Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Perincheri S, Siddon AJ. EBV+ DLBCL. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomadiffuseEBV.html. Accessed May 13th, 2024.
Definition / general
- Epstein-Barr virus (EBV) positive diffuse large B cell lymphoma is a clonal B cell lymphoid proliferation in patients without a history of immunodeficiency or lymphoma
- Other well defined EBV positive lymphoid disorders, such as plasmablastic lymphoma, diffuse large B cell lymphoma associated with chronic inflammation and EBV positive mucocutaneous ulcer, are excluded from this category
Essential features
- EBV positive clonal large B cell lymphoma in patients without prior history of lymphoma or immunodeficiency
- Associated with older age, predominant in males and often advanced stage at presentation
- Large transformed cells with a spectrum of morphologies seen in sheets or admixed in a polymorphous infiltrate
Terminology
- EBV positive diffuse large B cell lymphoma of the elderly
- Senile EBV associated B cell lymphoproliferative disorder
- Age related EBV positive lymphoproliferative disorder
ICD coding
Epidemiology
- Mostly older patients (> 50 years), with peak in the eighth decade; second smaller peak in the third decade (Oncotarget 2015;6:13933)
- M > F
- Higher incidence in Asia and Latin America compared with Europe
Sites
- Nodal and extranodal involvement is common
- Frequent extranodal sites: skin, lung, tonsil, gastrointestinal tract
- Younger patients (< 50 years) more likely to have predominantly nodal disease
- Bone marrow involved in ~10% of patients
- Reference: Clin Cancer Res 2007;13:5124
Pathophysiology
- In elderly patients, pathogenesis is thought to be related to multifactorial causes of immunosenescence impacting both innate and adaptive immune responses
- Alterations of the immune microenvironment may also contribute
- EBV dependent activation of proliferative, cell cycle and antiapoptotic cellular mechanisms via NFkB pathway, PI3K / AKT, MEK-ERK, MAPK pathways, enhancing CDK2 and phosphorylation of Rb protein and activation of BCL2 (Blood 2013;122:328)
Clinical features
- Variable clinical features
- B symptoms and advanced stage disease, especially in the elderly
- Often associated with high or high intermediate International Prognostic Index (IPI) score
- References: Am J Surg Pathol 2003;27:16, Clin Cancer Res 2007;13:5124
Diagnosis
- Tissue biopsy (lymph node / extranodal sites)
- Core beedle biopsy
- Excisional biopsy
Laboratory
- May have EBV DNA in blood or serum; however, this can also be seen in EBV negative diffuse large B cell lymphoma
- Elevated LDH
Prognostic factors
- Prognostic data derived mainly from retrospective studies
- Worse prognosis in older patients (> 45 years)
- In elderly patients > 70 years, B symptoms are associated with worse prognosis
- Monomorphic EBV positive diffuse large B cell lymphoma associated with worse prognosis in younger patients as compared with cases with T histiocyte rich or polymorphic large B cell patterns
- Prognosis varies with region (Asian data is controversial) (Blood 2013;122:328)
- Median survival is 2 years in Asian patients
- Worse prognosis than EBV negative diffuse large B cell lymphoma in Asian patients
- CD30 expression associated with worse prognosis in European countries
- Survival outcome has improved with the addition of rituximab to treatment regimens (Am J Hematol 2018;93:953)
Case reports
- 59 year old man with gastric ulcer (In Vivo 2018;32:413)
- 70 year old woman with lymphadenopathy (Intern Med 2018;57:1287)
- 81 year old woman with lymphadenopathy (Proc (Bayl Univ Med Cent) 2017;30:443)
Treatment
- No prospective comparative studies have been performed to evaluate treatment options
- No standard approach, treatment strategies similar to de novo EBV negative diffuse large B cell lymphoma
- R-CHOP, with overall response rates of 50 - 90% and complete response rates of 30 - 70% (Am J Hematol 2018;93:953)
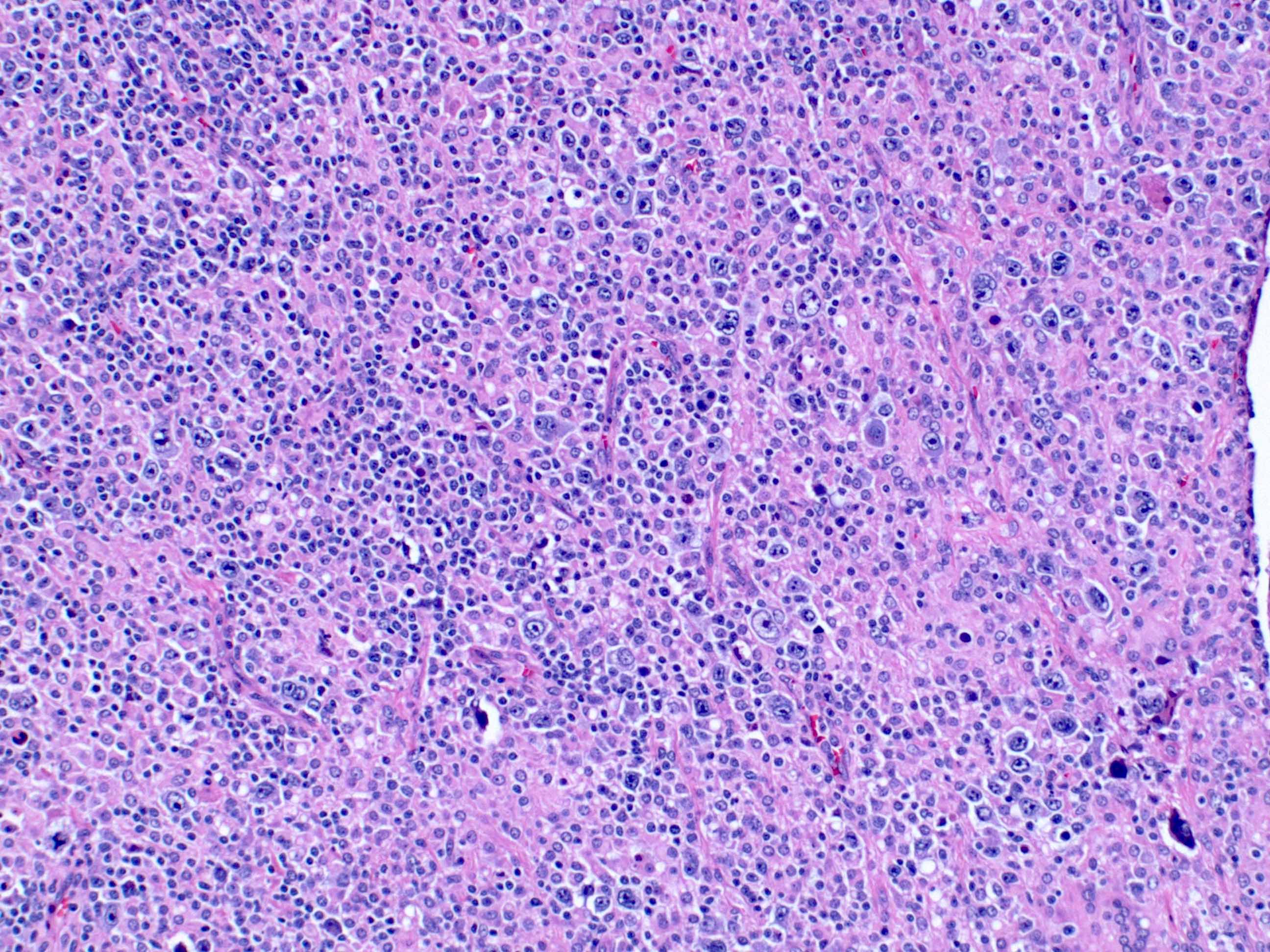
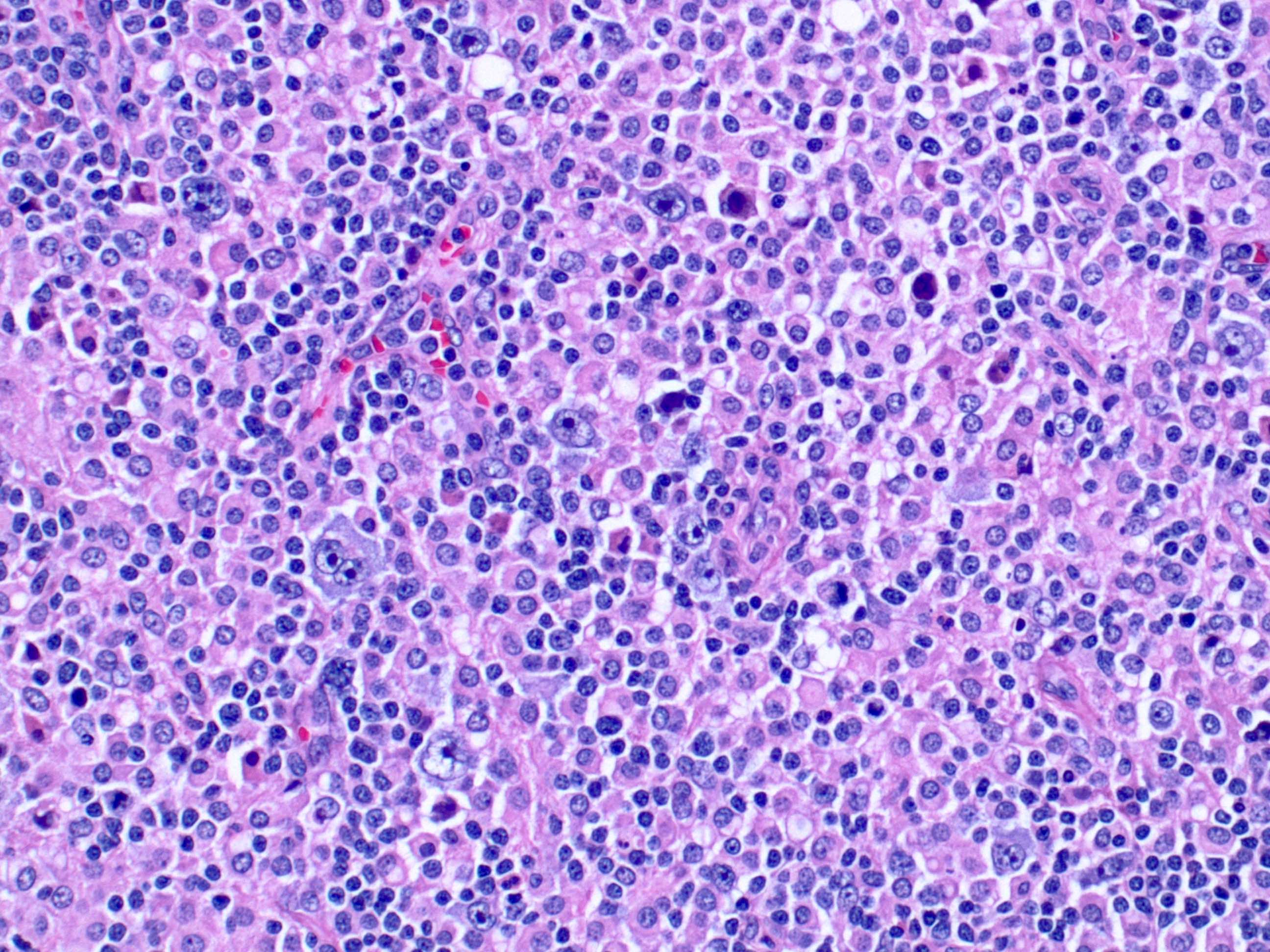
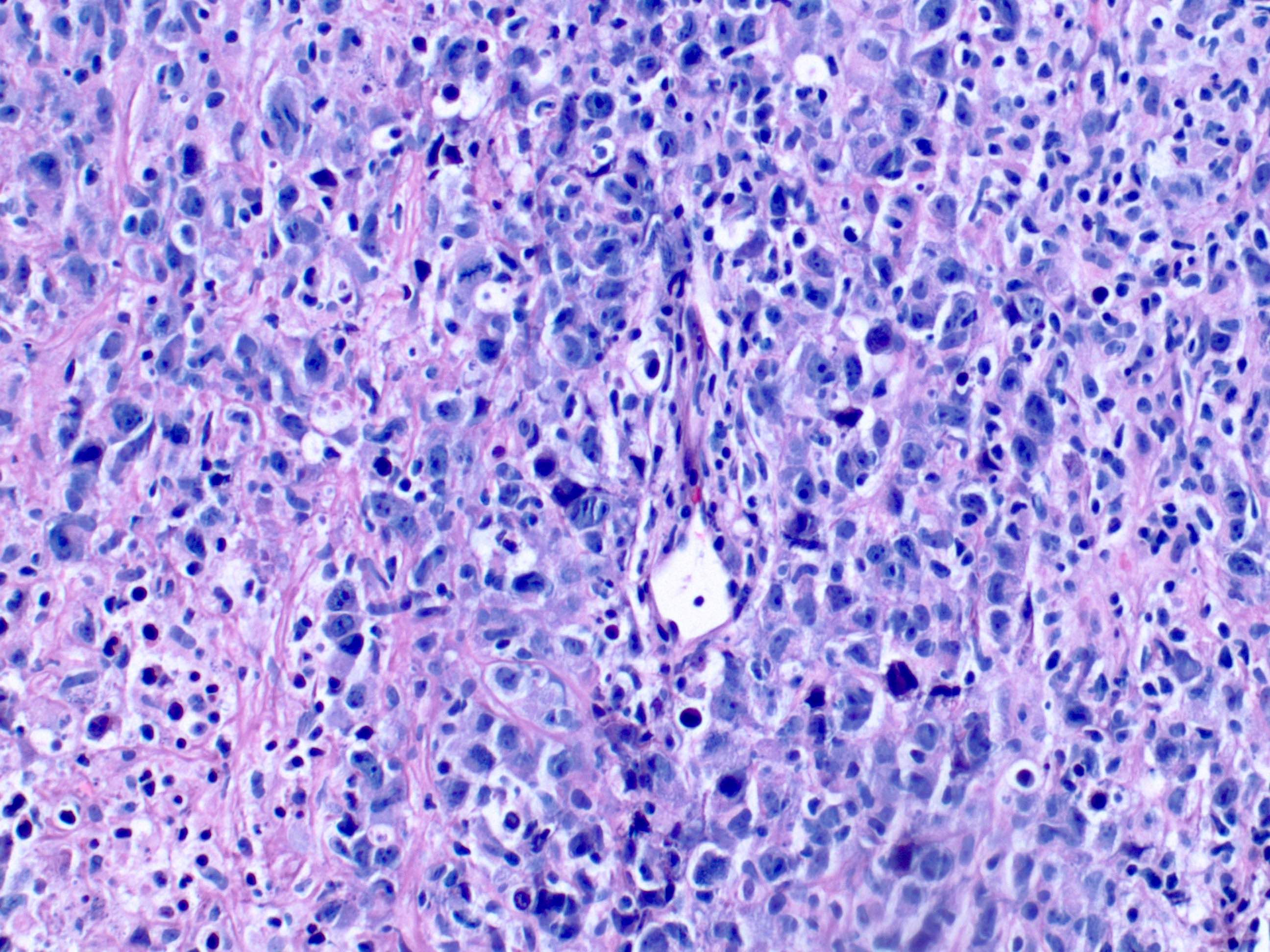
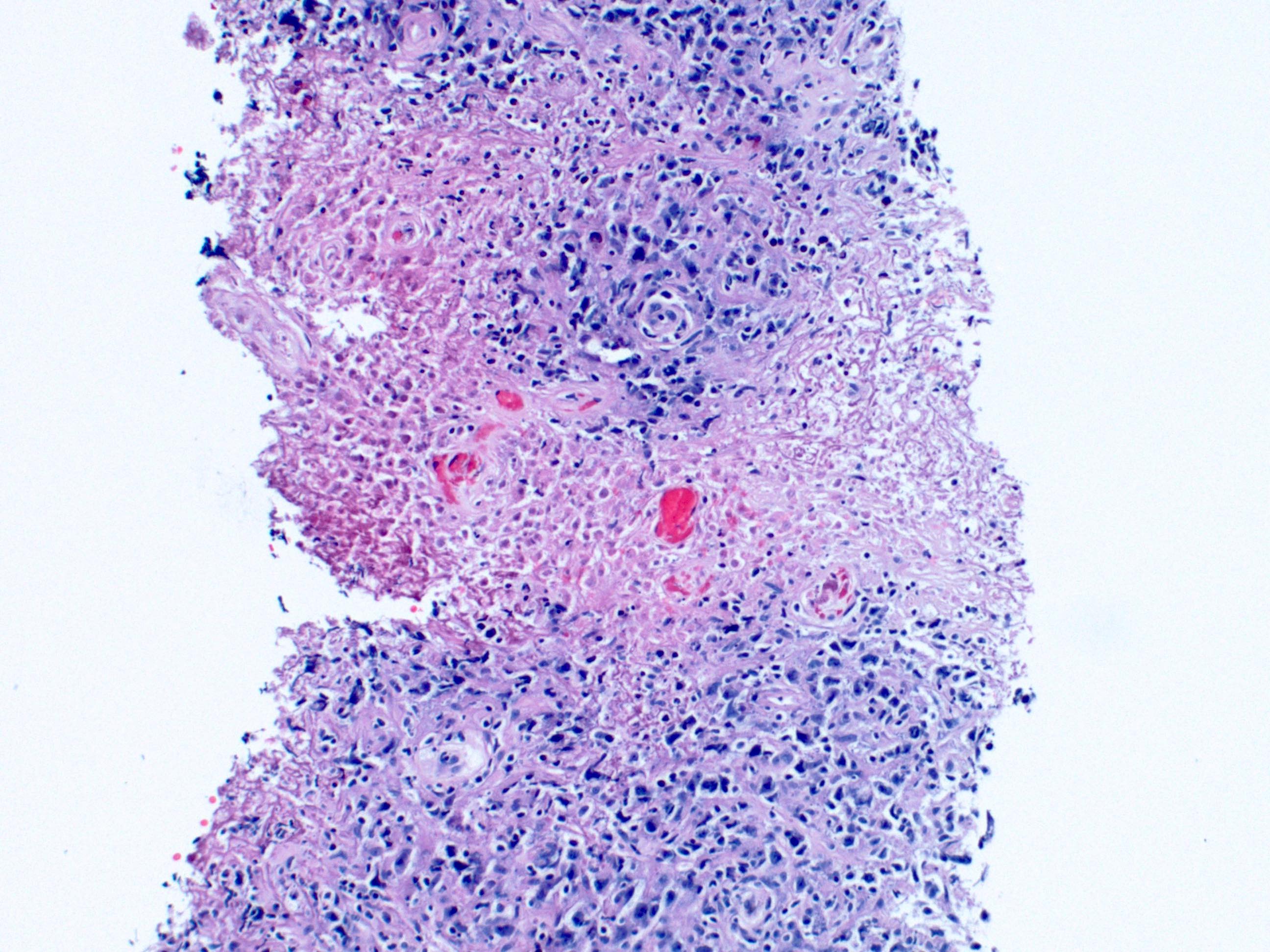
Microscopic (histologic) description
- Architectural effacement of site of involvement
- Geographic necrosis and angioinvasion may be present
- Neoplastic component comprised of large, atypical cells that can have an immunoblast, centroblast or Reed-Sternberg-like morphology
- 2 architectural patterns described (no known prognostic relevance) (Mod Pathol 2012;25:968)
- Monomorphic type: sheets of large cells resembling diffuse large B cell lymphoma
- Polymorphic pattern: variable amount of admixed reactive small lymphocytes, histiocytes and plasma cells (3 different subtypes described below)
- Canonical large B cell-like features: high density of large neoplastic cells and scattered Reed-Sternberg-like cells
- Hodgkin lymphoma-like features: lower density of Reed-Sternberg-like cells
- Posttransplant lymphoproliferative disease (PTLD)-like features: lower density neoplastic cells without Hodgkin-like features, may show plasmacytoid differentiation
- Typically, activated B cell subtype by Hans criterion
- No cutoff of EBV positivity in neoplastic cells; cutoffs ranging from 10 - 20% have been used in studies
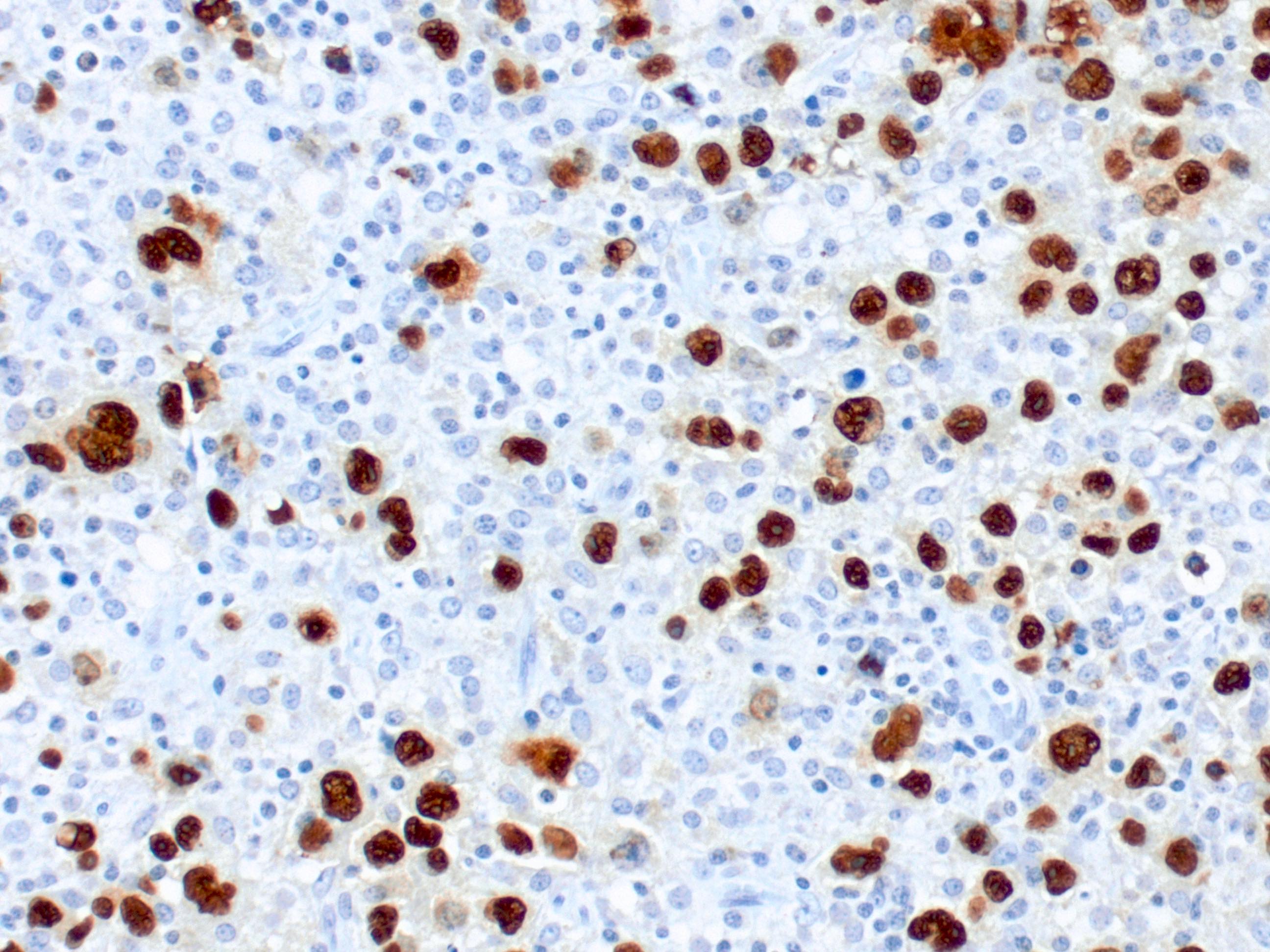
- Type II and less often, type III latency pattern based on EBNA2 and LMP1 staining patterns
Microscopic (histologic) images
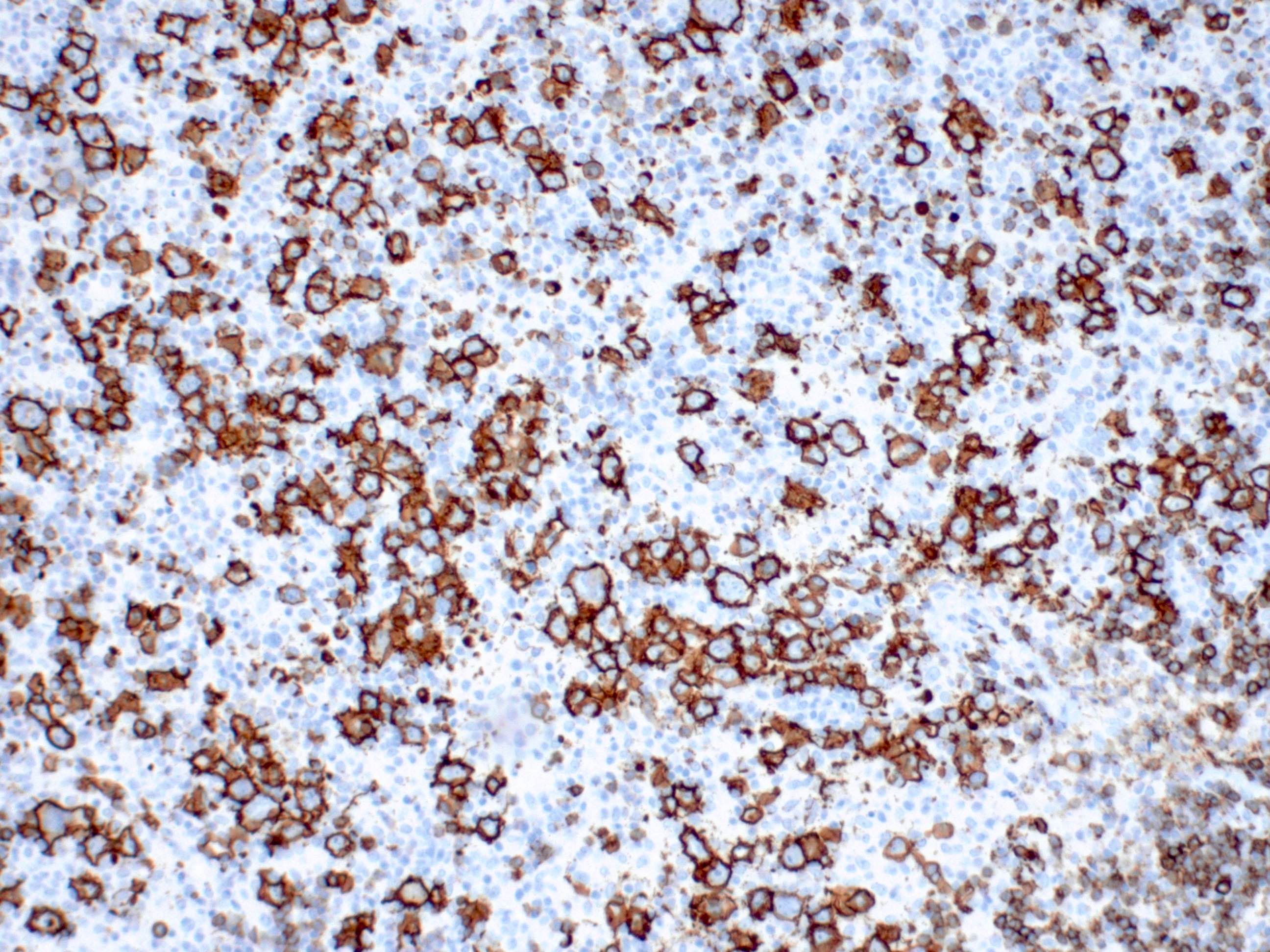
Positive stains
Molecular / cytogenetics description
- Monoclonal IgH rearrangements
Sample pathology report
- Lymph node, cervical lymph node, excision:
- EBV positive, diffuse large B cell lymphoma
- Microscopic description: The lymph node architecture is completely effaced by a variably sized infiltrate, including very large cells with irregular nuclear membranes, vesicular nuclei, distinct nucleoli and moderate amount of cytoplasm. There is a mixed infiltrate composed of small lymphocytes and histiocytes. The background is hyalinized, with areas of necrosis and foreign body giant cells. There are areas with residual small lymphocytes.
- Immunostains: The large neoplastic cells are positive for CD20, PAX5, CD30 and negative for CD15 and CD10. BCL6 stains a subset of the large cells. EBER and LMP1 are positive in the large cells. CD3 and CD5 stain the background small T cells. Ki67 stains the majority of the large cells with an overall staining of approximately 50%.
Differential diagnosis
- Diffuse large B cell lymphoma, NOS:
- Identical to the monomorphic variant but no evidence of EBV infection at the time of initial diagnosis
- EBER-
- Classic Hodgkin lymphoma:
- Plasmablastic lymphoma:
- Immunodeficiency associated lymphoproliferative disorder:
- History of primary or iatrogenic immunodeficiency
- EBV positive mucocutaneous ulcer:
- Sharply circumscribed, isolated ulcers oral mucosa GI tract and cutaneous sites
- Hodgkin / Reed-Sternberg-like or diffuse large B cell lymphoma-like morphology with deepest margin of a band-like infiltrate of mature lymphocytes
- Diffuse large B cell lymphoma associated with chronic inflammation:
- Occurs in the setting of longstanding chronic inflammation
- Commonly involves thoracic cavity
Board review style question #1
A 68 year old man with no prior relevant history presented with generalized lymphadenopathy. Excisional biopsy of a cervical lymph node shows large neoplastic cells with admixed small lymphocytes (see figure above). The large neoplastic cells are positive for CD20 and EBER. Which of the following immunophenotypes is most compatible with EBV positive diffuse large B cell lymphoma?
- Positive for PAX5, CD30, CD15 and CD10
- Positive for PAX5, BCL6, CD10 and CD138
- Positive for PAX5, CD30, BCL6 and MUM1
- Positive for CD79a, CD30, CD15 and negative for CD45
Board review style answer #1
Board review style question #2
Which of the following is true of EBV positive diffuse large B cell lymphoma?
- Only seen in patients > 50 years of age
- CD30 expression is associated with poor prognosis
- Younger patients have predominantly extranodal disease
- Disease usually shows a type I EBV latency pattern
Board review style answer #2