Table of Contents
Definition / general | Essential features | Physiology | Diagrams / tables | Clinical features | Laboratory | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Alyahya M, Saeed Kamil Z. Normal nail histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticnailhistology.html. Accessed September 10th, 2025.
Definition / general
- Nail unit is a semihard keratinous structure composed of an outer nail plate and inner soft tissue components including nail bed and matrix
- Nail histology requires an excellent knowledge of the nail apparatus anatomy with excellent clinical correlation (Calonje: McKee's Pathology of the Skin, 5th Edition, 2019)
Essential features
- Nail unit is composed of a semihard nail plate and underlying soft tissue structures including nail bed (75 - 85%) and matrix (15 - 20%)
- Nail matrix produces ~80% of the nail plate and contains more melanocytes (217 ± 84 per mm2) than the nail bed (45 ± 25 per mm2)
- Nail matrix has fewer melanocytes (200 - 217 per mm2) than skin (~1,150 per mm2)
- Skin melanocytes are active, while most nail matrix melanocytes and all nail bed melanocytes are inactive under normal conditions
- Normally, the nail matrix and bed epithelium are thinner and lack a granular layer and skin appendages, while the nail folds and epithelium of the hyponychium are thicker and contain a granular layer and skin appendages
Physiology
- The nail has different soft tissue structures that provide support, protection, tactile sensations and can be used as a defense or attack mechanisms; below are the major nail structures with corresponding functions
- Nail plate
- Semihard and convex keratinized structure arranged in a lamellar pattern (the visible nail itself) (StatPearls: Histology, Nail [Accessed 15 May 2024])
- Nail plate covers the underlying nail matrix and nail bed (Clin Dermatol 2013;31:509)
- Nail plate is composed of a very low percentage of water and fat and has a significantly higher percentage of cysteine than the stratum corneum (StatPearls: Histology, Nail [Accessed 15 May 2024])
- Upper surface of the nail plate displays multiple ridges that have a curved pattern during childhood; these can be used for identification purposes (e.g., identical twins and forensic services) (Clin Dermatol 2013;31:509)
- Curved pattern ridges disappear during adulthood and become longitudinal ridges (Clin Dermatol 2013;31:509)
- Nail plate blocks most ultraviolet B (UVB) light but allows more ultraviolet A (UVA) penetration (Mills: Histology for Pathologists, 5th Edition, 2019)
- Nail matrix
- Nail matrix accounts for 15 - 20% of the soft tissue structures underlying the nail plate along with the nail bed
- Distal portion of the matrix can be visualized in some digits, especially the thumb; known as lunula (a half moon shaped crescentic structure)
- In other people, this is fully covered by the proximal nail fold (PNF)
- Proximal nail matrix is located deep to the nail plate and is responsible for the formation of ~80% of the nail plate
- Dorsal smooth aspect of the nail plate is produced by the proximal nail matrix, while the ventral rough surface is formed by the distal nail matrix
- Nail matrix contains most of the melanocytes of the nail apparatus (Clin Dermatol 2013;31:509)
- Cul de sac is the anatomical space where the nail matrix resides; specifically, the nail matrix covers the plantar surface of this recess and extends into the proximal nail groove (Baran: Baran and Dawber's Diseases of the Nails and their Management, 5th Edition, 2019)
- Nail bed
- Nail bed includes the area between the distal part of the matrix (lunula) and the hyponychium, lying beneath the nail plate and accounting for 75 - 85% of the soft tissue structures underlying the plate (Clin Dermatol 2013;31:509)
- Nail bed attaches to the ventral surface of the nail plate providing support and adhesion to the nail plate (Clin Dermatol 2013;31:509)
- It is believed to participate (to a lesser extent) in the production of nail plate (particularly under pathologic conditions) (Actas Dermosifiliogr 2013;104:564)
- Nail bed is rich in blood vessels and glomus bodies, which are responsible for thermoregulatory function (StatPearls: Histology, Nail [Accessed 15 May 2024])
- Nail folds
- Proximal nail fold is an extension of the proximal finger skin that covers the nail plate and matrix
- Proximal nail fold and nail plate provide protection of the matrix from UV radiation
- Eponychium is the distal ventral part of the proximal nail fold, which forms the cuticle at the angle between the dorsal and ventral aspects of the proximal nail fold
- Cuticle is a layer of thickened stratum corneum that attaches firmly to the nail plate and protects the matrix from toxins, irritants and microbes
- Practice of cuticle removal frequently seen in manicure can potentially lead to infections and paronychia
- Lateral nail fold (LNF) is normal skin that surrounds the sides of the nail and is devoid of pilosebaceous units (Clin Dermatol 2013;31:509, StatPearls: Histology, Nail [Accessed 15 May 2024])
- Hyponychium
- Hyponychium is the skin that is distal to the nail bed and lines the free ridge of the nail
- Narrow orifice between the nail plate and hyponychium contains microorganisms (Staphylococcus epidermidis) and dirt that can transmit infections despite hand washing (Clin Dermatol 2013;31:509, Haneke: Histopathology of the Nail - Onychopathology, 1st Edition, 2017)
- Hyponychium is rich in nerve endings, which greatly contributes to finger sensitivity (Mills: Histology for Pathologists, 5th Edition, 2019)
- Nail plate
Clinical features
- Nails can be important clues to localized and systemic diseases; listed below are descriptions of several nail findings and diseases
- Splinter hemorrhage
- Damage to the nail bed capillaries that run along the dermis; can be seen in normal and disease status (Mills: Histology for Pathologists, 5th Edition, 2019)
- Leukonychia
- White discoloration bands of the nail due to impaired keratinization of the nail matrix
- This finding may be attributed to continuous stressors
- Longitudinal melanonychia
- Dark pigment bands of the nail due to accumulation of melanin pigment in the nail plate
- It may be difficult to distinguish benign pigment changes from melanoma; hence, a biopsy is often necessary to confirm diagnosis
- Onycholysis
- Loosening of the nail occurs if the distal nail plate is not firmly adherent to the underlying nail bed and other soft tissue structures
- Psoriasis, onychomycosis and trauma can cause this condition
- Onychomycosis
- Thick yellow nail plate due to fungal infection of the nail and the surrounding tissue
- Onychorrhexis
- This is manifested as longitudinal splits involving the distal free ridge of the nail plate
- Onychoschizia
- Involves the free ridge of the nail plate as a transverse lamellar splitting caused by breakdown of the intercellular adhesions
- Can be related to or exacerbated by frequent handwashing or mechanical trauma
- Paronychia
- When the nail folds and cuticle are traumatized, infection with inflammation, pustule and crust can occur due to loss of protective function
- Staphylococcal aureus is the most common cause of acute paronychia; in contrast, chronic paronychia is often associated with fungal involvement, particularly Candida species (Indian J Dermatol Venereol Leprol 2015;81:485)
- Squamous cell carcinoma
- Erythematous lesion that can damage nail structure
- Benign lesions such as verruca and onychomycosis could potentially mimic squamous cell carcinoma
- Treatment options include Mohs surgery or possibly amputation
- Subungual hyperkeratosis
- Abnormal keratinization process of the distal nail bed results in a thick keratin layer below the free ridge of the distal nail plate
- Various etiologies such as trauma, psoriasis and onychomycosis can lead to subungual hyperkeratosis
- Trachyonychia
- Impaired keratinization of the proximal nail matrix results in longitudinally rough and thickened ridges with nail brittleness
- Many dermatologic diseases such as psoriasis, lichen planus, atopic dermatitis and alopecia areata manifest clinically as trachyonychia (StatPearls: Anatomy, Shoulder and Upper Limb, Nails [Accessed 15 May 2024])
- Splinter hemorrhage
Laboratory
- Systemic laboratory tests for nail conditions are limited and mostly not significant; commonly used tests include
- Potassium hydroxide (KOH) preparation for the diagnosis of fungal infections (onychomycosis) (Mycopathologia 2013;175:315)
- Nail biopsy or swab for culture and sensitivity to detect microorganisms
- Special stains (PAS and GMS), direct immunofluorescence and immunostains are frequently used in the histopathology service for infections, immunobullous diseases and certain tumors, respectively
- Florescence in situ hybridization (FISH), polymerase chain reaction (PCR) and next generation sequencing (NGS) could be used, especially in diagnostically challenging tumors such as melanomas, to look for defining genetic mutations (Haneke: Histopathology of the Nail - Onychopathology, 1st Edition, 2017, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019)
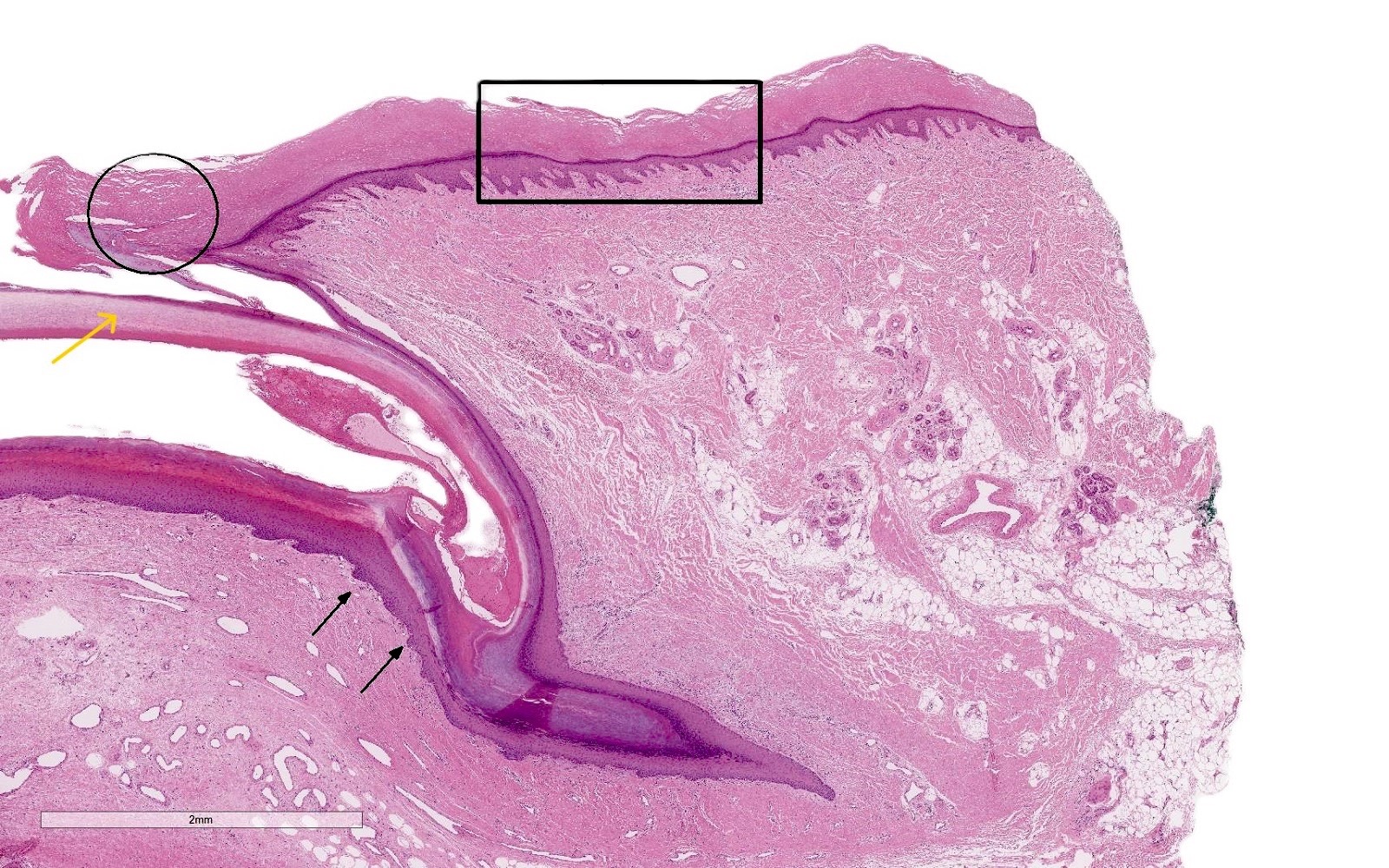
Microscopic (histologic) description
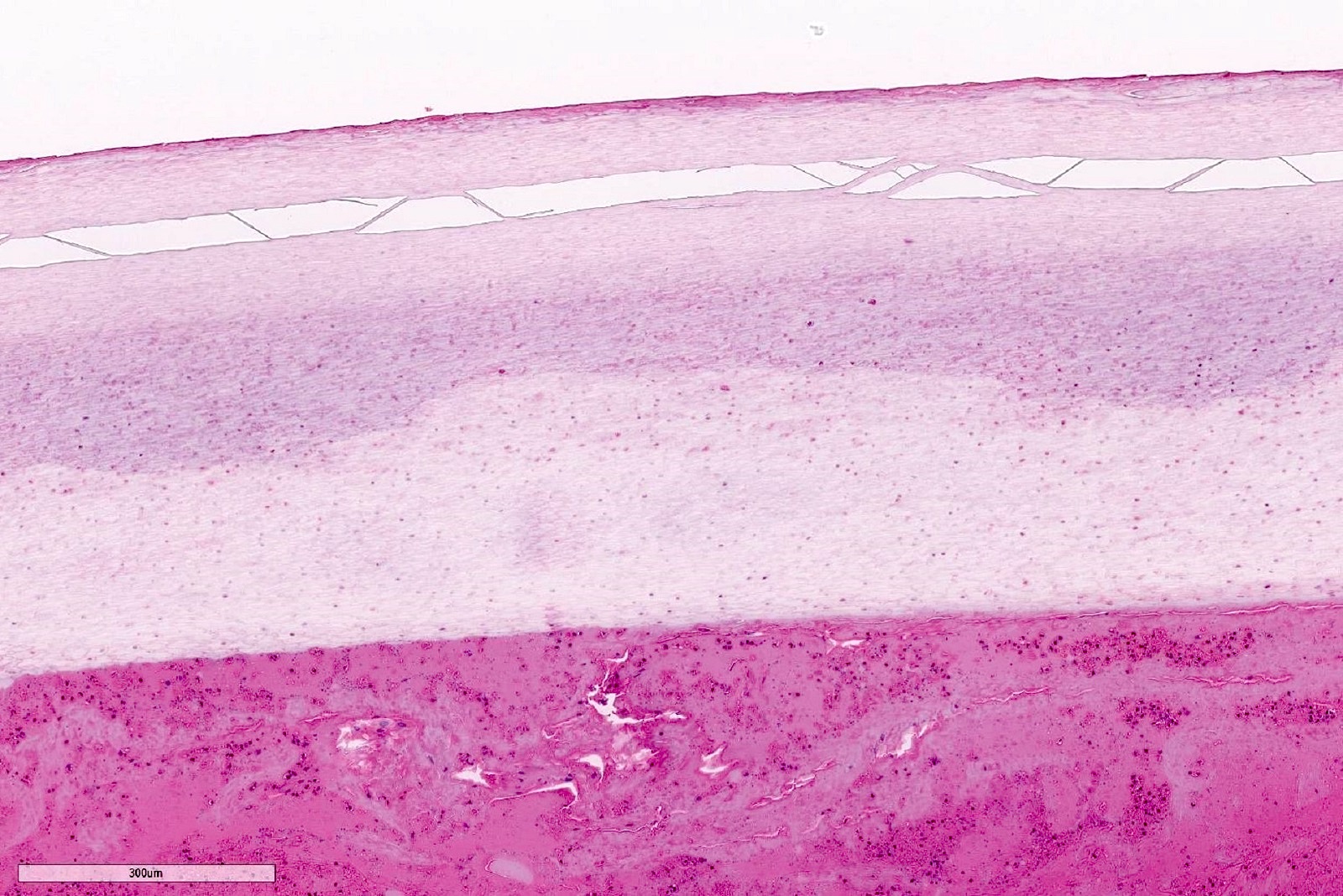
- Nail plate
- Composed of nonnucleated, irregular and polyhedral corneocytes distributed as back to back and interdigitating cells devoid of granular cell layer
- 3 layers forming the nail plate: a dorsal thin layer, intermediate thick layer and a ventral layer
- Corneocytes and nail plate size is in proportion to the individual's age (e.g., children tend to have smaller cells and adults have larger cells) (Mills: Histology for Pathologists, 5th Edition, 2019)
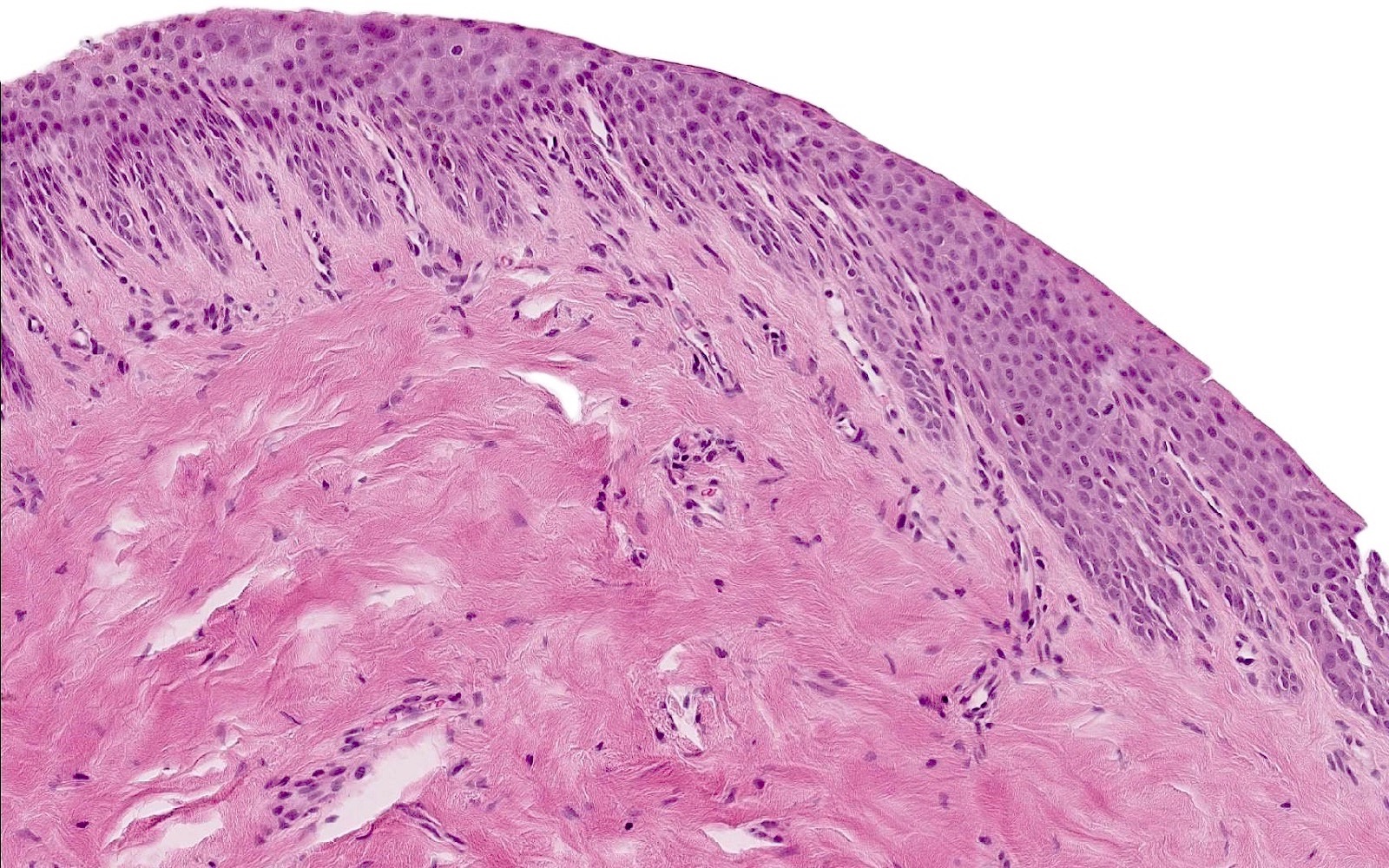
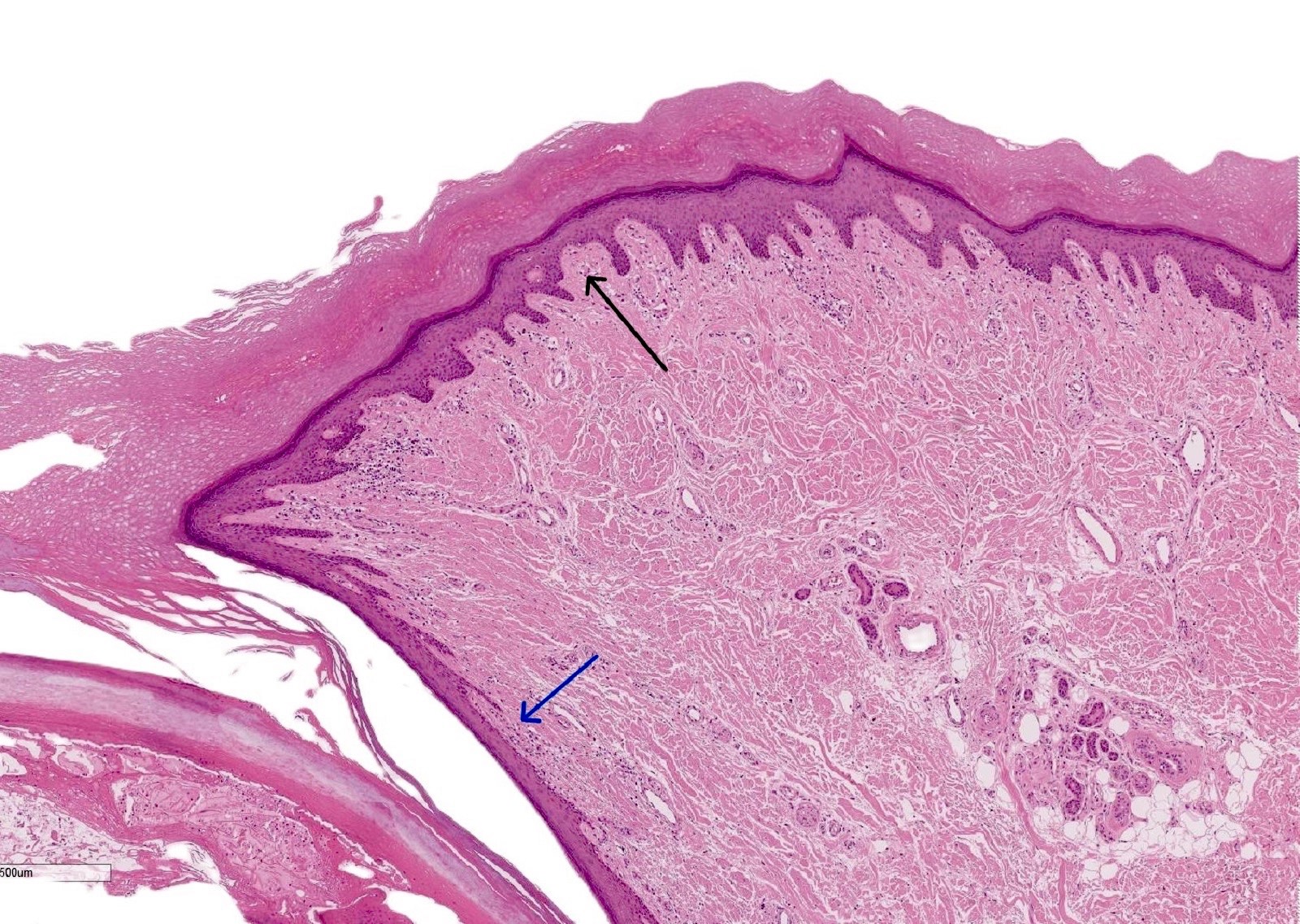
- Proximal nail fold
- Wedge-like invagination of a skin fold on the dorsal surface of the distal digit from which the nail plate emerges from underneath
- It has 2 layers of normal looking epidermis (similar to epidermis elsewhere): ventral (above the nail plate) and dorsal (making the dorsum of the finger skin) layers
- Both layers possess granular cell layer
- Dorsal layer contains sweat glands without folliculosebaceous units
- Ventral layer is thinner and devoid of skin appendages; known as eponychium (Mills: Histology for Pathologists, 5th Edition, 2019)
- Matrix
- Nail matrix lies beneath the nail plate and comprises 3 parts: dorsal, intermediate and ventral parts
- Intermediate part of the matrix is crucial as it is directly involved in the formation of the nail plate
- Matrix epithelium is thick with long and oblique rete ridges in the midline of the nail unit
- Matrix rete ridges are less prominent laterally
- Nail matrix epithelium is composed of 3 layers, from deepest to most superficial: basaloid, prekeratogenous and keratogenous
- Onychogenous band is an eosinophilic layer within the keratogenous zone that contributes to nail plate formation and lacks keratohyaline granules
- Distally, near the nail bed, the matrix epithelium becomes thinner and the onychogenous band is markedly reduced
- Does not contain a granular layer or pilosebaceous units
- Cellular composition of the matrix includes epithelial cells, few scattered melanocytes, Merkel and Langerhans cells (Mills: Histology for Pathologists, 5th Edition, 2019, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019)
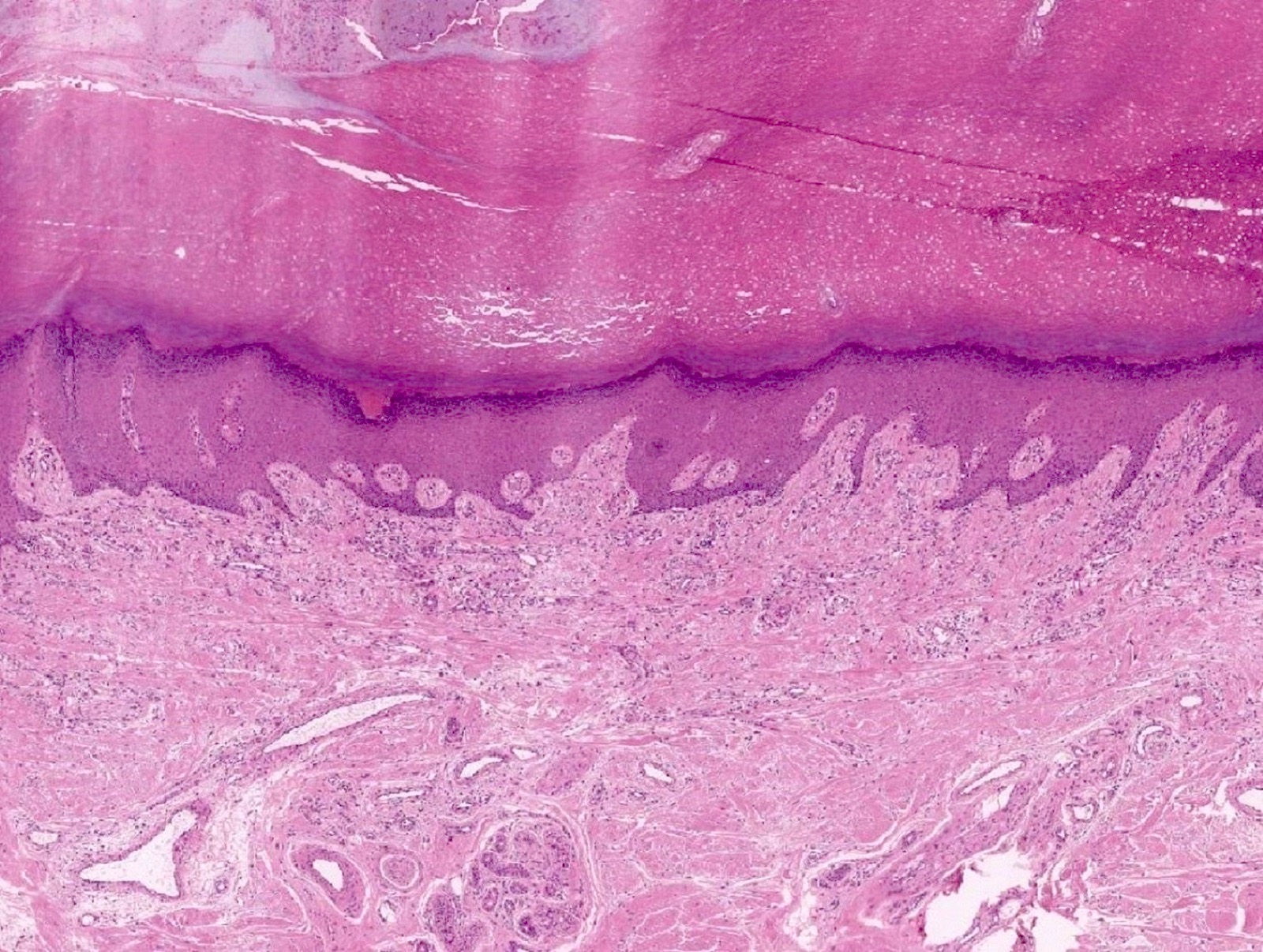
- Nail bed
- Nail bed features a thin layer of epidermis (3 - 4 cells thick) with sparse inactive melanocytes (~50 melanocytes per mm2)
- Another feature is the transition zone from living keratinocytes to dead ventral nail plate cells which is abrupt, occurring within a single horizontal cell layer, resembling the Henle layer of the inner root sheath of the hair follicle
- Less active than the matrix as observed by fewer active basal cells (low Ki67 index)
- No granular cell layer or pilosebaceous units are present
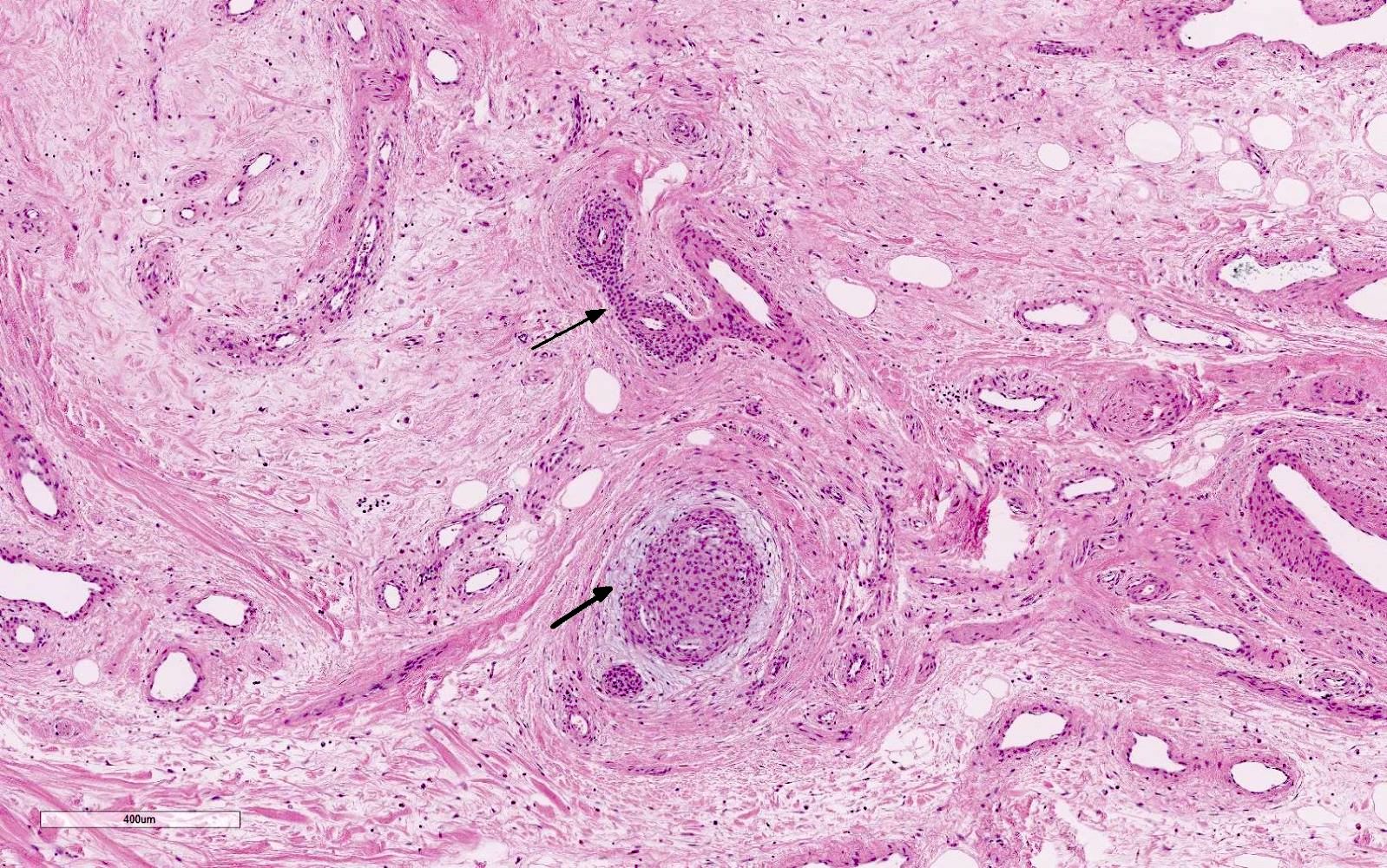
- Abundant small dermal vessels and glomus bodies are noted
- Dermal vessels are arranged on a longitudinal axis and are larger than those in the skin
- Keratohyaline granules develop in diseases such as psoriasis (Mills: Histology for Pathologists, 5th Edition, 2019, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019)
- Onycholemmal keratinization refers to a mode of keratin differentiation seen in the ventral epithelium of the proximal nail fold and nail bed, especially the distal bed (Am J Dermatopathol 2007;29:543)
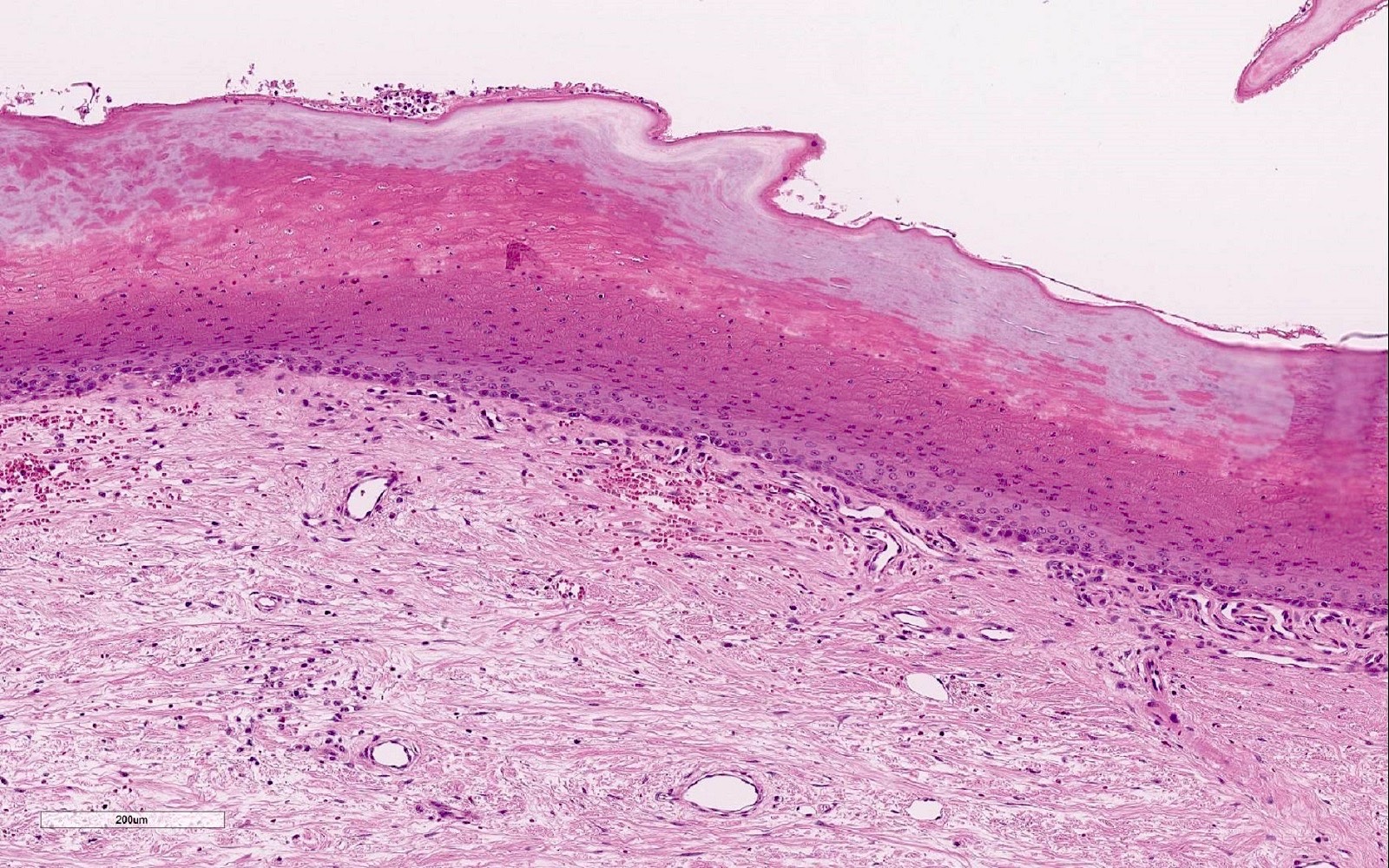
- Hyponychium
- Characterized by a transition zone (between the nail bed and fingertips) with thicker keratin layer, acanthosis, papillomatosis and a visible granular layer
- Skin appendages in the hyponychium include eccrine glands but hair follicles are absent
- First part of the nail unit that undergoes keratinization (Mills: Histology for Pathologists, 5th Edition, 2019)
- Lateral nail folds
- Histologically similar to the skin but no pilosebaceous units
- Also, acanthosis and papillomatosis are similar to the hyponychium (Mills: Histology for Pathologists, 5th Edition, 2019)
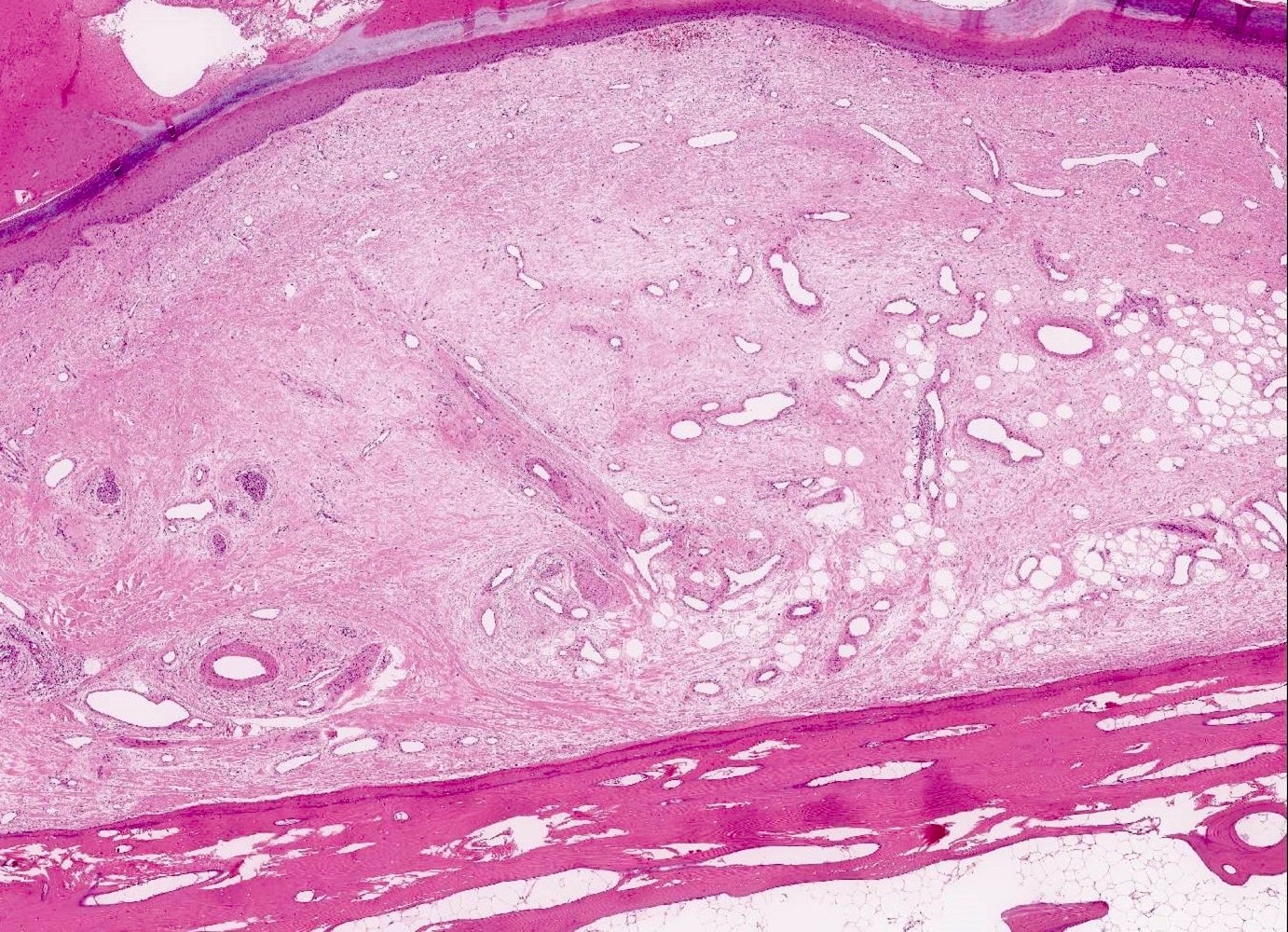
- Dermis
- Unique soft tissue structure devoid of subcutis, bonded by the underneath phalanx and linked to its blood and nerve supply
- Dermis of the nail bed is thick, dense, vertically oriented and composed of type IV collagen
- Dermis of the nail bed and matrix differs from the rest of the nail unit dermis as it contains specialized onychofibroblasts; hence, given the name onychodermis
- Dermis significantly helps in adherence of the nail plate to the phalangeal periosteum (Mills: Histology for Pathologists, 5th Edition, 2019)
- Nerve supply
- Generally, the nail unit (especially nail matrix and bed) is characterized by sparse nerve endings and rare Pacinian and Meissner corpuscles
- Pacinian corpuscles are mechanoreceptors structures sensing deep pressure and vibration; composed of concentric layers of Schwann cells and axons and located deep in the dermis and subcutis
- Meissner corpuscles are rapid mechanical receptors for light touch sensation; composed of multiple parallel layers of Schwann cells and axon and located in the superficial dermis
- On the contrary to nail matrix and bed, hyponychium and lateral nail folds contain more abundant nerve endings, Meissner corpuscles and Merkel cells mediating tactile sensation (Mills: Histology for Pathologists, 5th Edition, 2019)
- Blood supply
- Nail bed and matrix are well vascularized; however, the nail plate itself is avascular
- Paired digital arteries are responsible for the arterial blood supply to the nail bed and matrix
- Arteries are arranged vertically within the nail bed
- 2 veins located on each side of the plate in the proximal nail fold function as venous drainage of the nail unit (Mills: Histology for Pathologists, 5th Edition, 2019)
- Epithelial cells
- Matrix is characterized by its thick squamous epithelium composed of keratinocytes and active basal layer
- Basal layer is composed of immature basaloid cells which constitute the germinative layer and produce keratinocytes and subsequently the nail plate
- Nail matrix lacks a granular layer and is characterized by acanthosis and papillomatosis, which can also be identified in the hyponychium (Mills: Histology for Pathologists, 5th Edition, 2019)
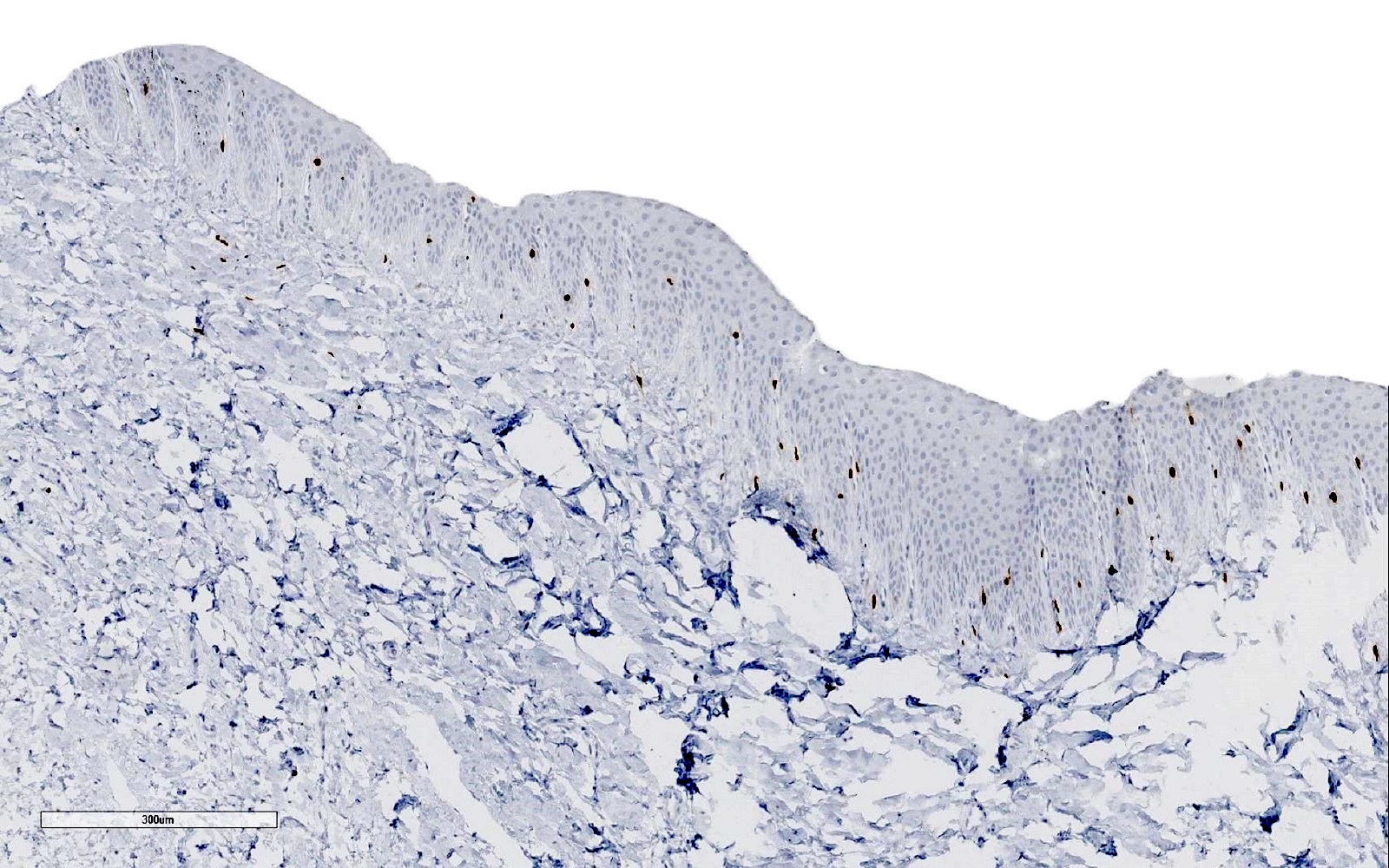
- Melanocytes
- Density of matrix melanocytes is lower compared to the skin
- Melanocytes are normally observed in the matrix with variable density, being less dense in the proximal portion and gradually increasing in number distally
- There are ~200 melanocytes per mm2 in the matrix compared to 1,150 melanocytes per mm2 in the skin
- Distribution of melanocytes in the matrix differs from the skin; matrix melanocytes are identified often by immunohistochemistry and distributed as irregularly scattered suprabasal cells (Am J Dermatopathol 2018;40:180)
- Melanocyte count in the distal nail matrix ranges from 208 to 576 cells per 2.784 mm2 or 4 - 9 melanocytes per 1 mm of nail matrix epithelium
- Melanocytes in the proximal nail matrix are inactive (no melanin production)
- 50% of the melanocytes in the distal matrix are active, while the remaining 50% are inactive
- Rarely, inactive melanocytes are present in the nail bed epithelium
- Factors such as UV rays and trauma may contribute to the increased density of melanocytes in the distal nail matrix (Mills: Histology for Pathologists, 5th Edition, 2019, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019)
- Langerhans and Merkel cells
- Merkel cells at a concentration of > 50 Merkel cells/mm2 have been identified in the basal cell layer of the proximal nail fold and hyponychium using indirect immunofluorescence and immunoelectron microscopy with the monoclonal antibody Troma 1
- Langerhans and Merkel cells have been detected in the matrix but their role is unknown due to lack of studies (Mills: Histology for Pathologists, 5th Edition, 2019)
- Lunula
- White color of this structure is due to decreased vascularity and loose dermal collagen (Mills: Histology for Pathologists, 5th Edition, 2019)
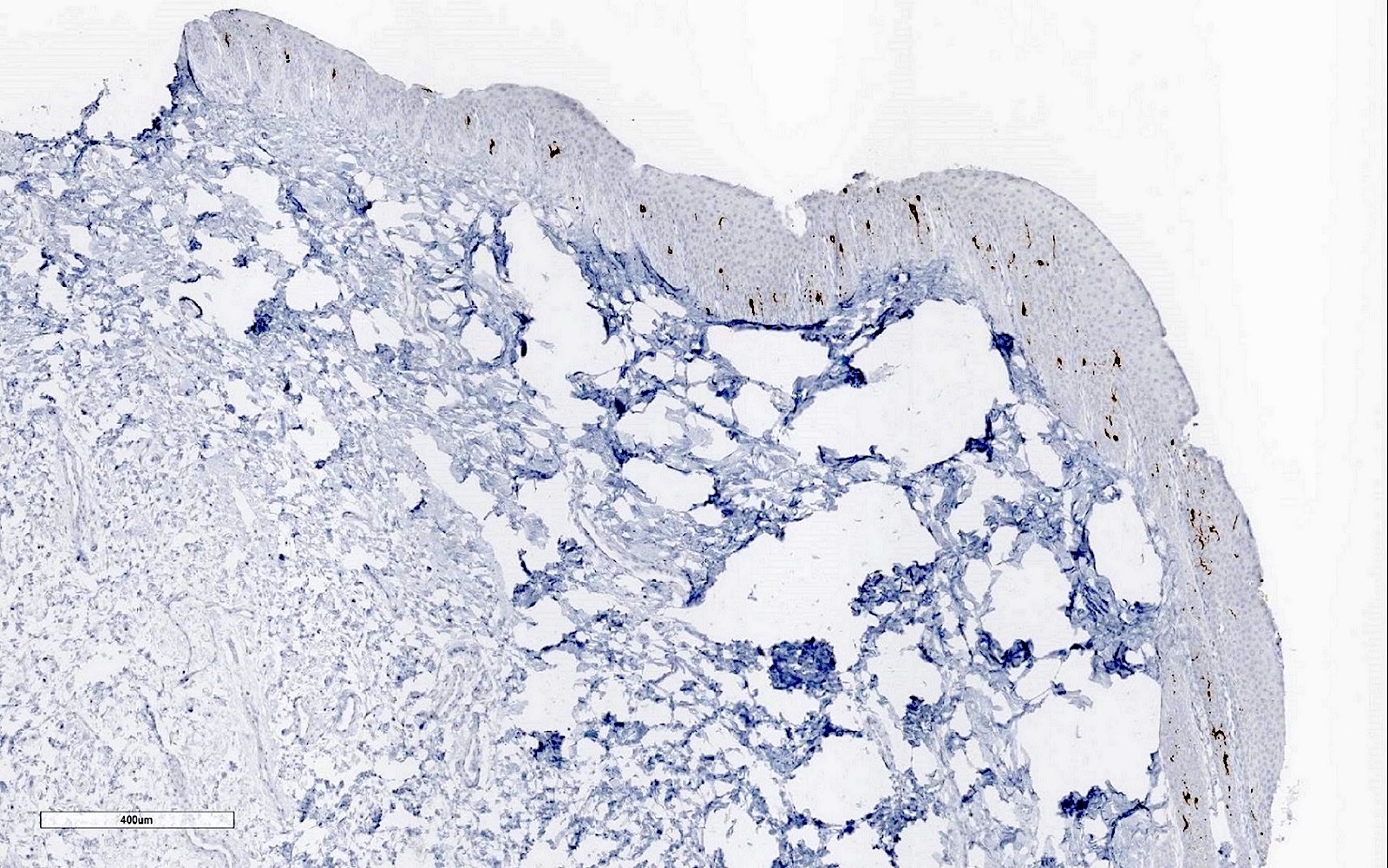
Microscopic (histologic) images
Positive stains
- Verhoeff-Van Gieson (VVG) stains and highlights the vertically oriented collagen fibers in the dermis of the nail bed and matrix
- Collagen IV: intense staining of nail matrix dermis
- AE1 / AE3 keratin highlights squamous epithelium in the nail unit
- CK20 can be used to highlight Merkel cells in the proximal nail fold
- EMA highlights scattered positive areas in the nail bed
- CEA is expressed in the nail bed epithelium, especially in the more distal portion
- CD10 stains the dermis of the nail bed and matrix
- Beta catenin staining in the nail matrix shows nuclear and cytoplasmic expression in suprabasal cells (Mills: Histology for Pathologists, 5th Edition, 2019)
- SOX10, HMB45 and MelanA highlight a few scattered melanocytes within the nail matrix and nail bed
- BCL2 is strongly positive in the ventral nail matrix epithelium (Mills: Histology for Pathologists, 5th Edition, 2019, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019)
- S100 is positive but should not be used alone, as many nail melanocytes are not reactive; it remains useful for evaluating pagetoid melanocytes in the nail plate and spindle cell melanoma (Calonje: McKee's Pathology of the Skin, 5th Edition, 2019)
Negative stains
- CK19 and CK20 are mostly negative in nail keratins apart from scattered weak expression (Mills: Histology for Pathologists, 5th Edition, 2019)
- p53: markedly reduced expression in the epithelial cells of the matrix (few scattered cells) (Mills: Histology for Pathologists, 5th Edition, 2019)
- Ki67: markedly reduced expression in the epithelial cells of the matrix (few scattered cells) (Mills: Histology for Pathologists, 5th Edition, 2019)
- PRAME is typically negative in normal nail and benign melanocytic lesions, while showing positivity in melanoma (however, correlation with morphology is imperative) (J Cutan Pathol 2022;49:610)
Practice question #1
Practice answer #1
C. Matrix and nail bed. The image shows a nail bed epithelium lacking a granular layer. The matrix and nail bed are the only structures of the nail unit that lack a granular layer. Answer D is incorrect because both layers of the proximal nail fold possess a granular layer. Answers A and B are incorrect because both hyponychium and lateral nail folds look similar to the skin and both structures show acanthosis and papillomatosis with a visible granular layer.
Comment Here
Reference: Normal nail histology
Comment Here
Reference: Normal nail histology
Practice question #2
Which of the following statements regarding nail apparatus melanocytes is correct?
- Nail apparatus melanocytes are higher in number compared to the skin elsewhere and are distributed along the basal layer
- Nail matrix melanocytes are fewer in number compared to the skin elsewhere and are distributed mainly as single cells along the basal layer
- Nail matrix melanocytes are fewer in number and less active compared to the skin and are irregularly scattered along the suprabasal layer
- Nail matrix melanocytes are very active compared to the skin elsewhere
Practice answer #2
C. Nail matrix melanocytes are fewer in number and less active compared to the skin and are irregularly scattered along the suprabasal layer. There are ~200 melanocytes per mm2 in the matrix compared to 1,150 melanocytes per mm2 in the skin elsewhere. Answers A and B are incorrect because they tend to be irregularly scattered within the suprabasal layers compared to the single melanocytes distributed along the basal layer in the skin. Answer D is incorrect because nail matrix melanocytes are mostly inactive, while skin melanocytes are more active.
Comment Here
Reference: Normal nail histology
Comment Here
Reference: Normal nail histology