Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Gilks CB, Huvila J. Abnormal uterine bleeding. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusdub.html. Accessed October 6th, 2025.
Definition / general
- In women of reproductive age: bleeding or spotting between periods, bleeding after sex, abnormally heavy periods or irregularity in timing of periods
- In postmenopausal women: any bleeding is considered abnormal uterine bleeding (AUB) (ACOG: Abnormal Uterine Bleeding [Accessed 25 August 2023])
Essential features
- Abnormal uterine bleeding is a clinical, not pathological, diagnosis and leads to large numbers of endometrial biopsies, accounting for most endometrial biopsies encountered in practice
- After ruling out significant endometrial pathology that can lead to abnormal uterine bleeding (e.g., endometrial polyp, hyperplasia, atypical hyperplasia, carcinoma, leiomyoma [submucosal], endometrial stromal tumors, endometritis, exogenous hormone effects, pregnancy related bleeding), a simplified descriptive sign out of these cases is preferable to a detailed histological description (suggested diagnostic terminology provided in Table 1)
- In women of reproductive age, the diagnostic sign out reflects the dynamic nature of the endometrium with cyclical changes (unlike small biopsies from most body sites where benign or unremarkable suffice if significant pathology has been excluded)
- In postmenopausal women, the normal state of the endometrium is atrophic / inactive; anything else is a significant histopathological finding
Terminology
- Dysfunctional uterine bleeding (DUB)
- Postmenopausal bleeding (PMB)
ICD coding
Epidemiology
- Women of any age but especially at menarche, perimenopause or after menopause
Sites
- Endometrium
Pathophysiology
- Significant pathology that can lead to abnormal uterine bleeding (e.g., endometrial polyp, hyperplasia, atypical hyperplasia, carcinoma, leiomyoma [submucosal], endometritis, exogenous hormone effects) must first be excluded (Medicine (Baltimore) 2018;97:e11457, Hum Reprod Update 2023;29:457)
- In the absence of a specific pathological diagnosis, as noted above, the pathophysiology of abnormal uterine bleeding is variable depending on age
- In premenopausal or perimenopausal women, it is often related to irregularity in the pituitary - gonadal axis, such that the endometrium fails to undergo uniform cycles of growth / secretory change / apoptosis
- In postmenopausal women, the most common cause is atrophy with bleeding from fragile vessels in the thinned endometrium
- Other causes of abnormal uterine bleeding that will not appear in an endometrial biopsy include adenomyosis or endometriosis
Etiology
- If significant underlying pathology has been excluded, the etiology of abnormal uterine bleeding can be related to anovulatory cycles (e.g., perimenopausal or polycystic ovarian syndrome) with prolonged growth of the endometrium, which then sheds irregularly rather than in the coordinated manner of a normal menstrual cycle (Curr Probl Pediatr Adolesc Health Care 2022;52:101185, Medicine (Baltimore) 2018;97:e11457, Int J Gynaecol Obstet 2011;113:3)
- Bleeding disorders or anticoagulant use can lead to abnormal uterine bleeding
- Exogenous hormone therapy can lead to abnormal uterine bleeding
Clinical features
- Biopsy is taken to exclude significant pathology (e.g., endometrial polyp, hyperplasia, atypical hyperplasia, carcinoma, leiomyoma [submucosal], stromal tumors, endometritis, exogenous hormone effects, pregnancy related bleeding)
Diagnosis
- Low power examination of the biopsy will establish adequacy of the specimen and rule out most of the important diagnoses that must be excluded
- Having excluded endometrial polyp, hyperplasia, atypical hyperplasia, carcinoma, leiomyoma, endometritis and exogenous hormone effects, a final diagnosis can be concisely reported from a limited number of descriptive possibilities (see Table 1) (Int J Gynecol Pathol 2019;38:119)
Table 1
Diagnosis Nondiagnostic sample (no endometrial tissue present) Proliferative endometrium Secretory endometrium Menstrual type breakdown Inactive endometrium Atrophic endometrium
Treatment
- Treatment of significant underlying pathology and if there is none, then observation or (hormonal) therapy to control bleeding, based on severity of symptoms
- If hormonal therapy is unsuccessful, surgical management (endometrial ablation, hysteroscopic endometrial resection or hysterectomy) is required (PLoS One 2019;14:e0219294)
Microscopic (histologic) description
- Nondiagnostic sample (no endometrial tissue present)
- Only use if there is no endometrial tissue present in the specimen (J Clin Pathol 2006;59:801)
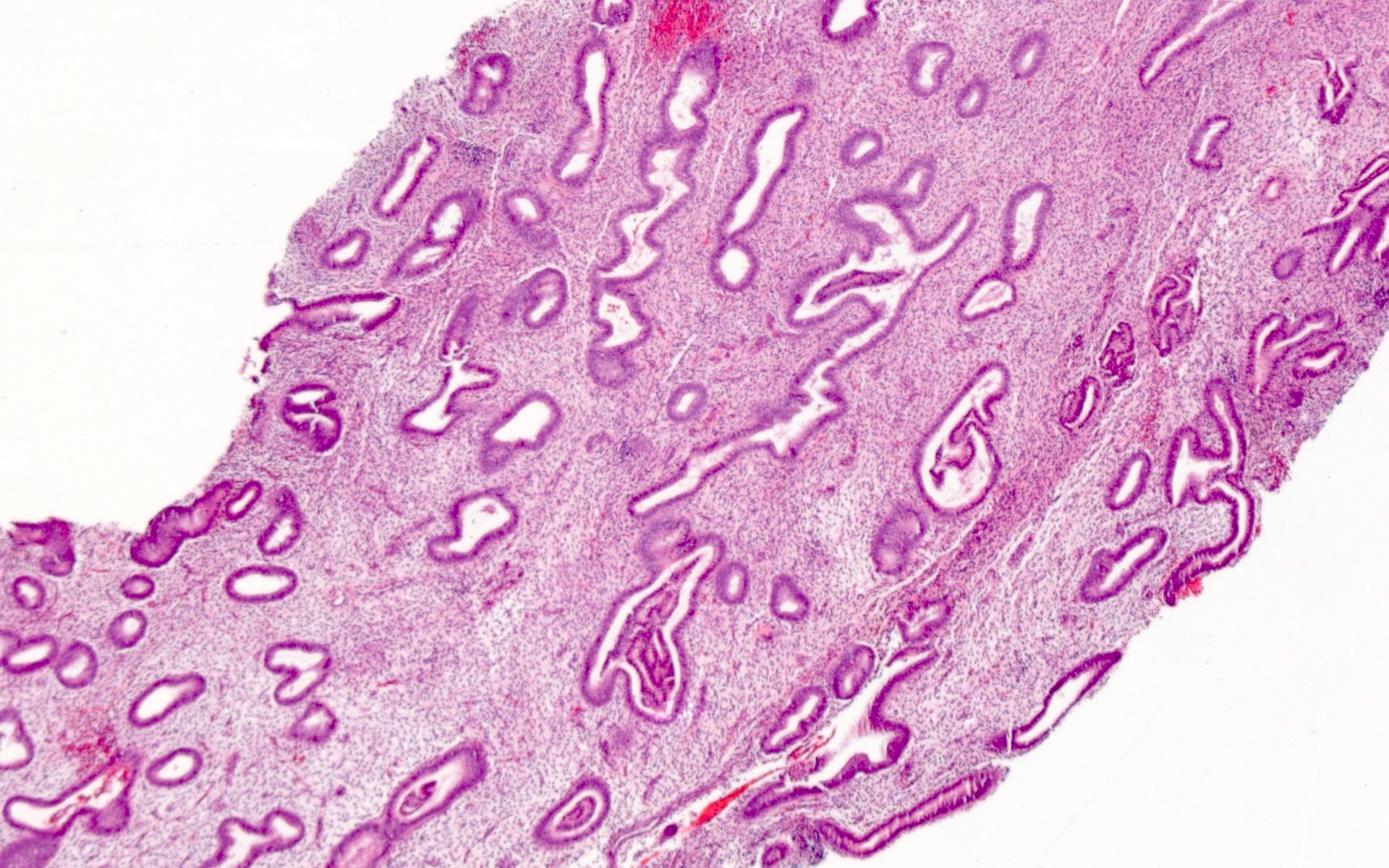
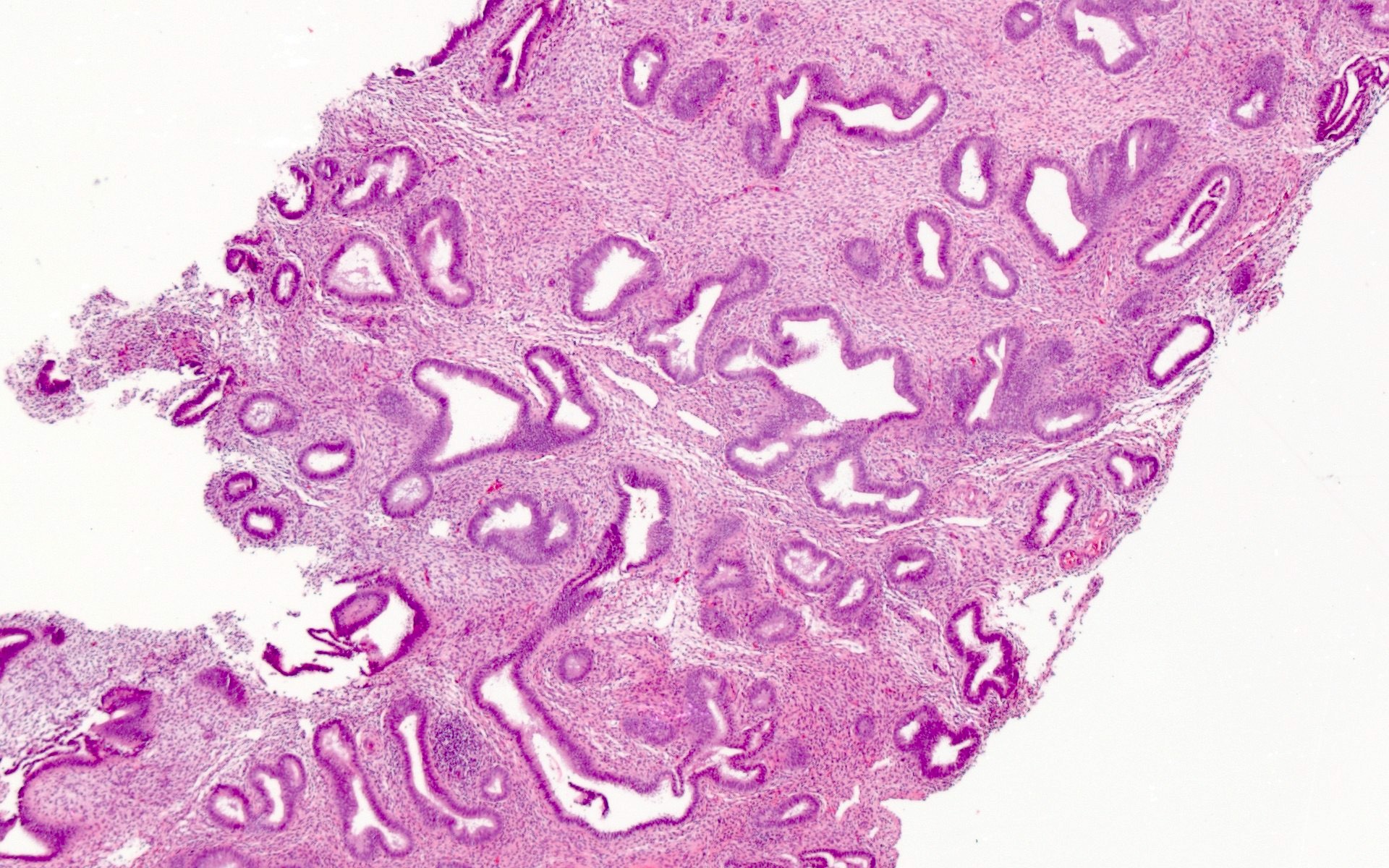
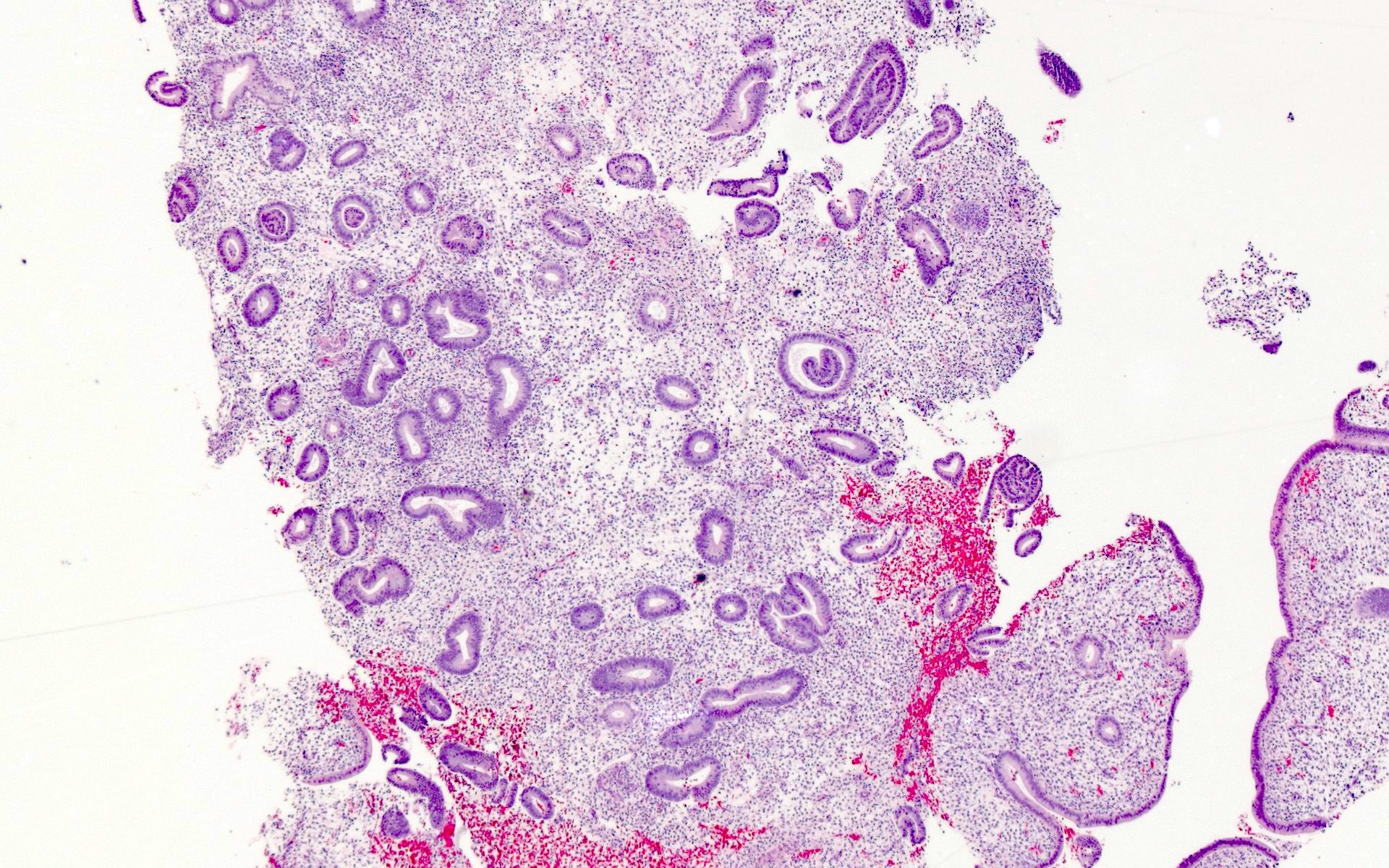
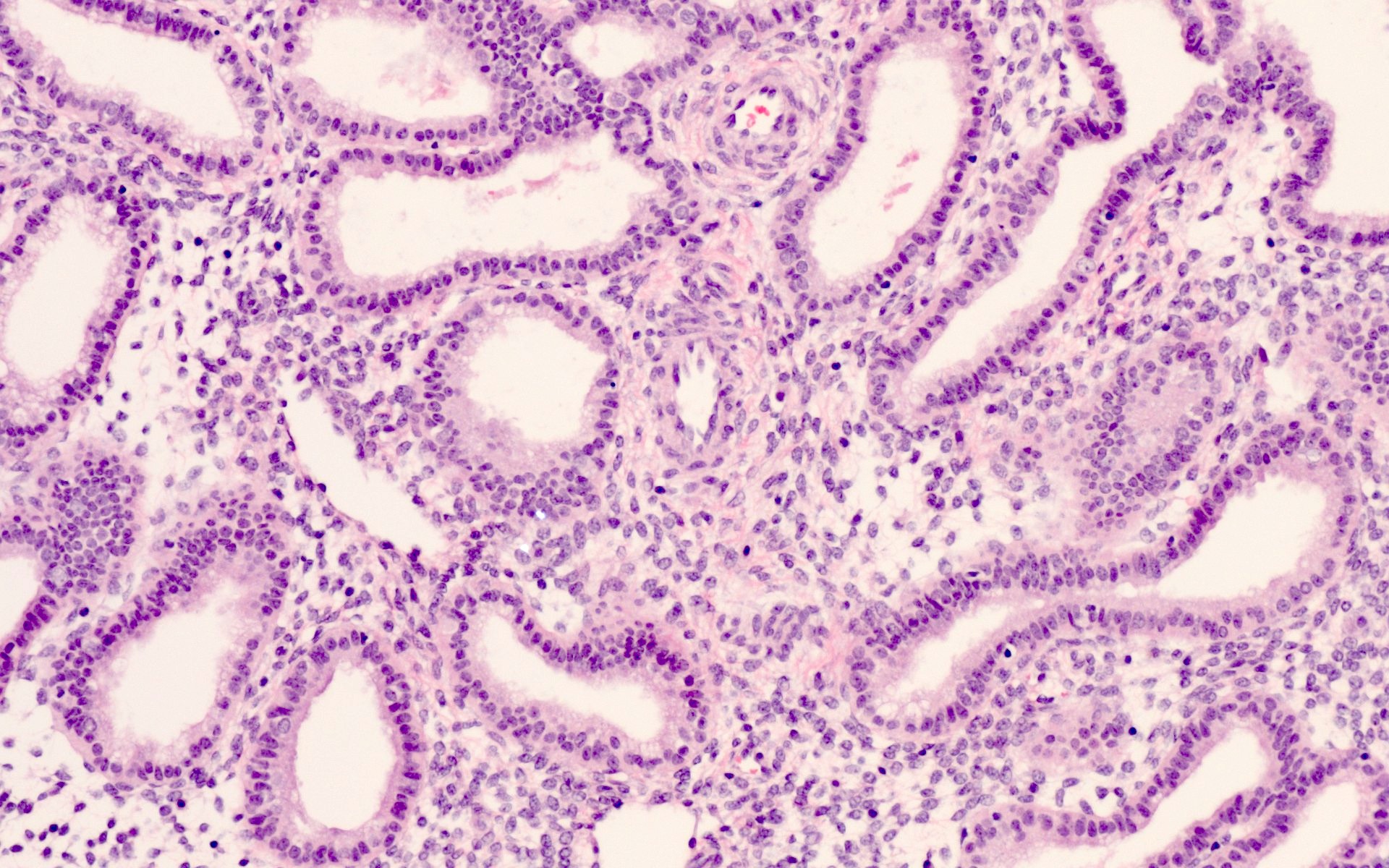
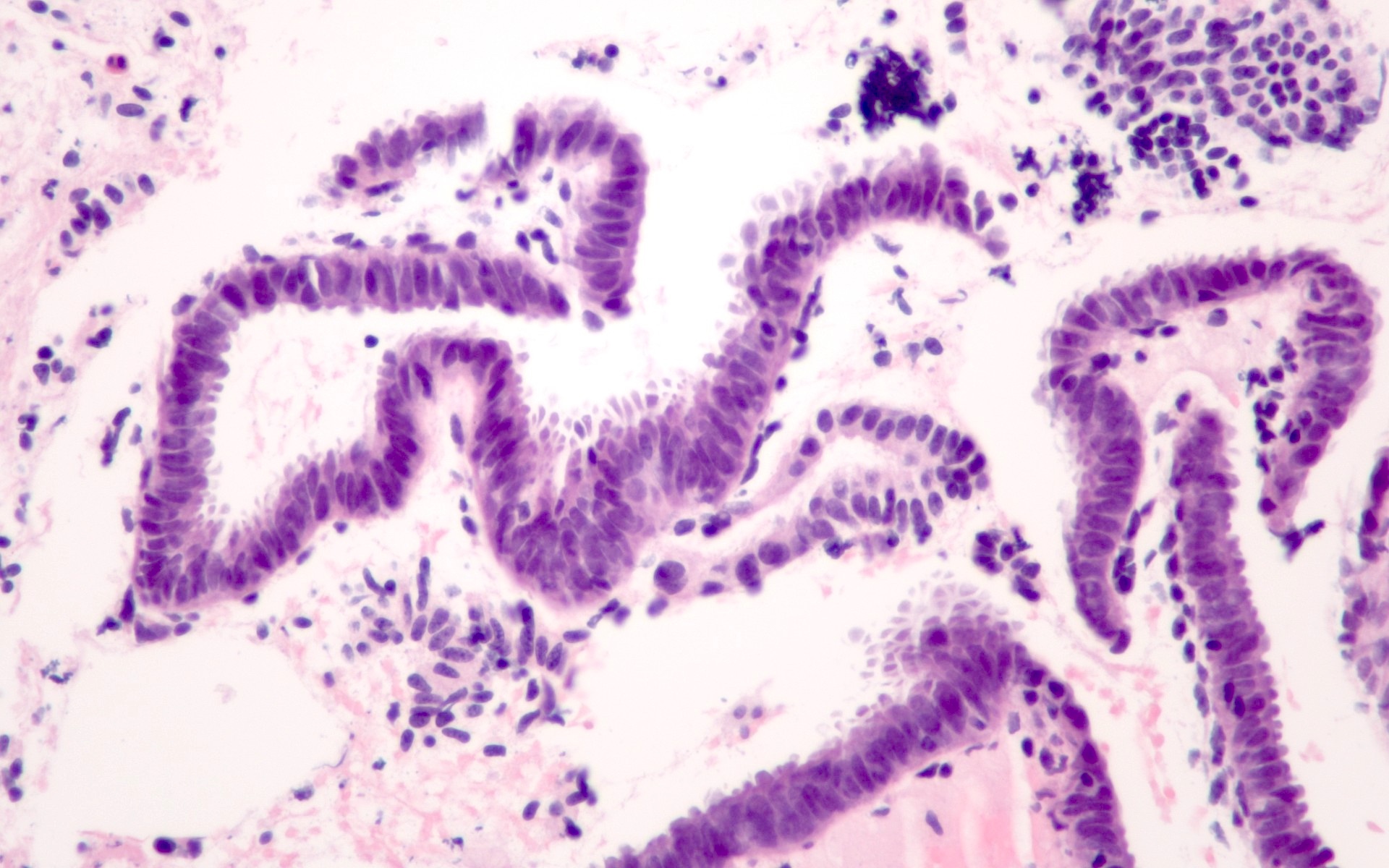
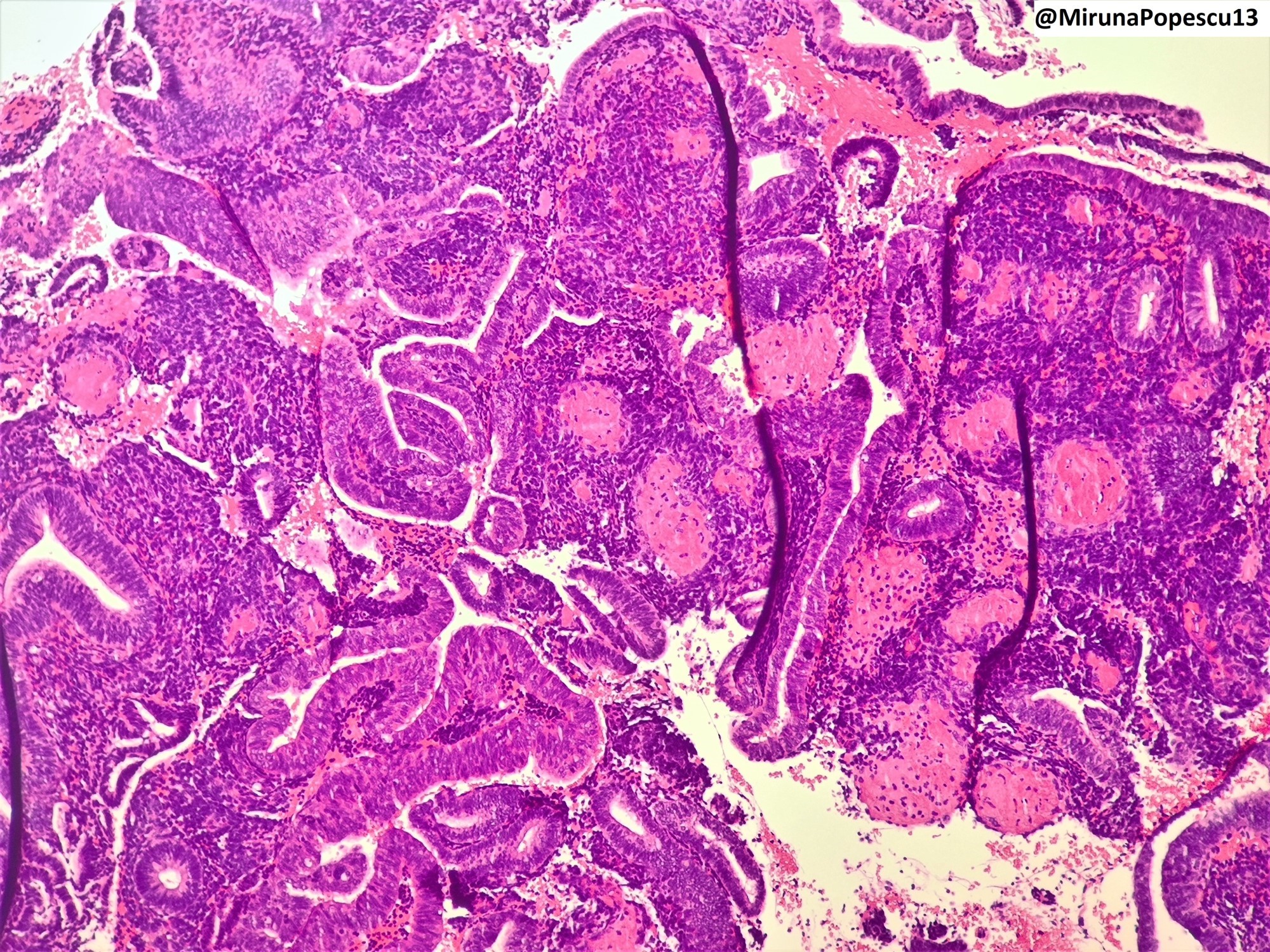
- Proliferative endometrium (see Microscopic images at Uterus - Anatomy & histology)
- Orderly and evenly spaced simple tubular glands, with mitotic activity readily identified in both glands and stroma
- If few mitotic figures, the prefix weakly can be used
- Diagnosis of disordered proliferative is made if there is some architectural irregularity but not glandular predominance, i.e., it is not hyperplastic; the distinction between disordered proliferative and proliferative is subject to interobserver variability and does not change management
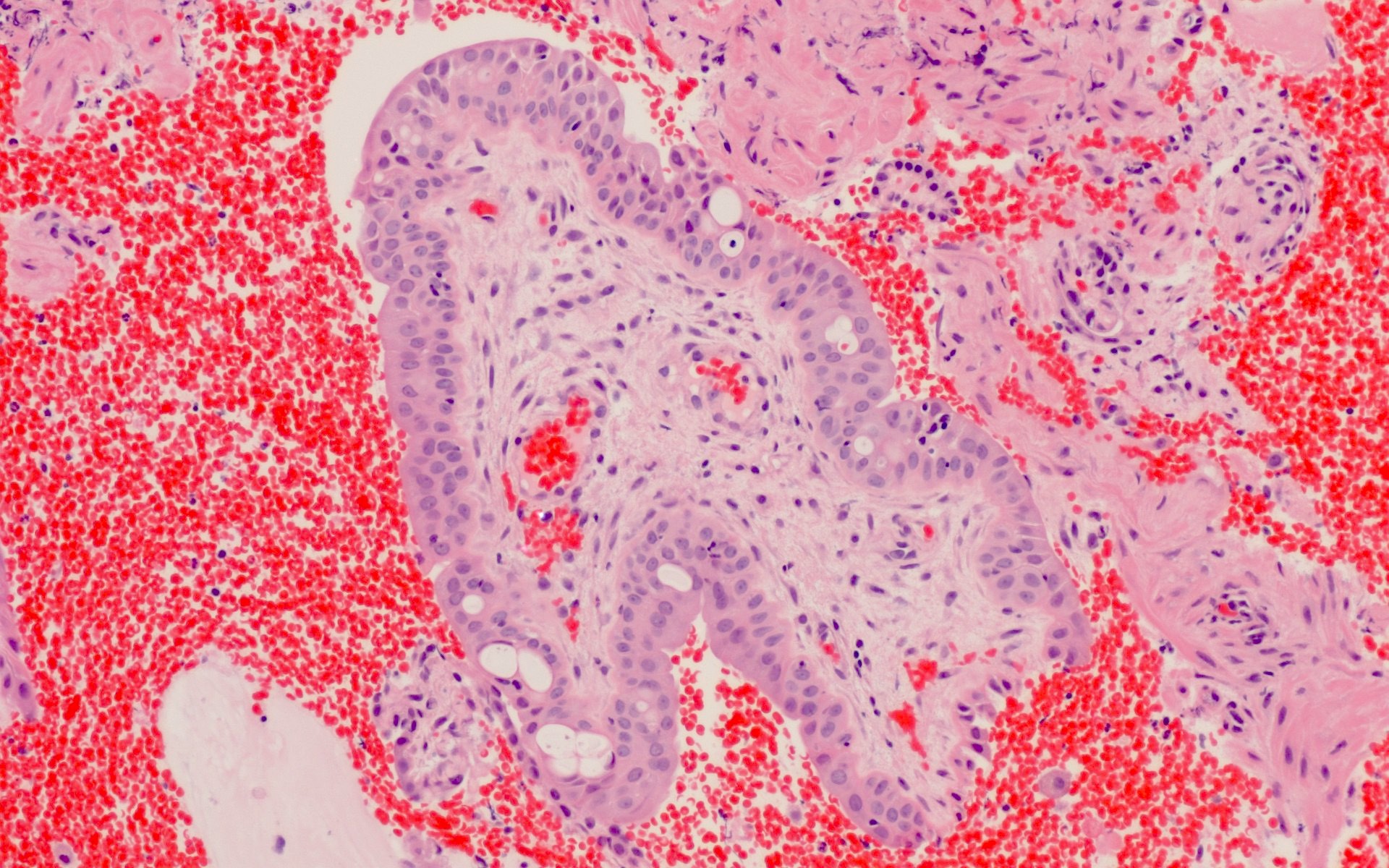
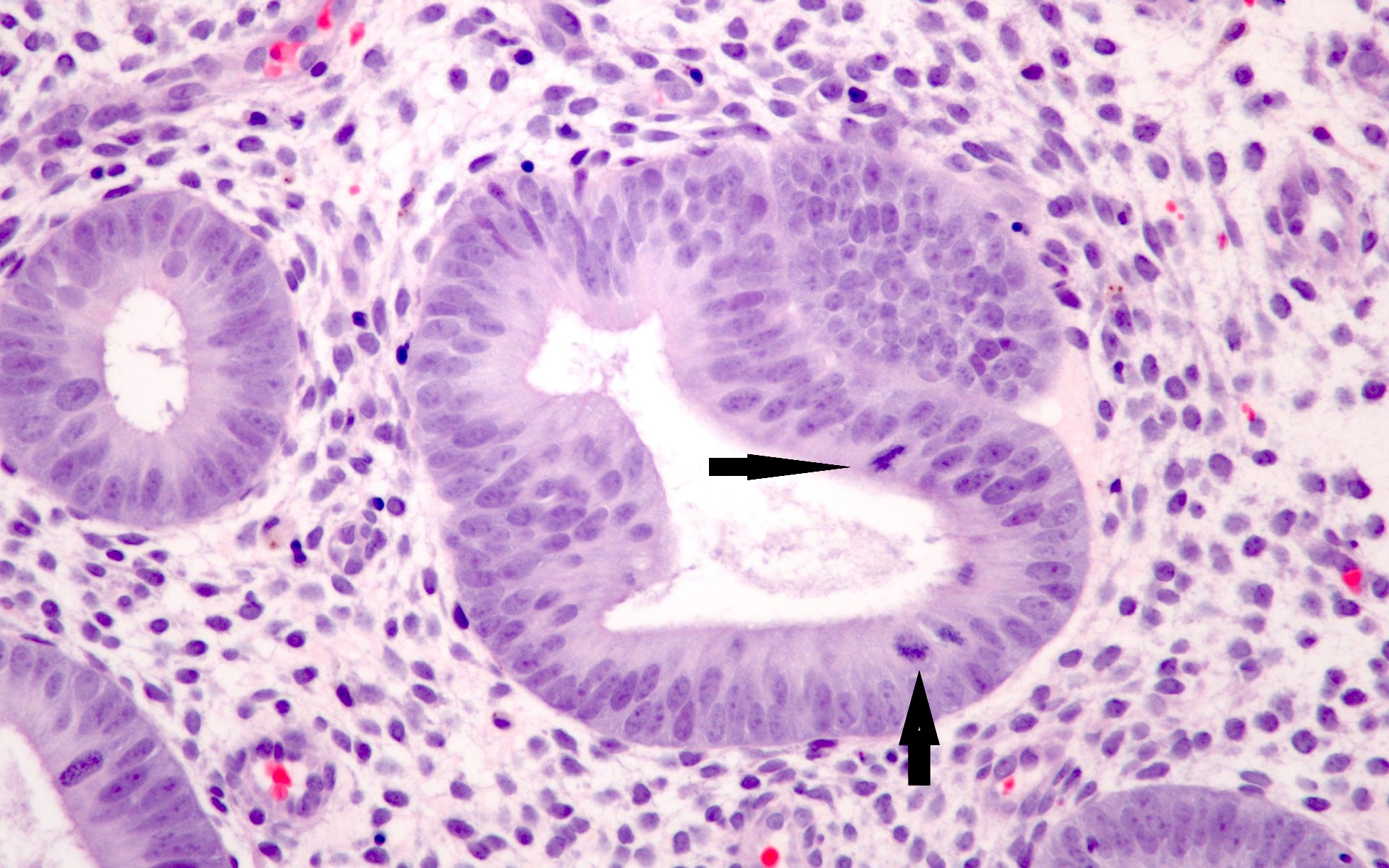
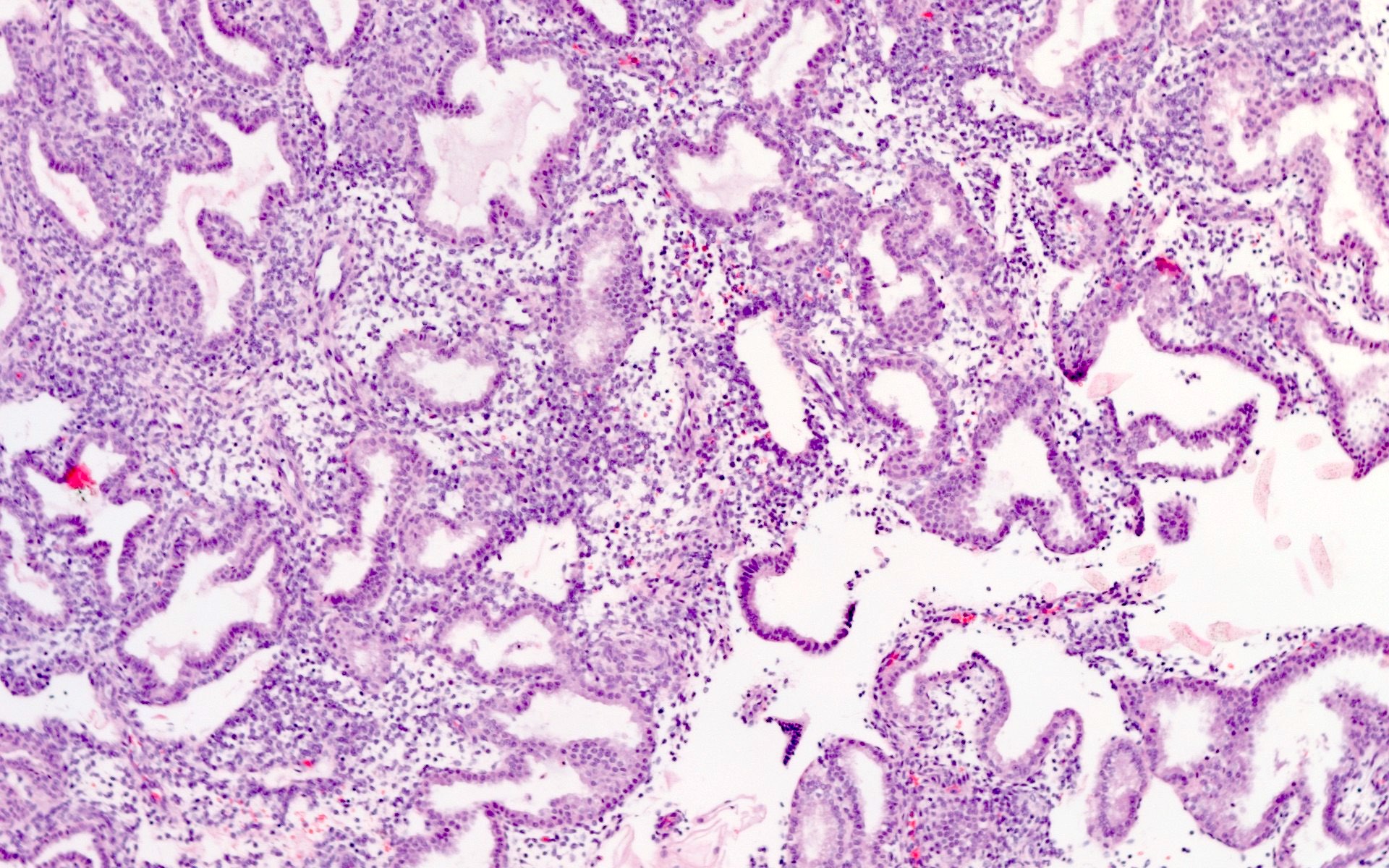
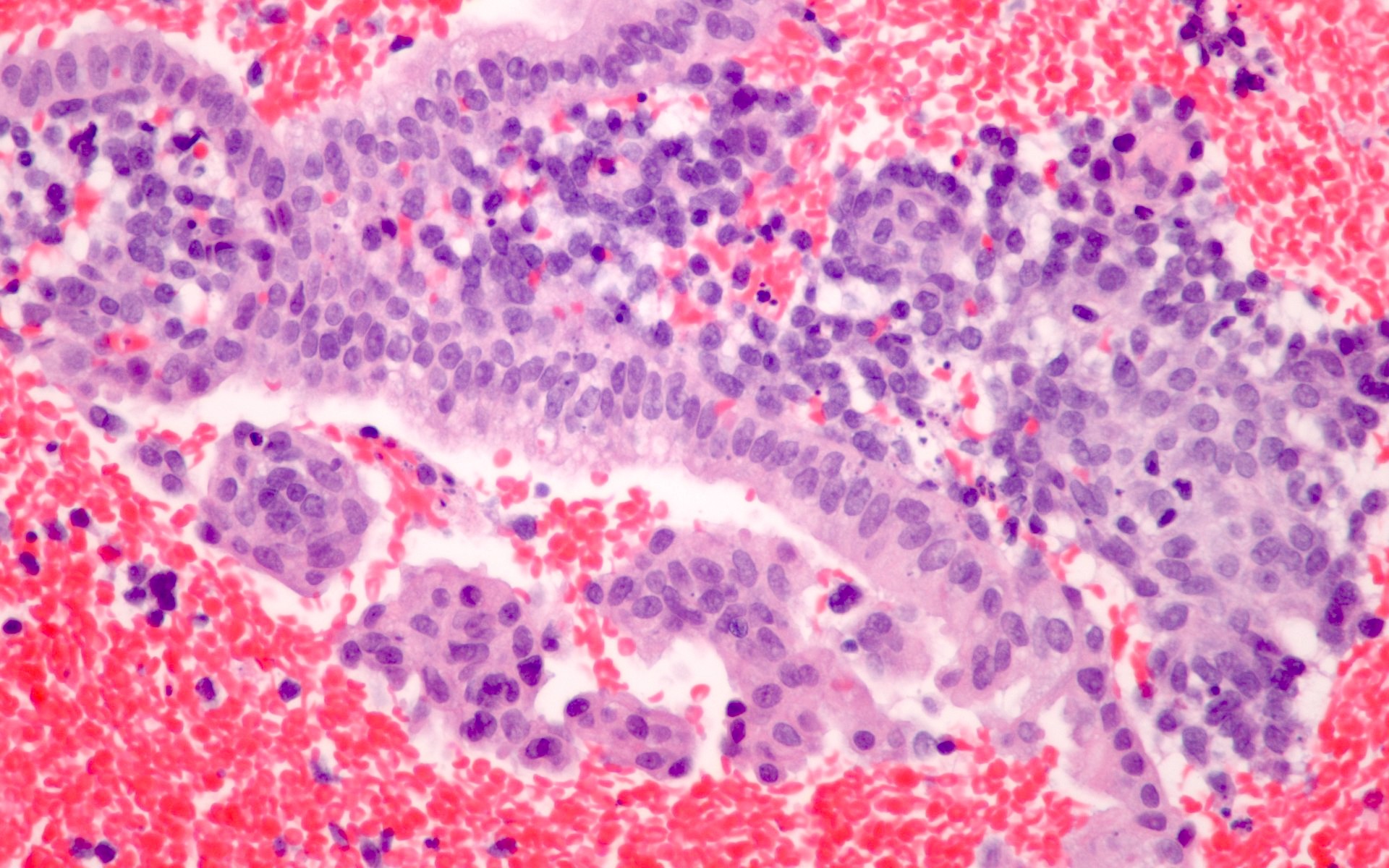
- Secretory endometrium (see Microscopic images at Uterus - Anatomy & histology)
- Variation through luteal phase but absence of mitotic activity in glands and evidence of secretory activity (cytoplasmic vacuoles that are subnuclear or supranuclear or intraluminal glandular secretions)
- Note that some vacuolization can be seen in proliferative endometrium
- If there is irregularity in the development of secretory changes or glandular architecture, a designation of irregular secretory endometrium can be used
- Hysteroscopy can show a polypoid appearance of the endometrium (so called secretory pseudopolyp); this is a normal finding of no clinical consequence
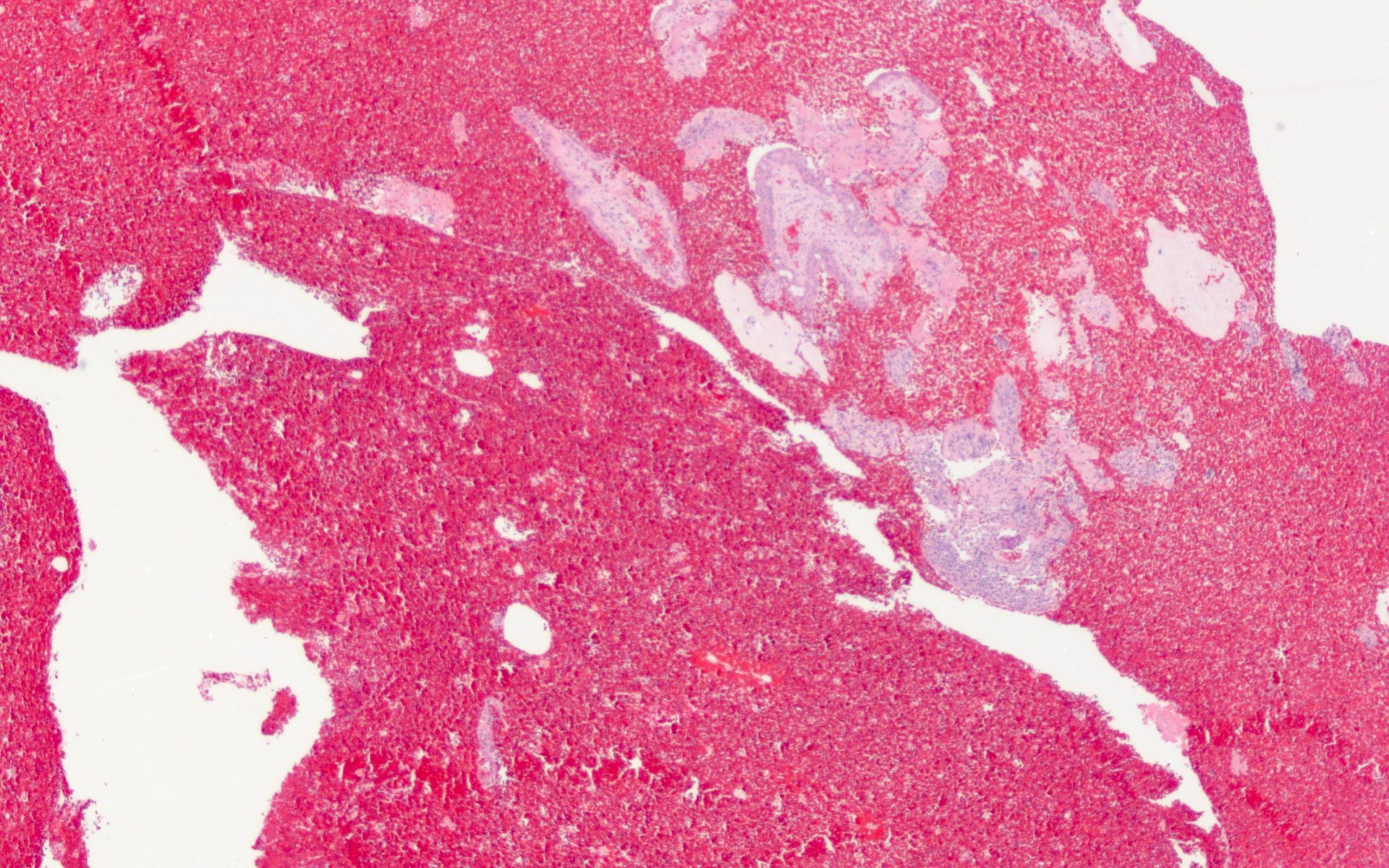
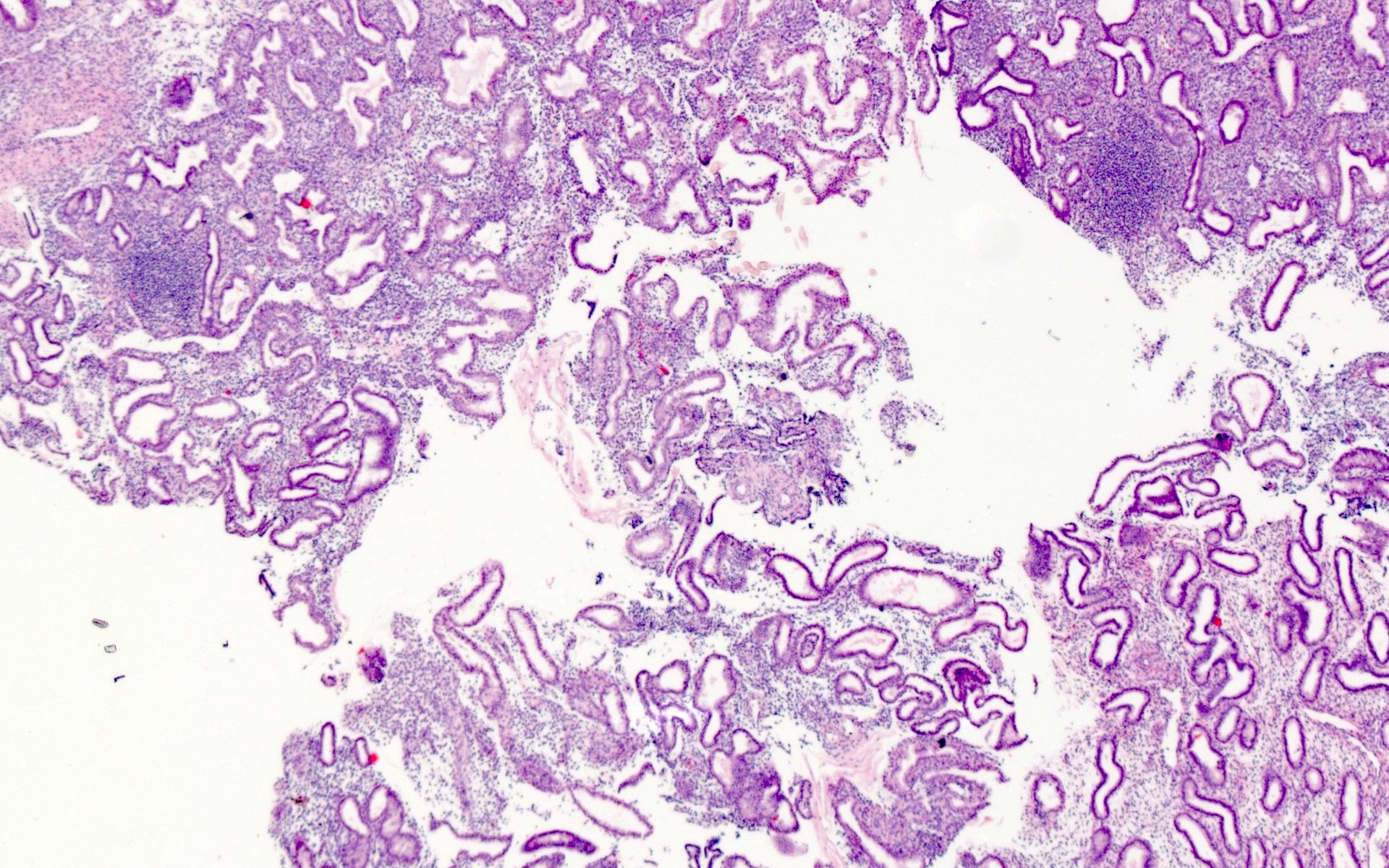
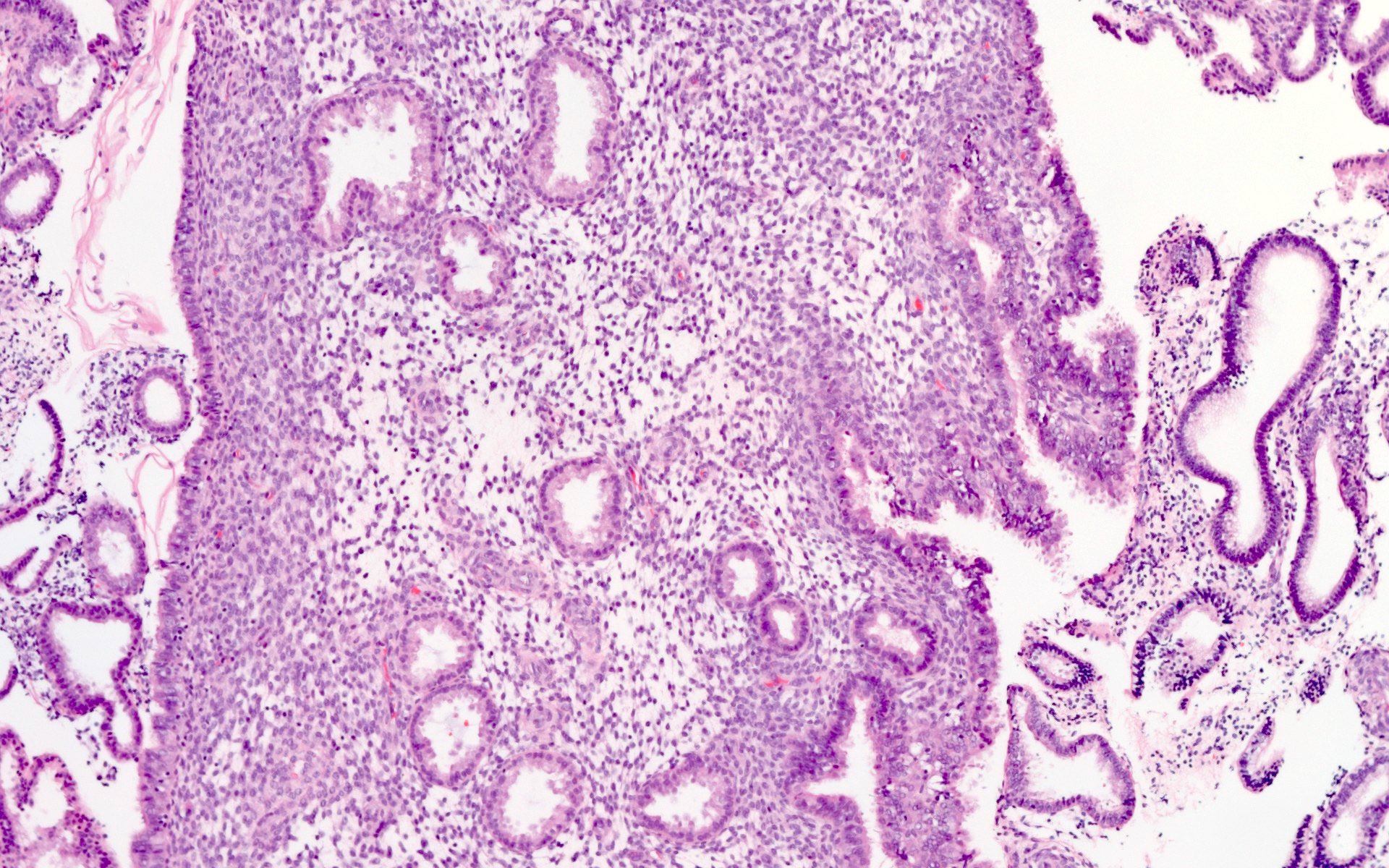
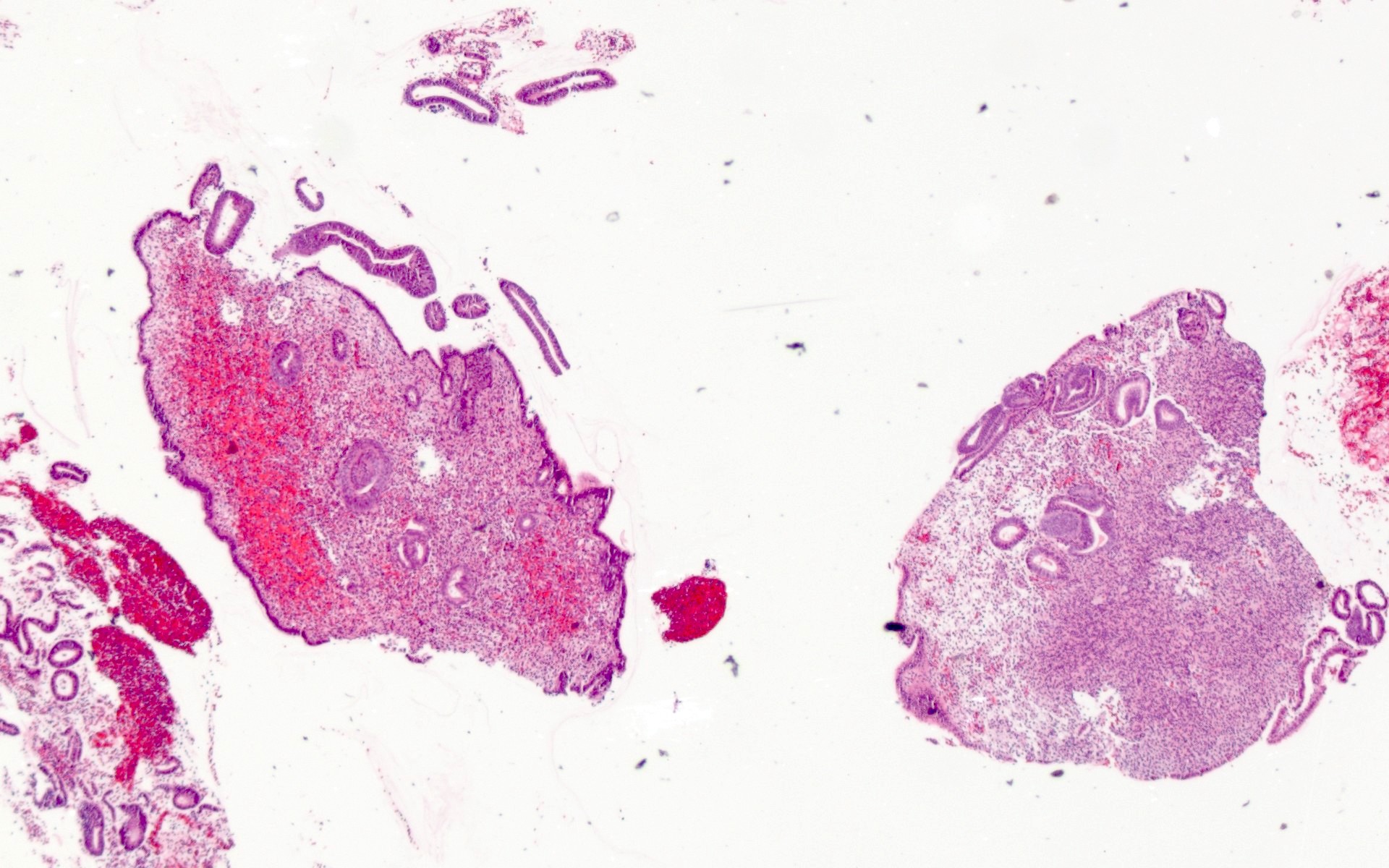
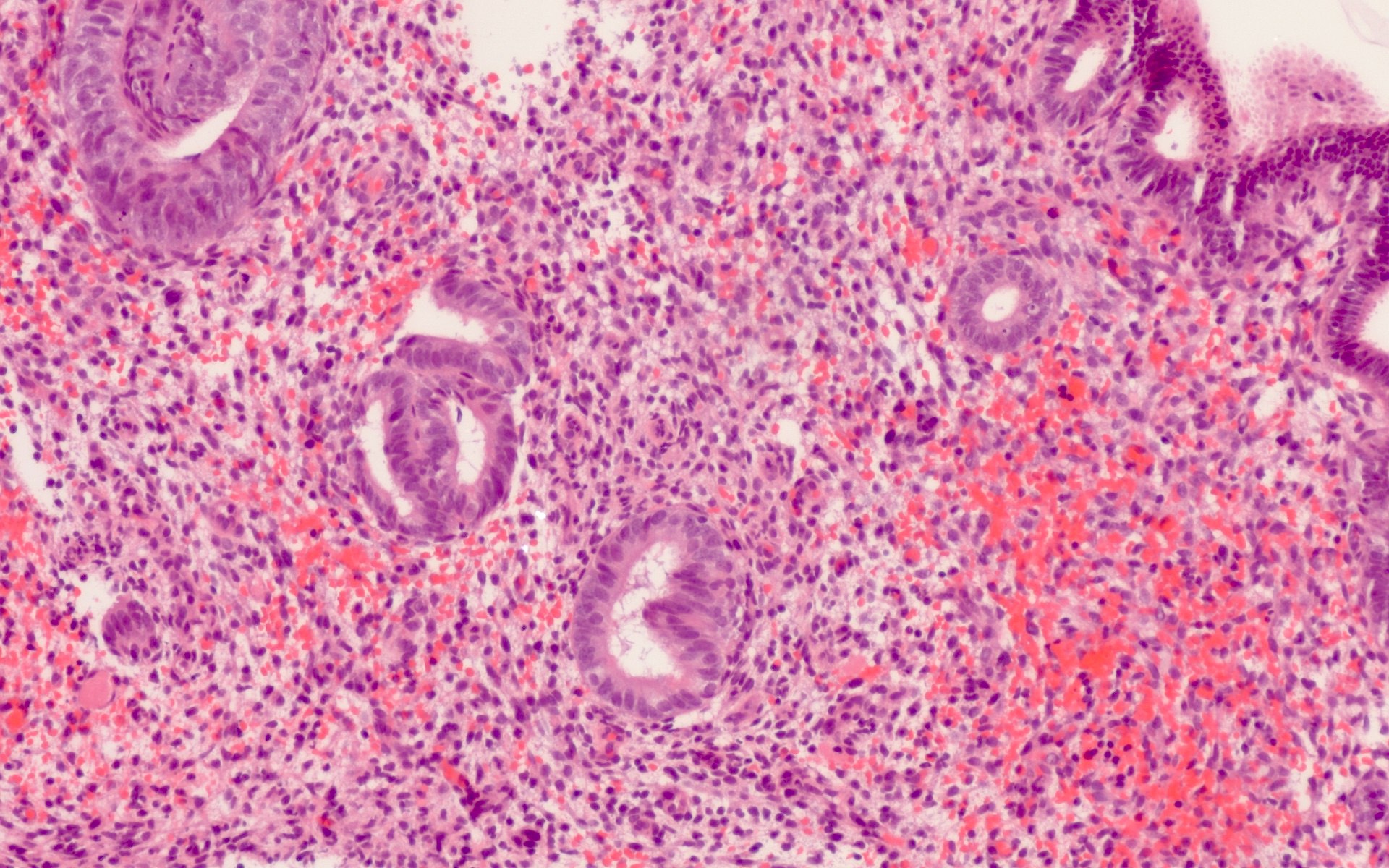
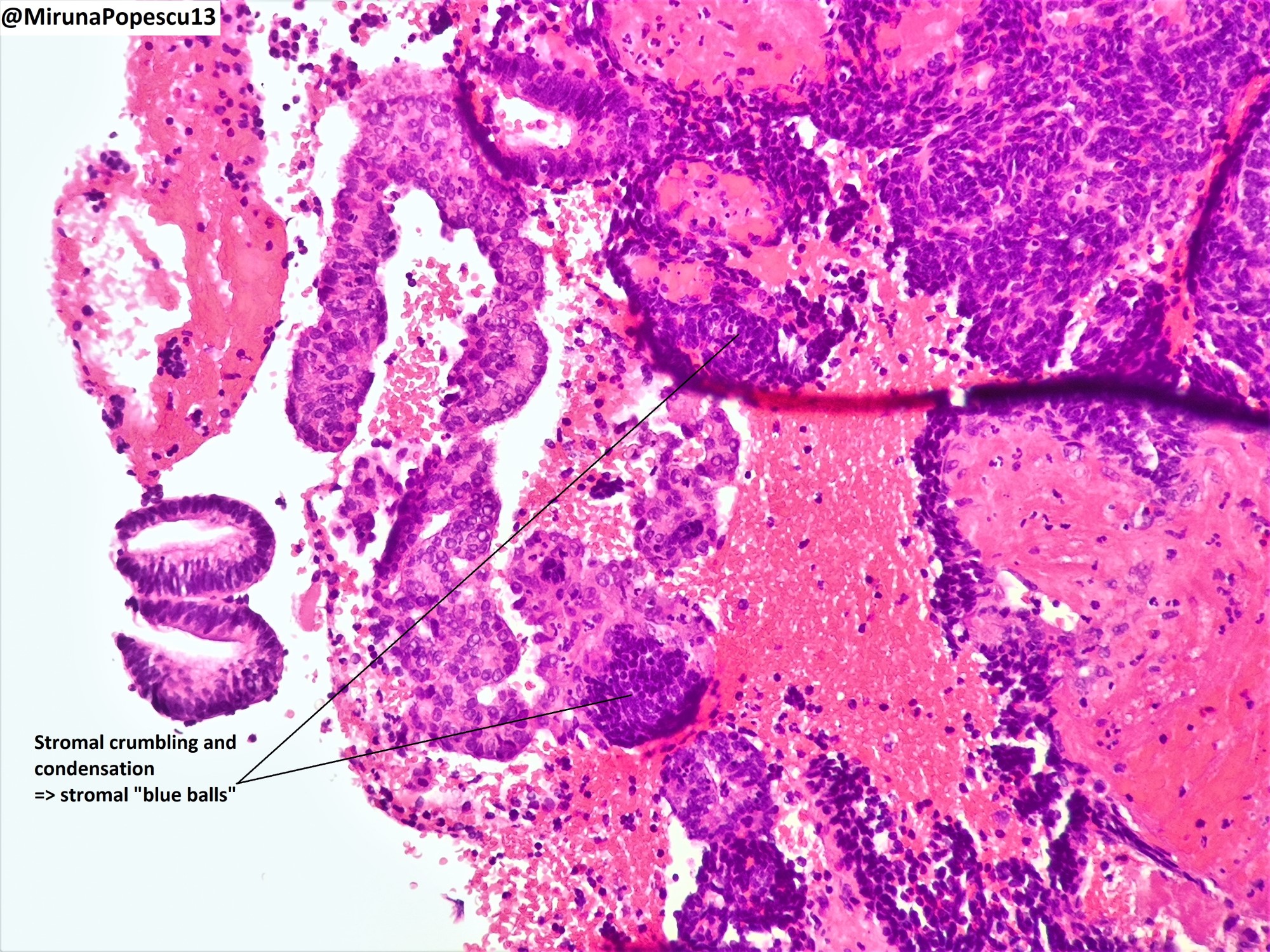
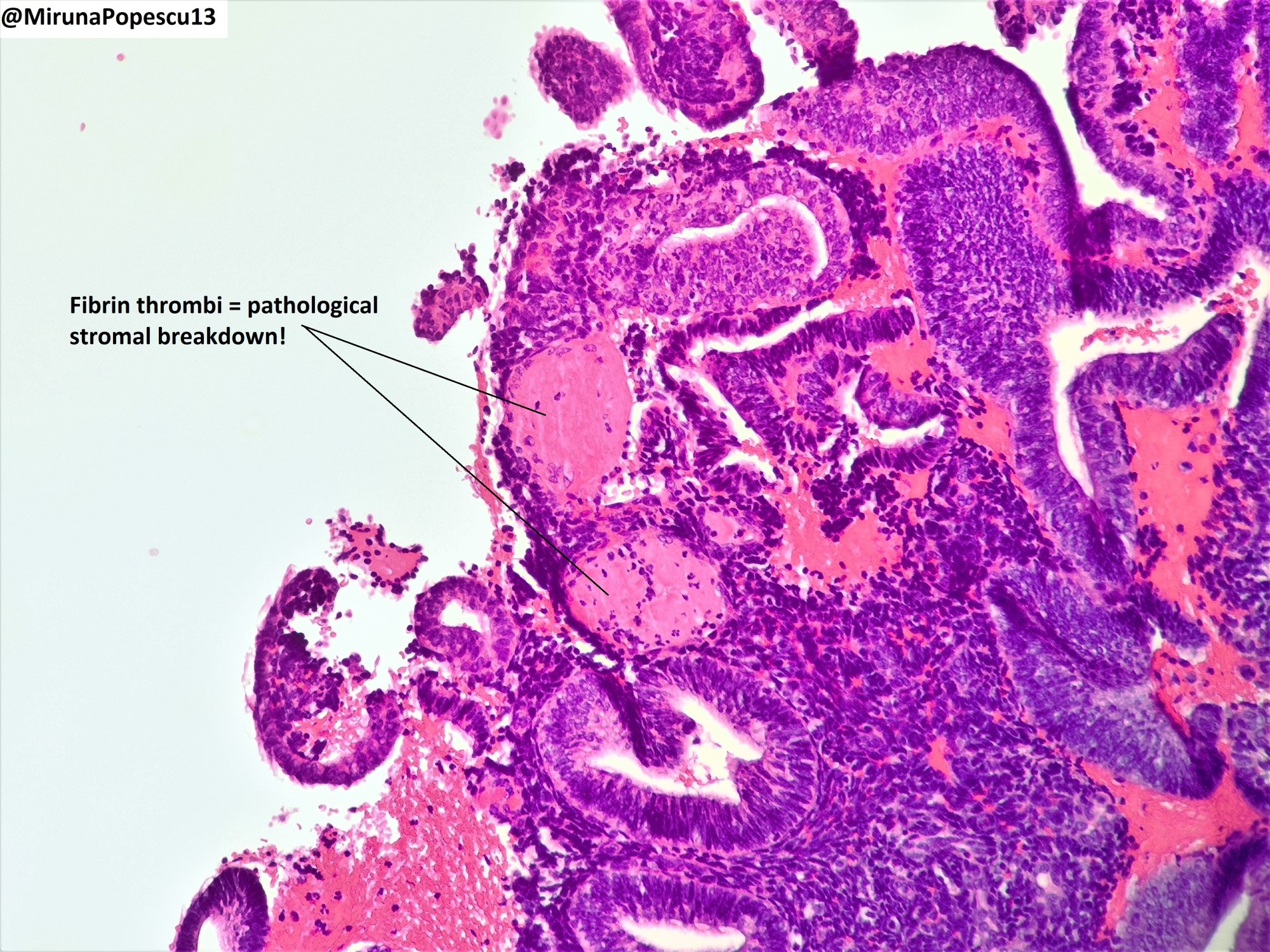
- Menstrual type breakdown (see Microscopic images at Uterus - Anatomy & histology)
- Apoptosis of glands and stroma
- Stromal cells may aggregate into tightly packed balls with condensed chromatin (i.e., blue balls)
- There have been recommendations to separate endometrial breakdown into that which occurs after ovulation and that which is not postovulatory but this is not of clinical relevance and is often impossible
- Inactive endometrium
- Endometrial glands lined by cuboidal or columnar epithelium without evidence of mitotic figures or hormonal effects
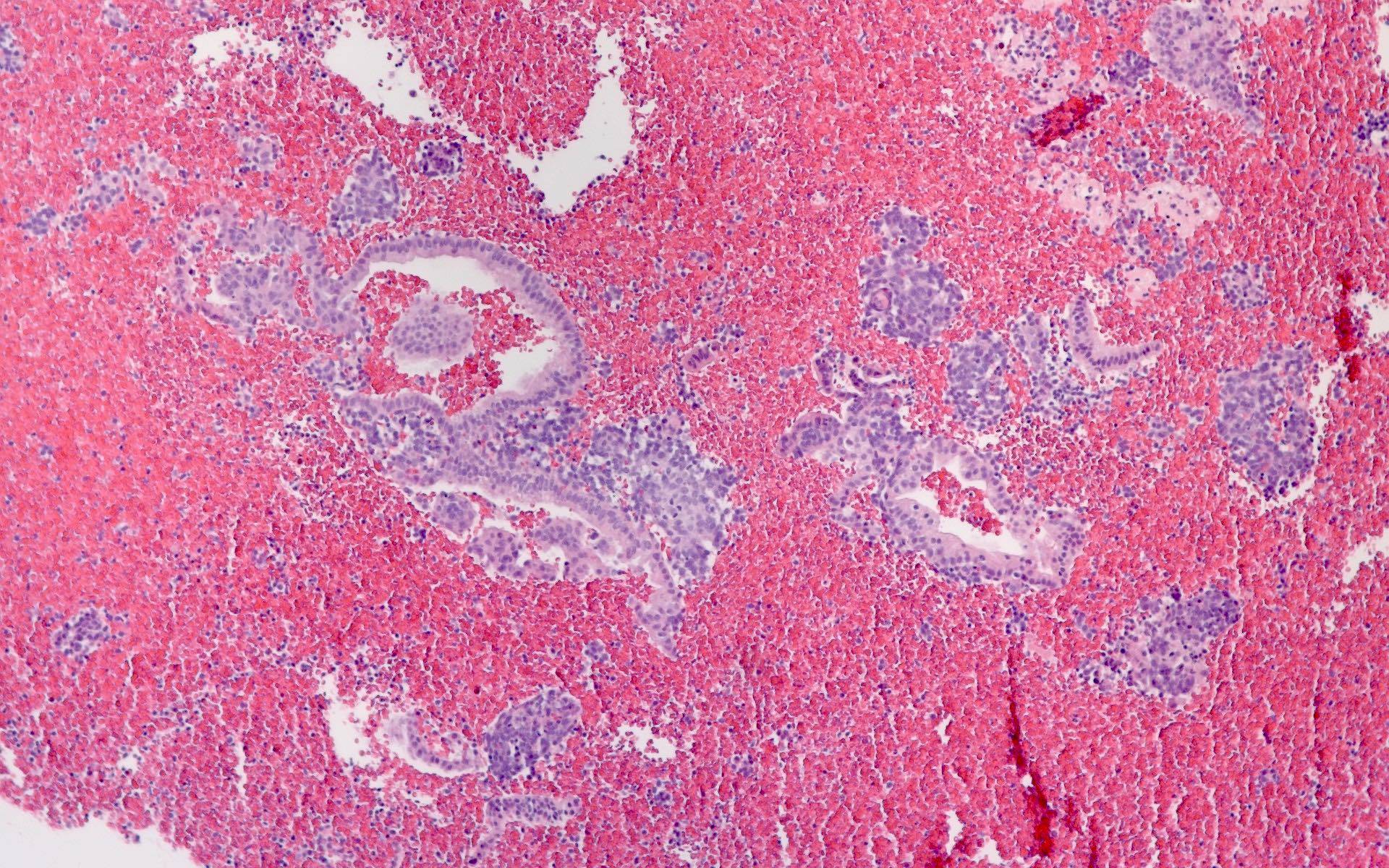
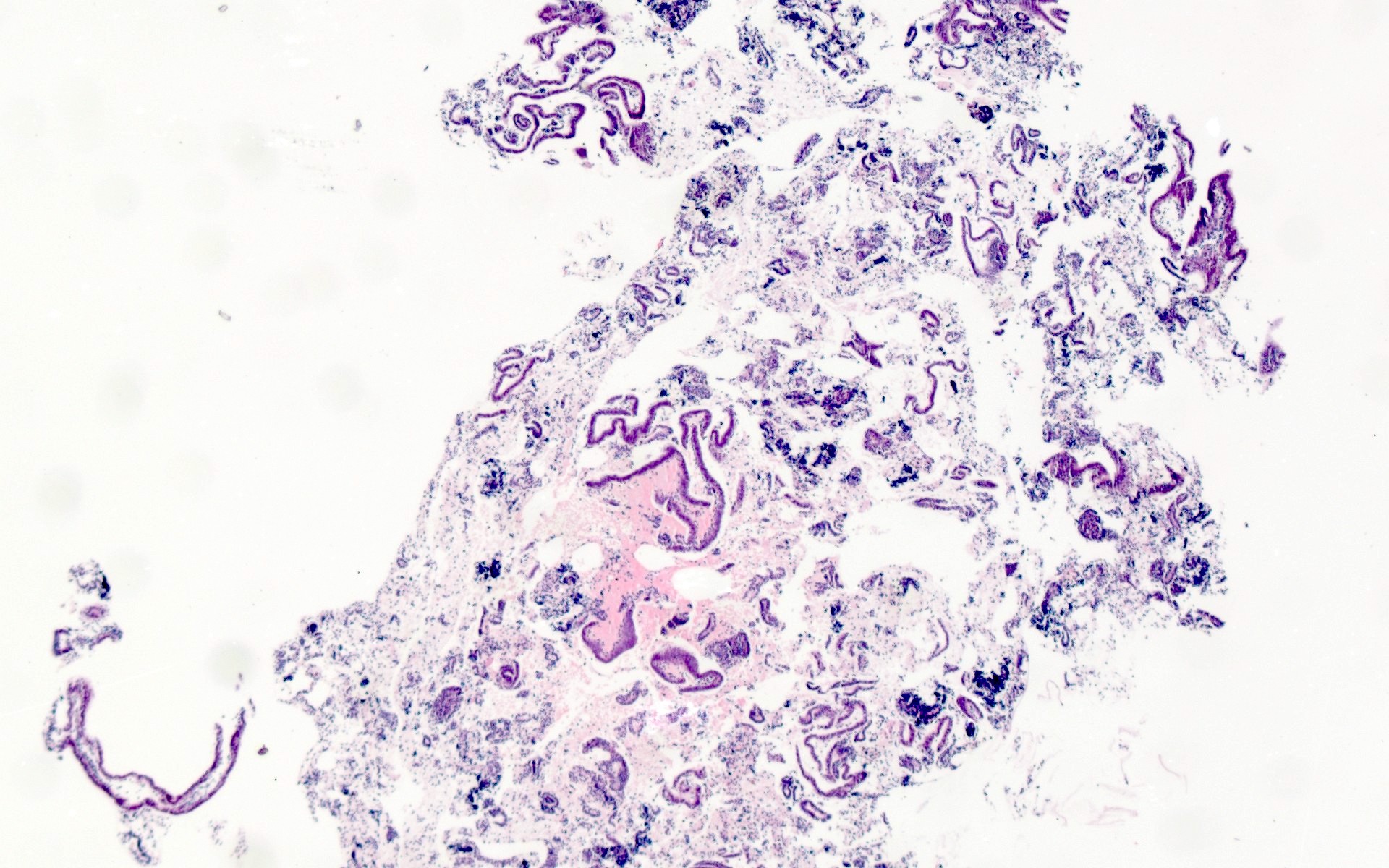
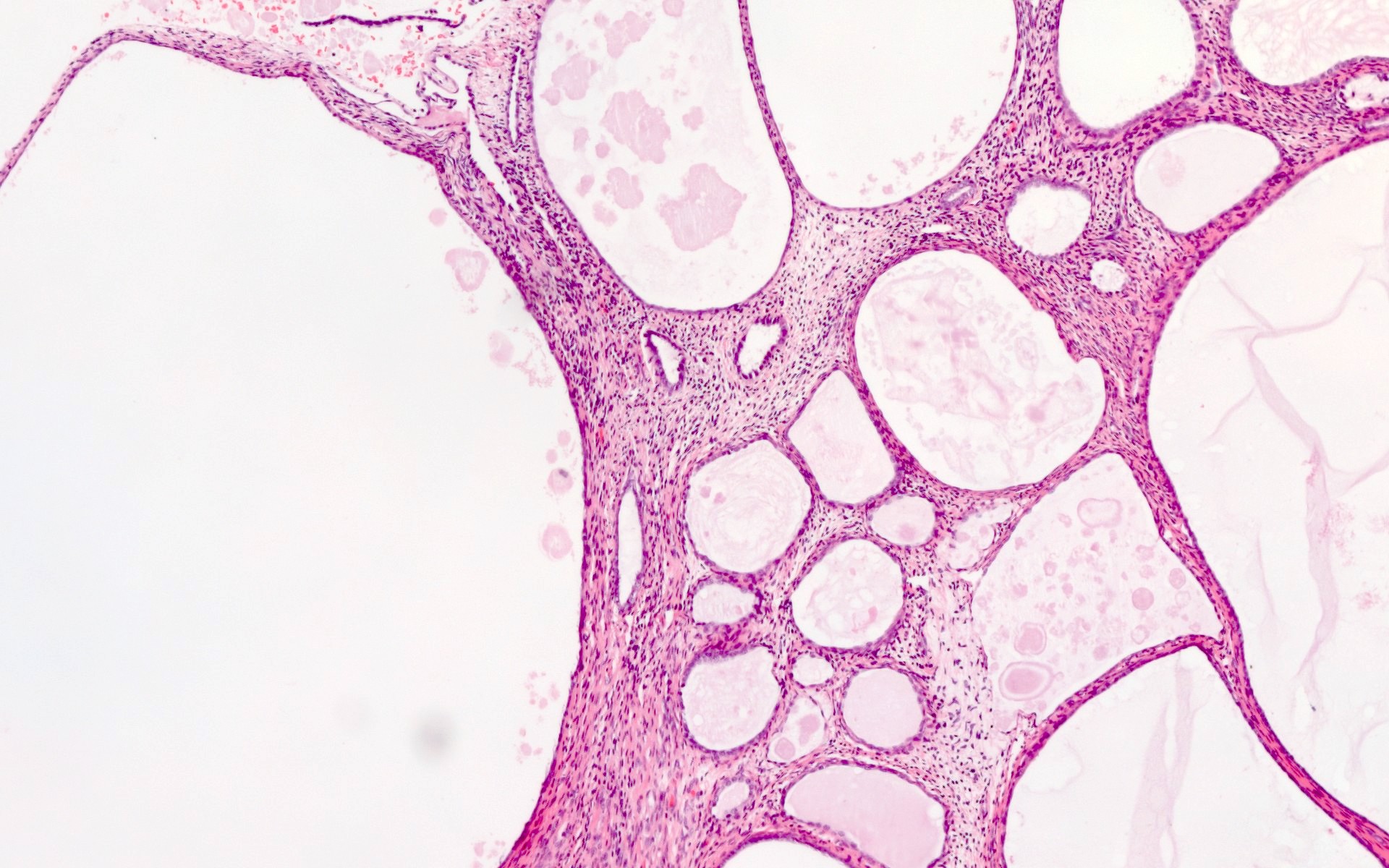
- Atrophic endometrium (see Microscopic images at Uterus - Anatomy & histology)
- Scant strips of cuboidal epithelium with little or no underlying stroma; this a normal finding after menopause
- There may be cystic dilation of the atrophic glands (cystic atrophy) but this is usually not appreciated in a biopsy specimen unless it is present within an endometrial polyp
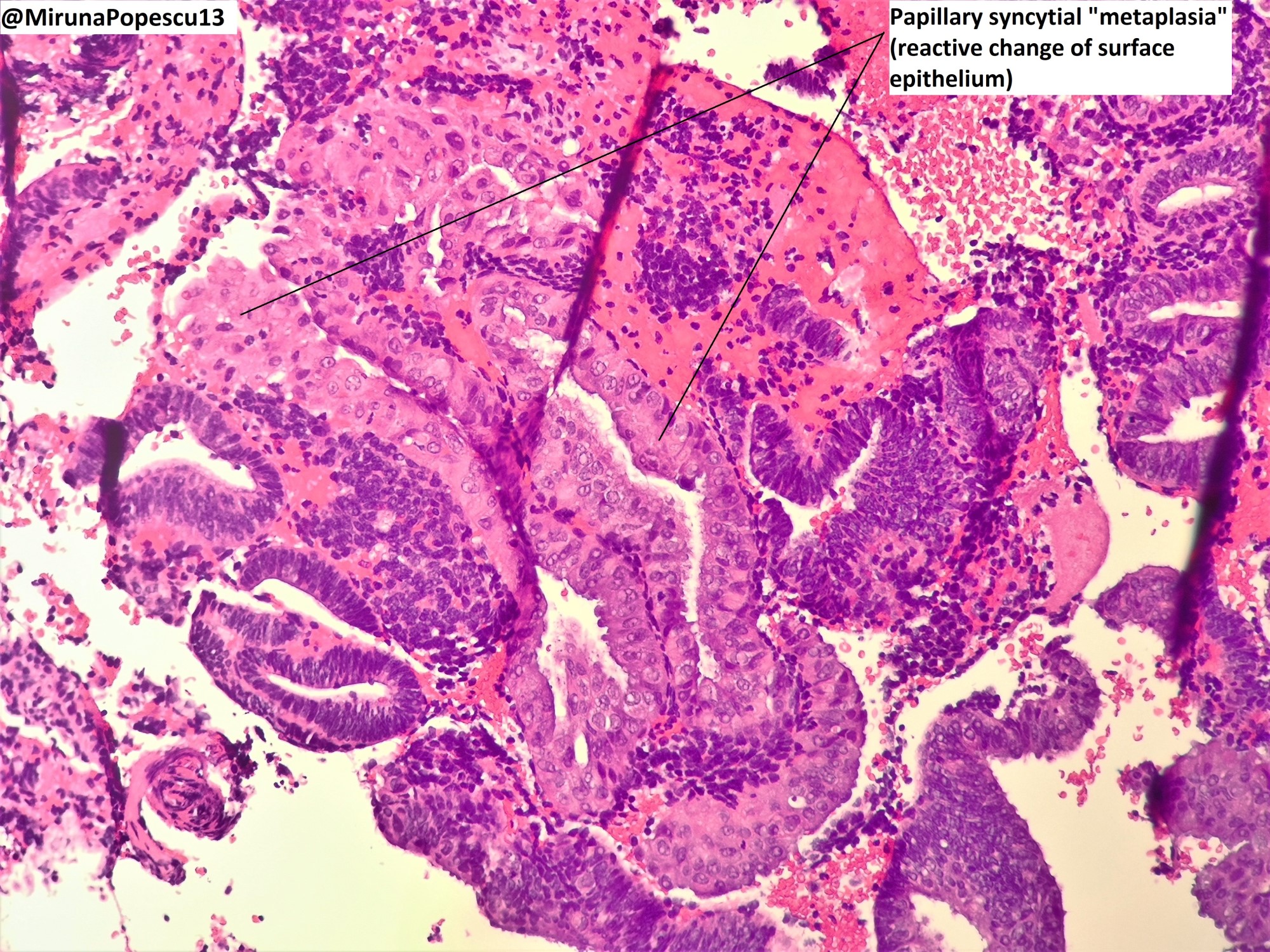
Microscopic (histologic) images
Sample pathology report
- Endometrium, biopsy:
- Atrophic endometrium (see comment)
- Comment: Negative for hyperplasia or carcinoma (please note that a comment is not needed for most endometrial biopsy specimens).
Differential diagnosis
- Endometrial polyp:
- Tissue fragments with abnormal glandular architecture and altered stroma (hypercellular or hypocellular and fibrous appearing), thick walled blood vessels
- Disordered proliferative endometrium:
- Irregular gland architecture compared to normal proliferative endometrium but without significant glandular crowding
- Nonatypical hyperplasia:
- Glandular crowding, with a predominance of glands over stroma, lacking cytological atypia
- Atypical hyperplasia (EIN):
- Both glandular crowding and distinct cytological differences in the epithelial cells lining the crowded glands, compared to the adjacent endometrial glandular epithelium (atypia)
- Carcinoma:
- Greater degree of glandular crowding and cytological atypia than is seen in atypical hyperplasia
- Leiomyoma:
- May not be sampled in a biopsy but if present, the cellularity of the smooth muscle is usually different (more or less cellular) than normal myometrium
- Stromal tumor:
- In the case of low grade endometrial stromal neoplasms, tissue fragments consisting entirely of bland endometrial stromal cells without glands, measuring 5 mm or larger, are seen on biopsy (Am J Clin Pathol 2014;141:133)
- High grade endometrial stromal neoplasms can be identified based on the high grade cytological features of the tumor cells, with brisk mitotic activity
- Confirmatory molecular testing for translocations associated with endometrial stromal neoplasms can confirm the diagnosis but is not completely sensitive (i.e., translocations are not identified in all endometrial stromal neoplasms) (Am J Surg Pathol 2011;35:1364)
- Endometritis:
- Histological findings vary depending on the infectious etiology
- In chronic endometritis, there are increased numbers of lymphoid aggregates, altered stroma, with more spindled morphology and plasma cells
- Exogenous hormone effects:
- Progestins result in hypodeveloped glandular epithelium with widely spaced simple glands, stromal predominance and decidual-like changes of the stromal cells
Additional references
Practice question #1
Which statement is true regarding endometrial biopsy for assessment of abnormal uterine bleeding (AUB)?
- Can be signed out with a final diagnosis of benign in most cases
- Can show a wide range of appearances that reflect the normal cyclical changes of the endometrium
- Is rarely indicated
- Must contain at least 15 fragments of endometrial tissue to be considered inadequate for diagnosis
- Will result in a histopathological diagnosis of abnormal uterine bleeding in most cases
Practice answer #1
B. Can show a wide range of appearances that reflect the normal cyclical changes of the endometrium. The findings in endometrial biopsies taken for abnormal uterine bleeding can show a wide range of appearances that reflect the cyclical changes in the endometrium in women during their reproductive years; accordingly, the histopathological diagnosis provides a description of the features observed microscopically (e.g., proliferative endometrium) and serves to exclude underlying pathology such as carcinoma. Answer A is incorrect because a simple diagnosis of benign, while true, does not convey sufficient information to guide treatment decisions. Answer C is incorrect because endometrial biopsy can be done safely as an office procedure for investigation of abnormal uterine bleeding and is a common surgical pathology specimen. Answer D is incorrect because an endometrial biopsy should only be considered inadequate for diagnosis if there is no endometrial tissue present. Answer E is incorrect because abnormal uterine bleeding is a clinical and not a histopathological diagnosis.
Comment Here
Reference: Abnormal uterine bleeding
Comment Here
Reference: Abnormal uterine bleeding
Practice question #2
Practice answer #2
A. Atrophic endometrium. The most common finding in a postmenopausal woman (defined as more than 1 year since last period) undergoing biopsy for assessment of abnormal uterine bleeding is atrophic endometrium. The chief clinical concern is that there is underlying carcinoma or premalignant change that is causing the abnormal uterine bleeding but that is not the case in most patients. Note that endometrial biopsy has a sensitivity of ~90% for the diagnosis of endometrial carcinoma but because most endometrial biopsies are from patients who do not have carcinoma, the negative predictive value is high (> 99%) (Int J Gynecol Pathol 2020;39:19). Answers B, C, D and E are incorrect because they are each encountered much less frequently in practice than atrophic endometrium.
Comment Here
Reference: Abnormal uterine bleeding
Comment Here
Reference: Abnormal uterine bleeding