Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Cazzato G, Ingravallo G. Leishmaniasis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorleishmaniasis.html. Accessed August 14th, 2025.
Definition / general
- Protozoal disease caused by over more than 20 Leishmania species, in both tropical and subtropical regions
- 3 main forms of the disease: visceral leishmaniasis (VL), cutaneous leishmaniasis (CL) and mucocutaneous leishmaniasis (MCL)
Essential features
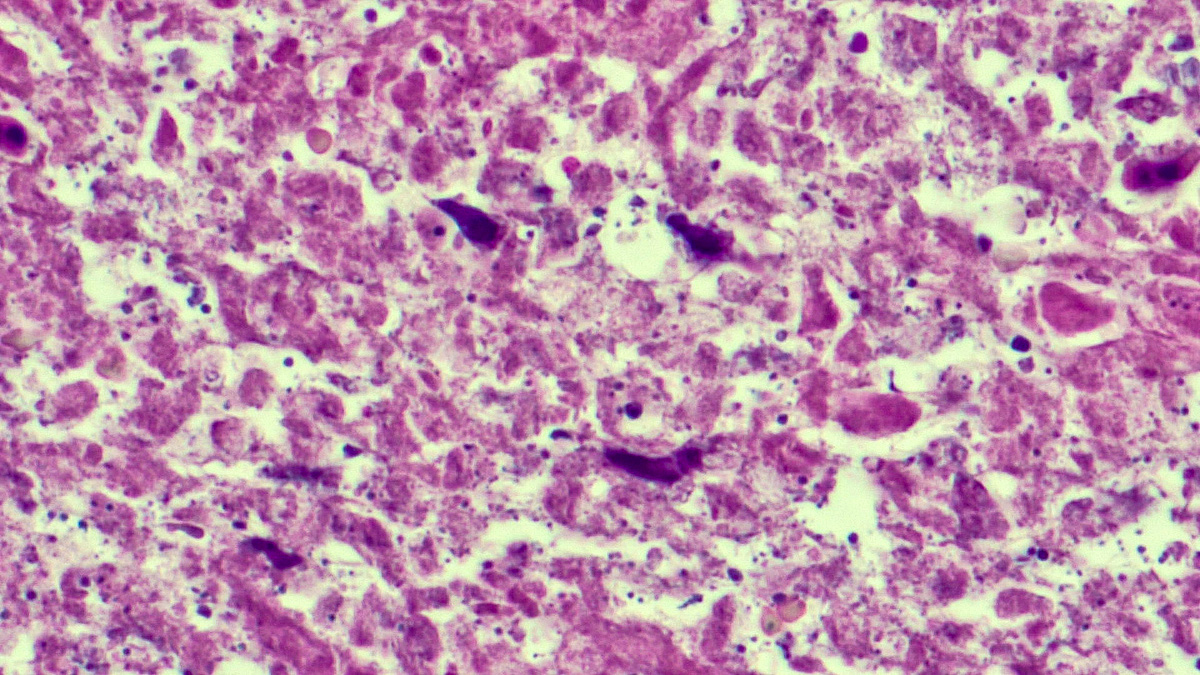
- In H&E, presence of small hematoxylinophilic formations that are round, uniform in appearance, intracytoplasmic and sometimes distributed around the outer rim of the vacuoles (the marquee sign)
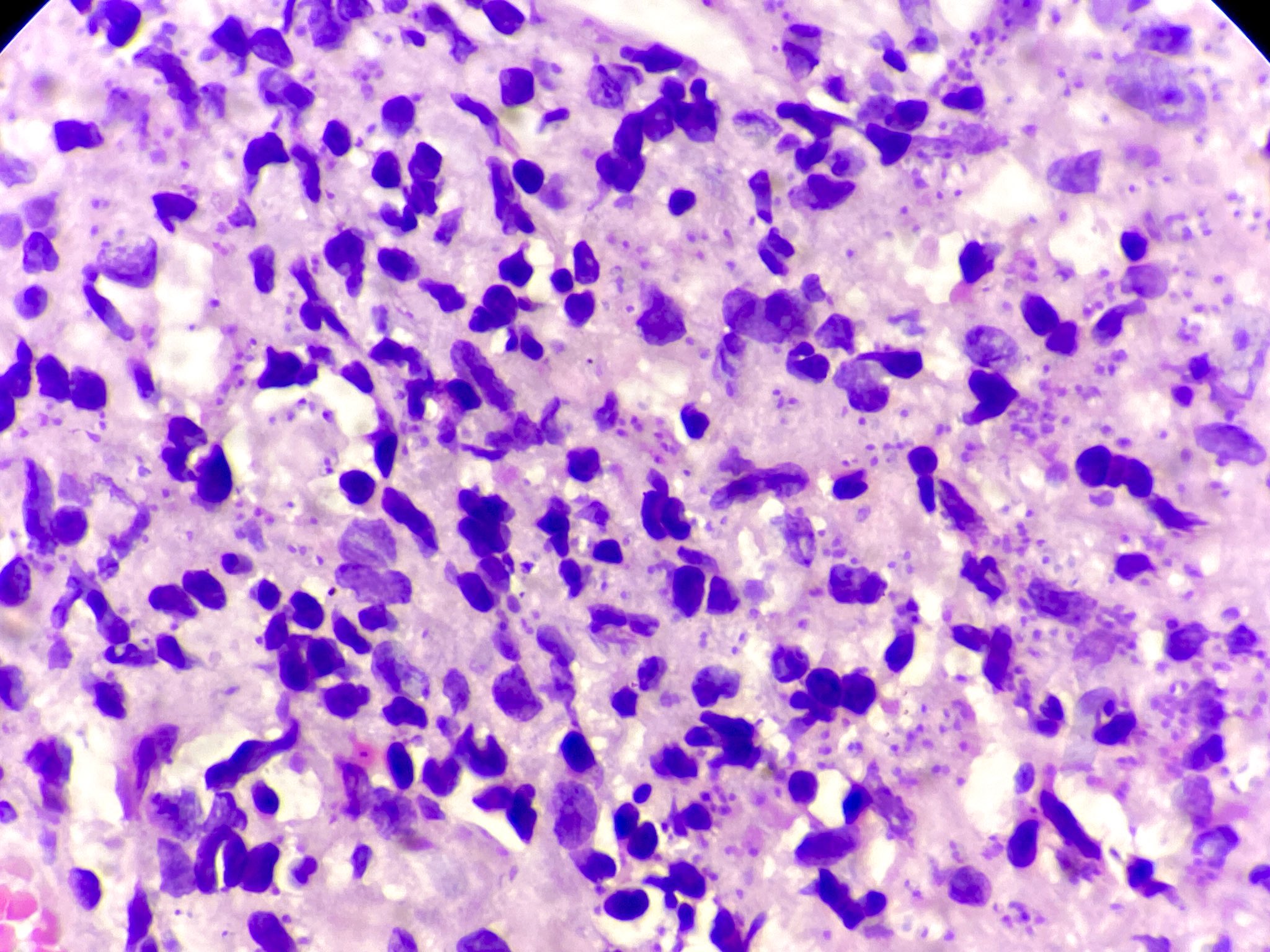
- Weigert iron hematoxylin may stain parasites better than H&E or Giemsa
- Immunohistostain using CD1a antibody is more sensitive than H&E
Terminology
- Oriental button
Epidemiology
- Cutaneous form is predominantly in the Middle East, whereas the mucocutaneous form occurs in South America (Brazil, Bolivia, Peru)
Sites
- Visceral (spleen, liver, bone marrow, lymph nodes and intestinal mucosa), cutaneous (skin) and mucocutaneous (skin and mucous membrane)
Pathophysiology
- Transmitted by the bite of infected female phlebotomine sandflies (infective stage: promastigotes)
- Promastigotes phagocytized by macrophages and other types of mononuclear phagocytic cells
- Promastigotes transform in these cells into the tissue stage of the parasite (i.e., amastigotes)
- Parasite, host and other factors affect whether the infection becomes symptomatic and whether it results in cutaneous or visceral leishmaniasis
- Sandflies become infected by ingesting infected cells during blood meals
- In sandflies, amastigotes transform into promastigotes, develop in the gut, then migrate to the proboscis (see Diagrams / tables) (Lancet 2018;392:951)
Clinical features
- Protozoal disease caused by more than 20 Leishmania species in both tropical and subtropical regions, such as Asia, Africa, America and Europe; not present in Australia and Pacific islands (StatPearls: Leishmaniasis [Accessed 15 March 2022])
- 3 main forms of the disease: visceral leishmaniasis, cutaneous leishmaniasis and mucocutaneous leishmaniasis
- Worldwide incidence of visceral leishmaniasis is 50,000 - 90,000 new cases per year (Front Cell Infect Microbiol 2022;11:839851)
- Worldwide incidence of cutaneous leishmaniasis is 600,000 - 1 million new cases per year
- Over 90% of mucocutaneous leishmaniasis occurs in Bolivia, Brazil, Ethiopia and Peru (Acta Trop 2022;228:106327)
- Produces crusted, indurated papule that slowly enlarges; the disease could evolve into a self limited clinical form or into a fatal systemic illness
- Possible coinfection Leishmania HIV
- Visceral (also called kala azar); parasites disseminate to the spleen, liver, bone marrow, lymph nodes and intestinal mucosa causing fever, weight loss, hepatosplenomegaly, anorexia, diarrhea, anemia, thrombocytopenia, hypergammaglobulinemia
- Rarely, it can also affect the skin: post kala azar dermal leishmaniasis (PKDL)
- Can resolve spontaneously or after therapy (early response mediated by Th2 lymphocytes, elevated levels of IL10, IL4 versus interferon gamma and activation of B lymphocytes); if left untreated, and in some predisposed individuals, it can be fatal in over 95% of cases
- Broadly divided into old world (the Eastern Hemisphere) and new world (the Western Hemisphere) (Parasitol Res 2021;120:1541)
- Old world: Leishmania infantum and L. donovani
- New world: L. braziliensis complex and L. mexicana complex
- L. braziliensis may also produce espundia, a destructive mucocutaneous form
- Human infection through bite of infected female phlebotomine sand flies; the sand flies inject the infective stage (i.e., promastigotes) from their proboscis during blood meals
- Clinical presentation and prognosis vary based on species, duration of infection and immune status of patient
- Cutaneous: usually located in exposed areas such as the face, scalp, arms or others
- Both in the old world and the new world
- Old world (also called button of the East world): L. major, L. tropica and skin strains of L. infantum
- L. major (wet lesions): exudative ulcers (3 - 6 cm), rapid evolution, evolution into a disfigured scar
- L. tropica (dry lesions): crusted plaques (1 - 2 cm), slow healing
- New world: L. peruviana, L. panamenisis and L. amazonensis
- Crusted papule (variable dimensions) with lymphatic dissemination around the surrounding areas which causes the formation of secondary ulcers (Microb Pathog 2021;152:104721)
- Disseminated (if immune system doesn't respond to invading parasites), recurrent (recidivans cutaneous) or post kala azar (rare, years after visceral disease) (Microb Pathog 2021;152:104721)
- Mucocutaneous: usually new world disease of rural and jungle regions
- L. braziliensis and L. panamensis produce granulomatous inflammatory lesions, initially located on the nasal cartilaginous septum (tapir nose); possible involvement of oral, pharyngeal or laryngeal mucosa with ulceration and mutilation (Biol Trace Elem Res 2021;199:3918)
Diagnosis
- Visceral leishmaniasis: serodiagnosis (immunocompetent individuals) using common tests, such as the immunofluorescence antibody test (IFAT), enzyme linked immunoassay (ELISA) or direct agglutination test (DAT); the rapid immunochromatographic test is also available and in some cases, bone marrow aspirate is required
- Cutaneous and mucocutaneous leishmaniasis: identification of parasites on H&E or in smears, by culture on specialized media, by Leishmania intradermal skin test (Montenegro test), by fluorescent antibody tests using the patient's serum or by PCR using species specific primers (DNA probes) (Appl Microbiol Biotechnol 2020;104:8105)
Case reports
- 9.5 month old girl with visceral leishmaniasis related hemophagocytic lymphohistiocytosis diagnosed by metagenomic next generation sequencing (mNGS) (Int J Infect Dis 2020;97:27)
- 50 year old man presented with a left eye caruncular mass of 5 year duration (Orbit 2015;34:232)
- 56 year old man with visceral leishmaniasis diagnosed by biopsy of an axillary lymph node (Genet Mol Res 2014;13:9960)
- 67 year old man who presented with inflammatory skin lesions on the scalp and face for the past 7 years (Infection 2021;49:177)
Treatment
- Organic salts of pentavalent antimony, antimoniate of N methylglucamine and sodium stibogluconate (Expert Rev Anti Infect Ther 2018;16:219)
- Amphotericin B and lysosomal preparation (Infect Dis Clin North Am 2019;33:79)
- Miltefosine (Curr Opin Infect Dis 2012;25:141)
Clinical images
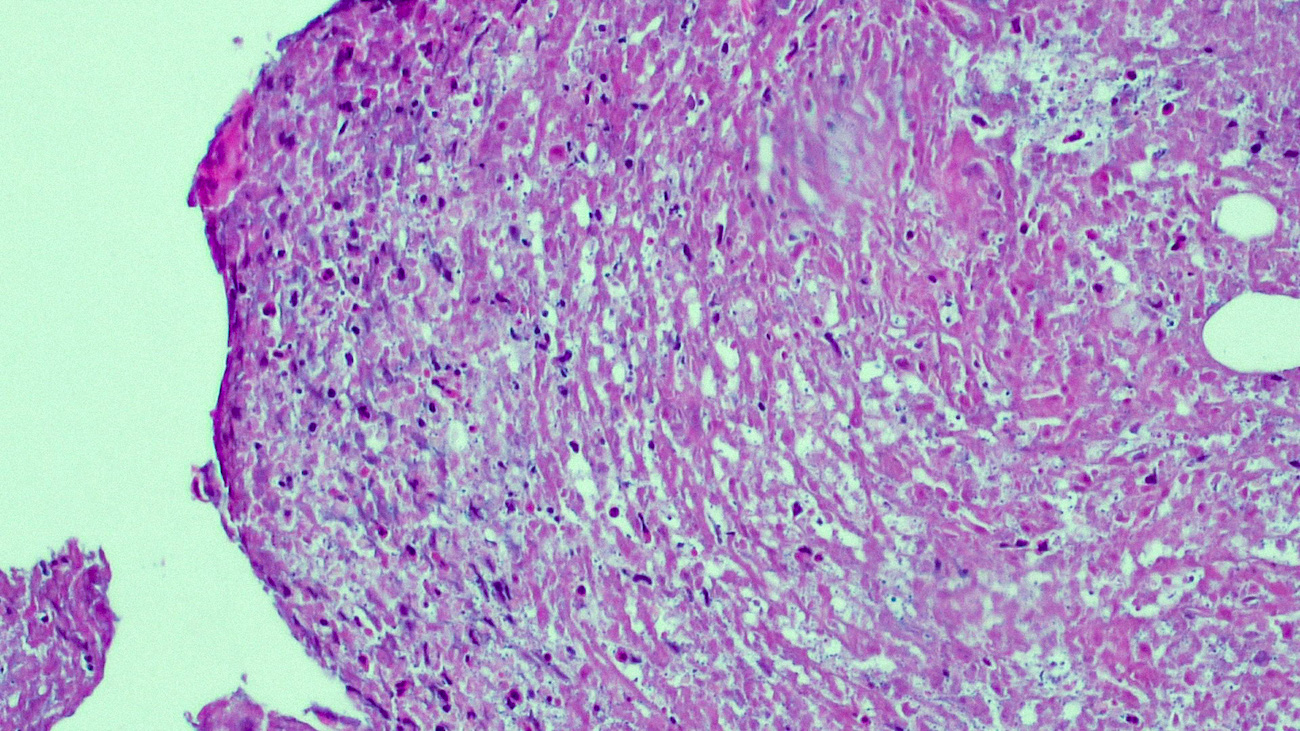
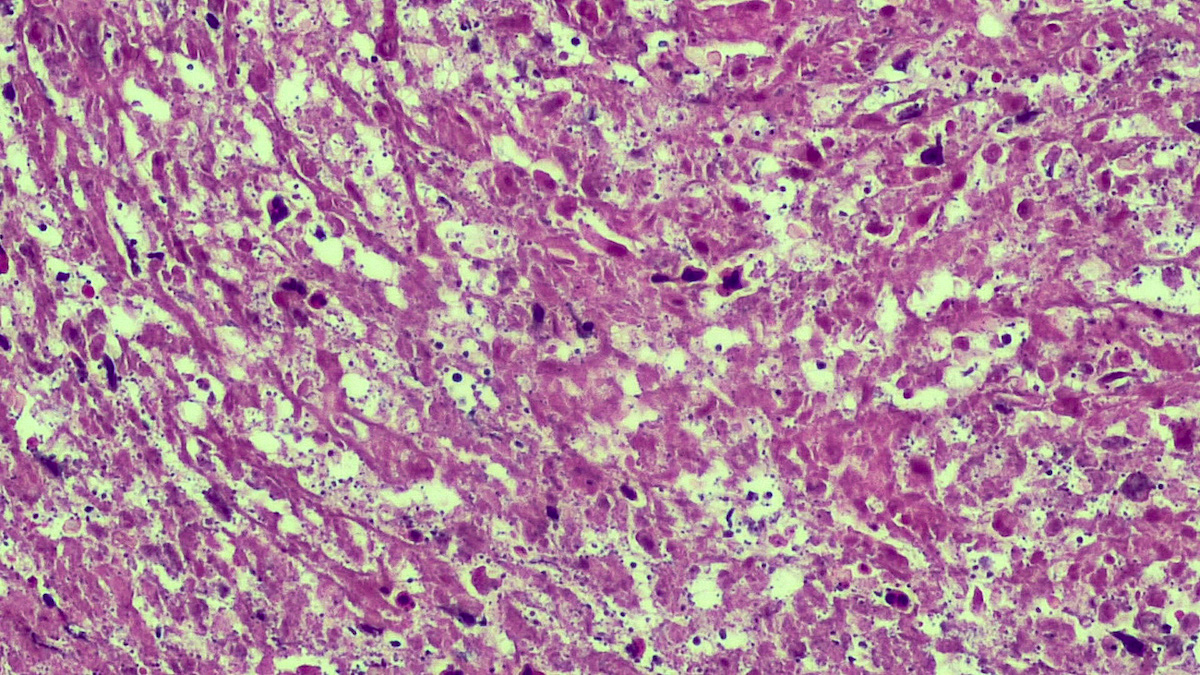
Microscopic (histologic) description
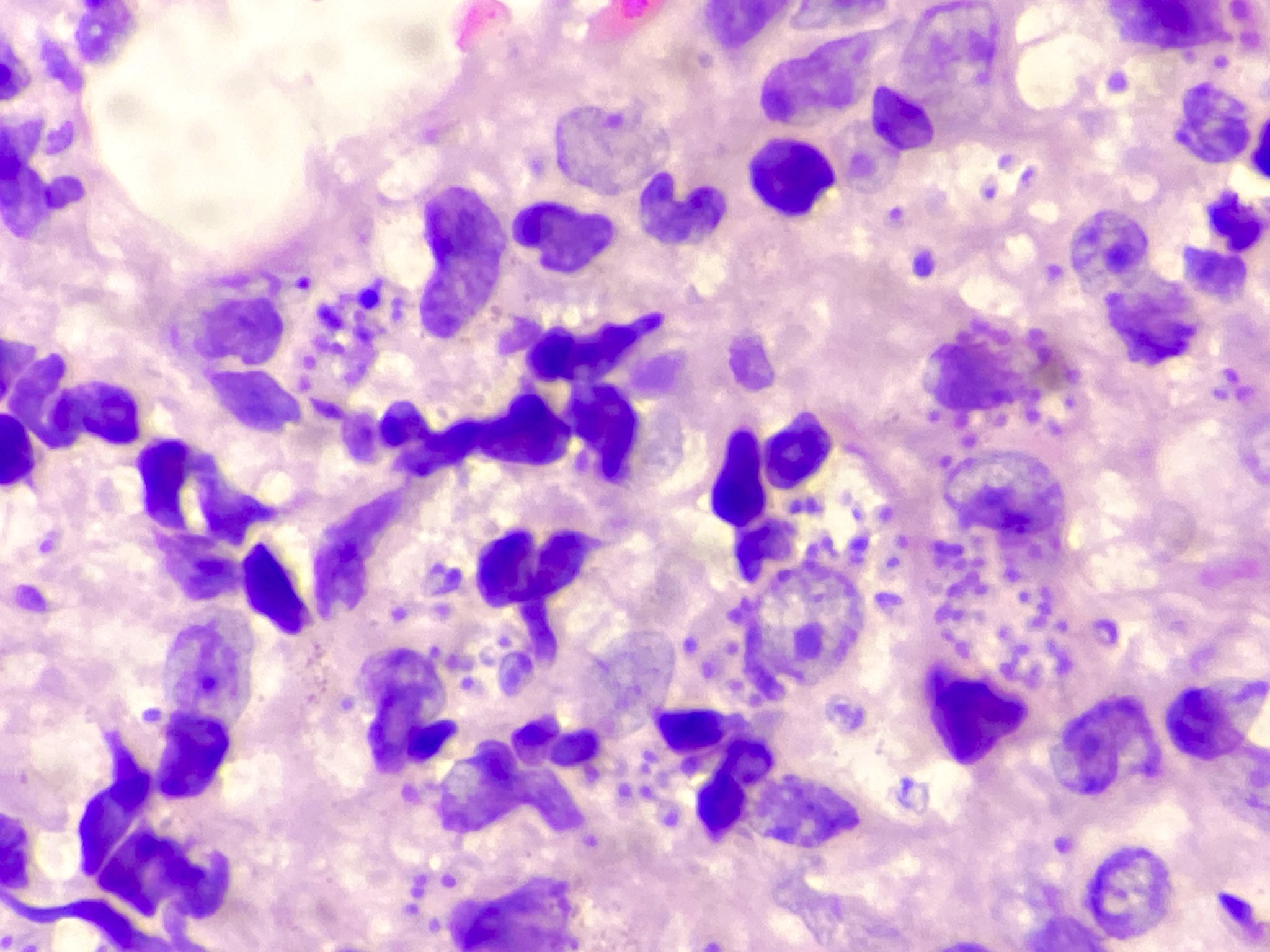
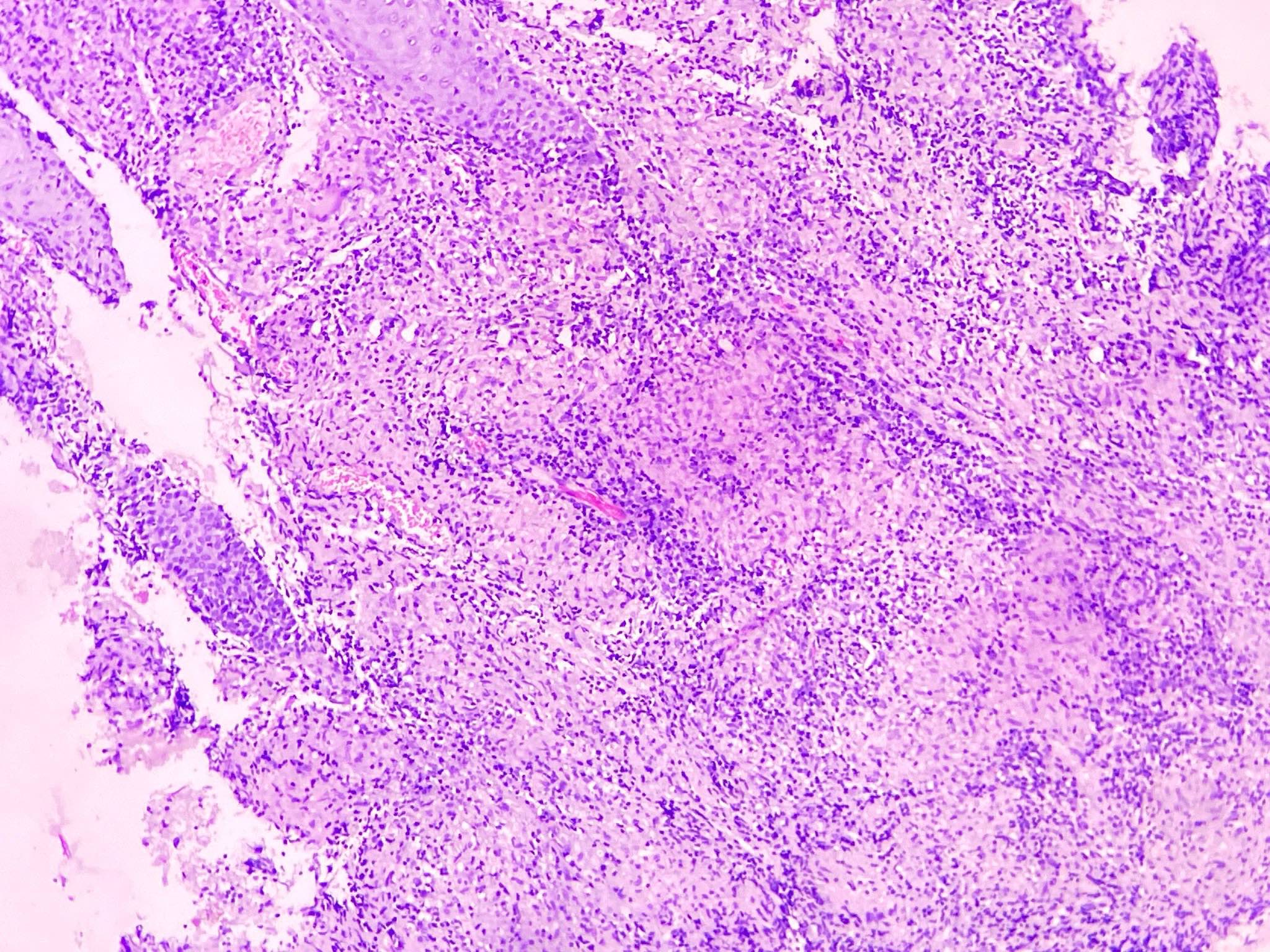
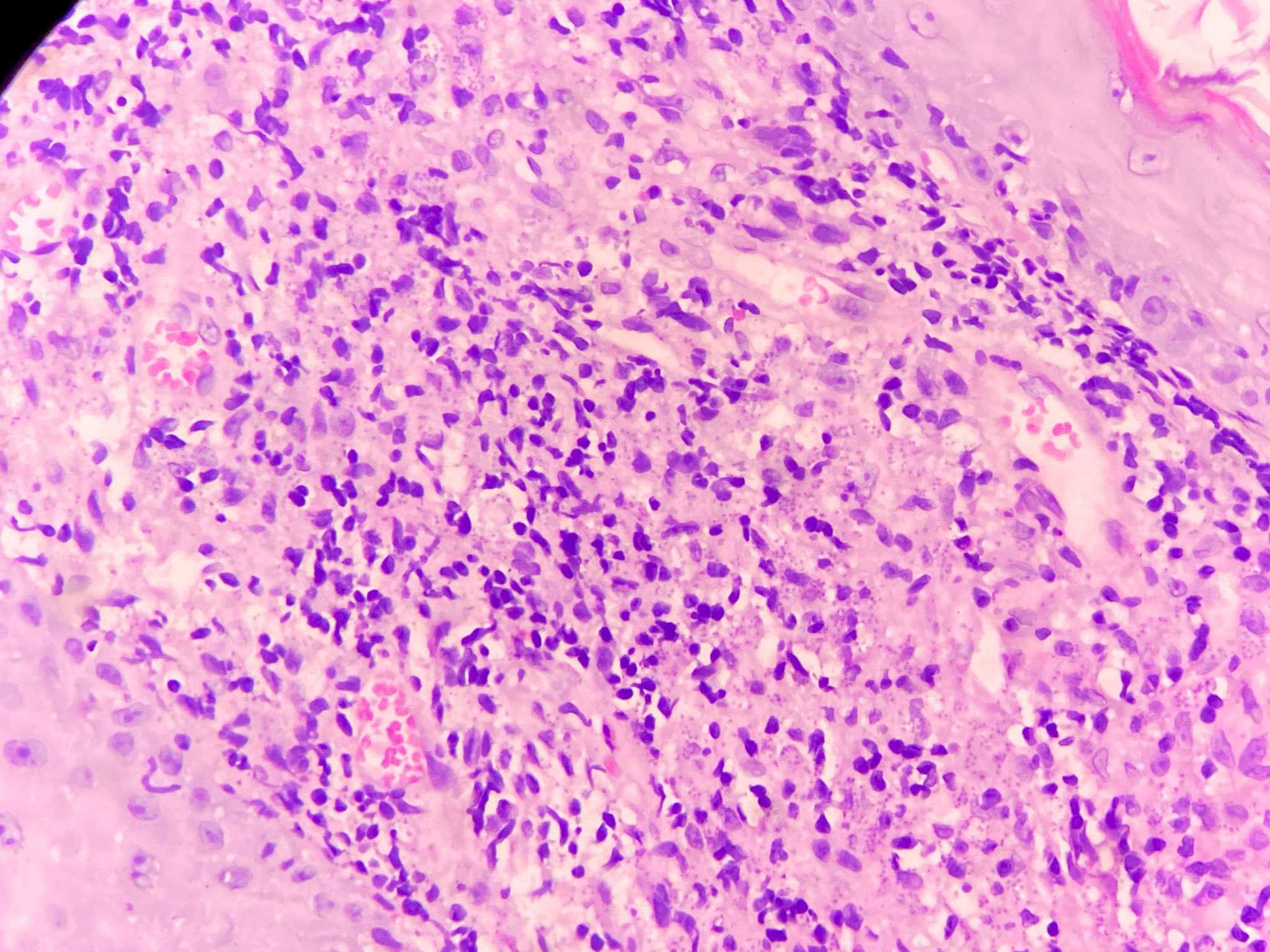
- In the skin, usually a granulomatous inflammation with the presence of histiocytes / macrophages that can (not always, so called uninhabited lesions) contain tiny, uniform, round, hematoxylinophils, intracytoplasmic organisms (amastigotes)
- In acute infections, there is a mixed inflammatory infiltrate with numerous amastigotes
- Reference: J Am Acad Dermatol 2015;73:911
Microscopic (histologic) images
Positive stains
- Weigert iron hematoxylin may stain parasites better than H&E or Giemsa
- Immunohistostain using CD1a antibody is more sensitive than H&E
- Reference: J Cutan Pathol 2019;46:90
Videos
Leishmania infection
Sample pathology report
- Skin, biopsy (usually punch / shave):
- Cutaneous leishmaniasis (see comment)
- Comment: Sections of skin and subcutis, including mainly lymphomonocyte and histiocytic inflammatory infiltration, sometimes with necrosis phenomena. Within the histiocyto-macrophage component, the presence of small hematoxylinophilic formations, round, uniform in appearance, intracytoplasmic morphologically suggestive of Leishmania amastigotes is described. It is difficult to appreciate the distribution of these corpuscles around the outer rim of the vacuoles (the marquee sign). Immunostaining with CD1a was focal positive.
Differential diagnosis
- Other infection (fungal, bacterial, insect bite, parasitic, viral):
- Exclude with tissue cultures and stains for microorganisms (e.g., Fite, GMS, PAS, Gram stain)
- Histoplasmosis (similar size and appearance) but without kinetoplasts present in leishmaniasis (tissue and blood microbial cultures, urine antigen test, travel history)
- Toxoplasma gondii
- Penicillium marneffei
Practice question #1
What types of vectors are the various species of leishmaniasis transmitted by?
- Bees
- Sandflies
- Ticks
- Wasps
Practice answer #1
Practice question #2
What kind of microorganism is Leishmania?
- Ectoparasite
- Helminth
- Microsporidia
- Protozoan
Practice answer #2