Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Durowoju L, Tretiakova M. Cystitis cystica and cystitis glandularis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladdercystitiscystica.html. Accessed August 4th, 2025.
Definition / general
- Proliferative or reactive changes occurring in von Brunn nests which acquire luminal spaces, become cystically dilated (cystitis cystica), undergo glandular metaplasia (cystitis glandularis) or intestinal type metaplasia (cystitis glandularis, intestinal type)
Essential features
- Extremely common incidental finding
- Develops in the setting of chronic mucosal irritation or inflammation
- Cystitis cystica and cystitis glandularis are frequently coexisting interrelated lesions
- Benign mimickers of invasive carcinoma
Terminology
- Cystitis cystica et glandularis (when combined features)
- Cystitis glandularis, conventional type
- Cystitis glandularis, intestinal type (preferred term: intestinal metaplasia)
- Proliferative cystitis (discouraged terminology)
ICD coding
Epidemiology
- Extremely common: 60% of normal bladders at autopsy (J Urol 1979;122:317)
- Can occur in males and females at any age (Arch Pathol Lab Med 2012;136:721)
Sites
- Bladder; neck and trigone are most common sites
- Also ureters (ureteritis) and renal pelvis (pyelitis)
Pathophysiology
- Reactive process in response to chronic irritation, infection, calculi, outlet obstruction, catheterization (Pathol Annu 1995;30:95)
- Urothelium proliferates and invaginates into underlying lamina propria
Etiology
- Chronic irritation / local inflammatory insult
Clinical features
- Majority are asymptomatic incidental findings
- May infrequently cause recurrent urinary tract infections
- Occasionally appears as polypoid or papillary mass on cystoscopy
- Cystitis glandularis can be associated with pelvic lipomatosis and bladder exstrophy
- Reference: Pathol Annu 1995;30:95
Diagnosis
- Diagnosis is by microscopic examination of resected tissue
Radiology description
- CT: hypervascular polypoid mass
- MRI T2: hyperintense vascular core with surrounding low intensity signal (Abdom Radiol (NY) 2019;44:3827)
Prognostic factors
- Reactive process without malignant potential
- May regress if the cause of irritation is removed
Case reports
- 16 year old boy with cystitis cystica and glandularis producing large bladder mass (JRSM Open 2018;9:2054270417746060)
- 37 year old man with cystitis glandularis treatment with oral cyclooxygenase 2 inhibitor (Int J Urol 2016;23:706)
- 46 year old man with cystitis cystica as a large solitary bladder cyst (J Endourol Case Rep 2017;3:34)
Treatment
- Elimination of underlying source of irritation
- Antibiotic therapy if associated with chronic urinary tract infections
- Occasionally surgical resection (transurethral) may be necessary
- References: BJU Int 2013;112:27, Indian J Urol 2016;32:329
Gross description
- Mucosa may appear grossly unremarkable
- Cystitis cystica appears as translucent submucosal cysts, mostly < 5 mm diameter
- Cystitis glandularis appears as irregular or nodular lesions with a cobblestone pattern or as a polypoid mass
- References: Pathol Annu 1995;30:95, Histopathology 2011;58:811
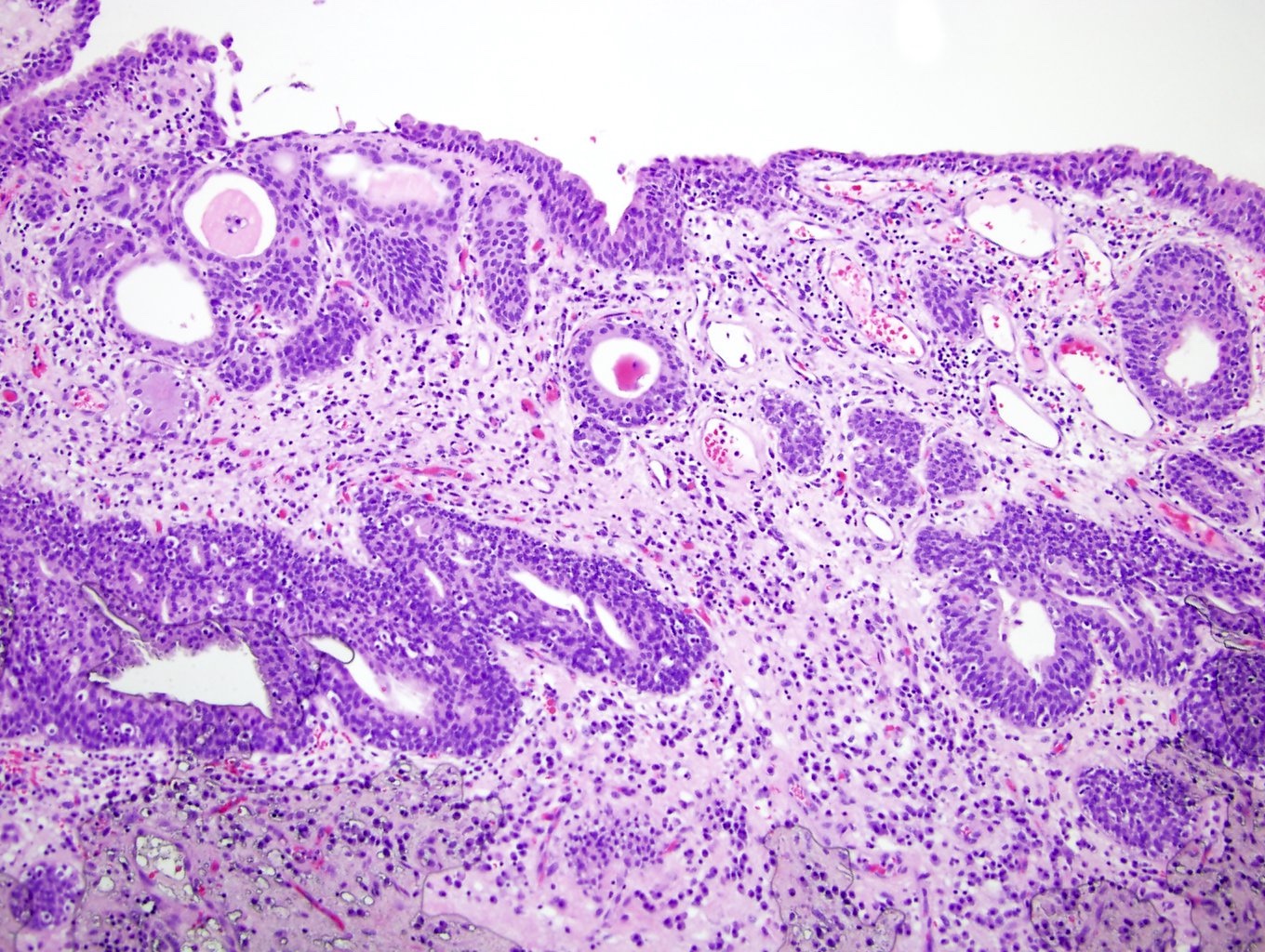
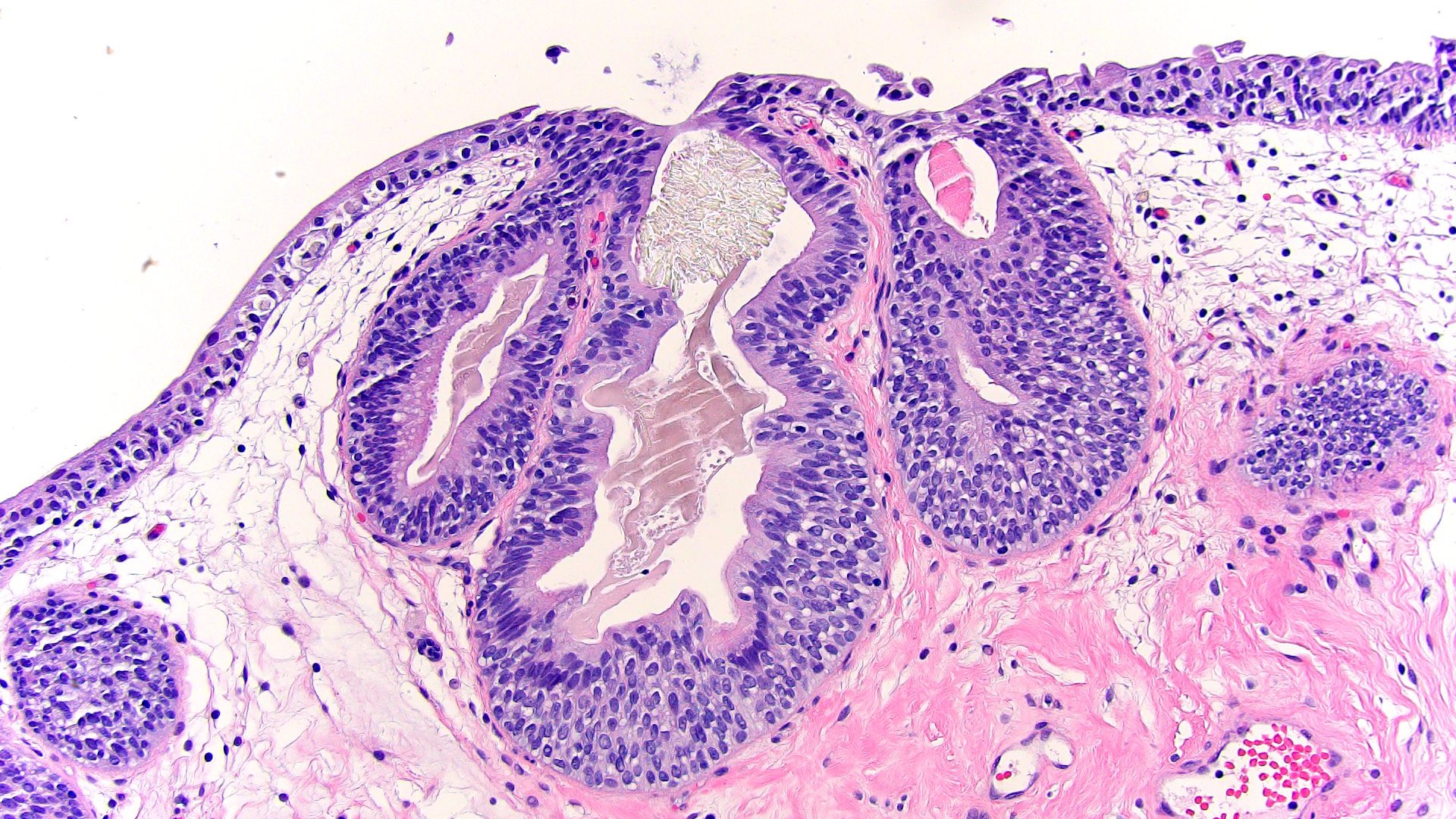
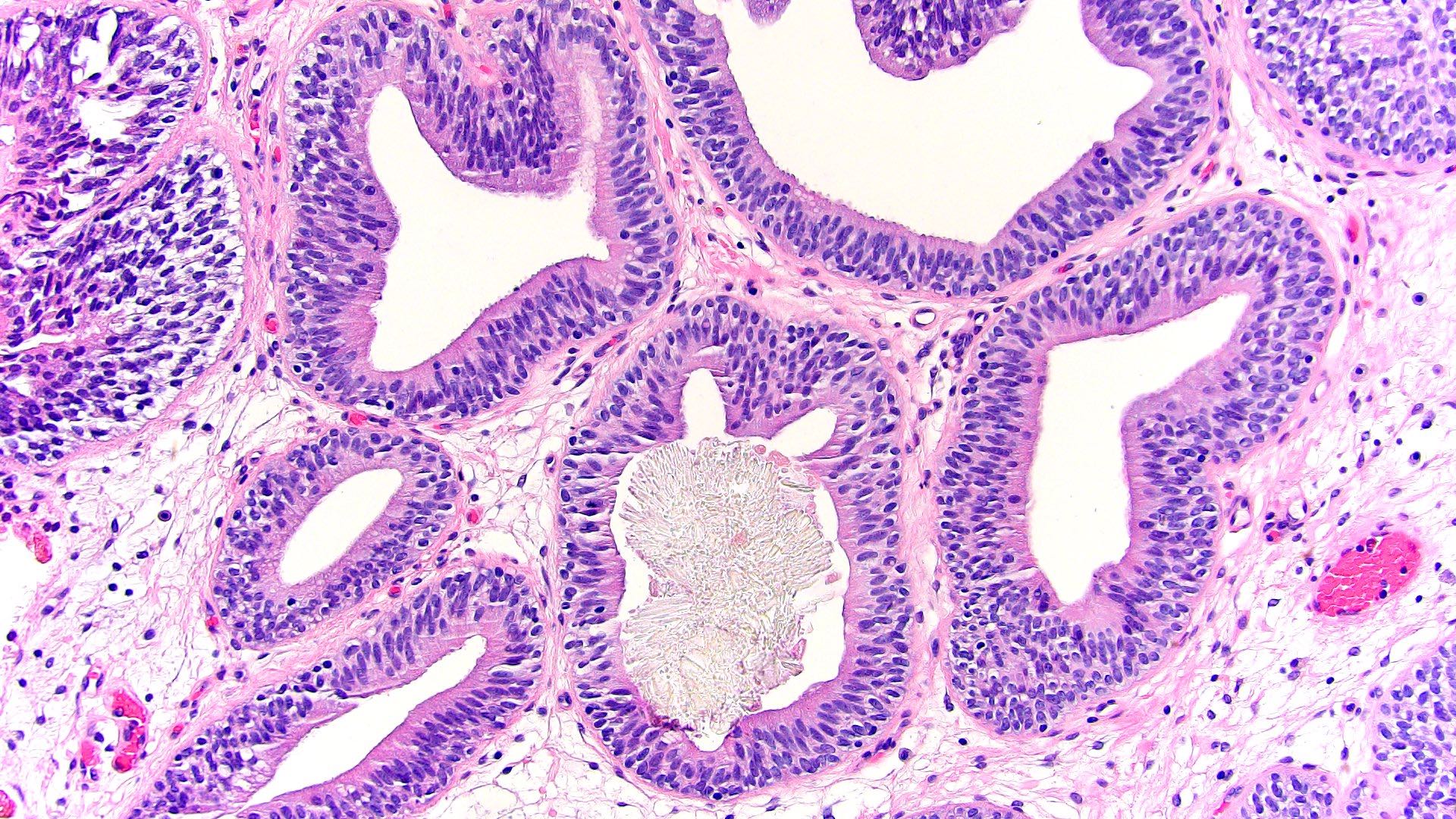
Microscopic (histologic) description
- Abundant urothelial von Brunn nests
- Often exhibit a vaguely lobular distribution of invaginations
- Noninfiltrative growth and variable connection to surface
- Gland-like lumens with columnar or cuboidal cells (cystitis glandularis)
- Cystically dilated lumens or cystic cavities filled with eosinophilic fluid (cystitis cystica)
- Majority of cases show coexistence of both patterns
- Cells lack significant atypia, mitotic activity, stromal reaction and muscular invasion (Ann Diagn Pathol 2019;38:11)
- Degenerative atypia occasionally present
Microscopic (histologic) images
Immunofluorescence description
- Cystitis glandularis demonstrates uniform membranous expression of beta catenin without cytoplasmic or nuclear localization (J Urol 2003;170:1892)
Positive stains
- GATA3, CK7 (full thickness), CK20 (umbrella cells), p63 (basal cell layer), uroplakin II / III, thrombomodulin, beta catenin (membranous), E-cadherin (J Clin Pathol 2016;69:307, Hum Pathol 2020;98:32, J Urol 2003;170:1892)
Negative stains
- CDX2, villin, MUC2, MUC5AC, beta catenin (nuclear) (J Clin Pathol 2016;69:307, Hum Pathol 2020;98:32)
Sample pathology report
- Bladder, trigone, biopsy:
- Urothelium with florid cystitis cystica et glandularis
- No neoplasm identified
- Muscularis propria absent
Differential diagnosis
- von Brunn nest hyperplasia:
- Urothelial mucosa budding of rounded nests into superficial lamina propria
- Lacks glandular type epithelium and cystic changes
- Urothelial carcinoma in situ involving von Brunn nests:
- Prominent cytologic atypia, increased mitoses and apoptotic debris
- Surface urothelium with carcinoma in situ
- Transurothelial CK20
- Inverted urothelial papilloma:
- Architectural complexity; trabecular / corded pattern
- Periphery of the lesion demonstrates a pushing border
- Invasive urothelial carcinoma, nested type:
- Variably sized nests infiltrating lamina propria and muscularis propria
- Cytologic atypia in deeper portion of tumor; high Ki67 proliferation rate
- Typically solid rather than cystic or glandular
- Invasive urothelial carcinoma, microcystic variant:
- Variably sized cysts and tubules infiltrating lamina propria and muscularis propria
- Greater cytologic atypia; higher proliferation rate
Additional references
Practice question #1
A 75 year old man presents with a polypoid bladder lesion on cystoscopy. Which feature could be present in nested variant of invasive urothelial carcinoma but should not be found in this entity?
- Background inflammation
- Expression of CK7 and CK20
- Invasion into muscularis propria
- Irregular nests variably distributed within lamina propria
- Mild cytologic atypia
Practice answer #1
C. Invasion into muscularis propria. This is cystitis cystica.
Comment Here
Reference: Cystitis cystica and cystitis glandularis
Comment Here
Reference: Cystitis cystica and cystitis glandularis
Practice question #2
Which is true about cystitis cystica?
- Considered a premalignant lesion
- Immunohistochemically negative for urothelial markers
- Part of morphologic spectrum with cystitis glandularis
- Rare finding
- Variably sized cysts are filled with extravasated mucin
Practice answer #2
C. Part of morphologic spectrum with cystitis glandularis
Comment Here
Reference: Cystitis cystica and cystitis glandularis
Comment Here
Reference: Cystitis cystica and cystitis glandularis