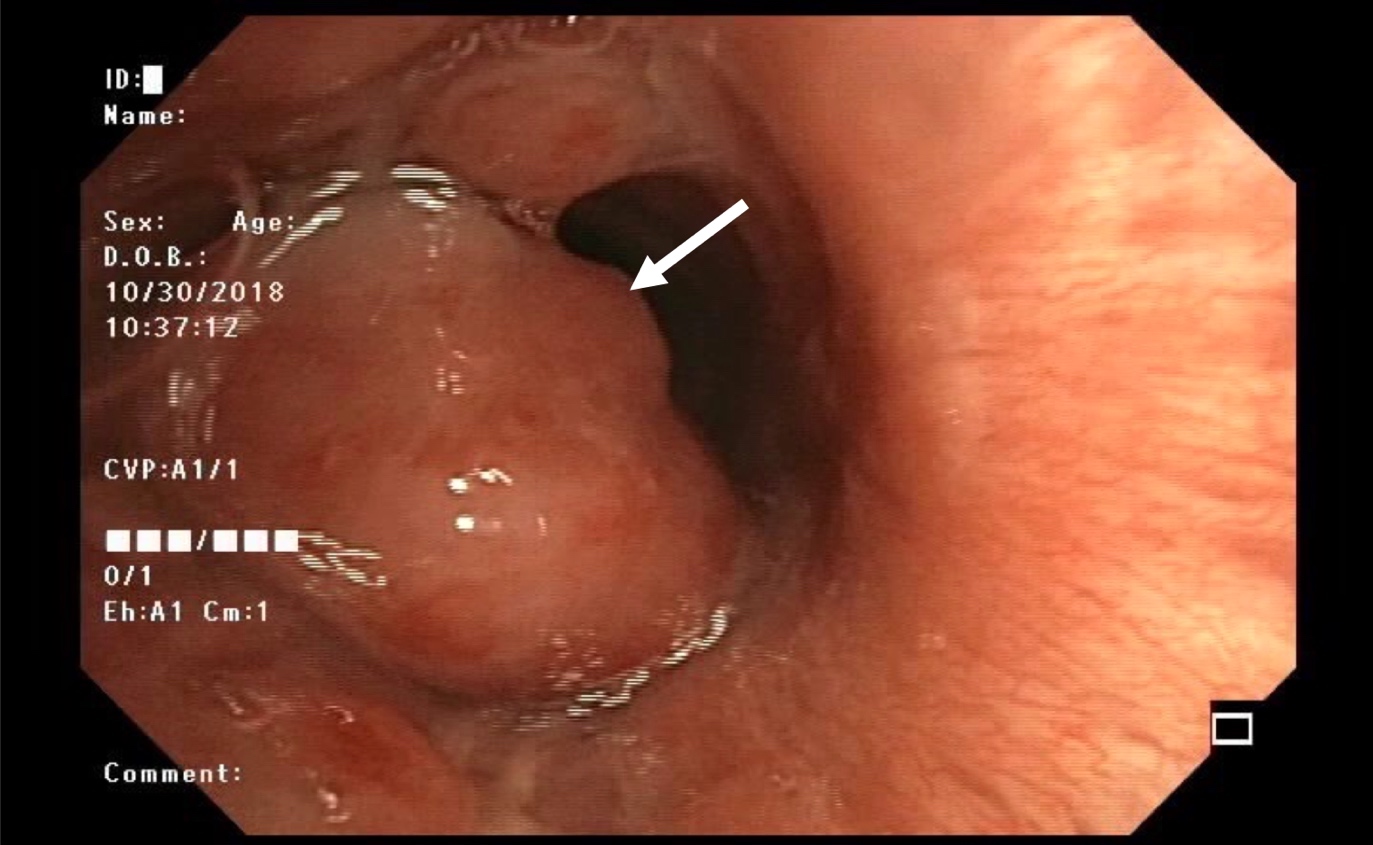
- Mostly due to tumor location (Chest 2017;151:1141)
- Peripheral carcinoids are commonly asymptomatic
- Centrally located carcinoids may present with dyspnea, cough, wheezing, hemoptysis, recurrent infection and pneumonia due to airway obstruction
- Paraneoplastic syndromes are uncommon and usually present in the setting of liver metastases (CMAJ 2017;189:E398)
- Carcinoid syndrome (< 2%): flushing, diarrhea, valvular disease
- Cushing syndrome (4%)
- Other rare endocrine syndromes
- Bronchoscopy shows polypoid endobronchial lesion in central airway
Diagnosis
- Diagnosis of carcinoid can be made on biopsy or cytology specimen but the distinction between typical and atypical carcinoid usually requires a surgical specimen, unless necrosis or mitoses are seen (Ann Oncol 2015;26:1604)
Laboratory
- Increase in plasma chromogranin A can be used but has limited specificity (Ann Oncol 2015;26:1604)
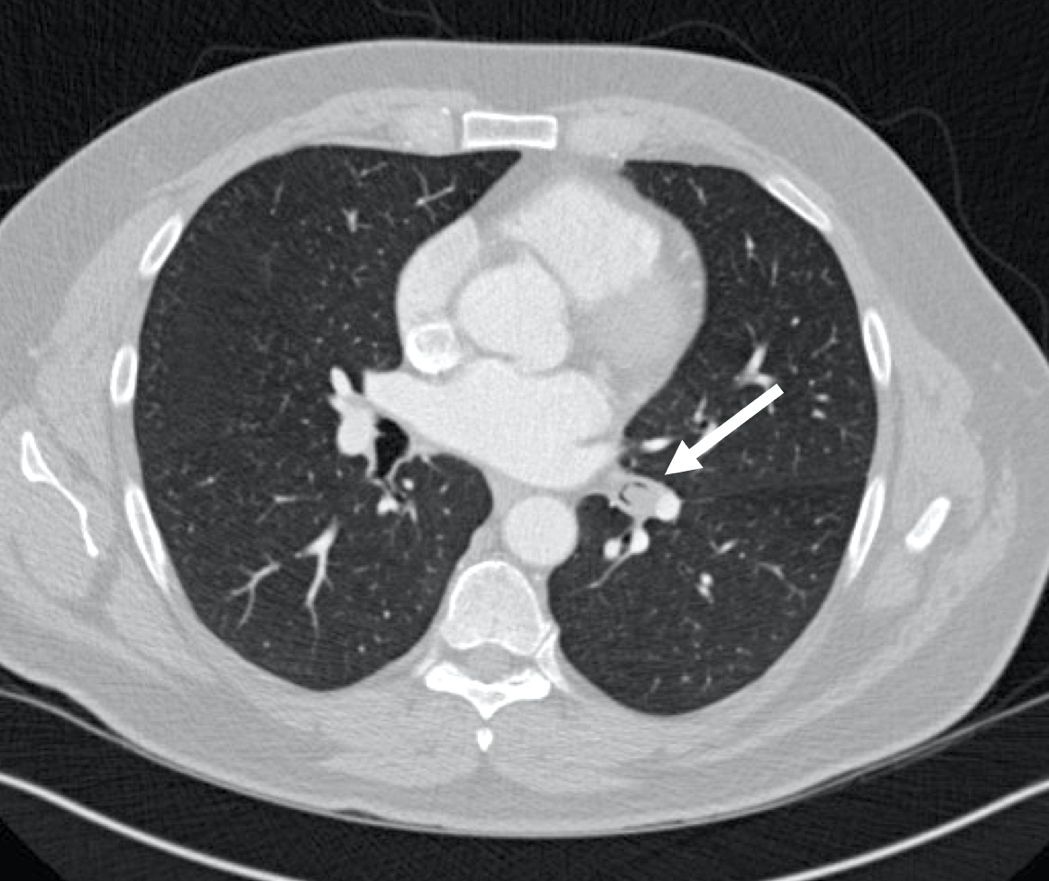
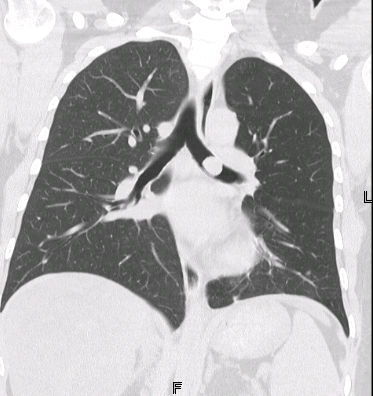
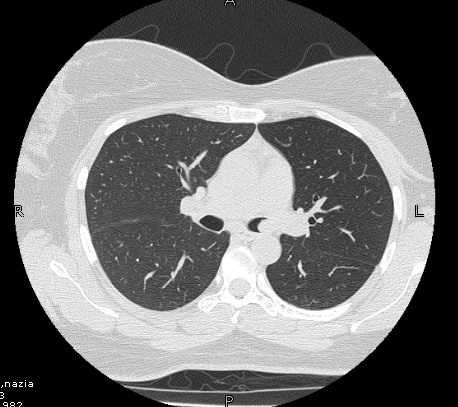
Radiology description
- Chest CT scan
- Lobulated and well circumscribed nodule implicating major bronchi
- Obstruction signs (atelectasis, bronchiectasis) can be seen (AJR Am J Roentgenol 2011;197:1073)
- Positron emission tomography (PET) scan: low to moderate uptake (mean standardized uptake value [SUV]: 3.4)
Radiology images
Prognostic factors
- 5 year survival: 90% (Arch Pathol Lab Med 2010;134:1628)
- Lymph node metastasis: 9%
- Distant metastases at time of diagnosis: 3 - 5%, mainly liver and bone
- Prognosis related to
- TNM staging (Am J Surg Pathol 2019;43:1291)
- Spread through air spaces: presence linked to a worse prognosis (J Thorac Oncol 2019;14:1583, Virchows Arch 2019;475:325)
- Ki67 immunostaining: utility remains controversial (Arch Pathol Lab Med 2018;142:947)
Case reports
- 25 year old woman with a postpneumonectomy-like syndrome (BMC Pulm Med 2019;19:44)
- 30 year old woman with hemoptysis and fever (Case #266)
- 30 year old woman with metastatic disease 7 years following surgery, which presented as a subcutaneous nodule (Medicine (Baltimore) 2018;97:e9415)
- 45 year old woman with MEN1 syndrome presenting with a typical carcinoid tumor in the lung and an atypical carcinoid tumor in the thymus (Ann Thorac Cardiovasc Surg 2018;24:147)
- 74 year old woman with pure ground glass opacity on chest high resolution CT (Surg Case Rep 2017;3:108)
Treatment
- Surgical approach is the primary therapy for localized and locoregional resectable disease (NCCN Guidelines: Neuroendocrine and Adrenal Tumors [Accessed 25 April 2023])
- Lack of consensus for unresectable and metastatic disease with options including somatostatin analogues (octreotide), targeted therapy (everolimus), interferon, chemotherapy and peptide receptor radionuclide therapy (Chest 2017;151:1141)
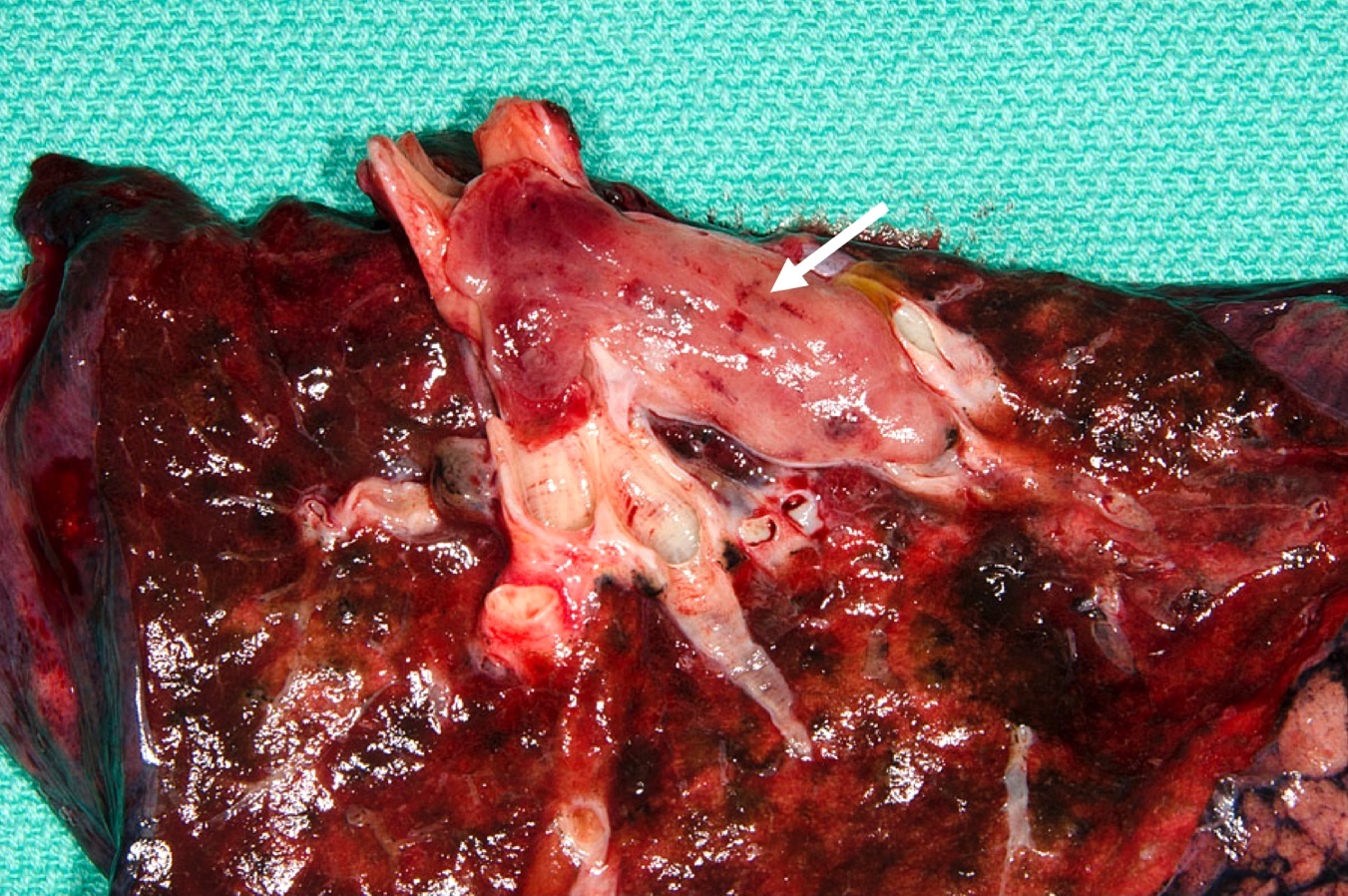
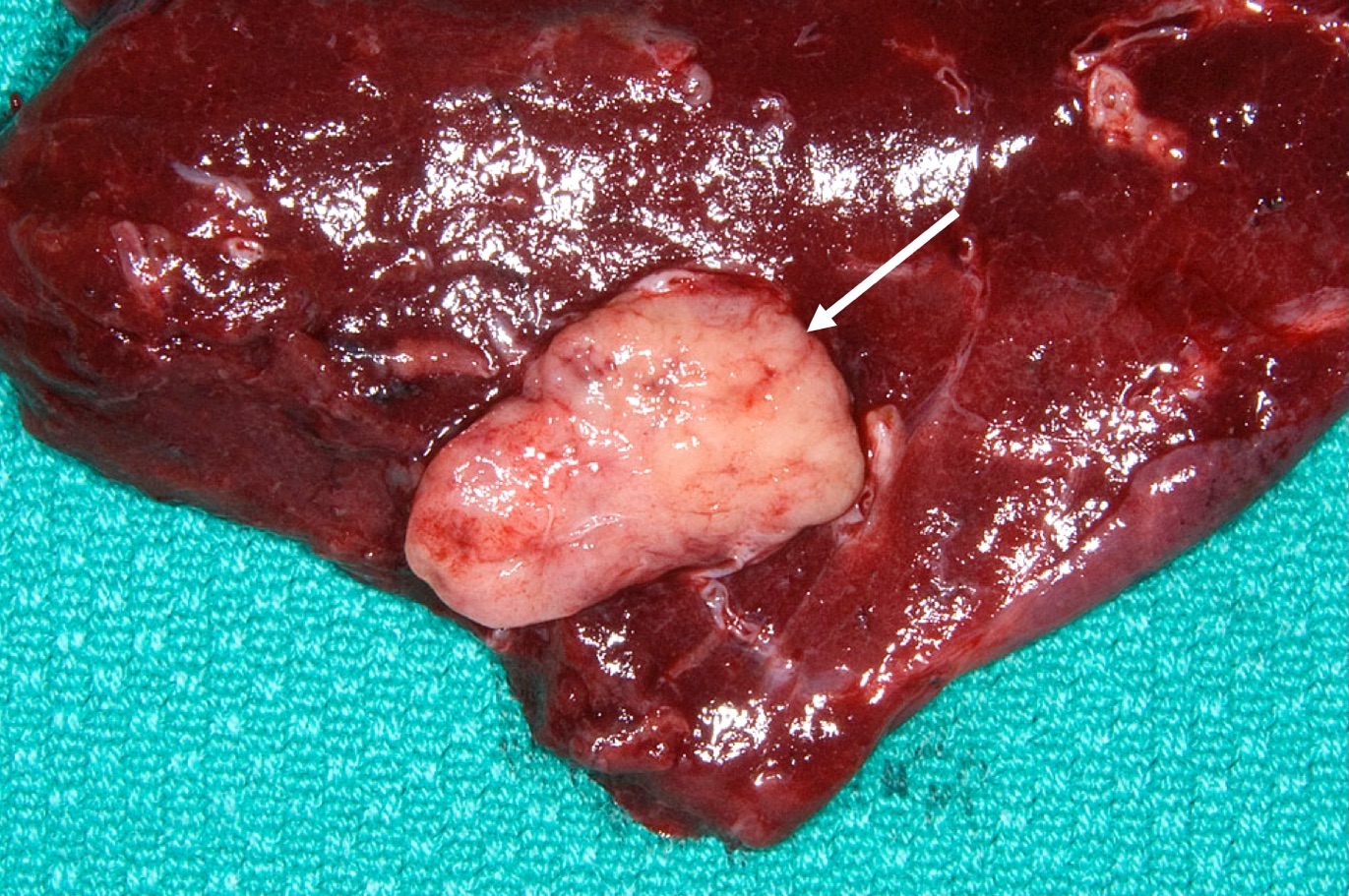
Gross description
- Well circumscribed, round to oval tan colored tumors
- Localization
- Frequently in bronchial lumen, sessile or pedunculated with partial or complete obstruction of the lumen
- Peripheral tumors may not be evidently located in airways
- Size range: 0.5 - 9.5 cm
- Reference: Lung Cancer Int 2015;2015:545601
Gross images
Frozen section description
- Homogenous population of cells with mild atypia
- Organoid pattern helps to distinguish from inflammatory cells
- Fine chromatin
- Mitoses are rarely seen on frozen section
- Hyalinization of the stroma and the presence of blood vessels may help to distinguish from carcinoma
- Reference: Hum Pathol 2009;40:1
Frozen section images
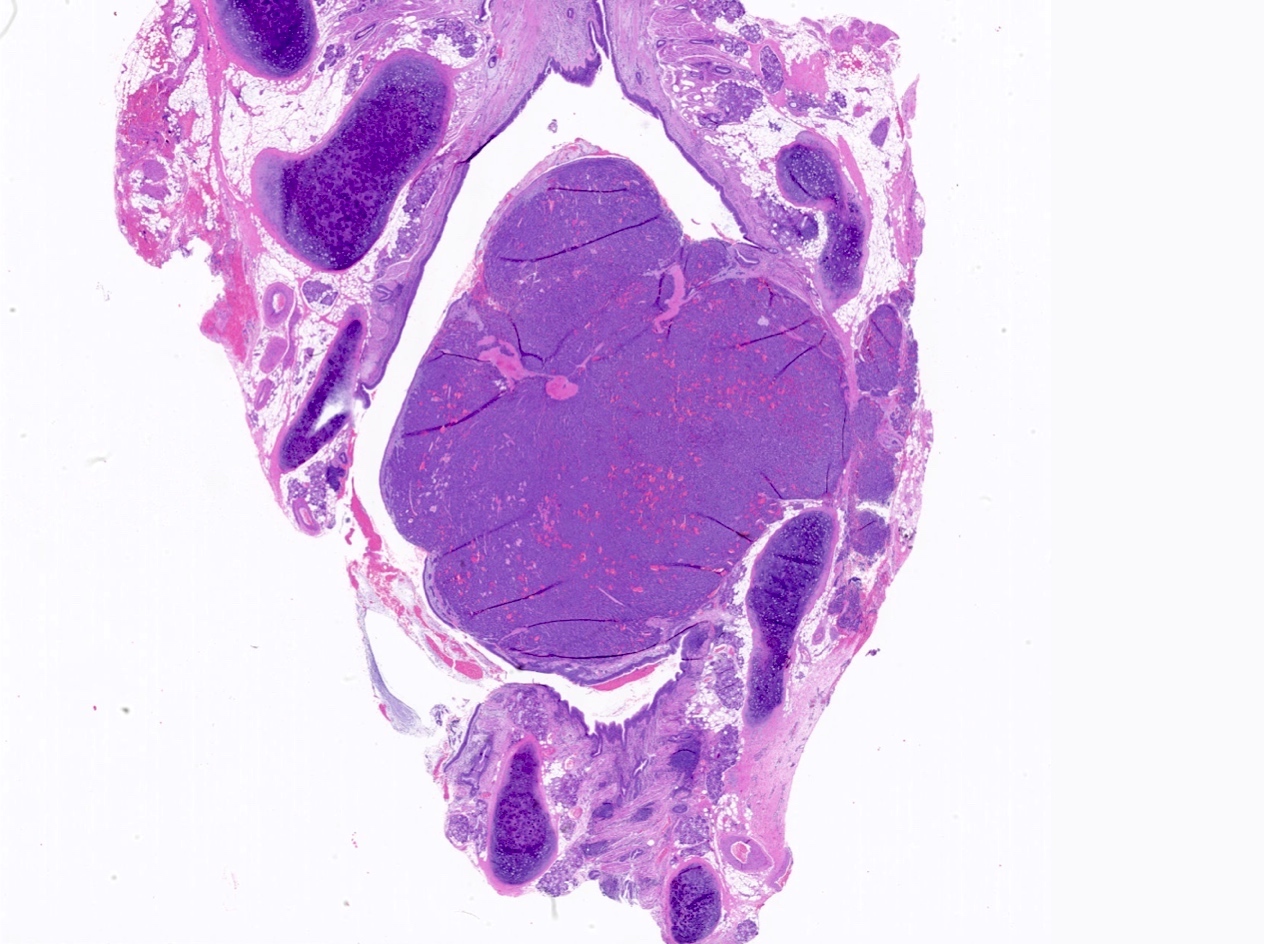
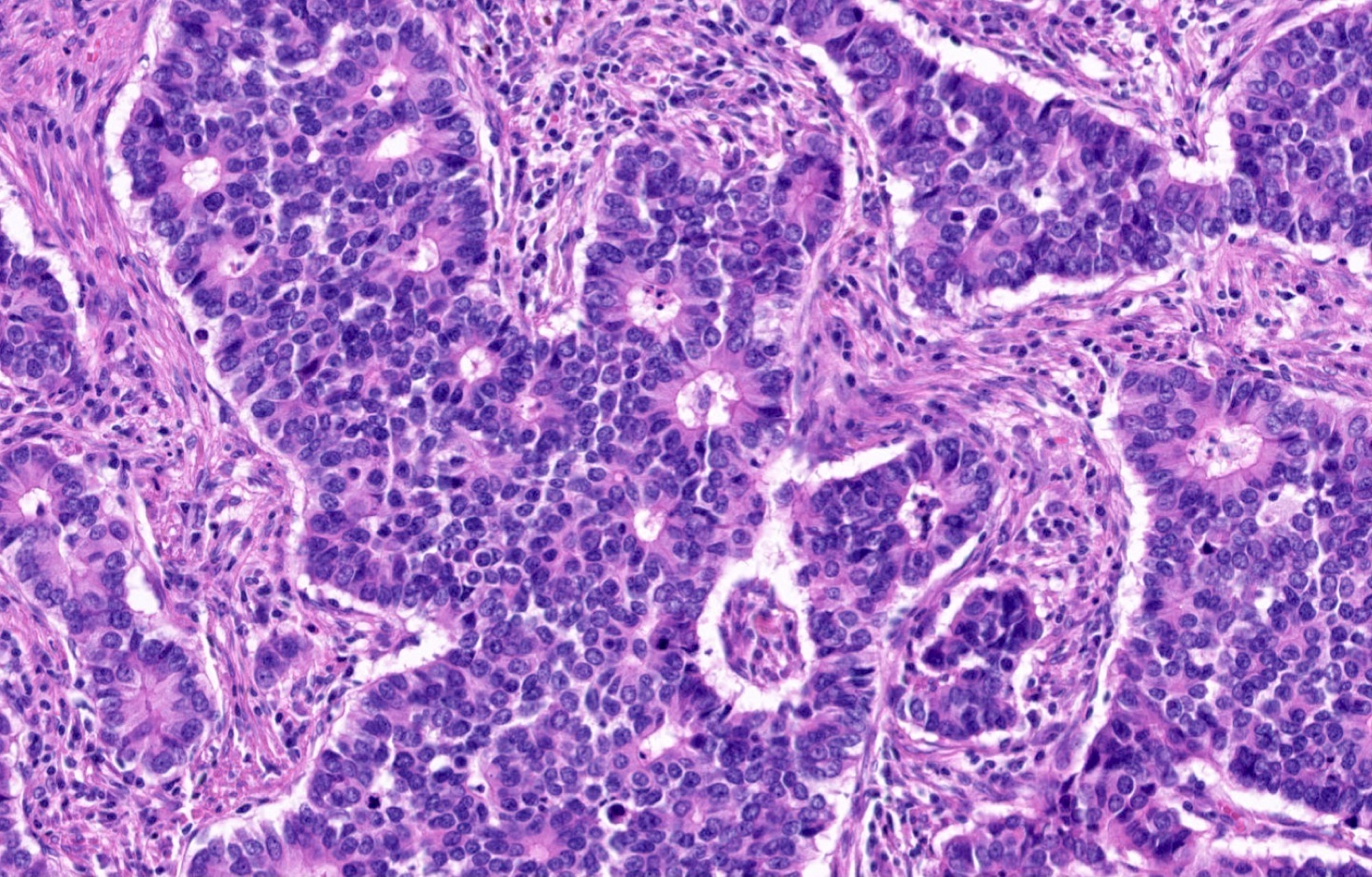
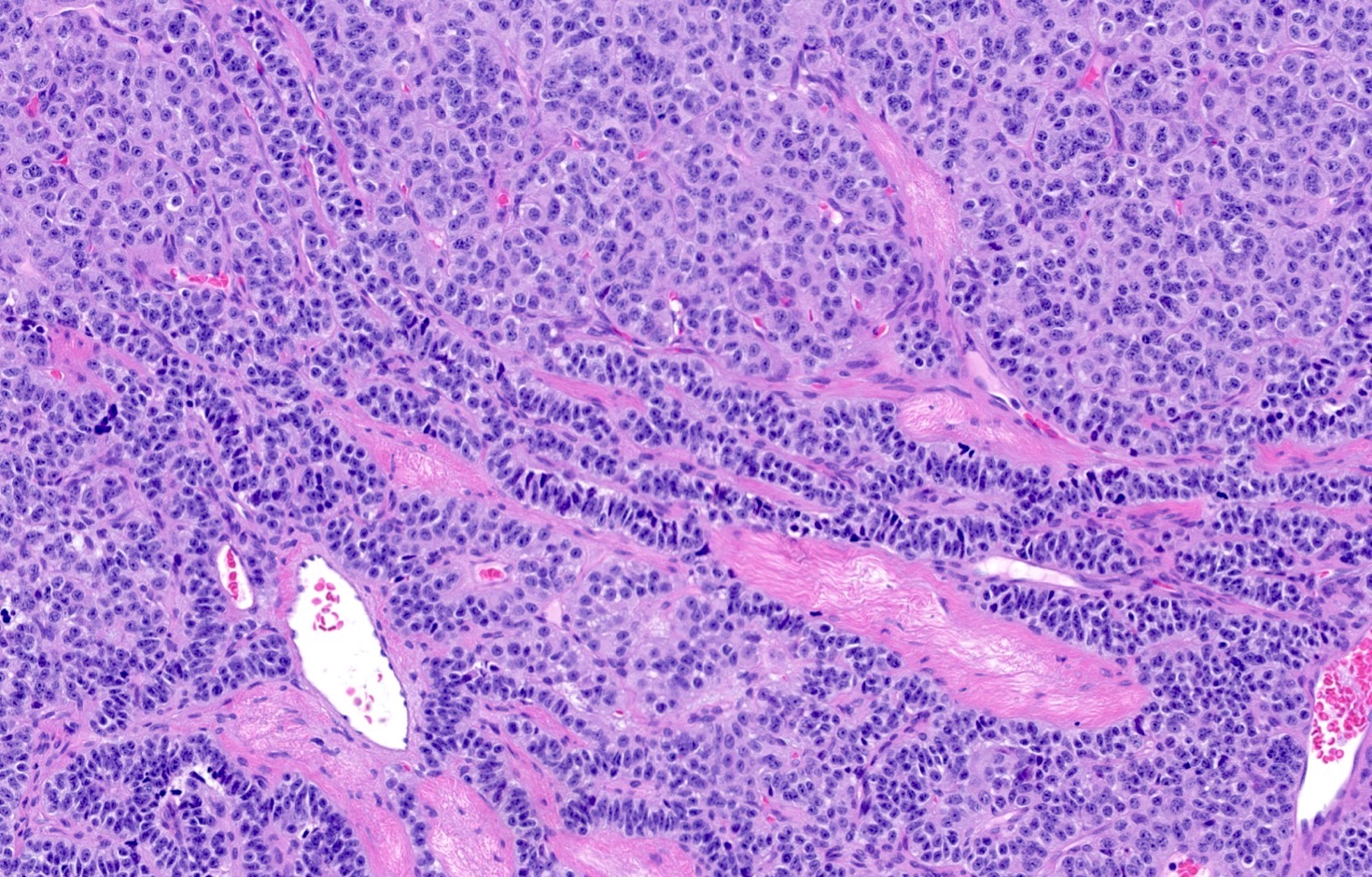
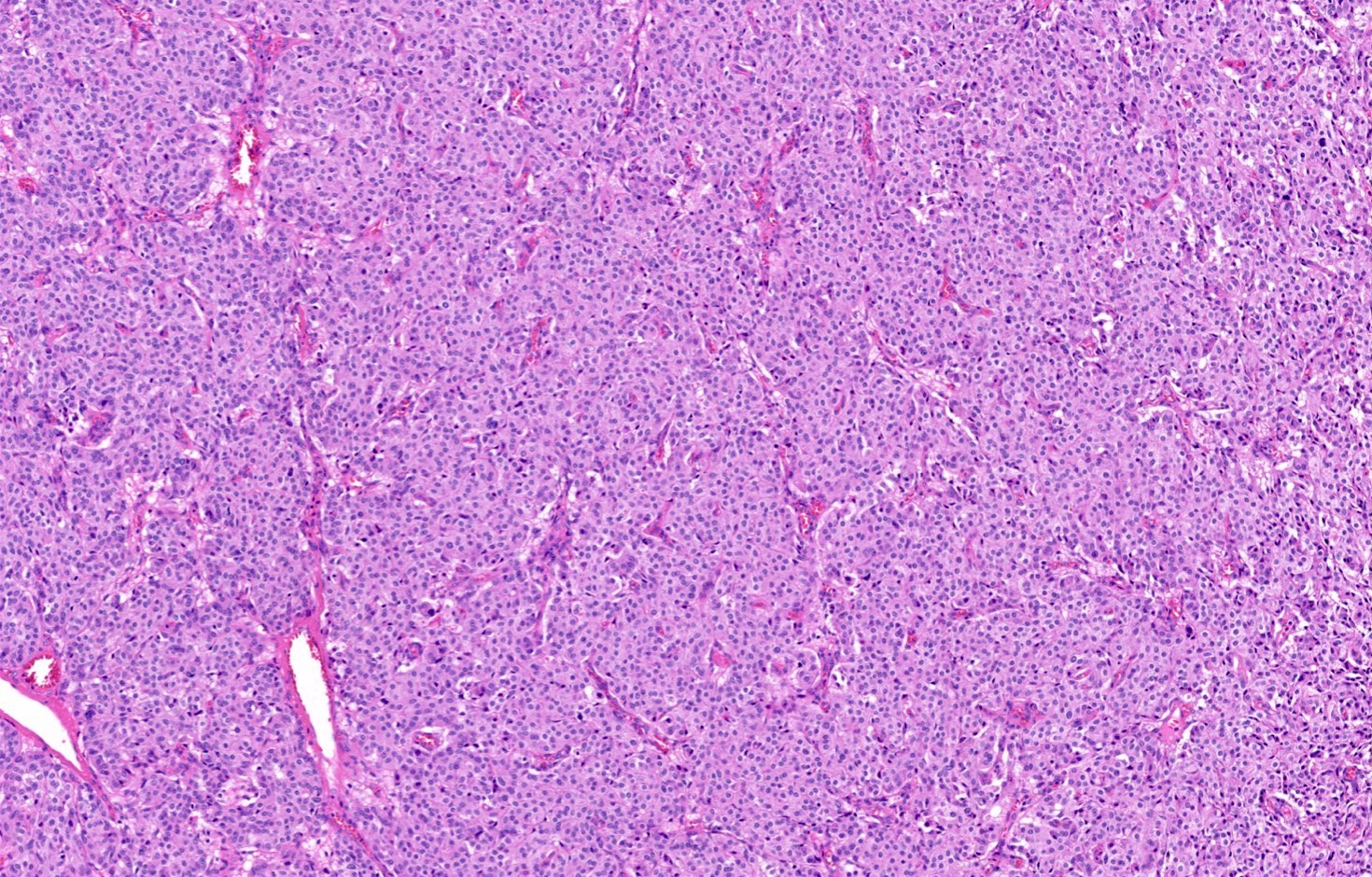
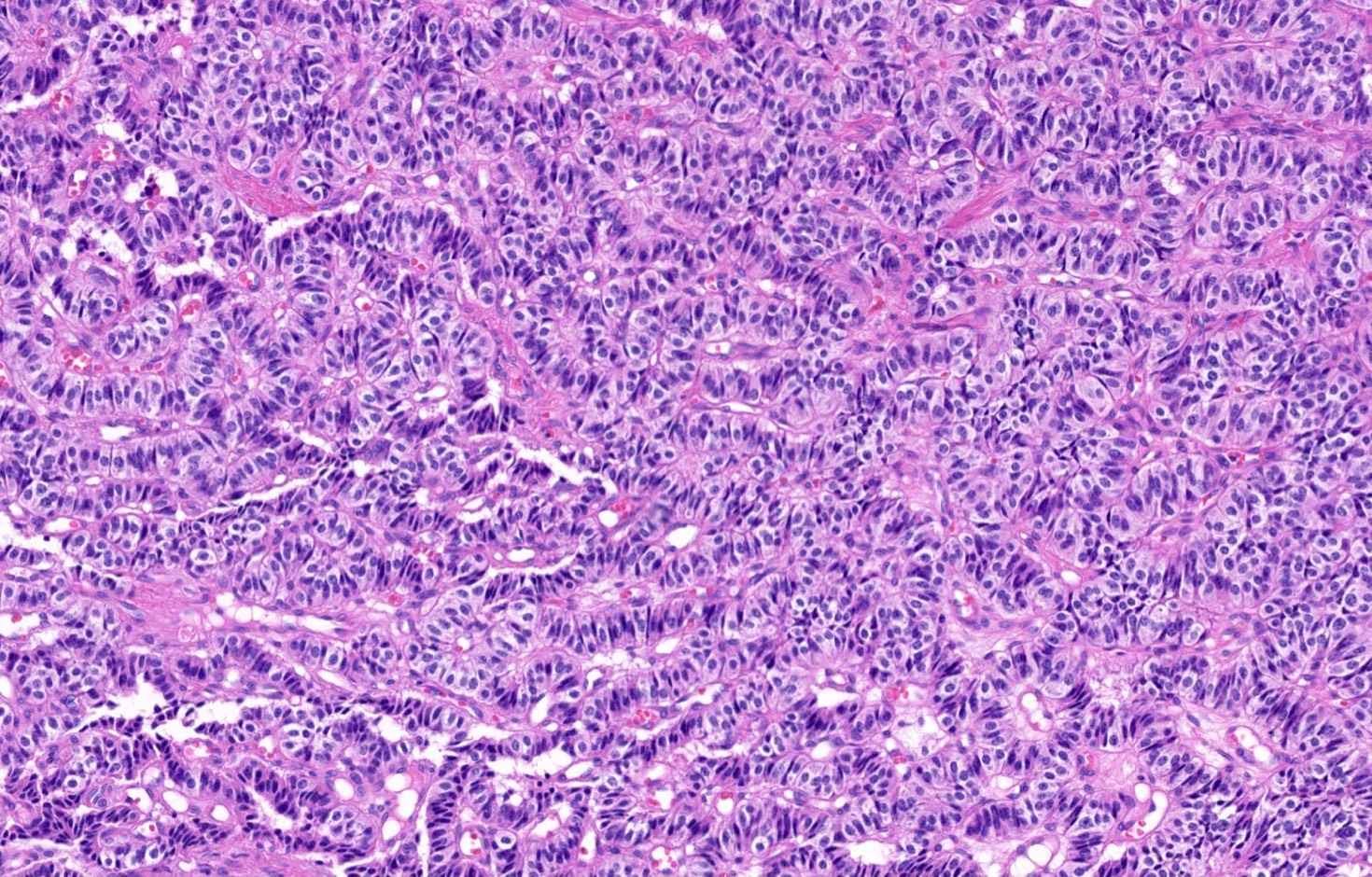
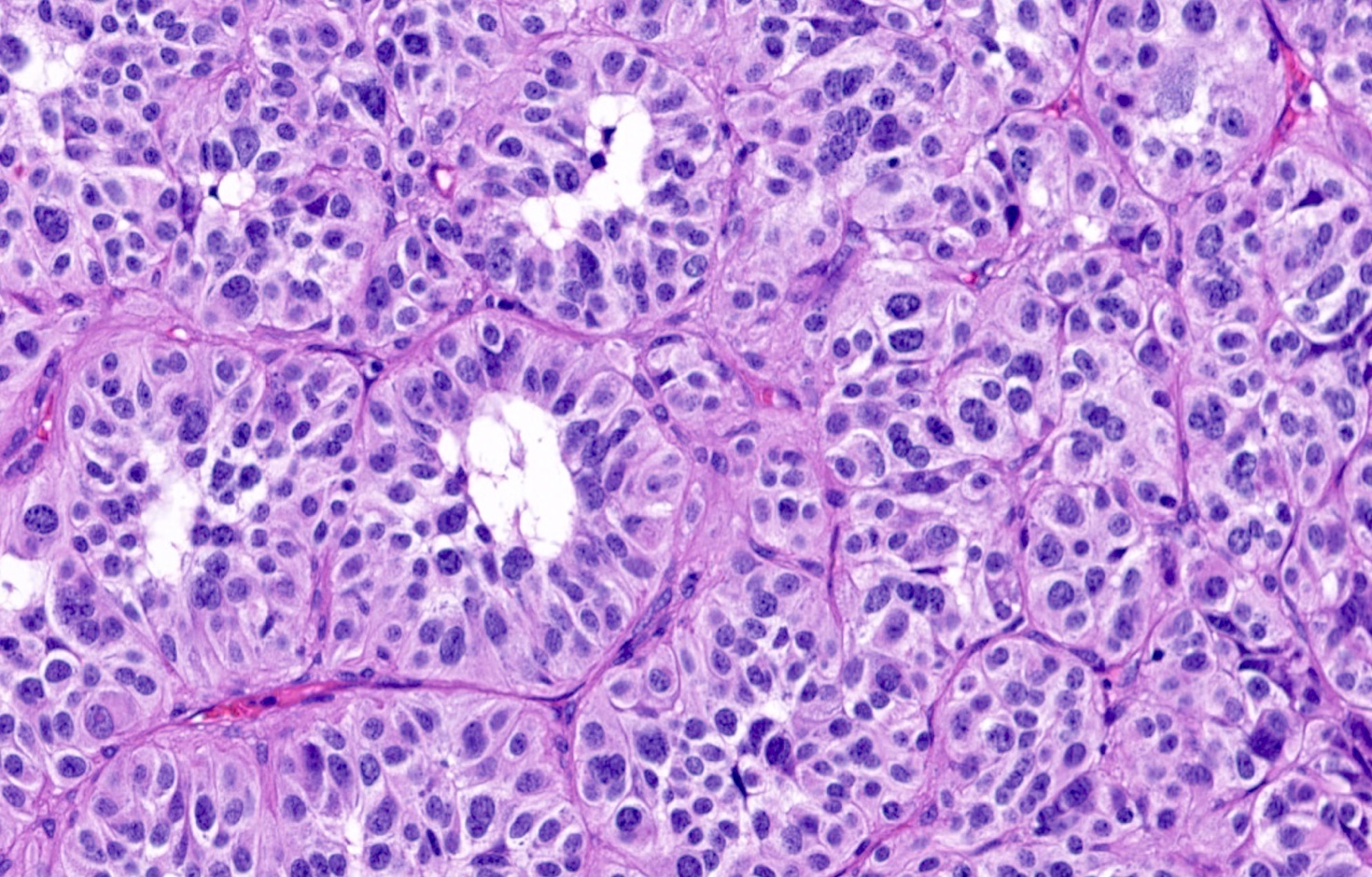
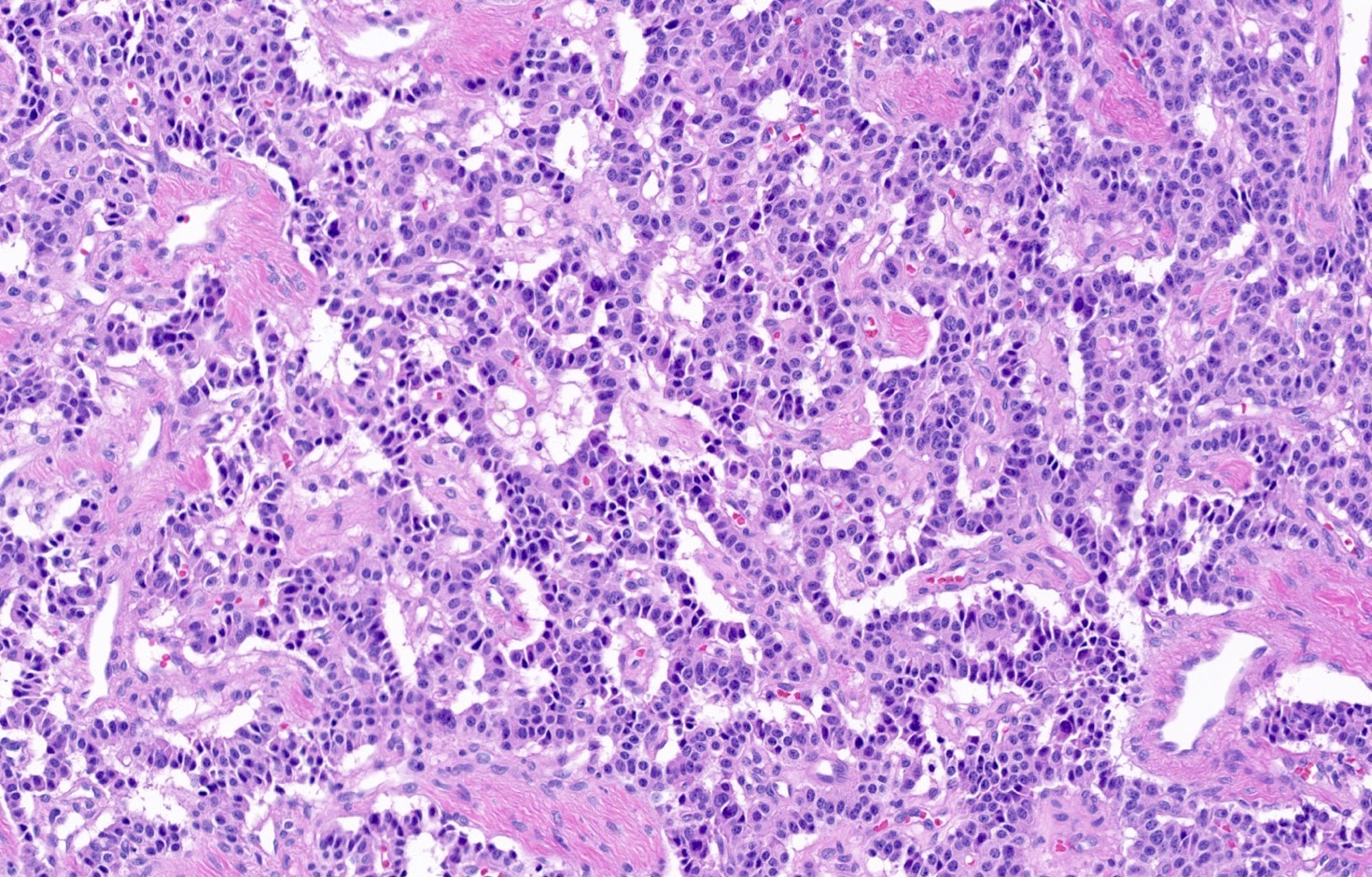
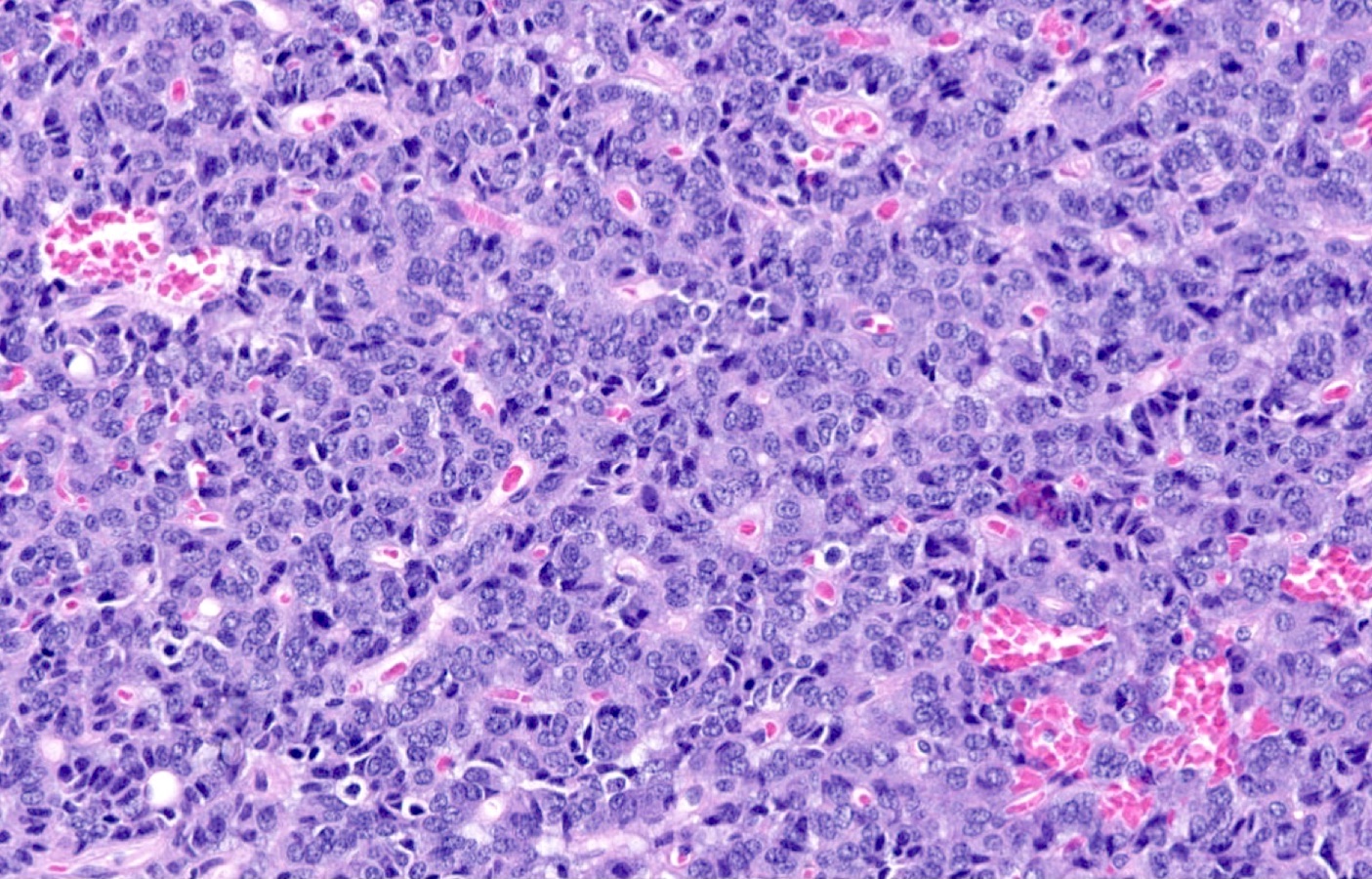
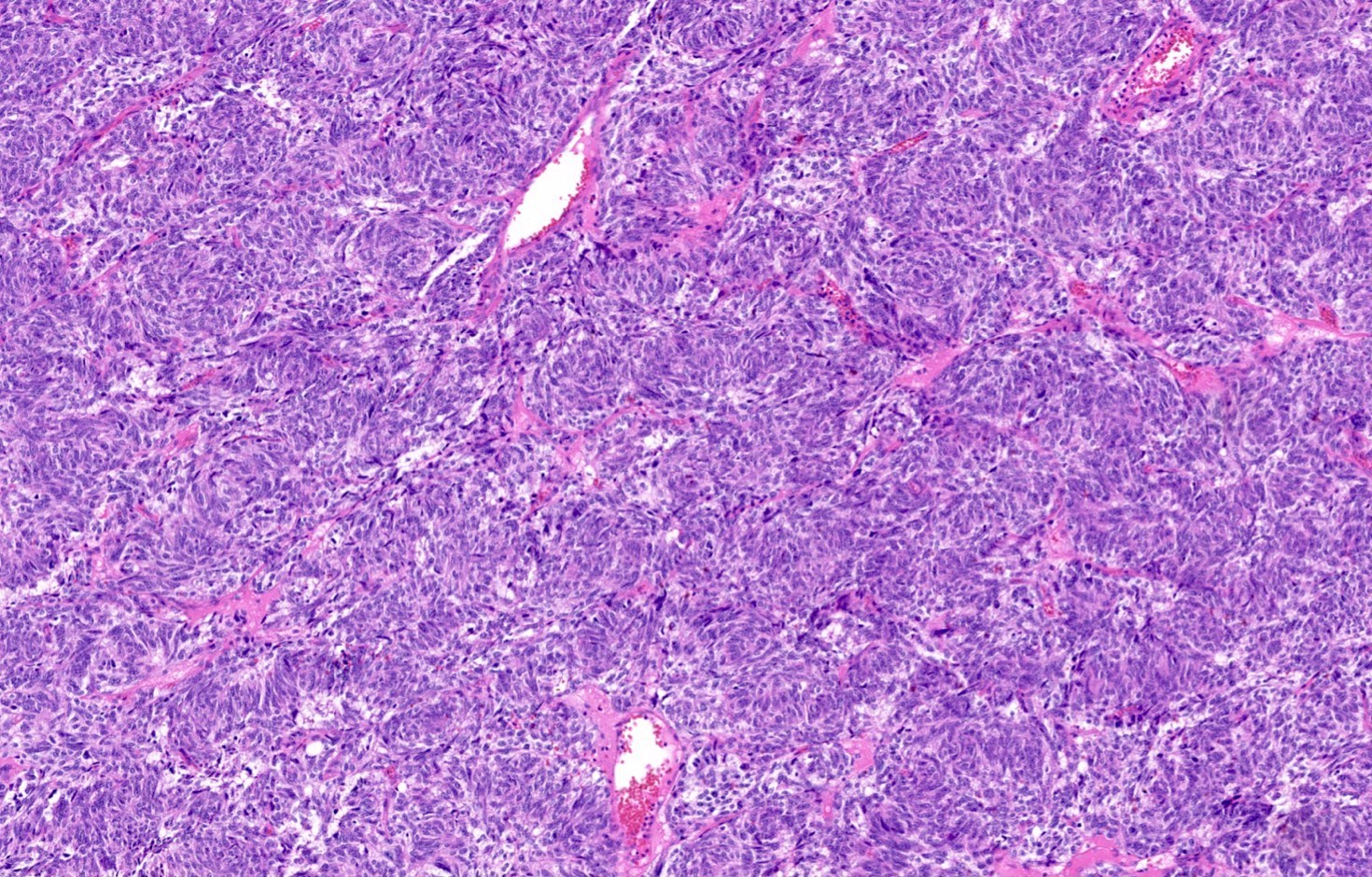
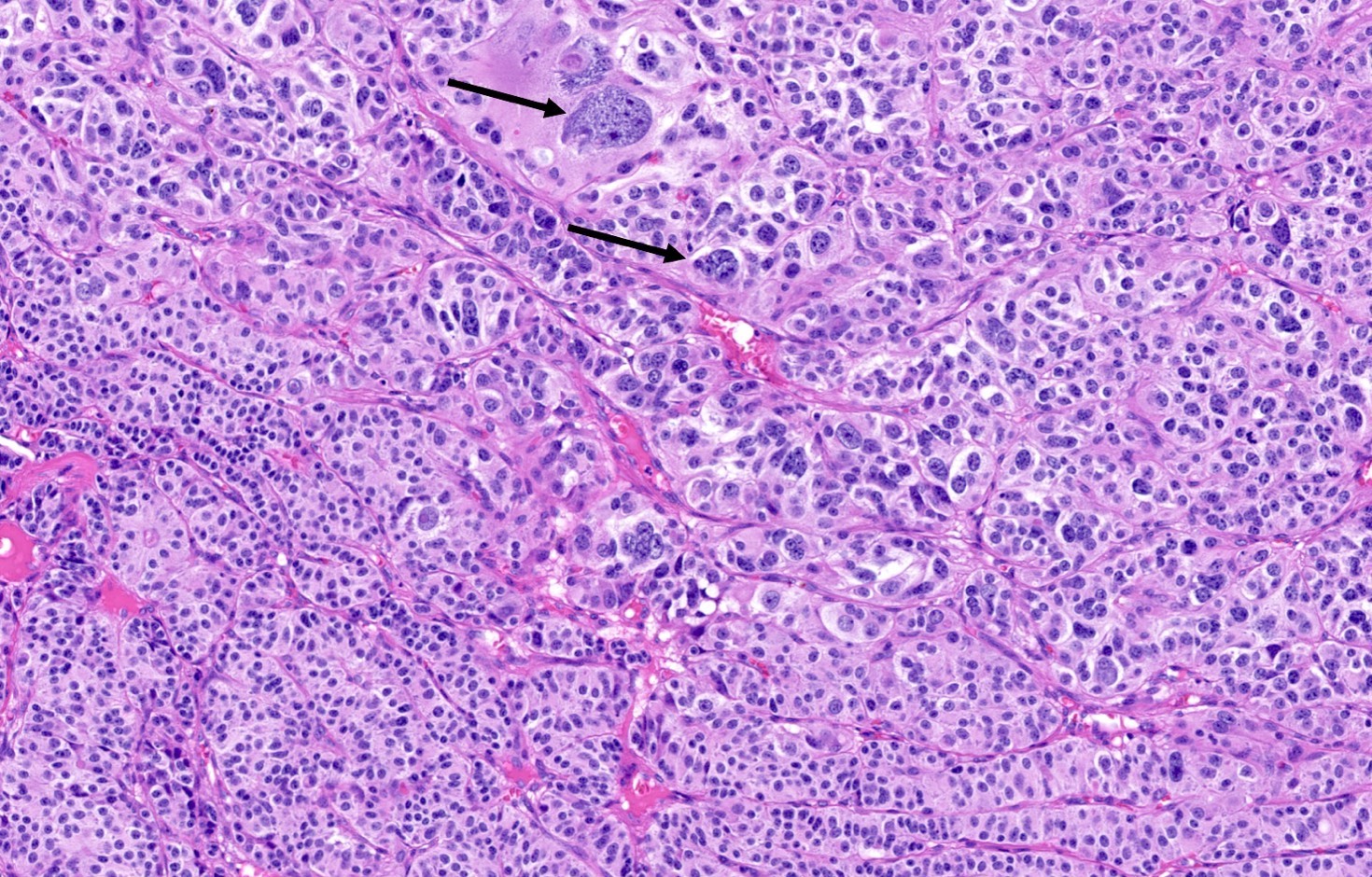
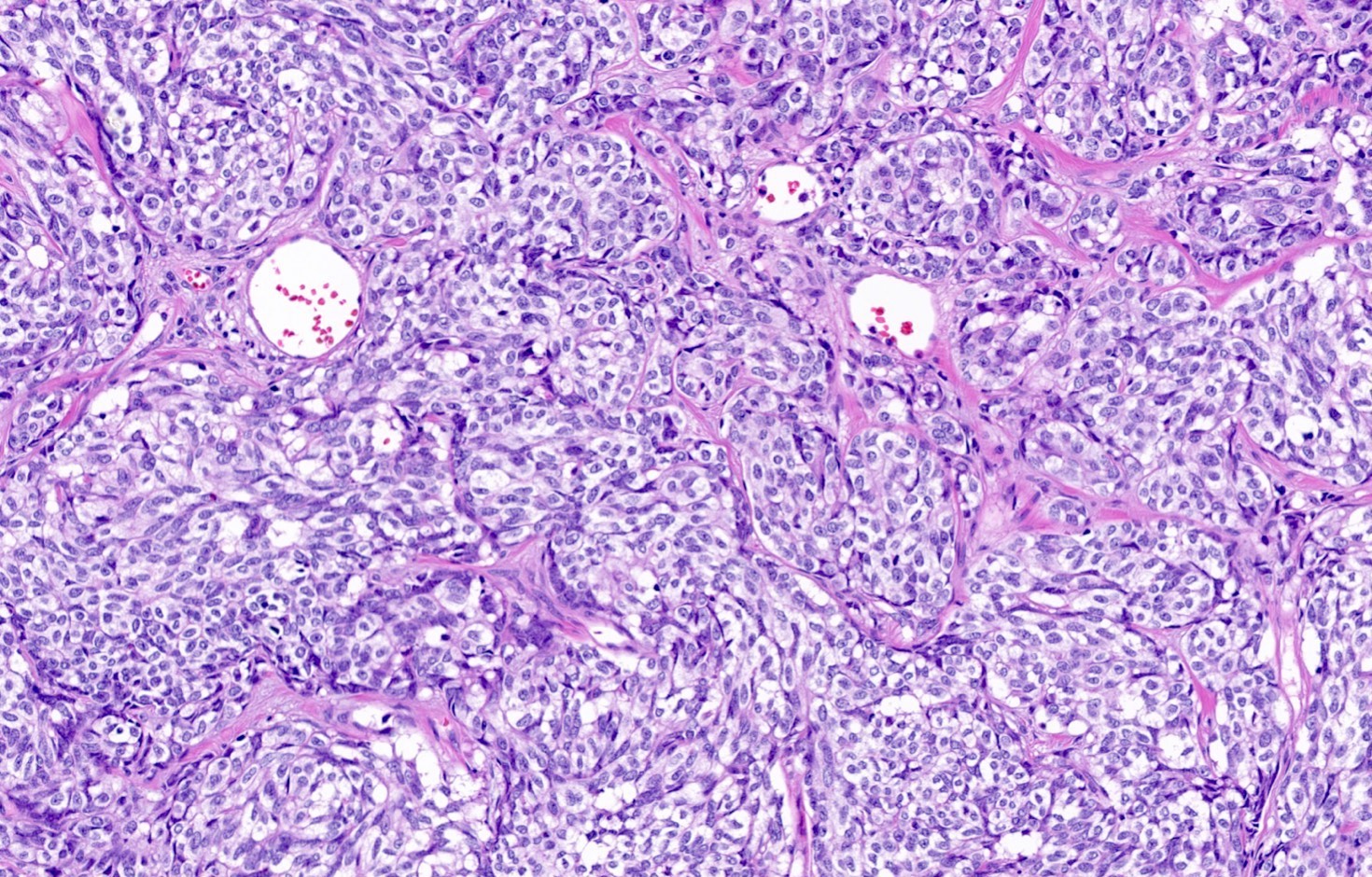
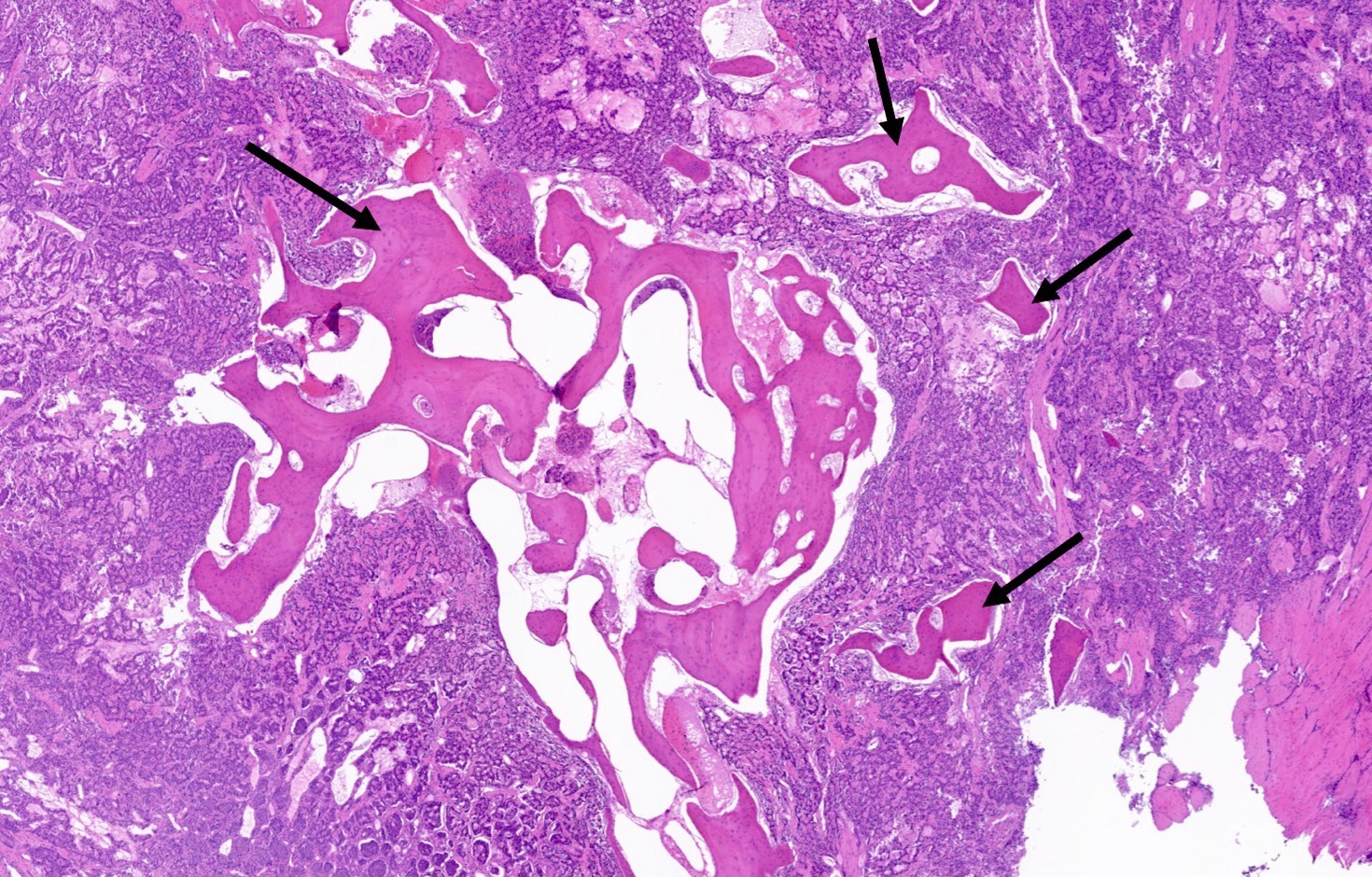
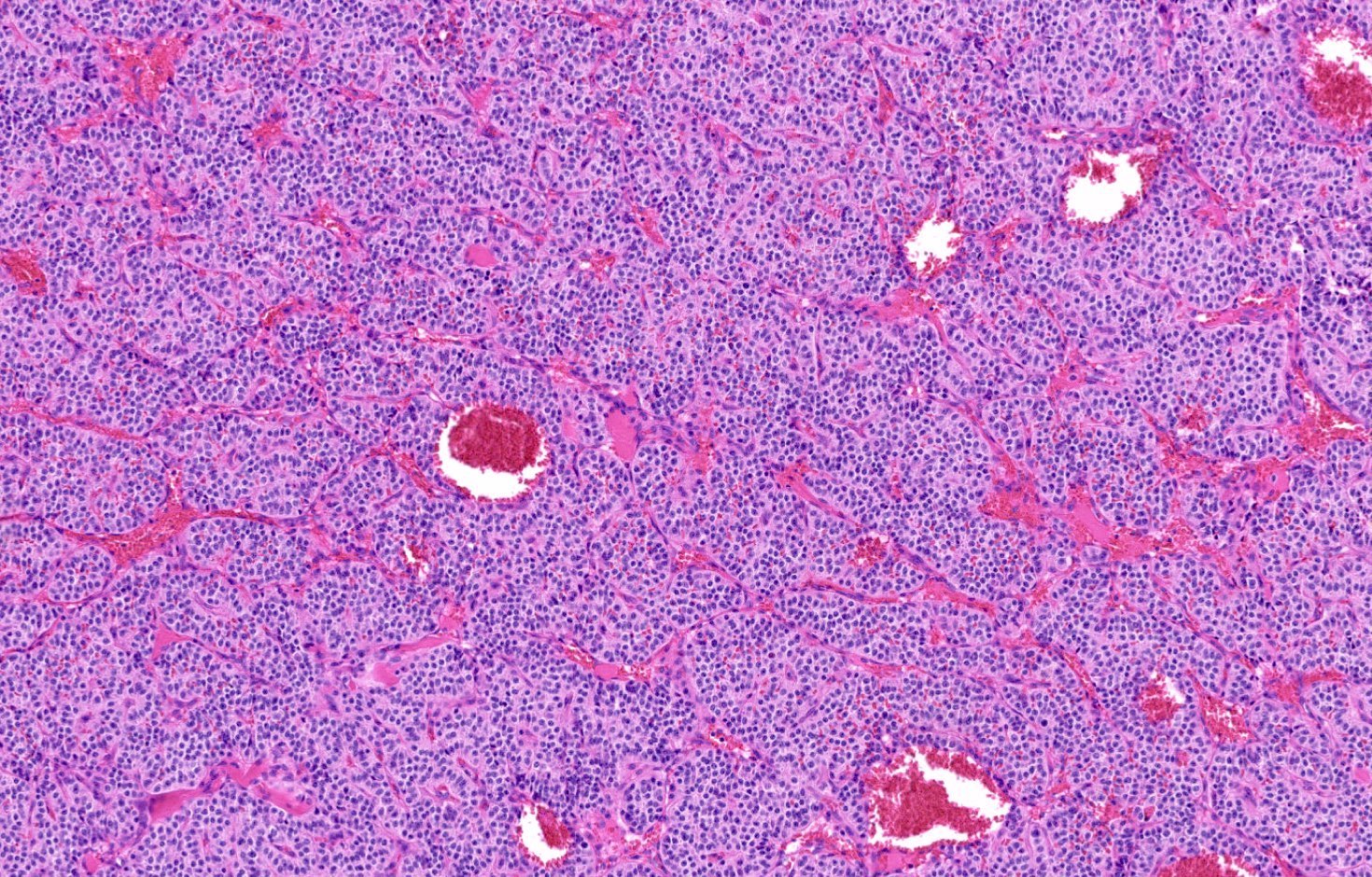
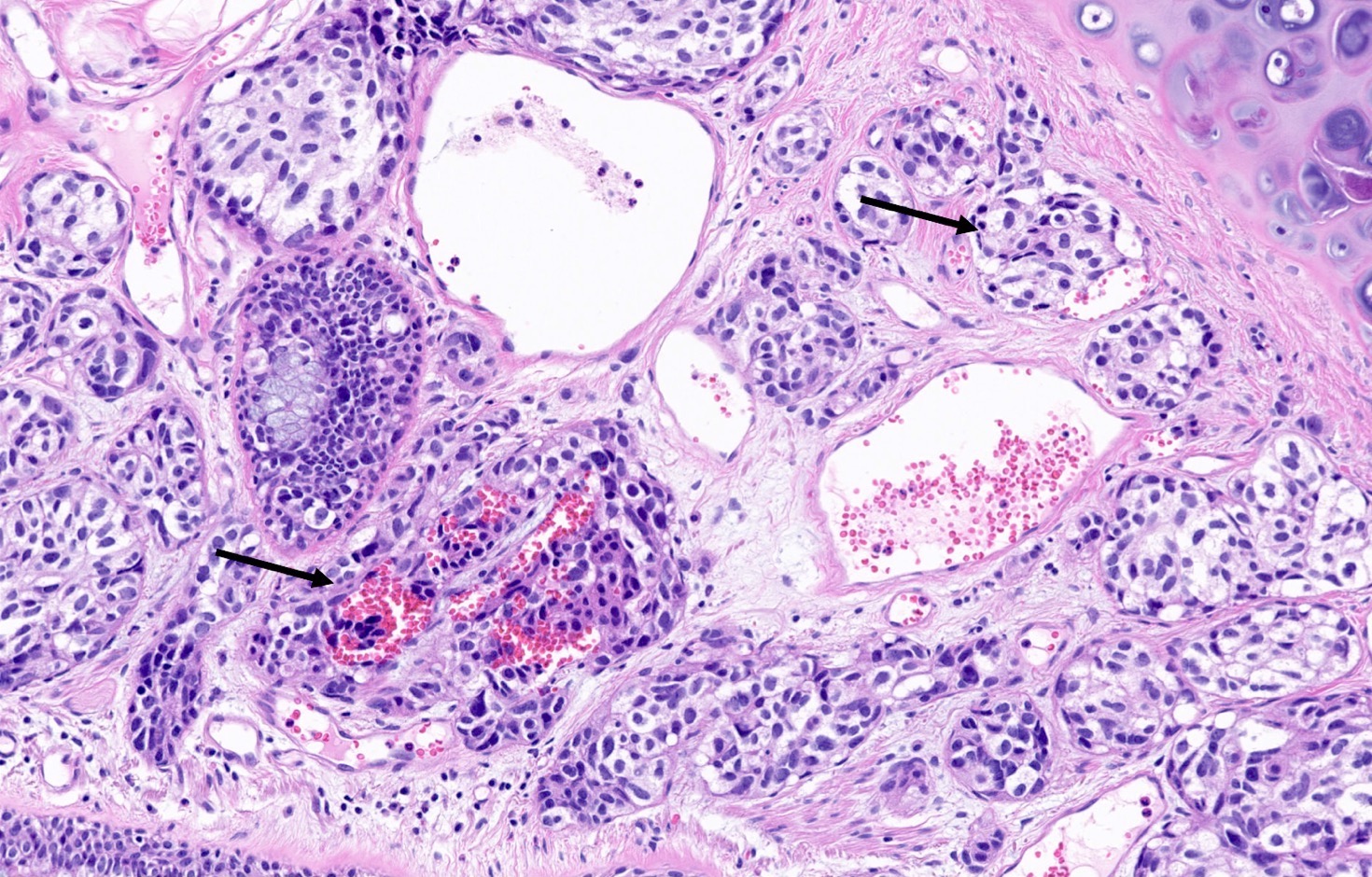
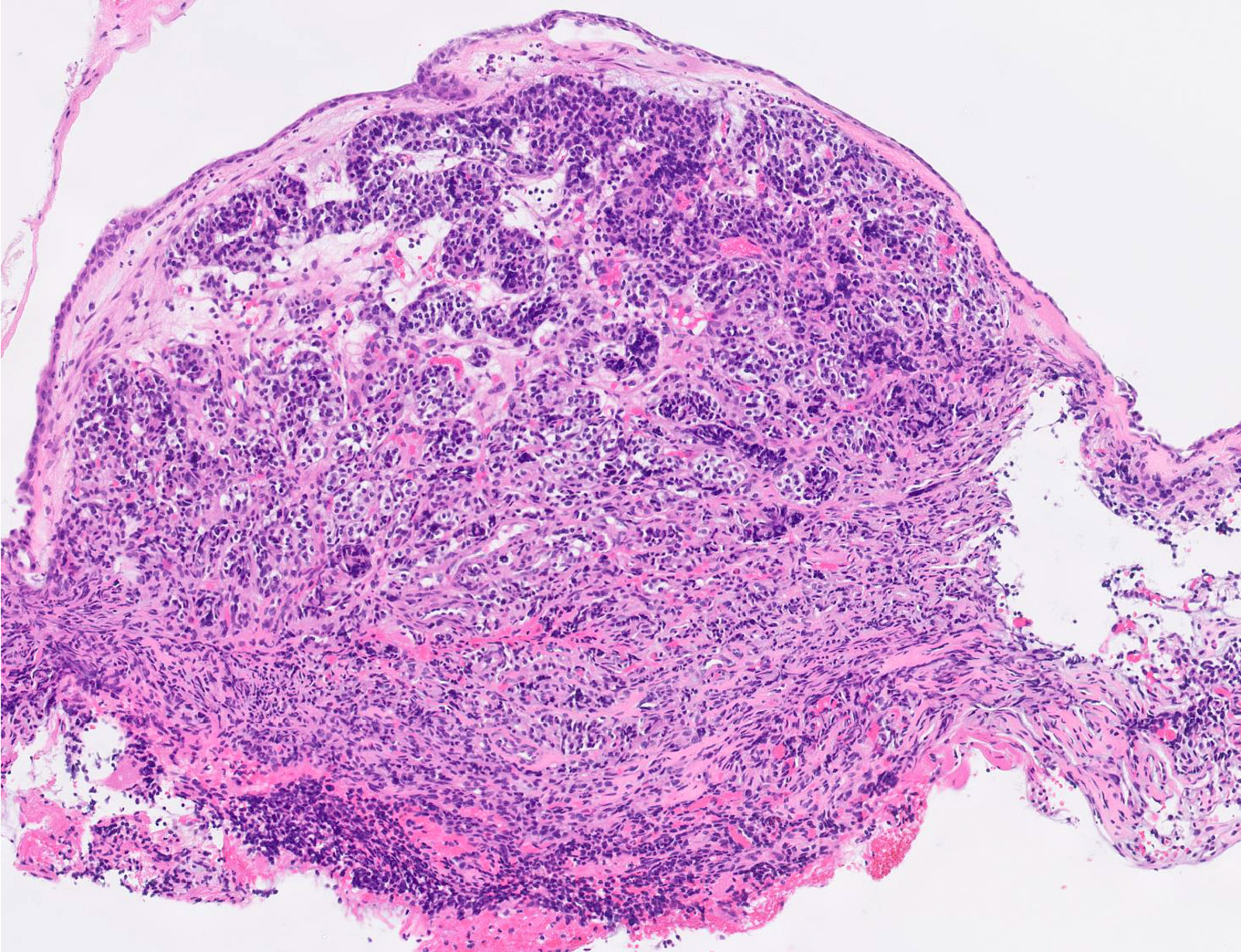
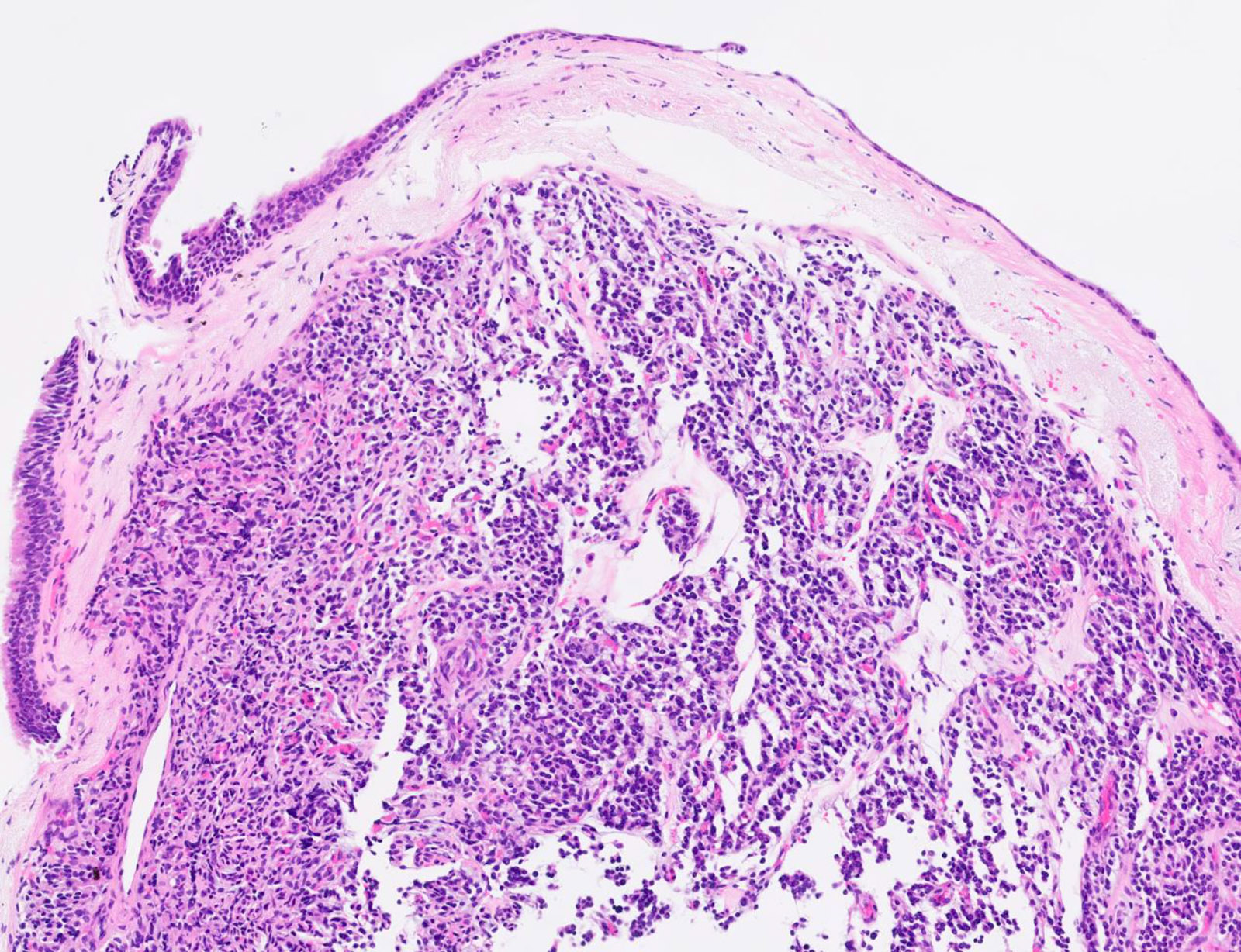
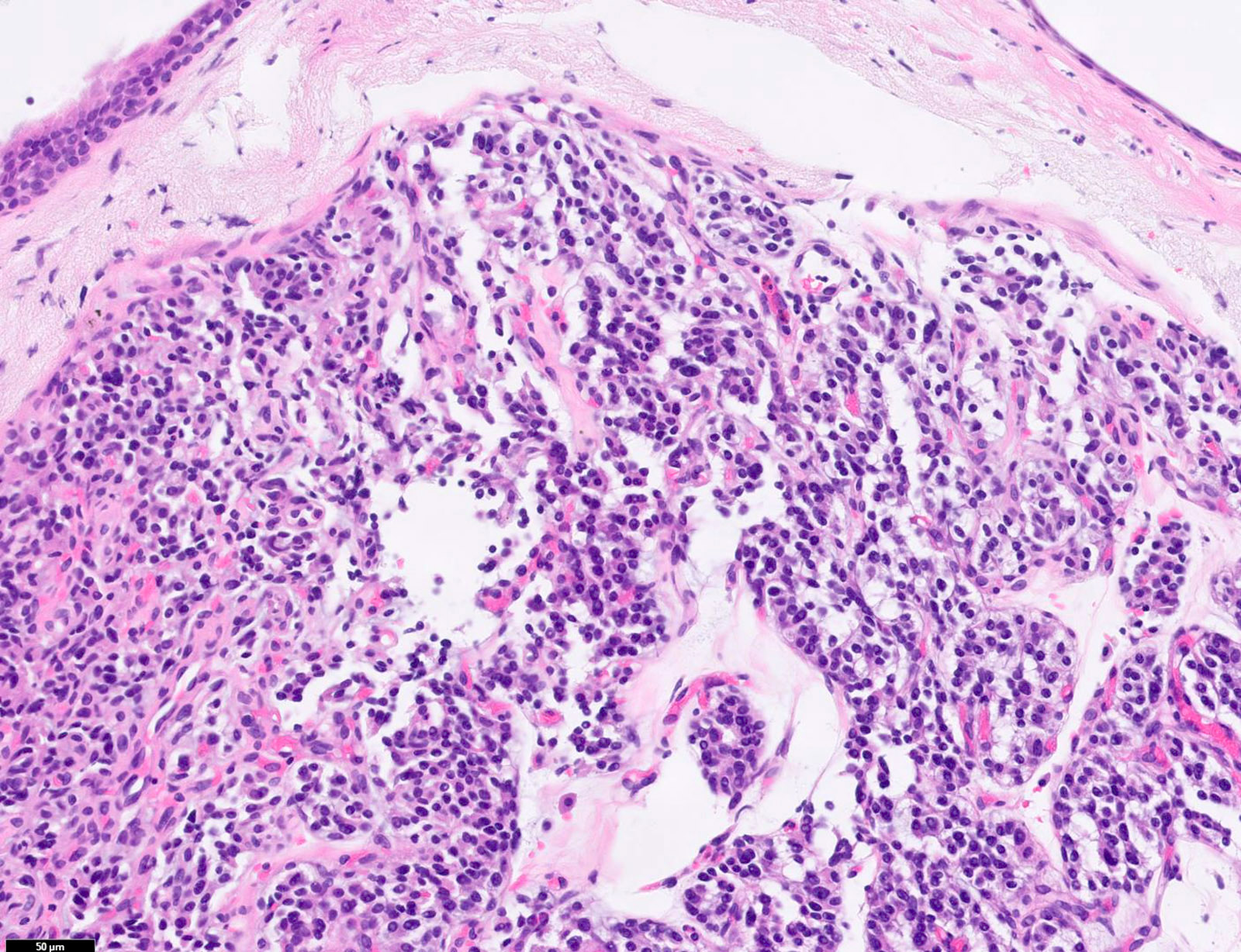
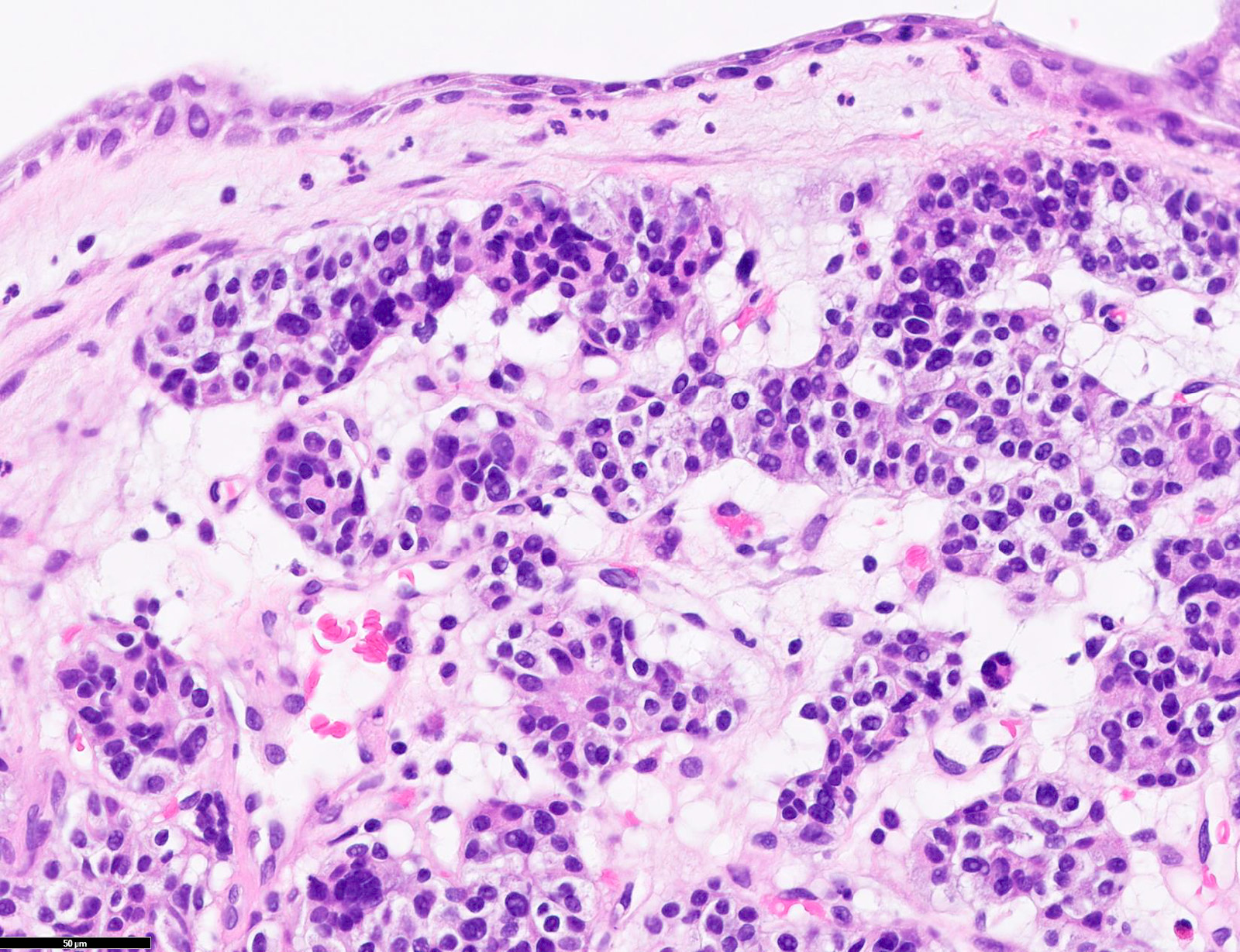
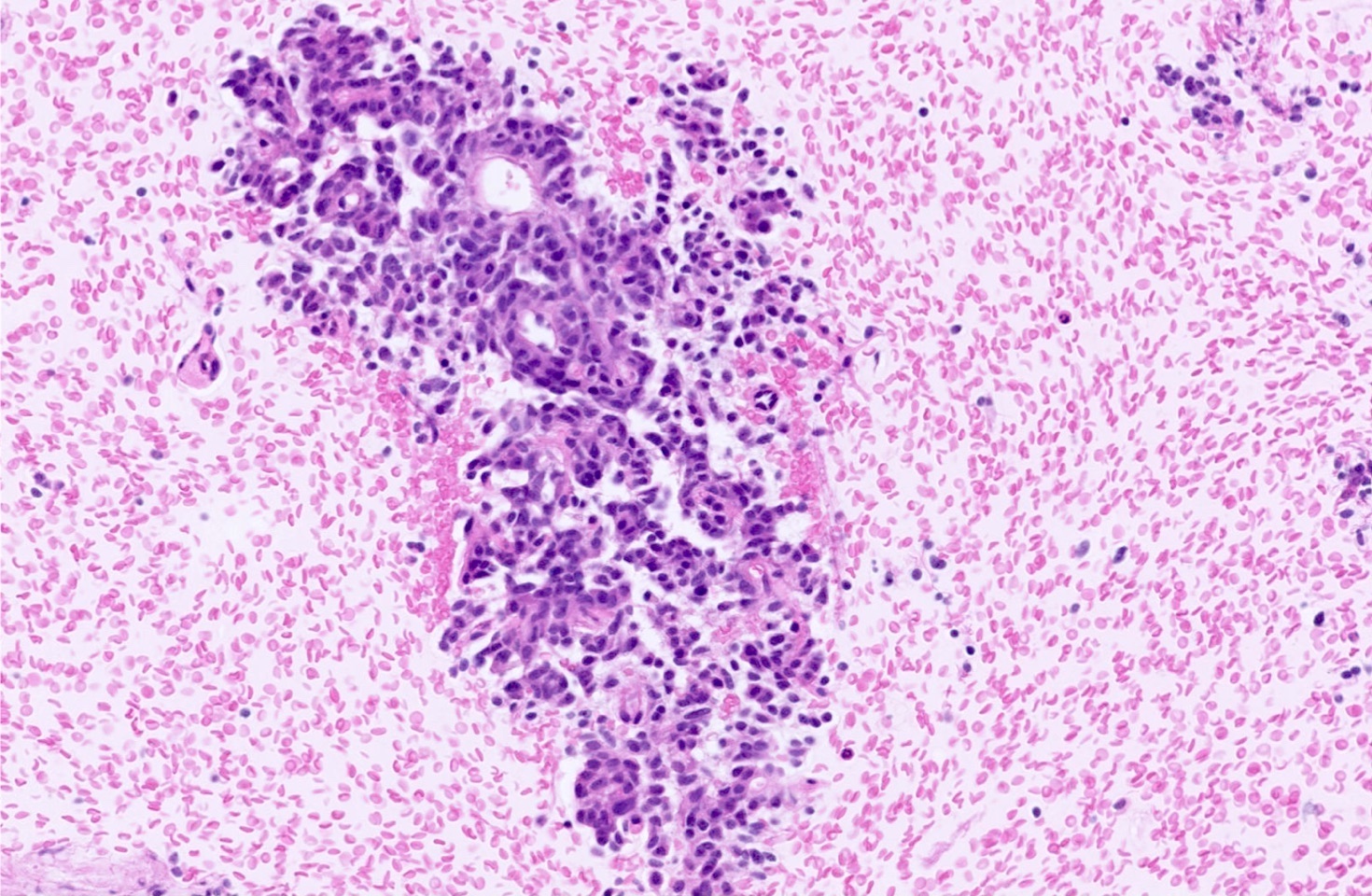
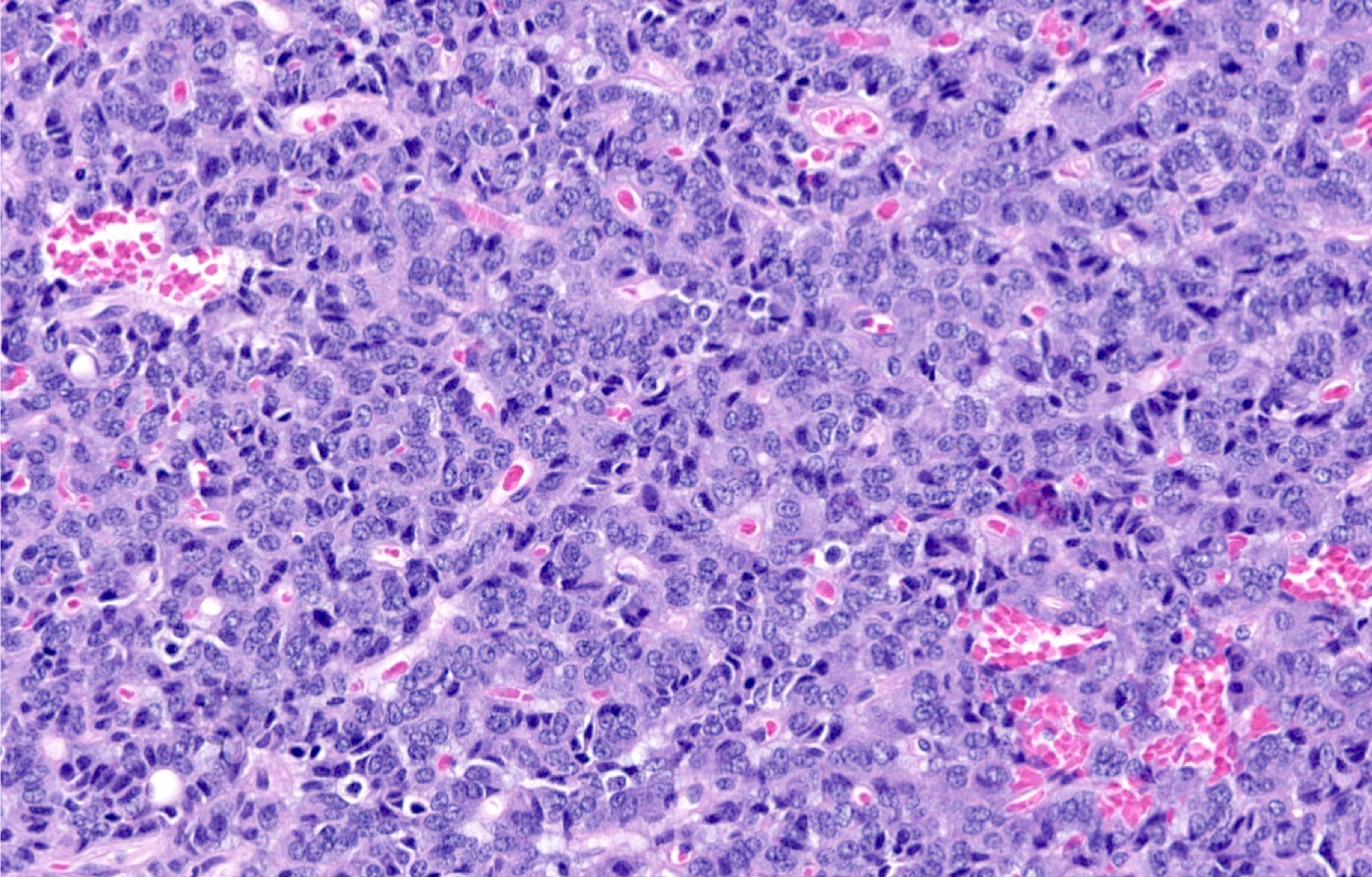
Microscopic (histologic) description
- Diagnostic criteria
- Neuroendocrine tumor with size ≥ 5 mm with < 2 mitoses/2 mm2 and absence of necrosis
- Neuroendocrine growth pattern (organoid, trabecular, rosette formation, nested) or pseudoglandular, follicular and papillary growth
- Tumor cells are uniform with a polygonal shape, round to oval nuclei with salt and pepper chromatin as well as inconspicuous nucleoli and moderate to abundant eosinophilic cytoplasm
- Spindle cells and clear cell features can be seen
- Stroma is fine and highly vascularized; hyalinization, cartilage or bone formation are possible
- Reference: Curr Oncol 2018;25:S86
Microscopic (histologic) images
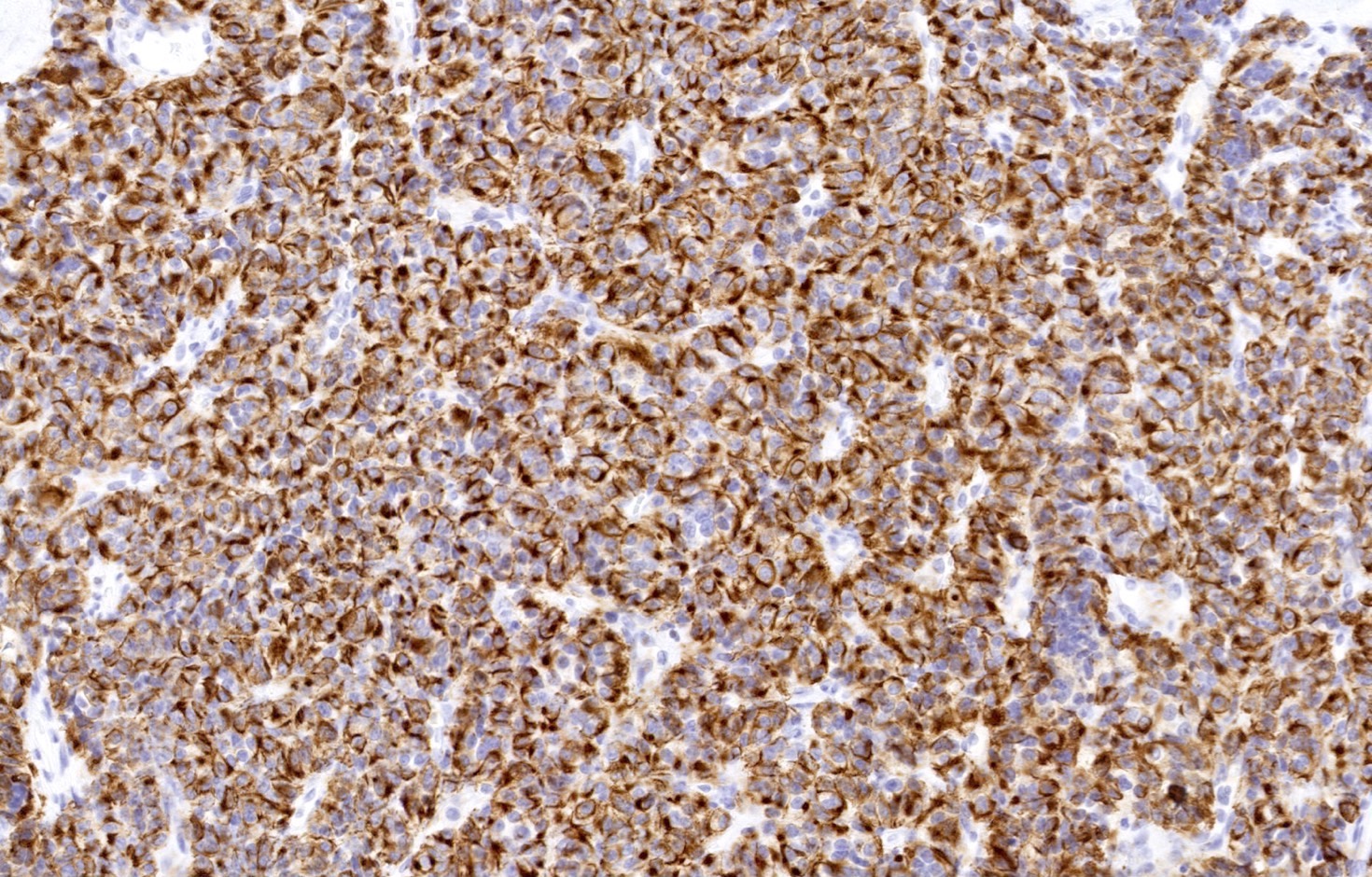
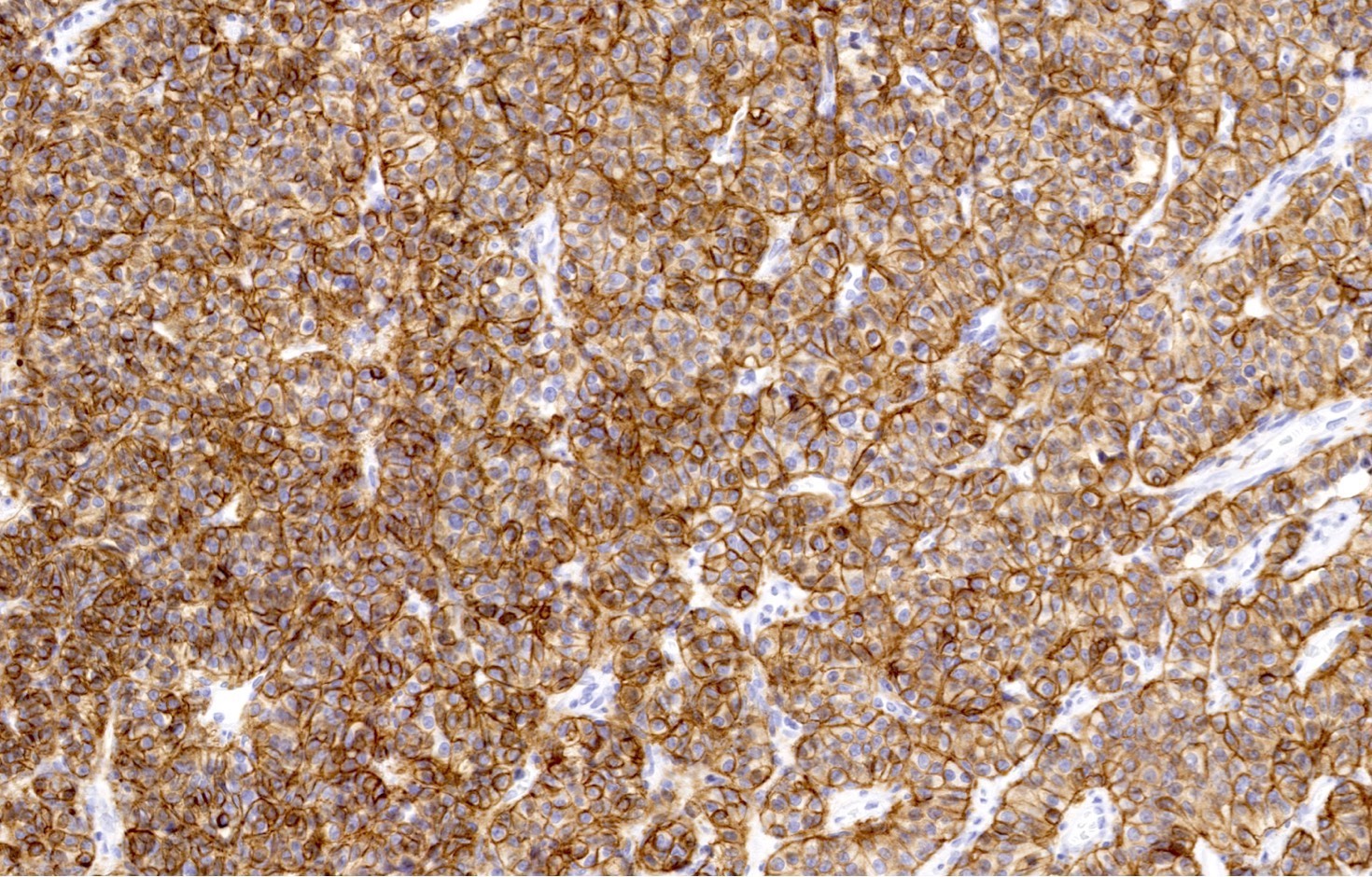
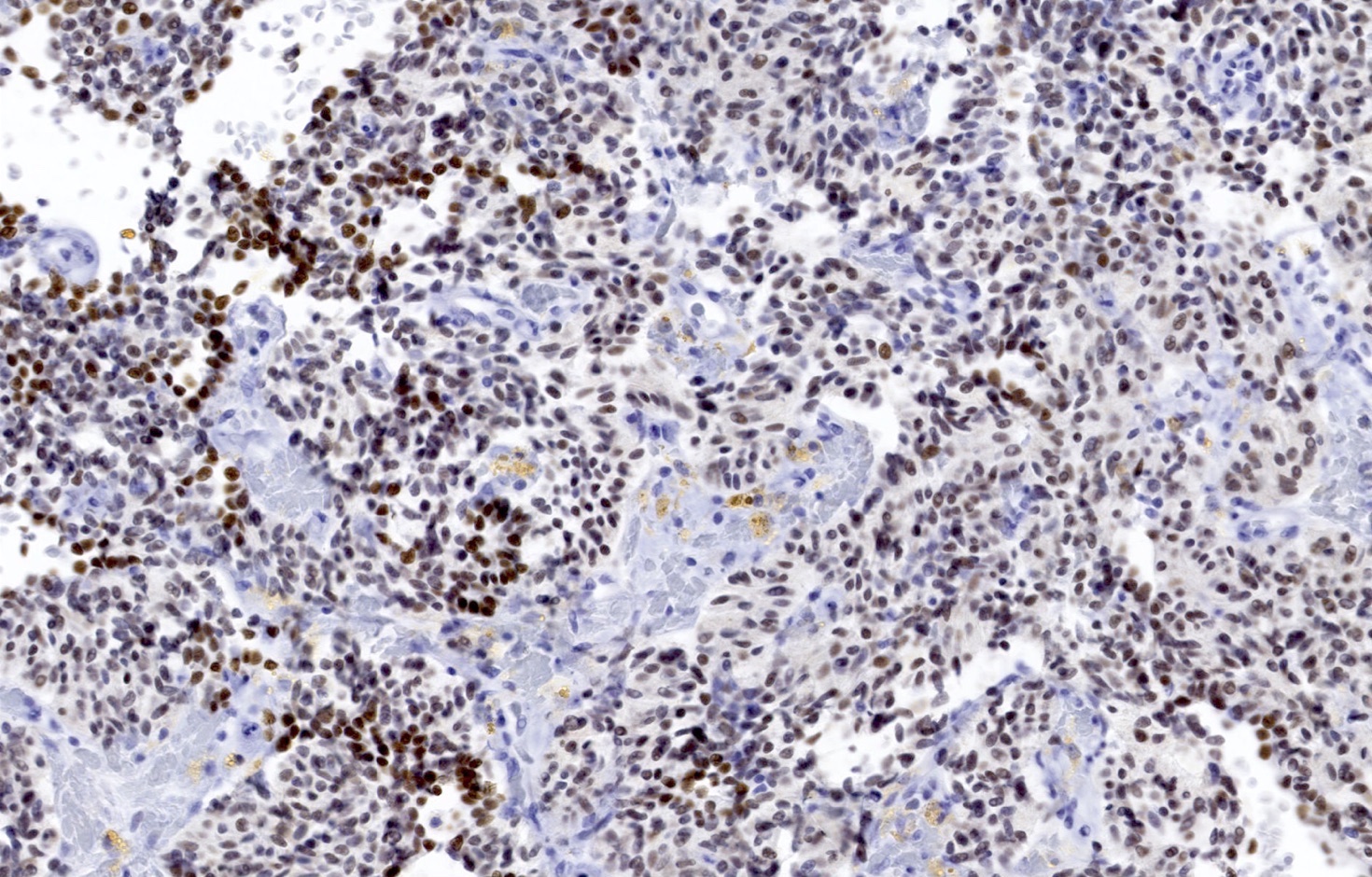
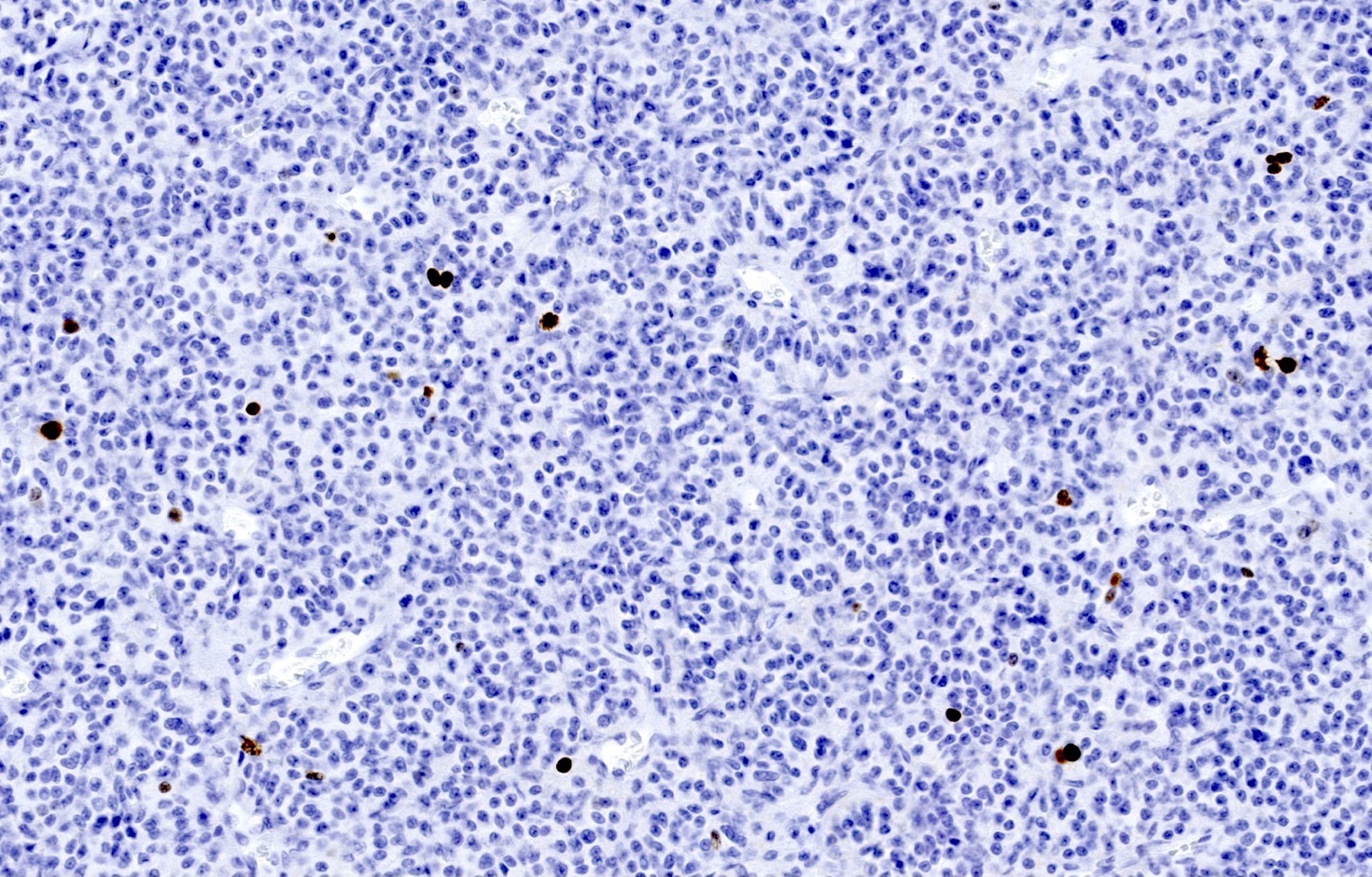
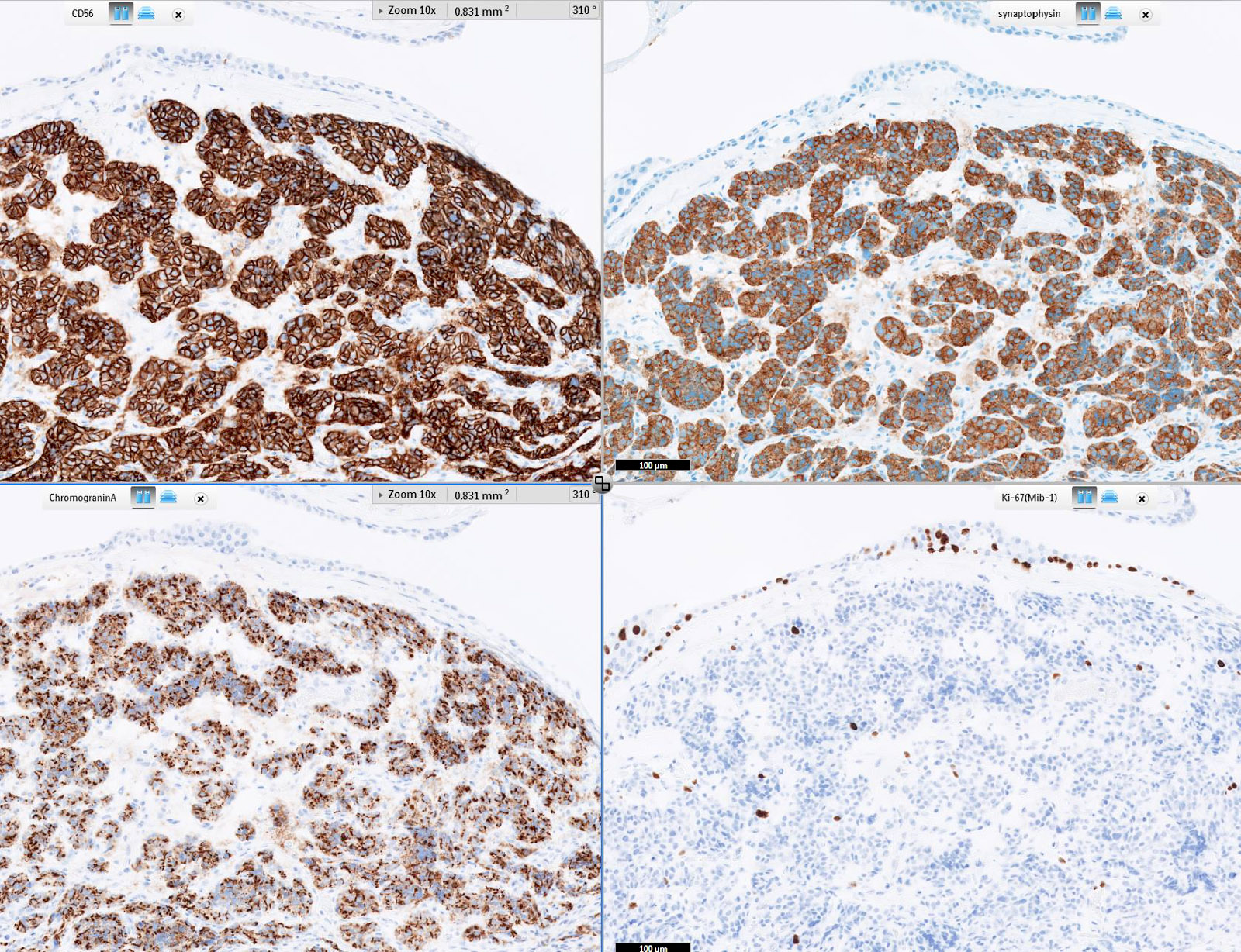
Contributed by Philippe Joubert, M.D., Ph.D., Jijgee Munkhdelger, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
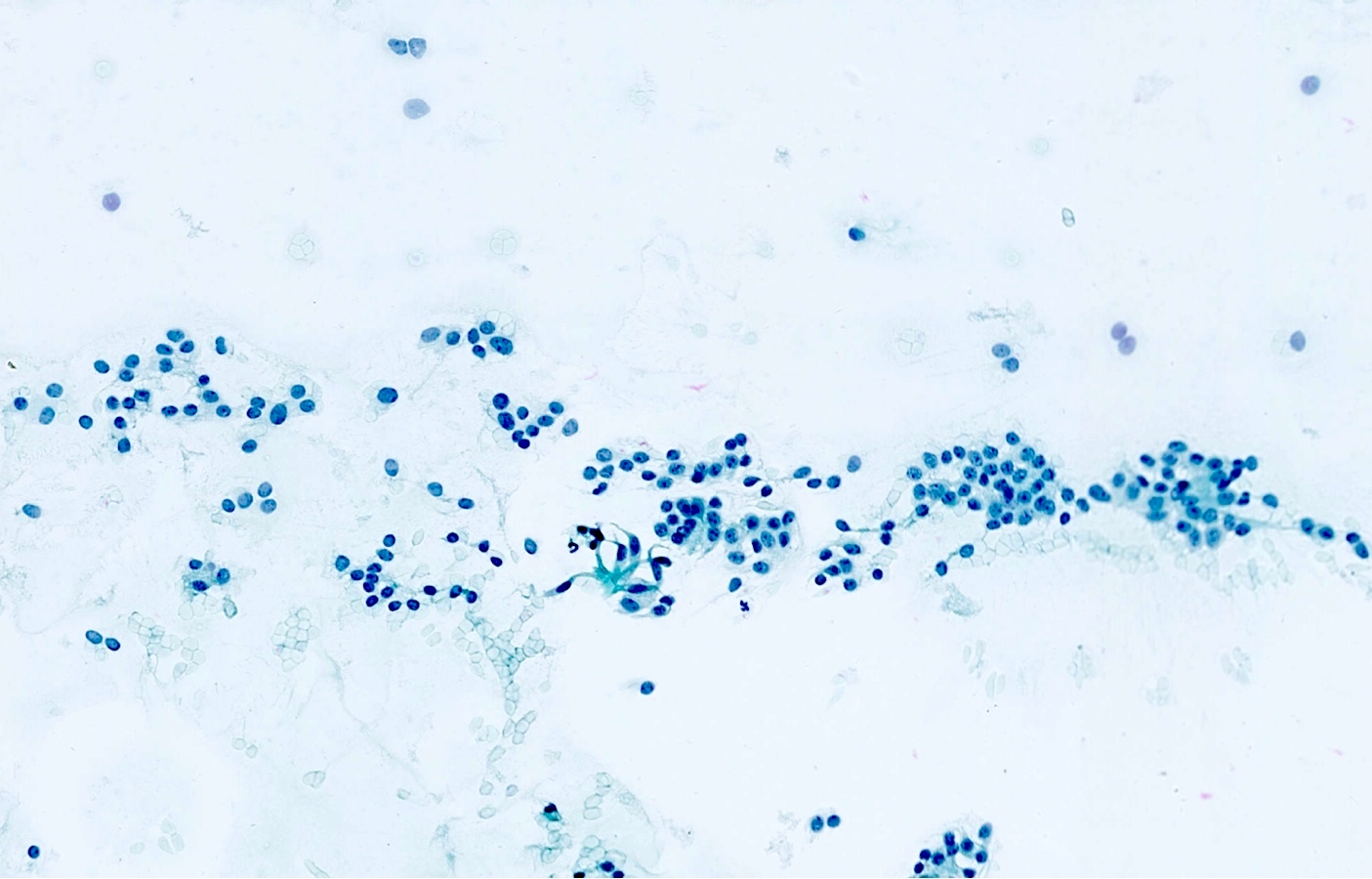
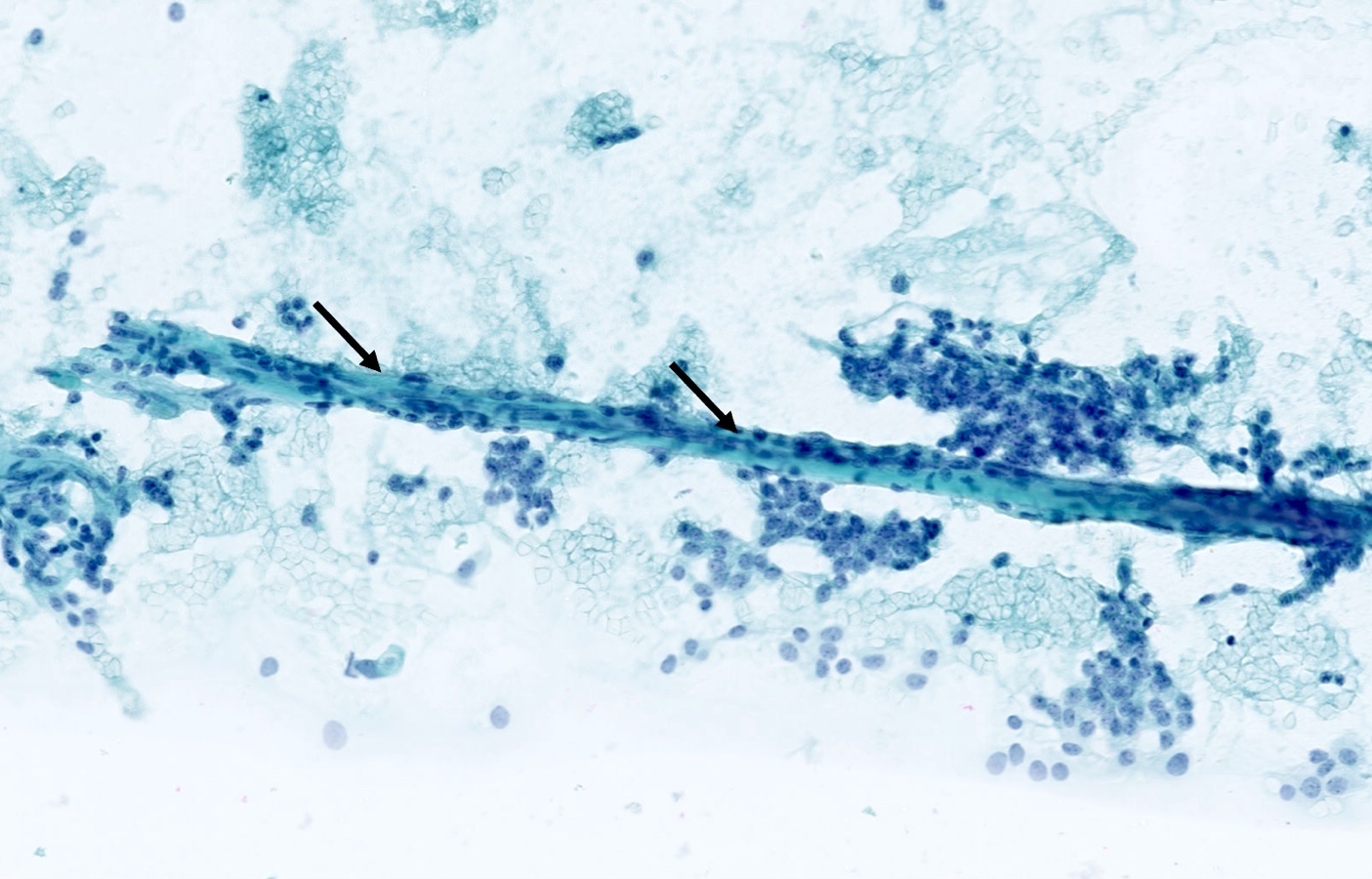
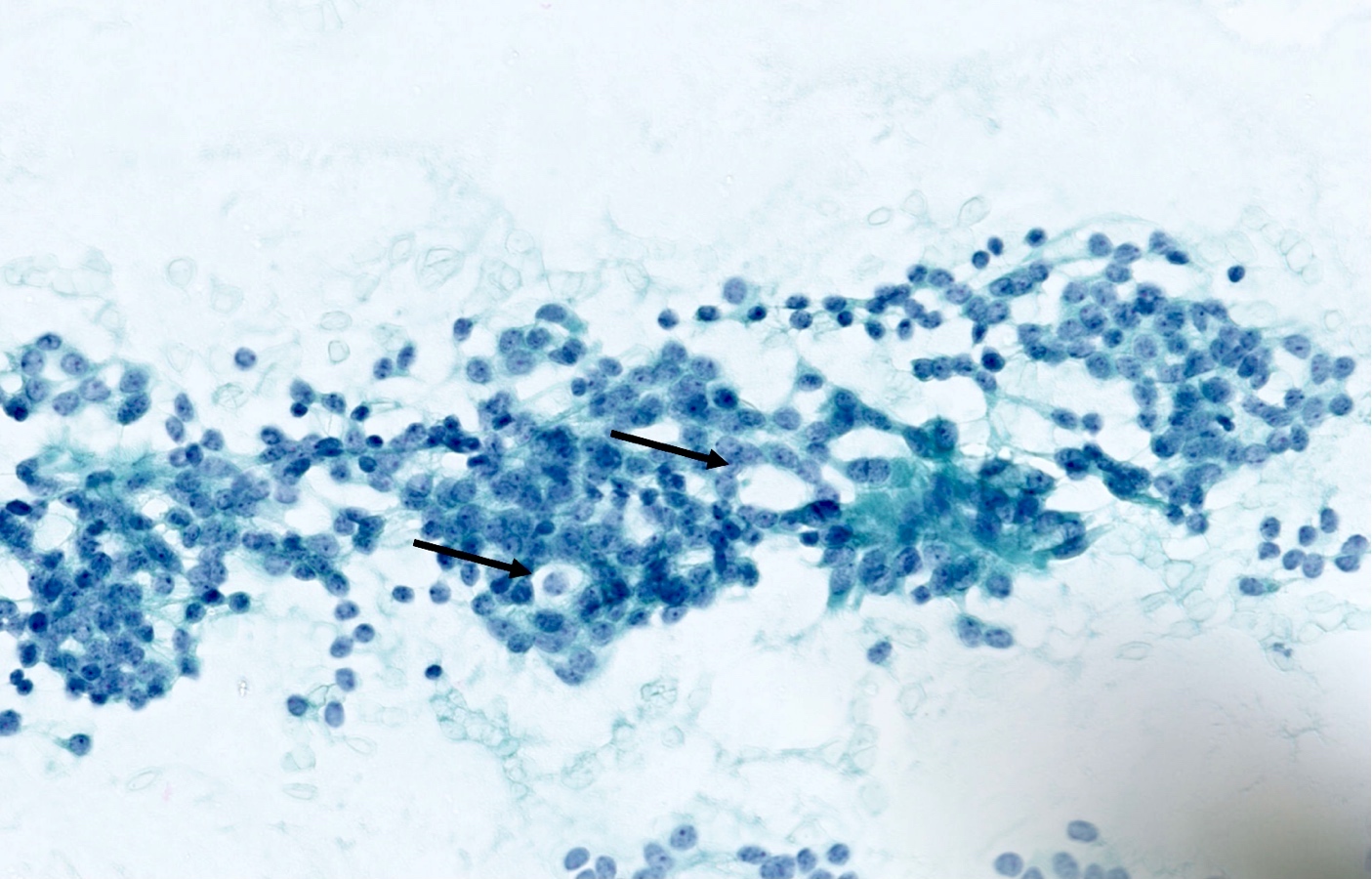
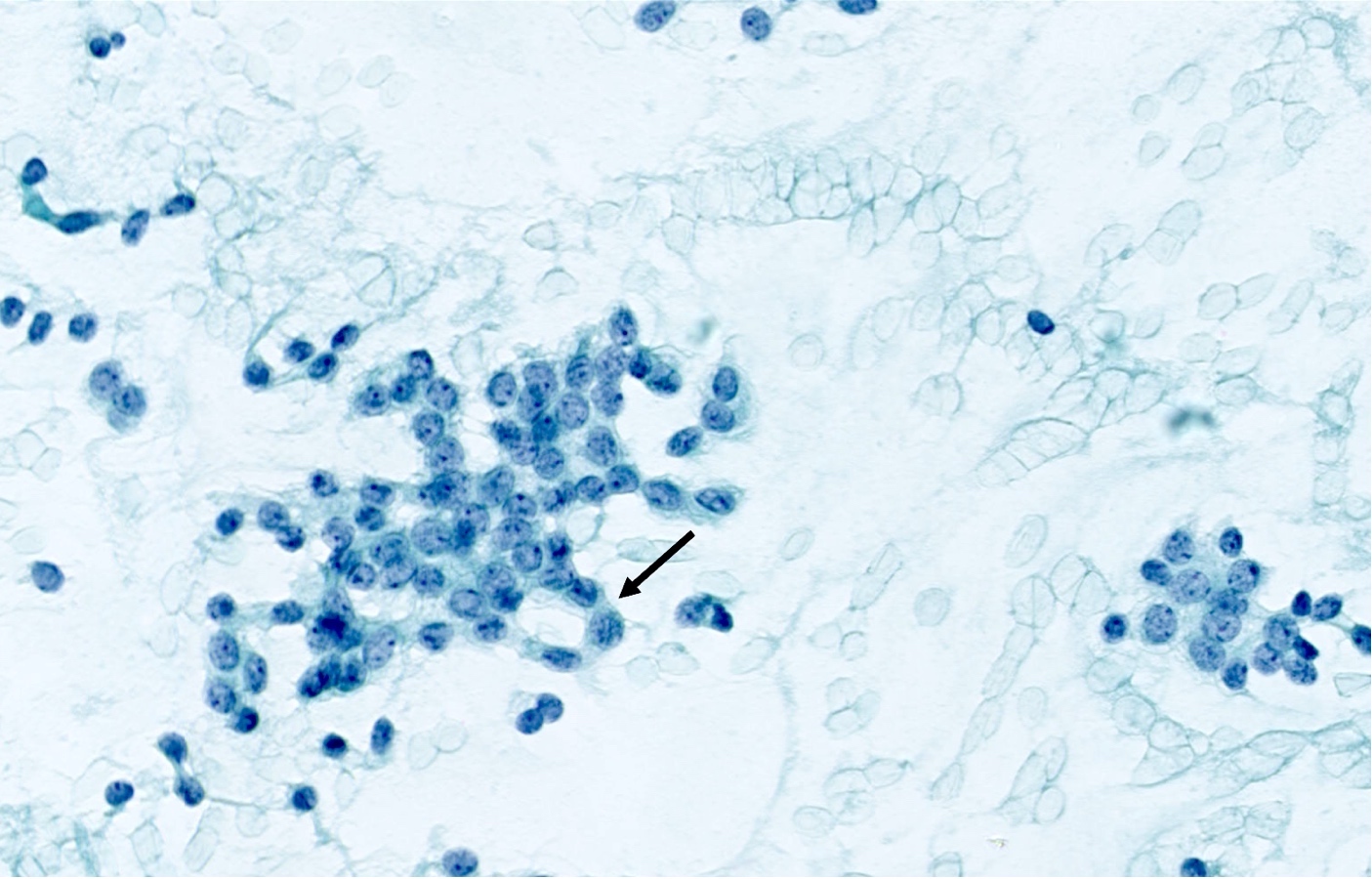
Cytology description
- Loosely cohesive groups and isolated cells sometimes around branching capillaries; rosette structures may be seen (Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 4th Edition, 2014)
- Uniform population of small tumor cells with round / elongated or plasmacytoid shape
- Smooth nuclear outlines, uniform with salt and pepper chromatin and a small nucleolus; no or rare mitoses
- Scant granular cytoplasm
- Absence of molding, nuclear crush and necrosis
Cytology images
Positive stains
- Chromogranin, synaptophysin, CD56 and INSM1: diffusely and strongly positive (Mod Pathol 2019;32:100)
- Pancytokeratins: positive, useful to distinguish from paraganglioma (Arch Pathol Lab Med 2010;134:1628)
- Ki67 (expected < 20%)
- Ki67 proliferative index does not have an impact on tumor classification; WHO classification states that is desirable to routinely report its value
- Mostly useful to discriminate between high grade neuroendocrine tumors (small cell carcinoma and large cell neuroendocrine carcinoma), on small or crushed biopsies in particular (Arch Pathol Lab Med 2018;142:947)
- Utility of differentiation between typical and atypical carcinoid is not proven (Virchows Arch 2017;470:153)
- TTF1: useful marker of pulmonary lineage in typical and atypical carcinoids but only positive in < 50% of cases
- TTF1+ carcinoids are more commonly seen in peripheral lesions and staining is commonly focal and weak (Hum Pathol 2004;35:825)
- Rb: preserved in the vast majority of pulmonary carcinoids (Transl Lung Cancer Res 2017;6:513)
Negative stains
- CDX2: negative in pulmonary carcinoids; highly specific to confirm an intestinal origin (Appl Immunohistochem Mol Morphol 2007;15:407)
- Calcitonin, PSA
Molecular / cytogenetics description
- Low somatic mutation rate
- Mutations in the chromatin remodeling genes, including MEN1 (Nat Commun 2014;5:3518)
Videos
Typical carcinoid tumor
Sample pathology report
- Right lung, superior lobe, transbronchial biopsy:
- Carcinoid tumor, not otherwise specified
Differential diagnosis
- Atypical carcinoid:
- Well differentiated neuroendocrine tumor with > 2 mitoses/2 mm2 or presence of necrosis
- Carcinoid tumorlet:
- Well differentiated neuroendocrine tumor with size < 5 mm and with < 2 mitoses/2 mm2 and absence of necrosis
- Small cell carcinoma:
- Scant cytoplasm, elevated nuclear to cytoplasmic ratio, nuclear molding, absence of nucleoli
- Ki67 proliferative index > 50%
- Large cell neuroendocrine carcinoma:
- Large cells, high grade nuclei
- High mitotic index, Ki67 proliferative index > 50%
- Paraganglioma:
- Cytokeratins are negative
- Also can have S100+ sustentacular cells
- Thyroid medullary carcinoma:
- Calcitonin+, CEA+
- Well differentiated neuroendocrine tumor of the gastrointestinal tract:
- Type A thymoma:
- p40+
- Neuroendocrine markers (chromogranin, synaptophysin) are negative
- Prostatic adenocarcinoma (if cribriform or neuroendocrine features):
- Breast carcinoma:
Additional references
Practice question #1
A 55 year old woman had a lower left lobectomy showing a well circumscribed flesh colored tumor. Histologic details are shown in the image above. Regarding this entity, which of the following statements is true?
- CDX2 is usually negative in the lung and is useful to differentiate from a metastasis of an intestinal origin
- Ki67 proliferative index is essential to grade this tumor
- Rb expression is typically lost in this tumor
- TTF1 is always positive
Practice answer #1
A. CDX2 is usually negative in the lung and is useful to differentiate from a metastasis of an intestinal origin. The image shows a tumor with a trabecular pattern and pseudorosettes. The stroma is highly vascularized. Tumor cells are monotonous with scant to moderate eosinophilic cytoplasm. Nuclei are round to oval with salt and pepper chromatin and inconspicuous nucleoli. No mitoses are seen. These features are consistent with a typical carcinoid lung tumor.
Ki67 immunostaining, counter to well differentiated neuroendocrine tumors from the gastrointestinal tract, is not essential to grade the tumor. The difference between typical and atypical tumor relies on mitosis count and the presence of necrosis. However, Ki67 is useful to differentiate from high grade neuroendocrine tumors (small cell and large cell neuroendocrine carcinomas) on small biopsies with artifacts. TTF1 is positive in only half of cases with a higher frequency in peripheral tumors. Rb expression is preserved in typical carcinoid lung tumors, unlike in small cell tumors.
Comment Here
Reference: Carcinoid tumor / neuroendocrine tumor, grade 1
Ki67 immunostaining, counter to well differentiated neuroendocrine tumors from the gastrointestinal tract, is not essential to grade the tumor. The difference between typical and atypical tumor relies on mitosis count and the presence of necrosis. However, Ki67 is useful to differentiate from high grade neuroendocrine tumors (small cell and large cell neuroendocrine carcinomas) on small biopsies with artifacts. TTF1 is positive in only half of cases with a higher frequency in peripheral tumors. Rb expression is preserved in typical carcinoid lung tumors, unlike in small cell tumors.
Comment Here
Reference: Carcinoid tumor / neuroendocrine tumor, grade 1
Practice question #2
Regarding typical carcinoid tumors of the lung, which of the following statements is true?
- Diagnostic criteria are based on mitotic rate and Ki67 proliferation index
- Most patients are smokers
- They are mostly found in peripheral airways
- They may arise in the context of diffuse idiopathic pulmonary neuroendocrine cell hyperplasia and tumorlets
Practice answer #2
D. They may arise in the context of diffuse idiopathic pulmonary neuroendocrine cell hyperplasia and tumorlets. Development of carcinoid tumors of the lung is not well understood but some cases are associated with diffuse idiopathic pulmonary neuroendocrine cell hyperplasia and tumorlets. The other statements are false. Even though lung carcinoids are found in association to airways and can be found all over the bronchial tree, most of them are centrally located (C). Typical carcinoids are not related to smoking (B). The diagnostic criteria of carcinoid tumors of the lung differ from the ones of well differentiated neuroendocrine tumors of the gastrointestinal tract (A). In the lung, the classification is based on mitotic count per 2 mm2 and presence / absence of necrosis. Typical carcinoids have a mitotic rate of 2 mitoses/2 mm2 and no necrosis, while atypical carcinoids have a mitotic rate of 2 - 10 mitoses/2 mm2 or a presence of necrosis.
Comment Here
Reference: Carcinoid tumor / neuroendocrine tumor, grade 1
Comment Here
Reference: Carcinoid tumor / neuroendocrine tumor, grade 1