Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Wilson K, Esposito M, Giubellino A. Tumor of the follicular infundibulum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocytictumorfollicularinfundibulum.html. Accessed September 26th, 2025.
Definition / general
- Rare, benign neoplasm that was first described in 1961 as a plate-like subepidermal epithelial tumor with a fenestrated growth pattern, cells with light staining nuclei and vesiculated cytoplasm (Arch Dermatol 1961;83:924)
Essential features
- Horizontal, plate-like organization of epithelial cells with abundant cytoplasm under the epidermis between adjacent infundibulum
- Dense elastic network beneath the tumor
- Anastomosing pale keratinocytes without atypia
Terminology
- Tumor of the follicular infundibulum (TFI)
- Infundibular tumor
- Tumor of the follicular isthmus
- Infundibuloma
ICD coding
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
Epidemiology
- 3 - 17/100,000 skin biopsies
- 60 - 70 year old adults
- Associated with Cowden syndrome (J Am Acad Dermatol 1995;33:979)
- Associated with Schöpf-Schulz-Passarge syndrome (Dermatology 1998;196:463)
- Associated with basal cell carcinoma (BCC), squamous cell carcinoma (SCC), nevi, acne scars, actinic keratosis, Hansen disease, vitiligo, discoid lupus erythematosus and lichen planus (J Cutan Pathol 2013;40:532)
- There is a slight female predominance but some report equal distribution (Case Rep Pathol 2019;2019:4606493, J Cutan Pathol 2013;40:532, Int J Dermatol 1996;35:282)
Sites
- Head, neck, trunk
- Other unusual reported areas include the vulva, other genital areas and extremities (Case Rep Pathol 2019;2019:4606493, An Bras Dermatol 2014;89:964, J Cutan Pathol 2013;40:532)
Pathophysiology
- Adnexal follicular proliferation with isthmic differentiation of the follicular epidermis
- Multiple infundibulomas accounts for ~7% of cases (J Cutan Pathol 2013;40:532)
- Currently debated among researchers; there are few case reports of tumor of the follicular infundibulum with sebaceous differentiation (Ann Dermatol 2011;23:198)
Etiology
- Etiology is not fully understood at this time
- Predominantly isthmic differentiation but sebaceous differentiation has been described (J Cutan Pathol 2001;28:314, Ann Dermatol 2011;23:198)
- Part of a nevus sebaceous (Korean J Pathol 2013;47:569, J Cutan Pathol 2015;42:645)
- Epidermal reaction to dermal fibrosis (Am J Dermatopathol 2015;37:535)
- Spectrum of basal cell carcinoma (Am J Dermatopathol 2009;31:634)
Clinical features
- Variable clinical presentation, although typically presents as hypopigmented, scar-like macules or flat papule on the head, neck or trunk
- Can present as a solitary papule / plaque or multiple eruptive macules / papules, both hyperpigmented and hypopigmented lesions have been described
Diagnosis
- Typically diagnosed on biopsy given the variable clinical presentation and overlapping features with other entities, including basal cell carcinoma, benign lichenoid keratosis and vitiligo
- Only histology with critical features can make the diagnosis (Int J Dermatol 1996;35:282)
- Critical biopsy features include
- Plate-like, horizontal growth
- Interconnected with elastin fibers
- Pale, abundant cytoplasm without cytologic atypia
Prognostic factors
- Benign
- Tumors of the follicular infundibulum or infundibulomas can arise in conjunction with other lesions and although not fully elucidated, have been reported to be associated with many entities across the spectrum from benign to malignant lesions, including basal cell carcinoma, actinic keratosis, desmoplastic malignant melanoma, junctional melanocytic nevus, epidermal inclusion cyst, among many others; extensively documented by Dempsey et al. (JAAD Case Rep 2018;5:15)
Case reports
- 53 year old man and 54 year old woman with TFIs that presented as flat, erythematous macules, both with chrysalis on dermoscopy (Skin Res Technol 2019;25:761)
- 69 year old man with atypical brown macule and an associated dysplastic nevus biopsied to rule out melanoma (JAAD Case Rep 2018;5:15)
- 70 year old woman with a vulvar ulcerated lesion with lichenoid change (Case Rep Pathol 2019;2019:4606493)
- 28 patients with TFI features (J Dtsch Dermatol Ges 2024;22:223)
Treatment
- Surgical excision typically curative
- Topical therapies, including keratolytics and corticosteroids, have been reported but were ineffective (Dermatol Online J 2010;16:14)
- Single case report of patient on etretinate showing slight improvement (Ann Dermatol Venereol 1987;114:55)
- Cryotherapy has shown some success (Int J Dermatol 1996;35:282)
- Long term follow up may be recommended due to (rare) potential for malignant transformation (JAAD Case Rep 2018;4:330)
Clinical images
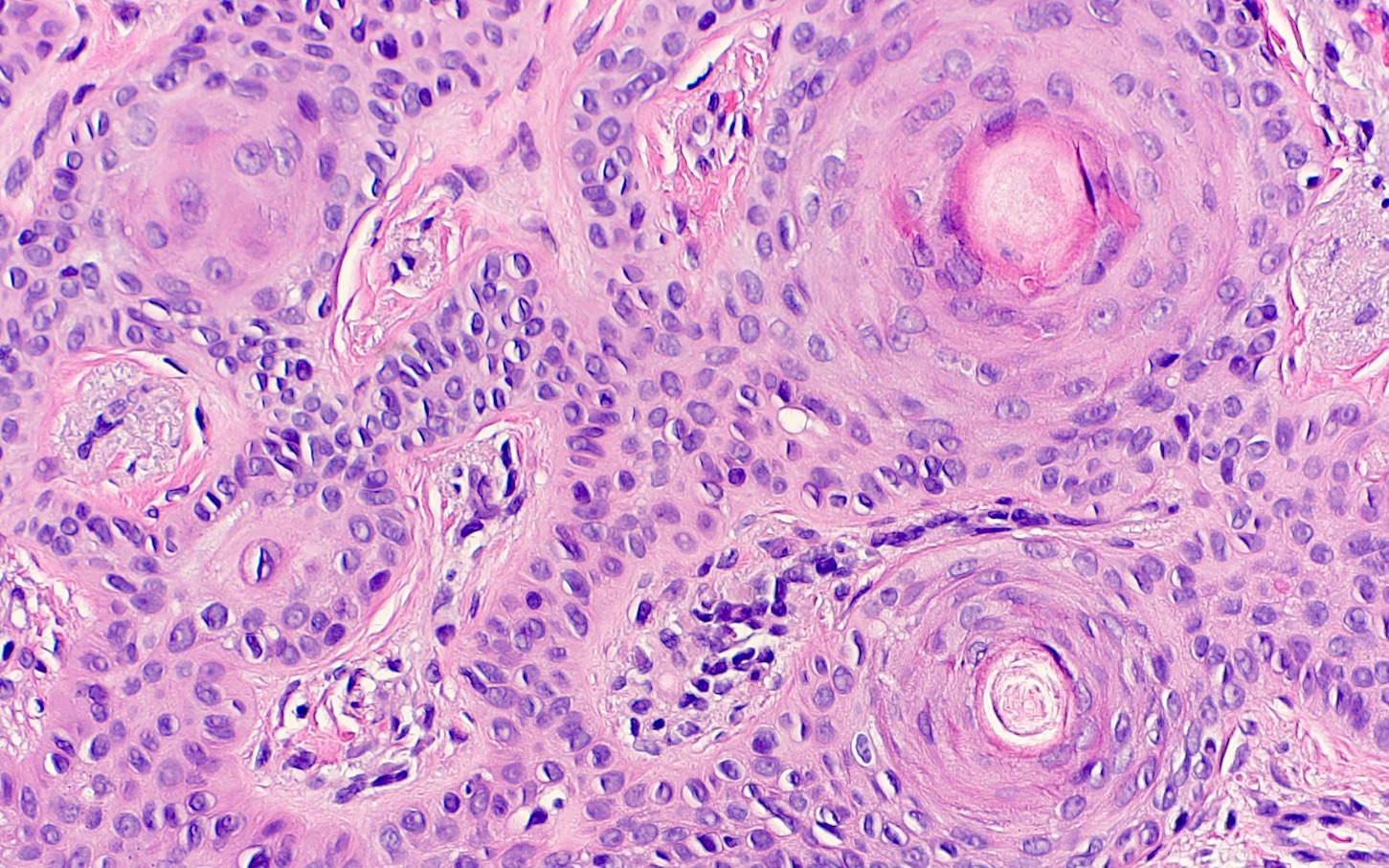
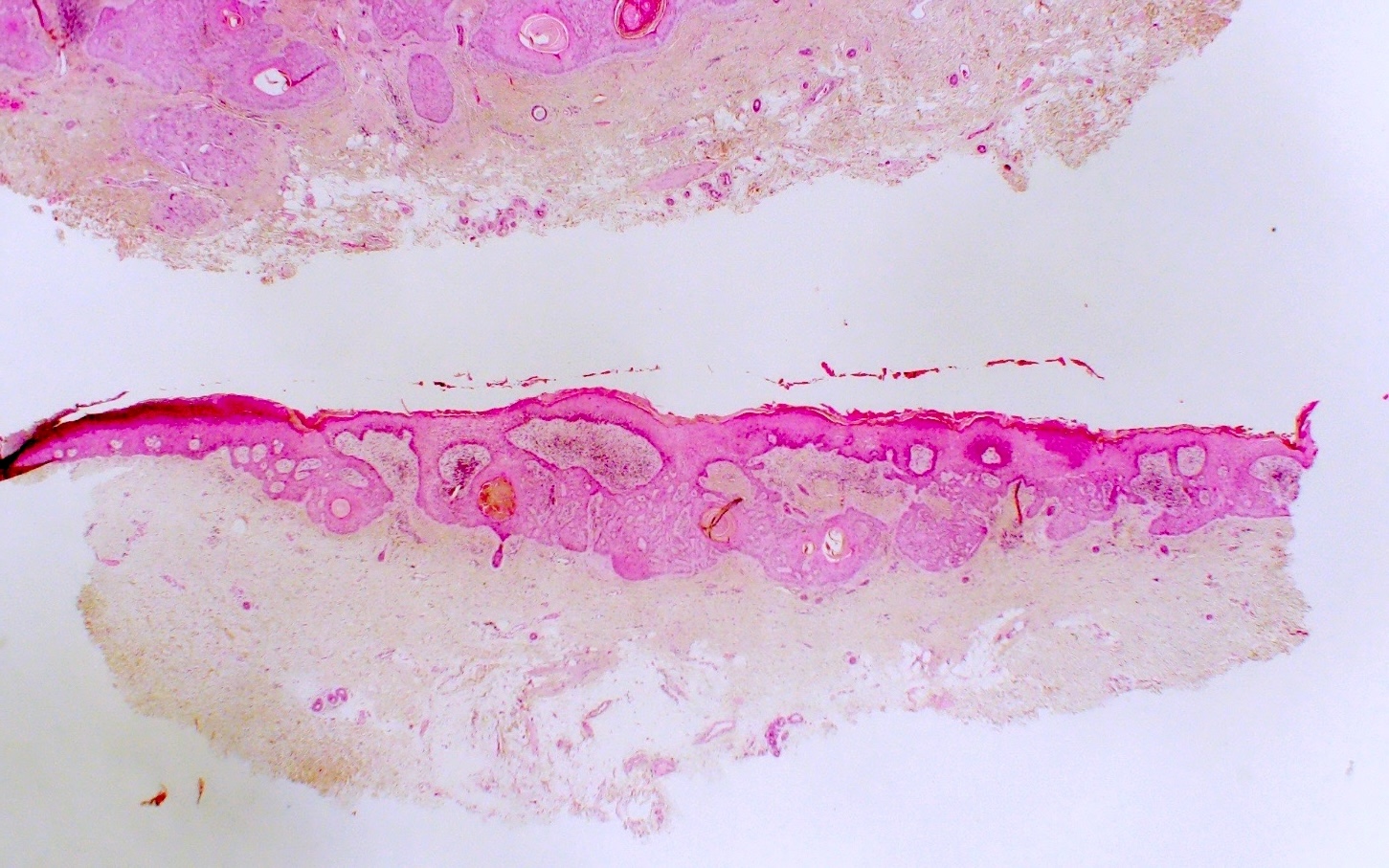
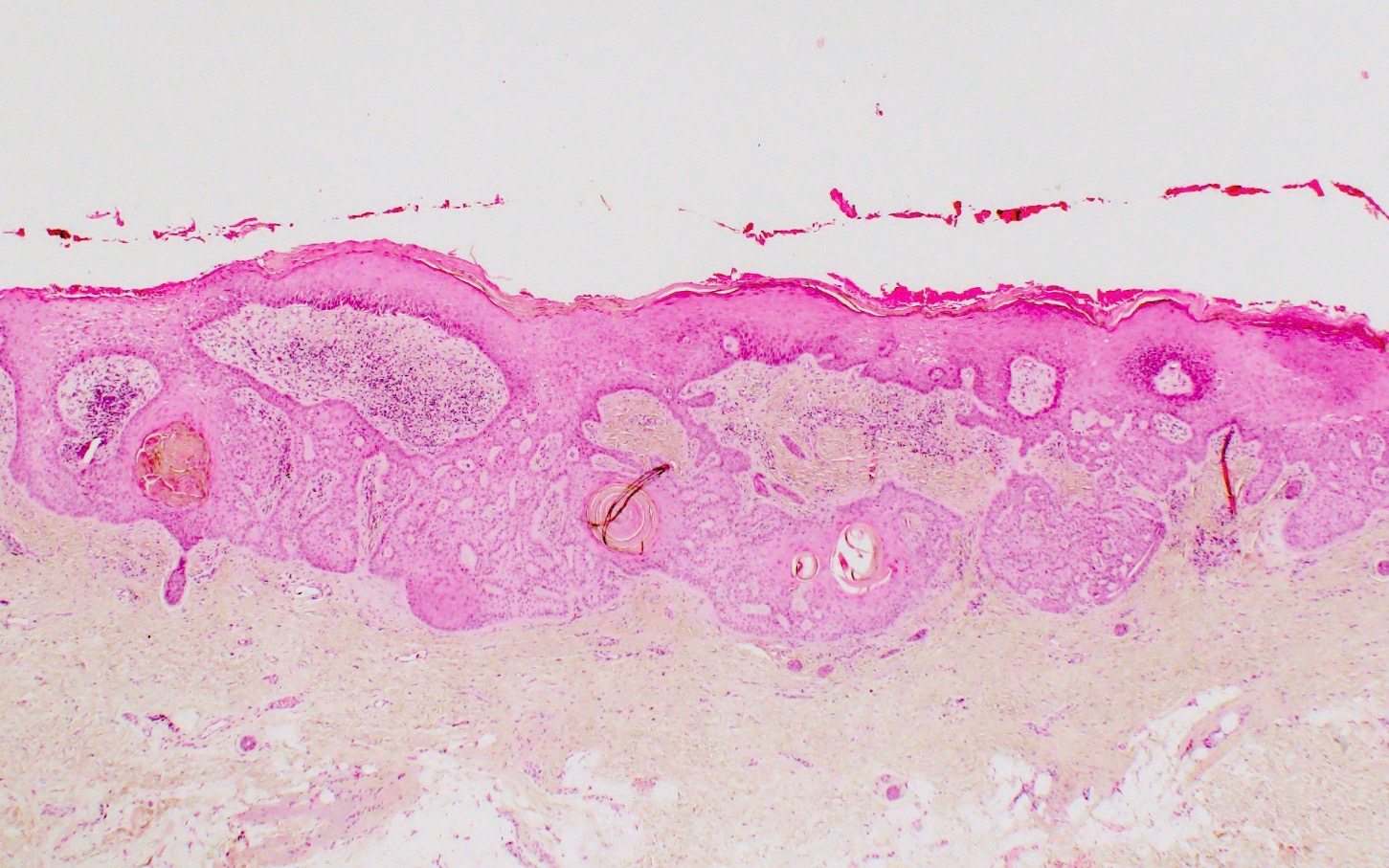
Microscopic (histologic) description
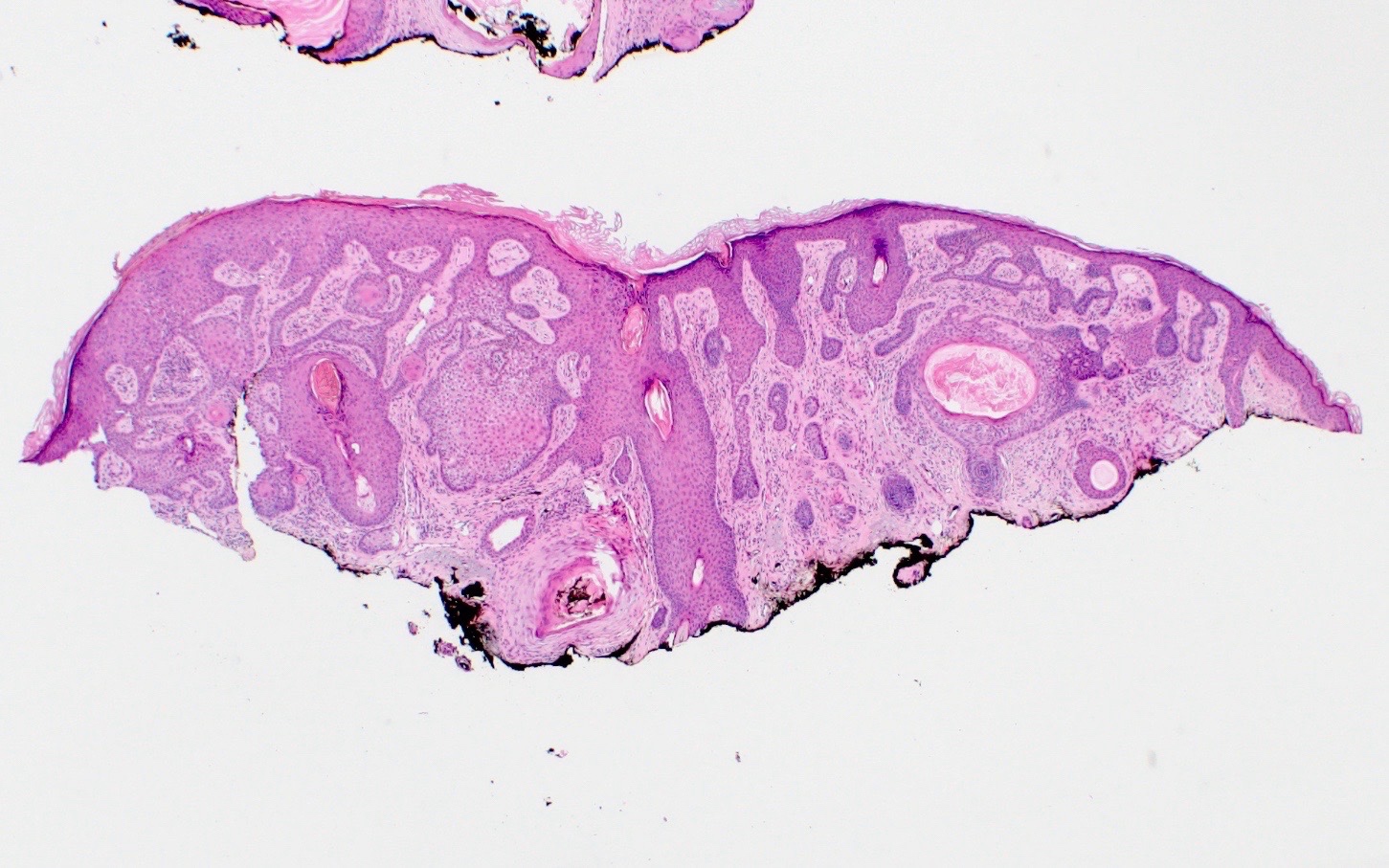
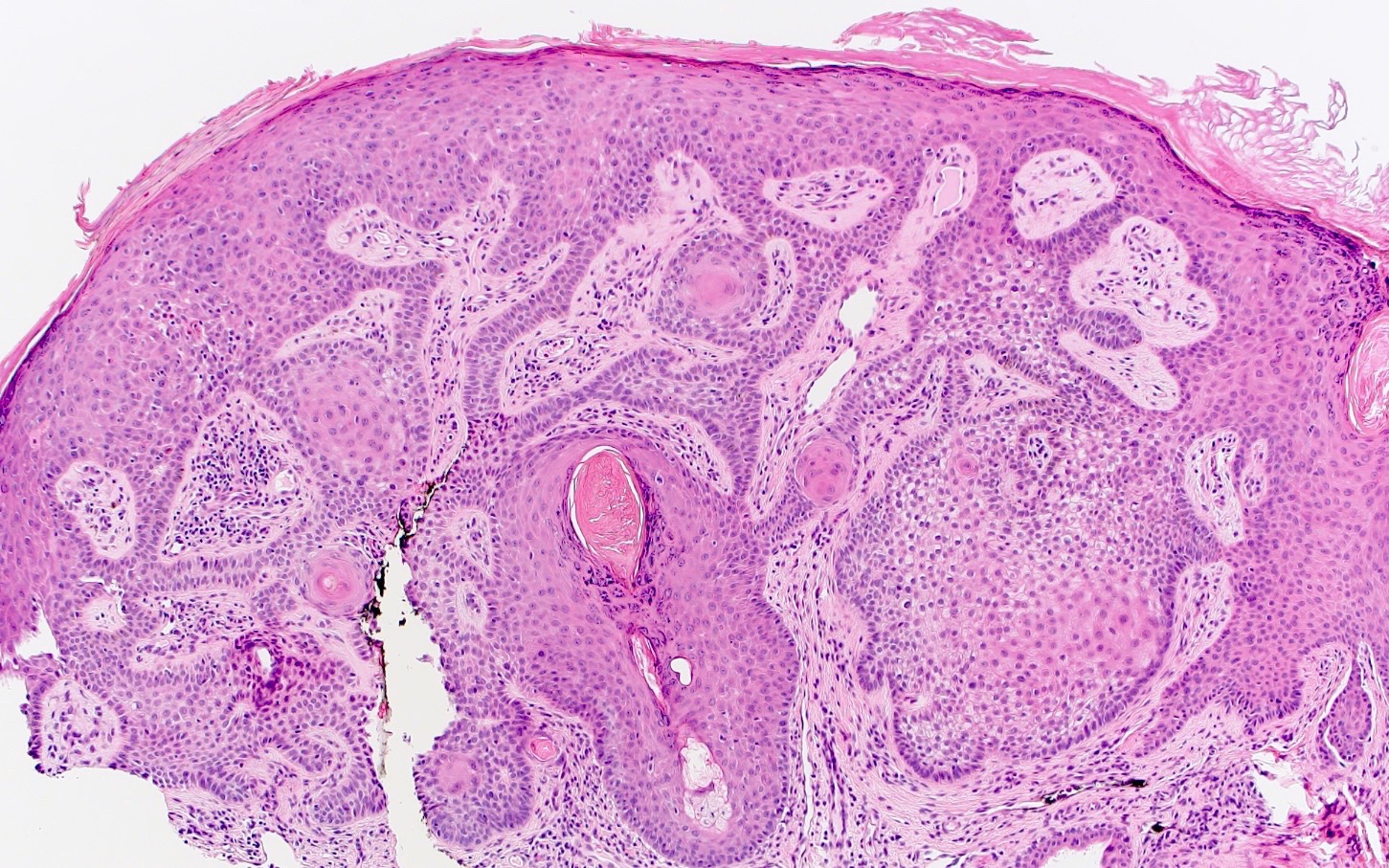
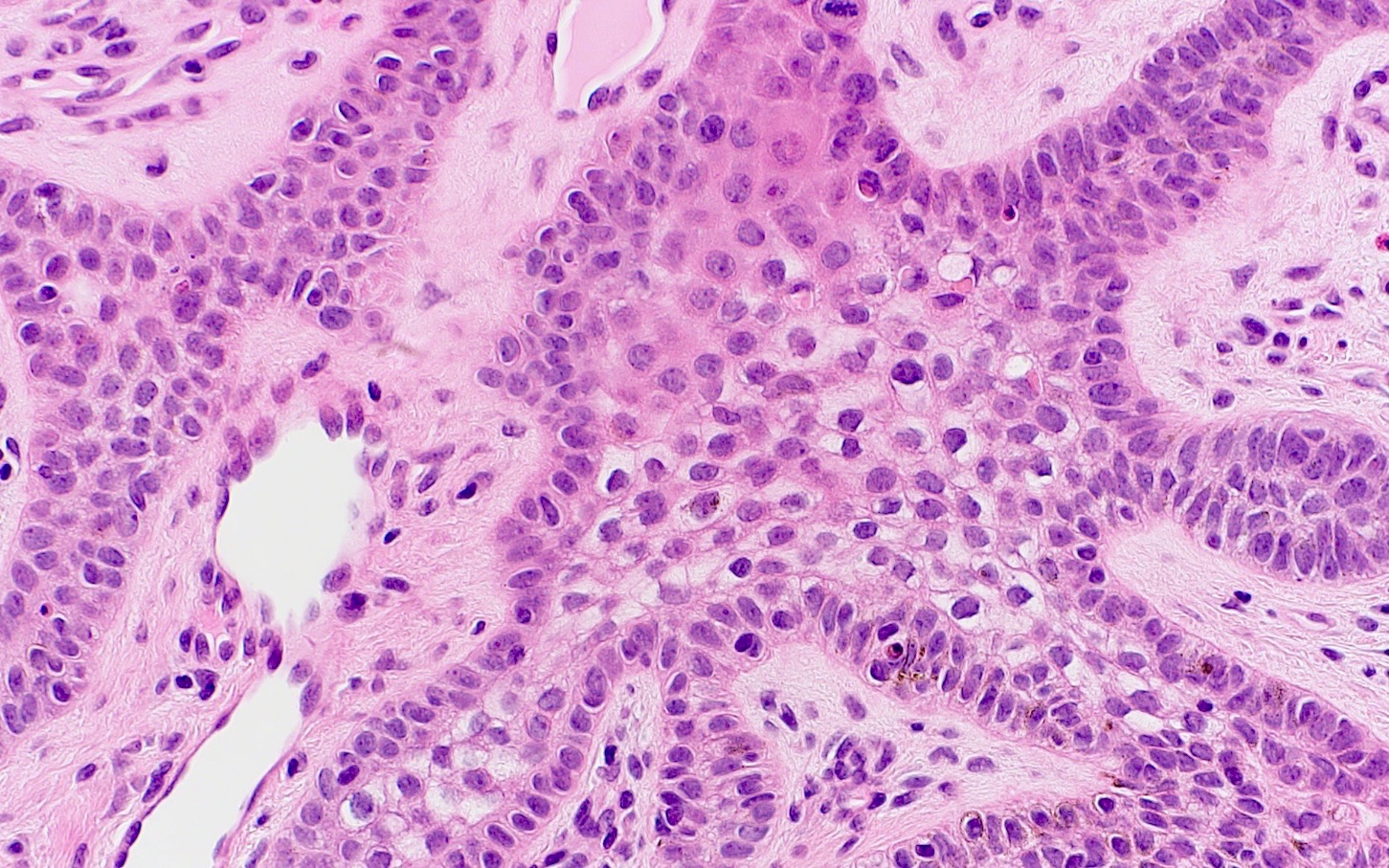
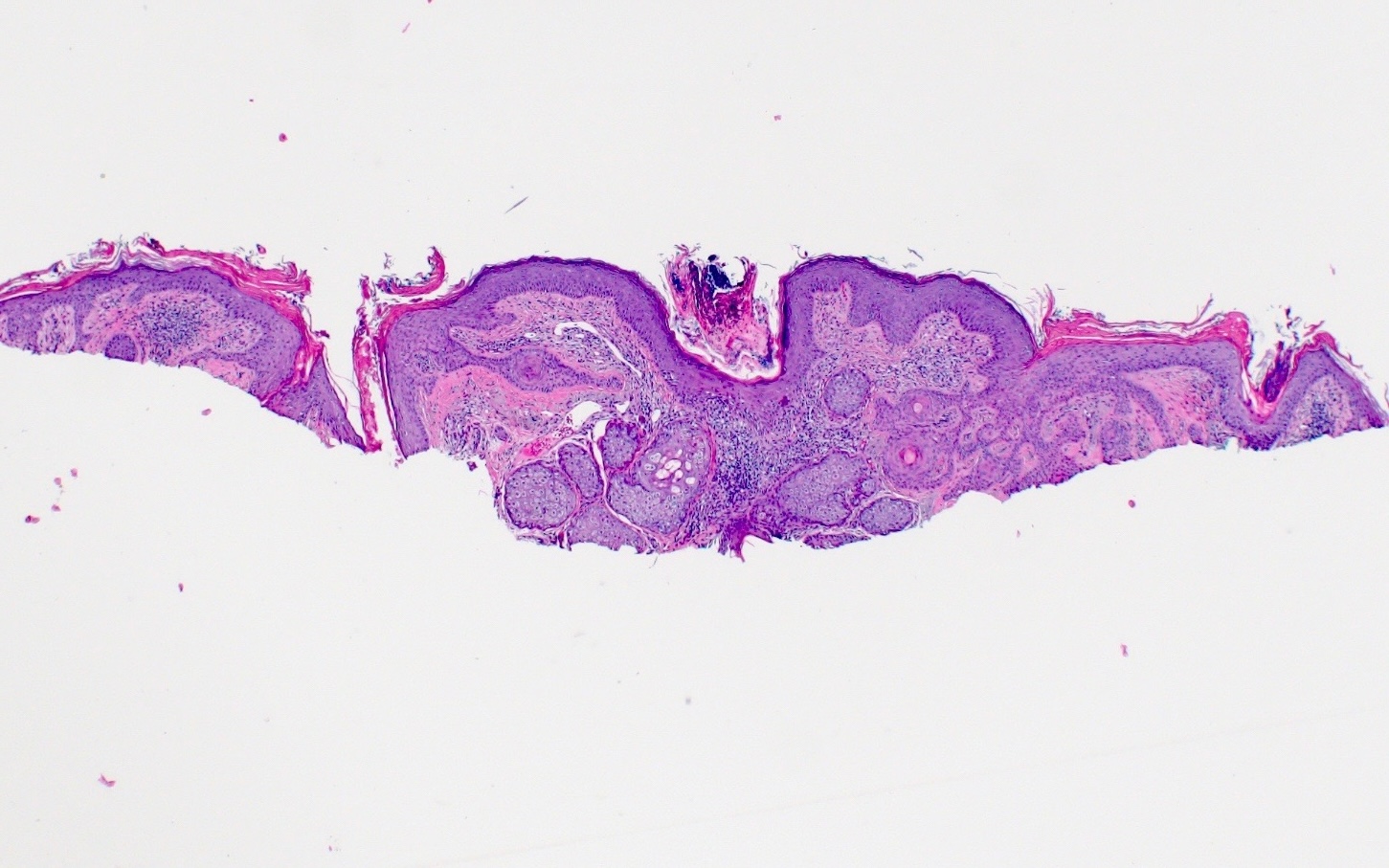
- Plate-like, superficial, horizontal proliferation of pale isthmic cells with eosinophilic cytoplasm, emanating from the epidermis
- Grow as strands in a fenestrated pattern
- Base can have basophilic palisading cells, with scant and fibrotic stroma
- No atypia
- Plate-like proliferation of pale staining epithelial cells
- Large, bland appearing, abundant eosinophilic cytoplasm
- Differentiation: isthmic, sebaceous
- Reference: J Cutan Pathol 2013;40:532
Microscopic (histologic) images
Positive stains
- Staining is typically performed to rule out malignancy with diagnostic emphasis placed on the lack of staining for markers indicative of malignant processes
- Single cell positivity for CK20, whereas basal cell carcinoma is CK20 negative (J Cutan Pathol 2013;40:532)
- PAS positive (An Bras Dermatol 2014;89:964)
Negative stains
Videos
Tumor of the follicular infundibulum (dermpath in 5 minutes)
Sample pathology report
- Skin, right upper cutaneous lip, shave biopsy:
- Tumor of follicular infundibulum
- Skin, right posterior shoulder, punch biopsy:
- Benign adnexal neoplasm / benign follicular neoplasm (see comment)
- Comment: The overall architecture of this tumor is most typical of tumor of follicular infundibulum, although there are also some focal features of trichilemmoma. Clinical correlation and follow up are recommended.
Differential diagnosis
- Infundibulocystic basal cell carcinoma:
- Often exhibits a superficial proliferation in anastomosing cords and strands of basaloid cells within the superficial dermis with peripheral palisading
- These proliferations typically lack pale cells, show frequent cytologic atypia and are associated with clefting between tumor cells / islands and mucin
- More frequent presence of multiple small cysts with cornified keratin
- Distinguishing features would be pale eosinophilic cytoplasm of TFI cells with bland appearance, unlike infundibulocystic BCC, which would have atypia and predominantly basaloid cells
- BerEP4 is positive
- Trichilemmoma:
- Lobular folliculocentric pattern
- Hyaline basement membrane
- Epidermal panfolliculoma:
- Typically pale cells with plaques limited to focal area
- Basaloid follicular hamartoma (BFH):
- Overlapping features include the anastomosing strands of bland basaloid cells; arises near normal hair follicles
- These basaloid cells are characteristically located in the dermis with a focal connection to the epidermis and can be folliculocentric
- Stroma surrounding BFH has increased fibrous tissue that can be CD34 positive, whereas TFIs exhibit a clear horizontal plate pattern with concentration along the dermoepidermal junction (DEJ); the surrounding stroma present a network of elastic fibers around the base of the tumor
Additional references
Practice question #1
A 54 year old woman presents with a well circumscribed, skin colored plaque on her cheek that has been present for years. She denies spontaneous bleeding from the lesion but she reports a personal history of skin cancer that was removed. A 6 mm punch biopsy was performed. Histopathology reveals interconnected cords of pale staining keratinocytes extending from the epidermis. There is no evidence of acanthosis, peripheral palisading or significant cytologic atypia. Which of the following is the most likely diagnosis?
- Basal cell carcinoma
- Clear cell acanthoma
- Desmoplastic trichoepithelioma
- Tumor of the follicular infundibulum
Practice answer #1
D. Tumor of the follicular infundibulum is a benign lesion that can be present for years and is characterized by dense elastic network and abundant pale keratinocytes with notable absence of characteristic features of basal cell carcinoma (BCC).
Answer A is incorrect because there is a notable lack of peripheral palisading and cytologic atypia on histology. It is important to note that both tumor of the follicular infundibulum and basal cell carcinoma can have peripheral palisading; however, tumor of the follicular infundibulum does not have basaloid cells but rather pale cells due to glycogen.
Answer B is incorrect because although clear cell acanthoma is a benign lesion, it typically presents on the legs and has a pink to brown color or more commonly, is red and shiny. On histology, although clear cell acanthomas have abundant glycogen containing cells, acanthosis is a typical feature.
Answer C is incorrect because desmoplastic trichoepithelioma is typically characterized by cords of basaloid cells, often in a dense fibrous stroma. Peripheral palisading is also a common feature on histology.
Comment Here
Reference: Tumor of the follicular infundibulum
Comment Here
Reference: Tumor of the follicular infundibulum
Practice question #2
Which of the following immunohistochemistry markers would be most helpful in differentiating tumor of the follicular infundibulum with its most common differential?
- BerEP4
- CD34
- CK5/6
- PDL1
Practice answer #2
A. BerEP4 is positive in basal cell carcinoma, which is the most common typical differential diagnosis for tumor of the follicular infundibulum. Answer B is incorrect because CD34 is seen in other adnexal tumors and trichoblastoma; however, CD34 would not help to differentiate a basal cell carcinoma from a tumor of the follicular infundibulum. Answer C is incorrect because CK5/6 is positive in squamous cell carcinoma (SCC). Answer D is incorrect because PDL1 is typically used for tumor sensitivities in melanoma, not for differentiating a basal cell carcinoma.
Comment Here
Reference: Tumor of the follicular infundibulum
Comment Here
Reference: Tumor of the follicular infundibulum
Practice question #3
Practice answer #3
B. Cowden syndrome is associated with the presentation of infundibulomas. Answer A is incorrect because there is no known association between Bowen disease and infundibulomas. The image shows plate-like, reticulated proliferation of keratinocytes that are branching from the epidermis and anastomosing in the reticular dermis, which is characteristic of TFI. Answer C is incorrect as there is no known association of Grover disease with TFIs. Additionally, the image does not show focal acantholysis, which is characteristic of Grover disease. Answer D is incorrect because tuberous sclerosis is not associated with TFIs. While tuberous sclerosis may present as hypopigmented macules on the skin similar to TFIs, they are the result of simple depigmentation rather than benign neoplastic growths arising from the hair follicle infundibulum.
Comment Here
Reference: Tumor of the follicular infundibulum
Comment Here
Reference: Tumor of the follicular infundibulum