Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Flow cytometry description | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Ghildyal A, Poveda J. Plasmablastic lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaplasmablastic.html. Accessed September 23rd, 2025.
Definition / general
- Aggressive large B cell lymphoma with plasmablast / immunoblast morphologic features with plasma cell differentiation, usually in association with immunodeficiency
Essential features
- Aggressive lymphoma with unfavorable prognosis (Am J Surg Pathol 2004;28:736)
- Distinct entity, according to the 2017 WHO classification
- Predominantly occurs in extranodal sites (most common in oral cavity)
- Commonly occurs in young adults with HIV infection or iatrogenic immunosuppression (Am J Surg Pathol 2004;28:736, Histopathology 2007;51:774)
- Pathogenesis is not well understood
- Requires histologic, immunophenotypic and clinical correlation for definitive diagnosis
- Monomorphic sheets of intermediate to large cells with plasmablastic / immunoblastic features, prominent nucleoli and positivity for plasmacytic markers (Am J Surg Pathol 2004;28:736)
Terminology
- Plasmablastic lymphoma (PBL); subtype of diffuse large B cell lymphoma with sufficient distinctive features that is now considered a distinct entity
ICD coding
- ICD-O: 9735/3 - plasmablastic lymphoma
Epidemiology
- Mostly occurs in adults with HIV infection or with iatrogenic immunosuppression
- In a 10 year study, most patients were men with a median age at presentation of 50 years (Am J Hematol 2019;94:E127)
Sites
- First described in the oral cavity (Blood 1997;89:1413)
- Presents frequently in extranodal sites, especially of the head and neck region
- Other common sites include skin, gastrointestinal tract and bone
- Nodal involvement is generally infrequent but is seen in 30% of posttransplant cases (Blood 2015;125:2323)
Pathophysiology
- Derived from post germinal center B cells (plasmablast)
Etiology
- Not well understood
- Epstein-Barr virus (EBV) positivity is observed in 75% of cases (Am J Surg Pathol 2014;38:875)
- Iatrogenic immunosuppression (e.g., posttransplant) and HIV positive patients
- Few cases are reported in immunocompetent individuals (J Med Case Rep 2011;5:168)
Clinical features
- Mass forming lesion in extranodal sites, typically in the context of HIV infection, iatrogenic immunosuppression and posttransplant setting
- Disease is commonly disseminated and higher stage at the time of presentation (stage 3 - 4) with bone marrow involvement (75% of HIV positive patients and 50% of posttransplant patients) (Blood 2015;125:2323)
- Elevated serum paraproteins may be detected
Diagnosis
- Requires correlation with clinical features to exclude plasmablastic plasma cell myeloma, including the presence of serum monoclonal proteins, SPEP / IFX studies and surveillance for lytic lesions
- Diagnosis can be complicated by overlapping morphologic and phenotypic features with plasmablastic plasma cell myeloma with extramedullary involvement
- MYC translocation is observed in approximately 50% of PBL cases (Am J Surg Pathol 2010;34:1686)
- EBV positivity is present in approximately 75% of cases but may be rarely detected in myeloma (Am J Surg Pathol 2014;38:875)
- Diffuse C-MYC expression by immunohistochemistry and high Ki67 proliferative index (70 - 90%) favors PBL over myeloma (Histopathology 2007;51:774, Blood 1997;89:1413)
Laboratory
- Serology for HIV
- Paraprotein levels may be elevated
- Monoclonal spike should not be present (Mod Pathol 2005;18:806)
Radiology description
- Typically presents as an extranodal mass
- Diffuse bone marrow involvement is seen in 30% of patients
- Findings can range from an inflammatory process to a destructive lesion of bone and soft tissue (Case Rep Ophthalmol Med 2018;2018:4746050)
- Imaging studies have been suggested for staging of the disease (Radiographics 2018;38:2051, Acta Radiol 2011;52:970)
Prognostic factors
- Prognosis is unfavorable
- Median survival is 6 - 12 months (Am J Hematol 2019;94:E127, Am J Surg Pathol 2014;38:875)
- MYC translocation is associated with worse prognosis (Blood 2015;125:2323, Am J Surg Pathol 2014;38:875)
Case reports
- 29 year old HIV positive man with a 2 week history of a gingival mass (J Clin Exp Dent 2020;12:e429)
- 39 year old man with 1 month history of swelling of the oral cavity (Medicine (Baltimore) 2020;99:e22335)
- 55 year old man with plasmablastic lymphoma of the small intestine (World J Gastroenterol 2012;18:6677)
- 59 year old man with painless rectal bleeding (J Med Case Rep 2011;5:168)
- 64 year old man with radionecrosis of the jaw (Int J Surg Case Rep 2016;29:94)
Treatment
- Newer treatment modalities using V-EPOCH (bortezomib with etoposide, prednisone, vincristine, cyclophosphamide and doxorubicin) have shown increased survival (Br J Haematol 2019;184:679)
- Despite newer treatments, prognosis remains unfavorable
Gross description
- No distinct or specific features on gross examination
- Soft tissue mass can be well circumscribed or irregular
- Cut surface is usually gray-tan to yellowish in color, with a fleshy appearance
Frozen section description
- Definitive diagnosis of plasmablastic lymphoma should be avoided at the time of frozen section, as definitive diagnosis requires phenotyping and clinical correlation
- Descriptive diagnosis, such as lymphoma with plasmablastic features or lymphoma with features suggestive of plasmablastic lymphoma, allows for adequate workup and definitive diagnosis
- Findings are similar to those seen on permanent sections; they consist of monomorphic sheets of intermediate to large sized cells with round eccentric nuclei
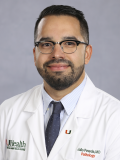
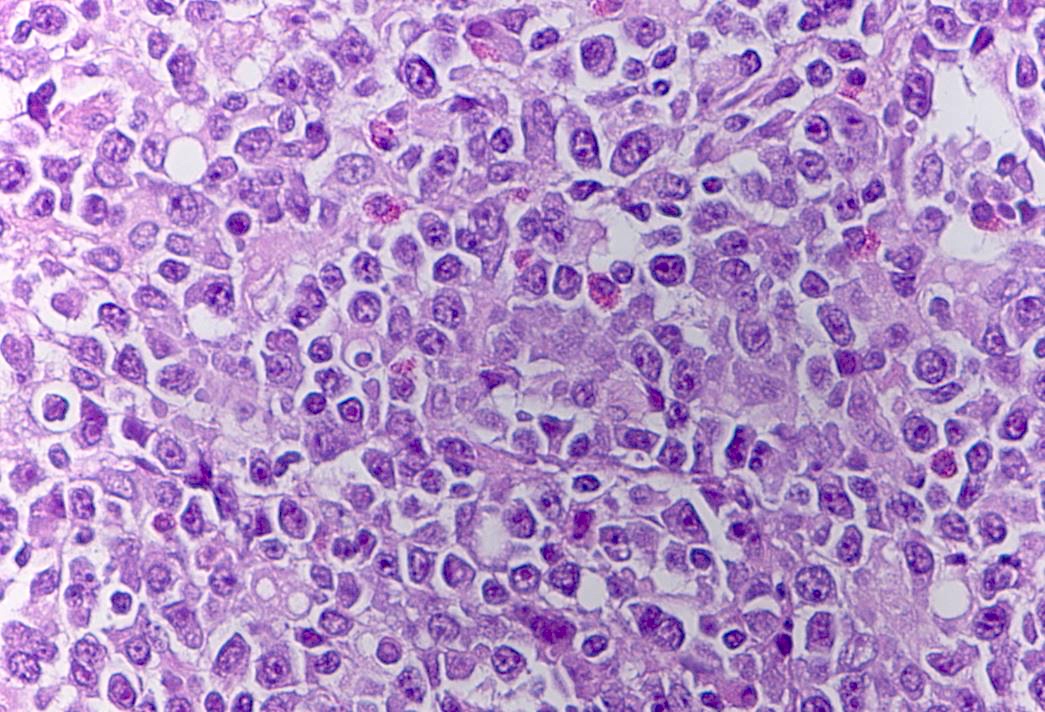
Microscopic (histologic) description
- 2 morphologic variants recognized: monomorphic PBL and PBL with plasmacytic differentiation
- Monomorphic PBL:
- Consist mostly of immunoblastic cells
- PBL with plasmacytic differentiation:
- Cells with plasmacytic differentiation / plasmablasts that are intermediate to large in size with round eccentric nuclei, prominent nucleoli and bluish cytoplasm (Crane: Survival Guide to Lymph Node Pathology, 2021)
- Seen more frequently in the setting of HIV infection
- Oral, nasal and paranasal sinuses are commonly affected
- Anaplastic / plasmablastic plasma cell myeloma is an important differential that needs to be ruled out
- Lytic bone lesions and monoclonal serum immunoglobulins can be seen in both
- Bone marrow is not frequently involved in plasmablastic lymphoma
- History of immune deficiency or EBER positivity by in situ hybridization is useful in establishing a diagnosis of plasmablastic lymphoma
- MYC translocation will favor plasmablastic lymphoma
- Cells with plasmacytic differentiation / plasmablasts that are intermediate to large in size with round eccentric nuclei, prominent nucleoli and bluish cytoplasm (Crane: Survival Guide to Lymph Node Pathology, 2021)
- Monomorphic PBL:
- Mitotic figures are increased
- Apoptotic cells and tingible body macrophages may be identified
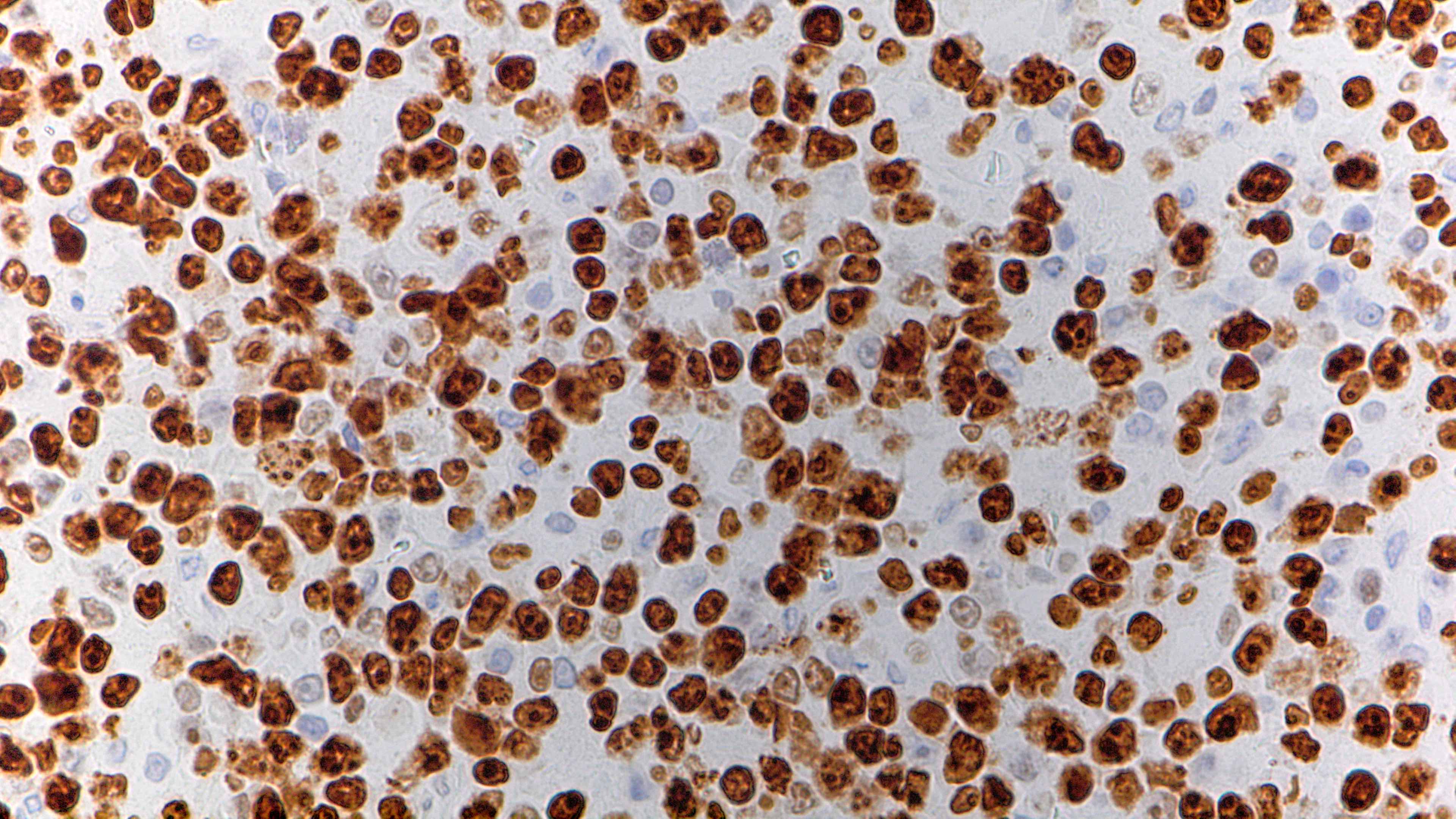
Microscopic (histologic) images
Cytology description
- Sheets of monomorphic cells of intermediate to large sized lymphoid cells with plasmacytic differentiation and immunoblastic or plasmablastic morphology
- Large cells with abundant basophilic cytoplasm; large nucleus with prominent nucleolus
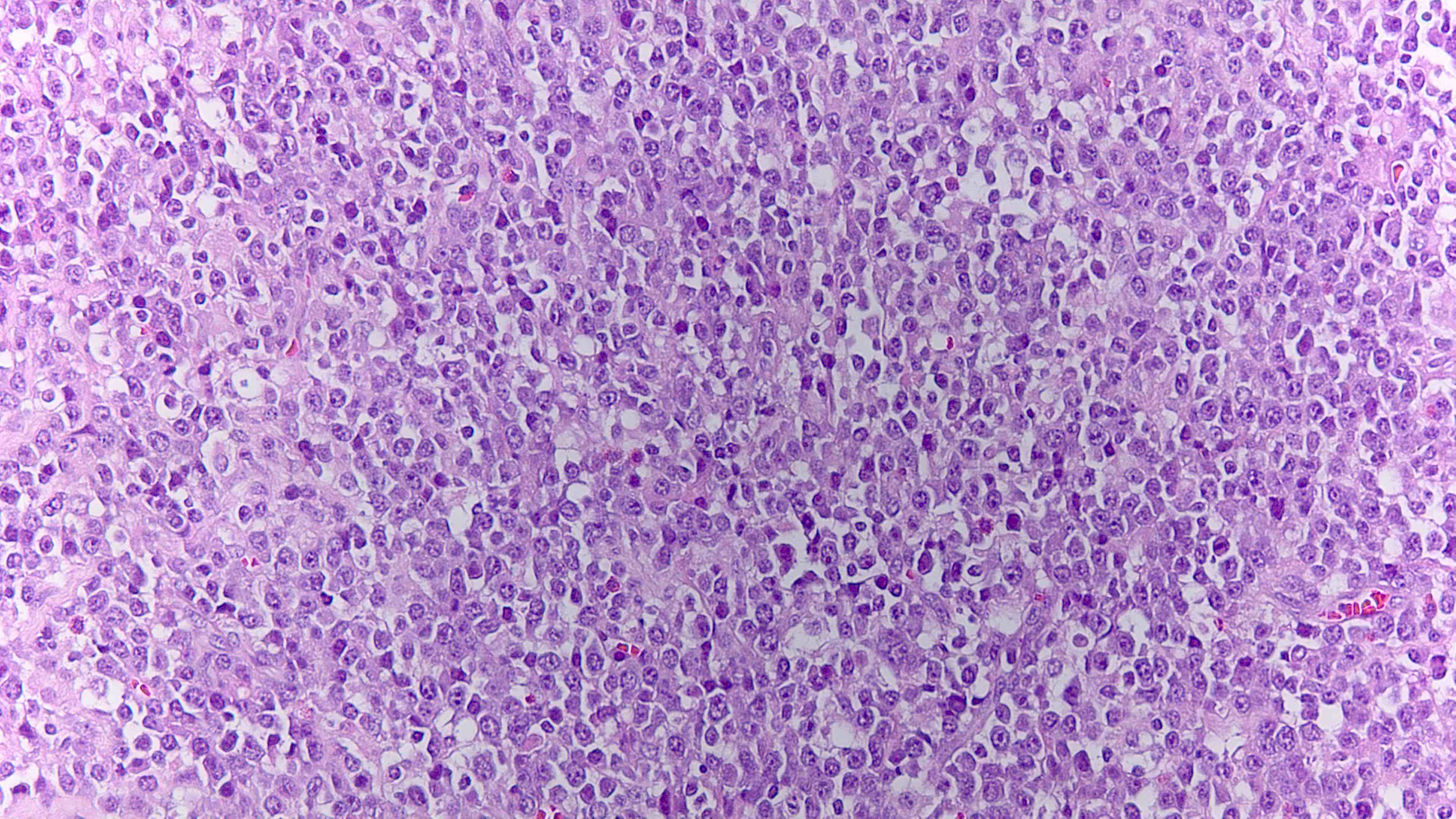
Positive stains
- CD138, CD38, MUM1, CD79a (40%) (Blood 2015;125:2323, Haematologica 2010;95:1342)
- CD30 and EMA are frequently expressed
- CD56 is detected in 25% of cases
- IRF4 / MUM1, XBP1 and PRDM1 are positive
- Ki67 proliferation index is high (> 90%)
- Cytoplasmic light chains are usually expressed
- EBER by in situ hybridization present in approximately 70% of cases (Am J Surg Pathol 2014;38:875)
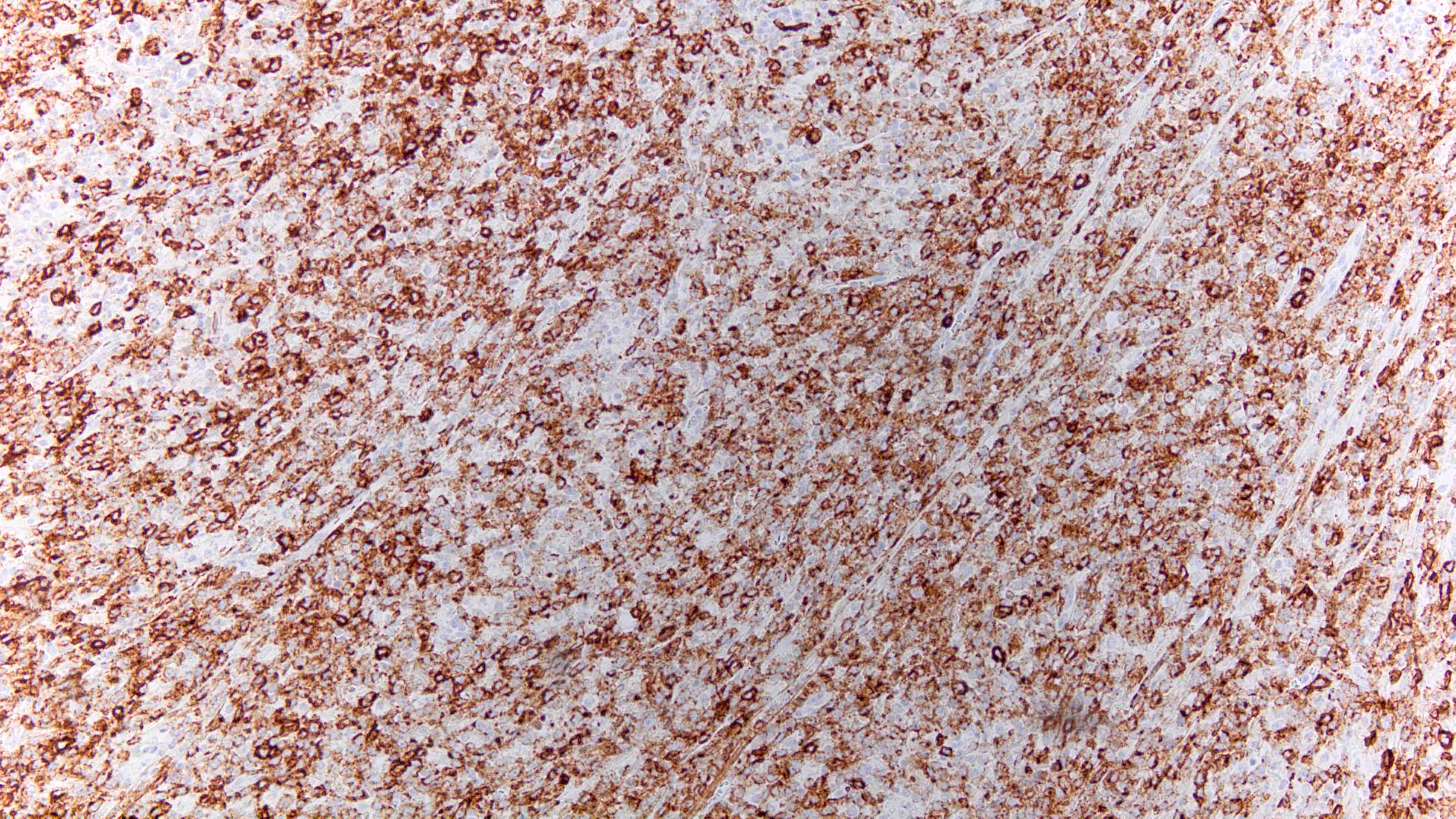
Negative stains
- CD20, CD45 and PAX5 (typically negative but may show weak expression in a subset of cells)
- HHV8
- T cell antigens are usually negative but may show aberrant expression (Mod Pathol 2018;31:718)
Flow cytometry description
Electron microscopy description
- Electron microscopy is not routinely undertaken for diagnosis
- Case studies that have incorporated electron microscopy have shown (Exp Mol Pathol 2011;90:85)
- Euchromatic nuclei with 1 or more nucleoli
- Numerous ribosomes
- Scant strands of rough endoplasmic reticulum
Molecular / cytogenetics description
- Genetic alterations in MYC gene are found in approximately 50% of cases (Mod Pathol 2017;30:85)
- MYC translocation, gain and overexpression at mRNA level
- Seen more often in EBV positive tumors
- PRDM1α gene mutations (missense mutations) are associated with PRDM1 / Blimp1 expression (Mod Pathol 2017;30:85)
- Clonal rearrangements in immunoglobulin genes
- Clonal IGH rearrangement is present
- More recent studies that used whole genome sequencing (WES) have found multiple mutations (Nat Commun 2021;12:5183)
- NRAS: 31% of cases, mostly missense mutations
- NOTCH signaling pathway: 26%
- STAT3: 25% of cases, clustered in the SH2 domain
- 47% of HIV positive patients
- 10% of HIV negative patients
Sample pathology report
- Anterior hard palate, biopsy:
- Plasmablastic lymphoma (see comment)
- Comment: Histologic sections consist of squamous lined mucosa diffusely involved by lymphoma. The lymphoma is seen in sheets and composed of large atypical plasmablasts. Apoptotic figures and brisk mitotic activity are seen.
- Immunohistochemical studies show that lymphoma cells are positive for MUM1, CD138 (variable), CD38 (variable), CD30 (variable) and C-MYC (~10%), while negative for CD20, PAX5, CD3 and HHV8. Lymphoma cells are lambda light chain restricted as detected by in situ hybridization (ISH). Kappa light chains are decreased (by ISH). Kappa light chains are markedly decreased (by ISH). EBER (by ISH) is diffusely positive. Ki67 proliferation index is approximately 100%.
Differential diagnosis
- Diffuse large B cell lymphoma with plasmablastic features:
- Plasmablastic / anaplastic plasma cell myeloma:
- More common in older individuals
- Serum paraproteins are elevated with monoclonal gammopathy
- Myeloma defining signs (CRAB: calcium elevation, renal insufficiency, anemia and bone abnormalities) usually present
- Bone marrow involvement common
- EBV infection and MYC translocation are less common
- Primary effusion lymphoma (PEL):
- Typically presents in cavitary spaces but may be mass forming (solid PEL)
- HHV8 (LANA) immunostaining will be positive
- Commonly coinfected with EBV
- ALK positive large B cell lymphoma:
- Typically lacks association with immunosuppression
- By definition, should be ALK positive by immunohistochemistry
Additional references
Practice question #1
Practice answer #1
B. Plasmablastic lymphoma. The patient is a 54 year old man with history of HIV who underwent biopsy of a hard palate mass. The lymphoma is present as sheets of large atypical cells with prominent nucleoli. Immunohistochemical studies showed that lymphoma cells were positive for MUM1, CD138, CD38, CD30 and C-MYC (~10%) and negative for CD20 (therefore, choices A and E are eliminated), PAX5, CD3 (choices C and D are eliminated), ALK (ALK positive large B cell lymphoma would be ruled out) and HHV8 (primary effusion lymphoma is ruled out). Lymphoma cells are lambda light chain restricted as detected by in situ hybridization (ISH). Kappa light chains are decreased (by ISH). EBER (by ISH) is diffusely positive. The history, site, morphologic appearance and immunohistochemical findings support a diagnosis of plasmablastic lymphoma.
Comment Here
Reference: Plasmablastic lymphoma
Comment Here
Reference: Plasmablastic lymphoma
Practice question #2
Which of the following stains is usually positive in plasmablastic lymphoma?
- ALK
- CD3
- CD20
- EBER
- HHV8
Practice answer #2
D. EBER by in situ hybridization can be seen in other entities such as large B cell lymphoma and primary effusion lymphoma; however, the other stains are negative in plasmablastic lymphoma.
Comment Here
Reference: Plasmablastic lymphoma
Comment Here
Reference: Plasmablastic lymphoma
Practice question #3
Which of the following gene rearrangements can be seen in plasmablastic lymphoma?
- BCL2
- BCL6
- IGH
- MALT1
- MYC
Practice answer #3
E. MYC translocation is seen in approximately 50% of cases.
Comment Here
Reference: Plasmablastic lymphoma
Comment Here
Reference: Plasmablastic lymphoma