Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Atwi D, Hassell LA. Mesonephric-like adenocarcinoma (uterus / ovary). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarymesonephriclikeadenocarcinoma.html. Accessed August 28th, 2025.
Definition / general
- Mesonephric-like adenocarcinoma (MLA) is a rare, recently recognized but frequently misdiagnosed subtype of gynecologic malignancy arising in the ovary and uterine corpus
- MLA shares morphologic, immunophenotypic and molecular characteristics with mesonephric adenocarcinoma (MA) except that mesonephric remnants are not identified in the former
- Entity is included in the 5th edition World Health Organization (WHO) classification of female genital tumors
Essential features
- Rare subtype of gynecologic malignancy with high risk of recurrence and increased tendency to metastasize
- Morphologic hallmark is the combination of architectural patterns in a tumor without squamous or mucinous differentiation; intraluminal dense eosinophilic secretions can be seen
- Low grade morphology with negative ER and PR should prompt the pathologist to perform additional stains
- PAX8, GATA3, TTF1, ER and PR are the main immunohistochemical stains that can be used to support the diagnosis
- Usually mismatch repair (MMR) proficient and p53 wild type
- KRAS mutation is commonly present
ICD coding
Epidemiology
- Endometrial MLA accounts for < 1% of endometrial carcinomas; limited epidemiologic data on ovarian MLA (Am J Surg Pathol 2019;43:389)
- Median age 61 years (range: 36 - 76), more commonly seen in postmenopausal patients (Mod Pathol 2021;34:1570)
Sites
- Uterine corpus and ovary
Pathophysiology
- Controversial whether MLA originates from mesonephric structures or represents Müllerian tumors that have acquired mesonephric characteristics
- Evidence supporting Müllerian origin with mesonephric transdifferentiation
- Endometrial MLA arises from the endometrium rather than myometrium
- MLA is not associated with mesonephric remnants
- Ovarian MLA has been found to coexist with other Müllerian neoplasms such as low grade serous carcinoma (Int J Gynecol Pathol 2020;39:84)
- MA and MLA share KRAS mutations but concurrent PIK3CA mutations, which are described in endometrioid adenocarcinoma, are also documented in MLA
- NRAS mutations may occur (Int J Gynecol Pathol 2018;37:448)
Etiology
- Unknown
Clinical features
- Patients with endometrial MLA may present with abnormal vaginal bleeding
- Patients with ovarian MLA may present with pelvic or abdominal pain and may be associated with endometriosis and other benign, borderline and malignant lesions of Müllerian origin (Am J Surg Pathol 2021;45:498)
Diagnosis
- Definitive diagnosis of MLA requires a surgical specimen
- Limited literature on the cytologic features of these tumors; may be identified on Pap test as atypical glandular cells (AGC) (Am J Surg Pathol 2021;45:498)
- MLA of the uterine corpus was correctly diagnosed on initial biopsy in only 32% of the cases in one study (Am J Surg Pathol 2021;45:498)
Laboratory
- Patient may have elevated tumor markers (CA125, CA19-9) (Int J Gynecol Pathol 2022;41:161)
Prognostic factors
- Factors associated with development of metastasis in mesonephric adenocarcinoma of the uterine corpus (Am J Surg Pathol 2019;43:12)
- Large tumor size (> 4 cm)
- Ill defined tumor border
- Advanced FIGO stages (III - IV)
- Presence of coagulative tumor cell necrosis
- High mitotic activity (> 10/10 high power fields)
- Lymphovascular invasion (Am J Surg Pathol 2019;43:12)
- Associated with aggressive clinical course (J Clin Med 2021;10:698)
- Tends to present with advanced stage (FIGO II or more)
- Increased risk of recurrent disease
- Increased tendency to metastasize to the lungs even for tumors with stage I disease
- Compared with other endometrial adenocarcinomas (Am J Surg Pathol 2021;45:498)
- Better overall survival than carcinosarcoma and serous carcinoma
- Equal overall survival to endometrioid grade 3
- Worse overall survival than endometrioid grade 1 - 2 carcinomas
Case reports
- 32 year old woman with coexistent endometrial mesonephric-like adenocarcinoma and endometrioid carcinoma (Diagn Pathol 2019;14:54)
- 58 year old woman with endometrial mesonephric-like adenocarcinoma presenting as an ocular lesion (Int J Gynecol Pathol 2022;41:161)
- 69 year old woman with synchronous ovarian and uterine mesonephric-like carcinoma that potentially arose from endometrioid adenofibroma (J Obstet Gynaecol Res 2023;49:1052)
- 70 year old woman with mesonephric-like adenocarcinoma arising from the uterine body and mimicking follicular thyroid carcinoma (Histopathology 2019;74:651)
- 71 year old woman with corded and hyalinized mesonephric-like adenocarcinoma of the uterine corpus (Hum Pathol 2019;86:243)
Treatment
- Surgical approach with total hysterectomy and bilateral salpingo-oophorectomy, with or without pelvic and para-aortic lymph node dissection, is the primary therapy
- Adjuvant chemotherapy and radiation therapy have been used
- Hormone therapy has been reported in 2 cases (Am J Surg Pathol 2020;44:429)
- No tumor specific treatment options have been elucidated for MLA
Gross description
- No distinctive macroscopic appearance compared to other endometrial or ovarian tumors
- Areas of necrosis and hemorrhage can be present
- Ovarian MLA is usually unilateral, ranging in size from 4 - 32 cm, with solid or mixed solid cystic, grey-white or yellow-tan appearance (Histopathology 2016;68:1013)
Microscopic (histologic) description
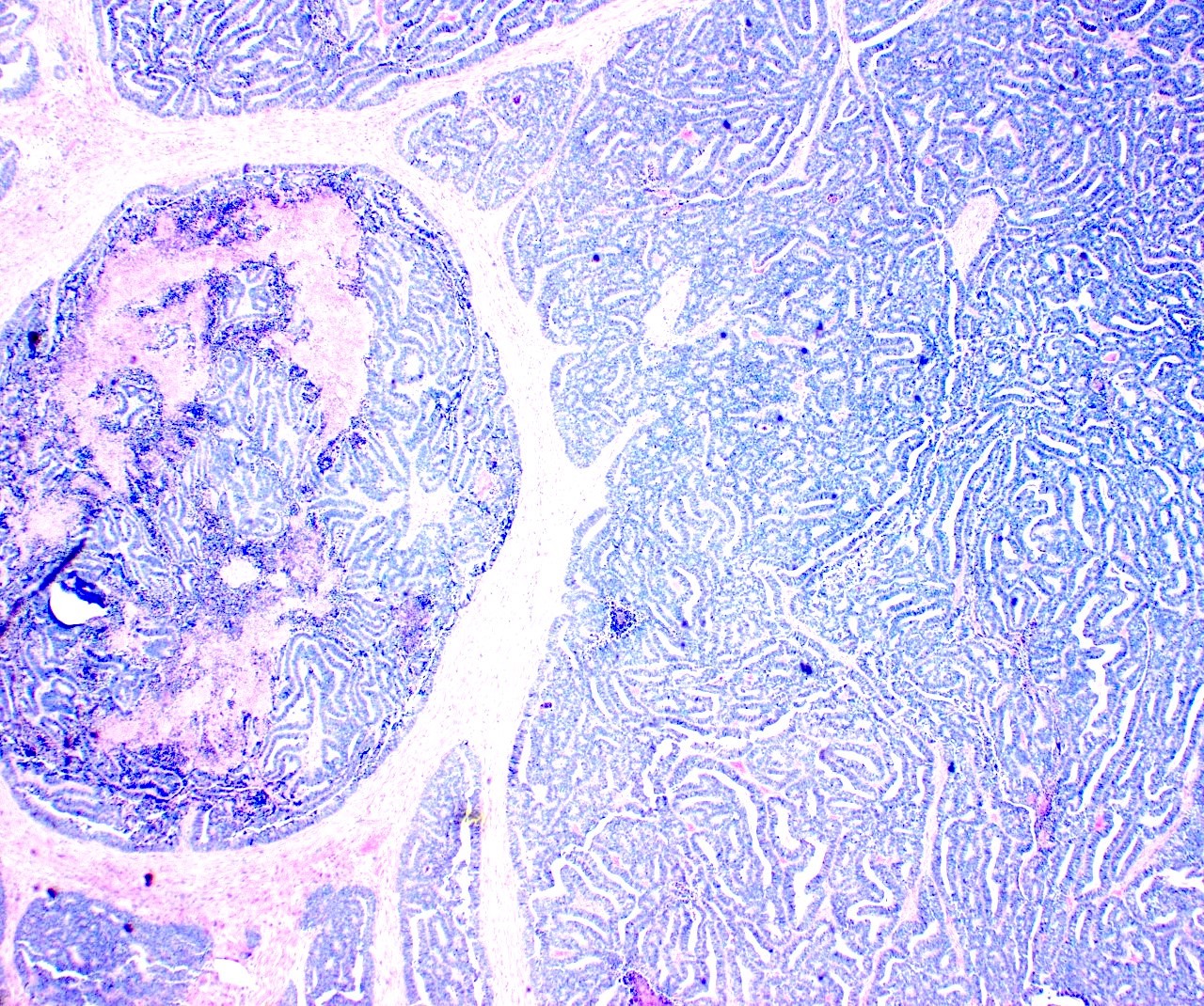
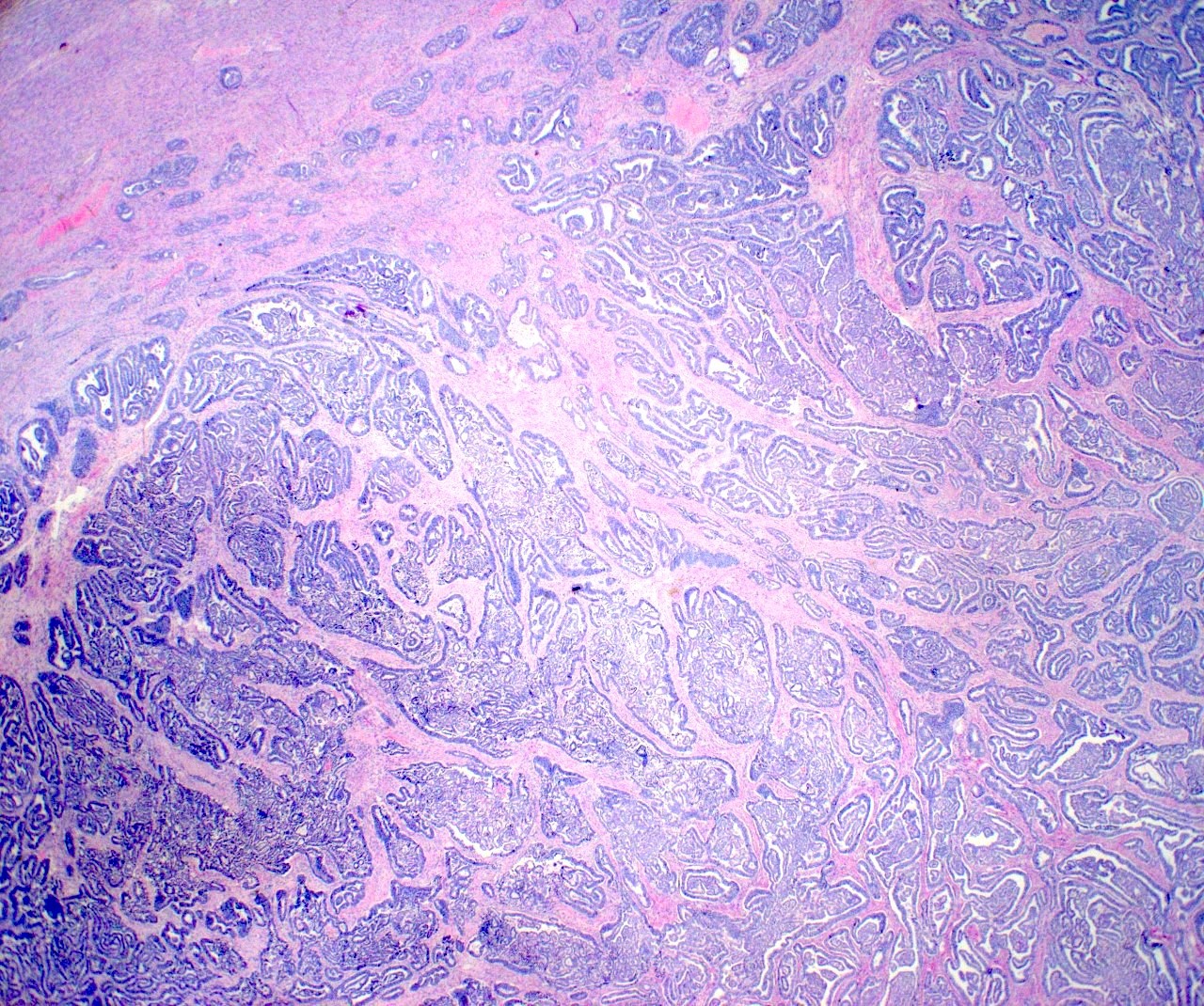
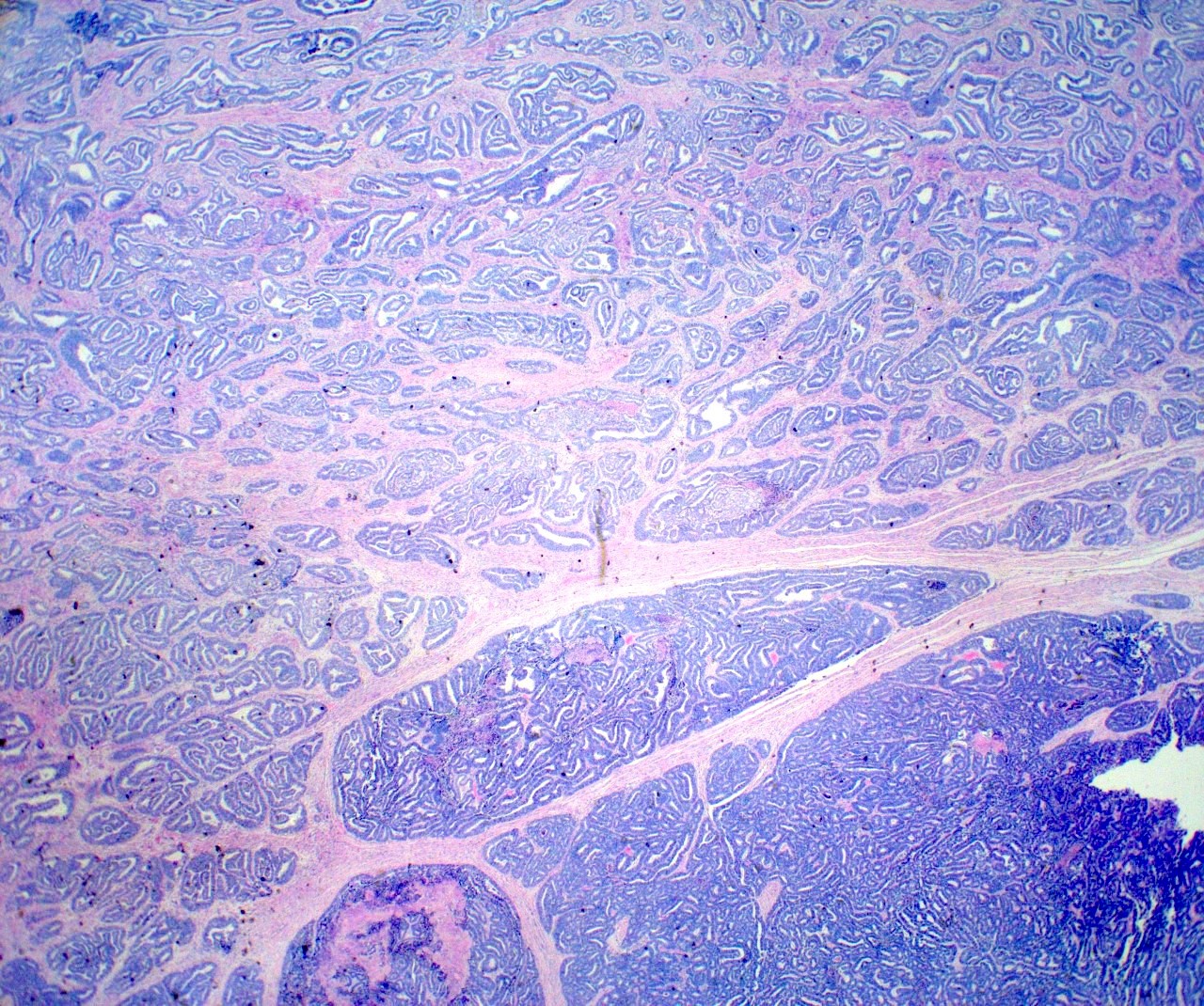
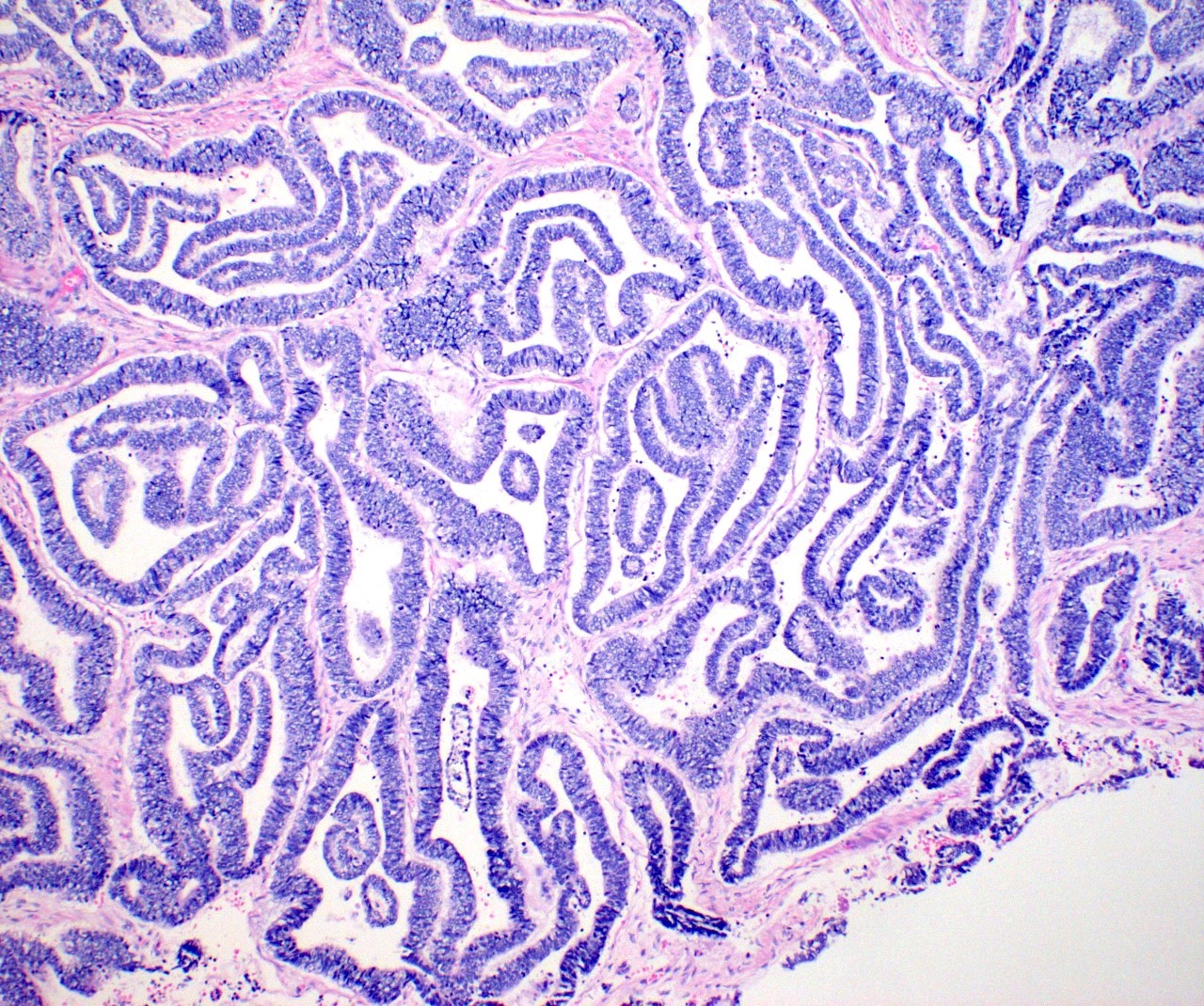
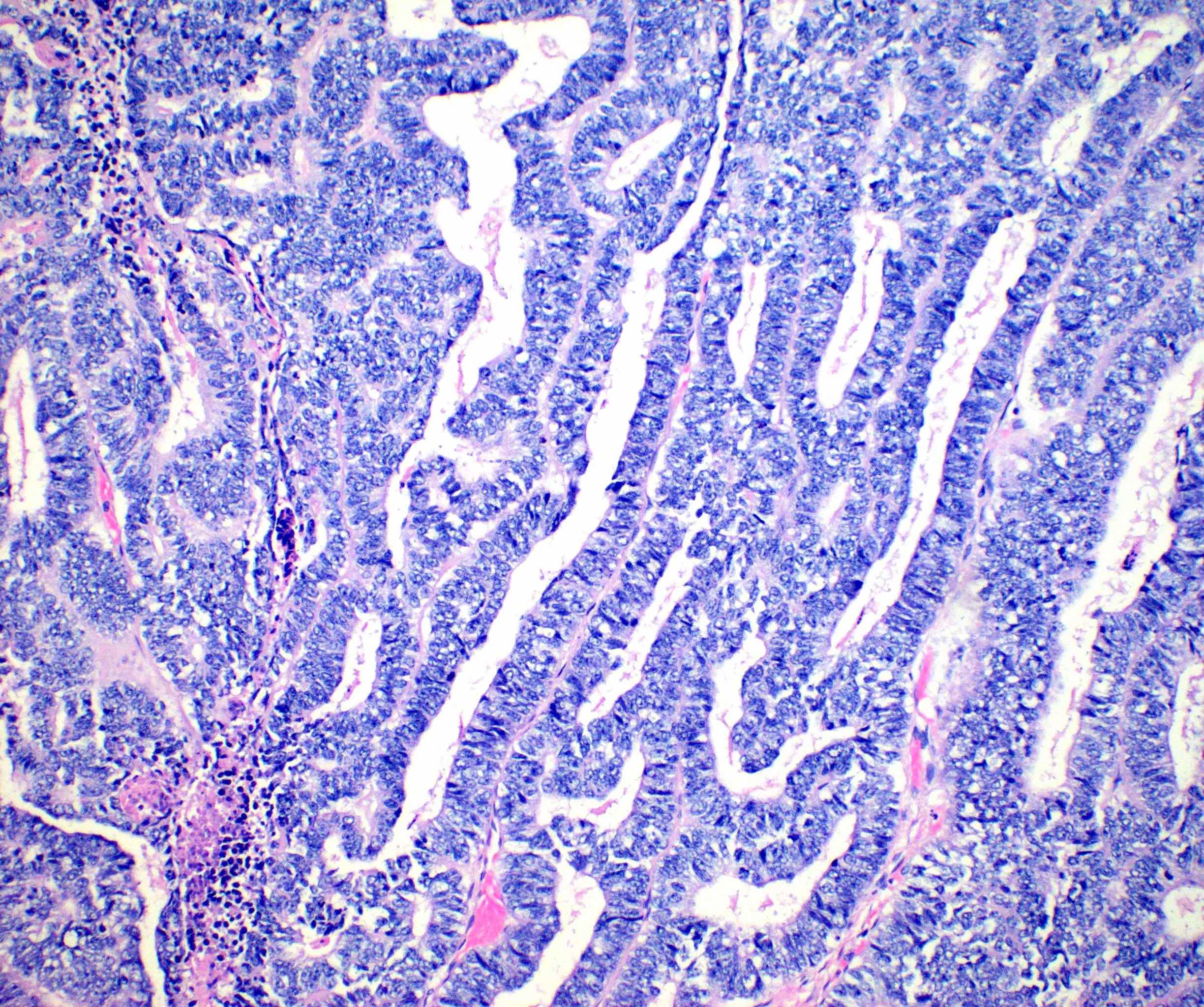
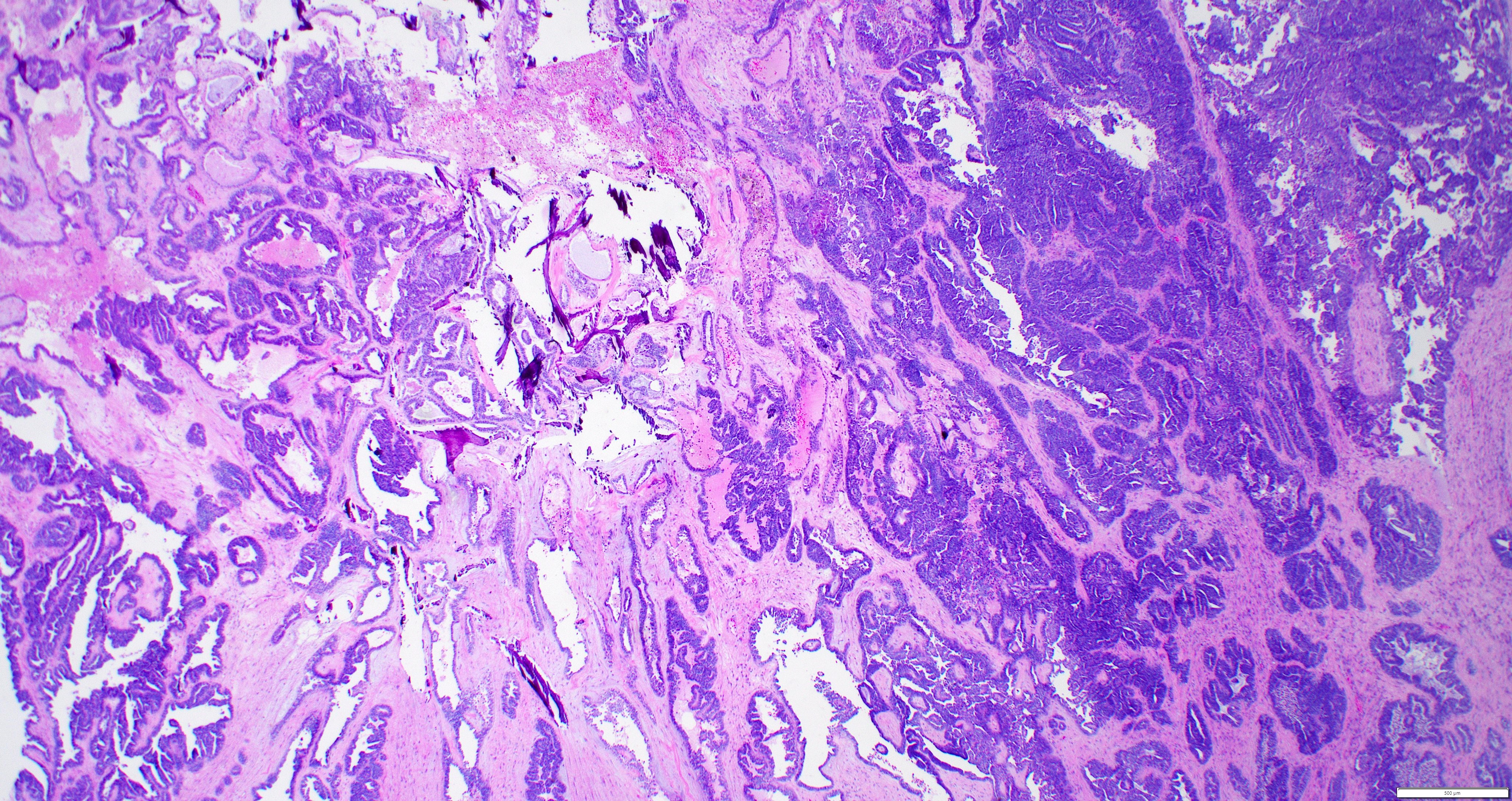
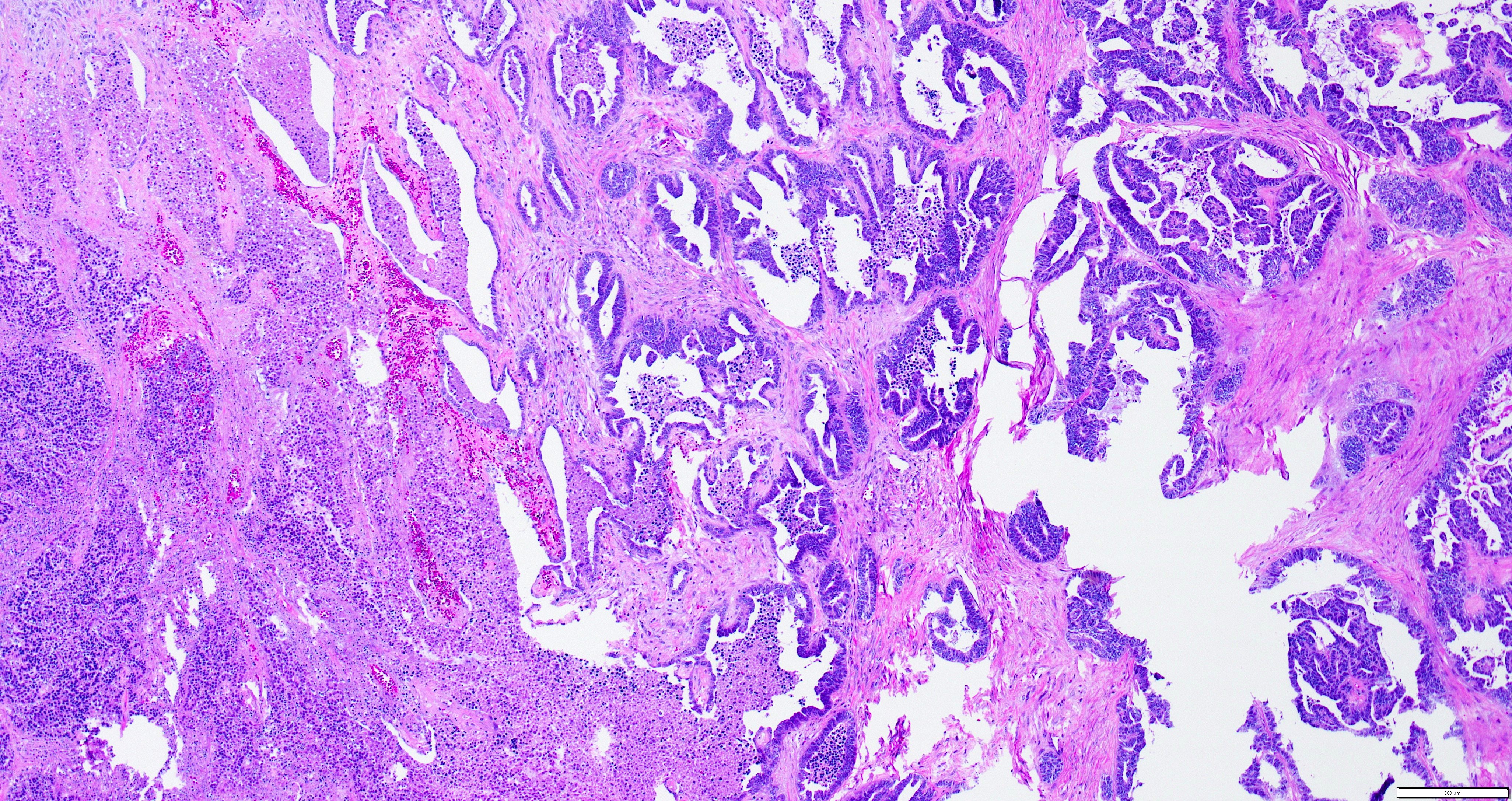
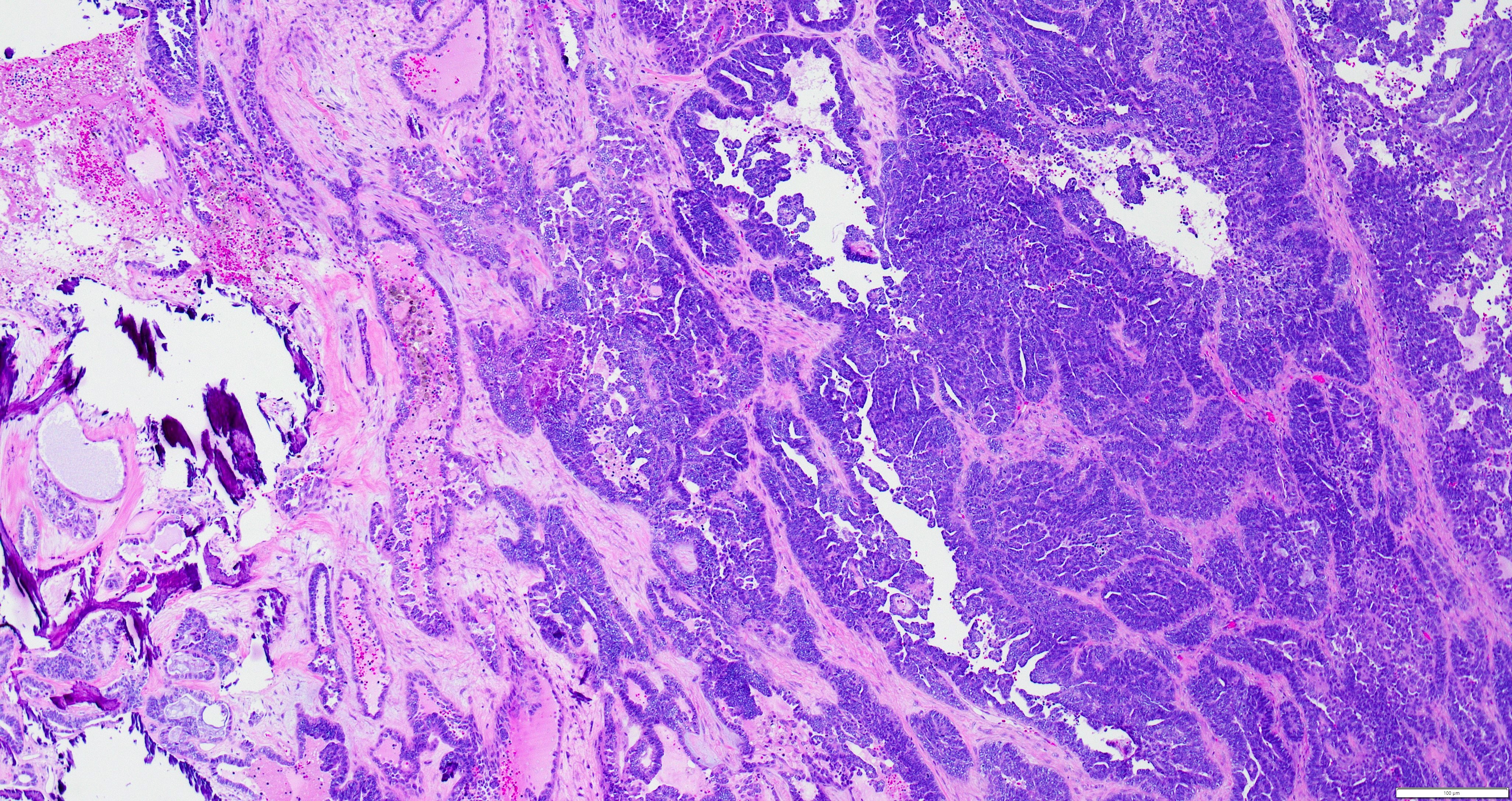
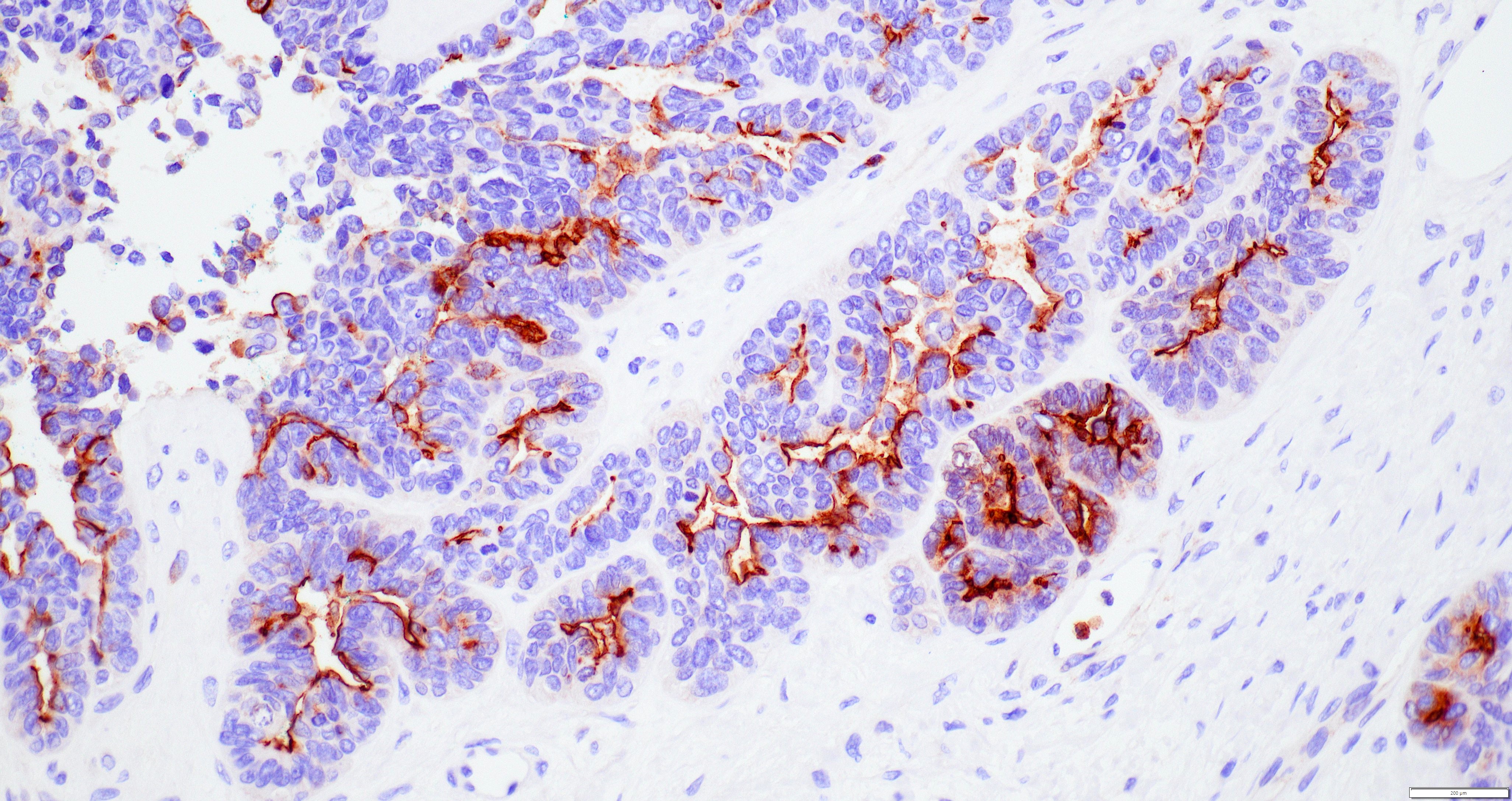
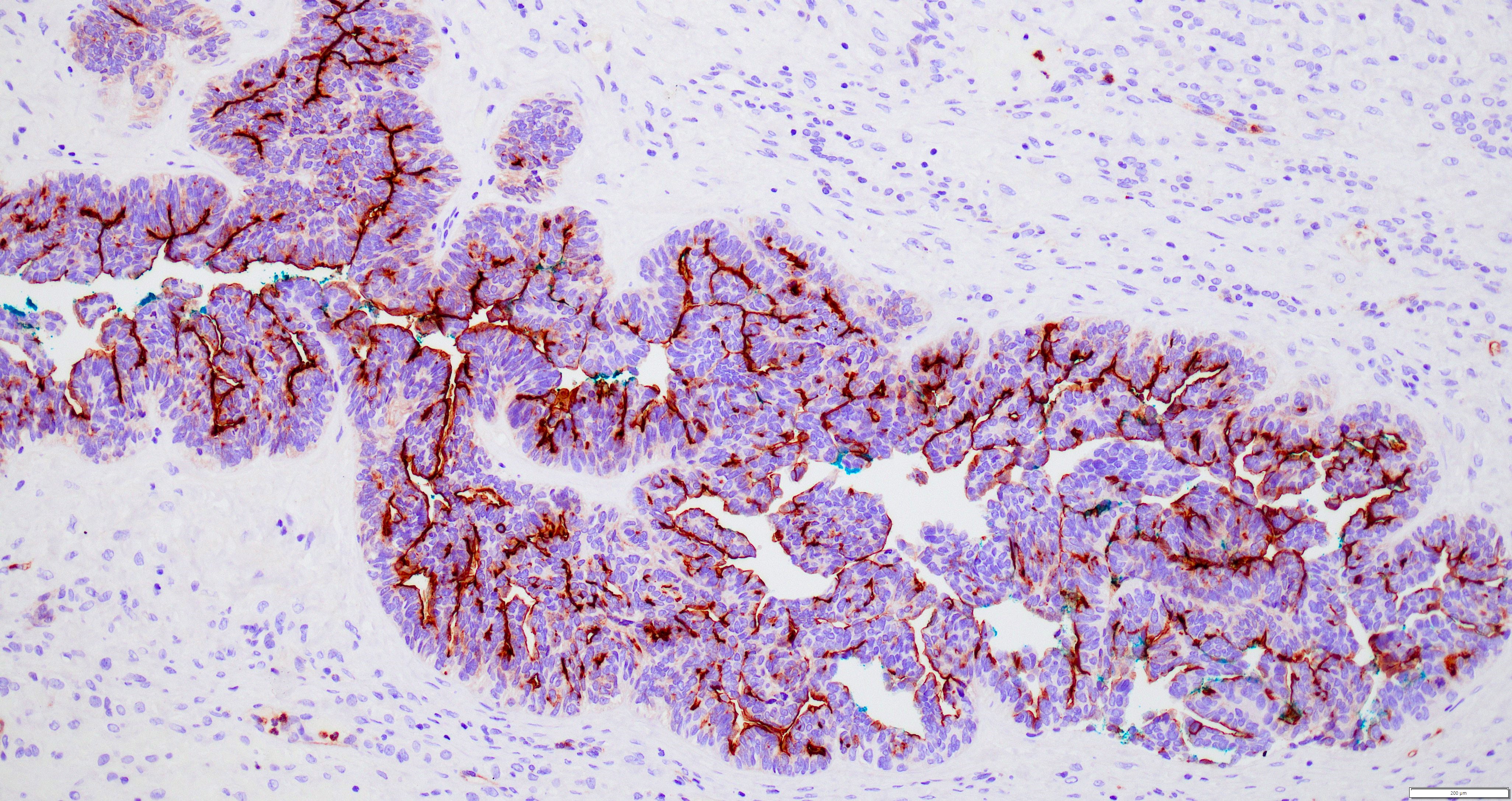
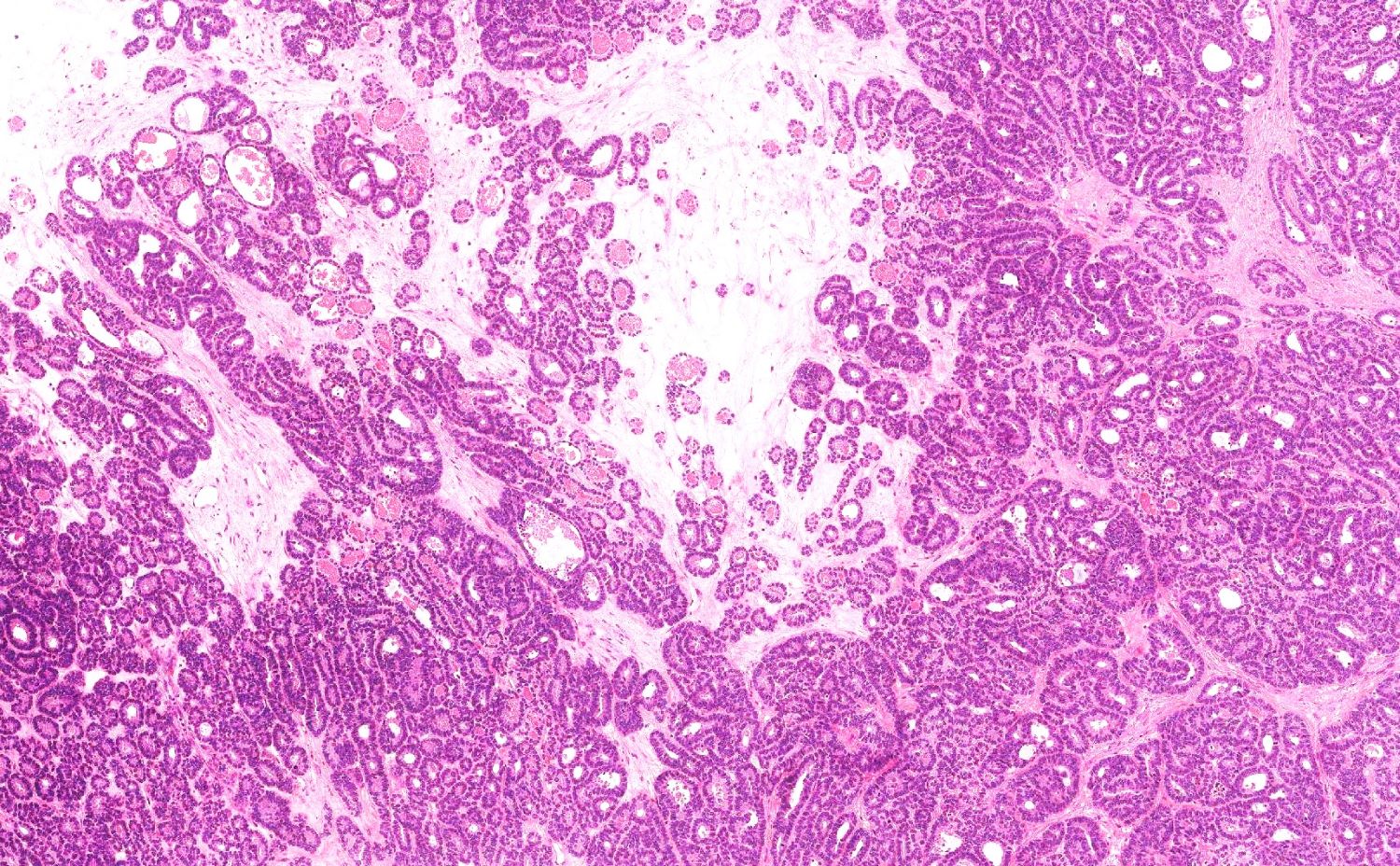
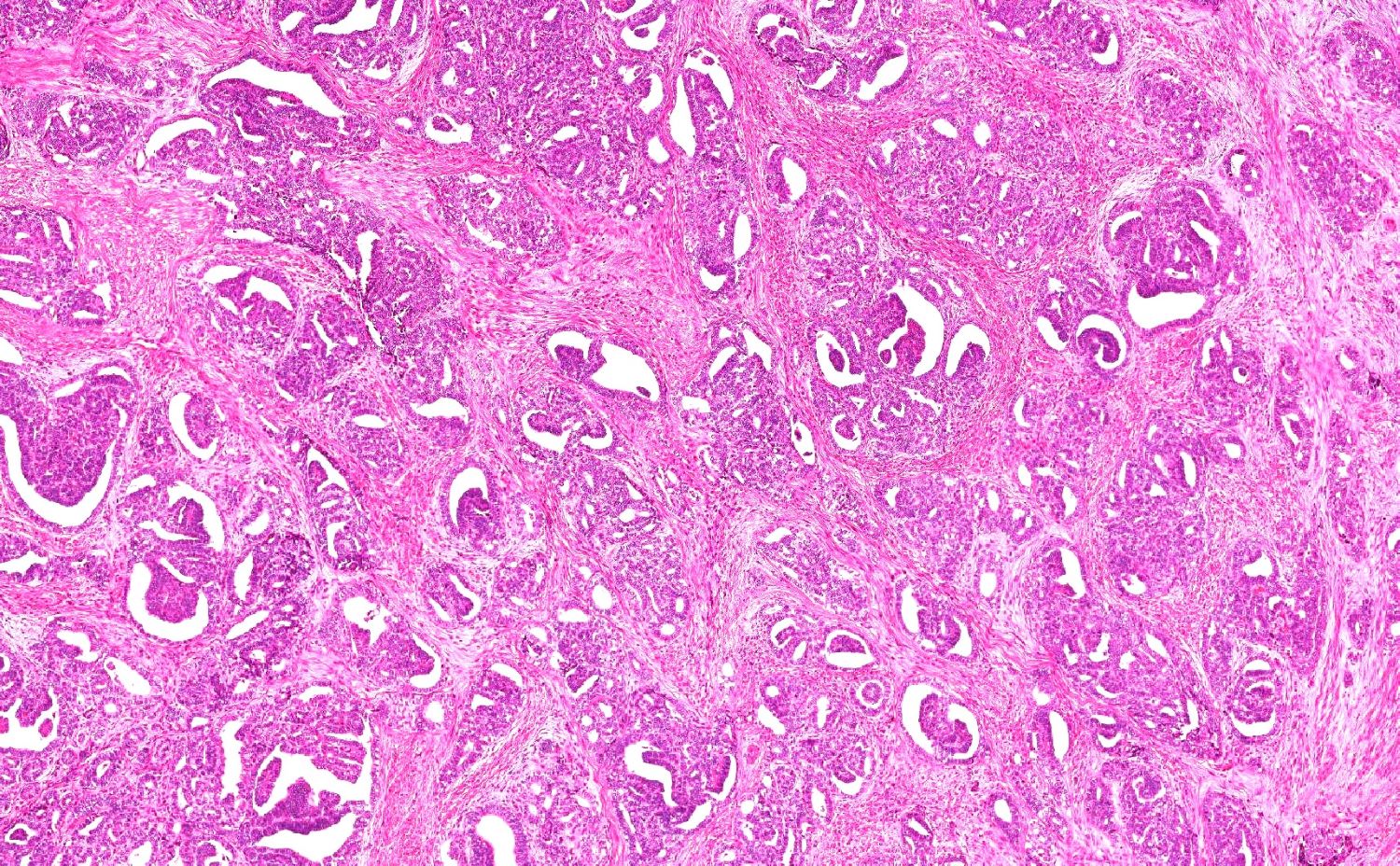
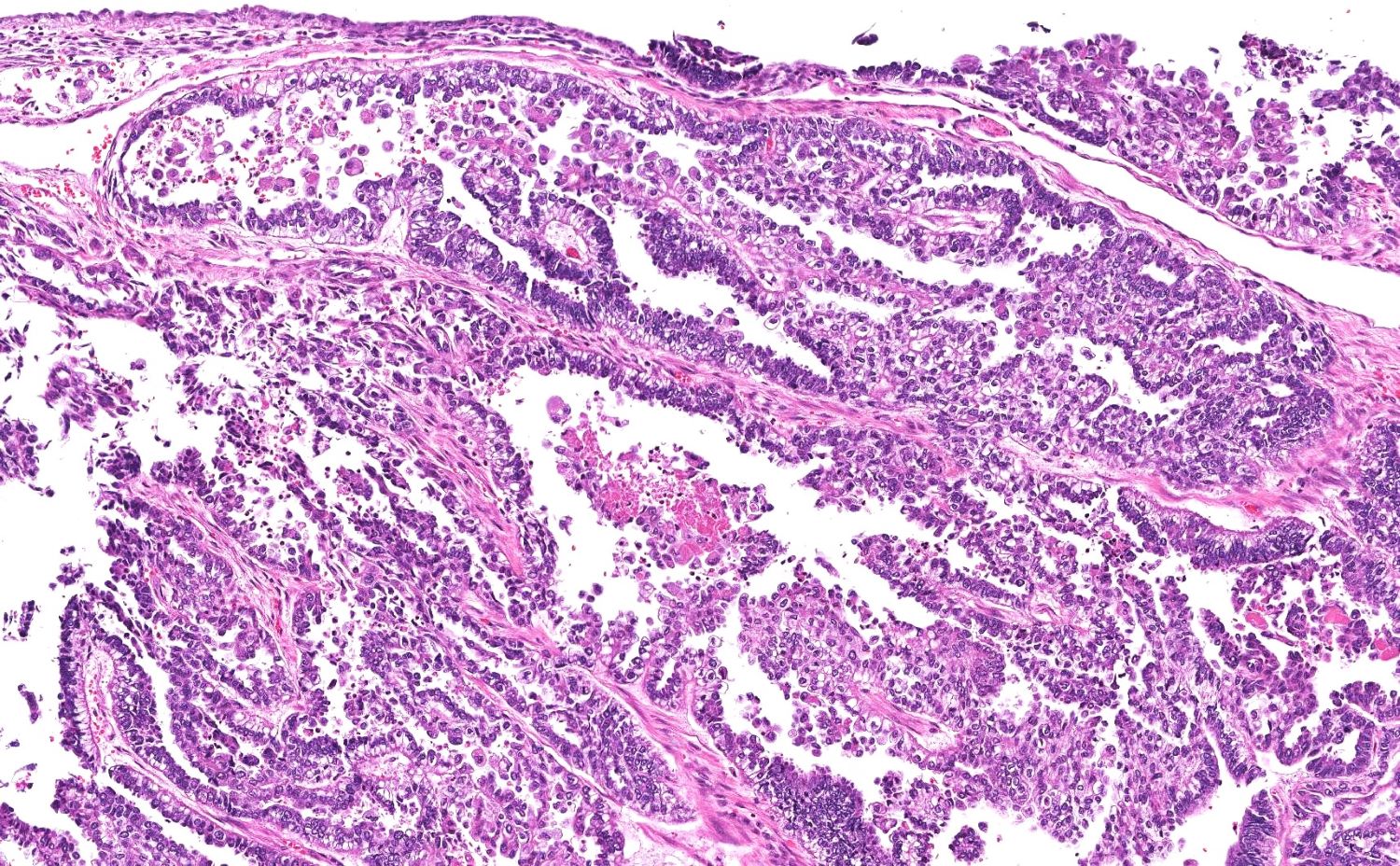
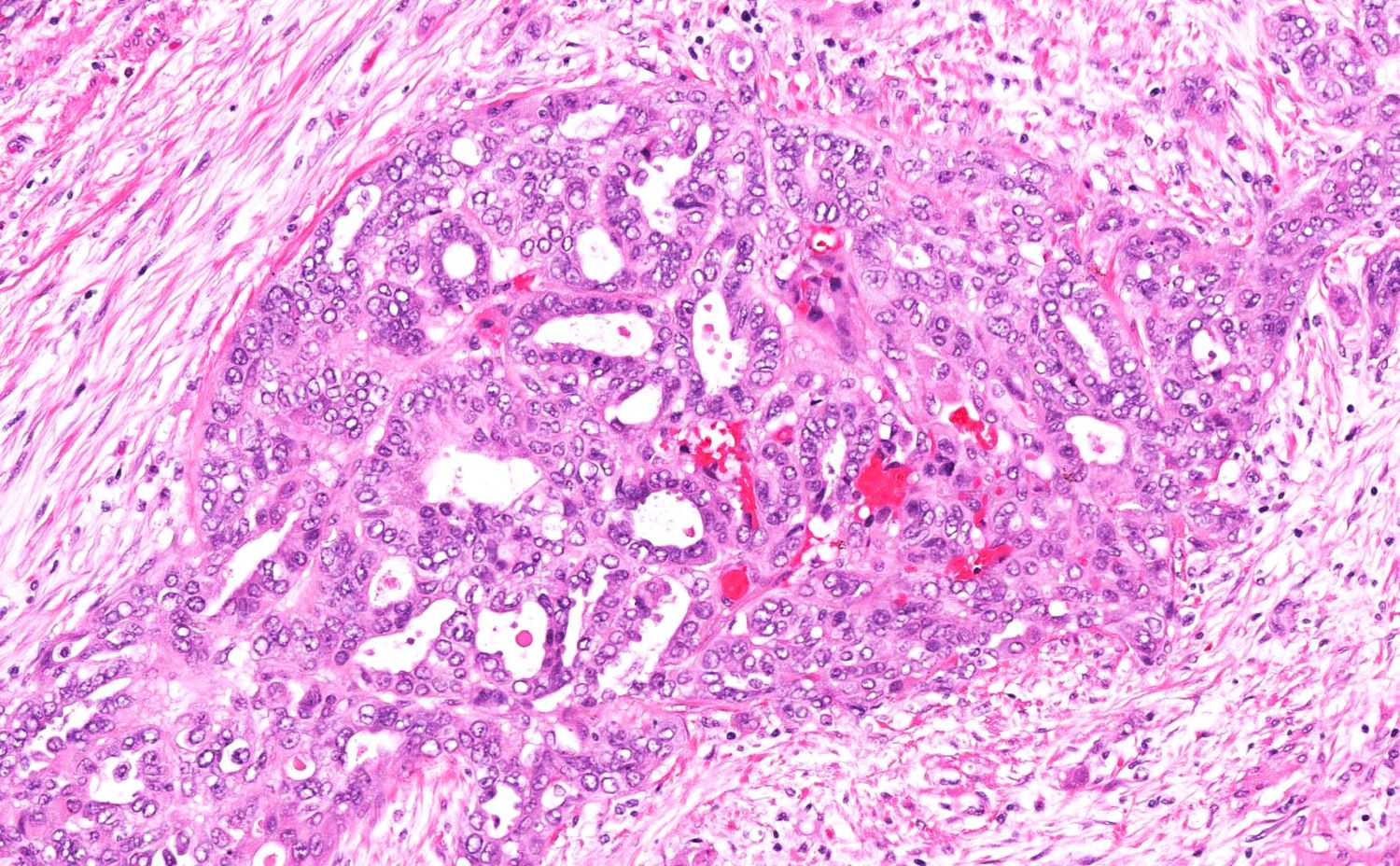
- Variety of histologic patterns that may be present within the same tumor
- Most frequently small tubules with ductal / glandular growth
- Papillary, solid growth, trabecular, retiform, sex cord-like, sieve-like, glomeruloid and spindle cell areas have all been described
- Luminal eosinophilic secretions are characteristic but not always identified
- Tumor cells can be flattened, cuboidal or columnar with mild to moderate cytological atypia
- Clear cell features can be seen but are less common
- High grade cytological atypia is usually not a predominant feature
- Nuclei show vesicular chromatin and nuclear grooves
- Sarcomatoid transformation has been seen in rare instances
- Squamous, ciliated or mucinous differentiation (metaplasia) are not present and there are no associated mesonephric remnants (J Clin Med 2021;10:698)
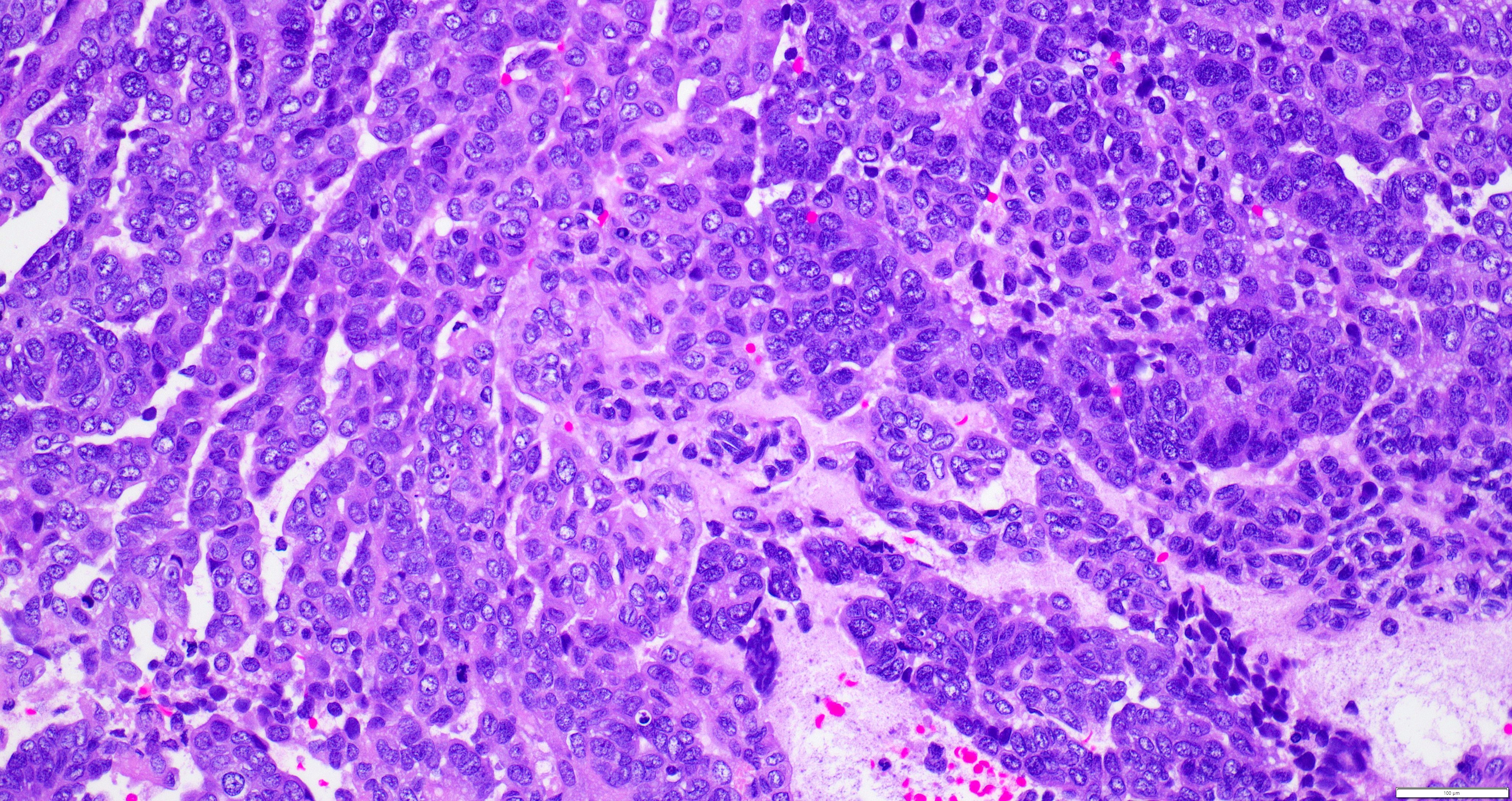
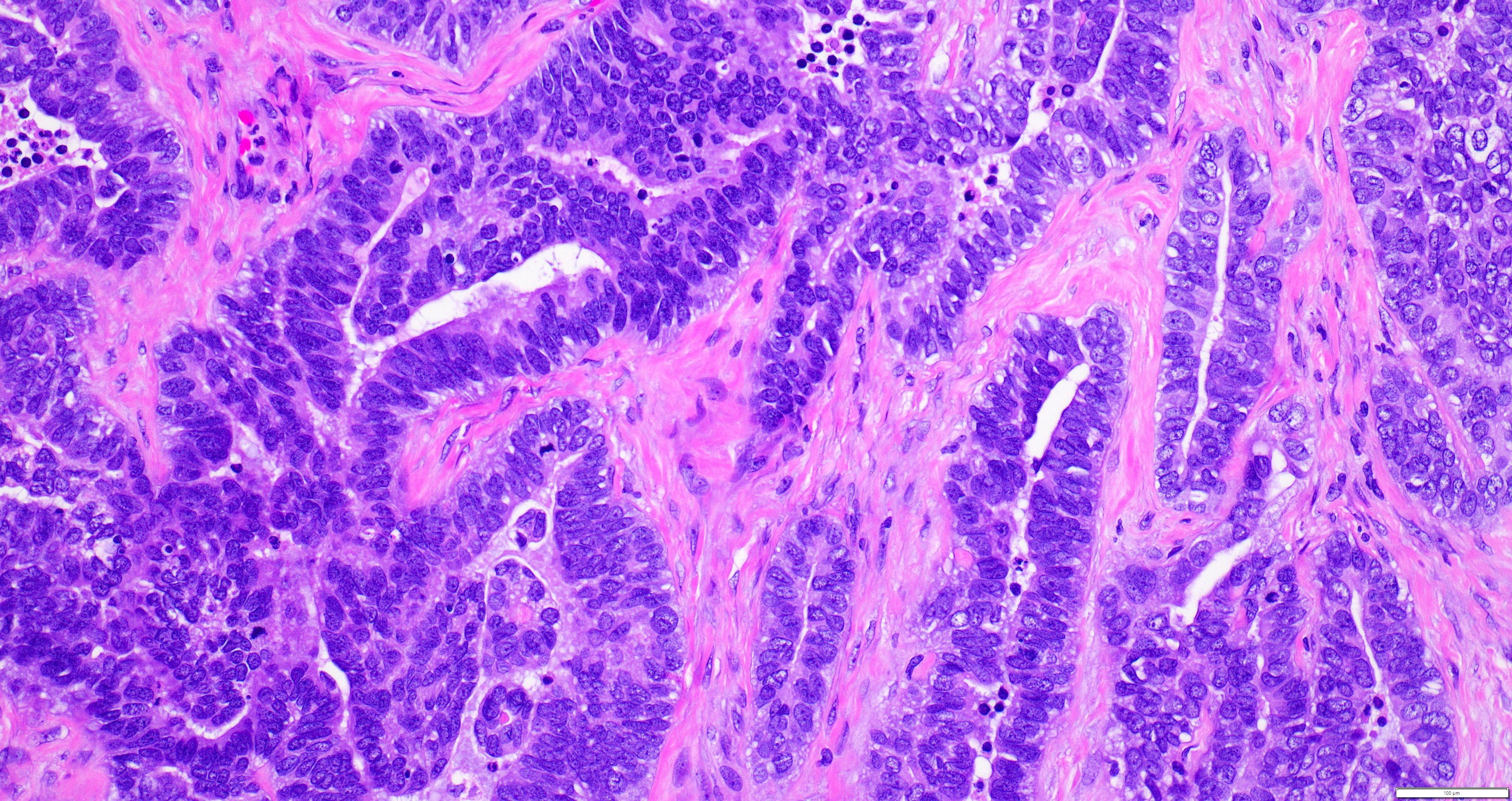
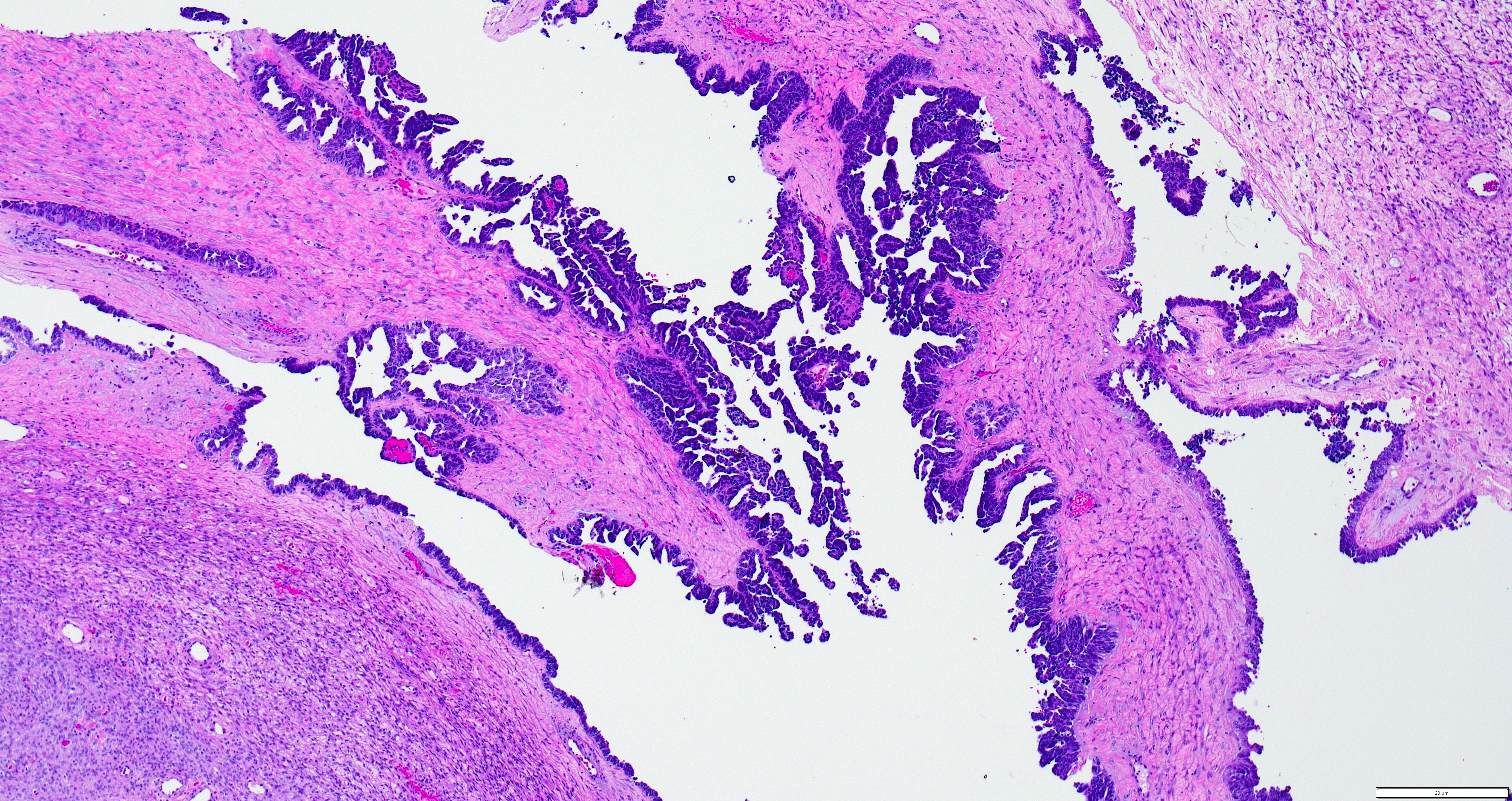
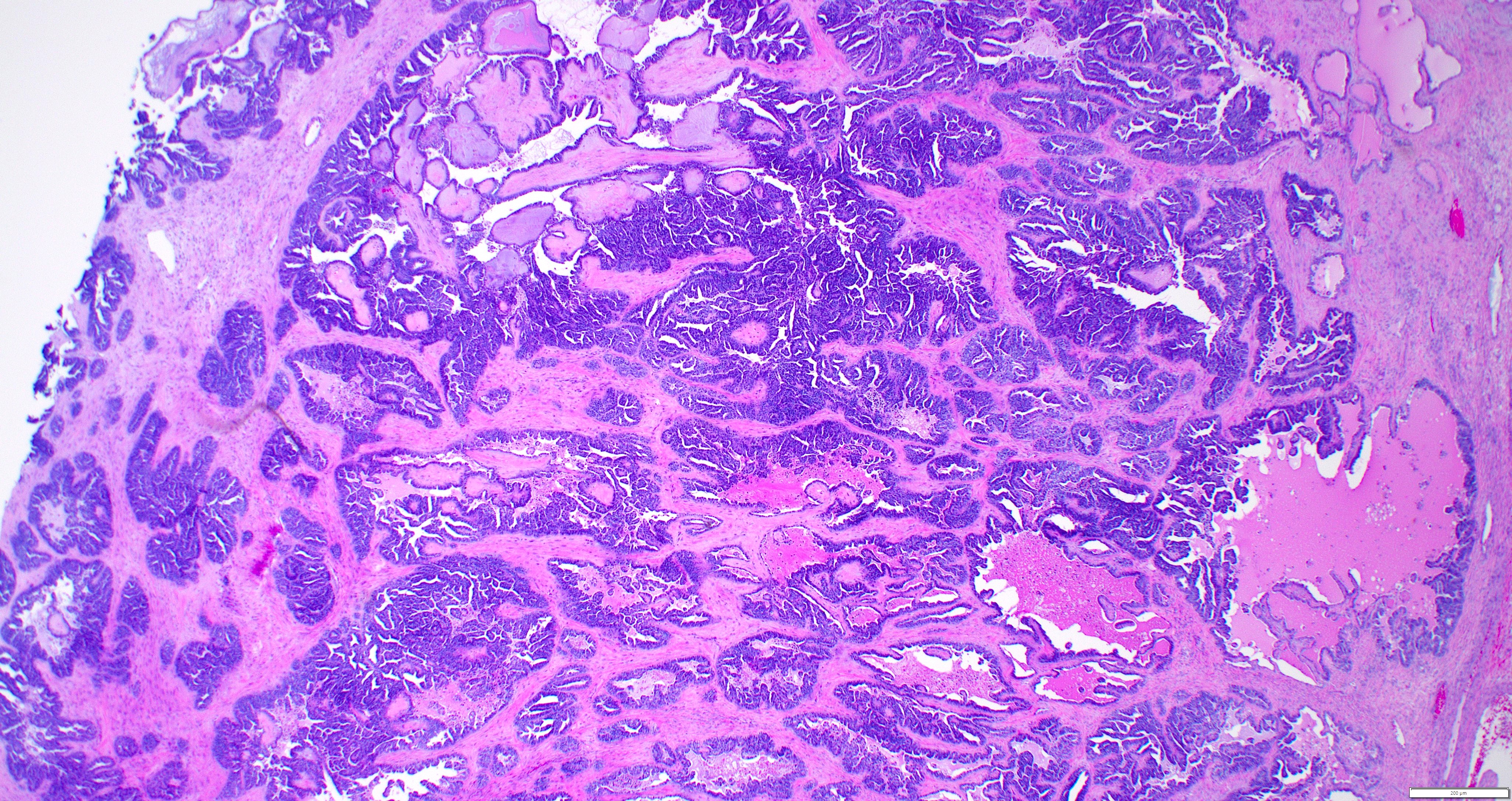
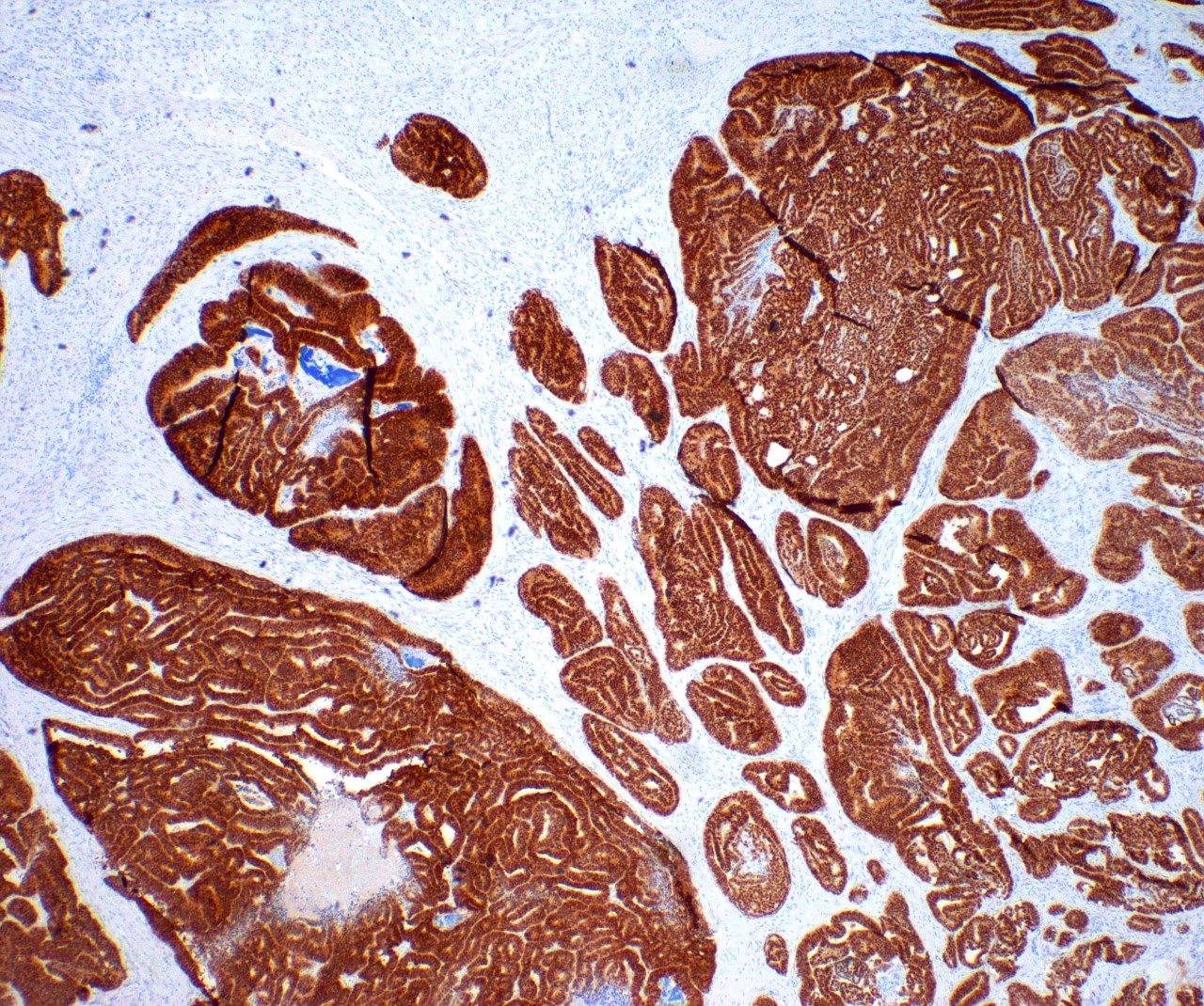
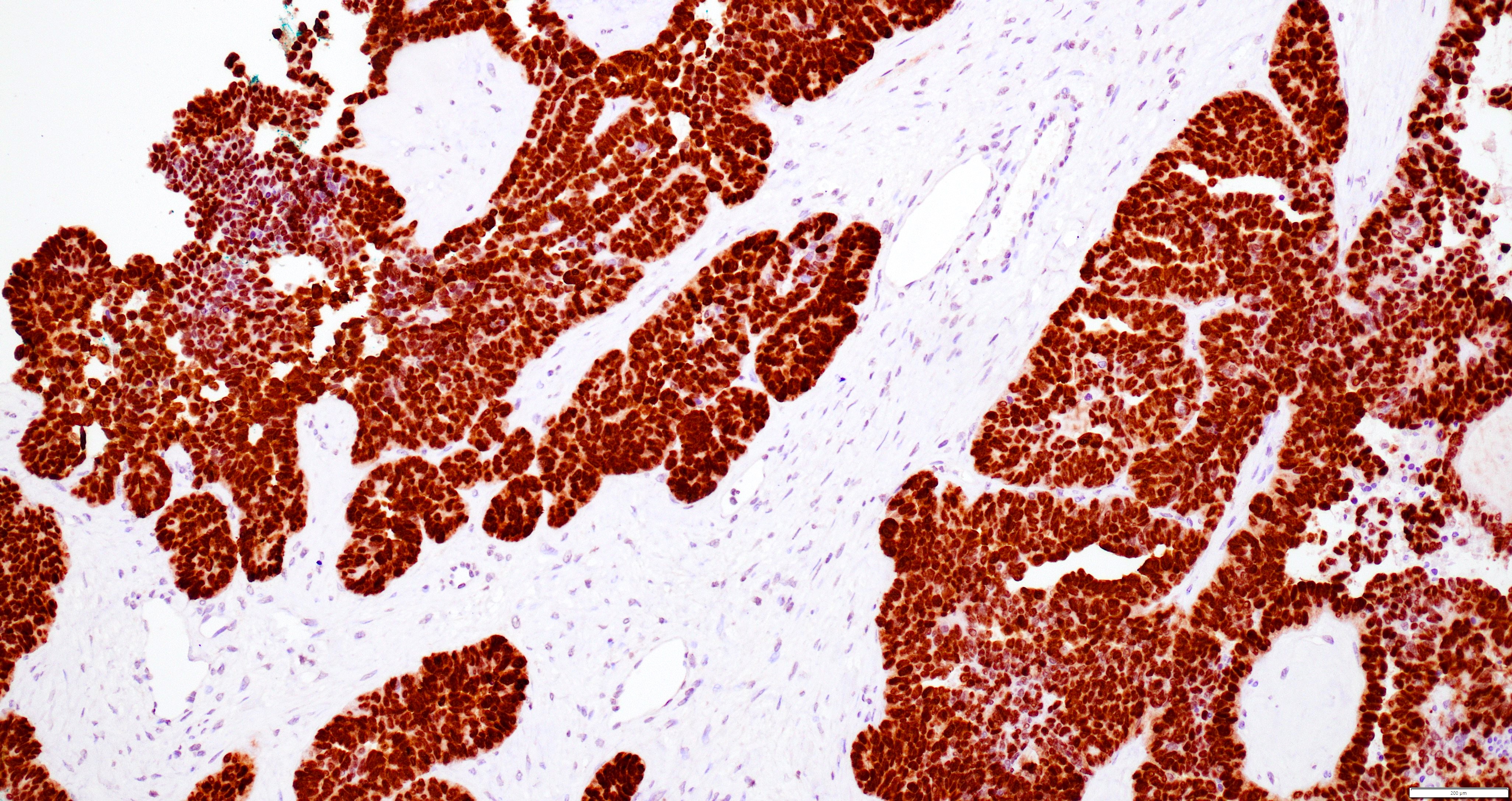
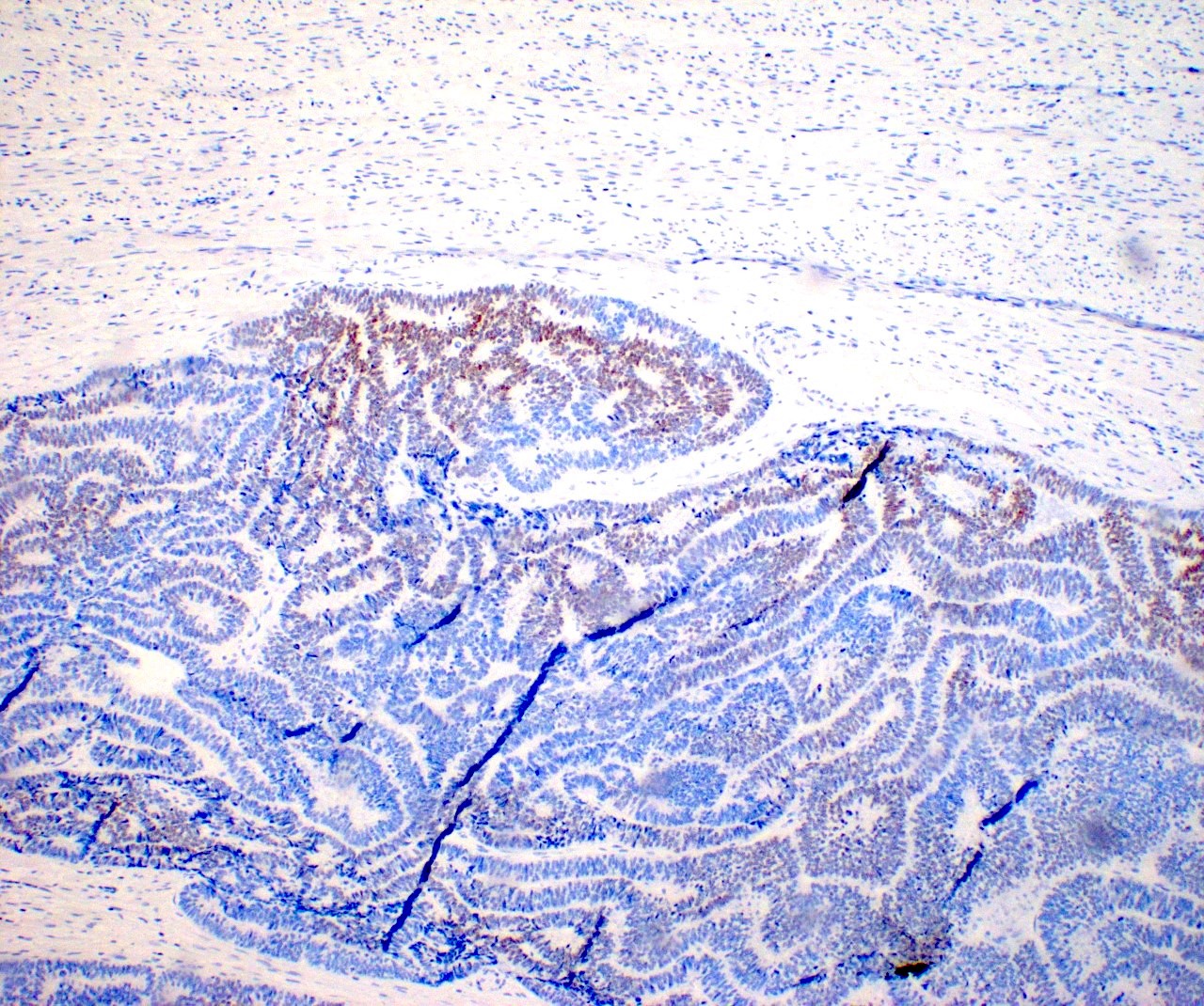
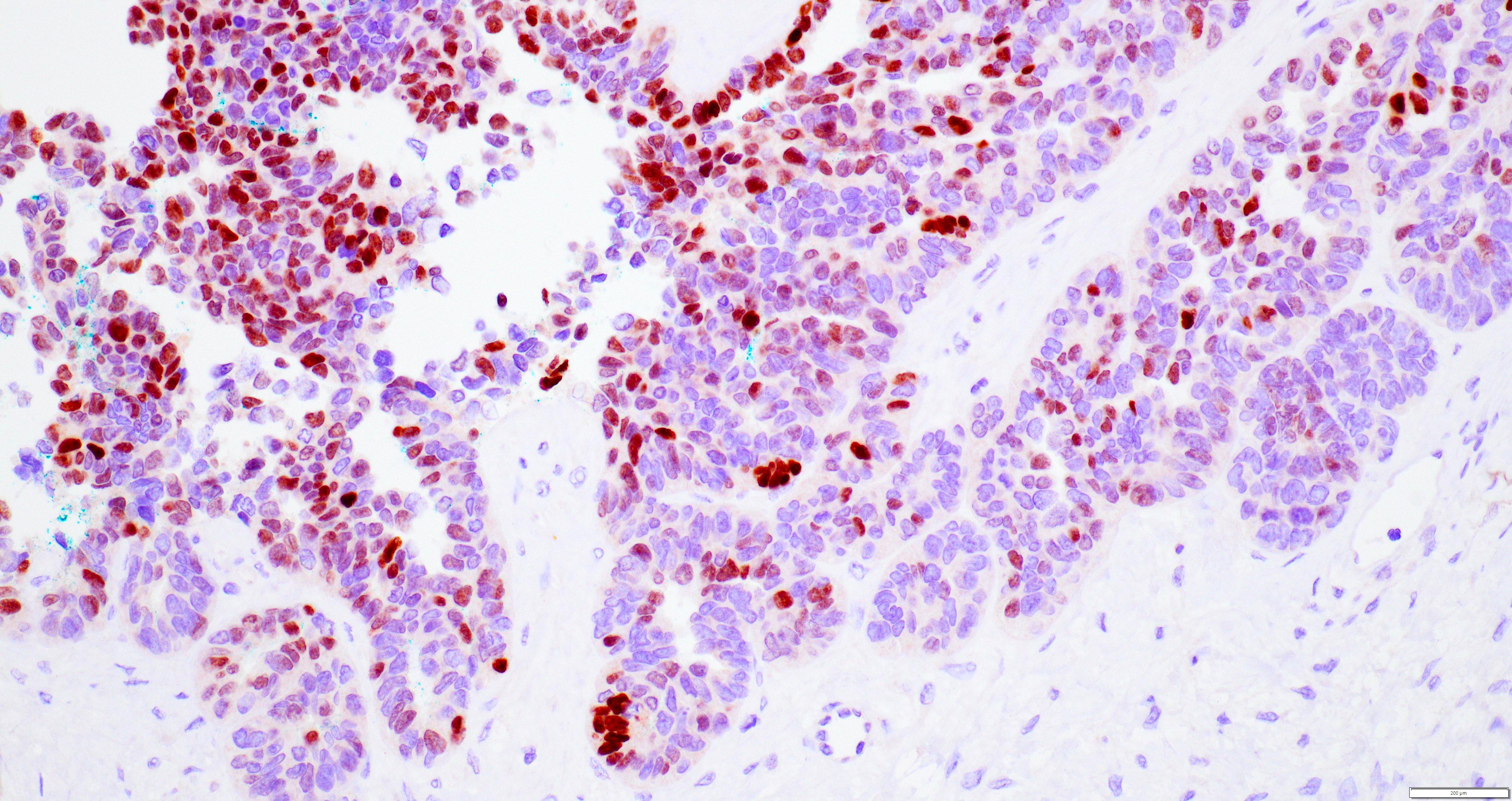
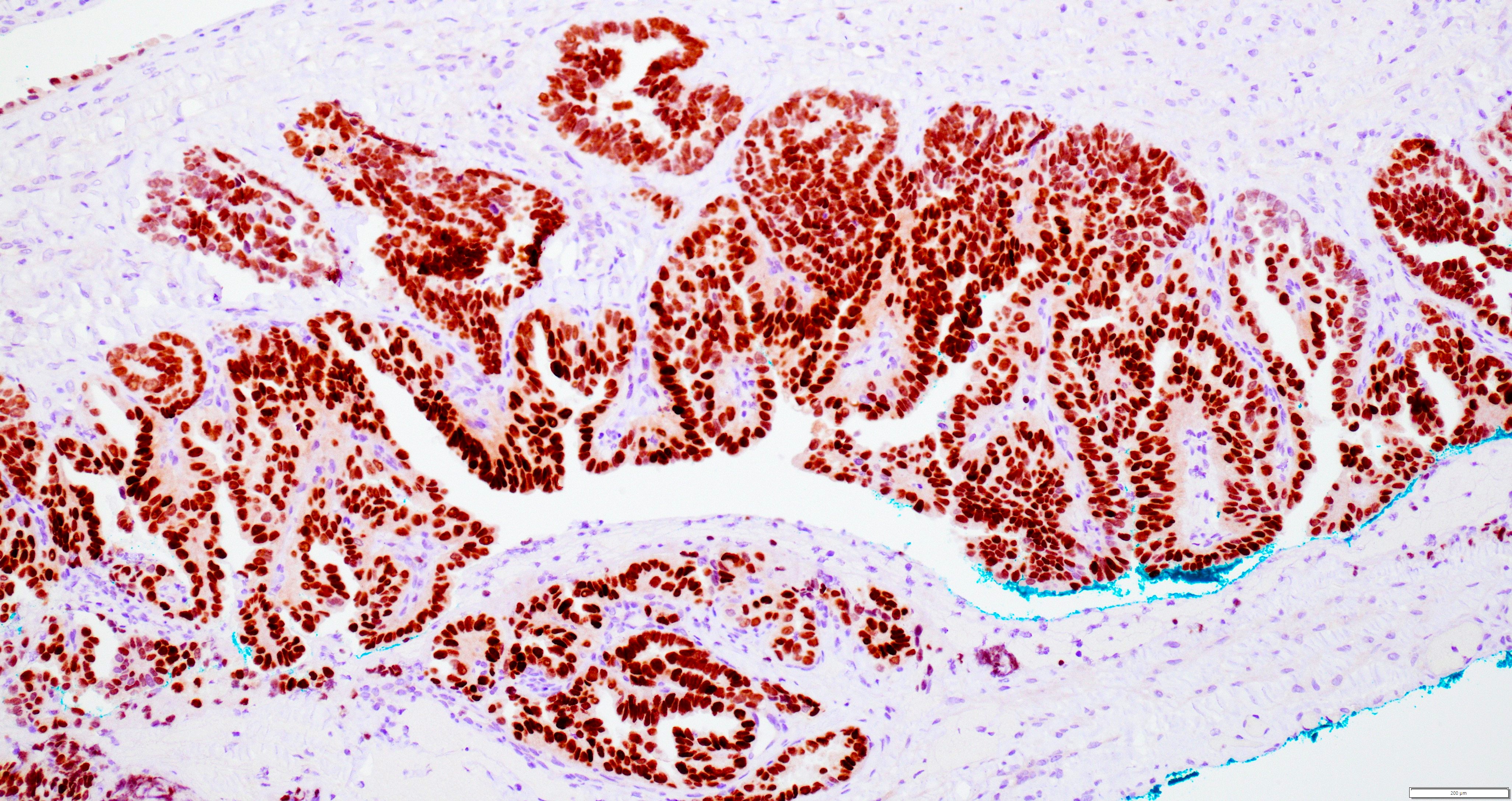
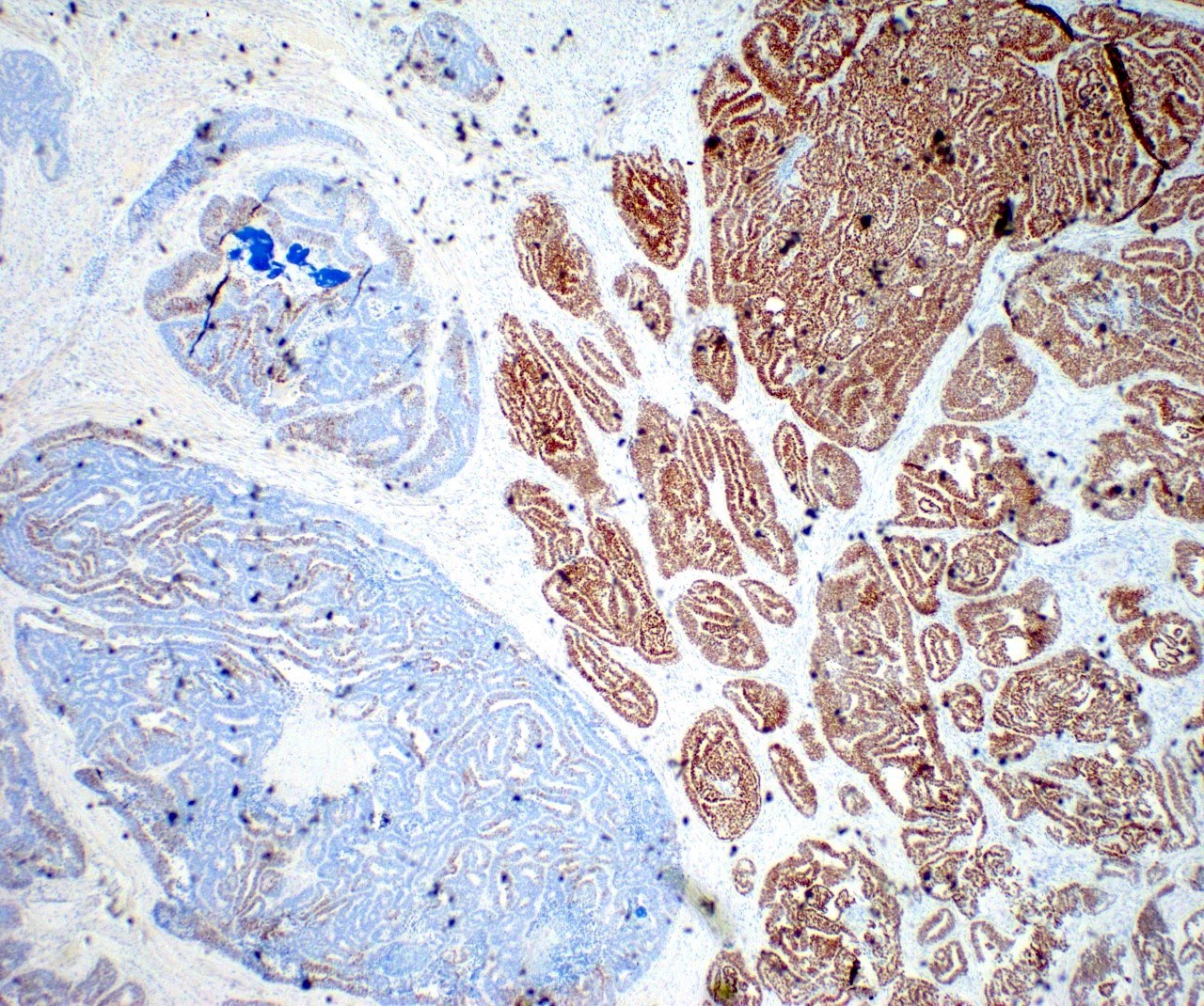
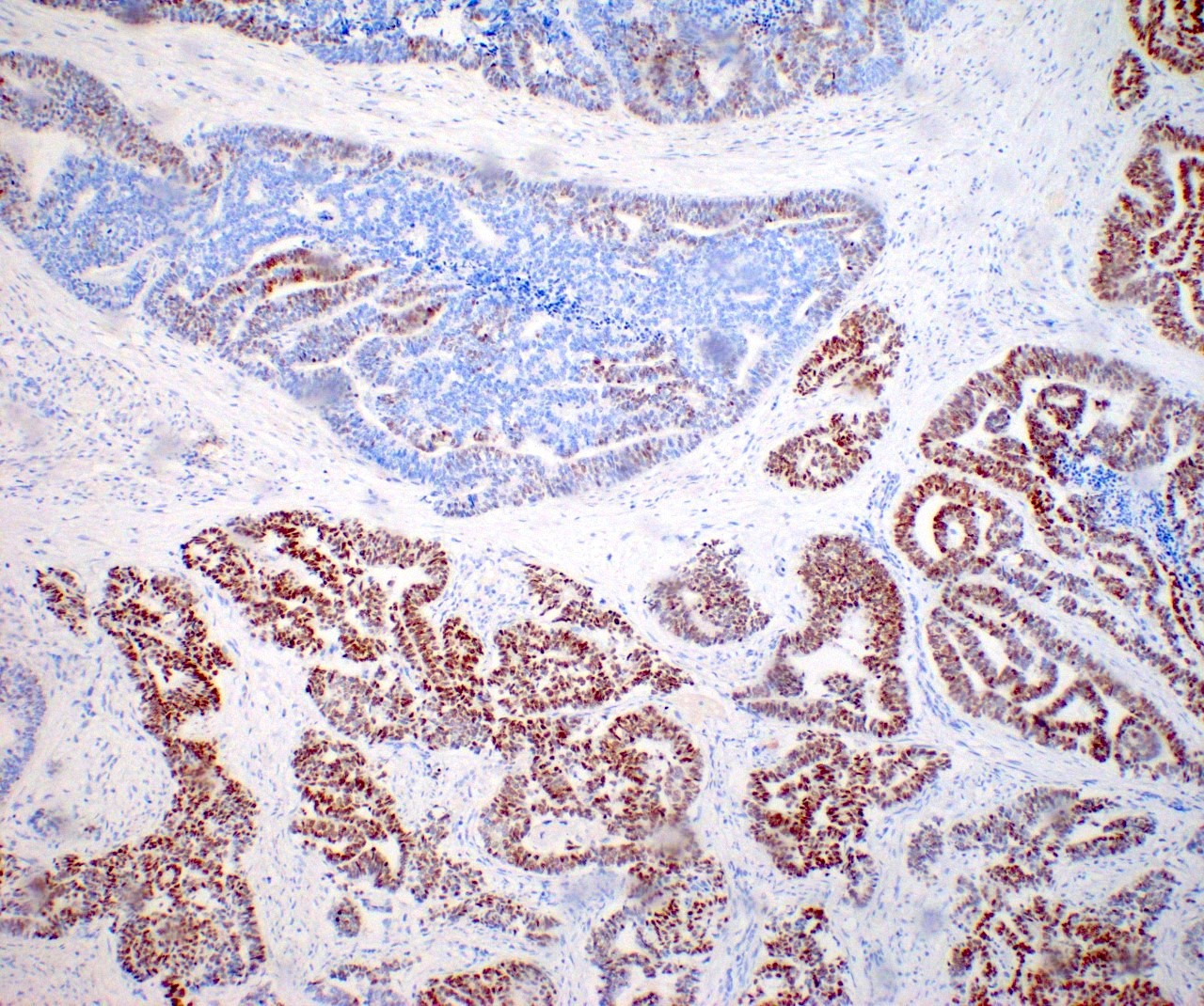
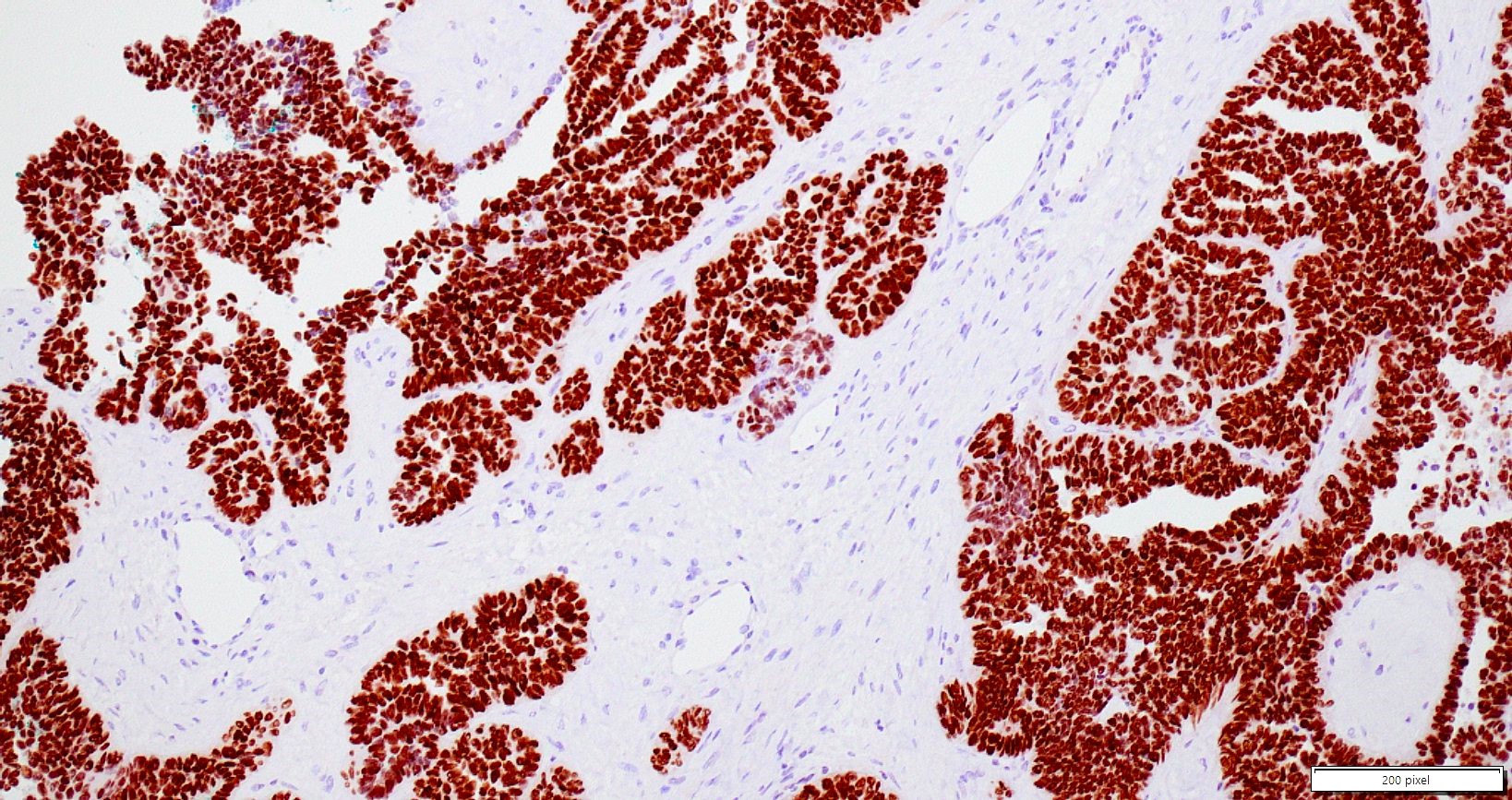
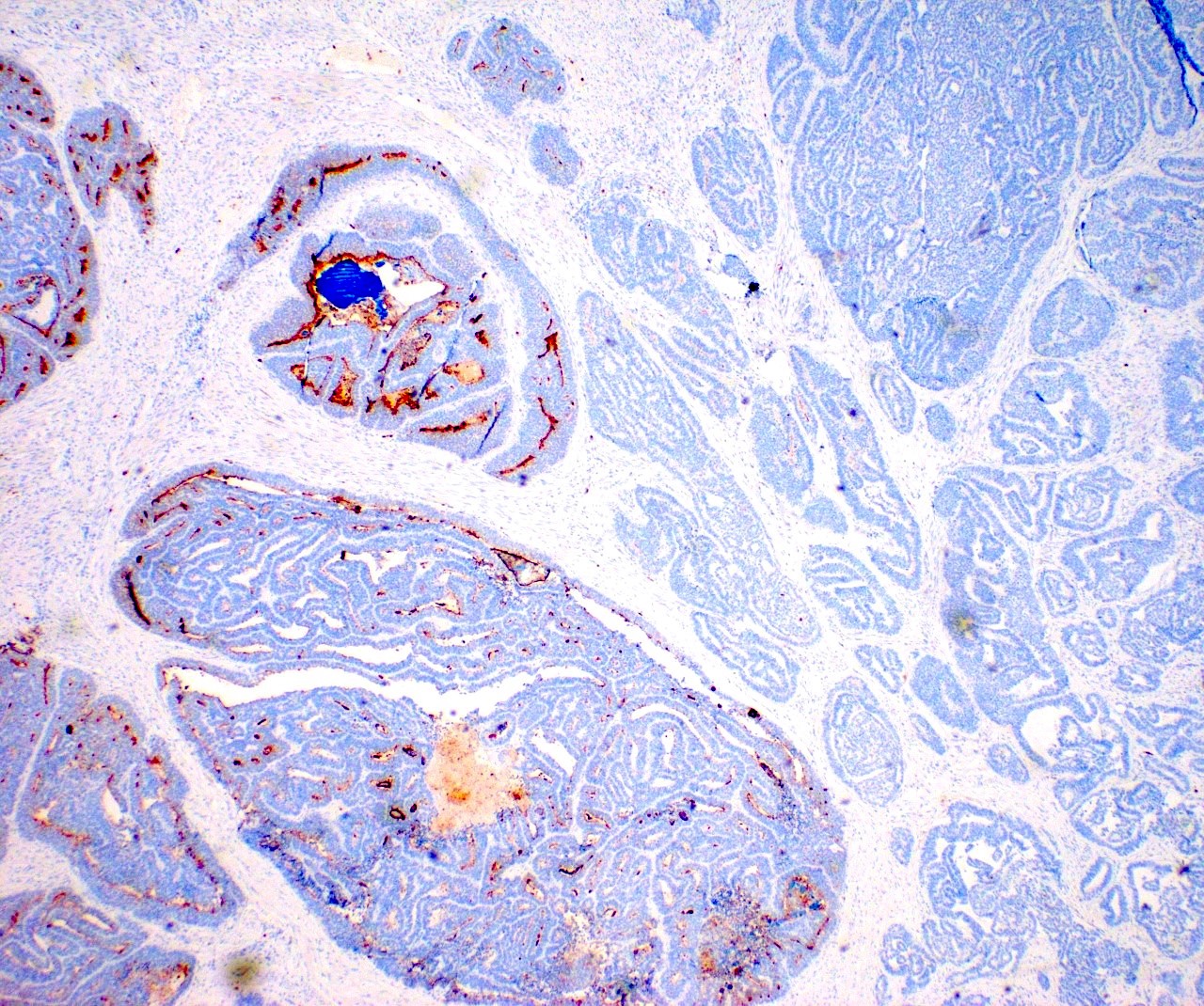
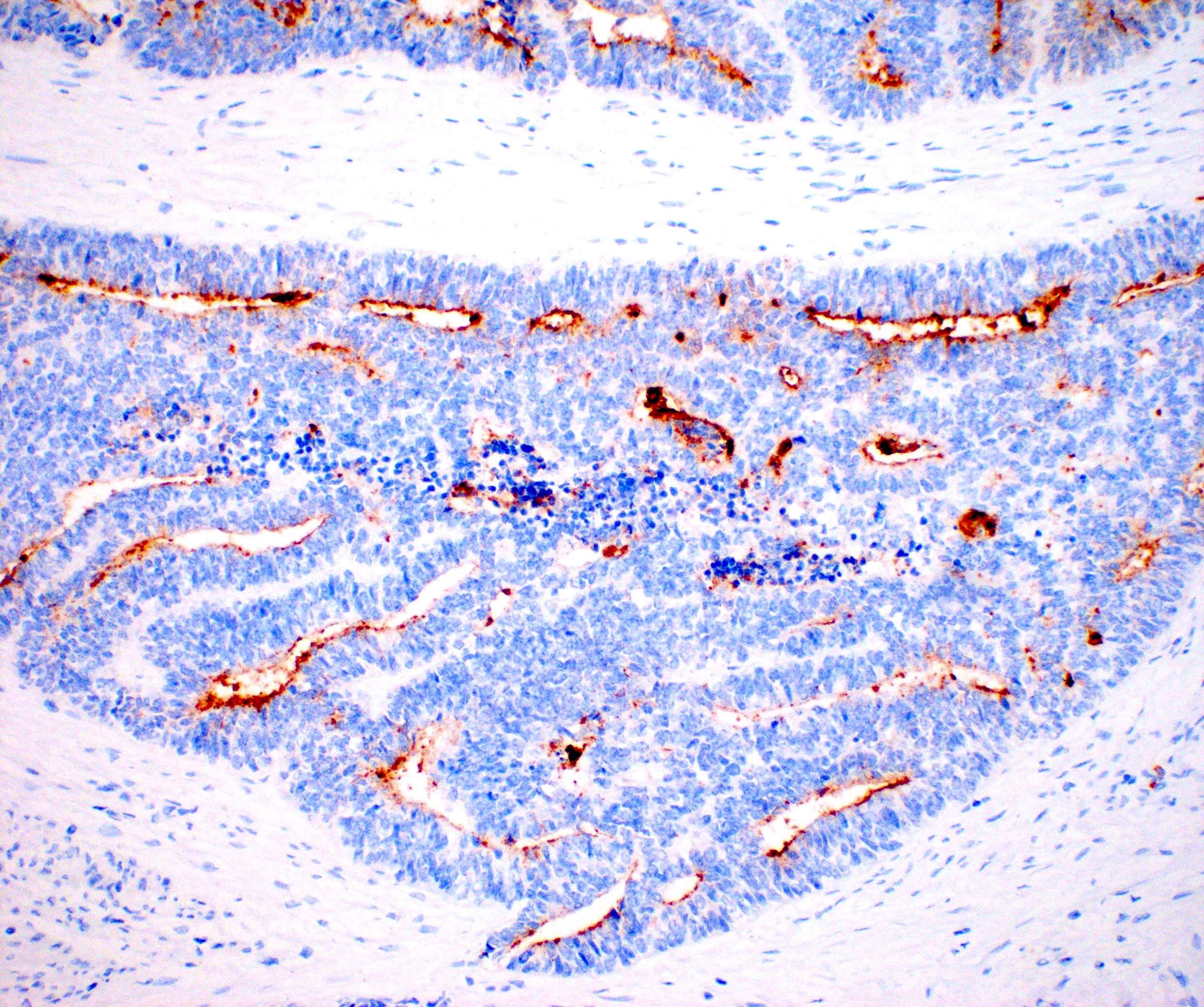
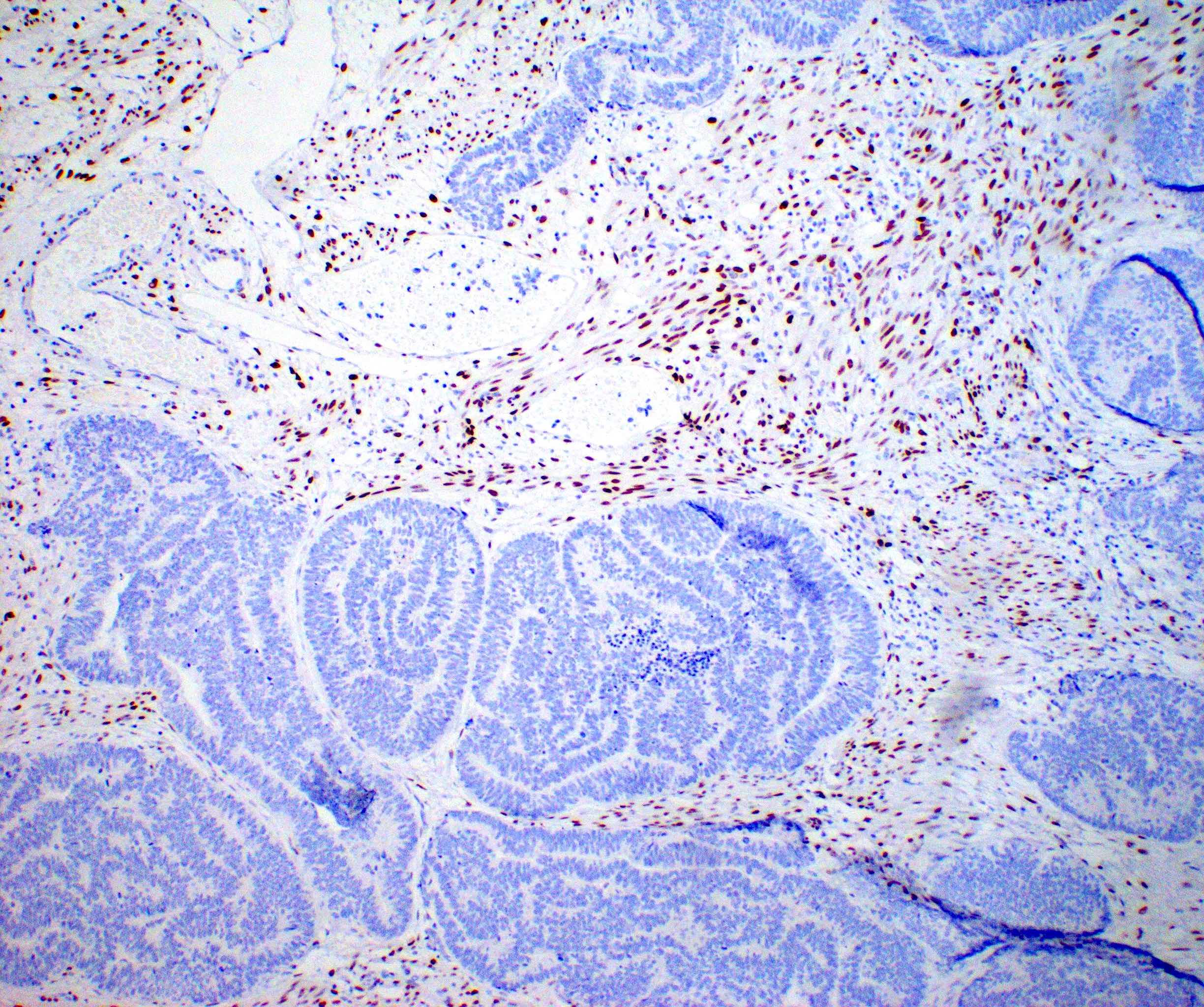
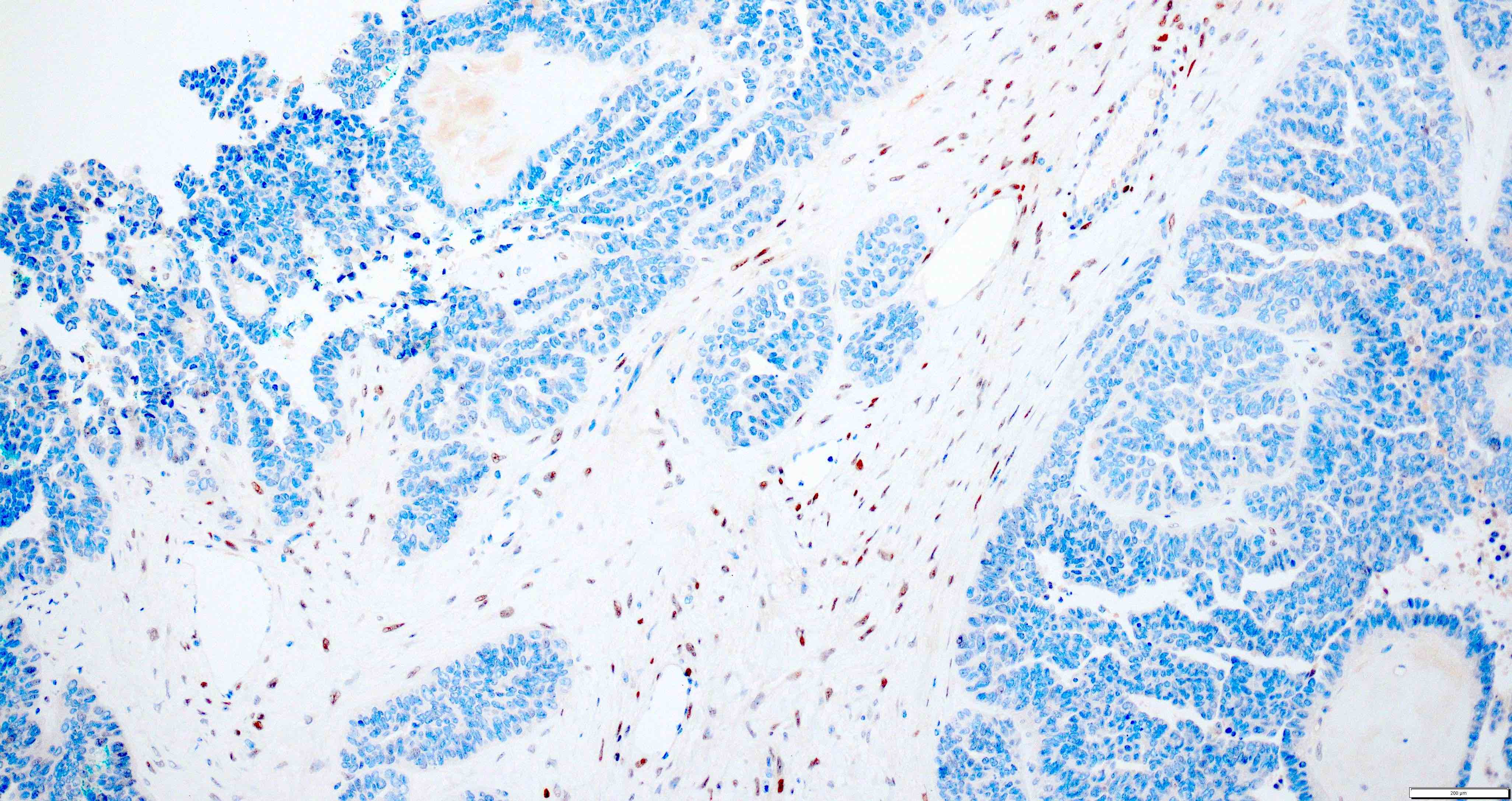
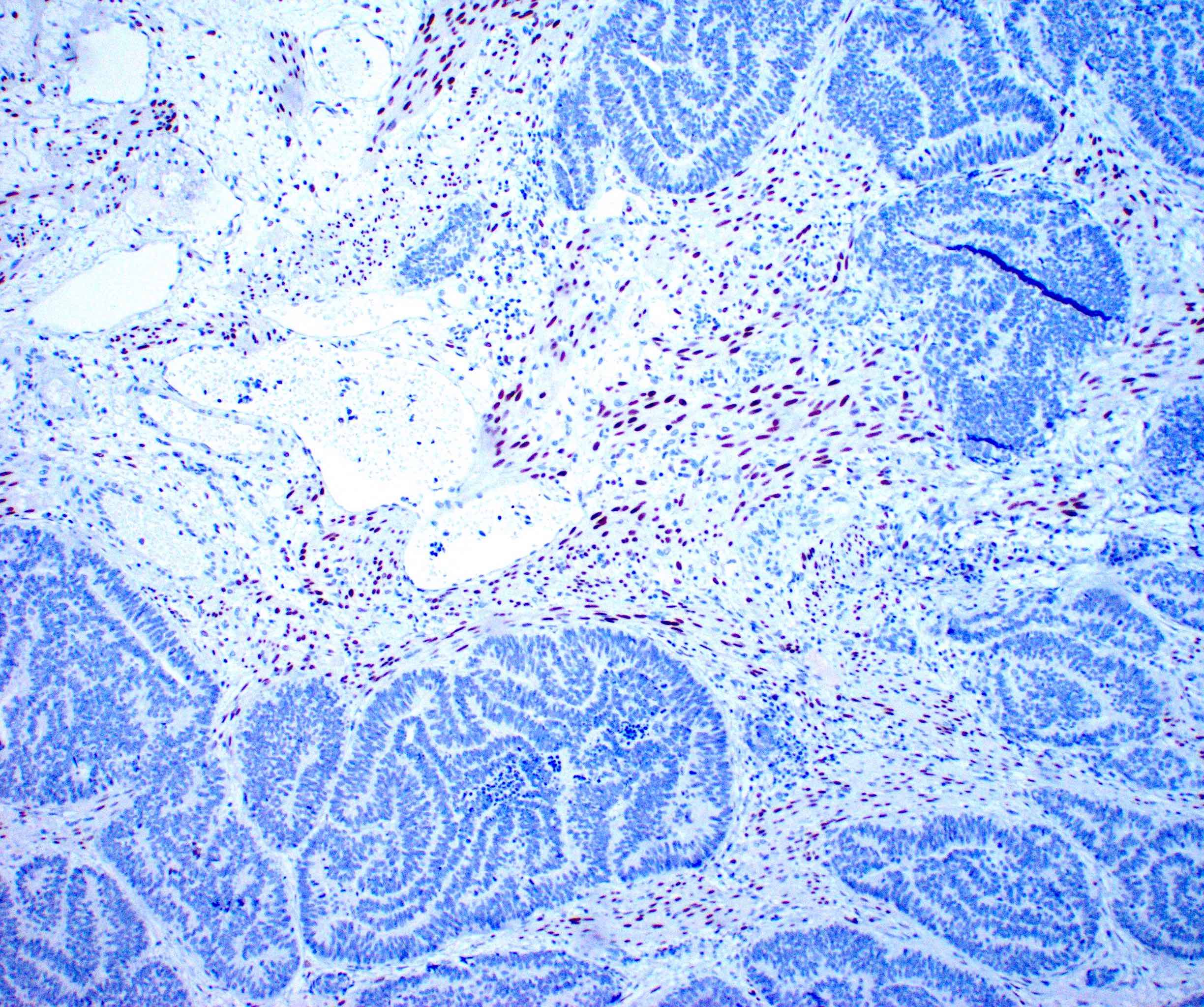
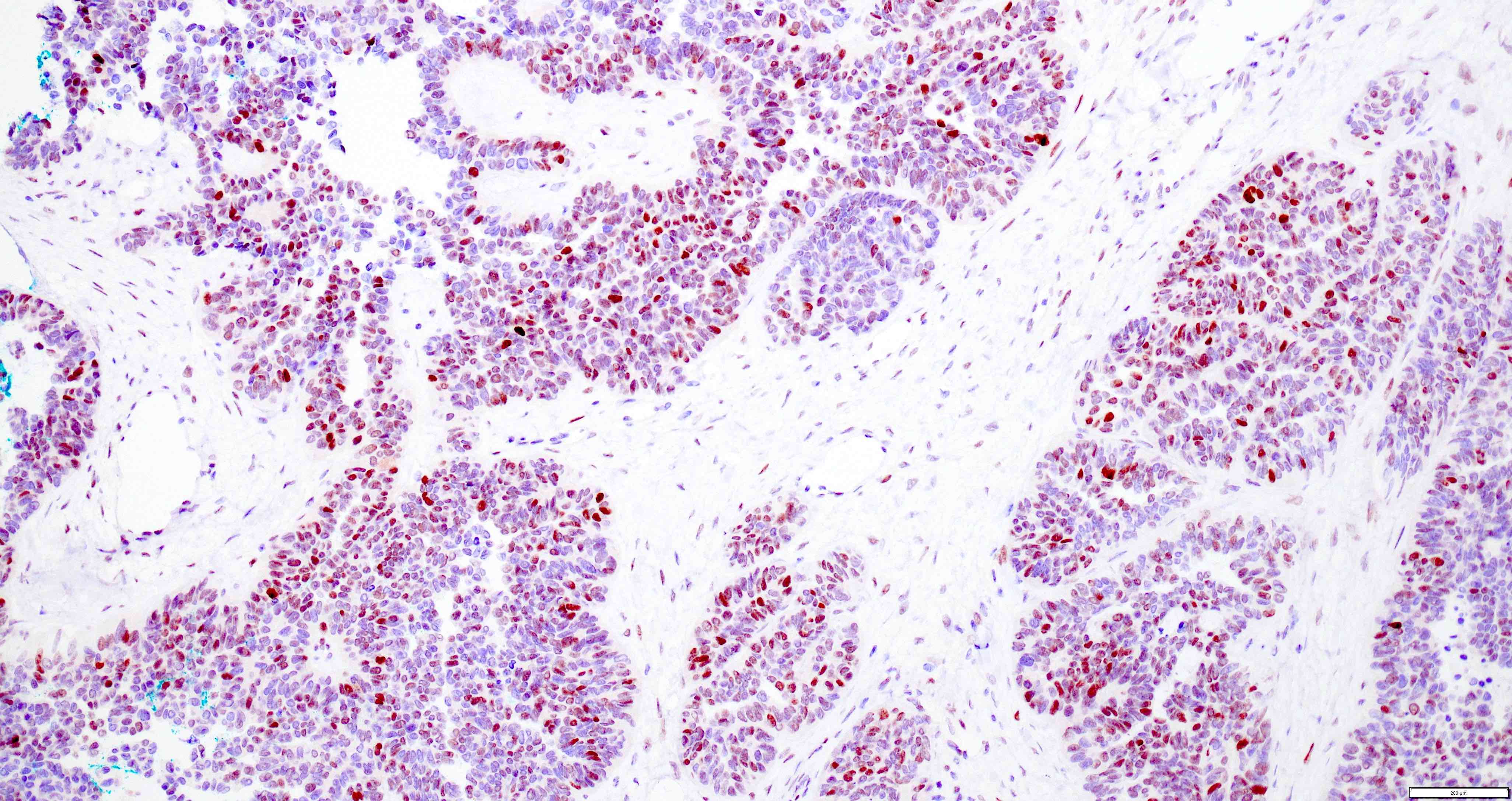
Microscopic (histologic) images
Contributed by Daniel Graham, M.D., Adele Wong, M.B., B.Ch., B.A.O. and Lucy Ma, M.D.
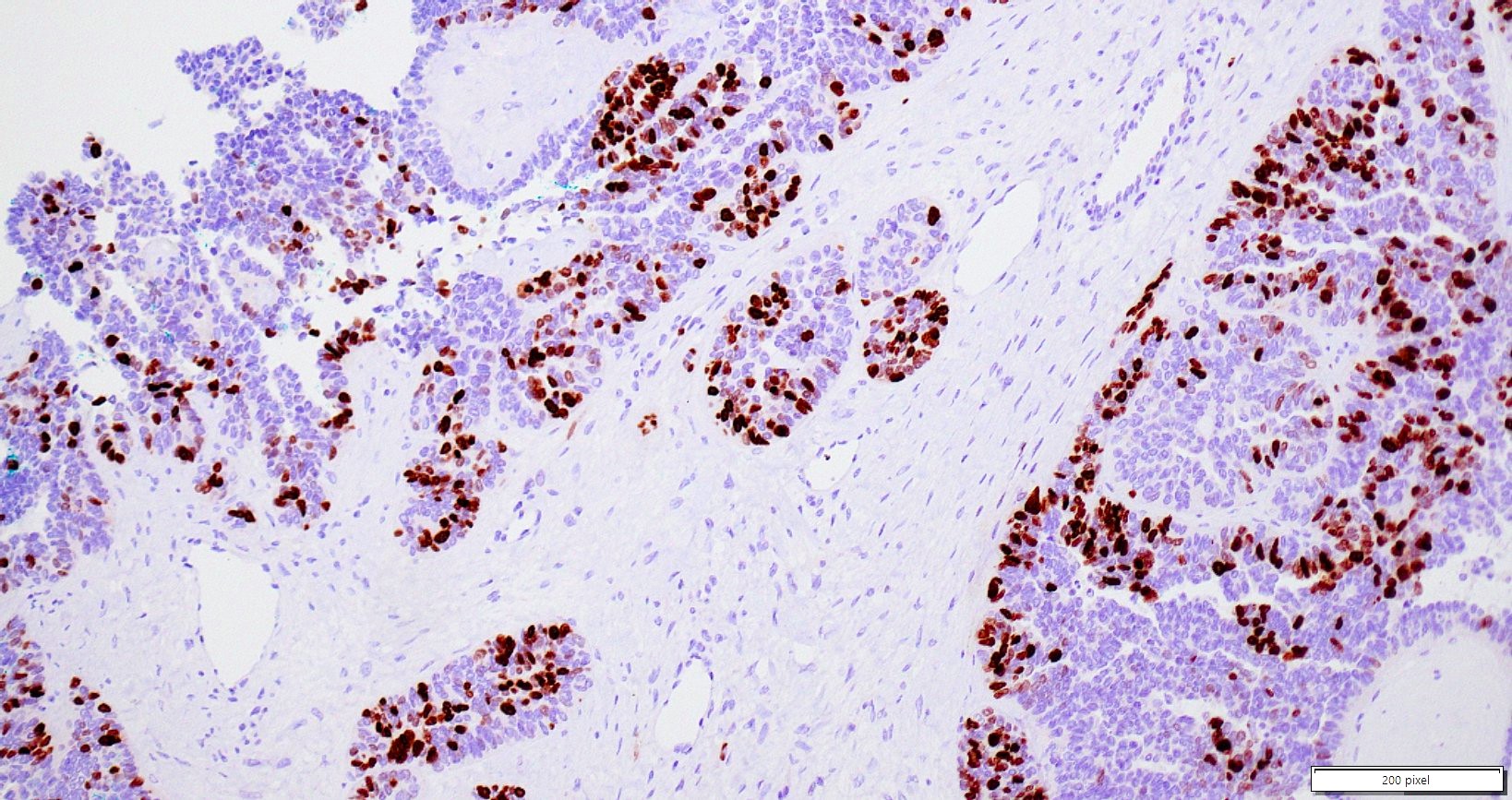
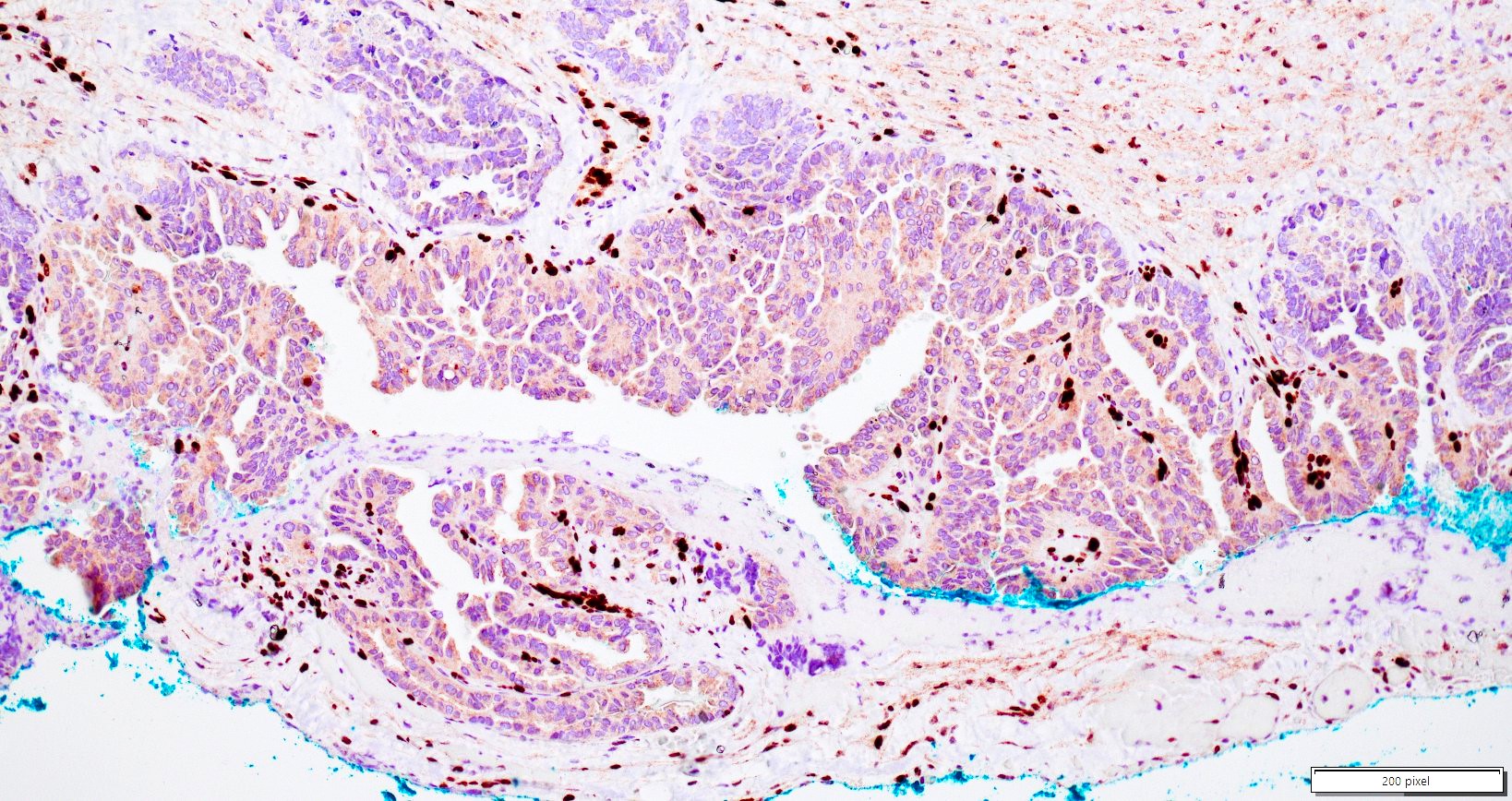
Positive stains
- PAX8: usually diffusely positive
- GATA3 and TTF1: focal or diffuse with inverse staining pattern described in several studies in the most recent WHO classification; cells positive for GATA3 are negative for TTF1 and vice versa (Am J Surg Pathol 2018;42:1596)
- CD10: focal and apical / luminal
- p53 wild type
- MMR proficient
Negative stains
- ER
- PR (more reliable negative marker than ER)
- Calretinin (usually negative may be focally positive)
- Reference: J Clin Med 2021;10:698
Molecular / cytogenetics description
- Majority of MLA shows KRAS mutation, most commonly G12V and G12D (Am J Surg Pathol 2020;44:429)
- Concurrent ARID1A and PIK3CA mutations are quite common
- PTEN mutation has been reported
- CTNNB1 hotspot mutations have been reported
- Copy number analysis: copy number gain of 1q and 10 are the most common, some have 1p loss (Mod Pathol 2021;34:1570)
- Usually does not have the common molecular abnormalities described in endometrioid (p53, MMR and POLE) (Mod Pathol 2021;34:1570)
- NRAS mutations may occur (Int J Gynecol Pathol 2018;37:448)
Videos
Mesonephric-like adenocarcinoma by Dr. Lewis Hassell
Sample pathology report
- Uterus and cervix, bilateral fallopian tubes and ovaries, total hysterectomy and bilateral salpingo-oophorectomy:
- Endometrial adenocarcinoma, most consistent with mesonephric-like adenocarcinoma (see comment)
- Comment: The tumor exhibits various growth patterns including small tubular, glandular and papillary areas. Tumor cells show diffuse immunoreactivity for PAX8 and focal immunoreactivity for GATA3 and TTF1. Despite the predominant glandular architecture and low grade appearance, the tumor is negative for ER and PR. The cervix is benign and mesonephric remnants are not identified. All these findings are most consistent with endometrial adenocarcinoma, mesonephric-like subtype.
Differential diagnosis
- Low grade endometrioid adenocarcinoma:
- ER and PR positive
- Small tubules with eosinophilic material are not commonly seen
- Lacks the heterogeneity of architectural patterns seen in MLA
- Squamous, ciliated or mucinous differentiation are not seen in MLA
- GATA3 or TTF1 expression are usually negative
- GATA3 expression can be seen in a 6% of endometrial carcinomas including endometrioid type but these cases were always TTF1 negative (Am J Surg Pathol 2015;39:1411)
- Clear cell carcinoma:
- May show variable architectural patterns and cytological atypia
- Positive HNF-1B, napsin A or alpha methyacyl CoA racemase (AMACR)
- Napsin A and HNF-1B usually negative in MLA but can be positive (Int J Gynecol Pathol 2022;41:161)
- Abnormal p53 and MMR can be seen in clear cell carcinoma, in contrast to MLA
- GATA3 and TTF1 are usually negative
- Serous carcinoma:
- Carcinosarcoma:
- Solid areas and spindled cell and sarcomatoid features
- Abnormal p53 expression
- Absence of KRAS mutations (Cancer Genomics Proteomics 2022;19:747)
- Primary lung adenocarcinoma in metastatic setting:
- Cervical mesonephric adenocarcinoma with the involvement of the uterine corpus:
Additional references
Practice question #1
A 55 year old woman was recently diagnosed with endometrioid intraepithelial neoplasia on endometrial curettage. The entire endometrium is submitted for histologic evaluation. Histologic details from one section are shown in the image above. The tumor cells are diffusely positive for GATA3 and PAX8 and focally positive for TTF1. ER and PR are negative. Which of the following statements is true regarding this entity?
- KRAS mutations, particularly G12V and G12D, are commonly identified
- MMR deficiency is present in half of the cases
- The tumor frequently shows p53 overexpression
- The tumor has better prognosis compared to low grade endometrioid adenocarcinoma
Practice answer #1
A. KRAS mutations, particularly G12V and G12D, are commonly identified. Despite the low grade morphology commonly encountered in mesonephric-like adenocarcinoma, the tumor has worse prognosis compared to low grade endometrioid adenocarcinoma. They do not show abnormal p53 expression and are usually MMR proficient. KRAS mutations are commonly seen, with G12V and G12D being the most common alterations identified.
Comment Here
Reference: Mesonephric-like adenocarcinoma
Comment Here
Reference: Mesonephric-like adenocarcinoma
Practice question #2
Which of the following statements is true regarding mesonephric-like adenocarcinoma occurring in the uterus?
- The tumor commonly expresses GATA3 and TTF1 immunohistochemically
- The tumor expresses hormone receptors similar to those seen in conventional endometrioid carcinoma
- The tumor is most often seen in the myometrium without a surface connection to the endometrium
- The tumor often shows DNA polymerase epsilon (POLE) mutation
Practice answer #2
A. The tumor commonly expresses GATA3 and TTF1 immunohistochemically. The finding of a hormone receptor negative, PAX8, GATA3 and TTF1 positive tumor is highly supportive of the diagnosis of mesonephric-like adenocarcinoma. While mesonephric remnants and mesonephric derived tumors are often found in paracervical or adnexal locations, this is not true of the mesonephric-like tumors in the endometrium, which have a surface component in virtually all cases. Most such tumors are of no specific molecular type.
Comment Here
Reference: Mesonephric-like adenocarcinoma
Comment Here
Reference: Mesonephric-like adenocarcinoma