Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Jain PV, Jorns JM. Tubular. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignanttubular.html. Accessed October 3rd, 2025.
Definition / general
- Special subtype of invasive breast carcinoma with favorable prognosis
- Composed of distinct, well differentiated angular tubular structures (> 90%) with open lumina, lined by a single layer of low grade malignant epithelial cells, with a fibrous / desmoplastic stromal response
Essential features
- > 90% of the tumor is composed of ovoid or angular tubules with open lumina lined by a single layer of epithelial cells with low grade nuclei and sparse mitoses (grade 1)
- ER positive and HER2 negative
Terminology
- Tubular carcinoma
- Invasive tubular carcinoma
ICD coding
Epidemiology
- 1.6% of invasive breast carcinomas
- Postmenopausal women, median age at presentation is 63 years
- Slightly higher incidence in white women than black women in the U.S.
Sites
- Breast, with no specific site of predilection
Pathophysiology
- Luminal A molecular subtype of breast cancer
- Hypothesis: may arise due to a sequence of events starting with flat epithelial atypia
- Co-occurrence of columnar cell lesions, atypical ductal hyperplasia / ductal carcinoma in situ and pure form of tubular carcinoma with the same cytologic nuclear morphology has been observed (J Urol 1992;147:322)
- Rosen triad: tubular carcinoma, lobular carcinoma in situ, columnar cell lesions (Adv Anat Pathol 2008;15:140)
Etiology
- No specific etiology: see etiologies associated with low grade, ER positive invasive breast cancer of no special type (NST)
Clinical features
- Can be multifocal / multicentric (20 - 55%) (Am J Surg Pathol 1997;21:653)
- May have family history of breast carcinoma (40%)
- Usually presents as early stage, pT1 and pN0 disease (Int J Radiat Oncol Biol Phys 2009;75:1304)
Diagnosis
- Histologic examination of tissue
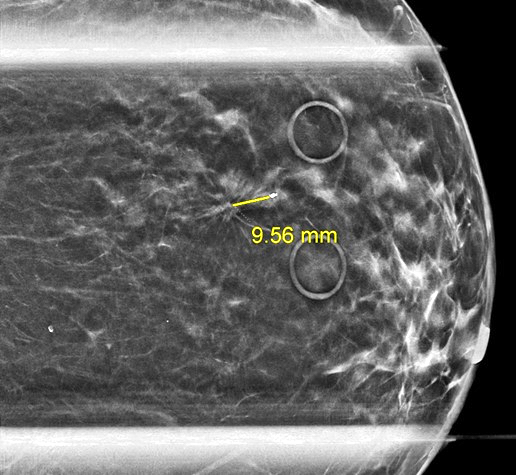
Radiology description
- Mammography: may present as a discrete or ill defined mass with well demarcated or spiculated, irregular margins, respectively or as an architectural distortion, with variable calcifications (Radiol Med 2006;111:773)
- Ultrasonography: hypoechoic mass with poorly defined margins and posterior acoustic shadowing (Tumori 2003;89:417)
- MRI: enhancing mass, enhancing focus or non mass enhancement (Egyptian J Radiol Nuc Med 2018;49:281)
Prognostic factors
- Well differentiated variant with very favorable prognosis (low rates of recurrence and metastasis) (Am J Surg 2009;197:674)
- Longer disease free and breast cancer specific survival with tubular carcinoma (n = 102) as compared to grade 1 invasive ductal carcinoma of no special type (n = 212) (J Clin Oncol 2010;28:99)
- Higher disease free survival was seen with pure tubular histology as well as if 3 criteria were met (≥ 70% tubules, pure grade 1 nuclei and no / rare mitoses) in a cohort of grade 1 - 2 tubular (n = 32) and invasive ductal (n = 115) carcinomas (Am J Clin Pathol 2004;122:728)
- Mixed with invasive ductal carcinoma of no special type has a worse prognosis (Hum Pathol 1983;14:694)
- Cause specific survival of 97% at 10 years (Eur J Surg Oncol 2005;31:9)
- 10 - 27% have axillary metastases, often micrometastases but still have excellent prognosis (Eur J Surg Oncol 2006;32:488, Breast J 2003;9:298)
Case reports
- 39 and 74 year old women who presented with tubular carcinoma in retroareolar and deep parasternal locations, respectively (Medicine (Baltimore) 2021;100:e24977)
- 46 year old woman with tubular carcinoma presenting as non mass enhancement (Egyptian J Radiol Nuc Med 2018;49:281)
- 63 year old woman with tubular carcinoma that spontaneously shrank from 9 mm to 4 mm on breast imaging during the 6 year interval from first identification to diagnostic biopsy (Radiol Case Rep 2015;1:68)
Treatment
- Surgery, either breast conserving surgery (lumpectomy) or mastectomy, with or without radiation therapy depending on surgery and clinical features (Breast Cancer Res Treat 2005;93:199, Breast J 2005;11:129)
- Axillary lymph node staging, including sentinel lymph node excision, may be safely omitted (Eur J Surg Oncol 2013;39:248, Ann Surg Oncol 2023;30:1042)
- May be offered anti-endocrine therapies
- Adjuvant chemotherapy is contraindicated
Gross description
- Spiculated tumor with a firm consistency; may have gritty texture if there are calcifications
- Mean size is 1.2 cm
- White, tan or gray in color
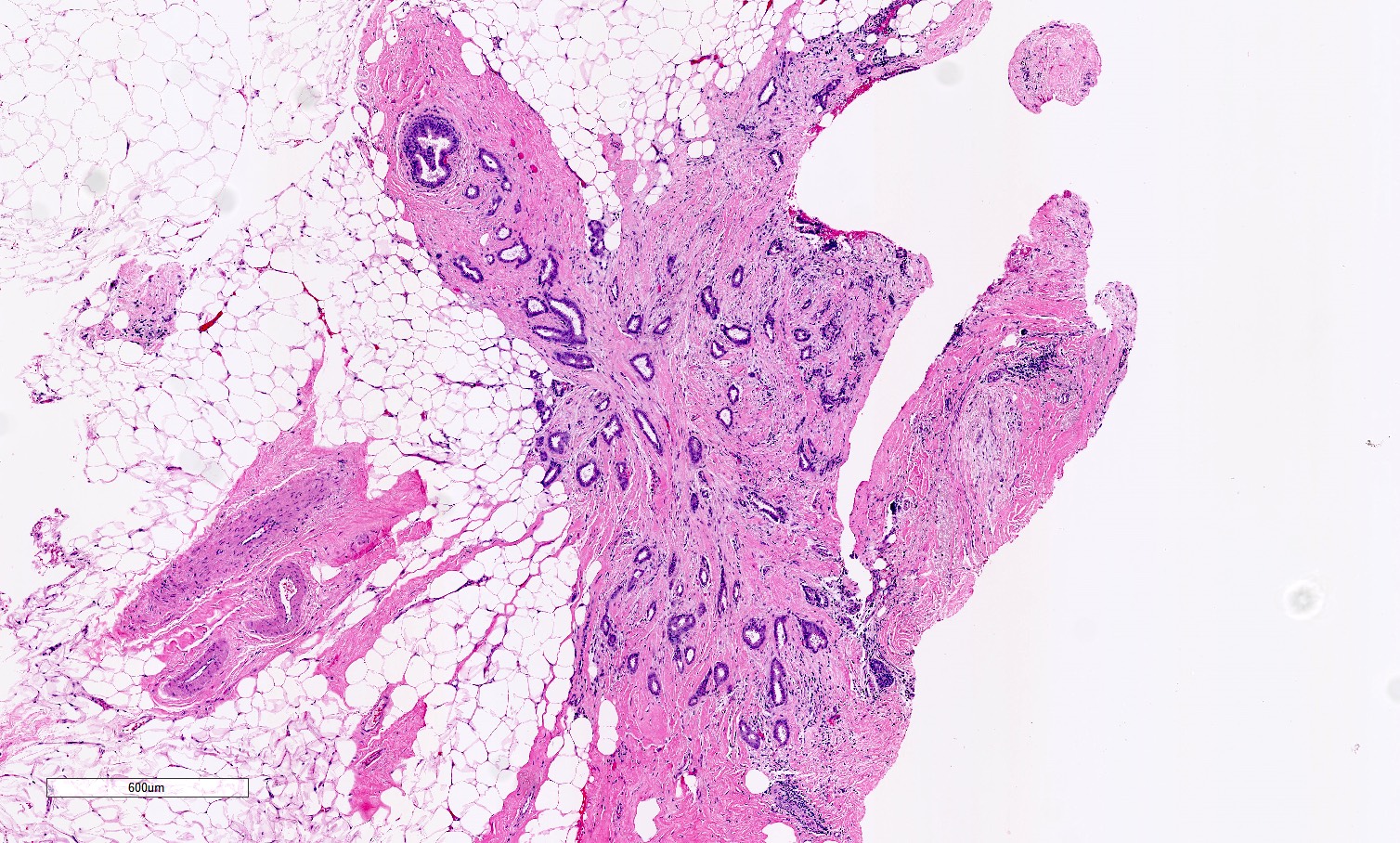
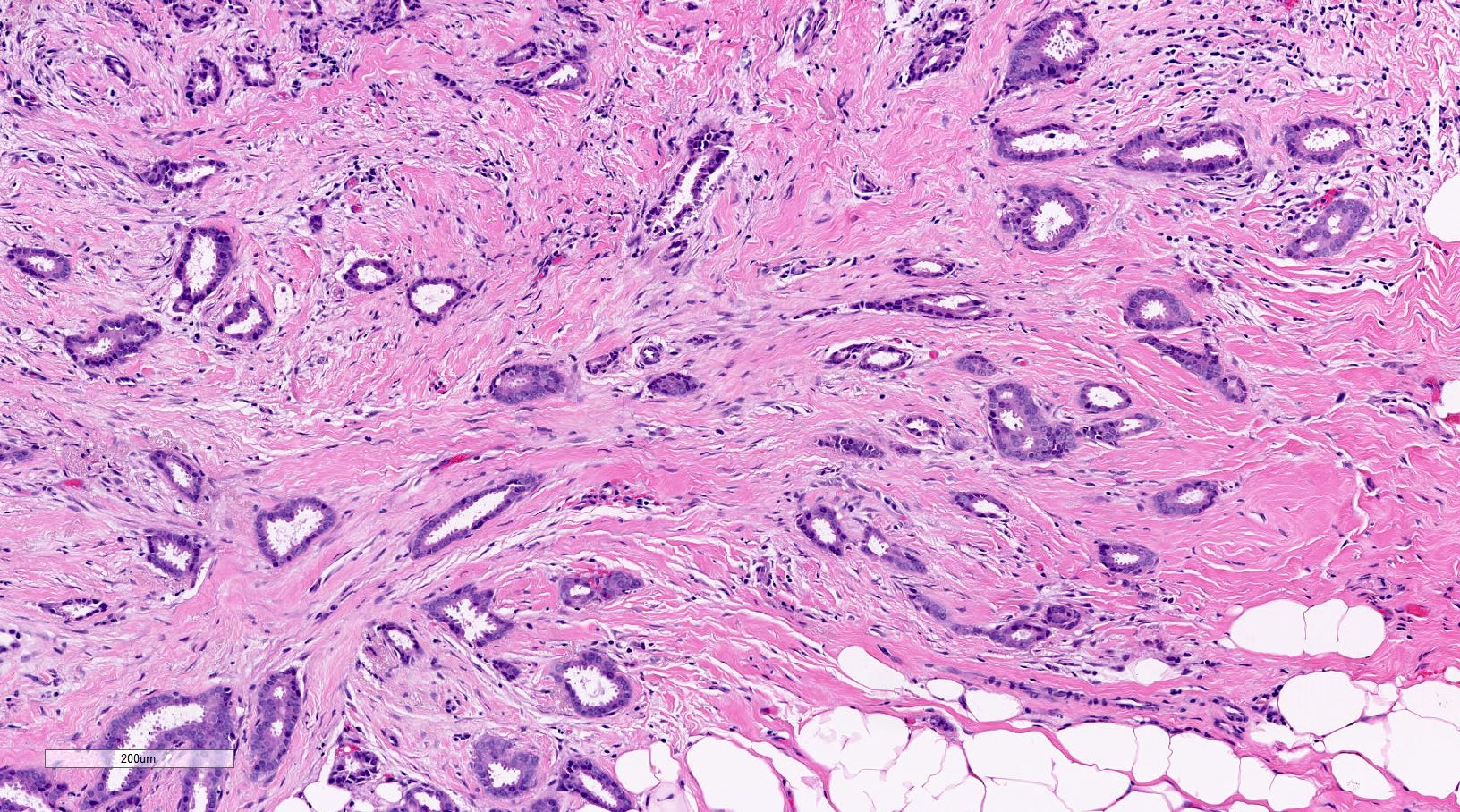
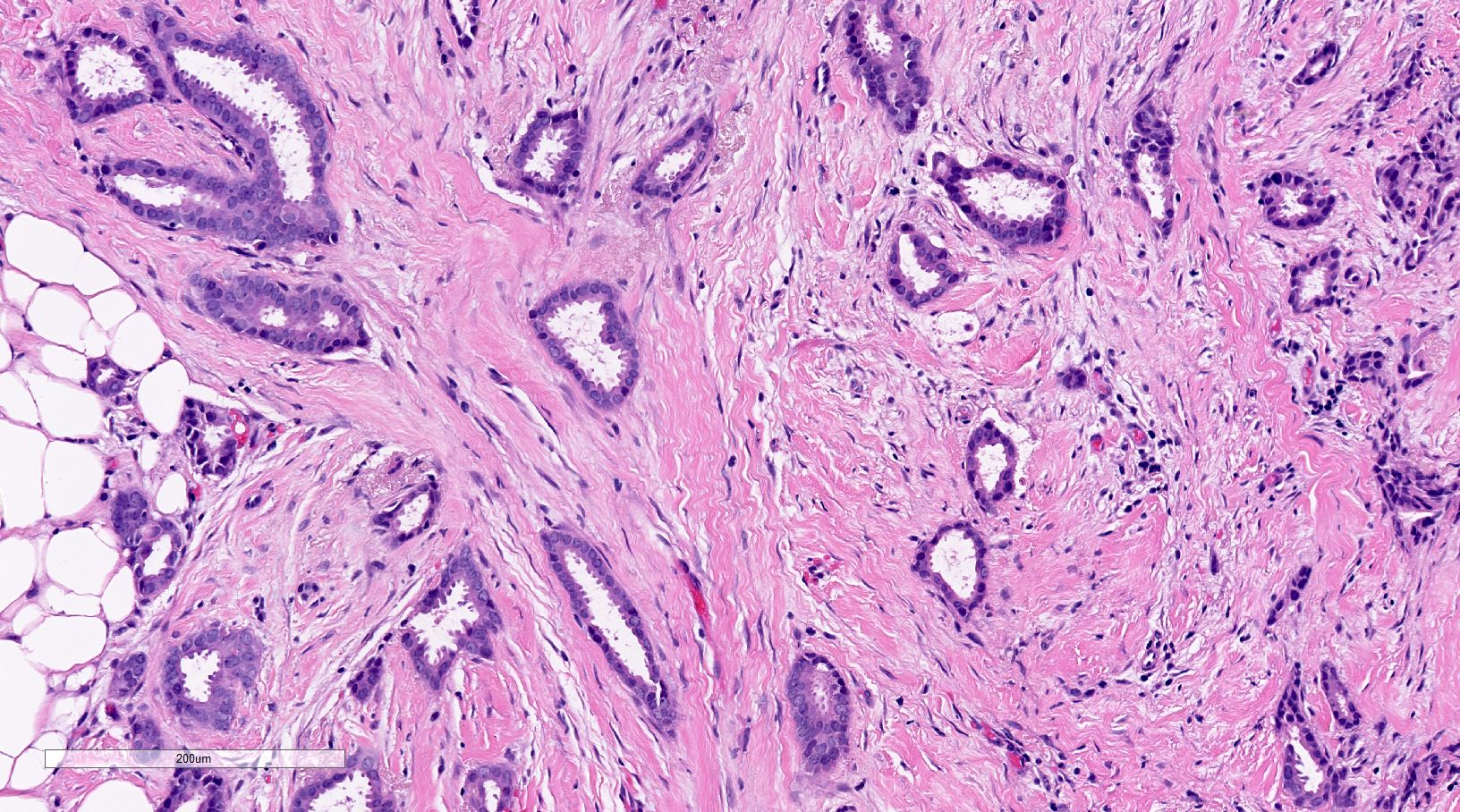
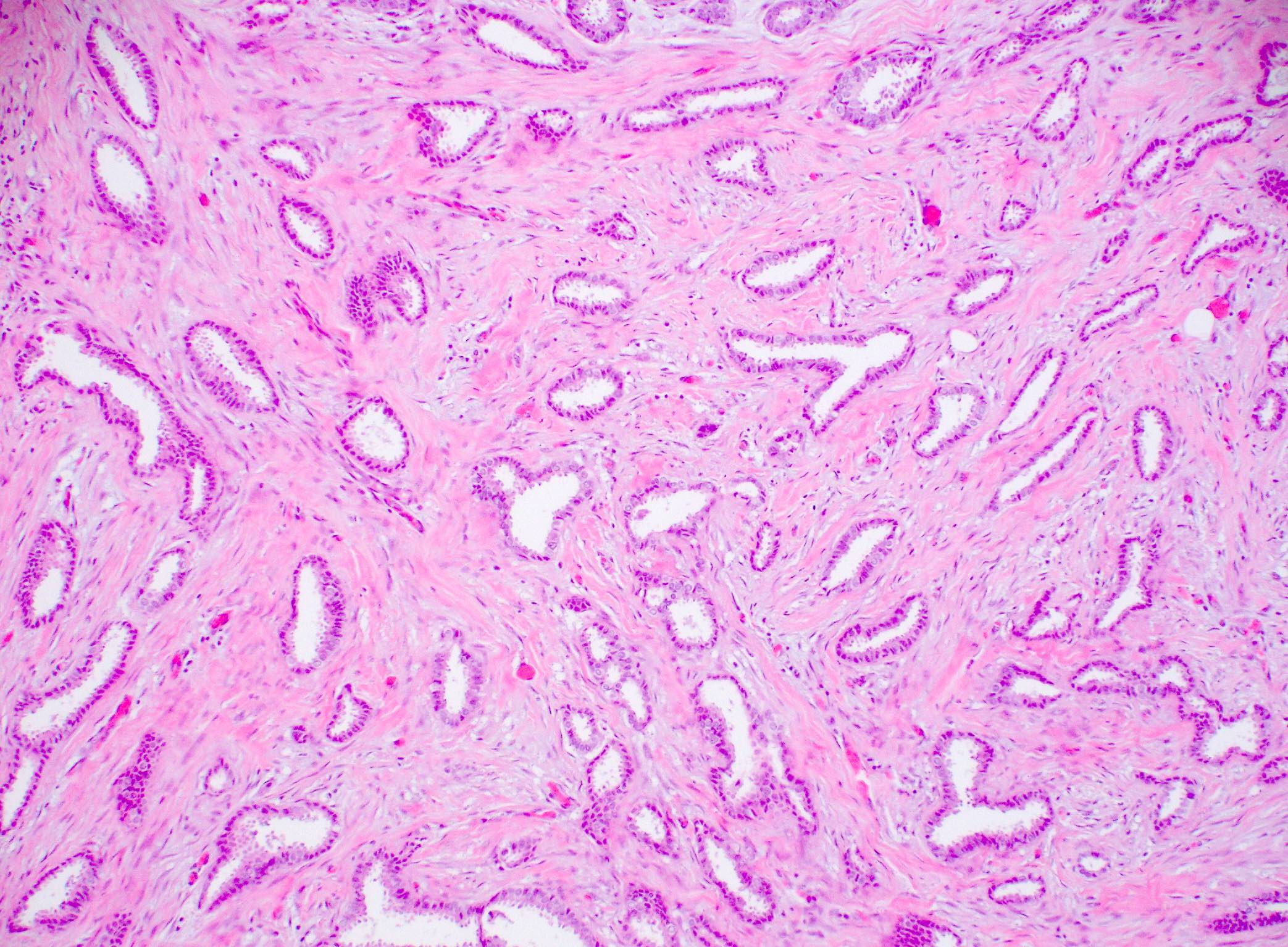
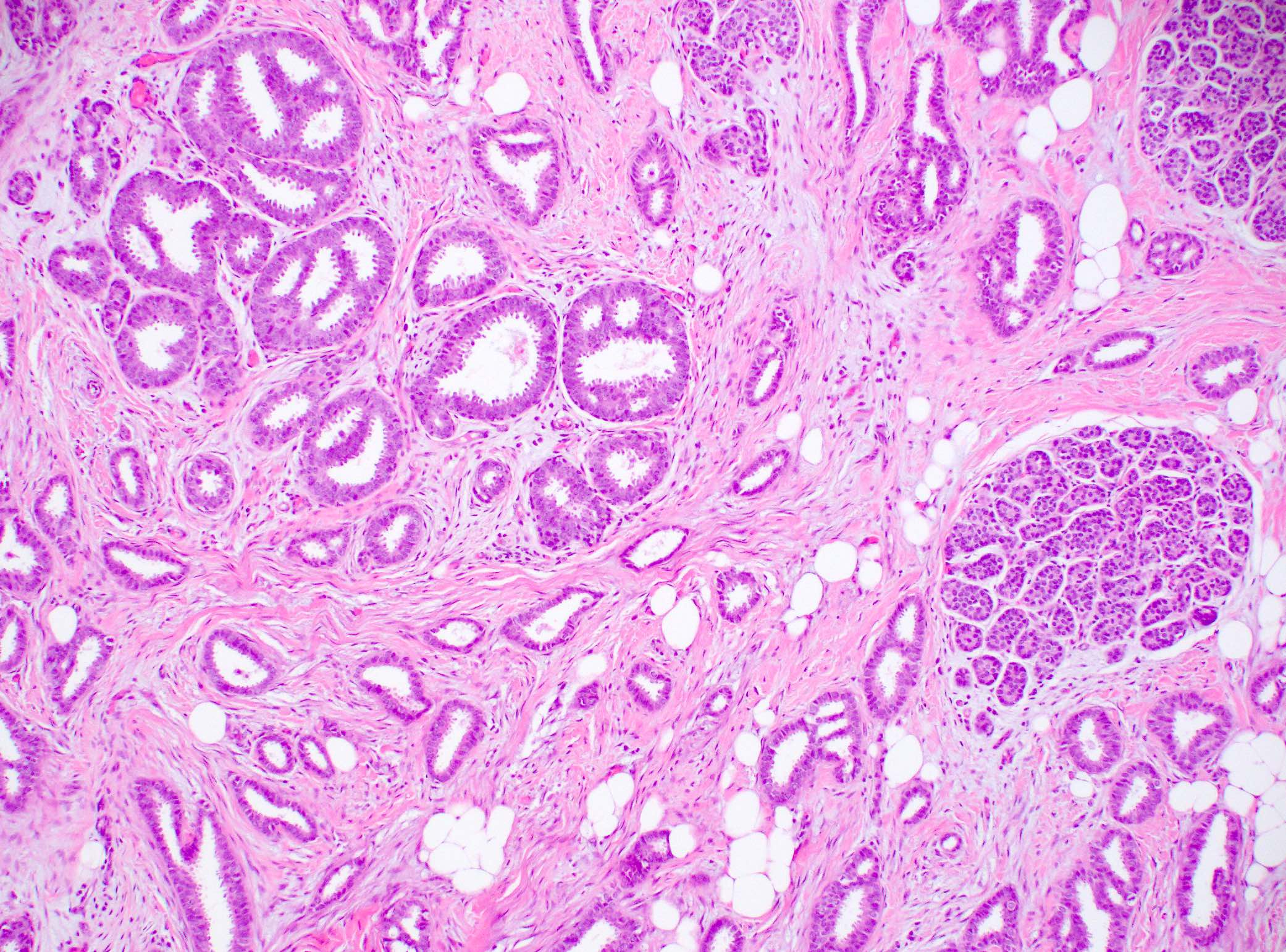
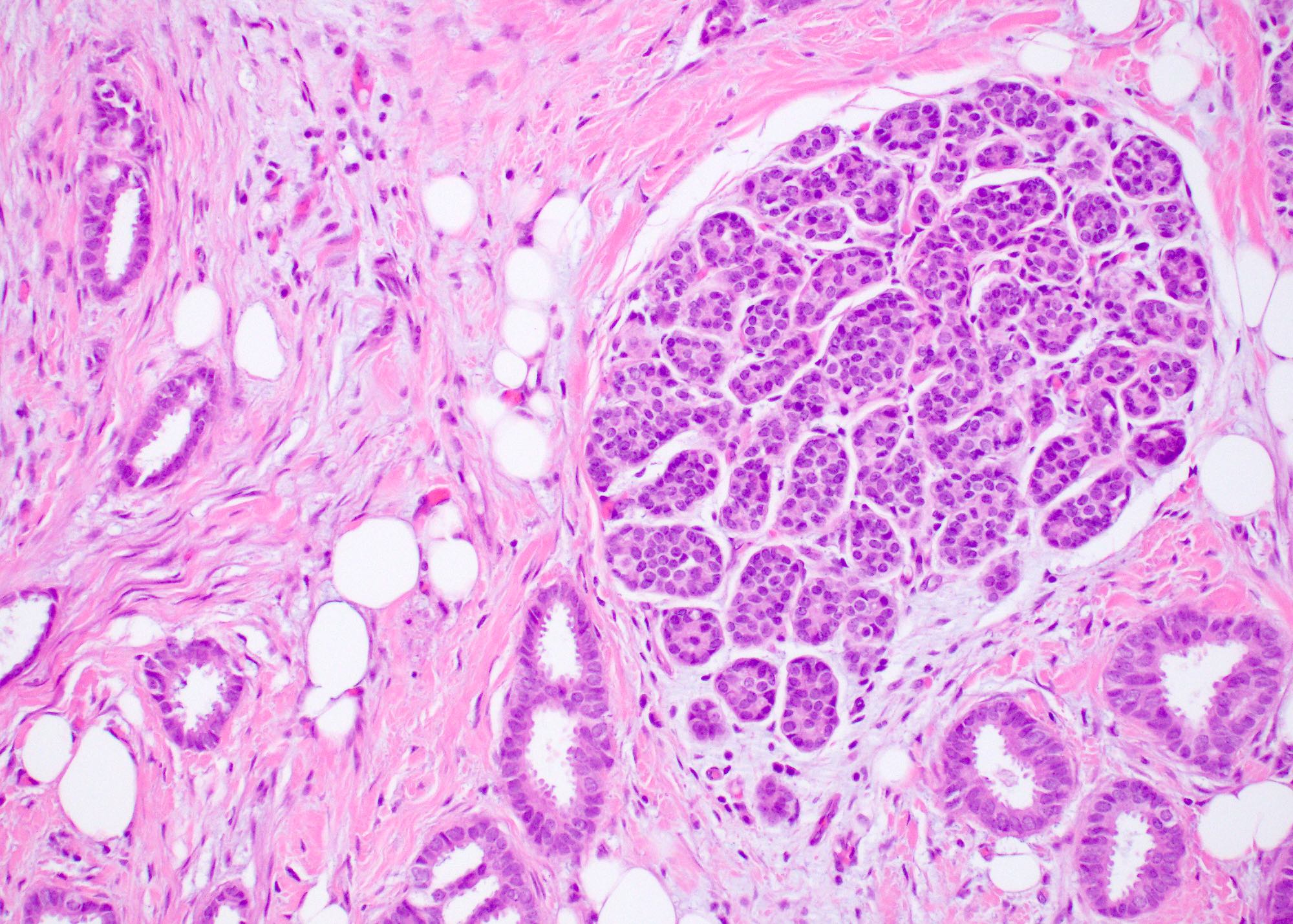
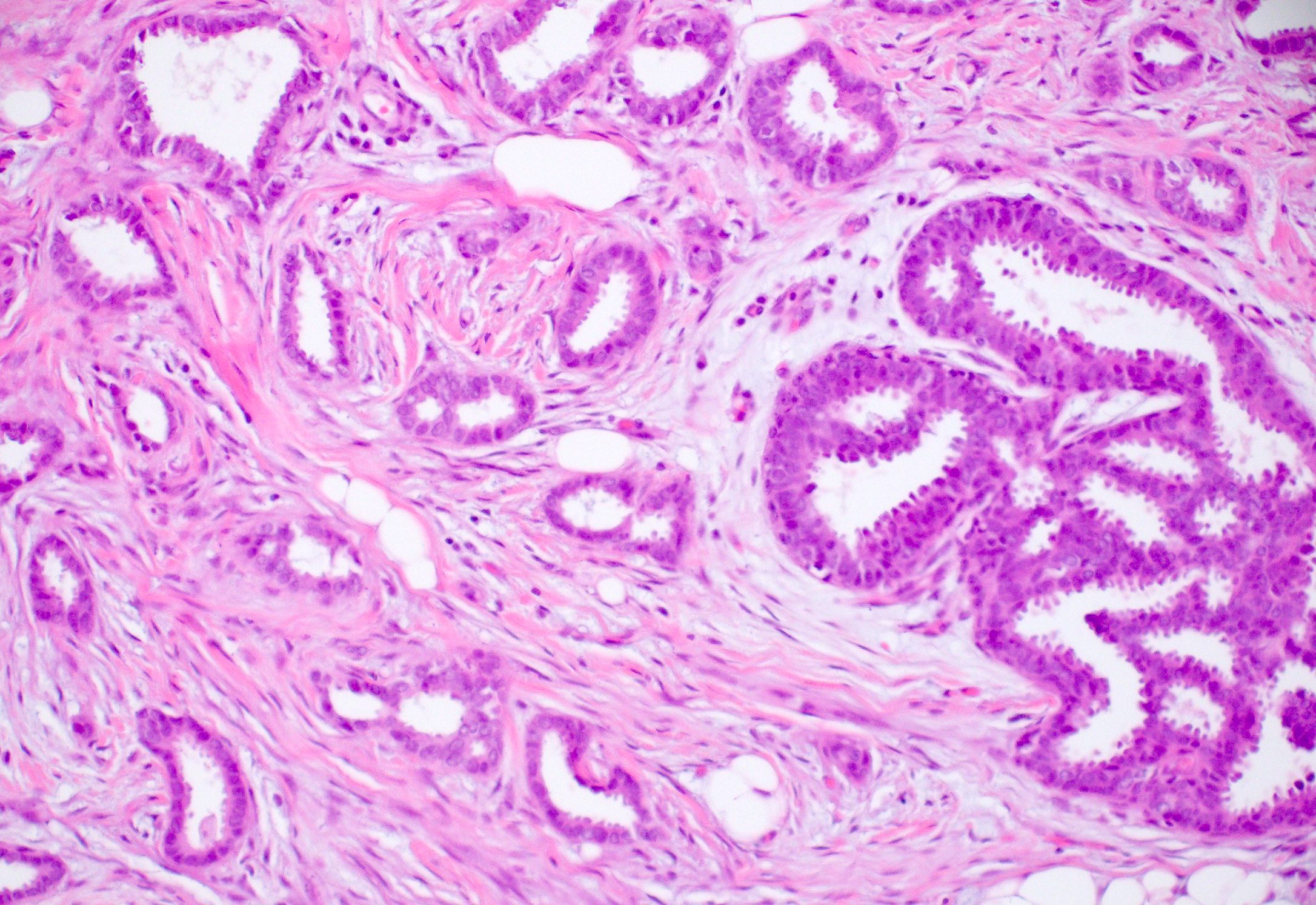
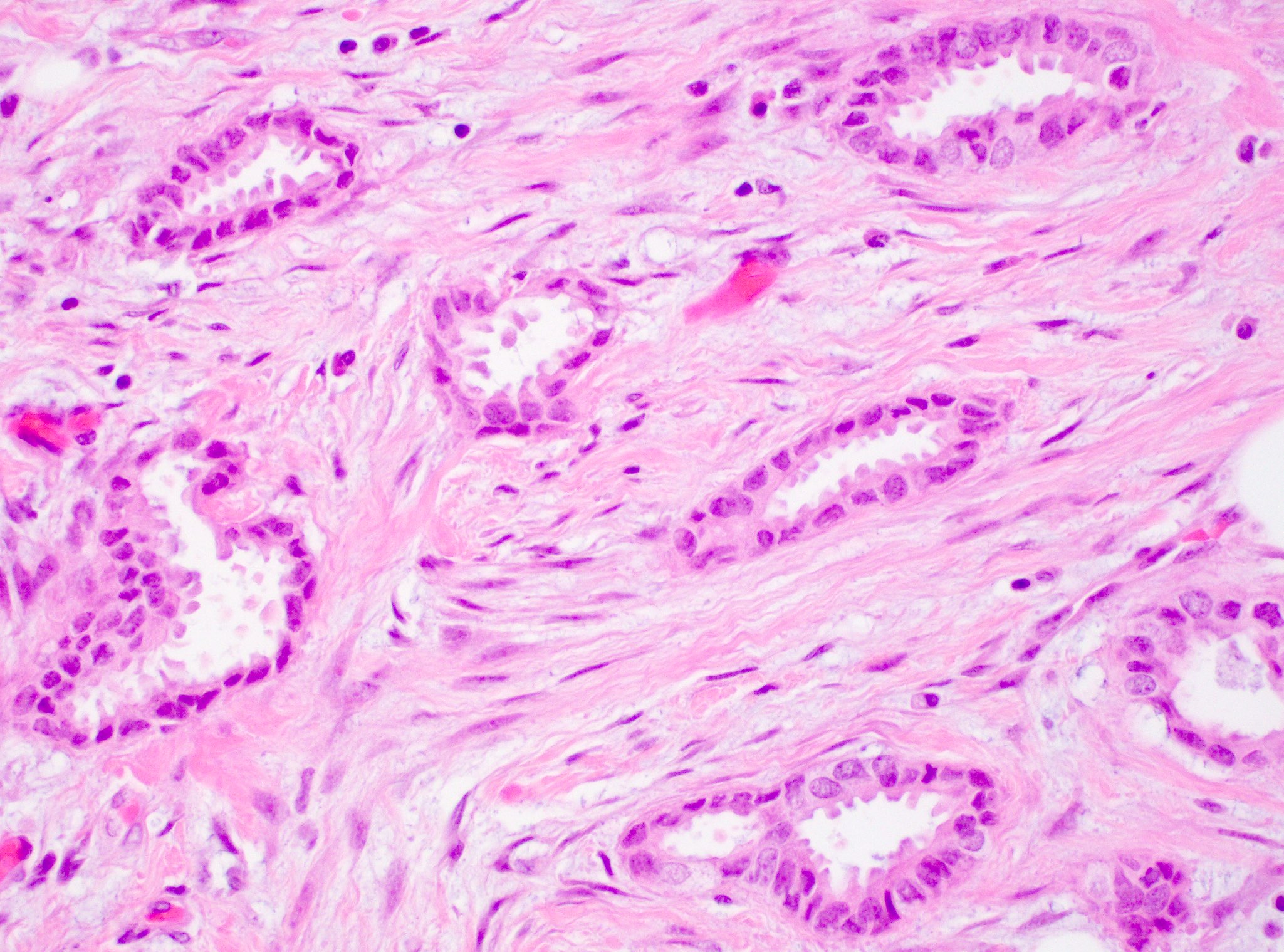
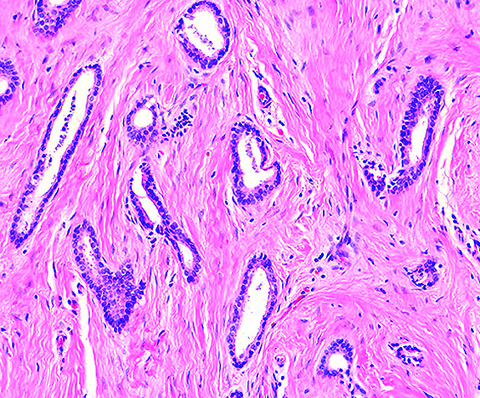
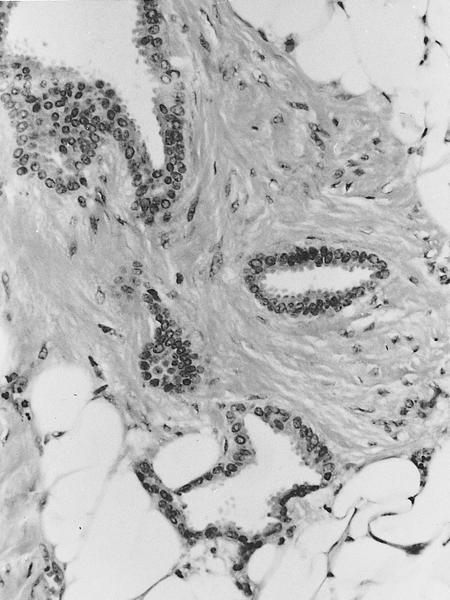
Microscopic (histologic) description
- Invasive breast cancer with infiltrative growth pattern, often with invasion into adipose tissue and with an associated fibrous or desmoplastic stromal response
- No myoepithelium surrounding the tubules
- > 90% of the tumor is composed of small, ovoid or angulated tubules with open lumina
- Tubules are lined by a single layer of epithelial cells with low grade nuclei and sparse mitoses (grade 1)
- Tumor cells often have apical cytoplasmic tufting or snouts
- Cells lining the neoplastic tubules are cuboidal to columnar with uniform, small to intermediate sized nuclei
- No significant cytologic atypia, multilayering or high mitotic activity (the presence of these would rule out tubular carcinoma)
- There may be luminal secretions or calcifications
- Tumor cells are ER positive and HER2 negative
- Recent study shows that the actual structure is not tubular, instead it simulates a beaded necklace
- 2 dimensional microscopy and 3 dimensional modeling studies revealed that structure resembled a necklace formed by a string of beads with the tubules visualized as blebs bridged together by solid cords of cells; continuous or branching tubules were not seen (Histopathology 2006;48:556)
- Desmoplastic or fibroelastotic stroma
- Frequent presence of associated nonobligate precursors:
- Columnar cell lesions (95%), in particular flat epithelial atypia (Am J Surg Pathol 2007;31:417, Pathol Int 2008;58:620)
- Atypical ductal hyperplasia
- ER positive low grade DCIS
- Rosen triad: tubular carcinoma, lobular carcinoma in situ, columnar cell lesions (Adv Anat Pathol 2008;15:140)
Microscopic (histologic) images
Contributed by Julie M. Jorns, M.D., Mark R. Wick, M.D. and AFIP
Cytology description
- Increased cellularity, somewhat angular or irregular or small tubular epithelial clusters and single epithelial cells
- Cells are bland and orderly with variable atypia and a variable number of prominent myoepithelial cells
- Features of malignancy such as nuclear atypia, absence of myoepithelial cells and cellular dissociation are subtle and hence diagnosis on cytology can be challenging (Acta Cytol 1997;41:1139, Am J Clin Pathol 1994;101:488)
Positive stains
- ER, PR and E-cadherin
- CK8, CK 8/18 (luminal phenotype)
Negative stains
- HER2 (ERBB2), HER1 (EGFR), p53 (Am J Clin Pathol 2006;126:55)
- Myoepithelial markers (p63, CD10, smooth muscle actin, CK5/6)
- P-cadherin
- CK5 / CK14 (luminal phenotype)
Electron microscopy description
- Ductal differentiation, no myoepithelial cells and no basement membrane
Molecular / cytogenetics description
- ER positive pathway alterations
- Frequent alterations: loss of 16q (78 - 86%), gains of 1q (50 - 62%), both usually occur concurrently
- Infrequent alterations: 16p gain, loss of 8p, 3p (the FHIT gene locus) and 11q (the ATM gene locus)
- Fewer overall chromosomal changes than invasive ductal carcinoma of no special type (Hum Pathol 2001;32:222)
- Clonally related to flat epithelial atypia and low grade DCIS (Am J Surg Pathol 2009;33:1646)
Sample pathology report
- Right breast, ultrasound guided core biopsy:
- Invasive mammary carcinoma with tubular features, preliminary modified Bloom-Richardson grade 1 (1+2+1) (see comment)
- Estrogen receptor: (91 - 100%, strong) positive
- Progesterone receptor: (91 - 100%, strong) positive
- HER2 / neu: (1+) negative for overexpression
- Comment: The carcinoma in this biopsy has entirely tubular features. If there is similar morphology in > 90% of the tumor on resection it would be best classified as an invasive tubular carcinoma.
Differential diagnosis
- Sclerosing adenosis:
- Overall lobular architecture but with distortion by fibrosis, compression of glands with 2 layers (inner epithelial and outer myoepithelial)
- Positive for myoepithelial markers (Appl Immunohistochem Mol Morphol 2006;14:71)
- Radial scar:
- Desmoplastic / elastotic stroma, bland tubules
- Does not infiltrate at the periphery
- Often has intermixed fibrocystic changes such as cysts and usual ductal hyperplasia
- Retained myoepithelial cell layer
- Microglandular adenosis:
- More rounded (not angulated) tubules with intraluminal colloid-like secretory material (Am J Surg Pathol 1982;6:401)
- Lacks myoepithelium but basement membrane material is present
- ER negative and S100 positive
- Mixed tumors with a combination of tubular carcinoma and another subtype of cancer:
- Should be reported when the tumor mass shows 10 - 90% tubular carcinoma (common) or ≥ 90% is tubular carcinoma and remaining tumor shows nuclear grade 3 (rare)
- Tubulolobular carcinoma:
- Mixed tubular and lobular components
- Not an entity in WHO
- Thought to be a variant of tubular carcinoma as they share similar architectural and growth patterns (tubulolobular carcinoma also resembles a beaded necklace but with longer connecting strands of single cells)
- Both show E-cadherin positivity
- Both show indolent clinical behavior
- Low grade adenosquamous carcinoma:
- Squamous differentiation
- Less uniformity (open and compressed tubules, nests)
- Often ER negative
- Low grade invasive ductal carcinoma of no special type:
- Similar low grade cytologic features to tubular carcinoma, with or without prominent apical cytoplasmic tufting but with more complex architecture
- Tumor shows multilayering, stratification, glandular fusion or branching and may have > 10% ribbons or cords
- ER expression is often high but may be of lower intensity in tubular carcinoma (i.e., third quartile or > 50 - 75%, expression) than in well differentiated invasive ductal carcinoma (i.e., fourth quartile or > 75 - 100%, expression) (Arch Pathol Lab Med 2014;138:1507)
Additional references
Practice question #1
A postmenopausal woman presented with a breast mass measuring 0.8 cm. Biopsy and resection showed the morphology seen in the image above in > 90% of the tumor. What is the expected immunoprofile?
- ER / PR positive, HER2 negative
- ER / PR positive, HER2 positive
- ER / PR negative, HER2 positive
- ER / PR negative, HER2 negative
Practice answer #1
A. ER / PR positive, HER2 negative. The tumor consists of infiltrative small, angulated tubules with a single layer of low grade neoplastic epithelium with prominent apical tufting, features diagnostic of tubular carcinoma. Tubular carcinoma is a luminal A breast carcinoma and thus is ER / PR positive and HER2 negative.
Comment Here
Reference: Tubular carcinoma of breast
Comment Here
Reference: Tubular carcinoma of breast
Practice question #2
A core biopsy of a breast mass shows an invasive carcinoma with tubular features. What are the essential criteria to diagnose this tumor as tubular carcinoma?
- > 90% tubules lined by highly pleomorphic epithelial cells and brisk mitosis
- > 90% tubules lined by low grade epithelial cells with sparse mitosis
- < 90% tubules lined by highly pleomorphic epithelial cells and brisk mitosis
- < 90% tubules lined by low grade epithelial cells with sparse mitosis
Practice answer #2
B. > 90% tubules lined by low grade epithelial cells with sparse mitosis. The diagnosis of tubular carcinoma or any special subtype of invasive breast carcinoma, requires that > 90% of the tumor show the specific diagnostic features of the special subtype. Thus, in the case of tubular carcinoma, > 90% of the tumor must have small, angulated tubules lined by a single layer of low grade malignant epithelium and sparse to absent mitoses. Because the patient underwent core biopsy, which is only a sampling of the tumor, the designation as tubular carcinoma should be reserved until the tumor is fully evaluated on subsequent resection. In such cases, a note or comment can be helpful (please see Sample pathology report for an example).
Comment Here
Reference: Tubular carcinoma of breast
Comment Here
Reference: Tubular carcinoma of breast