Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Etiology | Clinical features | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1Cite this page: Wei S. Poorly differentiated thyroid carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidinsular.html. Accessed September 29th, 2025.
Definition / general
- Malignant follicular cell neoplasm with limited evidence of follicular cell differentiation
- Intermediate clinical behavior between well differentiated (papillary and follicular carcinoma) and anaplastic carcinoma (Am J Surg Pathol 2007;31:1256, Surg Pathol Clin 2014;7:475, Lloyd: WHO Classification of Tumours of Endocrine Organs, 4th Edition, 2017)
Essential features
- Intermediate grade follicular cell carcinoma with limited evidence of follicular cell differentiation
Terminology
- Insular / trabecular carcinoma
- Primordial cell carcinoma
- Poorly differentiated follicular carcinoma
- Poorly differentiated papillary carcinoma
- Solid type follicular carcinoma
- High risk thyroid carcinoma of follicular cell origin
ICD coding
- ICD-10: C73 - malignant neoplasm of thyroid gland
Epidemiology
- Older patients, mean age 55 - 63 years
- 0.3 - 6.7% of thyroid carcinomas
- More common in Europe and South America than U.S. (Mod Pathol 2010;23:1269)
Etiology
- Iodine deficiency may be a risk factor; no association with radiation exposure (Clin Oncol (R Coll Radiol) 2011;23:261)
- Some tumors are de novo; some arise from dedifferentiation of follicular or papillary carcinoma
Clinical features
- Large solitary thyroid mass. Patient may have a history of recent growth in a longstanding uninodular or multinodular thyroid (Am J Surg Pathol 1984;8:655)
- Intermediate behavior between well differentiated and anaplastic carcinoma (World J Surg 2007;31:934)
- Has nodal and hematogenous metastases and 3 year survival of 38% (Langenbecks Arch Surg 2007;392:671)
- Extends to perithyroidal soft tissue in 60 - 70% cases
- Vascular invasion in 60 - 90% cases
- Regional lymph node metastasis in 15 - 65%
- Distant metastasis in 40 - 70%
Radiology description
- Ultrasound shows inhomogeneous hyoechoic mass (Cancer 2006;106:1286)
- Cold on scintigraphy and positive on FDG PET
Prognostic factors
- Tumors with overall 5 year survival rate: 60 - 70% (J Clin Endocrinol Metab 2014;99:1245)
- Poor prognosis associated with high stage and older age (> 45 years)
Case reports
- 4 year old girl with metastatic disease (Am J Otolaryngol 2009;30:61)
- 26 year old African American woman with benign biopsy but compressive symptoms (Case #435)
- 57 year old woman with unusual short term complete response to chemotherapy (J Clin Endocrinol Metab 2012;97:3046)
- 60 year old woman with metastatic poorly differentiated thyroid carcinoma within an intracranial meningioma (J Clin Endocrinol Metab 2014;99:3513)
- 64 year old woman with tumor arising from ectopic thyroid (Am J Clin Pathol 1995;104:408)
- 75 year old woman with superior vena cava metastasis (J Clin Oncol 2015;33:e119)
- 80 year old woman with neck mass (University of Pittsburgh: Case 24 - Neck Mass)
- 82 year old woman with extensive extracellular mucin in tumor (Hum Pathol 2005;36:698)
Treatment
- Total thyroidectomy, neck dissection, radioactive iodine and suppressive thyroxine
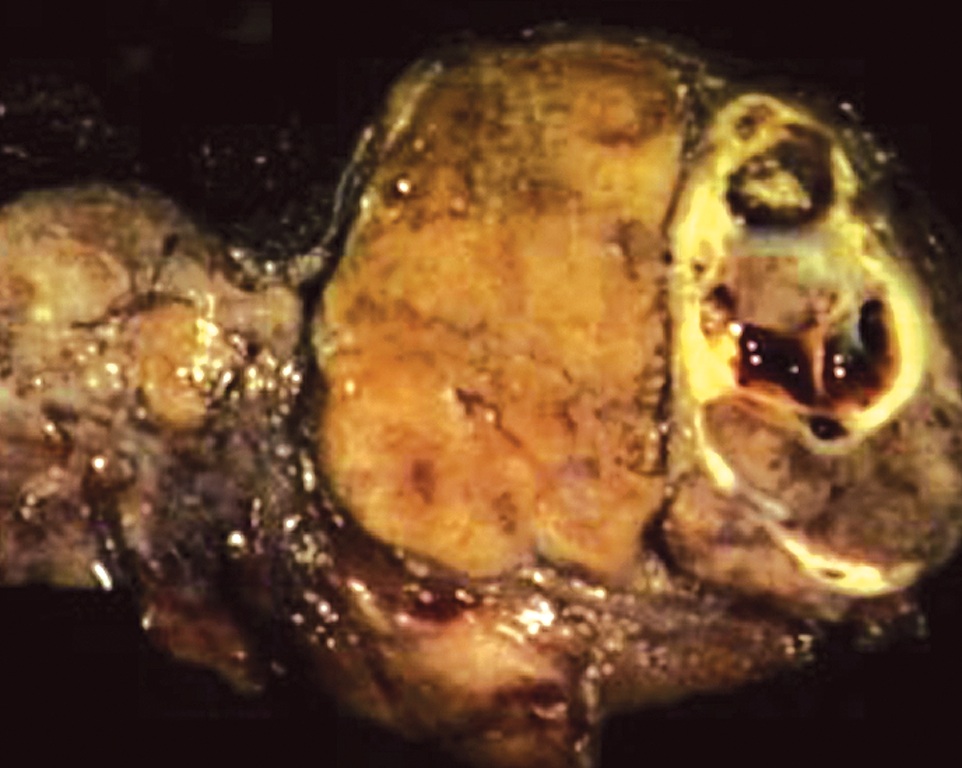
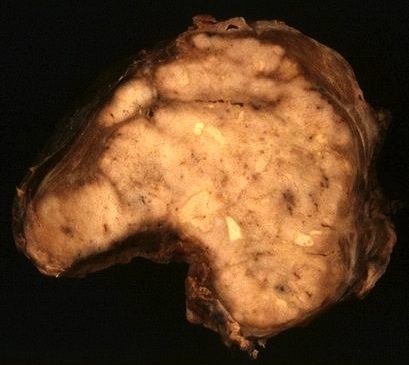
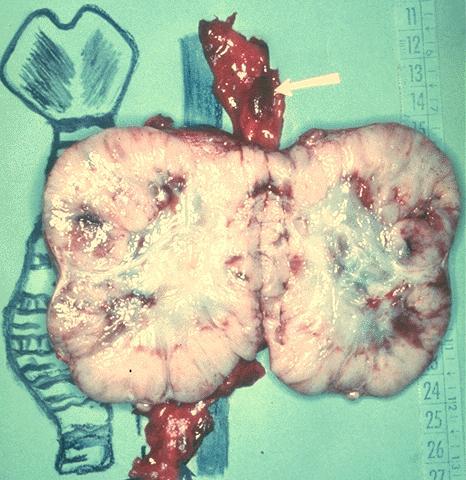
Gross description
- Large (median size: 5 cm), grayish white, some show soft pale areas of necrosis
- Pushing margins, may be partially encapsulated
- Can have satellite nodules (Am J Surg Pathol 1984;8:655)
Gross images
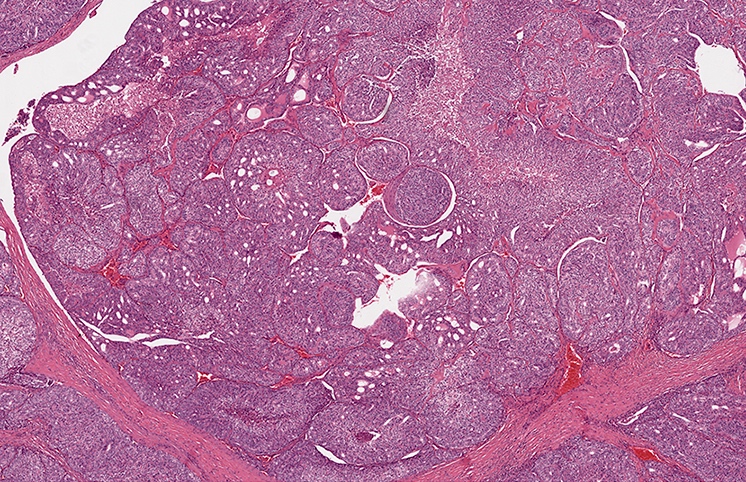
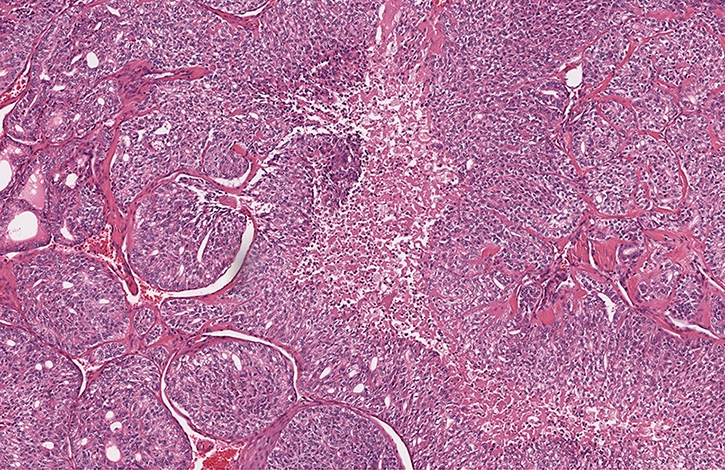
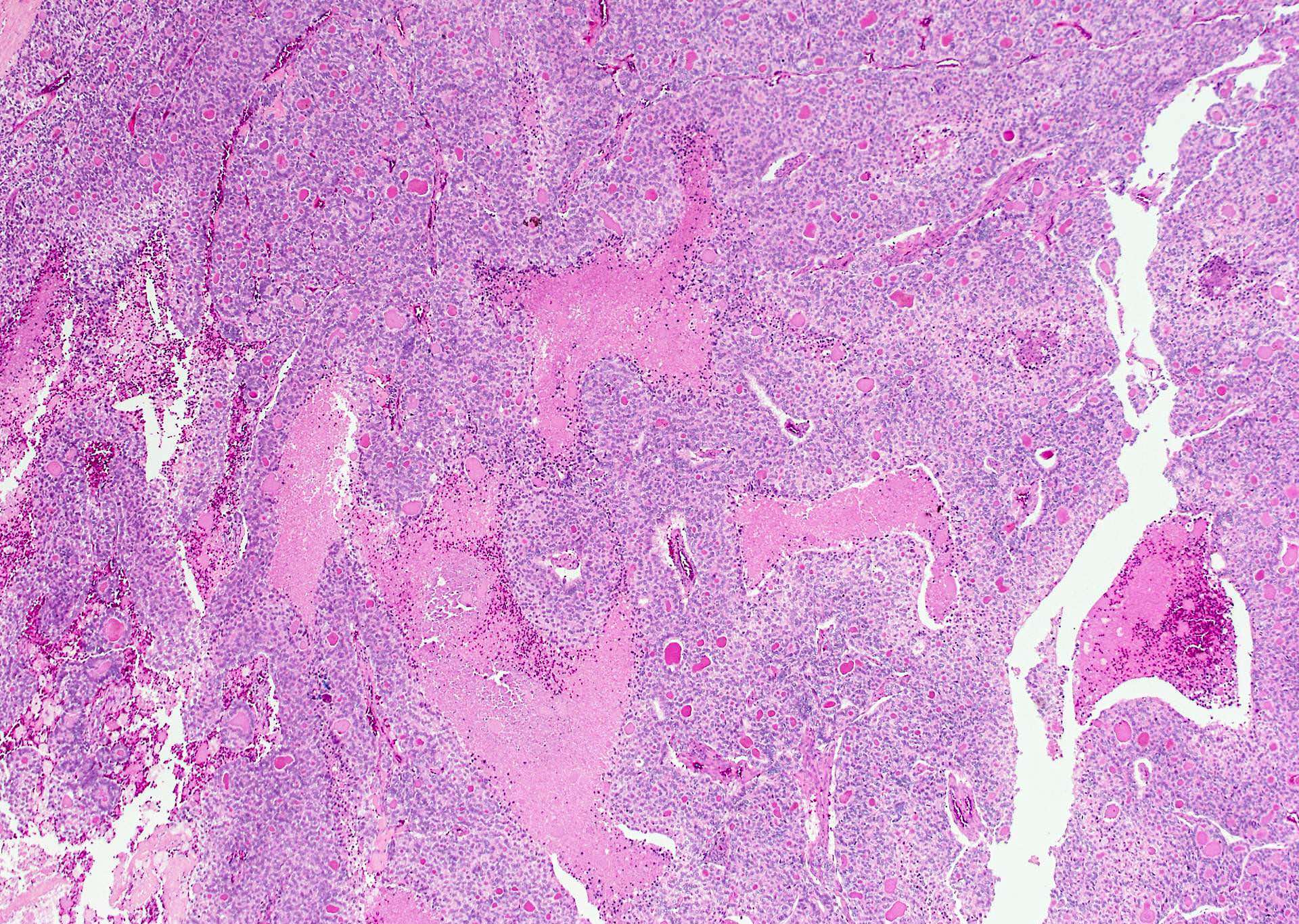
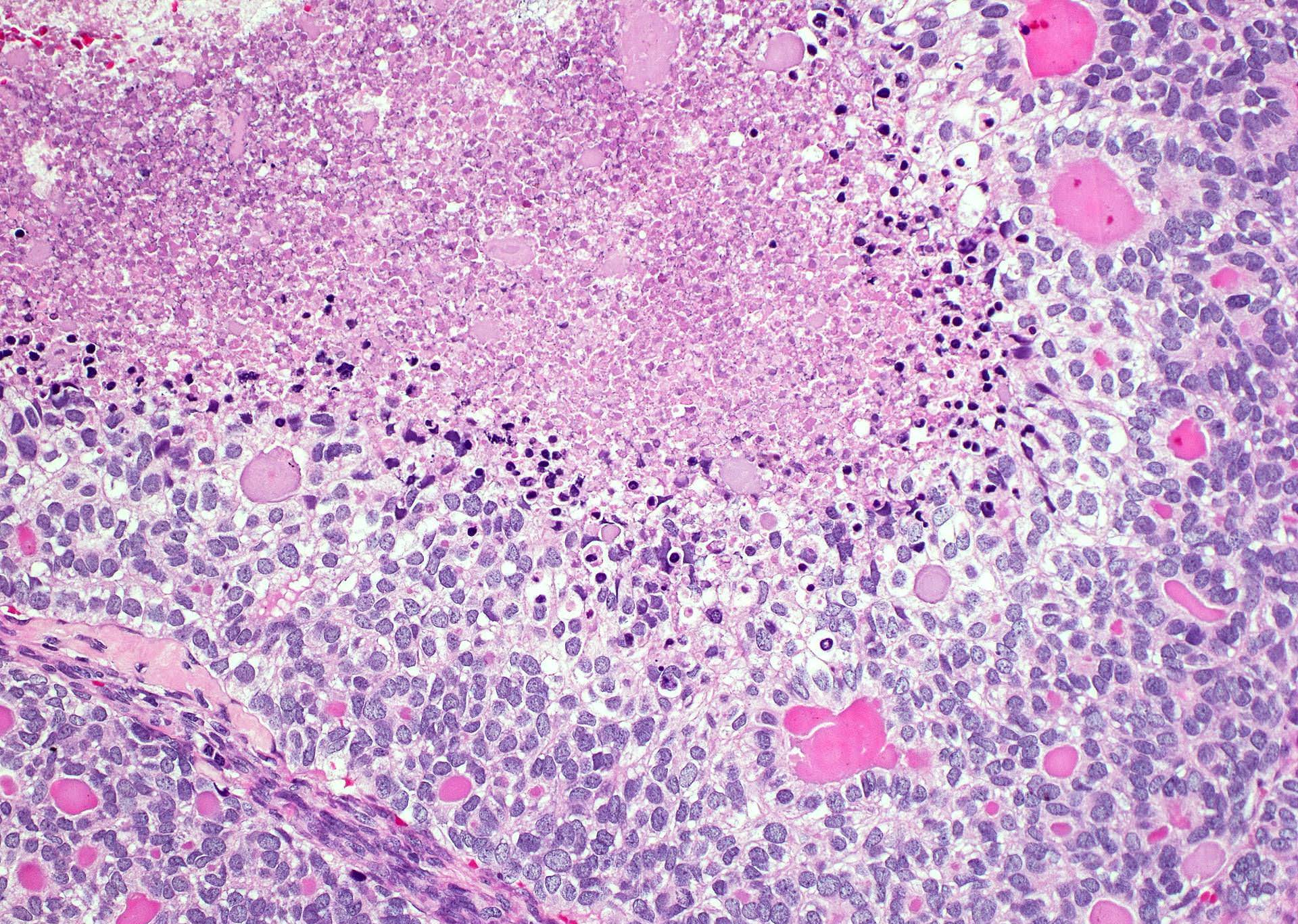
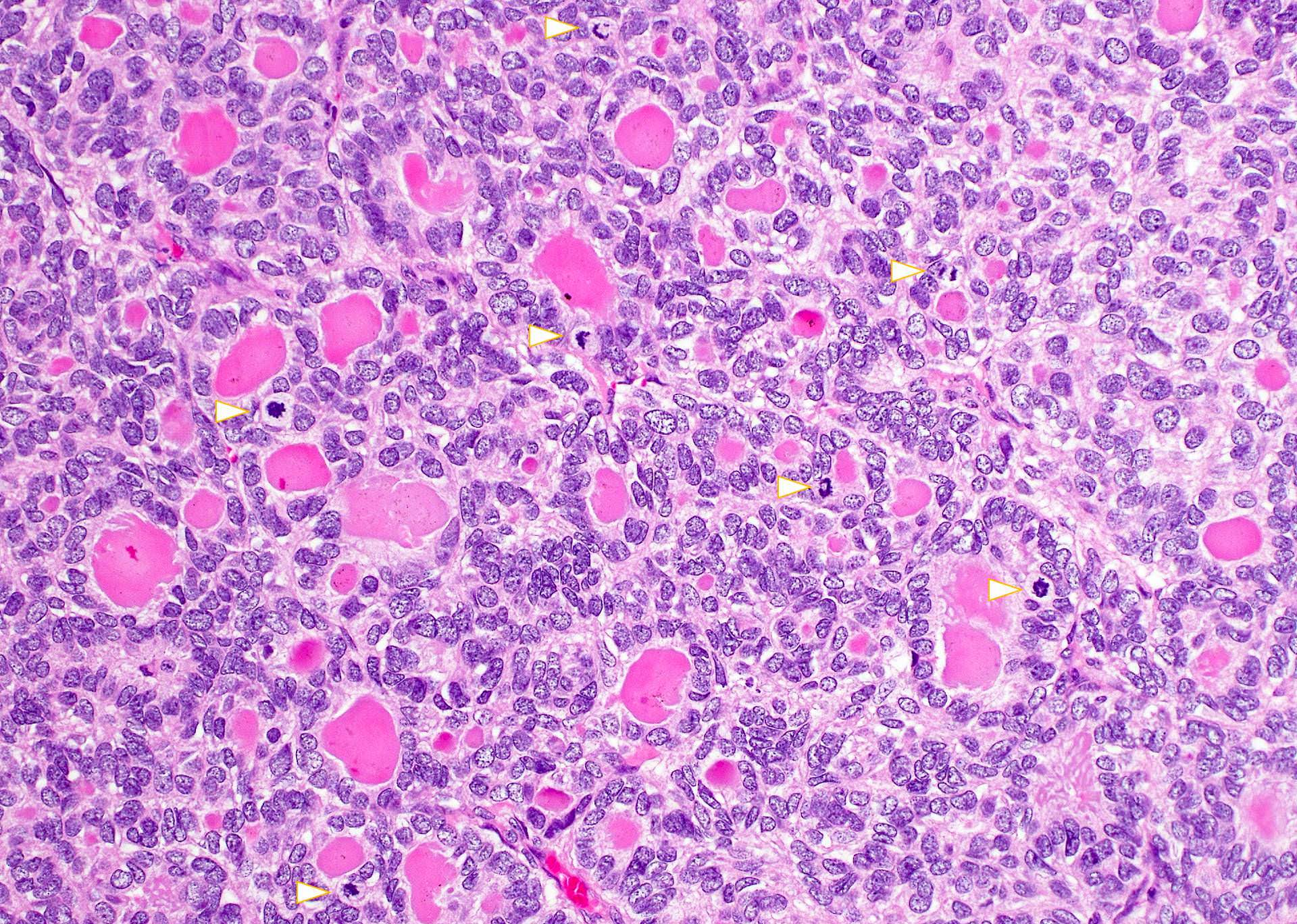
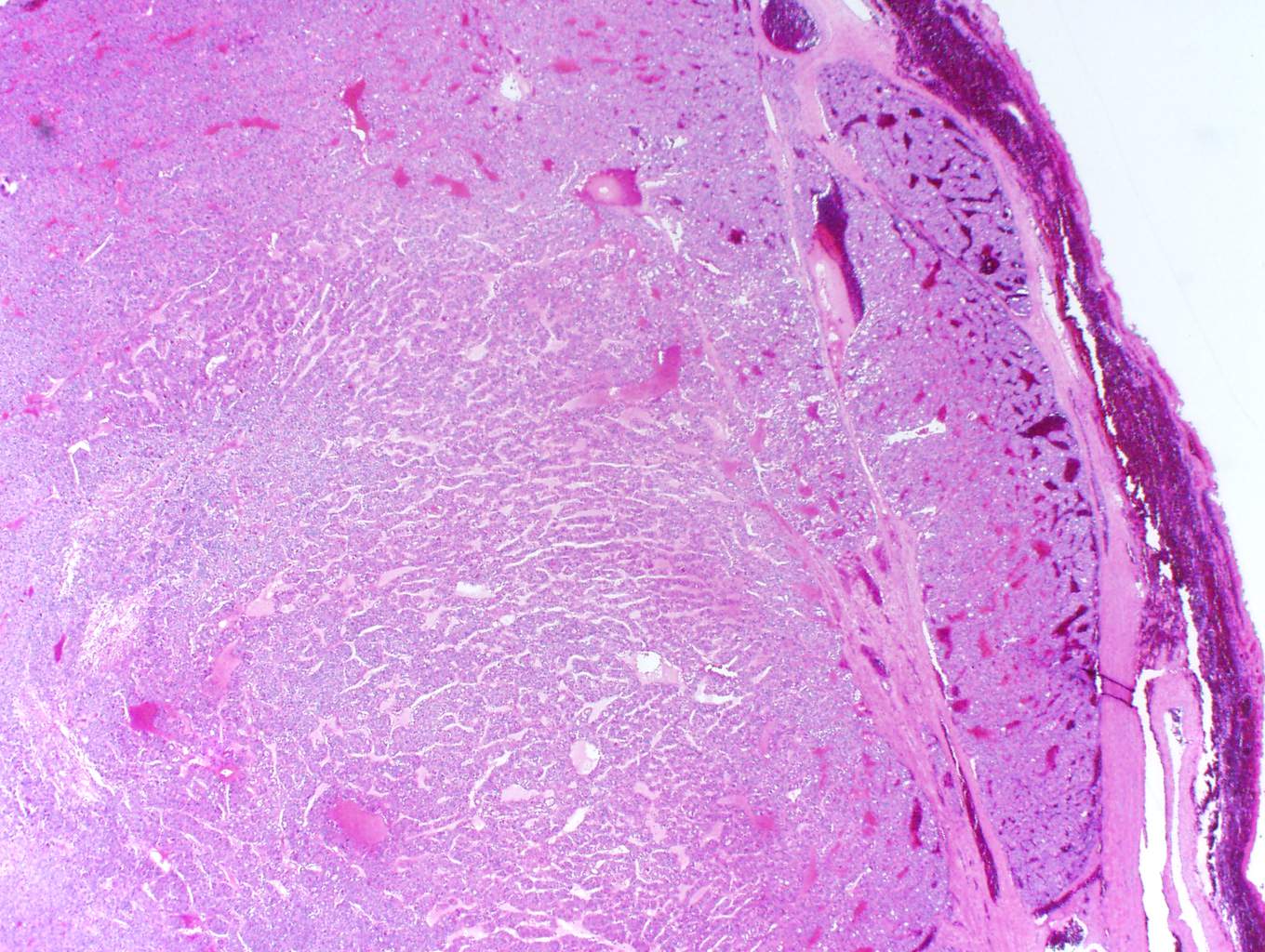
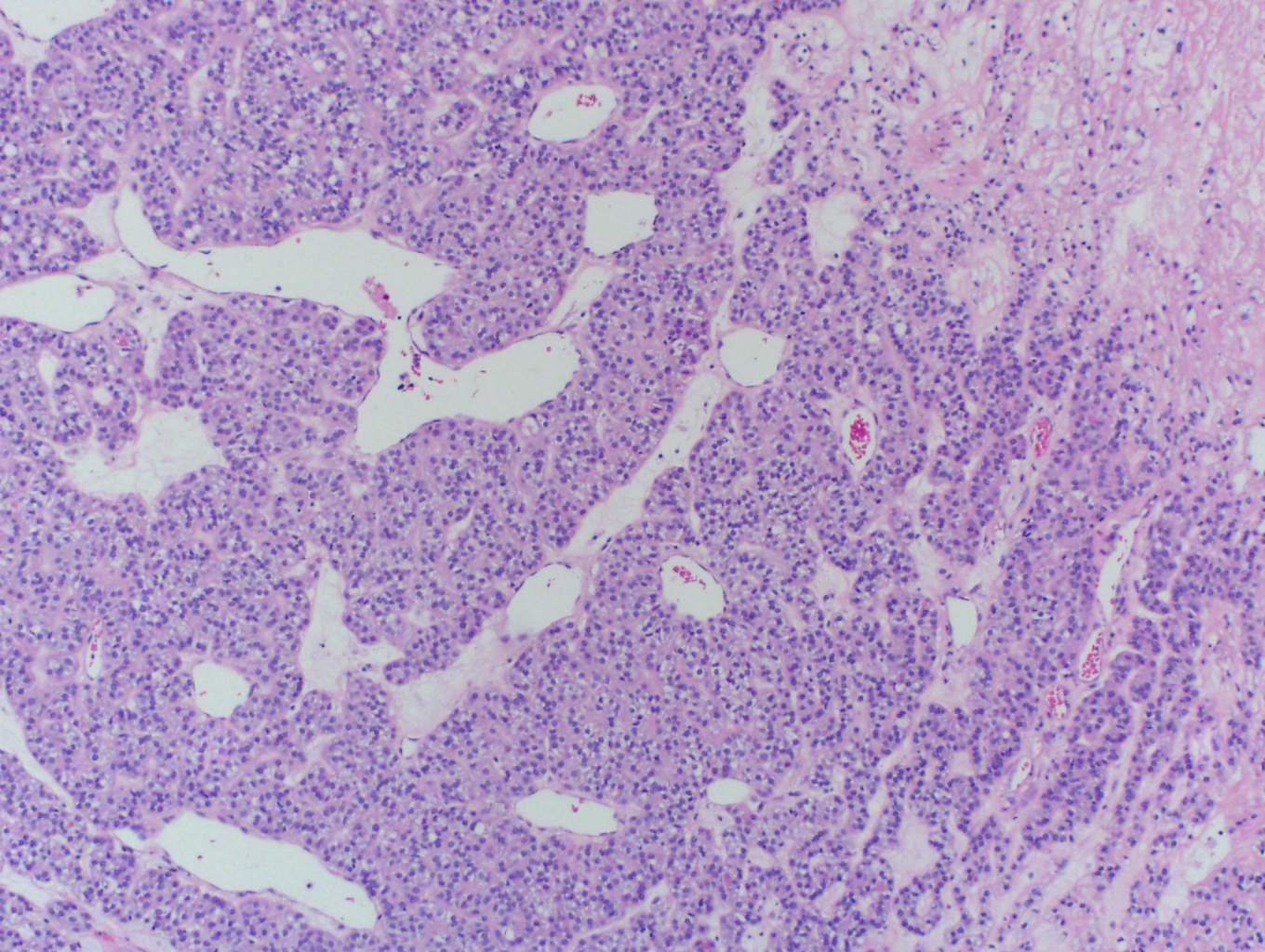
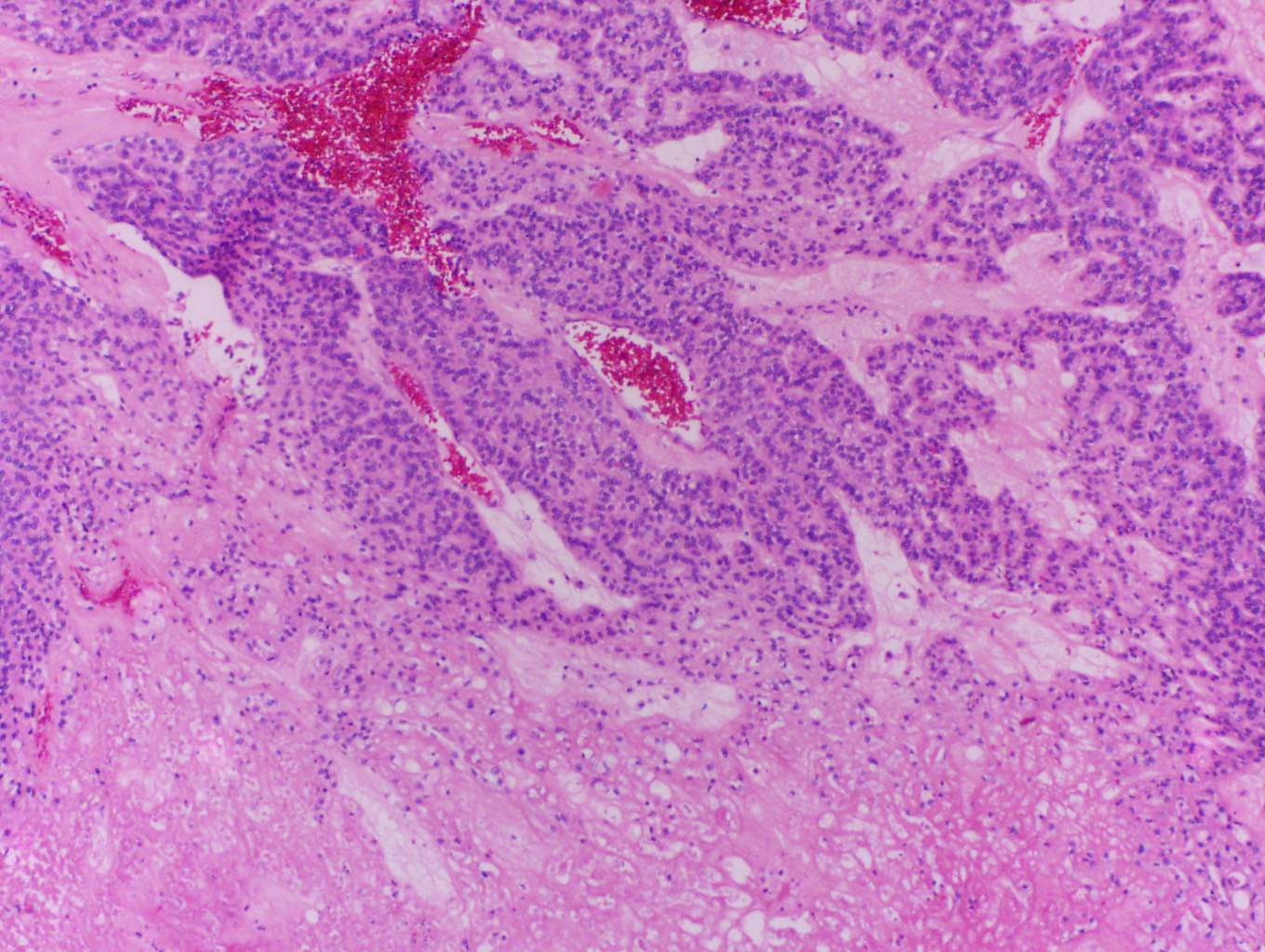
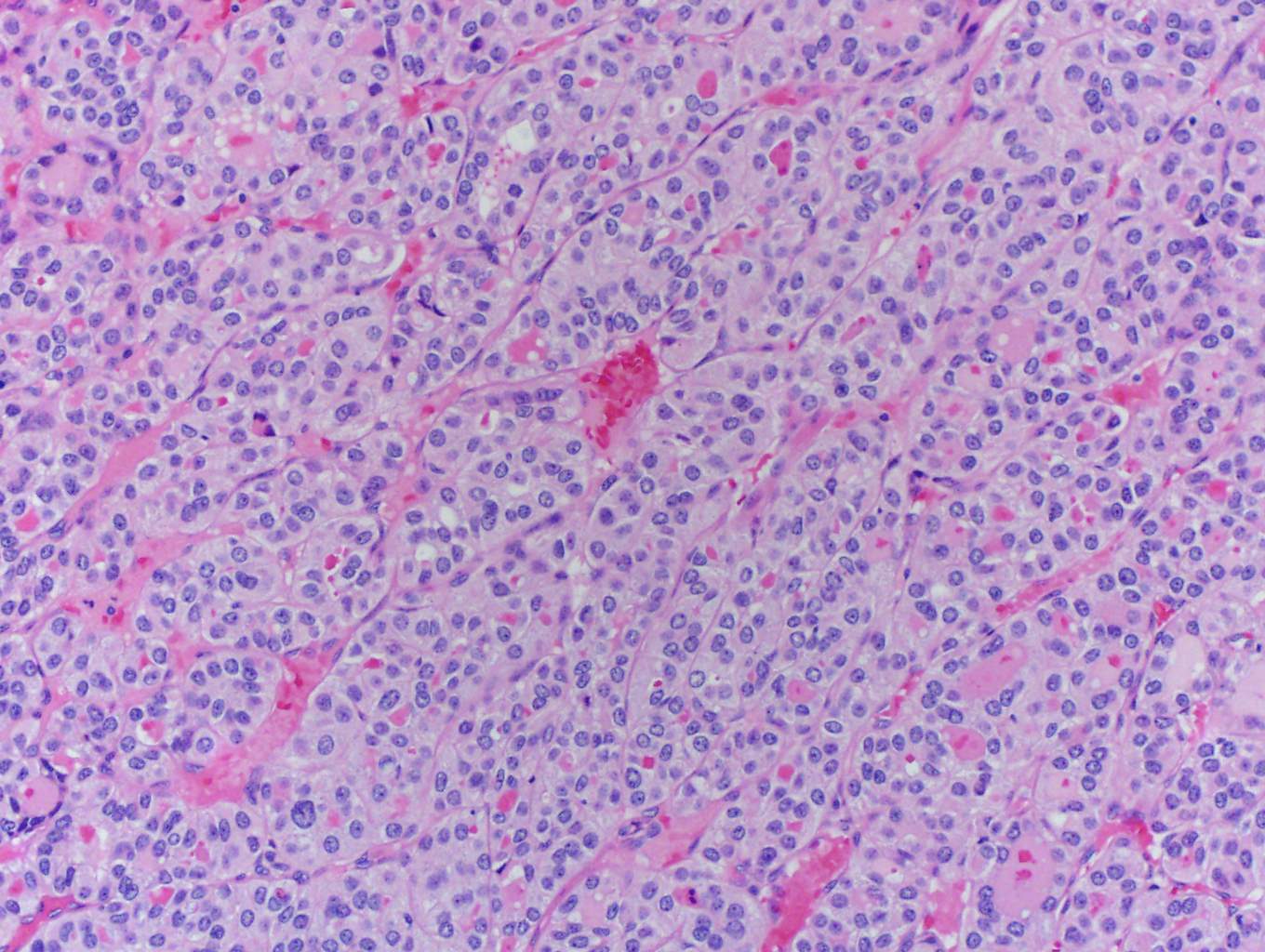
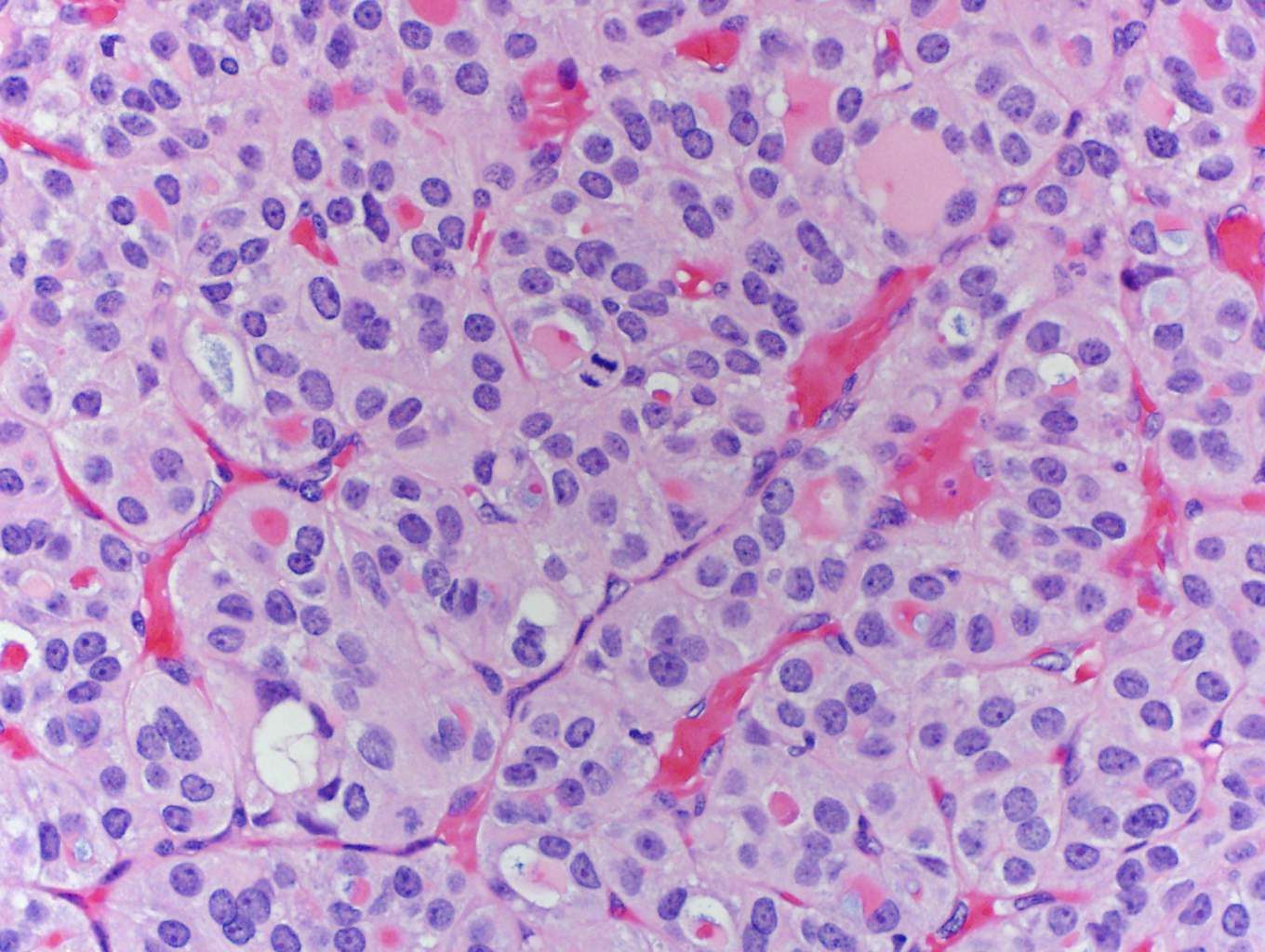
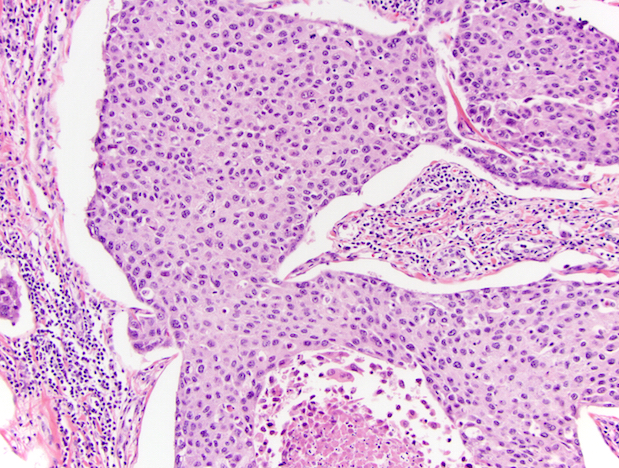
Microscopic (histologic) description
- Turin consensus diagnostic criteria:
- Solid / trabecular / insular growth pattern
- No nuclear features of papillary carcinoma
- Presence of at least one of following: convoluted nuclei, ≥ 3 mitotic figures/10 HPF, tumor necrosis (Am J Surg Pathol 2007;31:1256)
- Other:
- Prototypical type insular carcinoma: solid nests (may contain microfollicules) composed of small uniform cell with round hyperchromatic nuclei or convoluted nuclei, increased mitotic figures, necrosis (Am J Surg Pathol 1984;8:655)
- Others tumors: solid nests composed of larger more pleomorphic tumor cells; may have oncocytic cells, clear cells, signet ring cells or rhabdoid cells
- Component of well differentiated tumor (papillary or follicular carcinoma) may also be present
- As few as 10% of poorly differentiated carcinomas (in otherwise well differentiated carcinomas) may be associated with unfavorable prognosis (Am J Surg Pathol 2011;35:1866)
- May have peritheliomatous pattern (tumor cells around blood vessels with necrosis of tumor cells further away from vessels), vascular and capsular invasion (Lloyd: WHO Classification of Tumours of Endocrine Organs, 4th Edition, 2017)
Microscopic (histologic) images
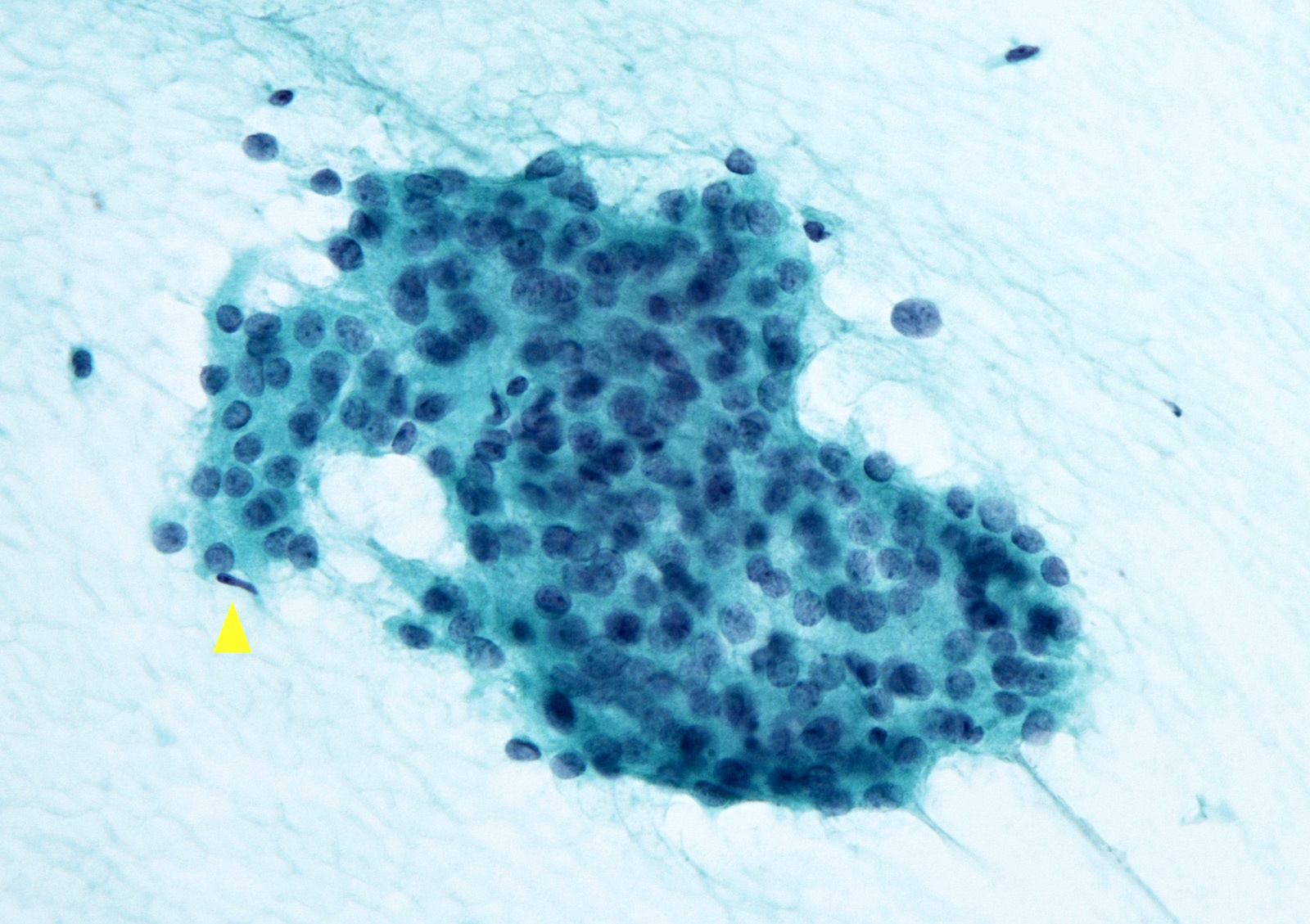
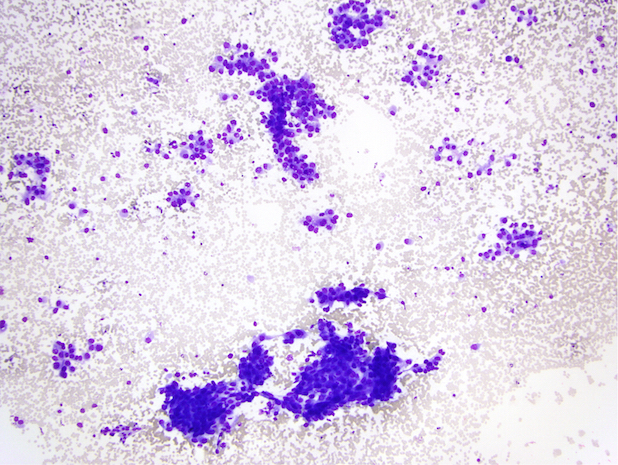
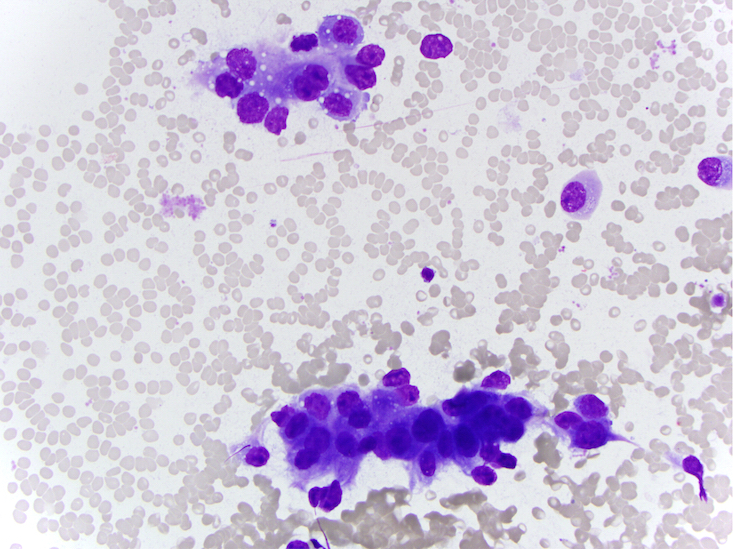
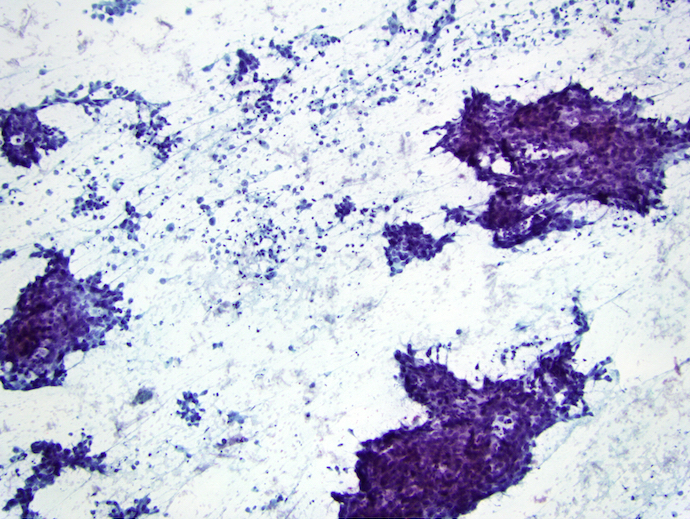
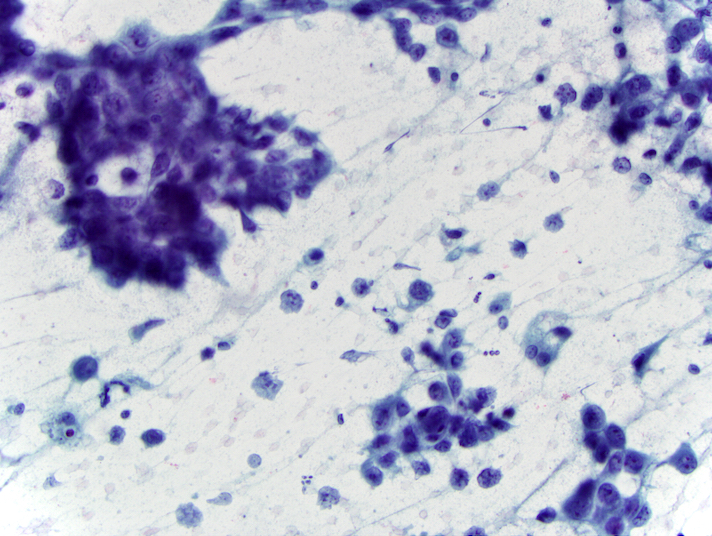
Cytology description
- Highly cellular, crowded cell clusters with solid, trabecular or insular morphology (Cancer 2009;117:185, Cytopathology 2016;27:176)
- Background of single cells with high N:C ratio
- May have necrotic background and increased mitotic figures
Cytology images
Contributed by Ayana Suzuki, C.T. and Shuanzeng Wei, M.D., Ph.D.
Images hosted on other servers:
Positive stains
- Keratin, thyroglobulin (decreased expression), TTF1, Ki67: 10 - 30% (Lloyd: WHO Classification of Tumours of Endocrine Organs, 4th Edition, 2017)
Negative stains
Molecular / cytogenetics description
- Alteration of early event of thyroid carcinogenesis: RAS family and BRAF mutation (Surg Pathol Clin 2014;7:475)
- Alteration associated with dedifferentiation: mutation of p53, TERT, CTNNB1 and AKT1 (Lloyd: WHO Classification of Tumours of Endocrine Organs, 4th Edition, 2017)
Videos
Poorly differentiated thyroid carcinoma by M. Brandwein (2020)
Differential diagnosis
- Anaplastic thyroid carcinoma:
- Completely lacks follicular differentiation, prominent nuclear pleomorphism and necrosis
- Generally thyroglobulin- TTF1- (Surg Pathol Clin 2014;7:475)
- Hürthle cell tumors:
- Poorly differentiated thyroid carcinoma can be predominantly composed of oncocytic cells (often with a small cell component) but also has necrosis and ≥ 3 mitoses/10 HPF
- Metastatic carcinoma to thyroid:
- Pertinent tumor history
- Medullary thyroid carcinoma:
- Also has nesting pattern
- In addition, has prominent vasculature, granular cytoplasm and finely stippled chromatin, calcitonin+ thyroglobulin- with amyloid
- Parathyroid carcinoma:
- PTH+
- Solid variant papillary thyroid carcinoma:
- Typical papillary nuclear features throughout
Additional references
Practice question #1
Which of the following features are not required for the diagnosis of poorly differentiated thyroid carcinoma?
- Absence of conventional nuclear features of papillary thyroid carcinoma
- Necrosis / convoluted nuclei / increased mitotic activity
- Solid, trabecular or insular growth
- Vascular invasion
Practice answer #1
D. Vascular invasion. The Turin criteria specify solid / trabecular / insular growth, lack of conventional nuclear
features of papillary thyroid carcinoma and one of the following: necrosis, convoluted
nuclei or increased mitotic activity (3 or more mitoses/10 HPF). Vascular invasion
may be seen in a variety of thyroid carcinomas and is an adverse prognostic factor
regardless of histologic subtype or grade.
Comment Here
Reference: Poorly differentiated thyroid carcinoma
Comment Here
Reference: Poorly differentiated thyroid carcinoma