Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Diagrams / tables | Pathophysiology / etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Negative stains | Videos | Differential diagnosis | Additional referencesCite this page: Bychkov A. Thyroglossal duct cyst. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidthyroglossal.html. Accessed August 14th, 2025.
Definition / general
- The most common developmental anomaly of thyroid gland, and the most common congenital neck mass
- Midline neck developmental anomaly due to persistence and cystic dilation of thyroglossal duct
- Thyroglossal duct (TGD) is the embryonic tract characterized by the presence of epithelial lined remnants and heterotopic thyroid tissue
- May appear as blind tubular structure in mid neck or as sinus tract connected to foramen cecum or suprasternal notch skin
Terminology
- Synonyms: TGD anomaly, TGD remnant, thyroglossal or thyreoglossal, thyroglossal duct or thyroglossal tract
- Sinus is a blind ending tract lined by granulation tissue leading deep inside from natural / normal epithelial surface, e.g. from cervical skin or foramen cecum to TGD cyst (the latter, even being epithelialized, is not considered as a normal postnatal structure)
- Fistula is a communication between two normal epithelialized surfaces, e.g. between skin and oropharynx via TGD tract / cyst, which is extremely rare (Laryngoscope 2009;119:2345)
- TGD fistula is often used erroneously to represent the discharging sinus
Epidemiology
- TGD cyst is the most common congenital anomaly of the neck in childhood, and the most common developmental neck cyst, accounting for 60% - 70% of all cases (Head Neck Surg 1982;5:134, Auris Nasus Larynx 2008;35:11)
- Mean age 30 - 40 years old, with 65% of cases being diagnosed before 30 years of age, and up to 25% in 50+ year old patients (Am J Surg 1988;155:741)
- Ratio of nondraining cyst to sinus or fistula is 4:1
- Discharging sinuses manifest at younger age (Eur Arch Otorhinolaryngol 2015;272:2513)
- M:F = 1:1 (Head Neck Surg 1982;5:134)
- Serial sections on autopsy identified TGD remnants in 7% of both adult and pediatric cohorts (Laryngoscope 1977;87:765, Ann Otol Rhinol Laryngol 2000;109:1135)
- Scintigraphy after TSH stimulation found TGD remnants in > 40% of thyroidectomized patients (Clin Radiol 2015;70:638)
- Out of several thousand TGD cysts described in series and case reports, only 20+ familial cases were published (Pediatr Surg Int 2005;21:593, OMIM - 188455)
Sites
- Appears in midline neck anywhere along path of TGD, from foramen cecum in tongue base to suprasternal region
- Most TGD cysts are connected to hyoid bone, which is excised during TGD excision (Sistrunk procedure)
- Prevalence (J Pediatr Surg 1984;19:555, Int J Pediatr Otorhinolaryngol 2003;67:1285):
- 75% thyrohyoid (between hyoid bone and thyroid cartilage)
- 25% suprahyoid, including submental
- 2% - 4% intralingual (base of tongue)
- Rare sites: suprasternal, intrathyroid, mediastinal
- TDG cysts may present lateral to midline in 1 - 2% but never lateral to large neck vessels
- Mainly deviate to the left, because levator glandulae thyroideae is ordinarily found to the left (Surg Clin North Am 1953:633)
- Often in the region of thyroid cartilage which moves superficial cyst from the median
- Can be dislocated due to inflammation / fibrosis or previous surgery (Int J Pediatr Otorhinolaryngol 2003;67:1285)
Diagrams / tables
Pathophysiology / etiology
- During embryonic development, thyroid gland remains connected to the foramen cecum (floor of primordial pharynx) and hyoid bone by TGD; the duct gradually disappears by the 10th week of development
- If involution fails, TGD remnants may persist anywhere along the pathway of thyroid descent
- The only normal remnant of the duct is the pyramidal lobe of the thyroid gland, which is seen in about 40% of the population (Thyroid 2013;23:84)
- Cystic dilation is a result of secretion from the lining epithelial cells
- Inflammation of lymphoid tissue adjacent to the TGD (repeated respiratory infections) may stimulate the epithelial remnants of thyroglossal tract to undergo cystic changes (BJS 1925;12:561)
- Sinus is formed secondary to trauma, inadequate surgery drainage or spontaneous rupture of infected TGD cyst, e.g. due to microbial contamination from oral cavity via foramen cecum
Clinical features
- Most patients are asymptomatic, with a slowly enlarging painless cystic mass in the midline anterior neck (perihyoid), 2 - 4 cm in size (Auris Nasus Larynx 2008;35:11)
- On physical examination, the cyst can be soft or firm and move upward on swallowing or protrusion of tongue
- Infected TGD cyst occurs in 30% of patients, who present with pain, local inflammation, sometimes with draining sinus or fistula (Semin Pediatr Surg 2006;15:70)
- After radiation therapy for unrelated head and neck cancer, TGD may enlarge and undergo cystic transformation (AJNR Am J Neuroradiol 2009;30:800)
- Lingual TGD cyst may cause dysphagia, choking and cough; in neonates, may cause feeding problems, respiratory compromise and even sudden death
- Rarely (< 1%), TGD may give rise to tumors, usually papillary thyroid carcinoma, but also benign follicular adenomas, including Hurthle cell adenoma
Diagnosis
- Based on typical clinical manifestations supported by radiological findings and confirmed by postoperative histopathology
- Ultrasound is the preoperative investigation of choice (Radiographics 2014;34:37):
- Echogenic characteristics of TGD cyst are cyst location, relation to the hyoid bone and echotexture of thyroid gland
- CT and MRI play a supplementary role to more accurately delineate anatomy of large cysts, and MRI may be utilized to define a residual fistulous tract in recurrent disease (Auris Nasus Larynx 2008;35:11)
Radiology description
- Ultrasound (Korean J Radiol 2015;16:419, Clin Radiol 2005;60:141):
- Midline (just under the hyoid bone) well circumscribed anechoic cystic lesion in simple TGD cyst
- Pseudosolid appearance, when the cyst contains a proteinaceous fluid, cholesterol crystals and keratin
- Heterogeneous pattern with internal echoes in cases of previous infection or hemorrhage
- Most pediatric TGD cysts have a pseudosolid appearance
- True solid component suggests risk of TGD malignancy
- CT with contrast shows a well delineated cystic lesion with capsular enhancement (especially in infected cysts), and its relation to hyoid bone (Indian J Surg 2011;73:28)
- MRI demonstrates low signal intensity with T1 weighted sequences and high signal intensity with T2 weighted sequences which do not restrict diffusion; expansion and destruction of the cartilaginous structure of the hyoid (Radiographics 2014;34:37)
- Scintigraphy potentially can detect functioning thyroid tissue in TGD (Thyroid 2007;17:341)
Radiology images
Prognostic factors
- Excellent prognosis after complete excision, even if carcinoma is present
- Recurrence rate after Sistrunk procedure is less than 5%; however, if the central hyoid bone is not removed, TGD cyst may recur in 25% cases (Surg Gynecol Obstet 1949;89:727)
- Risk factors for complications and recurrence are young age (< 10 y.o.), lobulated, infected or ruptured cyst, skin involvement and failure to excise the midportion of the hyoid bone and the suprahyoid tract (Am J Surg 1986;152:602)
Case reports
- Various locations
- Newborn with TGD cyst on the tongue base (Case Rep Obstet Gynecol 2016;2016:781630)
- Infant with lingual TGD cyst (Respir Care 2014;59:e98)
- 10 year old girl with intrahyoid TGD cyst (Indian J Otolaryngol Head Neck Surg 2007;59:366)
- 28 year old man with migratory TGD cyst (Indian J Radiol Imaging 2010;20:115)
- 31 year old man with intralaryngeal TGD cyst (Pan Afr Med J 2015;22:294)
- 40 year old woman with TGD cyst within the mediastinum (J Thorac Cardiovasc Surg 2007;133:1671)
- 45 year old woman with intrathyroid TGD cyst (Int J Clin Exp Pathol 2015;8:7229)
- Complications
- Infant died of fatal asphyxia by a TGD cyst (Am J Forensic Med Pathol. 2008;29:251)
- 6 year old girl with hypothyroidism after excision of TGD cyst (J Pediatr 2013;162:427)
- 14 year old girl with infected TGD cyst (Case Rep Dent 2011;2011:978263)
- 18 year old man with follicular adenoma in TGD (Braz J Otorhinolaryngol 2007;73:430)
- 18 year old woman with Hurthle cell adenoma arising in a TGD cyst (Head Neck 1993;15:348)
- 23 year old woman with infected TGD cyst (West J Emerg Med 2009;10:205)
- 28 year old man with follicular adenoma in TGD cyst and papillary carcinoma in the thyroid (Am J Otolaryngol 2005;26:348)
- 40 year old man with ruptured TGD cyst leading to xanthogranulomatous inflammation (Head Neck Pathol 2015;9:530)
- 46 year old woman with extravasation mucocele arising from a lingual TGD remnant (Case Rep Otolaryngol 2015;2015:326251)
- 55 year old man died of fatal asphyxia by a TGD cyst (J Clin Forensic Med 2006;13:349)
- 65 year old man with giant TGD cyst (Indian J Otolaryngol Head Neck Surg 2011;63:27)
- Unusual combinations
- 7 year old boy with double cyst originated from a single TGD (J Pediatr Surg 2008;43:748)
- 15 year old girl with cartilage within a TGD anomaly (Int J Pediatr Otorhinolaryngol 1988;15:205)
- 18 year old woman with epidermal, TGD and lymphoepithelial neck cysts (J Oral Maxillofac Pathol 2013;17:479)
- 20 year old man with ectopic thyroid in the floor of the mouth and functioning TGD cyst without orthotopic thyroid gland (Singapore Med J 2013;54:e149)
- 35 year old woman with metachronous TGD cyst and inferior parathyroid cyst (Kaohsiung J Med Sci 2008;24:487)
- 52 year old woman with ectopic thyroid nodule in TGD (Korean J Intern Med 2011;26:218)
- 85 year old woman with large TGD cyst and lingual hemangioma (BMJ Case Rep 2011;2011)
Treatment
- Surgery is routinely recommended for all patients with TGD cysts
- The treatment of TGD remnants, whether cyst or sinus / fistula, is a complete surgical excision using the Sistrunk procedure
- This consists of a block excision of the entire TGD to the foramen cecum, and removal of the middle third of the hyoid bone (Operative Techniques in Otolaryngology 2004;15:220)
- Incision / draining or sclerotherapy is strictly discouraged
Clinical images
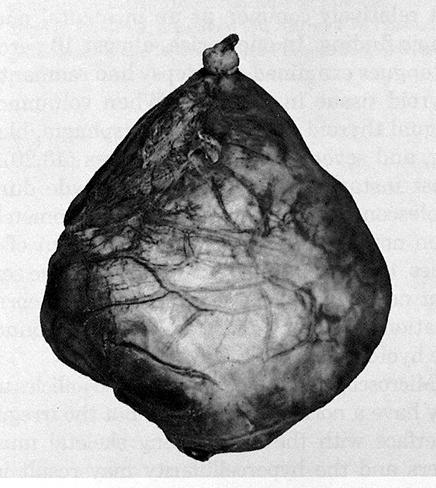
Gross description
- The thyroglossal duct is a continuous tract from the base of tongue, but occasionally is multiple and aborizing, with a dominant cyst and smaller cysts that are identified microscopically (J Pediatr Surg 1984;19:506, J Pediatr Surg 1991;26:766)
- Cysts are unilocular or multilocular with rounded, smooth external surfaces
- Cyst has a mean diameter of 2 cm, range 0.2 - 7 cm (J Am Coll Surg 2002;194:274, Endocr Pathol 2015;26:75), giant cysts >10 cm are also described (Ann Surg 1954;139:123)
- Cystic content includes clear mucinous or viscous fluid / gel having a broad range of color (clear, yellowish tan, reddish brown and grayish white) and degree of opacity; infected cysts contain purulent exudate
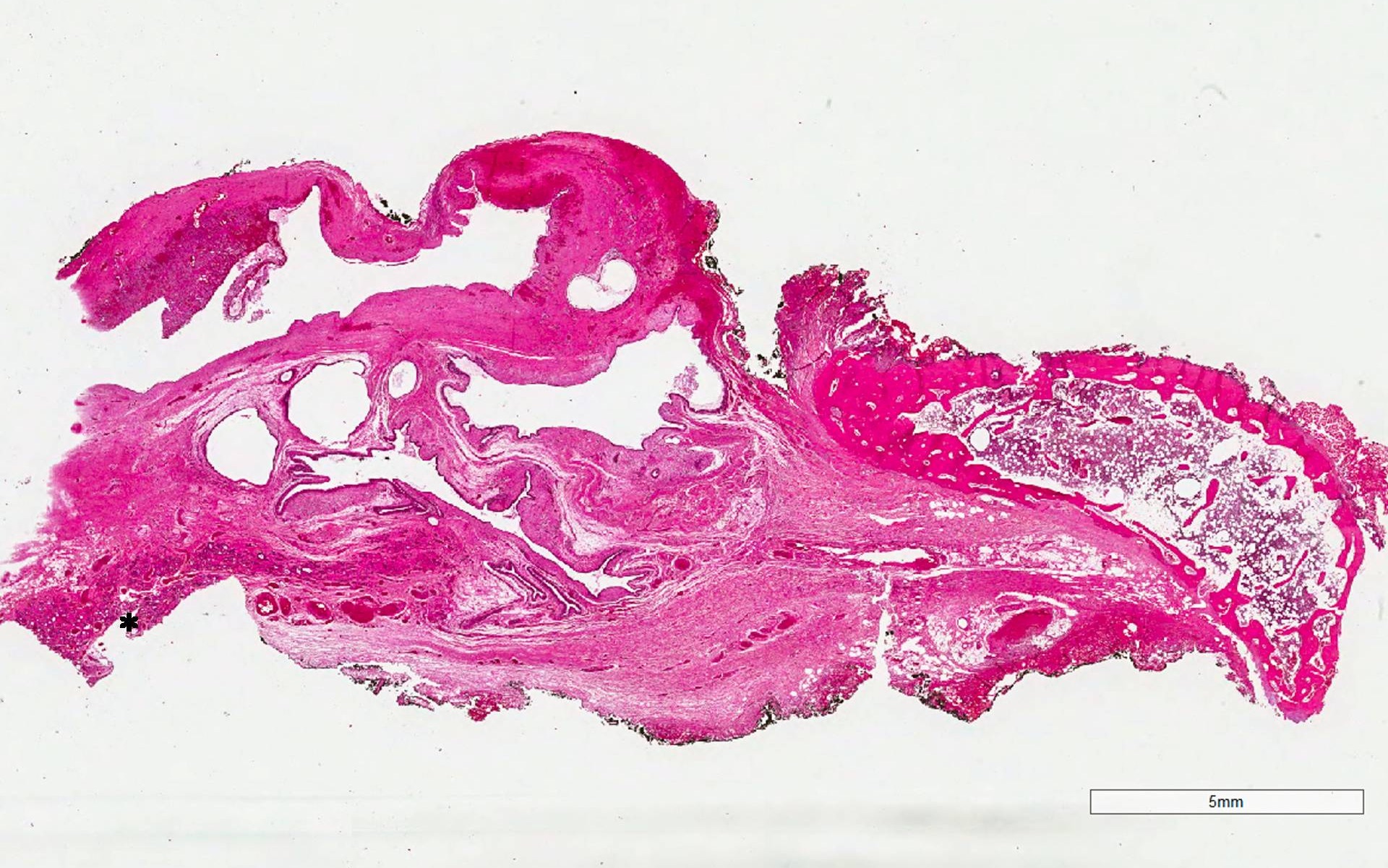
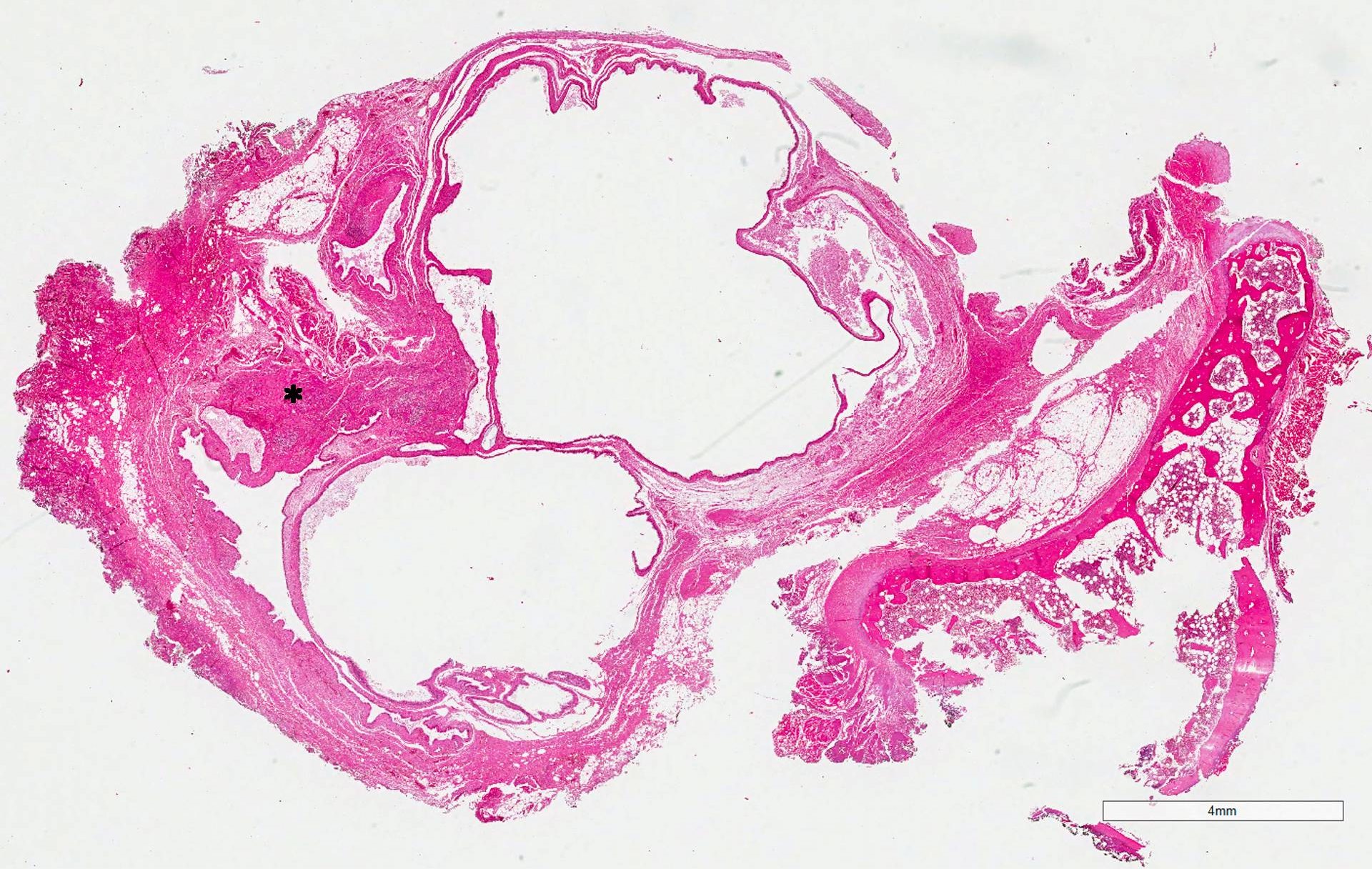
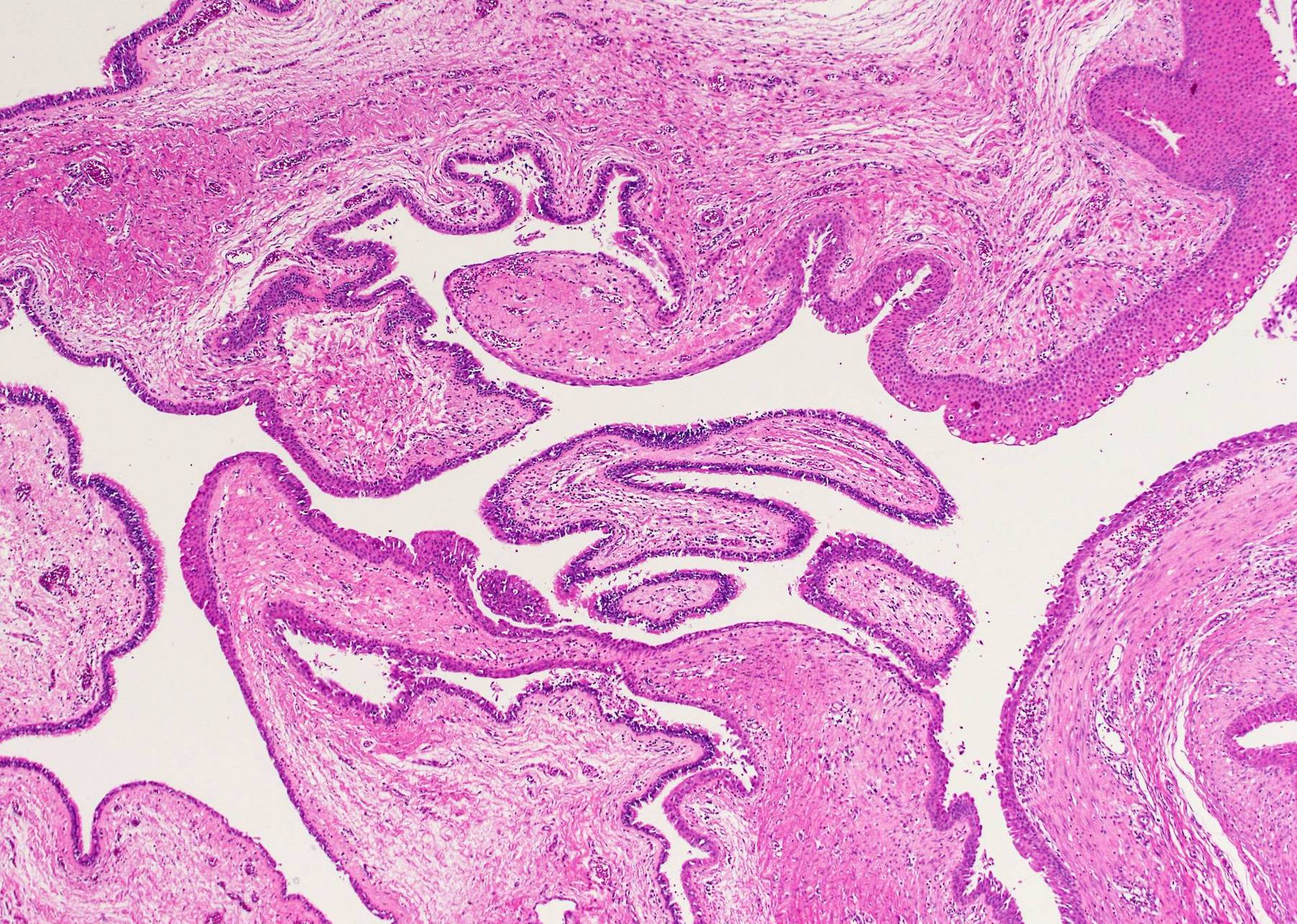
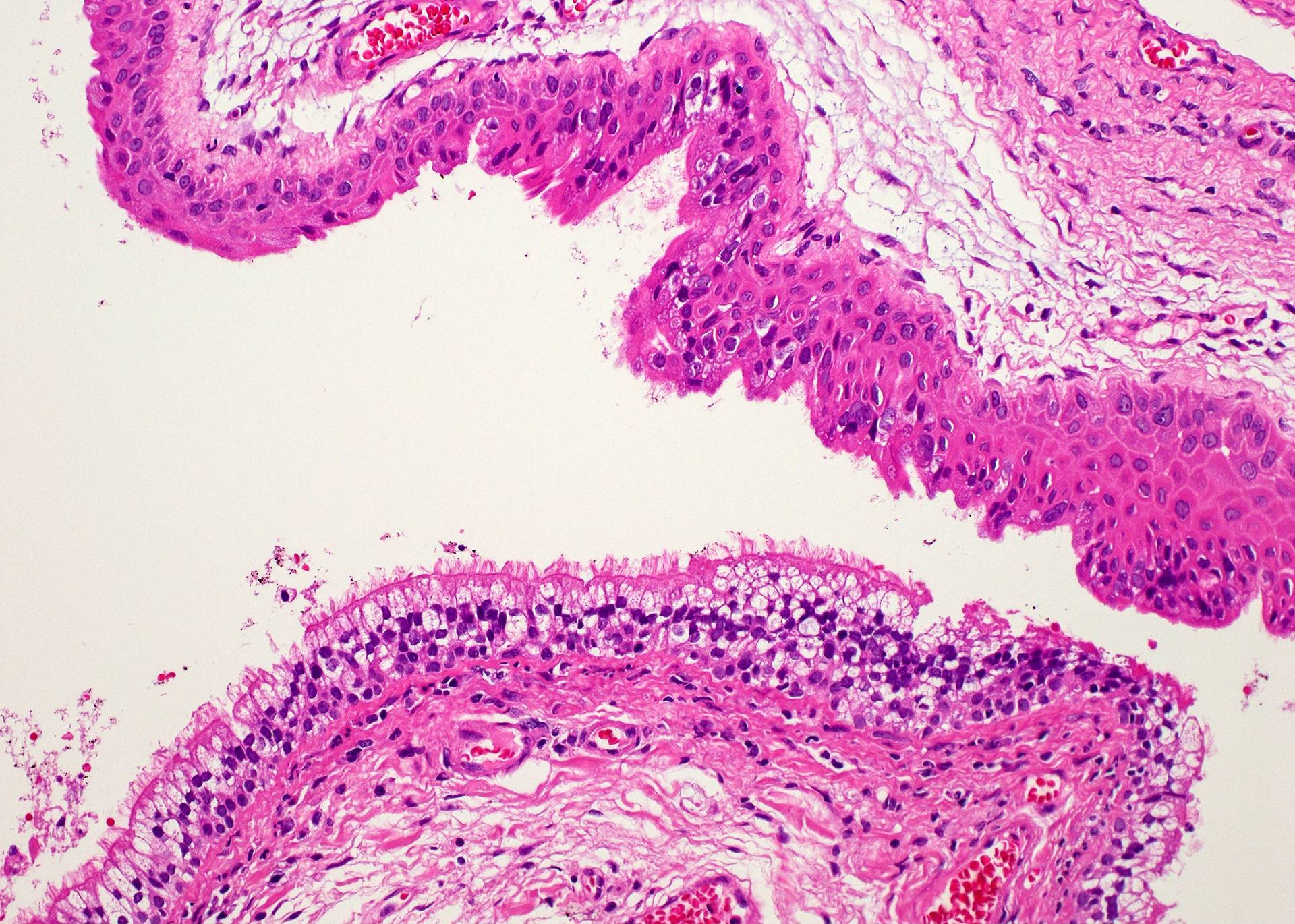
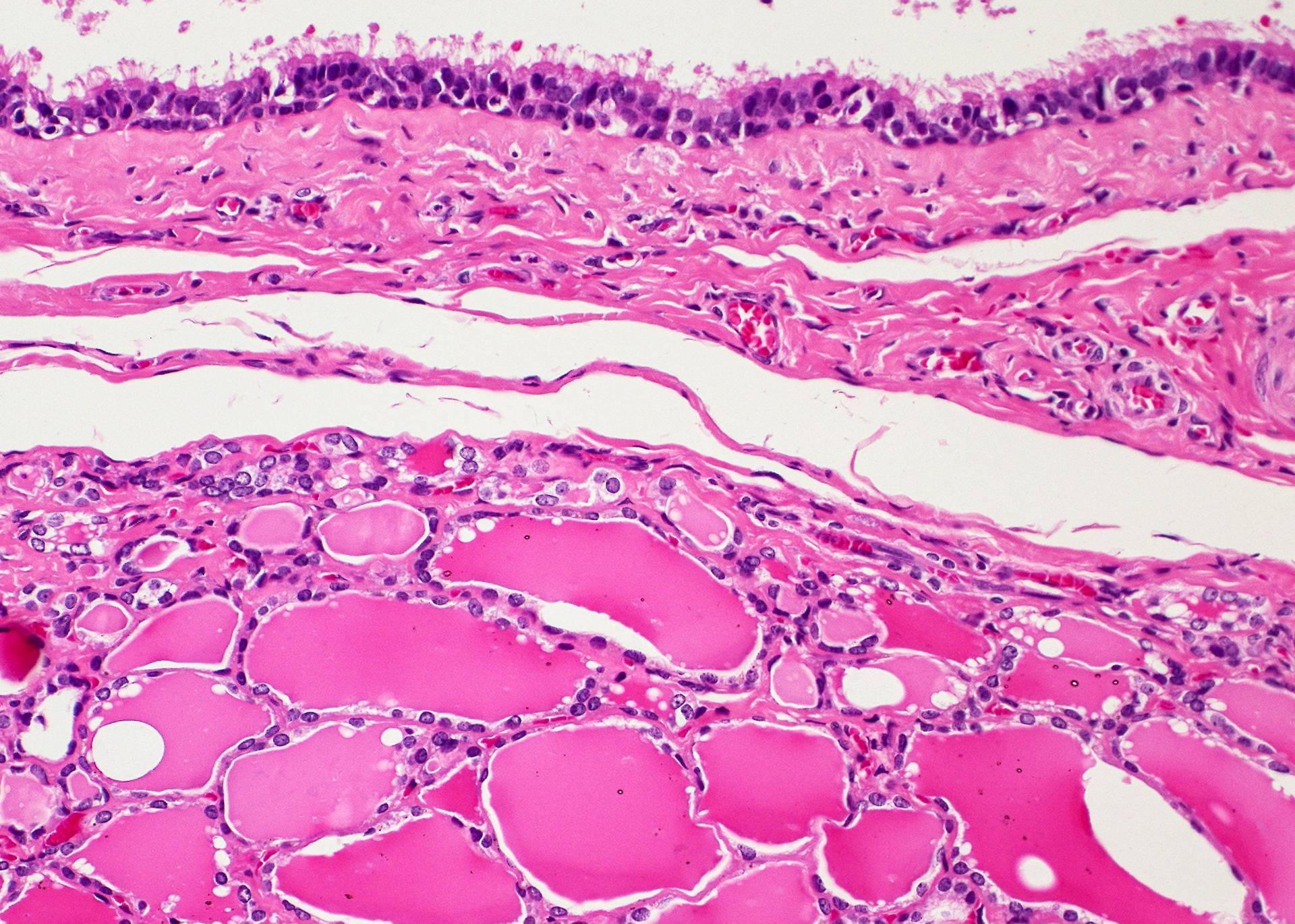
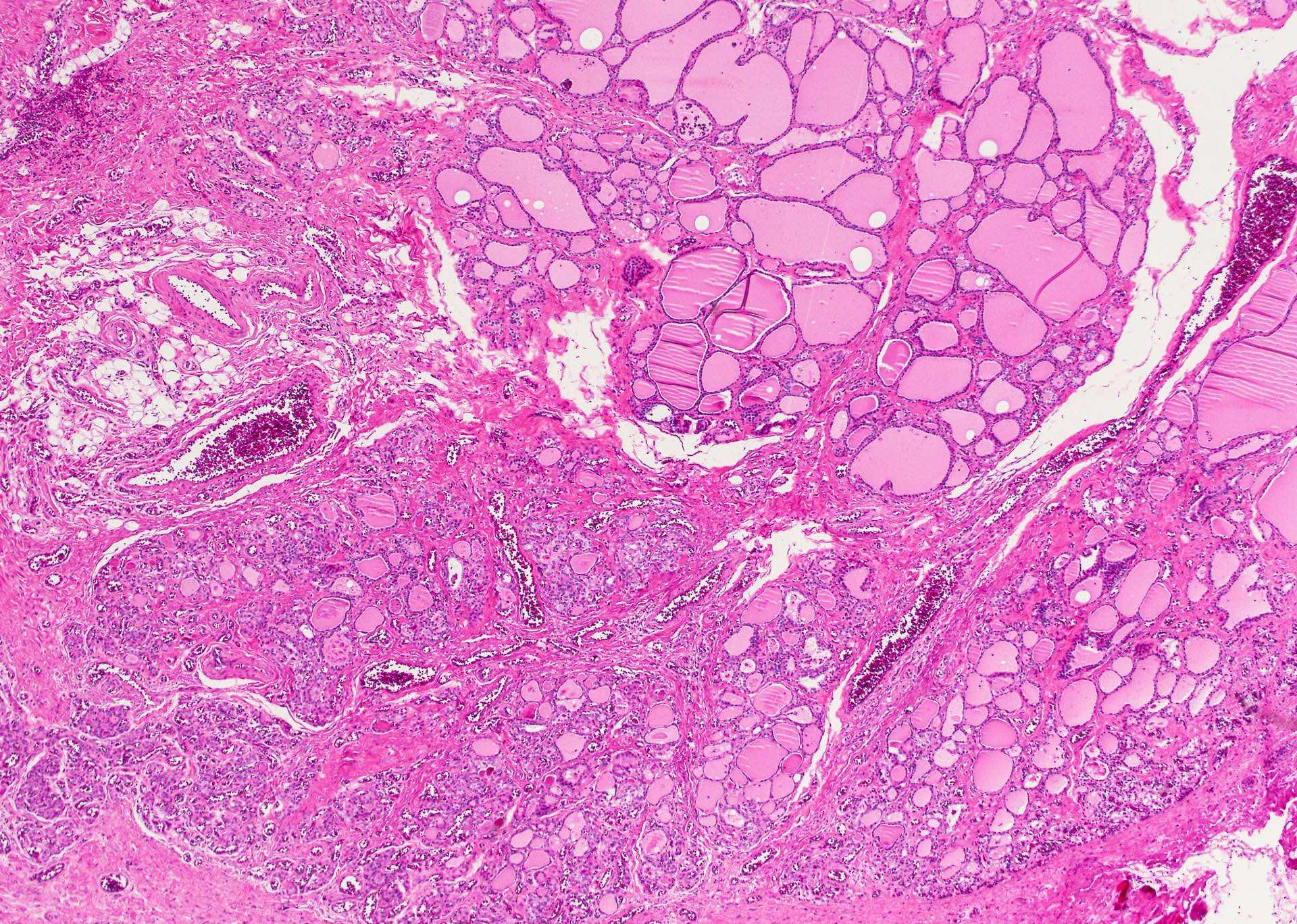
Microscopic (histologic) description
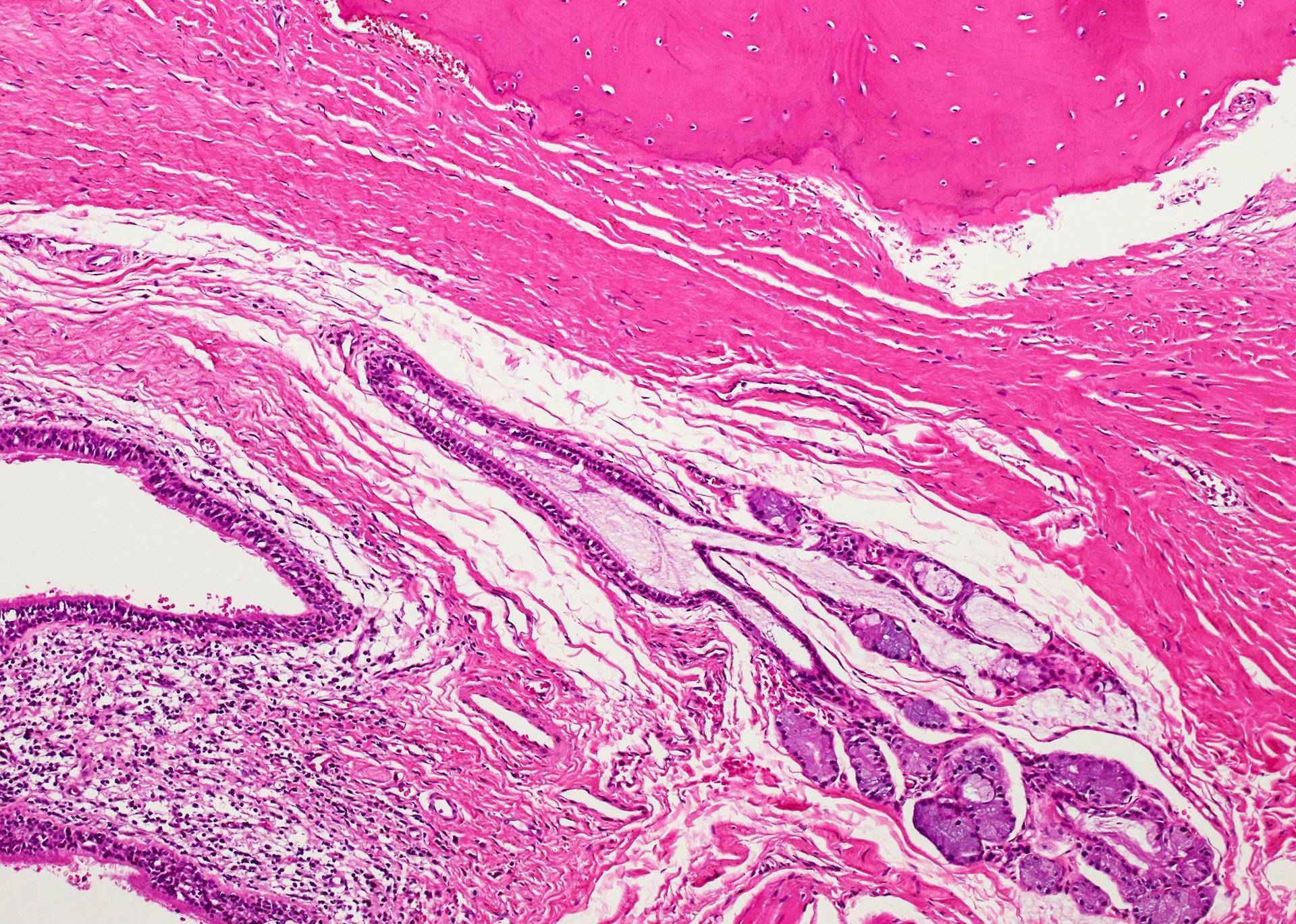
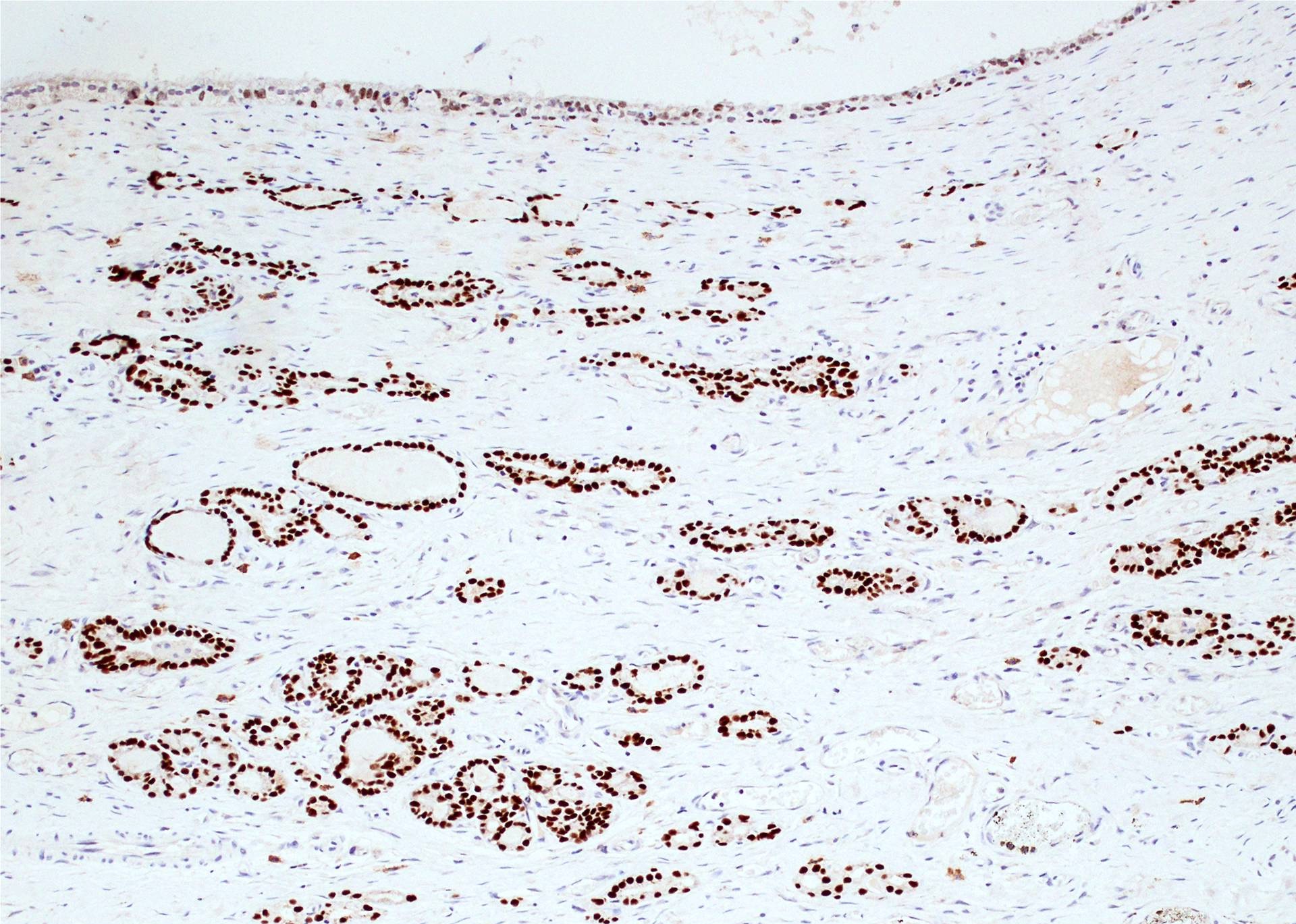
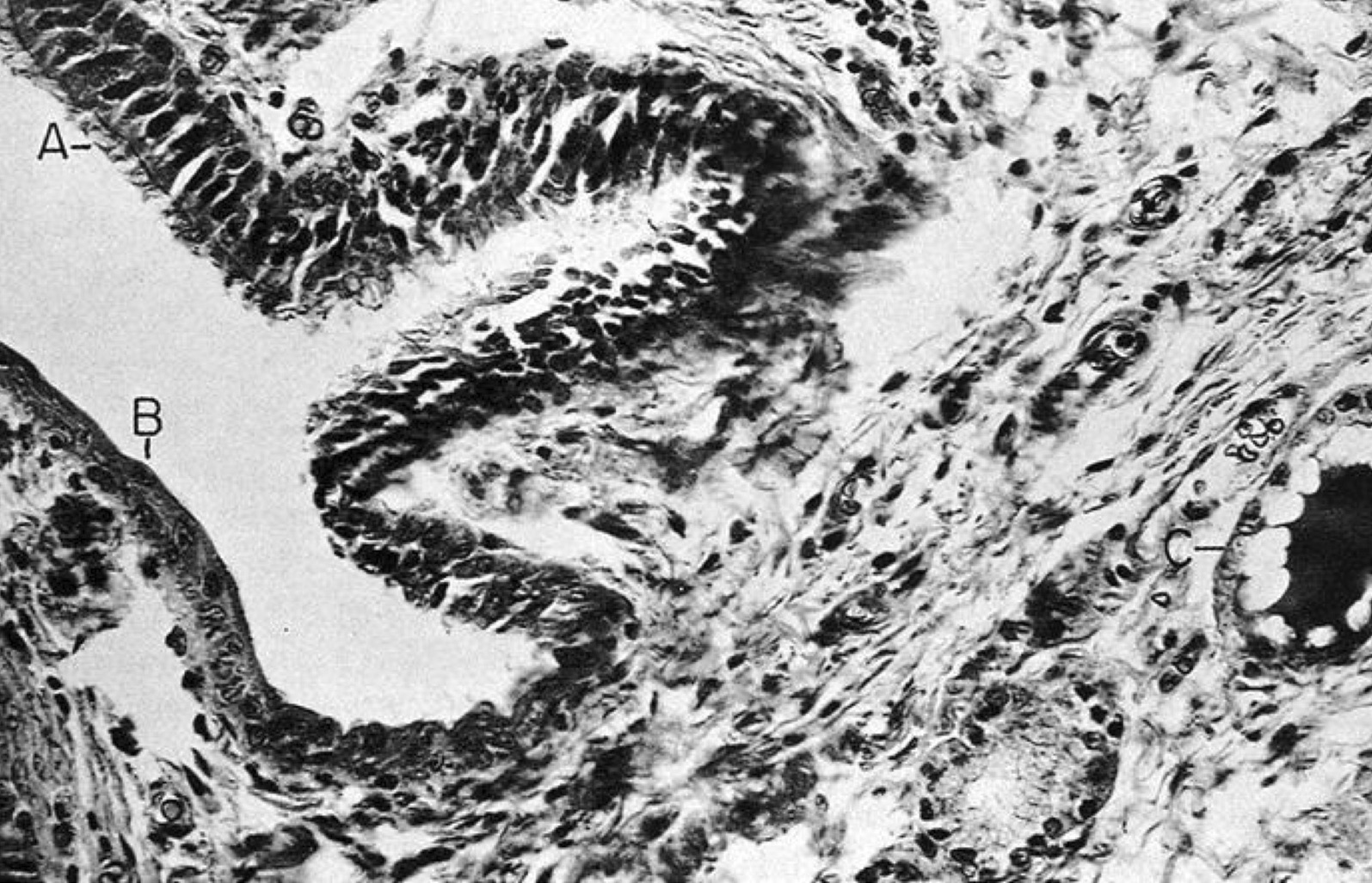
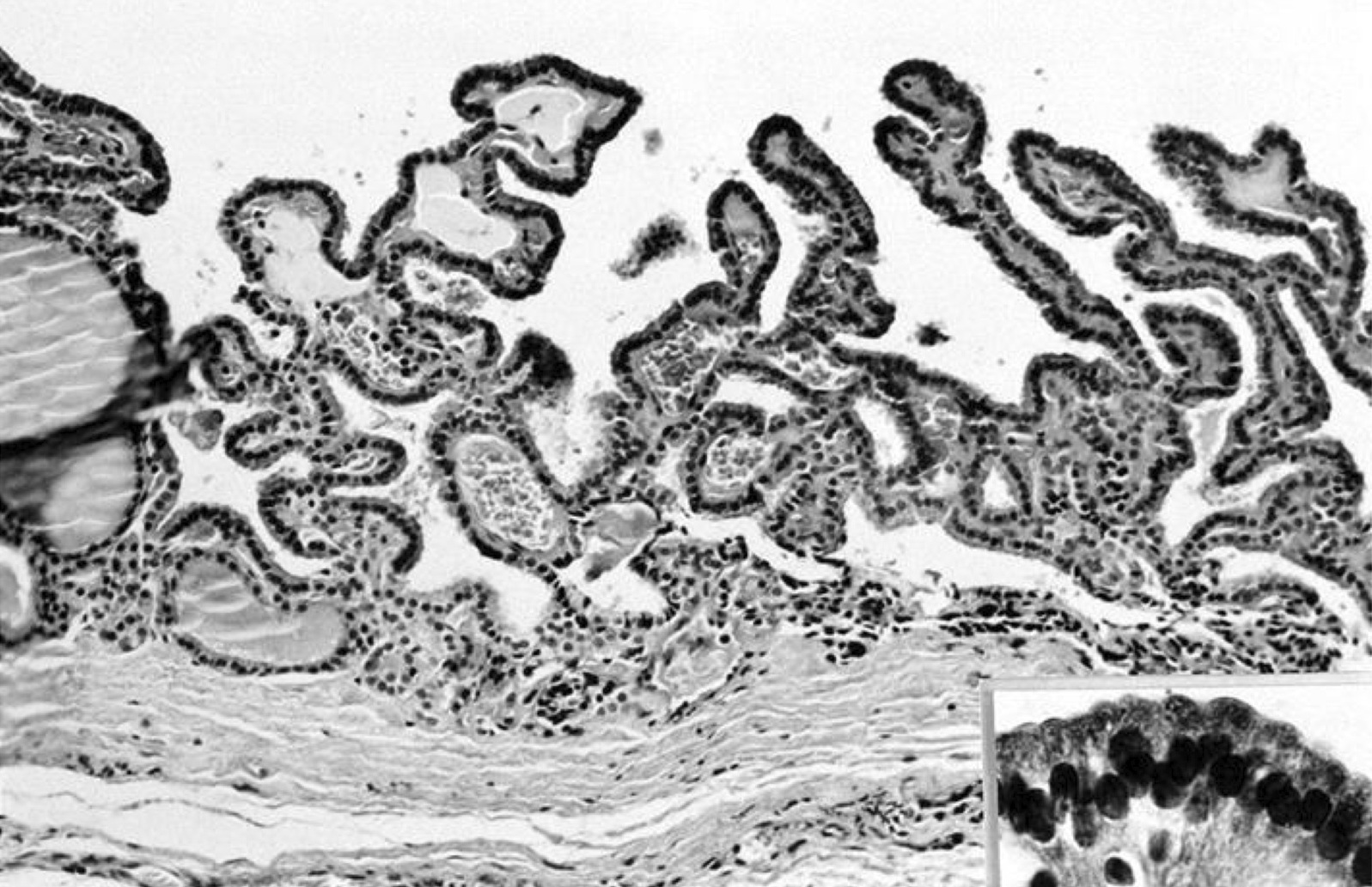
- Type of epithelial lining varies by site, and combinations of the types below can be seen in a single cyst (Head Neck Pathol 2013;7:50):
- Ciliated pseudostratified columnar (respiratory) epithelium in lower neck, perhaps due to its close proximity to upper respiratory tract
- Nonkeratinizing squamous epithelium in higher neck (near tongue and foramen cecum), also can be of metaplastic origin in inflammatory settings
- Stratified cuboidal epithelium at level of hyoid bone
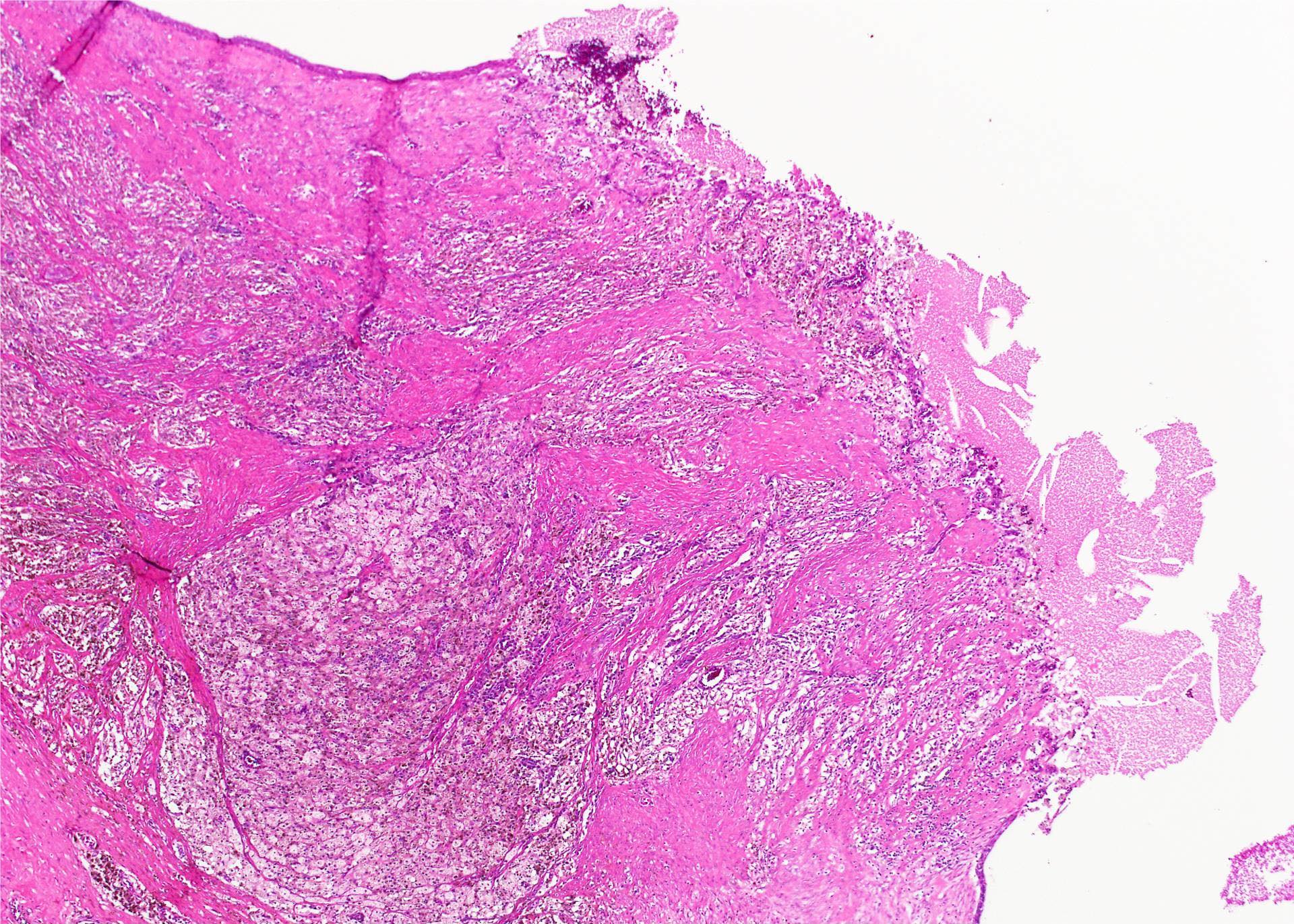
- Very often the cyst is denuded of epithelium, at least focally, which reflects epithelial damage by inflammation
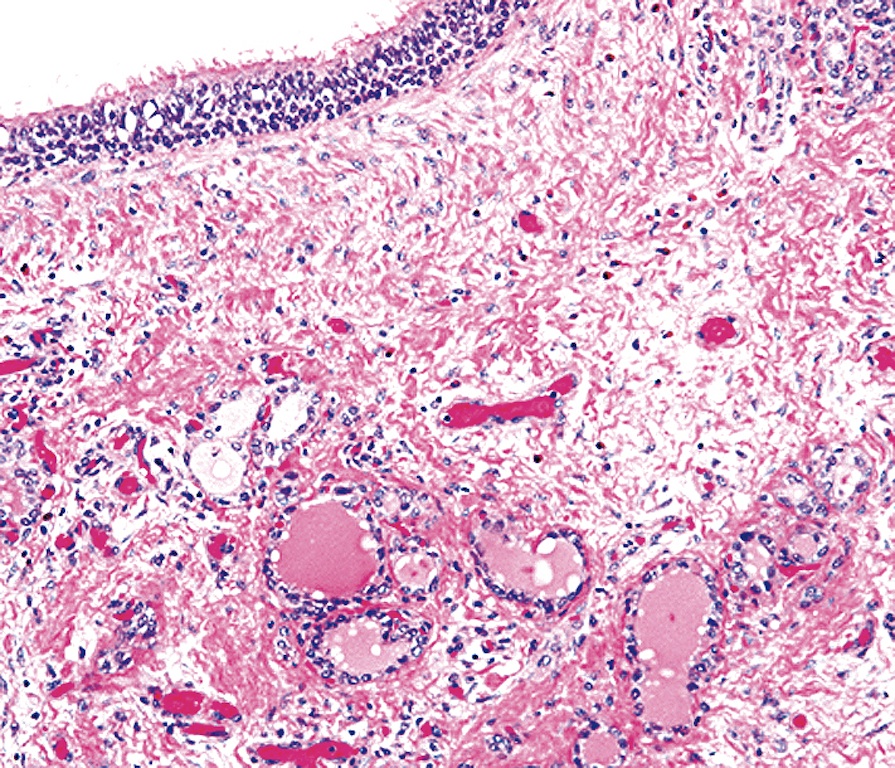
- Secondary inflammation is common, especially in sinus tract (J Pediatr Surg 1984;19:506):
- Intense lymphocytic infiltration, rarely arranged into lymphoid follicles
- Admixture of neutrophils (if the cyst is infected)
- Granulation tissue and fibrosis
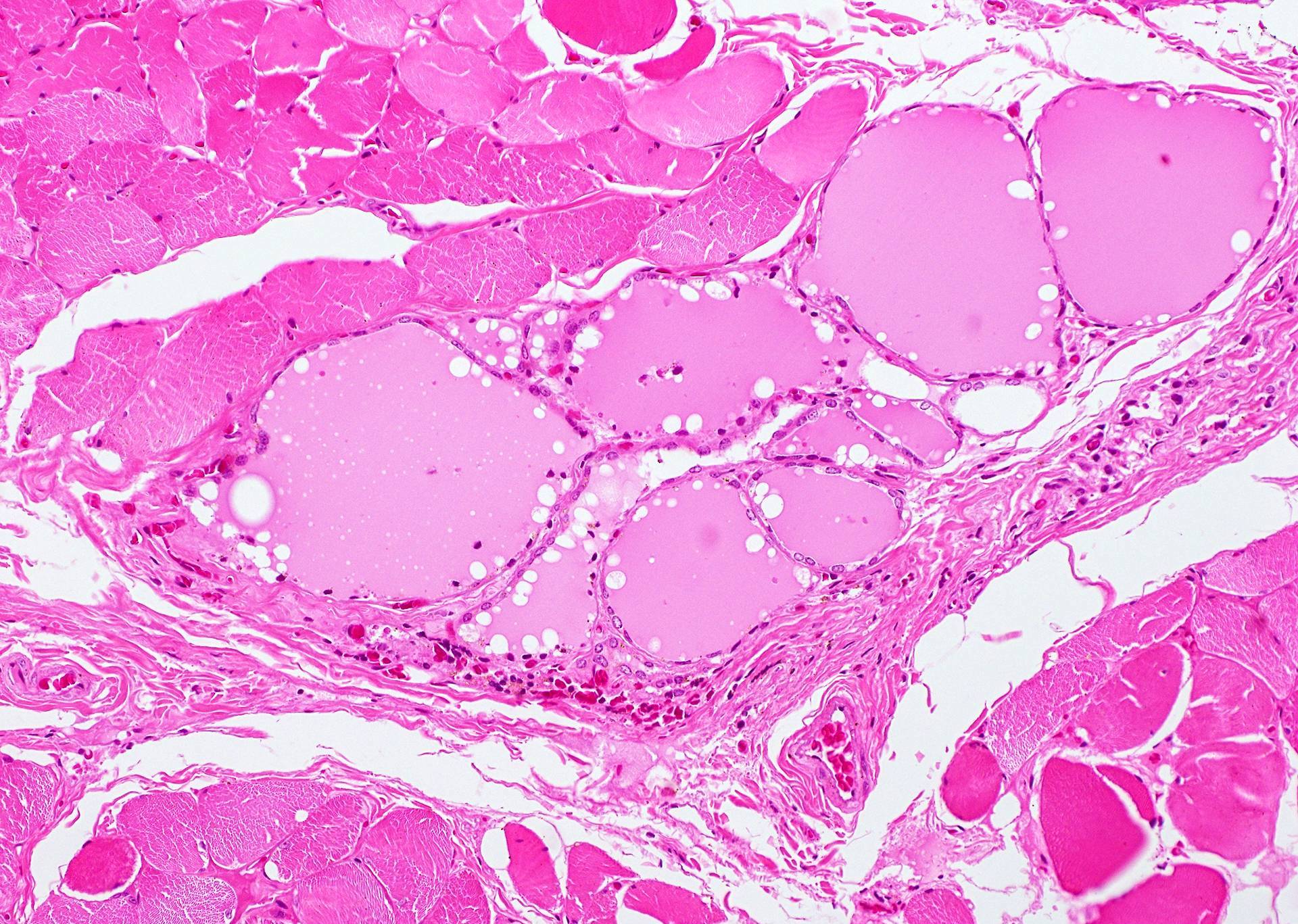
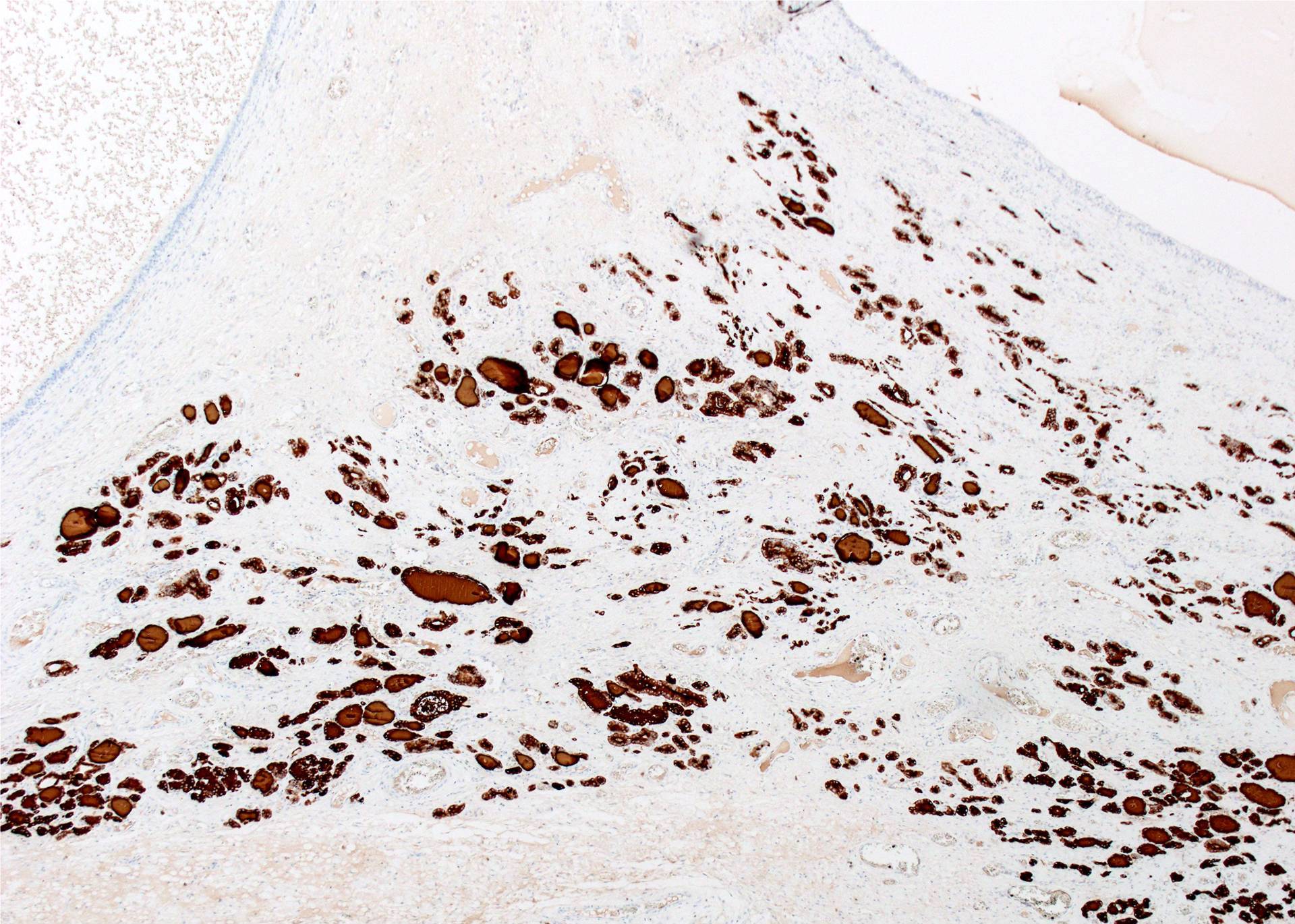
- Thyroid follicles in the cyst / duct wall:
- Found in 30% - 60%, with higher yield on serial sections
- More common in infra- versus suprahyoid remnants, on the right paramedian side (Ann Otol Rhinol Laryngol 2000;109:1135)
- Seen in small irregular groups
- Thyroid epithelium may be normal or rarely hyperplastic or neoplastic
- Thyroid tissue often hidden by inflammation (Laryngoscope 2001;111:1002)
- Absence of thyroid tissue does not exclude the diagnosis of TGD cyst
- Mucous salivary-type glands can be found in the cyst wall, frequently in lingual and suprahyoid locations (Ann Otol Rhinol Laryngol 1996;105:996)
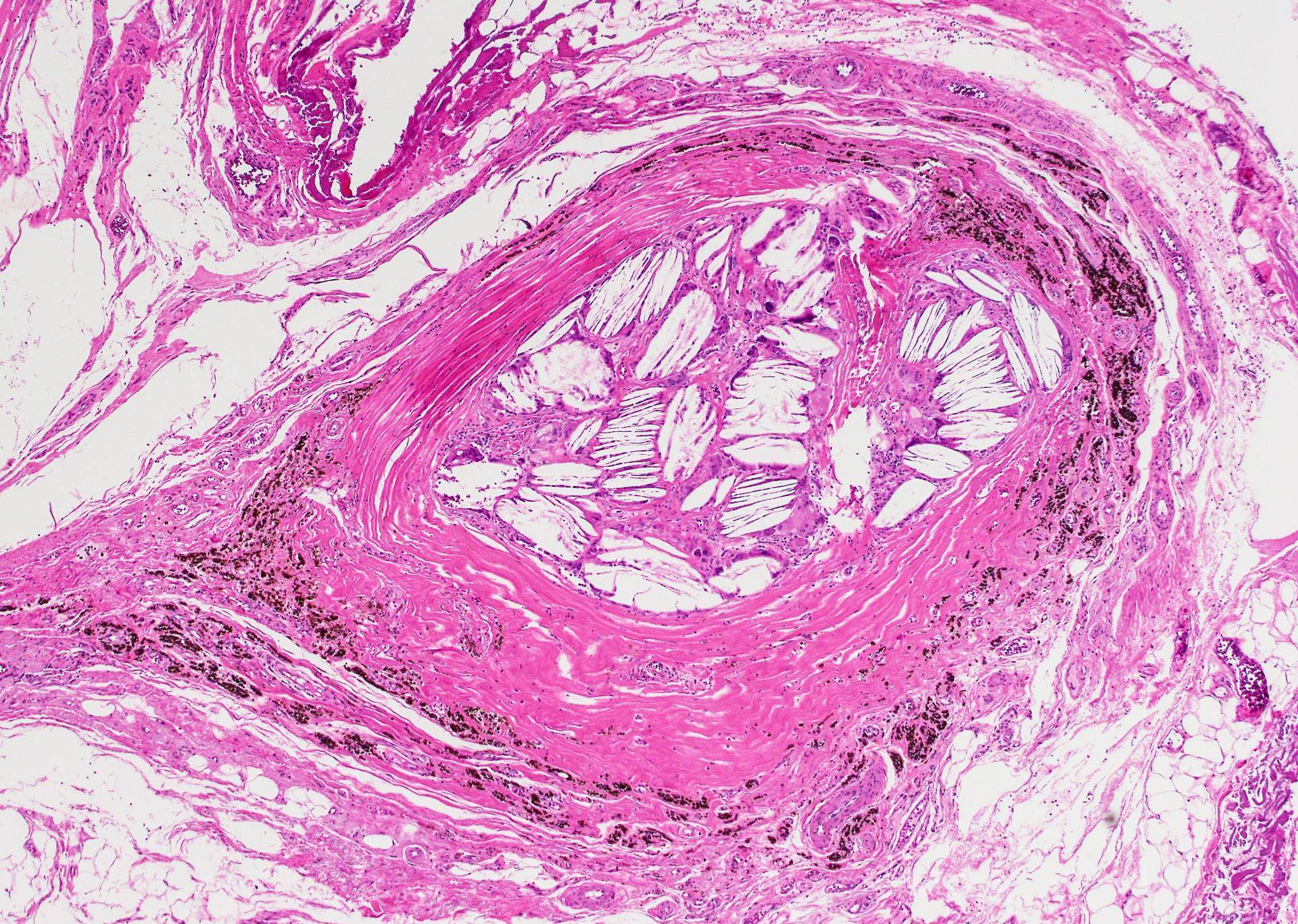
- Occasional inclusions:
- Skin adnexal structures (J Laryngol Otol 2004;118:996)
- Gastric mucosa (Gnepp: Diagnostic Surgical Pathology of the Head and Neck, 2nd Edition, 2009)
- Cartilage (Int J Pediatr Otorhinolaryngol 1988;15:205)
- Bone (J Laryngol Otol 1994;108:168)
- Cholesterol granuloma (Eur Arch Otorhinolaryngol 2009;266:1775)
- One study found that specimens clinically diagnosed as TGD cyst were classified based on histology as true cysts (50%), ducts without evidence of cysts (40%) and fibrous tracts (10%) (J Laryngol Otol 2000;114:128)
Microscopic (histologic) images
Contributed by Andrey Bychkov, M.D., Ph.D., Mark R. Wick, M.D. and AFIP
Images hosted on other servers:
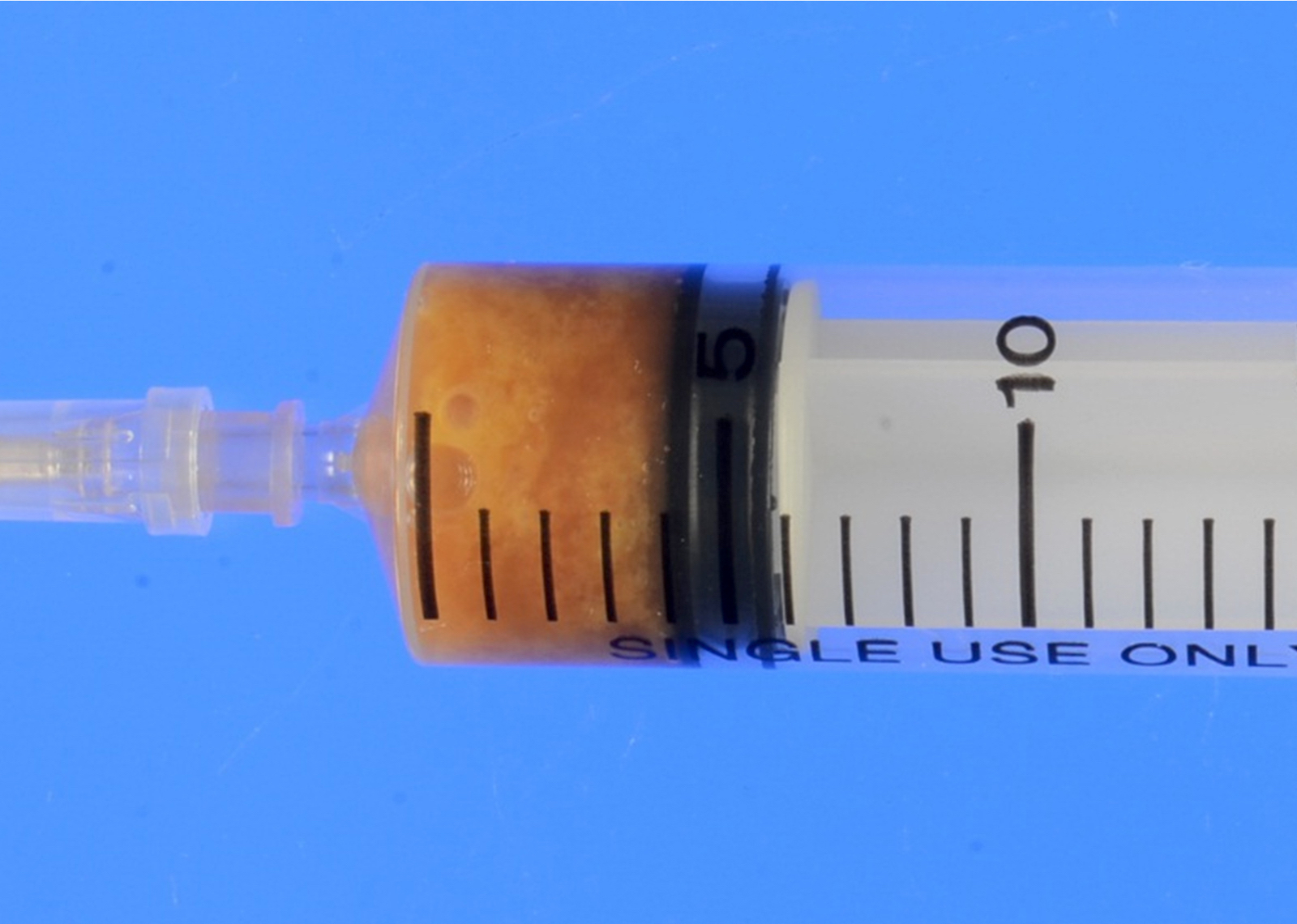
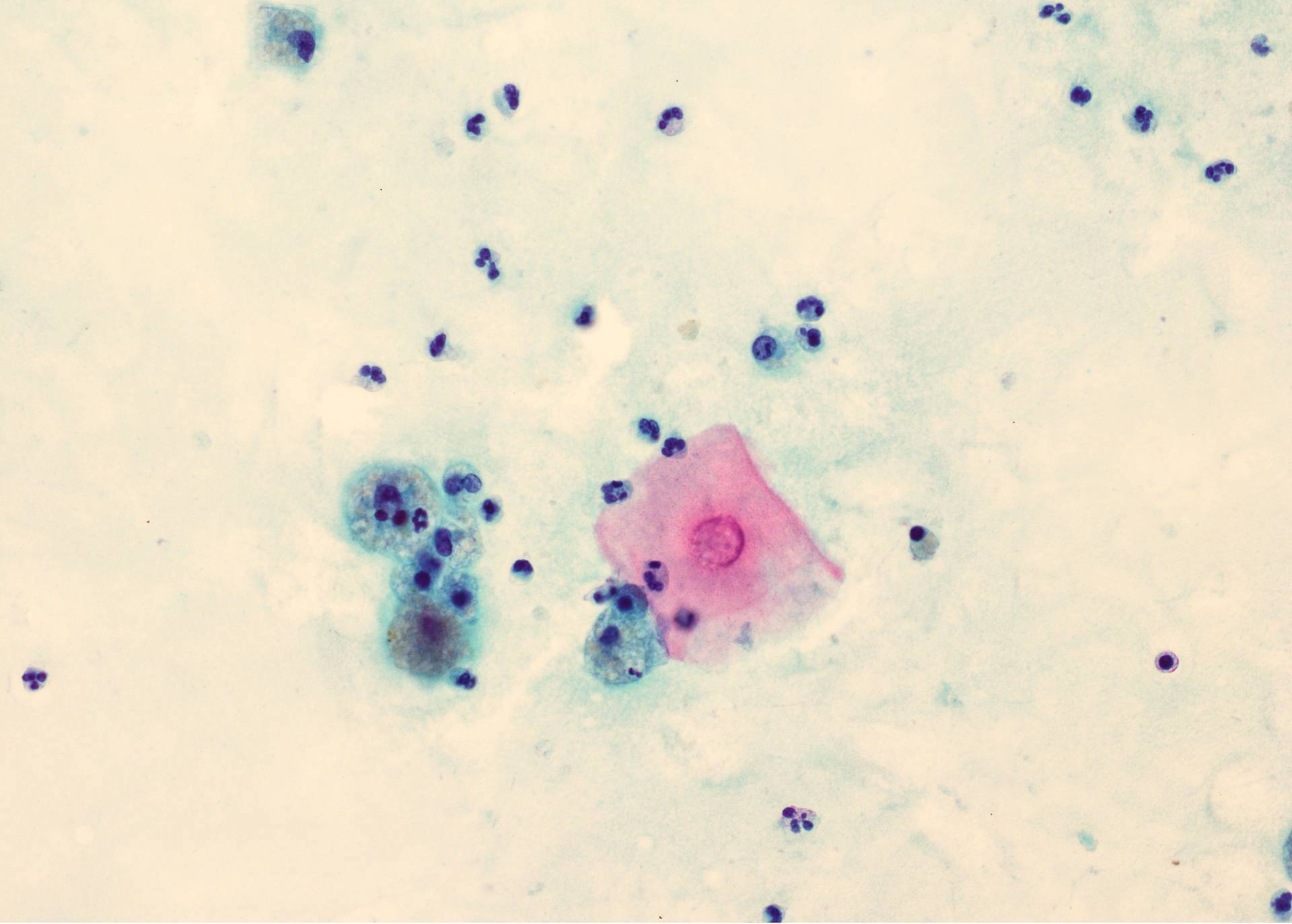
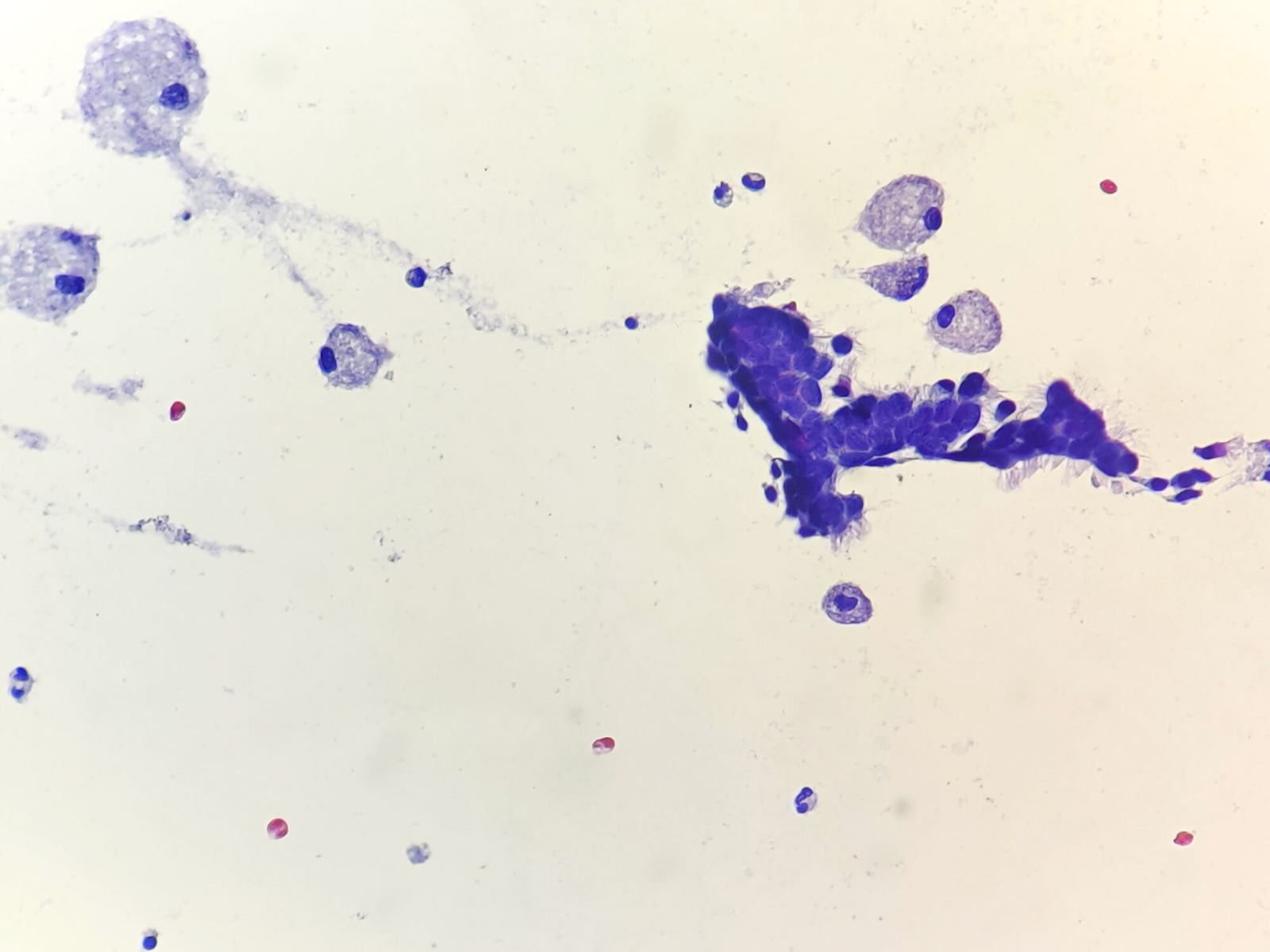
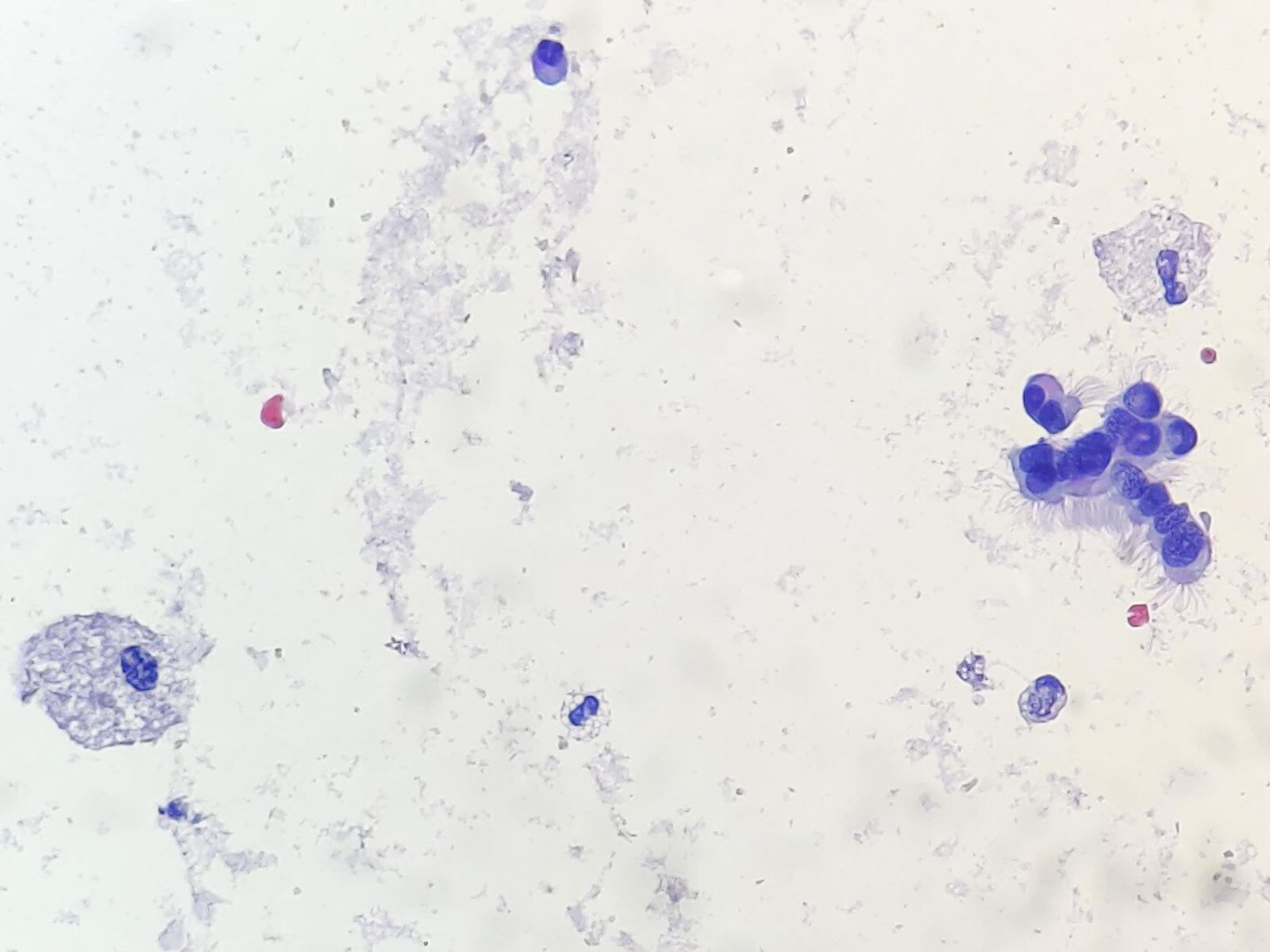
Cytology description
- Preoperative FNA is moderately sensitive but with many false negatives (Diagn Cytopathol 2005;33:365)
- FNA smears are of low cellularity, with predominant inflammatory cells outnumbering epithelial cells, similar to branchial cleft cyst:
- Macrophages, either foamy or hemosiderin laden
- Mature lymphocytes and neutrophils (predominantly if the cyst is infected)
- Squamous or ciliated columnar epithelium
- Colloid is common, ranging from thick and fragmented to thin and watery
- Admixture of cholesterol crystals
- Thyroid tissue found in < 10% of aspirates, likely due to deep embedding in the cyst wall
Cytology images
Contributed by Andrey Bychkov, M.D., Ph.D., Ayana Suzuki, C.T., Ram Kumar Kurpad R, M.B.B.S., M.D. and Y. C. Spoorthy Rekha, M.B.B.S., M.D.
Images hosted on other servers:
Negative stains
- Thyroglobulin negative epithelial lining, either respiratory or squamous (Virchows Arch 2005;447:9)
- Calcitonin, since C cells are absent in median anlage derivatives (Mills: Histology for Pathologists, 4th Edition, 2012)
Videos
Sistrunks Procedure for Thyroglossal Duct Cyst
Differential diagnosis
- Cystic lesions
- Dermoid cyst: filled with sebaceous material, lined by keratinizing epithelium, and having skin appendages in the wall, none of these is observed in TGD (J Pediatr Surg 1984;19:506), in addition, rarely inflamed; aspirate enriched with anucleated squames
- Epidermoid cyst / epidermal inclusion cyst: similar to dermoid cyst, but without skin adnexa
- Branchial cleft cyst: lateral location, lymphoid follicles in the wall; aspirate is more cellular with abundant squamous epithelium
- Lymph node metastasis of papillary thyroid carcinoma with cystic degeneration
- Rare developmental cysts: lymphangioma, lymphoepithelial cyst, thymic cyst (suprasternal), bronchogenic cyst, midline cervical cleft, teratoma
- Rare nondevelopmental cysts: ranula (upper neck), laryngocele, cystic degeneration of a colloid nodule
- Solid lesions
- Lingual thyroid: resolved by clinical and radiological modalities, orthotopic thyroid is often absent
- Pyramidal lobe of thyroid gland
- Lymph node with reactive hyperplasia
- Lipoma
- Squamous cell carcinoma: atypical cells
- Rare intrathyroidal TGD cysts can be confused with primary thyroid carcinoma
- Histopathological diagnosis of TGD requires optimally evidence of respiratory / squamous epithelial lining and thyroid follicles, which sometimes can be difficult to find due to inflammation and fibrosis; in these situations, a diagnosis of developmental cyst with comment (favor TGD cyst or branchial cleft cyst, etc.) may be an option