Breast
General
Staging
Last author update: 31 March 2022
Last staff update: 13 October 2023
Copyright: 2002-2024, PathologyOutlines.com, Inc.
PubMed Search:
Staging[title] breast carcinoma[title]
Page views in 2023: 47,873
Page views in 2024 to date: 18,340
Cite this page: Reisenbichler ES, Zynger D. Staging. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantstaging.html. Accessed May 6th, 2024.
Definition / general
- All carcinomas of the breast are covered by this staging system
- Breast sarcomas, phyllodes tumor and breast lymphomas are not staged using this system
Essential features
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
ICD coding
- ICD-10:
- C50.0 - nipple
- C50.1 - central portion of breast
- C50.2 - upper inner quadrant
- C50.3 - lower inner quadrant
- C50.4 - upper outer quadrant
- C50.5 - lower outer quadrant
- C50.6 - axillary tail
- C50.8 - overlapping lesion of breast
- C50.9 - breast, not otherwise specified
Primary tumor (pT)
- pTX: cannot be assessed
- pT0: no evidence of primary tumor
- pTis: ductal carcinoma in situ, Padget disease, encapsulated papillary carcinoma and solid papillary carcinoma
- pTis (DCIS): ductal carcinoma in situ without invasive carcinoma
- pTis (Paget): Paget disease without invasive carcinoma
- pT1mi: tumor ≤ 1 mm
- pT1a: tumor > 1 mm but ≤ 5 mm
- pT1b: tumor > 5 mm but ≤ 10 mm
- pT1c: tumor > 10 mm but ≤ 20 mm
- pT2: tumor > 20 mm but ≤ 50 mm
- pT3: tumor > 50 mm
- pT4a: extension to chest wall (not including pectoralis muscle)
- pT4b: edema (including peau d'orange), ulceration of skin or ipsilateral satellite skin nodules
- pT4c: both T4a and T4b
- pT4d: inflammatory carcinoma (involves > 1/3 of the breast skin, primarily a clinical diagnosis)
Notes:
- Lobular carcinoma in situ (LCIS) is no longer classified as Tis and is now considered a risk factor, not a malignancy
- For invasive tumors, do not include in situ tumor in the tumor measurement used to determine pT category
- Round invasive tumor size to the nearest millimeter, except if between 1.0 and 1.4 mm, then round up to 2.0 mm to avoid classifying as pT1mi
- Do not add tumor dimensions from the needle biopsy to the excision; use the maximum dimension in either the needle biopsy or excision for pT categorization (invasive tumor is larger in the needle biopsy than subsequent excision in 12% of cases, Am J Surg Pathol 2013;37:739)
- If multiple excisions, may want to report "at least pT_, a more accurate estimate may be based on imaging studies"
- If there are multiple simultaneous, macroscopically measurable, ipsilateral invasive tumors that are grossly and histologically not connected, use largest individual size, do not sum sizes; can use (m) suffix, e.g., pT1b(m)
- Contiguous tumor within the pectoralis muscle should be included in the tumor measurement to determine pT category
- In a postneoadjuvant specimen, measure the largest single contiguous focus; do not include the fibrous tumor bed without viable tumor
Regional lymph nodes (pN)
- pNX: cannot be assessed
- pN0: no regional lymph node metastasis histologically
- pN0(i-): no regional lymph node metastasis by histology or immunohistochemistry
- pN0(i+): isolated tumor cells (cluster ≤ 0.2 mm and < 200 cells)
- pN0(mol+): RT-PCR positive but negative by light microscopy
- pN1mi: micrometastasis (tumor deposit > 0.2 mm and ≤ 2.0 mm or ≤ 0.2 mm and > 200 cells)
- pN1a: metastasis in 1 - 3 axillary lymph nodes with at least 1 tumor deposit > 2.0 mm
- pN1b: metastasis in internal mammary sentinel lymph node with tumor deposit > 2.0 mm
- pN1c: pN1a and pN1b
- pN2a: metastasis in 4 - 9 axillary lymph nodes with at least 1 tumor deposit > 2.0 mm
- pN2b: metastasis in clinically detected internal mammary nodes with pathologically negative axillary nodes
- pN3a: metastasis in ≥ 10 axillary lymph nodes with at least 1 tumor deposit > 2.0 mm or metastasis to infraclavicular lymph node
- pN3b: positive internal mammary node by imaging with pN1a or pN1b
- pN3c: metastasis in ipsilateral supraclavicular lymph node
Notes:
- Lymph nodes, including sentinel lymph nodes, should be bisected along the long axis, not serially sectioned along the short axis; if the bisected halves are thick enough (> 2 mm), they should be further longitudinally sectioned (CAP: Cancer Protocol Templates [Accessed 31 March 2022], Mod Pathol 2010;23 Suppl 2:S26, APMIS 2011;119:868)
- Regional lymph nodes include axillary, internal mammary, supraclavicular and intramammary
- Isolated tumor cells = cluster ≤ 0.2 mm and < 200 cells
- Micrometastasis = deposit > 0.2 mm and ≤ 2.0 mm or ≤ 0.2 mm and > 200 cells
- Macrometastasis = deposit > 2.0 mm
- Count cells or measure tumor within a single lymph node cross section
- Measure only the largest contiguous focus of metastatic tumor cells; adjacent satellites are not included
- Extranodal extension should be included in the tumor deposit measurement
- The number of nodes with isolated tumor cells does not change pN category (e.g., 3 nodes with macrometastases plus 1 node with isolated tumor cells is pN1a, not pN2a)
- Direct extension of tumor into an intramammary lymph node is included as a positive regional lymph node
- Rounded tumor nodules without nodal tissue present in a nodal drainage area should be considered lymph nodes completely replaced with tumor, unless a vascular wall is present
- "Clinically detected" is defined as detected by imaging studies (excluding lymphoscintigraphy) or by clinical examination and having characteristics highly suspicious for malignancy or a presumed pathologic macrometastasis based on fine needle aspiration biopsy with cytologic examination
- In a postneoadjuvant node, measure only the largest contiguous metastatic deposit; do not add separate tumor deposits or include fibrosis without viable tumor
Prefixes
- y: preoperative radiotherapy or chemotherapy
- r: recurrent tumor stage
AJCC prognostic stage groups
- pTNM, tumor grade, ER, PR and HER2 status are incorporated into prognostic stage groups to refine prognosis
- Refer to the AJCC 8th edition for the stage group definitions
Registry data collection variables
Histologic grade (G)
- GX: cannot be assessed
- G1: low grade (score 3 - 5)
- G2: intermediate grade (score 6 - 7)
- G3: high grade (score 8 - 9)
Notes:
- To assign a histologic grade, assess and combine values for tubule formation (1 - 3), nuclear pleomorphism (1 - 3) and mitotic count (1 - 3) into a score
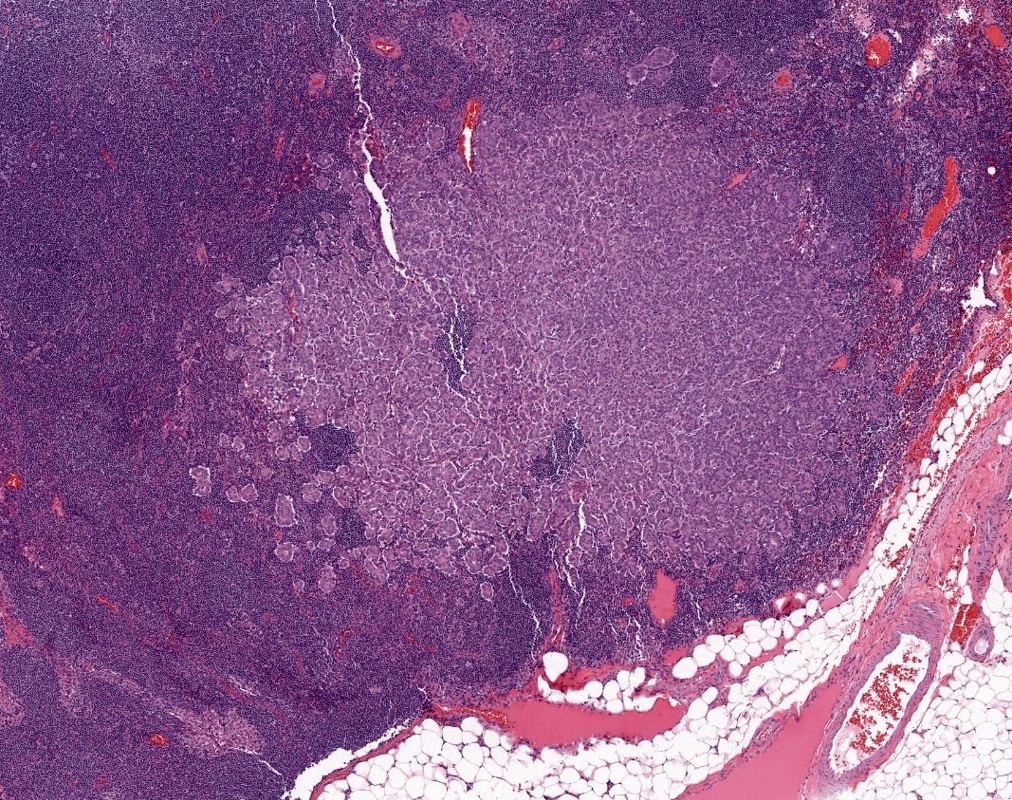
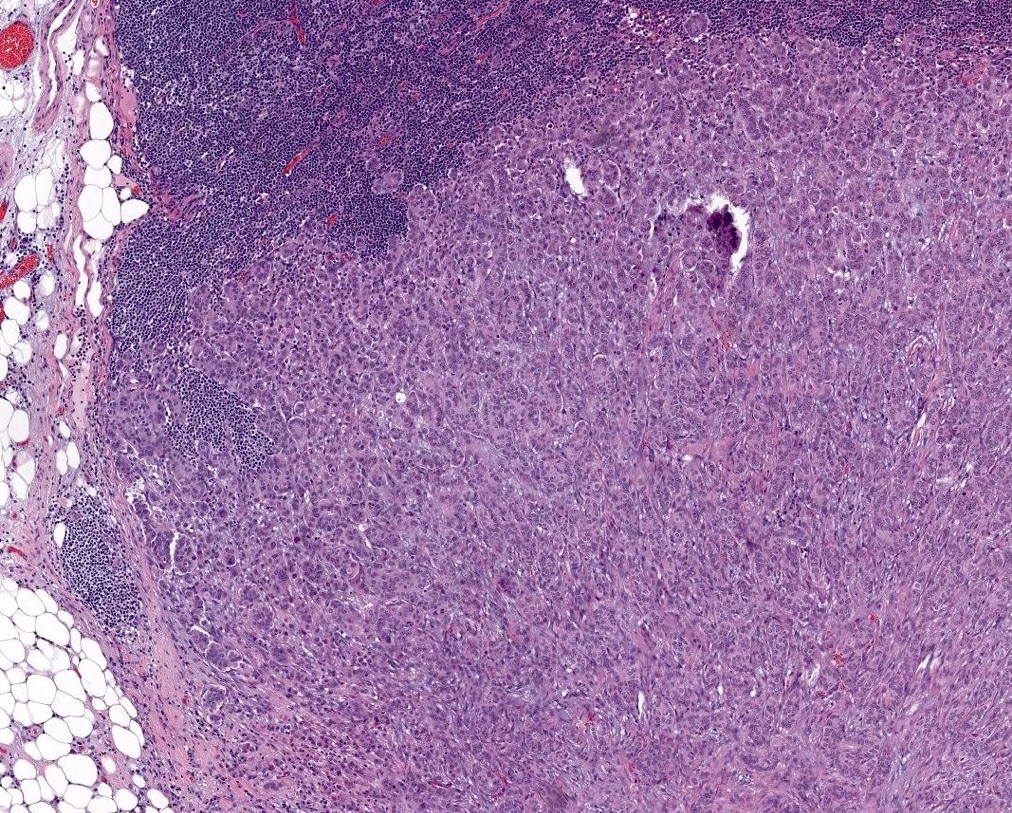
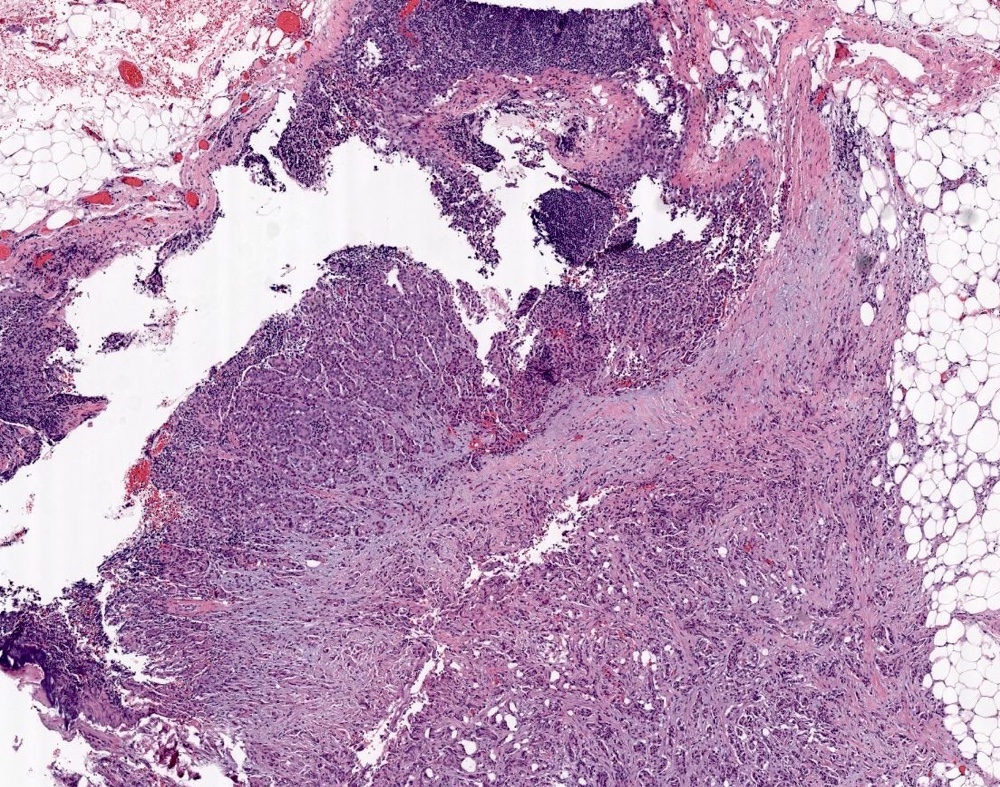
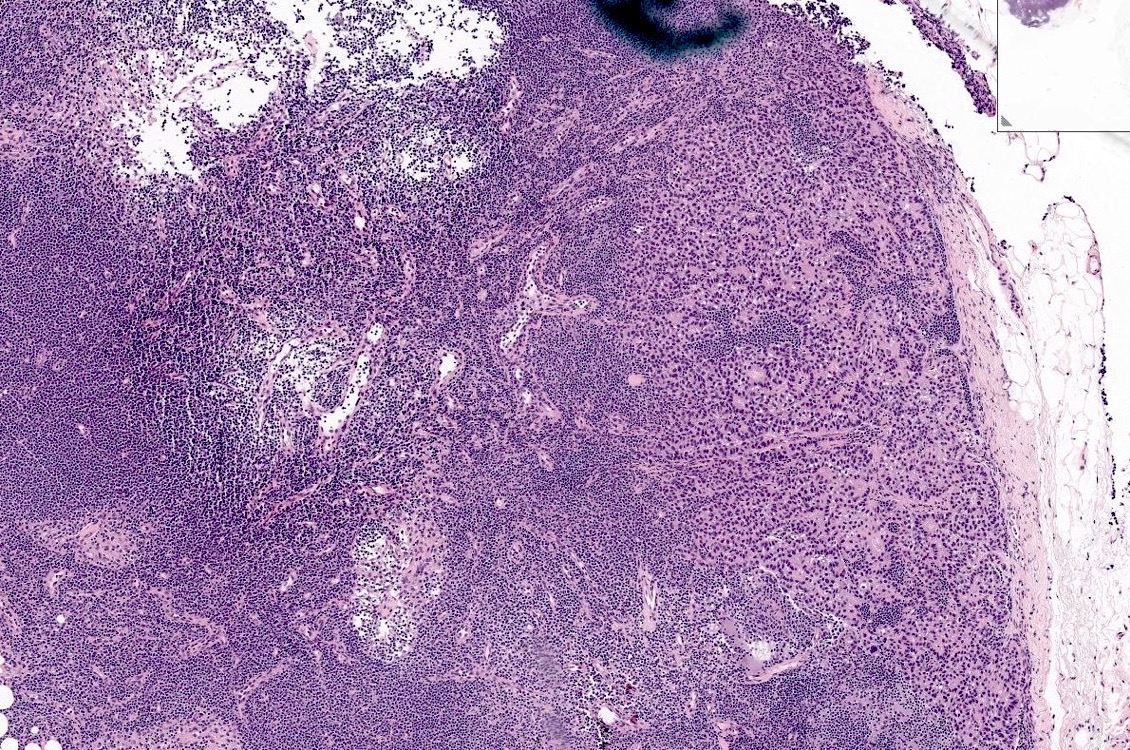
Gross images
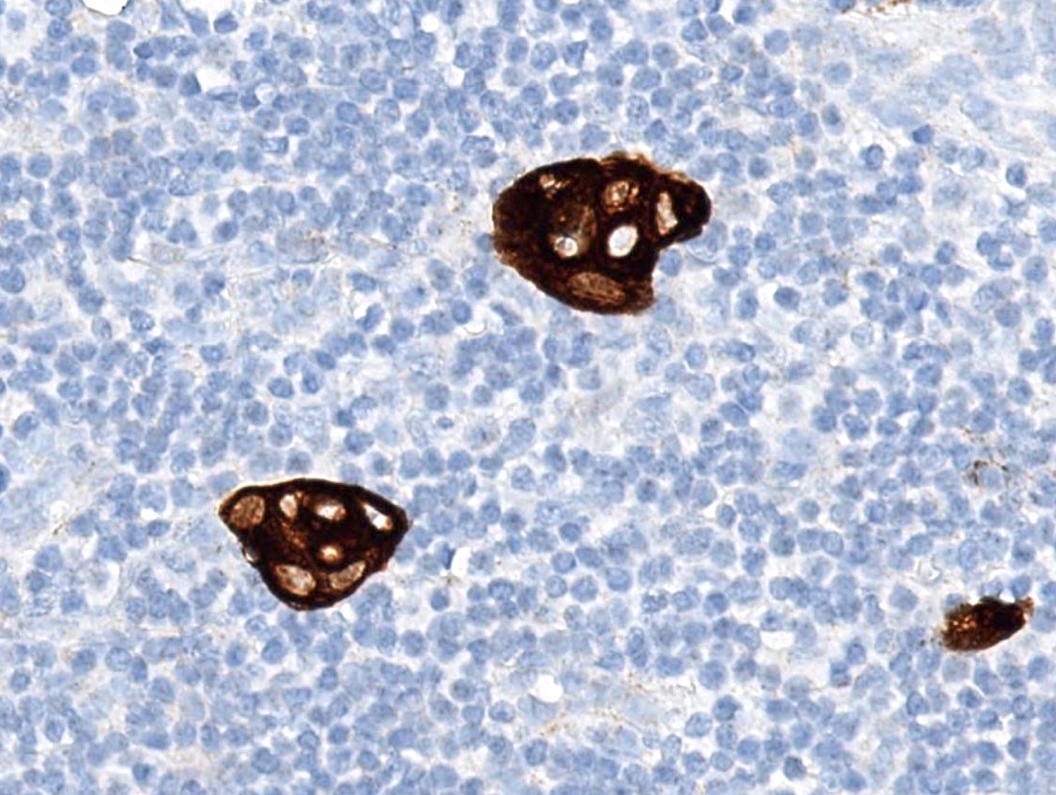
Contributed by Debra L. Zynger, M.D.

Bone metastasis (pM1)
Microscopic (histologic) images
Board review style question #1
What is the pN category for a patient with 1 macrometastasis, 2 micrometastases and 2 nodes with isolated tumor cells?
- pNX
- pN0(i+)
- pN1a
- pN2a
- pN3a
Board review style answer #1
C. pN1a. The number of nodes with isolated tumor cells does not increase the pN category.
Comment Here
Reference:
Breast - Staging
Board review style question #2
Which is the correct pT for a primary breast carcinoma that is 4 mm?
- pTis
- pTmi
- pT1a
- pT1b
- pT1c
Back to top