Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Parakh R, Tretiakova M. Intestinal metaplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderintestinalmetaplasia.html. Accessed May 13th, 2024.
Definition / general
- Replacement of urothelium by benign colonic or small intestinal epithelium, with presence of mucin producing goblet cells
Essential features
- Intestinal or colonic metaplasia: glandular epithelium with mucin secreting goblet cells (single or aggregates) replacing surface mucosa and von Brunn nests
- May coexist with cystitis glandularis, characterized by formation of glandular structures in lamina propria within von Brunn nests that have an innermost lining of columnar or cuboidal cells bound by transitional cells at periphery
Terminology
- Also called glandular metaplasia, colonic metaplasia or goblet cell metaplasia
Epidemiology
- Identified in 71 - 90% of bladders at autopsy (Acta Pathol Jpn 1981;31:545)
- Incidence increases with age; mean age of diagnosis 57 years (range 23 - 81 years)
Sites
- Lamina propria of trigone is most affected (Mod Pathol 2006;19:1395)
- Also seen in ureter and renal pelvis
- Mostly focal process but occasionally diffuse
Pathophysiology
- Metaplastic reactive alteration induced by chronic inflammation or irritation
Etiology
- Variation of normal histology
- Chronic inflammation, ureteral reimplantation, neurogenic bladder, bladder exstrophy, paraplegia, stones, long term catheterization (J Urol 1981;126:822, J Urol 1970;104:699)
Clinical features
- Incidental finding
- Hematuria, dysuria, urgency or obstructive symptoms
- Rare cases may form mass lesion (< 1 cm) with mucin extravasation; may be confused cystoscopically with neoplastic process or malignancy (Am J Surg Pathol 1996;20:1462)
Diagnosis
- Cystoscopy finding of irregular or minimally elevated mucosa in a symptomatic patient
- Microscopic findings of intestinal type epithelium with goblet cells replacing urothelium
Prognostic factors
- Long term follow up of intestinal metaplasia has confirmed a benign behavior (Urology 2008;71:915, Urology 1997;50:427)
- If associated with dysplastic changes, considered as a harbinger of adenocarcinoma; close follow up is warranted (Clin Cancer Res 2007;13:6232)
- If the lesion is extensive on initial transurethral resection, it is prudent to suggest area to be re-resected
Case reports
- 20 year old man with adenocarcinoma arising in residual native bladder in association with intestinal metaplasia and dysplasia of bladder mucosa, 17 years following gastrocystoplasty (J Pediatr Urol 2010;6:525)
- 49 year old man with hematuria and radiologic abnormalities with no visible lesions (J Surg Case Rep 2018;2018:rjy193)
- 60 year old man with spina bifida with bladder adenocarcinoma arising in intestinal metaplasia (Ann Diagn Pathol 2007;11:453)
Treatment
- May regress completely if pathogenic factor is removed
- Frequent monitoring if symptoms persist or if associated with dysplasia
Gross description
- Irregular, rounded focal elevations of mucosa
- Rarely polypoidal with mucinous extravasations (Am J Surg Pathol 1996;20:1462)
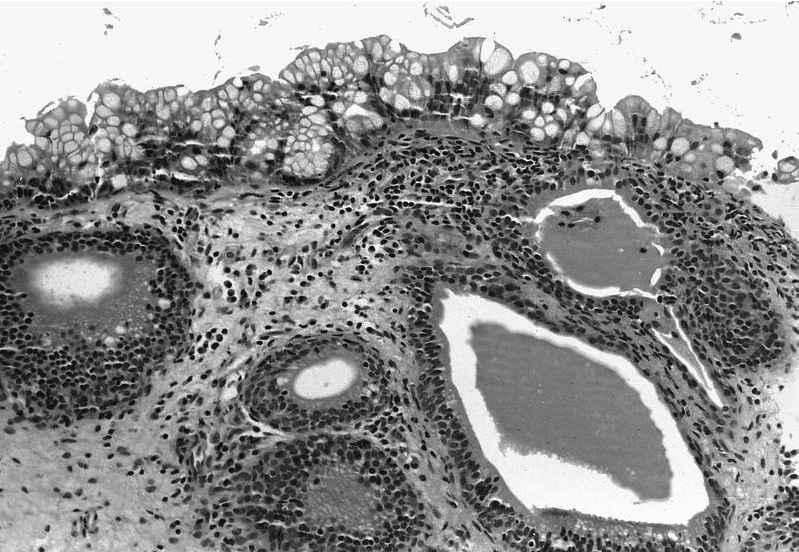
Microscopic (histologic) description
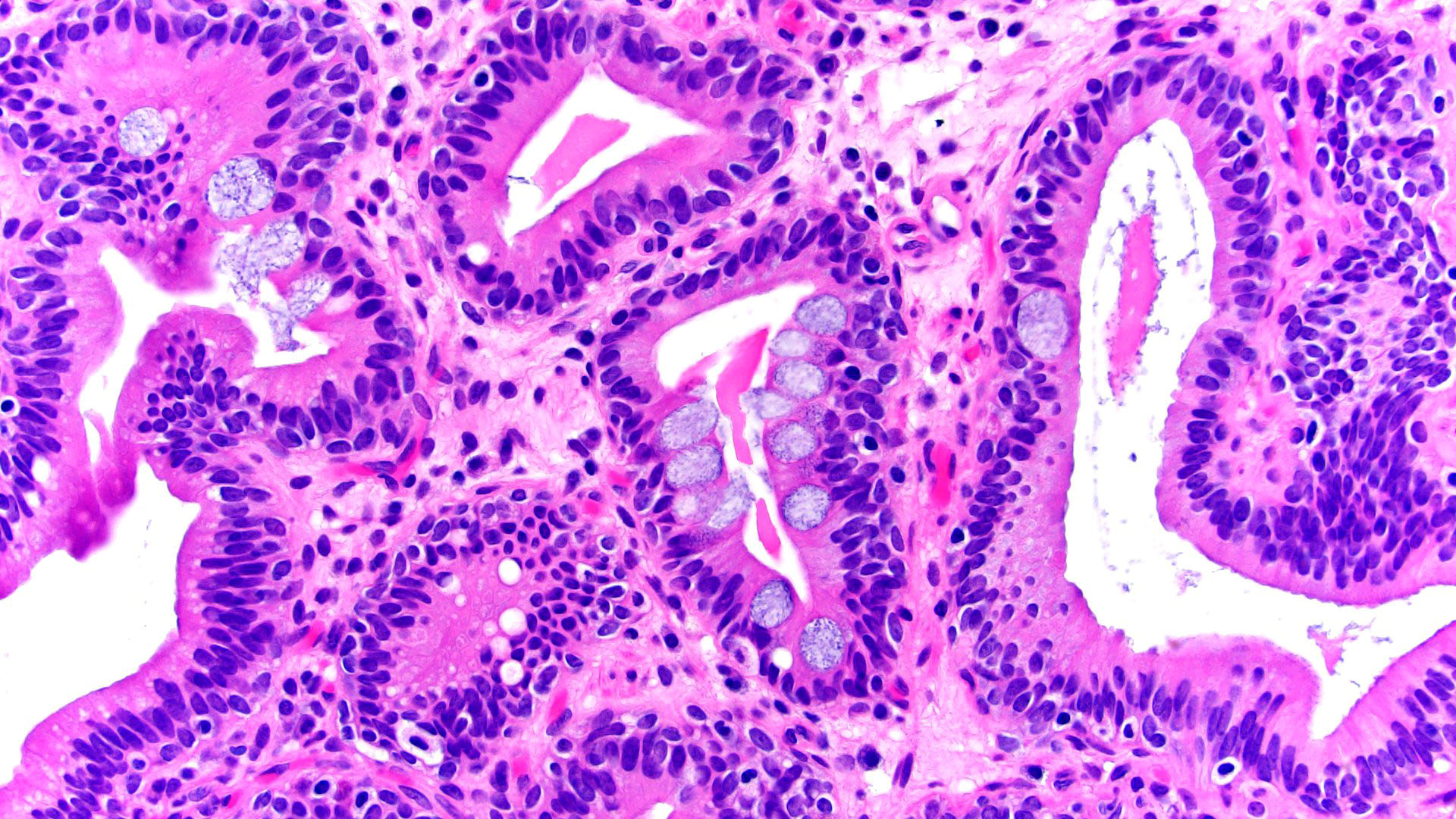
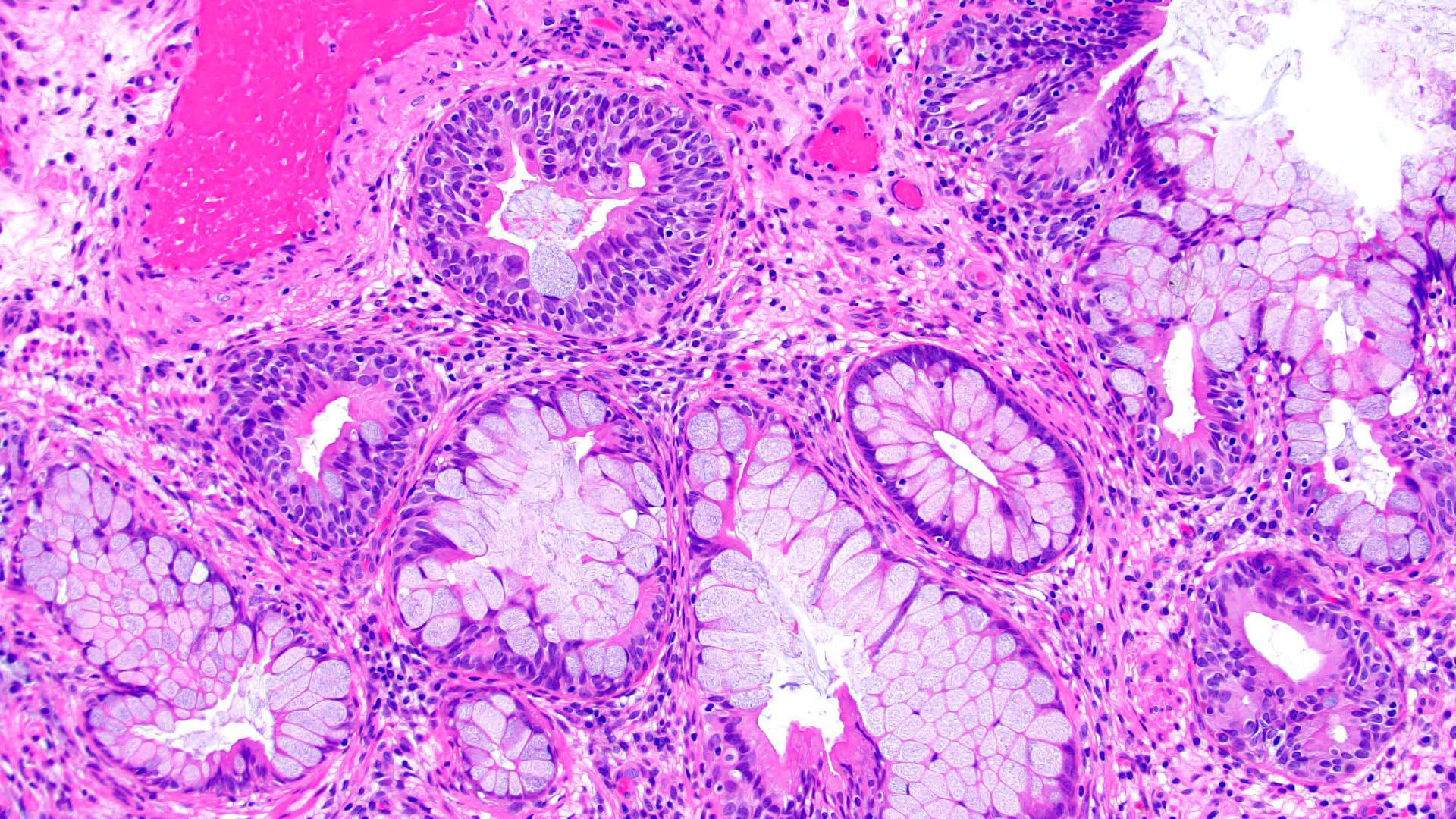
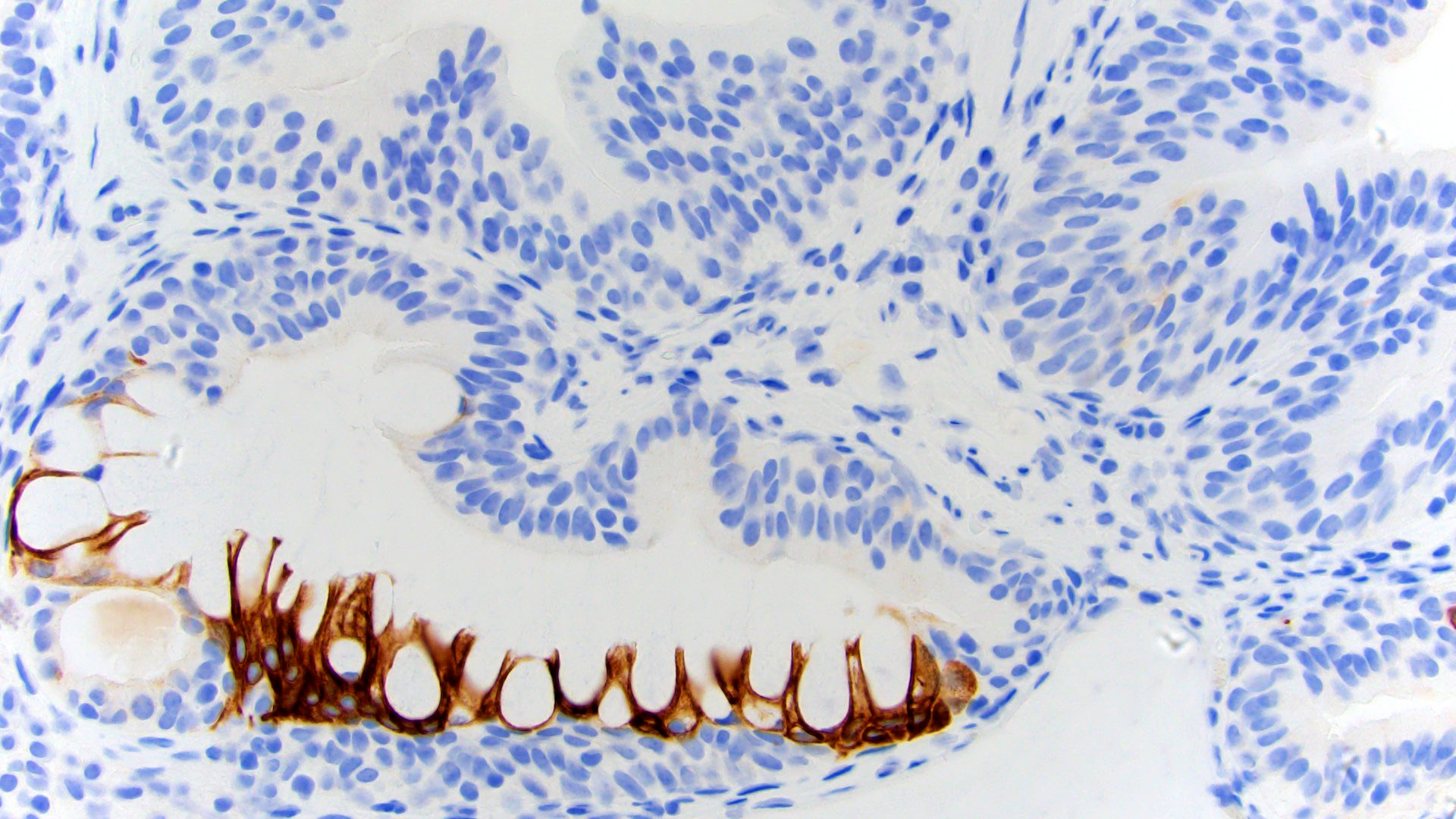
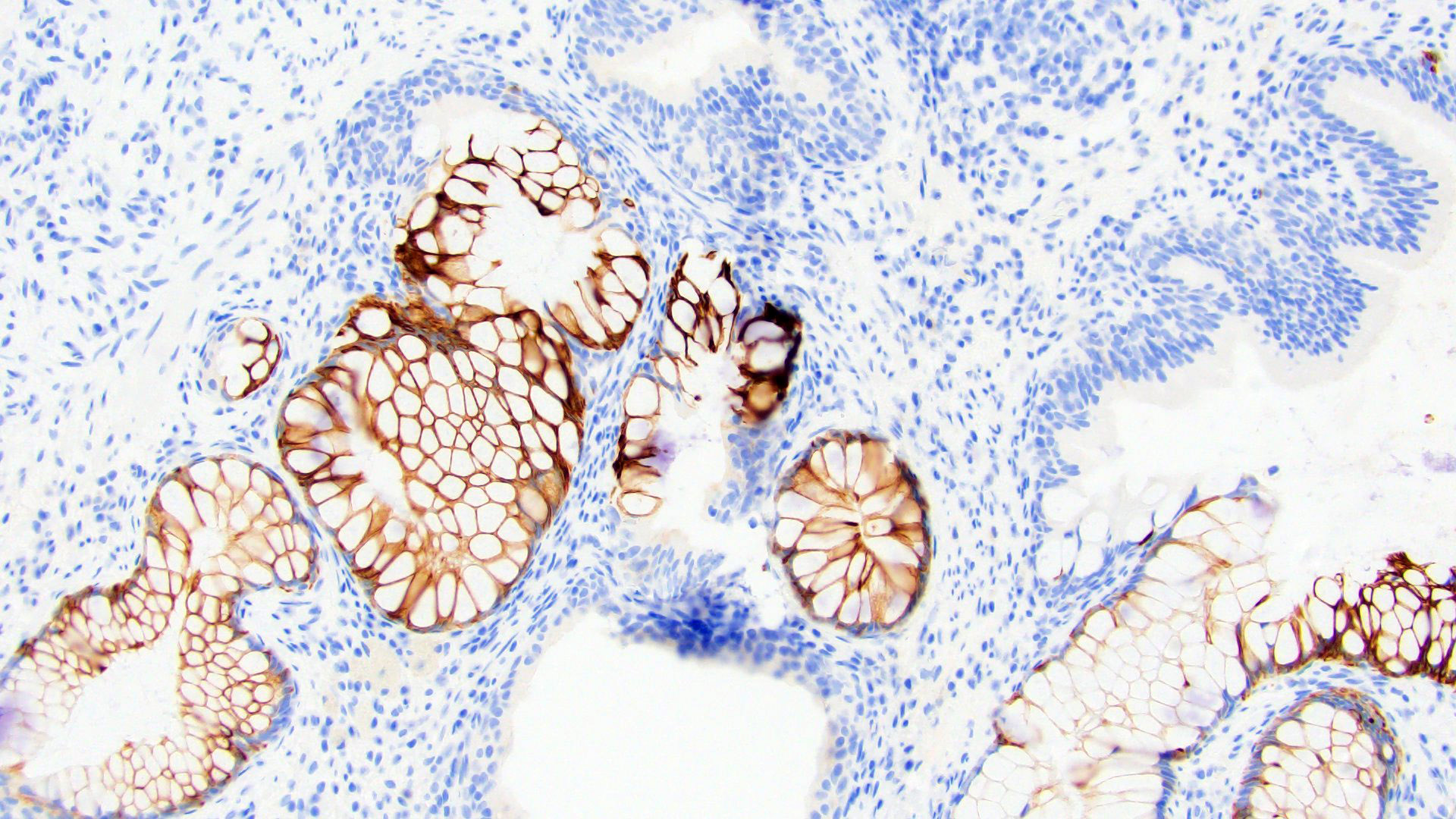
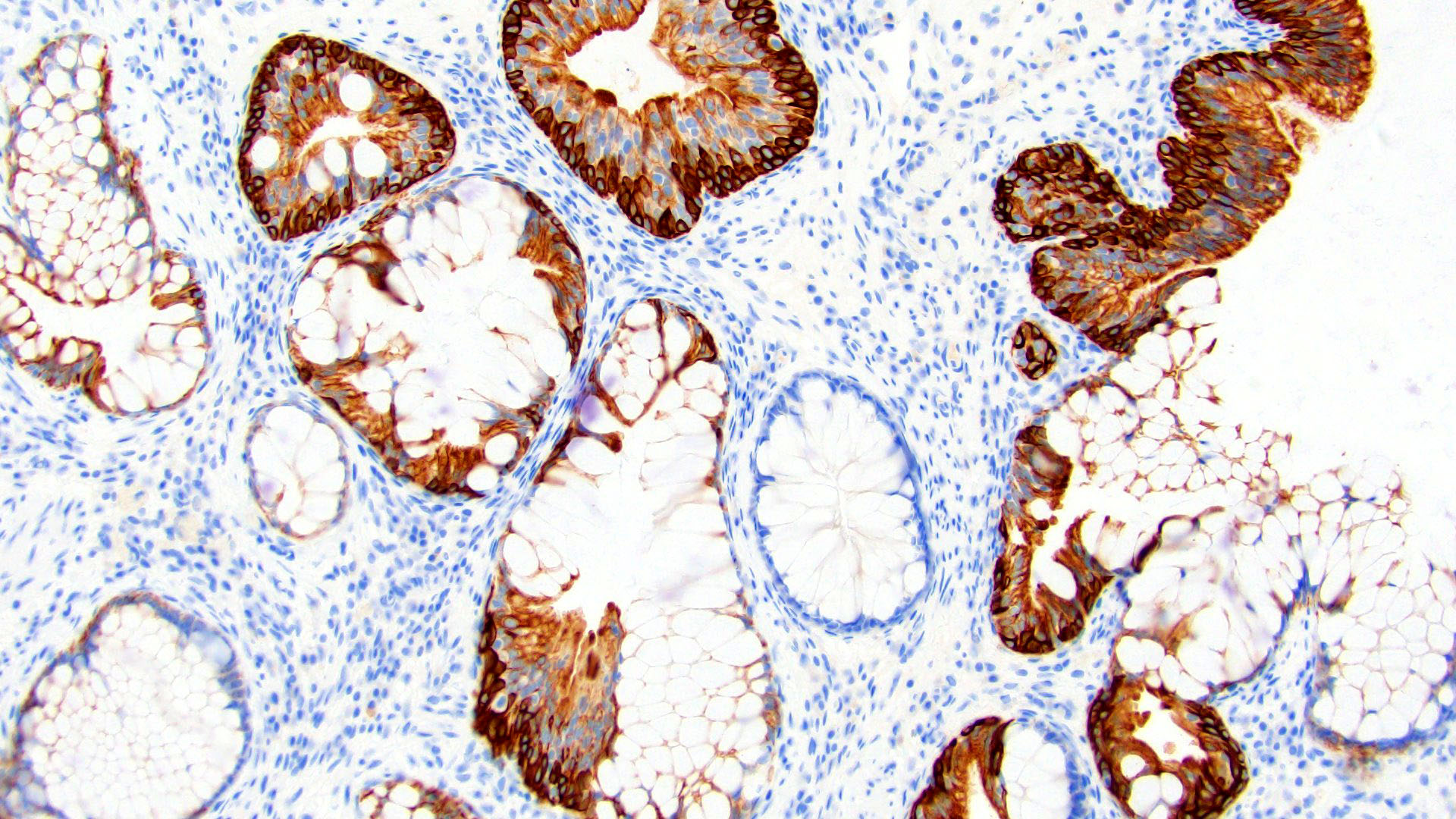
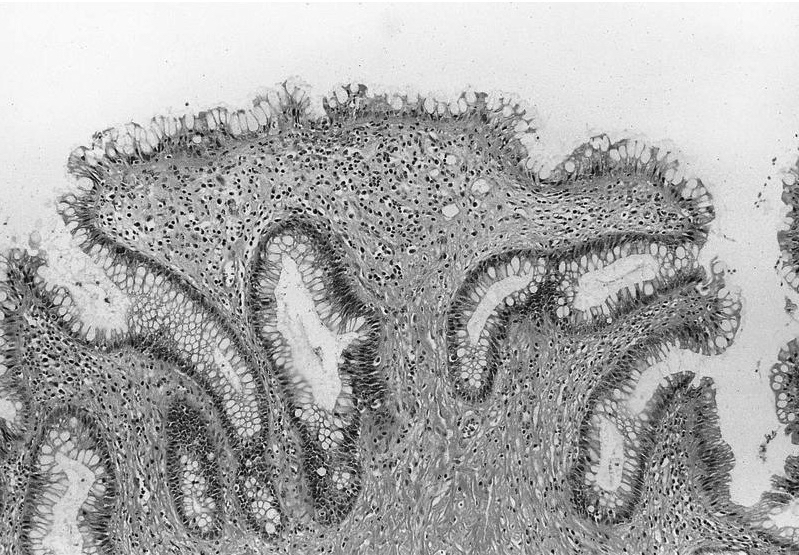
- Replacement of urothelium by tall columnar cells
- Presence of goblet cells (single or aggregates) within von Brunn nests; variable presence of Paneth cells (small, intestine-like) or neuroendocrine cells (rare) (Mod Pathol 2006;19:1395)
- May coexist with cystitis cystica or cystitis glandularis
- Mucin may be occasionally extravasated into the stroma
- No atypia, confined to the lamina propria, no involvement of muscularis propria
Microscopic (histologic) images
Cytology description
- Urine specimen: glandular epithelium with mucin secreting goblet cells
- Bland cytologic features
- No mitoses (Diagn Cytopathol 2008;36:181)
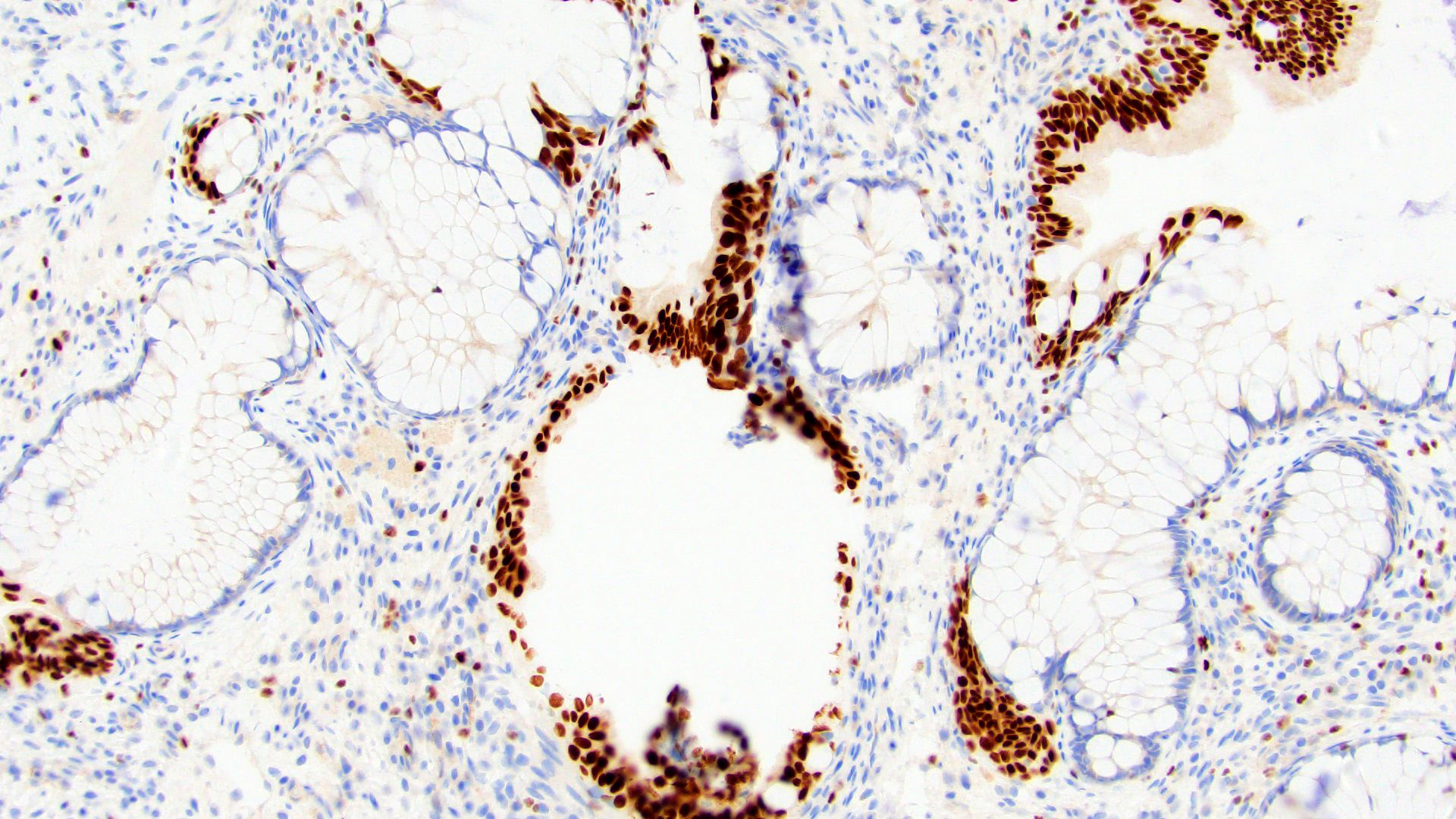
Positive stains
- Mucin stains have variable positivity
- CDX2 nuclear (83%), CK20 (Mod Pathol 2006;19:1395)
- Neuroendocrine markers in neuroendocrine cells (Histopathology 1990;16:365)
- Nuclear beta catenin
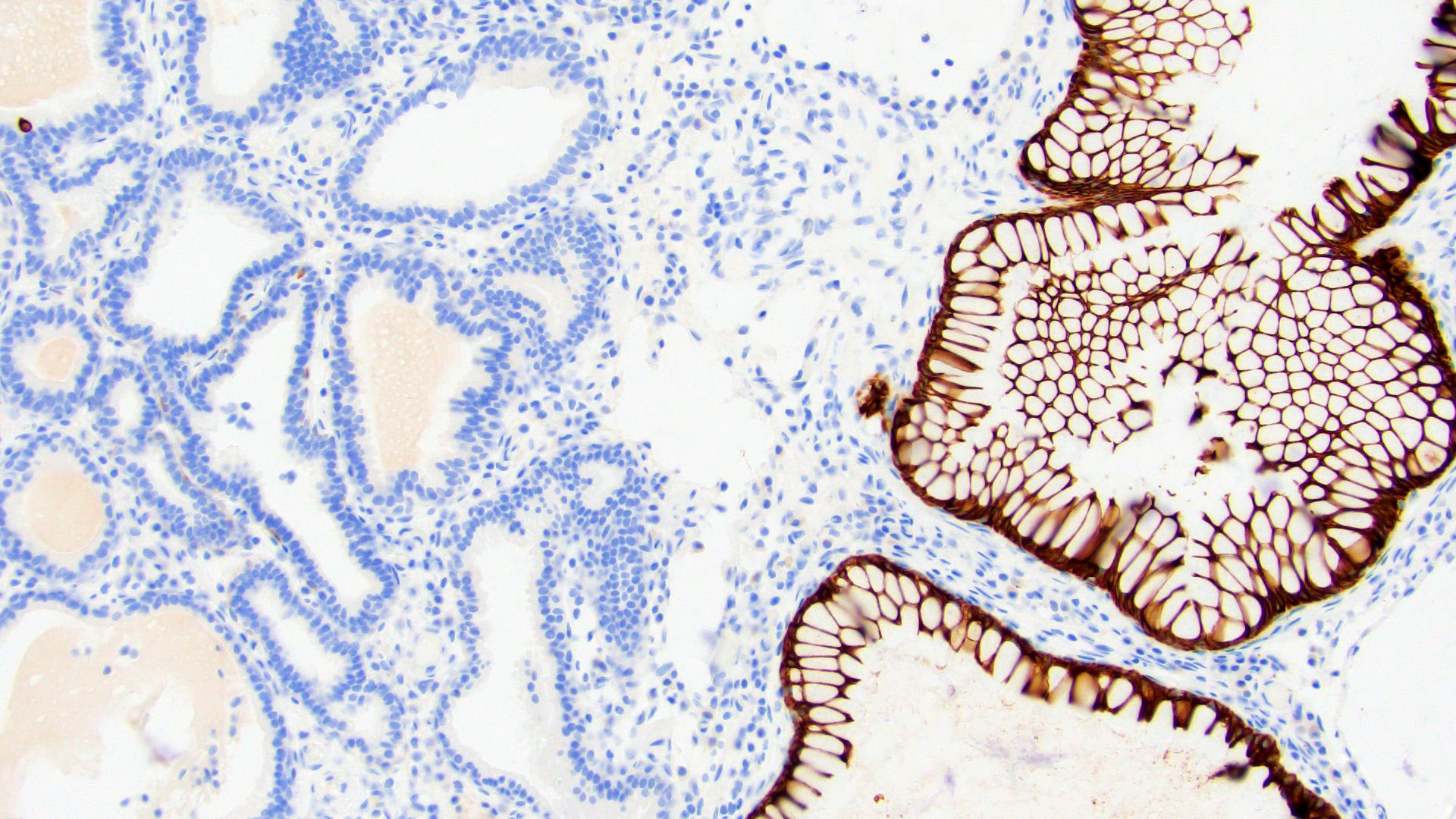
Negative stains
- CK7 (usually), HepPar1 (100%)
- GATA3, HMWCK
- Note: in the urinary bladder, intestinal metaplasia and typical cystitis glandularis have sharply contrasting immunoprofiles despite similar morphology (Mod Pathol 2006;19:1395)
Electron microscopy description
- Cystitis cystica:
- Lining cells: short microvilli on luminal surface (J Urol 1987;137:764)
- Taller cells: numerous membrane bound electron dense secretory granules (Br J Urol 1993;71:28)
- Not needed for routine diagnostic purposes
Molecular / cytogenetics description
- Associated with significant telomere shortening and cytogenetic abnormalities (Clin Cancer Res 2007;13:6232)
Sample pathology report
- Bladder, biopsy:
- Bladder mucosa with intestinal metaplasia (see comment)
- Comment: No evidence of dysplasia or malignancy in submitted tissue.
Differential diagnosis
- Neobladder derived from intestine (normal epithelium):
- Clinical history, villous atrophy, reactive atypia, lymphoid aggregates
- Mucinous cystadenoma:
- Mass lesion with orderly arrangement of the glands, lack of atypia, absence of invasion
- Villous adenoma:
- Central fibrovascular cores lined by pseudostratified columnar epithelium, stratification, crowding; rule out dysplastic changes
- Endometriosis:
- Endometrial-like glandular epithelium with associated stroma and old hemorrhage
- Endocervicosis:
- Mucin secreting endocervical glands with extravasation of mucin if ruptured, deep within viscus
- May present as mass lesion
- No atypia, mitoses or tissue reaction (Am J Surg Pathol 1992;16:533)
- Urachal remnant:
- Intestinal metaplasia with goblet cells is noted in 33% of urachal remnants (J Urol 1982;127:40)
- Adenocarcinoma - primary, metastatic or from renal pelvis / ureter:
- Infiltrative with extensive muscle invasion, anaplasia, mitotic figures and extensive mucinous pools (Hum Pathol 1997;28:1152)
- Urothelial carcinoma:
- Noninvasive and infiltrating urothelial carcinoma with glandular differentiation mimicking adenocarcinoma can be differentiated by high grade cytology and may be seen accompanying cases with extensive glandular metaplasia (Am J Surg Pathol 2009;33:1241)
Additional references
Board review style question #1
Board review style answer #1
C. Goblet cells. According to updated criteria, lesions containing mucin secreting goblet cells are classified as intestinal metaplasia and the term cystitis glandularis is discouraged.
Comment Here
Reference: Intestinal metaplasia
Comment Here
Reference: Intestinal metaplasia
Board review style question #2
Which of the following features is considered to be a feature of intestinal metaplasia?
- Dysplasia (cytologic atypia)
- Invasion of muscularis propria
- Paneth cells
- Presence of dissecting mucin
Board review style answer #2
C. The presence of Paneth cells is a small intestinal type of metaplastic change. The other features, such as the presence of dissecting mucin, cytologic atypia and invasion of muscularis propria, are helpful to evaluate presence of dysplastic changes or malignancy (well differentiated adenocarcinoma).
Comment Here
Reference: Intestinal metaplasia
Comment Here
Reference: Intestinal metaplasia