Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Vaughan VC, Wisell J. Basaloid follicular hamartoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticbasaloidfollicularhamartoma.html. Accessed May 7th, 2024.
Definition / general
- Rare, benign cutaneous lesion associated with inherited syndromes
- Confused histologically with infundibulocystic basal cell carcinoma
Essential features
- Benign cutaneous hair follicle hamartoma
- Can occur as papule(s) or plaque
- May be solitary, linear or diffuse in distribution (Indian J Dermatol Venereol Leprol 2019;85:60)
- Confused histologically with basal cell carcinoma or other benign basaloid dermal growths
- May occur spontaneously or as the result of inherited disorders
Terminology
- Basaloid follicular hamartoma
- Generalized basaloid follicular hamartoma syndrome: autosomal dominant variant
- Linear unilateral basal cell nevus with comedones: childhood form occurring in a linear distribution, often along the lines of Blaschko and may have associated comedones
- Generalized hair follicle hamartoma: multiple basaloid follicular hamartomas and coexisting alopecia and myasthenia gravis (Patterson: Weedon's Skin Pathology, 4th Edition, 2015, Chapter 33)
ICD coding
- ICD-10: Q82.5 - congenital nonneoplastic nevus
Epidemiology
- Associated with certain autoimmune diseases: myasthenia gravis, alopecia, systemic lupus erythematosus
- Happle-Tinschert syndrome (Dermatology 2009;218:221)
- Bazex syndrome, aka Bazex-Dupre-Christol syndrome (X-linked dominant)
- Nevoid basal cell carcinoma syndrome, aka Gorlin syndrome, aka basal cell nevus syndrome
- Generalized basaloid follicular hamartoma (autosomal dominant mutation) (J Cutan Pathol 2008;35:477)
- Brown-Crounse syndrome
Sites
- Skin of the face, trunk, limbs, scalp, axilla and pubic area
- Distribution may be localized or generalized depending on the variant (Arch Pathol Lab Med 2010;134:1215)
Pathophysiology
- Can occur sporadically or in association with genetic mutations
- Mutated PTCH (protein patched homolog) gene leads to disrupted tumor suppressor function
- PTCH abnormally binds sonic hedgehog (Shh), a protein signal involved in embryogenesis
- Constitutive activation of downstream signaling in transcription factors like Gli-1 and abnormal growth ensues (Arch Pathol Lab Med 2010;134:1215)
- Associated with autoimmune disease
Clinical features
- May occur as solitary or multiple hypopigmented to hyperpigmented papules, commonly over the central face
- May occur as a plaque or coalescing papules
- Lesions may be associated with alopecia, hypertrichosis or open comedones (J Cutan Pathol 2008;35:477)
- Unilateral variants may follow lines of Blaschko and can be associated with underlying neurological findings (Korean J Radiol 2014;15:534)
Diagnosis
- Diagnosis relies on recognizing the specific pathologic features
- Correlation with clinical findings is required
- Some authors have discussed the utility of immunohistochemical studies in distinguishing basaloid follicular hamartoma from basal cell carcinoma (Arch Pathol Lab Med 2017;141:1490)
- Significant morphologic overlap between other benign tumors of the follicular infundibulum as well as infundibulocystic basal cell carcinoma exists; some have argued that infundibulocystic basal cell carcinoma and basaloid follicular hamartoma are the same entity (J Cutan Pathol 2014;41:916)
Case reports
- 3 month old and 8 year old boys with Blaschkoid hypopigmented papules (Pediatr Dermatol 2017;34:e196)
- 5 year old and 9 year old sisters with malar papules and comedones (J Cutan Pathol 2008;35:477)
- 7 year old boy with truncal hypopigmented papules and ipsilateral medulloblastoma, diagnosed with Happle-Tinschert syndrome (Dermatology 2009;218:221)
- 9 year old boy with unilateral papules over the chest with associated limb shortening and ipsilateral hemimegalencephaly diagnosed with Happle-Tinschert syndrome (Korean J Radiol 2014;15:534)
- 27 year old woman with Gorlin syndrome and many basaloid follicular hamartomas over the upper body (Pediatr Dermatol 2018;35:e396)
- 47 year old woman with generalized basaloid follicular hamartoma syndrome who developed basal cell carcinoma in a pre-existing basaloid follicular hamartoma (Am J Dermatopathol 2015;37:e37)
- 64 year old man with an isolated hyperpigmented macule over the cheek (Dermatol Online J 2017;23:15)
- 70 year old man with flesh colored firm papule and central depression over the forehead (Ann Dermatol 2010;22:229)
- Three siblings with consanguineous parents and generalized basaloid follicular hamartoma (Arch Dermatol 1995;131:454)
Treatment
- Not officially considered a premalignant lesion
- Close follow up to monitor for progression to basal cell carcinoma should be considered
- Some patients may be at greater risk for development of malignancy such as those with basal cell nevus syndrome
- Those that arise in the setting of autoimmune disease may resolve with treatment of the corresponding autoimmune disorder
- Surgical excision with carbon oxide laser therapy and dermabrasion have been successfully used in a 14 year old boy with unilateral facial basaloid follicular hamartoma with no recurrence at 11 years (J Dermatol 2017;44:e278)
- Pulsed dye laser therapy was used with some success in the treatment of acquired basaloid follicular hamartomas on the face of a 68 year old man (J Clin Aesthet Dermatol 2018;11:39)
- Three children with basal cell nevus syndrome who had extensive basal cell carcinomas and basaloid follicular hamartomas were treated with 5-aminolevulenic acid photodynamic therapy with satisfactory cosmetic results lasting at least 6 years (Arch Dermatol 2005;141:60)
- Oral and topical retinoids have been used with some efficacy in an isolated case (J Am Acad Dermatol 2003;49:1067)
Clinical images
Frozen section description
- Basaloid follicular hamartomas may be seen on frozen section, especially during Mohs surgery
- The same diagnostic criteria apply for frozen section diagnosis as for the evaluation of paraffin embedded tissue
- Distinguishing between basaloid follicular hamartoma and basal cell carcinoma on frozen section is challenging
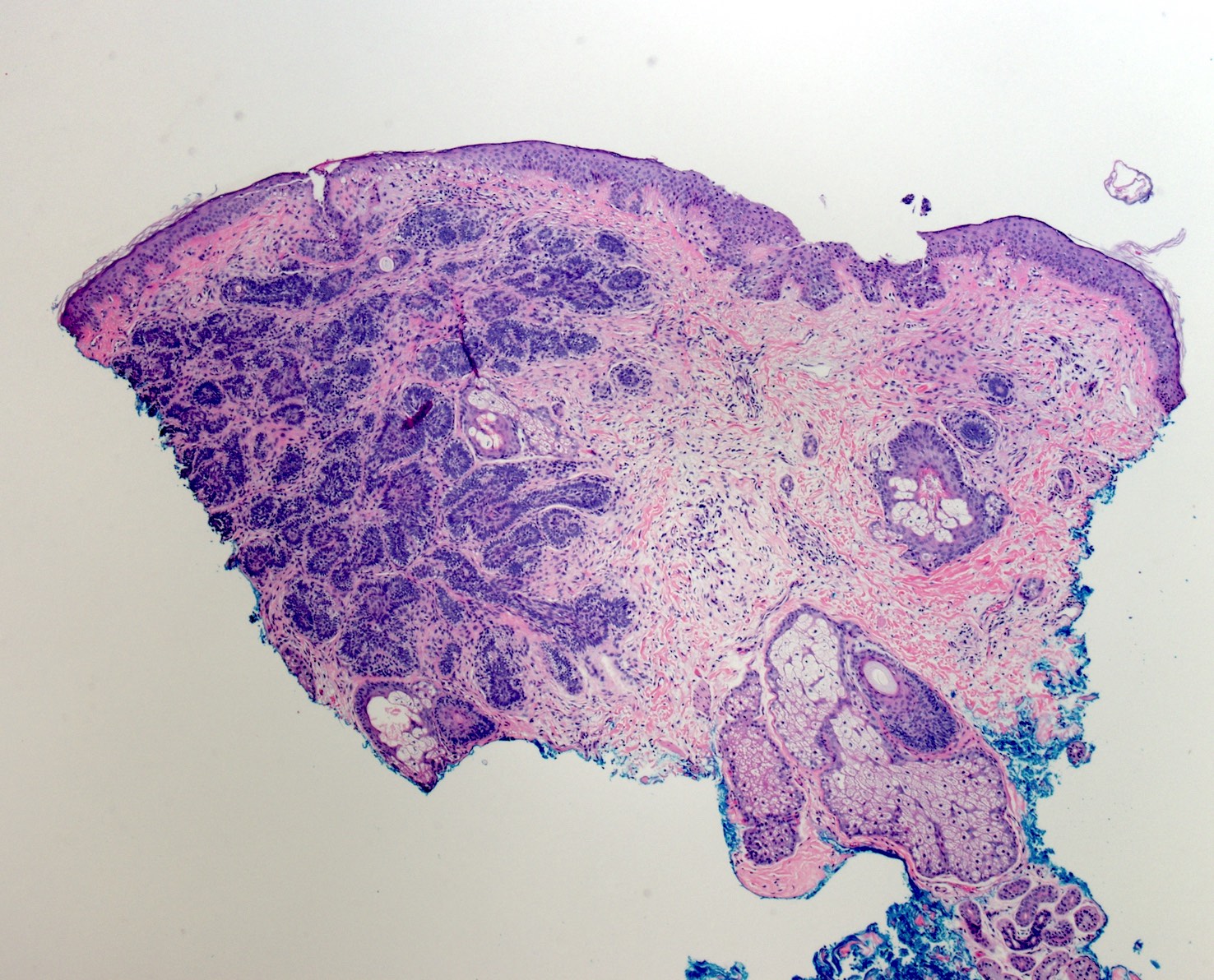
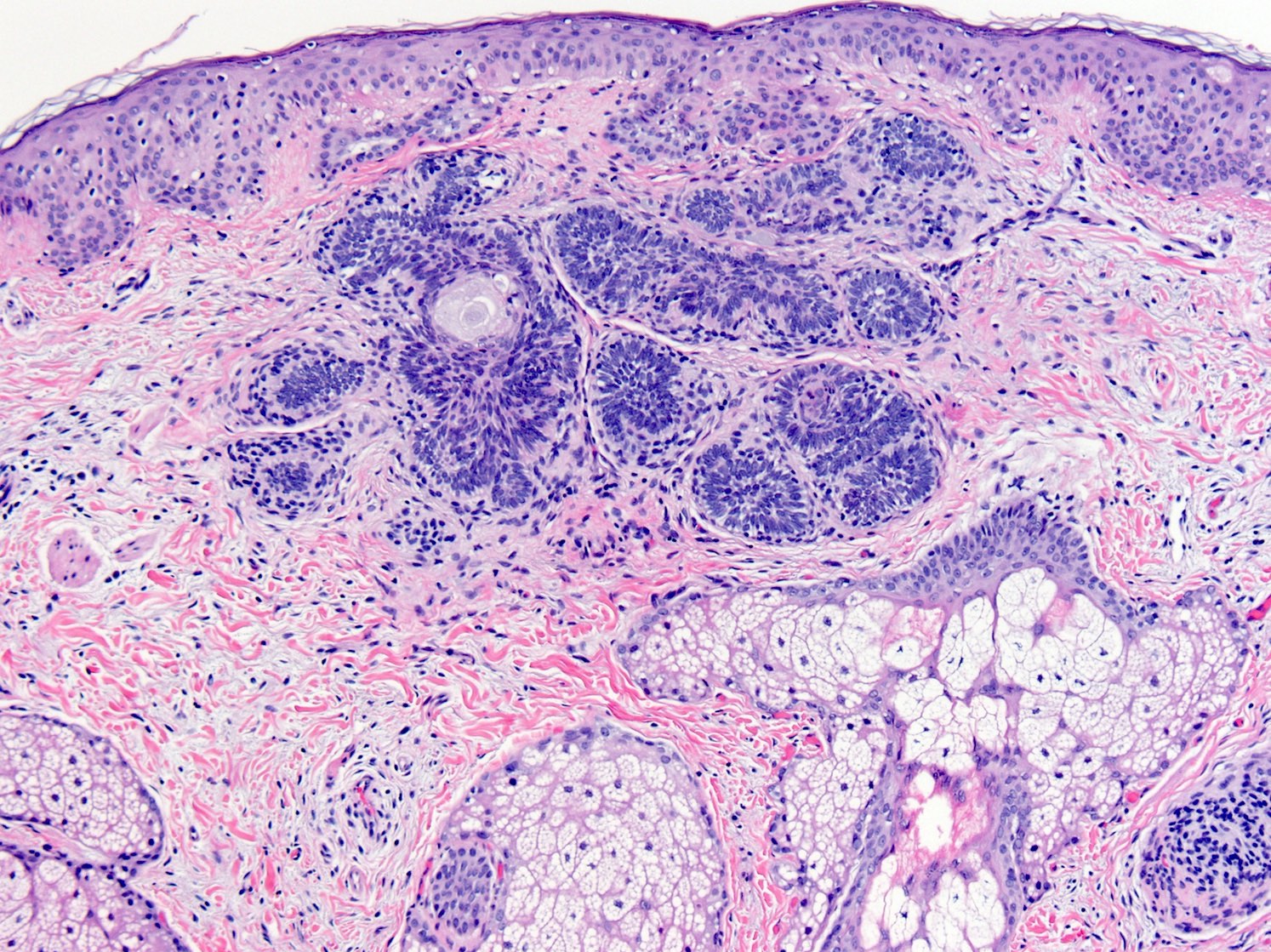
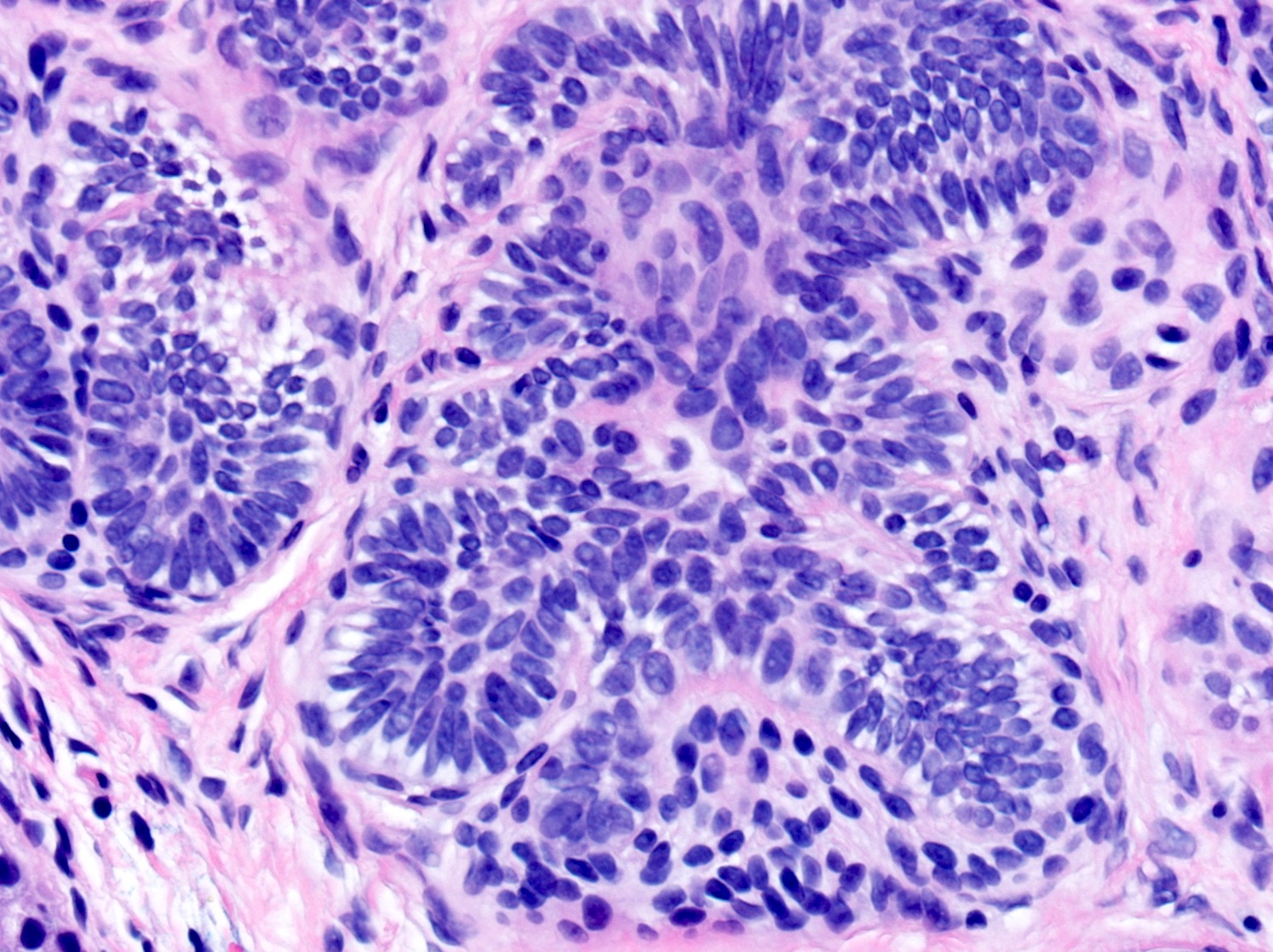
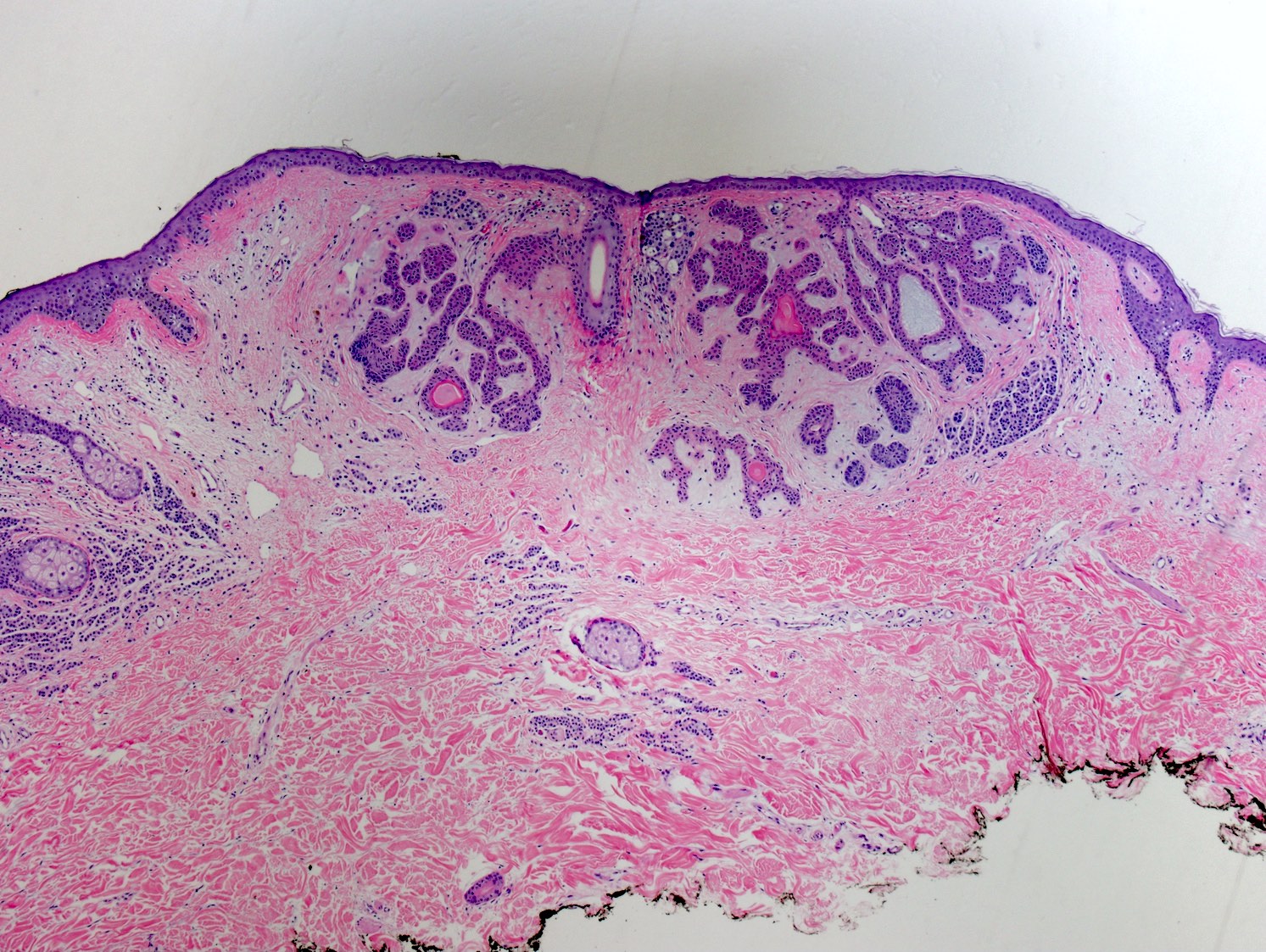
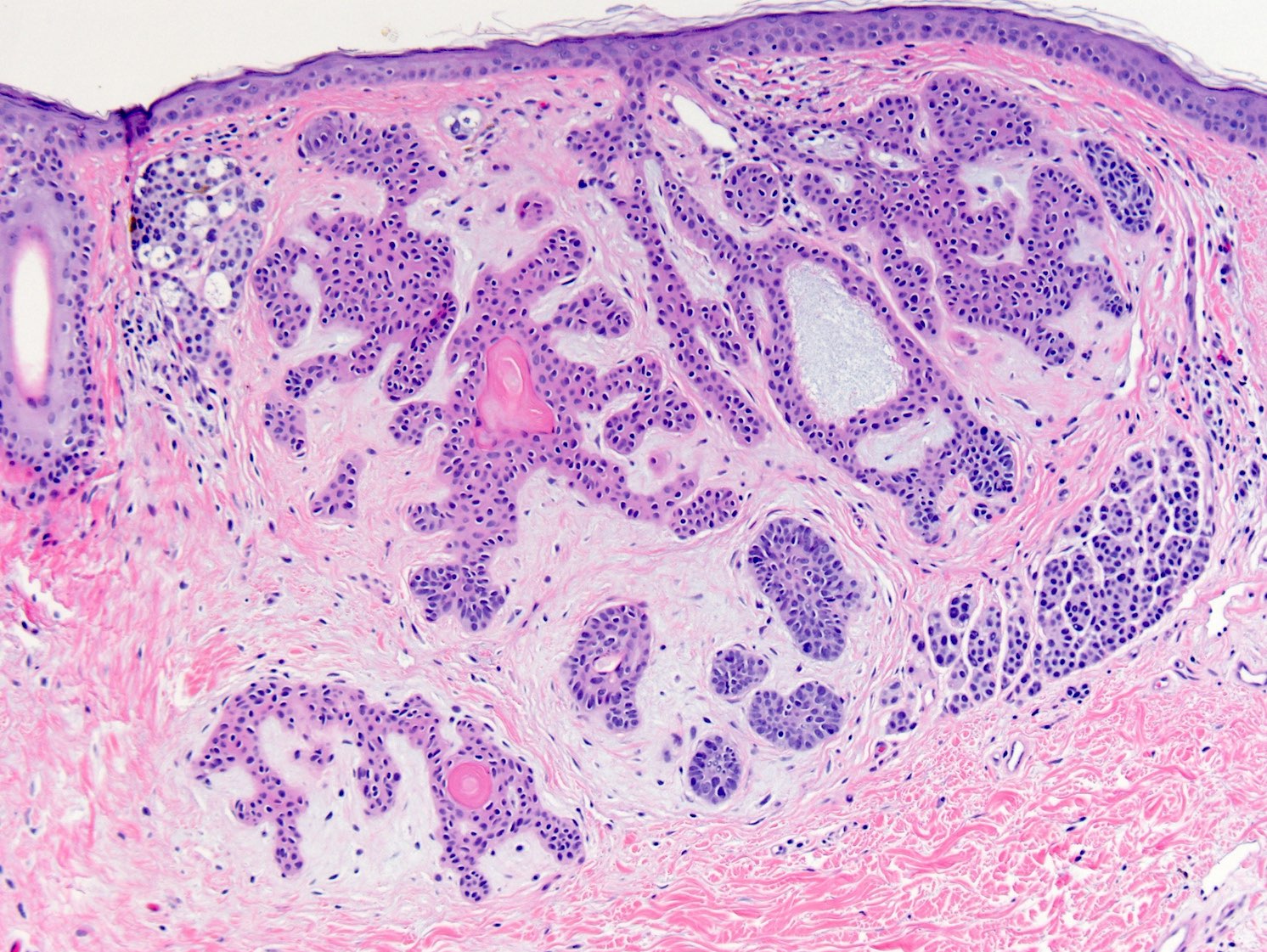
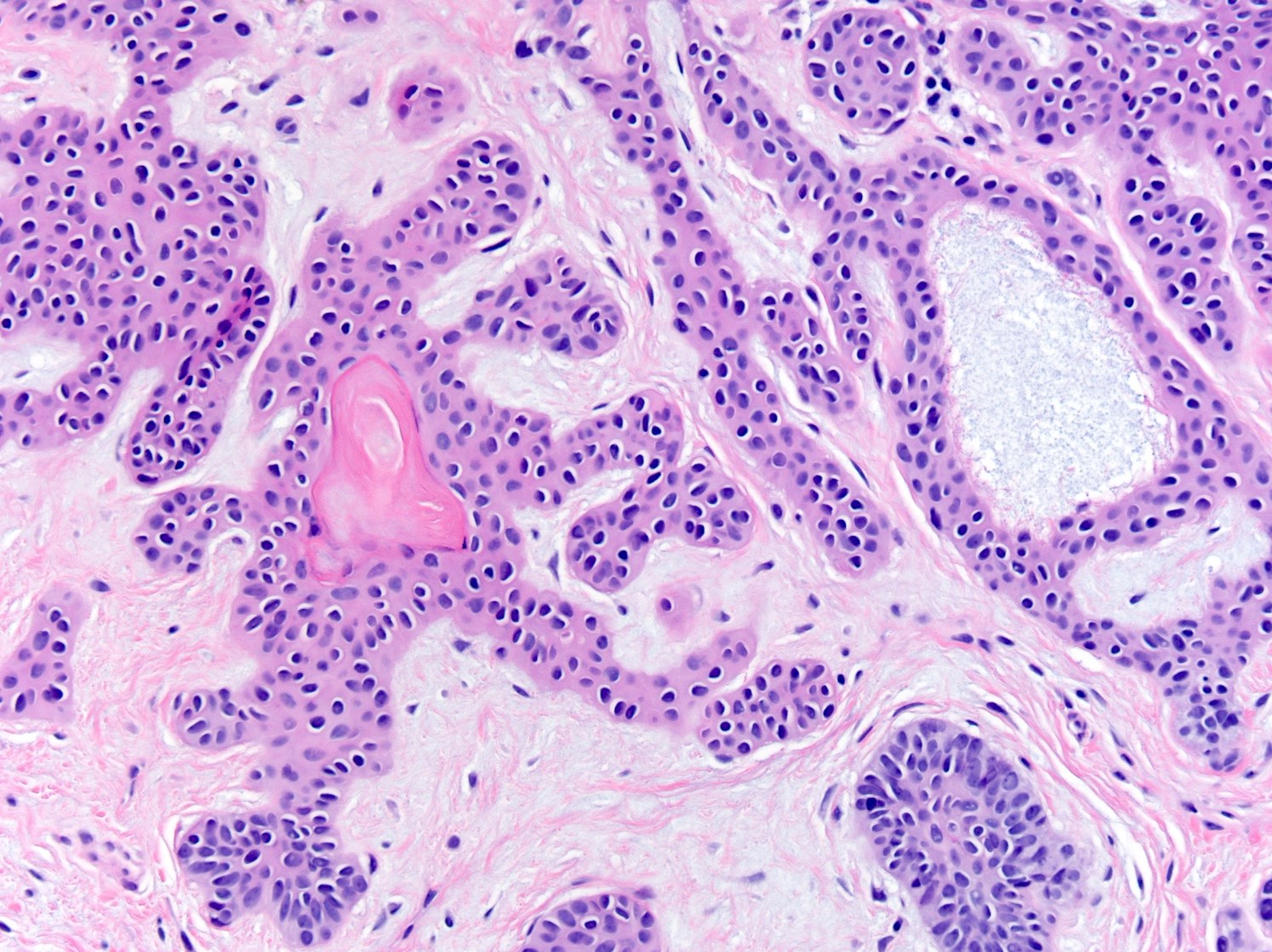
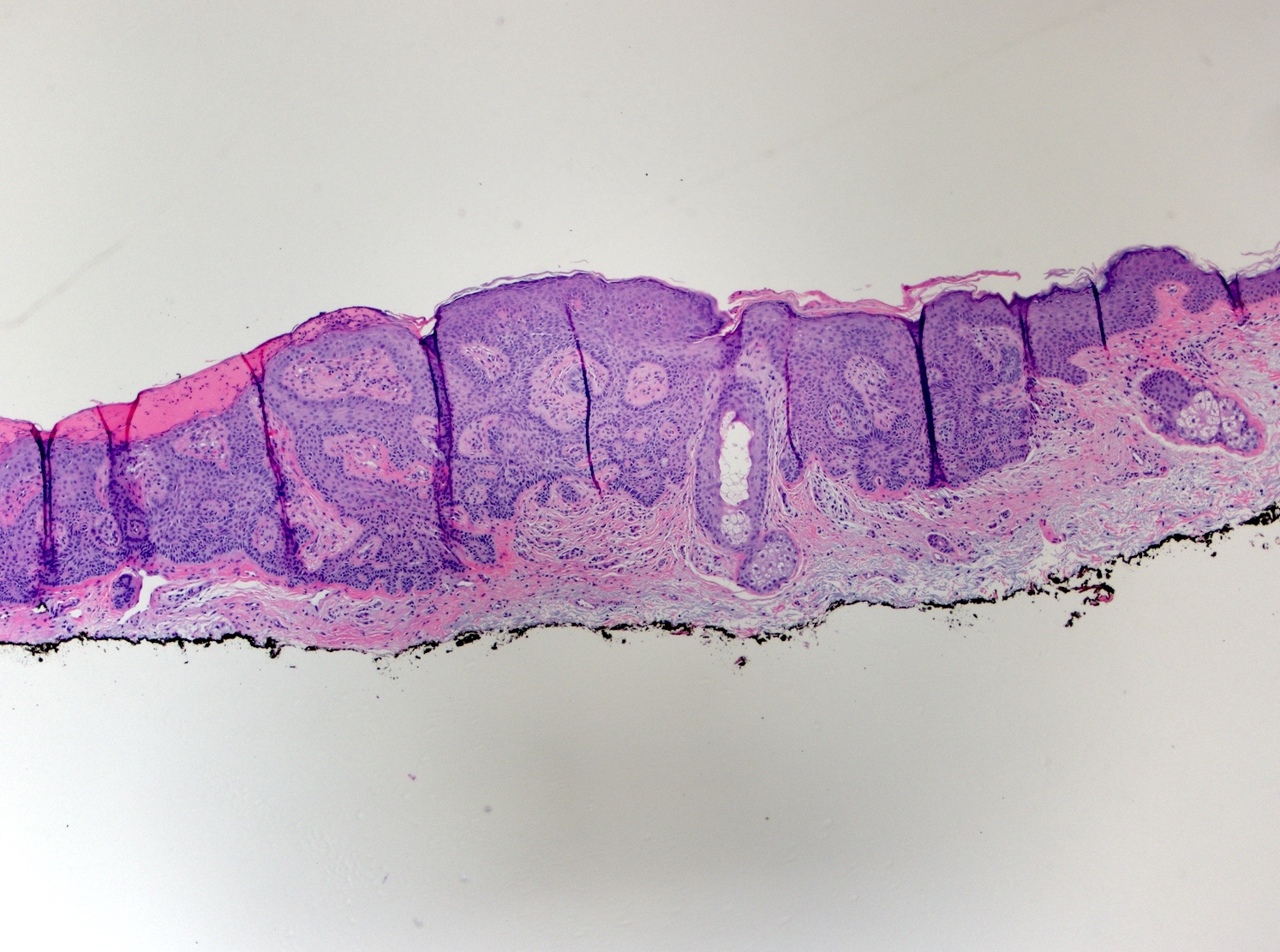
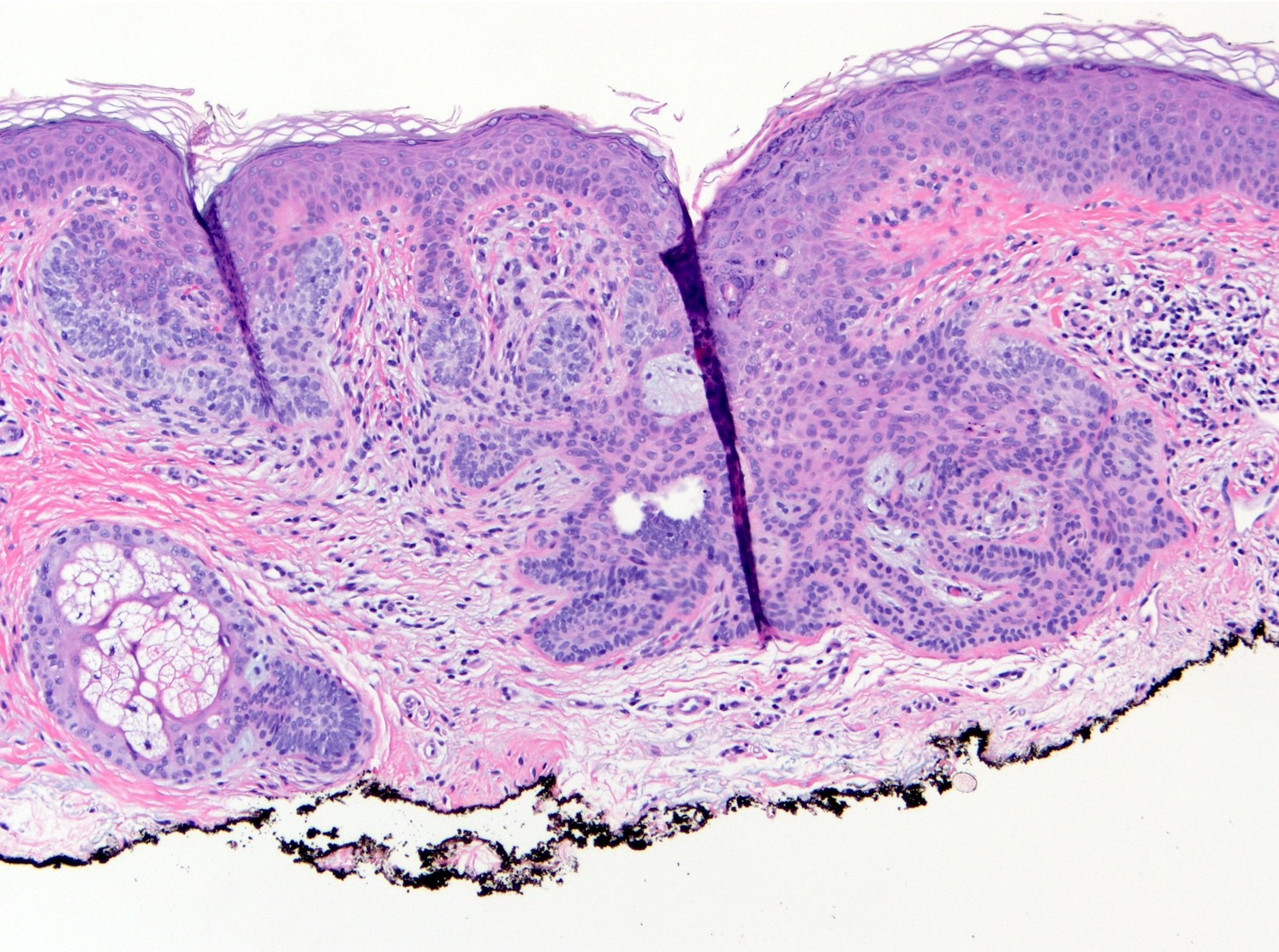
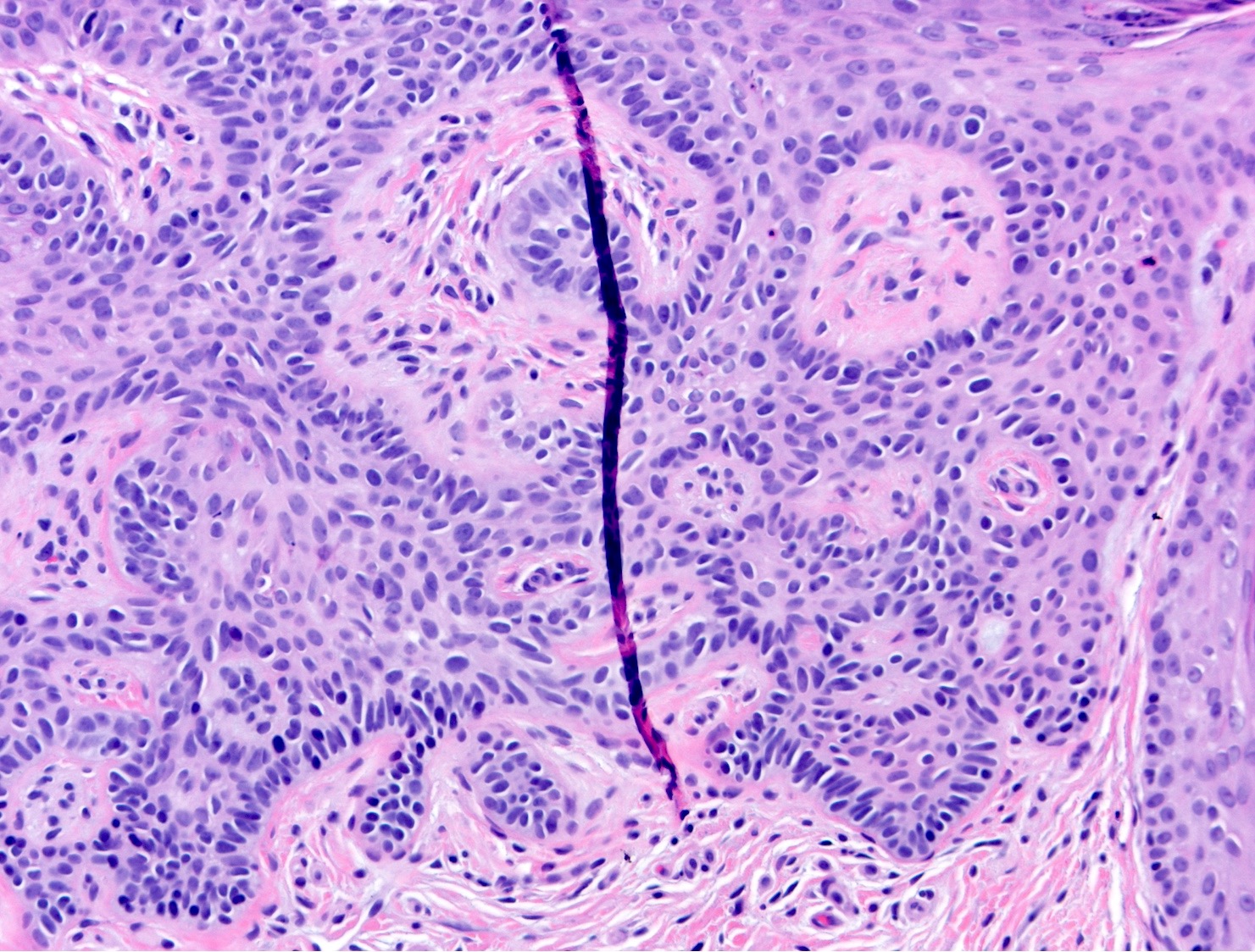
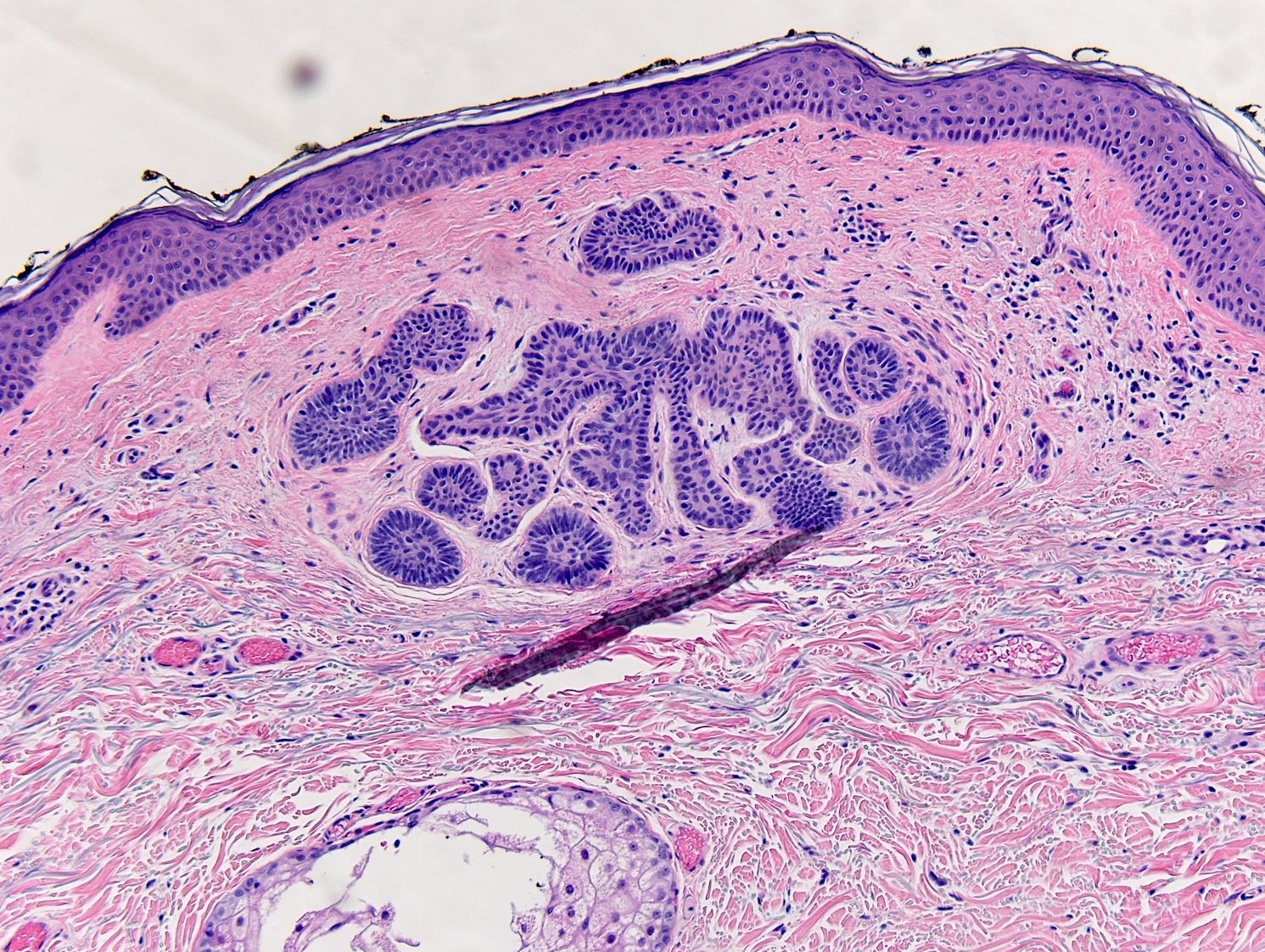
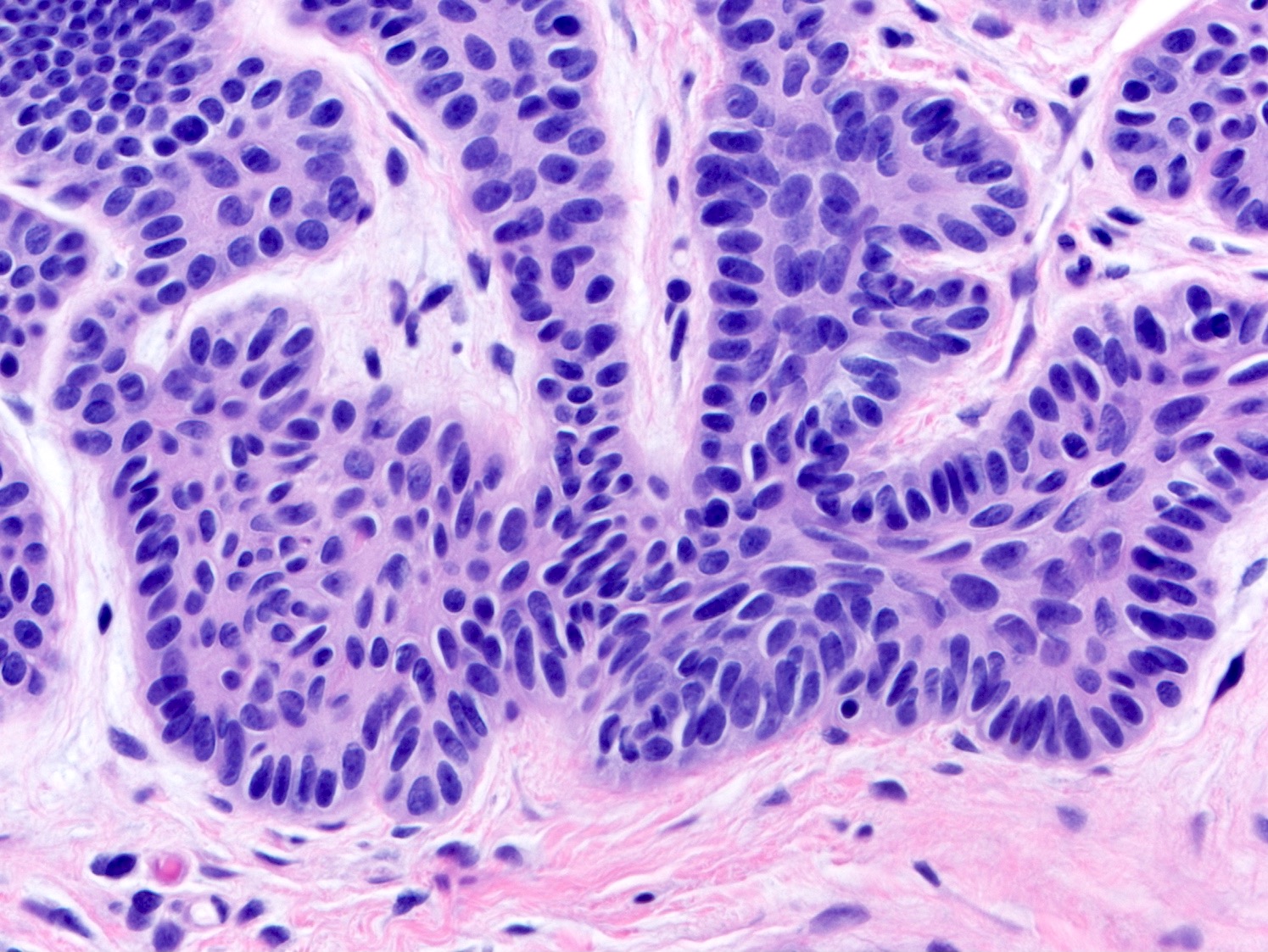
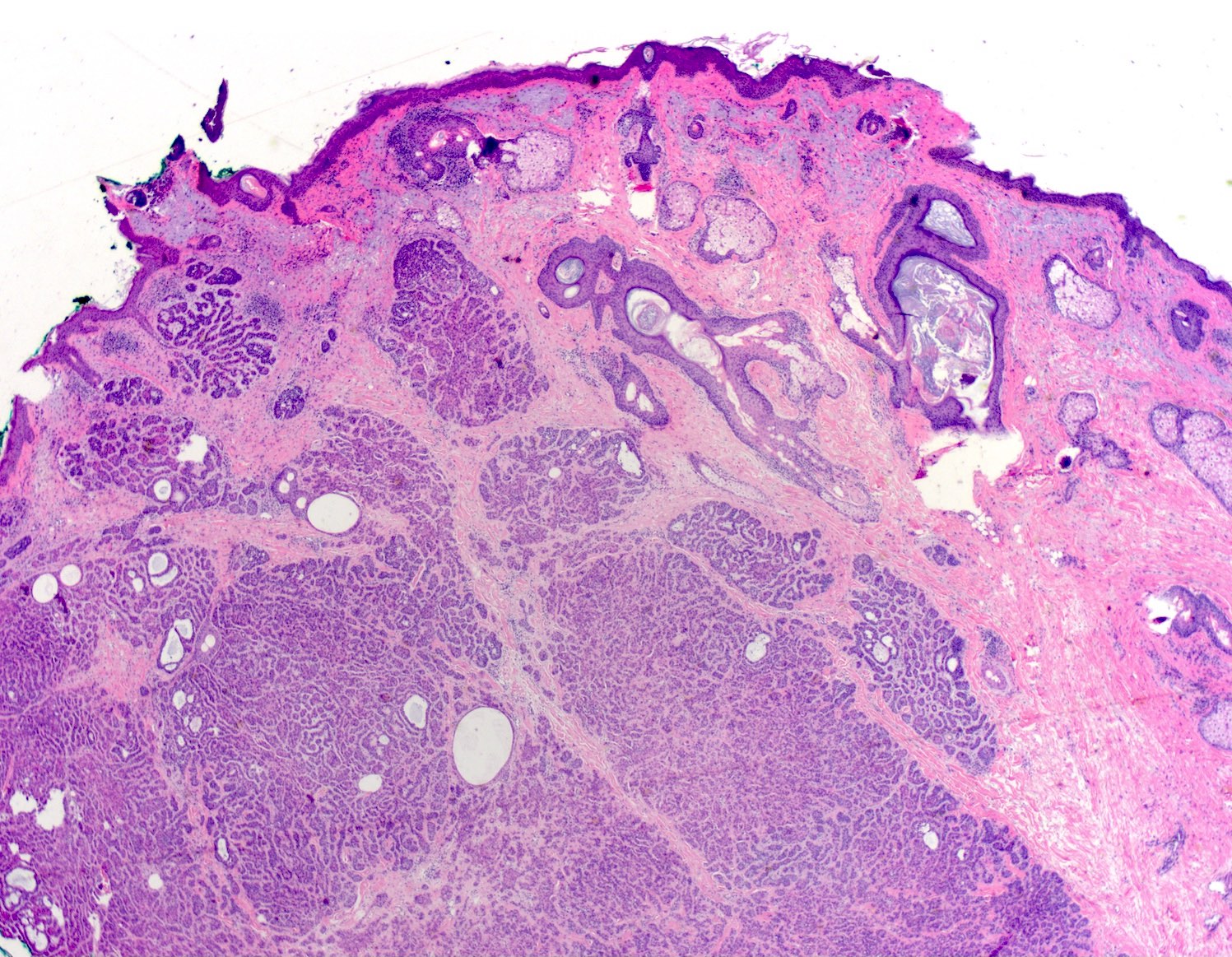
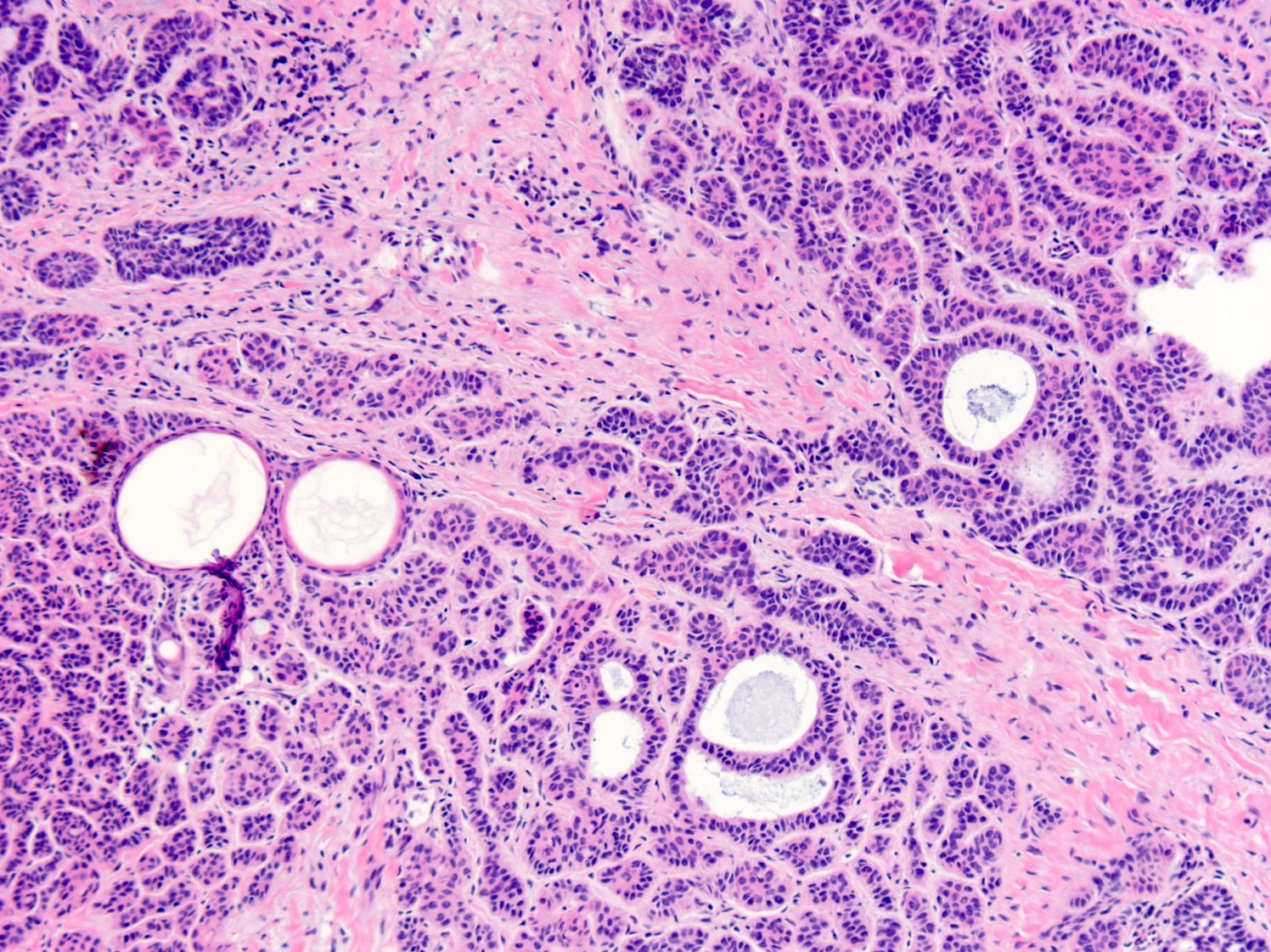
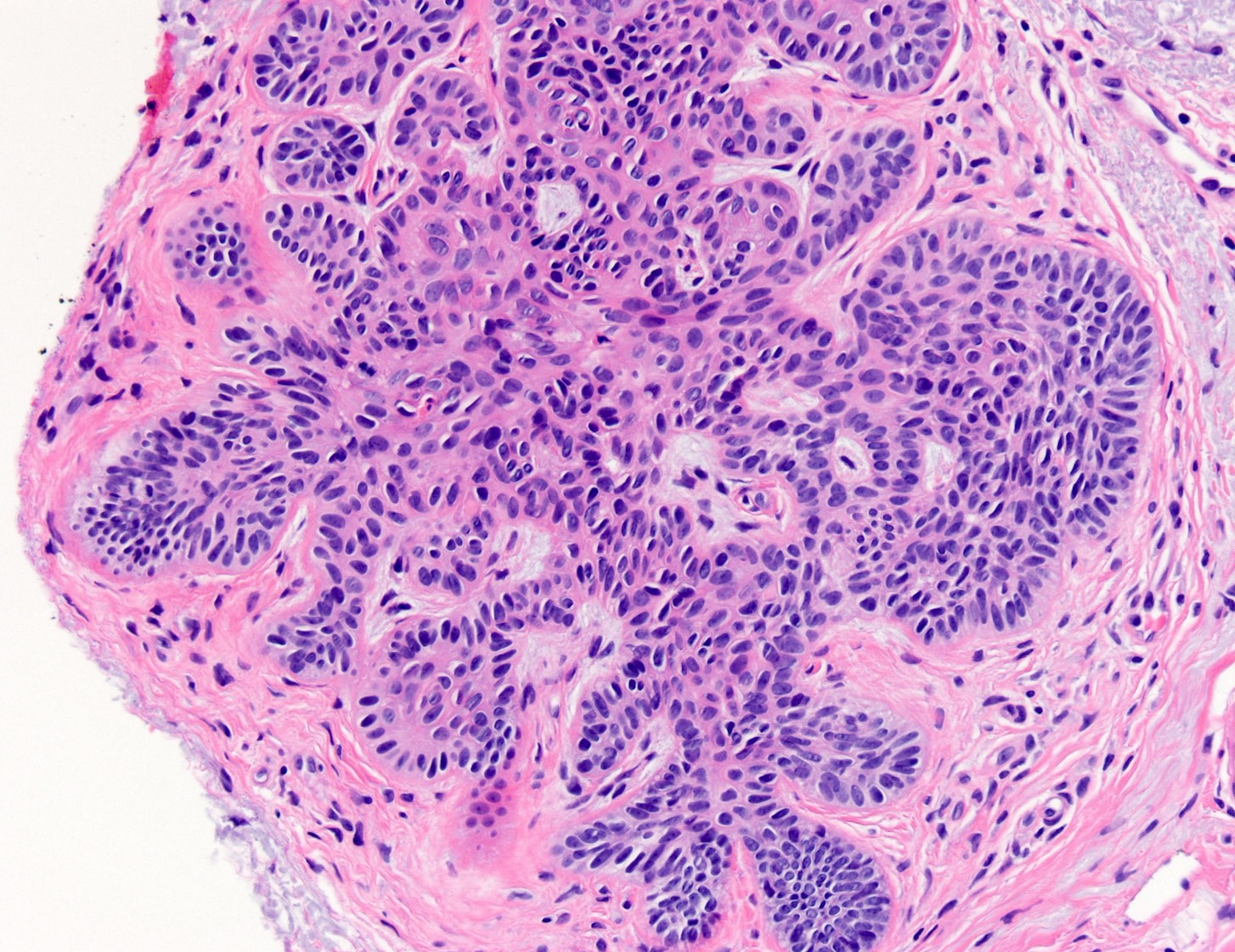
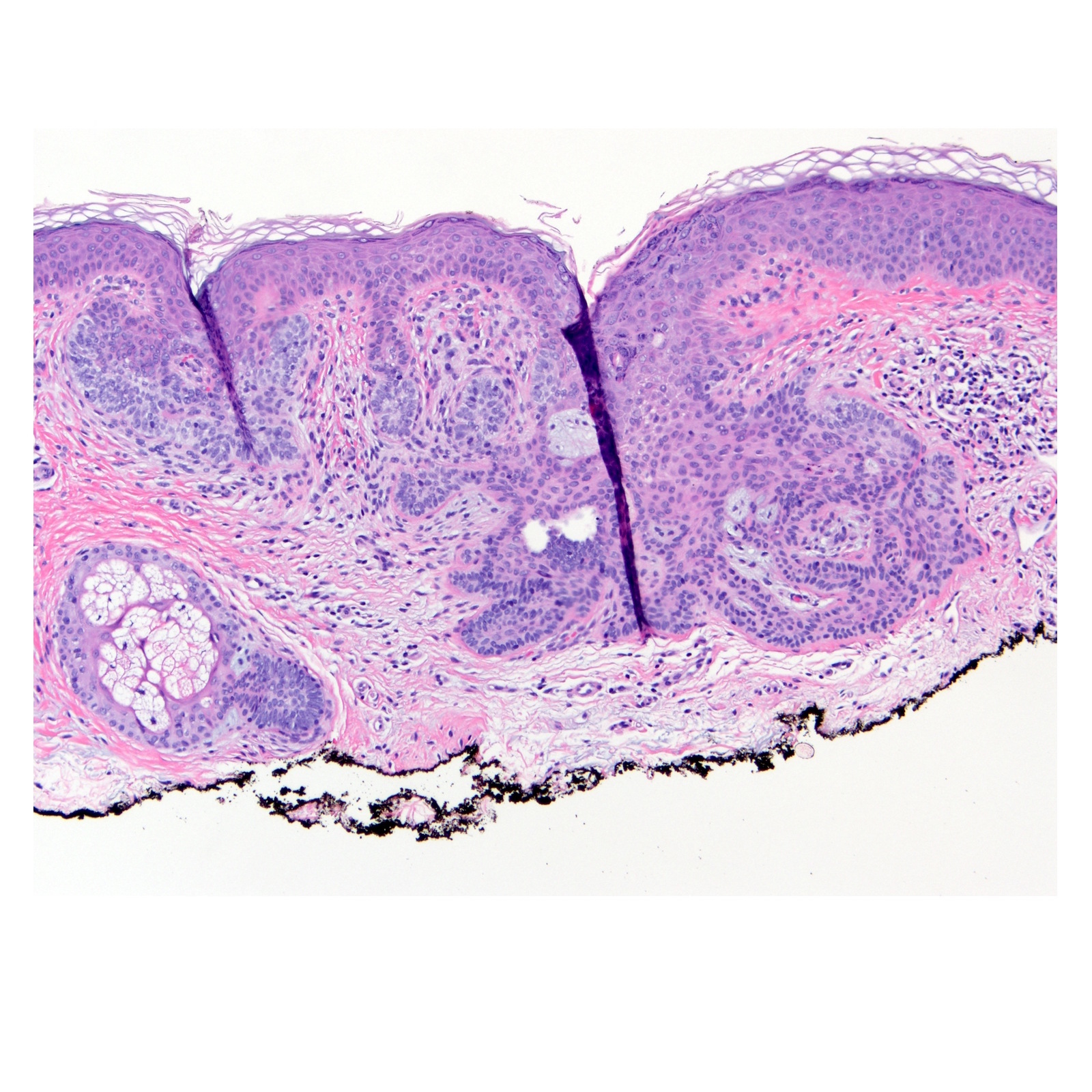
Microscopic (histologic) description
- Anastomosing strands of basaloid and squamoid cells with connection to the overlying epithelium
- Should only arise where normal hair follicles are present
- Bland cells without atypia, mitoses or apoptotic bodies
- Loose, cellular or myxoid stroma
- Horns, cysts and pigmentation may be present
- If peripheral palisading and retraction are present, they should be focal and less than the amount typically seen within basal cell carcinoma (Arch Pathol Lab Med 2010;134:1215)
Microscopic (histologic) images
Positive stains
- BCL2: stains peripheral basaloid cells; a diffuse staining pattern is observed in all basaloid cells in basal cell carcinoma
- CD34: stains the stroma around basaloid cells; the stroma in basal cell carcinoma may only rarely stain with CD34 (J Cutan Pathol 2001;28:538)
- CD10: stains the stroma around basaloid cells; both the stroma and basaloid cells in basal cell carcinoma may stain with CD10
- P40: strongly positive in basaloid cells
- CK20: focal positivity has been reported (J Cutan Pathol 2014;41:916)
- There is no specific immunohistochemical study for basaloid follicular hamartoma and studies analyzing sensitivity and specificity of markers are limited by the availability of this rare tumor
Negative stains
- Immunohistochemistry has not been widely studied in basaloid follicular hamartoma
Molecular / cytogenetics description
- Targeted next generation sequencing may be helpful in the diagnosis of patients with syndromic phenotypes
- The first family described with generalized basaloid follicular hamartoma was in North Carolina; there were 6 generations of affected members who had multiple flesh colored and hyperpigmented papules over the face, neck, trunk and arms, palmar / solar pits, scalp alopecia, milia and comedones (J Am Acad Dermatol 2000;43:189)
- The PTCH1 gene on chromosome 9q23 is implicated in both generalized basaloid follicular hamartoma syndrome (GBFH) and Gorlin syndrome; basaloid follicular hamartomas occur in both syndromes and some have suggested that these two diseases are on a spectrum (Anticancer Res 2018;38:471)
- Basal cell nevus syndrome may also arise as a result of PTCH2 mutation or SUFU mutation, a signaling molecule in the same pathway; as opposed to generalized basaloid follicular hamartoma syndrome, basal cell nevus syndrome is defined by the presence of jaw keratocysts, calcification of the falx cerebri, bifid ribs and macrocephaly
Videos
Clinical phenotype and molecular genetics of Basal cell nevus syndrome
Sample pathology report
- Skin, cheek, biopsy:
- Cutaneous adnexal neoplasm, morphologically consistent with basaloid follicular hamartoma (see comment)
- Comment: Basaloid follicular hamartoma demonstrates significant overlap between basal cell carcinoma and has been shown to progress to malignancy in some cases. Increased surveillance or complete surgical excision may be required depending upon the clinical circumstances.
- Microscopic description: Anastomosing cords of bland basaloid cells with peripheral palisading and surrounding cellular stroma. Rare papillary mesenchymal bodies are noted. Absent are mitoses, apoptotic bodies and atypical nuclear features.
Differential diagnosis
- Infundibulocystic basal cell carcinoma:
- Strikingly similar appearance to basaloid follicular hamartoma but is more likely to have atypia and mitoses
- Stromal retraction should be more prominent in basal cell carcinoma
- Some have discussed the presence of a myxoinflammatory stroma as a helpful distinguishing feature
- Clinical correlation and immunohistochemistry may aid in the diagnosis (Arch Pathol Lab Med 2017;141:1490)
- Trichoepithelioma / trichoblastoma:
- Benign tumor composed of separate islands of basaloid cells which may have peripheral palisading
- Islands may branch and are surrounded by a loose to fibrotic stroma
- Papillary mesenchymal bodies may be seen
- The presence of distinct rounded islands as opposed to multiple branching anastomoses signals the diagnosis
- Tumor of the follicular infundibulum:
- Helpful distinguishing features are a growth pattern along the dermal epidermal junction resembling superficial basal cell carcinoma with fenestrated areas
- Another helpful feature is the presence of pale staining glycogen containing cells that are reminiscent of trichilemmoma
- Pilar sheath acanthoma:
- Cystically dilated follicle with radiating acanthotic epithelial projections
- Trichofolliculoma:
- Central large dilated follicle surround by smaller secondary follicles
Board review style question #1
Board review style answer #1
B. Basaloid follicular hamartoma
Explanation: A) Basal cell carcinoma should have atypia; C) While, syringoma will have basaloid cells in the dermis, they are separate, small “comma-shaped” islands; D) Trichoblastoma will have rounded basaloid islands in the dermis that may focally connect as opposed to the more predominantly branching stranded pattern of basaloid follicular hamartoma; E) The classic intensely eosinophilic basement membrane material normally found in spiradenoma is lacking in this biopsy as is the “blue balls in the dermis” architecture
Reference: Basaloid follicular hamartoma
Comment Here
Explanation: A) Basal cell carcinoma should have atypia; C) While, syringoma will have basaloid cells in the dermis, they are separate, small “comma-shaped” islands; D) Trichoblastoma will have rounded basaloid islands in the dermis that may focally connect as opposed to the more predominantly branching stranded pattern of basaloid follicular hamartoma; E) The classic intensely eosinophilic basement membrane material normally found in spiradenoma is lacking in this biopsy as is the “blue balls in the dermis” architecture
Reference: Basaloid follicular hamartoma
Comment Here
Board review style question #2
- Basaloid follicular hamartoma has been reported to occur in both sporadic and syndromic forms. With which of the following syndromes is basaloid follicular hamartoma associated?
- Birt-Hogg Dubé syndrome
- Gorlin Syndrome
- Lynch Syndrome
- Rothmund Thomson
- Tuberous sclerosus
Board review style answer #2
B. Gorlin syndrome / Basal cell nevus syndrome
Explanation: A) Birt-Hogg Dubé is associated with fibrofolliculoma, trichodiscomas and acrochordons; C) the Muir-Torre variant of Lynch is associated with sebaceous adenoma, sebaceous adenocarcinoma and squamous cell carcinoma; D) Rothmund Thomson is characterized by poikiloderma and increased risk of basal cell carcinoma and squamous cell carcinoma among other findings; E) Tuberous sclerosis is associated with angiofibromas, subungual fibromas, connective tissue hamartomas (Shagreen patch) and hypomelanotic macules
Reference: Basaloid follicular hamartoma
Comment Here
Explanation: A) Birt-Hogg Dubé is associated with fibrofolliculoma, trichodiscomas and acrochordons; C) the Muir-Torre variant of Lynch is associated with sebaceous adenoma, sebaceous adenocarcinoma and squamous cell carcinoma; D) Rothmund Thomson is characterized by poikiloderma and increased risk of basal cell carcinoma and squamous cell carcinoma among other findings; E) Tuberous sclerosis is associated with angiofibromas, subungual fibromas, connective tissue hamartomas (Shagreen patch) and hypomelanotic macules
Reference: Basaloid follicular hamartoma
Comment Here